



Bringing Clinical Trials to Community Oncology
How APPs Strengthen Patient Care
SPOTLIGHTS: Karen Quick, Jennifer Hare and Correna Wells
Case Study: Hope Cancer Care of Nevada

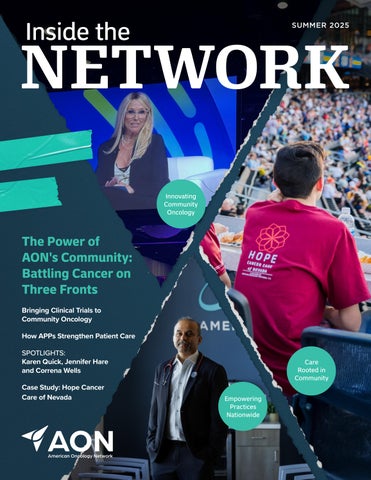
Innovating Community Oncology




Our strength lies in our ability to blend deep local connections— community—with the resources and expertise of a national network, empowering both our patients and the practices that serve them.
At AON, everything we do is driven by our mission to provide exceptional, patient-first cancer care in the communities we serve. This year’s COA 2025 Community Oncology Conference in April was a powerful reminder of why our mission—and our community—is so important. Surrounded by professionals who share a passion and dedication to community oncology, we had the opportunity to learn from some of the brightest minds in the field—leaders shaping the future of cancer care through innovation, collaboration, and an unwavering commitment to patients. And we are those leaders.
This year, 14 AON speakers took the stage, and more than 40 AON providers and leaders attended the event. The conference’s themes of transparency and advocacy, partnerships, and community aligned perfectly with our work at AON. We’re constantly acknowledging—and striving to remove—barriers to care, partnering to expand access to life-saving treatments, and working to ensure that every patient receives the highest quality care close to home. Our strength lies in our ability to blend deep local connections—community—with the resources and expertise of a national network, empowering both our patients and the practices that serve them.
But our strength also lies in the community we create for each other—the open conversations about what’s changing, what we’re learning, what’s working, and what we can improve. The relationships we build and the way we move seamlessly between teacher and student make us all better at delivering the exceptional, patient-first care our communities expect and deserve.
As I reflect on this year’s conference, one thing is clear: the future of cancer care is in our hands. Together, we will continue to push forward, advocate for our patients, and build a healthcare system that truly puts them first. Thank you for being part of this journey—and our community. Your dedication and compassion make all the difference.
Stephen “Fred” Divers, MD AON Chief Medical Officer
Navigating Persistent Financial Toxicity in the Patient Experience
Feature: Susan Sabo-Wagner, MSN, RN, OCN
At the 2024 Patient-Centered Oncology Care (PCOC) event, during a session titled, “Patient Experience is Improving Until Bills Arrive,” experts addressed how financial toxicity persists in the patient experience in cancer care, examining both progress and ongoing challenges.
Learn more
Nurses Can Help ‘Demystify’ Genetic Testing Results
Feature: Susan Sabo-Wagner, MSN, RN, OCN
Genetic testing results can have numerous implications in cancer care—from targeted treatment regimens to the need for family members to get tested. Oncology nurses are in a prime position to help guide patients through the process, according to Susan Sabo-Wagner, MSN, RN, OCN, NEA-BC.
Learn more
Navigating the Enhanced Oncology Model: Insights and Strategies from American Oncology Network
Feature: Melody Chang, RPh, MBA, BCOP
Melody Chang, RPh, MBA, BCOP, explains how American Oncology Network leveraged its experience with the Oncology Care Model to address challenges when adopting the Enhanced Oncology Model.
Learn more
Reversal of Executive Order 14087 Raises Questions About Future Drug Pricing Reforms
Feature: Melody Chang, RPh, MBA, BCOP
Executive Order 14087 aimed to reduce drug costs through Medicare negotiation, state support, and promoting competition, but its repeal halts these initiatives.
Learn more
Utilizing Intravenous Iron Injections to Improve Patient Outcomes
Feature: Melody Chang, RPh, MBA, BCOP
A discussion of comprehensive approaches to iron deficiency anemia (IDA), from its pathophysiology and diagnosis through various treatment options such as oral and intravenous iron formulations, addressing challenges such as hypophosphatemia, treatment adherence, insurance barriers, and future directions in patient care, emphasizing the importance of individualized treatment strategies and monitoring protocols to optimize outcomes.
Learn more
Team- and System-Based Approaches to Managing LEMS and Ensuring Access
Feature: Alti Rahman, MHA/MBA, CSSBB
Alti Rahman, MHA/MBA, CSSBB, discusses how comprehensive care coordination between specialists, proactive adverse effect management, and innovative care models can optimize treatment outcomes for Lambert-Eaton myasthenic syndrome (LEMS) patients, particularly those with dual diagnoses like small cell lung cancer (SCLC), while ensuring both clinical effectiveness and costefficiency through managed care strategies.
Learn more


Todd Schonherz Chief Executive Officer

Kristin Matisziw Chief Compliance & Risk Officer

Puneeth Indurlal, MD Senior Vice President Strategic Operations

Stephen “Fred” Divers, MD Chief Medical Officer

Mark Moch Chief Information Officer

Ryan Olson, MD Medical Director Pathology

Becca Bell Vice President Strategic Partnerships

William “Billy” Keeney Vice President IT Operations

Melody Chang Vice President Pharmacy Operations

Dave McBreen Vice President AON Pharmacy

David Afshar Chief Financial & Operating Officer

Karen Pilley Chief Revenue Cycle Officer

Joe Verschleiser Chief Growth & Performance Officer

Anthony Belott Chief Development Officer

Alti Rahman Chief Strategy & Innovation Officer

Charles “Charlie” Goddard, II General Counsel

Terri Casey Chief Human Resources Officer

Steve Swart Executive Vice President Practice Operations

James Gilmore Chief Pharmacy & Clinical Services Officer

Tena Messer Executive Vice President Practice Operations

Michael Essik Vice President Finance

Guy Messer Vice President Radiation & Radiology Services

Katie Goodman Vice President Clinical Research

Karen Quick Vice President Human Resources

Kyle Hendrickson Vice President Mergers & Acquisitions

Susan Sabo-Wagner Vice President Clinical Innovation

Caroline Hewitt Vice President Marketing
In this three-article series, we explore how community impacts the work of American Oncology Network (AON) at all levels. Local practices are deeply rooted in their communities, offering care that is personal, accessible, and connected to local support systems. At the same time, AON’s national community amplifies the work of these practices, providing them with the resources, innovation, and support needed to elevate care—whether through enhanced purchasing power, expert payer contracting services, or AI-driven analytics.
Finally, AON is part of a larger community of oncology professionals who collaborate at prestigious national conferences, publish research together, and conduct groundbreaking clinical trials. Each of these interconnected communities— local, national, and professional—works together to put patients first, prioritizing their experience and ensuring the highest quality of care.
Community is a powerful force—one that shapes our personal and professional lives. It offers support, fosters growth, and creates a sense of belonging. In healthcare, being part of a community is especially important for both patients and providers. It enhances the patient experience, improves care, and provides access to invaluable resources. Whether it’s the local practice connecting patients to nearby nonprofits for financial assistance, or a group of oncologists consulting with each other to improve patient outcomes, community is essential in value-based care.
SPECIALTY PHARMACY
With access to 99% of available oral oncolytics.
LAB & PATHOLOGY
Supporting more informed and timely clinical decisions.
RECRUITMENT & HR
Recruiting talent needed.
RADIATION & RADIOLOGY
Helping establish radiation and radiology services.
Payer relationships to navigate value-based care.
MiBA & IT
Delivering realtime, data-driven insights and education.
Helping launch or expand clinical research trials.
Leading negotiations to reduce costs.
Tracking and monitoring drug supply and inventory.
Optimizing payments and reimbursement.


ommunity-based oncology is the reason I am here today,” says Sunshine Maracle, a stage 4 metastatic breast cancer survivor treated by Dr. Raja Mehdi at Hope Cancer Care of Nevada (HCCN). Her experience as a patient was so impactful that she later joined AON as a regional physician liaison and project manager, driven by her desire to advocate for others to receive the same high level of care she experienced at HCCN,
Sunshine Maracle Hope Cancer Care of Nevada
right in their own communities.
“Dr. Mehdi taught me that patient care goes beyond treatment—it follows you home,” she explains. “From health expos and survivorship programs to community outreach, setting patients up for success in their battle is crucial.” Maracle adds, “It’s my home, my reality, my fight. It’s why I dedicate my life to ensuring others have the resources and support they need to keep fighting.”
Maracle’s sentiment reinforces what many in communitybased oncology know: there’s no place like home. While we often say this, in cancer care, it takes on added significance. Patients receive high-quality care in the places where they live, work, and raise their families, helping them stay within their comfort zone during one of life’s most challenging times.

Moreover, it’s the local connections that AON practices have built within their communities that enhance the patient experience. By linking patients to people and resources close to home, they can feel more socially connected—particularly older patients or those battling cancer without a strong family or support network. Knowing there are people and organizations in the community to lean on helps patients feel less isolated.
At Central Georgia Cancer Care in Macon, Georgia, Melissa Shaw, director of clinical projects, oversees a volunteer program for patients and caregivers through the practice’s nonprofit branch, the Central Georgia Cancer Care Foundation. “We started the volunteer program to introduce another layer of comfort for patients and their families. Many actively seek opportunities to give back,” Shaw explains.
Shaw also established a Patient & Family Advisory Council (PFAC), bringing together patients and caregivers to provide valuable insights on improving the patient experience (see article on page 10). This council gives members a chance to both offer and receive support as they navigate similar challenges, and Shaw appreciates the deeper connections she forms. “Working in a community-based oncology practice allows me to build meaningful, personal relationships with patients and their caregivers, and that’s been incredibly rewarding,” she says.
For patients without a strong support system—whether through family or caregivers—there’s a risk of physical and emotional isolation, which can impact both their ongoing care and long-term outcomes. Many individuals facing a cancer diagnosis may feel reluctant to share their experiences due to concerns about how others will respond. Fear of being treated differently or misunderstood can make it difficult to seek an emotional support network, even when it is most needed.
“Our volunteers have been instrumental in offering emotional support for patients who may be alone, providing a listening ear and someone to talk to,” Shaw explains. Knowing there are people and organizations in the community there to support them makes them feel more socially connected.
According to the American Cancer Society, middle-aged adults (ages 45–64) living alone are 1.43 times more likely to face health risks compared to those living with others. This highlights the need for patient navigation services to ensure better health outcomes—a service Jennifer Hare, clinical nurse navigator at Genesis Cancer and Blood Institute in Hot Springs, Arkansas, provides as part of her role in patient care coordination.
Since transitioning from her role as nurse manager to nurse navigator in 2022, Hare has been integral in building the practice’s patient navigation program. “Our practice grew so quickly after joining AON in 2018 that we realized we needed to enhance patient care,” she explains.
Hare and her team meet with each new patient to assess their needs, connecting them to the resources they require, and this includes tapping into the strong relationships they’ve built with local community organizations.
“We manage the process and connect patients with resources, but much of what we do is through our partnership with a community-based cancer nonprofit,” Hare says. In certain limited and carefully screened situations for patients facing barriers to care, the needs-based support can even include temporary housing and other non-medical assistance.**
Like Melissa Shaw, Hare treasures the deeper relationships that emerge in community-based oncology settings. Reflecting on some of her favorite memories, she shares, “I got very close with one patient and his family. He built me a buffet table out of a solid piece of cedar wood, and he also made a bench for Dr. Diver’s office.”
“I've even shared meals with patients and their families in their homes. You develop friendships because they’re more than just patients. This is a deeper relationship than you might have in a hospital setting. In some cases, you’re sitting beside them at the end of life.”
Jennifer Hare,
MSN, RN, OCN Genesis Cancer and Blood Institute

