
Commissioning
Framework
Adelaide Primary Health Network
(Adelaide PHN)
December 2024










Framework
Adelaide Primary Health Network
(Adelaide PHN)
December 2024








This Commissioning Framework is a practical guide to shaping the health system to deliver better outcomes for vulnerable people and a healthier Adelaide.
This Commissioning Framework documents the policy framework for how we undertake commissioning at Adelaide PHN.
The purpose of this Commissioning Framework is to: Outline a best-practice approach to commissioning, and Communicate this approach to stakeholders
Through this Commissioning Framework, we aim to:
Build a shared understanding of our commissioning approach with our partners, including consumers, commissioned service providers, and other key stakeholders and organisations; Describe our methods for commissioning primary health care services; Outline our commitments across the commissioning cycle.
The Commissioning Framework aligns with Adelaide PHN’s Strategic Plan, which was developed based on the Quintuple Aims. This ensures that our commissioning approach directly supports our strategic goals[1].
This framework is for internal and external audiences. The application of this framework provides a common direction for us to move forward together.



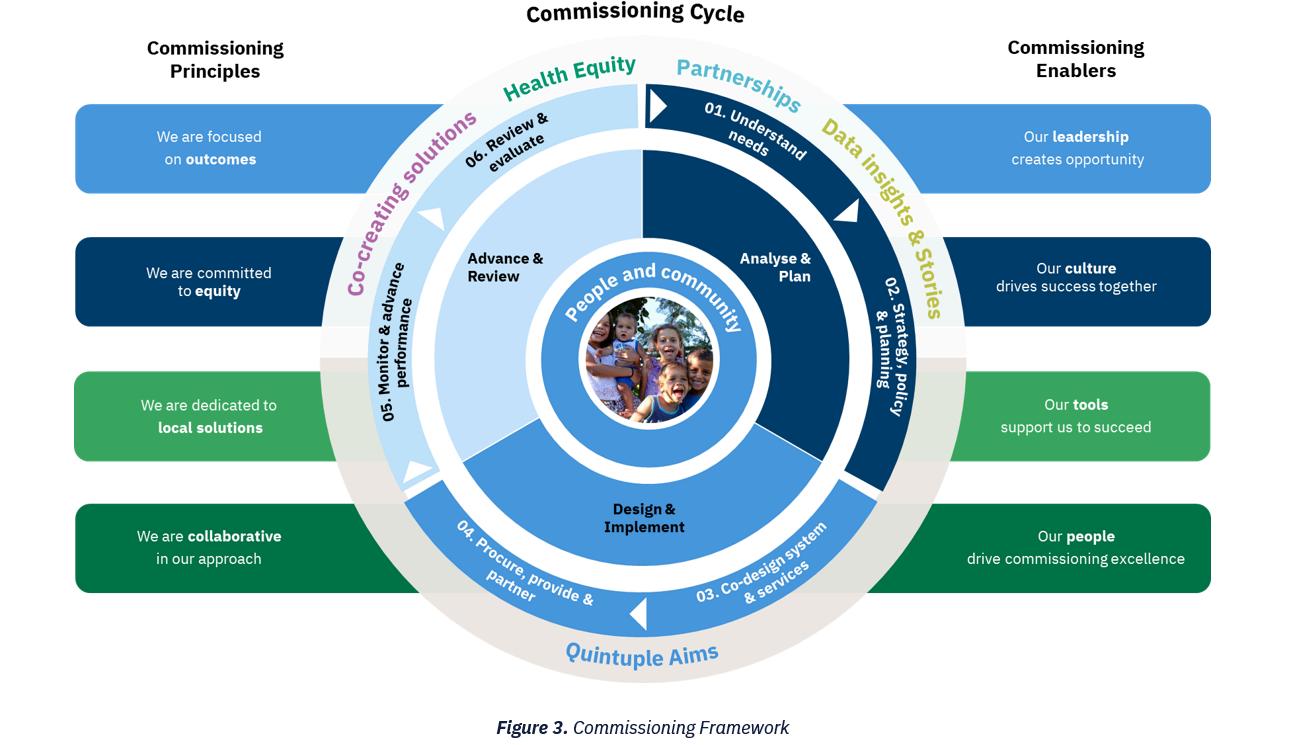
Our Commissioning Framework has three core parts:
The Commissioning Cycle illustrates the interconnected and ongoing nature of commissioning through six core stages, each with a distinct purpose The cycle ensures that primary health care services are commissioned with people and the community at the centre
While the Commissioning Cycle outlines a staged approach, the process is often more complex. Activities may run concurrently within each stage or recur as we adapt and refine our approach through continuous improvement. Our approach remains flexible, allowing us to adjust as needed
Our Commissioning Principles guide our approach, shaping our actions and choices They align with our vision, signature behaviours, key focus areas and strategies

