In this issue:
• NOT GOOD ENOUGH – BULLYING STILL A HEALTH HAZARD FOR DOCTORS IN TRAINING
• CONCUSSION COMPLEXITIES – HOW DOCTORS CAN MINIMISE THE LONG-TERM DANGERS OF SPORTS-RELATED CONCUSSIONS
• THE MAGIC AND MYSTERY OF THE AMA(SA) GALA BALL
• ADVOCACY AGENDA – WINS AND WISHES IN THE FEDERAL AND STATE BUDGETS

WINTER 2023 VOLUME 36 NUMBER 2
With more clinics across the state,
you’ll get a clearer picture.
OPENING SOON
Bringing MRI to the Fleurieu
Victor Harbor Town Centre
Adding to our existing clinics at Goolwa and Victor Harbor Hospital, this expansion of our radiology services creates capacity on existing services and allows us to bring Medicare supported MRI and Breast imaging services closer to those who live on the peninsula.
New Breast & Oncology Clinic


337 South Terrace
This is an expansion of our relocated breast services provided at St Andrew’s Hospital as well as a focus on oncology imaging and integrated healthcare making the patients journey as comfortable as possible.
For a clearer picture visit jonesradiology.com.au
medicSA is produced by the Australian Medical Association (SA)



Australian Medical Association (South Australia) Inc.
Level 1, 175 Fullarton Road, Dulwich SA 5065
PO Box 685, Fullarton SA 5063
Telephone: (08) 8361 0100
Email: medicsa@amasa.org.au
Website: https://www.ama.com.au/sa
Executive contacts
President
Dr John Williams: president@amasa.org.au
medicSA
Editorial
Medical Editor: Dr Roger Sexton
Editor: Karen Phillips editor@amasa.org.au
Advertising medicsa@amasa.org.au
Production
Catherine Waite
ISSN 1447-9255 (Print)
ISSN 2209-0096 (Digital)
Cover Dr Michelle Atchison welcomes Dr Williams as our new President. Photo - Brett Sheridan
Disclaimer
Neither the Australian Medical Association (South Australia) Inc. nor any of its servants and agents will have any liability in any way arising from information or advice that is contained in medicSA. The statements or opinions that are expressed in the magazine reflect the views of the authors and do not represent the official policy of the Australian Medical Association (South Australia) unless this is so stated.
Although all accepted advertising material is expected to confirm to ethical standards, such acceptance does not imply endorsement by the magazine.
All matter in the magazine is covered by copyright, and must not be reproduced, stored in a retrieval system, or transmitted in any form by electronic or mechanical means, photocopying, or recording, without written permission. Images are reproduced with permission under limited license.
AMA(SA) Doctors in Training Chair Dr Hayden Cain added ‘media spokesperson’ to his resume when the latest Hospital Health Check was released on 2 June. Dr Cain joined AMA(SA) President Dr John Williams in explaining to journalists the ‘unacceptable’ rates of bullying and witnessed bullying that continue to plague junior doctors in South Australia’s public hospitals. Dr Cain relished the opportunity to take important DiT advocacy into the public sphere via television cameras - his comments on the HHC results for the print media begin on page 20.
medicSA | 3 5 President’s column 6 Medical editor’s column 8 View from the top – new President Dr John Williams outlines a vision for his presidency 10 Under lights – awards, rewards and the AMA(SA) Gala Ball 12 Council news 13 AMA(SA) CEO moves on 17 Advocacy – our State Budget priorities 18 Advocacy – wins and questions from the Federal Budget 20 Much to do – Hospital Health Check results and commentary 23 Sock it to ‘em – news and views from the Crazy Socks for Docs Breakfast 28 More than a bump to the head – the latest research on concussion and CTE 32 Criteria for care – redesigning the principles for optimal recovery 36 Research briefs 40 On the trail of Flinders – an AMA(SA) Life Member examines the history of medical education at Flinders University 42 Student news 46 Magic and mystery – images from the AMA(SA) Gala Ball
Motoring – Dr Robert Menz takes on a big Toyota
Vale – remembering Dr Rosie Jones and Dr Peter Wells Contents
50
52
More reasons to switch

medicSA | 4
Quality cover that delivers value Whether it’s just for you or for you and your family, you can rely on our hospital and extras cover when you need it most. Service that puts you first You’ll be supported by a team that understands you and your profession. With a member satisfaction rating of 96% in 2023; you’re guaranteed to be our priority. Benefits up to the AMA list With AMA rates on Top Cover Gold hospital and no preferred providers, your needs will be protected as both a patient and a practitioner. SWITCH IN 2 EASY STEPS Choose the hospital and extras to suit your needs – we can provide a comparison with your existing fund 1 Apply online in 5 minutes or apply over the phone 2 Health cover designed for doctors
Already a member of Doctors’ Health Fund? Share the benefits of a community health fund Refer your eligible friends & family and you’ll each receive a $100 eGift Card when they join* Refer a friend www.doctorshealthfund.com.au/ refer-a-friend Join today 1800 226 126 doctorshealthfund.com.au * Refer a friend full terms and conditions doctorshealthfund.com.au/refer-a-friend IMPORTANT: Private health insurance products are issued by The Doctors’ Health Fund Pty Limited ABN 68 001 417 527, a member of the Avant Mutual Group. Cover is subject to the terms & conditions (incl. waiting periods, limitations & exclusions) of the individual policy, available at www.doctorshealthfund.com.au/our-cover. DHF 373_6/23
Dr Arany Nerminathan Member since 2018
President’s report
Dr John Williams

There are many doctors who have had much to thank Dr Chris Moy for over the past few years – years in which the advocacy and profile of the former AMA(SA) President and AMA Vice President have influenced policies and decisions at the state and national level, and made a real difference to how we’ve practised medicine and provided care during the pandemic.
I have more for which to thank Chris and our CEO at AMA(SA), Dr Samantha Mead. It was Chris and Sam who launched the campaign that led me to the vicepresidency and now presidency of AMA(SA). They overcame my ‘why me?’ doubts and eventually persuaded me to think ‘why not me?’.
It apparently is a first, having a regional doctor at the helm. Certainly it adds a layer of complexity in having the President available to join the many meetings and media appearances that are scheduled for and pop up in the diary of that person each month. But if there is anything positive that’s emerged during the pandemic it’s the understanding that we don’t have to be physically in the room for many of the tasks common to medicine, business and social interactions, and the role of technology in enabling other ways to meet, treat and engage. Scheduling a last-minute meeting with an AMA member or rearranging an appointment with the Minister isn’t the arduous task it once was. TV journalists may not like interviewing me on Zoom but they (usually) accept it. Videos and on-screen presentations can be shared with me in my rooms in Port Lincoln as easily as if I was joining a face-to-face taskforce in Hindmarsh Square. And, of course, we all know the contribution telehealth has made to managing our time and our patients’ needs over the past three years.
Of course, I will be visiting the city, regularly and often. AMA(SA) Council and Executive Board commitments are among those that cannot always be fulfilled appropriately in online gatherings. I could not participate in the State Budget lock-up on 15 June unless I took a physical seat. And the handover of the President’s Medal from my predecessor, Dr Michelle Atchison, to me required my joining Michelle, Sam and 150 colleagues at the AMA(SA) Gala Ball on 20 May. The Ball
marked my public ‘debut’, and that of our new Vice President, Associate Professor Peter Subramaniam, and we were honoured to have so many friends with us.
If the Ball was Peter’s and my ‘comingout party’, the Season is now in full swing. I was pleased to attend (in person!) the Crazy Socks 4 Docs Breakfast on 2 June and join the Chair of the Doctors in Training Committee, Dr Hayden Cain, to launch the 2022 Hospital Health Check later that morning. There is significant overlap between the two: the HHC survey demonstrates that junior doctors continue to be bullied and to bear other workrelated burdens that are unacceptable in 2023, and the result is often the type of mental health issue discussed at the breakfast. We must do better if we want bright, talented and dedicated people to be doctors and to lead the profession in the years ahead. Please read Hayden’s summary of the HHC survey results on page 20, and turn to page 23 for more Crazy Socks.
Otherwise, I continue to be involved in the development of a single employer model that achieves the AMA’s objectives for the future of general practice. It is heartening that partners in both levels of government and the local health networks can see the importance of this if we are to attract and retain junior doctors in general practice. I hope to bring an update in the next issue of medicSA
Similarly, we continue to advocate for limits on ‘scope creep’ and against any new interpretation of payroll tax legislation, both of which have immediate and longer-term implications for our capacity to care for patients and for the quality of care they can and will receive.
Finally, for now, I wish to thank Michelle for her leadership and for bringing me with her to this point; for Peter, AMA(SA) Council, the Executive Board and the AMA(SA) staff for all they have done and will do to support me; and for everything Sam has done for us during her four years as CEO.
As I said at the Gala Ball, I am determined that when you hear me speak in the next two years, you will hear your own voice. Please let me know your thought and concerns – I am your President.
medicSA | 5
UPFRONT
We must do better if we want bright, talented and dedicated people to be doctors and lead the profession in the years ahead.
From the medical editor
Dr Roger Sexton

Health is a battlefield.
Over the past few years, the health sector has experienced more examples of competitive inter-professional behaviour, such as with pharmacy, nursing and other allied health providers. The discourse has not always been flattering. It erodes trust and appears to our patients as self-interested. It may also contribute to suboptimal health care.
The argument for increased scope and autonomy usually centres on the presence of a clinical service vacuum created by over-burdened medical professionals who ‘need help’ because the community’s expectations for timely, convenient access to a doctor are not being met. Other health professionals sense an opportunity and step in to respond. The public respond positively, in the setting of a cashless society attuned to the Uber-eats model and expectations of immediacy and convenience.
But the public should be concerned about the (possibly) cocky and (probably) naïve health professional who may assume their undergraduate and post-graduate training gives them transferable ‘medical’ skills of a standard approximating that of their medically trained colleagues. But the equivalency of these other health professionals’ examination skills, pattern recognition, differential diagnosis, prescribing, special test ordering and interpretation should not be accepted without question. Trials of extended scope practice may have had a pre-determined outcome and may have been too readily accepted by politicians and the public as evidence of safe practice. The proposed pharmacy prescribing of the oral contraceptive, for example, warrants robust and independent scrutiny.
With patient safety at the heart of this, the statutory obligations of Ahpra and the relevant professional board to protect the public firmly sit in this space.
You will be aware of the trend in clinical product advertising that now proclaims, ‘If pain persists, see your health professional’. The public may have come to believe that diagnostic equivalency with a doctor is indeed true. Home delivery, Amazon, telehealth services, Dr Google, entrepreneurial internet-based ‘medical’
services and self-diagnostic online tools have all altered the health access landscape, too.
Other health professions seeking to increase scope of practice are responding to a need that we have not always been able to meet. We must acknowledge this and that time, case complexity and volume and infrastructure limitations in medical practice have contributed to this.
Meanwhile, the gap in service provision has become the perfect stepping-stone for others to progress their career, scope and business ambitions. The message here must be to tread very carefully’. With scope comes responsibility, accountability and high cost ‘med-mal’ insurance.
We must advocate for our own profession to develop its scope and capacity to meet patients’ needs. General practice has huge potential to do so but has been constrained by chronic bipartisan disinvestment in the sector. The opportunity exists to lead and engage more closely with other health professionals with enhanced scope within general practice. We can ‘grow the pie’ through innovation, solving patient health problems in a timely way and addressing health system problems such as ramping. This will drive a reallocation of resources to where they have the most impact.
Doctors who are life-long learners and work to and within scope are more satisfied professionally. As teachers, doctors can all contribute to improving the scope of practice of the others in our team without competition and work cooperatively with external health professionals for the benefit of patients.
Imagine where IT, remote monitoring, personalised medicine, overnight stay general practices, outreach home care, preventive health care can take us and what expanded roles are needed to achieve this. ‘Growing the pie’ increases everyone’s share through enhanced scope of practice, remuneration, capacity building, status, impact and influence. We solve more problems, improve our service to our patients, and secure the future of our profession.
medicSA | 6
UPFRONT
We can ‘grow the pie’ through innovation.


medicSA | 7 Avant, leading protection and support when it matters most Join today avant.org.au/practitioners 1800 128 268 IMPORTANT: Professional indemnity insurance products are issued by Avant Insurance Limited, ABN 82 003 707 471, AFSL 238 765. Please read the relevant Product Disclosure Statement or policy wording, available at www.avant.org.au before deciding whether to acquire, or continue to hold the product. *Accurate as at 30/06/2022. MJN1033 04/23 (DT-2889) Award-winning defence Our over 300-strong* medico-legal defence team provides you with on-the-ground support across Australia. Comprehensive support Access our medico-legal experts, 24/7 in emergencies, and risk advisers. As well as a comprehensive library of online medico-legal resources. Dr Mark Green Avant member Australia’s most popular medical indemnity insurer, covering over 50% of doctors
At your service
After beginning with sincere thanks to his predecessor, Dr Michelle Atchison, new AMA(SA) President Dr John Williams gave his Gala Ball audience an overview of what brought him to medicine and his vision for his presidency.



Across the country, the AMA and its members – like our clinical peers around the world – have been trying to do what we do in the face of perplexing, unfathomable resistance. It is one of the most complex, fractious, and frustrating periods in our history – and probably in medical history.
I’d like to acknowledge the moral injury that has emerged and afflicted us - a pain inflicted by working in a health system that at times hobbles our ability to deliver the best care that could be given with our current medical knowledge.
There has been immense pressure placed on and carried by health workers in clinics and hospitals and practices, residential facilities and homes. But we have pulled together and maintained our commitment to working with each other and with our colleagues, for each other and for our patients.
Who is John Williams?
I am the son of a farmer Gilbert from Brown Hill Creek then Angle Vale then Ungarra on the Eyre Peninsula, and Kay, a mid-wife, who worked in Cummins on the Eyre Peninsula.
I was encouraged to apply for university but was very surprised when I achieved to marks to enter medicine, and graduated from the University of Adelaide in 1993.
I worked at various metro hospitals, before returning to the University of Adelaide, this time to study music, a long-term interest that brings balance and creativity to my life.
I worked in various places around South Australia, including Strathalbyn, Woomera and metro Adelaide, achieving my GP fellowship along the way. I then spent three years in the UK, in hospitals and general practice.
We moved to Port Lincoln to care for my wife’s father who had a terminal illness, and soon discovered we had a child on the way. Port Lincoln has been a wonderful place to raise a child – beautiful surrounds, a less than five-minute commute and lovely schools.
During my 18 years in Port Lincoln I completed a masters of medicine in skin cancer management in Queensland.
My main professional interests are acute medicine, palliative and aged care, and skin cancer diagnosis and treatment.
Rural medicine really is in quite a state, demonstrated by small communities such as Streaky Bay where the local town council –usually involved in trash and road repairs – has stepped in using rate-payer funds to supply GP services. This really is market failure.
It’s in a regional area where you can clearly see the importance of the three pillars of practice: patient contact, which is the core and informs everything else; teaching and training; and research. You see how essential they are, how they work together to improve treatments and outcomes. You see the importance of building a positive culture of support with a team, skill improvement through self and other education, and empowerment through improving care, every day.
medicSA | 8
FEATURE
New President Dr John Williams, Immediate Past President Dr Michelle Atchison and Health Minister Chris Picton
Opposition health and regional health spokespeople Ashton Hurn and Penny Pratt
Dr Williams with the new Vice President, Associate Professor Peter Subramaniam
Managing doctors has been described as like trying to herd cats. But my experience is that when we talk about patient care and improving that service – it is much easier to unite doctors.
Why the AMA?
I’ve been an AMA member since university, and a member of the AMA(SA) Council for about eight years.
I’m intrigued and sustained by the insights and understandings of the mechanics of our health care system, and my involvement in the AMA has given me knowledge and perspective very difficult to obtain elsewhere.
I was invited by former President Dr Chris Moy to stand for Vice President to bring a rural perspective to AMA leadership in this state, as it was clear that rural medicine was struggling.
I bring to this role important characteristics. First, my experience as a rural GP.
I remember looking down over Port Lincoln Hospital during my first ED shift on call and thinking that anything that happens in Port Lincoln medically tonight I will have to deal with. Any accident. Any ambulance siren will be bringing them to me. Could I walk into the pubs and sports clubs and politely ask that everyone take it easy tonight?

But my experience really was that I felt more supported in Port Lincoln than in the Home Counties in England. I really experienced working in a team - GP and non-GP specialists, working collegially.
There was certainly a lot that I could deal with myself but being part of a team was and is really the most important thing.
Of course, as President I will and must serve as the representative of AMA members in the city, too.
The term ahead
While I believe that by fixing our most fragile services in public health we will find many of the solutions for the system as a whole, there are issues that require a close understanding of how they affect junior doctors and senior doctors, in the city or country, in public hospitals or private practice.
We have a health system in crisis, with ramping and surgery waiting lists just two signals of how difficult it is for patients to receive care.
We are still living with COVID-19 and its effects such as long COVID.
Perhaps most importantly, I’m looking forward to helping ensure our medical students and doctors in training are supported and can thrive in our thrilling and rewarding profession.
Taking patient care into the future, they will overcome challenges and embrace opportunities unknown to us today.
My time on Council and as Vice-President has increased my awareness of issues across our profession and the health system, and how these issues affect colleagues in all specialties and geographical areas.
My mission for my two-year term is to listen carefully to our members so that when I speak as President of the Australian Medical Association in this state, you will hear the collective voice of all South Australian doctors, all of us working for the improvement of health care and reduction in suffering of all South Australians.
medicSA | 9 medicSA | 9 For Sale BRAND NEW CORPORATE OFFICE SUITES – Options from 275sqm* up to 825sqm* total – Self-contained floors with excellent natural light – Suit corporate office, medical & consulting (stcc) – Prices from $1,700,000* *(Approx) RLA199257 RLA1842 Claudia Brace 0420 546 770 Jack Dyson 0448 685 593 Ben Parkinson 0407 710 389 Oliver Totani 0412 808 743 274 Pulteney Street, Adelaide SA For Sale by Expressions of Interest GALA BALL
Immediate Past President Dr Michelle Atchison warned her successor to set his alarm at 6.50 am and buy ‘three great suits’ during her farewell speech at the AMA(SA) Gala Ball on 20 May.
Dr Atchison said incoming President Dr John Williams should be ready for early-morning calls from ABC radio producers about ‘something you’ve never considered’ and have a change of clothes on hand for on-camera interviews.
The tips were among her hints for incoming AMA(SA) presidents, shared before she presented Dr Williams with the AMA(SA) President’s Medal.
Other tips were to record every meeting and phone call, carry extra AMA pins for official and social occasions, and to use the presidency as ‘a great excuse to buy nice clothes’.
‘Lastly,’ she added, ‘be kind to everyone. Kindness and a willingness to say yes opens doors.’
Speaking after a 40-minute presentation of magic from award-winning illusionist Matt Tarrant, Dr Atchison said she leaves the role ‘with feelings of sadness and satisfaction, and some disappointment’.
‘The disappointment comes because, as we all know, there are so many issues facing clinicians, and unfortunately there is so much to be done to support doctors, patients and communities to be able to give and receive the best health care possible,’ Dr Atchison said.
‘I feel sad, because I will miss many parts of this role – some of which I did not expect when I was elected President, even after my years on Council and my term as Vice-President to Dr Chris Moy.
‘As I’ve said many times in the past 24 months, there really is no way of knowing what it is like to be the President of the Australian Medical Association in South Australia.
‘The status of the AMA means that the President is the person, representing the AMA, that government and media turn to for
advice, direction and comments about virtually any matter relating to medicine or health care.’
Dr Atchison said the AMA(SA) President must move from knowing ‘a little about everything’ in their specialty to ‘knowing a little bit about all of medicine’.
‘Of course, the timing of my presidency was just impeccable,’ Dr Atchison said. ‘With COVID, ramping, and the GP crisis, everyone turned to us for help, guidance, information, and answers.
‘Some sectors of the media, the public and even our own profession, questioned the very foundations of medicine and scientific evidence – and while internally wanting to scream, I learned to keep my psychiatrist’s face on, repeat our message, and hope it would cut through.’
The satisfaction, she said, came from knowing that many people did listen, and the AMA’s work consequently led to positive changes for doctors and patients.
Earlier, CEO Dr Samantha Mead said she would leave her role as CEO to confront many of the same issues but from a different perspective, at the Australian Nursing and Midwifery Federation
During her speech, Dr Mead thanked Gala Ball platinum sponsor, MIGA, bronze sponsors, Genesis Care and ACHA, and wine sponsor, Auld Family Wines, for their support of the event, and acknowledged the importance of the relationship with ongoing partners Hood Sweeney and Norman Waterhouse Lawyers.
Dr Mead also highlighted the work of the DREAMIN Foundation, a South Australian not-for-profit organisation with close links to AMA(SA). She said DREAMIN provides health care to neighbours near and far, including at Maranatha Health in Uganda and the ‘HEARS’ Project in the Pacific Islands, and, closer to home, offering medical student and junior doctor scholarships.
AMA(SA) Outstanding Achievement Award - Dr Michael Rice
The recipient of the 2023 Outstanding Achievement Award is a man universally loved, respected and admired for a career in which he has devoted himself to the treatment and care of children since beginning his paediatric training at the then-Adelaide’s Children’s Hospital in 1962.
After furthering his training in internal medicine and paediatric haematology and oncology in Australia, the UK and United States, he established a specialty service for children with cancer at the Children’s Hospital, where a unit is now named for him.
He has been awarded the Howard Williams Medial from the Australian College of Paediatrics, the Medal of the Royal Australasian College of Physicians, the Centenary Medal and is a Member of the Order of Australia.