**Assistance programs are managed independent from AON; eligibility and availability vary, and all services are provided in accordance with applicable federal and state guidelines.
When facing cancer, patients and their families seek more than just medical expertise—they seek connection, support, and a sense of empowerment. At Central Georgia Cancer Care (CGCC) in Macon, Georgia, the Patient and Family Advisory Council (PFAC) provides exactly that.
This initiative allows patients and their loved ones to take an active role in shaping the care experience while offering healthcare providers invaluable community-driven insights.
Melissa Shaw, director of clinical projects at CGCC, has been instrumental in developing and leading the PFAC. “We started this council to ensure the patient’s voice is truly heard in our practice,” Shaw explains. “They bring invaluable insights that help us continually improve our care. It’s a partnership— patients feel empowered, and we, as providers, gain a deeper understanding of their needs.”
The PFAC includes individuals with lived experience as patients, survivors, and caregivers, offers valuable input on a range of topics—from clinical processes to the overall patient experience. Members meet periodically with healthcare team representatives to share perspectives aimed at supporting continuous improvement in the quality and accessibility of care. “This collaboration has helped us address key areas like patient satisfaction survey results, gaps in education, and even the redesign of our phone tree,” Shaw says. “Most recently, the PFAC has provided essential feedback on our check-in procedures and an initiative to better align patient and provider expectations.”
One of the council’s most dedicated members, Ms. Lawahna (Gale) Thaxton, finds strength in helping others navigate their cancer journeys. “Being part


Melissa Shaw, BSN, RN, OCN Director of Clinical Projects
of the council gives me a sense of control over my experience,” she shares. “Cancer can make you feel powerless, but having a voice in how care is delivered—helping make things better for the next patient—gives me purpose. I also love offering encouragement to patients and families just starting this process.”
Beyond benefiting individual patients, the PFAC has been a valuable resource for the entire oncology team. “By working closely with the PFAC, we can proactively identify challenges and address them with actionable solutions,” Shaw explains. “Our practice gains deeper insights into the difficulties patients face, allowing us to tailor care in ways that go beyond standard clinical treatment.”
As an ASCO Certified Practice, creating the PFAC aligns with the ASCO Oncology Medical Home (OMH) Model. It’s a way for CGCC to continuously improve the quality of patient care, which not only supports certification but also helps enhance the patient experience. Involving patients and their families in this process ensures CGCC meets their needs and improves care in ways that matter most to them.
“The certification is an achievement we’re proud of, but our motivation has always been high quality, patient-first care,” says Shaw. “This council is a perfect example of how community involvement makes that possible.”
From Your Community to Ours Your Community, Your Care, continued
Dana Zager, a clinical social worker at Zangmeister Cancer Center in Columbus, Ohio, understands the emotional toll cancer takes on patients, their families, and the healthcare teams who support them. For the past eight years, she has worked tirelessly to build strong relationships with individuals and organizations within the community—connections that provide essential support and comfort for everyone battling cancer.
A key focus of Zager’s work is supporting older adults, many of whom face cancer alone, either by circumstance or choice. The majority of patients at AON practices nationwide are seniors, a demographic for whom social support is crucial in coping with both diagnosis and treatment. According to the National Institutes of Health (NIH), strong social connections are linked to improved emotional resilience, better health outcomes, and even higher survival rates.
“The bulk of who we see are older adults, people who are either retired or entering a new phase of life,” Zager explained. “That transition can be hard. They find themselves isolated, and when they face a cancer diagnosis on top of that, it becomes even more difficult.”
She has seen firsthand how isolation impacts seniors, particularly those whose families live far away. “We encourage independence, but as people age and resources become limited, many of my patients find themselves stuck at home,” she said. “That isolation can be devastating.”
For patients like 87-year-old Ronald Kushmaul, Zangmeister is not just a place for treatment but a crucial source of connection and care. Kushmaul has been receiving care at Zangmeister for seven years. While he has a supportive family, Zager’s help with transportation has been invaluable.
“My wife is in the hospital, and I can still drive, but some days, I just can’t do it,” Kushmaul said. “Dana has gone out of her way to make sure I have a ride when I need one. All I do is call her, and within 20 minutes, I get a text that my ride is arranged. She makes sure I get home safely. She’s wonderful—she’s our go-to.”
Kushmal’s transportation is possible because of a partnership Zager established with a local nonprofit dedicated to improving access to care for cancer patients, especially when travel may be a barrier. By working with community organizations, she ensures that patients who might otherwise miss critical care have reliable access to appointments.

From Your Community to Ours Your Community, Your Care, continued
“If you don’t treat the whole person—if you don’t address the things that make it hard for them to get to treatment or take care of themselves—then services are lost, and patients miss timely care,” she explained.
Beyond transportation, Zager has cultivated partnerships that provide everything from mental health support to financial assistance. She has also introduced therapeutic services, including pet therapy and yoga, to help patients find comfort during treatment. “We have a great therapy dog, Howard,” Zager said. “He’s a fluffy Great Pyrenees. Patients schedule treatment on the days he’s here, and staff keep biscuits in their pockets. He’s a bright spot for everyone.”
She also created a lending library at Zangmeister by partnering with a local bookstore to stock shelves with donated books. “It’s a small thing, but it makes a big difference in their day,” she said.
Through all of these efforts, Zager’s community relationships help patients feel supported locally. “When we come together as a community, patients feel it. And that makes all the difference.”
For patients like Kushmaul, the benefits of these community connections extend beyond medical care. One of the highlights of the practice for him has been the rotating art exhibits Zager curates.
“Just yesterday, she had a new exhibit,” Kushmaul said, his voice brightening. “It’s beautiful. My granddaughter is studying pediatric oncology, and she would love this. The art is vibrant, lively, and really adds so much to the room. It just makes the space come alive.”
From supportive offerings through local partnerships to the uplifting environment of a thoughtfully-designed space, community connections enhance the patient experience. In community-based oncology, care includes understanding the broader needs of those we serve—supported by meaningful relationships with community organizations committed to improving the quality and accessibility of care.



At Zangmeister Cancer Center in Columbus, Ohio, healing extends beyond medicine—it is woven into the very walls of the practice. Here, a unique form of therapy is at work—not in the form of medicine or radiation but, thanks to the creative vision of Clinical Social Worker Dana Zager, through the vibrant hues and expressive strokes of local artists. Her extensive background in art and art therapy inspired her to create a rotating art gallery that elevates the patient experience and enhances the workplace for the oncology team.
“There was this beautiful, 27-foot-long wall with recessed downlighting, and I thought, ‘This is a perfect place for art,’” she explains. “When I approached the doctors with the idea, they were completely on board. Now, we have a dedicated gallery space featuring work from local artists.”
The gallery connects Zangmeister to the broader Columbus community. Exhibiting artists often have direct or indirect experiences with cancer. “Many have either battled cancer themselves or have loved ones who have,” says Zager. “They bring not just their art, but their stories, their emotions, and their resilience. It’s a powerful exchange—patients and staff get to experience their work, and in return, artists find a space where their creativity can bring comfort and hope.”
The gallery, which rotates artwork every few months, has quickly become a cherished fixture in the center. “Patients and caregivers love it,” Zager


Dana L. Zager, MA, ATR-BC, MSW, LISW-S, OSW-C, ACHP-SW Clinical Social Worker
shares. “It’s something new for them to look at, something that momentarily transports them away from the stress of treatment. For many, it sparks conversations and connection.”
Beyond enriching the patient experience, the artwork provides momentary sanctuary for staff who work in a high-stress environment. Having a visually soothing, dynamic space can provide a much-needed mental break. “Our team is deeply invested in patient care, and that can take an emotional toll,” says Zager. “Art creates moments of reflection and relief, even in the busiest of days.”
Artists also benefit from exposure. While Zangmeister does not facilitate sales, the artists can leave contact information. “It’s a beautiful partnership,” Zager reflects. “We provide a space for artists to share their work, and in return, they help us create a more welcoming, healing environment.”
Through this initiative, patients, caregivers, and healthcare professionals alike are reminded that even in the hardest times, beauty, creativity, and connection can bring light. Enthusiasm for the gallery has led to plans for expansion. With a growing waitlist of artists, Zager is exploring additional wall space within the center. “We’re booked through 2026,” she said. “It’s amazing to see how much this means to the community.”
In the world of community-based oncology, a practice is more than just a healthcare provider—it’s an integral part of the community it serves. Patients, families, and caregivers take solace in knowing this resource exists close to home, but when that local practice joins AON, it gains the strength and resources of AON's national community while preserving its unique local identity.
Embedded in their local communities, these practices now tap into a larger, nationwide community, further enhancing their ability to provide patient-focused care.
Practices that join AON go from having the support of their local community to becoming part of a much larger, nationwide network of oncology professionals. This unique combination allows for the best of both worlds: maintaining the local presence and community connections while benefiting from AON's national
resources. AON emphasizes the importance of local identity, ensuring that each practice retains its name and continues to be recognized as an integral part of the community.
Beth Gann, senior regional director of operations, explains, “That local name stays the same because we recognize the value of that practice’s relationship with their community. We value that sense of
community and ensure continuity for our patients. I think that speaks to our patient first mission and is a value of community oncology.”
While the thought of joining a larger national network may raise concerns for some practices, AON prioritizes smooth integration. The goal is to enhance, not replace, the practice’s existing operations. Rather than imposing changes, AON listens closely to each practice’s needs. “It starts with listening—every practice has its own culture and history, so we take the time to understand what they need and how we can best support them,” says Karen Quick, vice president of human resources. “We don’t mandate changes; instead, we ask, ‘What would be most helpful to you?’”
The AON team works closely with practices to learn their business operations, helping fill gaps with national resources. “From there, we provide resources and tools to make their jobs easier, whether that’s streamlining administrative processes, enhancing benefits, or offering compliance support,” Quick adds.
While the integration process may feel overwhelming at first, the personal connections made within AON create a strong sense of community. “Before joining AON, I worked for nine years in a large oncology office. While I was excited for a new role, I was very nervous about the prospect of working remotely for a large organization after being an 'in-office' employee,” says Anne Marie F. Rainey, director of value-based care. “My nervousness and worry could not have been more misplaced. So many have been welcoming,
inclusive, and enthusiastic about the work our team does each day. The AON team always works to put patients and practices first, fostering connectedness across the network.”
Gann also highlights the importance of personal relationships within the network. “I was fortunate to be part of planning the first AON operations meeting last year. Local clinic leaders were invited to learn and grow with each other. They were able to form connections with their peers and interact with our executive and senior management teams. It creates that larger sense of community where you are not on an island, but part of this bigger group of islands that are connected.”
One of the largest transitions for new practices is adopting AON’s technological systems. While some practices may be accustomed to paper-based processes, AON introduces digital tools like Workday and SharePoint that enhance efficiency. “One of the biggest adjustments for new practices is technology,” says Quick. “It can be a shift, but these systems ultimately make things more efficient and give practice leaders real-time insights into their operations. We guide them through that transition so it’s as smooth as possible.”
Reid Helgemo, IT project manager at AON, shares a firsthand experience about the value of these systems and the support within the AON community. “Having opened over 40 clinics, one thing that stands out to me in every single location is the unwavering dedication of the clinic staff to their patients. I know that when I’m on-site, it’s a challenging time for them—learning new systems, adjusting to new workflows—but despite all of that, patients never miss a beat with their care. It’s a constant reminder that the work we do in IT isn’t just about technology—it’s about supporting the people who make quality patient care possible.” From
When a practice joins AON, they gain access to a wealth of resources that help them provide even greater patient care. These resources support everything from streamlining operations to enhancing human resources. “Recruiting also plays a big role,” says Quick. “We support practices in finding the right people for key roles, leveraging sourcing tools and recruiting resources that many practices wouldn’t have on their own.”
Moreover, practices maintain that local connection that is vital to patient care, but with the benefit of national support. “When the practice joins AON, they retain all their community connections that benefit the patient, but now they have access to even more resources, allowing them to provide an additional layer of patient care,” Quick explains.
The value of being part of a larger community network goes beyond the resources and support—it’s about connection, trust, and shared commitment to patient care. As Gann puts it, “We need a community. We create our own community and develop those trust relationships. So, for me, that's the biggest part of the community, the network, just helping practices know that they're not alone and that they have a large support system behind them.”
At the end of the day, our job is about connection—connecting people to the resources they need, to each other, and to the larger AON community. When employees feel supported and know they’re part of something bigger, that’s when we truly become one team. And that’s what makes AON special."
Karen Quick Vice President of Human Resources

