Triumphs in Trials
What I Love About Being a Nurse
EMPLOYEE SPOTLIGHTS: Krystal Villasuso and Miranda Gibson
Rise and Shine and Eat Breakfast
Advancements in Immunotherapy and Targeted Therapy



Triumphs in Trials
What I Love About Being a Nurse
EMPLOYEE SPOTLIGHTS: Krystal Villasuso and Miranda Gibson
Rise and Shine and Eat Breakfast


FEATURES
06 Triumphs in Trials: A Spotlight on Cancer Clinical Trials Across the Organization

10 Advancements in Immunotherapy and Targeted Therapy In Gastrointestinal Cancers
16 What I Love About Being a Nurse

20 Unmasking the Silent Symptoms of Burnout and How to Extinguish It
PEOPLE AND PLACES
22 Leadership Spotlight: Curtiss McNair, Jr.
24 Employee Spotlights: Krystal Villasuso and Miranda Gibson
26 Nutrition Bites: Rise and Shine and Eat Breakfast
30 Patient Story: Jane Mackie
We welcome your feedback, article suggestions and photos (high resolution please). Email to AONCommunications@AONcology.com

In this edition, we highlight the remarkable advancements we have witnessed in practices across the network and focus on clinical research and trials, while also paying tribute to the extraordinary contributions of our nursing staff in honor of Nurses Week. We have made great strides in elevating patient care, and I would like to take this opportunity to share my thoughts on the transformative power of clinical trials and the innovative landscape of cancer care.
Clinical trials are at the heart of medical progress and hold immense potential for improving patient outcomes. They provide a platform for testing new treatments, exploring innovative approaches and expanding our knowledge base as caregivers. Our organization is at the forefront of clinical trials, offering more than 100 active clinical trials and participating in authored studies, and this is changing the landscape of cancer care. Our commitment to rigorous research and patient-centered care has resulted in improved patient outcomes and increased hope for those facing cancer diagnoses. The AON Research Committee, which will be spotlighted in the coming pages, ensures we continue fulfilling our mission of closing the cancer care gap and providing equitable access to cancer care.
Today, personalized medicine, targeted therapies and immunotherapies are revolutionizing the way we approach cancer treatment. These innovative approaches allow us to tailor treatment plans to each patient, increasing the likelihood of positive outcomes and minimizing unnecessary side effects. We are witnessing groundbreaking developments in precision medicine, genomics and biomarker-driven therapies that hold tremendous promise for the future of cancer care. As an organization committed to pioneering advancements, we are actively investing in research and development and fostering a culture of innovation. By staying at the forefront of these innovations, we can continue to provide our patients with the most effective, compassionate and personalized care available. I encourage you to take a moment to read Dr. Mikhail’s article on advances in cancer care and immunotherapy in gastrointestinal cancers.
The collaborative efforts of our multidisciplinary teams have resulted in significant breakthroughs. These achievements and commitment to continuously improving the care we provide are a testament to our dedication, scientific rigor and patient-centric approach. Thank you for your service to AON and our patients who face difficult journeys ahead.
Dr. Stephen "Fred" Divers AON Chief Medical Officer
“Our organization is at the forefront of clinical trials, offering more than 100 active clinical trials and participating in authored studies, and this is changing the landscape of cancer care.”
June is National Cancer Survivor Month. Hematology Oncology Clinic in Baton Rouge invited everyone to attend their Cancer Survivor Celebration event on Sunday, June 4 at St. Joseph Cathedral.
Learn more
According to the National Cancer Institute, the skin is our body’s largest organ, and it helps protect against heat, sunlight, infections and more.
Learn more
In an interview with Pharmacy Times, Dr. Stephen "Fred" Divers discussed the future of home infusion and drug development, and how both issues will be influential in the future of community oncology.
Learn more
Healthcare in Western North Carolina has undergone significant transitions over the last few years. Unfortunately, there is ongoing uncertainty for many patients facing a diagnosis of cancer.
Learn more
SouthFloridaCIO is the preeminent peer leadership network of South Florida chief information officers. SouthFloridaCIO is one of over 30 chapters of the Inspire Leadership Network, a national membership organization comprised exclusively of CIOs from public and private businesses, government, education, healthcare and nonprofit institutions.
Learn more
The majority (22 of 40) of biosimilars approved in the United States are used for the treatment of cancer or supportive care of patients with cancer, according to December 2022 data cited by the American Oncology Network (AON).
Learn more
In this episode of The Vitals, Oncology Nursing News® talks with Amber Pierce, RN, BSN, OCN, regional nurse director, about the importance of 2-step verification with nivolumab and relatlimab-rmbw (Opdualag), which was approved for patients with unresectable or metastatic melanoma in March 2022.
Learn more

























Clinical trials specifically for cancer care first occurred in 1955 and focused on patients with acute leukemia.1 Since the 1950s, clinical trials have advanced and improved, resulting in more targeted treatments and therapies for various cancer diagnoses. These instrumental clinical trials provide lifesaving opportunities for cancer patients who face a challenging journey to health and are beneficial to patients whether it is delivered through a large hospital system or community practice.
Having care options, including clinical trials, available locally makes a difference in the patient’s health outcomes. Currently, there are more than 140,000 clinical trials in the United States as of June 2023.2 However, there are still barriers that hinder many

patients from seeking out and enrolling into the trials, and this is found across all medical disciplines. Common barriers to enrollment are patient perceptions as well as patient eligibility. Other barriers keeping patients from enrolling include misinformation about a trial or not knowing of trial opportunities that are available, inaccessibility that comes with enrolling in a trial (such as travel time and costs among other tradeoffs), being in the placebo group and fear that the trial is a “last-ditch effort.”3
As a leader in healthcare and specifically oncology, AON is committed to cancer research and expanding access to clinical trials to ensure equitable patient care.4 Many AON practices are active research sites, including four that are strategic research sites for the Sarah Cannon Research Institute and six that offer diverse clinical trials to their
patients. Additionally, the practices across the network have collectively more than 100 active clinical trials.
AON further builds upon the goal of closing the cancer care gap through the Research Committee, which is dedicated to “serv[ing] the AON partner practice’s mission of providing patient access to community-based, oncology clinical trials through shared expertise and innovative research processes.” The committee is comprised of AON leaders and physicians across the network and works to ensure equitable access to clinical trials for all AON patients is available and that practices have the support they need to either deliver trials themselves or enroll patients into trials in the area. Current initiatives of the committee include developing an organic research network within AON, helping more practices become research sites including providing the support and guidance needed to be successful, and mentoring interested groups to develop new capabilities or grow capabilities in the sites already doing research.
“AON can help lay the groundwork for community practices to begin administering clinical trials,” said AON’s Vice President of Clinical Research Katie Goodman.

