Membership benefits
Resources and perks available State of the art
The Clinical Skills Simulation Laboratory refurbishment
50-year reflections
Drs Michael Poli and Peter Froud on 50 years as ADAWA members








Resources and perks available State of the art
The Clinical Skills Simulation Laboratory refurbishment
Drs Michael Poli and Peter Froud on 50 years as ADAWA members








I am sure you would be aware that membership renewals for 2023/24 have been issued and I would take this opportunity to again draw your attention to Council’s decision that ADAWA branch fees will not increase in 2023/24. This decision recognises that through prudent financial management, Council can support our valued members during challenging economic times.
It is important that ADAWA maintains our strength in numbers, especially as this allows us to advocate strongly to government, and other entities to achieve beneficial outcomes for our members and therefore the broader community.
Examples of our advocacy work include the recent engagement with the WA Department of Health, and our meeting with the Shadow Minister for Health Ms Libby Mettam, to advocate against the proposed regulation of private dental practices performing services under IV sedation. Increasing the regulatory burden on the dental profession will not only negatively impact dentists but has the potential to inflict unintended and disadvantageous consequences on the community, which is why this proposed change needs to be vigorously opposed. With your continued support, we can continue all the good work for the benefit of our members. Hence, I strongly urge you to renew your membership as early as possible, which will help your association continue to serve you in the best possible manner.
The next step in our continuous improvement process, which aims to ensure ADAWA remains relevant and delivers value to our members now and into the future, is the review of the ADAWA Constitution. T his is a vital step in the process, especially as the soon-to-be rolled out ADAWA Strategic Plan will require rules that are contemporary and fit for purpose, and which support the key identified strategic objectives of the Plan. The Constitution review, which will be undertaken by the ADAWA Constitution Committee, is expected to be completed early in the new financial year.
All the ADAWA Committees under the individual Chairs are working hard to ensure the progress of their objectives. I thank each dynamic and passionate committee member for their engagement.
Our ADAWA Helpline panel members are currently undertaking mental health first aid training, which will greatly enhance our ability to support members who access the service when they find themselves in challenging professional or personal circumstances and need an empathetic ear. Stay tuned for further updates on this soon-to-be-launched member service. I would like to finish this report by thanking all the hard-working ADAWA staff and our CEO, Trevor Lovelle, for all the work being done behind the scenes to ensure the renewals go smoothly and the membership benefits are explored and enhanced.
The ADAWA Council recognises the challenging economic conditions ahead for our members and has agreed there will be no increase to the ADAWA branch membership fee for 2023/24.
DPL has similarly agreed not to increase their fees for 2023/24, however there will be a small increase to the ADA Federal fee, and MDA indemnity premiums will increase according to your category.
Trevor Lovelle ADAWA CEOAre you aware of the many benefits that come with your ADAWA membership? Here, we feature some of the valuable resources and perks available to our members.

We keep our members up to date with information, support and advice. These include:
Emails :
Our fortnightly emails keep you in the loop with important updates, as well as news, events and CPD events.
The Western Articulator is a high-quality magazine (available in hard copy or digitally), produced exclusively for our members. Here you will find inspiring stories about your peers, CPD information and news. Contributions and editorial ideas from our members are always welcome. As an ADAWA member, you can also list Professional Notices in the magazine free of charge (for three editions). To discuss editorial, clinical articles or Professional Notices, email media@adawa.com.au
Our supportive Facebook groups are also available for you to ask questions or network within our private online community. ADAWA members can join our exclusive ADAWA Members Facebook group. Or our ADAWA Partners in Practice group is open to all members of the dental community, including practice staff.

In both the ADAWA Members and ADAWA Partners in Practice groups, members can advertise job opportunities on ‘Job-Day Mondays’. Members can also advertise job opportunities on our website free of charge. adawa.com.au/membership/classifieds
As an ADA member, you also have access to Peer. ada.org.au/Peer

If you are looking to get your practice accredited, Andrea Andrys at ADA House can offer guidance and support. Contact Andrea andreaa@adawa.com.au
Need HR advice? You can access information via ADA’s HR Advisory Service. Call 1300 232 462.
Members can access advice regarding prescription, over the counter and nutritional supplements via this service. ada.org.au/pharmaadvice
WA Dental CPD :
The WA Dental CPD program is world-class, with highly respected speakers offering a range of lectures, hands-on, and dinner courses. To find out about upcoming courses, visit adawa.com.au/cpd
New Practitioner Program
This program is specifically for dentists who have graduated within the last five years or dentists who have passed their ADC exam in the last five years, to learn and network in a supportive setting with their peers. The program culminates with the popular all-day education event, the Young Dentists' Conference.
MY DISCOUNTS An added perk is the many discounts you are entitled to as a valued ADAWA member.
As an ADAWA member, you can access great discounts with ADA Lifestyle Benefits. Here you can shop by brand (including Apple, Garmin, Samsung, endota spa, Lexus) or save money on gift cards, cars, dining out, fitness, electronics and more. ada.rewards-plus.com.au
ADAWA also work with a number of partners for additional benefits for our members. These include Bunnings Trade, Dental Stock Photos, AMA Finance, WA Energy, Invedent, ONDA and VPG Property.
ADAWA members are entitled to a 12% discount on health cover each year from HIF, when premiums are paid by direct debit. hif.com.au/adawa
MY CPD High quality CPD is of great importance, and at ADAWA, we have you covered!
If an ADAWA member has MDA/DPL through ADAWA, they can activate free Public Liability through Dental Essentials. Call Dental Essentials on (08) 9382 5614 – and let them know you are an ADAWA member. Dental Essentials will contact ADAWA to confirm you are a financial member, before setting up free Public Liability and sending you a Certificate of Insurance.
MY COMMUNITY Our members are the heart of our association, bringing strength and belonging to ADAWA. There are many ways to engage with the ADAWA community.
Our general meetings allow our members to keep up-to-date on what is happening behind the scenes at ADAWA. These highly social events start with an ‘Eat and Meet’ to allow members to network with their peers and after the formalities of the general meeting, they can learn from a guest speaker. adawa.com.au/membership/rsvp
There are many ways ADAWA members can give back to the community;
• ADHF programs These programs include: Rebuilding Smiles (supporting people who have experienced domestic violence, referred by domestic violence support agencies) Adopt a Patient (matching dentists with patients in need of complex dental treatment) and Dental Rescue Days (allowing a practice to allocate one chair, a half day or a full day to treat referred patients). For details on ADHF programs, contact Andrea Paterson, adminwa@adhf.org.au
• Dental volunteerism programs No matter how much time you have spare to give, there is a volunteerism option to suit! Go to adawa.com.au/our-association/volunteerism to find out about options.
Or for information about volunteering with Healing Smiles (treating female domestic violence survivors) email healingsmileswa@gmail.com
MY FUTURE ADAWA supports dental students to give them a smooth transition into practice. This includes:
ADAWA awards :
ADAWA is proud to sponsor leadership and academic excellence awards for dental students at UWA.
Graduate Guide
A compilation of a Graduate Guide for final year students introduces the newest dentists to the profession. This is also a valuable resource for practices looking to hire new graduates.