The AON team always works to put patients and practices first, fostering connectedness across the network."

Anne Marie F. Rainey, MSN, RN, CHC, CPHQ, FACCC Director of Value-Based Care
Being part of this community has given me a deep appreciation for the resilience and commitment of the clinic teams I work with. It’s a constant reminder that the work we do in IT isn’t just about technology—it’s about supporting the people who make quality patient care possible."
Reid Helgemo IT Project Manager

We need a community. We create our own community and develop those trust relationships. So, for me, that's the biggest part of the community, the network, just helping practices know that they're not alone and that they have a large support system behind them."
Beth Gann Senior Regional Director of Operations

We recognize that the heart of AON’s success is the unwavering dedication, passion, and sacrifice of our team members nationwide. Your relentless commitment ensures patients receive exceptional care close to home.
We understand that this journey is demanding. At times, it may feel like your efforts go unnoticed. However, please know that your hard work is seen and deeply appreciated. At AON, our strength comes from our people. Whether you’re providing exceptional patient care, supporting your colleagues, or helping us grow and innovate, your contributions are valued and appreciated.
Together, we have achieved remarkable milestones—expanding our reach to 20 states, enrolling over 445 patients in clinical trials, and processing millions of lab tests. These accomplishments are a testament to your collective efforts and unwavering commitment to excellence.
As we continue our mission to close the cancer care gap, let us remember that your resilience and compassion fuel our shared journey.
Together, we stand united in the fight against cancer.





From national conferences to community-based programs, American Oncology Network (AON) leaders are shaping the future of oncology care. AON is embedded in the broader oncology community, helping to lead the evolution of cancer care on a national scale. Through active roles in major organizations and participation in conferences such as the Community Oncology Alliance (COA), AON ensures that independent practices stay connected to innovation, policy development and research that directly benefit local patients.
This spirit of collaboration drives AON’s engagement with national organizations that influence oncology care models, set industry standards and advocate for sustainability. Whether through payer strategy or valuebased care initiatives, AON leaders serve on influential boards and committees, giving community oncology a seat at the table in important national conversations.
"Oncology is evolving rapidly, and it is imperative that community oncology remains at the forefront of these
changes. By engaging with national organizations, AON leaders are helping to drive discussions on payer strategy, value-based care, and the social determinants of health that impact patient outcomes," said Alti Rahman, chief strategy and innovation officer at AON. "Our commitment to thought leadership is evident in the number of AON experts serving in key positions, ensuring that we continue to push forward patientcentered, data-driven solutions."
At the American Society of Clinical Oncology (ASCO) 2024 Annual Meeting, the world’s premier oncology meeting, AON physicians presented groundbreaking research—from Dr. Ruemu Birhiray of Hematology Oncology of Indiana's work on follicular lymphoma to Dr. Ralph Boccia of The Center for Cancer and Blood Disorders' contributions in immunotherapy. Pharmacy Director Tamara Weinberg also spotlighted the growing role of medically integrated oncology pharmacies in modern care.

Meanwhile, at the Association of Cancer Care Centers (ACCC), AON’s Anne Marie Rainey, director of value-based care, has joined the board of trustees, driving nationwide initiatives to elevate care delivery and education.
In the world of value-based cancer care, AON took the spotlight at the Association for Value-Based Cancer Care (AVBCC) Summit. Key leaders like AON’s Chief Medical Officer, Dr. Stephen "Fred" Divers, Chief Pharmacy and Clinical Services Officer James Gilmore and Alti Rahman led discussions on AI, payer strategies, equity and the future of oncology pharmacy. Their insights reflect AON’s deep investment in transforming cancer care beyond the clinic.
On the business side, CEO Todd Schonherz and Alti Rahman are actively engaged in reshaping oncology strategy through platforms like the Cancer Business Forum, while Schonherz’s work with CanCare shows AON’s commitment to supporting the whole patient— mind and body.

AON also plays a strong leadership role at the Community Oncology Alliance (COA), advocating for independent oncology. Leaders like Dr. Divers and Alti Rahman serve on COA’s board, with Vice President of Clinical Innovation Susan Sabo-Wagner and Anne Marie Rainey co-chairing the Community Oncology Administrators’ Network (CAN).
Finally, at the National Community Oncology Dispensing Association (NCODA), James Gilmore’s executive council role further supports AON’s push for better-integrated pharmacy services in oncology care.
From research to policy, AON continues to lead with purpose—putting patients first, pushing boundaries and building what’s next in cancer care. Through its work with national organizations, AON is shaping the future of payer contracting, value-based care and initiatives addressing social determinants of health. By leveraging AI and strategic growth, AON keeps community-based practices at the forefront of innovation.

As we navigate the shift towards value-based care, it’s critical that we advocate for smarter reimbursement models, integrate data-driven payer strategies, and address health disparities. AON’s leadership in these national organizations allows us to have a seat at the table where we help chart the course for the future of community-based oncology.”
Alti Rahman, MHA, MBA, CSSBB Chief Strategy and Innovation Officer

STRATEGIC PARTNERSHIPS
In October 2024, AON partnered with Vantage Health Technologies, a division of the global healthcare social enterprise BroadReach Group, to implement its AI-enabled platform, SocialHealth360. This collaboration is one of many that expand AON’s professional community, integrating diverse expertise and global perspectives to enhance patient care.
The SocialHealth360 platform supports AON’s efforts to promote health equity across its network. Through this technology, patients are screened for social needs and connected to local community resources for additional support. The platform also enables AON practices to document time spent on these services, supporting implementation of the Centers for Medicare & Medicaid Services Principal Illness Navigation (PIN) program and ensuring practices can bill appropriately while providing comprehensive, patient-centered care.
The initial implementation phase has focused on improving patient navigation and care coordination, particularly for vulnerable populations.
Enhance patient experiences/outcomes
Reduce provider burnout
Lower overall cost of care
"Collaborating with forward-thinking firms like Vantage Health allows us to tap into a broader spectrum of expertise and innovation," said Alti Rahman, chief strategy and innovation officer at AON. "These partnerships amplify our impact in community-based oncology, enabling us to deliver more personalized and effective care."
Dr. John Sargent, co-founder of BroadReach Group, emphasized the mutual benefits of the partnership: "We bring best practices and advanced technology to AON, but this collaboration is a two-way street—we learn from AON as well. Together, we’re building solutions that expand access to resources and improve patient outcomes. Our collective efforts are driving sustainable, high-quality cancer care forward."
AON’s alliance with Vantage Health exemplifies its strategic approach to partnerships—engaging with world-class organizations that provide cutting-edge solutions and share a commitment to patientcentered care. Through these collaborations, AON continues to access the best and brightest innovations, ensuring patients receive the most timely and effective care available.

From Your Community to Ours Pioneering Progress, continued
AON had a resoundingly strong presence at the Community Oncology Alliance’s (COA) 2025 Community Oncology Conference, held April 28–29 in Orlando, Florida. The event, a premier gathering for community oncology professionals, brought together experts from across the country to discuss pressing industry challenges, share insights and collaborate on solutions that enhance patient care.
Dr. Stephen "Fred" Divers, chief medical officer, and Alti Rahman, chief strategy and innovation officer, played key roles as chairs of the six-member event committee, helping to shape the conference’s agenda. They, along with the full committee, delivered opening remarks on both mornings and provided closing observations at the end of the event.
The first day featured a robust lineup of AON professionals sharing their expertise across multiple sessions. Dr. Divers participated in the panel discussion “Evolving Successful Hospital & Independent Community Practice Partnerships,” offering insights into fostering collaborative relationships between hospitals and independent oncology practices.
Dr. Sunil Babu, with Fort Wayne Medical Oncology & Hematology, and Katie Goodman, vice president of clinical research, spoke on “Growing Clinical Trial Infrastructure & Access in Community Oncology,” emphasizing the importance of expanding clinical trials at the community level.
Melissa Shaw, director of clinical projects at Central Georgia Cancer Care, was a panelist for “The Value of Patient Advisory Boards,” discussing the role of patient feedback in shaping oncology practices (see page 10 for more info).
Cassandra Perkey, AON regional clinical pharmacist, shared her expertise in “Streamlining Pharmacist-Led Hyperglycemia Management in HR+ Breast Cancer: Overcoming PI3K/AKT Inhibitor Challenges,” addressing strategies for effective medication management.
Anne Marie Rainey, director of value-based care, presented “Building Effective Patient Navigation Programs,” focusing on how practices can better support patients through structured navigation services.
Guy Messer, vice president radiation & radiology services, contributed to the session
“Radiopharmaceutical Therapies: Business Mechanics & Operational Review,” exploring the operational aspects of advanced cancer treatments.
Dr. Ruemu Birhiray, with Hematology Oncology of Indiana, led the discussion “Is Mastocytosis Underdiagnosed?” examining gaps in diagnosing this rare condition.
Melody Chang, vice president of pharmacy operations, joined the panel for “Aiming for Accuracy in Non-Small Cell Lung Cancer Treatment: Precision Strategies for Oncology Pharmacists,” discussing advancements in precision medicine.
Alti Rahman spoke on “The Business Plan for Payer Contracting,” outlining strategies for negotiating effective payer agreements.
Lisa Poiry of Fort Wayne Medical Oncology & Hematology co-presented with COA’s director of state regulation and policy on “State & Local Advocacy: Reaching Your Local Elected Officials,” highlighting the importance of engaging policymakers.
Susan Sabo-Wagner, vice president of clinical innovation, participated in the panel “Practices Using Data to Engage Payers,” discussing how oncology practices can leverage data to improve payer relations.
The second day continued AON’s strong presence with discussions on key issues affecting community oncology. Dr. Brian Mulherin, with Hematology Oncology of Indiana, spoke on “How to Operationalize a Mental Health Program in Your Practice,” focusing on integrating mental health services into oncology care.
Katie Alexander, nurse practitioner and Central Region APP coordinator at Zangmeister Cancer Center, joined the panel “Leadership, Team Building & Culture in Community Oncology,” sharing strategies for fostering strong teams in oncology settings.







































