
















































26 Your obligations under the Official Languages Act
28 Dementia supports in the community
Welcome to the summer edition of Health Matters.




1 Community First Responders save life of teen at football match
2 Talking Point: HSE shows its Pride
4 In Focus: Injury units
6 Interview: my breast cancer journey
8 A Day in the Life: Carla McArdle, Clinical Specialist Podiatrist
9 In Focus: be SunSmart this summer
10 Spotlight on: new breastfeeding support guidance
12 What is: community rehabilitation residence
14 Digital Health Strategy - new roadmap launched
17 In Focus: Organ donation
20 Interview with HSE Dublin and Midlands REO Kate Killeen White
22 HSE Dublin and Midlands health region news and updates
20 Health regions overview and latest news
29 In Focus: 20 years of the smoking ban in Ireland 30 Interview with HSE South West REO Dr Andy Phillips 32 HSE South West health region news and updates 36 Innovation in the health services - examples of great work in action 38 Interview with HSE Mid West REO Sandra Broderick 38 HSE Mid West health region news and updates
Bowel
in
You might notice a slight change to the look and feel of the magazine as the organisation begins the transition to the HSE Health Regions. In each edition we are going to highlight the great work being done in each of the six health regions, the integrated care initiatives and innovations staff are carrying out.
In this edition, we talk to the six Regional Executive Officers to learn a little bit more about them, their priorities in both the short and long-term, as well as finding out what their approach to the large structural change will be.
The overarching theme from the REOs was one of positivity over the many benefits the health regions structure will bring to both staff and service users through the right integrated care at the right time, in the right place.
HSE staff were celebrating Pride Month in June along with the rest of the country. We highlight the work of the Reach Out Network, the HSE’s national staff network for Lesbian, Gay, Bisexual, Transgender, Queer, Intersex or Asexual (LGBTQIA+) staff and allies.
We also chat to a few members of the Reach Out Network to find out what Pride means to them.
We take another look at the Official Languages Act and what it means to our obligations as HSE staff. You may not be aware that your out of office response has to be in Irish or Irish and English, no longer in English only. With that in mind, we have drafted a number of responses to help you make the change.
Have a great summer.
Joanne Weston Editorand Wellbeing
Thanks to everyone who has submitted stories for this edition. If you would like to see your initiative or work featured, you can submit through our online form at https://www2.hse.ie/services/forms/health-matters-story-submission.html
Creative Director:Jane Matthews
Published by Ashville Media, Unit 55 Park West Road, Park West Industrial Estate, Dublin 12, D12 X9F9. Tel: (01) 432 2200 ISSN: 0332-4400
All rights reserved. Every care has been taken to ensure that the information contained in this magazine is accurate. The publishers cannot, however, accept responsibility for errors or omissions. Reproduction by any means in whole or in part without the permission of the publisher is prohibited. © Ashville Media Group 2023.
Members of the emergency services, volunteer responders and sports coaches from Newcastle West FC with Ewan John Sabu and his family.

The importance of having members of the public trained in CPR and the use of an AED (automated external defibrillator) has been highlighted following the rescue of a 13-year-old Limerick boy who suffered a cardiac arrest while playing football.
Ewan John Sabu from Newcastle West was playing football with his local team Newcastle West Football Club when he collapsed. His coaches immediately contacted the emergency services, started CPR and a massive multi-agency response was launched.
Ger O’Dea, Community Engagement Manager with the National Ambulance Service (NAS), said, “Community First Responders are integral to community resilience and NAS is committed to working within these communities to provide the quickest possible response to patient emergencies in order to achieve outcomes like this.”
When Ewan collapsed the emergency services were called. Volunteers from CRITICAL West Limerick Community First Responders (CFR) group were joined
by the NAS personnel, gardaí, the Limerick City and County Fire and Rescue Service, Templeglantine CFR group and an off-duty Red Cross EMT. A paediatric team returning to University Hospital Kerry from Crumlin Children’s Hospital also responded.
The emergency teams were able to restart Ewan’s heart and he was brought to University Hospital Limerick where he was stabilised before being transferred to Crumlin.
The family held a small event near their home in Newcastle West to show their appreciation to all those who helped Ewan. His mother Sandhya Parameswaran, who is a nurse at Dromcollogher and District Respite Care Centre, said, “The care Ewan received at the scene and in both hospitals was incredible. He was looked after so well by his coaches Niall, Mícheál and the parents who were there, by all the emergency services and medical teams, they are all heroes. It is thanks to them that Ewan is now back at Scoil Mhuire agus Íde where he is a first year student.”
If you are interested in joining a Community First Responder Group, contact www.becomeacfr.ie for more information.







The Reach Out Network, the HSE's national staff network for Lesbian, Gay, Bisexual, Transgender, Queer, Intersex or Asexual (LGBTQIA+) staff and allies, recently kicked off its 2024 Pride celebrations with energy and excitement.








Throughout the summer months, Reach Out Network members, HSE staff and allies will participate in Pride parades across the country from Brod na Gaeltachta in Donegal, to Galway, Roscommon and Cork, and many more in between.
The Network, which has been in existence since 2017, has members from all parts of the HSE. The Network acts as a representative voice for LGBTQIA+ employees, a forum where staff can discuss experiences and share insights in a safe space, and a resource on LGBTQIA+ topics. The Network has brought many benefits to HSE staff.
“To me, the Reach Out Network has always been about authentic support for being your true self in the workplace. It’s about welcoming sexual and gender identities in their wonderful diversity. It’s about belonging to a workforce that is courageous because we dare to include each member of staff in their unique wholeness” said Ray Leonard (They/Them), Senior Counsellor/Therapist, HSE National Counselling Service and Chair of the Reach Out Network.

The Pride flag serves as a symbol of the LGBTQIA+ community. The widespread use of the Pride flag allows LGBTQIA+ individuals to connect with each other and feel included regardless of their location.
Each year, the Pride flag is displayed at Dr Steevens’ Hospital and other HSE facilities during the month of June. Different versions of the Pride flag exist, with the colours and shapes on the flag representing specific groups of individuals. Given the evolving nature of the LGBTQIA+ community and society at large, the Progress Pride Flag integrates many of these flags into one.
If you are interested in joining the Reach Out Network, participating in a local Pride parade or running a Pride event in your workplace, contact diversity.HR@hse.ie for information and support. Further information on resources on Pride are available from the HSE Diversity, Equality and Inclusion webpage.
Denise Croke (She/Her)
Health Promotion and Improvement Officer (Stakeholder Engagement and Communications)
“Pride is a way of remembering those who have gone before us, paving the way for the scale of celebrations that are such an integral part of our life and culture now. As a younger person, seeing pride parades, and gathering the courage to join them, gave me my first real sense of community and belonging.”
Michael Craughwell (He/Him)
Senior House Officer in Histopathology, Cork University Hospital
“For me personally as a gay man, Pride is the antidote to the shame that, unfortunately, is a feature of the lives of many LGBTQIA+ people and must be overcome to thrive and lead a healthy and fulfilling life. From a professional viewpoint, it can therefore be the vehicle for promoting equity and inclusion in the health service.”
Ronán Brady (He/Him)
Senior Speech and Language Therapist
“Pride means so much. It means a time to celebrate with friends and family, to celebrate yourself and others who had to hide for so long, and to celebrate how far we have come in our little country. But Pride is also a time to stand up for our rights and remind those who want to oppress and put us down, that we are here, we are queer and we are not going anywhere!!”
Aoife Parkes (She/Her)
Speech and Language Therapist
“To me pride means living your life authentically and shamelessly. Not letting other people’s expectations
and limitations dictate your life, but shedding that and choosing freedom for yourself; proudly living the life you want. Pride means lifting each other up and supporting each other, recognising that there’s so much more we can achieve when we come together with love and acceptance than with hatred and shame. I believe pride is a choice we make, and a gift we give to ourselves and to others. Pride is for everyone.”
Cliff Carroll (He/Him)
NiSRP Helpdesk Supervisor
‘’Pride is a celebration of community, diversity, culture and love. Pride is also about recognising my own privilege, and using that privilege to empower others who may not have the same opportunities as I do. It is a time for reflection on the progress we have made and the work that still needs to be done.’’
Maria Hanrahan (She/Her)
Health Liaison Officer, Ukrainian Response
“For me, Pride is about freedom and inclusion. Freedom to be your true self without fear and without shame. It acknowledges the uniqueness of every person regardless of gender, orientation or appearance.”
Alistair Martin (He/Him)
Dental Nurse
“Last year I walked in my first ever Pride March, I was so nervous and what gave me a great boost and help with my confidence was seeing the kids/younger people who had come up from the country to be themselves. I would have never dared at that age but they loved seeing the various people in the Pride march and I could see it gave them confidence to be themselves.”
Orla Shiel (She/Her)
GUH Pride 24 Committee Member and Senior Occupational Therapist Emergency Department
“It is wonderful to celebrate Pride Month in June in Galway University Hospital with our patients and colleagues. During the month we will

raise awareness of LGBTQIA+ issues in healthcare and provide educational opportunities to staff on challenges that are specific to LGBTQIA+ patients. We want patients to feel comfortable coming here and to know this is a place they are welcomed”
Emma Homan (She/Her)
Communications Officer, National Screening Service
“Pride is like glitter – it sticks to everything and makes the world shine a lot brighter. It is about equality and embracing our authentic selves regardless of who we love or how we identify. It isn’t just about celebrating how far we’ve come but it’s also about recognising how far we still have to go.”
Dr Cal Mc Donagh (He/Him)
Senior Clinical Psychologist
“When I went to my first Pride - many years ago - I felt really worried that I would be judged. When I go to Pride nowadays it just feels amazing to be surrounded by people who accept me as me - and who I accept for who they are too! Getting involved might take some bravery but it is a powerful way to show that we care about each other and will be there for each other.”
Fran Glynn (She/Her)
Senior Radiographer, Galway University Hospital
“Pride to me means a myriad of positivity - acceptance, no judgement, unconditional love, self worth, unity and equality.”
When to visit an injury unit
Injury units treat recent injuries that are:
• not life-threatening
• unlikely to need admission to hospital
Useful information
• They can help with many of the injuries people go to the emergency department (ED) for. For example, broken bones, dislocations, and minor burns
• You can get treatment such as x-rays, plaster casts, and wound care in an injury unit
• If they cannot help with a particular problem, they will direct you to where you can get the right help.
• You do not need an appointment
• You may be referred to an injury unit by your GP or sent to one from an ED. If you have a referral, you do not have to pay a fee
Call 112 or 999 for an ambulance if: you need urgent medical attention or a life is at risk
When you arrive at an injury unit, you will be:
• registered and assessed by the nursing team
• treated by a doctor or advanced nurse practitioner (a specially trained nurse) depending on the care you need
• given details of any follow-up appointments you may need in the injury unit
• referred on to other services if needed
• If you are in an injury unit and need to go to an ED, you will be referred directly from the injury unit.
• Most injury units treat patients over 5 years of age. Some injury units have higher age limits.
• Injury units may not treat any child younger than 5 years
What injury units can treat Injury units can treat:
• broken bones, sprains and strains, from knees to toes
• broken bones, sprains and strains, from collarbone to fingertips
• minor facial injuries (including oral, dental and nasal injuries)
• minor scalds and burns
• wounds, bites, cuts, grazes and scalp lacerations (cuts)
• small abscesses and boils
• splinters and fish hooks
• objects stuck in eyes, ears or nose
• minor head injuries (fullyconscious patients, who did not have loss of consciousness or vomit after the head injury)
How much does it cost?
It costs €75 to attend an injury unit. If you are referred from an injury unit to an ED, you do not have to pay another fee.There is no charge for patients with a:
• Medical card
• Medical or GP referral letter
Find your nearest injury unit
• Bantry Local Injury Unit (five and older)
• Cashel Injury Unit (three and over)
• Dundalk Injury Unit (five and over)
• Ennis Injury Unit (aged five and over)
• Mallow Injury Unit (aged five and over)
• Mater Smithfield Rapid Injury Clinic (16 and over)
• Monaghan Injury Unit (five and over)
• Mullingar Minor Injuries Unit (16 and over)
• Naas Hospital Injury Unit (16 and over)
• Nenagh Injury Unit (five and over)
• Roscommon Injury Unit (five and over)
• St Columcille’s Injury Unit Loughlinstown (14 and over)
• St John’s Injury Unit Limerick (aged five and over)
• The Mercy Injury Unit (10 and over)

‘You have nothing to lose and everything to gain’
Aileen shares her personal breast cancer journey



Aileen Murphy (centre) pictured in the Ireland AM studios for her interview with presenters Muireann O'Connell and Tommy Bowe. Muireann is holding a framed picture of Aileen's father Tommy, whose Month's Mind was marked the day after the interview.
Aileen Murphy, a Staff Officer with HSE Mid-West Community Healthcare, took her advocacy for early cancer screening to a national platform this spring, when she appeared on Ireland AM for an inspiring and moving live interview with Tommy Bowe and Muireann O'Connell about her personal cancer journey over the past five years.
The interview coincided with a number of personal milestones for Aileen, both sad and optimistic.

“My father’s Month’s Mind was the next day, so the timing was quite difficult, but Tommy and Muireann couldn’t have been nicer, and sensitively took account of the closeness of dad’s death. On the other hand, since the interview, I have received the great news that I am out of remission,” she recalled.



“And the best news was to have been contacted by someone who saw the interview, to let me know they had got screened, and the cancer had been caught early enough for them to perhaps require not so much intervention. At the end of the day, that’s why I do this, and I know that Dad, who was a volunteer in the Daffodil Centre in UHL, would have been thrilled with that.”
Aileen’s message, which she uses her personal story to emphasise, is a simple one. “If you ever have any doubts about going for your breast screening appointment, or any health checks at all, please, just go and get checked. You have nothing to lose and everything to gain by getting checked, and doing so as early as possible.”
For Aileen, the sharpest irony was that her cancer was detected in August 2019 while she was working at BreastCheck in Cork. “It was just a few days before I was due to go on a week’s holiday when I found a lump. I knew it was a different type of lump, but I decided to take my holiday, and get it checked when I returned.”
She was soon scheduled for an ultrasound, and recalls her worry when the radiologist went quiet and told her that she didn’t like the look of what she was seeing on the scan. “When you hear that of course, it’s quite a concern, but of course, you are rationalising it and speculating if it might be something else.”
have a good week, and when I detected that pattern, I would always make nice plans, wear make-up and put on a new outfit. At the same time, it was very difficult on my mother and father.
“And one of the most difficult decisions I had to make was when I was asked whether I would freeze my eggs. That was very hard. I’d always wanted children, but that didn’t work out for me, and I had to consider that I was 45 and single, and so when presented with that question, I decided not to freeze my eggs. It was a pragmatic decision, but profoundly difficult and I can’t pretend that it has not been a huge loss.”
Throughout treatment, she explained that it has been the essential decency and support of people who have helped her get through. “You really find out who your friends are, and kindness manifests itself in some of the most unexpected ways, and from people of all ages, whether from family or neighbours or others you meet.”


A subsequent assessment at CUH revealed that she had Grade 3, Stage 3 Invasive Ductal Carcinoma. Within a month she had surgery, a wide local excision and total auxiliary clearance, and in October began 16 sessions of chemotherapy, followed by 23 sessions of radiotherapy. Ahead of therapy, she had left Cork and returned to live with her parents in Limerick. It’s a bitter-sweet period of her life which up-ended her, personally and socially. “It was a whirlwind period. Treatment was incredibly aggressive, and some of the treatment could be quite difficult. My hair was falling out within two weeks, and I was very sick… but then, I would
A year after starting treatment, she agreed to participate in a Clinical Trial at University Hospital Limerick and regards this decision as another way of creating a positive out of the illness. “The Cancer Clinical Trials team at UHL, and Dr Greg Korpanty, have been absolutely wonderful, so positive and empathetic. The drug I am being trialled on is one which will not just decrease the chances of the cancer coming back, but also one that will be a possible alternative to chemotherapy. I am privileged to be playing a part in something that might help other people, as well as helping me to adjust to my new life.
“I can’t say I am the same person I was prior to cancer, but I do feel a lightness in myself that comes from greater confidence, and also the advocacy work that I do. This is not only a way of giving back to everyone who has helped me, whether in BreastCheck, CUH, UHL, the Irish Cancer Society, the Daffodil Centre in UHL, and elsewhere. But I also want to help others who may be hesitating about getting checked. I have encouraged people, not just women, guys as well, to get checked, and I will do that for the rest of my life,” Aileen concluded.






Clinical Specialist Podiatrist in Diabetes, Community Healthcare Organisation DNCC, Dublin North Integrated Care Programme Chronic Disease (ICPCD), St Clare’s, Glasnevin
Carla McArdle, a Clinical Specialist Podiatrist within HSE since January 2023 and with considerable experience both professional and academic, “enjoys working with patients, helping them and making a difference for them.”
Carla explained her key role in a larger team of specialists. “I’m a Diabetes Clinical Specialist Podiatrist working within the larger multi-disciplinary team to assess, diagnose, and provide treatment to improve outcomes for patients with diabetes. The team I work with are fantastic, they are respectful, hardworking, progressive and supportive of each other.”
This role of Clinical Specialist Podiatrist appealed, as Carla said, “I felt I could apply my knowledge and experience to help improve patient outcomes and continue doing research in the area of diabetes.”
Carla is very clear on the importance of her work on the

quality of life of the people she works with, “I have an opportunity as a podiatrist to make an impact on our patients’ lives, to work with them, to empower them to look after their feet and understand the importance of diabetes and good foot health.
“Feet are often misrepresented as something that are deemed as a less important part of the body, and often people don’t realise the significance of having good foot health. Diabetic foot disease is one of the leading causes of lower limb amputations and we as podiatrists have the opportunity to change perspectives on foot health and therefore make a real difference in preventing these devastating consequences, improve life expectancy and maintain quality of life.”
It’s a varied role. “No two days are the same, on a clinical day I will see all types of patients with diabetes, typically who have had diabetic foot ulcers or previous
amputation/s and are at high risk of developing another foot ulcer. With each patient I will assess, diagnose and treat their footcare needs and devise their management plan. For some of the patients I see, I will have to seek immediate involvement from other members of the MDT for example from hospital Clinical Specialist Podiatrists, Public Health Nurses, and their GP.”
Carla’s favourite things about her role are “the people I work with, I look forward to coming to work and chatting with them (sometimes with a coffee) and also learning from them and their individual expertise.”
And Carla certainly has a busy and exciting life, with many interests.
“I love the outdoors – running, cycling and swimming. Any of these are my ‘go to’ to manage stress and maintain a healthy lifestyle. I also have two young daughters who keeps me active,” she said.

As part of the annual SunSmart campaign, the HSE’s National Cancer Control Programme, in collaboration with Healthy Ireland and cross-sectoral partners, are working together to support people to reduce their risk of skin cancer by protecting their skin from the sun. This is the fifth year the SunSmart campaign has been running and it has grown year on year. The campaign aims to reduce your risk of skin cancer by increasing awareness and engagement with the steps you, your family, friends and colleagues can take to protect your skin from the sun. We sometimes think Irish sun isn’t real sun, but skin cancer is our most common type of cancer in Ireland, accounting for over 11,000 cases annually. The
FOLLOW THE HEALTHY IRELAND SUNSMART 5 SS:
• Slip on clothing that covers your skin, such as long sleeves, collared t-shirts
• Slop on sunscreen on exposed areas, using factor 30+ for adults and 50+ for children. No sunscreen can provide 100% protection, it should be used alongside other protective measures such as clothing and shade
• Slap on a wide-brimmed hat
• Seek shade - especially if outdoors between 11am and 3pm - and always use a sunshade on a child’s buggy
• Slide on sunglasses to protect your eyes
number of people being diagnosed with skin cancer in Ireland is rising rapidly. Yet, in most cases, it is preventable by protecting skin from the sun's UV rays and not using sunbeds. Getting too much sun can be harmful whatever your age. It exposes you to UV rays that can damage your skin and lead to skin cancer.
It is important to remember the sun isn't only strong abroad. It can be strong enough in Ireland to damage your skin and is strongest during the middle of the day, typically between 11am to 3pm. Be prepared and enjoy the outdoors safely by following the SunSmart 5S’s. Even in cloudy conditions, UV rays can affect your skin.
The sun sends energy to Earth in a few different ways: visible
light that you can see, infrared radiation that you feel as heat, and UV radiation that you can’t see or feel. UV radiation is often confused with infrared radiation. The temperature, however, does not affect UV radiation levels. UV radiation can be just as high on a cool or even cold day as it is on a hot one, especially if skies are clear. Thick cloud provides a good filter, but UV radiation can penetrate thin cloud cover.
AS WELL AS THE 5 S’S IT IS IMPORTANT TO REMEMBER:
• Do not deliberately try to get a suntan
• Avoid getting a sunburn
• Never use a sunbed
For more information on the SunSmart campaign visit www.hse.ie/sunsmart, contact prevention@cancercontrol.ie or #SunSmart on social media.
New advice on mastitis and other breastfeeding challenges
Engorgement, blocked or narrowed ducts and mastitis are common issues for breastfeeding mothers. These can sometimes lead them to end breastfeeding sooner than they intended if the right support is not provided at the right time.
New advice for parents on mychild.ie and a factsheet for healthcare professionals provides a standardised evidence-based approach to these breastfeeding challenges.
The guidance also aims to reduce conflicting advice. For example, mothers affected by these challenges in the past may have come across advice to ‘pump and dump’ breast milk, but it is safe to breastfeed your baby when you have mastitis, breast abscess or other infection (unless they are very premature or their immune system is compromised).
They may also have been recommended to apply high intensity heat or to do a deep tissue massage if suffering from engorgement or mastitis, but this

advice has since changed. The guidance now is that mothers should choose heat and/or cold depending on what feels most effective and soothing to them. Applying cold packs (ice wrapped in cloth) can be helpful to reduce swelling and relieve pain. Very gentle breast massage (including arm pits, areas around neck and chest) also helps relieve congestion.
Engorgement
Breast engorgement is when breasts get too full of milk. This can leave them feeling hard and painful. It usually happens in the early days.
• Do plenty of skin-to-skin contact, responsive feeding and use the laid-back position.
• Gently hand express before feeding.
• Do reverse pressure softening to soften the areola.
• Very gently massage breasts in a circular motion.
• If wearing a bra, use one that fits properly and is nonpadded and non-wired. If engorgement is a challenge:
• Use ice packs every one to two hours and after a feed for 10 minutes.
• Take pain relief.
• Avoid excessive heat and deep tissue massage.
Narrowed or blocked ducts
If an area of your breast becomes inflamed, it can cause some narrowing in the milk ducts. This can make it difficult for the milk to flow freely.
• Follow the same advice as engorgement above and breastfeed as normal.
• If using a breast pump (for example, if the baby is unable to latch), avoid expressing excess milk beyond what the baby needs. Choose the correct flange size and suction pressure on the pump.
Mastitis is an inflammation of one or both breasts. Causes include unrelieved engorgement or a narrowed or blocked duct. Signs include a hard and painful lump, a hot and red wedge-shaped area of engorgement and a raised temperature.
• Follow advice above and contact your GP if there is no improvement, symptoms worsen or you have a sustained temperature of 38.3 degrees C or above.
• Continue breastfeeding, if possible. If unable to feed directly from the breast, hand express or pump just enough to soften the breast
• Get advice from a lactation consultant.
• Antibiotics may be required if the steps above don’t lead to an improvement within 24 hours.
• Avoid excessive heat to the breast or soaking them in warm water.
Topical treatments (lanolin or vaseline) are no longer recommended for milk blisters or lactation-related white spots. Do not pop blister. Instead, attachment and latch should be checked and baby-led feeding positions used. If expressing, use the correct flange size, make sure suction pressure is not too high or low, and always turn off before funnel is removed.
The factsheet contains a quick reference one-pager on managing these four breastfeeding challenges as well as more detailed information on each. There are also links to helpful websites, visuals and videos for therapeutic breast massage, breast compression, hand expressing, boosting breastmilk supply, medications and antibiotic advice, and using breast pumps correctly.
It was developed by a review group which included representation from lactation consultants, public health nurses, breast surgeons, GPs, pharmacists and volunteer breastfeeding organisations.

