

BUDGET FLATLINE
CALLS FOR A VITAL FUNDING INJECTION









Power your practice if a privacy breach or cyber incident occurs



These unwelcome events can be stressful, and costly, for you and your practice.








With Avant Practice Medical Indemnity Insurance, you’re covered for the actions of staff and claims made against the practice.



And if you run an eligible practice, it also includes complimentary Cyber Insurance to protect your practice against cyber extortion, privacy liabilities and damage to digital assets.

































WHAT’S INSIDE



FEATURES
REGULARS



EDITOR’S WORD
DON’T LET THE HEALTH BUDGET FLATLINE
It is imperative that the government addresses the health system crumbling before it.

The health workforce of NSW did an extraordinary job of rising to the unprecedented challenges of Covid-19. But faced with another crisis could it cope again? There’s a real fear that it might not.
Increasingly, our hospitals are having to do more with less. Workers from top to bottom are being pushed to breaking point and are increasingly heard wondering just how long they can continue.
Endless extra hours are worked with no extra pay, because there is insufficient workforce to fill the gaps. Employees have been asked to do jobs they are unqualified to perform. Units are using faulty equipment because there is no money to supply a replacement. There is genuine concern for the future of our health system and for all those who rely on it. In compiling our pre-budget cover story it was surprising to encounter doctors who were often not aware that the NSW health budget was effectively cut by 7% because of how miserly it was dealt with in last September’s budget. A woefully inadequate overall increase of 0.87% was gobbled up by health inflation estimated at 8%.
And when we asked doctors what they would ask Health Minister Ryan Park for the answer was universal. Money.
Why? Because they know their capacity to do more with less has already been exceeded. There’s now nothing left in reserve even as demand on the health system continues to grow.
In our pre-budget submission, AMA (NSW) has called for better pay and conditions for NSW doctors including modernised contractual and employment arrangements, award reform and greater transparency in regard to shortages.
We have further called for increased funding for effective, safe, planned delivery of non-urgent surgery in public hospitals by improving transparency of real waiting times, reducing non-urgent waiting lists and minimising the practice of outsourcing non-urgent surgery to private hospitals.
The government must act now to save its crumbling health system. dr. Rahni
AMA (NSW) BOARD
Dr Michael Bonning, President
Dr Kathryn Austin, Vice President
Dr Fred Betros
Dr Costa Boyages
Dr Brian Fernandes
Dr Amandeep Hansra
Dr Sanjay Hettige
Dr Kean-Seang Lim
Dr Theresa Ly
SECRETARIAT
Chief Executive Officer, Fiona Davies
Director, Workplace Relations
Dominique Egan
Director, Membership Engagement and Commercial Partnerships
Gary White Editor
Rahni Sadler
rahni.sadler@amansw.com.au
Staff Writers
Isabella Angeli
Isabella.angeli@amansw.com.au
Ally Chandler
Ally.chandler@amansw.com.au
Design
Rebecca Strahan
Advertising enquiries
Kirsty Smith
Kirsty.smith@amansw.com.au
Cover image
Hayden Brotchie Photography
By your side more than ever before.

Delivering you a whole new level of support in your professional and personal life, with services tailored for doctors.

PLAYING THE LONG GAME
Creating a health system for a lifetime.
 Dr Michael Bonning President, AMA (NSW)
Dr Michael Bonning President, AMA (NSW)
As I finish my time as your AMA NSW president, I entreat you all to fight for our health system, for the resources it needs now and into the future, our system deserves as much.
IT HAS BEEN A GREAT PRIVILEGE and pleasure to represent the interests of doctors, patients and the health system in our state. As I prepare for the end of my presidency of AMA (NSW) my wife, Claire, and I have been preparing for the birth of our first child. This has reinforced for me the generational nature and long cycle of reform and improvement that our health system requires to support our children and theirs through their many years of life.
What stands in the way of fundamental long-term change is the brevity of election cycles. Politicians need to balance demands for action and outcomes with the meaningful programs which may take several election cycles to show benefit.
In the medical field we use time to understand patterns of disease and challenges to the system, and we come to understand that there is signal amongst the noise as research and clinical experience slowly build a critical picture of change. That, however, can be perceived as inaction, which doesn’t play well with electors.
The timeframe of political decision making is therefore anathema to good use of limited health resources and often disadvantages programs that are developing evidence over prolonged periods which have the ability to affect the future health of many people. We see this in changes in scope of practice driven
by politicians around the country, a convenient approach that reduces the comprehensiveness of care even as the challenge of chronic disease grows.
The difficult political decisions, to fund hospitals for the services the public needs while also working to encourage measures to promote prevention against monied interests who promote gambling, junk food and disinformation via social media is a challenge that needs the long view of dedicated doctors. It needs the AMA to retain the mantle of holding strong on positions that while not being the most expedient solutions are ultimately the necessary ones for health outcomes over generations. The reason the AMA is respected and influential is because it takes this long view. In one of the articles in this edition of The NSW Doctor we discuss the harbinger of indemnity failures which have the potential to undermine our system of medical practice. Australia, and New South Wales in particular, provide excellent healthcare but that system is under pressure from many directions. To ensure our health system is fit for purpose in the future we need the long view, of which the AMA is a primary advocate.
As I finish my time as your AMA (NSW) president, I entreat you all to fight for our health system, for the resources it needs now and into the future, our system deserves as much. dr.

SYDNEY CITY LEXUS
EXCLUSIVE CORPORATE BENEFITS
Get exclusive benefits across a range of Lexus models with our Lexus Corporate Programme* at Sydney City Lexus.
THE BENEFITS FOR AMA NSW MEMBERS
Preferential Corporate Pricing3
3 year/60,000km complimentary standard logbook servicing4
Reduce dealer pre-delivery fee of $995 (ex GST)
Competitive total cost of ownership
Find out more at Sydney City Lexus.com.au/Corporate
To access the Lexus Corporate Programme please contact Ronald Chin from Sydney City Lexus on 0488 852 283 or lexus.reception@sydneycitylexus.com.au

ENCORE OWNER BENEFITS PROGRAM5
- Invitations to Exclusive Events
- DriveCare6 Assist
- Luxury Hotel Partnership Benefits
- Generous fuel offer
- Complimentary loan car and complimentary pick up and drop off when your Lexus is being serviced
- Complimentary wash and interior vacuum after each service
SYDNEY CITY LEXUS GLEBE | 36 - 38 Parramatta Road Glebe NSW 2037 | PH 02 9565 6363 | sydneycitylexus.com.au | MD053160
SYDNEY CITY LEXUS WATERLOO | 824 Bourke St Waterloo NSW 2017 | PH 02 8303 1900 | sydneycitylexus.com.au | MD053160
1. Terms and Conditions apply. Contact the team at Sydney City Lexus to learn more.
2. Eligible models for the Corporate Program are subject to change and may vary from time to time. Please contact Sydney City Lexus for more information.
3. Eligible members must provide such documentary evidence as Lexus or the Sydney City Lexus may reasonably require to confirm entitlement to receive preferential pricing. Visit sydneycitylexus.com.au/corporate for details and eligibility requirements.
4. Complimentary scheduled servicing expires at 3 years of 60,000km from the date of first registration, whichever occurs first.
5. Encore Benefits apply on new and demonstrator vehicles for a 3 year period from the date vehicle is first registered on or after 01/01/2020. Inclusions may change without notice. For full T&C’s and details see Sydney City Lexus or lexus.com.au/owners/benefits.
6. DriveCare as part of Encore Benefits applies for a 3 year period from the date a new or demonstrator Lexus vehicle is first registered on or after 01/01/2020. Coverage and service inclusions very dependent on vehicle location. For full T&Cs see Sydney City Lexus or lexus.com.au/smallprint/encore-terms.

HOW DID YOU GET TO WHERE YOU ARE?

 Fiona Davies CEO, AMA (NSW)
Fiona Davies CEO, AMA (NSW)
THE THEME FOR OUR RECENT International Women’s Day Event was “How did you get to where you are”. The inspiration was the discussions I have with younger people, who feel they need to know exactly what their life plan is. I know so many incredibly successful people who have had a varied journey to get to where they are. For me, the journey started with not getting into the law degree I hoped for, doing a business degree instead because my friend liked a boy who was doing the same degree. My first job was a secretarial role where I had to fudge my typing qualifications.
From there I was introduced to a job at the AMA, starting at a junior
had this wonderful job for over 10 years. While I had no plans for such a job, it remains a job I am proud of and enjoy every day (most days).
Even with a plan, there are so many things that happen in lifeillness, divorce, remarriage, disability - which can impact the trajectory of your seemingly well mapped out journey. In my discussions with Dr Kathryn Hutt, Medical Director for the NSW DHAS, she often reflects on the number of doctors, who find themselves deeply distressed that their plans for a successful career in concert with a thriving family or relationship sadly often prove challenging. Speaking about different paths won’t always take away the sadness or distress but it shows some empathy and reminds people that everyone has a how did you get where you are story. dr.