Throughout much of his career, he also served his country as a doctor with the Australian Army, including a tour to Vietnam as the doctor on the HMAS Sydney.
A Past President of AMA(SA) and former member of Federal Council, he was awarded the AMA Gold Medal in 2004. He was President of the Medical Benevolent Fund for 18 years and a much-valued member of the AMA(SA) Editorial Committee until December last year. He is an extraordinary, lovely man who embodies the characteristics that have made doctors the most trusted professionals in this country for decades.
medicSA | 10 GALA BALL
The AMA(SA) Gala Ball was the stage for public farewells from the outgoing President and the CEO.
AMA(SA) President’s Award - Dr John Nelson
The AMA(SA) President’s Award goes to a person who has possibly contributed more than anyone outside AMA(SA) Council to ensure the future of the AMA in this state.
In his professional roles, he was a staff radiologist or visiting specialist in at every major public hospital in Adelaide and several in regional South Australia, going on to combine his public hospital sessions with private practice.
With his medical knowledge and networks combined with his background as the chair and managing partner of a large health company, he provided exemplary service and calm, collected advice to the Executive Board, the CEO and the President after joining the Board table in 2018.
As Chair, he led the AMA through some of the most difficult years of our existence –years that included internal disruption, a once-in-a-century pandemic, the sale of physical assets and changes of operational leadership and staff.
His influence encouraged discussion and involvement and his clear vision have been admirable. We have appreciated his warm, consultative and inclusive approach; his integrity and honesty; and his balanced, ethical and trustworthy leadership.
Due to his retirement from practice, we reluctantly accepted his resignation from the Board earlier this year. His shoes, and seat, will be incredibly difficult to fill.
The Medical Educator Award - Professor Susanna Proudman

This year’s recipient of the AMA(SA) Medical Educator Award for outstanding contributions to medical education has been involved in medical education for a quarter of a century.
For many years she almost single-handedly ran the Adelaide Medical School’s rheumatology teaching program and she is a clinical lead in developing components of the new Bachelor MD course.
With research interests in rheumatoid arthritis and reducing the burden of disease associated with scleroderma and its complications, she has supervised students, is primary supervisor of the advanced trainees in rheumatology at the RAH, and is a Senior National Examining Panel member for the Royal Australasian College of Physicians.
Known for bringing passion for learning and for medicine to her teaching and for fostering a safe environment for students to ask questions and learn, she is a dedicated and inspiring role model for women aspiring to leadership positions in the academic and clinical sphere.
She is generous and always willing to help and intervene on behalf of the Adelaide Medical School, providing a critical conduit for the school to an invaluable resource of clinicians.
AMA(SA) Award for Outstanding Contribution to MedicineProfessor Paul Worley


This award goes to a man whose experience in medicine includes periods in public hospitals, local and rural health, and medical research.
His work in the science of rural community-based medical education, and its impact on addressing the shortage of doctors in rural and remote areas, is revolutionising medical education and rural medical workforce policy nationally and internationally.
He is a former Dean of the School of Medicine at Flinders University, where he established rural clinical schools and departments of rural health in South Australia and the Northern Territory … … and developed a medical program with a focus on recruiting and supporting Indigenous students and staff, recognised around the world.
He was the person to whom the Australian Government turned when they created the position of National Rural Health Commissioner.
He is a past President of the Rural Doctors Association of SA, a previous national Vice President of the Australian College of Rural and Remote Medicine, and an elected Fellow of the Australian Academy of Health and Medical Sciences.
He is committed to working with partners in academia, government and the medical profession to solve the medical workforce deficit and create an end-to-end medical school program, junior doctor training and registrar training and provide a dynamic, sustainable rural generalist workforce for our future.
medicSA | 11 GALA BALL
medicSA | 11
Council news
The meeting of 4 May was an important one to me. It was my last Council meeting as AMA(SA) President before the AGM that followed this meeting. The Council meeting itself was shortened to make way for the AGM but as usual it featured far-ranging discussions of areas we are working on.
This was the first meeting in about three years where COVID was not the first and most discussed topic! Not that any of us believe COVID has left us, or no longer has implications for our work and the health system, but it was good to give other topics the time they deserved.
May 2023
Instead of COVID, rural issues predominated, and I think will do so over the coming year, especially with a new rurally based President. There was discussion of the recent AMA(SA) meeting with Health Minister Chris Picton, in which support for general practices in the state’s south-east was a major topic. We were lucky to have AMA(SA) Councillor Dr Richard Try’s input in that meeting.
Incoming President Dr John Williams updated the Council on the current industrial negotiations for rural GP
contracts. It seems like just yesterday when the last contracts were signed off. An update on discussion around the single employer model for GP trainees occurred. If South Australia can lead the way on this funding model, I am very hopeful that we can attract and retain general practice trainees here in this state. They are sorely needed.
The Committee of General Practice remains actively involved in so many areas. Dr Bridget Sawyer spoke about ongoing concerns we have around the proposed Urgent Care Centres, particularly whether they will take pressure off ED departments and how they will be staffed in a period during which general practice is so under the pump anyway.
And then we moved on to the AGM, where Dr Williams and our new Vice President, Associate Professor Peter Subramaniam, took on their roles. We are privileged to have on Council now former Deputy Chief Medical Officer Dr Emily Kirkpatrick.
I look forward to being part of a strong, committeed Council and serving our new leaders in the two-year term ahead.
AMA(SA) COUNCIL AND EXECUTIVE BOARD
AMA(SA) COUNCIL
Office Bearers
President: Dr John Williams
Vice President: A/Prof Peter Subramaniam
Immediate Past President: Dr Michelle Atchison

Ordinary Members
Dr Vikas Jasoria
Dr Nimit Singhal
Dr Krishnaswamy Sundararajan
Dr Hannah Szewczyk
A/Prof William Tam
Dr Emily Kirkpatrick
Practice group/region representatives
Anaesthetists: Dr Louis Papilion
Dermatologists: Dr Karen Koh
Doctors in Training: Dr Hayden Cain
Emergency Medicine: Dr Cathrin Parsch
General Practitioners: Dr Chris Moy
Orthopaedic Surgeons: Prof Edward (Ted) Mah
Paediatricians: Dr Patrick Quinn
Pathologists: Dr Shriram Nath
Physicians: Dr Andrew Russell
Psychiatrists: Prof Tarun Bastiampillai
Public Hospitals: Dr Clair Pridmore
Southern: Dr Richard Try
Medical school representatives
University of Adelaide: Isaac Tennant
Flinders University: Jordyn Tomba
AMA(SA) EXECUTIVE BOARD
Dr Michelle Atchison, Dr Guy Christie-Taylor, A/Prof William Tam, Ms Megan Webster, Dr John Williams
SA MEMBERS OF AMA FEDERAL COUNCIL
Dr John Williams, Prof Ted Mah, Dr Clair Pridmore, Dr Hannah Szewczyk
medicSA | 12 NEWS
Dr Michelle Atchison
Immediate Past President
Search begins for new CEO
AMA(SA) Chief Executive Officer Dr Samantha Mead is leaving the organisation in June for a new role with the Australian Nursing and Midwifery Federation’s South Australian branch.

Dr Mead has been appointed Chief of Staff/Executive Director at the ANMF and will work alongside CEO/Secretary Adj Associate Professor Elizabeth Dabars. She begins her new role on 13 June.
President Dr John Williams said the process to recruit Dr Mead’s successor was underway.
Dr Williams thanked Dr Mead for her tireless determination to steer AMA(SA) through many difficult issues and to create organisational structures to take AMA(SA) and its members to a sustainable future.
‘I know the staff will miss your humour and your understanding, while Council and members will miss your passion for the medical profession and your contributions to developments in the sector during your time with us,’ Dr Williams said.
Dr Mead joined AMA(SA) in August 2019. She has led the
Secretariat and its efforts to support Dr Williams and previous Presidents Dr Chris Moy and, most recently, Dr Michelle Atchison.
At the AMA(SA) Gala Ball on 20 May, Dr Mead thanked Dr Atchison for being ‘a wonderful person to work with’.
She also thanked former President Dr Chris Moy, Dr Williams, the Council and the Executive Board.
She reserved special thanks for the ‘hard-working team in our office’.
Dr Atchison said AMA(SA) was privileged to have Dr Mead at the helm during one of the most complex eras in its history. As Chair of the Executive Board following Dr John Nelson’s resignation, Dr Atchison said Dr Mead had led the office to provide a ‘backbone’ for her during her presidency.
In April, AMA(SA) farewelled Dr Atchison and Dr Mead’s Executive Assistant Mrs Claudia Baccanello, who in 2021 was awarded the AMA(SA) Outstanding Achievement Award for her 17 years’ devotion and service to the AMA.


medicSA | 13
NEWS
Dr Michelle Atchison and Dr Samantha Mead thanking Mrs Claudia Baccanello (centre) for her service
Dr Samantha Mead being farewelled by AMA(SA) President Dr John Williams
Dr Samantha Mead




medicSA | 14 Support and guidance whenever you need it, from the experts in medical indemnity insurance. For assistance call our friendly team on 1800 777 156 or visit www.miga.com.au ...we’re here for you Insurance policies available through MIGA are underwritten by Medical Insurance Australia Pty Ltd (AFSL 255906). Membership services are provided by Medical Defence Association of South Australia Ltd. Before you make any decisions about our policies, please read our Product Disclosure Statement and Policy Wording and consider if it is appropriate for you. Call MIGA for a copy or visit our website. 1 75,000 bonus Qantas Points offer only available to registered Australian medical practitioners who first insure with MIGA in a fully insured category, as a doctor in private practice, for cover commencing in the period between 30 June 2023 and 31 July 2023, and who pay in full by 31 July 2023 or enter into a direct debit arrangement with MIGA by 31 July 2023, and pay at least one instalment by 24 August 2023, who have not exercised their rights to cool off nor had their insurance cancelled by MIGA, as per the terms and conditions of the Policy. MIGA Terms and Conditions for bonus Qantas Points for Fully Insured are available at www.miga.com.au/qantas-bonus-tc-pp. 2 A business must be a Qantas Business Rewards Member and an individual must be a Qantas Frequent Flyer Member to earn Qantas Points with MIGA. Qantas Points are offered under the MIGA Terms and Conditions at www.miga.com.au/qantas-tc. Qantas Business Rewards Members and Qantas Frequent Flyer Members will earn 1 Qantas Point for every eligible $1 spent (GST exclusive) on payments to MIGA for Eligible Products. Eligible Products are Insurance For Doctors: Medical Indemnity Insurance Policy, Eligible Midwives in Private Practice: Professional Indemnity Insurance Policy, Healthcare Companies: Professional Indemnity Insurance Policy. Eligible spend with MIGA is calculated on the total of the base premium and membership fee (where applicable) and after any government rebate, subsidies and risk management discount, excluding charges such as GST, Stamp Duty and ROCS. Qantas Points will be credited to the relevant Qantas account after receipt of payment for an Eligible Product and in any event within 30 days of payment by You. Any claims in relation to Qantas Points under this offer must be made directly to MIGA by calling National Free Call 1800 777 156 or emailing clientservices@miga.com.au. © April 2023 Earn 75,000 bonus Qantas Points when you first insure with MIGA by 31 July 20231 Plus earn 1 Qantas Point per eligible $1 paid to MIGA for your medical indemnity insurance2
Personal service
The newest Life Members of the AMA were honoured for their dedicated commitment to the AMA and their patients at a morning tea in Veale Gardens in May.

In welcoming the Life Members and their guests, Dr Michelle Atchison, at the time President of AMA(SA), said it was pleasing to be able to stage a ‘live’ event in what have been uncertain times.
‘The awarding of life memberships is a very important event on the AMA(SA) calendar,’ Dr Atchison said.
‘As members of this association for at least 50 years, our Life Members have led, participated in and witnessed innovations and changes that have revolutionised the practice of medicine and transformed people’s lives.
‘They have mentored and supported generations of junior doctors – the doctors who are now leading the profession and its development in the same way you have done.’
The specialties and interests of the members awarded life membership in 2023 and others who joined the ceremony reflected the range of expertise within the AMA: general practitioners, neurologists, ophthalmologists, urologists, paediatricians, anaesthetists and psychiatrists.

‘Without people who choose their specialty areas, and then devote their lives to helping people by treating or researching the relevant medical conditions, we would not have an AMA with the reputation and profile we do today,’ Dr Atchison said.
‘Despite the crisis in health care that is affecting so many of us

and our colleagues, doctors are the most trusted professionals in our society.
‘And the AMA, in representing doctors in all fields of clinical medicine, is among the most trusted and valued organisations.’
Dr Atchison said ‘a growing mistrust in science and evidencebased medicine’ had emerged during the pandemic.
‘It is vital, therefore, that governments and the media still come to us in the AMA for information, guidance and advice, because we are seen to speak for our patients and for doctors.’
Here today, we have representatives from across the profession.
The list of those we are honouring this year includes the following, and we will ask you to come up individually in a moment.
The new members are:
• General practitioner Dr Jonathan Cook
• Neurologist Dr Robert Hall
General practitioner Dr Michael Kain
• General practitioner Dr Suzanne King
• General practitioner Dr Ian Macintosh
• Psychiatrist Dr Raymond Taylor
• Ophthalmologist Dr John Willoughby OAM.
They were joined by former AMA(SA) President and general practitioner Dr Peter Joseph, who was unable to attend the 2022 ceremony. Dr Cook and Dr Taylor were absent from the morning tea.


medicSA | 15 ACCOLADES
Dr Samantha Mead, Dr Peter Joseph and Dr Michelle Atchison
Dr Robert Hall, Dr Margaret Wiese, Dr John Willougby OAM, and Dr Susanna King
Dr Michelle Atchison with ‘life members’ Dr John Willoughby OAM, Dr Robert Hall, Dr Michael Kain , Dr Susanna King, Dr Peter Joseph and Dr Ian MacIntosh


Recently fellowed? Get high quality protection and support for your career and life. Avant gives me the peace of mind I need for the next step in my career. Dr Amani Harris Recent fellow IMPORTANT: Professional indemnity insurance products are issued by Avant Insurance Limited, ABN 82 003 707 471, AFSL 238 765 (‘Avant Insurance’). Information provided by Avant Insurance is general advice only and has been prepared without taking into account your objectives, financial situation and needs. You should consider these, having regard to the appropriateness of the advice before deciding to purchase or continue to hold these products. For full details including the terms, conditions, and exclusions that apply, read and consider the relevant Product Disclosure Statement or policy wording, available at avant.org.au or by calling Avant Insurance on 1800 128 268. MJN1102 05/23 (DT-3012) Find out more avant.org.au/new-fellow 1800 128 268 Build your future with Avant. Medical Indemnity • Health Insurance • Travel Cover • Life Insurance • Legal Services • Finance
‘Big spend on health’
AMA(SA) President Dr John Williams has acknowledged the $2.3 billion additional investment in health in the 2023-24 State Budget handed down by Treasure Stephen Mullighan on 15 June.
AMA(SA) President Dr John Williams has thanked the State Government ‘for listening when doctors, colleagues and patients have described the challenges we face in providing and accessing health care’.
‘I hope to discuss the Budget measures in more detail with Health Minister Chris Picton and senior SA Health staff,’ Dr Williams said.
‘However, an initial review suggests that funding to avoid hospital admissions, and reduce ramping and bed block, both within hospitals and for primary and virtual health services, will be critical to the care we provide in the months and years ahead,’ Dr Williams said.
‘We are pleased to see the additional funding that recognises that COVID continues and will continue to affect our health workers and system capacity, and the State Health Control Centre is a very welcome component in monitoring and measuring system capacity and patient outcomes.
‘Of course, we still need the workforce to deliver these services, and we will work with the Minister and others on measures to attract and retain the best staff –including through the single employer model for our GPs and our ongoing efforts to eliminate bullying and improve conditions for junior doctors in our hospitals across the state.
‘In terms of rural health, the expansion of the Electronic Medical Records program is very important in linking doctors so they can provide consistent, informed care and advice. It was also pleasing to see a commitment to additional funding for the Mount Barker Hospital and $1 million to study the health needs of the Naracoorte region. But I saw little to address the health needs of families in the more remote areas of the state.’
Before the Budget, AMA(SA) outlined to media its priorities for State Government spending on health in 2023-24.
Keep people out of hospital
• Work with the Australian Government
to increase the investment in primary care where it is more effective – in general practice.
• Expand South Australia’s successful virtual health and telehealth services to care for people in their homes, reducing the burden on emergency departments.
• Introduce a central referral unit as the first step for patients, for more efficient triaging and transfers.
• Invest in development of the single employer model in the Riverland and rollout into other LHNs, which will support efforts to recruit and retain doctors in general practice.
• Work with universities to broaden exposure to general practice during medical school.
• Fund services to manage COVID testing and COVID and Long COVID patient care.
• Expand pregnancy advisory services, in line with the decriminalisation of abortion.
• Increase resources in public hospitals and Local Health Networks to cut essential surgery waiting lists.
• Expand palliative care services, including for clinical support in residential facilities.
• Improve EMR and transfer information and communication pathways
• Generate, measure and evaluate more data in public and private systems.
Increase mental health services
• Introduce a mental health strategy that covers acute and community access.
• Increase investment in the rural and remote mental health service and acute mental health teams.
• Support the Suicide Prevention Plan by funding the suicide prevention networks.
• Support new training positions in psychiatry, especially child and adolescent, to provide a pipeline for more psychiatrist in the state.
Expand and maintain the health workforce
• Invest in measures to ensure the workplace safety and culture legislation introduced in 2021 – which places responsibility on LHNs and their Boards – is improving conditions for health practitioners, including junior doctors.
• Increase the number of clinical academic positions/appointments in public hospitals and invest in research activities to attract and retain worldclass talent.
• Review current and future effects of COVID illness and leave on staff numbers, working conditions and morale.
• Attract talent through making South Australia a leader in ‘sustainable health’.
Improve rural health services
• Resolve the contract for rural generalists to support the future of rural GPs.
• Provide equity of access to health care for rural residents, including hospital beds, telehealth and acute mental health support.
• Provide a rural and remote orthopaedic service to support local services, facilitate and speed up transfers and bed allocation.
• Provide ongoing support for rural GP obstetricians in the form of comprehensive, affordable indemnity insurance.
Increase Indigenous health services
• Increase investment in Indigenous health, supporting the State Government’s commitment to a Voice for Aboriginal & Torres Strait Islanders.
• Measure all health initiatives against Indigenous health outcomes.
• Require all LHNs to develop, maintain and report on indigenous health outcomes.
medicSA | 17
STOP PRESS
Influence clear in ‘health budget’
The 2023-24 Federal Budget responded to AMA calls for investment in primary care
The Federal Budget released last month showed the Australian Government had listened to AMA calls for new initiatives to tackle the viability crisis facing general practices, improve access to general practice for vulnerable Australians, tackle inadequate Medicare indexation and make medicines more affordable for consumers battling with the cost of living.
AMA President Professor Steve Robson said the AMA had been calling on the government to make the 2023-24 budget a ‘health budget’.