“Whether practices need financial assistance or tech support related to trials, AON has the resources that allow physicians and their practices to become research sites or strategic research sites for our partner the Sarah Cannon Research Institute. This is only one benefit of being part of this growing network of community oncology practices.”
To effectively build a successful clinical research program, Dr. Ralph V. Boccia from The Center for Cancer and Blood Disorders in Bethesda, Maryland, and active member in the AON Research Committee recommended two considerations:






CARET-RIGHT Decide first whether the practice really wants to do clinical research. “This is a huge commitment that can be rewarding for patients, staff and doctors,” Dr. Boccia explained. “However, it requires the development of an infrastructure to support the program.”
CARET-RIGHT Then, employ and retain dedicated staff focused on the clinical research program. Dr. Boccia continued to share that a program of this caliber requires staff who are qualified and equipped to find and recruit patients into the program. These individuals also need to be able to effectively inform the patient about the trial, then gather consent from the patient and monitor those in the
Katie Goodman VICE PRESIDENT CLINICALTriumphs in Trials, continued
program closely. Additionally, this specific staff needs to be able to assess the efficacy and safety of the program, host regular key practice stakeholder research meetings, report on the program’s data and occasionally present findings at appropriate meetings and host sponsor monitoring.
Dr. Boccia is experienced in the vertical of clinical trials — leading the practice’s clinical research program that has been operating for 20 years. “We are approached daily with new trial opportunities,” Dr. Boccia said. “We are authors on abstracts at ASH (American Society of Hematology) and ASCO (American Society of Clinical Oncology) every year and have appeared in publications of major hematology and oncology journals.” Dr. Boccia himself has penned over 180 publications centered on clinical trials.
When asked for examples of how The Center for Cancer and Blood Disorders is involved in clinical trials, Dr. Boccia said, “We have been a part of developing many of the new drugs and therapies we use in clinical practice today and are a part of new therapies just approved or about to be approved. Examples are Avastin, Abraxane, Tagrisso, Revlimid, Pomalyst, Nplate, Optivo, Yervoy, Keytruda, Tecentriq, Venclextra, Vidaza, Reblozyl, Imetelstat, CAR-T for myeloma and the new bispecific epcoritamab (Epkinly). I could include other drugs we have helped develop, but the point is, this is very important work and very gratifying to patients, doctors and staff who are so much a part of this process.”
Another physician focusing on elevating clinical trials and addressing the present healthcare disparities is Dr. Ruemu E. Birhiray from Hematology Oncology of Indiana. With assistance from his daughter, Maya, they have created the D.R.I.V.E. initiative aimed at racial diversity in clinical trials.⁵ The D.R.I.V.E. acronym represents the following steps:
Cancer & Blood Specialists of Arizona *
Desert Hematology Oncology *
Genesis Cancer & Blood Institute
Hematology Oncology Clinic
Hope Cancer Care of Nevada
Messino Cancer Centers
Michigan Cancer Specialists
Oncology Hematology Associates
Summit Cancer Centers
The Center for Cancer & Blood Disorders
Vista Oncology
Zangmeister Cancer Center
* Coming in 2023
D: Diversity officer for clinical research studies.
R: Ranking for clinical studies.
I: Individual diversity, equity, inclusion and access plan.

V: Verification of study diversity.
E: Elevate and enhance training of minority investigators and research team members.
The future of clinical trials is bright and makes use of the advanced technology that is available today, including AI, according to Dr. Boccia. “Artificial intelligence is findings its way into clinical trial management, from patient identification and recruitment efforts to managing some of the tedious responsibilities of a clinical trial program such as data collection and reporting back to sponsors of data, which saves countless hours of CRC time.”
References:
To learn about AON’s active clinical trials, visit www.aoncology.com/clinical-trials/
1. Gehan, E. A., & Schneiderman, M. A. (1990). Historical and methodological developments in clinical trials at the national cancer institute. Statistics in Medicine, 9(8), 871–880. https://doi.org/10.1002/sim.4780090803.
2. NIH U.S. National Library of Medicine (2023, June 2). Trends, Charts, and Maps. ClinicalTrials.gov. https://clinicaltrials.gov/ct2/resources/trends.
3. Institute of Medicine (US) Forum on Drug Discovery, Development, and Translation (2010). Transforming Clinical Research in the United States: Challenges and Opportunities: Workshop Summary. NIH National Library of Medicine, National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK50895/.
4. (n.d.). Cutting-Edge Clinical Trials. American Oncology Network. https://www.aoncology.com/clinical-trials/.
5. Anderson, C. (2022, August 31). “DRIVE” Strategy Provides Framework to Promote Racial Representation Cancer Clinical Research. Inside Precision Medicine. https://www.insideprecisionmedicine.com/topics/oncology/drive-strategy-provides-framework-to-promote-racial-representation-cancer-clinical-research/
To send WellBeing messages to your colleagues today, visit Recognation via SharePoint.

“I see real-world evidence and racial diversity as pivotal to our success in offering and expanding clinical research programs into community practices,” Dr. Boccia voiced. “I am excited to be a part of this process.”