Yearbook
ADAWA produces a keepsake yearbook for graduating students.
Welcome to the Profession
ADAWA hosts a dinner to welcome newly graduated dentists into the profession and into the association.
MY VOICE
Whether it is meeting with the Minister for Health and Mental Health, teaming with affiliated organisations such as the Cancer Council of WA, or our Oral Health and Education Committee spreading the oral health message to the public, ADAWA is active in advocacy and ensuring the voice of each member is heard.
Dr Michael Poli says he and brother (and fellow dentist) Anthony initially wanted to study medicine. “However, being in the UK and under the famous NHS, Dad (a GP), said: ‘Don’t do medicine, do dentistry – 9 to 5, no home visits, no emergencies, no out of hours work’,” he recalls. “It was usual for him to have to see up to 60 patients in the morning, then house calls in the afternoon and then back for the evening session. He said that most of the time he would be writing out the scripts for the patient as they were walking into the room. He felt he was just a glorified clerk, not medicine at all. It was the main reason we moved to Australia.” Michael took his father’s advice and studied dentistry – and has always been an active and engaged member of the dental community. Michael was one of the dentists who set up the South West Dental Convocation, after he and the late Dr John Mathieson (Matho) started talking about the possibility of getting one or two specialists down to Bunbury to give a lecture.
“I think at the time there were five of us (not a big audience),” Mike recalls.
“However, I was allotted the job of asking the specialists, because I was able to successfully coax them down to Bunbury and the others made me the chairman. “
“We did speak with ADA about our scheme and at the time they preferred us to use the name that it now bears,” he says, adding that as more dentists came to practice in Bunbury, they expanded their thinking.
“We decided that we had better do more for the lecturers than a bottle of wine.”
“Fees had to be considered for venue hire and reimbursement for the lecturers’ time and expenses. So, we arranged overnight accommodation for them and fed them and still managed to present them with a bottle of two of the famed Margaret River wines. After a few years of ‘one-night stands’ and having attended several weekend conferences I put forward the idea of running a similar event.”
Michael also served as the ADAWA Country Councillor for a number of years. “Kim Mezger was executive officer at the time and I was almost always attending the General Meetings, coming up from Bunbury,” he says.

“He put me forward to be nominated for Country Councillor and I decided that it would be a great way to learn how ADAWA worked and what it did. I thoroughly enjoyed the experience and the insights I gleaned.
"When Brian Atkinson was the President, I had to help organise a country weekend
After half a decade as an ADAWA member, we spoke to Dr Michael Poli about his career.
conference in Bunbury with Dr Jim Ironside as the guest lecturer. That was a steep learning curve, but great experience. I was also involved in the initial liaison with the Dental Nursing Australia training organisation, founded by Sue Lawton.”
“Highlights of my career would have to be being able to associate with so many great specialists, who are always so helpful and other dentists that I was able to talk with at lectures/conferences and exchange experiences,” Michael says. There were also some memorable days in clinic. “Whilst in my second year of graduation, working for DHS in Paraburdoo, a frantic father on a Saturday afternoon, came to my house with his five-year-old child with a 10cm long chair spring – the hooked end of which was firmly caught between his upper centrals,” Michael recalls. “The father had not been able to remove it and was quite desperate. I took them to the surgery in the new hospital and successfully removed it without any trauma to the child. That was such an amazing realisation – being able to help people. Similarly, being able to use Relative Analgesia – I converted a lot of absolute dental phobics into normal fearless dental patients. That was so rewarding.
“Another highlight was the many years I spent as Dr Ian Rosenberg’s assistant each week for the whole of each Thursday –learning so much from him and getting to know Evan Kakulas doing the same thing in Perth. “I was (also) so very proud of my brother Tony when he became ADAWA President a few years ago,” he adds.
“The biggest changes that I have perceived are the almost total rejection of amalgam as a restorative material, one which has served the patients so well for so many years,” he says. “Another would be the more predictable use of implants in the right hands – and another really exciting one is the 3D printing of titanium for replacement of destroyed parts of the skeleton.”
ADAWA has also always been supportive along the way, with Michael choosing to keep his ADAWA membership even after moving interstate. ‘It is amazing to be part of a group that sticks together so well,” he says. “I have been over in Canberra since 2011 and I stayed an ADAWA member because I was so impressed the way the ADAWA functioned.
“On the occasion I have had to seek advice, either the office, CEO or President have been so easy to talk to, discuss the issues and help find a solution.”
“At present, I am working full-time in Defence and will eventually cut down to four days, then three days and then retired, but as to the timeframe – I don’t really have one,” he says. “My father was still in full-time medical General Practice at 80.”
After all these years, Michael says he gets a real sense of achievement by being able to relieve pain and restore function.
After half a decade as an ADAWA member, we spoke to Dr Peter Froud about his career.
When Dr Peter Froud graduated in December 1966 he had already joined the army as an undergraduate two years prior so he had some money to marry the love of his life.

Joining the army committed him to serving for four years, which he extended to six years to obtain a two-year posting in Singapore, before taking a discharge in Perth.
“I am originally from Victoria, but we decided to come to Perth because we had a child with cerebral palsy and he had problems with bronchitis,” he recalls. “This was a nice, dry climate and seemed like it was going to be the best for him. We came here in 1972 and never left.”
Peter went into private practice in the King’s Hotel Building in 1974 and bought Dr Rob Bower’s practice when he went to specialise in periodontics. He was in the CBD for the best part of 25 years, and after selling that practice at 55-years-old went to Collie with the intention of practicing there for 10 years until he retired. More than 20 years later, Peter is still there working two or three days a month to fill in for dentists when they are away and still enjoys it.
Over 50 years Peter says there have been a few highlights:
The army A memorable time with the army was the time he spent in Puckapunyal Victoria, treating the 20-year-old recruits. “There were four intakes of around 1200 young men each year and I think the average for each intake was about 3500 extractions,” he recalls. “In each intake there were four or five people that needed 32 extractions. Times have changed.”
Vietnam Peter spent time in Vietnam where he treated the teeth of locals, as well as army personnel. “Every week we would go to the local village, and people would line up,” he says. “You would inject 15-20 people along a bench and would start extractions along the other end. On the alternate weeks I used to go along to the local orphanage, which was run by an order of French nuns.”
Peter later went back to Vietnam with friend and orthodontist, Colin Twelftree, who had set up a dental project in Long Tan to provide dental care to the locals.
“Colin walked up the road to the nearby day care centre and when he came back his face was white as snow, all the kids were drinking cordial out of bottles and had rotten teeth. So with the help of the local health service, working with Australian volunteers, I believe things have improved considerably and Colin should get praise for setting that up.”
Volunteerism dental clinic Peter was also involved in volunteerism on home soil, and with the support of ADAWA, helped set up a dental clinic for children with cerebral palsy at the now Ability Centre, which operated for many years. “We called for volunteers, and had a therapist and volunteer dentists – we did a lot of good there,” he says.
Peter says composite is probably the biggest change he has seen over 50 years in dentistry.