Trial Library and American Oncology Network Partner to Expand Patient Access to Cancer Clinical Trials
Trial Library is a leader in AI-enabled clinical trial matching and patient navigation with a strong reputation in oncology.
Learn more
Woodlands Cancer Institute Relocates Its Medical Oncology Clinic in the Woodlands, Texas
Local oncology practice moves to a new location to continue providing enhanced cancer care to The Woodlands, Texas community.
Learn more
Florida Oncology and Hematology and American Oncology Network Open Second Naples Location and Welcome Dr. Deborah Glick
Board-certified hematologist Deborah Glick, MD, joins the physician team.
Learn more
American Oncology Network Launches CloudBased Laboratory Information System to Streamline Pathology Reporting for Oncologists
SigmaCore’s LabVizor streamlines pathology reports, enhancing efficiency for AON’s pathology and oncology labs.
Learn more
Florida Oncology and Hematology and American Oncology Network Welcome Dr. Michele Ramirez
Board-certified medical oncologist and hematologist Michele Ramirez, MD, joins the physician team.
Learn more
MidAmerica Cancer Care Joins American Oncology Network
MACC provides community-based oncology services to patients in the Kansas City metropolitan area and western Missouri.
Learn more
Florida Oncology and Hematology Relocates Fort Myers Clinic
Local oncology practice moves to a new state-of-the-art location to continue providing enhanced cancer care to the Fort Myers community.
Learn more
American Oncology Network Appoints Terri Casey as Chief Human Resources Officer
Charlie has built an impressive legal career, and his healthcare expertise makes him a perfect fit for this essential role.
Learn more
American Oncology Network Appoints Charlie Goddard as General Counsel
Charlie has built an impressive legal career, and his healthcare expertise makes him a perfect fit for this essential role.
Learn more
Fort Wayne Medical Oncology and Hematology Joins American Oncology Network
FWMOH operates across northeastern Indiana and is staffed by 16 Board-certified medical oncologists and two Board-certified gynecologic oncologists.
Learn more
Hematology Oncology of Indiana Physician Research Presented at 66th ASH Annual Meeting
The ASH Annual Meeting is recognized as a premier event for hematology research, with more than 5,000 scientific abstracts submitted each year.
Learn more
American Oncology Network’s Specialty Pharmacy Achieves ACHC Reaccreditation
ACHC accreditation reflects an organization’s dedication to meeting standards that facilitate a higher level of performance and patient care.
Learn more
Ohio State to Partner with Zangmeister Cancer Center to Expand Access to Cancer Care in Central Ohio
Alignment will speed up, expand access to communitybased oncology care.
Learn more
Zangmeister Cancer Center and American Oncology Network Welcome Dr. Katherine Exten
Board-certified medical oncologist Katherine Exten, MD, joins the physician team.
Learn more
Triple Crown Urology Opens New Hot Springs Village Clinic Location
Local urologic practice opens new location to provide excellent urologic care to the Hot Springs Village community.
Learn more
Genesis Cancer and Blood Institute Relocates Hot Springs Village Clinic to Larger Location
Local oncology practice moves to a new location to continue providing enhanced cancer care to the Hot Springs Village community.
Learn more
AON and Vantage Health Partner to Enhance Cancer Care with AI
American Oncology Network and Vantage Health Technologies partner to improve cancer patient outcomes with AI-enabled value-based care platform.
Learn more
Katherine Exten, MD Zangmeister Cancer Center
American Oncology Network Expands to Cape Coral Florida
Magali Van den Bergh, MD, Venkata Parsa, MD, and Shivtaj Mann, DO join the Cape Coral physician team as part of American Oncology Network.
Learn more
New Clinic Suite, Same Personalized Care: Woodlands Cancer Institute Expands Its Conroe Location
Local oncology practice expands its clinic moving to a larger suite in the same building to continue providing enhanced cancer care to the Conroe community.
Learn more
American Oncology Network Appoints Terri Casey as Chief Human Resources Officer
Terri’s impressive background in human resources, employment law, and healthcare allows her to bring a strategic and multidisciplinary perspective to leadership and talent development that makes her a perfect fit for this essential role.
Learn more
American Oncology Network Appoints Joe Verschleiser as Chief Growth and Performance Officer

Joe's deep experience in driving growth, executing strategic initiatives and leading operational improvements within healthcare organizations will be invaluable as we continue to strengthen our national presence and support the long-term success of our

At the end of 2022, Linda was willing to try anything. She trusted her doctors. They had caught it early. And despite her ongoing exhaustion, she had made it to every single appointment since her diagnosis nearly two years prior. But her now stage 3 breast cancer wasn’t responding to the usual treatments.
When her physicians at the American Oncology Network (AON) community oncology practice told her about a clinical trial she qualified for, she didn’t hesitate. It was the opportunity she had been waiting for—a chance to reclaim her life and her focus on the three young children who needed her. Now, in addition to the standard treatment options, Linda is utilizing investigational treatments that may improve her chances for a successful outcome.
For AON, clinical research is more than an opportunity—it’s a commitment to bringing cuttingedge, investigational treatments to patients like Linda in community oncology settings. The AON Research team works diligently to support providers, enhance patient care, and ensure that innovative therapies are accessible to those who need them most.
AON Research provides the expertise and resources to help oncology practices launch or expand clinical trials. By integrating research into community-based settings, AON ensures that patients can access investigational therapies close to home while providers gain valuable opportunities to participate in leading-edge studies.
AON offers a range of tailored solutions to help practices navigate the complexities of clinical trials:
Centralized management of regulatory submissions and documentation, including an integrated electronic Investigator Site File (eISF) for seamless tracking.
Utilizing trial-matching technology and feasibility assessments to streamline patient enrollment.
Promoting research opportunities within the medical and scientific communities.
Managing contracts, compliance, and optimizing revenue cycles through the Clinical Trial Management System (CTMS).
Standardizing standard operating procedures (SOPs), providing audit support, and ensuring regulatory compliance across research sites.
By expanding clinical trial access in local oncology practices, AON Research is improving patient outcomes, advancing oncology care, and positioning communitybased providers at the forefront of medical innovation. Through these efforts, AON is not only strengthening research capabilities but also shaping the future of cancer treatment—one trial at a time.
“We began offering Genesis Cancer and Blood Institute patients access to clinical trials through AON’s clinical research program three years ago,” said Genesis Cancer and Blood Institute Research Manager Laura Sellers. “AON’s regulatory and compliance expertise helped us launch the program, and the ongoing support we’ve received has allowed us to continue expanding while ensuring our providers remain focused on patient care rather than paperwork. Currently, we have 11 patients enrolled in trials, and we’re able to continually increase that number based on patient need—without expertise or resource constraints—because AON handles the regulatory submissions and documentation on our behalf.”
At the end of 2023, AON began investing in centralized clinical research infrastructure to support network practices. The expansion of central research services strengthens clinical trial operations by centralizing regulatory processes, data submissions, contract negotiations, and budget management. Streamlining these critical functions improves efficiency, reduces administrative burdens on individual sites, and accelerates study start-up timelines.
In addition to administrative efficiencies, the expansion incorporates enhanced patient screening through trial-matching software, improving recruitment and enrollment rates. Leveraging AI-driven tools and electronic health record (EHR) integrations allows research teams to identify eligible participants more effectively, reducing recruitment timelines and increasing trial diversity. Standardized SOPs further support
operational consistency across trials, ensuring adherence to best practices and regulatory requirements. These enhancements collectively position research institutions for greater scalability, improved sponsor collaboration, and the ability to conduct complex, multi-site studies with greater precision and reliability.