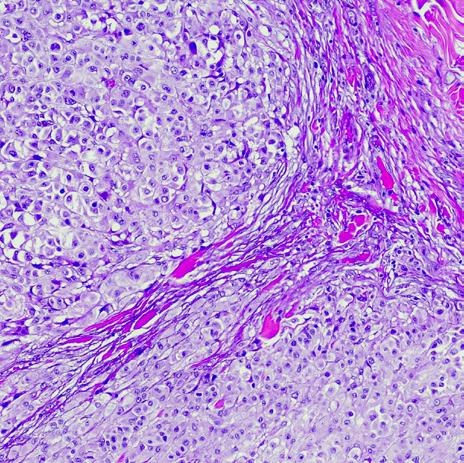
reatment of gastrointestinal (GI) cancers has evolved in the last two decades, which has contributed to significant improvements in the outcomes of many GI cancers. Immunotherapy and targeted therapy have revolutionized the treatment of patients with GI cancers in recent years. Not only have those treatments provided patients with better clinical outcomes but also have resulted, in many situations, in reduced treatment-related toxicity. As a result of developments in immunotherapy and targeted therapy, oncologists can provide patients, in many cases, with additional options beyond standard cytotoxic chemotherapy.
Immunotherapy is a novel treatment that allows the immune system to better recognize and fight cancer cells. Immunotherapy is currently being used in many stages of the treatment of GI cancers. In this section, we will summarize the advances in immunotherapy and describe its role in various phases of the treatment of GI cancers.
 Sameh Mikhail, MD ZANGMEISTER CANCER CENTER
Sameh Mikhail, MD ZANGMEISTER CANCER CENTER
In this review, we will describe the recent advancements in immunotherapy and targeted therapy with a special focus on gastrointestinal cancer.
Rectal Cancer: Approximately 5% to 15% of colorectal cancers have a sporadic or inherited deficiency of a mismatch repair protein (MMR). Typical treatment for patients with early-stage rectal cancer involves radiation therapy, chemotherapy followed by surgery. A recent study suggested that immunotherapy can possibly avoid the need for the typical treatment modalities. Patients were treated with the anti-PD1 inhibitor dostarlimab, which resulted in sustained complete pathological response in 12 patients with stages II and III rectal cancer. The patients received immunotherapy for at
least six months and were followed up with for at least six months after completion of dostarlimab (median follow-up is 12 months after study enrollment, range six to 25 months). Follow-up consisted of serial MRI, PET scan, endoscopic or digital rectal exam and/ or biopsy evaluations. None of the patients required any additional systemic therapy, radiation therapy or surgery. These results remain preliminary but are very encouraging for the small proportion of patients that have microsatellite unstable tumors.
Gastro-Esophageal Cancer: Similarly, a small proportion of patients with gastric cancer (3% to 6%) have deficient mismatch repair proteins and microsatellite unstable tumors (MSI-H). Given the favorable activity of immunotherapy in MSI-H advanced gastric cancer, a study was recently performed to evaluate the benefit of immunotherapy with ipilumumab and nivolumab in patients with earlystage MSI-H gastric cancer. Thirty-two patients were enrolled in the study and received the immunotherapy combination for a total of 12 weeks. Twenty-nine patients underwent surgery, 59% of whom had a complete pathological response. Three patients did not undergo surgery; two of whom refused surgery due to a complete endoscopic response with tumor-negative biopsies and normal imaging studies. One patient did not undergo surgery due to the presence of metastasis at enrollment. These results are also preliminary but remain a very exciting development that could change the standard of care for treating patients with MSI-H early gastric cancer.
Colon Cancer: A similar concept was also explored in patients with locally advanced colon cancer (CRC). At least two studies evaluated the benefit of neoadjuvant immunotherapy (PD-1 monotherapy) in patients with locally advanced MSI-H colon cancer. A study by Xiao B et al. enrolled 73 patients and demonstrated an 85% radiological response rate, including a 23% complete response rate and a 62% partial response rate. Of the 50 patients who underwent surgery at the time of presentation of the data, the pathological complete response rate was 57%. Similar results were observed in the NICH-2 trial. The trial enrolled 112 patients with locally advanced colon cancer to evaluate the benefit of a short course of ipilimumab (one dose) and nivolumab (two doses). The pathological response rate
was 99% with a complete response rate of 67%. It is worth noting that the median time from the first dose of immunotherapy to surgery was only five weeks. These results are very intriguing but need to be confirmed in larger trials.
Collectively, the studies outlined above suggest that immunoterapy may play a prominent role in the neoadjuvant treatment of patients with MSI-H gastrointestinal tumors. In many cases, immunotherapy can be better tolerated than cytotoxic chemotherapy, and evolving evidence raises hopes about possibly avoiding surgeries, chemotherapy and/or radiation therapy in patients who achieve a clinical and pathological complete response to immunotherapy.
CheckMate 577 demonstrated significant clinical benefit in patients with resected esophageal and gastroesophageal junction cancer who were treated with nivolumab for a year following the desophageal surgery. Of note, all patients had received neoadjuvant chemoradiation prior to surgery. Median disease-free survival was significantly better with nivolumab compared to placebo (22.4 versus 11 months). As a result of this study, nivolumab was approved by the U.S. Food and Drug Administration (FDA) as adjuvant therapy for patients with esophageal and gastroesophageal junction cancer who had residual disease following chemoradiation and surgery.
Typical treatment for advanced gastrointestinal cancers includes cytotoxic chemotherapy that can be associated with excessive toxicity. Several studies demonstrated improvement in outcomes of patients with advanced gastrointestinal cancers when treated with immunotherapy.
The combinations of atezolizumab plus bevacizumab as well the combination of tremelimumab plus durvalumab are associated with favorable outcomes in patients with