“Composite came out in the mid-60s and it was rubbish but eventually got better,” he recalls. “Certainly, endodontics has come a long way with rotary instruments. Implants and ceramics have also become much more important. Another big change was overnight wearing gloves and masks; it was a huge change.”
Throughout the changes and challenges, Peter says ADAWA has always been supportive. What’s next for Peter? He is registered until November, which will take him to 80-years-old – and he is still enjoying dentistry.
Why did you initially decide to join ADAWA Council 13 years ago as the DHS representative?
It was a combination of two things; one being that at the time the Director of Dental Health Services (DHS) was an ex officio member of the ADAWA Council and that arrangement had been in place for many years. Secondly, it was a great opportunity to continue on the good work that previous DHS Directors had done in forming very collegial relationships with ADAWA members, Council and Executive to progress the advancement of dentistry in WA, in the many forms that this takes.
What have been some of the highlights during your time on Council?
A main highlight was the way in which the ADAWA Council and Executive worked with DHS during the COVID pandemic. There was a significant body of work done by many people to assist those practitioners in private practice and DHS to understand what the COVID rules were at any
particular time as they did change often. In a general sense, other highlights were the ongoing work done by ADAWA Council and Executive in dealing with other issues that arose either on a State or National level.
What are your hopes for the DHS and ADAWA relationship going forward?
That the current excellent working relationship that exists continues and any expertise DHS has can be shared with ADAWA to improve how the business operates for the benefit of all the members.
What consultancy work will you be continuing?
At the moment I have just finished having two months' holiday and am now back at DHS doing some project work. My previous managerial role has been filled and Catherine Alford is now the Manager Central Clinical and Support Services.
What are your plans for retirement?
I have a number of things that are on my list to start.
These include travelling to Melbourne (often) to see our granddaughter, doing some walking on the Bibbulmun Track, riding on the Munda Biddi Trail, woodworking, learning to play the drums (I hope the drum teacher has a lot of patience as I have no sense of beat or rhythm), going to the gym to keep fit, gardening, overseas travel, starting up meditation on a more regular basis, doing some volunteering and learning some simple magic tricks to impress my granddaughter. I think that should keep me pretty busy once I stop work completely. Do you have a message you would like to leave for ADAWA members?
I would urge all dentists to become a member of the ADAWA so that the ADAWA is the true voice of dentistry in WA and speaks for all dentists. With a large membership base there is the opportunity for ADAWA to provide support to all members, in whatever way that is, so that each member recognises the value that belonging to ADAWA encompasses.
After more than a decade as the Dental Health Services Representative on ADAWA Council, Dr Martin Glick has retired.
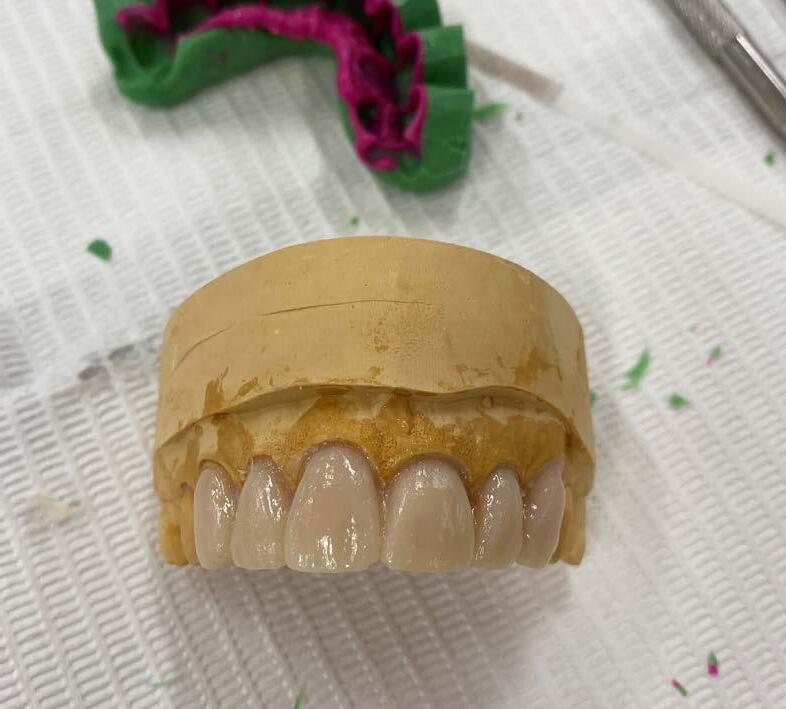
Gone are the aged and cracked phantom heads – The Clinical Skills Simulation Laboratory has been transformed into a state-of-the-art facility, with 71 phantom heads installed (replacing 56 phantom heads installed in 2001), under the tender of Dentsply.

“The CSSL refurbishment is an innovative, signature project that supports the UWA Dental School's strategic plan aligning with two current priorities set by the Vice-Chancellor, namely ‘The future of learning at UWA’ and ‘The UWA Student Learning Experience’.”
“The new CSSL will facilitate advancing academic excellence, promoting worldclass, technology-rich, hands-on learning, and enhancing the dental students’ clinical skills says Associate Professor Robert Anthonappa. “In addition, it will increase clinical efficiency, and notably, enhance the students learning experience within a competency-based pedagogy.”
Dean and Head of School/Director of OHCWA, Professor Hien Ngo, says the CSSL allows the Dental School to be viable into the future.
“Since the inception of OHCWA there has been a physical cap of 56 students per year,” he explains. “All dental schools in the Go8 University would be much larger than that (around 100 students in the Eastern States). This will allow the UWA Dental School to expand class size to 70 by bringing in 14 extra full-fee paying international students.”
He adds larger cohorts mean OHCWA can provide more services to the underserved communities in WA. Additionally, extra DMD students will also mean the School will be able to grow their DCD (Specialist) training program. DMD student, Ranundi De Silva, says there are standout features of the new clinic. “The convenience with the new phantom heads is a personal
A state-of-the-art facility
After months of planning, the refurbishment of the Clinical Skills Simulation Laboratory (CSSL) has transformed the facility.
favourite addition of mine, especially with the automatic suction that you can enable,” he says. “The closer replication to the ground floor clinic with the set-up for handpieces and light mirroring the GF clinic makes the transition between the simulation clinic and real clinic much smoother,” he adds.
Professor Ngo thanks all the donors who have contributed to date, especially the Western Australian Dental Foundation for driving the campaign, Associate Professor Mithran Goonewardene, Dental Cases Panel Pty Ltd, Delta Sigma Delta WA Graduate Chapter, Dental Unicon WA (Inc), Dental Study Group and new fellows of the WA Dental Foundation Dr Abhishek Singh, Dr Minh Dien Tran, Dr Meredith Arcus, Dr Ajitha Kanupuru, Dr Janina Christoforou, Dr Amit Gurbuxani, The Honourable Dr John Day and Dr Lahiru Chandraweera. ADAWA was also a donor.
“Although the facility is now operational, there is still an opportunity for members of the dental community to contribute to the project, in advance of the official opening,” says Dr John Day, Patron, Clinical Skills Simulation Laboratory Project, Western Australian Dental Foundation. “When students enter this room, they will see the names of the individuals and organisations who have contributed to support their skill development and will warmly welcome them into the profession as colleagues. I particularly encourage fellow dental graduates, who have benefited from being a member of the profession, to assist in leaving a legacy at the University for students of the future.”

For queries or to discuss making a contribution, contact:
+61 8 6488 4591, development@uwa.edu.au
To donate online, visit giving.uwa.edu.au and follow the prompts.
When Dr Emma Lewis received an email in 2021 from Dr Jacinta Vu requesting specialist volunteers join Healing Smiles, Emma was happy to reply to say she would be willing to help.