According to the AMA’s upcoming 2023 Public Hospital Report Card, the NSW Health system’s performance fell across the board.
Despite being the strongest performing State overall, NSW was one of only two States to fall across all four key performance metrics studied by the report card.
FEATURE
“All that holds the NSW health system together is the goodwill of devoted workers showing up, going above, beyond and even further to keep servicing the patients of this state. But as demand increases and resources are cut the workforce can’t and won’t continue limping along.”
Dr Michael Bonning, AMA (NSW) President
HEALTH WAS NEVER EXPECTED to be a priority in the Minns Government’s initial budget. It wasn’t a prominent issue during the Labor Party’s campaign leading up to last year’s State election. Consequently, the announcement of a mere 0.87% increase in health spending for 2023-24, bringing the total to $30.951 billion from the previous year’s $30.684 billion, was met with criticism. Dr Michael Bonning, President of AMA (NSW), labelled this increase as “paltry.”
Taking into account health inflation, estimated at 8% last year, the real terms of this increase amounted to a 7% decline. This has left the already strained NSW Health workforce grappling with a significant budgetary shortfall compared to the previous year.
Dr Bonning said the repercussions have been felt acutely across the State. “While the Covid threat has waned, the NSW Health system faces new and increasing challenges,” he said, “including ambulance ramping, hospital log jam, long planned surgery waitlists, and the pressure from our growing and ageing population with complex, chronic health conditions.”
“Our drastically overburdened health workforce cannot continue to perform under the current conditions and needs an urgent injection of health dollars,” Dr Bonning said. “I’m not sure the government realises how close the entire health system is to collapse.”
HEALTH SYSTEM IN DECLINE
The effect of the cuts is being felt at a time when New South Wales is facing record demand. Statistics paint a grim picture of a system in crisis.
According to the NSW Bureau of Health and Information, in the period between October 1 and December 31, 2023:
» Ambulance activity was higher than any quarter since the BHI began reporting in 2010 at 379,705 responses including a record 14,741 “highest priority – P1A” responses for patients with a life-threatening condition, up a staggering 34.8% (3,804) from the same quarter the previous year.
» There were 798,813 ED attendances, up from 790,309 in the same period last year, and up 2.9% on pre-pandemic levels.
» EDs continued to see more of the most urgent patients with 6,649 triage 1 presentations and 119,389 triage 2 presentations – both the highest of any quarter since BHI started reporting in 2010.
» While 58.1% of patients spent less than four hours in the ED, a slight improvement on the record low in the preceding quarter, one in 10 patients spent longer than 10 hours 30 minutes in the ED – well above pre-pandemic levels.
» There were 497, 870 admitted patient episodes – up 4.6% (21,838) from the same quarter the previous year.
» There were 230,643 acute sameday patient episodes – the largest increase (5.9%) in this type of care

compared to pre-pandemic levels.
» The average length of stay for overnight non-acute episodes was 16.7 days, 12.8% higher than prepandemic levels.
According to the AMA’s upcoming 2023 Public Hospital Report Card, the NSW Health system’s performance fell across the board. Despite being the strongest performing State overall, NSW was one of only two States to fall across all four key performance metrics studied by the report card. Patient outcomes worsened for the percentage of Emergency Department Category 3 patients seen within 30 minutes, the proportion of patients leaving the Emergency Department within four hours or less, median waiting time for elective surgery and the percentage of Category 2 patients seen on time (90 days).
“These figures should be a wakeup call for the NSW government,” Dr Bonning said. “The health system is crumbling under unprecedented demand, while staff try to manage after funding cuts delivered in the Minns Government’s first budget.”
DOCTORS AT BREAKING POINT
Meanwhile, the AMA (NSW) has been receiving calls from doctors
who are at wits’ end, barely able to function in their jobs because they don’t have the necessary staffing or equipment. Doctors report feeling at breaking point, grappling with a workload that far exceeds capacity.
“Lots of our long-term staff are leaving, reducing hours or not putting in extra hours and effort because it’s impossible to continue full-time in this environment,” lamented a metropolitan hospital specialist, who has felt the need to reduce her own workload under such conditions.
“In the hope that it might save me from leaving medicine altogether, I have dropped to half-time and resigned from many leadership roles and rosters.”
One doctor in a metropolitan Sydney hospital told The NSW Doctor, “It’s been happening over the past few months. We aren’t given staff to fill vacancies. We can’t backfill for maternity leave. I’ve never seen it like this. I don’t know
FEATURE
what we’re expected to do.”
A metropolitan hospital psychologist weighs in: “Staff are burning out due to the increased complexity, severity and number of patients. Budgets aren’t matched to population growth, so staff are expected to do the same amount with less resources.”
STAFF SHORTAGES REACHING CRISIS POINT
“The biggest State-wide issue is lack of staff, as there are not enough doctors and nurses to patient ratios,” a doctor-in-training who has worked in regional and metropolitan hospitals said.
“With many (doctors) calling in sick and quitting, the shortages burden existing staff. It’s a negative feedback loop reflecting a system that’s not coping which will get worse unless the NSW Government does something.”
Staff shortages are now so chronic that desperate measures

“Staff are burning out due to the increased complexity, severity and number of patients. Budgets aren’t matched to population growth, so staff are expected to do the same amount with less resources.”
Western Sydney surgeon
are used to spread out employees, with staff taking on roles they are unqualified or underqualified to perform while others simply take on a much greater workload, without additional remuneration.
WE ASKED OUR AMA (NSW) COUNCILLORS WHAT THEY WERE
SEEING ON THE GROUND: AMA (NSW) Councillor Dr Anne Rasmussen is a senior anaesthetist. She notes, “There’s been an attrition of experienced nursing staff across NSW. Obviously, the award is less for nurses in NSW, so we’ve lost nursing staff to Queensland in particular. In my field of anaesthetics, where we normally had nurses we’ve worked with for a long time, we’re now being introduced to the new anaesthetic nurse on the day, who’s actually never been in an operating theatre before, because she’s the only one who applied for the job.
“We as surgeons have been ordered to train nursing staff in theatre. My colleague in a metropolitan hospital has been asked to use nursing assistants to do what are traditionally nursing roles because of nursing shortages. That’s never happened in my career before but that’s probably the direction we’re heading to.”
A metropolitan staff specialist complained, “There is such a shortage of nursing staff in the Intensive Care Unit (ICU). Nurses are regularly deployed to wards whose processes they’re unfamiliar with, so ICU has a smaller capacity and must refuse patients. This results in inefficient and deficient care, and care for ICU patients decreases plus we have to delay or refuse new patients from ED.”
Fellow AMA (NSW) Councillor, Neonatologist Dr Eveline Staub said, “Staff shortages lead to a costly logjam, with the postnatal ward unable to meet the 11am discharge
FEATURE
“The NSW health system has repeatedly been recognised as one of the most effective systems within Australia. Despite its strengths, the NSW public health system risks losing its status if it is not possible to attract and retain doctors to work in it,”
Dr Michael Bonning, AMA (NSW) Presidenttime because the junior doctor who examines babies prior to leaving has higher priority jobs, including deliveries. Baby checks are their least acute task so mothers often wait all day for that examination then can’t go home until late afternoon, which causes bed block and patient flow problems that our department gets reprimanded for.”
LACK OF EQUIPMENT, RESOURCES
It’s not just staffing shortages, it’s equipment ordered, that has never arrived. Dr Staub said, “We have continually requested new equipment in anticipation of old devices becoming redundant, but it wasn’t approved so we had no functional equipment to cool babies after birth asphyxia, which is an essential service the Ministry tasks us with.”
“Scrambling ensued and the matter escalated through the hospital ranks until two new devices were ordered and delivered but they had to be paid for by donations, which is the desperate situations hospitals are finding themselves in across the State,” she added.
Another rural surgeon spoke of similar issues: “An ultrasound machine was approved but after the funding cuts last year we weren’t allowed to purchase it. As a result, we have to wait until the equipment is free which causes theatre delays and decreased efficiency. It all has a roll-on effect.”
Many doctors have expressed frustration at what they describe as an information void. “We put in for
funding for things we need urgently, and we just don’t hear anything.” A Western Sydney surgeon said, “No ‘yes’, no ‘no’, no nothing. It’s as if we never applied, and there’s no mechanism for asking where things are up to or why they haven’t arrived.”
One metropolitan hospital specialist lamented the lack of clarity from her facility’s management which doesn’t give prior notice to staff about resource cuts and refuses to reveal who makes such crucial decisions. “There’s no communication, no transparency, no accountability,” she said.
This western Sydney surgeon summed up: “It’s so short sighted. These financial plans are the ultimate false economy. There’s going to be cumulative delays in service, increasing inefficiencies in clinical services, it will impact and delay accessing care, particularly for elective cases. We need clinicians and associated services. It is selfdefeating to reduce costs and render yourself unable to care for any patients.”
AMA (NSW)’S SUBMISSION TO GOVERNMENT
In its submission to the Special Commission of Inquiry into Health Funding, AMA (NSW) wrote: “The New South Wales Government has dedicated significant funding to building new infrastructure, but there has not been the same resourcing dedicated to bolstering workforce numbers to staff the current and foreseeable institutions.”
In delivering AMA (NSW)’s prebudget submission Dr Michael

Bonning said, “We are calling on the Minns Government to commit to a substantial increase in health funding in the upcoming budget, as outlined in our submission.
In comparison to NSW, Dr Bonning said the Queensland Government increased its health budget by 9.6%. As the most populous state in Australia with an ABS Estimated Resident Population (ERP) of 8,339,300, NSW received $30,951 billion. Queensland, whose ERP is just 5,459,413, received $25.8 billion.
“Given NSW Health is the largest health care system in Australia and by the Department’s own admission one of the largest in the world, this hardly seems appropriate,” Dr Bonning said. “It is the people of NSW who will suffer,” Dr Bonning warned. “With less access to EDs, less urgent and non-urgent surgery, and our State’s innovative programs, such as the collaborative care projects, will be at risk.”
“The NSW health system has repeatedly been recognised as one of the most effective systems within Australia. Despite its strengths, the NSW public health system risks losing its status if it is not possible to attract and retain doctors to work in it,” Dr Bonning said. dr.