Advancements in Immunotherapy and Targeted Therapy in Gastrointestinal Cancers, continued
hepatocellular carcinoma. Similarly, immune checkpoint inhibitors plus chemotherapy (gemcitabine and cisplatin) are associated with improved outcomes in patients with biliary cancers compared to chemotherapy alone.
In advanced upper gastrointestinal cancers, immune checkpoint inhibitor combinations are associated with improved outcomes when combined with chemotherapy in the first-line setting. Subgroup analysis has suggested that the benefit of immunotherapy in this patient population increases as the expression of PD-L1 increases. PD-L1 is a protein on the tumor and surrounding cells that can be measured to predict the response of certain tumors to immunotherapy. In HER-2 neu positive metastatic gastric and gastroesophageal cancer, the combination of pembrolizumab plus trastuzumab and cytotoxic chemotherapy was associated with impressive response rates (74%) and duration of response. This combination is currently approved by the FDA in this patient population. Of note, pembrolizumab was also approved by the FDA for the firstline treatment of patients with advanced colorectal cancer and microsatellite instability. The immunotherapy combination of ipilimumab and nivolumab was also approved by the FDA for this patient population.
In summary, immunotherapy treatments are part of the treatment regimen for many GI cancers. They have helped improve outcomes for many patients with GI cancers, and in many cases, the improved outcome was not associated with increased toxicity. It is very likely that the use of immunotherapy will continue to increase over the next few years and will yield greater benefits to patients with GI cancers.
Targeted therapy is a novel treatment that has improved outcomes of many cancers including gastrointestinal cancers. Targeted therapy is a highly sophisticated treatment that recognizes certain genetic changes that lead to the growth and spread of cancer cells. Once the targeted therapy attaches to its target genetic alteration, it helps control the growth and spread of cancer cells. Targeted therapy options are being explored in various GI cancers. Some remain investigational while others have been adequately researched and are now approved by the FDA for routine use in patients with GI cancers that harbor special genetic changes.
Targeted therapy options continue to increase and have resulted in significant improvement in patient outcomes. Genetic mutations are typically tested using genetic next-generation sequencing (NGS), which has advanced significantly in the last few decades. NGS tests can test tumor biopsy or blood samples for genetic changes that can act as targets for targeted therapy. In the next section, we will summarize genetic changes related to various GI cancers and discuss potential targeted therapy treatments that have shown promising activity against those genetic changes.
HER-2 Neu: Approximately, 3% to 5% patients with CRC are HER-2 neu positive. Several combinations have been developed to target HER-2 neu positive CRC such as trastuzumab plus lapatinib or trastuzumab plus tucatinib. Additionally, single-agent fam-trastuzumab deruxtecan has demonstrated favorable activity in patients with HER-2 neu positive CRC with an impressive response rate of 45%.
BRAF: BRAF mutations are detected in approximately 5% to 12% of patients with metastatic CRC. Based on results from the BEACON trial, the combination of the BRAF inhibitor encorafenib and the EGFR inhibitor cetuximab has emerged as a recommended regimen in
patients with advanced BRAF mutated CRC following first-line therapy. This combination is currently approved by the FDA.
KRAS G12C: Although KRAS mutations are present in approximately 50% of patients with CRC, KRAS G12C, which is the only potentially targetable KRAS mutation, is present in only 3% of patients. The role of the KRAS G12 inhibitors, sotorasib and adagrasib, in patients with KRAS G12C mutant CRC is currently being evaluated. The combination of KRAS G12C inhibitors with EGFR inhibitors is a promising combination that is being explored in clinical trials.
Other Molecular Alterations: Molecular alterations such as RET fusion and TRK fusions are less common in patients with CRC (1% each) but can be effectively treated with targeted therapy. Selpercatinib (for RET fusions) and larotrectinib or entrectinib (for TRK fusions) are associated with a very favorable response rate in patients with the respective molecular alterations.
HER-2 Neu: The combination of trastuzumab, pembrolizumab and chemotherapy is now considered the mainstay of treatment of patients with advanced HER-2 neu positive gastroesophageal (GE) cancer in the first-line setting. Several trials, however, evaluated the role of HER-2 neu targeted therapy in the second line setting but, unfortunately, failed to demonstrate improved outcomes. Trastuzumab, iapatinib and adotrastuzumab emtansine have not demonstrated favorable efficacy in this patient population. Recently, however, the DESTINY-Gastric-01 trial has demonstrated improved outcomes of fam-trastuzumab deruxtecan in patients with HER-2 neu positive tumors in the second-line setting. This agent was associated with both favorable response rates and overall survival in the study population and was therefore approved by the FDA as the only second-line therapy in patients who have progressed on trastuzumab-based therapy.
BRCA Mutations: The PARP inhibitor olaparib is currently approved by the FDA in patients who have advanced pancreatic cancer that is stable following treatment with platinum-based chemotherapy. The
To celebrate Administrative Professionals Day, here are several interesting facts:
Administrative Professionals Day was recognized for the first time in 1952. 1
It was originally called Professional Secretaries Day until 2000 so that it was more inclusive to a wide variety of roles that are considered administrative support staff.¹
There are more than four million administrative professionals in the United States.²
References:
1. 5 things you didn’t know about administrative professionals. (2023). Post-It.com; MMM-ext. https://www.post-it.com/3M/ en_US/post-it/ideas/articles/5-things-you-did-not-know-aboutadministrative-professionals/
2. Fun facts about Administrative Professionals Day. (2016, April 27). Boston 25 News. https://www.boston25news.com/news/ fun-facts-about-administrative-professionals-day/245295957/
Advancements in Immunotherapy and Targeted Therapy in Gastrointestinal Cancers, continued
role of PARP inhibitors in other treatment settings in pancreatic cancer is currently being explored.
Other Mutations: Other alterations such as RET and TRK fusions are rare in pancreatic cancer but can be treated with selpercatinib (for RET fusions) and larotrectinib or entrectinib (for NTRK fusions). Similarly, KRAS G12C mutation is rare in pancreatic cancer. Studies are currently exploring the role of KRAS G12 C inhibitors (sotorasib or adagrasib) in this patient population.
FGFR 2 Alterations: FGFR 2 alterations are present in 16% of patients with cholangiocarcinoma including 20% of patients with intrahepatic cholangiocarcinoma. Recently, the oral FGFR inhibitors pemigatinib, infigratinib and futibatinib were approved by the FDA for patients with biliary cancers and FGFR alterations who have failed first-line therapy.
IDH Mutations: IDH1 mutations are present in approximately 25% of patients with biliary cancers. Ivosidenib was approved by the FDA in patients with biliary cancer and IDH1 mutations who have progressed on first-line therapy.
HER-2 Neu: Approximately 20% of patients with biliary cancers harbor a HER-2 neu molecular abnormality. Studies have suggested a potentially favorable effect of HER-2 neu targeted therapy such as trastuzumab plus pertuzumab or lapatinib, or trastuzumab deruxtecan in these patients.

BRAF Mutations: BRAF V600E mutation is present in up to 5% of patients with biliary cancers. Studies have suggested a favorable benefit of dabrafenib and trametinib in patients with BRAF V600E mutant cancers including biliary tract cancers. This combination was approved by the FDA in patients whose tumors harbor this mutation, have progressed on previous treatment and who have no satisfactory alternative treatment options.
Other Mutations: Similar to other gastrointestinal cancers, RET and TRK fusions are rare in biliary cancers but can be treated with selpercatinib (for RET fusions) and larotrectinib or entrectinib (for NTRK fusions) if present. Treatment of RET and TRK with their respective inhibitors is typically associated with a high response rate and favorable clinical benefit.
In summary, multiple new treatment modalities have evolved to help cancer patients and oncologists in the battle against cancer. Advances in the testing of tumors for genetic changes and in the discovery of targeted therapy and immunotherapy have provided cancer patients and their families with renewed hope of experiencing improved treatment outcomes without sacrificing their quality of life. Research will continue to help advance cancer treatment and possibly allow patients to triumph in the war against cancer.
WE'RE GETTING EXCITED FOR CLINICAL SUMMIT 2023!
Attendees will have access to exclusive learning programs such as Dr. Neil Love’s Research to Practice CME Program, AON research updates and more. Plus, dedicated time to network with fellow AON physicians, leaders and participating partners from across the nation.

It is not a shock to report that nursing is the nation’s largest healthcare profession and is expected to grow by over 203,000 new nurses each year through 2031, according to the American Association of Colleges of Nursing’s Nursing Fact Sheet.1 Nurses are also among the most trusted profession, securing the number one spot for honesty and ethics.2
“Nurses deliver great value to physicians and patients, and this is no different for our AON practices,” said AON Chief Medical Officer Dr. Stephen “Fred” Divers.
“Our nurses are well-educated and compassionate and bring a level of care that makes an incredible difference for our patients who are facing a challenging journey. While Nurses Week is only recognized once a year, we collectively share our gratitude for our nurses — and nurses everywhere — for their hard work and dedication to their patients.”
In honor of Nurses Week 2023, employees across the network shared why they decided to pursue a career in nursing and why they love what they do:

We became oncology nurses to serve this community of amazing people who need extra love and comfort. No one deserves to fight alone. We are committed to fight alongside them through laughter, encouragement and positivity. We feel we just belong here.”
It is the personal bond you establish with patients and their families — offering them hope and encouragement — as they face this serious illness. This, to me, is the most satisfying aspect of oncology nursing and is, in itself, the greatest reward.”