The budget’s focus on supporting general practice showed the government had been listening, Prof Robson said.
He said the budget outlined in some detail how the previously committed $750 million secured by the AMA as an election commitment would be spent, while also detailing significant new funding over and above this that will go straight towards addressing the viability crisis facing general practices and tackling out of pocket costs for patients.
‘The AMA welcomes the government investing a record $3.5 billion to triple the
bulk billing incentive for concession card holders and children under 16, with this applying to most GP consultations,’ he said.
‘With access to GP care getting more difficult for these patients due to increasing out of pocket costs, this targeted support is much needed and will make a real difference, especially in rural and regional areas.
’We were also particularly pleased to see the $445.1 million in additional funding for the Workforce Incentive Program, which has been underfunded for years. This extra money will encourage general practices to engage more nursing and allied health professionals and support the delivery of well-coordinated multidisciplinary care — all under one roof.
‘This will ease pressure on GPs and help make care more convenient and accessible for patients, and is based on what the AMA has long called for.
‘In addition, $99.1 million in new funding for GP consultations that last for sixty minutes or longer will help those patients with very complex health care needs and support GPs to spend more time with these patients.’
The government also announced the MyMedicare program, which will give patients the opportunity to voluntarily enrol with their preferred GP. This is intended to strengthen the role of general practice in the health system and follows a number of reports recommending the Commonwealth implement a system of Voluntary Patient Enrolment (VPE), and was called for in the AMA’s Modernise Medicare campaign.
‘The government has delivered its response to those recommendations and importantly has learnt from past mistakes, such as the Health Care Homes Trial, preferring a blended funding model in which additional funding is made available on top of existing fee for service arrangements. This also means that VPE will be tailored to the Australian context and will not follow the capitated model used overseas in countries like the United Kingdom.’
Professor Robson said while most of the implementation detail still needs to be worked through, it appears VPE will open up funding and access to additional telehealth services, enhanced GP led care for frequent hospital users, better targeted chronic disease items, and extra incentives for GP services in Residential Aged Care.
‘The AMA will be examining the details of the proposals more carefully and will work with government to ensure MyMedicare works for patients and GPs alike and results in genuine improvements in health care.’
‘The government has adopted reforms put forward by the MBS Review Taskforce including a six-minute floor for a Level B consultation item, the simplification of GP chronic disease management arrangements and the encouragement of longitudinal care. Critically, the savings generated by these changes are all reinvested back into general practice.’
The budget also contains $50 million for a wounds consumable scheme in general practice — a scheme first proposed by the AMA in submissions to the MBS Review Taskforce and further developed and modelled by the AMA in its Solutions to the Chronic Wound Problem in Australia paper.
‘I welcome the changes to the formula for indexing Medicare rebates that will
medicSA | 18 ADVOCACY
Dr Steve Robson
deliver an extra $1.5 billion over and above the former framework that had been in place since 1996 and saw the value of a patient’s rebate fall significantly in real terms. The AMA ran a strong campaign on the issue of Medicare indexation and the impact of the Medicare freeze, and tonight we’ve seen recognition of the successive underfunding in stealth of Medicare by substandard indexation.’
The budget also confirms the government is proceeding with its announcement to move, over time, 325 medicines to a situation where a stable and clinically suitable patient can access 60 days supply of their medicine and a 12-month prescription from their doctor.
‘This is good policy that is based on the independent recommendations of the Pharmaceutical Benefits Advisory Committee that will save patients’ money and free up GP time,’ Professor Robson said.
‘The AMA also welcomes the recent announcements regarding a crack down on vapes, with $234 million committed to addressing the issue, which is impacting the health of many Australians, including our children.
‘The government continues to make
welcome progress on the establishment of an Australian Centre for Disease Control, setting aside $91.1 million for its establishment over the next two years.
‘The forecasts in the budget suggest total expenditure on Medicare is going to be less than had been previously expected. Yet we know as a society we are growing in size, we are growing older, and we have more chronic disease.
‘The revised projections suggest we still have not rebounded from COVID-19 while patients have also struggled to access the care they need due to cost and the failure to adequately invest in our health system. This means patients will be diagnosed later in their illness, when they are much sicker and their care needs are more complex. This will have profound implications for our public hospitals that are already buckling under pressure.’
‘In our discussions with the Minister for Health he clearly indicated general practices was going to be a key focus for the government and tonight’s budget has demonstrated that commitment.
‘But there’s also a great deal of unfinished business in our health system. As the government approaches its second year in office, we know that much more
work is required in areas such as public hospital funding, prevention and supporting a sustainable private health care system, and I will advocate to government on these issues every day.’
AMA welcomes more affordable reproductive care
The Australian Medical Association has welcomed recommendations from a senate inquiry for an increase to MBS rebates for reproductive health care and improved access to a wider range of contraception.
AMA President Professor Steve Robson said the limited MBS items available were rarely appropriate to cover the cost of providing services, resulting in reduced access or out-of-pocket costs for providing reproductive care.
‘New and more appropriate MBS items will greatly improve access to reproductive healthcare for women across Australia,’ Professor Robson said.
The AMA’s submission also called for improved access to a wider range of safe and affordable methods of contraception, working through the Pharmaceutical Benefits Scheme and the Therapeutic Goods Administration processes,
something the inquiry included in its recommendations.
‘At the moment only selected basic oral contraceptives are available through the PBS. We know that GPs regularly see patients who are better suited to a non-PBS subsidised option, however this can be quite expensive, which means some people can’t afford them.’
While the AMA supports recommendations to make contraception health care services more affordable, including by having adequate funding through Medicare, Professor Robson warned that efforts to expand prescribing rights must not undermine patient safety or fragment care.
Professor Robson said the AMA also strongly believed that no one should not have to travel long distances to receive maternity care or abortions.
‘As such, we welcome the committee’s
recommendation that all Australian governments should ensure these services are available and accessible for all who need them, especially in non-metropolitan public hospitals.
‘We know there are issues with access to services, particularly in regional areas. It’s incumbent on governments to ensure women across the country can access the services they need.’
Professor Robson said while there was much to welcome in the report, the AMA was disappointed there were no recommendations on making pregnancy cover more accessible through private health insurance policies.
‘At the moment, pregnancy care remains at the top level of cover, making private maternity care unaffordable and inaccessible for many Australians.’
medicSA | 19 ADVOCACY
Dr John Williams @AMASApresident Dr Steve Robson @amapresident Dr Danielle McMullen @ama_vice AMA Federal @ama_media @ama_south_australia AMA(SA) @AMASouthAustralia Doctors in Training @AMASADIT Australian Medical Association (SA)
IN
STAY
TOUCH
Once again the AMA(SA) Doctors in Training (DiT) Committee has used the AHPRA Medical Training Survey (MTS) to develop our South Australian Hospital Health Check (HHC). The MTS is a survey that can be completed by all DiTs, in this case including all doctors who are yet to fellow with colleges, when they apply for reregistration.
In the latest survey, 21,857 DiTs responded Australia-wide, within which 1,568, or 7%, were from South Australia. Of the respondents in this state, 80% worked in hospital settings compared to community such as GP and two-thirds in metropolitan workplaces.
While South Australia has a multicultural medical workforce – onethird of those who responded obtained their medical degrees overseas – sadly only 1% were from First Nations backgrounds. From an AMA(SA) DiT perspective there were two main areas of focus for this year’s
data: bullying and harassment, and training and workload concerns.
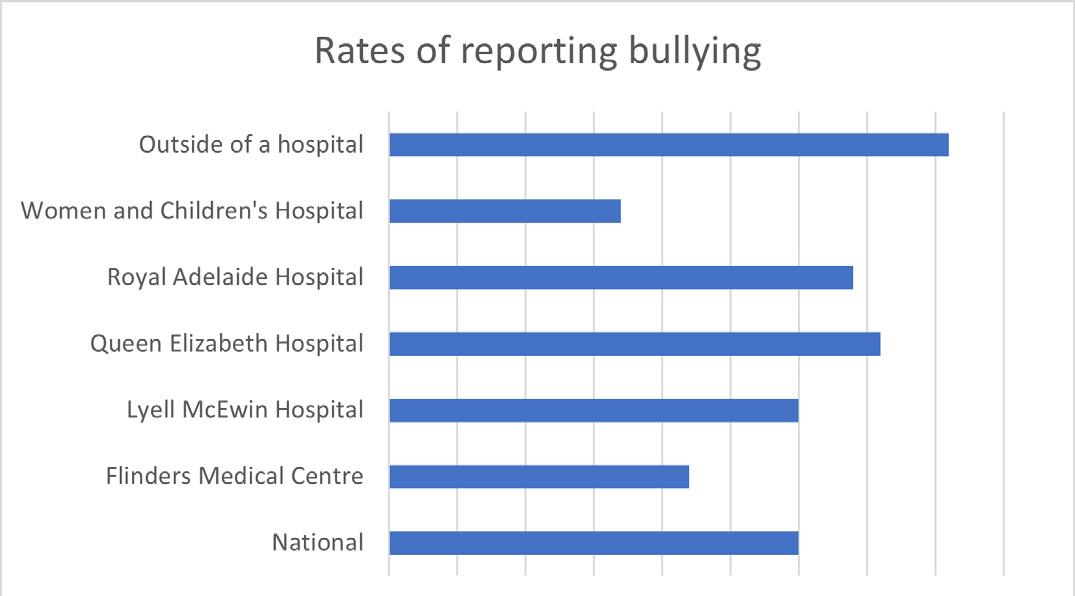
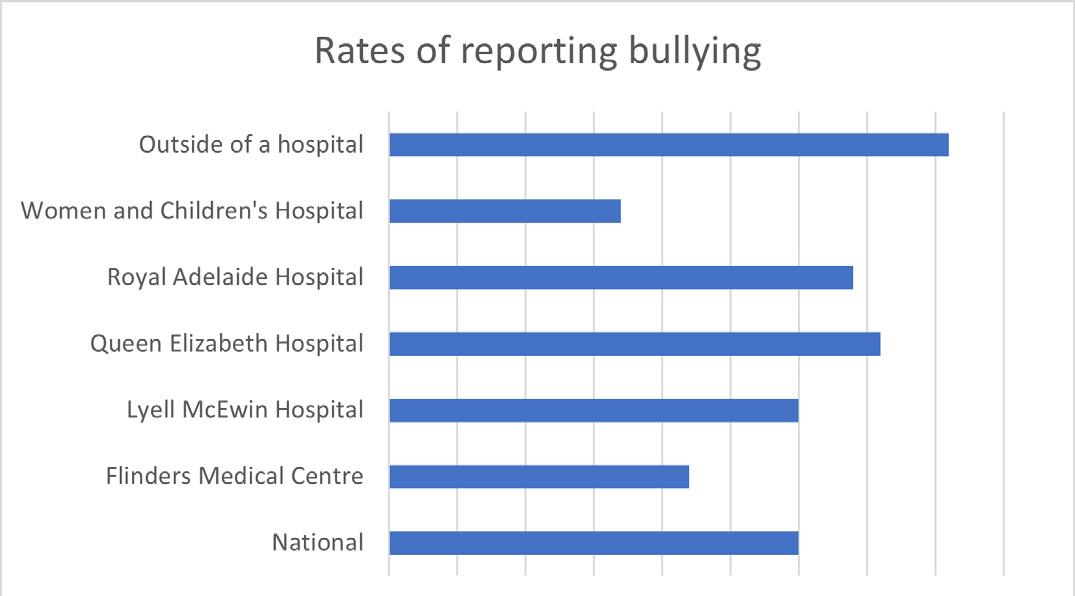
Bullying and harassment are still major issues for DiTs both in SA and around Australia and as such have been a key focus for AMA Council of Doctors in Training (AMACDT) for several years. This year’s survey demonstrated why it remains a problem. With the exception of Mount Gambier (29%) and Noarlunga (7%) all South Australian hospitals with enough respondents to allow analysis of results (n=10) had similar rates of doctors who had been personally bullied or harassed in the past 12 months ranging from 21 to 24%.
While this is low compared to the national average of 30%, a deeper analysis of the results shows a worrying trend. With three exceptions (Noarlunga at 21%, Mount Gambier at 25% and the QEH 27%), all South Australian hospitals had rates of having witnessed bullying or harassment higher than the nation average of 30%, led by WCH (41%), Modbury (39%), FMC (36%)


and the RAH (35%).
It may appear that the higher rates of witnessed compared to experienced bullying is less concerning. But we believe in South Australia that we may be underreporting the amount of bullying being directly experienced by DiTs, for reasons including a belief that nothing will be done and fear of repercussions.

In South Australia, it is more likely that the perpetrator of bullying is a senior clinician with only FMC (47%) having a lower rate than the national average of 48%. At the WCH, being bullied by senior clinicians accounts for 83% of the reported cases, followed by QEH (57%) and LMH (56%). Reporting rates of bullying varied greatly around the state from as low as 17% and 22% at WCH and FMC to 36% and 34% at QEH and RAH.

These concerning low rates of reporting are worsened when the reasons DiTs aren’t reporting bullying are considered. A majority of DiTs report feeling that ‘nothing
medicSA | 20 FEATURE Under
duress
The latest survey of junior doctors’ experiences shows much more must be done to attract, retain and develop the next generation, writes Dr Hayden Cain.
medicSA | 20
will be done’ (WCH 63% and FMC 60%) or that there will be career repercussions (WCH 74% and RAH 65%). The proportion of DiTs in South Australia indicating that these are the reasons for non-reporting is well above the national average of 51% and 55% respectively.
The one highlight from the bullying report was the effect of CALHN’s implementation of the Vanderbilt professional behaviours model. The Vanderbilt model developed at the Vanderbilt University in Nashville is an internationally recognised workforce culture program with a heavy focus on communication strategies. A key feature is the development of a peer-to-peer support model in which co-workers of equal seniority and similar specialties have informal conversations highlighting lapses in professionalism in a non-confrontational or judgemental manner.
While the RAH did have the highest rate of individuals experiencing bullying (24%, with 51% of the bullying by senior clinicians), it had the second highest rates of reporting witnessed bullying (34% behind only QEH with 36%.) The RAH also had a rate of follow-ups to bullying reports of 76%, far better than either FMC (46%) or LMH (38%), as well significantly better than the national average of 47%. Of the reports that were followed up, 69% of respondents indicated they were satisfied with the results – once again, far better than the national average of 59%.

While we must acknowledge the strains that COVID-19 and the junior doctor shortage in Australia have placed on the state’s health system, we are now well past the period of lockdowns. Still, the MTS is showing that working conditions for junior
doctors are not improving. Among the major metropolitan hospitals in this state, only the DiTs at LMH had equal ability to access study leave when compared to the national average of 64% and at WCH that number was only 49%.
In addition, respondents were also more likely to report that their work responsibilities sometimes or often impacted their ability to perform training requirements, compared to the national average of 41%. This was worst at WCH and FMC with 62% and 49% respectively. Excluding Mount Gambier (95%) all South Australian hospitals had fewer DiTs describing their education as ‘good’ or ‘excellent’ than the national average of 81%.

Workspaces affect wellbeing
However, not all the problems can be attributed to workforce shortages. Nationwide, 62% of respondents rated their workspaces as ‘excellent’ or ‘good’; in South Australia, only Modbury (63%) exceeded the national average in praising their workplaces. The worst-rated in South Australia were WCH (48%), Mount Gambier (50%), FMC (52%) and LMH (54%). Other than the RAH, our teaching spaces were also rated worse than the national average.
Given the DiTs’ responses, it is not surprising that significant numbers indicated that workplace issues affected their wellbeing. With the exception of Modbury (23%) and Mount Gambier (25%), all South Australian hospitals exceeded the national average of 28% in reporting that their workload negatively affected their wellbeing most of or all of the time. At the WCH, the rate was 41%, Noarlunga
36%, FMC 32% and at the RAH 31%.
More than 60% of respondents at the LMH, WCH, FMC and the RAH described their workloads as ‘very heavy’ or ‘heavy’well above the national average of 53%.
The MTS has shown that there are many issues affecting DiTs in this state that could affect their future careers. The proportions of DiTs reporting that they are concerned they will either fail to finish their fellowships or enter their chosen specialties are well above the nation average of 35%, at all sites. This prompts questions about whether they are considering careers outside medicine –and the survey suggests as many as 32% of DiTs are thinking about it.
The MTS data clearly shows there are many major issues affecting DiTs in South Australia, that if not tackled soon will only worsen. While the loss of accreditation of some rotations at the WCH have been discussed publicly in the media, the WCH is not an isolated case and all LHNs must start addressing their unique and shared issues as soon as possible.
Still, there are positive findings. First, the Vanderbilt program introduced in CALHN appears to be increasing the likelihood that DiTs will report bullying. Second, despite the current issues, we have a higher rate than the nation average of recommending our current workplaces. The AMA(SA) DiT Committee plans to use this data to advocate for change, including providing adequate work and teaching spaces at all sites, ensuring access to necessities for career progression such as study leave for all doctors, and encouraging close monitoring the progress of the Vanderbilt system and the viability of rolling it out to all SA Health sites.
medicSA | 21 DOCTORS UNDER DURESS
Iam writing this article after attending the Medical Board of Australia Conference, which had a focus on doctor wellbeing and the culture of medicine. This conference took place a year after the Culture of Medicine Symposium was held in Melbourne.

Although we have known for some time that the culture of medicine is suboptimal, the findings from the Medical Training Survey (MTS) have given us strong evidence to support this and has really put this issue on the agenda.

The MTS is a survey of doctors in training run by the Medical Board and was developed with input from stakeholders including the AMA’s Council of Doctors in Training. It has now run over four consecutive years and the 2022 results were released in January this year. There was a 56% response rate, giving us one of the most representative datasets that we have had access to.

Key findings
• 34% of respondents experienced and/or witnessed bullying, harassment, discrimination or racism
• 55% of Aboriginal and Torres Strait Islander trainees experienced and/or witnessed bullying, harassment, discrimination or racism
• Of those who experienced unacceptable behaviours, 70% did not report it
o 55% were concerned about repercussions if they did report
o 51% felt that nothing would be done about it if they did report
• 20% are considering a career outside medicine.
These results highlight deeply ingrained cultural issues, but also a system under strain. We know that our hospital and general practice systems are under pressure; if poor culture is driving junior doctors away from careers in medicine, the pressure on these systems increases.
Some states and territories, including South Australia, are using this data to create their Hospital Health Check reports. We hope that these reports will motivate the hospitals that are performing poorly to improve.

The AMA Council of Doctors in Training is using the MTS data to produce a second yearly report on how the colleges compare on factors including communication and engagement, examinations and assessment, supervision and teaching, and workplace environment and culture. We feel that it is important that doctors are well informed when applying for specialist training, and to highlight the colleges that are performing well and those that aren’t.
There is broader stakeholder engagement in tackling this issue. The National Medical Workforce Strategy included doctor wellbeing as a cross-cutting theme. The Department of Health has provided funding for a project to improve the culture of medicine that is headed by the Royal Australasian College of Medical Administrators. I attended the first meeting of the National Doctors Health and Wellbeing Leadership Alliance last month; its purpose is to lead implementation of the ‘Every Doctor, Every Setting’ Framework.
Although the negative impacts of poor workplace culture on doctors can’t be ignored, the most important aspect is the impact on patients. There is strong evidence that poor workplace culture leads to poorer patient outcomes. It is for this reason that governments, regulators and hospitals must prioritise improving medical workplace culture, and action is needed now. South Australia has taken the lead by legislating that hospital boards are responsible for the wellbeing of staff. Although this is a positive first step, there is yet to be change on the ground. For consistency across the country, health care settings need to prioritise the wellbeing of staff by managing psychosocial risks, and they need to be held accountable. I believe that the most appropriate way to ensure this is to include workplace psychosocial safety in the National Safety and Quality Health Service Standards.
While the MTS findings are concerning, the commitment to change is inspiring. The momentum to improving the culture of medicine can be felt and I am optimistic for a better future.
medicSA | 22 DOCTORS UNDER DURESS
medicSA | 22
Our patients ultimately pay the cost of doctors’ poor workplace conditions, writes AMA Council of doctors in Training Chair Dr Hannah Szewczyk.
Crazy for health
Crazysocks4docs founder Dr Geoff Toogood again chose to join colleagues and health partners for the Adelaide event on #Crazysocks4docs Day on 2 June.