Parents can find updated advice on engorgement, blocked or narrowed ducts and mastitis at www.mychild.ie/breastfeeding or by searching for these terms and ‘HSE’ on their browser.
The factsheet for healthcare professionals is available at the link below or by searching ‘HSE mastitis fact sheet’. https://www.hse.ie/file-library/mastitisfactsheet-for-healthcare-professionals.pdf
Home sweet home as residents move back into Millfield House


"I would take off my coat and move in here myself; I am over the moon that my brother can call a facility like this his home," said Sylvia Roche, sister of Millfield House resident Kieran.
Millfield House is a community rehabilitation residence in the heart of Cork city at Blackpool, which has reopened following extensive upgrade works.
The property initially opened as a 15-bedroom residential unit for people accessing Cork Kerry Community Healthcare Mental Health Services in December 2000. The residents had shared bedrooms; so, with the onset of the COVID-19 pandemic and the need for social distancing, the residents moved to a temporary property in the city, Garnish House.
Significant refurbishment efforts were then undertaken in 2023 for Millfield House to be repurposed as a six-bedroom community rehabilitation residence, adhering to relevant Infection Prevention and Control (IPC) standards. The residence has been completely renovated to enhance the living accommodation, which includes all single bedrooms with en-suites. There is a modern, bright and welcoming feel to the residence, designed by the team and residents to be as homely as possible. Each resident was afforded the opportunity to be involved in the project, including choosing paint colours, linen, cushions and furnishings for their bedroom spaces. There are communal dining and living areas, along with a large private garden - a real



bonus so close to the city centre.
“99% of the time, we are friends, the other 1% is when I get up too early in the morning and wake him up! The new building is very classy, it's clean and respectable. It helps me think 'I have my own place now, can do what I want, come and go as I want really.' It's good."
Head of Cork Kerry Community Healthcare Mental Health Services, Julie O’Neill said: “Through dedication and perseverance, we have transformed challenges into opportunities and we now celebrate the re-opening of Millfield House after its refurbishment. It is a testament to our commitment to providing exceptional care and support to our service users and a beacon of hope for a brighter future ahead.”
Assistant Director of Nursing Declan McCarthy said it took huge collaboration, communication and commitment from all parties - residents, peer advocates and the multi-disciplinary team - to make this dream a reality.
“The residents have an identity, they have personalised their spaces, there's a sense of hope. They are inspired and empowered by having a more individual way of life; being supported rather than us telling them how they should live their life.”
With the support of Cork Mental Health Association, four apartments in the new development across the way were also secured, to encourage those residents wishing to move on to a
more independent life. Four men have taken up residency in the new units, with the full support of the multi-disciplinary team across the way at Millfield House.
In December 2023, Millfield House and Apartments welcomed back residents from their temporary home at Garnish House. All were delighted to be back to the place they called 'home' with a shopping centre, cinema and cafes next door. The renovations have helped to transform the resident’s lives and they already have great joy and pride in their new environment. One resident Roy O'Neill, has been a resident for 20 years. “I'm out in the apartments now, I love it. A bit of independence and freedom but I still have the support of staff in Millfield House. It's very good and we love it.”
Another resident, Donal Murphy, who lives with Roy, said, “99% of the time, we are friends, the other 1% is when I get up too early in the morning and wake him up! The new building is very classy, it's clean and respectable. It helps me think 'I have my own place now, can do what I want, come and go as I want really.' It's good."
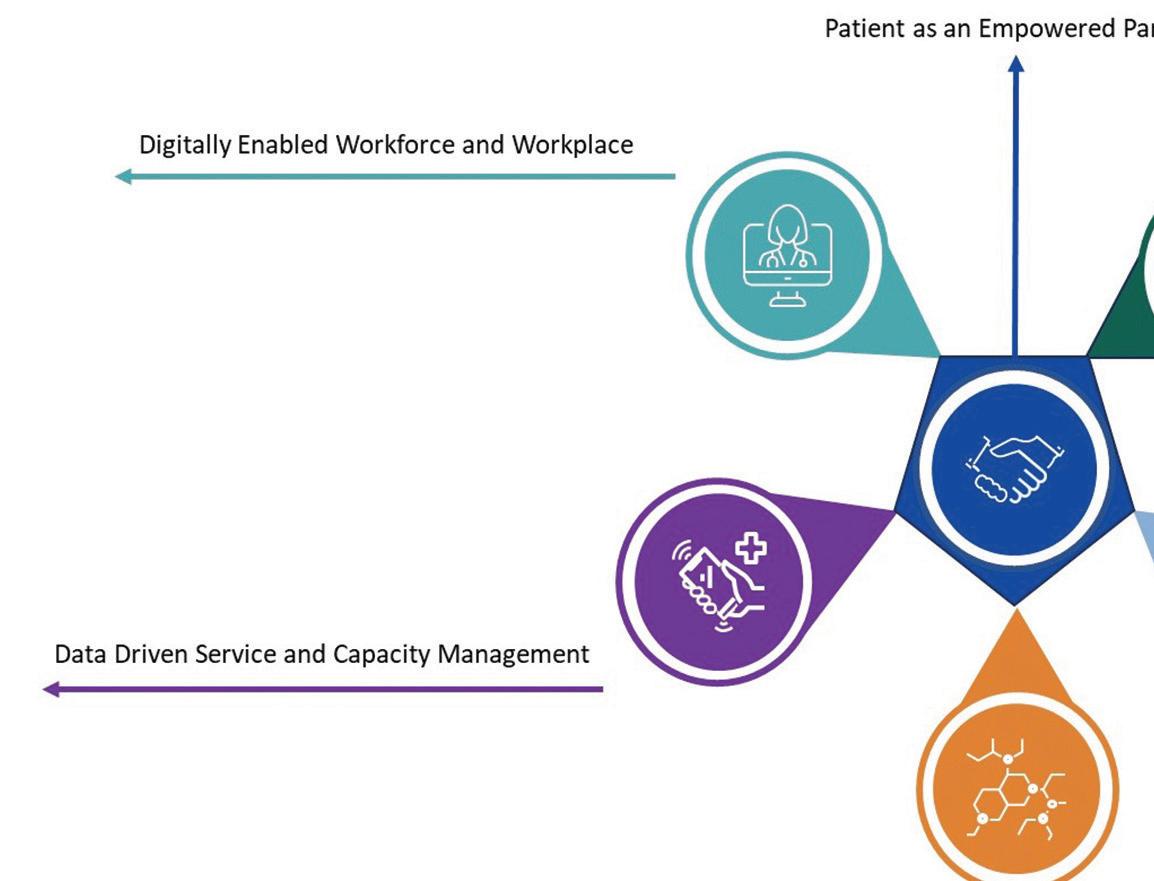
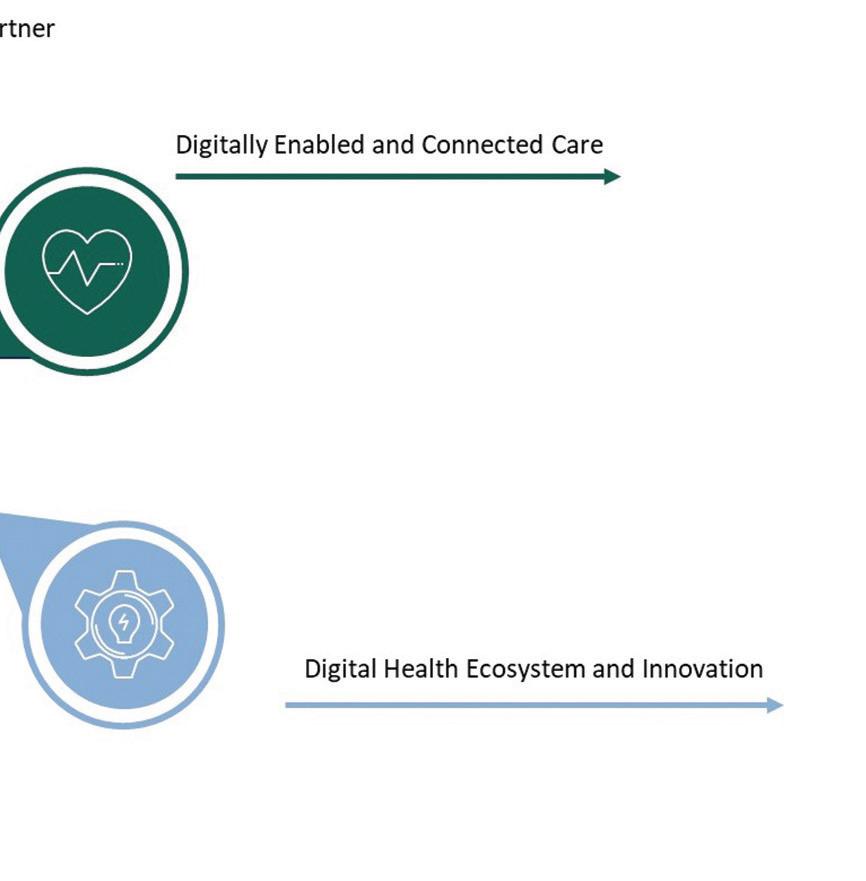
HSE Digital Health Roadmap will enforce common vision to drive innovation and heralds a new era
The pace of change in digital health is rapid and the collaboration between the HSE and the Department of Health to invest in, and implement a Digital Health Roadmap has reinforced the common vision to drive digital health innovations where the patient comes first. Minister for Health Stephen Donnelly launched the much anticipated ‘Digital for Care: A Digital Health Framework for Ireland 2024-2030' on 22 May. Paving the way to digitally transform health services in Ireland, the Framework’s vision of having ‘better health outcomes enabled by seamless, safe, secure and connected
digital health services and which support health and wellbeing for both our patients and providers’ heralds a new era for digital health in Ireland.
This vision will be supported by rolling delivery plans through the upcoming HSE Digital Health Roadmap that aims to accelerate digitalisation of health and social care services in future years.
It has been developed following a significant consultation process with the Department of Health and other key stakeholders and is both patient-focused and clinically led.
The HSE’s Digital Health Roadmap recognises the need

for sustained investment to achieve transformational goals, including the implementation of an Electronic Health Record (EHR), and Shared Care Record (SCR), allowing a single access point to health information for patients and staff.
We’ve already reaped the benefits of e-Prescribing and many health care areas have adopted some aspects of digital health, from video and phone consultation to remote health monitoring, and now as we look to the future, we can all embrace and welcome improved, integrated patientcentred care through the use of coherent eHealth solutions.
The HSE Digital Health Roadmap will be presented through the perspective of a single vision, 6 principles and defined initiatives

The HSE app is a new digital health service from the HSE that will give our patients secure personalised access to their health information, hospital appointments, medical cards and more.



A pilot is currently taking place to help gather valuable feedback to refine the app's functionality before it becomes more widely available. The first version of the HSE app will be available to the public at the end of this year, and will focus on hospital appointments for maternity patients. The first release of the HSE app will also give people reminders and advice about vaccinations and signpost to services and self-care supports. The HSE app will enable patients to carry a list of their current medications and in the future, their prescriptions.
The HSE app will also help you find HSE services near you, including urgent care and wait times where available, get support from HSELive and get notifications about your flu and COVID-19 vaccinations.
Anyone that uses public health services will be able to download and use the HSE app on their smartphone. It will evolve over time as services are integrated into the app with frequent updates, adding more services to the app in 2025 and beyond.
It’s your health service in your pocket –putting your health, in your hands. You can find more information on the HSE app at www.hse.ie/hseapp
Virtual Ward Programme supports patients to receive hospital care at home
The HSE’s National Virtual Ward Programme is launching the first two Virtual Wards in St Vincent’s University Hospital and University Hospital Limerick in June 2024. This exciting new HSE programme has huge potential and will help to expand our virtual services, leverage digital technologies and, most importantly, support patients who would prefer to receive their care at home.
So what is a virtual ward? Virtual Wards are a safe and efficient alternative to HSE bedded care that is enabled by technology. Virtual Wards support patients who would otherwise be in hospital to receive the acute care, monitoring, and treatment they need in their own home. The Virtual Ward model is supported by a strong evidencebase with many pilot projects internationally reporting improved patient and staff experience. Who is it for? The Virtual Ward service may be offered to suitable patients who are admitted to hospital with a respiratory or cardiac condition (in the initial implementation) and are medically stable, but require ongoing monitoring and care prior to discharge.
How does it work? The clinical team will work with patients, their families or carer to assess whether they might be suitable to be treated through the Virtual Ward service The clinical team will show patients the equipment they will be given and demonstrate how to use it. Training on how to use any equipment safely can be provided to family members or carers as well.
Once a patient is transferred to the Virtual Ward service, they remain under the care of the
consultant team that provided care in the hospital. A personalised care plan will be agreed between the patient, their carer, and consultantled care team.
The patients care will continue to be reviewed 24 hours per day, seven days a week by their consultant-led care team and they will agree the best ways to make contact – this could be by telephone or video call. They will also explain what to do if the patient feels unwell.
Patients are empowered to manage their condition by participating in monitoring their health at home and can feel reassured by having access to the Virtual Ward team at any time. The Virtual Ward team will be automatically alerted by the monitoring technology if the patient’s readings worsen, or if they are not responding to treatment as expected.
What are the benefits for patients? Research shows that availing of care at home in a Virtual Ward offers many benefits to patients, including:
• increased patient satisfaction with care
• reduced stress and anxiety that may be associated with a hospital stay
• better recovery due to healing in a comfortable and familiar environment
• lower risk of hospital-acquired infection and loss in muscle strength
• lower costs of travel to and from the hospital for patients, family, and carers
• lower chances of re-admission What are the benefits for staff?
The Virtual Ward model also offers significant benefits to staff with
high levels of staff satisfaction reported in pilot sites with the Virtual Ward model facilitating more one-to-one patient communication and care and presenting an opportunity for staff to expand their skillsets, particularly around virtual patient care. The acceptability and impact of the Virtual Ward model in the first two sites will be evaluated to inform the potential future expansion to other patient cohorts or additional sites.
The programme is a collaborative initiative bringing together stakeholders from E-Health Ireland, the National Clinical Programme Respiratory, the National Heart
Patients are empowered to manage their condition by participating in monitoring their health at home and can feel reassured by having access to the Virtual Ward team at any time.
Programme, St Vincent’s University Hospital and University Hospital Limerick. HSE enabling functions include Communications, Finance, Human Resources, the Office of Nursing and Midwifery Services Development, the National Health and Social Care Professionals Office. Patient Representative bodies are involved in the design and development of the service.
It is led by Prof Richard Greene, Chief Clinical Information Officer, and Deirdre McNamara, Director of Strategic Programmes, and is a key deliverable of the HSE Urgent and Emergency Care Plan.
The signing of the Human Tissue Bill into law by President Michael D Higgins is a significant milestone in the over 60 years of organ donation and transplantation in Ireland. With the planned introduction of altruistic donation and an opt-out register, there is a great opportunity to engage the national population in an important conversation about organ donation.
The official launch of Organ Donor Awareness Week 2024 was held at the Mansion House recently. The key campaign message continues to be built around sharing your wishes with your loved ones about organ donation with the
theme, Don’t Leave Your Loved Ones in Doubt. It is organised each year by the Irish Kidney Association (IKA) in association with the HSE’s Organ Donation Transplant Ireland (ODTI).
Dr Catherine Motherway, Clinical Lead, Organ Donation and Transplant Ireland, HSE, spoke at the national launch of the campaign and said, “For our deceased donor families, we know that the decision to donate organs of their loved one can bring hope and some solace in the midst of grief and we too will listen to their stories and the pride and joy that they have in their loved one’s life and final act of immense kindness.”
At any one time in Ireland, there are approximately 600 people active on waiting lists for organ transplants including heart, lung, liver, kidney, and pancreas.
282 Organ transplant operations were carried out in Ireland in 2023 (32 more transplants than in 2022). This activity could not have taken place but for the generosity of the families of 95 deceased donors and 30 living kidney donors.
In 2023, 54 liver transplants and six pancreas transplants took place at St Vincent’s Hospital, while seven heart transplants and 24 lung transplants were carried out at the Mater Hospital.
Last year, saw an increase in the number of kidney transplants taking place at Beaumont Hospital - 191 kidney transplants took place.
While 161 of these kidney transplants were from deceased donors which was an increase of 31 from the previous year there were also 30 living kidney donor transplants last year, three less than in 2022.
On 31 December 2023, there were 2,502 people in ireland with end-stage kidney failure undergoing dialysis treatment, but only one-fifth (approximately 500 people) of these are on the kidney transplant waiting list.











Behaviours need to be characterised by ‘support, compassion and inclusion for everyone’
“I want to grow this region to become the best place to grow up in, to live in and to work in.” That is the focus for new Dublin and Midlands Regional Executive Officer (REO) Kate Killeen White.
She has set out a clear priority for the health region: stabilising current services and putting the region on a sustainable footing from which to grow and develop. This means ensuring that we have the right budget and people, in the right place to cater for the health needs of the people who are using our services every day.
“The priority is stabilising services, ensuring an unrelenting focus on patient flow and, where we can, building on the strong partnerships with all of our stakeholders across services within the region, but also beyond the region and to ensure that our vision for our services and the needs of our patients are aligned,” she said.
“I think it is important that we don’t lose sight of the reason we are all here and that is to deliver services each and every single day to our patients and service users while we concurrently try to co-design a strategic roadmap for the region. But it really is very much about engagement, about being inclusive, about being compassionate and about bringing people and services together so we all know what our plans are, what our vision is and how we are going to get there.”
population of circa 1,077,639 providing health and social care services to communities living within Dublin West, Dublin South-West, Dublin South City, Laois, Longford, Offaly, Kildare, West Wicklow and Westmeath.
“I strongly believe that reorganising and integrating our services for the population we serve is the right thing to do and I am privileged to be in this role and lead this reform for our region . It’s an honour,” she said.
The region has strong and established clinical and modernised care pathways forged across hospital and community services and
“Compassionate leadership involves a focus on relationships through careful listening, understanding, empathising with and supporting..."
important voluntary partnerships which underpin the model of service delivery that has being built in the region heretofore.
Kate joined HSE Dublin and Midlands from her role as Chief Officer for South East Community Healthcare where, since 2019, she had operational responsibility for delivery of all HSE community services in Carlow, Kilkenny, South Tipperary, Waterford and Wexford, leading a workforce of nearly 5000 staff. A former barrister, Kate has more than 16 years’ senior operational experience across health, regulatory and legal environments.
The HSE Dublin and Midlands serves a
“This reform is not about starting over. It is important for us all to recognise what is working well and what could work better as part of this change. There is also substantial progress on patient pathways and patient flow and progress as part of the ECC programme with growing numbers of patients every day benefitting from these integrated care pathways. I think it is important to acknowledge all this work and recognise that this work represents the foundations from which we will build and grow.”
She aims to bring a compassion with her leadership, which she feels brings out the best in the people.
“Compassionate leadership involves a focus on relationships through careful listening, understanding, empathising with and supporting other people and enabling those that I lead to feel valued, respected and cared for so that they can reach their potential and do their best work,” said Kate.
“And I like to empathise with my colleagues and seek to understand the challenges that they face and I am absolutely committed to supporting others to cope with and respond to work challenges. I like to focus on enabling and supporting those that I lead to be effective and thrive in their work. That is really important to me.”
The new REO said she will be putting a clear focus on behaviours and ensuring staff reflect the values of the HSE. “I’ve been very focused on behaviours because I want behaviours to be characterised by support, compassion and inclusion for everyone, whether they are patients, staff or stakeholders. That is really, really important to me. I’ve been asking staff to not only hold a mirror up to themselves and make sure they are demonstrating the values of the HSE but also to call it out when behaviours aren’t characterised by support, compassion and inclusion for everyone.”
She acknowledged that staff have worries about the changes ahead but reassured people working in the region that the changes will be positive. “As with any change programme, it brings with it a level of concern or worry for people. I’ve deliberately made time to visit as many services as I can across the region and I will continue to do that because I think it is important to be visible and to communicate with staff. I want to ensure that staff know that I am familiar with what they are doing and I am supportive of what they are doing so that we can drive forward the change programme in a way that is consistent and in a way that is all inclusive,” said Kate.
“I really want staff to be enthusiastic, to feel

that they have co-operation and support and are working within a team for our region to deliver care and organise services so they make sense to the people we serve.”
The new Dublin and Midlands REO wants to thank all staff and partners for all they do every day in providing care to our patients and service users. “I can see the really good work that is happening every day and I really want staff to reflect on the work that they are doing, to see what we are doing right but also to figure out what we can do better and to bring that information and reflection into the co-design of the new region. Together, we will transform challenges into opportunities and ensure our continued success and make our region the best place to live in, work in and grow up in,” she said. “It is important that we get the restructuring right from the beginning and this will take time. I won’t necessarily have all of the answers straightaway and I know that can be a cause of concern but it is important that we take our time to do this and to do this right."
The Midlands Regional Hospital Tullamore (MRHT) has introduced a new initiative, the Chronic Obstructive Pulmonary Disease (COPD) Virtual Ward. This program launched in March 2024 with the aim of transforming the care of patients with COPD by using digital technology.
Upon attending the Emergency Department, COPD patients are identified as being suitable for this new service and are then enrolled in the COPD Virtual Ward, with their agreement.
At the heart of this new service lies the integration of digital health technology through the PatientMPower App. Through this user-friendly application, patients can report daily symptoms, and are equipped with a pulse oximeter to monitor vital health metrics including oxygen levels and heart rate on a daily basis. This data is then transmitted directly to the healthcare professionals' platform. Any deviations from target levels or concerning trends, trigger instant alerts, prompting timely intervention and personalised care plans to address emerging issues before they escalate.