Our Commissioning Enablers are tools, resources, and conditions that help us to achieve our goals by supporting commissioning excellence They ensure the necessary conditions and resources for success support our approach


Adelaide PHN is one of 31 Primary Health Networks (PHNs) across Australia and one of two in South Australia. PHNs are independent, not-for-profit organisations funded by the Australian Government.
PHNs deliver three core functions [2]:
Coordinate and integrate local health care services in collaboration with Local Health Networks to improve the quality of care, people's experience, and efficient use of resources.
Commission primary care and mental hea services to address population health need gaps in service delivery and to improve acc and equity
Capacity-building and providing practice support to primary care and mental health providers to support quality care delivery.
PHNs’ primary objectives are to keep people well, particularly people with chronic health conditions and mental health conditions and reduce avoidable hospital presentations in their regions. To accomplish this, PHNs deliver national programs using a 'place-based' approach – tailoring initiatives to meet their local population's health needs.


Commissioning involves assessing, planning, designing, selecting, monitoring, and evaluating services tailored to local health and service needs The commissioning cycle outlines the structured stages that guide commissioners through activities to continuously align the primary health care system with local health needs.
Commissioning also involves a relational approach focused on partnering and co-creating with communities, service users, providers, and system leaders This mindset encourages commissioners to coordinate and integrate primary care with other parts of the health system, build capacity, and provide support for quality care delivery.
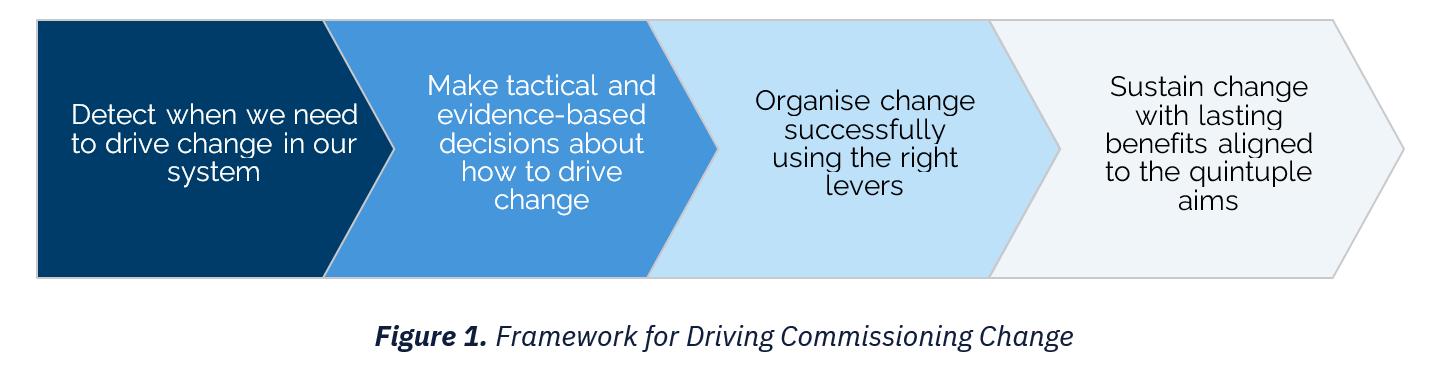
As a commissioner, Adelaide PHN balances the structured methodology with a relational approach to ensure primary health care services are tailored to local health needs (Figure 1).




Adelaide PHN’s Commissioning Framework aligns with the overarching PHN commissioning framework (Figure 3).

Understanding local health needs is the starting point of our commissioning approach.
To do this, we develop a clear picture of local health needs (demand) based on our priorities, with a particular focus on equity, and assess how well these needs are met through local health service mapping and analysis (supply).
Our annual Health Needs Assessment presents our evidence base regarding health needs and identified regional and local priorities unique to Adelaide PHN
In this step, we:
Build an understanding of health needs by establishing insights through detailed and systematic reviews of available data sources (qualitative and quantitative data).
Engage with communities, people with lived experience and stakeholders to gain a deeper understanding of the issues, opportunities, and priorities.
Assess the market’s ability to supply services to meet local health needs.
Use our Kitchen Table methodology to capture community views on their experiences with and expectations of the primary health care system
Capture Aboriginal and Torres Strait Islander communities and other priority groups’ views, including people with a lived experience, on their experiences with and expectations of the primary health care system.
Use a range of data and information sources, including quantitative and qualitative data, to build and enhance our understanding of health and service needs This may include existing reports or evidence, or the creation of new insights.