 By Dr Monica Wang, Associate Professor of Public Health, Boston University
By Dr Monica Wang, Associate Professor of Public Health, Boston University
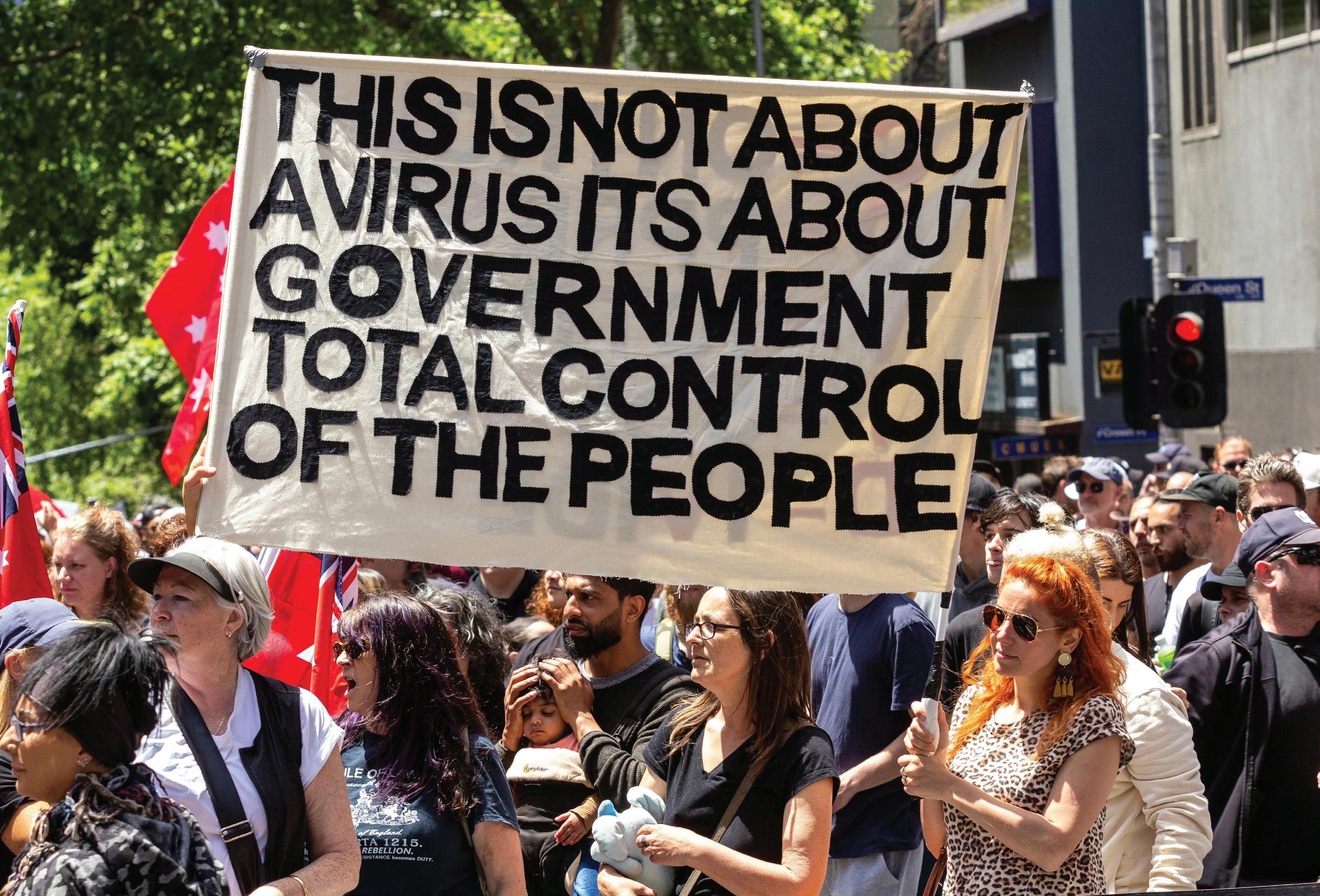
HEALTH MISINFORMATION IS RAMPANT ON SOCIAL MEDIA. Here’s what it does, why it spreads and what people can do about it.
THE GLOBAL ANTI-VACCINE movement and vaccine hesitancy that accelerated during the COVID-19 pandemic show no signs of abating.
According to a survey of U.S. adults, Americans in October 2023 were less likely to view approved vaccines as safe than they were in April 2021. As vaccine confidence falls, health misinformation continues to spread like wildfire on social media and in real life.
I am a public health expert in health misinformation, science communication and health behaviour change.
In my view, we cannot underestimate the dangers of health misinformation and the need to understand why it spreads and what we can do about it. Health misinformation is defined as any health-related claim that is false based on current scientific consensus.
One major reason behind the spread of health misinformation is declining trust in science and government.
OLDEST & YOUNGEST
Vaccines are the No. 1 topic of misleading health claims. Some common myths about vaccines include:
✘ Their supposed link with human diagnoses of autism. Multiple studies have discredited this claim, and it has been firmly refuted by the World Health Organization, the National Academies of

FEATURE
Sciences, Engineering and Medicine, the American Academy of Paediatrics and the Centers for Disease Control and Prevention.
Concerns with the COVID-19 vaccine leading to infertility. This connection has been debunked through a systematic review and meta-analysis, one of the most robust forms of synthesizing scientific evidence.
✘ Safety concerns about vaccine ingredients, such as thimerosal, aluminium and formaldehyde. Extensive studies have shown these ingredients are safe when used in the minimal amounts contained in vaccines.
✘ Vaccines as medically unnecessary to protect from disease. The development and dissemination of vaccines for life-threatening diseases such as smallpox, polio, measles, mumps, rubella and the flu has saved millions of lives. It also played a critical role in historic increases in average life expectancy –from 47 years in 1900 in the U.S. to 76 years in 2023.
The costs of health misinformation
Beliefs in such myths have come at the highest cost. An estimated 319,000 COVID-19 deaths that occurred between January 2021 and April 2022 in the U.S. could have been prevented if those individuals had been vaccinated, according to a data dashboard from the Brown University School of Public Health. Misinformation and disinformation about COVID-19 vaccines alone have cost the U.S. economy an estimated US$50 million to $300 million per day in direct costs from hospitalisations, long-term illness, lives lost and economic losses from missed work.
Though vaccine myths and misunderstandings tend to dominate conversations about health, there is an abundance of misinformation on social media surrounding diets and eating disorders, smoking or substance use, chronic diseases and medical treatments.
My team’s research and that of others show that social media platforms have become go-to sources for health information, especially among adolescents and young adults. However, many people are not equipped to manoeuvre the maze of health misinformation.
For example, an analysis of Instagram and TikTok posts from 2022 to 2023 by The Washington Post and the non-profit news site The Examination found that the food, beverage and dietary supplement industries paid dozens of registered dietitian influencers to post content promoting diet soda, sugar and supplements, reaching millions of viewers. The dietitians’ relationships with the food industry were not always made clear to viewers.
Studies show that health misinformation spread on social media results in fewer people getting vaccinated and can also increase the risk of other health dangers such as disordered eating and unsafe sex practices and sexually transmitted infections. Health misinformation has even bled over into animal health, with a 2023 study finding that 53% of dog owners surveyed in a nationally representative sample report being sceptical of pet vaccines.
Health misinformation is on the rise
One major reason behind the spread of health misinformation is declining trust in science and government. Rising political polarisation, coupled with historical medical mistrust among communities that have experienced and continue to experience unequal health care treatment, exacerbates pre-existing divides.
FEATURE

A study of misinformation spread on Twitter analysing data from 2006 to 2017 found that falsehoods were 70% more likely to be shared than the truth and spread “further, faster, deeper and more broadly than the truth” across all categories of information.
The lack of trust is both fuelled and reinforced by the way misinformation can spread today. Social media platforms allow people to form information silos with ease; you can curate your networks and your feed by unfollowing or muting contradictory views from your own and liking and sharing content that aligns with your existing beliefs and value systems.
By tailoring content based on past interactions, social media algorithms can unintentionally limit your exposure to diverse perspectives and generate a fragmented and incomplete understanding of information.
Even more concerning, a study of misinformation spread on Twitter analysing data from 2006 to 2017 found that falsehoods were 70%
more likely to be shared than the truth and spread “further, faster, deeper and more broadly than the truth” across all categories of information.
How to combat misinformation
The lack of robust and standardized regulation of misinformation content on social media places the difficult task of discerning what is true or false information on individual users. We scientists and research entities can also do better in communicating our science and rebuilding trust, as my colleague and I have previously written. I also provide peer-reviewed recommendations for the important roles that parents/caregivers,
policymakers and social media companies can play.
Below are some steps that consumers can take to identify and prevent health misinformation spread:
• Check the source. Determine the credibility of the health information by checking if the source is a reputable organization or agency such as the World Health Organization, the National Institutes of Health or the Centers for Disease Control and Prevention. Other credible sources include an established medical or scientific institution or a peer-reviewed study in an academic journal. Be cautious of information that comes from unknown or biased sources.
• Examine author credentials Look for qualifications, expertise and relevant professional affiliations for the author or authors presenting the information. Be wary if author information is missing or difficult to verify.
• Pay attention to the date Scientific knowledge by design is meant to evolve as new evidence emerges. Outdated information may not be the most accurate. Look for recent data and updates that contextualize findings within the broader field.
• Cross-reference to determine scientific consensus. Crossreference information across multiple reliable sources. Strong consensus across experts and multiple scientific studies supports the validity of health information. If a health claim on social media contradicts widely accepted scientific consensus and stems from unknown or unreputable sources, it is likely unreliable.
• Question sensational claims. Misleading health information often uses sensational





language designed to provoke strong emotions to grab attention. Phrases like “miracle cure,” “secret remedy” or “guaranteed results” may signal exaggeration. Be alert for potential conflicts of interest and sponsored content.
• Weigh scientific evidence over individual anecdotes. Prioritise information grounded in scientific studies that have undergone rigorous research methods, such as randomized controlled trials, peer review and validation. When done well with representative samples, the scientific process provides a reliable foundation for health recommendations compared to individual anecdotes. Though personal stories can be compelling, they should not be the sole basis for health decisions.
• Talk with a health care professional. If health information is confusing or contradictory, seek guidance from trusted health care providers who can offer personalized advice based on their expertise and individual health needs.
• When in doubt, don’t share. Sharing health claims without validity or verification contributes to misinformation spread and preventable harm.
All of us can play a part in responsibly consuming and sharing information so that the spread of the truth outpaces the false. dr.
Strong consensus across experts and multiple scientific studies supports the validity of health information.

What can doctors do to help stop the spread of misinformation?
1. Stay updated on emerging health myths or misinformation circulating online. New health misconceptions can emerge or old ones resurface, so being wellinformed about the latest trends in health misinformation, physicians will be better equipped to address them effectively.
2. For physicians who are already active on social media and find it to be a valuable platform for sharing information, they can leverage their presence to share evidence-based content and draw attention to prevalent misinformation. They can focus on providing accurate information through their own posts and educational materials, thereby ensuring a broader reach and impact.
3. It is important to note that directly engaging with misinformed quotes or individuals may not always yield the desired outcomes because it may reinforce existing beliefs. Engaging with misinformed content may also inadvertently amplify the spread of misinformation by giving it more visibility – even if a physician provides accurate information in response to a post, it may be overshadowed by the original misinformation, especially if it garners more attention or engagement. Additionally, engaging directly with misinformed
individuals can be time-consuming and emotionally taxing for physicians.
4. Most importantly, physicians can actively engage their patients during visits by asking questions about the sources and origins of the health information they encounter and directing them to reliable sources of information. Understanding the specific sources and channels through which misinformation spreads enables physicians to tailor their educational efforts and navigate the conversation more effectively. By approaching the conversation through humble inquiry, physicians can foster open and non-judgmental communication. This creates a supportive environment where patients feel comfortable sharing their concerns and uncertainties about health information. It also encourages patients to actively participate in their own healthcare decisions, promoting patient autonomy and empowerment. These steps can help doctors combat the spread of health misinformation and promote well-being on a larger scale
This article is republished from The Conversation under a Creative Commons license. Scan the QR code to read the original article with references.