I empathize with my patients with whatever situation they encounter. Our patients become family as we share laughter, tears and hugs during the challenging times in their lives.”
I am blessed to be able to care for such an amazing group of patients, from diagnosis to remission, or even to death. They are courageous, strong, caring and compassionate. I am living my God-given purpose.”

My job as a clinical nurse manager is to make sure that the patient is the number one priority. I am blessed to work with all those at HOC and truly enjoy my job. AON has been wonderful to work for, and they are always focused on the patient first.”

Being an oncology nurse is the most challenging, humbling, heartwarming and rewarding career. I wouldn’t change it for the world. It’s all I’ve ever known to be honest. I had leukemia as a child and so hospitals and doctor offices became a part of my normal everyday life. So, you see, I never really chose oncology. Oncology chose me.”

The patients and families I take care of are very special to me, and helping them through one of the hardest times of their life is beyond rewarding.”
I am in awe of what my patients trust me to do every day and feel blessed to be able to share in their lives. I have been in oncology my entire nursing career and don’t know of anything else I would rather do. I absolutely love my job!”

The bond I have with my patients is like no other and to be a light in the darkest time of someone’s life is special to me. I believe I was meant to be in this position for a reason and to wake up every morning knowing I am right where I need to be is a blessing.”
Oncology is one of the most difficult specialties to work in but truly one of the most rewarding. Cancer patients are facing a terrifying diagnosis and require a lot of compassion and guidance. I love trying to be that for people. Cancer is a difficult journey, and I hope that I can help make that journey just a little easier.”
The stories, lessons and blessings that my patients have given me over the past 26 years are the reasons I have stayed in oncology, where lifechanging experiences happen every day."



I love oncology nursing because I get to spend time with my patients. It’s a great feeling to hear patient stories and connect with them and know you can be a bright spot in their day.”


References:
1. American Association of Colleges of Nursing (n.d.). Nursing Fact Sheet. Retrieved May 24, 2023, from Nursing Fact Sheet. (n.d.). www.aacnnursing.org. https://www.aacnnursing.org/ news-data/fact-sheets/nursing-fact-sheet#:~:text=Nursing %20is%20the%20nation.
2. Brenan, M. (2023, January 10). Nurses Retain Top Ethics Rating in U.S., but Below 2020 High. Retrieved May 24, 2023, from https://news.gallup.com/poll/467804/nurses-retaintop-ethics-rating-below-2020-high.aspx.
3. PBS (2023, March 16). Pandemic burnout worsens nursing shortages in hospitals across U.S. PBS News Hour. Retrieved May 24, 2023, from https://www.pbs.org/newshour/show/ pandemic-burnout-worsens-nursing-shortages-in-hospitalsacross-u-s#:~:text=had%2C%20each%20nurse.-,The%20 national%20nursing%20shortage%20dates%20back%20 decades%2C%20but%20the%20COVID,are%20pleading%20 for%20more%20support.
American Oncology Network, a Rapidly Growing Network of Community-Based Oncology Practices, Receives Strategic Investment from AEA Growth
Learn more
EY Announces Todd Schonherz of American Oncology Network, LLC as an Entrepreneur Of The Year® 2023 Florida Award Finalist Entrepreneur Of The Year celebrates ambitious entrepreneurs who are building bolder futures.
Learn more
American Oncology Network Announces List of Research Studies Presented at the ASCO 2023 Annual Meeting
AON physicians and leaders share their latest cancer findings with fellow thought leaders at the annual conference.
Learn more
American Oncology Network Announces Texas as New Operating State with Launch of Community-Based Oncology Clinic
American Oncology Network expands into Texas with the opening of Lone Star Oncology.
Learn more
American Oncology Network Announces Expansion into Florida with New Community Oncology Practice Serving Safety Harbor and the Tampa Bay Area
New oncology practice Florida Oncology & Hematology is now open to patients. Learn more
American Oncology Network and Messino Cancer Centers
Welcome Neuro-Oncologist Jeanette Pueschel Larson, MD, to Physician Team
Dr. Jeanette Pueschel Larson joins the practice as the newest physician. Learn more

American Oncology Network Announces Alti Rahman as New Chief Strategy and Innovation Officer
Rahman joins AON with 15 years of experience in healthcare and oncology. Learn more
American Oncology Network Welcomes Susan Sabo-Wagner as Vice President of Clinical Innovation
Susan Sabo-Wagner joins AON effective July 3.
Learn more
Kandis Shumaker, BSN, OCN MESSINO CANCER CENTERS
What I love about oncology nursing is I get to help my patients journey through the hardest thing in their life. These wonderful patients have taught me to appreciate not just the golden moments in life but also the gut-wrenching times too because every day is a gift.”
The idea of “burnout” is not a recent finding. In fact, it was first termed by American psychologist Herbert Freudenberger in the 1970s when he published an article titled “Staff BurnOut;” however, the idea behind burnout had already been identified prior to it being officially named.1, 2 For Freudenberger, he was devoted to his position as a psychologist and carried two jobs helping patients in New York. His personal experience with burnout, including not being able to get out of bed, inspired his article that, while not thoroughly researched with extensive surveys, led to further analysis of the symptoms. Since then, burnout has been a popular topic in business, mental health and well-being.
According to the American Psychology Association, burnout is described as “physical, emotional or mental exhaustion accompanied by decreased motivation, lowered performance and negative attitudes toward oneself and others. It results from performing at a high level until stress and tension, especially from extreme and prolonged physical or mental exertion or an overburdening workload, take their toll.”3 Burnout can
be experienced during all points life and in varying degrees, whether it is at work, home or elsewhere. It may also be more common in certain industries than others. For example (and not surprisingly), healthcare workers are more vulnerable to burnout than other professions because of the high stress that is involved in the everyday tasks. While burnout may be experienced at different levels in different fields, it is a global concern and is now at an “all-time high,” according to a recent Gallup report.⁴
Here are several symptoms that may indicate burnout is on the horizon or already there:⁵

