





















































































































1 SunSmart innovation pilot scheme for school
2 Talking Point: HSE menopause policy
4 Steps to Health
5 Safe Harbour resources for bereaved children
6 What is: Children First?
8 Digital for Care - a look at continual digital innovation in our healthcare
13 Day in the Life: Tim Moynihan
14 Update from the Health Regions Programme Team
16 Update from HSE South West REO Dr Andy Phillips
18 HSE South West Health Region news and updates
22 Vaccines in the spotlight
26 Update from HSE Mid West REO Sandra Broderick
28 HSE Mid West Health Region news and updates
32 In Focus: My Medicines List
33 Celebrating National Breastfeeding Week
34 The Irish Language Act
36 Update from HSE West and North West REO Tony Canavan
38 HSE West and North West Health Region news and updates
42 In Focus: Managing records correctly
43 Spotlight on Climate Action
44 Rainbow Badge initiative
45 Alzheimer's Day marked with events
46 Update from HSE Dublin and South East REO Martina Queally
47 HSE Dublin and South East Health Region news and updates
52 Spotlight on procurement
53 Global health initiatives show HSE leading the way in co-operation
54 Spotlight on Screening
56 Update from HSE Dublin and Midlands REO Kate Killeen White
57 HSE Dublin and Midlands Health Region news and updates
62 Programme updates from across the health service
67 Patient safety
68 Update from HSE Dublin and North East REO Sara Long
69 HSE Dublin and North East Health Region news and updates
74 Events and conferences from across the HSE
78 Health and Wellbeing
80 Awards and accolades
Thanks to everyone who has submitted stories for this edition. If you would like to see your initiative or work featured, you can submit through our online form at https://www2.hse.ie/services/forms/health-mattersstory-submission.html
Creative
Welcome to the autumn edition of Health Matters.
We continue to highlight the great work being done in each of the six health regions. We also feature an update on the transition, with the Community Healthcare Areas and Hospital Groups to be stood down by the end of September.
In this edition, we again talk to the six Regional Executive Officers to catch up with their progress and priorities for the coming months. They each deliver a message to their staff as the organisation enters this new transition period.
We didn't exactly have a glorious summer, weather-wise, but that didn't stop the HSE teams up and down the country from getting their steps in while taking part in the annual Steps to Health challenge. We talk to one of the team leaders who reports that her band of newcomers to the challenge are already counting down to the next one.
Our main spotlight this edition is on Digital for Care. The publication of the HSE's Digital Health Roadmap has paved the way for digital health transformation in the health services.
One of the first projects will be the HSE app and it should become the main channel for people to securely access their health information and a range of services online.
Patients and service users will also see the benefits of the introduction of Individual Health Identifiers (IHIs). They will be crucial to a high-quality, safe and co-ordinated healthcare.
The Talking Point this edition is the very topical menopause policy that the HSE has adopted. It highlights the fact that the subject should no longer be taboo, particularly with 78% of the total health service workforce being female.
That's just a taster of some of the stories we have featured in this autumn edition.
Thanks to everyone who has submitted ideas and features for the magazine. I'm only sorry that we can't use all of the stories we get.
Joanne Weston Editor
Published by Ashville Media, Unit 55 Park West Road, Park West Industrial Estate, Dublin 12, D12 X9F9. Tel: (01) 432 2200 ISSN: 0332-4400
All rights reserved. Every care has been taken to ensure that the information contained in this magazine is accurate. The publishers cannot, however, accept responsibility for errors or omissions. Reproduction by any means in whole or in part without the permission of the publisher is prohibited. © Ashville Media Group 2024.






Transition year students in Castleisland Community College, Kerry were crowned winners of the Young Social Innovators 2024 for their skin cancer awareness project called the ‘Sun Smarties’.



Collaborating with the HSE’s Health Promotion Officers for Schools and Cancer Prevention, the school designed a four-step programme for other schools to follow to become a sun safe school. This included research with the whole school community, raising awareness through lesson plans and developing a sun smart charter.
Following their win, the school hopes to continue the project into the future leading other schools in
becoming ‘sun smart’. They are working with the HSE and the National Cancer Control Programme to become Ireland’s pilot school for their Sun Safe Programme.
The students were drawn to this project because skin cancer is the most common cancer in Ireland, with over 11,000 new cases diagnosed every year. This number is expected to double by 2045. This concerned them and they felt that education about skin cancer at a young age is key for prevention.






The winning students from Castleisland Community College.
Senior Health Promotion Officer for Cancer Prevention Shirley O’Shea was very impressed with the level of knowledge and research the students had carried out on skin cancer awareness.
“The project is really innovative and provides other schools with a model to implement into their own school based on very practical measures,” she said.
For more information about the NCCP Sun Smart campaign see, https://www.hse.ie/sunsmart


Dr Gráinne McNally, Chair of the Menopause Policy Working Group; Dr Colm Henry, Chief Clinical Officer; and Anne Marie Hoey, Chief People Officer. The Menopause Policy Working Group at the launch.
Menopause is a normal and healthy life stage. However, for some, it may not be an easy transition. There can be a wide range of symptoms which can vary in their severity and their impact on the individual and their working life.
Research has shown that the right approach and supports in the workplace, from both manager and colleagues, can improve the management of challenging symptoms. Having this support can enable employees stay in work and perform to their best. It is crucial that managers and colleagues understand the potential impact of menopause and know how to support these individuals.
Menopause is when a woman stops having periods completely. This is a natural part of ageing. Your periods stop due to lower hormone levels. This usually happens between the ages of 45 and 55. The average age in Ireland for a woman to reach menopause is 51. Yet, some individuals start to experience symptoms in their 30s or rarely even younger. You reach menopause when you have not had a period for 12 months.
Perimenopause is when you have symptoms before your periods have stopped completely. Symptoms can start up to seven years before your periods stop. Symptoms of menopause and perimenopause can
“Managers are not expected to be experts when discussing menopause. But they should have an understanding of menopause and of what supports are available to meet the needs of employees. They should also be open to having conversations with them.”
have a huge impact on a person’s working life and this needs to be acknowledged and supported. The Programme for Government 2020 made commitments to promote women’s health. This included an emphasis on women’s experience of health care and to support the work of the Women’s Health Taskforce. Menopause care was identified as a key action under the Women’s Health Action Plan 2022-2023. This plan commits to changing the approach to menopause care in Ireland. It also aims to increase public supports available to women before, during and after menopause.
The Civil Service Menopause in the Workplace Policy Framework was completed in October 2023. It provides an overarching structure to guide Civil Service organisations when developing menopause policies. It was in this context that the HSE Menopause Policy was developed through the Workplace
of the total health service workforce is female
At any one time the HSE could have approximately
of female employees within the age cohort of 45-55, when menopause usually happens
Health and Wellbeing Unit. This policy was launched on 10th March, 2024 by Dr Colm Henry, Chief Clinical Officer and Anne Marie Hoey, Chief People Officer. Two HSeLanD educational training modules have been developed to support the implementation of the policy. These include an information module for all employees and a manager’s module. The manager’s module outlines how to support employees who have symptoms that are impacting them at work. A dedicated HSE staff webpage
The Menopause Policy contains guidance for managers on how to have these conversations. It also outlines where to seek further support. This includes the Employee Assistance Programme and the Occupational Health service. Workplace adjustments are one area where managers may support employees. There are practical steps that can be implemented to support employees and lessen the impact of menopausal symptoms at work.
has also been developed. It outlines the policy and supporting resources, as well as signposting employees to relevant information about menopause and perimenopause. This includes their symptoms, possible treatments and other supports. The role of managers in supporting those experiencing menopausal symptoms is vital, not only for the person in question, but for their colleagues as well.
Speaking at the launch, Anne Marie Hoey said, “Menopause transition should be acknowledged in the workplace as a natural process and an employee should be able to seek support and discuss their experience of menopause openly.”
Managers are not expected to be experts when discussing menopause. But they should have an understanding of menopause and of what supports are available to meet the needs of employees. They should also be open to having conversations with them.
As we celebrate World Menopause Day on Friday 18th October 2024, the policy and eLearning training modules are now available to support our employees, as we make this positive change to open up the conversation about menopause in the workplace. In the words of Dr Colm Henry at the launch of the policy, “Talking openly, supporting and creating workplaces more attuned to people’s needs is simply a mark of confidence and strength in an entity such as the HSE.”
They can also be used to ensure that working conditions do not exacerbate symptoms. The policy sets out some examples of workplace adjustments for various symptoms of menopause. What is key is the conversation between the employee and the manager about how the symptoms are impacting them in work. And using that conversation to and explore workable adjustments to address the symptoms. It’s also
Specific research undertaken in 2021 to understand women’s experience of menopause in the workplace found that:
12% 43% 39% 22%
of menopausal women have given up work due to their symptoms
have considered giving up work due to their symptoms
have taken time off work due to menopause
have taken three or more days off work because of menopause
important to review these adjustments with the employee. The policy also gives guidance to employees on where to seek further external support. This includes:
• guidance on how to prepare for conversations with their local health provider
• signposting to treatment options
• links to lifestyle changes that may be helpful
• guidance on how to manage symptoms in work
Steps to Health 2024 was a great success this year with 1,117 teams and 8,441 staff participants registered for the challenge – this highest number of teams since the challenge began in 2017.
Over 1.75 billion steps were recorded on the Steps to Health app by teams from every county across the health services.
With over 79% of teams registered logging their steps and participating in the leader boards, 659 teams completed the challenge logging in their final step counts in week five.
The challenge is part of the staff health and wellbeing programme in the HSE encouraging staff to get up, get out and move more especially during the workday. It aims to help staff connect with colleagues and improve their health and wellbeing by being more active. Steps to Health encourages staff to not only take part but also to look at their activity levels and increase their physical activity beyond the five weeks of the challenge.
Teams are supported by a team co-ordinator and 95% of team co-ordinators reported they enjoyed it and would volunteer again.
The Steps to Health challenge has already made the team (pictured right) from Hospital One ward in Merlin Park Hospital in Galway happier and healthier and they are looking forward to the next one.
The hospital team, named Scrambled Eggs and Achin', walked wherever and whenever they could –they walked at work, up and down corridors, road, parks, beaches, bogs and hills, during work and when they were off.
“Some of us were lucky enough to count our steps while away in other countries like Italy, Tenerife and Portugal. One girl was on a Mediterranean cruise so she got her steps in by walking up and down the ship and also while the ship was docked in various countries in

“I enjoyed getting to know my colleagues a little more, we shared photos of our walks and adventures on the WhatsApp and we intend on keeping this up over the summer and sharing any local events in our areas,” said one.
The Steps to Health team would like to thank all the staff, teams and co-ordinators who took part in this year’s challenge and look forward to our 2025 challenge! We would encourage staff to get up and moving and keep stepping throughout the year ahead. Every move counts!
Visit www2.hse.ie/living-well/exercise/ for more information on being active.

Europe,” said team captain Karen Hughes, Senior Enhanced Staff Nurse, in the Merlin Park hospital ward.
The team consisted of nurses, care assistants, domestic attendants and porters.
“For most of us, it was our first time taking part in a step challenge. Our motivation was to try to get the steps in and get healthier,” said Karen.
The team took photos documenting their steps for the day and sent them on to Karen every night, which she used to keep track of their progress.
“One of the best bits was probably the fun we had talking about it every morning, seeing who had the most steps,” she said.
“It has made us healthier in general by continuing to get the steps in every day.
"I would recommend that everybody should take part in the challenge as it made us all get out walking.
"It was made fun too by chatting about it and also the sharing of photos of our walks within the WhatsApp group.”
Safe Harbour is a new, free illustrated storybook for children who have been bereaved by suicide. Written by Patricia Forde and illustrated by visual artist Bronagh Lee, this new HSE resource will empower parents or carers to have difficult conversations safely with their child around this sensitive topic.
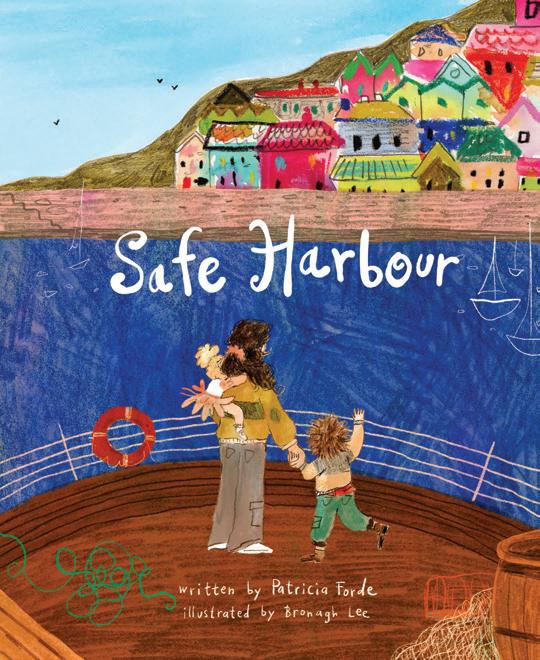
Safe Harbour is about a family—referred to as the ‘crew’—who are navigating their ship through life when something ‘terrible happens’. One of their crew dies by suicide. A child (who could be a girl or a boy) tells the story in Safe Harbour. They describe what their journey was like after the death of their Dad. The book contains lovingly crafted words and illustrations that are suitable for a child, and that they can relate to.
It is accompanied by Safe Harbour: A Helpful Guide for Parents and Carers, which outlines how parents or carers can practically use the book. The guide is also helpful for any professionals who would like to integrate Safe Harbour into their work to support a child who has been bereaved by suicide. The book is tenderly dedicated to bereaved children and families in Ireland.
Visit childhoodbereavement.ie/safeharbour for:
• more information on Safe Harbour
• downloads of Safe Harbour and Safe Harbour: A Helpful Guide for Parents and Carers – in English and Irish
• accompanying audio resources
• information on bereavement supports


a new free illustrated story book ‘Safe Harbour’/ Slán
The development of Safe Harbour has been led by HSE Resource Officers for Suicide Prevention in Dublin South, Kildare and West Wicklow Community Healthcare, with the Irish Childhood Bereavement Network (ICBN) within the Irish Hospice Foundation and the HSE National Office for Suicide Prevention (NOSP). It has been supported by Barnardos, HUGG (Healing Untold Grief Groups) and Pieta – and has included review and input from people with lived experience of suicide loss.
Safe Harbour is published as part of the HSE’s commitments to enhancing suicide bereavement supports in Connecting for Life, Ireland’s National Strategy to Reduce Suicide (2015-2024).
Safe Harbour and Safe Harbour: A Helpful Guide for Parents and Carers, are also available in print. To request printed copies, email safeharbour@nosp.ie.
Childhood should be a time of joy, growth, and limitless possibilities. Yet, far too often, children face unimaginable challenges and dangers. It is our collective responsibility to protect them from harm. It is our duty to stand up, to be their voice, and to create an environment where their innocence is cherished and protected. We all have a role in helping to protect children and young people from harm or abuse.
Children First provides a framework for identifying risks and responding to child protection and welfare concerns. Beyond our legal duties, by adhering to its principles, we can create a secure environment that supports the safety and well-being of every child.
The HSE Children First National Office are asking all HSE staff and services, including our funded and contracted services, to help promote Children First and raise awareness of key messages and responsibilities under Children First during the Awareness Week planned for 14th to 20th October 2024.
The HSE Children First National Office aims to support the HSE, and its funded services, to safeguard children through the effective implementation of Children First. We have a key functional role, at national and at local level, in supporting implementation, compliance and developing and delivering training







and other resources in relation to Children First.
Children First promotes the protection and welfare of children and outlines how to help protect them from harm or abuse.
The objectives of the Children First Awareness Campaign are to:
• Communicate the requirement for all relevant services working with children and young people to follow and/or develop policies and procedures to create a safe environment for children availing of a service (Children First Act 2015)
• Communicate the requirement for services working with children and young people to keep children safe from harm and to undertake Child Safeguarding Risk Assessments and develop and display Child Safeguarding Statements

• Communicate with mandated persons about their legal obligations under Children First and to all staff about their moral obligation to report child protection or welfare concerns
We focus on four key areas of work:
1. Supporting Community Healthcare Organisations and Hospital Groups to understand requirements and plan for effective implementation of Children First
2. Conducting Children First Compliance Assurance Checks to provide a level of independent assurance to services and HSE senior management
3. Delivering staff training and briefings, directly to staff
4. Developing new resources and policy documents in line with our Training and Resource Strategy
Key Child Safeguarding Messages for the Awareness Campaign
• All staff should promote the welfare of all children and where you have a concern in relation to the safety, welfare or protection of a child, you must report this to Tusla - Child and Family Agency
• All staff have a responsibility to report reasonable grounds for concern about the protection or welfare of a child to Tusla. Mandated persons have a legal obligation to report harm or the risk of harm to a child to Tusla.
• Read and follow the HSE Child Protection and Welfare Policy. This states that all staff irrespective of role, grade or position must promote the welfare of children and protect them from harm. A staff signature sheet in the appendices of the policy or an equivalent version should be used by line managers when keeping a record of this.
• Complete the mandatory eLearning programme 'An Introduction to Children First' on HSeLanD every three years. The certificate of completion should be given to your line manager to retain on file.
• Services working with children and young people are ‘Relevant Services’. They are legally obliged, under the Children First Act 2015, to: keep children safe from harm; undertake a child safeguarding risk assessment; develop a Child Safeguarding Statement.
• Adult-based services play an important part in the identification and assessment of child protection and welfare concerns. Consideration of the impact of parental difficulties on a child should be a routine part of practice in adult as well as in children’s services.
• Adults may also disclose abuse that took place during their childhood (Retrospective Abuse). Where there are reasonable grounds for concern that a child has been or is being abused or neglected, or a child is at risk of being abused or neglected in the future this information should be reported to Tusla. The ‘person subject to allegations of abuse’ may pose a current risk to children and this will need to be assessed by Tusla.
The HSE Children First National Office has a key functional role, at national and at a local level, in supporting compliance with the Children First Act 2015 and in developing and delivering training and other resources in relation to Children First.
‘An Introduction to Children First’ is a mandatory eLearning programme for all staff of HSE and HSEfunded services and must be completed on HSeLanD every three years.
The online interactive workshop aims to provide Mandated Persons with a clear knowledge of their roles and responsibilities.
•To register for additional optional child safeguarding training visit www.hseland.ie.
• The contact details for your local Training and Development Oicer and the HSE Children First National Oice who can provide guidance and support can be found on our website www.hse. ie/childrenirst
Quit4Youth is a seven-week stop smoking/vaping programme developed specifically for young people. It offers behavioural support in a fun, educational and non-judgmental manner.
When the Health Promotion and Improvement Department of the Health and Wellbeing Division were requested to co-facilitate this program with Youthreach in Galway City, the service became a ‘relevant service’ under the Children First Act 2015.
Relevant services are organisations that provide services to children and young people. They are required to complete a risk assessment to identify whether a child or young person could be harmed while receiving services. Relevant services must also develop a Child Safeguarding Statement which outlines any policies, procedures and practices to be observed to keep children availing of the service safe from harm. All staff should familiarise themselves with their local Child Safeguarding Statement.
This process of considering any risk of harm to children while availing of the service enabled the department to feel secure in delivering the programme in a safe and secure setting for the young people involved.
The HSE Children First website has further information and templates on competing Risk Assessment and Child Safeguarding Statements.
To access these resources and much for more information, visit www.hse.ie/childrenfirst

The two most significant drivers for digital health transformation in healthcare in Ireland are the increased demand for quality healthcare services and advancements in technology. Whether it’s in the technology industry or a healthcare organisation people around the globe are pulling in the same direction to drive digital health transformation forward.
The publication of the HSE’s Digital Health Roadmap paves the way to do just that. The digital health roadmap is part of Digital for Care, the new digital health framework for Ireland developed by the Department of Health. The roadmap details the plans for digital health transformation in Ireland. One thing that won’t change – we are all patients and we can evolve to be digitally empowered together. Technology alone will not drive digital health – it needs people. The promise of digital health transformation relies heavily on everyone involved to navigate our way together through awareness, education and participation.
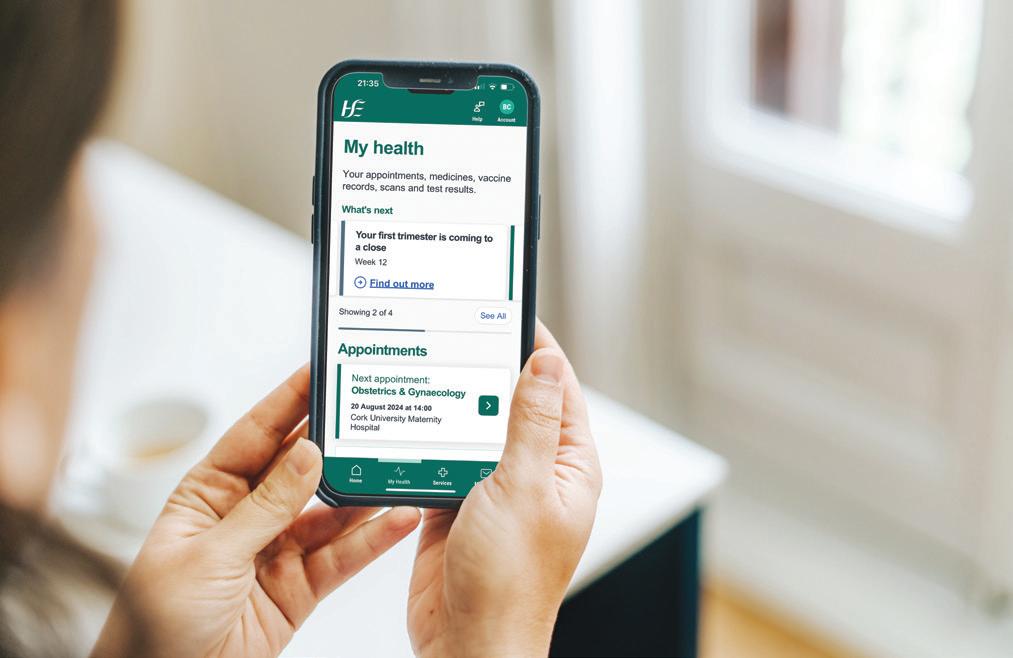
HSE app puts your health in your hands
The HSE app is one of the first projects delivered under Digital for Care.
Over time, the app will become the main channel for people to securely access their health information and a range of services online, with an initial focus on enabling people to access their hospital appointments, carry a list of their self-declared medication, COVID19 and flu vaccination records and digital versions of their European Health Insurance Card and Medical Card.
The first release later this year will focus on maternity services, expectant mothers will be able to view their hospital appointments, get appointment reminders and notifications, and receive week-by-week pregnancy information within the app. During 2025 people using the app will be able to see all their hospital appointments, along with their referrals and waiting list information.
The team is working with patients and clinicians to design the app and a pilot ran with a group of expectant mothers in Cork University Maternity Hospital in June of this year. Feedback from the pilot is already helping us to refine and improve the app’s functionality before its wider release.
The app was very well received during the pilot, with one expectant mother telling us, “The app has been amazing, very handy, and completely invaluable to me during my third trimester with all the extra appointments.”
To support the rollout, the project team is engaging with maternity services around the country.
The launch of the app is a significant step towards putting your health, in your hands and a great example of how the HSE is delivering Digital for Care.
You can find more information on the HSE app at www.hse.ie/hseapp
Learn more about Digital for Care: digitalforcare@hse.ie #DigitalForCare
What is the Individual Health Identifier?
The IHI is a unique, nontransferable number assigned to every individual using health and social care services in Ireland. The IHI ensures that each person is uniquely identified and their health records are accurately linked to them, eliminating the confusion that can arise from duplicate records or common names. Safe use of the IHI is governed by the Health Identifiers Act 2014.
The HSE Heath Identifiers Service (HIDS) manage the IHI Service.
For more info email us at: IHI@hse.ie
The benefits of the Individual Health Identifier
IHIs enable safe, efficient health information exchange, ensuring continuity of care and enhancing patient safety. The IHI enhances patient safety by accurately linking individuals to their health records, reducing medical errors, duplication, and improving care quality. The IHI will streamline care coordination, seamlessly transferring records when patients move between healthcare settings, reducing errors and omissions.
Individual Health Identifiers and Digital Records
IHIs are a critical enabler of the strategic objectives outlined in the Digital for Care framework. This framework highlights the importance of robust digital identities to support the

transformation of Ireland's health information system into one that is integrated, patient-centred, and fit for purpose. The use of IHIs is foundational in achieving this vision, enabling seamless integration of patient data across various digital health systems including Electronic Health Records (EHRs), Shared Care Records and the HSE App.
The Department of Health, along with the HSE’s Health Identifiers Service, is committed to continuing the roll-out and optimisation of IHIs, ensuring they are effectively integrated into all relevant health information systems. This commitment is part of our broader
aim to build a seamless, safe, and secure digital health ecosystem in Ireland enabling better health outcomes for all citizens.
More than just a number, the IHI is a tool for delivering high-quality, safe, and coordinated healthcare. As HSE staff, your dedication to integrating and promoting the IHI will become crucial. By embracing the IHI, we can enhance individual health outcomes and contribute to a more efficient and effective healthcare system for all. If you are a staff member who registers patients our top tips will help you record top quality, accurate data on our systems. Ultimately, this will help us to boost IHI Match Rates.
IHI Real-World ImpactVaccination Tracking: The IHI is vital for COVID-19 vaccination management. The IHI enables healthcare providers to accurately track vaccinations, ensuring timely doses and reducing missed or duplicate vaccinations. This efficient tracking is essential for managing the public health response and achieving high vaccination coverage.