Clinical trials are essential to advancing cancer treatment, yet many patients face barriers to participation. Expanding support services such as regulatory oversight, data management, and financial administration reduces the burden on providers and ensures practices can offer more trials, giving additional patients access to innovative therapies that could change lives.”
Katie Goodman, RN Vice President, AON Clinical Research
447
148
111
New patients participated in clinical trials at AON practices in 2024
Studies are currently open for enrollment through AON practices
Active studies are currently open with different study sponsors
123 AON patients are currently participating in clinical trials
Review AON clinical trial offerings here.
For more information about AON Research and how your practice can participate, contact Katie Goodman, vice president of clinical research, at Katie.Goodman@AONcology.com
Across AON’s national network, Advanced Practice Providers (APPs) are not only addressing critical gaps in oncology care but also cultivating a stronger, more interconnected professional community. AON is empowering APPs by providing specialized education, fostering peer connections, and amplifying their voices, ensuring they have the support necessary to thrive and continue delivering top-quality care to patients.
As cancer incidence rises in the U.S.—driven by increasing cases among young adults and the higher cancer risk associated with an aging population—the field of oncology faces a worsening shortage of physicians. In 2024, cancer cases surpassed 2 million for the first time in history, with numbers expected to keep growing. Compounding this crisis, 53% of oncologists report experiencing burnout, with 41% considering leaving medicine due to its severity, creating an unprecedented challenge in cancer care.
Amid these dire statistics, Advanced Practice Providers (APPs)—including Nurse Practitioners (NPs) and Physician Assistants (PAs)—are bridging the gap, delivering high-quality care while easing the burden on overextended oncologists and healthcare systems.
Well-trained to manage a wide range of responsibilities, APPs ensure that patients receive essential care. Their ability to work independently and collaborate with physicians allows for seamless continuation of care.
"APPs are stepping up in a major way," says Susan Sabo-Wagner, vice president of clinical innovation and leader of care coordination at AON. “They’re incredibly adaptable, capable of taking on a wide range of roles. Whether it’s seeing patients in tandem with physicians or managing urgent care cases, APPs help ease the burden on oncology teams. And in our valuebased care model, keeping patients out of the hospital is a key priority. APPs are critical in achieving that.”
Patients often don’t realize that APPs are highly educated professionals with advanced degrees and extensive clinical experience. Through rigorous
training, they gain the skills needed to assess, diagnose, treat, and manage a wide range of conditions, including cancer. Nurse practitioners typically hold a Master’s degree or higher and are board-certified in their specialties, while physician assistants complete advanced degree programs and pass national certification exams.
One oncologist who has seen their impact firsthand is Dr. Jeanna Knoble, a leader at Zangmeister Cancer Center in Columbus, Ohio. "We have grown our APP program significantly in the last few years. There have been challenges in adaptation, both with patients hesitant to embrace the change and physicians learning how to best utilize our APP providers in daily practice," Dr. Knoble admits. “But over time, our APPs have become one of our most valued resources, improving continuity and accessibility of patient care. Through working together and communicating closely, our APPs allow us to provide high quality care more efficiently and comprehensively. At the same time, this model helps us avoid work commitment overload, and physician burnout.
Despite the high level of training and expertise APPs bring to patient care, some patients remain hesitant to see them, expecting to interact exclusively with a physician. Educating patients on the value of APPs is an ongoing effort within AON, and perceptions are shifting. As more patients experience firsthand the care, compassion, and expertise APPs provide, they increasingly recognize them as essential partners in their cancer journey.
“APPs provide continuity, reassurance, and advocacy for our patients,” says Katie Alexander, an APRN at Zangmeister Cancer Center and AON’s regional advanced practitioner coordinator. “We make sure patients feel heard, cared for, and confident that they are receiving the best possible care—even when their oncologist is being pulled in multiple directions.”
For cancer patients, navigating their diagnosis and treatment can be overwhelming, and access to care
providers is essential. However, in a fast-paced oncology practice, physicians are often stretched thin, leaving patients with lingering questions or concerns. APPs play a crucial role in ensuring no patient feels left behind. They provide highly specialized care and offer an empathetic, personal touch that can make all the difference in a cancer patient’s experience.
Fostering Community and Elevating the Voice of APPs
“APPs are often the bridge between patients and comprehensive cancer care. Their role is expanding as they provide more direct care and manage long-term survivorship, significantly improving patient outcomes."

Katie Alexander, MS, APRN-CNP, OCN, BBA Nurse Practitioner; Central Region APP Coordinator
Alexander has been leading AON’s initiative to create a national community of APPs, connecting providers across practices, no matter their location, with the goal of having a leader to unify APPs in each AON region. Many APPs were working without a connection to the broader AON community before she took on the task of uniting them.
“We recognized that APPs needed visibility, representation, and leadership opportunities,” Alexander explains. “By giving them a voice and bringing them together through committees, we’re empowering them in new ways.”
Alexander’s approach to community-building has been multifaceted. She is establishing committees within the APP network where providers can collaborate on best practices, develop new initiatives, and share experiences. These committees also address specific challenges, such as varying state practice laws
and navigating different oncology specialties like survivorship care.
“There was a clear gap in communication,” says Sabo-Wagner. “APPs didn’t have a strong voice within the organization, and that needed to change. Katie’s work connecting APPs across the network has been transformative. Now they have a place for support and guidance.”
Sabo-Wagner is optimistic about the committees’ potential to strengthen the community. "The committees will be integral not just in supporting APPs, but in allowing them to shape their role in cancer care," she says. “For instance, one committee will focus on survivorship clinics. APPs are uniquely qualified to lead these, and we want them to develop processes and procedures for others to follow.”
Alexander launched the APPs initiative by setting up a dedicated portal on AON’s SharePoint intranet, which has become an essential resource for educational materials, tools, and oncology-specific information. The committees and the portal are connecting APPs who may never have met otherwise and are providing opportunities for them to learn from each other.

"The SharePoint page has been a game changer," Alexander notes. "It’s become a central hub where APPs can access the knowledge they need to succeed in oncology, and more importantly, it’s a place where they can connect with their peers and build relationships that ensure they’re well-supported."

AON’s focus on providing education and support ensures APPs are well-equipped to face challenges. "We want APPs to be at the top of their game," Alexander adds. "That’s why offering specialized oncology training is so crucial."
Although APPs have long been a critical part of the healthcare workforce, their role is often undervalued, especially in oncology. AON is changing that by providing APPs with the education and support they need to excel in their clinical roles and gain recognition within the organization.
This elevation of the APP role within AON is vital not only for the APPs themselves but also for the broader healthcare system. As more physicians and healthcare leaders recognize the value of APPs, AON is leading the way in promoting their essential contributions to cancer care.
Dr. Knoble credits Alexander’s leadership and AON’s support for helping successfully integrate APPs into the cancer care model. "Katie and her team have created a program that benefits everyone. Physicians see how APPs are enhancing patient care, and the APPs themselves feel empowered and supported," she says.
This partnership between physicians and APPs is essential to the ongoing success of AON’s cancer care delivery model. As Dr. Knoble explains, “The collaboration between physicians and APPs is crucial. We need to work as a team to provide the best care possible to our patients.”
This rapidly growing profession is poised to make an even greater impact in healthcare. APPs are among the fastestgrowing professions in the United States. According to the U.S. Bureau of Labor Statistics, demand for nurse practitioners and physician assistants is expected to grow significantly, much faster than the average for all occupations. Similarly, U.S. News & World Report’s Best STEM Jobs ranking placed nurse practitioners and physician assistants in the top ten, reflecting the increasing demand for these professionals.
With Alexander leading the charge, AON’s APPs are not just responding to today’s challenges but are shaping the future of cancer care. By creating a supportive community, offering continued education, and empowering these providers with a voice, AON is building bridges between healthcare teams and strengthening cancer care at every level.

“We're at a pivotal moment in healthcare, and APPs are more important than ever. By uniting them through education and collaboration, we're not just filling gaps—we're creating a stronger, more cohesive national community that benefits patients, providers, and the entire organization."
Susan Sabo-Wagner, MSN, RN, OCN, NEA-BC
Vice President, Clinical Innovation
For patients and even some healthcare professionals, the many acronyms representing the titles and credentials of Advanced Practice Providers (APPs) can be confusing. However, understanding these distinctions is key to appreciating the depth of training, expertise, and specialized care APPs bring to communitybased oncology. Here’s a breakdown of common acronyms and their corresponding credentials:
APRN: Advanced Practice Registered Nurse
Credentials:
• CNP: Certified Nurse Practitioner
• CNS: Clinical Nurse Specialist
• CRNA: Certified Registered Nurse Anesthetist
NP: Nurse Practitioner
Credentials:
• FNP: Family Nurse Practitioner
• AGNP: Adult-Gerontology Nurse Practitioner
• WHNP: Women's Health Nurse Practitioner
PA: Physician Assistant
Credential:
• PA-C: Physician Assistant-Certified
CNS: Clinical Nurse Specialist
Credentials:
• ACNS-BC: Adult Clinical Nurse Specialist-Board Certified
• PCCN: Progressive Care Certified Nurse
CRNA: Certified Registered Nurse Anesthetist
Credential:
• DNAP: Doctor of Nurse Anesthesia Practice

Strong social connections have the power to enhance resilience, extend longevity, and improve overall well-being.
If you want to go fast, go alone. If you want to go far, go together.” ~African Proverb
The idea of the stoic, solitary hero is a familiar one in popular culture. Action films like John Wick or Die Hard often depict lone renegades who overcome impossible odds through sheer intellect and brute force. Unfortunately, these types of films perpetuate what we now know to be a false narrative because strength isn’t found in isolation. The truth is, loners are not the strongest, nor do they go the farthest or survive the longest.
Human beings are wired for connection, and science confirms that our social ties play a crucial role in both physical and mental health. Stanford University researcher Emma Seppälä, Ph.D., who gave a popular TEDx Talk, The Power & Science of Social Connection, defines social connection as "the subjective experience of feeling close to and a sense of belongingness with others." She has observed that modern society is experiencing a growing crisis of loneliness, with detrimental implications for well-being.
In 2023, U.S. Surgeon General Dr. Vivek Murthy declared loneliness a public health epidemic, stating, " Loneliness is more than just a bad feeling— it harms both individual and societal health. It is associated with a greater risk of cardiovascular disease, dementia, stroke, depression, anxiety, and premature death."
A 2022 study from the American Medical Association (AMA) found that loneliness increases the risk of premature death by 26%.
The reasons for this growing crisis are complex. Many people today experience greater mobility, moving away from family and lifelong friends for work or other opportunities. Remote work, while offering flexibility, can also contribute to isolation. Social media, paradoxically, can create a false sense of connection while deepening feelings of loneliness. Without meaningful, in-person interactions, people may feel adrift and unsupported.
Recognizing the serious health risks of loneliness, healthcare providers are turning to social prescribing, a practice that integrates social support into medical care. Social prescribing involves connecting patients with community resources—such as volunteer groups, fitness programs, or social clubs—to improve wellbeing and reduce isolation.
AMA Journal of Ethics notes that social prescriptions are particularly valuable for older adults and those with chronic conditions, as they address not only medical needs but also the social determinants of health. Needing others isn’t a weakness—it’s a fundamental part of being human. Police officers are trained to “call for backup” for a reason. People who live long, healthy, and happy lives don’t go it alone—they build strong, varied social networks and lean on relationships for emotional and practical support.
The Link Between Social Connection, Health and Longevity
One study published by the National Institutes of Health (NIH) found that individuals with strong social networks experience lower levels of chronic stress, which is a key contributor to many health problems, including hypertension and weakened immune. These findings underscore that health isn’t just about diet or exercise—
it’s also about the strength of personal relationships.
According to the Centers for Disease Control and Prevention (CDC), strong social connections can lead to a 50% increased chance of longevity, lower rates of anxiety and depression, and improved immune function. In contrast, social isolation has been linked to an increased risk of heart disease, stroke, and dementia. Harvard T.H. Chan School of Public Health has also asserted that strong social connections can increase lifespan by as much as 50% and significantly enhance overall health.
People often prioritize eating well and staying active when thinking about health, but one critical factor is frequently overlooked: spending time with people they care about. Just as regular exercise strengthens the body, meaningful social interactions strengthen mental and emotional resilience. Making time for friends, family, and community isn’t just a leisure activity—it’s a vital part of maintaining overall well-being. Prioritizing social connections should be seen as an essential component of a healthy lifestyle, just like a balanced diet and regular movement.
So how can people make social connection as much of a priority as exercise and nutrition? Research suggests that fostering relationships requires intentional effort. The University at Buffalo School of Social Work recommends building a diverse support system that includes close family, friends, colleagues, and community members.
Schedule regular meetups with friends or family.
Join community groups, clubs, or volunteer organizations.
Prioritize face-to-face interactions over digital communication.
Reach out to those who may be struggling with loneliness.
Invest time in professional networks that provide mentorship and support.