management. By harnessing digital health technology, we are empowering patients to take an active role in monitoring their health, while facilitating timely intervention by healthcare professionals. Our goal is not only to prevent unnecessary hospital admissions but also to empower patients with a deeper understanding of their condition, fostering greater autonomy and improved quality of life.”
The digitisation of the Maternity Registration form has brought major efficiencies for both patients and staff at the Coombe Hospital.
In order to access maternity services patients are required to complete a Maternity Registration form. In 2022 there were 6,109 maternity referrals and 100% were received by post. From 2023, patients were offered a choice to either
complete the form electronically or by traditional paper and post.
Of the 5,818 women who registered for public antenatal care in 2023 70 (1.2%) opted for the paper version and the remainder 5748 (98.8%) used the electronic form.
The benefits include improved accuracy around patient data and better transcription of patient details, reducing the chance of any errors.
It is clear the overall benefit for patients is the ease of use, as the form is accessible and user-friendly. The average turnaround times for appointments is now 2-3 days, from 5-7 days with the paper system.
New mum Amy Keane said, “I registered easily online, it was really simple. And I received information about my appointment within three days."
Tallaght University Hospital (TUH) is to begin testing wearable devices which can be integrated into a digital platform for patients with severe asthma. The project has just received funding of €75,000 from the Public Service Innovation Fund.
This brand new venture has been led by TUH Respiratory Consultant Prof Patrick Mitchell, who is also an Associate Professor at Trinity College Dublin.
“Initially 50 patients attending TUH with a diagnosis of moderate to severe asthma will use a wearable device and a home spirometer (measuring lung function). This will allow patients to measure and record their sleep patterns, pulse rate, activity levels, and lung function on a weekly and/or symptom-prompted basis. The wearable device will link to a digital platform so results can be recorded. Those using the device will also be able to record patient-reported outcome measures (PROMs) over a six-month period.”
The new wearable device will then harvest this information to provide the medical team with a retrospective and objective dataset of results to

detail how the patient with asthma was doing over the preceding months. This will facilitate the detection of significant changes in their condition, which in the future will allow for early intervention and treatment, if needed.
Dr Natalie Cole, Head of Innovation at TUH, said, “This project promotes a novel approach that combines a digital interactive wearable, home lung function test, and integrative e-platforms for patients with severe asthma to enhance their overall management and self-care.”
Maree Healy, Registered Advanced Nurse Practitioner (RANP) in Tissue Viability, Midland Regional Hospital
Tullamore (MRHT) and Dr Mary Costello, RANP in Tissue Viability at the Laois/Offaly Public Health Nurse (PHN) group, together run an invaluable vascular outreach integrated care clinic for patients.
The clinics take place in Tullamore Primary Care Centre twice monthly. Patients have embraced this service for its practicality and convenience. Many patients no longer need to attend a busy hospital setting but can attend this community clinic which can be more accessible for many.
As part of this clinic they have developed a patient focused educational component. This educational
club titled ‘Legs 11’ addresses the learning needs of patients who are embarking on the journey of self-care post healing of a lower limb ulcer. Their inaugural event took place recently and had a good attendance from patients and family members.
Maree said, “Using educational material from the HSE and the Legs Matter organisation, the focus for ‘Legs 11’ is on rehabilitation for patients post ulceration, self-care, and education on the prevention of recurrence.”
Mary explained, “We will cover topics like skin care, leg exercises, compression therapies, modes and devices to apply and remove same, and will afford patients and their family time to ask questions.”

The Midlands Louth Meath CHO Social Work
Mental Health Services, including both the Child and Adolescent Mental Health Services and Adult Mental Health Services, showcased the work undertaken by mental health social workers across the region.
The conference was organised following the development of the MLMCHO position paper on the role of social work within mental health services as part of a bespoke piece of work undertaken by the principal social workers with Denise Keoghan, Organisational Development Practitioner in Leadership, Learning and Talent Management.
The purpose of the conference was to assist multi-disciplinary team members becoming more understanding of the range and depth of services and skills that social workers can bring to enrich and enhance service provision. This will contribute to better practice and better mental health outcomes for all our service users.
The position paper also wants to enhance and promote the strategic role that principal social workers play in the design and development of
the service and will lead to better recognition of social workers as valuable and equal members of Mental Health Services.
Social workers are an integral part of multidisciplinary teams located across the geographical area. Their work is embedded within the delivery of Mental Health Services in both adult and child and adolescent services. The role is central to the successful outcomes for people who use the service in the application of the systemic and biopsychosocial model of service delivery.
The conference was an opportunity to highlight some of the roles of social work within this delivery context. It explored areas such as recovery-focused practices, working with maternal mental health, developmental trauma/ trauma informed care, and family-focused interventions such as Family Talk. It also lookd at the values of non-judgemental and unconditional positive regard and how they inform social work practice, the use of Theraplay in social work practice, and mapping journeys to recovery in the context of co-produced multidisciplinary working.
A new injury unit has opened at Naas General Hospital. Patients with minor injuries such as broken bones, sprains, burns, wounds and minor head injuries can attend the walk-in facility located in Vista Primary Care.
Hospital Manager Naas General Hospital Kieran McDonald said, “We are delighted with this pilot service development and extension to our hospital services and

more importantly for our patients presenting with minor injuries who previously found themselves waiting for longer periods of time in the Emergency Department."
"The new injury unit is a walk-in service with no referral necessary and full diagnostics
A new AI-powered technology, driven by a smartphone app hailed a significant breakthrough in helping doctors at Tallaght University Hospital (TUH) diagnose early Alzheimer's and supports identification and recovery in many other serious conditions. GaitKeeper measures walking speed which is often referred to by doctors as the ‘sixth vital sign’.
GaitKeeper is so sensitive it can even indicate if someone could be living with early symptoms of Alzheimer’s disease or other disorders that affect the brain. This is important as new drugs,
expected to be approved in Ireland this summer, will for the first time offer treatments to those in the early stages of the disease.
Professor Seán Kennelly, Consultant Geriatrician and Director of the Institute of Memory and Cognition at TUH was lead clinician investigator in the GaitKeeper project.
“Using AI and AR, the GaitKeeper app captures over 20 points on a person’s body, 60 times per second as they walk, using a phone. This app represents a significant breakthrough and means gait assessments can be
are available on site," he added.
Head of Primary Care HSE
Dublin South Kildare West Wicklow Community Healthcare (DSKWWCH) Brian Kearney said, “The opening of this new injury unit in Naas means that patients will receive the right care at the right place, at the right time.”

Larry Keaveney, Digital Gait Labs; Lucy Nugent, CEO TUH; Professor Seán Kennelly, Consultant Geriatrician and Dr Aidan Boran, CEO of Digital Gait Labs.
conducted by anyone, anywhere, at any time. Gone is the need for specialised equipment like sensors, mats, or special clothing. The assessments can be done in nursing homes, GP practices, outpatient clinics, on hospital wards, and even in someone’s own home.”
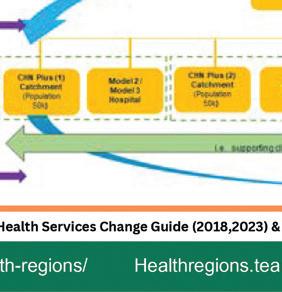
We are currently in a transition period in the move to the new structures both at the HSE centre and health regions. During this time, it is important that current systems will remain in place to ensure safe transition and to maintain services.
The target date for full completion of the following changes in structures and assignments is 30 September 2024.
The health regions team is working with colleagues from various teams to design how functions and roles will operate and transition to the new structures. This process is ongoing.
HR will lead on people transition activities. They will also provide guidance to health regions and the HSE Centre throughout the period of transition.
Many staff will have questions about when changes will happen, why they are happening and who will be affected.
National HR has developed a staff
Next steps as we continue this transition include:
• fulfilling direct reports of the CEO and REOs, prioritising the recruitment of national directors and health region EMTs
• fulfilling other roles on a function-by-function basis, including IHA manager and regional leadership roles
‘Q and A’ document to address questions about the transition to health regions. HR will continue to engage directly with staff and their representative organisations through each stage of the process. https://assets.hse.ie/media/ documents/Health_regions_ questions_and_answers.pdf
The HSE Centre will operate as the HSE's governing body, with a newly-defined relationship with the health regions. The purpose of the HSE Centre will be to support health regions, in fulfilling the functions of Planning, Enablement, Performance and Assurance (PEPA).
The HSE Senior Leadership Team will include the 6 Regional Executive Officers (REOs) and national directors for the following areas:
• National services and schemes
• Access and integration
• keeping some current systems in place to make sure we transition safely and always maintain services to ensure minimal disruption to patients and service users
• aiming to complete these changes by 30 September 2024
• progress detailed design of the Integrated Service Delivery Model for the Health Regions

• Clinical
• People
• Finance
• Technology and transformation
• Communications and public affairs
• Strategic infrastructure and capital delivery
• Internal audit

The HSE Health Regions Programme Team recently attended the International Conference in Integrated Care (ICIC24), hosted by the International Foundation for Integrated Care, in Belfast.
During the three-day event, ‘The Future of Integrated Care in Ireland’, supported by Slaintecare and the HSE, was the subject of a panel discussion featuring Dr Colm Henry, Dr Siobhan Ni Bhriain; and HSE West and North West REO Tony Canavan. A presentation entitled ‘Codesigning Integrated Service Delivery for the Irish Health Service’, authored by Nuala Scannell, Angela Ryan and Lisa McDaid, was presented by Nuala Scannell. Angela Ryan then presented the group’s ‘Design Methodology Approach to Developing an Integrated Service Delivery Model for Irish Health Service Executive's Health Regions’, authored by herself, Nuala Scannell and Lisa McDaid.
Lisa McDaid and Elaine Birkett from National Organisation Development and Design, Health Regions Programme team, hosted an interactive workshop titled ‘Creating the Conditions for Integration: Bridging Evidence, Policy, and Practice’ at the International Conference on Integrated care (ICIC24), attended by 90 participants. Amid Ireland's healthcare transformation with Sláintecare and health regions, the session


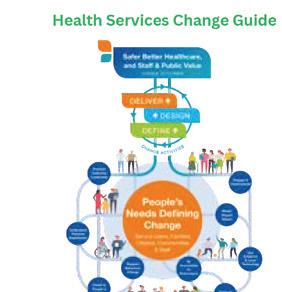






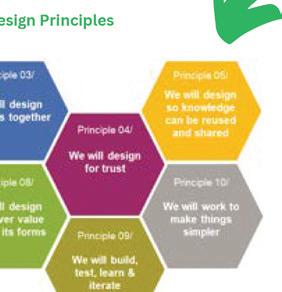
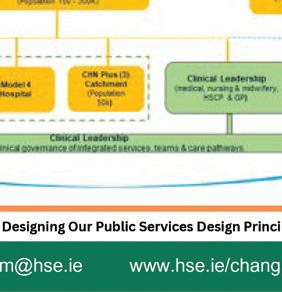
showcased practical uses of the People’s Needs Defining Change - Health Service Change Guide through real-life case studies.
Dr John Cuddihy discussed the importance of Strategic Change Leadership and the benefits of targeted bespoke supports from the Organisation Development and Design team for the Public Health Reform programme.
Dr Maria O'Brien focused on creating the conditions for change in the Integrated






Care Programme for Chronic Disease Management through the use of the Creating the Conditions for Change and Integration resource. The workshop emphasised the journey from evidence to policy to practice, offering insights into managing change, highlighting the significance of people and culture in integrated care and providing practical strategies for implementation in healthcare settings.

ENGLISH
Tá sé mar aidhm ag Acht na dTeangacha Oifigiúla in Éirinn 2021 cur le húsáid na Gaeilge i seirbhísí poiblí agus cuireann sé dualgais nua ar FnaSS agus ar eagraíochtaí eile san earnáil phoiblí.
Tá sé mar aidhm ag Acht na dTeangacha Oifigiúla) 2021 cur le húsáid na Gaeilge i seirbhísí poiblí agus leagann sé dualgais nua ar FnaSS agus ar eagraíochtaí eile san earnáil phoiblí. San eagrán deireanach de Health Matters, thugamar nuashonrú duit ar dhul chun cinn FnaSS go dtí seo ar na dualgais reatha faoin Acht. Tá acmhainn foirne nua á forbairt ag FnaSS. Tabharfaidh sé seo breac-chuntas ar na príomhdhualgais atá orainn go léir faoin Acht agus nascfaidh sé le raon nua acmhainní dátheangacha cabhracha ar shuíomh Gréasáin FnaSS. Rachaidh an saothar seo beo níos déanaí an samhradh seo.
Idir an dá linn, ba mhaith linn go ndéanfadh gach duine a léann an t-alt seo beart éigin. B’fhéidir nach bhfuil a fhios agat go gcaithfidh do fhreagra ‘as oifig’ a bheith i nGaeilge nó i nGaeilge agus i mBéarla. Ní féidir freagra ‘as oifig’ a bheith agat atá i mBéarla amháin. Caithfear an leagan Gaeilge a chur ar dtús, agus an leagan Béarla a chur ina dhiaidh.
Tá roinnt sampla anseo againn chun cabhrú leat an t-athrú sin a dhéanamh. Níl le déanamh agat ach an dáta a chur isteach i bhfoirm uimhriúil nó ríomhphost seolta a chur isteach mar is cuí.

Ireland’s Official Languages Act 2021 aims to enhance the use of the Irish language in public services and gives new duties to the HSE and other public sector organisations.
In the last edition of Health Matters, we gave you an update on the HSE progress to date on the current duties under the Act. A new HSE staff resource is being developed. This will outline the key duties we all have under the Act and link to a new range of helpful bi-lingual resources on the HSE website. This work will go live later this summer.
In the meantime, we would like everyone who reads this article to take some action. You may not be aware that your ‘out of office’ response has to be in Irish or Irish and English. You cannot have an out of office response that is only in English. The Irish language version has to be placed first, followed by the English version.
Here are a few examples to help you with your out of office responses. You just need to add the date in numerical form or enter an email address as appropriate.

Go raibh maith agat as ucht do ríomhphost, nílim ag mo dheasc faoi láthair ach beidh mé i dteagmháil leat ar fhilleadh dhom.
Táim ar saoire ó x go x
Nílim ar fáil faoi láthair, beidh mé i dteagmháil leat ar fhilleadh dhom.
Má tá ceist phráinneach agat déan teagmháil le (cuir isteach ríomhphost) nó téigh chuig ww.hse.ie
Níl sé de dhualgas dlíthiúil ár n-ábhar cothú sláinte go léir a aistriú, ach tá raon leathan díobh ar fáil againn le hordú i nGaeilge ar www.healthpromotion.ie. Nuair a logálann tú isteach ar an suíomh gréasáin cuir an focal Gaeilge isteach sa bhosca cuardaigh agus léireofar na hábhair cothú sláinte gur féidir leat a ordú.
Tá páirt gníomhach ag gach ball foirne agus ag gach bainisteoir seirbhíse in FnaSS chun a chinntiú go dtacaímid lenár n-othair agus lenár n-úsáideoirí seirbhíse a labhraíonn Gaeilge, agus go gcomhlíonaimid ár ndualgais nua agus reatha. Tá tacaíocht ar fáil ar HSELandD. Tá tuilleadh eolais faoi bhealaí gur féidir é seo a dhéanamh ar www.hse.ie/teanga.
Thank you for your email. I am currently away from my desk and will contact you upon my return.
I am on leave (from X to X date)
I am not available at the moment and will respond to you on my return.
Please contact (insert email) if you have an urgent request, or go to www.hse.ie
It’s not a legal duty to translate all our health promotion materials, but we have a wide range of them available to order in Irish on www.healthpromotion.ie. When you log on to the website, pop the word Irish in the search box and it will bring up the available health promotion materials that you can order.
Every member of staff and every service manager in the HSE has a role to play in ensuring that we support our Irish-speaking patients and service users, and meet our obligations both new and existing. Support is available on HSELand. For more information on how to do this, please visit www.hse.ie/teanga.

HSE staff and partners are continuing their support for the Dementia: Understand Together campaign by connecting with local Dementia Alliances and supporting actions such as dementia and brain health awareness events across the country.
In Mullingar, an event was organised to celebrate International Women’s Day in partnership with the Soroptimist Society. Over 100 people attended to find out about the impact of brain health on our health and wellbeing and how staying socially connected and engaged in community life can make all the difference.
The event was hosted by Sarah McCormack, National Healthy Ireland Lead, and guests including many health care professionals from the Midlands region heard from Cathy McHale, Registered Advanced Nurse Practitioner in the Institute of Memory and Cognition of Tallaght University Hospital, Kim Tully, Chief Executive of Engaging Dementia, and Fiona Foley, Senior Project Manager with National Dementia Services.
In Cork, Sheena Cadoo, Occupational Therapist at the

Some of the Dementia Inclusive Listowel Inter-agency group at the Memory Wellness and Dementia Awareness talk
Memory Technology Resource Room in Mallow, colleagues Margaret McEntee and Marguerite Doran, and Ber O’Leary from Kanturk Community Hospital helped to run an event aimed at raising awareness for dementia and giving some practical advice to individuals, groups and local businesses about how they can build a Dementia Inclusive Kanturk.
In Kerry, Deirdre Kearin and Dolores McElligott from the Cork Kerry Community Healthcare Team, and Catherine Murphy, Senior OT at Tralee’s Memory Technology Resource Room, organised a memory wellness event in
partnership with Dementia Inclusive Listowel. Dr Mary Buckley, Consultant Geriatrician at Kerry University Hospital, hosted this well attended evening with key speaker Dr Antoinette O’Connor, Consultant Neurologist at Tallaght University Hospital.
We all know the importance of engaging with people in communities to talk about dementia, the risk factors associated with developing dementia and helping people to access services and support at the right time – so it’s great to highlight HSE staff out making a difference in the local communities we support. If you’d like to share your local dementia initiatives, email understandtogether@hse.ie or to find out more about the campaign visit www.understandtogether.ie
It has been 20 years since the government introduced the Public Health (Tobacco) Act banning smoking in all workplaces, bars and restaurants. In that time, smoking rates in Ireland have fallen from 27% to 18%
On 29 March 2004 Ireland became the first country in the world to remove ashtrays from work desks as well as pub and restaurant tables. According to the World Health Organization (WHO), over one quarter of the world's population - 74 nations - now live in countries with complete smoking bans in indoor public places, workplaces and public transport.
Fines for breaking the smoking ban are set at €3,000 and the HSE National Environmental Health Service continues to enforce these measures. A key aspect of their work today is in relation to the sale of tobacco to minors. The HSE undertakes compliance checks, also known as test purchases, in retail outlets
HSE Quit services are free and available all year round. The Quit service provides personalised, evidencebased plans, tailored to each person’s needs, using any combination of the support options:
• an online-personalised Quit plan where people can track their progress
• face to face and group support from local community based services
to determine if retailers will sell tobacco products to minors. This has helped to contribute to a reduction of smoking rates among children, reducing from 19% in 2004 to 5% today.
“While it was viewed as a controversial measure at the time and faced stiff opposition, the positive impact that the smoking ban has had on public health in Ireland is clear. Over the past two decades, smoking rates have reduced significantly - particularly among children. Hundreds of thousands of people have given up smoking since 2004. We have continued to push ahead with measures to combat smoking because, simply, there is nothing good about this habit. It is addictive, it is lethal and I have yet to meet a smoker who is happy that they started.
Twenty years on from the introduction of the smoking ban, we now face new, worrying challenges posed by vaping. Minister for Health Stephen Donnelly has taken important steps to ban the sale of
• text message or phone support from the Freephone Quitline 1800 201 203
• a free Quit Kit to help prepare
• free Nicotine Replacement Therapy (NRT) and advice on how to use it
• daily tips and support from people who have quit and who are trying to quit on the Facebook page.
vapes to children and is examining further measures to address these challenges.”
- Tánaiste Micheál Martin
“I am worried however that since COVID we have seen a complete stall and even a slight rise in smoking prevalence therefore new and innovative policies will be required to truly realise the government’s goal of a tobacco free Ireland”
- Martina Blake, the HSE’s lead for the HSE Health & Wellbeing Tobacco-Free Ireland programme
The HSE Tobacco Free Ireland Programme carried out a public opinion survey to ascertain views on Tobacco Endgame policies in Ireland with majority public support (50% or greater) for the proposed policies. These proposals included the phasing out of tobacco sales to children, reducing nicotine in tobacco to make it less addictive and requiring tobacco companies to pay the state for the health costs due to the harm caused by tobacco products.
Andy’s global experience makes him a perfect fit for new role
Arriving in Ireland via the UK, New Zealand and Australia, South West REO Dr Andy Phillips has already overseen massive structural change across various healthcare systems.
He made the leap to Ireland because the changes proposed under Sláintecare excited his long-standing interest in integrated care.
“We call it integrated care but I think for people who use our services, it's just healthcare. We create these names but it really is just a great opportunity to do things at scale and really connect things better for the people that we’re privileged to serve,” he said.
He noted that all the health systems he worked in previously have all faced exactly the same issues as Ireland does now.
“They weren’t planning to support the health and wellbeing of communities in general. They were a sickness services and they continued to be a sickness services until they become overwhelmed,” he said.
Andy explained that health services are now improving services for people who have heart disease and stroke and other conditions that used to kill people off in large numbers. However, he said, we must plan for people who are living longer.
we'll have less of a challenge in terms of providing staffing. So our staffing models are going to need to change to evolve different types of staff with different types of skills in particular.”
He said that his first priority will be to look at unscheduled care - urgent and emergency care.
“The culture that we have to have around here is that having somebody in a trolley in an emergency department is terrible care, and we're not going to accept it. We’re going to work as a team and individuals to say there will be no trolleys in our emergency departments,” he said.
“In 10 years’ time, there will be an awful lot more people aged over 80 in our system and so we're going to need to evolve our services to support them.”
His next area to target is scheduled care.
“I think we need to plan for success in the health system. Success means rather larger numbers of people who are older and more frail, living with a myriad of complex physical conditions and some mental health conditions that we’re going to need to care for well into old age.
“In 10 years’ time, there will be an awful lot more people aged over 80 in our system and so we're going to need to evolve our services to support them. There will be a lot more dementia in our system and I don't expect that
“People waiting for years for operations or procedures is just not acceptable. If you think of people as your customers or clients, then having those customers or clients waiting years for what you had to offer is just not acceptable to anybody.”
He said that he always tries to balance six things when he is looking to make any changes in a system.
“The first is I'm trying to balance service quality – is the service safe, is it timely, is it equitable? It needs to be effective and person-centred. I need services that are high quality and the most pressing issue is access. Generally, people think
the service is pretty good, but the access is poor and part of the reason that the access is poor is we need to improve the productivity of the service,” said Andy.
“The second thing I need to balance is value for money. I'm trying to squeeze every little last bit of waste out of the system and make sure that what we deliver is a value to our customers, the people we are privileged to serve in the community. I'm trying to make sure that the outcomes that they get are the best for every euro that we spend.”
He explained that the third thing to balance is population health and accountability.
“It's not just about providing a service. I need to make sure I work with housing, employment, education, on their social determinants of health, which make up 80% of our health and wellbeing actually to get the best possible health outcome. So internally what I'm thinking is my job is to make sure that the people that I serve in Cork and Kerry are the healthiest people in the world.
“Then the fourth thing I have to balance is staff. We have maybe 20,000 working in our health area. If I was to reduce the absences by 3%, that gives me an extra 600 staff per year. So making sure that people have a good experience of work, that their health and wellbeing is good at work and that they enjoy their work is really critical to what I'm trying to achieve.”
He said equity was his fifth area that needed to be balanced, noting the inequities geographically and among different population groups designed into the system.
“The last thing I need to balance is climate change because we are one of the major polluters. But by changing the way we use our buildings, the way we use things like

anaesthetic gases and, in particular, the way we ask people to do a lot of travelling in cars, we can make a big impact.”
He said that success after 10 years will be measured on those six things.
“Some of the things such as population health are measurable over a longer time scale but there are much shorter term measures of success. I'm completely committed to Sláintecare and the requirements of thatpeople getting their outpatient appointments within 10 weeks, people getting their diagnostic treatments within 11 days and getting their operations within 12 weeks. All those are really critical.”