PRESERVING PRACTICE MEDICAL INDEMNITY BACK ON THE AGENDA

In September 2003, 4000 Australian doctors turned out to protest skyrocketing insurance costs, highlighting the urgent need for government intervention to ensure affordable medical indemnity, thereby safeguarding the accessibility and sustainability of healthcare services.
THERALLYWASheld following the collapse of one of the largest medical indemnity providers, United Medical Protection (UMP), and shaped much medical practice in Australia to this day. While the rally was a landmark event, it was the culmination of years of incremental concern about medical indemnity, an issue which is back on the agenda today.
THEHISTORY
Former AMA President, Dr Andrew Pesce recently presented at a meeting of Societies convened by AMA (NSW) about the issue of indemnity. Prior to the 1990s, he explained, doctors were rarely sued, and professional indemnity was offered by state-based medical defence organisations. Dr Pesce said in 1993, when he started in specialist obstetric practice, his premium was $400 per year. Over the course of the 1990s, the environment changed and there
was a significant increase in the frequency and size of claims against doctors. The AMA responded to increasing concerns by establishing a Medical Indemnity Taskforce which considered legislative and other reforms, such as a Lifetime Care and Support scheme for people suffering catastrophic injury.
Dr Pesce said that by 2000, significant risk premiums had been imposed on specialities such as obstetrics, neurosurgery and orthopaedics,andhisownpremium had increased to $40,000 per annum.Despitesignificantpremium increases, indemnity insurers were still at risk of insufficient funding for claims likely to emerge in future years.
Dr Pesce said that at the time, State and Federal governments saw this as a ‘doctor problem’, not an issue they needed to get involved in. Instead of seeking to deal with the issue of how injured Australians
were provided necessary care and support, governments focused on how the civil claims system worked, and ensuring medical indemnity insurers had adequate funds available to cover all likely claims against their doctor members.
They made indemnity insurance mandatory for all doctors, a requirement which has now transferred into national law. State and Federal governments also forced insurers to stop funding cover on the basis of collecting premiums to cover claims notified in that year – and instead made them collect sufficient funds to cover all claims incurred, even if not notified
This, combined with the collapse of HIH, the major reinsurer for many MDOs in 2001, meant most MDOs were made technically insolvent and UMP, Australia’s largest MDO, was placed under administration.
AMA (NSW) CEO Fiona Davies remembers the time well
In the 2024 renewal period, AMA (NSW) received more feedback from higher risk specialities such as neurosurgery and bariatric surgery that premiums had again increased significantly.
Ms Davies said, “Looking back, it was extraordinary remembering doctors fearful of losing their homes and most doctors in NSW having to pay an additional year of premium to stay in practice. Twenty years later, I can still recall the distress.”
The Federal Government had, up until this time, assumed commercial insurers would come in and take over the problem. They didn’t, leaving doctors potentially uninsured and withdrawing from services and the Federal Government with a signiicant crisis on its hands.
Dr Pesce said the AMA was able to negotiate significant reforms, including that the Federal Government offered a guarantee to MDOs to allow them to continue to operate, the establishment of the High-Cost Claims Scheme, the Premium Support Scheme and Run Off- Cover Scheme, which provided premium affordability and allowed doctors to retire without having to continue to pay excessive premiums. These hard-fought beneits achieved by the AMA remain to this day.
MEDICALINDEMNITY BACKONTHEAGENDA
Fast forward to today and indemnity is back on the agenda. AMA (NSW) President Dr Michael Bonning said AMA (NSW) is again being approached by concerned members,whodescribeincreasesto premiumsinhigherriskspecialities andsurchargesplacedoninsurance asparticularlyconcerning.
In the 2024 renewal period, AMA
(NSW) received more feedback from higher risk specialities such as neurosurgery and bariatric surgery that premiums had again increased significantly.
Dr Anne Rasmussen, anaesthetist and AMA (NSW) Councillor, said she is seeing doctors move out of subspecialties or change their practice due to indemnity costs. She said this had real life implications for patients and access to services, especially in smaller regional areas.
A spokesperson for leading medical insurer Avant said “We operate in an environment of stability where insurers are well capitalised, highly regulated by the Australian Prudential Regulation Authority and affordability is well supported by government schemes.
“We can’t speak for the rest of the industry, but Avant’s average rate increases have been below CPI for the last few renewal cycles. Some limited specialities have experienced double digit increases but this reflects significant increases in the frequency and severity of claims and represent less than 1% of our member base.”
As well as the increasing cost of indemnity, the AMA is concerned about a shift in the nature of claims, and the understanding of what is a reasonable and appropriate level of care.
Dominique Egan, AMA (NSW) Director of Workplace Relations said, “While many more claims are settling for understandable and appropriate reasons, including the distress that accompanies litigation, this means there is a lack of transparency regarding the settlement sum and the components of the settlement sum.”
Dr Bonning said the AMA was focused on the viability and sustainability of the indemnity system because it matters for doctors and patients. Dr Bonning said as governments found out in the early 2000s, doctors will change the nature of their practice due to risk. They will limit services in higher risk areas and consider whether they will provide services to private patients in public hospitals, all of which can impact access to care. AMA (NSW) CEO Fiona Davies said our message to all doctors, new or established, is that they should not take for granted the situation they enjoy. “Those wins were hard fought, and they need to be maintained. That is the ongoing role of the AMA,” Ms Davies said. dr.
KEY ISSUES AMA (NSW) IS CONSIDERING:
1.Should there be more oversight regarding the setting of premiums and the pricing of risk in a mutual environment?
2.Should the profession be considering other schemes such as nofault claim schemes?
3.Is the role and conduct of expert witnesses adversely impacting on settlements and claims?
4.Have the criteria for the payment of settlements changed in a way which could adversely impact safe clinical care?
VALE CLINICAL PROFESSOR SAXON SMITH AM

CLINICAL PROFESSOR SAXON SMITH’S DEDICATION TO AMA (NSW), where he served as President from 2014-16, and his influential positions on numerous medical councils and boards highlighted his leadership in the medical community. He worked tirelessly to represent doctors and patients: he spent 6 years as the NSW and ACT representative on the AMA Federal Council, 16 years on the AMA (NSW) Council and 10 years on the Board of Directors of AMA (NSW), including chairing the board for 2 years.
“Saxon was a thoughtful, compassionate colleague,” said Professor Brian Owler, AMA (NSW) President from 2012 – 2014, with whom Professor Smith served as Vice-President. “He was always available to support the important work of the AMA and we shared a deep commitment to not just supporting the patient in front of us but patients everywhere. He was the embodiment of the values of the profession and the AMA.”
Dr Brad Frankum served as AMA (NSW) Vice President when Professor Smith was President, also serving as a fellow member
AMA (NSW) PRESIDENT 2014 - 2016
It is with profound sadness that we note the death of highly esteemed and much-loved former AMA (NSW) President Professor Saxon Smith, a distinguished figure in dermatology, who passed away at the age of 47.
of state and federal councils of the AMA. Dr Frankum said “Rarely in life do we meet people who are unique and special and when we do, we should be grateful. Saxon was one such person. He was always wise beyond his years. He was quiet and unassuming but very determined. He was comfortable with the success of others. Indeed, he helped many achieve it and was interested in other people’s lives. He was humble yet confident.
“Saxon achieved a great deal in a relatively short period of time.” Dr Frankum went on. “He rose to the top of his specialty, combining clinical and academic work seamlessly. He rose to the top of the AMA and was liked and respected by all. He dealt with media with aplomb. He was a tireless advocate. He was worldly but had a wonderful cynical sense of humour. I just had a smile looking back through many of the text messages we shared over the years about a range of things. A lump in my throat, too.
“Saxon loved his wife Camille and his son Eliot completely and was very proud of them. It is profoundly sad that he had such a short time with them. It is a terrible loss for them and for all of us who knew Saxon for him to be gone so young. He will be greatly missed but fondly remembered.”
AMA (NSW) President Dr Michael Bonning said “Saxon, more than anything was my friend. The foundation of our friendship was the profession of medicine and our work with the AMA but there was so much more to a friendship with Saxon. He was kind and energetic and selfless.

Prof. Saxon Smith is invested as AMA (NSW) President by his predecessor Prof. Brian Owler
“He was always available to support the important work of the AMA and we shared a deep commitment to not just supporting the patient in front of us but patients everywhere. He was the embodiment of the values of the profession and the AMA.”
PROFESSOR BRIAN OWLER, AMA (NSW) PRESIDENT FROM 2012 – 2014
“Dr Hamish Gray said at Saxon’s funeral, “His professional achievements are a matter of public record, but we know the man, who was always so generous and so kind with his time and his thoughts.” That sums up Saxon. Even though he was the one doing it tough, he religiously checked in on friends, remembered important dates and events, sent good luck messages for exams, commiserated over challenges and defeats, supported others who had their own serious diagnoses, and was always around to bounce ideas off – even answering the odd dermatology question.
“While he was receiving treatment at Royal North Shore Hospital I visited often. There I met a medical student Saxon had encouraged to come and see him for advice about a career in dermatology. Saxon looked beyond his own circumstances, to see a world of optimism and opportunity that he wanted others to enjoy and pursue.
“My fondest memories are of Saxon at home. He on the recliner, me on the sofa. Like Statler and Waldorf we always had something to talk about. Saxon loved to delve deep into issues, and we would spend hours talking about whatever meant something in that moment –his practice, pathology rents, the tennis, what friends were up to, what to do about COVID, what to do about lunch, Eliot’s rugby game, Camille and Saxon’s plans for a pool. Very little was said about his

FEATURE


cancer. What so many of us long for in such a time is to remain the main character in our own story. Serious illness can rob us of that centrality as it selfishly expands to fill the space available to devote to others. Saxon however managed to remain himself and instead expanded his life to ensure no-one was excluded by his cancer.
“Life without him will be difficult, but what I will carry forever is the magnificence of the way Saxon lived.”
During his tenure as AMA (NSW) President Professor Smith advocated for healthcare equity
“Life without him will be difficult, but what I will carry forever is the magnificence of the way Saxon lived.”
AMA (NSW) PRESIDENT DR MICHAEL BONNING
and spearheaded public health campaigns, notably in sun protection, where his research on sunscreen usage reshaped consumer awareness. He found many people were not aware that sunscreen had an expiry date, that it deteriorated when stored above 25 degrees, and needed to be reapplied after two hours.
His extensive research led to over 90 publications, earning him the Adrian Johnson Prize for his work on topical corticosteroid phobia. In 2019 he was admitted to the Roll of Fellows with the Australian Medical Association (AMA) for services to medicine and the association.
In 2022 he was awarded an Order of Australia AM in the general division for significant service to medicine as a dermatologist and researcher and to professional societies.
Professor Saxon Smith’s passing is mourned not only by the medical community but also by his family, including his wife Camille and his son Eliot. dr.
DONATIONS IN PROFESSOR SAXON’S SMITH’S NAME CAN BE MADE TO THE MEDICAL ONCOLOGY CLINICAL TRIALS, ROYAL NORTH SHORE HOSPITAL USING THE QR CODE HERE.