“I have always enjoyed volunteer work and have fortunately had the opportunity to be involved with other organisations including treating cleft lip/palate patients in the Philippines, general oral surgery for patients in Nicaragua and Alachua County in Florida, as well as more recently alongside a multidisciplinary team in Cambodia. It is a real privilege to help people in this way and seems a natural choice with the qualifications we have worked hard to obtain."
“I find the work extremely rewarding,” she adds. “It is not only providing the oral and maxillofacial surgery itself but problem solving with the
challenges that you often faced with such as language barriers, equipment and environmental situations.”
So far, the treatment Emma has provided for Healing Smiles patients has been mainly extractions. “One particular patient required multiple extractions as part of her overall treatment plan – all of which were difficult and required a surgical approach,” she says. “The treatment required a couple of visits so the fact she returned for her treatment is always encouraging!”
Emma says she often responds better to last minute calls for help to treat Healing Smiles patients, which Sandra Wood (Healing Smiles Volunteerism Coordinator) understands. “As a surgeon, we are brought up making last-minute decisions and squeezing people in; it is not unusual to have a day’s plan change several times.
The more you do, the more you can do Oral and maxillofacial surgeon Dr Emma Lewis has begun volunteering with Healing Smiles and encourages other specialists to get on-board.
ADAWA members are entitled to a 12% discount on health cover each year when premiums are paid by direct debit. Existing HIF members need only call or email to have the discount applied to their membership.
Visit hif.com.au/adawa and use the access code ADAWA Alternatively call HIF on 1300 13 40 60 or email sales@hif.com.au
"I have also provided advice regarding impacted teeth, possible facial fractures and medical-related questions.”
When asked about the feedback received from Healing Smiles patients, Emma says they are always grateful and humble. “Our work is often one aspect to their overall care and so we may only treat them the one time,” she adds. “This may be at a real low point for them, especially if they are in pain or having to lose teeth unexpectedly.
“The nice thing about being part of a group like this, is that often we will receive feedback through the other treating members and Sandra is also very good at keeping us informed. Whilst we may all provide the treatment in our various offices, this is when you really feel like you are part of team accomplishing a common goal to help these patients in need.”
To other specialists considering volunteering, Emma encourages them to put up their hand. “Volunteering is highly rewarding
and made easy when part of a great organisation such as Healing Smiles,” she says. “The key is having a person such as Sandra, who is the glue to keeping the process in motion and coordinated. The work would also not be possible without the help and support from my office team.
I think it would be fair to say that we all live busy lives and often putting your hand up to be involved can be quite daunting with thoughts of where it will fit in.
“I really believe in the adage: ‘the more you do, the more you can do’. Helping people is in our nature and what we are good at, so it’s a no-brainer to me!”
For more details about volunteering with Healing Smiles, email healingsmileswa@gmail.com
We are so grateful for specialists like Emma for their time, flexibility and expertise. They make such a huge difference for our clients."
Sandra Wood

We are lucky to have a new speaker join WA Dental CPD’s 2023 program – respected periodontist from Melbourne Dental School, Dr Luan Ngo, who will be travelling to Perth in July to present two hands-on courses.

Graduating with honours from the University of Melbourne, Luan worked in General Dentistry for three years when he was looking for a challenge and periodontics was the perfect fit.
“I ended up starting an MPhil, which turned into a PhD,” he recalls. “My PhD topic was very much perio related, so it was a natural progression to then specialise. I really do enjoy non-surgical therapy. It’s very therapeutic to watch the calculus come off teeth.
“I love the mix of (for me at least) root debridement and
supportive periodontal care, where I can almost work in autopilot mode, and the very challenging surgeries we do in periodontics.”
As well as a respected specialist, Luan is a passionate educator, and is the convenor of the specialist Periodontics program at Melbourne Dental School.
“There are many reasons why I enjoy teaching. I believe it keeps me on my toes. I am also passionate about Periodontics and hope my passion rubs off on the students I teach.”
Perth practitioners will have the chance to see this passion in action, when Luan presents two courses in July – ‘Minimally Traumatic Tooth Removal’ and ‘Crown Lengthening for the General Dentist’, alongside Dr Cindy Nguyen.
We caught up with periodontist, Dr Luan Ngo.
Minimally Traumatic Teeth Removal will cover effective techniques for minimally traumatic tooth removal, as well as techniques and indications for tooth socket preservation. This course will feature a hands-on component, which will enable participants to practice tooth extraction, tooth sectioning and socket preservation techniques under supervision.
Crown Lengthening for the General Dentist will cover surgical crown lengthening indications and techniques. The hands-on component of the course will include surgical crown lengthening on pig jaws.
Dr Luan Ngo and Dr Cindy Nguyen will present Minimally Traumatic Teeth Removal on Saturday July 1 and Crown Lengthening for the General Dentist on Sunday July 2.
www.adawa.com.au/product/minimally-traumatic-tooth-removal www.adawa.com.au/product/crown-lengthening-for-the-general-dentist

“I hope the attendees will gain some skills, which they can directly apply to their clinical practice. I will hopefully explain how an understanding of the biological processes will improve the success of treatment and lead to predictable outcomes.”

Infection Prevention and Control: Achieving Best Practice is the most highly attended ADA NSW CPD course for four consecutive years; a fact which makes me both proud and humble. More than 3500 people have attended this constantly evolving presentation and I'm delighted to be returning to WA to present the course again in August. Part of the reason why this course resonates with the profession, beyond the requirement for practitioners to have contemporary Infection Prevention and Control (IPC) knowledge, is because it focusses on building team confidence and highlights how IPC matters from a business continuity perspective beyond simply preventing the transmission of infection.
From my perspective, there are three areas impacting IPC for dentistry in WA:
1. The Dental Board of Australia shifting away from a prescriptive approach to IPC
2. Evolving healthcare consumer expectations for IPC safety and quality; and
3. Pressure to take action to address sustainability opportunities while keeping patients and staff safe.
Kylie
Kylie Robb is a powerhouse advocate for best practice in infection control standards for every dental practice in Australia.”
Bite Magazine
I am a supporter of the Dental Board of Australia’s huge shift away from prescribing specific IPC guidelines to the expectation that practitioners exercise their own professional judgement to manage IPC risk. This approach provides an exceptional amount of flexibility to adapt to changing circumstances and evidence and this is appropriate.

The COVID-19 pandemic has highlighted the importance both of stringent IPC measures and increased consumer awareness of infection risks associated with visiting health care facilities. This is a good thing as it promotes a safer and healthier environment for both patients and practice teams. My course addresses how practitioners can face challenges to implement and sustain quality improvement initiatives at a practice level particularly when dealing with workforce shortages and higher turnover of staff.
The pressure from various sources to adopt or at least think about a sustainability mindset to minimise the environmental impact of patient care is not going away. While I think we still have a way to go before sustainability of itself is a key driver for change, the sheer volume of plastic required and increasing waste from an IPC perspective is obvious. I agree the cost alone of paying for all these single use items where it is questionable as to whether they are reducing the risk of infection transmission is valid concern. My course outlines how to objectively review the resources in use from an IPC risk management perspective to minimise cost – but not safety.
I really enjoy presenting this course and can’t wait to come back to WA again in August.
Infection Prevention Control Perth
Wednesday August 16
Infection Prevention Control Geraldton

Saturday August 19
Register at adawa.com.au/cpd
Fantastic program! I feel much more accountable with implementing infection control protocol in my workplace.” Dental Assistant
Kylie Robb MHSM,GradCert IPC, CICP-A, MAICD, FACIPC ADA NSW Head of Practice Services shares her IPC insights for WA dentists.
Endorsed and delivered by the ADA, this course is for dental practitioners, dental practice team members, industry and/ or product representatives that require infection prevention and control (IPC) education that is specifically in relation to the practice of dentistry in Australia. This is a vibrant and engaging course that incorporates reflective activities, plenty of videos, engaging quizzes and useful insights that are immediately applicable for every dental practice.
This is a constantly evolving course that has supported thousands of practice team members across Australia to continue to confidently manage IPC risk to protect the public.
We know that practice teams that have a good understanding of the most important elements of IPC leads to benefits such as:
• improved efficiency by streamlining processes
• being more sustainable by reducing single use plastics using risk-based principles
• using evidence and best practice concepts to seek and identify quality improvements
• having more confidence with creating and following policies thereby reducing variation; and
• creating a culture of continuous quality improvement ensuring services are person centred, safe and effective.
Over 3500 people have attended this constantly evolving, real time, ADA course to reflect the dynamic landscape that is IPC.
6.5 CPD
Wednesday August 16 2023
Registration from 8.30am Course 9.00am to 5pm
ADA House 54-56 Havelock Street West Perth
Lunch, morning and afternoon tea
$ $275 ADA Members $412.50 Non Members
Kylie Robb is the Head of Practice Services for ADA NSW and has been instrumental in advocating for best practice in infection prevention and control (IPC) standards for the oral health profession in Australia and around the world.