6 things you might not know about your IHI
1Everyone resident in Ireland availing of public services has been assigned an IHI. If you are living in Ireland, you likely already have an IHI.
2Once an IHI is assigned to you, it remains yours for life, even after you pass away.
3No need to memorise your IHI – it is a 10-digit number that's managed for you.
4To locate your IHI, you need to provide at least five pieces of personal information: your first name, surname, DOB, sex, and at least one other info item including your PPSN, address, Eircode, mobile, or your mother’s birth surname.
5Your IHI is already on your GP record, vaccination record, medical card record, national cancer screening record and the hospital PAS system records.
6Your IHI will be visible to you on the HSE App when it is launched later this year.
5 tips will help you record top quality data
1Name: Record the legal name (not nickname or pet name). Check spelling and use proper capitalisation.
2Mother’s Birth Family Name: Record Mother’s Birth Family Name where the field is available. This never changes throughout the lifetime of a person.
3Eircode: Record the Eircode where the patient knows it. Format: XXX XXXX.
4Mobile Number: Record without spaces, hyphens, or text annotations. Format: 08xxxxxxxx or +3538xxxxxxxx.
5General: Record all fields. Use legal names. Use fields as intended – no extra notes fields. No special characters in fields (* $%&”+).
The first Virtual Wards at St Vincent's University Hospital (SVUH) and University Hospital Limerick (UHL) launched in June of this year, marking a significant advancement in Irish healthcare.
Virtual Wards allow suitable patients to receive acute care, monitoring and treatment in the comfort of their own home. Through the use of technology, hospital teams can efficiently monitor and care for patients remotely.
The Virtual Ward initiative supports Ireland's Digital for Care framework and aligns with the HSE’s Urgent and Emergency Care Plan 2024 by promoting patient-centric, costeffective healthcare delivery. It also brings major benefits for the health system by managing hospital bed availability, reducing waiting times for acute care admissions and improving healthcare efficiency.
Aoife Halpin, CNM 3 of the Virtual Ward in SVUH:
“I have received overwhelmingly positive feedback from colleagues and, most importantly, from our patients. This project has truly focused on enhancing the quality of life and care for our patients, allowing them to receive exceptional clinical support without the need for prolonged hospital admission. This initiative not only highlights our commitment to patient-centred care but also marks a significant step forward in modern healthcare delivery.”
Speaking about their experience on a Virtual Ward, one patient shared:
“I’m much happier and less stressed knowing I am being looked after from home. I feel supported and








looked after, not having to worry about my heart or BP dropping as it is all monitored and taken care of. It is giving me a new release in this time of my life and I am a lot more relaxed now that I have slept through the night for the first time in a long time.”
Prof Richard Greene, Chief Clinical Information Officer, highlighted the benefits: "They have the potential to empower patients, providing them with greater control over their healthcare experience. From an operational standpoint, Virtual Wards seamlessly integrate into existing hospital workflows, leveraging state-of-the-art telehealth technologies for real-time communication between patients and their healthcare teams. This

advanced approach not only enhances patient safety but also optimises resource allocation within hospital settings, thereby significantly enhancing the overall experience for both staff and patients navigating the Virtual Ward care system."
Deirdre McNamara, Director of Strategic Programmes: "Virtual Wards have the potential to play a pivotal role in revolutionising hospital care and how we ensure our acute care capacity meets growing demand, while ensuring better patient access to care, outcomes and experience. The opening of these first Virtual Wards is a significant milestone, achieved thanks to the dedication, collaboration and expertise of all partners involved.”
from the Home Support Service in Tralee, County Kerry, describes his day and the impact his service users have on him
8am My working day begins at 8am, as part of a team of Health Care Assistants in the Home Support Service who visit a specific group of service users in the Tralee area. Our aim is to use a person-centred approach while providing care to our service users.
The service users are always waiting for my arrival - this tells me that each person values my visit and this key service.
11am By now, I have visited a number of service users with varying needs. Service users may require help with mobility or personal care, enabling them to start their day.
Later in the morning, the service users I visit may have listened to the radio or read the newspaper. I strike up a conversation on the day’s news and they will voice their opinion. Their opinion, for the most part shows their life’s values, which is a

great education for me. I did not envisage this insight when I became a Health Care Assistant in the Home Support Service.
1pm On my lunch break, I meet up with another member of the team – this is important downtime. After lunch I visit my next service user who will have different care needs.
The most pivotal rules for me as a Health Care Assistant are confidentiality and safety. It is a privilege to be welcomed into a service user’s home and I respect this. The trust a service user places in me is truly humbling.
It is imperative to have the support from the organisation one represents, this is very evident with my employers. The day may present a challenge and that is where assistance from our line manager and home support office is necessary. The late afternoon is
treated no differently to the early morning in terms of approach, yet so contrasting when dealing with unique personalities and varying care needs.
When posed the question ‘what do you enjoy the most about your career’ the word that struck my mind is ‘values’. The trust built up is unique, the advice and education is a two-way street and the appreciation from the service users so rewarding.
This job is so fulfilling for me personally. One thing I am certain, if I am a service user in the years that are ahead of me, I would prefer to be in my own home. I would give a huge welcome to the person who comes through the door to care for me and who promotes my independence. I would pass on the values that I am experiencing now as a Health Care Assistant to the person looking after me in the future.
To find out about the reforms being introduced to the Home Support Service, see page 64.


We are currently transitioning to the new health regions structure. From 1st October, each health region will be responsible for providing both hospital and community care for the people in that area. By the end of September, Community Healthcare Areas and Hospital Groups will be stood down. Until the new structures are fully implemented, there will be a period of transition, every effort will be made to minimise disruption to patients and service users, staff and services and the focus will remain on providing safe services during this time.

Recruitment is progressing in appointing the Health Regions Executive Management Team (EMT) members.
IHAs will be the substructures within each of the 6 health regions. There will be 20 IHAs in total. They will serve a population of around 300,000 and will take account of local geographies, population size, needs and services. Implementing the new structures will see hospitals and community services within the IHA under one IHA Manager. This will support local decision-making and planning to meet local needs. These changes will facilitate the move to more integrated patient-centred care. The IHA manager roles will not result in an increase in senior management staff numbers in the HSE. They are being funded and organised by restructuring existing senior management positions.

A patient and service user partnership proposal was finalised and approved in early 2024. A plain English version of this proposal was completed in July 2024. The implementation of this proposal will keep the voices of patients and service users at the centre of health regions’ design and service delivery going forward.
Read the plain English patient and service user partnership proposal here on https:// healthservice.hse.ie/
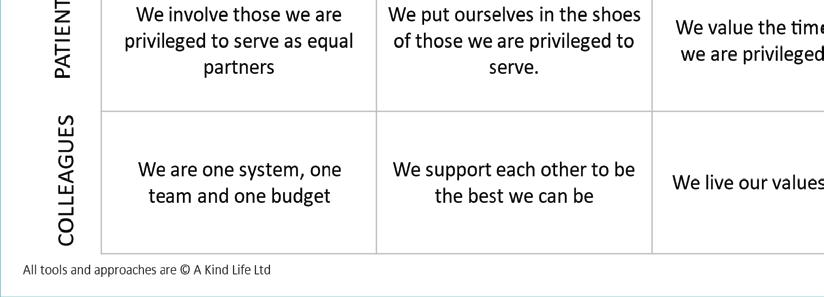
Ireland is undergoing a significant transformation in its healthcare system with the implementation of Sláintecare and the establishment of health regions. These initiatives aim to create a more integrated, efficient, and patientcentred healthcare service. People’s Needs Defining Change – Health Service Change Guide outlines nine priority areas essential for creating the conditions for successful integration. Lisa McDaid and Elaine Birkett from the National Organisation Development and Design (OD&D) team hosted an interactive workshop at the ICIC, Belfast, April 2024. It was titled ‘Creating the Conditions for Integration: Bridging Evidence, Policy, and Practice’. It brought together leaders, researchers, clinicians, managers, community representatives, patients, and caregivers from around the world engaged in designing and delivering integrated health and care. The session focused on practical applications of the Health Service Change Guide. During the workshop, participants shared their insights on their experience of what works in each area for integrated care:
• Practice Collective Leadership: Engage with the voluntary and community services and ensure clear sponsorship and communication with senior leadership. Encourage peer support and maintain strong multidisciplinary leadership.
• Support Behaviour Change: Hold regular meetings, practice compassionate communication, and build foundational capacity. Circulate information and create opportunities for open discussion.
• Engageand Communicate: Early and ongoing engagement with stakeholders is vital. Foster a speak-up culture and involve patients and the public, using digital tools for timely communication.
• Model Shared Values: Align actions with core values like care, compassion, trust, and learning. Ensure equity, accountability, and build trust by involving staff

and patients in service design.
• Understand Personal Experiences: Tap into people's experiences, conduct monthly check-ins, and address concerns sensitively to help people adapt to new practices. Use personal stories as platforms for change.
• Invest in People and Teams: Continuous professional development and team-building are essential. Provide ongoing training, celebrate success, and hold ‘town hall meetings’ for stakeholder engagement.
• Be Accountable for Performance: Ensure clarity of outcomes, benefits realisation, and professional supervision. Set SMART objectives and ensure local ownership.
• Use Evidence and Lever Technology: Use data, evidence, and technology to inform practice. Communicate changes with stakeholders, use common data sets, and engage stakeholders before planning.
• Network and Partner: Build networks and partnerships within the health and social care system. Ensure no key stakeholders are left behind and use a person-centred approach.
For more information, visit http://www.hse.ie/changeguide

The Health Regions Programme Team is running a series of webinars in 2024. These webinars will provide an update on the implementation of health regions. The first webinar in the series took place on Thursday 27th June. It included a focus on population-based planning. The webinar also covered:

• implementation of the health regions
• regional health profiles
• Health Atlas
The next webinar will take place on Thursday, 26th September at 1pm. Details of the webinar will be published on https://healthservice. hse.ie/staff /latest-healthregions-updates/ Watch back the health regions webinar from Thursday, 27th June on YouTube

It’s been a very exciting and enjoyable few months getting to know the services and communities in Cork and Kerry. It’s mostly been about building relationships, connecting people and working with the Senior Leadership Team of leaders in Public Health, Hospitals and Community on agreeing the culture of HSE SW. Together, we have agreed that our purpose is to make our community proud of their health service by making commitments within our HSE values.
At the outset I said that I wanted there to be kindness to the community we’re privileged to serve, to our hard-working staff and to our governors who have accountability for us.
My priority from the outset has been to deliver Sláintecare. That is to successfully integrate services and meet the waiting time commitments of a maximum 10 days for diagnostic testing, 10 weeks for an outpatient appointment, and 12 weeks for an elective procedure or operation.
To make this a reality, we held a number of workshops and engagements to develop Scheduled Care and Unscheduled Care plans for the region, and there are six exciting projects coming from the Integr8 workshops. I have said that I have no tolerance for patients waiting on trolleys and we’re working on initiatives like eliminating delayed transfers of care, putting in place Virtual EDs, implementing the SAFER bundle, hot clinics, navigation hub, dedicated patient flow managers to make a real difference to patient flow before we enter the winter period.
I’m also looking forward to delivering our next Integr8 workshops, bringing together 300 influential staff to start to build a social movement to embed Sláintecare across all our services.
We’re also working on putting in place the
organisational structures that will ensure a smooth transition from CHO and hospital structures to HSE South West. This has included moving many staff to co-locate the functions and enable clinical service development and I thank the teams who are facilitating this huge task.
As well as focusing on immediate operational matters, we’re also looking to the next five years and beyond as we create a vision not just for HSE South West, but for the people of the region which will support them to be the healthiest people in the world.
I know that this is an uncertain time for all our hard-working staff. We are making very significant changes to working practices and places of work as well as the managers and leaders that staff
“At the outset I said that I wanted there to be kindness to the community we're privileged to serve, to our hard-working staff and to our governors"
report to. I ask in advance for your patience, understanding and forgiveness as we move forward with urgency and pace. I want everyone to feel listened to, involved and that we do things together. There are challenges, but this is an exciting time as we work together to build the health service which the people of Cork and Kerry can be proud of.
As we approach winter, please give careful consideration to getting your winter vaccines, protecting yourself, your patients and your loved ones at home from COVID-19 and influenza.

‘We are a team and we respect one another and each other’s wellbeing is a priority at work’
Bernadette Horgan-Edmead and her team recently received the Psyched recognition award for their commitment to promoting staff wellbeing and recognising mental health at work.
When Bernadette started as Dementia Care Coordinator in March 2023, the team of community dementia support workers (CDSWs) were exhausted. Working with such a diverse needs-set can be very isolating and CDSWs are at high risk from work-related stress and burn-out. Meeting the needs of the CDSWs is integral to providing a high-quality service.
Bernadette said she values the importance of nurturing wellbeing and a sense of inclusion and teamwork. She takes several small and effective initiatives to support her team in the Dementia Care Coordinator Service CHO4.
Back - Kelly Kerrin Relja, Joan Dineen. Front - Bernadette Horgan-Edmead, Jillian Preston Keily, Aileen McCarthy, Nuala Murphy and Martha Buckley.
The CDSW work under the dementia care coordinator service and are the only team of its kind in Cork and Kerry. Each CDSW offers people living with dementia one-to-one personalised care, recognising and valuing each person’s dignity, respecting them and tailoring responses to their unique needs.
The CDSW work in their client’s home and at community events developed by the service, bridging the gap from home to the community, encouraging participation, promoting inclusion and reducing isolation. They use local networks and community amenities for their clients to remain socially connected.
Bernadette is constantly finding ways to enhance the working experience for her team in order to provide our clients with the best service then can hope for.
A simple initiative like scheduling regular team meetings has really helped develop the morale and confidence for the CDSWs. Team meetings give the CDSWs a chance to share goals and share experiences.
In January she organised an in-house training day. It was the first time the team all met together since the service started in 2012.
They invited members of the primary care team to come and meet the team and they all expressed the gratitude for the team and the amazing work they do. Knowing your part of a wider team helps to reduce the loneliness of being a lone worker.
Residents with dementia in a Cork community nursing unit (CNU) have been benefitting from a new ‘Snoezelen’ room for multi-sensory stimulation that is equipped with a Tovertafel or ‘magic table’. This is a project which allowed the staff to connect with the residents through purposeful play with the Tovertafel and gentle stimulation for residents that can reduce stress, tension and allows recuperation in a controlled multi-sensory environment by the Snoezelen room.
Multi-sensory rooms relieve the pain and stress associated with dementia and it also helps to improve the residents’ ability to focus, communicate, and remember. The Tovertafel or ‘magic table’ has a huge impact on residents with
dementia. Maintaining cognitive skills is the most important goal in this respect. People with dementia are confronted with things that they are no longer able to do on a daily basis. Playing with the Tovertafel allows them to experience what they can still do.
“We see residents begin to move who otherwise would have remained inactive. It puts a smile back on people's faces and encourages interaction. It's the best thing we have seen so far to enhance joy in the lives of people with dementia. This is also effective for staff - we can see a lot of enthusiasm when the table is turned on as they are getting an opportunity to connect with residents through playing,” said staff member Salini Vasudevannair.

Gathering of Kindness, HSE South West at Vertigo in the County Hall. Pic: Brian Lougheed
Healthcare staff from across Cork and Kerry joined together on 28th June for the HSE South West’s ‘Gathering of Kindness’. Staff across HSE South West were invited to join in, either online or in person.
A dynamic programme of events was enjoyed by all, including an overview from REO Dr Andy Phillips on what he coins as ‘mindful kindness’, a presentation from Tim Keogh of ‘A Kind Life’, an address by Professor Cath Crock from the ‘Hush Foundation’ on the importance of practicing kindness in healthcare settings, a breathing workshop with Leo Daniel Ryan (Innate Strength), and an insightful session on mindfulness in action led by Dr Stephen Halpin.
We also heard from healthcare staff on what kindness means to them, make sure you catch it on https:// www.youtube.com/@ HSESouthWest
This event was the first of many, leading to other 'Gatherings of Kindness' across both Cork and Kerry – stay tuned for more!


HSE South West have installed swim distance marker buoys at Kells Bay Beach, in Cahersiveen, Co Kerry.
The new swim distance markers have been placed at 100m intervals to create a 600m sea swimming circuit at the popular Kells Bay Beach. Information signage has also been erected by Kerry County Council to identify and explain how to use the swim distance buoys.
The installation of the swim distance markers in Kells Bay Beach provides increased opportunities for safe and enjoyable physical activities, adding healthy habits in our daily and weekly routines. The swim distance marker buoys will encourage safer swimming among novice and experienced open water swimmers.
Sharon O’Sullivan, Health and Wellbeing Manager, Cork Kerry Community Healthcare, highlighted the importance of this initiative, which facilitates safe physical activity and wellbeing, adding, “As a coastal county, we have a tremendous asset available for everyone to enjoy. I am confident that the swim markers will encourage existing and new users to get into the water and swim, an activity that is good for mind and body.”
Further information available from Water Safety Ireland at www.iws.ie.
A new HSE-funded health strategy supporting Roma families in Cork and Kerry 'Te Rodel Nevo Drom’ (We are Looking for A New Way) was launched at the Tralee International Resource Centre (TIRC).
Commissioned by TIRC in December 2022, with support from HSE Cork Kerry Community Healthcare, Dr Patricia Kennedy took on the role as lead researcher for the project to develop a strategy for Roma Families in Cork and Kerry, in collaboration with Roma peer researchers and with the guidance of a research advisory group.
A consultation process, which involved talking with over 60 representatives from the Roma community, NGOs and statutory agencies, was completed between January and April 2023. The experts by experience, Isac Ianko and Marcela Venzel were key to this research and they brought the voice of their community with them.
“This strategy for Roma health needs was researched in our community. It represents our Roma world and our journey today,” said Marcel, while Isac added, “This work, which we have been part of, shows clarity and simplicity. All of the findings mentioned in this strategy are essential to our Roma community.”
Head of Primary Care for HSE Cork Kerry Community Healthcare Priscilla Lynch said, "I welcome the recent establishment of Roma
supports in Cork and future supports in Kerry, which will add greatly to our capacity to meet the needs identified and recommendations made in this consultation.
“I would also like to acknowledge the role of our Community Work and Social Inclusion departments in Cork Kerry Community Healthcare, in supporting partnerships with the NGO sector at community level. Their excellent work reflects the analysis in Sláintecare that acknowledges social exclusion and we strive daily to remove any barriers that stand in the way of doing the right things for patients that need care.”
Co-ordinator of Tralee International Resource Centre Mary Carroll said, "We have been working with the Roma community for many years and this research is the voice of the Roma in Cork and Kerry themselves, which is the key to the way forward and effecting real change for this community, who have experienced significant levels of adversity.
"The findings cover the health and social needs of the Roma and the key is that they have been translated into actions - some of which can be progressed immediately, while others will require longer term planning. Actions include the need to improve awareness, to celebrate Roma culture, increase access to translation, develop a Roma info line and work specifically with Roma women."
A summary of the strategy is available in leaflet format, and in several languages for the Roma community to access. It is available from TIRC on 066 712 7918 or by emailing reception@tirc.ie. The strategy document is available at www.hse.ie/romahealthstrategy and on the TIRC website (www.tirc.ie).
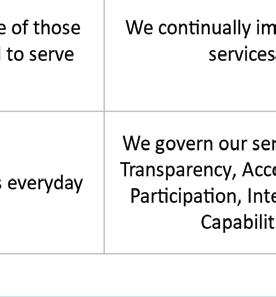
The HSE South West Health Region has pledged to make the community proud of their health service by outlining a number of commitments within the values of the HSE.
REO Dr Andy Phillips has been meeting with senior leaders across the region in areas of Public Health, Hospitals and Community and together they have agreed the culture of HSE South West going forward. The implementation of the Integr8 system of values will discussed and developed with staff with continuing Integr8 workshops.