102-year-old

as a Doctor of Pathology. Images: supplied.

Health Hero
DR MONICA BULLEN
A former microbiologist, flight sergeant, tennis player, tai chi master and devout Catholic, at 102 Dr Monica Bullen is AMA (NSW)’s equal oldest member.
MONICA BULLEN WAS a brighteyed, post-war medical student at Sydney University when a senior doctor asked her, “Why do you want to become a doctor Monica? You have beautiful eyes, why don’t you just marry one?”
“This doctor clearly didn’t know Monica, or how determined she was,” Monica’s nephew Bernard Chapman told The NSW Doctor.
Growing up during the Great Depression, Monica was a gifted student, but funds wouldn’t stretch to allow her to finish school. After doing a secretarial course she took up a position at a printer.
Inspired by the exploits of pioneering Australian aviator Nancy Bird Walton, Monica co-founded the Australian Women’s Flying Club in 1938. Fascinated by aviation, with an eye on events in Europe, the women felt it important to learn to fly in order to make themselves available in the event of war.
Throughout her training Monica learnt aircraft operation and maintenance, navigation, meteorology, Morse code, signalling, aircraft recognition, armed and unarmed defence and other battle skills.
In 1941 Monica joined the Royal Air Force in the Women’s Branch known as the Women’s Auxiliary Air Force (WAAF), serving as a signal operator until the end of the war. Women did not serve on the front line, but

she hoped they could fill roles left absent by men.
“The Minister for Air very early on said that no WAAFs were going to go overseas. So, we knew whatever we did would be at home,” Monica told The NSW Doctor.
Monica used every bit of ingenuity to finish her high school diploma. “She was naturally gifted at maths so didn’t need much help,” her niece Monica Chapman recalls. “A family friend taught her French and for the other subjects my aunt, in her twenties, somehow learned these at a boys’ public school.”
That determination took her through to graduation as a doctor of pathology and an esteemed career as a microbiologist at Royal Prince Alfred Hospital.
“I always wanted to be a pathologist,” Monica said. “I loved the laboratory work.”
“I used to go and visit when I was a kid,” her niece said. “She used to tell me about these discoveries she’d made, and I could see how chuffed she was. I didn’t really understand what she had achieved I just know they made her so proud.”
Faith has always been important to Monica who until a couple of years ago attended mass every day. In later life she kept fit playing tennis, she mastered tai chi and continued Spanish lessons well into her nineties.
Asked on her 100th birthday the secret to a long life, she replied, “If you want a long life it helps to pick your genes well. My mother died at 101.” dr.
Inspired by the exploits of pioneering Australian aviator Nancy Bird Walton, Monica co-founded the Australian Women’s Flying Club in 1938.

Saving sleep saves lives… and a whopping 66 billion health dollars… so why isn’t the government doing more?
DEAD TIRED

Rahni Sadler chatted with Michael Mosley who participated in a clinical trial at Flinders University, documented in the SBS series Australia’s Sleep Revolution.


Q. What percentage of Australians suffer moderate to severe sleep issues and how much is it costing the Australian economy?
The estimate is 40% of Australians at a cost of $66 billion.
Q. As a society do you think we take sleep issues as seriously as we should?
Absolutely not. Individuals take it seriously because it affects them so badly but governments on the whole don’t prioritise it. They don’t see it as something that they should action or do anything about or indeed encourage ways of preventing insomnia.
Q. As compared to other severe health issues like smoking, diabetes and heart disease where does sleep fit in the degree of seriousness?
I think that sleep is one of the drivers of most of those chronic conditions. We know that if you aren’t getting
good quality sleep, then that massively increases the impact on your brain – anxiety, depression, it accelerates the risk of dementia, type two diabetes, hypertension. Sleeping less than six hours a night is associated with increased mortality risk.
Q. Why do you think sleep has fallen through the cracks?
I think it’s something we all kind of take for granted. One of the things I discovered making this series is that politicians seem to be enormously sleep deprived, so perhaps they regard it as a perfectly normal thing. The other thing is obviously that doctors and health professionals enter the profession and are often chronically sleep deprived themselves because they’re put through horrible regimes.
Q. What are the long-term implications of not taking action
to address sleep issues, not just for those who suffer from insomnia but for our health dollars?
The long-term consequences of not dealing with sleep issues are going to be humungous. I think that you are going to be paying the consequences of today’s inaction in the future. And that’s something that you hope would focus politicians’ minds.
Q. Do you think there is still work to be done in terms of the way doctors are rostered on?
Absolutely. I mean my hope is that it has improved a lot already. When we were part of the EU there were rules and regulations brought in to limit the hours that doctors in the UK can work, but to be honest an awful lot of doctors go outside those norms because they see it as important for their career and they can be hanging around the hospital for insane amounts of time.
Q. What advice do you have for doctors who work extraordinary hours or do demanding shift work? If you’re doing shift work, it’s important to bring healthy food with you. You might consider bringing a lightbox because when you’re feeling lonely, feeling tired, rather than drinking huge amounts of caffeine, one way to brighten yourself up is with exposure to bright light. Also watch out when you’re driving home because an awful lot of car accidents happen the morning after a long night shift.
Q. As practitioners do you think doctors have enough in their toolkit to deal with serious long term sleep issues?
Absolutely not. Unfortunately, doctors get very little training in sleep. The natural inclination is to prescribe medication (which is) good for dealing with short term distress but not for chronic long-term problems. Doctors are not equipped to
actually deal with insomnia, they don’t understand it, they don’t know how to treat it and they don’t have the time to treat it, which is why you need referrals to specialist sleep clinics and psychologists who can give you CBTI, but the trouble is there just aren’t very many of them. That’s because they’re not funded. My understanding is in Australia this treatment is expensive and therefore inaccessible to many people.
“Lack of sleep affects pretty much every system in the body and therefore it seems entirely logical to me that you would want to treat one of the primary drivers of ill health rather than just dealing with the consequences.”
Michael Mosley
Q. In your tv series the issue is raised that maybe we are treating things the wrong way round?
When I was at the Flinders Institute coaches said quite often, they find that people who came in with depression and anxiety, if you treat their sleep then the depression and anxiety go away. So, it can be more cost effective to treat the insomnia than to treat the depression and anxiety which anyway is quite often resistant to treatment.
Q. What advice do you have for the Australian government?
I hope that this documentary series will shame them into action or at least encourage them into action. You had this parliamentary inquiry held in 2019. You had this full report,
filled with recommendations –none of them implemented as far as I know.
Q. Can you tell us about the nature of the Flinders University trial?
The idea was 30 chronic insomniacs with a range of sleep problems and eight weeks for the Flinders team to try to sort it out. It’s a multidisciplinary team; psychologists, doctors, sleep scientists, technicians, data analysts etc. and what they want to do is create an effective program which can be rolled out, so it wouldn’t be dependent on having a specialised team, this was a kind of trial of concept if you like and the results as you will see in the series were just outstanding. I believe they’re planning to publish soon.
Q. When you say rolled out, it’s something people will be able to access easily?
It’s something that could be done online, which could support doctors delivering it. Initially it’s about the diagnostics then it’s about the delivery and then it’s about assessing the impact of the various interventions in a sleep lab. But once you’ve done all those things, you can start to put together a program which could be extremely cost effective, which could genuinely deliver a sleep revolution. dr.
Michael Mosley is a science presenter, journalist and executive producer. He studied medicine at the Royal Free Hospital Medical School. After graduation he became disillusioned with his chosen speciality, psychiatry, and joined the BBC. He is best known for his advocacy of intermittent fasting and low-carbohydrate diets. In 2021 he presented Australia’s Health Revolution for SBS, a series which helped eight Australians to reverse their type 2 diabetes with a lowcalorie diet and lifestyle changes.
HEALTH HACKATHON
Inspiring the next generation to tackle the health challenges of the future

OVER TWO JAM PACKED DAYS, the Prevention Education and Research Unit (PERU), Regional Industry Education Partnerships from the Dept. of Education, and the Ministry of Health hosted the inaugural Health Hackathon at Westmead Hospital. 27 students from Colyton, Erskine Park, Model Farms and Windsor High Schools participated in the event.
THE AIM: To upskill students through industry connections, broaden awareness of careers in health and empower students to develop a health education campaign on an issue of their choosing.

THE WINNER: ‘‘You Don’t Need Vapes to Have Fun!’’ by Model Farms High School, chosen for its simple yet effective approach in engaging young people and utilising infamous TikTok trends to raise awareness of the harms of vaping and denormalise it amongst adolescents.
“For vaping, it would be a reality check of what actually can happen to your body. Because a lot of people, they think that ‘Oh yeah it’s not going to happen to me.’” - Student, Model Farms High School
Feedback revealed a significant improvement in students’ understanding of the health industry, with many expressing a newfound interest in careers in health.
“It’s been great fun. I got to know a lot about things like AI, marketing, social media, what is behind what we actually see – what is behind the screen, and about NSW Health, and how much our government spends.” – Student
Feedback from school staff echoed these sentiments.