Kylie is a Fellow and Board Director of the Australasian College of Infection Prevention and Control and Adjunct Lecturer for the University of Newcastle. Kylie has post graduate qualifications in IPC and Health Services Management and holds the award of Credentialed Infection Control Professional – Advanced (CICP-A) and routinely presents on leadership for IPC, quality improvement, clinical governance, and dental practice sustainability.
Kylie has been recognised by the World Health Organisation’s Western Pacific Regional Office for her dental IPC expertise and the Society for Healthcare Epidemiology of America through her appointment onto their coveted International Ambassadors Program.
Western Australia Dental Update
Join Dr Nabil Khzam at the 2023 Dental Update conference at ADA House on SUNDAY 18 JUNE 2023

9:00am - 5:00pm
PRESENTED BY:
Dr Janice Kan
Evolution from All on 4 to AUDENTES –
Instant final full arch implant bridge at implant surgery
Dr Nabil Khzam
Lasers in Periodontics
Professor Camile Farah
Real-time digital biopsy: Endless possibilities

Dr Tim Silbert
A Simple Diagnositc Matrix and Tips and Tricks to make your endodontic treament easier
Dr Lee Kaing

Dentoalveolor Surgery: Clinical cases and discussion
RSVP TO reportsnkperio@gmail.com
ENDOD ONTIC STUDY CLUB FOR P RACTITION ERS IN PERTH
Join us for an evening of conversation with Dr Stephen Kwang on some interesting endodontic cases along with any of your clinical experiences you would like to discuss
This study club is exclusive to dentists in Perth wishing to further their knowledge on the biological basis of endodontic therapy.
CPD = 1 hour
6:30pm, Friday 14 July 2023
Venue: Floreat Endodontics Unit 3, 434 Cambridge St. FLOREAT WA 6014
Please RSVP by 30 June 2023 via email: studyclub@floreatendo.com.au
Parking available on site
There will be a substantial hands-on component to the course. Lecture component:
• Recognition of appropriate cases
• Case work-up
• Rationale for the design of relevant restorations
• Material options
• Occlusal registrations and articulation
• Bonding and cementation protocols
The practical component will focus on minimal preparation techniques:
• Multiple porcelain veneer tooth preparations
• Multiple ceramic only/partial crown preparations
• Predictable impression techniques
• Provisional restoration manufacture
The focus will be on receiving practical tuition and guidelines for the diagnosis and treatment planning processes required to facilitate multiple restorative dentistry.
SPONSORED BY

13 CPD Fri 3 - Sat 4 November 2023
Registration from 8.45 am
Course 9.00 am to 5 pm
UWA Dental School
17 Monash Avenue, Nedlands
Lunch, morning and afternoon tea
$ 2,035 inc gst MEMBERS
Dr Asheen Behari is a general practitioner in private practice in Claremont, Perth. He graduated from the University of the Witwatersrand in 1993, subsequently completing a Post Graduate Diploma in Clinical Dentistry in Oral Implants at the University of Sydney. Dr Behari is a Clinical Associate lecturer in the Discipline of Oral Rehabilitation at the University of Sydney. He is actively involved in facilitating continuing education programs and in mentoring others. His general practice is focused on restorative and implant dentistry.
Dr Paul Gorgolis is a general practitioner currently in private in Wembley Downs. He is a Fellow of the International Congress of Oral Implantologists. In London, he developed the UK’s first multi-disciplinary general and specialist practice where patients could be comprehensively managed and treated “under one roof”. Dr Gorgolis is an experienced clinician who coruns hands-on ceramic courses for the ADAWA and has been a lecturer and tutor to dental students at the UWA and The University of Adelaide.
To book, visit adawa.com.au/cpd
ADAWA works closely with a number of partners and affiliates, resulting in strong relationships with like-minded organisations and associations. We also work with partners to provide member benefits for ADAWA members, including discounts on advantageous products and services.
Access unique and accurate dental images for your presentations and all your practice marketing via Dental Stock Photos. ADAWA members are eligible for a 20% discount off the Recommended Retail Price to purchase photographs. Go to dentalstockphotos.com/pages/ada-wa-members-information to find out more.
Bunnings Trade and ADAWA are delighted to announce a partnership which gives you the opportunity to join the PowerPass Membership Program. To sign up or link your existing PowerPass account, please contact OrganisationsWA@bunnings.com.au
Local company WA Energy is stepping up to offer ADAWA members big discounts on dental practice energy bills. ADAWA members are eligible for new energy pricing and to have smart solar installed for $0 upfront. Email
ADAWA wants to support your practice with an easy to use and easy to implement system that enables you to manage your supply ordering and stock hassle-free. That’s why you’ll get 10% off Invedent as an ADAWA member. Visit invedent.com


ADA members are eligible to receive up to $2,000^ cashback on top of the cashback offer from the bank or lender (if eligible) on home loans successfully settled between 1 January 2023 and 31 December 2023.
Phone 1800 262 346 or email info@amafinance.com.au to find out more.
As one of ADAWA's valued corporate partners, ONDA provide timesaving services to our members, which are tailored to the busy dental professional. Until the end of the financial year, ONDA are offering our members a 15% discount on all new sign-ups to their financial admin services.
Contact george@ondagroup.com.au to book your free consultation.
Boutique commercial property company, VPG Property, is partnering with ADAWA to look after our members’ business and personal property needs. VPG Property is offering a free initial property consult to ADAWA members. vpgproperty.com.au

The issue of mental health has become a topic of interest in Australia over the last decade. The increasing complexity and pace of modern life means that balancing the day to day demands of work, home and family can be very challenging. This workshop will explore what we mean by good mental health and how we can nurture it in our day-to-day lives.
The workshop will cover:
1. An overview of psychological stress, how it develops, and how it can affect our health and wellbeing

2. How to recognise the signs of psychological distress, both in ourselves and others

3. An exploration of the skills required to maintain good mental health. This will include practical day to day strategies that workshop participants can immediately begin to use
4. A discussion of current issues: what is adding to the stress of individuals, what is minimising stress for individuals, and how they can improve the situation
The workshop will be highly interactive, with both didactic and experiential activities, and opportunity for questions and discussion.
3 CPD
Saturday 22 July 2023
Registration from 8.45 am Course 9 am to 12 pm
ADA House 54-58 Havelock Street, West Perth
Morning tea
$ 319 inc gst
MEMBERS
ABOUT THE PRESENTER
Ms Alexandra Hof has run a number stress management workshops for dentists. So she knows how dentists think and what our issues are. She completed a Master of Clinical/Health Psychology at Curtin University in 1994. Alex runs a private psychology practice in Perth, as well as providing workshops and presentations on a range of mental health topics. She has a strong interest in preventative mental health interventions.




A field of 22 players met at Hartfield Country Club in Forrestfield for the third fixture of the WADA Golf season. This event was sponsored by Insight Dental Ceramics, and we were pleased to be joined by Insight owners and ceramists, Andres Vivanco and Angus Wilshaw, for the day.