Technology funded by the Mercy University Hospital Foundation, which is used to assess the severity of liver disease, is now operational at Mercy University Hospital in Cork.
Traditionally patients needed to have a liver biopsy to assess and tell if there was significant permanent damage in the liver, but the new FibroScan works like an ultrasound and is quick, non-invasive, and painless. The FibroScan gives a computer generated image and a readout that tells exactly what the damage to the liver is by quantifying the amount of fat in the liver, as well as identifying if the liver has scar tissue or if there is serious liver disease such as cirrhosis.
It is now possible to readily determine which patients with liver disease are at risk of
complications and need to undergo regular surveillance for complications, and possibly be referred to transplant assessment. It allows medical teams at ‘The Mercy’ to reassure other patients that their liver disease is not progressing, and they can be discharged from hospital clinics to the care of their primary care physician. This will in turn free up clinic space for patients who need appointments.
Professor Martin Buckley, Gastroenterology Specialist at Mercy University Hospital, explained that patients with all types of liver disease will benefit from assessment by FibroScan. “By using the FibroScan we can work out if the liver disease is serious or has long term implications; or if the patient is able to avoid invasive unnecessary investigations.”
WATCH HERE: https://www.youtube.com/watch?v=-rYbYh4hHbA
Welcome to Westfield Integrated Care Centre in Ballincollig, Co Cork - one of the biggest integrated care buildings in the country, at almost 70,000 square feet of accommodation.
The flagship building opened in January 2024 and is home to both the Integrated Care Programme for Older Persons (ICPOP) and the Integrated Care Programme for the Prevention and Management of Chronic Disease (ICPCD). These work side-byside towards the ultimate aim - keeping people out of hospital, where appropriate, receiving the care they need close to their homes.
Paddy, who uses the services of ICPOP at Westfield, said, “The facilities are absolutely beautiful. Dr Tim [Consultant] and the staff are stunning. The whole experience is more than what I expected. I would advise anyone to come here, it's so encouraging, so relaxing and so reassuring to have a facility like this here.”
Angela is busy with her pulmonary rehab in the gym on the ICPCD floor. “I have asthma and find it very hard to breathe at times but since I came here, there's a great improvement in me. Before I thought going up the stairs was a terrible

burden but now I realise that's exercise. I'm really delighted with the staff because they are so good to me.”
The large building is bright, modern and welcoming. Each floor is home to a team of specialist nurses, consultants and related professionals such as speech and language therapists, physiotherapists and occupational therapists who work out of the brand new building with full ventilation and access to large gym and clinical spaces.
People using the integrated service report faster referral times and a multi-disciplinary approach that allows them to see several healthcare professionals at one visit, rather than having to travel to separate appointments.
Within an integrated health service, individuals receive a continuum of health promotion, disease prevention, diagnosis, treatment, disease selfmanagement, rehabilitation and palliative care services that are co-ordinated across different providers and healthcare sites. Such an approach places people at the centre of care, with services planned around them according to their needs. ICPCD shifts the focus of healthcare away from secondary care sites and back to the community.
HSE CEO Bernard Gloster launched an ambitious plan to reduce the health inequalities and challenges faced by the Travelling community in Cork and Kerry.
Six Traveller organisations worked together with the HSE Cork/Kerry Traveller Health Unit to develop the Cork Kerry Traveller Health Implementation Plan ‘Missling on the Tobar’.
The centrepiece of the event was a play produced by Traveller organisations for the event, depicting the challenges Travellers face in accessing public services.
The five-year plan identifies Traveller health priorities including: mental health and suicide; the
impact of trauma on Traveller community health; addiction and access to culturally appropriate services across the region; the impact of lifelong discrimination and racism experienced by Travellers; the impact of poor accommodation and barriers to education as key social determinants; Traveller chronic ill health; the need for culturally appropriate health promotion for Traveller men and cultural supports, such as horse projects; the need for culturally appropriate health promotion for LGBTI+, older Travellers and disabled Travellers; and access to services for Travellers in rural areas.
www.hse.ie/eng/services/publications/cork-kerry-traveller-health-implementationplan.pdf




Solace Café, a HSE-funded out-of-hours support service in Cork city for those experiencing mental health difficulties, “will save lives” according to Minister Mary Butler at its official opening.
The Cork service is the first of five planned around the country. It provides a safe and welcoming service for adults who need help and support when facing mental health difficulties, or distress.
The Cork café is a collaboration between the HSE and Cork Mental Health Foundation. The team includes a manager, service coordinators, peer connectors, volunteers and admin staff. Together, they provide personalised support plans that are tailored to each individual's unique needs and circumstances, operating during evenings and weekends in a non-clinical environment.
Since opening in Cork in July 2023, Solace Café has provided support to more than 376 people. Of these, 206 received social support and 107 received peer support.
The need for the café was acknowledged in the ‘Model of Care for Crisis Resolution Services’, which recognises that when individuals experience a mental health crisis, it often happens outside of the regular working hours and that those experiencing mental health crisis require specialist services to provide brief, person-centred, intensive supports in a timely way.
HSE National Clinical Adviser and Group Lead for Mental Health Dr Amir Niazi spoke at the launch and said that the centre is the first of five planned such cafés in the country. “This will be a learning site … this knowledge is not available in books, we learn from people delivering and receiving services.”
Tess O’Donovan, Chief Officer for Cork Kerry Community Healthcare, congratulated all those who put significant time and effort towards bringing Solace Café to fruition. He added that the café provides a secure haven for individuals seeking support, with the goal of avoiding crisis and reducing the need for hospitalisation.

HSE Cork Kerry Community Healthcare took great pride in hosting a highly anticipated event recently: The Child and Adolescent Mental Health Services Collaboration Day.
This was held at the Oriel House Hotel in Ballincollig and was attended by CKCH Chief Officer Tess O’Donovan and the new HSE South West Regional Executive Officer, Dr Andy Phillips.
The event garnered significant attention and enthusiasm from a wide spectrum of participants, including CAMHS team members hailing from both Cork and Kerry. In attendance were representatives from all community teams, specialised units, the dedicated staff of the inpatient care facility and members of the Cork Kerry Community Healthcare CAMHS Governance Group. Their collective presence fostered a vibrant atmosphere of collaboration and knowledge exchange.
Set against the backdrop of recent challenges,
A free community health festival helping older adults connect, access information and support positive health and wellbeing took place in Cobh Community Hall in April with a great turnout from local residents.
Launched by Dr Andy Phillips, Regional Executive Officer of HSE South West, ‘Keep Well, Keep Movin’ brought older adults together to showcase a wide range of community, voluntary and primary care services which promote enhanced physical, social, cognitive, mental health and wellbeing.
Dr Phillips, spoke on the importance of introducing physical activity into our daily lives to help maintain physical and mental health and to help reduce the risk of developing long-term conditions.
“There is excellent evidence that physical activity
including the enduring impact of the Covid 19 pandemic, the unveiling of the Maskey Report and recruitment hurdles, this gathering stood as a symbol of resilience and unity. It provided a unique opportunity for professionals across various disciplines within the service to come together and reflect on the journey thus far, celebrate successes and navigate the path forward.
The Collaboration Day served as more than just a discussion forum; it was a celebration of progress and a testament to the commitment of all involved to deliver exceptional care to our community’s most vulnerable members. Throughout the day, attendees engaged in lively discussions, shared valuable insights and showcased practices that continue to elevate the standard of care delivery within our community.
In essence, this event underscored the resilience and unwavering commitment of Cork Kerry Community Healthcare to the well-being of our community’s children and adolescents. Moving forward, CKCH remains steadfast in our mission to build upon the momentum generated by the Collaboration Day and continue driving positive change in the realm of mental health services.
also boosts your self-esteem, mood, sleep quality and energy. For providing services to older people, movement is one of the 4Ms alongside delivering what matters to the person, optimising their medication and supporting mental well-being,” he said.
The health festival included guest speakers on Nutrition, Singing for the Brain, Physical Health, Falls Prevention and Sleep Hygiene. Festival-goers also enjoyed a more hands-on approach with a Drum Fit demonstration - a low impact physical activity which aims to improve circulation, brain function and wellbeing.
Attendee Eleanor McSweeney shared her experience. “I had a great day and really benefited from the health information available. I particularly liked the music and movement. All the presentations were relevant to people of any age. I hope that we see more events like this organised in the future. Thanks to the wonderful HSE staff who made the event possible.”
The Making Every Contact Count (MECC) programme is a pivotal initiative in healthcare, designed to empower healthcare professionals to proactively engage patients in discussions about lifestyle changes. By addressing key risk factors and promoting preventive measures, MECC aims to curb the onset of chronic diseases.
This proactive approach enhances patient wellbeing and also reduces the burden on healthcare system. Through comprehensive training and resource development, MECC aims to equip healthcare professionals with tools to integrate health conversations into routine care. The following examples highlight how MECC translates into tangible actions, fostering healthier communities one interaction at a time.
The recent opening of a specialist clinic for lymphoedema and lipoedema patients at Summerhill Primary Care Centre, Co Meath, signifies a crucial development in
addressing these conditions. This clinic facilitates access to multidisciplinary teams, and have forged connections with local fitness centres, emphasising movement and aquatic exercise vital for lymphoedema management. Having completed the MECC training programme, the team proficiently deliver MECC brief interventions, prompting positive feedback from service users.
in East Cork
2023, MECC Health Promotion Lead Máire O’Leary, collaborated closely with Niamh Motherway, Assistant Director of Public Health Nursing, to ensure the entire public health nursing team completed MECC training. This involved eLearning and workshops attended by 32 staff, including public health nurses and registered general nurses in Middleton and Carrigtwohill. Mairead O’Driscoll, Public Health Nurse with the North Lee team (pictured below), noted the value of MECC's health behaviour change framework in patient interactions “We can still
incorporate these brief interventions regardless of how busy we are. It might be two minutes of a brief intervention that can be invaluable.”
In 2023, the Occupational Therapy team serving Co Clare transitioned into a MECC site, a role they continue to fulfil in 2024. Led by Annemarie Delaney, Occupational Therapy Manager of Clare Primary Care and Older Persons Service Occupational Therapy, and supported by Sinead Reidy, Senior Occupational Therapist, the team collaborated to develop a MECC Implementation Plan. This comprehensive strategy encompassed communication, resource allocation, intervention recording, and quality enhancement processes. Bernadette Mullins, Health Promotion and Improvement Officer, provided vital support throughout. Nine MECC health promotion leads within Health Promotion and Improvement across the county are actively assisting services and managers in implementing MECC within teams and services.


Ireland having the longest life expectancy in the EU is something to be celebrated. However, with an ageing population there is an increased need for age-attuned healthcare services.
Co-production and collaborative working are fundamental values of the National Clinical Programme for Older People (NCPOP).
Partnering with Age Friendly Ireland, NCPOP established the Older Persons Reference Group
Talking Mats support residents to feel empowered
Members of the older person’s reference group share what matters to them during a recent engagement.
(OPRG) to ensure the voice of older adults is at the centre of everything we do. The OPRG has membership from each of the 31 Older Persons Councils in Ireland, which represent older people in all communities.
The forum provides a space for the NCPOP to harness the insights and experience of our older adult population and facilitates their input into the co-design and improvement of Ireland’s health and social care services. It also offers a two-way communication space between the local and regional Older Persons Councils, Age Friendly Ireland and NCPOP.
Feedback by members of the OPRG on the purpose of the group has been uniformly positive:
“By participating in the reference group, older adults can develop a stronger sense of agency and advocate for positive changes that directly impact their lives and wellbeing.”
To date, the forum has had three meetings which have provided valuable insights into what is most important to older adults in terms of health services. Communication between the older adult and providers and ensuring everything we do is based on what matters to them, has been a central theme.
Talking Mats is a picture based communication tool which supports people express their views and feelings, in line with the Assisted Decision Making (Capacity) Act 2015. Talking mats take an individual’s wishes into account at all levels of decision making about their lives- it uses a selection of communication symbols covering a variety of topics.
Once a topic has been chosen, the resident is given options one at a time and asked to think about each one. It is placed on the Talking Mat to indicate how they feel about it.
In January 2024, the topic ‘activities currently being offered to residents’ was explored in St John’s Community Hospital, Enniscorthy by the Speech and Language Therapy and Social Care teams. 16 of the residents on a long-stay ward were introduced to the talking mat format. They were asked what they liked to do, did not like to do and what they were not sure about. Residents were also given the opportunity to express individual wishes.
"It
gave the quieter residents a platform to give information. The approach is easy and effective to get a true understanding of what the residents want."
The staff doing the Talking Mats with the residents reported the approach helped to empower residents to give feedback in an objective manner. It included all people irrespective of cognitive decline, receptive and expressive communication difficulties to have an opinion on what they would like/ do not like to do. The format and pictures helped to keep focus, increase understanding and get more expressive communication. It gave the quieter residents a platform to give information. The approach is easy and effective to get a true understanding of what the residents want. Going forward Talking Mats will continue to implemented on a variety of topics, including food preference and advance planning.
Having worked on the frontline as a nurse, HSE Mid West REO Sandra Broderick understands the challenges facing staff across health and social care services, her most recent roles have given her an understanding of the opportunities to overcome those problems through collaboration across services and delivering integrated care.
Sandra was the first REO to take office back in December. She has already made an impact on the ground and is keen to keep the momentum going as the region, similar to other regions, continues to respond to a number of challenges.
“The Mid West is a unique area, we serve a population that has seen a 45% increase in the over 65 age group per the 2022 census, a key feature of our population is the socioeconomic deprivation experienced by a significant proportion of our residents. To respond to those unique challenges we are fortunate enough to have employed the most wonderful and committed staff where we have an ability to draw on multiple layers of expertise”
“We have to work with our multi agency partners; our local authorities, on things like access to housing and housing stock; with our partners in education, to support people to remain in education and our many other stakeholders and partner organisations to address the wider detriments to health. One of my key priorities when I took up the position as REO was to understand the profile of our population, their needs and how we commission and reform our services to meet the unique needs of service users across the HSE Mid West. We have the knowledge and expertise to devise and deliver regional solutions to address our regional challenges.”
Sandra has extensive experience in leading and delivering health and social care services in the UK and in Ireland. Sandra worked in
General Nursing with the NHS in both community and acute services, and then moved into various healthcare management roles across the NHS including senior advisory roles within health and social care.
She returned to Ireland in 2019 to join the HSE as Assistant National Director for Older People Services, leading this service from the HSE’s national community operations team.
While acknowledging the challenges the HSE Mid West is facing with regards access to
“I am an innovator, I’m not afraid to try new things to try to make things better."
urgent and emergency care, she highlighted that there is much reform already delivered, and a committed workforce to deliver additional reforms to integrate services across the region to deliver care closer to people’s homes; some examples of this include the region standing up a satellite dialysis unit in Ennis, delivering more community care options such as sub-acute care for older people and strategically planning additional services to meet respite service demand for people living with disabilities across the Mid West. In addition to this, the region is building on the acute strategic capacity plan to deliver at least 50 additional acute beds per year over the next five years.
She said her priorities are delivering on the region’s five-year capital plan, addressing access challenges in both acute and community services, particularly through the delivery of the acute bed capacity plan,
delivering additional AMU hours of service, investing in additional respite provision for people living with disabilities and through delivering digital enabling solutions.
“I consider myself to be innovative, I am not afraid to try new things to try and make things better for our service users and staff. And we do need a fresh approach to how we do things and how we make our services more integrated. We have challenges here in the HSE Mid West, certainly, but we are working on it together and we will overcome those challenges. There is no problem too big that we can’t solve when we all come together,” said the new REO.
She praised the staff and said she looked forward to working with them to make the services better for the population.
“We have excellent clinicians and support staff that have the expertise to continue providing world class service delivery, we have a focused and committed leadership team. I recognise that there has been sustained pressure on the staff across the region, starting during the pandemic and there hasn’t been much easing in that pressure in terms of demands for health and social care services. Yet the staff continue to be amazing and have shown such a ‘can do’ attitude in their efforts to deliver the best care for patients and service users,” said Sandra.
“I get great feedback on our services but I accept that it not the lived experience of everyone who accesses our services. But for every negative story I hear, I hear 10 positive ones. I believe we do listen to the feedback from our service users, this being evident in the many wonderful initiatives delivered in response to the hospital inpatient survey.”
She said that she will measure her success over the next few years on the delivery of that five-year plan.
“We must deliver that plan if we are to achieve the success we need. We also need to retain

our amazing staff, as well as attracting new people to our workforce that we require to deliver all our new services,” said Sandra.
“It is about bringing care to people closer to their home and redistributing some of our resources to improve population health in areas of greatest need, that they are supported to be more proactive about their health and preventing illness.
“Another success factor will be how we actually integrate our staff, that there isn’t, perceived or otherwise, a big wall between acute, public health and community services. That we are one health service. We can achieve that with buy-in from our staff and by getting rid of the bureaucracy that can sometimes limit our ability to do things more efficiently and better for our patients and our staff."
The dedicated Cataract Clinic (DCC) for ophthalmology outpatients at Nenagh Hospital has emerged as a leading centre for cataract surgery pre-assessment, with more than 40% of patients having surgery within a month of consultation, and 90% undergoing their operations within four months
A GP-referral service, and the only one of its kind in Ireland, the DCC was established in July 2022 at the hospital’s modern Lough Derg suite alongside five other eye clinics - laser, intra-vitreal injections, post-operative review, pre-op assessment, and a day clinic for routine appointments.
The DCC runs twice monthly, each appointment providing patients with a consolidated, comprehensive range of tests and examinations— including consultant appointment—that traditionally would have required multiple visits.
“We’re very excited about what we’re providing for our patients, which is revolutionising patient care while reducing waiting times,” said Adebusola Owokole, Perioperative Clinical Nurse Manager
(CNM2) in the Ophthalmology Department.
“The DCC has brought together and streamlined processes into a single-day, single-location service that raises the standard of surgical pre-assessment excellence, improves the wait time for surgery, and helps ensure a satisfactory outcome.”
Led by Consultant Ophthalmologist Mr Conall Hurley, the DCC’s multidisciplinary team includes a senior medical and nursing staff, an optometrist, healthcare assistants and administrative support. Prior to the implementation of the DCC Model, most cataract patients had average wait times of two to four years for the procedure. Since the opening of the stand-alone, high-volume, consultant-led DCC in Nenagh in July 2022, the total number of patients waiting for a procedure has reduced from 647 to 131. The number of patients waiting longer than 12 months has decreased from 134 to just 10 and the average wait time for patients on the day case waiting list has reduced to four months - and continues to fall.
THE Patient Advocacy Liaison Service (PALS) of UL Hospitals Group is looking for volunteers to join their teams at University Hospital Limerick and, for the first time, Croom Orthopaedic Hospital, to welcome patients and visitors, assisting with way-finding and general queries, and helping people to give feedback on their experience of hospital service.
As hospital ambassadors, PALS volunteers are an important element of UL Hospitals Group’s efforts to improve care standards and the overall patient experience in our hospitals. The volunteers, dressed in distinctive red jackets with an embroidered gold logo, have multiple roles, including giving directions and accompanying patients to appointments, providing information for patients and visitors, and gathering patient feedback.
The service wants hear from people who are available to volunteer either in UHL or Croom
Orthopaedic Hospital for a minimum of three daytime hours per week, Monday to Friday.
Brian Kelly, a retired local authority official who has been a PALS volunteer at UHL since 2007, said anyone with free time to spare could volunteer for a role he has found to be “hugely rewarding”, for himself and for the people he assists in the hospital.
Liz Barry, PALS Manager in UHL and Croom, said the experience of Brian, who applied to volunteer after retiring from work, is typical of many people, who sign up for a variety of reasons, from a specific interest in healthcare to a general wish to use free time to do something positive to their local community.
Anyone interested in volunteering for PALS should send an email outlining their details and available hours, to UHLPals@hse.ie
Anne Quinn, Margie Sheehan, Linda Fahy, Verena Tarpey, Dr Seàn Kelliher, Catherine Corbett, Sarah Nash, Professor Clodagh O’Gorman, Alison McCaffrey.
The Rainbow Badge is a simple visual symbol identifying its wearer as someone an LGBTQI+ person can feel comfortable talking to about issues relating to sexuality and gender identity. It shows that the wearer is there to listen without judgement and signpost to further supports if needed. The Children’s Ark joins healthcare facilities across the country by taking part in this initiative.
Staff in the Children’s Ark at University Hospital Limerick (UHL)wearing this badge are signalling to the young people in the service that they are open to having conversations about sexuality and gender identity. The launch of the Rainbow Badge initiative was marked by an event in the CERC at UHL.
Professor Clodagh O’Gorman, Consultant General Paediatrician at UHL and Chairperson of Paediatrics at the University of Limerick explained why the initiative is important.
“Many people still feel afraid to disclose their sexual or gender identity - being unable to do so often increases their risk of physical and mental health problems. At the Children’s Ark, we want to provide a safe space where the young people using our service feel comfortable discussing any issues relating to their sexuality."
The Children’s Ark is the first service at UL Hospitals Group to take part in the HSE Rainbow Badge
A new simulation facility at University Hospital Limerick (UHL) is providing undergraduate and postgraduate doctors, nurses and allied health professionals with simulation training in a range of clinical procedures. Housed in the Clinical Education and Research Centre (CERC) at UHL, the CERC Simulation Lab has a wide variety of equipment in its simulation-based education and training programmes, including full-body manikins and task trainers (adult, paediatric, maternity).