Dr Toogood reminded a roomful of doctors, medical students and friends at the Adelaide Convention Centre that Crazy Socks aims to increase awareness of the importance of doctors looking after their own mental health.




Dr Toogood and co-host Dr Roger Sexton – medical director of Doctors’ Health SA and medical editor of medicSA were joined in Adelaide by Dr Ben Bravery, psychiatry trainee and author of The Patient Doctor Released in 2022, The Patient Doctor details Dr Bravery’s experiences of illness and the health system after being diagnosed with colorectal cancer when aged 28.
Other speakers included Federal Health Minister Mark Butler and panel members Dr Sian Goodson, Chair of the RACGP in SA; Ms Isla Woidt of the Commission for Excellence and Innovation in Health; University of Adelaide Dean of Medicine Professor Danny Liew and paediatric rheumatologist Dr Gráinne Murray.
AMA(SA) Council members and staff donned their most colourful footwear to celebrate Crazysocks4docs Day and acknowledge the importance of doctors caring for their own mental health.
AMA(SA) Doctors in Training Committee Chair Dr Hayden Cain (left), Dr Louis Papilion and Associate Professor William Tam (centre) and Mrs Catherine Waite were amoung Council and staff members parading their socks for a very worthy cause.
medicSA | 23 DOCTORS UNDER DURESS
Crazy Socks founder Dr Geoff Toogood at the Adelaide Crazy Socks 4 Docs Breakfast
MC Paul Kitching (right) interviews guest speaker Dr Ben Bravery
Chief Public Health Officer Professor Nicola Spurrier with AMA(SA) CEO Dr Samantha Mead
Painful procedures
Health SA medical director Dr Roger Sexton.

We all know the feeling of being in a long traffic jam, suddenly stuck behind a big truck, unable to see anything and not knowing what has happened to cause the delay.
Then you turn on the radio and learn there has been an accident, that emergency services are in attendance and that there will be a two-hour delay before traffic can move again.
The situation is annoying but easier to cope with when you know what’s going on. So, you get on with doing something while you wait.
This is the situation that faces many doctors undergoing an Ahpra investigation. The lack of information about the progress of their complaints and what will happen next is frustrating and distressing. Doctors want to know the next steps and how long they will take, and they want the matter resolved so they can get move on.
This process can take many months and the impact on the health and wellbeing of doctors is unpredictable. Whether the complaint is minor or major, the doctor’s response may be the same. It may range from mild to severe, but it is universally distressing and may precipitate a strong sense of unfairness, guilt, embarrassment, anger, depressed mood, despair, and even thoughts and plans of suicide.
Complaints can alter the way doctors practise following the notification. They may avoid certain patient problems and types, practise more defensively, become less engaged with professional life, avoid colleagues and clinical meetings, over-
investigate, work shorter hours, refer patients more often and become more suspicious of their patients. Personal and marital relationships may suffer.
Some complaints are known to be vexatious, frivolous or mischievous. The Medical Board and Ahpra have recognised this and over the past two years introduced a panel of assessors who look for these and filter them to avoid them being processed in the standard way. This has reduced the waiting times for complaints to be fully resolved from about eight to about three months. For most doctors, this is still a purgatorial wait.
A study from the UK’s General Medical Council several years ago highlighted the number of doctors who had suicided while undergoing or in response to a complaint. A similar study in Australia has identified 16 doctors in the past four years who have suicided while undergoing the complaints process. While the link has not been proven in all cases, the GMC experience and the experience of the treating doctors working in the doctors’ health programs around Australia suggests the link very strongly.
Doctors can misunderstand the triggers for notification and the complaints process and what will happen. The medical defence lawyer has a critical role here to explain this, but a doctor who is notified of a complaint can also benefit from the advice of a senior medical college who can put the complaint into clinical perspective. Catastrophic thinking is often out of proportion to the nature of the complaint. Timely advice is critical for perspective –and can be life-saving.
A complaint may arise in the setting of a doctor carrying an excessive burden, the extent of which is so great that the complaint is the straw that just cannot be borne. A doctor’s burden can compound and be acute and long-standing. Contributing factors may be directly related to work, such as a patient death, excessive workload, business duress, financial debt, or overcommitment to college roles; or indirectly related, such as marital and relationship duress.
The lonely, overworked doctor who is depressed may start to take risks (a recognised symptom of depression in men) and cross boundaries or upset patients with their lack of empathy.
Ahpra is looking closely at this issue. It has established an internal team to examine the complaints experience and the impact of notifications.
The value of a comprehensive medical check-up by an independent treating GP for a doctor undergoing the complaint process has also been discussed. This recognises that a doctor undergoing a complaint may have undiagnosed physical and mental health problems that have contributed to the situation. It is also an opportunity to improve the health of the doctor over the longer-term.
The process of complaint resolution is stressful but the outcome should not be catastrophic for the doctor or their family. The regulator, insurers and the profession must take all possible steps to make the process is efficient, fair, transparent, humane and supportive, for the benefit of all involved.
medicSA | 24 medicSA | 24
DOCTORS UNDER DURESS
Changes to Ahpra processes are adding more pressure to already burdened doctors, writes Doctors’
Complaints under consideration
Medical Board of Australia Chair Dr Anne Tonkin says the Medical Training Survey has important results for clinical workplaces.
As chair of the Medical Board of Australia, Dr Anne Tonkin is the among the first to admit there are many myths and legends surrounding the regulation of professional standards.
Yet Dr Tonkin is quietly confident that when her term concludes at the end of 2024, the regulator will have significantly improved the complaints process experience for most health practitioners as well as patients and their families.
During her term of office, Dr Tonkin has sought to de-mystify the process –particularly around mandatory reporting and the recent measures to enable the publishing of the names of practitioners considered to be a danger to the public.
‘I’ve been working very hard to try and put a human face to the process that isn’t too scary,’ she says. ‘We’ve made a lot of progress in that direction.’
Many clinicians have expressed concerns that the rules around mandatory reporting mean doctors should fear sharing their mental health or addiction challenges with their general practitioners. But Dr Tonkin says nothing could be further from the truth.
‘One of my goals is to reduce the fear of mandatory reporting and have people understand that if they have a mental health issue of any kind the best thing is to get help early before the health issue becomes an impairment,’ she says.
‘We don’t need to know about health issues at all – we only need to know when someone is impaired to the point when they are a danger to the public.’
Patience in reiterating the message in a range of forums – from conferences to medical defence organisations – and with different parts of the profession has been the key to putting a human face to the regulatory process.
‘I’m trying to get that message out but there’s a lot of myth and legend out there
and I’m trying to counteract it,’ she says.
The complaints process is not intended to be punitive, she explains, but the job of the MBA is to take action only if required to protect the public.
If a doctor has taken steps to ensure a mistake is unlikely to recur, the regulator needs to take no further action.
Also unfounded, she says, is fear surrounding the new amendment to the National Law to allow the names of practitioners to be published before a complaint has been finalised. Dr Tonkin says the provision is only likely to be applied where unregulated practitioners pose a threat to public safety.

She says that of the 6,000 complaints the Australian Health Practitioner Regulation Agency (Ahpra) receives each year, it is likely to be applied to fewer than five.
‘There are strict legal considerations about when you can do it and when you can’t; it would be taken very seriously. There seems to be a sense out there that everyone who gets a notification would be named and that’s absolutely not what it is going to be,’ she says.
She also denies that the complaints process is used as a weapon in professional rivalries and that the system is weighted against doctors.
The vast majority of complaints come from patients and their families, says Dr Tonkin, and there are measures in place to test the motivation of complaints by practitioners with sanctions for those using complaints maliciously.
Ahpra is also working hard to reduce the complaints process timeframes and a new IT system to be introduced in the next six months aims to help practitioners monitor the progress of complaints.
‘There are signs that the MBA’s partnerships to improve the culture of the medical professional are having traction, says Dr Tonkin. A key part of this has been
the Medical Training Survey, which has been valuable in demonstrating the impact of poor culture in some organisations.
‘First Nations trainees are reporting bullying harassment and racism to the level of over 50% whereas the incidence among other trainees is around 33% or so,’ Dr Tonkin says. ‘(The survey finding are) making overt things that have been a bit covered up.’
The feeling at the recent Doctors Health and Wellbeing National Alliance, hosted by the Federal AMA, was that there is a willingness at high levels to do something to improve the culture of health organisations – valuing people and ensuring good working conditions to prevent bullying, she says.
‘There is a real sense that the time for talking is over and the time for doing is here. I’m really optimistic that we are about to see some changes.’
There’s still plenty more work to be done though, says Dr Tonkin. The challenge of regulation is to predict the next challenges to medical professionalism. Issues such as on-demand e-prescriptions, cosmetic injectables and artificial intelligence are already posing issues that will require regulatory attention.
‘Rules around professionalism haven’t kept pace with the changing business models,’ she says. ‘We must keep updating guidelines to help practitioners stay within the professional boundaries the profession needs.’
medicSA | 25
DOCTORS UNDER DURESS
A catalyst for care
As a successful gynaecologist, Dr Fariba Behnia-Willison thought she could fix most of the problems that came through her door with skilled surgery.
But in 2010 she realised there was a need for a new, holistic approach to gynaecology and women’s health. Twelve years later, her passion to do things differently has led to her business FBW Gynaecology Plus and the charity Desert Flower becoming the Accelerating Women & Championing Health National 2023 Telstra Best of Business Awards winner.
Iran-born and Germany-trained, Dr Behnia-Willison was experienced in addressing the often-silent suffering experienced by women with gynaecological problems. But in 2010, while working as a surgeon in Adelaide, she was forced to reconsider her approach when challenged by a 30-year-old breast cancer patient who had experienced a double mastectomy, lost her ovaries, and was taking Tamoxifen as part of her breast cancer treatment.
‘She tearfully told me that she had been previously dismissed by seven other
gynaecologists who had all told her there was nothing they could do to help her. In fact, she should be happy that she is alive,’ Dr Behnia-Willison recalls.
The patient said intimacy was impossible due to the excruciating pain she experienced as a side effect of her breast cancer treatment. Her genitalia were so painful that even sitting was problematic. ‘She said: “I cannot be a mother; I cannot be a lover; What is the point of prolonging life if there is no quality of life?”,’ she says.
‘That question confronted me because it forced me to change my view as a surgeon and as a women’s health provider. In this instance there was proof that even my advanced surgical skills and knowledge of traditional HRT were not going to assist this patient.’
Dr Behnia-Willison decided a better approach would be to use platelet-rich plasma (PRP) encourage tissue regeneration as treatment for severe vaginal atrophy.
The patient’s quality of life changed significantly and her confidence in the regenerative powers of PRP solidified to the point that during her next appointment she asked for an injection of PRP in her face.
‘This was the catalyst for me to write to GPs as I wanted to conduct a study on 100 women, and I asked them to refer me women with similar conditions.
‘To my surprise, I received many referrals quickly, even for other conditions such as treatment-resistant vulval lichen sclerosus,’ says Dr Behnia-Willison.
This led Dr Behnia-Willison to research other regenerative modalities besides surgery, and eventually to complete a PhD.
She established a centre of minimally invasive surgery and regenerative medicine with a multi-disciplinary approach to women’s health, recognising that her patients’ individual social, emotional and economic circumstances should influence their treatment plans – and that women should be involved in the decision-making process.
Her patients have access to a physiotherapist, pain specialist, colorectal specialist, urologist, sexologist, nutritionist, naturopath, and counselling.
Dr Behnia-Willison says women’s health beyond childbearing is a ‘forgotten area’,
indicated by the fact that the largest proportion of funding allocated for women’s health goes to fertility treatment.
She says people are reluctant to talk about sexual intimacy but that it is important for women’s health, and especially that of older women, as it reduces the risk of stroke and heart disease, increases testosterone levels and improves sleep.
Her aim is to use surgery only when it is necessary. When it is, she uses noninvasive and minimally invasive treatments, regenerative medicine and surgical procedures, such as single-incision laparoscopic, scarless and robotic surgery.
As part of a second PhD she is developing a biodegradable graft that may help treat pelvic organ prolapse and incontinence, which affects 50% of women over 50.
‘Having won at the State of the Telstra Business Award finals, we have been able to gain traction in securing increased interest with our potential investors to bring this product to the commercial market, so it will be a cost-effective option for those millions of women experiencing prolapse symptoms, not just in Australia, but world-wide,’ she says.
Dr Behnia-Willison is also working to expand the Desert Flower South Australia Centre she founded alongside daughter Nadia Willison, and colleague Dr Tran Nguyen. The centre works with women who have experienced female genital mutilation as well as women transitioning and war victims with genital trauma.
‘People don’t realise that female genital mutilation occurs every 16 seconds and it is happening even here in Australia,’ she says.
Her dream is to expand Desert Flower nationally and to recruit a team of young specialists and establish FBW clinics in Iran and Vietnam.
She hopes the Telstra awards will inspire other women to work for change they believe in – particularly migrant women and those in her Iran who are fighting for social change.
‘I want to give back and inspire these women to work hard with kindness and tenacity,’ she says.

medicSA | 26
ACCOLADES
New labs to explore cancer links
South Australian researchers will lead international studies into inflammation and cancer.
South Australia’s capability in immunotherapy is set to receive a significant boost with three new laboratories in the South Australian Immunogenomics Cancer Institute (SAiGENCI), led by internationally recognised researcher Professor Brendan Jenkins.

After working in the US and as the Head of the Centre for Innate Immunity and Infectious Diseases at the Hudson Institute in Melbourne, Prof Jenkins will move to SAiGENCI in July. He has already begun the quest to attract the world’s best and brightest minds to establish the new labs in Adelaide.
The three new labs, each staffed with between 10 and 15 people, will focus on basic discovery and translational research in innate immunity and inflammation, adaptive immunity, and immunotherapy, in a quest to understand the role of the immune system in treating some of the most lethal cancers.
‘From a scientific perspective, the fact that SAiGENCI is a brand-new medical research institute being built from the ground up was very appealing, as well as being part of something new and driving a culture of research excellence,’ says Professor Jenkins.
The aim is to fill a gap in research and discovery around cancer inflammation, the immune system and immunotherapy in South Australia and to collaborate with other researchers and clinicians, also working towards biobanking of clinical samples (such as patient tumours, serum and plasma) to help validate foundational research.
‘Discoveries based on basic research ultimately underpin clinical trials, so my research program will be about making those discoveries related to the immune system and cancer that can be translated through our clinical connections,’ he says.
Prof Jenkins is particularly interested in
the role of the immune system in stomach, lung and pancreatic cancers. His research will investigate manipulations of the immune system, including making tumours more visible to cancer-killing immune cells and changing the inflammatory response to stop cancerous tumours from developing.
‘These are among the most lethal and common cancers in the world and represent at least one third of all cancers with a link with chronic inflammation – for example, gastritis and stomach cancer, pancreatitis and pancreatic cancer, hepatitis and liver cancer.
‘There is a very strong association between inflammation and cancer, driven by uncontrolled activation of the immune system’, Prof Jenkins says.
‘We’re looking at how we can modify and activate various cell types in the immune system to target these cancers.’
He says current immunotherapies based on immune checkpoint inhibitors and more recently CAR T-cells are not effective on many prevalent cancers.
‘Immune checkpoint inhibitors have only been around for the last decade and at the moment the current immunotherapy drugs are still very limited to a few protein targets.
‘We can’t rely on the very few check point inhibitors that make up immunotherapy currently. We need to understand more about the innate and adaptive immune systems where we can identify new targets of the immune system that can be used in therapy.
‘We’ve only scratched the surface into how we can modulate the immune system to benefit a patient with cancer. Being at the early stages is exciting, because there is scope to do cutting-edge research to better understand how the immune system drives these cancers and how we can put the brake on these cancers by altering the immune system.’
While SAiGENCI has a government establishment grant to help recruit the best researchers in the field, there is also a need to attract external funding. Professor Jenkins will be bringing grants from the US Department of Defence to research stomach cancer and pancreatic cancer, but the drive for more independent funding will be ongoing, he says.
‘Current funding in Australia for basic medical research is just dire,’ he says. ‘The federal government has been great at putting in millions of dollars for the Medical Research Future Fund for clinical or translational research, but unfortunately NHMRC funding for basic research discoveries which ultimately underpin translational research is inadequate.
‘Researchers spend so much time on their computers writing grant applications – when you only have success rates around 10% with many excellent grant applications being unsuccessful because of a lack of available funding, most people are just wasting their valuable expertise writing grants they may never get.
‘There is an absolute need to increase the funding for basic research in Australia especially in cancer research, which will eventually lead to new clinical trials.
‘One of the beauties of the establishment grants that SAiGENCI has is that it does offer up to five years for research positions. It is a very good incentive to recruit people to the state because it gives them some job stability over the short term.’
medicSA | 27 IN PRACTICE
Professor Brendan Jenkins
A bumpy ride
Doctors have a major role in minimising the impact of on-field concussion injuries, writes South Australian Sports Medicine Association CEO Danielle
Grant-Cross.
The outcomes of on-field collisions in recent Australian football matches have brightened the spotlight on how concussion should be identified and managed. Sport-related concussion affects athletes and participants at all levels of sport, from the part-time recreational athlete to the full-time professional. Increasing concerns about the incidence and possible health ramifications have reinforced the need to diagnose and manage concussion safely and appropriately.
Every year in Australia more than 3,000 people are hospitalised after being concussed playing sport, and it is estimated an additional 9,000 players are concussed but do not seek medical attention. Brain Injury Australia estimates as many as 30,000 players won’t report their concussion to teammates, coaches or family because they fear being removed from play. A cultural shift is required as this often invisible injury is ignored.
Doctors are at the forefront of managing concussion, in clinics and hospitals and on the sideline when assessing injuries. Obvious issues for treating doctors include understanding the current best practice to manage these injuries, the time it takes to treat these injuries effectively and managing pressure from athletes, parents, clubs and players to permit the player to return to sport.
Legal cases relating to high-profile athletes’ concussion injuries have increased awareness of concussion and the potential links with chronic traumatic encephalopathy (CTE) and other serious outcomes. This has led to extensive discussion around diagnosing and treating the injury, the rehabilitation process and return to sport decisions. Different sporting organisations have their own concussion policies and varying levels of medical support on the sideline. The lack of consistency can lead to confusion and ultimately affect the injured athlete.