Staying connected can be tough for remote workers or those far from loved ones, but technology also helps bridge the gap, supporting relationships and a sense of community.
Schedule virtual gatherings using apps like Zoom or FaceTime to stay connected with loved ones.
Join online communities—such as Facebook groups and Reddit forums—to engage with people who share similar interests.
Network virtually through platforms like Eventbrite and LinkedIn that frequently host online professional meetups, webinars, and industry-specific discussions.
Playing multiplayer games, joining trivia nights, or participating in book clubs are fun, interactive ways to bond with others.
Make new friends on sites like Meetup, Bumble BFF, and Discord that facilitate new connections and ways to grow your social circle from a distance.
Staying socially engaged—whether in person or online—is a key part of maintaining mental and emotional well-being. Making the effort to nurture relationships in both physical and virtual spaces can help reduce feelings of loneliness.
In the rush of daily responsibilities, relationships often take a back seat. People assume their relationships with family, friends and colleagues will always be there, but without effort, connections can fade. Even a simple text message to check in can significantly strengthen relationships and improve both parties' sense of connectedness. Taking responsibility for maintaining social ties—through small but meaningful gestures— can make all the difference.
Strong social networks aren’t just a luxury—they’re a necessity for a long, healthy life. Whether in personal relationships or professional environments, prioritizing community and collaboration can lead to greater well-being, resilience, and longevity.
CASE STUDY

Hope Cancer Care of Nevada was established in 2009 by Raja S. Mehdi, MD, a Board-certified medical oncologist, to provide state-of-the-art cancer treatment and personally tailored programs designed to put the body, mind and spirit at ease as it heals. Since then, the center has expanded to three locations where Dr. Mehdi, four advanced practitioners and 34 support staff provide comprehensive and personalized care to every patient.
Hope Cancer Care’s mission of treating the whole patient is complemented by its philosophy combining leading medical treatments with the ability to focus solely on patients’ recovery –an approach that allows Hope Cancer Care’s highly trained staff to craft individualized treatment programs for each patient.
One physician
Four advanced practitioners
Three locations
As business and care models evolved over the years, oncology practices like Hope Cancer Care of Nevada faced a growing number of increasingly complex obstacles that threatened their ability to remain independent. Among the most challenging were the cost of oncology drugs—biologics in particular—and managing relationships with insurance companies.
“Procurement of drugs was becoming almost prohibitive for smaller practices. And then, even if you managed to acquire the drugs for your patients, you had the complexities and headaches of dealing with insurance companies,” said Dr. Mehdi. “So those two main issues led us to look for a practice management partner.”
The decision to seek out a network partner presented another challenge—finding the right philosophical fit. Dr. Mehdi noted that many networks had immediate disqualifiers, including being backed or owned by pharmaceutical or insurance companies.
“In my mind, those types of networks were not truly patient-centered,” he said. “They probably provide good care, but philosophically, it was not a good match for us.”
Dr. Mehdi quickly determined the American Oncology Network (AON) checked all of Hope Cancer Care of Nevada’s partnership boxes and joined the network in 2019. His decision was validated from the start, when his team flew to Florida to meet with AON’s leadership.
One of the primary attractions of AON was its promise to let Hope Cancer Care’s providers continue to practice oncology in the manner they feel is best for their patients—a promise that Dr. Mehdi says he sees no signs of being broken in the long-term.
It was very attractive to me that the person at the helm is a physician who is still seeing patients and is still heavily engaged in patient care. They are obviously patient-centered.”
Raja S. Mehdi, MD Hope Cancer Care of Nevada

Equally important, AON fulfilled another key requirement for Hope Cancer Care in that the benefits also extended to the non-clinical side of the house. Streamlined processes have helped ease administrative burdens, allowing the practice to keep pace with the rapidly evolving healthcare landscape.
“The way that AON helped the practice navigate the changes made joining the network almost seamless,” said Andrew Fisher, senior regional director of operations. “And now, there is less on their plates, which allows them to focus on other priorities. With the oncology and drug landscape constantly changing, the practice feels such relief having AON resources behind them, to take on the majority of that for them and guide the practice.”
Dr. Mehdi says he also benefits from the business resources AON brings to the table. His attention is no longer divided between patient care and human resources, procurement and other activities that fall outside the clinical scope.
“It’s like I just became a real doctor all over again. I can stay completely focused on the patient because half my mind is no longer occupied with
administrative issues,” he said. “We are able to function more efficiently as individuals and be even more patient-centered than before. With AON, we may not do everything the same as before, but at the end of the day, the compass is pointing toward the patient.”
Fisher adds that, since the merger with AON, the staff has the time, tools and other resources to really put the patient first. “They’ve had nothing but positive reviews from patients who came with them through the merger. All the way around, the best part is how patient-centered it is and how it has enabled them to do that wholeheartedly—not just with the best of intentions.”
AON has opened numerous doors for Hope Cancer Care of Nevada with opportunities to provide expanded services that align well with its mission of patient-centric, whole-person care. One of those is AON’s full-service centralized specialty pharmacy. Hope Cancer Care patients benefit not only from rapid access to cutting-edge medications but also from in-home delivery of their prescriptions in just days.
Patients frequently provide positive feedback, often focused on the outreach undertaken by the AON pharmacy team even when that communication is to share that they are unable to fill a particular prescription.

“They’re always communicating with the patient, letting them know why and where they must transfer the prescription, giving the patient all the information needed to connect with that new pharmacy,” said Fisher. “Their dedicated AON representative is always in contact with them and looking at their numbers to make sure they’re not having any problems with any part of the pharmacy service, which is just great.”
The ability to enhance lab services was another benefit for Hope Cancer Care. Though their license exempts them from having full laboratory capabilities, the ability to offer patients on-site draws rather than sending them to a laboratory service provider is a significant convenience.
Another value-add program is AON’s Referral Base Management Program, which provides the structure and support needed for an effective physician liaison.
Despite their best efforts and intentions, previous attempts to implement a referral base management program had fallen short. AON’s template has made all the difference.
Hope Cancer Care has launched several new patient advocacy initiatives with AON’s support. The AON Cares Foundation and the establishment of a local CPAN Chapter in 2023—the first on the west coast—demonstrate the practice’s commitment to supporting patients and their families. The participation in the Nevada Oncology Society, a division of ACCC, and hosting an Annual Survivorship Event attended by over 250 patients and their family members further illustrate their dedication. Hope Cancer Care also organizes quarterly health fairs and vendor fairs and partners with organizations like Fighting Pretty, Breast Cancer Warriors of Las Vegas, and La Roche-Posay to offer robust support to patients, including patient support kits.
“We were able to tap into AON’s experience, knowledge and expertise, which was significant. We’ve seen great results from the program,” said Dr. Mehdi.
One of the most immediate benefits Hope Cancer Care realized from its partnership with AON came at the outset of the COVID-19 pandemic. While many healthcare organizations were scrambling for supplies and figuring out how to continue providing patient care safely, AON was disseminating protocols, cleaning and disinfecting supplies and personal protective equipment (PPE) to all its practices.
“AON was two steps ahead at all points during the pandemic,” said Fisher. “The information that they provided was extremely valuable and allowed the practice to notify their patients whenever a change occurred. AON made sure they always had enough PPE, even though their practice required new masks for every encounter. The level of support was absolutely astronomical.”
As Hope Cancer Care of Nevada settles into another year as an AON practice, they are looking ahead at ways to optimize the relationship. The practice offers patients access to the American Oncology Cares Foundation (AON Cares), a nonprofit organization that provides financial support for essential living expenses such as rent or mortgage, utilities, transportation, and food, allowing them to focus on what matters most: their health and well-being.
They are also adopting AON’s care coordination services and have added a clinical research division with a dedicated coordinator. Doing so, says Fisher, will provide additional support for patients without taking staff away from other core responsibilities.
Ultimately, Hope Cancer Care sees its relationship with AON as both enduring and mutually beneficial. One that gives them “a real shot at maintaining our independence and proving that community-based oncologists are still viable,” said Dr. Mehdi.

The way that AON helped the practice navigate the changes made joining the network almost seamless, and now, there is less on their plates, which allows them to focus on other priorities. With the oncology and drug landscape constantly changing, the practice feels such relief having AON resources behind them, to take on the majority of that for them and guide the practice."
Andrew Fisher Senior Regional Director of Operations American Oncology Network