CARET-RIGHT Being cynical or critical of self or work.
Difficulty getting up.
Irritability or impatience with others.
Lacking energy.
Difficulty concentrating.
Lacking satisfaction from achievements.
Being disillusioned about job.
CARET-RIGHT Using food, drugs or alcohol to feel better or not feel.
CARET-RIGHT Difficulty sleeping. CARET-RIGHT Experiencing unexplained headaches, stomach or bowel problems and other health concerns.
Burnout is often mistaken for exhaustion, which is temporary. It can also mirror symptoms of other medical conditions such as depression. A main difference, however, between the two is that burnout is often associated with a specific situation or scenario while depression does not always have a specific trigger.⁶ From a professional standpoint, burnout can result in a decrease in work performance and lack of collaboration, which can create further stress and frustration. Additionally, if burnout is not taken seriously, it can result in fatigue, insomnia, emotional distress, heart disease, high blood pressure and an increased vulnerability to other diseases.⁵
AON provides all employees with an employee assistance program (EAP) through ComPsych Guidance Resources. The program provides confidential 24/7 support, resources and information around a variety of focuses including work-life balance and emotional support. To access the EAP, visit guidanceresources.com and enter your employee ID.
References:
1. Information, N. C. for B., Pike, U. S. N. L. of M. 8600 R., MD, B., & Usa, 20894. (2017). Depression: What is burnout? In www.ncbi.nlm.nih.gov. Institute for Quality and Efficiency in Health Care (IQWiG). https:// www.ncbi.nlm.nih.gov/books/NBK279286/#:~:text=The%20term%20%E2%80%9Cburnout%E2%80%9D%20 was%20coined
2. Malesic, J. (2022, January 1). Burnout dominated 2021. Here’s the history of our burnout problem. Washington Post https://www.washingtonpost.com/history/2022/01/01/burnout-history-freudensberger-maslach/
3. American Psychological Association. (n.d.-a). APA Dictionary of Psychology. Dictionary.apa.org. https://dictionary. apa.org/burnout
4. Beheshti, N. (2022, June 22). New Gallup Workplace Report Says Employee Stress Is At An All-Time High. Forbes. https://www.forbes.com/sites/nazbeheshti/2022/06/22/new-gallup-workplace-report-says-employee-stress-is-at-anall-time-high/?sh=6cee21e2335c
5. Mayo Clinic Staff. (2021). Know the signs of job burnout. Mayo Clinic. https://www.mayoclinic.org/healthy-lifestyle/ adult-health/in-depth/burnout/art-20046642

6. Cleveland Clinic. (2022, February 1). Burnout: 5 Signs and What to Do About It. Cleveland Clinic. https://health. clevelandclinic.org/signs-of-burnout/
7. Information, N. C. for B., Pike, U. S. N. L. of M. 8600 R., MD, B., & Usa, 20894. (2017). Depression: What is burnout? In www.ncbi.nlm.nih.gov. Institute for Quality and Efficiency in Health Care (IQWiG). https://www.ncbi. nlm.nih.gov/books/NBK279286/#:~:text=The%20term%20%E2%80%9Cburnout%E2%80%9D%20was%20coined
Luckily, there are ways to stop burnout in its tracks. According to the Mayo Clinic, burnout can take a toll on both your physical and mental health.5 Here is where to start if burnout begins to creep in:
Find support by talking to someone, whether that be a supervisor, an individual outside of work or someone through an employee assistance program (EAP).
Look for relaxing activities that allow for both physical and mental recovery.
Get moving and exercise. Being outside has been proven to boost mental wellness.⁷
Try to get more sleep.
Give a go to mindfulness practices.

1. How long have you been with AON?
Since April 2021.
2. What does a "day in the life" look like for you in your role?
My daily tasks surround making sure my team has all the tools they need to perform their jobs effectively all while assessing the laboratory needs in our network and creatively developing ways to grow our service line. I also troubleshoot problems throughout the network on a daily basis, communicating with lab teammates and leaders, physicians, senior leadership and other stakeholders.
3. What goals are you and your team working to achieve?
We are always looking to optimize lab operations at the central lab as well as the lab operations on the clinic side. One of our major forward projects and top priorities right now is assessing various options to partner for NGS (nextgeneration sequencing) testing at the central lab in Fort Myers.
4. How does your role contribute to AON's overall mission and goals?
Among laboratorians across the globe, there is a statistic called the 70/70 rule. This rule states that 70% of all medical decisions are based on laboratory data and 70% of a patient’s medical record is made up of laboratory data. While many medical and laboratory journals agree to disagree on the full truth of this statement, I believe the first half regarding medical decisions
is true. With this thought, the lab contributes to AON’s overall mission quite nicely. AON stakeholders have partnered together to ensure the long-term success of community oncology with the focus of providing the highest quality care for our patients. The lab is a major contributing factor that directly aligns with this mission and is a driving force that helps make it achievable.
5. What are you most proud of when it comes to your team and department?
My team does whatever it takes to get the job done. Going the extra mile and putting our patients and providers first are normal and occur without fear of contradiction. They truly embody servant leadership and are tenacious when it comes to all they have been given responsibility for. I am proud of the sacrifice they display not only for our patients but also for their fellow teammates. If there were such an award, I would award all of them with the “GSD” award: “Getting Stuff Done.” I am honored to lead this team.
6. What principles guide your work and vision?
1 Corinthians 9:19, 22b sums this up for me. This is my fundamental core belief and is the basis of my doctoral research: “For though I am free from all men, I have made myself a servant to all, that I might win them more; I have become all things to all men, that I might by all means save some.”
20 questions with
7. How do you define the word success?
For me, success is the manifestation of practice makes better, hard work, learning from failure, loyalty and persistence.
8. How do you lead your team? What is your leadership style?
My leadership style would be considered Situational/Agile/Adaptive. This is also called “New-Age” Leadership. It works well for me simply because I believe leadership is “whatever you need at the time,” and this is facilitated through personality in action. This comes from my fundamental Christian beliefs and faith.
9. What's your favorite part about working for AON? Why AON?
My favorite part of working for AON is being aligned with like-minded professionals who really care not only about our patients but our teammates. This is exemplified by our CEO and trickles down to every staff level at AON. I truly believe AON is making a difference in the lives of our patients and teammates alike.
10. What has been the most memorable moment for you while you've worked for AON?
Getting a call from a provider who had a critical patient in need of our services. The lab team came together alongside the provider, pathologists and other stakeholders to ensure the most accurate and rapid turnaround time for these sensitive and critical results (48 hours). Had these tests been sent out to a reference lab, the provider would not have gotten results until about seven to 10 days conservatively! It was one of the highest levels of communication and teamwork I’ve seen at AON to date!
11. What motivates you to get up and get to work in the morning?
The fact that I don’t “get” to or “have” to go to work — I MUST! If I am to accomplish the
task that I was placed on this earth for, coming to work is necessary, and it is a privilege I get to do this at AON.
12. What is a quote you live and/or work by?
“Be Intentional.” It’s hanging on the wall in my office.
13. What are your favorite hobbies outside of work?
Golf, more golf and fishing with my dad.
14. What is your favorite book (or books)?
The Bible and any book on leadership.
15. What is a fun fact about you?
I am a lucid dreamer and can fly in my dreams. Sometimes I can wake myself up from a dream if I don't like it. Crazy I know!
16. What piece of advice would you give your younger self?
Stay focused and stay on the path.
17. List three adjectives that describe your personality.
Humorous, adaptive and logical but reasonable.
18. What is one of your favorite travel destinations, or where do you hope to travel to in your lifetime?
Ocho Rios, Jamaica, is my favorite vacation spot. I would also like to travel to Israel.
19. Who is your hero?
My grandmother who lived to be 99 years old.
20. If you had three wishes, what would they be?
Of course, more wishes in perpetuity!
Krystal has been with AON since its inception and is now the associate director of revenue cycle. Her previous roles were as a business office manager and then as a revenue cycle optimization analyst. Her first AON Go-Live was when Genesis Cancer and Blood Institute joined in 2018. “I love working with supportive colleagues and leadership,” Krystal shared. “AON has always supported a culture of continuous learning, which is inspiring and makes me feel my work has an impact.”
Being in her current position has offered her the opportunity to tackle the challenges of working through the many areas of the revenue cycle. Krystal also enjoys collaborating with the