The library at University Hospital Kerry (UHK) is now a modern, technologically enhanced learning space supporting evidence-based practice, research, innovation and lifelong learning thanks to a recent renovation.
Dr Colm Henry, HSE CCO, launched a five-year strategy for the HSE Library in March 2024. A key deliverable of this strategy was to bring all HSE Libraries up to the required standard for health libraries. UHK library was first on the list for its relaunch this year and was long overdue for a renovation. The library is a unique learning environment in a busy hospital which cultivates research, allows space for thinking, growth and innovation. The next library earmarked for improvement is MRH Mullingar.
NDTP, UHK, and HSE Library contributed to the full renovation of the library and library classroom. The newly renovated library space has eight new computers for staff, Wi-Fi-boosted hotspots, dedicated training and study space, and a robust health science print collection.
Professional library staff are on-hand to assist with health science research queries. Additionally, there is an

area dedicated to 24-hour computer access for staff.
The space is a great resource for staff and students working at UHK.
Prof Brian Kinirons, Medical Director of NDTP, opened the space in May. Those who attended the launch included several doctors, the UHK Library team of Jennifer Butler and Mary Lehane, UHK Deputy Manager Anna O’Shea, National HSE Librarian Aoife Lawton, Area Library Manager South Brendan Leen and UHK Librarian Melanie Surkau, who was on career break.
A newly-constructed Wellbeing Room, part-funded by the HSE, has opened at The Glen Resource Centre in Cork city, providing a space to run valuable health and wellbeing programmes and community services.
The local community can enjoy a wide variety of free programmes in collaboration with the Health Action Zone, Dillon's Cross Project, Cork City Partnership and Cork Prison, with popular courses including: The Sláintecare Healthy Food Made Easy Programme, barista courses, pilates, mindfulness and much more.
The Wellbeing Room is funded by HSE/ Cork Kerry Community Healthcare and Cork City Council. This project was funded by HSE Community Work/Social Inclusion, Sláintecare Healthy Communities and by the Community Recognition Fund (Department of Community and Rural Development) administrated by Cork City Council Community Culture and Placemaking Directorate.
Sorcha Ní Chrualaoich, HSE Principal Community Worker with Cork Kerry Community Healthcare, welcomed the
launch of the Wellbeing Room. “The Health Action Zone and community health work partners here are committed to providing an exciting programme of activities to people in the Glen, Blackpool, Ballyvolane, Mayfield and the wider community healthcare network, which further enhances the health and wellbeing of the local community here.”
Catherine McCullagh, Healthy Food Made Easy (HFME) Tutor, said, “I just finished my HFME tutor training and I can’t wait to start delivering community courses soon. The room is fantastic.”
Top: Hannah Healy, HSE and Nicola Brett, HSE at the launch of the Glen Resource and Sports Centre Wellness Room.
Bottom: Cllr Oliver Moran and Sharon O’Sullivan, HSE at the launch of the Glen Resource and Sports Centre Wellness Room.
Photos Darragh Kane


The COVID-19 and flu viruses circulate at high levels this time of year. As a healthcare worker, you’re at high risk of being exposed to these viruses. You also risk exposing your colleagues, family and vulnerable patients to serious illness.
The best way to protect yourself and the people you care for this autumn is by getting your COVID-19 and flu vaccines.
You will find vaccine clinic details listed at HSE.ie/staffclinics from October 2024.
You can get both the COVID-19 and flu vaccine together during the same appointment, or you can get them at different times if you prefer.
Dr Colm Henry, Chief Clinical Officer, highlights the pressure these viruses cause in our health service and urges everyone to get vaccinated.
“Flu, COVID-19 and other respiratory viruses are highly contagious and high levels of cases can create additional pressure on our healthcare system. Last year, only 37% of healthcare workers received the flu vaccine and less than 19% received the COVID-19 vaccine. I encourage all health and social care staff to avail of the vaccines, to protect yourselves, your families and your patients over the winter months,” he said.
“Infection prevention and control guidelines are also an important tool in protecting ourselves and those we care for, supporting us in delivering safe care to patients across our health service.”
Dr Eimear Burke, Consultant in

Public Health Medicine at the HSE National Immunisation Office, highlighted why the flu and COVID-19 vaccination programmes are so important for healthcare workers in particular.
“Apart from clean water, vaccines have saved the most number of lives out of any other public health initiative. It's had the biggest impact in terms of mortality and reducing vaccine-preventable diseases.”

Dr Burke continued, “Getting vaccinated is one of the best ways to help you and your family to stay well this winter. It also helps to prevent the spread of flu and COVID-19 to vulnerable patients. You can find out more at www.immunisation.ie.”
Protection from previous vaccines or a previous infection weakens over time, and the COVID-19 and flu viruses are changing. As a healthcare worker, it’s important to stay up-todate with the latest COVID-19 vaccines, and to get your flu vaccine as early as possible every autumn.
Dr Sarah Geoghegan, National Immunisation Advisory Committee (NIAC) Clinical Lead, emphasised the importance of healthcare workers getting both vaccines to protect themselves and the vulnerable people they care for. She notes that the vaccines may not be as effective in certain highrisk groups, so it’s crucial for the people looking after them to be vaccinated.
“One thing that is really important to understand about both the flu and the COVID-19 vaccine is that unfortunately it doesn't work as effectively in some of the highest risk groups, such as immunocompromised patients, those receiving chemotherapy and adults over 80,” she said. “So even if these groups are vaccinated and in hospital, they may still get COVID-19 or flu. So it's really important that the people looking after them are vaccinated as well.”
You can learn more about the benefits of vaccines by logging into HSeLanD and searching for the ‘Flu and COVID-19 Vaccines for Healthcare Workers – protect yourself, protect others’ module. This is a 15-minute online course designed to educate and inform healthcare workers about the COVID-19 and flu vaccines. It also addresses some of the myths surrounding them.
Everyone is at risk of becoming sick from flu or COVID-19
Even in healthy young people, COVID-19 and flu can cause fever and fatigue. It can take up to a week or longer for you to recover. The risk of serious illness is higher in people over 50 and those with a weak immune system.
Here are five things you should know about your recommended vaccines:
1. Vaccination is best protection against viruses
Vaccination is the best protection against viruses like COVID-19 and flu
To prevent the spread of COVID-19 and flu to others, it is important to follow infection prevention and control procedures, such as good hand hygiene. However, the best way to protect yourself from catching these viruses is by getting vaccinated.

2. Immunity from infection weakens over time
If you have had the COVID-19 infection in the past, you may have built some immunity but this protection will weaken over time. Getting the COVID-19 vaccine will top-up your immunity against COVID-19 for the months ahead. Getting the flu vaccine is the best way to protect yourself against flu. The flu vaccine helps your immune system produce antibodies to fight infection. If you got the flu vaccine between October 2023 and April 2024, you will need to get vaccinated again this year to protect yourself.
3. It is easy and free to get vaccinated
You do not need to travel far to get the vaccines and they are available free of charge. COVID-19 and flu vaccines may be available where you work or you can go to a local participating GP or pharmacy.
4. The vaccines are safe and effective
The HSE only uses vaccines when they meet the required standards of safety and effectiveness and after the European Medicines Agency (EMA) has licensed them. Vaccines offer strong protection, and effectiveness can vary from person to person. However, if vaccinated people do get sick, they are likely to have milder symptoms.
5. Where you can get your COVID-19 and flu vaccines
You can get your COVID-19 and flu vaccines from early October. It’s safe to get both vaccines at the same time. You will get one vaccine in each arm. You can also get each vaccine at a separate time if you’d prefer. They will still work the exact same way. Vaccine clinics in hospitals and community settings will be listed at HSE.ie/staffclinics from October 2024.

Measles is a highly contagious viral disease that continues to pose a significant threat to global health, despite the availability of an effective vaccine. Outbreaks can have devastating consequences, particularly for children, and can put pressure on healthcare systems. To reduce the risks and curb the resurgence of measles, many countries have started ‘catch-up’ campaigns. These campaigns aim to vaccinate people who missed their routine vaccinations.
In response to a rising number of measles cases in Ireland, a Measles Incident Management Team (IMT) Communications Subgroup group was established. It includes representatives from the National Immunisation Office (NIO), Health Protection Surveillance Centre (HPSC), National Social Inclusion Office (NSIO), Departments of Public Health and National Communications.
The IMT began with a thorough analysis of public health data, which revealed vaccination gaps. A combination of access barriers, misinformation and vaccine fatigue or hesitancy may all have contributed to lower immunisation rates than desired.
Recognising the urgent need for intervention, a working group came together to design a
“A combination of access barriers, misinformation and vaccine fatigue or hesitancy may all have contributed to lower immunisation rates than desired.”
targeted catch-up campaign for Ireland.
The group worked together to support the rollout of a public-facing campaign, using a mix of digital and traditional media channels. One of the key objectives of the campaign was to encourage people to get the vaccine if they missed out getting it when it was offered to them before. The campaign specifically targeted at-risk groups as defined by the IMT.
The target audience was separated into demographics with the lowest vaccination rates, such as young children, young people and harder to reach communities. To tackle misinformation, the group launched an extensive education campaign.
The MMR vaccine was provided free of charge and HSE clinics were set up in addition to GPs offering the vaccine.
Reaching a wide audience
The MMR vaccine catch-up campaign ran on national and local radio, digital audio and digital display ads. HSE Live opened a dedicated Measles line on 19th March to support people to book a vaccination appointment, reassure citizens with facts on measles and give them guidance after confirmed cases in Cork University Hospital and Midlands Regional Hospital.
Resources were developed to support the campaign, including a ‘Think Measles’ information leaflet and a public poster which was translated into 15 languages.
To date, the MMR catch-up campaign has resulted in an additional 10,000 people being vaccinated through the programme.
Respiratory syncytial virus (RSV) causes hospitalisations every winter and sometimes serious illness, especially among young infants. Newborn babies in Ireland can now get protection from RSV through the RSV immunisation pathfinder programme.
The RSV immunisation pathfinder programme is great news for new babies and their parents. Each winter, four out of every 100 infants are hospitalised due to RSV, with some infants needing special treatment in intensive care units. A further 50 out of every 100 infants will get RSV, and many will need medical care from their GP or the emergency department of a children’s hospital.
Dr Éamonn O’Moore, HSE National Director for Health Protection, explained, “The RSV immunisation pathfinder programme is being delivered by trained midwives in all maternity settings in the Republic of Ireland after birth and before the baby is discharged. The immunisation is provided free of charge. A similar programme in Galicia in Spain was very successful where 90% of babies were immunised leading to a big drop in RSV hospital cases there.
Vaccination is one of the most important things we can do to protect our families. Vaccines teach your child’s body how to make special proteins called antibodies, which protect them from serious illness when they come into future contact with an infection. All vaccines used in Ireland are proven to be safe and effective.
Childhood vaccines are free of charge from your general practitioner (GP). They are given over five visits at 2, 4, 6, 12 and 13 months of age. Your child will get booster vaccines in school to top up their protection as they grow.
Recently in Ireland, we have seen a rise in measles and whooping cough infections, and so vaccinating your child remains as important as ever.
Each winter, four out of every 100 infants are hospitalised due to RSV, with some infants needing special treatment in intensive care units. A further 50 out of every 100 infants will get RSV, and many will need medical care from their GP or the emergency department of a children’s hospital.
“This year’s programme is a ‘pathfinder’ which will allow us to explore and analyse how best to improve health and to provide information and experience on rolling out any future programmes. It finishes at the end of February 2025 when the winter season draws to a close and RSV levels drop naturally.”
There have been 69 cases of measles in Ireland in the first six months of 2024 and sadly one person has died from measles. Measles can cause severe complications including pneumonia, inflammation of the liver or inflammation of the brain (encephalitis). Getting two doses of the MMR vaccine is the best protection against measles. The MMR vaccine is given at 12 months and a second dose is given in junior infants. At present, children get a whooping cough vaccine as part of the 6-in-1 injection at 2, 4 and 6 months and two further boosters given in junior infants and first year of secondary school. It’s very important that babies are protected against whooping cough; one in every two babies under six month of age who gets whooping cough will need hospitalisation. A whooping cough vaccine is also recommended in pregnancy. Vaccinating the mother during pregnancy protects baby for the first few weeks of life, until they get their own vaccinations. This is best given between 16 and 36 weeks of pregnancy, and is available from your GP.
If your child has missed vaccines or is late for vaccines, they can catch-up. This is particularly relevant at the moment for children who have not yet had their MMR vaccine. Contact your GP practice to discuss catch up childhood vaccination to ensure your family is fully protected, or find further information at www.immunisation.ie.

We have been working for several months to establish the new regional leadership team. I am optimistic that we will have the majority of the team in place when the new regions are officially established in October.
The team will work collaboratively to develop a strategy for integrating community and acute services to improve healthcare delivery for our patients taking a population health approach.
I recognise that we have continued to see very high volumes of patients seeking urgent and emergency care. I know that this has placed extraordinary pressure on staff right across our services. I want to thank you for the flexibility and dedication you continue to demonstrate as we deal with this demand. We will continue to assess how best to deliver services ensuring we achieve the right balance, delivered in the safest possible way.
“We
In April, Minister Donnelly announced a number of initiatives for the Mid West. We are making great progress with some of the initiatives including the construction of a new 16-bed inpatient block at University Hospital Limerick to be completed this coming winter.
These include the two 96-bed blocks for UHL and additional wards blocks for Ennis, Nenagh and St John’s under the Acute Inpatient Hospital Bed Expansion Plan.
The Improvement Programme Board is also guiding the implementation of integrated care pathways and service improvements across the region focused on patient flow and delivering on the promise of Sláintecare to ensure services are provided closer to the patient and at the point of least complexity.
These include the expansion of Medical Assessment Unit services at Ennis, Nenagh and St John’s; the opening of an Acute Virtual Ward at UHL and a social inclusion inreach pathway for
will continue to assess how best to deliver services ensuring we achieve the right balance, delivered in the safest possible way"
We are also advancing plans to add sub-acute/ community rehabilitation beds in Tipperary and Clare to address capacity challenges and improve patient flow this winter.
Earlier this year, I established a Regional Improvement Programme Board. The Board is the driving force to ensure the timely implementation of a range of projects and initiatives in the short, medium to long term which will respond to increasing demand for acute and community services across the Mid West region.
patients attending the Emergency Department.
This winter we will continue to face challenges matching demand and capacity. We will use all the levers available to us so that we deliver safe care to our community and work to meet their healthcare demands. Taking care of our own health and safety is crucial, not just for us but for our families and patients too. I encourage you to consider getting your winter vaccines to stay protected and healthy.
Over the coming months, I’m looking forward to working with staff to deliver on the reforms needed in our region.



International Day of the Midwife was a day like any other for the hardworking midwifery staff at University Maternity Hospital Limerick (UMHL)… and also the most special of days for eight new-born babies who arrived into the world during those 24 hours.
The first new arrival at the hospital at 3.47am, when Limerick city mum Maja Stypula gave birth to a little girl.
Other happy new mums that day included Edjan Des Santos, Dromcollogher, Co Limerick, and Sinéad Grene, Ballybricken, Co Limerick; while Amy Power from Ennis, Co Clare gave birth to twins.
These and the mothers of all UMHL new-borns on International Day of the Midwife were presented with commemorative birth certificates.
Among a variety of activities in UMHL to mark this global red-letter day, there was also a visit to the maternity hospital by Transition Year students from across the Mid West region to meet with midwives and hear from them about the pathways and benefits of midwifery as a career option for school-leavers.
Some of the staff midwives at UMHL have been speaking about the sense of fulfilment from working in midwifery.
Staff Midwife Amy Downes explained, “Being a midwife fulfils me in a way that I don’t think anything else ever could. I feel so unbelievably honoured to have the opportunity to positively impact people’s lives at such a fundamental time, whatever the case may be. I’m thankful to every family that has let me be a part of their journey—it’s a true privilege.”
L-R; Maja Stypula with her new-born daughter, and midwives Cynthia Meehan (left) and Ciara Keane (right) and student midwife intern Leah Maria Donnelly; New mum Amy Power with UMHL staff midwives Tara McMahon (left) and Dawn Halpin; Edjan Des Santos, Co Limerick, and her newborn baby with midwives Cynthia Meehan (left) and Ciara Keane (right) and student midwife intern Leah Maria Donnelly
Parenting is often described as the most rewarding yet challenging job in the world. In Co Clare, the Circle of Security (COS) parenting programme has become a beacon of hope and support for many families seeking to build stronger, healthier and secure relationships with their children.
COS is an internationally recognised, evidencebased parenting programme designed to enhance the bond between parents and their children. The programme is rooted in attachment theory, which emphasises the importance of a secure parentchild relationship in the healthy development of children. The programme helps parents to tune in and respond to the emotional needs of their children in ways that promote secure attachment. In Co Clare, the COS Parent Programme is facilitated by trained professionals dedicated to helping parents to navigate the complexities of raising children. The programme is currently offered through Primary Care Children’s Services such Psychology and Speech and Language Therapy. It is also offered in other family related
services such as Clarecare; Family Resource Centres; CAMHS; the Children’s Disability Network Team (CDNT) and Adult Mental Health. All of these services are working together in an integrated way to deliver, evaluate and further develop this programme in Clare with the hope of making it more widely available in local communities and indeed across the Mid West.
Circle of Security is now available for the classroom so that teachers can identify the meaning behind children’s behaviour and find new ways to respond to children that welcomes connection and supports learning. COS Classroom is now being offered to primary school teachers by the National Educational Psychology Service (NEPS) in Clare.
Sarah, a mother of two, said, “I have the tools now to improve the happiness in our home.”
John, a father, noted, “Every parent should do this course as it teaches you to be more understanding to your child’s needs and tackle situations differently.”
The HSE teamed up with Sport Ireland and its network of local sports partnerships during the summer to raise awareness of HSE Injury Units in the Mid West and the expertise they offer to people who sustain a sports injury.
Dr Damien Ryan, Consultant in Emergency and Clinical Director for Urgent and Emergency Care at UL Hospitals Group, said, “During summer, we typically see an increase in people coming to the injury unit with broken bones, sprains and other injuries that occurred during sports and outdoor activities, like injuries to ankles, wrists and fingers. We are partnering with Sport Ireland to highlight the excellent service provided by the experienced doctors, advanced nurse practitioners and nurses at the three Injury Units here in the Mid West - your first port of call for sports injuries this summer.”

Éamonn Phelan, County PRO, Limerick GAA; Mike O’Riordan, County Secretary, Limerick GAA; Dr Cormac Mehigan, Emergency Medicine Consultant, UL Hospitals Group and Seamus McNamara, County Chairperson, Limerick GAA.
Dr Úna May, CEO of Sport Ireland, said, “We are thrilled to be involved in the promotion of the Injury Units in the Mid West. It’s important to know where you can find your nearest injury unit, especially at this time of year when we are all enjoying the longer days by getting outside and being active.”
Locally, UL Hospitals Group launched an initiative with GAA clubs across Limerick, Clare and Tipperary to promote Injury Units in the Mid West. The group also partnered with public libraries across the region.
Two new nurse-led pathways have been developed for New Onset Atrial Fibrillation and Congestive Heart Failure.
The pathways reflect the spirit of collaboration between the Medical Assessment Unit, Ennis and the Integrated Care Hub Ennis to ensure that patients in the region have faster access to cardiology services, diagnostics, and expert intervention. It is anticipated that the pathways will platform greater links and expansion of innovations to enhance patient services in the future

Nenagh Hospital’s Healthy Ireland committee’s latest collaboration with the Tipperary Arts Office has seen an exhibition of fine art prints on display throughout the hospital’s public areas during the summer.
The joint initiative was mounted to promote positive health and wellbeing through artistic engagement, for the hospital’s service-users, members of the public and staff.
A visually stunning array of fine art prints by contemporary Irish artists, the 32 works encompass a variety of styles, including the work of celebrated Irish printmakers such as Alice Hanratty, Des MacMahon, Suzannah
O’Reilly and David Lilburn.
The fine art prints on display at Nenagh Hospital represented a variety of printmaking processes, including screen printing, lithography, intaglio and relief printing, conveying subject matter that ranges from colourful streetscapes in screen print to monochrome figurative etching.
This collaborative initiative follows the successful Tipperary Arts Office/Nenagh Hospital partnership in the arts office’s 2024 Bealtaine programme, which showcased a live musical recital in the hospital foyer by clarinettist Deirdre O’Leary and flautist Susan Doyle.