“They have learnt about different careers and roles available in the health system. They have learnt to work as a team to create and implement a campaign about a health issue that they feel is important” – Staff member
University of Sydney Faculty of Medicine & Health director, Professor Smita Shah said the Hackathon was a crucial step in preparing young minds to tackle the health challenges of the future.
“This is an example of how, when kids feel empowered and then really want to make a difference in our schools.” dr.
Catriona Lockett, Research Officer, Kym Rizzo Liu, Project Manager, Prof. Smita Shah OAM University of Sydney, Faculty of Med. & Health Dir.
NAVIGATING LIFE AS A NEWLY MINTED SPECIALIST

Anaesthetist Dr Katherine Jeffrey shares her journey into the world of anaesthetics.
HAVE YOU EVER HEARD OF THE “JULY EFFECT” or “Black Wednesday”? They are terms from the US and the UK respectively, which refer to the time of year when new medical graduates enter the hospital system. The theory goes that as the influx of new doctors arrives, medical errors skyrocket and patient outcomes drop. Despite the fact this so- called “July effect” has been debunked (1,2) the impression remains.
Day one of the medical new year brings not only new graduates but new consultants. They hit the wards, bringing fresh ideas and new skills, maybe from an interstate or overseas fellowship, to apply to new patients.
Consultants, be prepared for the stigma of the “July Effect”. On day one you become “the boss”, the person to call when the registrar cannot get a secure airway. Administration/ teaching duties are increased, and you face the regular diary check to remind yourself when you are on call. Learn to deal with new and tricky financial responsibilities.There’s a more complex tax return, MDO insurance, income protection and the first steps into home ownership.
Recognise that post-Covid, the employment market is very different. There are fewer staff specialist positions. VMO roles are considered the more flexible option and are increasingly the only option for employment in hospitals. There is now a known shortage of anaesthetists in the NSW public
system, particularly in the peripheral metro hospitals and regional/rural facilities. With the NSW Government Inquiry into Healthcare Funding and stories alleging price gouging by locum agencies(3) as well as the possibility of changes to the remuneration of NSW doctors, many are reassessing employment choices(4)
Even the private hospital system is no longer as attractive to anaesthetists. Private health insurers are capping payments to reduce costs and increase profits, and changes in the RVG (relative value guide) have led to the modification in remuneration for anaesthetists which many say is for the worse.
When you add other post Covid issues such as “Compassion Fatigue”(5), with many looking for a better work-life balance those first months can feel like a hostile journey.” dr.
Dr Katherine Jeffrey is a Consultant
Anaesthetist at Gosford Hospital (VMO) and a Staff Specialist at Nepean Hospital. Dr Jeffrey also works as a Medical Retrieval Consultant for CareFlight, NT.
Questions to ask yourself as a new consultant
Simple principles to help you navigate this large step, as a “newish” consultant (Year 4 out), other specialties and junior doctors.
• Whatlifestyleyouwant(part-time/full-time)? Family commitments
• VMOvsStaffSpecialist? Basically, contractor VS salary plus benefits including TESL, super and leave
• PublicvsPrivate?Think about responsibility, or as one colleague once explained, “with or without registrar” and the financial benefits
• Makelifeeasier.Payaprofessional.Tax, insurance, mortgage broker, cleaner, gardener, nanny
• Howmanyhospitalsdoyouwanttoworkin?
• Whaton-callcommitmentsareyouwillingtoaccept? Whodoyou wanttoworkwith?(Inanaestheisa,thatiscommonlyasurgeon.)Apoor relationshipwithasurgeonislikeabadmarriage
• Doyouwantapassionproject? Mine is Bridging the Gap and doctor education/welfare.
• CareerDiversiication Mine is RetrievalMedicine and Anaesthesia
• Willyoupayitforward?Teaching, administration, research, voluntary work, quality assurance, AMA advocacy, or in your professional college
• EducationColleges/professional organisations run courses on transitioning into consultancy
• DON’Tbeafraidtoaskforhelp.Youshouldneverfeelalone.
The journey into consultancy can be complex. However, if you plan, ask questions, do your research, use the resources available in all specialties, the transition will be smoother. For Katherine’s References, please scan the QR code.

THE DOCTOR IN R.M.WILLIAMS WILL SEE YOU NOW...

Here at The NSW Doctor, we pride ourselves on covering the issues big and small. This edition I’m hot on the trail of a mystery - when did it become mandatory for so many doctors to wear R.M. Williams boots?
MY INTEREST WAS PIQUED by a rumour that an unnamed neurosurgeon has a nine pair collection. Tucked away neatly, in order by colour, awaiting their turn on a fortnightly rotation. There are surplus sets for gardening and other household chores.
This sparked a very unscientific Instagram poll from the AMA (NSW) account which found 64% of participants voted yes to our question asking doctors if they wear RM Williams boots to work.

“The story of RMs for Australian doctors has been evolving for more than 20 years.”
Michael Bonning, President AMA (NSW)
Now let’s just get this straight. I’m not talking about in every medical workplace. Although RMs are no stranger to the operating theatre, from my observations it’s Crocs that reign supreme in there, followed by runners. Some of our members have professed to wearing Wellington boots. Whatever gets the job done.
Maybe there’s a clue in the latter choice of footwear. Easy to pull on and off and extremely comfortable.
I decided to do some qualitative research, or in other words, I started asking doctors “What’s with the RMs?” “When did it start?” “What do the colours say about the wearer?”
I didn’t have to go far. AMA (NSW) President Dr Michael Bonning is rarely seen without his RMs. He’s

been spotted addressing media conferences, presenting awards, attending meetings and seeing patients in his classy old RM boots.
He has even been photographed riding a bike in the hospital in them! (Okay – it was a stationary one) Dr Bonning tells us his current pair has lasted 22 years and they’re still going strong. “It’s simple” he tells me “Doctors love them because they are good boots and they have never let anyone down. The story of RMs for Australian doctors has been evolving for more than 20 years.” He goes on. “The trend was kicked off by male JMOs in rural hospitals and over the years has reached metropolitan hospitals across Australia.”
Asking around other doctors I find a range of responses. This one from a doctor at Royal North Shore Hospital “When I’m walking around
COLUMN
the hospital, I usually see about 70% of male doctors and 30% of female doctors wearing them. It’s about the time that doctors are on their feet and the support that their feet need.”
Another, from Blacktown Hospital tells me “Women have often worn ballet flats, but realistically it’s hard to wear them all day, your feet get too sore and there’s not enough support for the days moving around the hospital. The requirement of a closed toe shoe limits our options.”
This one comes from Dubbo. “We wear these boots because they are easy to throw on in the morning and easy for doctors who get a call during the night to come into the hospital immediately. The leather is flexible and durable for doctors who bend down to check on patients in hospital beds.”

Now, who wears what colour and why? I took my intrepid reporting into the world of DITS, and this is what one of our younger members told me “Doctors-in-training usually wear chinos, as they aren’t senior enough to be required to wear a suit. The chinos go much better with the brown boots. Consultants usually wear a suit in private practice and obviously black boots are the way to go with the suit.” dr.
Members can purchase a pair of RM Williams boots using the affiliate link in the member portal or by scanning the QR code on the left. The more RMs purchased by members through the link, the more likely we are to secure an exclusive discount code for our doctors.
Member Get Member
If you are a current member of AMA (NSW) you will receive an e-gift card for each new member you refer to join AMA (NSW).

As an AMA (NSW) member, for every new member you refer, we’ll reward you with a gift card. The more people you recommend, the more gift cards you’ll receive! Find out more at the QR code.

WORKPLACE RELATIONS
ARE YOU GETTING ALL YOUR ENTITLEMENTS AS A REGIONAL VMO?
A VISITING MEDICAL OFFICER (VMO) who is appointed to provide services at a regional hospital (known as a “regional VMO”) under the standard Fee-for-Service or Sessional Determination is entitled to additional entitlements over and above those who provide services at metropolitan hospitals. A list of regional hospitals is included in each VMO Determination.
VMOs who provide services at a Rural Doctors Settlement Package (RDSP) Hospital will be remunerated under the RDSP arrangements unless they also provide services at a regional hospital and choose to be remunerated under standard Fee-for-Service or Sessional arrangements.
Below we summarise the additional entitlements for regional VMOs under standard VMO Determinations.
Cancelled operating theatre time
Under the Fee-for-Service and Sessional Determinations, VMOs may be paid for cancelled operating theatre time where inadequate notice is provided. Payment will be made provided the VMO attends the hospital for the relevant period to attend to quality assurance and other activities unless excused from attending by the hospital.
A regional VMO (other than a sessional anaesthetist) can claim payment for the cancelled operating theatre time where less than 14 days’ notice is provided of cancellation. A regional VMO anaesthetist working
under a sessional arrangement can claim where less than 28 days’ notice is provided.
Call-backs Sessional arrangements
A VMO engaged under a sessional contract is paid for services provided pursuant to a call-back (whether rostered on-call or not) as follows:
a) services provided within the hours of 8.00am to 6.00pm Monday to Friday are paid at the ordinary hourly rate plus a loading of 10%;
b) services provided outside the hours of 8.00am to 6.00pm Monday to Friday are paid at the ordinary hourly rate plus a loading of 25%; c) services provided on a public holiday are paid at the ordinary hourly rate plus a loading of 50%.
A regional VMO engaged under a sessional contract will be paid a further loading of 10% on call-back services (whether rostered on-call or not) if the VMO’s usual place of residence is within a 50-kilometre radius of the regional hospital where the service was provided.
Fee-for-Service arrangements
Call backs (referred to emergency after-hours medical services) under Fee-for-Service contracts are those services initiated by the hospital for patients who require immediate treatment on a weekend, public holiday or outside the hours of 8.00am and 6.00pm on weekdays.
A VMO is remunerated for emergency after-hours medical services at the rate of 110% of the relevant fee payable under the contract.
A regional VMO will be paid 120% of the fee payable for an emergency after-hours medical service provided the VMO’s usual place of residence is within a 50-kilometre radius of the regional hospital where the service was provided.
Professional support
A regional VMO may claim a Professional Support Payment (PSP) of up to $15,000 (incl. GST) each year. Claims may be made for reimbursement of expenses which include (but are not limited to):
• Travel, accommodation, conference costs for CPD;
• Costs of locum cover while the VMO is on unpaid leave;
• Such other item/s in connection with the ongoing professional support of the VMO as the LHD/ Hospital may approve.
A regional VMO may claim reimbursement of up to $10,000 (incl of GST) each calendar year if the VMO:
1. has been continuously appointed at a regional hospital for the immediately preceding 12-month period; and
2. over the preceding 12 months at (at least) one regional hospital has under a sessional contract provided at least 450 ordinary and/ or call-back hours or under a feefor-service contract has provided services involving fees of at least $100,000; and
3. usual place of residence is within a 50-kilometre radius of (at least) one regional hospital where services have been provided.
WORKPLACE RELATIONS
A regional VMO may claim reimbursement of up to $5,000 (incl. GST) each calendar year if the VMO: 1.has been continuously appointed at a regional hospital for the immediately preceding 12-month period; and
2.has participated in a one in four or more frequent basis over the preceding 12 months in an on-call roster or emergency after-hours medical services roster; and 3.usual place of residence is within a 50-kilometre radius of (at least) one regional hospital where services have been provided. The PSP may be claimed each calendar year (1 January to 31 December) and accrues for up to two years.
AMA(NSW) review of the Determinations
AMA(NSW) has been in discussions with the Ministry of Health regarding amendments to the Determinations. The issues AMA(NSW) has raised with the Ministry include:
• indexing of the PSP which has not been increased since 2007;
• the payment of an appropriate loading where the experience of the junior medical staff at the hospital necessitates greater reliance on and attendance by the on-call VMO; and
• the payment of remuneration for services provided from home or elsewhere. dr.
AMA(NSW) encourages VMOs to familiarise themselves with their entitlements under the Determinations and to contact the AMA(NSW) Workplace Relations Team by email workplace@amansw.com.au or telephone (02) 9439 8822 . Please reach out to us if there are other changes you would like to see.
PERFORMANCE MANAGEMENT BEST PRACTICE
IT’S A NEW YEAR and a good opportunity to review current processes and establish best practice for performance management moving forward. Performance management can tie up a lot of time for Practice Owners and Practice Managers and it’s also one of the most common matters about which AMA (NSW)’s Workplace Relations team is asked to assist.
Set Clear Expectations
It’s important to set clear performance expectations as soon as possible, regardless of whether it’s for a new or current employee. Setting expectations puts you and the employee on the same page regarding what an acceptable level of performance may look like.
Informal Feedback
Build informal conversations into day-to-day work or have regular check-ins. This takes away any unnecessary formality and helps to make these conversations feel more natural.
Recognising and acknowledging good performance can be equally as valuable as addressing areas of concern. Communicating what your employee is doing well helps them feel valued, engaged, and encourages them to continue to perform those tasks at that level.
Identify any areas of improvement in their performance and address it as early as possible. The earlier you address it, the higher the likelihood that the concern will be resolved efficiently. Make it clear what is expected moving forward and
what the employee needs to do to reach this performance standard. Communicate how you will be supporting them and ask them if they would like any other forms of support. Helping them feel heard will encourage buy-in and motivate the employee to work towards a shared purpose.
It’s best practice to always document any conversations addressing underperformance for your own records in case you need to refer to these further down the track.
Formal Performance Management
Despite our best efforts, sometimes the employee continues to fail to meet the minimum acceptable standards of performance. There may be some variation in how you formally manage performance issues depending on whether your employee is within their minimum employment period (MEP) and how much more opportunity you are willing to give the employee to improve. MEP is the minimum length of employment the employee needs to be employed for before they can access an unfair dismissal claim if terminated. The MEP is 6 months (or 12 months if the business has less than 15 employees).
Within MEP
You may wish to place the employee on an informal coaching plan, or depending on the extent of their underperformance, you may wish to terminate. There is no requirement under the Fair Work Act (FWA) to provide a reason when terminating an employee.

