g n i t e e M l a u n n A N AA
k o o L y l r Ea
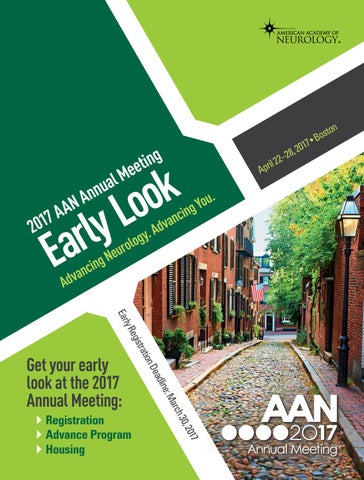
7 1 0 2
y. g o ol r u e N g in c n a v d A
. u o Y g n i c n a Adv
e: dlin Dea ion trat egis ly R Ear
}} Registration }} Advance Program }} Housing
7 201 30, rch Ma
Get your early look at the 2017 Annual Meeting:
ton s o •B 7 1 , 20 8 2 22– l i r Ap