It was another glorious Perth autumn day with the recent rains providing lush but challenging conditions at Hartfield. Scoring reflected the tough conditions for some (well me really) and others blossomed.
The winner stood alone with 38 stableford Pts – Patrick Douglas, Ian McCarrey scoring 37 points came in second. David Owen was a close third with 36 points.
• 1st Patrick Douglas
• 2nd Ian McCarrey
• 3rd David Owen
• 4th Michael Whitford
The winner’s prize was presented by Andres and Angus. Andres and Angus presented Patrick Douglas with the winner’s prize. Our thanks are extended to Andres and Angus for their generous support.
4th hole Ian McCarrey Health Practice Brokers
6th hole Stu Phillips Swan Valley Dental Laboratory
12th Hole Simon Tee Dentsply Sirona
15th Hole Dean Hanson Healthlinc
18th Hole Simon Tee Longest Drive
Special mention to a new member Jun Liew who scored a great 42 Pts, and when his handicap becomes official, he should put in some challenges for the top awards.
We also welcomed our latest new member in Dean Hanson.
Our next fixture is at Joondalup Country Club on Friday, June 16. All interested golfers are welcome to join us for a game.
Good golfing, Frank Welten WADA Golf Captain Dentistgolf@gmail.com
What do you think is the most concerning procedure in so far as creating adverse outcomes in general dental practice today?
Ask yourself the question, and then read on as Dr Mike Rutherfo rd, Senior Dentolegal consultant for Dental Protection, sets it out .
The first response we often get to this question is: ‘Is it wisdom teeth?’, to which we will reply ‘Yes…. No…. Yes!’

Quite reasonably, you may then ask ‘Well is it or isn’t it?’ to which we would respond: Yes it is! But no – because it is not the number one issue we see (but it does produce some eye watering big numbered claims).
To explain this further, endodontics is by far the most common area of adverse outcome, and in particular fractured rotary files, so while that is very concerning in itself, these are contained or discreet problems. What this means is that at best a specialist endodontist removes the fractured file and there is no residual harm to the patient, or if it can’t be removed well then there may be an uneasy feeling that the tooth may fail one day but then it lasts indefinitely regardless; or worst case the tooth is lost and then remediation is required for one tooth. As a generality this is able to be done predictably, relatively simply and at not a great cost, generally.
But wisdom teeth – now there’s a can of worms. When things go wrong during general dentist third molar removal the best we can hope for
is a second surgery, often under GA by an OMFS colleague. That’s the best we can hope for – so at best your patient gets to be miserable twice, require a GA and take more time off work. That’s the best. And the worst? Well everything from a fractured mandible; to a potentially life threatening compromised airway from infection, inflammation or surgical emphysema; or a permanent paraesthesia of the Inferior Dental or Lingual (or both) nerves. So, we have all just read over that last sentence and moved on, but lets just back up a moment: a permanent paraesthesia of the inferior dental or lingual nerves. Have a think about this – this is a permanent impairment to the joy of kissing, perhaps the joy and/or ease of eating, sometimes a lifetime of worry that those around us will think if we slur our words, or, if we have food on our face and don’t realise. It’s an impairment to our working life and our job prospects.
Dental Protection uses the classic case of the French Horn player as an example of when specific warnings need to be given about potential nerve damage: the professional musician French Horn player who suffered an IDN paraesthesia and lost his livelihood and his sense of self, which was devastating. But what about your patient? What about the teacher, the receptionist, the salesperson, the waiter, the
barrister, the doctor – they are all impacted in their working and social lives by altered nerve function subsequent to third molar removal. In Australia, and in some states in particular, we are witnessing more frequent litigation around third molar injuries and a significant increase in general damages – what is often colloquially called “pain and suffering”. Partly the higher payments are due to the age of surgical patients. To use the same comparison, our endodontic patients are generally older and have less frequent and severe residual harm. Our third molar patients are generally young, and have to live with any incapacity for far longer. They are usually at an age when they are likely to be seeking employment, seeking relationships and social interactions. When a claim is made against a dentist it is often accompanied by an expert report – that is a report written by either a general dentist or an oral surgeon commenting on all aspects of the patient interactions and treatment that led to the adverse outcome. Unfortunately for many of our Members, the expert providing the report finds that the records and consent process are often easy. The first consideration is why? Why did you recommend the removal of this/ these third molars? Even here we often do not document and explain well. It’s obvious isn’t it? – just look at
the OPG! – I am afraid today that this doesn’t wash and neither does the long gone era of you have had ortho treatment, so now you need your third molars removed. If we don’t write a history and examination findings (of pericoronitis or whatever) we can’t record a diagnosis, and if we don’t record a diagnosis, how can we have valid recorded consent from our patient? Doing this is not in itself difficult, and it is therefore incredibly frustrating for the dentist involved and for Dental Protection to not be able to defend the integrity of a Member’s treatment when the documentation around the diagnosis and consent process consists of: needs eights out or similar.
To be clear, needs eights out or similar
• Is not a history
• Is not a description of the examination
• Is not a diagnosis
• Is not options presented including do nothing and specialist referral, risks and warnings presented including personalised particular risks and considerations (university exams, friends wedding, proximity of IDN, occupation of patient), consent discussed, costs involved, description of procedure, likely post op journey and cooperative requirements from the patient (such as rest, don’t exercise vigorously).
Despite all the lectures we attend and all the articles we read, and the fact that we communicate all this to the patient we, as a profession, are still not good at writing this discussion down.
Then what about assessment of difficulty (not just proximity to vulnerable structures)? This unfortunately is where things go wrong in many instances, and again is low hanging fruit for the dental expert report. Of course it is easy to be clever in hindsight but too often it is difficult to defend a Member’s decision to go ahead themselves, to not warn patients of the difficulty and offer to refer, and secondarily – to push on when the going gets
tough with no clear idea of what they are going to do next. If we miss the opportunity to refer a complex case prior to attempting removal, we should not miss the opportunity to refer when the complexity becomes apparent during surgery. Prolonged unsuccessful attempts at tooth removal is in nobody’s best interests. I am sorry if this article sounds dogmatic and prescriptive but Dental Protection is assisting with an increasing number of third molar cases that lack the required recordkeeping, consent and complexity analysis to defend vigorously. Inferior Dental or Lingual Nerve damage harms our patients but it also harms the dentist involved.
A Dental Protection Member, Dr B, phoned having received a statement of claim from a well known compensation law firm, accompanied by a scathing expert dental report and a demand for a six figure settlement sum. Our Member was devastated and having reviewed the case believed that there was nothing reasonable that he could have done to avoid the unfortunate outcome – paraesthesia of the left side Lingual Nerve distribution following removal of teeth 28, 38 some twelve months prior. Dr B was also confused, as the patient, Ms X a 27-year-old had not attended for post op review and had been lost to regular recall. This was the first time Dr B had become aware of the issue. Dr B did remember this patient well due to a mutual interest in horse jumping, and remembered that the procedure went without complications and he had removed both 28 and 38 simply with forceps using a non-surgical approach. The presenting condition had been described in his records as: 38 - persistent pericoronitis. Dr B also recalled that he had only removed the left side teeth as Ms X was changing careers and had little disposable income, but he had warned her that the right side, which had also been symptomatic, required attention.