The first prize winner at the 2024 UL Hospitals NCHD Conference was Dr Gideon-Phil Meyer, Registrar Emergency Medicine, UHL for his Quality Improvement project and platform presentation entitled ’Get it on time, Every time: A Parkinson’s Disease Quality Improvement Project’.
The annual conference helps
NCHDs (Non Consultant Hospital Doctors) at UL Hospitals Group enhance their research experience, while providing them with an opportunity to present their research, audit and quality improvement projects from this training year.
More than 150 abstracts were submitted in a cross-faculty
Dr Gideon-Phil Meyer with Dr John McManus, National Doctors Training and Planning (NDTP) Lead, UL Hospitals Group and Consultant Physician; and Professor Tony Holohan, Director, Centre for One Health, Adjunct Full Professor of Public Health, UCD, Adjunct Professor in School of Medicine, Trinity College Dublin and former Chief Medical Officer.
conference at the Clinical Education and Research Centre (CERC) in University Hospital Limerick, incorporating paediatrics, surgery, anaesthetics, medicine, obstetrics and gynaecology, interns, psychiatry, radiology and general practice, with prizes for best abstract presentation in each department.
New audiobook resource reached 1,300 listeners in its first month
A partnership of community and maternity hospital-based mental health services in the Mid West has launched a new audio edition of a successful HSE self-care workbook to support and empower women from conception, through pregnancy and post childbirth.
‘My Perinatal Self Care Workbook’ is the collaborative brainchild of personnel and service-users at Mid West ARIES, Mental Health Services and the Specialist Perinatal Mental Health (SPMHS) team at University Maternity Hospital Limerick (UMHL).
The free audiobook is the latest iteration of a publication that was
released initially in traditional book form in October 2023. It provides an accessible ‘any place, any time’ option for those who wish to make use of the resource while on the go or at home. Providing crucial support for women throughout the perinatal period, the online version of the workbook is available at https:// tinyurl.com/Perinatal-SelfCare-Course and accessing the new audiobook version couldn’t be easier. There is no need for an app download or account set-up – you can simply stream or download it free from: https://tinyurl.com/PerinatalSelf-Care-Audiobook
The idea for the workbook emerged from the feedback of women who attended a workshop on self-care at UMHL in April 2023 at Limerick’s Castletroy Park Hotel, organised by SPMHS team lead and Consultant
Nenagh Hospital staff this summer marked another significant advance in healthcare for women in the Mid West region, with the opening of the first Colorectal Pelvic Floor Clinic at the hospital’s Regional Hub for Women’s Health.
The clinic not only allows patients of the Mid West to access treatment locally for the first time, but also significantly reduces the time between the first symptoms of faecal incontinence and diagnosis and treatment of what can be a very debilitating condition for patients.
Management and staff in Nenagh have been working with colleagues across UL Hospitals Group for more than 18 months to progress the clinic, which is just one of the
services being offered at the hospital’s Ambulatory Gynaecological Unit (AGU).
The Colorectal Pelvic Floor Clinic is the latest in a range of services that have been provided at the AGU since it opened in March 2022, including abnormal intrauterine bleeding, chronic pelvic pain, evaluation of adnexal mass, vulval issues, sexual minority health, and amenorrhea in adolescence.
These services are one-stop ‘see-and-treat’ gynaecology clinics where women can be assessed and treated following a GP referral. This healthcare model aims to improve access to diagnostics and treatment, resulting in fewer hospital visits and reducing overall
Perinatal Psychiatrist, Dr Mas Mahady, and Advanced Nurse Practitioner (ANP), Perinatal Mental Health, Pauline Walsh, with input from Mike O’Neill, manager of Mid West ARIES, the recovery education service for mental health in the region. The content covers the basics of self-care and wellness during the perinatal period, and how to support your physical health, emotional wellbeing, and develop and maintain healthy social connections throughout. There are worksheets and planning aids to help you develop your own personalised self-care toolkit; encouraging messages of hope from women who have been on their own perinatal mental health journey; as well as contact details for a range of community-based support services throughout Limerick, Clare and Tipperary.

wait times for women.
Speaking at the end of the first clinic in the early summer, Ms Christina Fleming, Consultant Colorectal Surgeon and Clinical Lead for the Colorectal Pelvic Floor Service, said she was particularly struck by “the enthusiasm and support of staff for advancing the healthcare of women in this region”.

Showing how easily the audiobook can be accessed on smartphone are: Pauline Walsh, ANP, Perinatal Mental Health Service, UMHL; and Margaret Keane, Education, Training and Development Officer, Mid West ARIES.
This July saw HSE Mid West community healthcare staff and residents from the Thomond and Sarsfield units in Limerick move into the new 50-bedded St Camillus Community Nursing Unit.
Limerick-based HSE Mid West Community Healthcare sites Roselawn House and Castletroy Primary Care Centre ushered out June in style when they were awarded the Silver Level Smarter Travel Mark from the National Transport Authority Smarter Travel Programme.
The Roselawn and Castletroy sites were among the first community healthcare sites in the country to receive the award for their efforts to support active and sustainable commuting and reduction in single person car usage amongst staff.
As part of its Climate Action Strategy, the HSE is committed to achieving net-zero emissions no later than 2050, delivering healthcare which is environmentally and socially sustainable and improving staff health and wellbeing.
"As part of its Climate Action Strategy, the HSE is committed to achieving net-zero emissions no later than 2050"

The bright and modern design provides a far better living environment for residents and brings the accommodation in line with regulatory requirements. Residents, family members and staff welcomed the move into the new Aisling and Saoirse units, which provide replacement beds for existing residents.
At the time of going to press, staff were making preparations for the second phase of the project, with the construction of 25 additional replacement beds.

What is a Medicines List?
Do you keep a list of your medicines? Can you describe and discuss your medicines with healthcare professionals and family when you want to? The HSE encourages everyone who takes regular medicines to keep an up-to-date list of their current medication by using the HSE’s ‘My Medicines List’. Now available in 52 different languages, ‘My Medicines List’ is a list of all the medicines and supplements you take. Keeping a medicines list can help you know and keep track of your medicines. It can also help you when you are discussing your medicines with a healthcare professional.
“I recognise the importance of encouraging everyone on medication to keep their own medicines list. Healthcare systems are not seamless and the information we share as

individuals contributes to our own safety. The HSE ‘My Medicines List’ provides an excellent template, now available in 52 languages. Medication is the most applied intervention in patient care, an up-to-date medicines list captures vital information for sharing at every healthcare interaction. When the question is ‘what medication are you taking?’, the answer is ‘I have it listed here on my medicines list’.” - Bernie O’Reilly, Chair of Patients for Patient Safety Ireland.

My Medicines List QR code
Where can I get a medicines list?
Hard copies of the ‘My Medicines List’ in English are available via www. healthpromotion.ie and medicines lists are available for download in all 52 languages on www.hse.ie/ safermeds.
The National Medication Safety Programme has also created a video with comprehensive guidance on how to use a medicines list, also available on the Safermeds website or at https://www.youtube.com/ watch?v=-92LfGenHbo .
At some point in our lives, we all take medication. For those of us who take multiple medications daily, it can become confusing to keep track. While it is a simple tool, keeping a medicines list is a handy resource that has been shown to help reduce medication related harm. It is helpful for patients and all those involved in their care including GPs, pharmacists and family members.
We encourage everyone on medication to keep and regularly maintain your medicines list. Share these resources with family, friends, colleagues and networks.
Sheila Lucey is a public health nurse and lactation consultant based in West Cork. She welcomed the recent updated guidance for staff on the prevention and management of common breastfeeding issues.
“There can be a continuum from engorgement to ductal narrowing to non-infective mastitis to infective mastitis and to breast abscess. It’s important that all staff caring for breastfeeding mothers and babies give consistent, evidence-based advice to mothers, and to know what’s no longer recommended,” she said, referring to the new fact sheet for healthcare professionals, which can be found at hse.ie.
She recently provided support to Kelsie, a mother of two living in Schull, helping her overcome persistent blocked ducts and mastitis with her daughter Halle, now aged one year and two months.
“I met Kelsie multiple times over the last year and got to know her and her daughter Halle well during that time. When I first met Kelsie, we discussed what her breastfeeding goals were and, as problems arose, I saw her more regularly at my clinic or at the breastfeeding group in Bantry.
“Kelsie’s had troublesome and
persistent blocked ducts on one side in particular, which can be common. Kelsie is also mother to her three-year-old son, so she did very well balancing caring for her new daughter Halle and overcoming more issues second time round with breastfeeding.
“I encouraged Kelsie that it was perfectly safe to continue feeding Halle even during mastitis and we discussed watching out for signs of starting blocked duct/mastitis. I am delighted to have played a part in helping Kelsie and Halle's breastfeeding journey and I recommend colleagues and mothers to try out local breastfeeding services available in every country, many of which are run by public health nurses.”
Kelsie said she was very grateful for the expert help and advice from Sheila in getting through the persistent issues she had with blocked ducts.
Kelsie described some advice that helped her – this included putting cold face cloths from the fridge to the breast after a feed and sometimes warm cloths before a feed helped to get the milk flowing. She also needed to take the antibiotic Flucloxacillin on two occasions after her symptoms were not resolving.
“It’s important that all staff caring for breastfeeding mothers and babies give consistent, evidence-based advice to mothers, and to know what’s no longer recommended.”

Kelsie said her experience of breastfeeding both her children was very different. She would advise mothers experiencing issues with blocked ducts to follow advice from a trusted healthcare professional such as a lactation consultant, as it can be confusing with many people offering advice.
“I wouldn’t have been able to breastfeed for eight weeks, let alone exclusively breastfeeding Halle for eight months, without the constant support from the breastfeeding group and help from Sheila,” she said.
National Breastfeeding Week
2024 takes place from October 1st to 7th and this year’s theme is ‘supporting you from bump to baby and beyond’.
Parents can get breastfeeding advice on mychild.ie






Tá sé mar aidhm ag Acht na dTeangacha Oifigiúla in Éirinn 2021 cur le húsáid na Gaeilge i seirbhísí poiblí agus cuireann sé dualgais nua ar FnaSS agus ar eagraíochtaí eile san earnáil phoiblí.
Faoin Acht ní mór go leor faisnéise agus acmhainní FnaSS a chur ar fáil i nGaeilge agus i mBéarla. Is ceanglas dlíthiúil é seo do sheirbhísí poiblí san áireamh FnaSS. Baineann sé le gach ball foirne agus tá sé riachtanach:


• an Ghaeilge bheith le feiceáil ar dtús, roimh an Béarla (mar shampla i gcomharthaí, faisnéis, tuarascálacha bliantúla agus ríomhphoist)
• ní cheart go mbeadh an téacs sa Ghaeilge níos lú ná an an téacs sa Bhéarla
• caithfidh aistritheoirí Gaeilge atá cáilithe aistriúcháin a dhéanamh. Ná húsaid seirbhísí ar líne/idirlíon mar ní chomhlíonann siad na caighdeáin Ghaeilge atá riachtanach. Chun cruinneas a chinntiú tá sé riachtanach go mbeadh cainteoir líofa Gaeilge chun athbhreithniú dheireanach a dhéanamh ar chomharthaí, plaiceanna agus eolas clóite.




Ó tháinig an t-eagrán deireanach de Health Matters amach, táimid ag obair ar acmhainní Gaeilge atá éasca le húsáid a chur ar fáil don fhoireann. Cabhróidh na hacmhainní nua seo leat na ceanglais dlí a bhaineann le gach ball foirne de chuid FnaSS a chomhlíonadh. Tá treoirlíne dhátheangach clóite againn anois don fhoireann agus tá eolas gréasánbhunaithe don fhoireann maidir le conas na hoibleagáidí dlíthiúla a chomhlíonadh curtha ar fáil againn www.hse. ie/irishresourcesforstaff



D’fhostaithe san earnáil phoiblí a bhfuil Gaeilge acu agus ar mhaith leo líonrú le fostaithe eile i nGaeilge san earnáil phoiblí www.greasangaeilge.ie
San áireamh leis na hacmhainní ar líne seo an t-eolas seo a leanas maidir le hAcht na dTeangacha Oifigiúla (OLA):
• Cumarsáid scríofa

• Páipéarachas agus comharthaí
• Ainmneacha, seoltaí agus teidil foirne
• Fógraí taifeadta

• Freagraí ríomhphoist uathoibrithe
• Fógraíocht (earcaíocht agus fógraí poiblí san áireamh)
• Lógónna
• Foilseacháin
• Gearáin faoi sháruithe OLA
• Cumarsáid phoiblí nach bhfuil clúdaithe faoin OLA
• Acmhainní aistrithe (frásaí úsáideacha, teidil foirne, comharthaí agus leathanach gréasáin)


Má tá aon tuairimí nó ceisteanna agat maidir le hAcht na dTeangacha Oifigiúla i FnaSS seol ríomhphost led’ thoil chuig ATO@hse.ie
Buíochas agus go n-éirí an t-adh libh!
Ins an eagrán seo, táimíd ag fágaint slán lenár beirt Oifigigh Ghaeilge.


Thugadar an-tacaíocht do sheirbhísí an FSS (HSE) ins na ról acu, ag cur chun cinn na Gaeilge agus ag comhlíonadh ár ndualgaisaí fé Acht na dTeangacha Oifigiula.
Le blianta beaga anuas, is leis an Rannóg Cumarsáide agus Gnóithí Poiblí san FSS (HSE) atá Bairbre Uí Thaighneáin (bunaithe sa Tulach Mór) agus Carmel Mac Domhnaill (bunaithe in Luimneach) ag feidhmiú.
Thar ceann na seirbhísí uile agus lucht fóirne go léir a fuair a comhairle agus tacaíocht, gabhaimíd fíor buíochas do Bhairbre agus Carmel agus guímíd gach rath orthu agus iad éirithe as.


Míle buíochas: go n-eirí an bóthar agus slán libh.







Ireland’s Official Languages Act 2021 aims to enhance the use of the Irish language in public services and gives new duties to the HSE and other public sector organisations.
Under the Act, lots of HSE information and resources have to be provided in Irish and in English. This is a legal requirement for public services including the HSE. It applies to all staff and it is essential that:

• Irish appears first, before English (for example in signs, information, annual reports and emails)

For public sector employees who speak Irish and would like to network with other public sector employees in Irish visit www.greasangaeilge.ie

• the Irish language must not be smaller in size than English text
• qualified Irish translators must carry out translations. Translations must not be done through online/internet services as these do not meet the standards of Irish required. To ensure accuracy it is essential that you have a fluent Irish speaker to review any signs, plaques or printed information before sign-off.

Since the last edition of Health Matters came out, we have been working to provide easy to use Irish language resources for staff. These new resources will help you meet the legal requirements that apply to all HSE staff. We have now have a printed bi-lingual guideline for staff and web-based information for staff on how to meet the legal obligations: www.hse.ie/irishresourcesforstaff

• Automated email replies
• Advertising (including recruitment and public notices)
• Logos
• Publications
• Complaints about OLA breaches
• Public communications not covered under the OLA
• Translated resources (useful phrases, staff titles, signs and webpage)


If you have any comments or queries in relation to the Official Language Act in the HSE please email them to ATO@hse.ie



These online resources include the following information:
• Information on the Official Languages Act (OLA)
• Written communications

In this edition we want to say many thanks to our two Irish Language Officers who have been instrumental in promoting Irish and supporting HSE services to meet their duties under the Official Languages Act. Bairbre UiTheighneain (Tullamore) and Carmel MacDomhnaill (Clare) have been working in the HSE as Irish Language Officers, most recently assigned to the Communications and Public Affairs Division. On behalf of all the services and staff who were helped and supported, we would like to wish Bairbre and Carmel a happy and healthy retirement.

• Stationery and signs
• Names, addresses and staff titles
• Recorded announcements

Míle buíochas: go n-eirí an bóthar agus slán libh.




I want to update you on the work underway in the West and North West as we stand up our regional structures.
Over the past number of months we have been putting our health region management team in place. This team will support the delivery of patient services across the whole region and is an important building block for the rollout of integrated care for our communities.
We now have most of this team in place and hope to finalise the remaining roles in the coming months. This team will take up their new roles on 1st October allowing us to work collaboratively to achieve the best possible health outcomes for people living in our region.
This is really important as we bring all of our services in counties Donegal, Sligo, Leitrim, West Cavan, Mayo, Roscommon and Galway together.
The transition to Health Regions is an opportunity to enhance how and where we provide healthcare. It will allow us to plan and deliver our services around the specific needs of our population in the West and North West.
One of my priorities as REO is to make sure that we integrate our services as much as we can and in ways that are meaningful for our patients.
The patient is the ultimate beneficiary when the structure allows for decision-making to be made regionally and locally.
I also believe our staff will see a major improvement in how they are able to carry out their work and care for their patients under the new structure.
We continue to be in a period of change, and that can be challenging for all of us as we adapt to new structures and new ways of working, but one thing that won’t change is our commitment
“The patient is the ultimate beneficiary when the structure allows for decision-making to be made regionally and locally."
to our patients. I’m deeply appreciative of the impact all our staff make on the health and wellbeing of our communities.
As we enter autumn I want to take the opportunity to encourage all our staff to get their booster vaccines. We know healthcare workers are at increased risk of exposure to flu and COVID-19 and I would urge all staff to protect themselves and others with vaccination.
I’m looking forward to working with all our staff across the region to deliver an integrated and progressive health service for the population we serve.
"We know healthcare workers are at increased risk of exposure to flu and COVID-19 and I would urge all staff to protect themselves and others with vaccination."

Ringing the bell on the completion of her cancer treatment, 22-year-old Nora Goaley shares her special moment with Patricia Gleeson, CNS in the AYA Cancer Service at GUH.
A university student who was supported on her cancer journey with specialist services for teenagers and young adults has praised the supports on offer.
AYA (Adolescent and Young Adult) Services provide specialised care to patients aged between 16 and 24 year old who face unique challenges in their journey.
Nora Goaley (22) from Corofin in Galway has attended the
Disability Services Sligo, Leitrim and West Cavan (SLWC) are the first in the country to roll out simulation education within Intellectual Disability Service (IDS).
The Centre for Nursing and Midwifery Education (CNME) has teamed up with the Simulation Committee in Sligo University Hospital and the Intellectual Disability Services SLWC to devise a method of bringing simulation to those working within IDS.
The project has been hugely successful and staff are embracing and enjoying this new way of learning. It has been running since September 2023. Simulation takes place fortnightly in community settings throughout SLWC.
AYA service at Galway University Hospital throughout her cancer journey.
“In April 2023 I was diagnosed with Hodgkin’s lymphoma and entered the AYA service. The support of this service has meant so much to me. If I needed any advice or any help understanding my diagnosis even more, I was able to contact the service and that was such an amazing help to me and my family.
“The service also supported me through college and ensuring I was able to do my exams at a later date. Having this support allowed me to carry on being able to do everything I wanted to do and have somewhat of a normal life, as well as balancing this diagnosis,” she explained.
AYA services provide a holistic approach to young patients living with and beyond cancer. The AYA service carries on beyond chemotherapy into the time when a patient enters remission. Support is provided by a group of physicians, specialised nurses, social workers and psychologists to help the young person get back to their peer groups, get back to school and to help them with any potential long-term side effect such as depression.
Patricia Gleeson, Clinical Nurse Specialist in the AYA Cancer Service at GUH, supports young patients and their family and works alongside their treating teams, whether that is medical oncology, haematology, palliative care, radiation oncology or surgery.
“I understand the unique and different needs of young people with cancer and I am available to support those needs throughout their cancer journey,” she added.
By providing onsite simulation education, staff are empowered to incorporate up-to-date evidence-based practice into improving the care they provide on a daily basis. The simulation education is tailored to address the bespoke needs of each unit.
Service users from the Disability Services in SLWC have recently moved from residential living to community living. This has been a time of unprecedented change for staff and people with intellectual disabilities. Simulation education provides staff with the knowledge they require to negotiate and thrive in their new working environment whilst optimising the care and support they provide.
One year after launching in Donegal, the HSE Pathfinder team has been called out to the homes of more than 500 older people in the region, and managed to keep 81% of patients safely at home.
Letterkenny Pathfinder is also the first pilot site nationally to trial an innovative new point-of-care blood test. The bedside blood test means the Pathfinder Advanced Paramedic can analyse patient blood samples for dehydration and infection markers in their own home and relay the results directly back to their GP for a decision about their onward care.
Pathfinder is a partnership between the National Ambulance Service (NAS) and Letterkenny University Hospital (LUH). The team respond to 999/112 calls for older people (over the age of 65) with the aim of assessing and treating the person in their own home. The national programme was rolled out in the Letterkenny region in April 2023.
Raphoe couple Claire and Frank Laird have shared their experience of using the service in recent weeks. Frank became unwell at home and their GP called for an ambulance. The Pathfinder team were able to treat Frank at home instead of bringing him to the emergency department, and with targeted supports and a number of follow-up visits including physiotherapy, the team helped to get Frank back on his feet again.
“I can’t say enough about the Pathfinder team. Frank was adamant he didn’t want to be admitted to hospital and the team made several visits to ensure he had everything he needed and was recovering well at home. They were a great support to both of us, he was a star pupil and responded really well, thanks to all the extra help we got. I’d love for more people to know about Pathfinder, because it’s such a fantastic service,” said Claire.

Rebecca Swann, Senior Radiographer; Patricia Lee, Support Services Manager; Georgina Kilcoyne, Assistant General Manager, SUH; Ann Marie McGovern, Catering Manager; Martin Casserly, Environmental and Waste Co-ordinator; and Morna O’Hanlon, Health Promotion and Improvement Officer.

Sligo University Hospital (SUH) has been awarded its second Green Flag after a successful re-certification audit by An Taisce. The internationally recognised Green Flag was awarded following a rigorous assessment process. It recognises the commitment of hospital management and staff, HSE Estates, the NUI Galway Medical Academy and the hospital’s Green Campus Committee to developing the hospital as a healthcare facility delivering both high-quality care and improved public health and wellbeing in an environmentally responsible and sustainable way.
Martin Casserly, Environmental and Waste Co-ordinator at SUH, said: “This second green flag has been awarded in recognition of SUH’s commitment to a sustainable health care system and greener campus.
“Sligo University Hospital has implemented a number of successful initiatives to date relating to energy, waste, water, and biodiversity. Such initiatives have included the phase out of single-use cups from the canteen, a tap replacement programme to reduce water wastage, the installation of an onsite food composting unit to compost hospital generated food waste and the creation of the SUH Garden project to preserve and enhance biodiversity on campus.”
University Hospital Galway (UHG) has become the first hospital in Ireland to introduce a new device designed to help patients suffering from heart failure better monitor their fluid levels in the body. Sheila Concannon from Spiddal was the first patient in Ireland to be fitted with this early warning sensor which alerts medics to the patient’s condition worsening.
Over 10,000 new cases of heart failure are diagnosed annually in Ireland; it is a significant public health priority with patients requiring frequent hospitalisations. Patients with heart failure are commonly advised to closely monitor signs of swelling and other symptoms like fatigue, shortness of breath and chest pain. Despite these measures, many patients end up back in the hospital within months after a heart failure hospitalisation, often due to fluid build-up in the lungs.
This new sensor directly measures the volume of fluid build-up, allowing cardiology teams to monitor patients remotely, which can help avoid
Professor Faisal Sharif, Consultant Interventional Cardiologist at UHG, with Sheila Concannon, patient.

unnecessary visits to hospital. The device gives clinicians access to real-time information about their patient’s heart health which in turn results in more rapid interventions.
This procedure was carried out as part of a clinical trial led by Professor Faisal Sharif, Consultant Interventional Cardiologist at UHG.
“Since the implant, I haven’t had to travel to hospital as often as I used to and it takes just a couple of minutes to do my readings and saves me so much time instead of coming all the way to hospital. I can’t even feel the device is there which is great. I am very thankful to Dr Sharif and his team for all their continued help and support.”