VICE PRESIDENT, HUMAN RESOURCES
At AON, Human Resources plays a vital role in transforming a network of independent oncology practices into one cohesive, supportive community. Karen Quick, vice president of human resources, sees this integration as more than just onboarding—it’s about partnership.
1. How long have you been with AON?
I've been supporting AON since its inception in 2018 when we onboarded our first practice.
2. How does Human Resources help transform AON's national network of practices into a cohesive and supportive community?
HR is at the heart of making sure practices feel supported as they transition into AON. When a practice joins, the decision has been made at the leadership level by physicians and administrators, but the staff—nurses, office managers, front desk teams—weren’t necessarily part of that decision. For them, this kind of change can feel unsettling. Our role is to ease that uncertainty and make sure they know we’re here to help. We want every employee to feel valued, heard, and connected to the larger AON community.
3. What do you envision to further strengthen the AON community?
One thing we’ve discussed as an HR team is the importance of continuously listening to our employees. What are our employees’ perceptions about working with AON?
Culture will be a major focus in the coming years, especially as we continue growing so quickly. Each of our practices has its own culture, and I think we have an opportunity to step back and make sure we’re fostering an inclusive culture across the entire organization. I want every employee, whether they are a nurse in Arkansas,
a phlebotomist in Maryland, a patient services specialist in Georgia, a pharmacy technician in Florida, or one of our many support services team members working from home, to feel truly connected to AON.
And when I say connection, I mean more than just logistics—I mean a shared mission, and I believe we all feel connected to AON’s mission. How could we not? We’re providing lifesaving care. That’s something I always emphasize, especially during difficult conversations—how does what we do impact our patients? How does it help our employees feel a sense of purpose within the organization? That’s a key part of culture, beyond just mission statements.
This is especially important for remote workers. When you’re not physically in a practice or an office with colleagues, it’s easy to feel disconnected. That’s why I’m excited about the different ways we can strengthen culture and connection. We have employees working in clinics, we have teams supporting them from other locations, and we have remote employees across the country. That means we need multiple approaches to making sure everyone feels part of the larger AON network.
It’s crucial to be intentional about connection. Whether through improved communication strategies, fostering engagement across different work environments, or reinforcing our shared mission, we have so many opportunities to strengthen our community. I’m excited about what’s ahead.
4. What are you most proud of when it comes to your team and department?
There are so many things I’m proud of with our team, but I’m most proud of the collaboration that exists and how our HR team works together. A day never goes by that somebody doesn't reach out to lend a virtual hand, ask if someone needs help, or see what they can take off someone else’s plate. That collaboration and openness have allowed our team to come into spring. They just bloom, right? Because in that kind of environment, everybody strives to be and do their best, and I think that’s exceptional.
5. How do you define the word success?
Success, to me, isn’t something I measure in personal achievements. Instead, I see it in the relationships I build—with my team, my colleagues, and the people who trust me enough to seek my perspective. When someone reaches out—not just for answers, but to brainstorm ideas or navigate a challenging situation—it tells me I’ve fostered an environment where open dialogue and collaboration thrive.
Creating that kind of safe space is what matters most to me. It’s never about saying, ‘This is the way it has to be.’ It’s about partnership—bouncing ideas off one another and growing together.
Beyond that, success is also about seeing the HR team invest in their own growth and development. But that’s never just about me. It’s the collective effort of our entire HR leadership team, all of us working with the same mindset and mission: to support and empower our people. I want to make sure that’s recognized—because real success is never a solo effort.
6. What’s your favorite part about working for AON? Why AON?
There are two things I love, and they’re the reason I decided to join AON. I love being able to work with new practices that join the organization. I’ve been through—and I don’t like the term—an “acquisition”, so, I experienced that roller coaster. Everything you go through, all those emotions, it’s a grieving process— recognizing and acknowledging this contributes to being successful at onboarding employees. I know it’s not a cookie-cutter approach. So, I love that I can really partner with our operational leaders and actively participate in
ensuring we take into consideration each practice’s unique approach and that we’re mindful of things that are very important to maintain.
The other reason is more personal. I lost my husband to cancer 12 years ago. Having an opportunity to personally give back because of the experiences we had allowed me to make a life-changing decision about leaving a job after 18 years to join an organization that supports oncology. Pair that personal motivation with the work we do here at AON, and that brings me joy. That’s why I’m here and why I love supporting AON.
7. What has been the most memorable moment for you while you’ve worked for AON?
There have been so many. I think every time we go live with a new practice, it’s something to celebrate. Those are always memorable moments because we’ve gone through all those steps to get to that point. The day is here. The excitement of being in the practice on go-live day, you know, it’s hectic and busy, but the energy that’s there— and just being able to be there as a resource—because emotions are very high. Not leaving that entirely to the practice leadership, who are also going through their own emotions. It goes back to those touchpoints and those opportunities to create relationships.
8. What motivates you to get up and get to work in the morning?
Knowing that what I do makes a difference, ultimately, to the patients. We ensure our employees are empowered to provide exceptional care. I love what we do. I love the team that I’m part of. I look forward to going to work. No one day is ever as expected or the same. So, it’s that variety, too. That’s true about any role within HR, but I feel like it’s amplified because of AON’s mission.
9. What is your favorite book (or books)?
I’m a big fan of James Patterson. Right now, I’m making my way through the Alex Cross novels. I enjoy stories with lots of twists and turns. In a previous life—or maybe in my next one—I think I would have loved to be a crime scene investigator. When I was deciding on a career in college, I almost chose to become a paralegal because I enjoy investigating, uncovering, and solving riddles. I think that’s a helpful mindset to have in HR, too, because a lot of what we do involves solving riddles.
10. What are some fun facts about you?
I love animals. I have two very, very spoiled dogs right now. I don’t know if people would find this a fun fact, but I’ve also discovered running later in life and just completed my first half marathon. I also love being outdoors, which is one of the reasons I love living in Florida. There are so many opportunities to explore nature. I’m 10 minutes from the beach, and the cruise port and Cape Canaveral are in my backyard. I can watch rocket launches from my front yard.
11. What piece of advice would you give your younger self?
I’d tell my younger self to be less rigid and not approach situations in black and white terms. I’d advise embracing opportunities to partner with leaders and be involved in decision-making, rather than focusing on things having to be a certain way just because that’s what the policy says. Adopt flexibility, openness, and embrace the partnerships you can build.
12. List three adjectives that describe your personality.
I don’t take myself too seriously. I think humor is extremely important. I’m passionate—not just about what I do, but about several different things. I feel like I have a passionate personality. I also consider myself open, and I hope people find me approachable because that’s important to me.

13. What is one of your favorite travel destinations, or where do you hope to travel to in your lifetime?
One of my favorite places I’ve traveled to so far is Hawaii. As part of my job, I travel to different parts of the country, and I was there for the opening of our practice. It was gorgeous. I’m not a fan of the cold, but I’d love to visit Alaska or the Canadian Rockies—someplace completely different from where I live in Florida because I find that exciting.
14. Who is your hero?
One of my heroes is Abraham Lincoln. I’m a history buff, and I love history. I feel like what he accomplished, the risks he took during such a pivotal time in our country, and his decision to stand up for what he knew was right—despite it dividing the country significantly—took a lot of courage. The other hero is my dad. He’s always been there for me and supported me. He never tried to hold me back if he was concerned about my decisions, he always supported me.
15. If you had three wishes, what would they be?
I wish we had better—and more—ways to fight cancer. I wish our doctors and providers had even stronger resources in the fight our patients are going through. We’re very fortunate to participate in research and clinical trials, but I just wish those results would come to market faster.

Easing financial burdens so patients can focus on healing.
As cancer diagnoses rise, the need for financial support grows—but available funds are limited. American Oncology Cares steps in to help, providing financial assistance to qualified adult cancer patients for essential non-medical expenses.
To date, we have raised over $215,000 and granted nearly $100,000 to patients, easing the burden of living costs such as rent, utilities, transportation, and food.
• Program launched October 2023.
• AON contracted with nonprofit America’s Charities to administer and manage American Oncology Cares.
• America’s Charities responsible for patient application review and distribution of patient grants.
• Monies raised in your state, benefit patients in your state.
• Active cancer treatment.
• Over 18 years old.
• Household income at or below 200% of the U.S. Federal Poverty Guidelines.
• Complete online application.
• Housing expenses, utility bills (gas, water and electric), and transportation and food costs associated with travel for cancer treatments.
• Qualified applicants can receive a grant of up to $1,500 and may receive assistance twice per calendar year.


Donate to benefit cancer patients To apply
Clipboard-Check Program Criteria for Your Practice/State
• Please contact Kembly.Mourelo@AONcology.com



AON RESOURCE ADMINISTRATOR, CARE COORDINATION
or Correna “Cory” Wills, oncology is deeply personal. Both of her parents battled lung cancer, forcing them to make the heartbreaking decision of choosing which one would receive treatment. Years later, her husband was also diagnosed with cancer. These experiences fueled Cory’s passion for ensuring that no patient or family has to navigate their journey alone.
As a resource administrator in AON’s care coordination department, Cory dedicates her days to connecting patients with essential resources— transportation, food, housing, and more. She meticulously researches and verifies services, and then updates the patient resources page that
is available in the patient section of all practice websites to make life easier for those fighting cancer. Her commitment stems from her personal experience and an unwavering belief that access to these resources directly impacts patient outcomes.
Cory began her medical career 20 years ago as a medical assistant before transitioning into oncology and hospice care. She’s been with AON for nearly four years and embodies AON’s values of compassion and advocacy, ensuring every patient is treated like family.
For Cory, it’s not just about care—it’s about making a difference. And she does, every single day. Thank you, Cory.

At AON, we know that social connections are essential to overall well-being, health, and longevity. Feeling connected to your colleagues can make work more enjoyable and help create a supportive, thriving workplace community.
Here's how you can stay connected:
Update your Employee Snapshot in Workday—help colleagues get to know you!
Send a note of encouragement using the AON Your WellBeing Recognation cards. A simple message can brighten someone’s day!
Visit AON's WellBeing program summary on

CLINICAL NURSE NAVIGATOR
or Jennifer Hare, nursing is more than a career—it’s a calling. With over 20 years at Genesis Cancer and Blood Institute in Hot Springs, Arkansas, she has dedicated much of her life to oncology care. Originally a clinical nurse manager, Jennifer transitioned into the role of clinical nurse navigator in 2022 to build a program designed to provide personalized support to cancer patients.
Jennifer’s role is dynamic. She meets with every new oncology patient to guide them through their diagnosis, coordinates essential support services, and ensures they have access to resources like home health, nutrition assistance, and financial aid. Her work is deeply rooted in advocacy, and she has been instrumental in
connecting patients with community resources that provide gas and grocery gift cards, bill assistance, and even free lodging for those traveling for treatment.
Her passion for patient care stems from her belief that oncology is about more than just treatment—it’s about relationships. “These patients become part of our family,” she says. “Being there for them, whether it’s answering their questions or simply holding their hand, makes all the difference.”
Jennifer’s unwavering commitment ensures that no patient walks their cancer journey alone. Thank you, Jennifer, for your dedication and compassion!
Every day, AON employees go above and beyond—not just for patients, but for each other. In the challenging world of cancer care, there are those who bring light, strength, and kindness to their teams.
Whether it's a colleague who lifts others up, a mentor who leads with compassion, or a team member who makes every day a little brighter, we want to celebrate them.
Help us recognize the people who make a difference.
Email Marketing@AONcology.com to share their story.