Unfortunately on receipt of the clinical records by the Dental Protection Consultant it was evident that Dr B’s memory was better than his record keeping and detail was unfortunately very light. So what did the scathing expert report say?
Well, it started with a criticism of the lack of history taking - 38 –persistent pericoronitis – for how long, how often? What about the 48? Unfortunately the records were silent about this side. Risks and warnings given. What risks and what warnings were discussed, what about the particular risk for this particular patient that the third molar roots were in apparent close proximity to the IDN on both sides? The report commented on the proximity of the IDN to both lower molars and opined that this proximity warranted a referral to an oral surgeon, and although the injury occurred to another nerve (the Lingual N), on the balance of probabilities (in the expert’s opinion) the patient would have been less likely to incur this adverse outcome in the hands of an oral surgeon. Why was removal of all four third molars by an oral surgeon not recommended or even discussed?
Furthermore given the unfavourable root pattern of the 38 and the proximity of the IDN, opined the expert, if our member did carry out the procedure this should have been approached surgically with root division, to decrease the risk to the IDN.
On review of all the records of other practitioners who had seen her, it became evident that Ms X had not returned because after not being able to reach our Member on the provided mobile number, she had presented at the local hospital emergency department with severe neuropathic pain in the tongue three days post op (the weekend of course).
The attending OMFS reported CBCT examination had revealed a significant portion of the lingual bone plate was separated. Again the expert postulated that the ill advised use of forceps in the presence of IDN proximity and unfavourable root pattern had also increased the likelihood (when compared with surgery and root division) of a lingual plate fracture. This fracture had likely caused the Lingual Nerve trauma which presented as a distressing intermittent burning dysthaesia.
It is easy to write a critical report in hindsight knowing the unfortunate outcome, but the flawed consent and record of conversation around why Dr B treated as he did, made defence difficult. Again it was also difficult to defend our Member’s well intentioned forceps approach in view of the IDN proximity and the appearance of the root structure on the OPG. Our Member was trying to make this extraction as simple and as least expensive as reasonable for his patient.
Fortunately the burning dysthaesia subsided, but to a persistent and permanent partial numbness of the tongue. Ms X’s solicitors were able to emphasise the distress that this change to Ms X’s articulation of her words caused her, and the devastation of not being able to continue with her training as communications consultant because of this. In consideration of the ramifications of this injury on Ms X’s lifestyle and psyche, Dental Protection settled for a significant sum.
Dr B remained distressed by the outcome of his wellintentioned treatment and was offered collegiate support and recommended minor oral surgery courses to attend. At Dental Protection’s suggestion Dr B approached the oral surgeon he referred patients to, who offered to let Dr B assist in theatre for a few sessions to hone his skills.

I wish I could say this was just a story. I wish I could say it’s in isolation. But I can’t. We need to be giving greater consideration to our assessment of wisdom teeth, and to our documentation of the pre treatment discussions, or not only could we find ourselves in Dr B’s shoes, but also, we will cause more patient’s like Ms X issues, that could have been avoided.
When managed effectively, good communication provides many advantages to both the practice and individuals. Good communication often leads to increased productivity, a more positive work culture and greater cooperation and collaboration within the practice. Ensuring communication is prioritised also reduces the likelihood of conflict at work and promotes employee retention in the long run. This article sets out several key steps to ensuring you are well underway to fostering good quality communication in the workplace.
Have well established communication channels
Ensuring that practice-wide communications are made regularly and to a central location is key. It is recommended that practices use a dedicated platform or location to distribute important messages clearly and promptly. By streamlining all communication to a minimal number of platforms, employees are more likely to stay up-to-date and well informed. Methods of mass communication might include an electronic or physical notice board, or alternatively, periodic staff emails could be sent when important information or notifications need distributing. Regardless of what type
of platform the practice wishes to use to communicate, staff should be made aware of what/where this will be and how often they should be required to check this platform. The practice should also establish clear reporting structures. For example, it should be clear who employees can communicate any absences, grievances, rostering issues or payroll concerns to. Reporting structures can be communicated and publicized via company policies and documents such as an employee handbook.
Ensure staff are well trained and understand the importance of good patient communication
While communication between employees is important, the nature of customer interactions can also have a major impact on the practice. It is recommended that employees are made aware of service level expectations for when communicating with patients of the practice. Generic customer service training and refreshers could be used to remind staff of expectations, reinvigorate the team, and ensure that high levels of service are upheld.
Setting up regular meetings with employees to check in, discuss
We often hear that communication is important in the workplace, however, refining the ability to communicate well with a range of employees can often prove to be rather challenging.
updates and generally build good rapport is a great way to ensure that management personnel within the practice lead by example and show what good communication should look like. Setting up regular meetings creates a perception that communication is a priority and ensures that staff are regularly engaged with. Regular meetings provide an opportunity to deliver practice updates and allows issues to be addressed on a consistent basis, rather than only addressing once they have escalated and become more complex.
While group meetings serve their purpose, 1:1 meetings with individual employees provide a great opportunity for management personnel to practice active listening and build understanding and rapport. Periodic 1:1’s give management great insight into how an employee is tracking, allows
issues to be discussed in a more private context and creates a sense of trust and care from an employee perspective.
Understand different communication styles in the workplace

Understanding that everyone is naturally going to communicate in different ways is key to overcoming communication barriers at work and avoiding conflict. Understanding whether someone may be an assertive or passive communicator can be beneficial in building an understanding of how to approach and manage certain individuals. Learning to respect, tolerate and adapt to varying communication styles will make the workplace a more harmonious and productive environment.
For more information on this article please call the ADA HR Advisory Service on 1300 232 462.
Private practice, Perth Oral Medicine and Dental Sleep Centre, West Leederville
Adjunct Senior Lecturer, The University of Western Australia, Dental School, Nedlands
An 82-year-old male was referred to Oral Medicine for severe dry mouth that he noted about 1 year (May 2022) prior to his presentation. The onset of his symptoms was sudden and progressive, and he now reports reduced saliva and difficulty in swallowing food. Upon further questioning, he also reports dry and irritated eyes noted at the same time as his dry mouth. His medical history is significant for hyperlipidaemia, type II diabetes and stage IIIc melanoma, managed with surgery and adjuvant pembrolizumab infusions (commenced in April 2022). His other medications include 10mg rosuvastatin and 500mg metformin.

My examination revealed the presence of moderate salivary gland hypofunction including frothy saliva, a lack of pooling of saliva in the floor of mouth, and a lobulated, fissured tongue (Figure 1). The intra oral mirrors were noted to stick to the buccal mucosa and there was lack of saliva secretions upon palpation of the submandibular glands. No regional lymphadenopathy was palpable extraorally. Temporomandibular joints and muscles of mastication were within normal limits. Normal mouth opening and mandibular range of motion was noted. No other oral mucosal swellings or lesions were noted. MRI imaging of the major salivary glands were unremarkable.
Based on the history and clinical findings, what is the most likely cause for the patient’s salivary gland dysfunction?
a) Salivary gland neoplasm
b) Dehydration
c) Type II diabetes
d) Pembrolizumab
Answer: d
Cancer immunotherapy is quickly becoming a central pillar of cancer therapy. The first series of cancer immunotherapy constituted the immune check point inhibitors (ICIs). ICIs are monoclonal antibodies that work by blocking immune checkpoints, negative regulators of T cells that are co-designated by tumours to induce T-cell exhaustion and suppress anti-tumour immune activity. As these drugs increase immune activity, ICIs can induce a wide variety of inflammatory side effects known as immune-related adverse events (IRAEs). IRAEs typically develop within the first few weeks to months after initiating treatment, but can occur anytime, even after treatment has been discontinued. The most common organ systems affected include the gastrointestinal tract, endocrine glands, skin and liver, however evidence on the effects on oral mucosa and salivary glands are
emerging, with an estimated incidence of 7% in patients treated with ICIs.

This case is an example of ICI – induced Sjögren's syndrome-like reaction. Sjögren's syndrome – like reactions, have been reported in patients treated with durvalumab, avelumab, pembrolizumab, nivolumab and ipilimumab. Clinical features include abrupt onset of severe xerostomia, salivary gland hypofunction, ocular dryness, and rarely bilateral parotid swelling. Patients may demonstrate reduced whole unstimulated salivary flow rate, or visible signs of oral mucosal dryness. Additional systemic features of Sjögren's syndrome (e.g., cutaneous, articular) can be present. A small proportion of patients may demonstrate positive serology (6% - 14%), while histopathological features of minor salivary gland biopsies in affected patients have ranged from mild non-specific chronic sialadenitis (50%) to focal lymphocytic sialadenitis of varying severity.
Management varies from lifestyle changes (e.g., increased hydration, avoidance of caffeine), saliva replacements (e.g., Biotene®, Oral 7®, Xylimelts®, sugar-free gum), and systemic sialagogues such as pilocarpine. In severe cases, discontinuation of ICI therapy and initiating systemic steroids with or without additional immunosuppressive agents (e.g., hydroxychloroquine) have been utilised. Caries prevention must be considered given the increased risk of dental caries in the setting of hyposalivation.