The new ED facilities will be constructed in the courtyard connecting into the existing ED. The existing ED will also undergo major refurbishment as part of the plans.
The ED extension will provide additional patient cubicles including isolation facilities, a gynaecology treatment suite and associated staff
and clinical support facilities. This extension will support full separation of adult and paediatric care. There will also be a significant improvement in streaming of patients and resuscitation facilities for critically unwell patients presenting to the hospital. The ground floor also has a single storey
section to provide extra support accommodation for the emergency department.
The AMAU is designed to support the ongoing development of the acute medical programme with patient assessment cubicles, isolation facilities, and private spaces for patient consultations. This unit is designed to receive the patient directly from their GP and transfer, when appropriate, to the ED. This unit is linked directly into the inpatient services and will form part of an acute unit.
Catherine Donohoe, Hospital Manager at MUH, said, “We are delighted to be progressing this essential project which includes the expansion and renovation of the ED and a new AMAU at Mayo University Hospital. This project will have a transformative impact for our hospital and will result in a much better patient experience.”

The Irish summer showers did not dampen spirits in St John’s Community Hospital recently, with the hosting of the first Wise Roots age-friendly festival.
In fact the event was such a success, it has been decided it will become an annual event.
Residents, patients, staff, families and friends old and new, gathered together to enjoy the musical talents from local legends and meander through the craft stands from creative artists.
Bridget and Tabby Callaghan opened with a performance that had the hospital rocking. The Kelly family followed with a toe tapping traditional music session that saw some avid dancers take to their feet.
The Sligo Age Friendly ambassador, Sandy Kelly, was the headline act with an array of memorable songs for all to enjoy. The Sligo-Leitrim Filipino Association Dancers wowed the crowd in colourful costumes with

a traditional and cultural Philippine folk dance called Singkil. To wrap up the show, St John’s Community Hospital's own superstar Seamie Cawley performed some classics with a little help from Ruby, a greatgranddaughter of one of the residents.
Nicola Scanlon Fox, Director of Nursing at St John’s,


Clockwise from left to right: Tabby and Bridget Callaghan’s energetic performance had the hospital rocking; the Sligo-Leitrim Filipino Association Dancers wowed the crowd in colourful costumes; residents, families and friends enjoyed a variety of musical performances; Special guests Sandy Kelly and Sligo Rose Megan McCormack.
said, “The atmosphere was amazing through all areas of the hospital, with heart-warming scenes of residents and their families making memories and enjoying an afternoon of entertainment. A huge heartfelt thank you to all our musicians and artists and all staff who participated. Staff were rewarded for their hours of planning and organising with remarkable job satisfaction to see the event plans come to reality.”
“The atmosphere was amazing through all areas of the hospital, with heart-warming scenes of residents and their families making memories and enjoying an afternoon of entertainment."
See festival highlights at https://youtu.be/Dnfri3NxJsM

The introduction of a NurseLed Urology Clinic at Roscommon University Hospital for Lower Urinary Tract Symptoms (LUTS) has significantly enhanced patient care, reduced wait times, while also reducing the number of patients who require consultant urologist review.
The clinic was established to provide a focused targeted urological assessment of symptoms, as well as treatment, support, and education to enable patients to manage their urological condition without surgery and to reduce wait times for LUTS assessment and management.
Prior to the commencement of the Advanced Nurse Practitioner (ANP) LUTS clinic in February, patients requiring ongoing nursing management or intervention were referred to University Hospital Galway. Wait times from referral to review have decreased from one to two years to six to eight weeks at present, with 156 new patients assessed between February and June.
LUTS and specifically male LUTS is one of the most prevalent complaints presenting to urology outpatients. Research conducted by the National Clinical Programme in Surgery (NCPS) revealed that male LUTS is one of the more common causes for referral to a urologist in the Saolta University Health Care Group.
Michelle Healy, ANP and Clinic Lead, said, “We are providing care to patients as close to home as possible and our patients always comment on how easy it is to travel to Roscommon, and how tremendous the service is. So it's wonderful to see that the clinic is already making a significant difference in the lives of our patients.
“This clinic is the first step towards a more comprehensive approach to LUTS care. It will ensure that patients are assessed and treated in a timely manner, that patient outcomes improve while hospital admissions are reduced, and free up consultants to see patients with more complex urological conditions.”

The newly updated HSE National Records Retention Policy provides guidance on how to manage records, including how long to keep each type or category of record. This policy, which was updated in April 2024, replaces earlier versions. You can find this updated guidance on the revised HSE record retention policy on the staff webpages in the proceduresguideline section.
https://healthservice.hse.ie/staff/ procedures-guidelines/recordretention-policy/ This version includes information on types of data and how long to keep each type of record.
As a HSE employee, you are responsible for:
• managing records correctly
• reading and understanding the sections of the policy that apply to your area of work
Our responsibilities around managing HSE records correctly includes old files in locations that may be no longer in use.
“HSE staff and managers must manage records in accordance with the HSE’s retention periods outlined in the policy, and any relevant laws or regulations. We are asking and encouraging all of our staff and managers to become familiar with the updated policy and the requirements around managing all records. This updated policy replaces earlier versions and a list of records and their definitions are included in the policy. In revising this policy, the HSE acknowledges its General Data Protection Regulation (GDPR) responsibilities.” - Ann Sheehan, the Policy Programme Lead for National Records Retention.
The length of time to keep records varies according to the type of data or record, and the reason for keeping it. Full details are in the newly updated policy.
In accordance with the GDPR principle of 'storage limitation', you should only keep data for as long as it is required. Ensuring that records are destroyed when no longer needed reduces the risk of information becoming irrelevant, excessive, inaccurate, or out of date. Retaining records beyond the required period increases the risk of a data breach.
The retention period of records containing personal information must be recorded in your service’s Record of Processing Activity (ROPA). This is a legal requirement under Article 30 of the GDPR Act. You will also find guidance on how to complete a ROPA, including a template on the HSE staff webpages.
Each service area is responsible for applying this policy to their records and creating a local implementation plan. Both physical and digital records should be managed properly.
If you're unable to comply with any aspects of this policy, email the national records retention team at nrrp@hse.ie for support.
Ann Sheehan, Policy Programme Lead for National Records Retention Email: nrrp@hse.ie
To celebrate World Water Day, HSE Capital and Estates, through its Green Healthcare Programme, ran an online Introduction to Water Efficiency Training for Healthcare Staff.
By conserving water, we can protect this valuable resource, along with reducing water and energy bills.
HSE Capital and Estates Sustainable Infrastructure Office provides a range of supports, via its Regional Sustainability Officers, to Energy and Green teams and support their efforts to conserve water including: providing technical training for healthcare facility, maintenance and estates staff; undertaking water surveys to develop metering plans and identify water saving projects; developing case studies and guidance; collaborating with Uisce Eireann; and supporting acute hospitals participating in the Water Stewardship Programme.
To deal with the growing health impacts of climate change, we aim to reduce food waste by 50% by 2030.
To mark National Food Waste Recycling Week, HSE Capital and Estates through its Green Healthcare Programme held an online webinar featuring case studies in two HSE acute hospitals. The food waste reduction benefits of Real Time Patient Food Ordering at Our Lady of Lourdes Hospital Drogheda was presented by Dolores Donegan, Programme Manager in RCSI Hospital Group. The introduction of On-Site Food Waste Recycling in Sligo University Hospital was presented by Ann Marie McGovern and Martin Casserly, Catering Manager and Environmental and Waste Management Coordinator in Sligo University Hospital.
The HSE is committed to reducing food waste by providing Food Waste Reduction Training for all staff (for more information contact sustainable.infrastructure@ hse.ie), applying a food waste compositing system and a brown food waste bin in healthcare facilities, and using technology to assist with food waste reduction.

Laura Burke, Director General, EPA, and Dr Philip Crowley, National Director Strategy and Research HSE, at a recent ‘Environment, Health and Wellbeing’ event hosted by the HSE, EPA and the Economic and Social Research Institute (ESRI).
Recognising their mutual commitment to protect and enhance human health and the environment, the HSE and the Environmental Protection Agency (EPA) recently agreed to work together.
The work will include promoting the role the environment plays in improving the health of the population and protecting people from environmental risks to their health and wellbeing with a ‘one health’ lens.
Together, they will implement the complementary actions in the recently published HSE Climate Action Strategy and across our health service and audiences.

The Caring with Pride: LGBTQI+ Healthcare Across the Lifespan Conference took place in Dublin Castle recently. The event was hosted by Linn Dara Schools, Children's Health Ireland (CHI), Children's Health Foundation and HSE Dublin South Kildare West Wicklow Community Healthcare. It aimed to advance inclusive healthcare for lesbian, gay, bisexual, transgender, queer/questioning and intersex (LGBTQI+) individuals throughout their lives.
The annual conference serves as a vital platform for sharing the latest research, lived experiences and insights into the implementation of the HSE
Rainbow Badge. This initiative focuses on improving healthcare for LGBTQI+ people. The conference provided an essential opportunity to listen, learn and reflect on the unique challenges faced by the LGBTQI+ community in health services. It also highlighted progress and launched the updated HSE Rainbow Badge Implementation Toolkit—a valuable resource for anyone supporting inclusive healthcare in their workplace.
This year’s gathering saw over 200 enthusiastic delegates engaging in dynamic presentations, lively panel discussions, and inspiring
Conference organising committee: Anne Kehoe, Dani Hall, Matt Swain, Angela King, Mike Healy, Margaret McQuillan, Karina Grehan, Laura Finnegan, and Michael Foley.
abstract and poster presentations. Delegates included experts, researchers, service providers and service users.
LGBTQI+ individuals face unique healthcare challenges, including increased risk of poor mental health and higher rates of self-harm and suicidal ideation compared to their heterosexual peers. Eyeopening research by BelongTo and Trinity College revealed that three out of four LGBTQI+ service users in Ireland feel their healthcare providers lack the necessary knowledge and confidence to address LGBTQI+ issues.
Delegates also heard about the progress of the HSE Rainbow Badge initiative and the importance of promoting inclusivity and support for LGBTQI+ individuals across their lifespan.
Mike Healy, Director of Nursing, Mental Health Services, provided an overview of the Rainbow Badge's development in Ireland and showcased the new updated toolkit. He emphasised that the HSE Rainbow Badge initiative empowers healthcare staff to create an open, nonjudgemental and welcoming space for all.
If you are interested in rolling out the Rainbow Badge in your area, find the updated HSE Rainbow Badge Implementation Toolkit at https://www.hse.ie/eng/services/ list/4/mental-health-services/camhs/linn-dara-inpatient-unit/hse-rainbow-badgeimplementation-toolkit.pdf



















September marks World Alzheimer’s Month, an annual opportunity to raise awareness for dementia internationally and to challenge any stigma surrounding the condition. The HSE’s Dementia: Understand Together campaign aims to do this, 365 days a year, and is proud to stand in solidarity with over 64,000 people with dementia in Ireland, their carers and supporters.
One of the greatest ways we can help people understand more about dementia, is to tell their stories.
Jennifer Manning, a Clinical Nurse Manager from the Community Hospital of the Assumption in Thurles has recently helped to do just that by supporting filming at the Thurles Memory Café in The
Bookworm book shop, which takes place on the first Wednesday of each month. The video will help share the experiences of Marguerite Keating, who has young onset dementia, and is working with Jennifer and the team to grow and promote Memory Cafés at a wide range of venues and dates across Co Tipperary.
Jennifer explained, “We were delighted to showcase the Thurles Memory Café as part of this video series. We have a great bunch of people attending from all walks of life. We have great fun together while sharing important information about health and wellbeing and giving practical advice and support. Marguerite has been integral in helping to grow the number of


memory cafés in Tipperary, she inspires people to get involved through her boundless enthusiasm and I’m sure a lot of people see her and think – if she can do it, well then so can I! That’s why storytelling is such a great way of helping others to see just what can be done when we work together. I hope people see the videos and think about what they can do to welcome and include people with dementia in their own communities.”
We know that there are initiatives like this up and down the country. Community champions and national partners are holding inclusive walking tours, art exhibitions or sing-alongs, making their spaces, beaches and parks accessible and talking about dementia to colleagues and customers.
This World Alzheimer’s Month we’re encouraging all staff to help us tell these stories to highlight the importance of social inclusion and creating dementia inclusive communities. We hold regular sessions with community champions to share practical examples of things they are doing on the ground, and we can put you in touch with staff-led initiatives and like-minded champions in your local area.
There is a wide range of resources to help you and people in your community, from training options to templates for social media and local news. You can sign up to receive regular newsletter updates at www.understandtogether.ie/get-involved or email us at understandtogether@hse.ie

Since I commenced as Regional Executive Officer (REO) of HSE Dublin and South East, I have been delighted to witness the breadth of integrated work ongoing throughout our region. Our Enhanced Community Care (ECC) programme, for example, delivers care closer to people’s homes, shifting care to the community, a fundamental principle of Sláintecare.
We have been working to define the boundaries of our three Integrated Health Areas (IHAs). The IHAs will bring together acute and community services in each area, as well as our voluntary providers, and will be crucial to supporting and enabling integrated care.
Following engagement and consultation with a broad range of stakeholders, the boundaries of our IHAs, of which there are three, have been defined as follows: Carlow, Kilkenny and South Tipperary; Waterford and Wexford; and Dublin South and Wicklow.
Each IHA will be led by an IHA Manager who will be accountable for the operational planning and delivery of integrated health and social care services to their local populations.
One of our main priorities for the coming months is to address the pressures on access to our services. We have unprecedented levels of demand on our existing health service delivery model. We must design, scale up and implement a more sustainable, integrated and fit-for-purpose model of service delivery that will allow us to improve access to our services.
Population health is a key priority and central to our health planning. By supporting people to improve their own health, by making healthier choices easier and by looking at health as a societal issue - housing, education and equity - we can have a real impact on health outcomes.
We will continue to engage, communicate and listen to our staff during this period of change. An engaged and committed workforce is key to supporting and driving the service improvement and service redesign required.
I want to once again thank staff for their support to date as we bring our community and hospital services together. As we move forward, change will present opportunities and challenges. I would encourage staff to focus on the opportunities as we work together towards a more integrated health service for the people we serve.
And finally, as we approach the healthcare system’s busiest time of year, I would like to appeal directly to staff to avail of the free vaccination clinics taking place across our region. Vaccination is the safest and most effective way to protect against flu and COVID-19. We know the impact these illnesses can have on our health and the pressure they put on our health system. It is vitally important that we protect ourselves, our loved ones and our service users this winter.

Acute and Community colleagues from across the South East came together on 16th July to discuss the successes and learnings from various Enhanced Community Care (ECC) programmes in the region.
Held in the RCSI Building in University Hospital Waterford, attendees heard multiple presentations including:
• Integrated Cardiology Service for Wexford
• Health Promotion and Improvement: Health Behaviour Change in Practice
• Integrated Diabetic Services in Carlow and Kilkenny
The team from Ireland East Hospital Group who were in attendance.
Eithne Mullen, IEHG’s Director of Strategy, Transformation and Improvement, said, “The event today acts as a great reminder of why ECC is so important. ECC’s ultimate goal is to treat people closer to home, helping them avoid long waits in busy EDs and alleviate pressure on our hospitals. We can see from the presentations today that this is already happening across the South East.”
There was also a poster presentation on the day. The posters allowed the services to illustrate what improvements have been made to the areas they work in and how this has helped keep people out of hospitals.
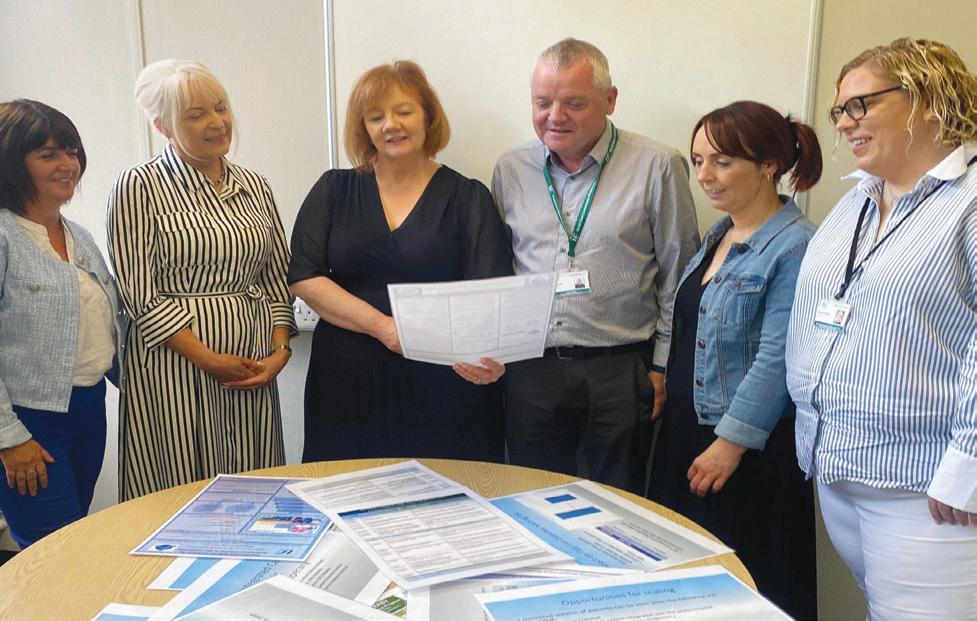
The Shankill primary care team in Community Healthcare East were delighted to receive electric bikes earlier this year. The team worked in collaboration with their Health Promotion and Improvement colleagues and Bleeper Bikes to make this project happen.
The staff bike-share project has enabled them to choose a healthier way of travelling to domiciliary visits.
“It has reduced our car usage and the bikes are a visual reminder to our local community that choosing a greener way to travel will have a better impact on our environment,” said a member of the team.
“Our multidisciplinary team here at Shankill

Primary Care are enjoying the extra fresh air and exercise during their working day. It was a great initiative and we were thrilled to be a part of it.”
A large crowd attended a Health and Wellbeing Fair in the Little Bray Community Centre. The aim of the event, organised by Bray Area Partnership in collaboration with Health and Wellbeing, Community Healthcare East, HSE, was to inform the local community of the health and wellbeing services available to them. The fair showcased a number of Sláintecare Healthy Communities Programme services available to people living in the community, such as the HSE Stop Smoking Service, Parenting Programmes, Healthy Food Made Easy, and Social Prescribing.
Over 20 community-based services involved in delivering a wide range of health and wellbeing supports were on hand to offer advice and answer questions. Healthy snacks were provided to all who attended, and the fair included Healthy Food Made Easy demonstrations and was closed out by the local Chéile Community Choir.
The event was an important development in the Sláintecare Healthy Communities initiative which was launched in Bray two years ago. The event proved to be a fun, interactive and innovative way to connect the community in Little Bray and beyond to local health and wellbeing supports. Another local health and wellbeing fair is planned in Bray later in the year.

Tánaiste Micheál Martin was the guest of honour at Peamount Healthcare recently.
He was on hand to present a Local Hero Award to the staff of St Brid’s Neuro Disability Unit, and to other local recipients of the awards. The awards recognise individuals, groups or services that have made a valuable contribution to the community in the wider Clondalkin area.
An Tánaiste unveiled a plaque marking the occasion, stating, “I am delighted to be invited here at Peamount Healthcare today to acknowledge and celebrate the recipients of the Local Hero Awards. These are groups and individuals who work tirelessly for the benefit of their communities and who ask for no thanks. They represent the true meaning of community spirit. I'm privileged to be able to share the gratitude of the community with them this evening.”
He was also there to mark the reopening of St Luke’s Church of Ireland Church as a meeting and multi-faith room, following a conservation project.
St Luke’s is an early 20th century corrugated iron clad church on the Peamount 65-acre campus. Peamount Healthcare, with the assistance of the South Dublin County Council Architectural Conservation Officer, were a recipient of a grant towards the repair and conservation of the church under the Historic Structures Fund.
The funding made completion of repair and rejuvenation works of this historic building possible, preserving it to be used as a meeting space and safeguarding it into the future. The works included halting the degradation of the building, preserving it as a building of architectural and social significance, and ensuring it would remain as an integral feature of the Peamount Healthcare Campus.
A new ‘Solace Café’ opened on 24th May in Cabinteely, Dublin 18. It is intended for any adult experiencing a mental health crisis or anyone supporting someone in crisis or experiencing a mental health difficulty that is causing emotional overwhelm or a feeling of being unable to cope.
The friendly Solace Café team will welcome you in a warm, supportive environment and support you through listening, signposting and crisis resolution skills.
The café is delivered by Aware in partnership with St John of God’s Community Mental Health Services and
People living with chronic disease are benefiting from SMILE 2, a virtual health support service which monitors their health remotely. Participating patients’ health is monitored daily by a team of triage nurses through wearable devices, offering early intervention and care as needed.
HSE Community Healthcare East. It is a fantastic addition to mental health services offered in the area, and an innovative alternative to A&E during mental health crises that don’t require medical attention.
The café operates out of Urbun Café in Cabinteely, Thursdays to Sundays from 5-10pm. The actual Urbun Café will be closed to the public during Solace Café operating times. Please book ahead on the day through the website www.solacecafe.ie –this is to ensure that the service isn’t crowded in any particular moment and everyone gets the attention they deserve.
The service across counties Carlow, Kilkenny, South Tipperary, Waterford, and Wexford was developed by the HSE in direct response to a need from patients. We know patients with several chronic diseases often end up in the emergency department (ED) or admitted to hospital, often because they don’t recognise the deterioration of their condition and seek support in time.
The remote monitoring and timely advice from the triage nurses is proving effective in addressing this for patients. The SMILE service is delivered by Caredoc out of hours GP co-operative in partnership with the HSE Enhanced Community Care (ECC) programme, South East Community Healthcare and Sláintecare.
Preliminary data collated by the service show that for patients who have been in the project for at least six months:
• 48% have had less ED attendances this year as compared to before they joined
• 52% had less nights in hospital
• 79% have had to attend their GP less on an urgent basis
• 64% have had a reduction in periods of deterioration in their condition, which set off the remote monitoring alerts
Retired ships cook Tony Reck (60s) from Wexford is living with COPD, type 2 diabetes, and arthritis which he attributes to his years on the stormy seas, often having to use his knees as ‘shock absorbers’ in the ships galley during particularly turbulent weather.
“It really gives a peace of mind, knowing your health is being constantly monitored. You don’t always notice changes yourself but the nurses will. Everything is uploaded, all meds uploaded, how you’re feeling, your mood, and general wellbeing are all included. I log in twice a day. If something’s odd, they ring me.”
The first Smoke and Vape Free Homes challenge was successfully delivered in Bray, Co Wicklow. This piece of work was a collaboration between HSE Health and Wellbeing and Bray Area Partnership’s Community Tobacco Worker following completion of a recent local We Can Quit programme.
As part of the Smoke and Vape Free Homes challenge, nine households signed up and committed to a number of pledges to create smoke and vape free environments around the home. The pledges included making rooms in the home smoke and vape free and not smoking or vaping around children, both inside and outside the home.
As part of the four-week challenge participants received a weekly update on topics such as the impact of second-hand smoke as well as weekly phone support from the Tobacco Community Worker. A poster competition, where children from participating households could enter a drawing of a smoke and vape free home, further supported the challenge.
The challenge demonstrates an innovative way to inform people of the harm and risks associated with smoke in the home environment. The challenge does not focus on forcing people to quit but simply encourages and informs participants on the benefits of a smoke free home environment through the pledges they commit to and the weekly content of the challenge.