WORKPLACE RELATIONS
However, we strongly recommend providing a reason in writing as to why they are being dismissed to mitigate risks around adverse action claims (claims an employee can submit when they believe they have been unlawfully terminated). This is because there is no length of service requirement for an employee to access adverse action claims.
Outside of MEP
Under the FWA, employers are required to afford procedural fairness and justify the outcome when it comes to disciplinary processes. This includes providing notice, affording the employee the opportunity to bring a support person to the meeting, giving a reasonable timeframe for them to consider their responses, and considering their responses before determining an outcome. There must be evidence and documentation throughout a formal disciplinary process and the outcome must be proportionate to the degree of underperformance and other factors. The outcome for a first formal disciplinary process around underperformance could be a warning and a formal performance improvement plan (PIP), for example.
No One Size Fits All
Speak with our Workplace Relations team so you can receive tailored advice and templates for your employee’s situation as there are several considerations and risks to consider. dr.
The AMA (NSW) Workplace Relations Team is available anytime to help members at no extra cost. Contact us at workplace@amansw.com.au or on (02) 9439 8822.Please email workplace@amansw.com.au or call (02) 9439 8822.
OFFSETTING
AWARD-COVERED EMPLOYEES, including private practice support staff, health professionals, and nurses are entitled to overtime, penalty rates, loadings, and allowances in certain circumstances.
‘Offsetting’ describes the practice of paying an employee a flat contractual rate higher than the award minimum for all hours of work, set at an amount intended to cover the employer for those extra award payments.
Otherwise known as ‘setoff’, offsetting is popular as it streamlines payroll processes. However, there are some important considerations to be aware of to make sure the practice is meeting its minimum obligations and to limit the risk of any underpayment claims.
Is it possible to offset?
Off-setting is normally fine, as long as:
a)The employee is still receiving overall at least what they would under the award;
b)The employment contract contains an appropriate offset clause;
c)The employer keeps accurate time and wages records for all hours worked.
How do I make sure the employee is still receiving what they would under the award?
It’s important not to ‘set-and-forget’ above-award rates. While it’s not required to check every pay period,
the smaller the difference between the flat rate and the award rate, or the more overtime, weekend, and public holiday work the employee performs, the more frequently you should check that you’re meeting your minimum obligations.
To do this, compare the minimum award entitlements for each hour worked to what the employee was actually paid over a particular pay period.
For example, let’s say you pay a part-time Level 3 receptionist under the Health Professionals and Support Services Award (HPSSA) a flat $32/hour. The employee works 20 hours a week, comprising two 6-hour shifts on Monday and Tuesday (12 hours), and 8 hours on Saturday.
As at the time of publication, the minimum rate for a Level 3 is $25.88 and the Saturday penalty rate is $38.82.
For the week, the employee was paid $640 ($32 x 20). The total award entitlement was $310.56 ($25.88 x 12) plus $310.56 ($38.82 x 8), which equals $621.12.
As you can see, the $640 is greater, so no extra payment would be required.
However, if that employee had picked up an additional overtime shift, or the Monday was a public holiday, it’s likely the flat $32 would no longer be sufficient. In that case the practice would be liable to backpay the employee the difference between what was paid and the total amount owed under the award.
This is one of the reasons why it’s important to keep accurate time and wages records for all employees.
WORKPLACE RELATIONS
Overtime and penalty rates aren’t the only award obligations to consider, there are also shift loadings, annual leave loading and specific allowances that may apply.
AMA (NSW)’s Workplace Relations Team can also help you check that you’re offsetting correctly.
What does the employment contract need to say?
The contract should stipulate for what purpose the flat contractual rate is paid.
It’s very important to get the wording right, so our AMA (NSW) template contracts include a model offset clause which we provide to members at no extra cost.
The Federal Court recently held that where an employment contract didn’t have an appropriate offset clause, the business was required to backpay the employee to the minimum award overtime rates for overtime worked, despite the fact the employee had already been paid more overall.
Overtime and penalties can range from 150% to 250% of the minimum rate in the HPSSA and Nurses Awards, so it’s important to have a carefully crafted clause in place in your employment contracts if you want to offset lawfully.
What about annual leave loadingcan it be offset?
Both the HPSSA and Nurses Awards stipulate that during a period of annual leave, employees are entitled to annual leave loading, (normally 17.5% of the minimum rate for their classification), on top of what they are ordinarily paid.
Some practices who offset do include the annual leave loading
in the flat rate (in other words, they pay the same rate during periods of annual leave).
However, technically under these Awards, annual leave loading should be paid on top of the ordinary pay. Therefore, we advise that annual leave loading should not be included in the flat rate.
Let’s go back to our example of the Level 3 receptionist on $32/hour. 17.5% of the minimum award rate ($25.88) is $4.53. Adding this on top of the ordinary pay ($32), we get $36.53. This would be the minimum annual leave loaded rate.
What if I pay an annual salary instead of an hourly rate?
The HPSSA award allows Support Services employees at Levels 8 or 9, and Health Professionals at Levels 2,3 or 4 to be paid an annualised salary that includes entitlements such as overtime, penalties, and annual leave loading. In these circumstances it’s possible to avoid having to pay an extra amount during annual leave.
Annualised wage arrangements don’t apply to Support Services employees classified Level 7 or below, so won’t be available for most reception staff. There is no annualised wage arrangements clause in the Nurses Award.
Are there any other options to avoid paying extra during annual leave?
Both awards allow Individual Flexibility Arrangements (IFA’s) to be entered into, which are written agreements between employee and employer that change how certain clauses apply. For example, stipulating that annual leave loading doesn’t apply.
There are significant drawbacks with IFA’s. They can’t be included in the initial offer/contract of
employment and can only be negotiated separately after the employee starts. An employee can also unilaterally withdraw from an IFA with 13 weeks’ notice.
The agreement also needs to leave the employee better off overall than they would be if the agreement wasn’t made and “meet the genuine needs of both the employee and employer”. Clause 5 in each award sets out all the requirements for IFA’s.
What’s the best option?
In most cases, the simplest option for the practice, while still adhering to all requirements would be to -have an appropriate offset clause in the employment contract; -periodically check that the employee is still receiving at least what they would under the award, as needed, and; -pay annual leave loading separately.
It’s also important to keep abreast of minimum award wage increases as they occur. dr.
Our Workplace Relations Team can talk through your particular circumstances and provide any template resources you require. For more information, please email workplace@amansw.com.au or call (02) 9439 8822
VOICE OF THE PROFESSION
By maintaining a strong and ongoing presence on mainstream and social media AMA (NSW) ensures that the association remains firmly at front of mind as the state’s peak body for doctors. We’d like to thank all the doctors who have contributed to our media coverage in recent months.




Bureau of Health Information quarterly figures released in March showed record demand on the state’s health system in the period between October 1 and December 31. Dr Michael Bonning was quoted widely on tv, radio, print and online reiterating the message that an urgent injection of funds is needed in the upcoming budget to save our crumbling health system.

AMA President Professor Steve Robson was quoted in The Australian calling for an independent body to conduct a review of the remuneration arrangements between private health insurers and private hospitals to ensure the viability of the sector.

Dr Bonning reminded patients on tv and radio to keep up regular GP checks and not to rely solely on advice from pharmacists as the pharmacy-prescribing trial is expanded in NSW.