With children and adolescents, a conservative, individualised approach to diagnosis and management is recommended due to a slower rate of recovery. It can be difficult to navigate
between the player/patient, parent, and education provider, with the medical practitioner playing an important role here. A ‘return to play’ or ‘return to learn’ letter can be used by doctors.
Some players and coaches may not be aware of the dangers related to concussion and therefore push to minimise the injured player’s time away from the game. The ’if in doubt sit out’ message requires more support, and the use of high-profile ambassadors will add value to changing attitudes and practices. Increased education will help doctors and other sideline medical support (sports trainers, first aid and first responders) manage the pressures of those around them.
Dr Marc Cesana and Dr Karthik Badrinath – both part of the medical team supporting the Adelaide Football Club –say the role of the doctor in managing
concussion must be to protect the player.
‘In the AFL, athletes have more exposure to concussion education and therefore have increased awareness of concussion and support the diagnosis and any precaution around treating concussion,’ Dr Cesana says.
‘AFL coaches and support staff are also educated about concussion management and are always supportive of medical advice.
‘Community and amateur sport may not have a medical team supporting their club. Many clubs and teams do have accredited first aid or sports trainers or volunteers on the sideline who are critical in recognising concussion injuries and referring to a doctor who understands concussion management.’
Dr Badrinath says 95% of concussion
Source: https://www.sportaus.gov.au/__data/assets/pdf_file/0005/683501/February_2019_-_
medicSA | 28 IN PRACTICE
Concussion_Position_Statement_AC.pdf
Return to Sport Protocol for children 18 years of age and under
symptoms are resolved in between 10 and 14 days, especially with appropriate recognition and management. But a small number of concussion injuries require more complex management and referral to doctors with relevant expertise.
The challenge, Dr Badrinath says, is that there is no test that can diagnose concussion with 100% certainty. Tools such as the SCAT 5 assess symptoms, but honest, comprehensive reporting by the athlete is central to the diagnosis.
They say issues can arise when players, sports officials and parents do not understand or recognise concussion symptoms beyond the headaches and dizziness that commonly are associated with the condition.
‘The best management is recognising the potential for a concussion injury and removing the player from the game immediately, without returning to play until they have received appropriate assessment.
‘If concussion symptoms are not recognised and acted on there is the risk of short, medium or long-term consequences.’
Dr Cesana says some of the technology and practices employed by the AFL may be adapted for use at the local level.
Adelaide Football Club concussion management
• Medical staff are attentive and watch the incidence in real time.
• Medical staff watch the replay vision on the sideline with the technology available.
• Look out for certain signs, loss of consciousness, staggering, inability to retain their balance and with any of these areas identified the person is presumed concussed and cannot return to play.
• Any possible concussion is assessed, including using a SCAT5 test, in a quiet place away from the sideline.
• The replay vision is often reviewed again in the rooms.
• Doctors discuss the vision and review the baseline concussion testing to identify whether the player appears concussed.
• The player does not drive home and has someone stay and observe them overnight.
• The next day, the club doctor reviews the player, who is advised to rest for between 24-48 hours.
• Players are monitored daily by the club doctor.
Return to play protocol is split into
three phases – REST, RECOVERY and RETURN TO FULL ACTVITY.
• A normal SCAT 5 is required to move from the rest phase into the recovery phase.
• A further normal SCAT 5 is required to move out of the recovery phase and into the return to full activity phase.
• Contact training cannot start before a Cognigram test is undertaken to compare post-concussion performance to their pre-season baseline.
• A player can only return to the game when all phases are completed with no recurrence of symptoms and the test results return to baseline.
• Other information can be obtained from family or housemates that live with the player.
• A player will be cleared to play only when the doctor is happy with all stages of protocol and a detailed discussion has taken place with the player. Short, medium and long-term risks must be discussed with the player.
• An individualised approach is needed as symptoms can differ between people and according to age and gender. The Community Concussion program is soon to be rolled out across South Australia. The aim is that by 2026, sporting
codes will have adopted concussion protocols to ensure clubs and their officials, parents, players and sports trainers have a clear role in understanding and identifying the impact of concussion, acting appropriately to minimise further risk, and seeking medical assistance to reduce long-term impacts. Concussion policies and procedures will be automatically adopted, and actioned without hesitation with medical and sporting organisations agreeing to a consistent approach.
There is much work to do in this space and we are all aware of the ongoing concerns in relation to identifying concussion, the management and framework, referral and rehabilitation back to school, work and sport.
For more information about sportrelated concussion visit:
Australian Sports Commission Guidelines
• Concussion in Sport – Position Statement
• Sport-Related Concussion Treatment Pathway
• 5th International Conference on Concussion in Sports consensus statement
New courses for concussion management
The latest guidelines on sports-related concussion will be released in mid-2023, following the 6th International Consensus Conference on Concussion in Sport (ICCCS) held in the Netherlands in October 2022. These guidelines from the world’s concussion experts will be used to develop updated concussion guidelines for sport in Australia and around the world.
The SA Sports Medicine Association (SASMA) has received funding from the Office for Recreation, Sport and Racing to deliver a concussion education program over the next three years. A Concussion Steering Committee has been established to guide the development of the program. A focussed effort is required to align Australia’s sporting and medical organisations’ policies and procedures, based on the ICCCS latest report, and create a consistent approach to managing concussion.
Adelaide Football Club Doctor Marc Cesana, says that updated concussion education could increase doctors’ knowledge and confidence in diagnosing and managing concussion injuries, recognising it is potentially not commonly seen in general practice.
It is proposed that practical support will be offered to general practice to help identify the injury using the current SCAT 5 tool and the latest international guidelines and guide concussion management and rehabilitation protocols. GPs interested in attending the concussion management workshops should contact SA Sports Medicine Association.
medicSA | 29 IN PRACTICE
Concussion complexities
Adelaide-based neuroscientist Professor Robert Vink says general practitioners and other health practitioners involved in contact sports must ensure they are informed about the latest research into traumatic brain injury and its links to concussion.
Prof Vink says recent research provides ‘irrefutable evidence’ that there’s a link between repeated concussions and the potential for developing chronic traumatic encephalopathy (CTE),’ Prof Vink says. ‘But there are still questions over how to manage players who demonstrate symptoms and behaviours associated with concussion, and especially those who have been repeatedly concussed.
CTE is a progressive and fatal brain disease associated with the accumulation of a protein known as hyperphosphorylated tau that affects cognition and behaviour.
In February, the Boston University CTE Center announced that it had diagnosed 345 former National Football League (NFL) players with CTE among 376 former players studied.
‘Everyone reacts to concussion differently, and GPs and others must recognise that,’ Prof Vink says. ‘Research has shown that 20 per cent of people don’t recover in 12 days. We know children take longer to recover. Girls take longer to recover.
‘It’s the ones who have persistent symptoms who we think are at risk of developing CTE.’
‘We’re asking GPs and other health professionals to become educated about the symptoms and behaviours that indicate a player has not recovered from the concussion and if there are persisting symptoms, then the player does not return to play until a health professional has provided the OK.
Professor Vink is a University of South Australia neuroscientist whose interest in sport-related concussion came through
his background in traumatic brain injury (TBI) research and the long-term consequences of TBI. He is the immediate Past President of the International Neurotrauma Society and the current Chair of the Board of Connectivity: Traumatic Brain Injury Australia.

‘I have always been puzzled as to why players with an injured knee will not return to the field for two or three weeks – or whatever the accepted medical recommendation is for that injury – but when a player injures their brain, there’s a rush to get them back on the field,’ Prof Vink says.
‘Fortunately, that’s changed. But we are still in need of strict rules and guidelines that prevent a player returning to the field after a concussion, and especially repeated concussions.
‘We need guidelines that recognise that each person must be managed individually, according to their symptoms and behaviours.
‘Players’ long-term health must trump any short-term desire for on-field success.’
As recently as 2019 professional sport was reluctant to accept that CTE was linked to TBI incurred during sports contests. The Australian Sports Commission’s 2019 Concussion Position Statement noted that ‘there is currently no reliable evidence clearly linking sport-related concussion with (CTE)’ and suggested that studies ‘have not adequately controlled for the potential contribution of confounding variables such as alcohol abuse, drug abuse, genetic disposition and psychiatric illness’.
But four years later, Prof Vink says, there is no doubt. Even the Australian Government is convinced: the Senate Community Affairs References Committee is due to report in June 2023 on what it learned from witnesses and submissions to its inquiry into sportsrelated concussion.
‘Concussion in sport is not a new phenomenon and despite occurring over decades and being very poorly managed
relative to modern standards, we do not see an epidemic of CTE in the community, either in Australia, the US or anywhere else in the world,’ he says.
There is mounting evidence. Prof Vink says post-mortem studies have shown that donated brains from US professional football (NFL) players have a CTE incidence of 99%. This falls markedly to about 8% when brains are randomly selected and all US football exposure is included (amateur youth, high school, college and professional NFL), suggesting that professional NFL football is a major contributor to the high incidence of CTE in US football.
US research has also shown an incidence in all athletes of less than 5% while the general, non-athletic population had a CTE incidence of approximately 1%.
‘Presumably, the general population sample included cases of domestic violence, assault, exposure to explosive devices and epilepsy, all of which can also result in CTE,’ he says.
‘A much smaller Australian study reported an incidence of 57% in donated brains of professional athletes who played in sports with risks of repetitive head injury, and markedly lower incidence of CTE in the general population.
‘In summary,’ he wrote in his submission to the Senate inquiry, it seems clear that repetitive head injury in professional football athletes is a major risk factor for CTE development.’
Prof Vink’s research, published in Scientific Reports in 2021, found that a single concussive episode does not activate the biochemical pathways that have been linked to development of CTE. At least three concussive events are required to activate these pathways, and even then, if there is sufficient time for total brain recovery between concussive events, these CTE pathways are not activated.
‘With concussion, we saw recovery quite quickly. But with repeated concussion, there was not such quick recovery.
medicSA | 30 RESEARCH
A South Australian neuroscientist is calling for concussion to be manged as carefully as all other sports injuries.
medicSA | 30
Biochemical things were happening in the brain. These things, as it turns out, are associated with CTE,’ he says.
‘It is allowing time for total recovery from concussion that is the critical factor in reducing the likelihood of CTE.’
In the Scientific Reports paper, Prof Vink and his colleagues show how repeated concussions can cause CTE and a way to block it with a specially developed drug.
‘Tau protein tangles are a feature of CTE, which reportedly leads to memory problems, confusion, personality changes, aggression, depression and suicidal thinking,’ Prof Vink says.
‘Our research shows that by blocking substance P with a specific drug, we can prevent the tau protein tangles from developing in the brain and causing neurological problems.’
The treatment was successfully tested in animal models, giving hope that CTE can be prevented in humans.
He says the treatment has been proven
safe in phase 1 trials and is ‘ready to go’. However, trials cannot proceed until a biomarker is found that will enable its efficacy to be tested on living people suspected of having CTE.
‘We’re just waiting for the development of a surrogate marker for CTE a living person. Once you have that, you can look at the effects of the drug on the marker.
‘But there’s a lot of research, especially in the US, looking for that blood biomarker.’
For now, Prof Vink says, concussion must be managed using best-practice guidelines customised to the individual and their symptoms. He says everyone involved in sport – players, coaches, teachers, managers and health practitioners – should be educated to identify and manage the symptoms of concussion, and to understand the risks if it is not managed correctly.
He also advises that players be required to complete a course to ensure they
understand the risks and are less likely to insist on competing too soon after a concussion, and agrees that a ‘national concussion registry’ be established to record incidents and their management and to track brain health over time.
He says Connectivity offers courses to educate people about CTE and the risks posed by repeated concussions.
‘I don’t believe any sports administrator wants to see a player injured or at greater risk of brain damage in later life, Prof Vink says. ‘I think they just need more education.
‘With GPs and health practitioners providing informed guidance, and acceptance of the very real danger of repeated concussions, you can reduce the incidence of CTE.’
Information about Connectivity Traumatic Brain Injury Australia courses and other education and research programs is available on its website
Red area shows where the brain is inflamed, which has been shown to occur after concussion

medicSA | 31 RESEARCH
The road to recovery
The inclusion of advance recovery room care has been shown to have significant impacts on post-operative outcomes, writes Professor Guy Ludbrook.
Access to surgical care, and indeed other forms of healthcare, is likely to be unavailable in a timely manner unless initiatives are found that can be shown to improve outcomes at sustainable costs.

Surgery is needed to treat something like one-third of healthcare conditions, yet increasingly long waiting lists were an issue even before COVID. The aetiology is complex but is contributed to by factors including the needs of an ageing comorbid population and economic challenges.
If we turned to just one economic indicator of the future challenges in health care it might be the rapidly climbing old-age dependency ratio in developed populations. A population with more elderly people, and fewer productive younger people, faces the same sustainability challenges as a pyramid investment scheme.
Mechanisms outside health to address this pyramid, and its consequences, include to increase birth rates and immigration. Mechanisms within health include a focus on improved population health and preventative healthcare, but also must include high-value (improved outcome and manageable costs) in surgery and perioperative care.
System redesign in surgery and perioperative care
A group of clinicians and quality and safety organisations, led by CALHN and the University of Adelaide, staged a National Summit on 6 March 2020 to examine what is needed. Attended by 80 key stakeholders and opened by the South Australian and federal health ministers, the Summit identified eight principles on which to base improvement.
Advanced Recovery Room Care
At the Royal Adelaide Hospital (RAH) we were aware of a high incidence of early post-operative complications in recovery rooms and the wards, and we had some pilot data to suggest brief high-acuity care might help. We were also aware of a paucity of evidence of benefit of postoperative high acuity units.
We then designed a system of pre-operative risk identification and stratification of medium-risk patients, with referral of medium risk patients to an anaesthesia-led multidisciplinary model of 24 hours of high acuity care. This Advanced Recovery Room Care model, ARRC, adopted seven of the eight Summit Principles – we see inclusion of primary care, Principle 3, as an important future priority. The results of a prospective study of ARRC were published in May 2023, and demonstrate a very large positive impact.
What we found
The key findings are shown in the figure from JAMA Surgery 2023 In addition:
• there was no evidence of a shift in burden to primary care
• there is a possible halving of mortality at three months post-surgery; 12-month figures will be reported separately in the literature
• formal cost-effectiveness Markov modelling shows that ARRC is ‘better and cheaper’, and identifies what should be priorities to provide further improvement.
medicSA | 32 RESEARCH
What we learned
The exact individual mechanisms behind the benefits of ARRC are not certain, but what we feel is important is:
• excellent communication between craft groups before, during and after surgery
• pre-operative formal risk stratification and triage for all scheduled cases
• active management from arrival in recovery, the time when adverse events are most frequent
• avoiding hypotension and precisely assessing and managing fluids – the dangers of hypotension and fluid under- and over-load are well understood for end organs such as the kidney, bowel, brain and heart
• collection of relevant data on outcome and cost – it takes six weeks for return on investment from ARRC (late effects on re-admissions, rehab care etc) and we see patent outcome effects out to at least 12 months.
Perceived risks
We know this ARRC model provides benefit at the RAH. It should be, and is being, considered or started in other jurisdictions in Australia and NZ. It is, however, seductive to believe all existing or planned high-acuity units will provide the same benefit. We know there is a large range of capacities in existing high acuitytype postoperative units. The model we use has very strict requirements with very high compliance – poor outcomes with imperfect compliance with existing peri-operative models such as ERAS are now well described
Parallels with TGA processes for therapeutic goods should be considered. Alternatives to proven products which are not shown to have ‘substantive equivalence’, should be carefully studied prior to routine adoption.
Next steps
The success of the ARRC model is just one example of how we can start to address the hidden pandemic of complications and cost facing surgical care.

Following the success of National Summit I, which engaged stakeholders and generated the Principles which underpinned ARRC, Summit II is planned for 13-15 July, again in Adelaide. It has speakers from key stakeholders across Australia, but is intended to harness expertise and existing ideas through an interactive format. We welcome all to come and share their ideas. Details are available at https://thehiddenpandemic.com
Summit Principles
1. Consumer-centric: planning/goals based on consumers’ expectations, needs and values, informed through evidence; individualised to risk.
2. Risk stratification mitigation: formal risk assessment; risk: identified, matched to pathways, with mitigation strategies.
3. Primary care: preventing complications starts with primary care; systems with excellent communication/coordination; cost-effective modes of care.
4. Systems thinking: systems re-engineered with: best evidence, minimal variation, and focus on STEEEPTM. Quality measured and benchmarked.
5. Value-based proposition: Value (outcomes vs cost) as the ultimate focus, with value for all stakeholders.
6. Evidence-based care: Evidence underpinning all care; systems regularly reviewed, and gaps addressed in a structured manner.
7. Performance measures: To guide value, performance capturing structures, processes and outcomes; measures are: consumer-relevant, risk-adjusted, benchmarked, factored into initiatives, openly shared, formally acknowledged.
8. Communication and accountability: shared decision making; clear communication, documentation, and accountability throughout the journey; information accessible to all.
medicSA | 33
Professor Guy Ludbrook with his team
AI for accuracy
Artificial intelligence is being applied to assist in as many aspects of medicine as it is in other sectors, with benefits for practitioners and patients.
It’s early days but artificial intelligence (AI) applications are dramatically improving the personalisation of medical treatment, improving the accuracy of diagnostics and robotic surgery, and driving administrative efficiencies.
South Australia is positioned to become a leader in the application of AI in health – but more needs to be done to provide the regulatory environment and to foster an innovation ecosystem, says Professor Seyedali Mirjalili, director of the Centre for Artificial Intelligence Research and Optimisation at Torrens University Australia.
‘AI can be very helpful, especially when you are dealing with high volume of data that humans are not capable of understanding and analysing. It is being used a lot in imaging – CT, Xray and MRIs – it can look into the history of millions of other images and learn how to recognise complex patterns such as tumors and provide
quantitative assessments of radiographic characteristics,’ explains Professor Mirjalili.
‘The other main use I am excited about is the use of AI in robotic and telesurgery. The AI algorithm helps the surgeon perform the procedure, and the robotic system can be much less error-prone than humans, especially in minimally invasive surgery.
‘AI systems can efficiently evolve over time and transfer the learning to other AI systems accurately and quickly – unlike humans, who can take a lot longer to learn new techniques and teach it to others.’
Professor Mirjalili says that in an age of increasing medical complexity and cost, AI has the potential for administrative efficiencies, providing 24/7 advice for patients through the use of smart chatbot technology such as ChatGPT (Chat Generative Pre-trained Transformer), and for scheduling appointments.
Australian AI innovation to help measure brain atropy
Australian researchers have used artificial intelligence to develop a world-first benchmark for measuring brain atrophy in neurodegenerative diseases, including Alzheimer’s disease.
Assessing the onset and progression of Alzheimer’s using MRI has traditionally been challenging as changes in the thickness of the brain's cortex are often in the sub-millimetre range.
Advanced machine learning techniques are routinely used in brain research to assess changes in cortical thickness, but until now, a lack of a clinically accurate ‘ground truth’ dataset meant we could not evaluate their sensitivity to the detection of small atrophy levels.
Scientists from CSIRO and the Queensland University of Technology have used machine learning to produce a set of artificial MRI images of brains with predefined signs of neurodegeneration in the cortex region, the outer layer of the brain most affected by Alzheimer’s.
Prior to this breakthrough, published in Medical Image Analysis, the only way to get a ground truth measure of cortical thickness was by studying the brain post-mortem.
This new technique allows researchers to set the amount and location of brain degeneration they want to compare against so they can get a clear picture of what method of cortical thickness quantification performs the best.
The technique can test the sensitivity of methods to a miniscule level. It can determine whether a method can detect changes in thickness of just 0.01 millimetres.
The technique can be applied to research in any brain disease that involves neurodegeneration, representing a significant step forward to better understanding dementia and other debilitating brain diseases. It can also potentially be used to predict the level of cortical degeneration a person can expect over time.
The synthetic dataset images have been made publicly available so clinicians and scientists can use the synthetic images to conduct their own assessments of cortical thickness quantification methods.
medicSA | 34
RESEARCH
AI is already helping automate doctors’ workflow and improve efficiencies through converting text to voice and automated data mining from different sources, he says.
One of his research projects at the private Torrens University, based in Adelaide, involves building an AI system to facilitate the early detection of mental health conditions in children, so they may be referred to psychiatrists.
The research team is building a system that uses large data sets to identify the probability of a child having, for example, an 80% chance of attention-deficit/hyperactivity disorder (ADHD), based on the parents’ responses to a standardised questionnaire.
The next step will be to build a database of text and video to help with another layer of diagnostics, with the final objective of commercialising the system.
Professor Mirjalali predicts more use of AI in precision medicine, providing treatments based on a person’s unique genes and proteins, by using AI to analyse large data sets.
“Typically, treatments are based on cohorts and groups,’ he says. ‘But we are unique as humans and diseases develop uniquely in our bodies, and there is always a unique solution. AI can hyperpersonalise medical treatment.’
AI is also being used to analyse large amounts of data to identify drug targets and optimise the end design of clinical trials.
South Australia, with its growing international reputation as a site for clinical trials, is well positioned to be a leader in AI applications for health, says Professor Mirjalili. But, he adds, there is more to be done to foster collaboration between technology companies, researchers, regulators and healthcare providers. He says the state government has shown a commitment to invest in AI and digital health, with initiatives such as the Digital Health Cooperative Research Centre and the creation of a dedicated AI hub. Major entities and organisations such as the Australian Institute for Machine Learning, MIT big data living lab, Google cloud, and Amazon AWS are part of the conversation.
‘Adelaide is attractive because of the city’s high-tech capabilities and world leading data ecosystems, supported by universities that are making significant progress in this space, leading in international research,’ he says.
‘We need to have all the players working together to accelerate the development of AI and its adoption.
‘With recent concerns about cyber security, we need better policies in place to ensure that data is used ethically and responsibly – and that includes regulation around data sharing, data storage, and data access.
‘We also need guidelines and policies to ensure AI is used ethically, adhering to patient autonomy and non-discrimination.
The fuel of AI systems is data, and if data is biased towards a gender or race, the outcome of the AI will be biased too.’
Ensuring that the application of AI is transparent – rather than a black box with data in and recommendations out – is an important piece of the adoption puzzle, says Professor Mirjalili.