initiative, however, it is anticipated that this initiative will be rolled out to services across entire group.
The HSE provides education and training for all staff who want to take part in this initiative. When staff members sign up to wear the badge, they acknowledge why the project is needed and commit to providing an environment that is open, tolerant and inclusive. The aim of this initiative is to actively break down barriers which LGBTQI+ people may face when accessing healthcare.
Dr Dani Hall, Consultant in Paediatric Emergency Medicine at Children’s Health Ireland (CHI) who launched the Rainbow Badge at CHI, spoke about the positive impact that the badge has had there.
“We’ve surveyed our staff at CHI on their experiences of wearing the HSE Rainbow Badge. The responses have been so positive, both in terms of interactions with other staff, and with young people and their families," she said.
"There’s an overwhelming feeling of pride: pride in taking part in the initiative, the message the badge sends to LGBTQI+ staff and patients, and pride in representing the community in healthcare.
"It’s also described as a symbol of safety and inclusion for patients and their families.”
In addition to regular teaching, several other events have been hosted in the CERC Simulation Lab since the summer of 2022, including advanced cardiac life support (ACLS), clinical induction training for Interns, MRCPI examinations, organ donation education, basic ECHO training, and Adult Critical Care Transport training.
Dr Sarah Carroll, Senior Simulation Technician, ULHG, who has been closely involved in developing simulation scenarios, researching and sourcing equipment and managing the simulation events, said: “It has been an honour for me to be involved in the development of this facility, working to ensure that students are provided with the best possible learning experience.”
In a proactive effort to tackle the growing concerns surrounding secondary school refusal among parents and educators, Clinical Psychologists at the Ennis Primary Care Centre (HSE) have introduced a three-part series of collaborative workshops.
These workshops offer vital support and guidance to families and schools grappling with this issue.
Emphasising a holistic approach to care, the initiative seeks to cultivate a culture of collaboration among parents, schools, and mental health professionals.
The psychology service has noted a significant surge in referrals for teenagers experiencing self-reported anxiety, particularly those with school refusal. School refusal, often a symptom of underlying social anxiety, has become a pressing concern in recent years.
The three half-day workshops represent a significant stride towards effectively addressing the multifaceted challenges associated with school refusal. Parents are offered the three workshops within one-month intervals, allowing them time to consolidate and practice the information provided.
The first two workshops are facilitated by Senior Clinical Psychologist Sian Harris, Clinical Psychologist Dr Colette Conroy as well as Assistant Psychologists Samira Barar and Melissa Garrihy.
The final workshop is facilitated by both clinical psychologists and educational psychologists and is offered to both teachers and parents together.
Every secondary school in Co Clare has attended a half-day workshop delivered by HSE Primary Care Psychology and NEPS. The workshop focuses on developing an understanding of what schools currently offer, what services offer and how we can develop to further support the students who are struggling with attending schools. Great consideration was given to the early stages of anxiety and highlighting the importance of having early conversations with parents when they begin to get concerned about students.
Dr Conroy, who was involved in the development of the workshops, emphasised the importance of
early intervention and collaborative support in tackling school refusal.
“By bringing together parents, schools and mental health professionals, we have created a proactive community that addresses the unique challenge of school refusal that teenagers face in today’s complex world,” she said
Feedback from early participants has been overwhelmingly positive, with many expressing gratitude for the opportunity to connect with other parents facing similar challenges and to gain practical strategies for supporting their children. Building on the success of the workshops, the service has developed follow-up programmes for teenagers, including a cognitive behavioural therapy group, a mindfulness group and a furniture upcycling group.

Some of the upcycling projects completed by the teenagers.
Ennis Hospital has just passed a major milestone in its continuing service development with the formation of the hospital’s first ever dedicated multidisciplinary team of allied health professionals.

also the complex needs of the individual during hospital stays.
The move complements Ennis’s existing physiotherapy team with a full-time dietitian, a speech and language therapist, two occupational therapists and a medical social worker, providing the hospital’s inpatients with access to a full range of allied health disciplines.
This will lead to more efficient and safer discharges or transfer of patients from Ennis Hospital, either to their homes or to community residential care, in line with clinical model of care criteria that emphasise the need to address not only the admitting diagnosis of the patient, but
Shirley Real, Allied Health lead, UL Hospitals Group, explained, “The benefit of full Allied Health teams in acute hospital settings arises from the requirement to address the total needs of the patient, and not just their acute illness. So there is an immediate benefit to patients in the hospital. Up to this point, only physiotherapy and dietetics was available in Ennis, so this provides more comprehensive support for their assessment, treatment, and rehabilitation, as well as planning for their discharge.
“Rehabilitation is core to the care of people, particularly in a hospital like Ennis, where patients tend to have an older age profile, and are likely to have needs that are more complex. Rehab ensures earlier discharge, and safer discharge, which in turn means that readmission becomes less likely.”
78 new beds promised for St John’s Hospital in Limerick City are to be fast-tracked and it is hoped the development will be completed ahead of the projected completion date of 2029/31.
Hospital CEO Emer Martin said that St John’s was committed to fast-tracking the development, with the completion of the business case in a matter of months, moving on then immediately to the planning process and design.
She paid tribute to the hospital staff for its continued dedication to delivering excellent care to the people of Limerick and the wider Mid West.
“We were delighted by the inclusion of our planned expansion in the national plan by Minister Donnelly and the HSE. This will ensure that the physical environment here at St John’s will match the incredible care delivered by our staff,” she said.
Ms Martin added that the project will also ‘make a huge contribution to the delivery of healthcare in the Mid West region as St John’s will more than do its share in the wider response to overcrowding here’.

‘I want to shout about BowelScreen from the rooftops!’
Mary Kennedy from Castleknock in Dublin was at the centre of the HSE’s campaign for this year’s Bowel Cancer Awareness Month. She wanted to talk publicly about her bowel cancer screening story to encourage other people to take part in screening.
Mary was 61 when she took her first BowelScreen test at home. “I’d heard about BowelScreen from radio adverts and from friends. When the letter arrived inviting me to take part I didn’t hesitate; BowelScreen is free and is another way I can look after my health.”
She had no symptoms of bowel cancer. “I was walking, swimming and enjoying my retirement. I wasn’t losing weight or fatigued, and I didn’t see blood when I went to the loo,” she said.
Less than two weeks after she had posted back her test kit, Mary received a letter from BowelScreen saying that her test result showed traces of blood that were not visible to the eye, and that a BowelScreen nurse would phone her to arrange a further test called a colonoscopy.
“About a month later I went for the colonoscopy,” said Mary. “This involved a thin, flexible tube with a small camera at the end that looked at the inside of my bowel. Later I was told that samples taken from my bowel during the colonoscopy showed I had cancer. To hear I had cancer, the ‘c’ word, was a real shock to me. It was a lot to take in. It took me a while to be able to say the word. It was such a whirlwind that I didn’t tell people until just
Mary is keen to encourage everyone aged 59-69 to choose screening. Her story appeared in several newspapers and online during Bowel Cancer Awareness Month. You can read Mary’s blog on screeningservice.ie


"I was walking, swimming and enjoying my retirement. I wasn’t losing weight or fatigued."
before my surgery. After further tests I met with my consultant who explained the diagnosis and what surgery would involve. There was support at every stage from the BowelScreen team.”
Mary had keyhole surgery to remove the cancer and, fortunately, didn’t need further treatment. “Even though I had cancer I feel so lucky. I’m so glad I chose to take the BowelScreen test, and my cancer was discovered early. I had a good experience with the whole programme. I’m so grateful for screening,” she said.
Mary wanted to share her story, hoping it would encourage other people to register with BowelScreen, and to take the test when it arrives in the mail. “I want to shout about BowelScreen from the rooftops,” she said. BowelScreen is one of the four screening programmes of the National Screening Service (NSS), which launched this year’s campaign with the message that it’s never too late to take your first test: “Whether you’re choosing screening fo the first time or have previously received a test kit but didn’t use it, make April the month you get in touch with BowelScreen. Or register online to find out more and take part.”
The NSS ran an advertising campaign on radio and social media, supporting people throughout the month to #ChooseScreening. The campaign gave information about what BowelScreen does, how common bowel cancer is, the symptoms of bowel cancer, and how to contact and register with BowelScreen.
BowelScreen was introduced in 2012 and offers free athome screening (FIT test) for bowel cancer to men and women aged from 59-69.
The latest National Cancer Registry of Ireland (NCRI) data shows:
• The rates of colorectal cancer in men have shown a significant downward trend of 2.5% per year following the introduction of screening, with a smaller but still decreasing trend (0.3% per year) in women since 1994.
• The proportion of cases diagnosed with early-stage cancers (Stage 1 and Stage 2) is much higher in screened men (64%) and women (62%) compared to non-screened age groups of men (37%) and women (39%).
• There has been a significant decreasing trend in mortality over the 1994-2019 period and particularly noticeable in the 70+ year male age group.
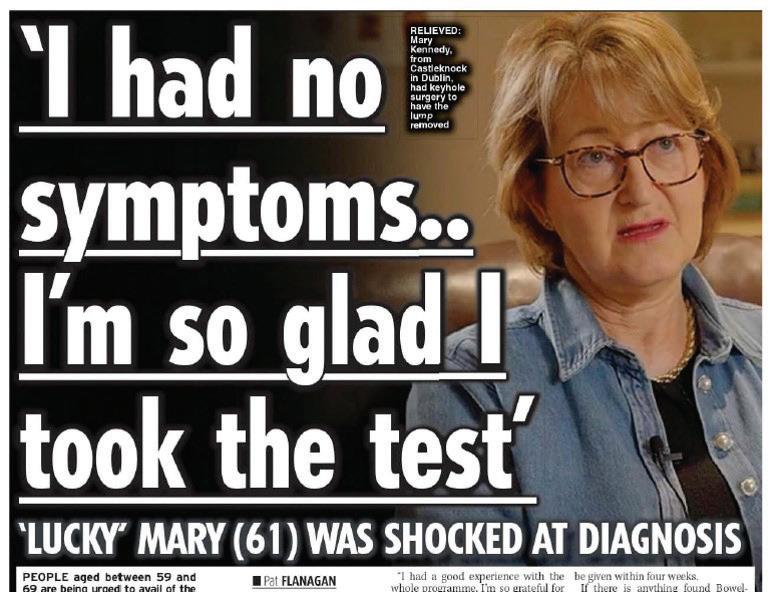
“I do think that local-based decision-making is key to all of this and empowering staff to be able to do that.”
There should be no serious obstacles from implementing the vision of the health regions, according to new Dublin and North East REO Sara Long.
“It’s a highly evidence-based vision, it’s a great vision for staff and for service users so there shouldn’t actually be anything that deters us from the delivery of that vision,” she said.
The REO explained that while the sound vision for the regions should ensure its success, the challenges will come in the transitional period.
“As with anything, it is important to manage the change and the transition and that is probably the challenging time. But it is about working with people and communicating with our staff, our patients and people who accesses our services to get through it together,” said Sara.
Sara recently took up her new role, coming from the Education Authority in Northern Ireland, where she was Chief Executive. She previously enjoyed an extensive career within Health and Social Care including management posts in both acute services and community care across the Western Health and Social Care Trust, most notably as its Director of Performance and Service Improvement.
Sara has extensive experience in overseeing reforms and transitions. She worked on the processes to bring together acute services and community services under five NHS Trusts in the North based on geography in 2007, so is very experienced in overseeing transition.
“I have experienced health and social care from a number of angles, and really enjoyed the experience," she said.
"In addition to my role in bringing together the acute and community services under five NHS Trusts, in my time with the Education Authority I oversaw a major improvement programme and improvement journey.
"When I saw the REO post and everything that was happening in terms of integration,
population-based health, with a focus on the health outcomes, it really felt like a wonderful opportunity to be able to come and contribute to delivering that reform agenda,” she explained.
“Key to the transition is planning and preparation. For me, it is about communicating and making sure that everyone knows what is happening. Like all things, it is about people: taking people with you on the journey.
"It is about the patient, ultimately, and putting the patient right at the centre and making sure that everything that you do makes sense for the patient and that there is no unintended consequences from structures that actually
“The key to a successful transition is preparation and planning.”
make things more difficult for patients and service users, not less.”
Sara said her goals for year one are familiarising herself with the people and services in the region and building up working relationships to drive the change forward.
“It is important that I establish myself and make those connections because if we are going to be genuine about working collaboratively and in partnership throughout the regions and back and forth with the centre, with those big partners, then it is really important that I take my time in the first year to put my energy into building and growing and developing those relationships and getting to know people,” she said, adding that a priority will be getting her own team in place on the ground.
"I have already met some of the staff working across community and hospital services in the
region and I look forward to meeting more over the coming months," explained Sara.
“We need to start to see and feel a bit what this integration is going to mean. Okay so it’s a long-term project and it won’t all be completely nailed, we won’t have it all right, but we definitely need to have something that signals that clear move and that clear step towards integration, in managing the change through in the first year.
"The new IHA structure will be key to this. What we don’t want to do in the middle of all the change is to make any backward steps and I think that is really important.”
The vision she has for the Dublin and North East health region over the next 10 years is for the population-based health to be firmly embedded.
“The big thing for the 10-year vision is around the population-based health outcomes and we are only starting that now. That is probably something that we would want to see the dial shift slightly on in that first year even if we haven’t got it all cracked.
"The vision for population-based health is that the needs of the population drive the service delivery, they drive the decision-making around service developments and funding, and that you are able to develop services specific to your population and ensure that their needs are being met.
"That will have to be delivered in an integrated way and in 10 years, you would like to think that there are networks of care, there are clinical networks and there are linkages between them and that the patient or people living in the region can move freely between them and can do so at their own local level.”
The new REO assured staff that they will be empowered at a local level under the health region structure.
“I do think that local-based decision-making is key to all of this and empowering staff to be able to do that," said Sara.

"All the evidence will tell us that change that is owned and managed by the teams that deliver it is the most successful change, and that highly developed and highly performing teams are those that produce the best outcomes for patients.
"It is about harnessing and enhancing that at a local level and really getting that right that we can enable and empower staff to do that."
At the end of the day, she explained, the ultimate benefit from the changes is improved health outcomes for patients and for everyone who accesses our health and social care services.
“Integration is about making the services easier to navigate and making sure the people who need to access services gets the right care right place right time and combining that with the population health based approach.
"That is all important but that is still just about the process. If we are going to get serious about population-based health, then we must see an improvement in the health outcomes for the patient,” added Sara.
The new building for Ballybay Primary Care Centre is expected to be complete by autumn 2025.
Proposed services that will be delivered from the primary care centre include GP services, public health nursing, social work, occupational therapy, psychology, physiotherapy, counselling services, speech and language therapy, community intervention team, dietetics and a smoking cessation service.
The total HSE area of the Ballybay PCC is circa 13,350 sq ft and is designed across three floors.
The lower ground floor will consist of bookable rooms for HSE services, a large adult therapy area and an adult treatment room. This floor is also made up of HSE ancillary facilities such as store
rooms, communication rooms, cleaner’s stores etc.
The ground floor will consist of clinical rooms for HSE services including public health nursing and bookable rooms for other services. This floor will also have a group education and training room, parent and baby room and a children’s therapy area. The ground floor will also contain the main HSE waiting area and HSE reception.
The first floor will feature administration accommodation and will also include staff welfare facilities such as the staff canteen, WCs and staff changing area.
Josephine Collins, General Manager Primary Care, Community Healthcare Cavan, Donegal, Leitrim, Monaghan, Sligo, said “The new centre is part of the ECC programme, which aims to enhance and increase community health services and reducing pressure on hospital services. The new centre will offer these services to people in the local community making access to healthcare as convenient as possible.”
MISE Day Services in Monaghan has been shortlisted for the category 'Day Service of the Year' in the National Healthcare Awards 2024. This category examines how a service provides community integration and active citizenship within the local community to the attendees of that service.
The decision to apply for the National Healthcare Award was made by the people who access their day service supports at MISE (the Irish for me) Day Service so they could showcase their great service at a national level.
MISE is a day service for adults with intellectual disabilities located in the Diamond Centre, Monaghan Town. There are a total of 13 people who attend this day service.
There are two staff employed at the day service.
MISE Day Service strives to enable the people using the service to make their own choices in planning and developing their own day services. MISE Day Service provides opportunities such as working with the local County Council, Cavan/Monaghan Education and Training Board, National Learning Network, Advocacy projects and Employability services.
MISE Day Service commenced one-to-one outings for individuals attending the service. Four events were scheduled in March, including a trip to Dublin Zoo, a day trip to the Comic Book Convention, a train trip to visit to the Dublin museums and a Drogheda shopping trip.




Dublin and North East Regional Green Committee, tasked with overseeing the implementation of the ambitious HSE Climate Action Strategy 2023 to 2050, has been launched.
Approximately 100 people from across the healthcare sector in the Dublin and North East attended the event in the City North Hotel and Conference Centre in Gormanston, providing a valuable opportunity for information sharing, networking among teams and building momentum to move forward with Climate Action Strategy priorities.
Some 33 posters from staff in Hospital Groups, Community Healthcare Organisations, Section 38 and 39 agencies and the Community and Voluntary sectors were displayed showcasing the many initiatives being undertaken across the DNE region.
The event was attended by Dublin and North East Regional Executive Officer Sara Long who said it was heartening to see so much good work was already going on across many areas and that the launch would act as a catalyst to drive the strategy forward at a regional level.
“This event marks the first step in our implementation of the Regional Green Committee which is tasked with driving the strategy forward

Mellany McLoone, Chief Officer, CHO DNCC; Peter Smyth, Assistant National Director, Capital and Estates; Sara Long, REO, Dublin and North East; and Kevin Sheridan, Project Manager, Capital and Estates.
in a collaborative and integrated way in our sites across Dublin and North East. We have a real opportunity to achieve progress towards these targets. The good news is that the actions that are taken on this journey can be clearly measured and evaluated, so we will know what progress we are making,” she said.
Nominations will now be sought from across the sites in Dublin and North East to join the Regional Green Committee with the expectation that the first meeting will take place at the end of June.
The posters can be viewed at this link: https:// publuu.com/flip-book/439574/1121744
A second cohort has completed the Multi-Disciplinary Leadership Programme - Embracing New Ways of Working, which is run in conjunction with the RCSI. The participants came from across all services in CHO DNCC as well as Section 38 colleagues.
This second programme focused on those who provided services to the following Networks: Cabra, Clontarf, Coastal, Kilbarrack, Finglas and Swords as well as some employee with a cross CHO remit.
The programme is underpinned by the work of Professor Michael West and his book: Compassionate
Leadership: Sustaining Wisdom, Humanity and Presence in Health and Social Care.
The group was extremely lucky to have Professor West attend on the day. He spoke to how impressed he was with the work of the groups and how they have shown the tangible benefits of Compassionate Leadership in Healthcare. Organisers would also like to express thanks to Caroline and Tina from RCSI for their experience and expertise. Also thanks to Angela Hughes and the National ECC programme for the ongoing support in the running of the programmes.
Cavan, North Dublin, Louth, Meath and Monaghan.
makes things ‘a little less lonely’ for visitors
Making Memories Café in Whitehall is flourishing and providing a lifeline into society for many older people in the Dublin city suburb.
The community-led initiative was officially launched in May, but opened back in September.
The café, which is open to service users on the last Tuesday of each month, is run by local volunteers, many of whom have had family members affected by dementia or Alzheimer’s. They have guest speakers who come to give a brief talk on relevant topics for attendees and everyone is more than welcome.
It was first set up following huge demand of an existing café led out by Advanced Nurse Practitioner in Mental Health Regina Lafferty in Naomh Barrog.
“Our partners in the Alzheimers Soceity of Ireland (ASI) were advocating that such a service would flourish in Dublin North Central (DNC). DNC serves one of the oldest population demo graphs nationally with nearly 50% of recipients of HSEfunded home support living in the area are living with a cognitive impairment or dementia,” explained Niamh Martin, CNM2 Primary Care.


“Driven by a desire to provide a meaningful educational resource for the community, myself and Amanda Wilkinson [CANP Mental Health] joined forces and set up a committee with key stakeholders in the community.
“The committee involved the GAA (Whitehall Colmcille’s), Larkhill Credit Union, ASI, persons affected by dementia and Dublin City Council. This collaboration, both across HSE sectors and NGOs, has led to the successful establishment of this resource in the community. This initiative runs on goodwill of a partners - the GAA donate the premises, a local business woman - Celine from Couverture Cakes - donates cakes on a monthly basis for free, and the HSE Mental Health services supported with the initial set up costs, such as crockery and equipment.”

At the launch, Norma Gill, whose father Harry suffers with dementia, described the café as a safe space to meet others with similar experiences, a space that made everything “a little less lonely” for her mother Pauline.
“On a day-to-day basis, you wouldn’t get to meet people like that,” she said, adding that the experience has been “powerful and special”.
The 2024 Making Every Contact Count (MECC) Champion event took place in the Lecture Hall, St Mary’s Hospital, Phoenix Park recently.
The MECC Champion initiative is organised by Health and Wellbeing in HSE Community Healthcare Organisation Dublin North City and County (CHO DNCC) and began in 2023 to support healthcare professionals in completing training and implementing MECC in their practice.
This year, 43 healthcare professionals from across CHO DNCC have taken on the role of MECC Champion and will work to support the implementation of MECC in their teams. The MECC Champion event brought the network of MECC Champions and the local HSE Health Promotion and Improvement Officers together to share experiences, build relationships and celebrate successes to date.
The MECC Champions were welcomed to the event by Ellen O’Dea, Head of Service for Health & Wellbeing in CHO DNCC, and Bríd Greenan, MECC Mobiliser for CHO DNCC before a video celebrating the achievements of the initiative in the past year was shown.