Lismore general surgeon Dr Sue Velovski spoke on behalf of AMA (NSW) to James Valentine on ABC 702 to mark the second anniversary of the devastating floods in her area. Dr Velovski made some strong points about the need for greater government support for health providers, particularly GP practices in the wake of natural disasters.


Across the media Dr Bonning again explained that the health system is log jammed because there are not enough resources being provided to deliver the surgical care people need and that funding ratios between state and federal governments need to be fixed.
Dr Bonning was asked to discuss the rollout of an RSV immunisation for infants in WA and calls for other states to follow.


The AMA called for restrictions on social media posts pushing a harmful message about tanning. The messaging harks back to the bad old days of using sun tanning accelerators and false claims that sun exposure and tanning are healthy.


In the Sydney Morning Herald Dr Bonning commented on the appointment of a 20-member panel to guide the Special Commission of Inquiry into Healthcare saying he would have liked to have seen more perspectives from frontline health workers.


As February rolled around Dr Bonning did a series of interviews on payroll tax which drew this response from Premier Chris Minns who, as reported in The Daily Telegraph called additional payroll tax charges on GPs “a massive new tax”. The premier stated “We’re having good conversations with those organisations and peak bodies and we’re going to make sure that bulk billing and GP access by the general community is available to the people of NSW.”
Over summer Dr Bonning spoke about a spike in mycoplasma pneumonia or “Walking pneumonia”. High rates of ED admissions for children with pneumonia was addressed again in February in The Sydney Morning Herald (SMH).



Vaping is an issue Dr Bonning addressed in the media and at state and federal inquiries.

Western Sydney GP Dr Kean-Seng Lim spoke on ABC News Breakfast about bulk billing and the shortcomings of Medicare.


On Channel Nine fellow Western Sydney GP Dr Ken McCroary reassured Sydneysiders that the risk of contracting asbestos related health complications from mulch was low.


Anaesthetist Dr Katherine Jeffrey was quoted on behalf of AMA (NSW) in The Daily Telegraph in relation to new ED wards at Nepean and Prince of Wales hospitals for patients under the influence.

AMA (NSW) President Dr Michael Bonning joined forces with the Road Trauma Support Group for a highly successful campaign picked up by all major media called “Speak Up and Step In to Save Lives”. The campaign urged everyone to step in and stop a drunk/impaired/tired driver before they get in the car.
AMA (NSW) is always looking for informed spokespeople. If there is a subject on which you feel confident to be called on to speak about please email magazine@amansw.com.au

It has been a busy few months at AMA (NSW). Here’s a recap of some of the information we’ve conveyed via email & press release.
Special Commission of Inquiry into Healthcare (SCOI)
In November we provided members with an update on the SCOI including a link to the terms of reference and AMA (NSW)’s initial submission. AMA (NSW) President Dr Michael Bonning thanked the nearly 1000 doctors who responded to our workforce survey which informed our initial submission and will help inform future submissions. He also informed members that AMA (NSW) Director of Workplace Relations Dominique Egan, was working with HWL Ebsworth lawyers in coordinating our response.
In December, the President updated members on the new SIRA guidelines which give SIRA broad powers to regulate doctors and other health providers. AMA (NSW) has concerns about these guidelines and communicated this to members, providing access to the submissions on the matter. All members were invited to the SIRA Regulatory Framework Briefing on 14 March 2023.
AMA (NSW)’s Workplace Relations team continued to brief specific members such as VMOs, Staff Specialists, Doctors-in-Training and Practice Managers. In December we notified VMOs of the upcoming Re-appointments, provided further information on VMO Determinations as well as an update on the SCOI.
A subsequent update on the topic was emailed early this year.
The Practice Managers Newsletter in December recapped a busy year in the industrial relations space, including updates to the new workplace sexual harassment positive duty laws and fixed term contract changes. In February 2024 updated information on the ‘Changing Loopholes’ No. 2 Bill was provided. These resources are available in the AMA (NSW) members portal. If you are a Practice Manager and not receiving these updates, please email us at magazine@amansw.com.au.
Our Doctors-in-Training (DITs) Committee Co-Chairs Dr Sanjay Hettige and Dr Jacqueline Ho have kept up regular content via email and social media on issues that directly impact DITs.
AMA (NSW)’s loyal media connections are engaged through regular media releases. In March AMA (NSW) demanded an urgent injection of funds in the upcoming state budget after BHI figures indicated record demand on the NSW health system. In February, we reiterated concerns about the impact of cuts on palliative care services, calling for funds to be restored in the budget. AMA (NSW) also congratulated Australians of the Year Professor Georgina Long
and Professor Richard Scolyer. In December AMA (NSW) renewed calls for the Commonwealth Government to remove the exclusion of telemedicine, emails and phone calls from laws relating to Voluntary Assisted Dying, and launched the Road Safety campaign titled ‘Speak Up and Step in to Save Lives’, in partnership with Road Trauma Support Group NSW.
One of our most successful forms of communication is our fortnightly ‘Feel Good Friday’ newsletter that not only showcases the fantastic commercial partnerships that benefit AMA (NSW) members it also includes important AMA news and events, a noticeboard, a fortnightly Health Hack as well as the most laughable social media medical misinformation. dr.
We want to make sure our valued members are receiving all the information they need, so send us an email at: magazine@ amansw.com.au to let us know what you want to hear more about.
EVENTS
UNLOCKING KNOWLEDGE AND CONNECTION

Starting

Starting Private Practice Masterclass
“Really great content from AMA (NSW)
AMA (NSW)’s Unlocking Knowledge and Connection Event was held at Pullmans Hyde Park, Sydney, over the weekend of 16 and 17 February 2024 three events; the Practice Managers Masterclass, a Starting Private Practice Masterclass and a Member meet Member evening.
The highly popular Practice Managers Masterclass teaches practice managers the skills, tips and tricks vital to running a successful practice. It’s presented by AMA (NSW)’s Workplace Relations team and includes presentations from Tyro Health, Cutcher & Neale and HWL Ebsworth.
Doctors looking to start their own private practice as well as those
speakers,
I definitely will be reaching out for more expert guidance. Extremely delicious food and drink options, my money was very worthwhile.”
Practice Managers Masterclass, Sydney



Member meet Member evening
“All presenters were engaging and informative. All topics were relevant and current, thank you AMA (NSW), well worth attending.”
looking to streamline practices joined AMA (NSW) for The Starting Private Practice Masterclass. Participants heard from our professional legal and WR team on a range of topics including tax, billing, employing and managing staff as well as a cyber security presentation from Aparna Sundararajan of Cyber CX, Scott Chapman Partner at HWL Ebsworth Lawyers and Stuart Chan Partner at Cutcher & Neale. Doctors and practice managers engaged in a panel Q&A with Dr Kathryn Austin, AMA (NSW) Vice President and Obstetrician and Gynaecologist, and AMA (NSW) Member and Psychiatrist Dr Namrata Shetty.




EVENTS
ORIENTATION WEEK 2024










THE AMA (NSW) TEAM toured hospitals across the state during 2024 Orientation Week for first year Doctors-in-Training.
The team of Workplace Relations Advisors outlined the many benefits available to members and provided recruits with guidance on topics including payslips, leave entitlements and remuneration.
The team visited nine hospitals, including Westmead Hospital, Sydney Local Health District, St George Hospital, Liverpool Hospital, Wollongong Hospital, Tamworth Base Hospital, John Hunter Hospital Newcastle, Tweed Hospital and Bankstown-Lidcombe Hospital.
Doctors-in-training were offered free scrub caps when signing up and entered into a raffle to win free membership, a $100 gift card or a $50 gift card. They were also provided with resources including the new DIT Pay Guide. The lucky prize winners have been contacted! dr.

THE JOINT MEDICAL PROGRAM is a two-stage five-year program comprising of a Bachelor of Medical Science (stage one) and Doctor of Medicine (stage two), offered jointly in partnership by the University of Newcastle and the University of New England (UNE). Dr Madeleine de Carle was awarded the prize for topping years four and five.
Dr de Carle said “I worked really hard. It’s always been really important to me from a patient perspective that I learn as much as possible, but I was quite surprised I achieved the highest results given I was in a cohort of incredible people who also worked really hard”.
Dr de Carle was the first (UNE) student to win the award which she says is testament to the Armidale medical school and the work that is put into developing their clinical school.

EVENTS
CONGRATULATIONS TO DR MADELEINE DE CARLE, THE RECIPIENT OF AUSTRALIAN MEDICAL ASSOCIATION (NSW) LIMITED PRIZE FOR THE JOINT MEDICAL PROGRAM

Growing up in Sydney Dr de Carle cites as her inspiration her mother Larissa, a vet and her “pop” David, a gastroenterologist. “For me medicine was the perfect mix between spending time with people and doing maths and science. I didn’t get into medicine straight away but I was able to work hard and get in eventually thanks to the joint program.”
Dr de Carle is a strong advocate for the AMA “I’ve been involved with the AMA (NSW) from the end of medical school and at the beginnings of being a JMO. I am now a part of the doctors-intraining committee. It’s great to see the advocacy work that you guys are doing for JMOs, it has been wonderful to see and it has definitely been felt on our end from myself and my colleagues.”
“Thanks so much to AMA (NSW) for the $1000 prize. It absolutely useful; I have travelled around for regional and rural rotations, so it has really helped with the finances and transport to those rural towns.” dr.



You can find a more comprehensive list of benefits and more information at www.amansw.com.au or email members@amansw.com.au



























Join AMA (NSW )
As the state’s peak medical-political lobbying body, AMA (NSW) is dedicated to providing its members with representation on a variety of medical issues, workplace relations advice, representation and commercial benefits.
Members of AMA (NSW) also belong to Federal AMA, which is consistently ranked among the nation’s most effective and trusted member organisations.
The strength of AMA (NSW) lies in its representative reach across the state’s geographical zones and the profession’s specialty groups. By playing a pivotal role in the formation of public health and hospital policy, AMA (NSW) is in a strong position to represent the individual needs of members and their patients.
“The AMA has always supported my dream, and supported equity and justice. The AMA is an important voice for doctors, patients and our health profession. Importantly, the AMA provides individual assistance and support to doctors when they most need it.
That’s why I’m a member.”
Professor Kelvin Kong
PROFESSOR KELVIN KONG Worimi, ENT Specialist, AMA (NSW) Member
Support us to support you. Scan the QR code to join us today!