The Community Healthcare East Wicklow Physiotherapy Service recently held an event to showcase examples of service improvement initiatives taking place across the county. The presentations included a CHO-wide Paediatric Clinical Pathways Project, a Living with Parkinsons class in Arklow, a Rathdrum-based Low Back Pain Programme, and a ‘going greener’ initiative in Carnew to reduce the number of paper referrals. The physiotherapists based within the Chronic Disease Team presented on their Pulmonary Rehabilitation fast-track service, while the Older Person’s Wicklow ICPOP team presented an overview of their service in its first two years. A falls prevention pathway was also highlighted.
The Bray-based Primary Care team demonstrated how they are utilising the new Primary Care Centre to its full potential by showcasing their Low Back Pain Pathway, Total Knee Replacement Class and GLAD programme for knee osteoarthritis, all of which have had a significant impact on waiting times for these conditions.
The event was a huge success and has inspired other members of the team to explore other initiatives that will continue to provide a quality service to all of our Wicklow residents.
“Parkinson’s disease affects everyone in different ways. There are so many ways that it affects people, so accessing something like a physiotherapy and speech group just allows people to maintain their function as it is, and manage their condition a little bit better,” according to Sean Cusack, Senor Physiotherapist, HSE Arklow Primary Care Centre.
“Exercise is one of the best treatments for Parkinson’s disease, so that’s where our group comes in. It can be a very daunting time when someone receives a diagnosis of Parkinson’s disease, but there is a lot of support in the community that can help.
Local primary care centres like ours here in Arklow offer a range of supports to people living with Parkinson’s disease. We offer physiotherapy, speech and language therapy, nursing, occupational therapy, dietetics, psychology and counselling. One important support is a monthly physiotherapy and speech and language group that runs
here in Arklow Primary Care Centre.”
Laura Nuzum, Speech and Language Therapist, Arklow Primary Care Centre, explained, “Typically we would see people individually first for speech therapy. We would run through exercises with them to improve the loudness of their voice, maintain the voice that they have or improve it. Likewise, they would be going to physiotherapy - maybe at the same time.
“We decided to run the group as a maintenance for those exercises that they’ve learned in either physiotherapy or in speech therapy. So they’ve got the benefit of meeting each other and maintaining the exercise and the practice.”
Brian Duane, who attends the weekly group, said that he finds it “reassuring to meet other people who have the same kind of complaints so you know you’re not alone. You pick up bits of information about what’s going on - like the Parkinson’s choir”.
For more information go to the Community Healthcare East YouTube channel.
Community Healthcare’s Carlow District Hospital has joined in the implementation of the national RESIST hand hygiene campaign.
RESIST is a brand for a number of initiatives under the HSE’s Antimicrobial Resistance and Infection Control programme (AMRIC).
One of these initiatives is a rollout of the RESIST hand hygiene awareness programme. The programme promotes a combination of hand hygiene training with standardised national training materials. Hand hygiene has been at the forefront of all of the initiatives that the HSE has been implementing to reduce the spread of COVID-19. The RESIST campaign aims to refresh hand hygiene messages and to keep promoting the importance of clean hands.
Carlow District Hospital is a 17-bed facility located on the HSE’s Athy Road campus in Carlow. The hospital provides short stay transitional care, respite services for older persons, palliative respite care and palliative care support for end of life.
Speaking at the launch of RESIST in Carlow District, the hospital’s Clinical Nurse Manager 2 Noeleen English Hayden said, “Carlow District Hospital has an excellent record in hand hygiene but we are always looking to improve our standards. The RESIST programme will help us to do that and we are delighted to have been selected to be part of the rollout in HSE residential facilities.”
People with musculoskeletal disorders (MSDs) and arthritis often experience challenges at work which can cause temporary and permanent work absences. Work absences have a high cost to both the person (loss of earnings and reduced quality of life) and to the state (cost of welfare payments and reduced workforce).
Work-Able Solutions is an occupational therapy vocational rehabilitation service for people with MSDs and arthritis. It provides early access to individualised evidence-based interventions to help people with MSDs and arthritis remain in or return to work.
This project is funded by the Sláintecare Integration Innovation Fund (2022) for a 24-month pilot and is being led by the National Clinical Programme for Rheumatology; and Dr Yvonne Codd, Assistant Professor in Occupational Therapy, School of Medicine Trinity College Dublin. The pilot is delivering services across Dublin South, Wicklow, Kildare, and Waterford and is linked to St Vincent’s University Hospital, Naas General Hospital and
Thank you to all those who participated in the Community Healthcare East six-day HSE Foundation Programme in Sexual Health Promotion. Delivered by the Community Healthcare East Health Promotion and Improvement team, the course enhances participants’ capacity to incorporate sexual health promotion into their work through
Waterford Primary Care.
Work-Able Solutions is available to working age adults, with an MSD or arthritis, currently in paid employment or in receipt of illness benefit for more than six months, and who have a self-reported work concern. Referrals are accepted from primary care and rheumatology multidisciplinary teams. Each client receives a two-hour initial assessment followed by four one-hour intervention sessions delivered by a skilled occupational therapist. Intervention is flexible in timing and delivery may be face-to face or virtual, and includes a workplace visit. As of March 15th 2024, the pilot has been operational for 10 months and 248 clients have been referred. 40% of these referrals have come directly from primary care. 67% of the clients are female and 30% of the clients are the sole income earners in their household.
The median age is 43 years. Preliminary findings show high work retention at discharge with 73 of the 77 clients who completed the programme remaining in or returning to work.
the development of their comfort levels, confidence, knowledge and skills in relation to sexual health. Course content includes sexual rights and the law, healthy relationships, contraception and STIs, menstrual wellbeing and gender identity. For more information email healthpromotioncheast@hse.ie or visit www.sexualwellbeing.ie.

Procurex Ireland returned to the RDS in April with a mission to innovate, educate and collaborate, connecting buyers and suppliers within the public procurement community. As the largest purchaser in the State, HSE Procurement signalled its continued commitment for engagement with the marketplace and once again championed as an official event partner.
The National Director of HSE Procurement, John Swords, took to the stage and addressed the audience in terms of HSE and public procurement.
Referencing a number of key areas for procurement including sustainability, innovation and the importance of having ‘one voice’ to the marketplace for public procurement, he also emphasised the significance of maximising procurement in providing support for effective and efficient patient care.
Speaking about the new Integrated Financial
Management and Procurement System (IFMS) he said “It will become the single source of information for HSE Procurement to assist the supply base and position our requirements in an accurate way to the market, benefits accrue both sides with that, in achieving maximum value supporting patient care delivery.”
Speaking after the event, he said, “This has been a very positive experience for engaging with in excess of 800 delegates including current and prospective suppliers for the HSE. Our key message has to centre on the importance of the patient being the focus and that all our procurement opportunities should contribute to improved patient care. We have also had the opportunity to network with our public sector colleagues and trade organisations, this collaboration is a very important aspect of making progress together.”
As the largest purchaser in the State with an annual procurement spend of €4.9 billion, the HSE Climate Action Strategy 2023 -2050 signals HSE Procurement as a key enabler and support service to deliver climate action. It is a key mechanism for influencing the environmental and social impact of the products (both clinical and non-clinical) necessary to ensure the safe delivery of healthcare.
The current HSE Corporate Procurement Plan echoes this commitment outlining that the health service will play a central role in delivering green public procurement working in collaboration with the marketplace to achieve sustainability goals.
In this regard, HSE Procurement in partnership with HealthTech Ireland, the Sustainable Enterprise Skillnet and 20FIFTY Partners recently launched a new programme to promote sustainable procurement practices in the healthcare industry.
It involves skills and talent development initiatives to enable a best-practice sustainable procurement approach.
Welcoming the announcement of this new initiative, the National Director of HSE Procurement, John Swords, said, “This approach highlights the importance of linking commercial training to that of public procurement training which will be critical to maximising results.”
The first programme will kick-off in September with further cohorts to follow.

In late 2022, the HSE was approached with an invitation that would mark the beginning of an impactful collaboration with the health authorities in Tanzania.
The Tanzanian Ministry of Health (MoH) and the Tanzania President’s Office for Local Authorities and Regional Government (PORALG) extended the offer, signalling a potential partnership to address critical healthcare challenges in the East African country.
Recognising the urgent need to bolster primary healthcare (PHC) services, the MoH and PORALG identified this area as a top priority for potential collaboration with the HSE. The HSE Global Health Programme embarked on an exploratory visit to Tanzania in April 2023 to lay the groundwork for long-term partnership plans. The collaborative efforts aimed to not only address immediate healthcare challenges, but also to establish a framework for sustainable impact and long-term capacity building.
Integral to the success of this collaboration was the development of national strategies aimed at improving healthcare quality and accessibility, aided by the technical expertise of the HSE.
Furthermore, the collaboration extended to the development of customised quality improvement training for healthcare staff

working in primary healthcare facilities. This initiative aimed to equip frontline healthcare providers with the skills and knowledge necessary to deliver high-quality care.
The collaboration between the HSE and Tanzanian health authorities represents a beacon of hope in the realm of global health. Through strategic planning, capacity building, and customised training initiatives, this partnership aims to drive sustainable improvements in healthcare quality and accessibility.
It highlights the fact that a small amount of support from the HSE can have a big impact on the health and lives of people in Tanzania. And there are benefits for the HSE too. Those involved from Ireland enhance their knowledge of different ways to do things, different health systems and skills such as improved communication and techniques. The Irish service benefits as the employee implements techniques and skills learned.
The HSE Global Health Programme is partnering with the Irish Global Health Network (IGHN) for the upcoming conference, ‘Fostering Humanity: Promoting Health Equity for a Better Planet’, taking place from 2nd to 3rd October 2024. This pivotal event is a special opportunity to delve into critical global health issues, exchange knowledge, and foster partnerships that drive
health equity and sustainability worldwide. IGHN Conference 2024 will cover a wide range of themes such as climate change and health and equity in healthcare. With issues like COVID, the Ukraine conflict, migration and climate change we have a growing appreciation of the transnational nature of health issues, determinants and solutions.
Attendees can avail of 20 CPD points for the full two-day conference. You can get more information and register by visiting IGHN Conference 2024 https://globalhealth.ie/conference-2024/
Clinical Midwife Manager Amy Farrelly, working in the Diabetes Service at the Maternity Unit in the Regional Hospital Mullingar, Co Westmeath says that when women in the midlands with type 1 diabetes discover they are pregnant, she is often the first to know. “Women with type 1 diabetes have called me before they’ve told their partners,” she said.
The risk of diabetic retinopathy may increase during pregnancy. It is a complication of type 1 and type 2 diabetes which can cause the blood vessels in the retina become blocked and damage a person’s sight. However, when retinopathy is caught early, treatment is effective at reducing or preventing damage to the sight.
A new nationwide service for women with diabetes who become
“Over
pregnant was rolled out last year by Diabetic RetinaScreen. The screening programme worked with 19 maternity hospitals, including the Regional Hospital Mullingar, and diabetes healthcare professionals such as Amy to deliver more frequent screening to eligible women. The pilot screening project was supported by the Women’s Health Fund and the initiative is a commitment under the Women’s Health Action Plan.
The introduction of the screening initiative is “brilliant”, Amy explained. “As soon as I get a due date I fill in the form and send it off to the Diabetic RetinaScreen team, and I know the women will be offered eye screening.”


Amy said that when women with diabetes become pregnant, they don’t generally think about their eyes. “They are more worried about the impact of their diabetes on the baby. But the risks for the mammy are just as relevant.”
600 women have been cared for through the new screening initiative. The benefit to these women extends beyond their pregnancy and they have the opportunity to access diabetic retina screening for the rest of their lives."
Over 600 women have been cared for through the new screening initiative. The benefit to these women extends beyond their pregnancy and they have the opportunity to access diabetic retina screening for the rest of their lives.
Will Kennedy, NSS Public and Patient Partnership representative

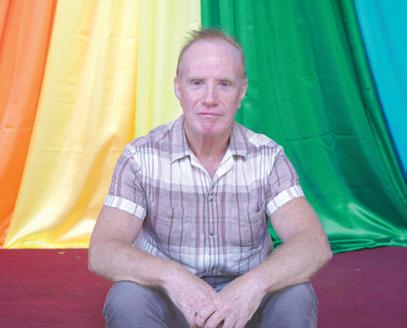
The National Screening Service (NSS) has an active Patient and Public Partnership (PPP). Its PPP volunteers are at the centre of what they do and are involved in their decisionmaking processes.
NSS Chief Executive Fiona Murphy described how important our PPP is to screening. “People who have taken part in screening are often our best advisors. Our commitment is that we will value your input, we will listen to what you have to say and involve you,” she said.
Earlier this year, NSS ran a public campaign to recruit new PPP volunteers from all communities and backgrounds. The campaign ran across social media, websites, press and radio, and internal channels and was shared with our stakeholders. The results from the first week of the campaign were positive with a top blog engagement rate of 51%. The information leaflet and application form had the highest downloads from the NSS webpages. HSELive and Facebook had 12,490 impressions, and LinkedIn had almost 4,000. From over 70 expressions of interest, they currently have 20 applications.
Pivotal to this campaign’s success was the support from two of the volunteers Will Kennedy and Linda Sice Brogan. Along with NSS Chief Executive Fiona Murphy, Will and Linda gave interviews on local radio and to national press.
Will Kennedy joined the PPP four years ago.
“One of the main reasons I joined was because the NSS was developing an equity framework, and as a queer man I felt I could represent people like me. I would have an opportunity to voice the concerns of my community and help to make the service more equitable and equal,” he said.
Linda Sice Brogan has equally found it a positive experience. “Being involved in the Patient and Public Partnership means that we have a voice in shaping services and ensuring that decisionmakers understand how things can be improved, and also know what is working well. It’s very rewarding and I feel heard and included.”
For more information about the campaign and joining our PPP, email ppplead@screeningservice.ie
It is often the people who would most benefit from screening who are the least likely to participate. Research shows that it is through community activation –empowering and informing community healthcare workers and peer educators –that health behaviour change happens within communities.
Since 2022, the National Screening Service (NSS) and the National Cancer Control Programme (NCCP) have been working in partnership with Pavee Point Traveller and Roma Centre in Dublin. Mary Brigid Collins, Co-ordinator of the Pavee Point Traveller Primary Health Care Project, explained the importance of this work.
“We know that disadvantaged groups are diagnosed with cancer at a later stage and have worse outcomes, and that cancer screening plays a big role in the early detection of cancer,” she said.
The partnership involved working with the Traveller Primary Healthcare Workers who delivered peer education and community outreach to Traveller communities in Finglas and Blanchardstown. An important part of this work was the co-design of education sessions with the NSS and NCCP, adapting existing resources to make them culturally appropriate for the Traveller community.
The healthcare workers carried out fieldwork in their communities, providing support, information and resources to people about how to prevent cancer, and about how cancer can be found earlier through screening. A number of people took part in the bowel, breast and cervical screening programmes as a result of the project.


Over the past few months, I have been meeting with my colleagues across the region to discuss how we can deliver the finest care possible. It was great to get out and about and meet with people as we work to stabilise and develop services.
We remain fully committed to developing our services while keeping them on a sustainable footing, and we are committed to delivering the best care for the benefit of the population that use our services as well as for the thousands of staff that work in the region.
We want to expand the initiatives that are working well. This is very important and is currently being achieved by the interim Regional Management Team, operating within the existing structures of Community Healthcare and the Hospital Group.
I had a productive first engagement with the management team about delivering healthcare in the region and identifying the next steps to explore how we can best achieve our goal of an overarching, integrated region.
We have approved a new Regional Director of Finance and Regional Director of People and Culture. We are close to appointing a Regional Director of Planning and Performance and a Regional Director of Communications and Public Affairs and will soon have our full team in place. We are in a time of change and from 30th September, we will be introducing the Integrated Healthcare Areas (IHAs).
Our priority for the coming months is fundamentally to ensure we meet the needs of the
people we serve and we do that by enhancing essential services and improving access to them. It is crucial that we work tirelessly together to achieve this. We will be bedding in our leadership team over the next few months and our leadership must focus on developing a culture of compassion, unwavering patient safety and clinical expertise.
As we move into autumn and winter, our services will be particularly busy. We are encouraging our staff to consider the HSE’s winter vaccination programme commencing in early October.
This includes free flu and COVID-19 vaccination to recommended groups, including healthcare workers.
Flu and COVID-19 are expected to be widely circulating this autumn and winter. Getting both vaccines will protect and support our staff in our critical care services and ensure those caring on the frontline are not overrun, so we can protect the capacity we have for those most in need.
It is essential to take up this opportunity to get the vaccine as early as possible to protect ourselves, each other, our family and the people we are here to support.
We must take this opportunity to take action to improve patient care.
Please continue to work with us as we progress. It will be a tricky time and we don’t have all the answers yet. However, we must work together and continue to display the behaviours of supportive, compassionate and inclusive healthcare.

A Kildare cancer patient believes being on a drug trial at Tallaght University Hospital has kept him alive for the past two years.
John Donovan from Kildare is being treated for an advanced form of kidney cancer at Tallaght University Hospital (TUH). Since November of 2021, he has been taking part in a trial for a new drug called Belzutifan
which, he said, “is after keeping me alive for the past two years.”
John is retired and has three grown-up children and seven grandchildren. He has just turned 70 and lives in Ballintore near Narraghmore in Co Kildare. Five years ago, doctors discovered he had advanced cancer in his one remaining kidney and in his lungs. He was then put on immunotherapy drugs.
In 2021, when John’s medication stopped working and his tumour began to grow again, he was asked if he would like to take part in a trial for Belzutifan, which fights cancer by blocking a key player in its growth process. It is described as a SACT (Systemic Anti-Cancer Therapy), a term which covers all anti-cancer drugs.
Heather Sloane, Clinical Nurse Manager, has been caring for John at the hospital. She confirmed John would not have had access to this drug in Ireland without being part of the clinical trial at TUH. Over 100 patients are currently taking part in clinical cancer trials at the hospital, exploring new therapies for bladder, prostate, pancreatic and renal cancer.
Praising the staff in the Cancer Clinical Trials Unit in TUH, John said, “As well as caring for you they are like a family, the staff in the unit are just wonderful. I feel 100% cared for by Heather, Ashley, Una and Dr Raheel and would recommend taking part in a drug trial to anyone who is offered the chance. We must find new cures for the future.”
With further funding of €8,000 from the National Dementia Office, the Laois/Offaly Psychiatry of Later Life (PoLL) and Cognitive Assessment Service teams focused on promoting access to local services and resources for people living with dementia and their significant others.
Key areas of development included providing access to a local memory technology library, publishing a booklet highlighting supports and services for carers across Laois/Offaly, and staff development training.
The memory technology library has been in operation for the past two years. It has a range of items such as phones, radios and voice activated devices, as well as sensory objects such as weighted blankets and lap mats.
Access to these resources can provide families with an opportunity to consider alternative approaches to support
connection and comfort during different stages of care. The development and publication of the ‘Who Cares?’ booklet aimed to share information on the available supports and services to caregivers across Laois/Offaly. It is a valued resource for local families and care providers. It includes an updated ‘Directory of Supports and Services for Older People in Laois and Offaly’ recently published following the involvement of other local organisations.
PoLL staff members also attended bereavement training to further support families in the service and found it beneficial in their day-to-day work.
“Access to these resources can provide families with an opportunity to consider alternative approaches to support connection and comfort during different stages of care."
The third NCHD Research Competition was hosted recently by the National Doctors Training and Planning (NDTP) Training Leads, Prof Robert Eager and Dr Darragh Shields in collaboration with Prof Martina Hennessy, the Chief Academic Officer (CAO) for Dublin Midlands Hospital Group (DMHG).
The CAO is responsible for developing a structured and integrated approach to research, innovation, education and training for all healthcare professionals in the DMHG. The NDTP Training Leads play an important role in supporting the wellbeing, education and training of non-consultant hospital doctors (NCHDs) across the DMHG.
This year, an extended invitation was given to advanced nurse and midwife practitioners.
The event featured expert speakers who focused on research which aligned with the day's theme. It was a successful opportunity for NCHDs to present their projects on original research, a completed audit cycle or a quality improvement project, to represent their respective hospitals and receive recognition for their efforts.
Additionally, the event provided valuable insights for research enthusiasts, with talks on topics including ‘Getting started in research’, 'Mixed Methods Research', 'Patient and Public Involvement, ‘Inclusive Research’ and clinical trials. The event included a panel discussion focusing on the balance between clinical practice and academic work.
Experienced and early career researchers provided perspectives on professional growth, challenges, and the harmonious relationship between clinical practice and academia. They delivered insightful advice and motivation.
There were seven oral presentations representing Tallaght University Hospital (TUH), Midlands Regional Hospital Portlaoise (MRHP), St Luke’s Hospital (SLRON), St James’s Hospital

(SJH), The Coombe Hospital (CWIUH), Midlands Regional Hospital Tullamore (MRHT) and Naas General Hospital (NGH).
The oral presentations were judged by Prof Hennessy, CAO, Dr Shields, NDTP Training Co-Lead, and Dr Elaine Burke, Assistant Professor in Medical Education, TCD.
The winner of the NDTP NCHD Research prize was Dr Helena Dolphin, a specialist registrar in Geriatric and Stroke Medicine in TUH. Second prize went to Dr Colina Nicholas, a senior house officer in MRHP.
Dr Emer Herlihy (SLRON), Dr Michael Cronin (SJH), Dr Somaia Elsayed (CWIUH), Dr Dineshkumar Subramaniam (MRHT) and Dr Syeda Mona Rizvi (NGH) were highly commended on excellent presentations.
Prof Martina Hennessy, CAO DMHG; Dr Colina Nicholas, SHO in MRHP, who was runner up; winner Dr Helena Dolphin, a Specialist Registrar in Geriatric and Stroke Medicine in TUH; and Dr Darragh Shields, NDTP Training Lead for DMHG.