Standardisation and interoperability of systems to enable the integration of new and existing health systems, and a culture of innovation, will also be vital.
‘Medical professionals should not be afraid that they will lose their jobs,’ he says. ‘AI will make their jobs easier, so we will see gradually machines do the leg work and humans do the tasks that require special skills such as strategic decision making, persuasion and caring.’
EASTERN SUBURBS VR GP
Hazelwood Clinic is a well established GP owned and operated practice.

We are seeking a VR GP to join our busy Eastern Suburbs practice – 2-4 sessions per week to full-time.
We are a private billing practice with well equipped consulting rooms and a friendly and supportive medical, nursing and admin team and value a respectful team environment.
We provide a wide variety of medical services including onsite Spirometry, 24 Hour blood pressure monitoring, Holter monitor and ECG
Enquiries to Jenny Lambert, 0419 409059 or email jennylambert@hazclin.com.au
medicSA | 35 RESEARCH
Professor Seyedali Mirjalili
Research briefs
Unblemished skin may be sun-damaged
A University of Queensland study has found skin with few visible freckles or blemishes may still carry sun-damaged DNA mutations that can trigger cancer.
Researchers investigated the relationship between the number of mutations found in ‘normal looking’ skin and the number of a person’s past skin cancers

Lead author and PhD candidate Ms Ho Yi Wong said the findings show Australians can have a high number of mutations in skin they think looks normal.
The study of skin samples from the forearms from 37 skin cancer patients had an average four to five times more mutations in normal-looking skin compared to similar studies overseas –possibly due to Australia having at least twice the amount of ultra-violet light than the United Kingdom and Europe.
The study next matched people of the same age and sex who had a different number of skin cancers and found a 45% difference between the groups, with a much larger number of mutations on the forearms of those with more skin cancers.
The findings explain in part why people with a single skin cancer have a much higher chance of developing others in the same area of the body.
Funding for detecting silicosis research
Monash University has secured funding of over $400,000 across two projects to improve early screening and detection of silicosis, an incurable and deadly occupational lung disease caused by breathing in silica dust.
The project aims to obtain a unique biochemical profile of the body’s response to silica, to develop a signature of ‘biomarkers’ in exhaled breath.
Monash Biomedicine Discovery Institute’s (BDI) Head of Respiratory Pharmacology Associate Professor Jane Bourke plans to test a number of drugs to reverse scarring of the lungs and has developed a model for testing silicosis drugs in human tissue.
‘We will take microscopic slices of tissue from human lungs, donated but not used for transplantation,’ she said. ‘We will expose them to silica dust and inflammatory protein cocktails found in the lungs of silicosis patients to cause lung damage and scarring.
‘This will mimic the environment in the silicotic lung. Then we can test two anti-fibrotic drugs (already approved and shown to be effective in another lung disease) and two promising novel in-house drugs to target inflammation and fibrosis in silicosis.’
Key to fighting inflammation in severe COVID-9 cases
A University of Queensland-led study into how immune cells respond to the COVID-19 virus is helping develop treatment to prevent runaway inflammation in patients with severe COVID-19.
The study found most immune cells which contribute to chronic inflammation are not infected with the SARS-CoV-2 virus. Uninfected cells - macrophages - detect damage and death in neighbouring cells and trigger a strong inflammatory response.
Anti-inflammatory drugs are currently given to hospitalised COVID-19 patients after the virus has peaked, to mitigate the overactive immune response but the drugs make patients susceptible to secondary infections.
The IMB research team is investigating how to selectively target macrophages without compromising the body’s ability to fight against the virus, in order to reduce the incidence of severe COVID.
With the new understanding of how macrophages work, the researchers aim to design anti-inflammatories that can be administered earlier, to prevent inflammation getting out of control.
The researchers say this is a way to future-proof against new variants of COVID-19 and also future pandemics and infections.
medicSA | 36
e-skin breakthrough
Scientists at UNSW Sydney have combined artificial synapses with advanced sensors to mimic the properties of human skin, in new research published in Advanced Functional Materials

Inspired by the human skin, researchers have developed an electronic device w able to detect mechanical stimuli for information processing, including gesture and handwriting recognition, with ultralow power consumption.
In biological nerve systems, sensory organs such as skin can detect stimuli and the generated signals can then be transmitted to the human brain via neurons and synapses for processing and eventually, response.
“People can feel pressure, pain, and interact with the surrounding environment through physical contact via the skin,” says Professor Dewei Chu, lead author of the study.
“Our system is proposed to mimic the functionality of the human skin, and several skin-like capabilities have been demonstrated.”
“The electric current that powers our device corresponds to the strength of the connection between two neurons. And we applied electric stimuli to control the device conductance to emulate human synaptic behaviours,” says Prof. Chu.
The complete system consists of the neuromorphic computing device, combined with highly responsive sensors.
The sensors can detect subtle human motion and monitor physiological signals.
Cure for MND closer
Research at The University of Queensland is a step closer to viable treatments, and ultimately a cure, for motor neuron disease (MND).
In their paper in Molecular Psychiatry, researchers have identified biochemical changes in a protein that is affected by MND.
They ran two research projects looking at how TDP-43 proteins, essential in the health of motor neurons, become dysfunctional.
They found diseased versions of TDP-43 can damage healthy versions of the protein, which may create a cycle of protein dysfunction and degeneration over time.
It also discovered that biochemical pathways which control neuron death are triggered early, even before MND symptoms begin.
The authors say pharmaceutical drugs that can prevent neuron death and this TDP-43 protein dysfunction are needed to change the course of the disease.
Researchers are now treating genetically modified mice with MND with different pharmaceutical drugs that specifically target the underlying causes of the disease, and correct the disease mechanism.
Arterial stiffness novel factor
Arterial stiffness may be a novel risk factor for metabolic syndrome in teens, a paper published in the American Journal of Physiology-Heart and Circulatory Physiology concludes.
Metabolic syndrome is the constellation of three or more of abdominal obesity, insulin resistance, hypertension, and hyperlipidemia. Metabolic syndrome increases the risk of worsening obesity, type 2 diabetes, cardiovascular disease, and premature death.
A new risk factor for childhood and adolescent metabolic disease such as obesity and insulin resistance is arterial stiffness. This risk factor is being established as a potential cause of type 2 diabetes among adults globally. However, it is not clear whether arterial stiffness causes metabolic syndrome.
The study of 3,862 adolescents aged 17 years who were followed up until age 24 years found worsening arterial stiffness was associated with a 9% risk of metabolic syndrome in males but no statistically significant risk among females.
Arterial stiffness potentially caused metabolic syndrome; however, metabolic syndrome did not cause arterial stiffness. The pathway through which arterial stiffness caused metabolism syndrome could be partly explained by an increase in fasting insulin (12% contribution) and low-density lipoprotein cholesterol (9% contribution).
medicSA | 37
From fiction to fact
New medical evidence shows consuming cranberry products is an effective way to prevent a urinary tract infection (UTI) before it starts, confirming folklore.
A global study looking at the benefits of cranberry products published in Cochrane Reviews, has determined cranberry juice, and its supplements, reduce the risk of repeat symptomatic UTIs in women by more than a quarter, in children by more than half, and in people susceptible to UTI following medical interventions by about 53%.
Medical scientists from Flinders University and The Children’s Hospital at Westmead looked at 50 recent trials that included almost 9,000 participants.
The studies included a range of methods to determine the benefits of cranberry products. The vast majority compared cranberry products with a placebo or no treatment for UTI.
They determined drinking cranberries as a juice or taking capsules reduced the number of UTIs in women with recurrent cases, in children, and in people susceptible to UTIs following medical interventions such as bladder radiotherapy.
Senior author Professor Jonathan Craig, Vice President and Executive Dean of the College of Medicine & Public Health at Flinders University, says the real benefits of cranberry products became clear when the researchers expanded the scope of the review to include the most recently available clinical data.
‘This is a review of the totality of the evidence – and as new evidence emerges, new findings might occur. In this case, the new evidence shows a very positive finding that cranberry juice can prevent UTI in susceptible people,’ Professor Craig says.

‘We have shown the efficacy of cranberry products for the treatment of UTIs using all the evidence published on this topic since the mid-1990s.
‘The earlier versions of this review didn’t have enough evidence to determine efficacy and subsequent clinical trials showed varied results, but in this updated review the volume of data has shown this new finding.’
The authors say while most UTIs are usually effectively treated with antibiotics, they can be recurring in some people. Cranberry products provide a harmless form of prevention.
They conclude that while cranberry
products do help prevent UTIs in women with frequent recurrence, more studies are needed to further clarify which people with UTI would benefit most from cranberry products.
This new evidence might be particularly useful given recent concerns raised by the medical profession about the potential overuse of antibiotics in treating UTIs following trials to allow pharmacists to prescribe antibiotics for ‘uncomplicated UTIs’.
Omega -3 key to preventing early births
New guidelines call for the monitoring of pregnant women’s omega-3 fatty acid status.
Pregnant women with low levels of omega-3 should have their omega-3 fatty acid status monitored and provided with supplements to prevent premature births, according to new pregnancy care guidelines.
The latest National Health and Medical Research Council (NHMRC) and Department of Health National Pregnancy Care Guidelines say there is evidence that women with a singleton pregnancy with low serum levels of omega-3 fatty acid are at higher risk of early preterm birth. Supplementing the levels of omega-3 among women with low levels of the fatty acid reduces their risk of early birth.
The advice is based on a Cochrane systematic review of more than 70 randomised controlled trials of almost 20,000 women with mainly singleton
pregnancies. The review indicated that omega-3 supplementation from early to mid-pregnancy until birth resulted in a reduced risk of:
• early preterm birth by 42% (from 46 to 27 per 1,000 births)
• preterm birth by 11% (from 134 to 119 per 1000 births).
The guidelines recommend that GPs conduct screening and supplementation from early-mid pregnancy until birth.
SA Pathology and the South Australian Health and Medical Research Institute (SAHMRI) are evaluating the implementation of the omega-3 guidelines recommendation, with the aim of reducing the number of early preterm births.
The omega-3 status test can be performed on the same sample as the First
Trimester Screen, at no additional cost, through the South Australian Maternal Serum Antenatal Screening (SAMSAS) Program.
The test can be ordered by ticking the box on the maternal serum screening test form.
This form is available online here or via the template available in medical software (latest version, accessible here).
Omega-3 status test results will be reported to the requesting provider as standalone report and will also be available on OACIS. Results of the omega-3 status will come with associated recommendations on whether to supplement or not.
medicSA | 38
RESEARCH
PhotoiStock, Yuriy Gluzhetsky
Report notes value of VAD option
The reflections provided to the Voluntary Assisted Dying Review Board by patients and family members have reinforced the importance of VAD as an end-of-life option in South Australia.
Board Presiding Member Associate Professor Melanie Turner said the patients’ and family members’ comments demonstrated that VAD provided ‘relief from suffering for patients and comfort for the bereaved’.
Assoc Prof Turner was speaking as the first Voluntary Assisted Dying (VAD) Quarterly Report was released on 7 June.
Between 31 January, when South Australia’s VAD laws took effect, and 30 April, 28 South Australians received a VAD permit. Of these, 12 people died, including one who died without using the medication available.
They were aged from their 40s to their 90s. Seven had terminal cancer and five had degenerative neurological conditions.
Eight people self-administered medication, and three were supported by
medical practitioners.
On average, the length of time from making a first request to access VAD and receiving an outcome on an application for a permit was 25 days. For all 28 permit applications, the Chief Executive of Department for Health and Wellbeing provided a decision within the three-day timeframe required by the Act.
The next phase of the program will involve expanding services in regional areas.
Assoc Prof Turner urged clinicians to consider registering for training, ‘so they too can support South Australians with the care they may need, no matter where they live in the state’.
The report indicates there are 60 medical practitioners who have completed the mandatory training, with a further 45 registered or part-way through. Of these, 29% are based in regional South Australia. Feedback from family members highlights the importance of trained, considerate clinicians at the end of life.
Virtual home care
A new digital health project will use virtual care and telemonitoring to support people with chronic disease in low socio-economic areas to reduce pressure on crowded hospitals and GP clinics.
The $1 million project led by Flinders University, ‘safe@home’, aims to provide affordable and effective primary care services to reduce emergency department and hospital admissions, GP clinic waiting times and ambulance ramping.
The project will link SA Health and other agencies including the Northern Adelaide Local Health Network, the Adelaide Primary Health Network, Australian Telehealth Society, Digital Health SA and Integrated Cardiovascular Clinical Network SA.
Professor Robyn Clark, from the Flinders College of Nursing and Health Science says
the project will focus on creating a robust primary care framework for people living with high needs, such as heart failure, diabetes, hypertension and chronic obstructive pulmonary disease (COPD).
‘Along with providing quality care in the home setting, we aim to improve the every day quality of life for these patients by giving them more regular health checks and access to professional help,’ says Professor Clark.
‘The clinical decisions and actions taken based on information obtained by monitoring will alter patient wellbeing and outcomes.’
The new project will engage and train clinicians across disciplines (doctors, nurses and allied health) in both hospital and primary care to create a new digital health workforce.
Comments included:
‘The doctor’s visit was more than we could have hoped for, she was kind and compassionate as well as being professional and respectful of my husband’s wishes. At each visit it was stipulated that my husband was in control of this process and could stop it at any time if he chose.’
The laws include many safeguards to ensure only eligible people can access VAD and protect vulnerable people from coercion, abuse, and exploitation.
VAD is available for people who meet strict criteria, including having an incurable, advanced and progressive disease, illness, or medical condition expected to cause death within 6 months (or 12 months for a neurodegenerative condition), and that is causing suffering to the person that cannot be relieved in a tolerable manner.
The quarterly report can be viewed here and more information about South Australia’s Voluntary Assisted Dying laws can be found here
Home telemonitoring and virtual care will involve consumers in their model of care and give them incentive to increase their self-care and self-monitoring to manage their conditions.
It also will be used to develop a business model using routine Medicare item numbers for primary care and a framework for scaling into routine care, including refinement of the interfaces with the electronic medical records and patients’ clinics.

medicSA | 39 RESEARCH
STOP PRESS
PhotoiStock, Erdark
With lofty ideals
Flinders
Flinders University and Flinders Medical Centre are named after the British navigator and explorer Matthew Flinders. His was a life of discipline, youth and adventure – lessons for us all.
Student days
In early 1974, a group of students assembled outside the Sports Centre. We were the inaugural class in Medicine at Flinders University. The university had begun as an offshoot of Adelaide University only 10 years earlier, and then assumed its own identity.
Setting up a medical course was the brainchild of Professor Peter Karmel, the first Vice-Chancellor of Flinders University and a Professor of Education. Karmel’s mantra was ‘experiment and experiment boldly’, and his legacy is perpetuated in the ‘Karmel Endowment Fund’ that supports research endeavours throughout the university.
Of course, as 17-year-olds straight out of school, we did not know any of this. In the second year, when mature age students were accepted, they provided seniority and good balance to our obvious youth.
Much of the construction and ethos of the school was overseen by the founding Dean, Professor Gus Fraenkel, but my earliest memories are of commencing studies ‘up the hill’ in the School of Biological Sciences. This was because at that stage the medical school was just a shell, still under construction.

There was a bare site for the construction of the new school. Professor Fraenkel’s basic premise was to combine teaching, research and clinical medicine in the one location. This was a lofty
ideal that was largely realised. He attracted talented teachers, researchers and clinicians from around the world.
The calibre of the research can be seen in the standing of the work produced and grants obtained over recent decades. There is a thesis that good research underpins good clinical practice, and this proved to be the case.
Like many courses of the day, our program was a general introduction to Biology, Chemistry and Physics. We were lectured by Jo Orbach (biology), Professor Malcolm Thompson (chemistry) and Professor Alex Hope (physics). I recollect practical classes where we distilled DNA and operated on rats for neuroanatomy.
In second year, we made our way to the medical school, one step behind the builders. A medical library was constructed, along with an anatomy laboratory/museum and a series of cubicles adjacent to the library for student study. It was all new and exciting.
Professor Fraenkel espoused the links between research, teaching and clinical care. He was of German origin, educated in Oxford, spent time in Hamilton, Ontario, where he obtained the advanced model for Flinders, and Dunedin; and then he was head-hunted to move to Adelaide.
Really though, I am getting ahead of myself – the need for another major hospital in Adelaide was perceived by the government of the day when Sir Thomas Playford was the premier. His was a Liberal Government, but that changed when Mr Donald Dunstan became Premier.
Construction started on the site of an old tuberculosis sanitorium. There are photographs of Mr Dunstan ‘turning the first sod’ astride a large Caterpillar tractor – just hidden behind him is the actual operator.
However, it is teachers who make a medical school, not buildings. The novelty of this new medical school attracted people from all over the globe. I wonder if they knew what they were getting into? They came to southern Adelaide in remote South Australia from Europe, America and Africa.
These were very talented people, but what really characterised their teaching was a strong personal interest in the students and delivering the best teaching possible.
Given the vast array of talent and teaching, what became of us all? I focus on a photograph taken at the graduation of the final class, which shows that 42 doctors graduated from an initial class of 64. I don’t think this could have been anticipated from the outset, and it makes me wonder about the selection of students. Of course, students change and develop, some gravitate to different fields, while others have their initial choices confirmed. Many became practitioners of medicine and there have been countless outstanding careers among the graduates.
medicSA | 40 NEWS
University was founded with the spirit of innovation and curiosity that motivated the man after whom it was named to explore the oceans, writes the author of a new book about the medical school, Dr David Wattchow.
Dr Wattchow’s graduating class outside the lecture theatres. He has attempted to identify and locate the class members, as below: (Back row, from left) ophthalmologist Peter Ingham, psychiatrist and geriatrician Geoff Seidel, surgeon Greg Otto, psychiatrist Deborah Blood, GP and anaesthetist Richard Watts, Tauny Southwood (Professor of Paediatrics (Rheumatology), Birmingham, UK), Gawler GP Rupert Thorne, Jamie Cooper AO (Head of ICU, Alfred Hospital, Melbourne), ophthalmologist John Glastonbury (Queensland), Hamilton GP Mike Forster, Di Campbell, physician Robert Van Den Burg (SALHN),GP Gary Shanks, author David Wattchow, dermatologist Lachlan Warren (WCH), ophthalmologist Paul Runge (returned to US), GP Steve Deller, GP Robert Pegram, Kate Burgess (Indigenous and women’s health), GP and psychiatrist Kingsley Wood, psychiatrist Peter Papay, liaison psychiatrist Rob Gribble (Alfred Hospital, Sydney)

(Middle) GP and surgeon Arnold Seglenieks (Millicent and New England), Chris Baggoley AO (former Chief Medical Officer of Australia), GP Dorothy Jones, GP Jenny Wood, GP Val Luckman (then Summers), GP and bariatrics surgical assistant Helen Patroney, GP Julie Forsyth, anaesthetist Suzy Szekeley, GP David Sare (Byron Bay)
(Front): GP Steve Byrne, neurologist Heather Waddy, orthopaedic surgeon Mike Sandow, Claude Wischik (Professor of Neurophysiology, Cambridge, UK, before moving to Scotland), dentist and oral surgeon Paul Duke, GP Deborah Pfeiffer (later involved in breast cancer screening), GP Robert McIver, psychiatrist Marion Catford (then Drennan)
Absent: anaesthetist Wendy Graham (Germany), psychiatrist David Kelly, Craig Shearing

As a member of the inaugural class of the Flinders Medical College in 1974, the medical school at what is now Flinders University has always had a big place in my heart.
When it (and I) began, the medical school was somewhat of an experiment, as Flinders University had only just formed a separate entity from the University of Adelaide. Now, nearly 50 years later, the experiment can be seen as successful. My book gathers my recollections of my time and experiences at Flinders University (School of Medicine) and Flinders Medical Centre (FMC). ‘As the twig is bent, so grows the tree’ is a proverb that refers to the shaping effects of early childhood, on personality and career. I have expanded its use here as I have detailed the influence of Flinders on my career, from my time as a neophyte student through to research training, specialist training and my life as a consultant surgeon. The memories are laced with humorous anecdotes along the way. Necessarily my history leads on to my recollections of training in surgery, and in research. I also reflect on the special roles of the clinicians’ special purpose fund, the Deans and CEOs and on philanthropy.
This work has opened the processes and world of popular publishing to me. It has made me realise what is involved by way of structural considerations and editing. While it has become apparent that the publisher makes the real profit, any earnings from this publication will be donated to the school’s research efforts.
- Dr David Wattchow
medicSA | 41 NEWS
Dr Wattchow operating in FPH
Christine Mausolf President

With the welcoming of our first years and now junior committee, the Flinders Medical Students’ Society (FMSS) has been able to start staging many of our pre-clinical events. The sporting rivalry between MD1 vs MD2 students began with our sports night continued with our annual netball game on campus. The MD1s came in very enthusiastically, with home-made banners and lots of crowd support, however for the first time in two years the MD2s took home the trophy. This is a great way for the two cohorts to get to know each other and find common interests outside medicine. Our FMSS Vice President External, Angelina Arora, organised an International Women's Day Stall in the library, handing out purple ribbons and bringing awareness to the day and what it means for women in medicine and more broadly in society.