Aileen Convery, MECC Champion and physiotherapist in the Blakestown Community Healthcare Network, presented on the MECC Lifestyle series project delivered in the area in collaboration with the local HSE Health Promotion and Improvement Officer. This project consisted of a monthly event for staff themed around one of the MECC lifestyle topics to encourage them to complete the eLearning module on that topic.
A panel discussion also formed part of the event, chaired by Roisin Lowry, Health Promotion and Improvement, Health and Wellbeing Manager CHO DNCC. Panel contributors included Denniele Vicente, Physiotherapist, Cabra Network, Navan Road Primary Care, and David Creed, Prevention Coordinator in North Dublin Regional Drug and Alcohol Task Force. Two service users one from St Joseph's Mental Health Intellectual Disability Service and another from the Dublin North West Integrated Care Centre gave an account of the positive impact the implementation of the MECC programme by staff has had on their health.


For more information on MECC or the Champion initiative in CHO DNCC, please contact Bríd Greenan at brid.greenan@hse.ie.
The survey included the experiences of people who received care or died in various settings

The HSE welcomed HIQA’s findings of the National End of Life Survey 2023. It is the first national survey of its kind, providing important insights into patients’ end of life care experiences across Ireland. The survey results are on www. yourexperience.ie
A detailed response report, ‘Listening, Responding and Improving’, was also published by the HSE in the publications section of www.hse.ie. This report outlines the work under way to address the issues highlighted in the survey.
In total 4,570 bereaved family members and friends participated in the survey. The findings showed that almost 74% of participants rated the care that their relative or friend received at the end of their life as ‘very good’, 15% rated it as ‘good’, while 11% said that their relative received ‘fair’ to ‘poor’ care. The survey included the experiences of people who received care or died in various
Back: Elizabeth Kinsella, Patient and Service User Experience (PSUE); Cara Regan Downey, PSUE; Gavin O’Dowd, Department of Health; Tracy O’Carroll, HIQA. Front: Aileen Killeen, patient representative; Edel Mulligan, PSUE; and Zara Dagg, HSE End of Life co-ordinator, Midland Regional Hospital Group.
settings. The most common place of death was a hospital (39.4%), followed by a nursing home, home and hospice. The people who died experienced a variety of pathways of care involving multiple care settings and services in the last months and days of their lives.
The most positive ratings of overall care at the end of life were from bereaved relatives of people who died in a hospice, with almost 94% of people rating the overall care that their relative or friend received in a hospice at the end of their life as ‘very good’.
Participants highlighted positive experiences across several areas of care, including the respect and dignity with which their relative or friend was treated and the standard of care provided by staff. The survey found that most
"Participants highlighted positive experiences across several areas of care, including the respect and dignity with which their relative or friend was treated and the standard of care provided by staff."

Aileen Killeen, patient representative; Joe Ryan, HSE National Director, Patient Service User Engagement; and Zara Dagg, HSE End of Life co-ordinator, Midland Regional Hospital Group.
participants had confidence and trust in the healthcare staff who were caring for their relative or friend, and felt that they explained their relative or friend’s condition and care in a way that they themselves could understand.
However, the survey also identified several areas where care could be improved. Issues that were highlighted included the continuity, availability and responsiveness of care, timeliness of care and support for emotional needs. For example, 23.9% of participants answered ‘no’ when asked if there was good coordination between the different services and staff that cared for their relative or friend in the last three months of their life. Some participants also felt that their relative or friend did not get help from healthcare staff as soon as they needed it.
Bernard Gloster, HSE CEO, said, “Improving the experience of end of life healthcare services is a key priority for us. This survey provides valuable information and important insights across our services in hospitals, hospices, nursing homes and the community. It lets us know what is working well, such as hospice care which is rated highly, and also, perhaps more importantly, the areas where we can and must improve.”
The HSE response report outlines how a range of quality improvement plans are already under way both at national and local levels across all care settings. These include;
• Hospice Friendly Hospitals, a partnership with the Irish Hospice Foundation, which aims to improve end-of-life care in acute hospitals which is underpinned by the Quality Standards for End-of-Life Care in Hospitals.
• Caru, a continuous learning quality improvement programme developed by the Irish Hospice Foundation and the All Ireland Institute of Hospice in partnership with the HSE available to all nursing home staff across Ireland.
• Care of the Deceased Guidelines - all of the expected practices hospitals and care settings should follow when caring for someone who has died, is in development and due for publication later this year.
• Implementation of the Assisted Decision Making Capacity Act – to ensure everyone is supported to make their own decisions about their end-of-life care as far as possible.
• Development of three new hospices in Drogheda, Tullamore and Cavan to ensure every region in the country has access to hospice care.
• The HSE has worked in collaboration with the Department of Health and HIQA in developing design guiding principles that will align new community nursing units to national policies and standards. For patients this will mean a reduction in the
use of multi-occupancy rooms and an increase in the provision of more communal social spaces, following best practice in the delivery of end of life care.
Dr Feargal Twomey, Clinical Lead, HSE/RCPI National Clinical Programme for Palliative Care, said, “As a normal part of living, dying, death and bereavement will affect each of us and those close to us at some stage. The experiences of the care that the HSE provides before and at the end of a person’s life have a huge impact on each person and those close to them, both around the time of the person’s death and during the grieving process for those who survive them.
“We welcome and support the first National End of Life Survey and the vital feedback provided by bereaved family members on the care received by the person close to them who has died.
“While it is encouraging to hear reports of the good care people received, the HSE hears the views of and acknowledges the impact on those people who had a poorer care experience. We are sorry that not every person received the care they should have.
“I can provide assurance that the HSE is developing and will continue to develop general and specialist services to ensure that into the future we will provide the best levels of palliative care, end of life and bereavement care for people who need them across all care settings.”
The National End of Life survey is part of the National Care Experience Programme – a partnership between the Health Information and Quality Authority (HIQA), the HSE and the Department of Health.



The Green Team at St Fintan’s hospital teamed up with Portlaoise Tidy Towns recently for a visionary project which saw the planting of trees and hedgerow for biodiversity improvement on the campus.
The staff-led Green Team (pictured above) meets regularly

to identify and implement sustainability enhancement and energy efficiency improvements within the campus. It is supported by the regional HSE Capital and Estates Sustainability and Energy Officers.
Working with Brian Gaynor of the charity Trees on the Land,
who supplied the trees for planting, and some of the day service users from the campus, staff volunteers planted over 240 native trees and over 160 metres of native hedgerows across three locations on the campus over the course of the day.
There was great comradery on the day and the team managed to exceed the expectations of the day by planting all the provided trees and hedging by early afternoon. Everyone - staff, service users and external experts - all came together to dig and plant, towards the shared ambition and worked great as a team.
Once properly established, the trees and hedgerows will add to the biodiversity of the site providing food and shelter for insects, birds and other animals.
St Fintan’s is one of 15 pilot sites in the HSE Capital and Estates Green Spaces Pilot Project. As part of this project, they are developing a site specific Green Spaces Action Plan, and from these pilot projects the HSE will develop guidance for healthcare facilities who want to improve their green spaces.

The project is in line with the HSE Climate Action Strategy 2023-2050 which has clearly stated objectives on the future treatment and use of green spaces. The strategy is to improve biodiversity and optimise the use of green space for the promotion of health and wellbeing of patients, staff and local communities.
“I go home happy every day knowing that I’ve made somebody’s life a little bit better,” according to Paula Curran, Health Care Assistant (HCA) working in the Day Centre for Older Persons in Clonskeagh Hospital, Dublin. Paula has been in her role for a number of years and really enjoys her work. “On average, on a weekly basis here, we would see between 75 to 80 clients –different people every day. Working as a Health Care Assistant I love making people feel happy. I love being able to do things for them. We work very well as a team here in Clonskeagh.”
Explaining how the HCA is a key member of the team, Dr Nichola Boyle, Consultant Geriatrician at Clonskeagh Hospital, said, “The work of the HCA is important in the multidisciplinary care we provide. They complement the work that the nursing staff do in terms of the social and emotional support provided to the clients. They provide a link between the community and the centre for the clients.”
For Maureen Mullen, a client at the Day Centre, Paula’s role is a vital part of her daily routine: “I love it here – it’s somewhere to go and they are all very nice.
Paula Curran
Paula’s so good for doing our hair and our nails and she keeps us all going all day.”
Paula said she would encourage anyone thinking of becoming a Health Care Assistant to ‘go for it’.
“I would really strongly advise them to pursue it. It’s just so good to interact with older people here. Older people need us and it’s such a rewarding job. I go home happy every day knowing that I’ve made somebody’s life a little bit better.”
Acknowledging the great work done by Paula and the many other
Health Care Assistants across the country, Anne Marie Hoey, HSE Chief People Officer, noted that HCAs constitute 14% of Health Service workforce and work across many sectors.
“They are an integral part of the multidisciplinary team and contribute towards providing patient centred care. I acknowledge the work that has been carried out through the Health Care Assistant project to roll out the recommendations of the Review of Role and Function of Health Care Assistants report.
We have recently reviewed and issued updated job specifi cations for HCAs and information is now available at https://www.hse.ie/eng/ about/who/healthbusinessservices/hbshumanresource/patientclient-care-health-and-social-care-assistants.html
“When I look back in five years’ time I would like to be able to say that we actually made a difference to the health of the people that are living in our region,” explained new West and North West Health Region REO Tony Canavan.
“And I don't mean that in a general way. I mean that when we look at our cancer services that we can see that there are measurable improvements in the survival rates and the outcomes for people that have cancer in the West and the North West.”
The very experienced new appointee has spent most of his working life within the health services, joining back in 1993. His most recent role was as CEO of the Saolta Hospital Group. He has firm goals in the short, medium and long-term for the new health region.
“The short term from now until the end of September is to get the health regions management team in place and there’s a bit of work going on around that. That is an important building block,” explained Tony.
“In the medium term, access is going to be one of the key priorities: access to emergency care, access to elective care, and access for services like our cancer services or even access to community disability services and so on.
“In the longer term, it is then about trying to make a kind of sustainable and meaningful improvements in the health outcomes for people living in the region.”
He said the biggest challenges will be around working in an integrated way and working in partnership.
“On the hospital side, we've done reasonably well over the last 12 years in integrating the hospitals across the West and North West. They work well together and they see themselves as functioning as part of a wider network.
“But there’s still 14,000 people that leave our region every year to receive care elsewhere.
Those people should be receiving that care within our region, so there's more work to do on that front.
“And then we also need to integrate our hospitals with our community services. There’s a big body of work to be done to ensure we're providing people with care and more appropriate setting that we're not as reliant on hospital care for and for all of those services.
“They allow us to generate that local decision-making local autonomy and ownership. It leads to a more sustainable health service.”
“The other big challenge within that is integrating within community services themselves. There’s still a big divide between primary care, for example, and mental health or big divide between primary care, mental health and disability services, and social care. So there's a further degree of integration that needs to take place between those services to ensure they function more effectively together.”
He said that once the focus is consistently on the quality of care and every argument you make is rooted in improving the quality of care that is provided, then people will come on board with the changes.
“We are constantly looking at our geography and how we provide a high quality of care. Each decision focuses on delivering the right
are in the right place. In doing this we might not win everybody over on every decision but we will see enough people come on board to allow us to make meaningful and sustainable change.”
He insisted the patient is the ultimate beneficiary when the structure allows for decision-making to be made regionally and locally.
“If you bring decision-making closer to where patients receive care and you improve the timeliness of it, you also improve the relevance of the decisionmaking. If you do the opposite, if you push it over to a central approach, you achieve the exact opposite. It becomes more and more and more disconnected from services.
“It’s that connection between decisionmaking and where people receive care that's important. It allows people living in our region to start to take ownership of their care. They don't see the health services as some remote thing that happens and is decided upon somewhere else but something actually that takes place within their own communities, and it's something that they can contribute to as well.

“If you bring decision-making closer to where patients receive care and you improve the timeliness of it, you also improve the relevance of the decision-making."
“That’s what I think is the real promise of these new structures. They allow us to kind of to
generate that local decision-making, local autonomy and ownership. It leads to a more sustainable health service.”
He insisted that staff will see a major improvement in how they are able to carry out their work and care for their patients under the new structure
“People in the health service want to do a good job and they believe that the way to do that is to first of all be clear about what they're trying to achieve and to be given the autonomy then to get on with it and to do the job that they're trained to do. I think the new structure will deliver that,” he concluded.
Portiuncula University Hospital and Community Healthcare West have introduced the new ‘Getting to Know What Matters to Me’ communication passport for people living with dementia.
The communications passport is a resource designed to reduce communication barriers and enhance the overall experience for people with dementia who utilise both hospital and community services. It can also be adapted to suit any individual who has difficulty communicating.
The Dementia Quality Improvement Committee at Portiuncula University Hospital implemented the initiative in response to recommendations outlined in the Irish National Audit of Dementia Care in Acute Hospitals Report.



Sharon Donoghue,Emily McElroy, Paula Noone, Angela Donnellan, Paula Daly, John Brennan, Anita Blake, Siobhan Coen, and Maura O'Connell at the passport launch.
The aim of the passport is to assist an individual who is receiving professional care and is unable to effectively disclose information about themselves, especially if they have special requirements or preferences.
The person, along with their family or carers, are asked to record information in the communications passport that will help them communicate, such as their personal history, likes and dislikes, important people or places in their lives, and normal routines and abilities.
Saolta University Cancer Network are delighted to have progressed to the next stage of accreditation with the Organisation of European Cancer Institutes (OECI). The OECI programme is considered internationally as the gold standard for cancer care. It focuses on enabling a complete quality system for cancer diagnosis, care, education and research.
By participating in this prestigious accreditation process, the Saolta University Cancer Network has committed to ongoing quality improvement in cancer care through research, innovation, partnership and patient empowerment.
The Saolta cancer programme provides a wide range of cancer services to a population of 830,000 people across the west and north west. In line with the national model of care, complex care is located
at University Hospital Galway with satellite centres delivering care closer to home in Letterkenny University Hospital, Sligo University Hospital, Mayo University Hospital and Portiuncula Hospital.



Dr Manvydas Varzgalis, Tony Canavan, Professor Maccon Keane, Geraldine Cooley, Professor Michael Kerin, Olive Gallagher, Dr Joseph Martin, Dr Gerry O’Dowd, Dr Andrew Hodgson,
Sandra
Burke, Senior OT; Ruth Dwyer, CNS Older Persons; Nicola Crean, ANP, Older Persons; Dr Gerry O’Mara, Consultant Geriatrician; Kate Donlon, ANP, and Hazel Cooney, Senior Physio.
The Roscommon Frailty Intervention Team (RFIT) have received the President’s Award for the Best Poster Presentation at the annual conference of the Irish Gerontological Society as well as Best Platform Presentation at the British Geriatric Society (BGS) autumn meeting in Glasgow.
RFIT is a unique, fully staffed, clinical service which was introduced at Roscommon University Hospital three years ago to provide a holistic assessment and brief intervention to patients over 65 presenting with frailty.
The team is led by Consultant Geriatrician Dr Gerry O’Mara and consists of an advanced nurse practitioner in frailty, senior physiotherapist, senior speech and language therapist, senior dietitian and senior occupational therapist with access to clinical pharmacy and medical social work.
Dr O’Mara and his team received the President’s Award for the Best Poster Presentation at the annual conference of the Irish Gerontological Society for their poster entitled, ‘Falling, Forgetting and Wetting - Normal Pressure Hydrocephalus; A disease made for Frailty Clinics’.
The team then went on to be awarded Best Platform Presentation at the British Geriatric Society meeting for their presentation entitled, ‘The Patient is the Expert of their Experience’.
Dr O’Mara said, “Our goal is to keep older people out of hospital and help them maintain their independence. Because of the team's multidisciplinary nature, we can provide expert assessment of gait, functional and cognitive ability, speech or swallow disorders, and nutritional concerns in one session.”
The sod has been turned on a new €14 million 12-bedded in-patient unit at the North West Hospice.
The HSE-funded new build will comprise of an extension to the current building to include a 12-bedded unit (12 single rooms) as well as outpatient facilities. The existing in-patient unit will be refurbished to house the Palliative Care teams.
Patients will have access to their own bedrooms in this new state-of-the-art build, which will increase their dignity and privacy and benefit their families. The project aims to be complete by the end of 2025. The clinical services at North West Hospice provide palliative care services for people with life-limiting illnesses where they are residing, be that at home, in a nursing home, hospital or in its hospice.
Palliative care involves meeting an individual and assessing their needs and those of their families, spiritually, physically, socially and emotionally. These needs are then addressed with the aim of improving quality of life for the patients and their family. In order to provide this care, North West Hospice has a team of professionals including doctors, nurses, social workers, physiotherapists, occupational therapists and chaplaincy services.
North West Hospice Manager Nuala Ginnelly said, “This development is essential to meet the current and future needs of patients and families in the local community. We would like to reassure people that services will run as normal during the period of construction.”
HSE Community Healthcare West and the Department of Health launched a landmark report entitled: ‘The Pilot Implementation and Evaluation of the interRAI Family Carer Needs Assessment’, in Tuam, Co Galway.
The report was the culmination of a three-year project that piloted an internationally validated instrument that assesses the support needs and health and well-being of family carers.
This was the first time the Carer Needs Assessment form was tested in Ireland, which was made possible by Government funding received under the Dormant Accounts Fund. Family carers
and health and social care professionals from across HSE Community Healthcare West and many voluntary agencies attended the event.
Speaking at the event, John Fitzmaurice, Chief Officer, HSE Community Healthcare West, thanked the family carers and the health and social care professionals who participated in the pilot programme and said: “The process of systematic assessment ensures family carers are identified and recognised, acknowledges their right and entitlement to access supports, have their own needs documented and responsive actions taken to meet those needs.”.
The National Ambulance Service (NAS) has made a significant investment in training and equipping islanders on Arranmore Island off the coast of Donegal.
A group of volunteer islanders recently received Emergency First Responder Certificates from NAS at a special presentation held on the island. The event also marked the delivery of a new ambulance vehicle to the island to replace an older vehicle.
Emergency First Responder Group leader John McCafferty and his team of volunteers received their certificates from John Joe McGowan, NAS General Manager Operations – West.
Speaking at the presentation, Mr McGowan said, “I am delighted to be here and to be able to present Emergency First Responder Certificates to John McCafferty and the group. They are making a real difference on this island and the National Ambulance Service is delighted to support them and all their work as First Responders providing assistance to their fellow islanders and visitors to Arranmore when they need it. They are a very valuable resource and deserve great credit for their efforts.”



He also said that the provision of a new ambulance on the island was very welcome and that it was a valuable resource for the entire community.
In addition Dermot Monaghan, Chief Officer, Community Healthcare Cavan, Donegal, Leitrim, Monaghan, Sligo was present to give details about the provision of an Emergency Care Information Sheet which has been distributed to every home on the island.
Mr Monaghan said the information sheet contains important resident and visitor medical emergency information for people while they are on the island.
The Community Healthcare West (CHW) Cultural Harmony project ran from October to December 2023 as a result of funding awarded through Healthy Ireland Staff Health and Wellbeing and Creative Ireland. The project involved engaging with a diverse group of staff from across CHW to explore the music and song of their culture and to record a number of pieces of music to be played in healthcare settings across the region.

music was added to enhance where appropriate. The result was an 18 track CD/MP3 file which is currently being distributed to CHW venues to be played in public waiting areas.
The first output of the project involved three engagement sessions with participants from a variety of countries. In addition to this, a further engagement session was held with Western Traveller and Intercultural Development which deliver the Traveller Primary Healthcare Service in conjunction with the HSE in Galway.
Once the engagement sessions were held, recording sessions were held locally to facilitate staff.
Once all the recordings were complete, the tracks were mixed and mastered and accompanying
The project proved to be extremely successful as it engaged participants from a range of cultural backgrounds including Ireland, Nigeria, South Africa, Sudan and India, along with musical representation from Ghana, the Philippines, South America and Sri Lanka to name but a few.
The resulting musical track provides a mix of Irish music and music representative of a range of cultures which echoes the service users who access the services of CHW and will be listened to in the waiting areas.
Patients seeking treatment for the respiratory conditions COPD and asthma have seen their hospital waiting lists cut dramatically as a result of the new Integrated Care Hub in Galway.
Where once patients would face waits of up to three years to access services, the Integrated Care Hub, funded by HSE Enhanced Community Care, is ensuring full access to services within a matter of weeks.
Dr Sinead Walsh, Respiratory Consultant and Respiratory Lead for the Galway City Integrated Care Hub, welcomed the new services as a major step forward in reducing wait times for patients. “This has been an absolute game changer for patients. Previously they were waiting a number of years to even access a respiratory specialist. Now they know they’ll be seen within a number of weeks,” she said. Since commencing the consultant-led diagnostic clinic in a community setting, almost 250 patients
have been reviewed by Dr Walsh and her integrated respiratory specialist team in various community locations throughout the county. GPs refer directly to the integrated respiratory clinic, thereby avoiding the acute hospital waiting lists.
Noel Downes has been accessing the hub for his asthma since last summer. “I’m asthmatic and have been for the last 15 years. It has been an excellent service. I’ve been able to have one-to-one service with the professionals. Just the convenience of being able to come out here as well with the traffic and the anxiety about parking at the main hospital.”
During their visit, patients can also meet with one of the respiratory nurse specialists at the hub, such as Phillipa Needham. “My role here is to ensure patients fully understand their diagnosis following their consultation with the consultant. I go through the patient’s treatment plan in detail. I also answer any questions they might have," said Phillipa.
For the month of February, 12 different Emergency Departments competed in the increasingly competitive Ireland’s Fittest Emergency Department challenge.
Staff from across the country clock the kilometres they have walked, ran, cycled and swam. All activity is recorded on strava, then calculated into points, with a weekly national scoreboard published. This is a fun challenge, but also a great way to encourage staff to spend more time outdoors.
There were 72 on the winning Tallaght University Hospital ED team, with representatives from the nursing, medical, healthcare assistants, administration, phlebotomy, physiotherapy, social work and occupational therapy disciplines taking part. The competitive streak was real with increasing urgency to get more kilometres on the clock and stay ahead of the competition!