different practices and provider specialties to optimize workflows, improve data collection and increase practice financial performance to ensure patient care is billed and collected correctly. “It has been a tremendous experience seeing the technology and treatment development expand in cancer treatment,” she explained.
When she is not working, Krystal loves spending time with her family, either hiking or relaxing by a pool on a hot Florida day. She enjoys attending live music and local symphony concerts with her husband. Krystal and her husband are both members of their local Native Plant Society and spend time gardening, on trails or at their local botanical garden.
Miranda is the lead nurse at Georgia Oncology and Hematology Consultants in Brunswick, Georgia, where she has worked for the past 15 months. Prior to that role, she served as a nurse manager. Her journey into oncology began during her time as a new nurse graduate, and she shares that oncology quickly became her passion.
“As an oncology nurse, you become part of a person’s life during what is quite possibly the most difficult time they have ever experienced,” Miranda shared. “Through my years in oncology, I have laughed, cried and developed special bonds with my patients. They become more like family. The impact they have made on my life truly reinforces that I am exactly where

I am meant to be. Caring for patients with cancer has made me able to appreciate how beautiful and fragile life is.”
Her commitment to oncology led her to AON. She found that AON’s values and the support offered to patients and staff surpassed her expectations, and she considers herself continuously inspired to work with an organization that puts patients first. “I am so thankful for the opportunity to continue to share my knowledge
July 3-28
July 3-28
July 10-14
July 17-18
July 24-28
and experience with Dr. Moran and the staff,” Miranda explained. “They truly exemplify the AON C.A.R.E. values, and I consider myself fortunate to be a part of this amazing team.”
In her downtime, she enjoys spending time with her husband, kids, and most of all, her two grandchildren. She loves being at the beach and traveling to tropical places. Miranda also keeps herself busy by custom decorating sugar cookies.
 Oncology Dietitian AON Care Management
Oncology Dietitian AON Care Management
"Breakfast is the most important meal of the day.” How many times have we heard this popular saying? This adage does carry merit as research has shown the benefits of eating breakfast. But even with this knowledge, we still give several reasons for not eating breakfast such as not being hungry in the morning, having nothing to eat in the kitchen as well as not having enough time for a meal before heading out for the day.
Is skipping breakfast really harmful to your health? Here are a few factors you’ll want to consider when thinking of your next breakfast meal.

According to research, a regular breakfast is linked to improved overall health, including better diet quality and weight management and decreased risk for some chronic diseases. Research suggests that breakfast eaters have improved concentration and problem-solving abilities, better attitudes toward work and school, and higher productivity in the late mornings. Athletes and physically active individuals who eat breakfast also experience the benefits of breakfast and have higher endurance levels.
On the flip side, research repeatedly finds that breakfast skippers have an inadequate
fruit and vegetable intake, higher consumption of soft drinks, increased tobacco use, less endurance and decreased physical activity, poor dental health, and lower academic and work performance. Skipping breakfast is also associated with chronic inflammation leading to increased risk for diabetes, hypertension, heart disease and cancer. In addition, studies reveal that breakfast skipping (both occasional and frequent) is associated with depression and restless sleep.
Breakfast provides a great start for eating well and a healthy lifestyle. Breakfast leads the way for eating more fruits, vegetables, whole grains and calcium-rich dairy foods. Those who eat a morning meal usually consume more vitamins, minerals and fiber. Whereas those who skip breakfast are more likely to miss out on the key nutrients that a morning meal brings.
Research supports that those who eat breakfast are less likely to be overweight and that morning meals help with weight loss and healthy weight maintenance. It is speculated that breakfast plays a role in regulating appetite, hormone levels and the
number of calories we burn throughout the day even though the reasons for these results are not exactly clear. It could be that eating breakfast, like being physically active, is a common behavior among those who maintain a healthier weight. The foods chosen at breakfast may be another factor. Regularly choosing highfiber cereal topped with nuts or seeds and milk has been linked to a healthy weight, thanks to the satiety from the meal’s fiber and protein. Timing can also be a reason. Compared to skippers, breakfast eaters are less likely to be overly hungry for a midmorning snack or lunch and, therefore, have less impulsive snacking habits or an urge to eat larger portions for lunch. It is important to note that eating breakfast meals that are higher in calories is associated with a higher body mass index (BMI).
Starting the day with a healthy breakfast can benefit your heart, digestion, bone health and blood sugar management. This could be related to the foods consumed at breakfast such as whole-grain breads and cereals, dairy foods, whole fruits and 100% fruit or vegetable juices. Researchers are finding that breakfast may also help regulate blood glucose, insulin levels and fat metabolism as well as reduce the risk of metabolic syndrome.

Choose whole foods and avoid processed foods that have extra sugar and are high in sodium and fat. Aim for 15% to 25% of your total calories for the day (based on 2,000 calories), which equates to between 300 and 500 calories. Another great tip is to include foods from at least three different food groups on your breakfast plate. Examples of quick, simple nutritious breakfasts:
CARET-RIGHT Hard-cooked egg, high-fiber bran muffin and sliced banana.
CARET-RIGHT Whole-grain toast slathered with a thick layer of peanut butter and a glass of 100% orange juice.
CARET-RIGHT Fresh berries topped with Greek yogurt and whole-grain cereal.
CARET-RIGHT Oatmeal with added walnuts and diced apples topped with a dash of cinnamon.
CARET-RIGHT Breakfast burrito with scrambled eggs, black beans, salsa and a sprinkling of crumbled feta cheese wrapped in a whole-grain tortilla shell.
INGREDIENTS
1 peeled banana
¾ cup oats
1 egg
1/2 cup plus 1 tbsp plain Greek yogurt
1 tsp cinnamon
Pinch of salt
1/4 cup blueberries
1/4 cup sliced strawberries
Sprinkle of shredded coconut
1. In a bowl, add banana, oats, egg, one tablespoon of yogurt, cinnamon and salt.
2. Use a fork to mash the banana to create a batter with an even consistency and then transfer it to a heated skillet.
3. Cook over medium heat for about five minutes. Use a spatula to flip and break up the pieces into a scrambled-egg consistency.
4. Cook, stirring frequently, until the scramble is golden brown and chunky like soft granola.
5. Using a cereal bowl, pour the remaining yogurt into the bowl and then divide the scrambled oats into thirds.
6. Place the first third on the yogurt base, scatter the blueberries on the first layer, top the blueberries with the next third of scrambled oats, layer the sliced strawberries next and add the final third of scrambled oats.
7. On top, sprinkle with shredded coconut and enjoy.
NUTRITIONAL INFORMATION:
Per 1 Serving
Calories: 330
Protein: 19.2g
Carbohydrates: 39.5g
Dietary Fiber: 7.1g