We have also welcomed the new cohort of clinical science students, helping them orientate to the unfamiliar world of Flinders medicine and university life – it can be a daunting proposition when you have just finished high school. Finally, working with the Australian Medical Student Association (AMSA), Tom Cliffe (FMSS Senior AMSA representative) has marked the start of our annual Vampire Cup. Here, medical schools across Australia compete to donate the most blood and plasma from 1 April to 28 May. Red Cross visited the library to encourage students to donate and answered any questions they had, and assisted them in booking their next visits. As students we soon become aware of the significance blood donations have in health care, with one in three Australians needing blood products. The Vampire Cup initiative has been a great way to encourage students and their families or friends to donate, sometimes for the first time - and hopefully not the last. We encourage anyone who is eligible to donate.
FMSS also focuses on student advocacy, with one of our goals for the year being better integration with the NT medical students and a focus on the health of First Nations people. We are proud to announce better representation within the FMSS committee with four First Nation students assisting us with advocacy and events this year. Having spent 14 months in the NT on placement, I have been able to work closely with the FMSS NT students and with them develop a better plan for integration of resources and student integration; we hope to implement the plan in 2024. We are also looking forward to staging more online academic and information nights together, as well as better integration for advocacy.
With First Nations health as a focus, we were excited to work with our Indigenous representatives to release ‘Closing The Gap’ merchandise for students to purchase. FMSS has also hosted its inaugural First Nations communication workshop. Due to its success we hope to continue hosting it in the years to come.
It has been a pleasure returning to the vibrant campus at Bedford Park in Adelaide, with lectures and placements as well as social events in full swing. I am very grateful for the time I spent in the NT and would like to encourage more students and doctors to consider working in Alice Springs and Darwin and the surrounding communities. My experiences have been like nothing I have been exposed to previously, reshaping the way I view medicine and healthcare and how my own values sit within this new perspective. With the help of FMSS NT, I hope to further share my learnings with the students in South Australia and form a stronger alliance between the states.

medicSA | 42
UNIVERSITY MEMBERS
FLINDERS
International Women's Day stall
MD2 Netball team MD1 netball team
Vi-Seth Bak President

The start of the year has whizzed past us and the University of Adelaide’s medical students find ourselves at the business end of semester 1.


Our first full-scale MedCamp in three years was held across the weekend of 17-19 March. The joy around the return of this much-cherished event was matched by the backdrop of blue skies and amazing sunsets from atop the campsite’s hills above Normanville. Our first-year students made the most of the opportunities to get to know each other and learn from workshops including suturing, plastering, and blood pressure taking, run by several student clubs. Organisers of the James Bond-themed Jazz Night were less lucky with the weather, but the heavy drizzle could not deter students determined to enjoy the music played by their peers’ bands. Coats were donned and ponchos were handed out, and the medical student spirit and good times prevailed.
The inaugural Adelaide Medical Students’ Association’s Careers Conference, held at the Adelaide Convention Centre in late March, gave students an opportunity to broaden their horizons and network with like-minded attendees and presenters. Attendees heard from a fantastic program of speakers including Professor Paul Kelly, Professor Helen Marshall, Dr Vijay Roach and AMA(SA)’s own Dr Chris Moy and Dr Hannah Szewczyk.
In the upcoming month, we are hosting the first event of which we hope will be an exciting start for a new student interest group focussing on clinical ultrasound. We have recently seen a great desire from students to develop their knowledge and skills in this
increasingly important modality. With the help of Adelaide Health Simulation and their cutting-edge equipment and facilities, we hope this group will create much needed opportunities for students to learn and further their ultrasound skills to improve their future clinical practice.
With exam time around the corner, our EdPrograms team has been hard at work organising revision lectures and high-quality mock OSCEs for our fourth- and fifth-year students. These endeavours can involve well over 100 student volunteers acting as examiners and SPs across each day, and are held in the same simulation centre, using the same advanced B-line simulation recording and review technology, with which students will be examined in their real assessments.
Approaching rapidly is the introduction of changes to PGY1 and PGY2 medical training under the new AMC Prevocational Training Framework. The framework is being introduced nationally from 2024. This year’s medical school graduating classes will be the first cohorts to train as junior doctors under the new scheme, which reframes term requirements for PGY1 and imposes term restrictions on PGY2. Assessment also receives an update, with a later introduction of Entrustable Professional Activities and e-Portfolio into the framework. These are significant changes, and the AMSS is working with SAMET to communicate to students, particularly those graduating this year, the implications of this new framework for them. The monitoring of any issues that arise with the implementation of the new framework is likely to be a part of DiT advocacy over the coming years.
medicSA | 43
ADELAIDE UNIVERSITY MEMBERS
A plastering workshop
Final-year students at MedCamp
Your Super, your choice
New laws for public sector fund.
The information in this Promotional Feature contains general advice and is provided by Hood Sweeney Securities Pty Ltd, AFSL 220897, ABN 40 081 455 165. That advice has been prepared without taking your personal objectives, financial situation or needs into account. Before acting on this general advice, you should consider the appropriateness of it having regard to your personal objectives, financial situation and needs. You should obtain and read the Product Disclosure Statement (PDS) before making any decision to acquire any financial product referred to in this Promotional Feature. Please refer to our FSG (available at https://www.hoodsweeney.com.au/assets/general-assets/Hood-Sweeney-Securities-FinancialServices-Guide.pdf) for contact information and information about remuneration and associations with product issuers.
For medical professionals in the South Australian public health sector, it's important to have a superannuation fund that aligns with your specific financial goals & objectives.

Under new laws that took effect in Nov 2022, members of the Super SA Triple S superannuation fund, including doctors in the public health sector, can now choose the superannuation fund they wish to contribute to
Until the new laws were enacted, public servants were required to be members of one of Super SA's superannuation funds Medical professionals can now consider which superannuation fund is appropriate for them
In addition to helping you navigate superannuation funds, Hood Sweeney Securities (AFSL 220897, ABN 40 081 455 165) can also help you review your existing investments and discuss ways to optimise your portfolio for growth and stability
Senior Financial Planner and Representative of Hood Sweeney Securities Pty Ltd

AFSL 220897
ABN 40 081 455 165
daman.arthur@hoodsweeney.com.au
Jackson Harvey Financial Planner and Representative of Hood Sweeney Securities Pty Ltd


AFSL 220897
ABN 40 081 455 165

jackson.harvey@hoodsweeney.com.au
We work with you to develop a comprehensive financial plan that considers your current income, expenses, assets, liabilities, and long-term financial goals
Contact Hood Sweeney Securities to schedule a FREE consultation with a financial planner.
| Promotional Feature |
Daman Arthur
www.hoodsweeney.com.au
Answering the call
Adelaide clinicians, backed by generous donors, are performing lifechanging plastic surgeries and training local staff to correct burn and bear injuries in Bhutan.
The small mountainous country of Bhutan will soon have its only plastic surgeon – a specialist trained through a fellowship sponsored by Interplast at Adelaide’s Queen Elizabeth Hospital.

With bear maulings and terrible burns from kerosene cooking fires common place in Bhutan, the fellowship addresses a significant need, says Adelaide plastic surgeon Dr Tim Proudman AO, who has long been part of the program.
After a four-year hiatus due to COVID restrictions, an Australian team of specialists, including Dr Proudman, other surgeons, anaesthetists, hand therapists and nurses, will visit the country. In the interim, Dr Proudman, his wife Dr Susanna Proudman, the Interplast team and many generous donors have raised around $160,000 for the program.
The team will take its own equipment to manage a backlog of cases for a week-long stint in June and another two-week stint in October, developing the skills of local medical staff.
‘We’ve been going for many years but with COVID it all stopped. In the interim we’ve been working towards training the fellow, Dr Sonam Jamtsho, in plastic and reconstructive surgery and he has been at the TQEH since February,’ says Dr Proudman.
‘Sonam is coming with us in June and the idea is that he will return to Bhutan next year to establish plastic and reconstructive surgery there.
‘Treatment for burns in Bhutan is very limited – it’s a very rural country with most people living in the foothills of the Himalayas in areas very difficult to access by road. They often travel by mule and they use kerosene for cooking and heating.
‘There are a lot of burns, especially of small children, and they finally come to our attention when they have developed contractures. Staff generally don’t know how to debride the
wound and prevent contractures. That’s where there is huge unmet need.’
Facial injuries caused by black bears are also challenging.
‘The danger is that Sonam will be overwhelmed by the unmet need. We need to expand the program and bring on more surgeons to develop their skills and develop a functioning service that meets the needs of the local people,’ says Dr Proudman.
While there are several major hospitals in Bhutan, many patients are seen in remote clinics and Interplast Australia helps to provide clinical support through email and training via ZOOM, as well as providing regular visits from Australian specialists.
Dr Proudman says working with Interplast has demonstrated the need for visiting clinicians to relate simply with local staff and patients and establish what they think is important rather than making assumptions. Most of the medical staff have learned English at school, which helps build relationships.
‘Bhutan is an interesting country culturally – it’s a monarchy with a Gross National Happiness Index. They are very adherent to their traditional cultural mores. It’s a very equal society; doctors get paid the same as cleaners and they have a different way of working. You have to respect that people do things differently’, he says.
‘People sometimes think of plastics as being about aesthetics, but you really appreciate what a difference it can make to people’s lives when you can repair an injury or congenital defect that has a significant impact on a subsistence lifestyle.
‘Many of the patients we see are farmers who depend on their being able to perform manual labour. In a place where they don’t have much welfare, it completely changes lives if they are able to resume or start working.’
People can help support the program by contacting Interplast
MEMBERS
1
Mystery Tour
International magician and illusionist Matt Tarrant bewildered his audience at the AMA(SA) Gala Ball on 20 May. For more about the Ball, see page

1. Dr Patrick Kennewell and Dr Louisa Edwards

2. Madeline Porter and Alexandra Talbot of Norman Waterhouse


3. Dr Lakshmi Nath and Dr Shriram Nath

4. Front L-R: Alexandra Talbot, Anastasia Gravas, Thomas Tagirara, Alexander Belperio, Li-shern Sim ; Back L-R: Madeline Porter, Stefanie Magliani, Lincoln Smith, Divya Narayan, Marissa Mackie
5. Dr Michelle Atchison, Dr John Williams and Associate Professor William Tam

6. Kelli Blakely and Adam Blakely
2 3 4 5 6
medicSA | 46
SOCIAL
7. Benita Rajvi, Angelina Arora, Kevin Huang, Christine Mausolf, Chelsea Gosden and Dr Hayden Cain


8. Illusionist Matt Tarrant and Dr Catherine Skinner

9. Dr John Williams and Joanne Thompson

10. Dr Ben Teague, Dr Nimit Singhal and Dr Deepti Singhal
11.

medicSA | 47 SOCIAL 11 10
9 8 7
Former AMA(SA) Executive Board Chair Dr John Nelson (second from right) with Selene Clark, Georgia Nelson, Cathy Nelson and Tom Nelson
The inaugural Australian Medical Students’ Association (AMSA) Careers Conference was held at the Adelaide Convention Centre on 29 and 30 March. It brought together 250 medical students and 30 speakers from around the country to showcase the diverse career paths possible after graduating from medical school, and to help students prepare for the workforce. The conference concluded with a cocktail night at which students could network with each other and conference speakers including former AMA Vice-President Dr Chris Moy and Australia’s Chief Medical Officer Professor Paul Kelly.
1. Panellists Dr Claire Demeo and Dr Sam Paull


2. Chief Medical Officer Professor Paul Kelly being interviewed by AMSA volunteer Ashraf Docrat
3. Kylee Nuss, Dr Abby Moore, Dr Jessica Martyn, Dr Lloyd Weird, Dr Harry Gaffney and AMSA volunteer panel chair Jasmine Davis

4. Former AMA Vice-President Dr Chris Moy and AMSA President Tish Sivagnanan

5. The Networking Cocktail Night

6. AMA NSW President Dr Michael Bonning, AMA Council for Doctors in Training Chair Dr Hannah Szewczyk, Jasmine Davis and AMA(SA) DiT Chair Dr Hayden Cain

medicSA | 48 SOCIAL
3 5 6 1 4
2
2
The Royal Flying Doctor Service’s (RFDS) staged its annual ‘Wings For Life’ Gala Ball at the Adelaide Entertainment Centre on 20 May, with 1,000 guests attending for an ‘Out of this World’ experience. More than $290,000 was raised to support the RFDS’s program for the purchase and replacement of the ‘flying intensive units’ that help the organisation provide care to the most remote areas of the country.






1. Sue Arlidge, Angelique Galea, Dr Sally Cole, Annabel Smith, Dr Jessica Martyn, Chris Green (RFDS), Mandy Smallacombe, Adrian Smallacombe, Dr Susie Keynes
2. Event photo
3. Tony Vaughan ASM, Premier Peter Malinauskas, the Governor of South Australia, Francis Adamson AC, and Peter de Cure AM
4. Leanne Liddle, Professor Jonathan Craig, Health Minister Chris Picton, Jaqueline Goodall and Connie Blefari
5. Dr Mardi Steere and Andy Steere
3 4
medicSA | 49 SOCIAL
6. Event photo 5
6 1
On the beaten track
Size matters when handling rough terrain, writes Dr Robert Menz
Having recently tested the smallest Toyota, I was lucky enough to spend a week in the biggest one.

LandCruisers have been around since 1951 but were first seen in Australia in 1958 when Thiess Bros imported a dozen to assist with the construction of the Snowy Mountains Hydroelectric Scheme. The story goes that Thiess was so impressed with those early LandCruisers that he lobbied Toyota to become the official distributor and the LandCruiser then became the first Japanese vehicle to be regularly exported to Australia. Toyota still uses Australia as its main test bed for the LandCruiser, given the variety of harsh terrains and also huge variety of road quality.
The 300 series was introduced in 2021. It has proved so popular that the waiting time for one is now about 12 months. The test vehicle was a middle-of-the-range VX. All 300s are mechanically the same with a 3.3 L twin turbo V6 diesel delivering 227 kW and 700 nM through a 10-speed automatic gearbox to all four wheels.
The GX retails for just under $100,000, increasing to just over $150,000 for the GR Sport. The VX sits right in the middle at $125,000.
The VX is very comfortably appointed, including many of the
luxuries and safety features found on most luxury cars. Even the GX is equipped with smart entry and keyless start, Apple CarPlay, digital radio, climate control air conditioning, reversing camera and safety issues including lane departure alert with brake to steer (which does take a bit of getting used to but is a very positive safety feature).
Upgrading to VX adds sidesteps and roof rails, wireless phone charging, front and rear parking sensors, rear cross traffic alert, auto levelling headlights, heated and ventilated front seats and a sunroof.
The top-of-the-range Sahara ZX also adds a hands-free back door with kick sensor, rear torque sensing LSD, adaptive variable suspension, a cool box between the front seats, dual rear seat entertainment screens, heated and ventilated second row seats. heated steering wheel and 20-inch alloy wheels with appropriately low-profile tyres not necessarily an advantage for off-road driving. And five seats rather than seven.
One of the really neat features was the large, double-hinged bin between the two front seats that can be opened by the driver or the front-seat passenger. The dashboard is a traditional two-dial affair, and the large central touchscreen screen can be used to control most of the infotainment. There are buttons under the air
medicSA | 50 MOTORING
conditioning vents that also manage some of these functions.
As with all Toyota vehicles there is a five-year unlimited kilometre warranty. There is also a further two years of engine and driveline warranty provided the vehicle has been maintained as per the service book, and three years of complimentary access to Toyota Connected Services that provides stolen vehicle tracking, automatic collision notification and an SOS emergency call function. Toyota has a capped fixed price service program for the first five years or 100,000 km at $375 per service but these need to occur every six months or 10,000 km, whichever comes first.
This large four-wheel-drive is not a particular convenient city car. Even with all the cameras and alarms I found it difficult to park in standard carparks. The boot is huge and Toyota claims 2000 L of storage space with the middle row of seats folded down. The car is also massive: over 2 1/2 tonne, nearly 5 metres long and a shade under 2 metres wide and high. However, this makes for superbly comfortable driving. Around the city, speed humps can be ignored and on country roads it’s a matter of setting the cruise control and selecting your favourite podcast or music Apple CarPlay. If you’re not concentrating and approach the white line at the edge of your lane not only does the steering wheel vibrate but the car brakes and loses about 5 km/h, which is the ‘brake to steer’ function mentioned above. Many folk will buy these for towing, and the big ’Cruiser is rated to 3.5 tonnes.
The only annoying quirk to this otherwise fabulous machine was the factory-fitted side step, which I found to be quite narrow and not especially helpful when climbing into the vehicle.
I managed more than 1,000 km in the week I had the ’Cruiser. This included a trip to Port Augusta and Quorn. I drove through Balaclava and Blyth, past Wirrabara, and then turned left to traverse the bridle track described as suitable for novice 4WDrivers. www.alltrails.com/explore/recording/bridle-tracklower-flinders--2. I recommend taking a passenger as there are several gates.
The initial several hundred metres were quite interesting as it had been raining and the uphill section, though not particularly steep was slippery and muddy and challenged the 300. In low ratio and with the central differential lock there were occasions when all four wheels were spinning and the big ’Cruiser simply slipped sideways into someone else’s tracks. Traction would have been improved with proper off-road tyres, but this option was not fitted to the test vehicle.
The view from the top is fabulous and being a clear day I could see Ports Pirie, Bonython and Augusta, as well as the nearby Port Germein gorge.
The following day, with family and including my granddaughter safely strapped in her car seat, we drove to Quorn for a walk around the little known Quorn Native Flora Reserve https://www. frc.sa.gov.au/__data/assets/pdf_file/0038/879743/Quorn-Flora. pdf, which preserves some of the local vegetation in this interesting transition zone between the hills with its slightly

higher rainfall and the arid Willochra plain to the north. We followed this with a visit to the Main Street playground then coffee and delicious home-made scones at the delightful Teas on the Terrace. www.teasontheterracequorn.com.au
I also managed a work trip to Murray Bridge via Mannum Falls for a picnic lunch and an overnighter to Victor Harbor.
In summary, the latest LandCruiser really does deserve the moniker ‘King off the Road’.
- Dr Robert Menz is a GP and enthusiastic motorist. Any members who would be interested in sharing the pleasure of test driving and writing about new cars are welcome to make contact through the AMA office.

medicSA | 51
MOTORING
Dr Rosemary Anne Jones
MB ChB FRCOG FRANZCOG
1938 - 2023
Dr Rosemary Anne Jones, better known as Rosie, was born Robert Anthony Jones in Worcester, England, 17 November 1938.* The youngest of three children, Rosie recalled being an avid reader as a child and quite the scholar of Latin. She attended Shaftesbury Grammar School in Dorset and graduated when she was 16 years old, subsequently studying medicine at the University of Bristol.
After graduating in 1962, Rosie worked in several hospitals around Bristol where she met and married her first wife. They then went to Uganda, Rosie working as a government medical officer at Kabale Hospital in Uganda from 1965 to 1967.
It was while in Uganda that Rosie first developed an interest in obstetrics and gynaecology. She returned to the UK for a few months before moving to South Africa in March 1968; there, she took up a position as registrar in anaesthetics, obstetrics and gynaecology at Edendale Hospital in Natal.
From 1970 to 1973 Rosie was registrar in obstetrics and gynaecology at the Groote Schuur Hospital in Cape Town. She was a staunch opponent of apartheid, working in hospitals that mostly treated black and coloured patients, and she even attended African National Congress meetings. Rosie returned to the UK in 1973 where she held positions as research fellow then senior registrar in obstetrics and gynaecology at The New John Radcliffe Hospital in Oxford.
In 1974, Rosie saw an advertisement in the British Medical Journal for a locum role in Dubbo, New South Wales, which offered excellent pay. Rosie successfully applied and immigrated to Australia with her family in October 1974, and she worked as regional senior specialist for the Dubbo and Orana region for almost five years.