The competition is just three years old and this year was TUH’s second time to enter, having missed out narrowly last year coming in second place. There was a collective determination to win this year. Working in such a busy department, the challenge was wonderful for staff morale. The competition created a great atmosphere and was a wonderful way to get to know colleagues. Every grade and discipline took
Senior Dental Surgeon Dr Adrianne Dolan has been named the Colgate Caring Dentist of the Year.
A special needs dental surgeon, Dr Dolan was nominated by the parents of her patient Emily (11), who has Sturge-Weber syndrome, a neurological condition which makes her prone to life threatening conditions.
“To be recognised as a caring dentist is an acknowledgment of the commitment that I, along with the incredible teams in HSE and in my area Dublin South West and Kildare West Wicklow, have to the patients. I must recognise the important role played by my dental surgery
assistant, Margaret Curran and the support over the years of Drs Louise Dockry, Siobhan Doherty, Ann McKeon and Barney Murphy and Dr Gillian Boucher-Hayes and my colleagues who take on a lot of the emergencies to allow me to have time for children and adults with additional needs. We have amazing nurses, senior nurses, hygienist and clerical staff and it is this collective effort that allows us to provide the level of care that has led to this award,” she said.
Dr Dolan has been caring for Emily since she was very small. She sees Emily, who also has sensory issues making dental treatment challenging, every six months.
part; it really was a team effort. The team battled wind, rain and snow each week to get the kilometres in to earn those precious points! Encouraging one another along the way it was also a great way to form some healthy habits.
Congratulations to all of the team that took part. In the end it was a tight margin with the team winning by 185 points. Every kilometre really did count!
However the empathy and caring nature of Dr Dolan allows Emily gain confidence and comfort in the dental chair. She was described by Emily’s mum as ‘kind, professional, witty, caring and engaging’.
“Every day, I have the opportunity to make a positive impact on the lives of my patients, and this is such a rewarding experience. My journey as a dentist has been incredibly fulfilling, and it's a privilege to have been nominated, let alone win, this award. This award isn’t just a recognition of my efforts but a testament to the collective commitment to compassionate dental care provided by all nominees,” she said.
The HSE’s National Service Plan (NSP) 2024 was published on 13 February. It sets out a partnership approach to the type and volume of health and social care services to be delivered by the health service in 2024 within the allocated budget of €23.5bn which is 4.6% above last year’s budget. The NSP for 2024 is a continuation of the work of the preceding year and represents another year of growth. Together, the two years will see the number of staff increase by +9,000 WTE.
The NSP is guided by the primary considerations of the Programme for Government, the priorities set by the Minister for Health, Sláintecare and the component plans resulting from that policy. In addition, NSP 2024 which is the final year of our current Corporate Plan, continues to move the HSE towards the fundamental goal of universal healthcare. This is in line with the ambitions of Government including the Partnership Principles (April 2023) and the HSE Health Regions Implementation Plan (July 2023).
The focus of NSP 2024 is on the public need as it relates to:
1. Delivering urgent and emergency care
2. Addressing waiting lists and times to deliver equitable, timely and transparent access
3. Enhancing mental health and disability services
4. Managing our workforce who are fundamental to delivering care across our country
5. Ensuring value for money in the provision of high-quality healthcare infrastructure















In 2023, we continued to work to address challenges in our health and social care system, particularly in relation to access. Significant progress was made on change and reform in the health service to improve the experience and outcomes for the people we serve, including commencement of the establishment of six new operational Health Regions, a process expected to be complete in 2024. This restructuring, coupled with the change in size, purpose and function of the HSE at national level (the Centre), aims to deliver services that are:
• Integrated, locally planned and delivered
• Easier to access and navigate for patients and their families
• Available closer to patients’ homes when they need them – right care, right place, right time
Partnership, collaboration and integrated working has to become ‘the way we do our business’ to ensure delivery of quality, person-centred care. Our planning recognises and seeks to respond effectively to significant, long standing challenges that exist within our health and social care service, by working smarter together and making the best use of investments already within our system.
NSP 2024 is the first National Service Plan which required the approval of both the Minister for Health and the Minister for Children, Equality, Disability, Integration and Youth, following the transfer of functions in respect of disability services to the Department of Children, Equality, Disability, Integration and Youth.
If you would like further information on the National Service Plan, please contact the National Strategic Planning Team in the Office of the Chief Strategy Officer at planning.ddg@hse.ie or telephone 021-4923531. The National Service Plan is available at: https://www.hse.ie/eng/services/publications/serviceplans/hse-national-service-plan-2024.pdf
Extensive coordinated service planning occurred across the HSE to ensure the affordability and deliverability of our NSP 2024 in light of the significant challenges presenting a complex context that requires careful monitoring and management.
Addressing waiting lists and times: We will continue to deliver equitable, timely and transparent access.
• The multiannual Waiting List Action Plan will reduce and reform waiting lists, spanning acute and community settings beyond urgent and emergency care.
• Activity targets in the areas of inpatient, day case, outpatient and GI scopes have been increased by 5% on the 2023 outturn
Delivering urgent and emergency care: While our urgent care services are delivering more care to more patients each year, this has resulted in services being under pressure almost all year round.
• The HSE Board is overseeing a multiannual Urgent and Emergency Care (UEC) Plan 2024-2026 as part of a new UEC programme that is focusing on what is working well
• In 2024, the HSE will improve access to urgent and emergency care by implementing the year one commitments of the new multiannual UEC Plan related to the four pillars of priority focus: hospital avoidance, emergency operations, in-hospital operations and discharge operations
• In parallel, longer-term enabling programmes will add much needed capacity, an increased number of GPs delivering care to our population and key digital requirements for integrated care Community: The Enhance Community Care Programme (ECC) will continue to roll out nationally to ensure more people can access healthcare in their local community rather than within the acute hospital
setting. These measures will include:
• Delivery of over 141,000 patient contacts through 28 Integrated Care Programme for Older Persons community specialist teams, and over 228,000 patient contacts through 28 Integrated Care Programme for Chronic Disease community specialist teams
• Completion of up to 240,000 community radiology tests alongside up to 161,000 tests across areas such as echocardiography, spirometry and natriuretic peptide blood tests, totalling over 400,000 tests
Mental Health:
• Our focus is on prioritising child and adolescent early intervention, enhancing early interventions for adult mental health services and improving access to personcentred mental health services
• Targets for mental health services are in excess of those set for 2023 with the target for the number of children and adolescents to be seen in 2024 25% higher than the 2023 outturn.
Disability:
• An extensive and ambitious programme of work is ongoing to improve timely access to services, including in the areas of day, respite, multidisciplinary, residential, home support, neuro-rehabilitation and personal assistance services.
Investment:
Core revenue budget allocated to the HSE for 2024 is made up of €20.7bn provided by Department of Health and €2.8bn provided by Department of Children, Equality, Disability, Integration and Youth in respect of specialist disability services.
Included in the budget is €162.8m additional investment to focus on areas of high-priority need:
• €56m Access and Capacity
• €13.6m Better Services
• €29.1m Workforce and Reform
• €64.1m Disabilities
of all attendees at emergency departments aged 75 years and over to be discharged or admitted within six hours of registration
of children aged 24 months to have received the MMR vaccine
of new patients to be accepted onto the nursing caseload and seen within 12 weeks
inpatient and day cases to be discharged
women in the eligible population to have had a complete mammogram
personal assistant service hours to be delivered to adults with a physical and / or sensory disability
home support hours to be delivered to persons with a disability
child and adolescent mental health referrals to be seen by mental health services
home support hours to be provided to 54,100 older people
persons to be covered by medical cards
Every change brings fresh opportunities for our health services, says new REO
Throughout her career of over 30 years in health service leadership, Martina Queally has been involved in and led healthcare reform. She is excited and enthused by the latest restructuring that the health regions will bring. Every part of the journey, she insists, has brought the Irish health system to where it is now.
“Sometimes people cynically say that we are going back to the future. We’re not. Every part of our journey has brought us to where we are now. Every iteration of the system has brought with it an opportunity to learn,” she said.
The HSE Dublin and South East REO said senior managers such as herself who have overseen previous changes have a responsibility to carry forward the things that work well.
“It’s not just out with the old and in with the new. It’s about seeing what works well and bringing that with us to the new system. Equally a health organisation is a living organisation, it has to change and adapt because our demands are increasing and changing. We need to have a system that is dynamic and agile.”
Martina has decades of experience in the HSE, with particular expertise in strategic change management in public services and integrated service delivery. Since 2015, as Chief Officer in HSE Community Healthcare East, she has led the planning and delivery of all community health services in South Dublin and Wicklow, a range of national programmes, and a combined HSE and voluntary workforce of 4,000 staff.
Her clinical background is as a nurse, midwife and public health nurse and she counts herself lucky to have found a career that she loves.
“I work hard but it is very enjoyable and rewarding. I am passionate about what I do and absolutely committed to delivering better healthcare. I started with a very simple goal when I was a nurse and that was to help people. To this day my ambition is to improve healthcare services for the public. I’m a qualified coach and
in coaching they always say that if, in your job, you are following your own values then you will have a more positive experience,” she said.
“I took various turns in my career that led me to gain a depth and variety of experience, both clinical and management. This experience has given me a valuable insight into the healthcare system, its challenges and the opportunities that now present.”
Martina is a firm advocate of the triple aim of high-performing health systems as outlined by the Institute for Healthcare Improvement.
“It’s not just out with the old and in with the new. It’s about seeing what works well and bringing that with us.”
“It has three domains. The first is patient experience – timely, effective, efficient, safe and equitable healthcare which is the mission of Sláintecare. The second domain is per capita cost. We have finite resources which we have to make the most efficient use of We all need to be cost conscious. A sustainable model for the people we serve is important,” she explained.
“Population health is the third domain which represents the best money we can invest in healthcare. If we can be really effective in the area of prevention: supporting people to improve their health, making healthier choices easier and looking at health as a societal issue – housing, education and equity, how we organise our society - we can have a real impact.”
She said a fourth domain, healthcare team
wellbeing, was added to the framework in 2014.
“There is strong evidence that if we mind our workforce and are a compassionate employer we have a much higher quality service,” she said.
“This involves creating the best possible environment for our staff to operate in. We have a very educated and committed workforce. Obviously we are in a very competitive marketplace so retaining our staff is a real challenge. Undoubtedly, the health service provides multiple opportunities for professional development, upskilling and career progression. As an organisation the HSE strives to support staff to achieve their career goals in a workplace which is fulfilling and meaningful.”
She stressed that getting the right management structure in place is an immediate priority, in addition to making sure the transition does not impact negatively on service delivery.
“The establishment of the regional management team and operational construct must support and drive the service improvement and service redesign that is required. A high performing health service needs the correct management design,” she said.
“The vision and principles of Sláintecare are ambitious but achievable. Sláintecare reform is transforming how we deliver healthcare in Ireland, putting people at the centre of the health system and developing primary and community health services. I am absolutely focused on optimising the opportunities presented by the establishment of the region and transforming health and social care services - ensuring that the right care is delivered in the right place and at the right time” she said
Martina recognises that one of the biggest challenges encountered during healthcare reform is maintaining services while concurrently introducing change. Strong, stable and visible leadership along with an engaged and enthusiastic workforce are critical success factors

to assure stability during significant structural reform.
An immediate priority for Martina is addressing the current pressures on scheduled and unscheduled care. An ageing population along with an increase in complexity of care continue to place unprecedented levels of demand on our existing health service delivery model. There is an absolute requirement to design, scale up and implement a sustainable and fit for purpose model of service delivery.
She highlighted the need for improvements in ICT and digital infrastructure. “For a modern workforce that is expected to be efficient, effective, timely and fast paced, we need to really accelerate the digital and ICT innovation to support our staff to do their best work and to operate at the top of their licence,” she said.
Martina concluded, “During the last few months, I have met with staff and teams across the region. The unwavering dedication and commitment I see from staff across all areas, day after day, continues to fill me with immense pride. I am excited to be on this journey in healthcare reform and look forward to the next steps in this journey.”
The six-month milestone in the development of cardiac care services in the Co Wexford area was marked with an open day hosted by the HSE’s Integrated Cardiology Service for Wexford in the Enniscorthy Primary Care Centre.
In addition to a display of items tracking the history in development of cardiac care services in the county, including its latest phase in integrating with community healthcare services, the HSE’s Quit team of Stop Smoking Advisors were also invited along to be part of the presentations.
The open day was an opportunity to showcase work such as the Integrated Community Cardiac Rehabilitation Programme and Lipid Clinic in community healthcare services locally.
The Integrated Cardiology service is a new initiative of the HSE, under the Sláintecare plan for Enhanced Community Care. Patients are referred by their GP or practice nurse to a service which includes a consultant or nurse specialist-led Cardiology clinic and newly launched Community Cardiac Rehabilitation programme. The Cardiac Rehabilitation programme, now operational in the Enniscorthy Primary Care Centre, is an expansion of the service originally established in Wexford General Hospital in the early 1990s.
These new services reflect the Sláintecare vision of
providing the right care, in the right place, at the right time. Services are led by Dr Cyril James, Consultant Cardiologist, Integrated Care, Wexford General Hospital and South East Community Healthcare, with additional clinical services provided by his team of clinical nurse specialists, physiotherapist and cinical psychologist further enhancing access to essential cardiac services throughout Co Wexford.
In addition to Dr James, those to address the gathering in Enniscorthy on the day included Consultant Physician and former Clinical Director of Wexford General Hospital Dr Colm Quigley, who has been supporting the roll-out of the integrated service.



In applying the learning from the results of the staff survey 2023 and using the 9 behaviours of Values in Action (ViA), a series of management engagement and culture improvement events have been planned for Community Healthcare East
Despite positive progress, it is also clear that there are areas for improvement and a key purpose of the sessions is to find out how the participants would like to influence the approach to building a more positive and patient-centred culture. A core component of the sessions is to work towards identifying interventions that will improve the working
environment for our networks and teams.
The first of these Culture Engagement ViA sessions took place in April. This initial event, run by HR in partnership with the National ViA Team, captured feedback to help shape the roadmap to enhance the culture as we move into a period of service transition. Improved communication and more frequent engagement with senior management was a recurring theme, which positively reinforces the need to follow through with more engagement sessions and ultimately deliver on the identified recommendations. It is planned to take the next sessions out into the service areas.
The new Respiratory Pulmonary Function Testing (PFT) Lab in the Bray Integrated Care Hub aims to further integrate hospital and community respiratory care to provide patients with advanced diagnostics and streamlined healthcare pathways. GPs in the area can now refer patients directly for pulmonary testing in the community, reducing waiting lists for respiratory consultants and allowing testing faster and closer to home.

Dr Alessandro Franciosi, Minister for Health Stephen Donnelly meeting with Rachel Anglin, in the newlyestablished Pulmonary Function Testing (PFT) Lab in the Integrated Care Hub, Bray
The local respiratory team collaborated with colleagues in St Vincent’s (SVUH) to establish a network link between SVUH, St Michael's Dún Laoghaire and the Hub’s IT systems. Results from the PFT Lab in Bray can now be accessed remotely by hospital consultants who review the
Information sharing and collaboration are key components of work to reduce tobacco use in the Dublin and South East region. With this in mind, stop smoking advisors in Community Healthcare East established a Tobacco Stakeholder Engagement Group last year that brings together those working hard on the ground in our communities and hospitals to make a tobacco free
test findings and provide a comprehensive report to the GP. The service has been in operation in Bray since January. To date, 333 patients have been assessed. 32% of patients haven’t required further input, while 37% of patients were referred onto a respiratory clinical nurse specialist in the community. ability, speech or swallow disorders, and nutritional concerns in one session.”
Ireland a reality. The goals of the group are to:
• improve dialogue and communication between stop smoking stakeholders
• increase support for the services provided by stakeholders that relate to smoking cessation
• increase confidence for referring across services. The first Tobacco Stakeholder Engagement Group meeting for Dublin and South East took place in October 2023. Community and hospital-based HSE colleagues, along with community organisations and national charities were invited, with over 20 in attendance on the day; demonstrating the level of interest in this work amongst stakeholders. Another successful meeting was held in March 2024 and the group look forward to more insightful and impactful meetings in 2024.
The fifth annual East Coast Area Diabetes (ECAD) Programme study morning took place earlier this year. The theme was ‘Moving Forward with Integrated Diabetes Care’.
Professor Ronan Canavan, ECAD Programme Chair, and Martina Queally, as REO of Dublin and South East, spoke at the event. Tributes were paid to the late John Fennell, former HSE Primary Care Manager, for his work laying the foundation for the current Enhanced Community Care and Chronic Disease structures.
Keynote speaker, Dr Soon Song, NHS Consultant Diabetologist and Physician, spoke about ‘Supporting Young People Living with Type 2 Diabetes’.
Other presentations included Chronic Illness Rehabilitation and Exercise, Perinatal Care in Diabetes, the Role of Continuous Glucose Monitoring in Integrated Care, Enhanced Community Care in Practice,

and Language Matters in Clinical Interactions Around Diabetes and Obesity.
Special thanks to Professor Ronan Canavan, Dr Lisa Devine, Dr Gráinne Ní Ghairbhí and Pamela McCann for their role in planning the event.
Southside Travellers Action Group and their partners in Community Healthcare East launched a documentary about the hugely successful Wagon Project. The launch took place in the Lexicon Library in Dun Laoghaire. The 10-minute documentary was produced by students from the Dun Laoghaire Institute of Art, Design and Technology.
The Wagon Project was instigated by two Traveller men who wanted to pass on the custom of building a traditional barrel top, old-style Traveller wagon to the younger generation. Led by Southside Traveller Action Group (STAG) through a Men’s Shed programme, the project developed into a thriving cross-sector initiative with many services coming together to offer their support and expertise. The initiative was supported by the Resource Officer for Suicide Prevention, Traveller Mental Health Coordinator and Health and Wellbeing from HSE Community Healthcare East.
Other partners included the Children and Young People’s Services Committee (CYPSC), Healthy Ireland, Hazel House Café and Woodwork School in Tribradden, Tusla, Dún-Laoghaire Rathdown County Council, and the Institute of Art, Design and Technology (IADT). The aim of The Wagon Project was to promote positive mental health among Traveller men and young Travellers through culturally appropriate means.
Watch the documentary on The Wagon Project here: https://youtu.be/bC4eBiV9Ay4
Eoin Morrissey, Waterford CCC; Agnes McDermott, Waterford GAA; and Connecting for Health Lead Tracy Nugent with Waterford hurling stars Tadhg de Búrca and Jamie Barron, and manager Davy Fitzgerald.
The Connecting for Life team in HSE/South East Community Healthcare is delighted to welcome the launch of a signage initiative across GAA clubs in Co. Waterford, in which ways that you can mind your mental health and the promotion of HSE funded services are available if you need to access support. The signage was developed in collaboration with Healthy Waterford, Mental Health Ireland and the Waterford GAA Health and Wellbeing Committee. Speaking of the initiative at the launch, Agnes McDermott, Waterford GAA Health and Wellbeing Committee, said that each of the 51 clubs across Waterford City and County will receive a sign with clear mental health messaging and information on

the key supports available. The signage will also be displayed in the two county grounds, Walsh Park in the city and the Fraher Field in Dungarvan, as well as in the SETU Sports Arena in Carriganore, Waterford. Tracy Nugent of the HSE Regional Suicide Resource Office and lead for Connecting for Life, the HSE Suicide Prevention Strategy, emphasised the importance of including the steps for accessing support and the key 24/7 services. These services are there whenever they are needed, day or night and so they are the relevant ones for people to know. Where appropriate, these national services signpost to local services and are often the first port of call for someone in distress.
Sheryl John, Clinical Specialist Speech and Language Therapist, and Paula Koechlin, Senior Counselling Psychologist, North Wexford Child and Adolescent Mental Health Services (CAMHS) team sought to enhance young people with moderate to severe mental health difficulties through participation in a creative arts group. They successfully applied to the Creative Communities Programme to run an eight-week Creative Arts Group. The Creative Communities Programme is funded through Wexford County Council’s Art Office and the Creative Ireland Programme.
The group met in Arnold House, Enniscorthy for two hours a week over eight weeks during the summer holidays. Two visual artists, Deirdre Travers and Sonya Weston, and two CAMHS clinicians were present. There were 19 participants aged 14 to 17 years. The participants learnt new art mediums including lino printing,
mono printing, collage, painting which was then published in to a book.
Outcome measures showed that 80% of participants’ overall score had improved at the end of the group and they had fewer internalising and externalising symptoms. They also indicated reduced anxiety levels, reduced discomfort talking in a group setting and improved confidence.
Parental feedback was very positive and 100% would recommend attending the group. Parents reported improvements in their child’s mental health, including in confidence, openness to trying things in school and reduced stress. They reengaged in art activities as a coping strategy. The young people attending the creative art group reported improved mental health outcomes. This group highlights the importance of partnerships in delivering health care that is person-centred and cost effective. The team look forward to developing partnerships with other agencies.
The first Diabetes in Pregnancy (DIP): A model of care for Ireland (2024) was launched recently.
This model of care (MoC) was written by experts by experience (women who experienced diabetes in pregnancy) and experts by knowledge (members of the clinical multidisciplinary team). The importance of person-centred individualised care and the multidisciplinary team are themes throughout the document.
The working group was expertly chaired by Prof Fidelma Dunne and Prof Mary Higgins. The virtual launch received significant interest, with 488 attendees and positive feedback.
The impact of DIP for both mother and baby can be farreaching. We now understand that children born to mothers with diabetes have an increased lifetime risk of diabetes and obesity and may also be at increased risk of neurocognitive dysfunction. Mothers with pre-gestational diabetes (PGDM) may experience worsening of diabetes-related complications (retinopathy and nephropathy)
because of pregnancy. While those with gestational diabetes mellitus (GDM) have an increased lifetime risk of type 2 diabetes mellitus and cardiovascular disease. This MoC is designed to support standardisation of care for PGDM and GDM, irrespective of geographical location and encourage best clinical practice.
Implementation of the MoC is in progress. Women with GDM have been added to the successful Prevention Programme arm of the Structured Chronic Disease Management Programme in
General Practice. Since 1 January 2023, all individuals who receive a diagnosis of GDM and/or preeclampsia during pregnancy (estimated 7,000 women in Ireland a year) are eligible to join this programme, regardless of whether they have a medical card or are private patients. Joining this programme entitles each individual to an annual review with their GP to identify their risk factors for diabetes and cardiovascular disease and to develop a personalised care plan to address these risks.
Self-Management Education and Support Programmes for Pre-Diabetes and Type 2
Type 2 diabetes (T2DM) is a preventable medical condition for many people. International evidence shows people at risk of developing T2DM who follow a structured lifestyle intervention programme may reduce their risk of disease progression by up to 60%.
The HSE has created selfmanagement education and support (SMES) programmes for people most at risk (pre-diabetes
diagnosis) and those with new or existing T2DM.
The SMES programmes are evidence-based, quality-assured and have been created in partnership with people living with the conditions. SMES programmes recognise that the most important person, in the care of these conditions, is the person living with them. A person living with prediabetes or diabetes requires time
and support to understand what the condition is, how to treat and manage it and the serious nature of the condition if not treated. Programmes are available inperson or online. Participants gain knowledge, skills and confidence to engage in behaviour changes to benefit their health. They learn how to self-care and treat the condition in partnership with their GP and health care teams.
The National Screening Service (NSS) has developed a new eLearning resource about diabetic retina screening for health and social care staff. This 15-minute module is available on the HSE learning portal HSeLanD. It was developed to help health and social care staff to identify people who are eligible for diabetic retina screening, explain the screening journey, and support people in their care to take part in Diabetic RetinaScreen.
Specifically, the new eLearning module provides information about:
• the screening journeyregistering patients, the screening tests and screening results
• supporting access to screening, including those with language difficulties and accessibility needs
• diabetic retinopathy, and talking to patients about reducing the risk of developing this serious eye disease
• the limitations of diabetic retina screening
• useful resources including leaflets, videos in multiple languages and easy-read materials.
The resource has been created for use by GPs, diabetes nurses, practice nurses, dieticians, podiatrists, primary care staff, health promotion staff, and anyone who has an interest in diabetes care. The module is available to staff in Ireland within the hospital and community setting in the HSE, in the voluntary hospital sector, and in associated non-government organisations working in health or allied services.