As commissioners, we identify needs to make informed decisions on where resources are best allocated to drive outcomes and equity.
By triangulating our understanding of local health needs and service gaps, we can identify opportunities for improved health outcomes and prioritise resources to where they are most needed.

Use triangulation to generate rationale or decision making in prioritising resources and funding to where they are most needed.
Share a summary of our priorities through the annual Health Needs Assessment.
Address population and communityspecific challenges and priorities by applying a place-based approach to identify needs and equity gaps
Set priorities in partnership with our combined Advisory Councils, PHN Board, PHN staff, and other subject matter experts to direct resources and funding to where they are needed most.


Strategic planning creates the blueprint for the future of primary health care services.
As commissioners, we lead strategic planning to ensure the primary health care system operates in an integrated way.
Our planning focuses on designing services based on health needs, allocating resources effectively, and addressing current and future health challenges
In this step, we:
Develop our Strategic Plan through engagement with our stakeholders and partners.
Plan to align our commissioning intentions, activities and resources with the future direction set in our Strategic Plan.
Lead and participate in forums with system leaders to integrate health services across the region.
Engage with our communities to ensure their views shape our Strategic Plan and focus areas. Mobilise our stakeholders to build a shared understanding around our vision for system change.
Provide system leadership to align and partner with communities, commissioned service providers, health organisations, and other key stakeholders.
Partner to improve health equity and access by planning, designing, and delivering inclusive, culturally safe, and appropriate services across the primary health care system

To achieve this, we develop a vision and strategy that enables us to align our planning and stakeholders around a common purpose.
Our Strategic Plan outlines our blueprint for the future, and we express our commissioning intentions through our Activity Work Plans.

Partner with other funders to jointly commission services where it will improve outcomes and health equity. Document our vision, plans and intentions in our Activity Work Plans to ensure transparency and engagement with our stakeholders.
Partner with health providers, non-forprofit organisations, Aboriginal Community Controlled Health Organisations (ACCHOs), Aboriginal Community Controlled Organisations (ACCOs) and other stakeholders to pool resources, connections, and expertise to achieve mutual goals.



Co-design is a collaborative process to design services that achieve health equity and improve outcomes.
As commissioners, we draw on the expertise, experience, capabilities, and knowledge of community members, including people with lived experience, and other key stakeholders to develop solutions that meet identified needs
By leveraging local insights, we design services that deliver the best experiences and outcomes for the people we serve
In this step, we:
Co-design services with communities, including people with lived experience so their perspectives shape the service.
Co-design evidence-based services with providers and subject matter experts.
Focus on outcomes-oriented design to ensure each activity delivers measurable improvements in health equity and outcomes.
Grow networks of people with lived experience and involve them throughout the commissioning cycle, including in advisory and decision-making forums.
Design place-based solutions tailored to the needs of communities where services will be accessed
Provide resources to strengthen organisational and sector capability for effective co-design. Co-design logic models with stakeholders to ensure activities align with the desired outcomes
Share the results of co-design exercises with stakeholders to 'close the loop'

To achieve this, we engage people authentically, meaningfully, and early in the commissioning process.
While design aligned with our Partnering Framework can occur at any step of the cycle, it is expected during this stage.

Build co-design capability within our team and foster partnering.
Engage and communicate transparently throughout the co-design process to ensure alignment across all stakeholders





Selecting the best service delivery method helps optimise outcomes from our investments.
As commissioners, we typically commission non-government and private service providers to deliver primary health care services.
We commission services through tenders, grants, and other opportunities To do this, we develop plans, undertake approaches to market and run effective evaluations to secure the right services and providers for each context
In this step, we:
Develop plans to understand the market and determine the most appropriate approaches to market to secure the right services and providers for each context.
Build market capacity by helping providers understand the expectations and requirements to apply for tenders, grants, and other opportunities.
Run a transparent process to select services and providers that meet the requirements.
Use proportional approaches to tenders, grants and opportunities that balance collaborative and competitive approaches.
Actively shape the market by encouraging new entrants, particularly smaller providers, ACCHOs and ACCOs, and by reshaping the existing market through transparent approaches to procurement
Build capacity and address barriers to participation, especially for smaller providers, ACCHOs and ACCOs.
Apply best practices, including interviews and alternative methods for ACCHOs, ACCOs and smaller providers, to encourage participation.

This process leads to contracts that are focused on outcomes with agreed mechanisms to achieve results and measure success.
We advertise tenders, grants, and other opportunities on the Tenderlink portal, and announce the results through our communication channels.