Jennifer Lafferty, MS, RDN, CSO, LDN, FAND Manager, Oncology Nutrition Services
For the eighth year running, U.S. News & World Report has ranked the Mediterranean diet as the world’s best, as well as the best diet for diabetes, gut health, and mental well-being. This way of eating emphasizes whole plant foods—fruits, vegetables, whole grains, beans, nuts, seeds, legumes, pulses, herbs, spices, and olive oil—as well as seafood, lean poultry, and moderate amounts of dairy. Red meat, foods high in saturated fat or added sugar, and alcohol are consumed minimally to complement or enhance the main meal. No major food groups are eliminated, making this diet flexible, delicious, appealing, and sustainable.
The same principles found in the Mediterranean diet span a variety of other healthy cuisines. Although Blue Zones—geographical locations associated with health and longevity— like Sardinia, Italy, and Ikaria, Greece, follow the Mediterranean diet, people in other Blue Zones, including Okinawa, Japan; Loma Linda, California; and the Nicoya Peninsula, Costa Rica, also follow plant-based diets that lead to longer, healthier lives.
Meditarranean Diet Guidelines
Daily
• Most of the diet is plant-based. The macronutrient pattern is about 65% carbohydrates, 20% fat, and 15% protein.
• Foods may be raw, cooked, ground, or fermented but not highly processed.
• Water is the primary beverage, with moderate amounts of coffee and tea. Wine may be included in some cultures but is limited to small glasses with meals.
• Beans or lentils are eaten daily.
• Bread is typically whole grain or sourdough.
Weekly
• Snacks are typically nuts and seeds.
• Omega-3 fatty acid-rich fish is consumed in small portions about three times a week.
• Eggs are included up to three times per week.
• Added sugar is restricted to no more than 28 grams daily, or seven teaspoons.
Monthly
• Dairy comes primarily from unsweetened natural yogurt or cheese, such as feta, and is eaten in small portions a few times a month.
• Red meat is restricted to small portions (2 ounces) about five times per month. Processed meats are not consumed.
The Mediterranean diet is the most researched diet in history, with data collected since the early 1950s. The plant-focused diet pattern and other lifestyle factors in Blue Zone communities have also been well documented and consistently show impressive outcomes for health, well-being, and longevity.
Following plant-focused diet patterns, such as the Mediterranean diet, is associated with a lower risk for major chronic diseases like heart disease and diabetes. The diet can also help people achieve sustainable weight loss and prevent obesity. Evidence shows a lower risk for cognitive decline and dementia, positive changes to mood, and healthier bones. By preventing and combating chronic disease, overall longevity and health span are enhanced.
Research currently supports reductions in risk for breast and colorectal cancer with these diet patterns, with a growing body of evidence forming for others. Current diet recommendations for cancer prevention and survivorship align with many of the principles of Blue Zones and Mediterranean diet patterns.
The American Institute for Cancer Research recommends:
• Filling at least two-thirds of each plate with plant foods.
• Emphasizing colorful fruits and vegetables at every meal.
• Choosing high-fiber whole grains and legumes regularly.
• Limiting red meat intake to less than 18 ounces per week and avoiding processed meat.
• Replacing sugar-sweetened beverages with water, tea, coffee, and milk.
• Choosing whole or minimally processed foods.
• Avoiding alcohol.
Plant-focused diets are thought to reduce cancer risk due to the high intake of vitamins, minerals, phytonutrients, and other anti-inflammatory compounds it provides.
Connect at the Table for Good Health and Longevity
The health benefits of the Mediterranean diet go beyond food to encompass a lifestyle where the dining table is also the place to cultivate and nurture strong family and community relationships. Eating with others is a unifying hallmark of all the world’s healthiest communities. Friendship and social connection provide intellectual stimulation and emotional support, both important dimensions of wellness.
Studies of the healthiest cultures in the world show that maintaining strong social connections helps people maintain good health and slows cognitive decline. On the other hand, loneliness has been linked to increased risks for heart disease, diabetes, depression, anxiety, dementia, and early death.
Taking the time to connect over a meal has become less commonplace in our modern, fast-paced society, but it would benefit us all to bring it back.
Take the Challenge: Connect at the Table
Connection through food can be as simple as intentional family meals or lunch with coworkers. Make it a priority to attend or host healthy food gatherings— perhaps serving flavorful Mediterranean dishes at your next casual family dinner, book club, game night, or birthday celebration. Potlucks, cooking classes, and food festivals also provide great opportunities to enjoy connection and community through food.
Follow our tips for building an easy and healthy Mediterranean mezze sharing board using a delicious lemon herb vinaigrette or find your own Mediterranean and Blue Zone recipes online.
Mezze (or meze) is an assortment of small dishes eaten as appetizers or a light meal. Its contents vary by region, but the concept of enjoying savory, healthy foods remains the same. Marinated vegetables, fruit, nuts, cheeses, and dips and spreads such as hummus, yogurt, and baba ghanoush are common.
PREP TIME: 30 MINUTES

Build Your Own Mediterranean Mezze Sharing Board:
Choose at least one item from each category below to build your board. Enjoy with friends and family!
Sauce, Dip or Spread
Tzatziki, Hummus, Yogurt, Muhammara, Pesto, Baba
Ghanoush, Tourlou
Bread Pita bread, Whole grain bread, Sourdough
Marinated or Pickled Foods
Olives, Roasted red peppers, Peppadew, Pepperoncini, Artichokes
Vegetables Cucumber, Cherry tomatoes, Carrots, Roasted cauliflower or Brussels sprouts
Fruits Figs, Peaches, Cherries, Berries, Grapes
Nuts and Seeds Pistachios, Marcona almonds, Pepitas, Walnuts
A Touch of Sweetness
Fig jam, Honey, Pomegranate or date molasses
Fresh Herb Rosemary, Thyme, Basil, Parsley, Dill
Makes 1/2 cup
INGREDIENTS
¼ cup fresh lemon juice
1 small garlic clove, grated 1 teaspoon Dijon mustard ¼ teaspoon sea salt, more to taste
INSTRUCTIONS
Freshly ground black pepper
½ teaspoon honey or maple syrup, optional
⅓ cup extra-virgin olive oil
½ teaspoon fresh or dried thyme
1. In a small bowl, whisk together the lemon juice, garlic, mustard, salt, pepper, and honey, if using.
2. Drizzle in the olive oil while whisking and continue to whisk until the dressing is emulsified. Alternatively, combine everything in a jar with a tight-fitting lid and shake to combine.
3. If your dressing is too tangy, add more olive oil, to taste.
4. Add the thyme, and season to taste.
Store in the refrigerator for up to one week. The olive oil will solidify slightly in the fridge. To soften, let the dressing sit at room temperature for a few minutes and stir before using.
Adapted recipe from: Love & Lemons.
The islands of Ikaria in Greece and Sardinia in Italy share a belief that family and community come first, and this mindset significantly contributes to the remarkable longevity these regions are known for.

In Ikaria, an island nestled in the Aegean Sea, strong family bonds and community engagement are central to daily life. Multigenerational households foster deep connections and mutual support, providing emotional security and a sense of purpose for the elderly. Older adults are not isolated—they are nurtured, included, and often looked to for guidance.
Ikarians also lead vibrant social lives within their communities. Neighbors gather regularly for communal meals, religious celebrations, and informal visits, which helps maintain emotional closeness and reduce feelings of loneliness. Their strong familial ties and active participation in village life sustain both physical and mental health, even into advanced age.

In Nuoro, Sardinia, a unique social fabric supports longevity. Family is at the heart of Sardinian culture, with multiple generations often residing together. Like the Ikarians, they revere elders as family cornerstones, imparting wisdom and maintaining traditions. This deep respect ensures they remain integral to daily life, providing continuous emotional support and a profound sense of belonging.
The broader community thrives on reciprocity and mutual aid. Neighbors frequently share resources and gather for social events, strengthening bonds and alleviating stress. This blend of familial respect and communal cooperation fosters an environment where individuals feel valued and supported.
What we can learn from these people who love people is that genuine connections and a strong support system are essential to a fulfilling life. Whether in our personal relationships or professional environments, prioritizing community, respect, and collaboration can lead to greater well-being, resilience, and longevity—lessons that Ikaria and Sardinia have exemplified for generations.
Tracy's story demonstrates the healing power of strong social connections

Tracy’s journey is one of resilience and an unwavering commitment to helping others. A patient of Dr. Rangappa Rajendra at Oncology/Hematology of Loudoun and Reston, she’s twice survived breast cancer and turned her personal battle into a mission to uplift and support those facing similar challenges. Her passion for advocacy and community outreach has not only transformed her own life but has had a profound impact on countless others. From leading breast health workshops to championing equity in care, Tracy’s dedication to ensuring that every patient has access to the resources and support they need is inspiring.
To expand access to breast health education across the DC metro area, Tracy became a certified Breast Health
Educator for Y-Me Breast Cancer Foundation, leading workshops to inform and empower women. She also provides online support to newly diagnosed patients through the “In Your Shoes” program. Later, Tracy took on the role of Executive Director for Breast Cancer Network of Strength, where she worked to ensure underserved women received mammograms and essential care.
In addition, she helped her sorority launch an annual sewing event to create “Kozy Caps” for women undergoing cancer treatment.
“I feel that God carried me through this journey so that I could be a source of strength and comfort for others who would travel this road,” she says. “I work hard to educate providers on how my organization can help patients with support programs and treatments.
I also challenge my organization to be more active in meeting the needs of those who may not have the support that I had on my treatment journey.”
Tracy’s own cancer journey began in 2000, when she was the president of the local Alpha Kappa Alpha sorority. She had just returned home from an event honoring their collaboration with the American Cancer Society when a self-breast exam—something she had long advocated for—led her to discover a lump. Although her primary care physician suggested she could wait until after the holidays, Tracy was determined to get answers.
“I went to another doctor immediately, crying and screaming. They sent me for a biopsy. Three days before Christmas, I received the results: ‘You have cancer.’ I got in my car and drove 10 hours to my mom’s house!”
"I want to thank Dr. Rajendra and his team for two cancer journeys with me and my family. You were with me every step of the way."
She cannot stress enough the importance of having a support network. “If you know someone who is diagnosed, talk to them about the people you know who survived. Give them hope. Understand that there are moments through the journey that a patient might not be able to show gratitude, but they are truly grateful for your care and concern.”

Born and raised in Nashville, Tracy received her degree in Marketing and Business Administration from Middle Tennessee State University. She moved to Virginia to begin working in the pharmaceutical industry, building a successful career that took her around the world. But her diagnosis turned her life upside down.
“Because I’d attended so many events with the American Cancer Society, I had some idea of what I needed to do. But it was overwhelming. I had to see a surgeon, and there were so many tests and choices to make.”
Fortunately, Tracy was surrounded by a strong community. Family, sorority sisters, friends, and church family all rallied around her, accompanying her to treatment, making sure she was eating, and offering constant encouragement. She fondly recalls her dear friend Mr. Ganell, who, despite his own Stage 4 cancer diagnosis, “called every Sunday at 1:00 to pray with me.”
In 2021, twenty-one years after her initial diagnosis, Tracy faced breast cancer once again. She was diagnosed with ER PR-positive breast cancer and underwent a double mastectomy. “I had a tough year of recovery, but just like my first diagnosis, thankfully no nodal involvement. I take all this to mean that God has decided that my work is not yet done.”
Now, Tracy is healthy, traveling, and continuing her mission to serve others. Her journey is a testament to the power of faith, perseverance, and the strength of a supportive community. Just as her own network of loved ones played an essential role in her recovery, she has devoted herself to being that pillar of support for others. Through her advocacy, outreach, and compassion, Tracy has not only survived but thrived, proving that healing extends beyond medicine—it flourishes in the love and care of a community.
“I want to thank Dr. Rajendra and his team for two cancer journeys with me and my family. You were with me every step of the way. Your care, your patience, and your encouragement have allowed me the ability to continue to do all the things that God has planned for me. I am so grateful for you!”












Step into the future of oncology at AON’s Clinical Summit 2025: Tomorrow’s Oncology Today, where cutting-edge advancements meet real-world impact. Join fellow oncologists and healthcare leaders in Dallas, Texas, from November 7–8 at The Ritz-Carlton Dallas, Las Colinas, for two days of education, collaboration, and innovation.
Through expert-led sessions and dynamic discussions, attendees will gain valuable insights, expand their expertise, and connect with peers—all in a setting focused on advancing oncology, enhancing patient care, and driving value-based treatment forward.
Be part of the conversations shaping tomorrow’s oncology, today. Watch your inbox! This special event is by invitation only, and we’d love to see you there.