It is a legal requirement for the undertaking to ensure that all staff are appropriately trained and competent to work with medical ionising radiation. Numerous in-house training programmes have been developed by individual radiological services, based on international guidelines. These courses in radiation protection vary in content and duration, depending on the cohort of staff in attendance and their level of occupational risk to exposure. Clinical staff who attend these sessions may often have to attend similar training programmes delivered in other locations when they change employment throughout the year. This repetition is an unnecessary burden on local radiation protection teams and a misuse of time for the clinicians.
Clinical staff who attend these sessions may often have to attend similar training programmes delivered in other locations when they change employment throughout the year. This repetition is an unnecessary burden on local radiation protection teams and a misuse of time for the clinicians.
The National Radiation Protection Committee (NRPC) and the National Radiation Protection Office (NRPO) commenced the development of a suite of online training resources for radiation protection. The aim of this programme was to provide national standardised training information based on international guidelines, to support all staff in understanding the principles of radiation protection, how to limit their exposure and what to do in the event of something going wrong.
This national programme is designed to standardise training and promote safe practice. It will support the important work of local radiation protection teams however, it does not replace the need for more in-depth, onsite training for those at high risk of occupational ionising radiation exposure. Both modules are available on the HSeLanD platform. Certificates of attendance will be issued on completion of the modules and will be valid for a period of two years across all locations.
Work is continuing on key projects to support the reform of home support services and the establishment of a Statutory Home Support Scheme. Workstream membership includes staff from home support services, nursing and HSCPs that work with home support service users, their families and carers.
Home support care will be extended to adults over 18, allowing us to provide home support to people with physical or intellectual
disability, mental ill-health or frailty within our communities in their own homes.
HIQA standards for Home Support Providers will be developed to provide standardisation of care and parity for service users. This will provide additional support for staff.
A new HSE home support service operating model, co-developed with staff from across our services, will provide standardisation and quality assurance to home support care
workers and their wider teams.
The home support service ICT system will be service user-focused, automate work, reduce paperwork, support staff in case management, help with staff rostering and improve communication between staff and service users.
Staff will be provided with information and training to support them to work effectively in advance of regulation and the implementation of new ways of working.
The legislation was enacted in May 2023 and should officially take effect this summer. The aim of the Patient Safety Act 2023 is to further embed openness and transparency across the Irish healthcare system as it applies to private and public healthcare.
In part, it sets out the legal requirement for open disclosure when one of a list of 13 Notifiable Incidents occurs. Notifiable Incidents are defined and itemised in the Act 2023 and predominantly describe events where the patient or service user sadly died.
This Act builds on current Open Disclosure policy, which is being updated to align with it. Whilst the HSE is working towards standardising requirements to make it as seamless as possible to implement the Patient Safety Act 2023, there are some elements specific to open disclosure as described in it:
• The legal requirement for open disclosure applies to one of 13 Notifiable Incidents only. The HSE Open Disclosure Policy applies to all patient safety incidents.
• The health services provider must notify the relevant regulator within 7 calendar days from when one of the Notifiable Incidents is identified. This will be in addition to other regulatory reporting requirements, for example, reporting a Serious Reportable Event to the regulator. Where the Notifiable Incident is also a Serious Reportable Event then it needs to be reported via NIMS as a Notifiable Incident and as an SRE via the current reporting mechanisms.
• Reporting a Notifiable Incident to the regulator must be via the National Incident Management System (NIMS). For users of the system, such as HSE staff, they must
access the NIMS incident record and complete a form on the incident record page and submit that electronically to the regulator. This function is currently being built and will be ready for June 2024. For private providers, an electronic portal is being purpose built to enable Notifiable Incident reporting. The portal will be accessible through the relevant regulators website pages.
• The Act makes it a legal requirement to assign a designated person to support their relevant person throughout the open disclosure process of a Notifiable Incident. This is in line with current policy and adds weight to the importance of this role. A designated person is not only desirable but essential.
• The Act is specific as to what must be covered at an open disclosure meeting and within the written follow-up. This is being aligned in the HSE Open Disclosure Policy however, the Act requires that the written record following an open disclosure meeting is shared with the patient or their relevant person within 5 calendar days of the meeting.
• There are offences and penalties that apply to noncompliance with the Act, specifically when the regulator is not notified or an open disclosure meeting is not held as set out in the Act. Importantly, not undertaking open disclosure is detrimental in any situation, in particular where a patient or service user was harmed and may lead to compounded harm. It could be reputationally damaging for an organisation and lead to mistrust in the health services provider by the service user and their relevant person.
Further information on the Patient Safety Act 2023 and resources will be available on healthservice.ie/staff
Psychosis is a condition that affects the way the brain processes information. It affects 3% of the population. Psychosis is associated with an array of mental illnesses including schizophrenia, bipolar affective disorder and severe depression. There are often long delays between people starting to experience symptoms and accessing mental health care.
Early intervention in psychosis (EIP) services provide rapid access to expert assessment, a range of evidence-based interventions including medication, psychosocial, physical health, and vocational support. Evidence indicates that EIP services reduce relapses, improve outcomes and save the economy money. The Early Intervention in Psychosis National Clinical Programme, Model of Care was published in May 2019 and there are five EIP teams in operation in Ireland.
The National Clinical Audit of Psychosis in England, Wales and Ireland is run each year across all Early Intervention in Psychosis teams in England, Wales and, for the past three years, Ireland. The audit is conducted as a collaboration between Royal College of Psychiatrists and Health Quality Improvement Partnership (HQIP) in the UK. The audit standards are based on NICE guidelines for Early Intervention in Psychosis.
Ireland’s participation this year was part funded by the HSE Quality and Patient Safety Directorate and HSE Mental Health Operations. The findings demonstrate timely access to care and high rates of uptake of evidence-based interventions including
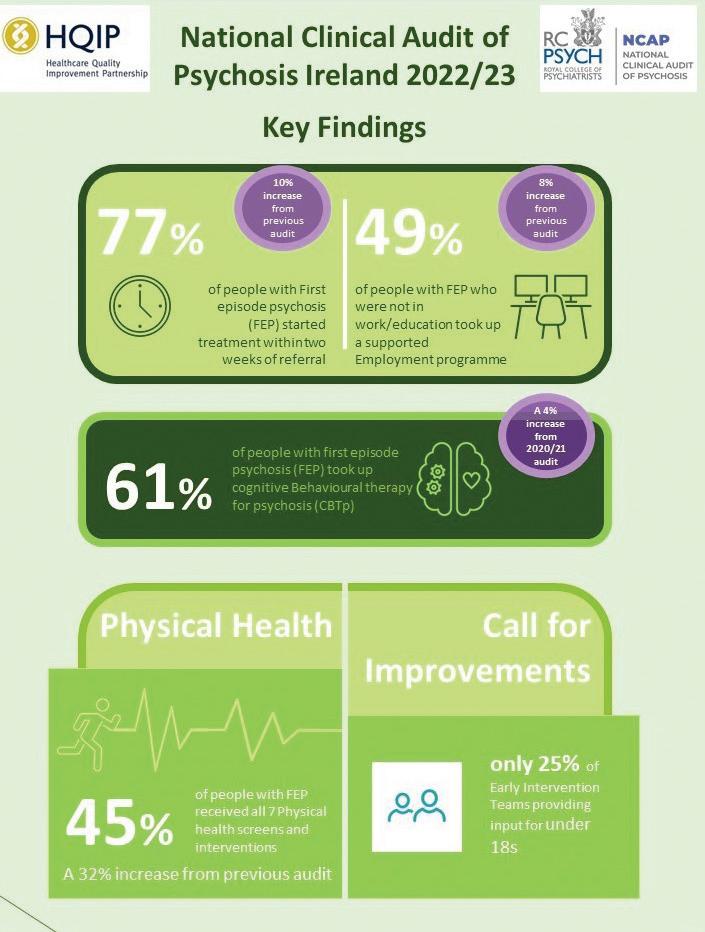
psychological interventions, employment support and family interventions.
People with psychosis die 15- 20 years earlier than the general population. The leading cause of ‘years of life’ lost in this population is disparities in physical health, such as cardiovascular disease. Once-off ministerial funding supported the introduction of Point of Contact Testing Devices to each of the EIP teams. This is likely to have supported the improvements of 32% seen in the physical health screening and intervention audit standard in 2023.
As part of the implementation of National Clinical Guideline No 21, a range of resources have been developed for staff and the public on the Resources for staff and the public on the appropriate prescribing of psychotropic medication for non-cognitive symptoms in people with dementia.
A prescriber information leaflet and a document to support comprehensive assessment. The prescriber information leaflet provides an overview of the recommendations and good practice points of National Clinical Guideline No 21, and additional information on comprehensive
assessment and signposting to additional resources and information.
An information leaflet for people with dementia and their family carers and supporters is available in a Plain English and Easy Read format. The leaflets explain what psychotropic medications are, when they may be prescribed, possible side effects, the importance of regular medication reviews and signposts to additional information.
A 30-minute HSeLanD module ‘Support pathways for people with non-cognitive symptoms of dementia’, is for all staff who provide care to people with dementia.

Sligo played host to health and social care colleagues from the HSE West and North West health region as they celebrated a significant milestone in the ‘Delivering Change Together’ programme. This experimental initiative, aimed at fostering collaboration and building the region's capacity for change, marks a pivotal moment as the area transitions to a new operating structure.
Led by the region's CEO and Chief Officers, the programme brought together diverse stakeholders from different services. It was designed as a multi-disciplinary effort, drawing upon the expertise of various disciplines.
At the heart of the programme was the Community of Practice (COP) model, employing action learning approaches to address common challenges encountered during change initiatives. Participants
engaged collaboratively within their COPs, sharing insights and problemsolving strategies across services and disciplines.
During the celebratory event, attendees had the opportunity to hear from representatives of the eight Communities of Practice, who shared their experiences and reflections on the Programme, both the positive and challenging insights.
HSE CEO Bernard Gloster expressed gratitude to participants for their dedication to improving services, emphasising the importance of locally-led innovation.
The newly appointed Regional Executive Officer, Tony Canavan, underscored the role of an integrated structure in fostering unity of purpose and connectedness within the organisation.
Participants expressed their enthusiasm for the journey ahead and Dermot Monaghan,
Chief Officer, noted the palpable commitment to embracing change and driving forward the health region’s agenda.
Moreover, as discussions unfolded, it became apparent that while much progress has been made, challenges lie ahead, particularly regarding the transition to local decision-making structures. However, there was resounding support among delegates for this transition, recognising it as a vital step towards delivering more effective and responsive health services to the community.
Looking ahead, the programme has set a precedent for future initiatives aimed at driving innovation and collaboration within the health and social care sector. Its success serves as a beacon of hope, inspiring stakeholders to continue working together towards a shared vision of improved healthcare delivery.
For more information on the programme you can email changeguide@hse.ie or visit www.hse.ie | Follow us on X @HSEchange_guide | LinkedIN page Health Services Change Matters

Sarah O’Brien, National Lead HSE Healthy Eating Active Living Programme, and Veronica Conti, Project Manager in the HSE Healthy Eating Active Living Programme, launch the new resource, alongside Gael Coman, age 4.
HSE Health and Wellbeing hosted a webinar on Effective Communications for Child Health and Obesity recently. It aimed to introduce different ways of communicating about child health and obesity to inspire support for solutions and a belief that we must take action as a society, instead of making people think about individual blame and crisis.
Sarah O’Brien, National Lead of the Healthy Eating Active Living Programme, shared insights from the complex systems map from the 2007 Foresight Report. This map illustrates the connections and interdependencies across home, community and society that influence the environments we live in and our overall health. In short, how what surrounds us shapes our health.
Sophie Gordon, Principal Communications Strategist at FrameWorks UK, provided a template for effective communications in child health covering:
• an introduction to framing and why it matters
• evidence-based, practical communication tips and advice for communicating about children’s health
• how to build understanding, and increase support for policies and programmes that will help children thrive
In addition, the webinar launched a new resource ‘Improving Children’s Health in Ireland - A communications guide for talking about child health and obesity’ that summarises the key recommendations, provides practical guidance, and includes examples of how to apply them.
A recording of the session is available to view on the HSE YouTube channel.
The HSE national Family Recovery Advisory Group and Maynooth University Centre for Mental Health and Community Research are jointly hosting a one-day in-person conference on 3 September to explore, develop and promote opportunities for ‘whole family’ policy and practices in mental health services in Ireland and across the world. This conference aims to be inclusive of the lived experience of mental health challenges and to support and empower both decision makers and those working with people with lived experience and their families/supporters.
Key topics to be addressed will include:
• the economic case for whole-family approaches
• overcoming the barriers to/challenges of a whole-family approach within existing services
• examples of international best practice in policy and implementation
• key areas to consider for family empowerment
• next steps for Ireland in terms of family-focused policy and practice
This conference is free and open to anyone with an interest in familyfocused approaches and practices within mental health services, including mental health professionals across all disciplines, families and individuals with lived experience of mental health difficulties, and academics and researchers with interests in the field.
For more information, please contact Dr Christine Mulligan at Christine.Mulligan@mu.ie
Every Move Counts - New guidelines aim to encourage people of Ireland to sit less
The HSE and Department of Health have recently launched the new National Physical Activity and Sedentary Behaviour Guidelines for Ireland, bringing Ireland in line with the World Health Organisations (WHO) recommendations on physical activity.
Many factors influence people’s ability and capacity to be physically active. While some of these factors such as access to affordable leisure opportunities, safe routes for walking and cycling are outside the direct control of individuals. There is a lot that individuals can do to be more active every day.
The National Physical Activity and Sedentary Behaviour Guidelines for
Ireland form part of a suite of policy documents that collectively aim to enable a systems approach to promotion and participation in physical activity in Ireland.
Speaking at the launch event, Professor Breda Smyth, Chief Medical Officer at the Department of Health explained, “We hope to encourage people of all ages around the country to prioritise their health and wellbeing by increasing their levels of physical activity. The more time spent being physically active, the greater the health benefits – even relatively small increases in moderate level physical activity can contribute to improved health and quality of life.”
The benefits of regular physical
activity, at moderate to vigorous levels, for our overall health are immense. It improves our heart health, reduces risk of developing cancer and chronic diseases such as type-2 diabetes, and can improve our mood and sleep.
In adults, higher levels of sedentary behaviour are associated with cardiovascular disease, cancer and type-2 diabetes. Sedentary behaviour would include most desk-based work, driving a car, and watching television or other screen time activities. Replacing this sedentary time, where possible, with activity, even light intensity activity – essentially moving more everyday – is also strongly advised to protect health.”

Key updates in the guidelines include:
• physical activity at moderate to vigorous levels can be accumulated across the week,
• replacing sedentary time with physical activity of any intensity, including light intensity, and
• an emphasis on including muscle-strengthening activity every week.
New recommendations for each age group include:
Infants aged less than a year should:
• be physically active several times a day in a variety of ways, particularly through interactive floor-based play
• not be secured for more than one hour at a time (such as prams or strollers, high chairs, or strapped on a caregiver’s back)
Children aged 1-2 years should
• spend at least three hours in a variety of physical activities at any intensity, spread throughout the day
• Not be secured for more than one hour at a time (for example, prams or strollers, high chairs, or strapped on a caregiver’s back) or sit for extended periods of time
Children aged 3 - 4 years should
• spend at least three hours in a variety of physical activities at any intensity, of which at least one hour is moderate-to vigorousintensity physical activity, spread throughout the day
• not be secured for more than one hour at a time or sit for extended periods of time
Children and adolescents aged 5-17 years, including those living a disability should
• do at least an average of one hour per day of moderate-to vigorous-intensity, mostly
aerobic, physical activity, across the week
• additional activities that strengthen muscle and bones, should be incorporated at least three days a week
• for some people with certain disabilities (for example, erebral palsy, muscular dystrophy) a reduced level of physical activity may be adequate to attain significant health benefits, considering their higher energy cost of physical activity
Adults aged 18-64 years, aged 65+ including those living with a disability
• at least two hours and 30 minutes to five hours of moderate-intensity aerobic physical activity; or at least one hour and 15 minutes to two hours and 30 minutes of vigorous-intensity aerobic activity throughout the week
• additional muscle-strengthening activities at moderate or greater intensity that involve all major muscle groups are recommended on two or more days a week
• as part of their weekly physical activity, older adults (aged 65+) and older adults living with a disability should do varied multicomponent physical activity that emphasises functional balance and strength training on three or more days a week, to enhance strength and capacity and to prevent falls
Limiting sedentary activity is also a key recommendation across all age groups and sedentary time should be replaced with any type of physical activity. Screen time is a very common type of sedentary activity, particularly screen time for young children and adolescents. Screen time includes time spent watching screen-based entertainment (TV, computer and mobile devices).
More information on the new recommendations is available here - follow the conversation online #EveryMoveCounts
Sarah O’Brien, National Lead HSE Health Eating Active Living Programme, said, “As well as regular planned physical activity such as taking part in sports, going to the gym, walking or cycling for travel and pleasure, we all need to be moving more every day, and cutting back on the amount of time spent sedentary. But we know how busy life can be for many. Simple ways to start incorporating more activity into day to day life could be walking to work instead of driving, taking the stairs instead of the lift, if catching the bus, get off a few stops early. Reduce the amount of time we spend on screens, whether watching TV, playing games or scrolling through social media on our phones. Instead of a cinema playdate bring the children and their friends to a local playground to run around and climb safely.
We welcome the newly updated guidelines and are hopeful that they will inspire more people to take those important steps towards a healthier future.”
The new guidelines for Ireland, bring national recommendations for physical activity in Ireland in line with the best evidence, adapting the WHO guidelines for the Irish context and now include specific guidelines for younger children and on sedentary behaviour.
The updated guidelines are primarily designed to support practitioners in health, social care, education, sport and exercise to understand and promote physical activity. As well as those working in planning, transport, community and economic development in local authorities. They also provide clear guidance and messages for people on the amount and types of activity they should be doing regularly to improve their health and wellbeing.”

The World Health Organization Arts and Health Lead, Christopher Bailey, visited Saolta Hospital Groups’ University Hospital Galway (UHG) as part of Creative Brain Week. The programme is run by the HSE in collaboration with Creative Ireland, the Arts Council and the Healthy Ireland Department of Health.
UHG was selected for this visit, given its long-standing and exemplary arts programme, which has been in place for over 20 years.
Creative Brain Week week provided an opportunity to explore innovations in areas of social development, technology, the arts, entrepreneurship, brain health and physical health. Integrating arts and creativity into healthcare and social development can have profound benefits for individuals and communities alike
Events like Creative Brain Week offer a platform for sharing knowledge and experiences, fostering innovation, and highlighting the connections between creativity, brain health, and overall wellbeing.
Sarah McCormack, HSE Healthy Ireland Lead, who manages the arts and health programme in the HSE, emphasised how important it is to engage and learn from leaders in the area of arts and health and to also showcase the work we are doing in Ireland, which is viewed as a world leader in this field.
“In partnership with the Department of Health, we are continuing to work with Creative Ireland and the Arts Council to expand arts and health across the HSE for the benefits of all – our patients, staff and visitors. A big thank you to Saolta Management and particularly Margaret Flannery for a wonderful showcasing of the arts and health in an Irish hospital setting.”
The first event of the Healthy Islands initiative took place on Tory Island, which is located 15km north of Donegal.
Islands, by their nature are remote and those living there may experience feelings of isolation and social disconnection. HSE Heathy Ireland Health and Wellbeing is providing €54,000 to 11 islands to support a suite of Healthy Islands initiative. The islands, which are off the coast of counties Donegal, Mayo, Galway and Cork, are receiving a share of this funding for initiatives they proposed based on the population of the island. Working in collaboration with Age Friendly Ireland, the island communities will implement various health-promoting projects and initiatives as part of the overall Healthy Ireland implementation.
HSE
The initial focus on Tory Island was to get feedback from the local community on their health and wellbeing needs. An information day, focused on community engagement, showcased resources and supports on quitting smoking, reducing alcohol consumption, healthy eating, mental health and physical activity. There was also information about the new Age Friendly Ireland Healthy Home initiative which aims to support people to live in their own home with dignity and independence, for as long as possible.
Throughout the day healthy food and refreshments were served, with local musicians providing entertainment.
For further information, please contact healthyireland@hse.ie


Join our Patient and Public Partnership network.

We want to hear from people of all backgrounds.
Be part of a strong volunteer network of people willing to share ideas and life experiences to improve our National Screening Service for breast, bowel and cervical cancer, and for an eye disease in people with diabetes.
No specific experience or time commitment necessary; training is provided. We can help if you have access needs.
Healthcare professionals are welcome to share this network opportunity with your patients.
Email: ppplead@screeningservice.ie
Web: https://tinyurl.com/PPP-NSS Help make our screening services better for everyone.