Agree contract and payment terms, with accountability mechanisms based on the size, complexity and risk involved. Engage with providers throughout the tender journey, offering support, guidance and transparency while maintaining probity.
Ensure transparency and provide advance notice of opportunities to support quality responses.
Work with preferred commissioned service providers to develop contracts including agreements on governance, performance indicators and reporting requirements
Provide feedback to all participants to encourage future participation.


Monitoring performance ensures our services are effective, providers are accountable, and both are continuously improving
As commissioners, we measure, monitor, and drive continuous improvement to advance performance to deliver outcomes.
We work to create an environment where providers can thrive and are supported to achieve health equity and outcomes
To do this, we work with commissioned service providers on the implementation, management, and ongoing monitoring of services.
In this step, we:
Measure and monitor performance to uphold high standards and ensure accountability for health equity and outcomes.
Engage and support providers in continuous improvement by sharing performance data and insights
Measure, monitor and drive performance by tracking key metrics including the quintuple aim, discussing performance, and supporting providers to improve.
Partner with commissioned service providers on implementing, managing, and monitoring services
Use a range of commissioning levers to drive performance and accountability for health equity and outcomes.
Use a balanced set of indicators to measure and monitor performance.
Share data, analysis, and insights with providers to help them identify areas for improvement

We use a range of levers to drive performance improvement and engage providers in this process (see Commissioning Levers).
Our view of health system performance is shared through our Annual Reports

Use a range of levers to drive systemwide improvements.
Set and communicate clear performance expectations and drive performance through monitoring and accountability
Foster a culture of collective learning within and across organisations to advance performance by sharing best practices Maintain clear performance expectations and communicate them clearly.



Reviews and evaluations are planned, systematic collections and analyses of information and data related to PHN activities that assess the effectiveness, efficiency, and appropriateness of our services and drive continuous improvement
As commissioners, we conduct evaluations to inform decision-making, re-design, and shape future planning.
To achieve this, we create high-quality logic models and develop evaluation plans early. Our contracts provide agreement on which services are delivered and the approach through which they are evaluated
In this step, we:
Plan fit-for-purpose evaluations that are supported by strong logic models. Select evaluation methods aligned with our intended outcomes.
Establish data needs and resolve gaps as part of our early evaluation planning Partner with research organisations to build the evidence base.
To do this, we work with commissioned service providers on the implementation, management, and ongoing monitoring of services
Plan with the end in mind by co-designing robust logic models for evaluations.
Use contract reporting requirements to gather data for reviewing and evaluating services
Match evaluation efforts to funding level, risk, innovation, or strategic importance.
Draw on providers’ expertise to inform evaluation findings.

We use reviews and evaluations to grow the evidence base on what works, identify improvement opportunities, and ensure valuedriven decision making.
Where appropriate, we share review and evaluation findings to inspire continuous improvement

Use evidence to drive decision-making and implementation according to findings.
Apply best practices and scale innovation across the region based on evaluation findings and recommendations.
Share insights from reviews and evaluations to inform best practice and continuous improvement.
Share findings to spread knowledge, encourage best practice, and promote continuous improvement
Expand the evidence base of pilots and prototypes, ready to localise and scale if they prove effective and value driven. Recommission services in a planned, safe way when necessary.


The following principles underpin our commissioning approach (Figure 4).
We are focused on outcomes
We are committed to equity
We are dedicated to local solutions
We are collaborative in our approach

Use insights and evidence to inform decision-making. Apply logic to clarify our pathways to impact.
Adopt a person-centred approach by partenering with communities and people with lived experience to ensure services meet health needs. Prioritise cultural safety to meet the unique needs of Aboriginal and Torres Strait Islanders and other priority groups.
Commission place-based services to deliver localised care Co-design solutions that build on local strengths
Build strong partnerships to achieve mutual goals
Create a connected system to integrate health care and other sectors


The following enablers support our commissioning approach (Figure 5).
Our leadership creates opportunity
Our culture drives success together
Our tools support us to succeed
Our people drive commissioning excellence

We lead and influence the health system to drive meaningful change Our internal leadership strengthens our PHN, while our external leadership harnesses collective skills and resources for broader impact.
We build a safe and inclusive primary health care system by living our signature behaviours. These behaviours support us to address challenges together with our communities, people with lived experience, commissioned service providers and partners.
We equip our team and providers with the structures, systems, processes, and tools needed to improve health equity. These resources support operations, team-based care, and integrated care.
We foster professional and personal growth opportunities, including diversity and cultural capability, for our team and providers By cultivating an inclusive environment where they can thrive, we focus on what truly matters for communities and providers.