A multi-disciplinary committee from Laois/Offaly Psychiatry of Later Life (PoLL) has developed an initiative to enhance the care provided to older people living with dementia in the Midlands. They were awarded a quality improvement grant of €8,500 by the National Dementia Office to carry out this work.
The committee includes an advanced nurse practitioner, clinical nurse specialist, speech and language therapist, health care assistant and service users. The aim of the project was to develop a multi-sensory outdoor experience in the garden of the Maryborough Approved Centre in St Fintan’s Campus in Portlaoise.
Following review of dementia-friendly guidelines and conversations with current service users, a design incorporating different scents, textures and visuals was formed. This immersive, tranquil environment with a variety of plants, trinkets and seating is used on a daily basis by service users.
Tribute paid to Ross Murphy at NAS staff memorial annual golf event
Current and former National Ambulance Service (NAS) staff and friends got together at the beautiful Moate Golf Club in Co Westmeath recently to participate in the NAS staff memorial annual golf event.
On everyone’s mind was the untimely passing of paramedic colleague Ross Murphy from Maynooth, Co Kildare, whose funeral took place on the day prior to the event. The golfers paid tribute to Ross by lining up for a minute’s silence before play commenced, as Ciaran Byrne (Keggsy) played a lament on the bagpipes.
The event is held to remember service veterans who have passed on and to raise some funds for a local good cause. Some 38 golfers braved inclement weather as the golf commenced.
The annual celebration is also designed to give retirees an opportunity to meet with former colleagues and keep in touch with the emergency services community.
The outing was expertly organised by Jon Ryan, Advanced Paramedic and Jason Masterson (Newcastle RRV Station). Current and former NAS staff from many areas of the country made the journey to the 18-hole parkland course.
“Everyone had a great day out and Moate Golf Club really welcomed the group,” said Jon. “It was great to see so many retired personnel meet with former colleagues and enjoy a fun day of golf and also remember those who have passed on, particularly Ross Murphy.”

Inclusivity and accessibility for all patients is essential in the everchanging world of healthcare. For neurodivergent people, dealing with the intense stress of an Emergency Department (ED) can be particularly challenging. The ED at Tallaght University Hospital (TUH) is addressing these challenges head-on, setting a standard for neurodiversityfriendly care.
The ED at TUH is supporting the diverse needs and experiences of neurodivergent patients in innovative ways. Central to this initiative is the development of comprehensive guidelines for staff, helping them to effectively communicate with patients who identify as neurodivergent. These guidelines cover a range of communication strategies tailored
to individual needs. They help create a supportive and understanding environment from the moment patients enter the ED.
The ED has also set up a dedicated sensory room. Sensory challenges, such as sensitivity to light and noise, can increase stress and anxiety for neurodivergent people in busy ED environments. The sensory room provides a calming space to relax, away from overwhelming stimuli. This demonstrates the hospital’s commitment to accommodating diverse sensory needs and its dedication to improving the overall patient experience.
Dr Aileen McCabe, Consultant in Emergency Medicine at TUH, emphasised the significance of

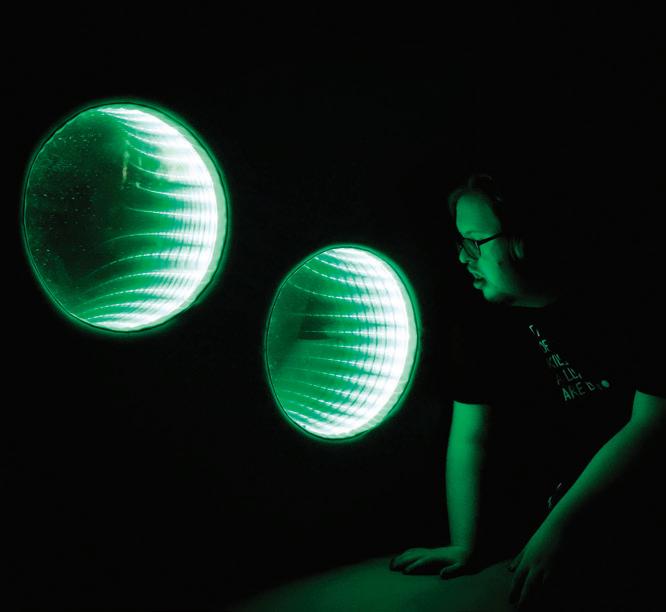

these initiatives.

“Our goal is to ensure that every patient receives the highest quality of care, tailored to their individual needs. By fostering a neurodiversity-friendly environment, we are not only improving patient outcomes but also promoting inclusivity and understanding within our healthcare system.”
Tullamore Ambulance Station crews recently invited the local community to learn about the day-to-day, life-saving work of the HSE National Ambulance Service (NAS).
People with an interest in the National Ambulance Service were asked to drop into the station, located in the grounds of the Midland Regional Hospital, Tullamore. They met the team and learned about the work that NAS does to meet the needs of their local community.
On the day, visitors viewed the range of NAS vehicles and equipment used. In addition, Community Engagement Officer Amanda Ross demonstrated CPR on one of the customised manikins used for training.
A training overview was given by

Phelim Nevin, Education Competency Assurance Manager. Visitors also learned how the NAS College campus in Tullamore is playing a leading role in training and educating Ireland’s next generation of paramedics. The NAS Education Campus in Tullamore has seen many student paramedics successfully complete the degree programme. The campus is one


of three which serves the HSE NAS College, established to deliver essential education to new recruits to the service. The other campuses are based in Tallaght, Dublin, and in Ballinasloe, Galway. Its Midlands location means the campus is accessible to students from all over Ireland, and positioned to deliver first class clinical and operational skills to its students.




Staff from the National Immunisation Office at the National Immunisation Conference.



Careful planning and preparation are required to effectively manage energy supply disruptions. A power outage or loss of heating in a healthcare setting can have serious consequences. It can impact patient and service user care. By planning for this, we can help ensure the safe delivery of services to patients and service users. HSE managers should put measures in place to ensure services are delivered safely.
The HSE checklist and guidance from HSE Emergency Management will support staff and managers in:
• preparing for disruptions to the fuel and energy supply
• developing contingency plans for essential supplies, alternative sourcing, and backup power
• raising staff awareness of contingency plans, including their roles and responsibilities

Emergency management contacts
HSE National Emergency Management Office national.em@hse.ie | 01 778 5122
HSE East Major Emergency Management Office emergency.planning@hse.ie | 01 675 4100
HSE South Emergency Management Office emo@hse.ie | 021 492 1622
HSE West Emergency Management Office emergency.managementwest@hse.ie 091 775 933
You will find the energy disruption guidance, checklists and related supports on the staff section of the HSE website: https://healthservice.hse.ie/staff/procedures-guidelines/
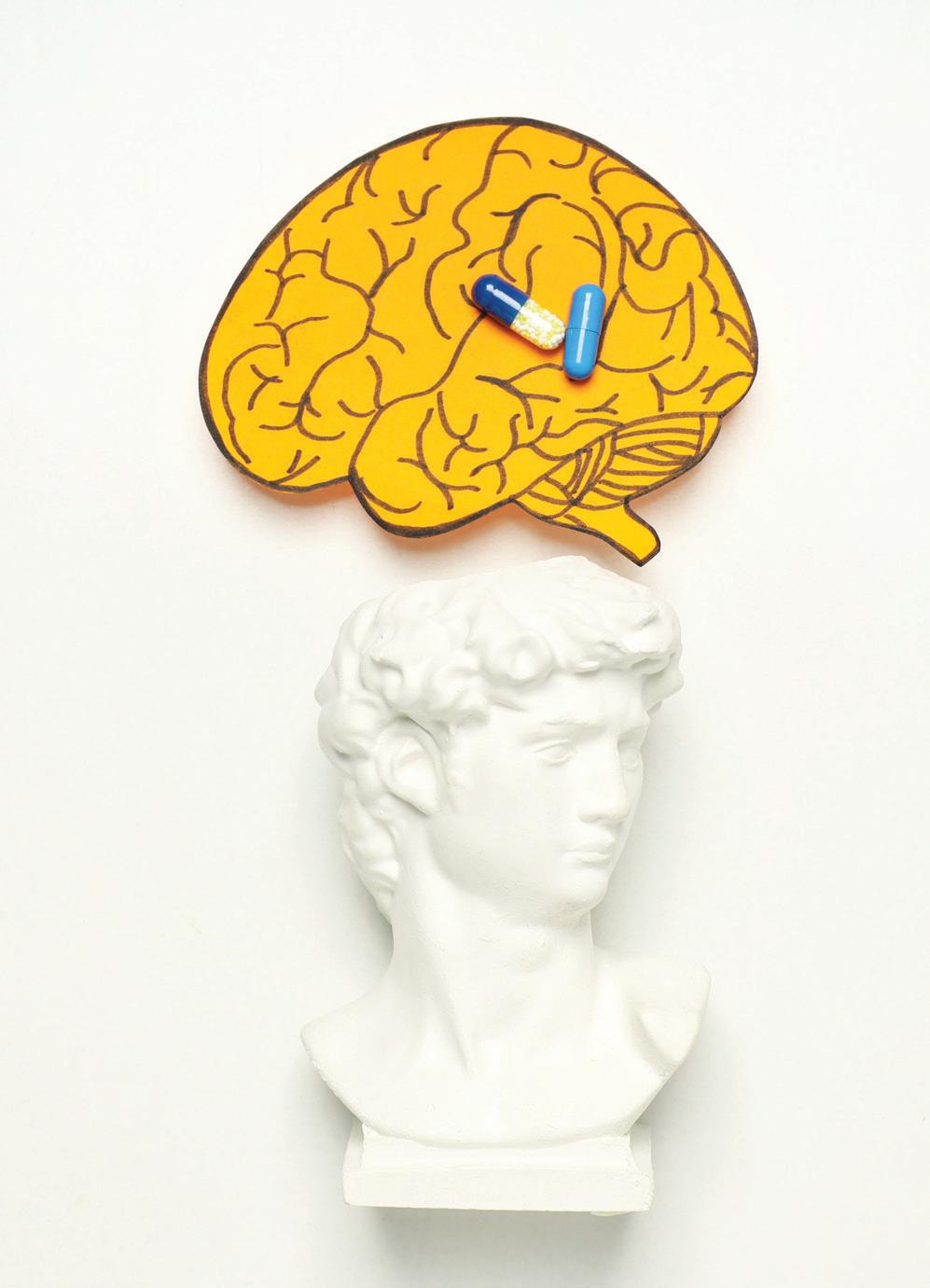
A new Community Cancer Nursing eLearning Programme is now available on HSeLanD.

The target audience for this training programme is primarily registered nurses working in the community setting including: PHNs (Public Health Nurses), community nurses, general practice nurses and nurses working in CIT (Community Intervention Teams). However, any nurse or Health and Social Care Professional (HSCP) who is interested in learning more about cancer and the effect it has on the person should complete the programme.
An Implementation Programme for National Clinical Guideline no. 21 (NCG no. 21; Appropriate prescribing of psychotropic medication for non-cognitive symptoms in people with dementia) is under way by the National Dementia Services. A key element of this is the delivery of a Facilitator Education Programme. The Facilitator Education Programme was piloted in three sites and is currently undergoing national roll-out. As part of the pilot phase, the programme was delivered in Bantry General Hospital.
Staff who attended this education programme became Local Facilitators and delivered a number of education sessions, as outlined below:
• Delivering person-centred care for non-cognitive symptoms of dementia
• Prescriber education: Implementation of NCG no. 21
• Using quality improvement methodology to support the implementation of NCG no. 21
The implementation of NCG no. 21 in Bantry General Hospital has been led by Teresa Bohane, ANP Dementia and Annette Collins, CNS Dementia. Speaking about her involvement, Teresa outlined, “It was fantastic to be involved in the programme. We are very lucky to have had strong clinical and non-clinical management support for this work. Release of staff is an ongoing challenge and what we found worked well was to run the education sessions before or after mandatory education such as manual handling.
“Taking part in the audit and receiving our audit findings has been very helpful to highlight areas where things are working well and other areas where practice needs to improve.”


The programme will ensure that community-based nurses are equipped with the knowledge, skills and attitudes to safely provide care to individuals with cancer at all stages of their cancer journey.

Noreen Galvin, Dementia Quality Improvement Assistant Director of Nursing for the area has liaised closely with the team in Bantry throughout their implementation journey. “Teresa, Annette and their team have worked incredibly hard to make this project a success in their setting. I will continue to support them as they deliver education sessions. This education programme is crucial to reduce inappropriate prescribing of psychotropic medications.”
Find more information about the Implementation Programme for National Clinical Guideline no. 21 and access relevant resources at https://www.hse.ie/eng/dementiapathways/resources-for-practice/ implementation-of-national-clinicalguideline-no-21/


The Home Support Service aims to enable older people to continue to live in their own homes with confidence, security and dignity. The service is highly valued by service users and their families. It also enables many older people to return home following acute hospital admission. To ensure that this service continues to meet their needs, regulation and reform of the Home Support Service is a Government and HSE priority.
The Government, through the Department of Health, is currently finalising legislation to provide for the licencing and regulation of home support services for persons 18 years and over. The legislation will establish HIQA as the regulating authority and once the regulations are issued these will be followed by HIQA




standards. Each provider of home support services will have to comply with the regulations and standards in order to obtain and maintain their licence to provide home support services. Alongside the Government changes, the HSE is designing a new Home Support Service delivery operating model. The new operating model will enable the HSE to be compliant with the home support regulations that are due to be published. It also aims to standardise the delivery of home support services across the health regions. A series of workshops, consultations and meetings have taken place to identify best practice and common issues to inform the new operating model and make sure that it meets the needs of the service users, their families and staff providing home support.
"To ensure that this service continues to meet their needs, regulation and reform of the Home Support Service is a Government and HSE priority."

The HSE Health Protection Surveillance Centre (HPSC) has launched a new Respiratory Virus Notification Data Hub to provide the latest data for COVID-19, influenza and RSV cases in Ireland. The hub also includes data on hospitalised cases, ICU cases, deaths and outbreaks in Ireland.
The data hub will tell the story of the winter virus season as it happens in Ireland, says HPSC Director Dr Greg Martin.
“This is the first time that Irish respiratory virus data has been
interactively available in a way that makes it easy to track several winter respiratory viruses and compare seasonal variations. It provides respiratory virus data in an up-to-date, dynamic and timely manner and tells us when the viruses circulate in the community, the severity of illness due to the viruses and which age groups and counties are most affected by the virus,“ he said.
“The hub is an additional tool to be used in combination with HPSC’s existing outputs, which together will be used to inform and guide health service preparedness and response for winter resilience planning.”
The data hub has come about
through collaboration between HPSC and People and Place Ltd. Other key stakeholders include laboratories and clinicians, who notify respiratory virus cases, and Departments of Public Health, who manage the surveillance system at regional level.
The data hub will be updated weekly on Wednesdays and data can be downloaded from the hub if necessary. The hub is available at https://respiratoryvirus.hpsc.ie/
The National Clinical Programme for Older People (NCPOP) has published the Knowledge and Skills Framework for Healthcare Professionals Working with Older People, which will be a key resource enabling the provision of integrated interdisciplinary health and social care.
It can be used in conjunction with the Eclectic Framework which describes the core competencies for interprofessional collaboration in integrated care for older people.


This framework was developed through a co-design process with nursing, health and social care professionals and pharmacy representatives forming a working group under the governance of the National Clinical Programme for Older People. NCPOP would like to acknowledge the work of all the individual healthcare professionals who gave generously of their time to support the development of this framework.

blocks for developing shared values, understanding each other’s role, developing teamwork, communication and collaboration. It also describes the core and enhanced knowledge and skills required of individual healthcare professionals working with older people.
The framework describes the knowledge and skills shared by teams, which are core building
It can be used by teams and individual healthcare professionals, to identify areas for improvement and development, in relation to meeting the needs of older people accessing services, across acute, community and residential healthcare settings.
The framework can be access at https://www.hse.ie/eng/about/who/cspd/ ncps/older-people/resources/.

The successful implementation of the SAP HR and Payroll system by the National integrated Staff Records and Pay Programme (NiSRP) in HSE West was delivered in May 2024. 14,500 HSE employees and their teams in the West are already seeing the benefits.
SAP HR and Payroll, including the rollout of HR and Payroll Self Service for employees and managers, continue to enhance processes for paying staff, recording HR actions and maintaining accurate staff records.
Bernard Gloster, CEO of HSE, congratulated NiSRP and HSE West staff on this achievement. “NiSRP is enhancing HR and Payroll administration across our health system which is also giving staff additional control of their own information. I want to thank all of the personnel involved for their effort, skill and commitment. This is a transformational programme with important benefits for employees and the organisation and is delivering strong stakeholder engagement and support.”
Ivan McConkey, AND, Programme Director NiSRP, added, “I would like to thank the NiSRP team, our Shared Service partners and all staff in HSE West for their support and co-operation enabling another successful implementation. This brings the total number of staff in the HSE that are being paid and benefitting from the SAP HR and Payroll system to 98,500. The next implementation is underway in HSE North East and we look forward to working closely with our colleagues in the region.
HSE person-centred planning resources are now available for people with a disability who avail of adult disability services. These resources support each person to make their own choices and decisions while helping them to live their best life now, and plan for the future.

The resources, which are also available in easy-to-read format, include:
• information on person-centred planning for adults with a disability
• information for the role of families and circle of support
• eLearning module for staff with certification
Person-centred planning is grounded in a rights-based approach to the provision of services and supports. We all want to spend our days in a meaningful way – in our family roles, our jobs, with friends and in our valued social roles in the community. In adult disability services, this starts by getting to know the person first, building a trusting relationship and developing a person-centred plan with each person.
Bernard O’Regan, Assistant National Director, Disability Services, HSE, said, “These resources build on the significant work in disability services to ensure each person’s service is based on a person-centred plan that reflects the will and preference of the person supported. These resources are now available for the 21,000 people with a disability and their families who attend adult disability day services in over 1,200 locations around the country.”

Tommy Gorman, who features in the eLearning module, said, “My keyworker Catherine helped me and my circle of support to focus on my abilities and skills. I have a person-centred plan, my own home, a job and friends.”
Access the HSE person-centred planning resources at https:// www.hse.ie, searching for personcentred planning resources.
Each member and associate member of the National Cancer Control Programme (NCCP) Alliance was presented with a plaque at a dedicated event at Farmleigh House and Estate, Phoenix Park recently.
Representatives from the NCCP, hospital Psycho-Oncology teams, the Department of Health and the community cancer support centres and services as well as cancer patient representatives were all in attendance.
“This day marks a significant milestone in our collective efforts to support cancer patients and their families throughout Ireland. These centres provide invaluable psychosocial support and survivorship programmes, ensuring comprehensive care for those living with and beyond cancer,” according to Prof Risteárd Ó Laoide, National Director, HSE NCCP.
The NCCP also launched the Alliance Annual Report for 2023 at the event, highlighting the impact of this important work and the increasing demand for cancer support services.
There are 16 members of the Alliance and these organisations provide professionally delivered cancer support services free of charge to anyone affected by cancer including patients, family and friends.

Pictured Below: Noemi Palacios, Catherine Hogan, Dr Rachel McNamara and Jared Gormly, Head of the Spark Innovation Programme.



The Patient Safety team, part of HSE Incident Management of the National Quality and Patient Safety Directorate, celebrated two wins recently. The team won a Bright Spark Award at the recent 2024 HSE SPARK Summit and were also awarded funding as one of the Q Exchange 2024 winning ideas to support their project ‘Patient Safety Learning – Reaching the right people for action’.
Lorraine Schwanberg, Assistant National Director, Incident Management, Catherine Hogan and Noemi Palacios of the Patient Safety Together team, collaborated with Dr Rachel McNamara and Linda Klotzbach of the SPARK Innovation Programme to expand the reach of HSE National Patient Safety Alerts (NPSAs). Together, supported by the HSE NSPA Committee, they received the National Innovation Award in the Best Design Led category for their work.
Meanwhile, under the theme of ‘How can we improve across system boundaries?’ Patient Safety Together’s project was successful as one of the winning ideas from over 180 applications across Ireland and the UK. It is one of only 20 projects selected and the only project in the Republic of Ireland.
The project will involve the development of a codesigned multimedia resource pack for healthcare services and patient advocacy groups.

We continue to build on excellent foundations
Over the last few months, we have been working to recruit a senior management team for the HSE Dublin and North East Region to support the delivery of health and social care services across the region. The HSE Dublin and North East Region will be divided into four Integrated Health Areas (IHA). These are Louth Meath, Cavan Monaghan, Dublin North County and Dublin North City and West.
"During recent visits to Kells, North Dublin and the National Ambulance Service, I have had the opportunity to meet some of our dedicated staff across the region. I look forward to getting out to visit more sites and meeting more staff in the coming months."
IHAs will bring together both acute and community services as well as other non-HSE providers. This will be crucial to supporting and enabling integrated care. We now have identified four Integrated Health Area Mangers. We have also identified a Regional Director of People and Regional Director of Finance. The recruitment of other members of the team is progressing and we are working towards the 30 September to transition to the new health region structures. Over the next few months I will work with the senior management team to get the IHA structure in place.
During recent visits to Kells, North Dublin and the National Ambulance Service, I have had the
opportunity to meet some of our dedicated staff across the region. I look forward to getting out to visit more sites and meeting more staff in the coming months.
I would like to thank all our staff working in the Hospital Groups and the Community Health Organisations. I want to recognise and acknowledge all they have achieved and the progress they have made in delivering safe accessible care to the people living in this region. As we transition to the new structures and the IHAs, we will continue to build on the excellent foundations that are already in place, to ensure that we deliver improved health outcomes for patients and everyone who accesses our health and social care services.