Sugars: 8.2g
Fat: 5.2g
Saturated Fat: 1.6g
Sodium: 280.3mg
For complete recipe and nutrition facts: Eating Well



Ja ne was feeding her horses on a beautiful fall evening with good temperatures and no wind. Sitting close by in his wheelchair was Don, Jane's husband of 17 years. He wasn’t feeling well, so he went back to the house to wait for dinner.
Now all alone, Jane was carrying feed buckets when all of a sudden it felt like her world was spinning. “It was like everything was going in slow motion and so many things were running through my mind. I think angels must have guided me because it is the length of a football field from the barn to the house.”
Miraculously making it back to the house, she immediately collapsed
onto the couch. “I was able to reach for my cell phone and dial 911 then I handed the phone to Don,” said Jane. After going to her small-town hospital emergency department, she was flown via helicopter to the larger hospital in Springfield. Within 24 hours she was having brain surgery.
Before this life-changing dizzy spell Jane was busy being Don’s caretaker for about five years. She literally took care of him 24 hours a day. He had many health issues including 13-hours a day of home dialysis treatment for his failing kidneys. It makes total sense why Jane didn’t realize she was sick too.
Instead of realizing the symptoms
of extreme fatigue were due to her being sick, she just shook it off thinking it was exhaustion from her caregiver duties and taking care of their small farm with horses and chickens. “Whenever I got a moment to sit down, I would say to Don, I am tired…bone tired.”
After her first brain surgery in October 2014, they didn’t find anything wrong. Sadly just a month after her surgery, she lost her loving husband Don.
Then, three months later, Jane was experiencing dizziness again, suffering another stroke. A second brain surgery followed in January 2015. This time they found melanoma on her
brain and right lung.
Still dealing with excruciating pain and could hardly move, it was discovered that Jane also had melanoma on her spine. So on May 2016, she had her first spine surgery, “The surgeon cut from the base of my neck down my upper spine about 11 inches long.”
Even though the doctor with a grim response said she has melanoma cancer and there’s not much they could do, Jane said she felt relieved to finally know the cause of her fatigue and pain.
And with a slight laugh she said, “Of course that wasn’t good enough for me, so I went back a month later with the same pain and symptoms, and they found more melanoma requiring a second surgery in July 2016. This time cutting six inches further down my spine.”
As a mother of three adult children and with eight grandchildren, Jane is used to taking care of others. But now she is forced to depend on others for help she explained, “It’s difficult for me to rely on others, but I’ve learned
to appreciate the help and to listen to my body. When I am tired, I really am and need to take a rest.”
After having to drive an hour away from where she lived to Springfield’s hospital for treatment, Jane was thrilled when Oncology Hematology Associates (OHA) opened up a clinic in Monett only 10 minutes from her home.
Affirming that she was one of the first patients to be seen at OHA Monett, “I am sorry that so many people are sick, but I am happy that Oncology Hematology Associates is here to take good care of us. I’ve seen the clinic grow so much, and there are many services available to patients.”
Jane went on to explain how she is a living miracle, having survived and endured four major surgeries, radiation and cancer treatments since October 2014. “We are so blessed with medical technology right now, with immunotherapy and many new medications being approved every day!”

She also referred to her OHA oncologist Dr. Holden as a "blessing" for the care and treatment they provided. Continuing, “I know
Roger Holden, MD, PhD ONCOLOGY HEMATOLOGY ASSOCIATES
“I know OHA/AON is a business, but it takes special people to understand what cancer patients are going through and to help guide you. Dr. Holden gives me personal care and attention and truly listens to me, and I appreciate that.”Melanoma is the most dangerous type of skin cancer that starts in the cells that produce melanin.
Patient Story: Jane, continued
OHA/AON is a business, but it takes special people to understand what cancer patients are going through and to help guide you. Dr. Holden gives me personal care and attention and truly listens to me, and I appreciate that.”
OHA medical oncologist, Roger Holden, MD, PhD, said “With extensive disease, brain cancer and melanoma, if it was eight years ago, she wouldn’t be here with us today. But with new advances especially with immunotherapy treatments, it’s helping to keep our patients surviving longer.”
With excitement in his voice, Dr. Holden continued, “Jane is now cancer-free and her outlook is great!”
Jane is thankful for her wonderful family, especially her son, Josh and his wife, Sara, for driving her to treatments. Her faith also gives her peace with the cancer diagnosis. “We are all going to hit a point where we just don’t go one more step. And I know whatever happens, I’m not alone.”
She credits her Lord and Savior Jesus Christ, emphasizing, “He is my friend and with me all the time, as well as my
provider and protector.”
Instead of focusing on the things she can’t do anymore, Jane decided to learn new things and took a woodworking class. Proudly stating, “I learned to hand carve, and I was able to make a beautiful bookshelf for my grandchildren. I hope this leaves a positive legacy and memories for them about going to grandma’s farm."

"I recommend not only for cancer patients, but everyone should be open to new things and don’t be afraid to try something new,” said Jane.
PATIENT TREATED AT:
Eight Goals of the National Cancer Plan

Prevent cancer. Detect cancers early. Develop effective treatments. Eliminate inequities. Deliver optimal care. Engage every person. Maximize data utility. Optimize the workforce. Learn more about 2023’s National Cancer Plan by visiting nationalcancerplan.cancer.gov/.












At AON, we’re making great strides toward closing the cancer care gap by ensuring every patient has access to the care needed to help fight their cancer.
With an expanding network of more than 190 providers across 19 states, our practices are not only in big cities, they’re in rural areas where medical resources are scarce. Our clinicians are interconnected across state borders and focused on driving change by remaining at the forefront of new discoveries. Together, we’re doing more.
To drive equity forward, we aim to deliver precision medicine as a standard of care, adopt next-generation sequencing and provide structure to genomic data and more.

At AON, you’re part of a fast-growing network that’s setting great things in motion, exploring new horizons and breaking barriers to cancer care — where the future of cancer care is bright. Visit