In late 1979 Rosie moved to Port Adelaide and set up a private practice, later moving to North Adelaide, where she continued to practise until her death. In tandem with the private practice, over the years Rosie held roles including as senior visiting medical specialist at Queen Elizabeth Hospital, board member of LeFevre and Port Adelaide Hospital, senior visiting medical specialist at Lyell McEwin Hospital, and senior visiting medical specialist at Queen Victoria Hospital’s Mid Trimester Abortion Unit. Rosie had two proud claims to medical fame. One was her research and work prescribing hormone replacement therapy for menopausal women. The other was her pioneering work in performing Australia’s early, and South Australia’s first, laparoscopic surgical procedures in 1989.
From 1996, Rosie also worked with Dr Rob Lyons at the South Australia Gender Dysphoria Unit, prescribing affirming hormones for trans clients and also performing small procedures. In 2009 she was a founding member of the Australian and New Zealand Professional Association for Transgender Health (ANZPATH), which from 2019 became AusPATH.
Rosie was not just an advocate for trans health care; she was trans herself. Rosie was one of the earliest members of The Beaumont Society – an organisation for trans cross-dressers in the UK – and served as a trustee of the Beaumont Trust, founded in
1974 to educate the public about trans issues. She was a contemporary of Virginia Prince, one of the first transgender advocates, who published the ground-breaking magazine Transvestia. In 2004, Rosie made the decision to transition medically and began living fulltime as a woman. She described great support and affirmation from the hospitals, her patients and her family when she informed them. Rosie married her second wife as soon as same-sex marriage legislation was passed in Australia.
Rosie also had a long-term commitment to voluntary assisted dying (VAD), in part influenced by the death of one of her brothers. In 2005 Rosie became co-founder of the South Australian initiative Doctors for AMA Neutrality on Voluntary Euthanasia. This later expanded to become a national group, morphing into the present Doctors for Assisted Dying Choice. She was an ambassador for VAD in South Australia, and the legislation passed in June 2021 came into effect two days after Rosie’s death.
Throughout Rosie’s life she had a passion for classical music, and she was a strong supporter of the Adelaide Symphony Orchestra. Another of her passions was reading, and she belonged to several book clubs over the years, notably the George Hassell
medicSA | 52
VALE
Dr Rosie Jones as photographed for the book 100 Women
book club. She took great pleasure in gardening, supported several charities – mainly nature-based and wildlife campaigns – and was always broad-minded in her politics.
Rosie’s diverse human interests and professional endeavours have left a legacy of humanitarian and empowering work that gave individuals sovereignty over their own bodies. Rosie was complex, colourful and quite the character, memorable to all who met her.
Dr Rosie Jones died on 28 January 2023, aged 84. She is survived by her two daughters, Stephanie and Helen.
- Professor Noah Riseman of the Australian Catholic University, who interviewed Dr Jones for the Australian Queer Archives, provided this obituary on behalf of her family.

*It is generally considered best practice not to refer to trans people by their previous names unless they indicate that it is okay to do so. Rosie specifically requested that the photograph of herself pre-transition be in her funeral booklet. medicSA was asked by the family to include Rosie's previous name for this obituary.

medicSA | 53 VALE
Medical student Robert Jones at the University of Bristol
Dr Jones performing surgery at Groote Schuur Hospital, Cape Town, circa 1970
Dr Peter Wells
MBBS MRCGP 1936 - 2022
Peter Wells was born on 31 January 1936 in Adelaide, the eldest child of Harold and Irene. Harold worked as a clerk and his mother had emigrated to Australia from the UK.

Peter’s sister Pauline was born in 1940. Peter’s family life was simple as finances were tight. Travel was very local and infrequent and trips to the movies were big treats. With an English mother Peter and Pauline were taught good manners and taught how to dress and behave appropriately.
Peter was educated at Rose Park Primary School and later Adelaide High School. During these years he played the flute (encouraged by his father who was a talented flautist) and loved to play tennis. He performed well academically, and his father encouraged him to consider attending university despite knowing that this would put great financial stress on the family. Peter graduated from Adelaide High with one of the highest scores in the state and was granted a scholarship to study medicine at Adelaide University.
While at university he travelled around on a BSA Bantam motorbike. He would also ferry his mum on the back so that she could visit her mother in Lockleys.
Peter commenced his medical career at the newly finished and modern Queen Elizabeth Hospital. During this time, he attended a party with staff from the hospital and met his future wife, Pat. Pat recalls that she reluctantly attended this party as she was tired – her nursing friends insisted she come along. Mum describes that there was a lot of laughter and noise – she was sure patients in nearby wards must have heard the commotion. She met Dad, they married in 1960 and they remained happily together for 62 years. They only ever spent a night apart if a hospital admission necessitated they be separated.
Peter and Pat had three children: Stuart in 1962, Susan in 1965, and Richard in 1970. We were all encouraged to study hard and make the most of our education, and we all attained degrees in medicine or science. Peter expected us to maintain his standards
of punctuality, manners and having respect for all. He instilled in us that the number one priority was family and dropping other things to help other family members was of paramount importance.
Peter became a general practitioner, working in the suburbs around Marion and Glenelg. General practice at that time included obstetrics and minor surgery, and he was a sought-after GP anaesthetist. Pat recalls many nights when he would be called out multiple times to deliver babies and attend to emergencies at home. Before working in general practice, he worked as a government medical officer in Alice Springs, which included working with the Royal Flying Doctor Service. With her RN qualifications, Pat would sometimes accompany him on the plane journeys. He left this job after about a year as he didn’t like the bureaucracy in Canberra telling him what he could and could not do!
He also liked to stand up for those who were vulnerable. He and many of the other local GPs at the time volunteered as duty doctors for a month each year at the Kate Cocks Baby Home, where unmarried women would have their babies. The babies were quickly removed after birth and adopted out to married couples. Peter was compassionate towards the young women and cross when some of the other staff treated them poorly.
In his early years in general practice Peter was heavily involved in the local Southwestern Suburbs Medical Association as secretary and chairperson. He was also chairperson of SAPMEA. In these roles he followed the development of the Flinders Medical Centre and the new Flinders Medical School with great interest. Unlike many of his peers he was excited to see change and embraced the development of a new centre of medical excellence. His enthusiasm for the Flinders University Medical School contributed to the decisions by Susan and Richard to study medicine at Flinders University.
During the 1960s and ’70s Peter worked very long hours. In 1974
VALE
medicSA | 54
Peter Wells at 30 Euston Square, the London headquarters of UK College of GPs.
he felt burnt out and needed a circuit breaker. The family spent a year in Bristol, where he worked as a locum doctor and studied for and passed the UK MRCGP.
As he slowly relinquished obstetric and anaesthetic duties, Peter enjoyed teaching the next generation of GPs. He worked as a specialist GP in the Flinders Medical Centre emergency department, encouraging young doctors to consider general practice as a vocation, and he supervised GPs enrolled in the GP training program at his practice. He was delighted when Susan joined him in practice at Seacombe Medical Centre in 1991.
He remained enthusiastic about general practice but was concerned about the loss of obstetric, surgical and anaesthetic skills in city practices. He was, therefore, equally delighted when Richard chose a surgical career. Peter read medical literature extensively and made sure both of us kept our knowledge updated!

Over the next two decades Peter continued to love his work (his patients were very loyal, and he thought of many of them as special friends), his love of travel continued and he, Pat and sometimes other family members would travel to many parts of Australia and around the world. The UK was always his favourite place. He loved the quote ‘When a man is tired of London, he is tired of life’.
Peter retired at the age of 75. This was not an easy transition for him as work had always been such a significant part of his identity.

Life outside medicine
Peter also loved his cars and tractors.
He and Pat purchased an almond orchard at Sellicks Hill in the ’80s. They would spend many weekends enjoying the peace and learning a little about the tough world of agriculture. Here he bought his first tractor and was never happier than when he was out and about riding on it. Pat and Peter subsequently built their dream home on five acres in the Hills where he always had his tractor nearby to manage the property and slashing the grass was a pleasurable pastime.
After relocating to the suburbs just before he turned 70, he was overjoyed when Richard purchased a hills property, and a new tractor was available!
Nine grandchildren (now aged between 15 and 35) and one great grandchild (now aged one) brought great joy to Peter. Peter was the wise grandfather who was able to give all sorts of practical advice about life in general and his grandchildren savoured their time with him. Just five days before his death he celebrated Stuart’s 60th birthday with a family dinner and was excited to hear that a second great-grandchild was on the way.
Peter was a wonderfully loyal friend to many from all walks of life. He gave speeches at many weddings and was asked to give eulogies at multiple funerals. He and Pat travelled widely, both with family and with many groups of friends they had met here and abroad over the years.

Health issues in recent years resulted in frailty and coupled with the restrictions of the COVID-19 pandemic slowed his activities. Nonetheless he remained living at home with Pat until an acute medical event two days before his death. He remained sharp witted and continued to extensively read medical and other literature during these years.

medicSA | 55 VALE
Peter celebrating his 70th birthday at theSeacombe Medical Centre
Peter (centre) with his wife Pat, daughter Sue, and sons Peter and Stuart
RACGP Fellowship Ceremony 1993
Work laws to affect doctor employers
Changes to Fair Work legislation have implications for doctor employers, writes Norman Waterhouse’s Lincoln Smith.
On 6 December 2022, the landmark Fair Work Legislation Amendment (Secure Jobs, Better Pay) Act 2022 (the Amendment Act) received Royal Assent. The Amendment Act will implement changes to federal industrial relations laws, including the Fair Work Act 2009 (Cth) (the FW Act). The amendments to the FW Act are extensive and are occurring between 7 December 2022 and 6 December 2023.
In this article, Norman Waterhouse’s Employment and Safety team summarise some of the key changes brought about by the Amendment Act and how they will affect your workplace.

Fixed-term contracts
The Amendment Act aims to strengthen job security for workers and encourage secure and permanent employment. From 6 December 2023, employers will be prohibited from entering fixed-term contracts where:
• the contract is for two or more years
• the term of the contract and any renewal and extension in the contract exceeds two years
• there is an option to extend or renew the contract more than once
• the previous fixed term contract was for the same or substantially the same work
• there is substantial continuity of the employment relationship during the period of the new contract and previous contract.
There are some limited exceptions where a fixed-term contract of more than two years will be permitted. These exceptions include, among other things, if the employee is engaged during emergency circumstances or during the temporary absence of another employee (e.g., maternity cover). Importantly, employers will bear the onus of establishing that their fixed-term contracts are not in breach of the new requirements or are otherwise exempt.
Similar to their obligations to casual employees (as noted below), employers
also must provide a Fixed Term Contract Information Statement to employees who enter a fixed-term contract.
Employers should review their current fixed-term employment arrangements, with particular attention to the number of fixed-term arrangements implemented (i.e., how many previous fixed-term contracts have been issued to a particular employee) and the removal of renewal terms in those contracts.
Flexible working arrangements
The Amendment Act has implemented a more prescriptive process for an employer to follow if they receive an employee’s request for flexible working arrangements. Within 21 days of receiving a request, an employer must:
• approve the request
• have discussed and agreed to the requested work arrangement, or
• have discussed and refused the requested work arrangement and provided ‘reasonable business grounds’ for the refusal.
The Amendment Act also empowers the FWC to deal with disputes resulting from such a request. Employees will be able to commence proceedings in the FWC if the employer refuses their request or fails to respond within 21 days. The FWC will have broad powers to make a range of orders when arbitrating such disputes.
Other changes
‘Pay secrecy’ – clauses in current employment agreements will have no effect, and their inclusion in future employment agreements is prohibited. Further, employees have the discretion to disclose their pay and any other employment terms relevant to their pay.
‘Sexual harassment’ – sexual harassment in connection with work will be expressly prohibited, with employers now vicariously liable (unless particular exemptions are satisfied). The FWC can, on application by an aggrieved party, make a ‘stop sexual harassment order’.
‘Casual conversion’ – while not an amendment arising from the Amendment Act, the rights of casual employees in the FW Act were strengthened in the Fair Work Amendment (Supporting Australia’s Jobs and Economic Recovery) Act 2021. These changes were largely bolstered by landmark findings of the Federal Court of Australia in 2020 (and the High Court of Australia in 2021) regarding the nature of casual employment.
A casual employee is now defined in section 15A of the FW Act as a worker who is granted ‘no firm advance commitment to continuing and indefinite work according to an agreed pattern of work’.
Further, the FW Act now imposes a statutory obligation on an employer to offer casual employees the right to convert to permanent employment, where the employee:
• has worked for their employer for 12 months; and
• has worked a regular pattern of hours for at least six months on an ongoing basis, and
• could continue working those hours as a permanent employee without significant changes.
However, an employer is entitled to not make (or refuse) an offer for conversion on ‘reasonable grounds’, which includes where the casual employee’s position will cease to exist within the period of 12 months of the decision not to offer the conversion, or the employee’s hours of work will be significantly reduced during that period.
When engaging a new casual employee, employers must provide each new casual employee with a Casual Employment Information Statement as soon as practicable after the worker is employed, but ideally at the time of hiring.
For more specific information or advice regarding the changes and the impacts they may have on your workplace, please contact Lincoln Smith, Principal, on (08) 8217 1203 or at lsmith@normans.com.au
medicSA | 56 MEMBERS
Events
23-24 Jun
MEDCON23
Perth, WA
https://www.medcon.edu.au/
27 Jun
Specialist Medical Colleges Careers Expo 2023
Adelaide, SA
https://www.eventbrite.com/e/ specialist-medical-colleges-careersexpo-2023-tickets-586548902557
19 Jul
Service fees
Adelaide, SA
https://www.ama.com.au/sa/event/ service-fees
10-11 Aug
Royal Australasian College of Surgeons Tristate NT, WA & SA Annual Scientific Meeting
Darwin, NT
https://surgeons.eventsair.com/ tristate2023/
26-27 Aug
Rural Doctors Association SA (RDASA) Masterclass 2023
Adelaide, SA
https://rdaa.com.au/Aus/iCore/ Events/Event_display. aspx?EventKey=MC2023
19 Oct
Rural Medicine Australia (RMA) 2023
Hobart, Tas
https://rma.acrrm.org.au/program/ abstracts
If you are a not-for-profit organisation wanting to promote your major scientific or educational event please contact medicSA@amasa.org.au with details of your event including registration links for consideration of inclusion.

medicSA | 57 MEMBERS
Dispatches
2023 AMA(SA) COUNCIL MEETINGS
The next meetings of AMA(SA) Council will be held on Thursday, 3 August, and Thursday, 7 September, at 7 pm. Members may attend Council meetings as observers. If you are a member and wish to attend the May or June meeting, please call 8361 0100 or email admin@amasa.org.au
NEW MEMBER PORTAL
Have you logged in to the new AMA Member Portal? If you have forgotten your password, you can reset it here.
When you log into the portal you will be greeted by an onboarding process that allows you to update your details, choose how you would like to present yourself to other members, and indicate which networking and other experiences you are interested in.
Once you’ve had some time to get to know the portal, we hope you’ll share your feedback with us at www.ama.com.au/mp
AMA(SA) MEMBERSHIP RENEWALS
Please note that annual memberships of the AMA expired on 31 December 2022. If you wish to renew your membership or discuss details with our team, please email membership@amasa.org.au or call 8316 0108 before the office closes at noon on Wednesday, 21 December 2022.
A reminder that you can access your tax receipt by logging into your member portal on the AMA(SA) website (www.ama.com. au/sa) using your email address and password. Alternatively, please call us on 8361 0108 and our team will help you.
ACCESSING THE AMA FEES LIST
The latest AMA Fees List is available and can be accessed by AMA members at no cost at https://feeslist.ama.com.au/ using your login details.
HAVE YOUR CIRCUMSTANCES CHANGED?
If your place of employment, employment status or contact details have changed recently, perhaps because you’re no longer a student, you’re working part-time, or you’ve recently retired, please let us know so we can update your details.
If you’ve been a student member but are no longer a student, please let us know so we can upgrade you to a doctor’s membership. You’ll then have access to a range of additional state and federal benefits, including the Medical Journal of Australia (valued at more than $230) and the AMA List of Medical Services and Fees (valued at $499), which are not available to student members.
If you have any questions about your membership, please contact us at membership@amasa.org.au
Visiting Endocrinologist - Stirling Central Health Clinic
RICHARD HAMILTON MBBS, FRACS, plastic surgeon, wishes to notify colleagues that his private clinic Hamilton House Plastic Surgery is fully accredited under the rigorous Australian National Standards (NSQHS) for health care facilities and also by the American Association for the Accreditation of Ambulatory Surgical Facilities International (www.AAAASF.org).
Richard Hamilton continues to practise plastic and reconstructive surgery at Hamilton House, 470 Goodwood Road, Cumberland Park with special interests in skin cancer excision and reconstruction, hand surgery and general plastic surgery. He also conducts a ‘see and treat’ clinic for elderly patients with skin cancer. Convenient, free, unlimited car parking is available.

Richard also consults fortnightly at Morphett Vale and McLaren Vale, and monthly at Victor Harbor and Mount Gambier/Penola. He is available for telephone advice to GPs on 8272 6666, and readily accepts emergency plastic and hand surgery referrals. For convenience, referrals may be faxed to 8373 3853 or emailed to admin@hamiltonhouse.com.au
For all appointments phone Richard’s friendly staff at Hamilton House 8272 6666. www.hamiltonhouse.com.au
Expressions of interest are sought from an Endocrinologist wishing to provide clinical services in Stirling on a sessional basis. You will have access to a modern, fully furnished consulting room located alongside the Stirling Central Health Clinic. The number of sessions and days of the week are negotiable.
For all inquiries, please contact Warren Glasspool, Practice Manager on 8370 9777.
CHRISTOPHER WURM, MB BS FRACGP FAChAM, Addiction Specialist advises that he will consolidate his consulting to Sefton Park from July 2023 and continue facilitating workshops with the Black Dog Institute.
He has limited scope to see privately referred patients at CALHN Hospital Avoidance & Supported Discharge Service, Shop 5, 221 Main North Road, Sefton Park, Tue/Wed: Tel. +61 8 8342 8600, Fax +61 8 8342 0053.
He will leave Paragon Medical Centre and no longer offer driver’s licence assessments
medicSA | 58
MEMBERS
Member Services



You can find further information about accessing member benefits and services when logged into the AMA(SA) member portal



AMA(SA) preferred providers

medicSA | 59 MEMBERS

P: 0412 956 272 E: info@amasalending.com.au www.amasalending.com.au 1. AMA (SA) members are eligible for a cashback per application successfully settled during the promotional period. 2. Promotional period – The loan is lodged and settled between 1 January 2023 and 31 December 2023. 3. AMA (SA) members are entitled to receive the cashback in addition to any bank/lender cashback offers (if eligible). 4. AMA (SA) Members will be eligible to a cashback on home loans successfully settled during the promotional period as per the below schedule under the following conditions: i. Net loan value $400,000 - $750,000 receive $500 cashback. ii. Net loan value $750,001 – $1,500,00 receive $1,000 cashback. iii. Net loan value above $1,500,000 receive $2,000 cashback. 5. The net loan value used to calculate the cashback is calculated after considering any offset balances or redraw facilities, as AMA Finance Brokers receives their share of commission after the aggregator/licensee split on the net loan amount. 6. The eligible cash back is calculated on total consolidated loan value per loan settled. 7. The eligible cashback will be paid within 12 weeks from the date of successful settlement by AMA Finance Brokers directly to the member’s nominated bank account only. 8. Refer to the bank/lender cashback terms & conditions. ^Terms & conditions. GET UP TO $5K CASHBACK ON HOME LOANS Hartley Financial Pty Ltd. AFSL & ACL: 480751. ABN: 22 124 384 274. If you’re not an AMA (SA) member, join and you will receive the AMA (SA) cashback offer and the other benefits of membership. Net loan value $400,000 - $750,000, receive $500 cashback Net loan value $750,001 - $1,500,000, receive $1000 cashback Net loan value above $1,500,000, receive $2,000 cashback from the bank or lender (if eligible) on home loans successfully settled between 1 January 2023 and 31 December 2023.^ $2K CASHBACK ON TOP OF THE CASHBACK OFFER AMA members are eligible to receive up to