Annemarie has her life transformed by move to own home
Over the last number of years, there has been a major change in the provision of residential support to persons with a disability. There has been a move away from caring for persons in residential institutions to providing care and support to them in their local communities.
Over the last six years, the HSE has opened three community-based homes across Cavan and Monaghan. These houses were chosen carefully based on the needs and wishes of the residents and their families. In total, there are now 13 HSEdesignated residential disability centres in Cavan and Monaghan which are all registered with HIQA. All centres operate the community living model.
Community living offers the prospect of an improved lifestyle and quality of life over institutional care for people with intellectual disabilities.
Residents from congregated settings have moved to community-based homes over the last number of years. Residents have settled very well into their new homes and have become an integral part of their communities, making friends with neighbours and participating in local activities such as sports
Staff in Sullivan Centre, Co Cavan, organised a 5km memorial walk in remembrance of their late colleague Stephen Brennan. It was a huge success and they raised €4,052 which was donated to the Irish Cancer Society. The organisers would like to express their sincere thanks to all who supported and participated in the fundraising.
clubs, Tidy Towns groups and church choirs.
Annemarie Reilly, resident of Oakvale House, Cavan, explained how she feels about living there. “I love it, because the staff are nice. They help me,” she said.
Lorna McMenamin, Key Worker, Oakvale House, said decongregation means getting involved with many things and ensuring that the residents have access to their hobbies and social interaction.
“We help Annemarie through residence meetings each Sunday or Monday that we hold within the home. Staff and key workers support Annemarie through person-centred plans and goals.
Annemarie states what activities she would like to carry out during the week.”
Edel Quinn, Head of Service for Disabilities for HSE Community Healthcare Cavan, Donegal, Leitrim, Monaghan, Sligo (CH CDLMS), said, “The move to community living would not be possible without the support of the residents, families, staff and the HSE. It is important to acknowledge the positive impact the move to community living is having on transforming the lives of people living with intellectual disabilities.”
https://www.youtube.com/watch?v=8jI6775MLIo
In honour of Nursing Day, Cavan Monaghan Disability Services (CMDS) celebrated by creating a meaningful word cloud.
Registered Nurse Intellectual Disabilities (RNIDs) shared what being an RNID means to them, embodying a commitment to working towards equity, inclusivity, compassion, and care. These heartfelt reflections highlight the profound dedication and values at the core of the local nursing team.
“Additionally, we had the privilege of speaking with our service users, who shared their perspectives on the invaluable role of RNIDs. Their uplifting stories highlighted the profound impact of support, empowerment and care provided by our RNIDs, showcasing the diversity and positivity within the role,” a representative of CMDS explained.
“Through these interactions, we were reminded of the unwavering commitment and profound difference our RNIDs make in the lives of those they support. Their dedication and compassion continue to inspire us every day.”

HSE Dublin and North East Health Region REO Sara Long with some of the NAS team, including NAS DIrector Robert Morton, Head of Integrated Service Operations David Clarke; and National Operations Manager Gavin Doyle.
Sara Long, Regional Executive Officer (REO), Dublin and North East paid a visit to the National Emergency Operations Centre (NEOC) in Tallaght, where she met with the Director of the National Ambulance Service (NAS), Robert Morton, as well as Head of Integrated Service Operations East, David Clarke.
Sara received a brief on the organisation of the NAS nationally, it’s disposition in Dublin and the North East specifically, as well as some of the trends in demand and developments in service delivery.
She also received a tour of the facility from the National Control Operations Manager, Gavin Doyle, and spoke to some of the call takers, dispatchers and clinicians to get an appreciation of their work and of the coordination that goes into matching the service user with the most appropriate resource in the shortest time possible.
The HSE Community Healthcare Cavan, Donegal, Leitrim, Monaghan, Sligo (CH CDLMS) Disability Services can confirm that the location of the new interim Children’s Respite Centre for Monaghan will be at Urbalkirk, approximately 8km from Monaghan town.
The Cavan Monaghan Disability Services management team completed a procurement process with existing contracted service providers to provide the interim children’s respite service. This was on the basis that it would be a five bedded residential respite house inclusive of a self-contained apartment, would be delivered with full-time nursing support and that the service must be operational no later than 1st October 2024.
The Talbot Group has been awarded the contract to deliver the interim children’s respite service in Monaghan and has secured the
CHO Dublin North City and County (CHO DNCC) have launched its Online Service Directory, an online signposting tool to support our staff, GPs, and healthcare professionals to access information and contact details for health interventions, available through our 12 Community Healthcare Networks (CHNs). Details of services from Primary Care including Social Inclusion, Mental Health, Older Persons, Disabilities, Health and Wellbeing as well as the local NGOs have been included, broken down and categorised by Community Healthcare Network (CHN). Content on the site will be managed by the Communications Department supported by
property at Urbalkirk, Monaghan. The renovation and development works required for the property have been identified and the engaged contractor has commenced the necessary works to the property. This includes a studio style apartment with a separate entrance and another ground floor bedroom which will be wheelchair accessible. The respite house will have a further three bedrooms upstairs as well as a relaxation/playroom.
The Talbot Group held an open recruitment day for the respite service in the Four Seasons Hotel in Co Monaghan in June. The HSE has been advised by the Talbot Group that this was a very successful recruitment initiative with no immediate requirements for further recruitment days.
HSE CH CDLMS Disability Services continue to work closely with the Talbot Group to have the service commenced by 1st October 2024.

nominated content leads in each of the services.
The development of an online service directory was identified as one of the main objectives for under the Communications and Engagement work stream under the CHO DNCC Sláintecare Action Plan 2023-24.
They would like to thank everyone who contributed in to bringing the project to a successful conclusion. There has been a truly integrated approach to this initiative with colleagues from all services contributing to the project.
The directory can be accessed via this link: https://healthdirectorydncc.hse.ie/
This Directory provides a wealth of useful information. If there are additional services that you feel you would like included, please contact our Communications Department at comms.dncc@hse.ie and the team will direct your query to the appropriate content lead.

A plan to deliver 3,352 new beds to the system between 2025 and 2028 has been unveiled by Minister for Health Stephen Donnelly.
Our Lady of Lourdes Hospital in Drogheda and Our Lady's Hospital in Navan are to receive 127 new acute beds.
112 of those beds will be in the Drogheda hospital whilst Navan will receive 15 new beds.
The 3,352 beds include 355 replacement beds.
Following the announcement, Minister Donnelly said, “I am delighted to be announcing this landmark expansion of hospital beds across eight
hospitals in the Dublin and North East region. This investment recognises that our growing and ageing population are placing more demands on our healthcare services and I am determined to drive forward with expansion that ensures people have access to the right care in the right place at the right time.
“This ambitious plan will be delivered in phases, with extensive additional capacity planned for Beaumont and the Mater Misericordiae University Hospital and further increases planned in hospitals across the region.
“These are significant expansions that aim to deliver increased capacity in order to better meet the needs of the population across the North Dublin, Cavan, Monaghan and Louth areas.”
“These are significant expansions that aim to deliver increased capacity in order to better meet the needs of the population across the North Dublin, Cavan, Monaghan and Louth areas.”

A pilot art project has been introduced following consultation with the Traveller Community around a means to identify mental health issues and promote positive mental health among young people and their families.
Copper Art was identified as the tool of engagement. This is a collaborative initiative with five Traveller projects in CHO DNCC along with the HSE, Mental Health Service Coordinator for/with Travellers, Youth Mental Health Coordinator and NGOs of Mental Health Services across the region. It has supported the engagement of harder to reach Traveller male and females.
This project has proven to engage young people and their families in open discussions around mental health by addressing fears and stigma of accessing services and talking about mental health. Throughout this process, Travellers and mental health services have engaged with each other resulting in improved relationships and cultural understanding.
The mental health services themselves have fully engaged with this pilot and are working with the Traveller Community to enhance cultural awareness and improve pathways to access.
Copper Art has facilitated shoulder-toshoulder engagement and conversations with peers through the workshops. The services have shared information and signposting around access, along with gaining a valuable insight into Traveller Culture. This has informed how they can adapt their service to ensure a safe cultural environment and access for all.
From these workshops it was identified by the young people and the Traveller projects that they would like to exhibit their artwork at an open day and invite family, friends and Mental Health services, to celebrate each other’s work and promote Traveller Pride.
Some of the participants from the workshop showcasing their wonderful designs.




Staff from the National Immunisation Office at the National Immunisation Conference.



A series of national immunisation conferences took place across the country, thanks to the efforts of the National Professional Development Co-ordinators for General Practice Nurses (PDCGPN) in collaboration with the National Immunisation Office.
PDCGPN comprises just five members: Mairead Murphy, HSE Community Health Care West Galway, Mayo and Roscommon, Area F; Marie Cantwell, HSE Community Healthcare Dublin North City and County, Area A; Elizabeth Carroll, HSE Community Healthcare South Tipperary, Carlow/ Kilkenny, Waterford and Wexford,
Area C; Kathy Taaffe, HSE
Community Healthcare Cavan Donegal Leitrim Monaghan Sligo, Area F; and Marie Courtney, HSE Community Healthcare Cork Kerry, Area D.
A pre-conference survey was issued in advance which aimed to assess attendees’ pre-existing knowledge in several key areas.
The results highlighted both strengths and areas for improvement, guiding future learning initiatives, which suggests a need for enhanced pre-conference learning materials on key topics.
The post-conference survey indicated that 85% of attendees felt
their learning needs were met. Key learning outcomes included improved knowledge of vaccine administration and cold chain management, enhanced skills in patient education and vaccine safety and increased confidence in handling immunisation data.
Organisers strongly encourage all HCPs involved in immunisations to avail of all the resources on Padlet, including the resource pack.
The resource pack contains information on immunisation guidance, medicine protocols, links to online learning and sample templates for consent and competency assessment.
Access the national immunisation conference series resources on the Padlet platform
Leads from the Healthy Eating Active Living Programme and the National Healthy Childhood Programme hosted a webinar that brought together researchers, practitioners and policy makers to learn about the latest research, developments and resources in child health and weight.
Sarah O’Brien, National Lead Healthy Eating Active Living Programme, facilitated the webinar. In her opening remarks, Dr Abigail Collins of the National Healthy Childhood Programme highlighted that one in five children in Ireland live with overweight or obesity. This rises to one in four adolescents.
The webinar also included an address by Minister of State in the Department of Health, Colm Burke, who stressed the concern with these figures being higher for children living in areas of disadvantage.
A panel discussion, which included Dr Celine Murrin; Geraldine Sexton, Senior Project Dietitian Healthy Eating Active Living; and Dr Anne Marie Hourihan, Senior Clinical Psychologist, Weight Management Services Children and Young People (CHO5), rounded out the webinar.



Kate Ryan and Siobhan Maher, both Social Worker Team Leaders, Safeguarding and Protection Team, running an information/awareness stand in Kilkenny to mark World Elder Abuse Awareness Day.
A number of events were held across the HSE to mark World Elder Abuse Awareness Day in June. Elder abuse is a significant health and social issue. It can be a difficult topic to raise but by doing so the HSE can assist those in need of protection. Raising awareness in a social forum such as services or in public spaces helps to reduce stigma and makes the topic accessible.

By marking this day, the HSE highlights its commitment to protecting the most vulnerable and promoting services that safeguard adults.
It focused on a new resource, ‘Talking to your child about health and weight’, that can be found on healthpromotion.ie.



The full recording of the webinar can be found here: https://www.youtube.com/ watch?v=snEFPDAq0zw

Events included learning seminars held in Donegal, Ballyshannon, the Mid West, Cork/Kerry, CHO East and CHO DNCC. The National Safeguarding Office held a conference in the Aisling Hotel with speakers from Sexual Assault Treatment Units, Galway Rape Crisis and the Dewis project in Wales.
Information stands were held in Tipperary University Hospital, Wexford General Hospital and Kilkenny shopping centres and libraries. Services marked the day with coffee mornings/afternoon tea and combined discussion/information with music song and poetry. These services include community nursing units and day services in Ballymote, Sligo, Leitrim, St Mary's Castleblaney, Merlin Park Hospital, St Francis day centre and Sacred Heart Hospital, Roscommon.
Conference organisers: Michael Ryan, Ellen Forkan, Donal O’Keeffe, James Harrington, Jacopo Villani, Sean O’Connell and Rosemary Ryan.
Mental health service users and family members were key stakeholders in the organisation of the recent Mental Health Engagement Conference 2024: Implementing our Framework.
The HSE Mental Health Engagement and Recovery Office (MHERO) is committed to ensuring that the voices of people with lived experience inform service development and improvement. It is working to support an on-going process of change in mental health services, towards services that prioritise recovery and ensure that those requiring their supports feel respected, valued and understood.
Meaningful mental health engagement is a respectful, dignified and equitable process. It uses the perspectives of service users and their family members, carers and supporters to make
“The
mental health services better.
The conference was held in Dublin with 200 delegates and 100 online attendees. It was part of the HSE commitment to engage with people with lived experience of mental health service use, their family members, carers and supporters at a national level. It allows them to explain how they can influence and improve the mental health system outlined in the Mental Health Engagement and Recovery Strategic Plan 2023-2026 - Engaged in Recovery.
The conference, which was co-designed by an organising committee comprising people who use and provide mental health services, aimed to celebrate the value of lived experience in shaping mental health services. It generated ideas of how services can be improved in three priority areas:
Mental Health Engagement Framework and the evidence it will produce will ensure that we become a world leader in the reform of mental health services, where the centrality of lived experience is the norm."


communication, crisis response and family involvement. It reflected on how best to implement our new Mental Health Engagement framework as a community.
The conference was opened by Dervila Eyres, the Assistant National Director, HSE Head of Operations Mental Health.
“The Mental Health Engagement Framework and the evidence it will produce will ensure that we become a world leader in the reform of mental health services, where the centrality of lived experience is the norm,” she said.
A powerful panel discussion followed, with people with lived experiences and service providers, discussing challenges and how the HSE is trying to tackle these with specific projects. Joanne O’Meadhra, while talking about her experience of admission to psychiatric hospital, asserted, “communication is paramount to everything in relation to mental health services.
Oftentimes the communication I was met with was jargon, medical terminologies, there was a lack of communication in certain areas, and there’s definite room for improvement.”

The HSE held a national conference in Portlaoise to celebrate the annual International Day of the Midwife. This is the third year that the National Women’s and Infants Health Programme and the Office of the Nursing and Midwifery Services Director hosted this event. A conference planning committee grouped early in the year to plan and ensure that the event ran smoothly, presented valuable networking and learning opportunities and was enjoyable to attend. The theme for this important day of recognition of midwives
and student midwives was ‘From Policy to FrontlineMidwives making progress’. It encapsulated the progress of service delivery by midwives and the multidisciplinary teams that occurs throughout the country within our maternity services.
Over 180 midwives and student midwives attended the conference and availed of opportunities to network with their peers, demonstrate the tremendous work that has been undertaken and the many improvements that have been realised in individual maternity units.
The conference showcased exemplars of midwifery practice and shared innovative ways of addressing and combatting the challenges, including using ‘human centres design’ in implementing new initiatives, the HSE Climate
The HSE Dublin and Midlands held its inaugural Nursing and Midwifery Conference recently, showcasing nursing and midwifery clinical expertise across the region.

The theme of this year’s conference was Connect, Collaborate, Change. This theme is aligned to the strategic priorities of the Chief Nurse, Department of Health and of the health service. The line-up of speakers focused on the integrated care agenda and the current environment of change and innovation.


Michelle Waldron, Sinead Heaney, Margaret Quigley, Angela Dunne, Professor Jane Sandall, Mary Rowland, Clare Kennedy (chairperson), Emma Doody, Siobhan Canny, Ann MacIntyre and Dr Karn Cliffe. * Missing from the photo Dr Maria Healy, Amy Carroll, Niamh Meleady and Cormac McAdam.
Action Strategy and how midwives can support sustainability, knowledge and practices in midwifery settings in Ireland and good practices with sleep, health and wellness.
The progress of the implementation of the National Maternity Strategy was outlined by Angela Dunne, National Lead for Midwifery NWIHP. She highlighted many of the significant achievements in relation to antenatal education, clinical guidelines, and infant feeding.

Mary O'Kelly, Michael Buckley, Kate Killeen White, Eileen Whelan and Trevor O'Callaghan.

This conference represents the first collaboration of nursing and


midwifery colleagues from hospitals and communities in the new HSE Health Regions and included engagements with nurses and midwives from all specialties within the HSE Dublin and Midlands region. HSE Dublin and Midlands provides health and social care services to Dublin west and south-west, Laois, Longford, Offaly, Kildare, West Wicklow and Westmeath. Key topics included community general nursing and public health nursing; mental health nursing; safe nurse staffing; integrated care; education and research; digital healthcare; leadership and governance; and workforce stability and wellbeing.
At the conference, Eileen Whelan, Chief Director of Nursing and Midwifery, Dublin Midlands Hospital Group, launched the DMHG Nursing and Midwifery Implementation Strategy and Action Plan 2024 – 2026.


Active Healthy Me is an exciting health, wellbeing and physical activity programme that aims to increase the knowledge and understanding of people with disabilities on the importance and benefits of being physically active, how to live a healthy lifestyle and the opportunities that are available to participate in sport and physical activity within their local community.
It is a partnership programme with Active Disability Ireland and the HSE that is aimed at people with disabilities attending day services across the health services.
There are approximately 6,000 frontline staff in 1,000 adult disability day services supporting 20,000 adults, so the potential for this programme is huge.
The programme has been running since 2022. It was developed, tested and refined with involvement and feedback from people living with disabilities attending over 18 different day services across the country. The overall feedback continues to be positive.
The programme is going from strength to strength. Active Disability Ireland are now working directly with over 440 disability


services to support their development and growth in physical activity and to support their connection with their local community services. It is supported by Health and Wellbeing staff in the community who are trained to deliver support sessions and workshops for disability service staff. This is part of wider work to integrate health and wellbeing into disability services.
Active Healthy Me also aligns with the HSE New Directions approach of supporting adults with disabilities who use day services in Ireland. staff. This is part of wider work to
For more information see https://activedisability.ie/active-healthy-me/



Data published in June 2024 from the Childhood Obesity Surveillance Initiative (COSI): Round 6 2022-2023 shows one in five primary school children are living with overweight and obesity. While prevalence has not increased since COSI Round 5 2018-2019, and most children in Ireland have a healthy weight (73%), a significant percentage (17.7%) live with overweight and obesity.
The research, commissioned by the HSE, also finds a greater prevalence in schools that participate in the Delivering Equality of Opportunity in Schools (DEIS) programme (25.4%) versus schools that do not (16.1%).
The latest survey findings show:
• In an average classroom of thirty children, six will have overweight or obesity
• In DEIS schools one in every four children have overweight or obesity
• Less than one in every 10 primary school children have underweight and no differences in the proportion of children were seen across areas of disadvantage
• No differences, in all categories, were seen between urban and rural areas
• The majority of schools have a curriculum, environment and activities that are known to promote positive health outcomes
• Few schools have fresh fruit or vegetables (free or paid for) available to children during the school day
Professor Cecily Kelleher, University College Dublin, who leads the team of researchers working on the Irish arm of COSI at the National Nutrition Surveillance Centre said, “The health of our children, largely predicts the health of our future adult population. We know that childhood obesity is largely preventable through effective policies that can intervene early to create environments and behaviours that support healthy growth and development for all children. Robust population surveillance efforts like COSI are a valuable means of accessing our progress and the impact of these interventions over time.”

The full research report can be accessed online on the Health and Wellbeing home page https://www.hse.ie/eng/about/who/healthwellbeing


The HSE National Cancer Control Programme (NCCP), in partnership with Healthy Ireland, runs the SunSmart campaign from April to September. The aim of the campaign is to reduce your risk of skin cancer by increasing awareness of, and engagement with, the steps you, your family, friends and colleagues can take to protect your skin from the sun and highlighting the importance of not using sunbeds.

The Annual Awards for Excellence in Public Relations, organised by the Public Relations Consultants Association, took place in June 2024 and we are pleased to announce that the HSE NCCP and Healthy Ireland won the award for the ‘Best Public Information Campaign’ for the SunSmart campaign. Judges highlighted that the campaign “demonstrated well-identified objectives and audiences, strong research and hard-working execution”.
Dr Breeda Neville, Specialist in Public Health, HSE NCCP, said, “The SunSmart campaign has grown year on year with more engagement and coverage of skin protection being displayed across media outlets. The skillset and knowledge of the communications group working on the SunSmart campaign has allowed for all the various campaign elements to work well and facilitated an engaging and comprehensive multi-channel approach.”
For more information visit hse.ie/sunsmart or #SunSmart on social media.

A service designed to safely bring children and teenagers back to their local hospital once they no longer require specialist Dublin-based care was recognised recently by winning an Irish Healthcare Centre Award.
The IPATS (Irish Paediatric Acute Transport Service) Repatriation Service aims to provide care and support for children and families during a very stressful time. It also ensures a flow of children into and out of the specialist hospitals so that every child can get the most appropriate care when they need it most.
IPATS is part of the Critical Care and Retrieval Service (National Ambulance Service) known as NASCCRS.
Dr Cathy Gibbons, National Clinical Lead for IPATS, said the NASCCRS IPATS Nurse-led repatriation team were thrilled to win the Irish Healthcare Centre Award in the Child Health and Wellbeing category in May 2024.
“Feedback from CHI, regional paediatric departments and most importantly, patients and their parents, has been overwhelmingly positive. The award was in recognition of the work done to date, and the team are looking forward to a busy and exciting year ahead,” Dr Gibbons said.

1 Sustainable Buildings and the Green Environment
Scan the QR code We’re taking action across the health service on:
4 Greener Models of Healthcare
3 Sustainable Procurement
2 Transport and Mobility
5 Water and Waste Management
6 Adaptation and Resilience


Vaccines are safe and effective and provide the best protection from flu and COVID-19.
You can get both vaccines at the same appointment.


Vaccines may be available at work and are also available free of charge from GPs and Pharmacies








If you work in healthcare, you are at increased risk of being exposed to flu and COVID-19 Visit the HSE website for vaccine information and resources