As immunotherapy continues to evolve, the rate of IRAEs will likely follow. As such, it is important for oral health practitioners to be aware of IRAEs and associated oral mucosal and salivary manifestations.
For further reading
Klein, B. A., Alves, F. A., de Santana Rodrigues Velho, J., Vacharotayangul, P., Hanna, G. J., LeBoeuf, N. R., Shazib, M. A., Villa, A., Woo, S.-B., Sroussi, H., Sonis, S., & Treister, N. S. (2021). Oral manifestations of immune-related adverse events in cancer patients treated with immune checkpoint inhibitors. Oral Diseases, 28, 9– 22.


In our increasingly digital world, dental industry businesses are finding it harder than ever to stand out from the crowd. With the huge amount of content we are all consuming these days, it can be difficult to gain the attention of potential customers, associates and collaborators, and dental industry businesses must have a brand image that is recognised and trusted. With human attention span decreasing, currently at 8 seconds, it’s more important than ever to stand out from the crowd when you want to share information or get the
As mentioned previously, with collective attention spans decreasing, the first impression of your business will either keep your potential audience reading or send them away within 8 seconds.
attention of your audience. That’s why using professional images and videos across all your marketing and PR is imperative in today’s world. Also, in any specialised industry, particularly dental, images must also be authentic. That means that what actually happens in the surgery should be depicted in the images. There are many ‘stock’ photo companies where you can purchase dental images, but often the images are photographed under ‘studio’ settings and some are not even using the correct tools.
If you want to keep your audience coming back to read your articles, blogs and more, you must establish a recognisable brand your audience can trust. Your brand image is more important than you might think!
There’s no point in choosing stunning images if they don’t show what really happens in a dental clinic, the tools used, or if they are not relevant to dental industry standards. Your potential audiences’ brains will recognise and turn away from inauthentic images – every time.
ADAWA members are eligible for a 20% discount off the Recommended Retail Price to purchase photographs from Dental Stock Photos. Go to dentalstockphotos.com/ pages/ada-wa-members-information for details.
With Dental Stock Photos you can rest assured our images are taken by dental professionals who know the industry inside out! With over 2500 dental images available, taken by highly skilled and experienced photographers who are continually adding new stock, you are sure to find the dental clinic images you are looking for.
are the 3 reasons why authentic, professional
can make a difference to your brand
Rural Health West has been working closely with The University of Western Australia to develop placements aimed at increasing the profile of rural practice for the future dental workforce. Rural Health West Senior Workforce Consultant Brooke Wilson said the idea first came about nearly eight years ago when she struggled to recruit dentists into rural locations, despite strong demand from employing practices. “There seemed to be very little interest from dental graduates to consider roles in the country, as they had received little to no exposure to rural practice during their studies.
“The only ‘rural’ placement option was Bunbury, which is really a large regional city and not particularly reflective of practising in locations such as Esperance, Kununurra or Katanning.”

The stars aligned for Brooke when she crossed paths with specialist paediatric dentist and UWA senior lecturer in clinical dentistry, Dr Jilen Patel, about 18 months ago.
“Jilen provides visiting dental services in the Kimberley and he was quite concerned about the lack of dental care available to the remote communities there. He was really passionate about addressing that service gap and recognised that providing dental students with immersion opportunities could be a potential solution.”
Since that time, Jilen and Brooke have been working to get rural and remote clinical placements off the ground for UWA’s dental students.
“It’s been a huge exercise in logistics, as well as stakeholder relationships. Dental students need close clinical supervision and as many of the
After years of planning and collaboration, dental students in Western Australia now have more opportunity to complete clinical placements in rural and remote locations as part of their studies.Article provided by Rural Health West
remote communities are unable to provide this supervision, we can’t just send a student out alone. There also needs to be a supervisor. We also then needed to identify clinics willing to host the students and their supervisor and arrange patient appointments. Plus finding accommodation, which can be scarce in many rural towns, funding for travel etc. It has been a huge effort from all involved.”
These efforts have paid off with the first remote placement taking place in April with two dental students, Hayden and Wendy, and clinical supervisor, Dr Tracey Gold, spending two weeks working out of the dental practice at the Derby Aboriginal Health Service in WA’s Kimberley region. Tracey said the experience was very beneficial for the students to see how dentistry works in a remote setting.
“Many of the appointments over the fortnight were not planned, they mostly required emergency treatment and the students got to understand the burden of disease in such remote locations,” said Tracey.
However, Broome also has a shortage of dentists and the waiting list for an emergency appointment can be up to six weeks.
“So there is truly a dire need to increase the number of dentists choosing to practise rurally, and that needs to be nurtured and encouraged among aspiring dentists.” Dental student Wendy said the experience has given her a greater appreciation of the inequity of health services in the country.
“Every patient we saw had so much work that needed to be done; and it wasn’t work that should be delayed, such as patients with acute pain for weeks and months."
"It felt great to provide such a vital service; it was very rewarding. However, there needs to be better access to care, both emergency and preventive.”
sterilisation; however, we had to do that ourselves, so we had a quick crash course in that. We also learnt to problem solve when we encountered issues with equipment, as you can’t duck out to the nearest supplier.
“It was also valuable to work alongside allied health professionals. Dentistry in Perth can be quite isolating, but working in an allied health setting like DAHS, we were able to witness how intra-professional clinical communication and integration can lead to better overall health outcomes.”
At the completion of their time in Derby, the trio travelled to Broome to visit the dental facilities at Broome Regional Aboriginal Medical Service and two private clinics.
hours away – to see a dentist.
Dental student Hayden said the placement had inspired him to return. “In the city, we wouldn’t be doing the type of work we were undertaking while in Derby. We’ve done lots of oral surgery, extractions, fillings and witnessed the impact of people being unable to access the care they need.” Wendy said while the clinical experience was fantastic, the experience was beneficial in other ways. “In Perth, we would have nurses who would take care of
Brooke said the students appreciated the chance to see the variety of practice they could expect in the country.
“Both Hayden and Wendy seemed quite keen to explore options to work in both the Aboriginal health setting, as well as private practice. There are plenty of opportunities available to them and certainly many potential job offers on the horizon for them in the future.”
“In Derby, there is no permanent dental care and people need to travel to Broome – about 2.5
WA Dental CPD recently went international with the Oral Medicine Rojak course held in Singapore in April. Many attendees were able to combine CPD with a short holiday! Thank you to presenters, Drs Amanda Phoon Nguyen and Tom Huang.

ADAWA is proud to sponsor a number of awards at the UWA Dental School’s Annual Prize Giving Ceremony. Support for our members starts from the time they are in Dental School, right through to their retirement and beyond.
A special congratulations to the deserving recipients (pictured with ADAWA President Dr Amit Gurbuxani and ADAWA CEO Trevor Lovelle);

Kaylee Wong
ADAWA Branch Prize recipient
Sarah Boon
ADAWA Prize for Academic Excellence in Dentistry
Scott Santarossa
ADAWA Award for Leadership Excellence in Dentistry (not pictured)
In a wonderful display of interdisciplinary education, Master of Pharmacy final year students, UDSS, UWA Dental School and ADAWA recently collaborated to host a workshop about oral health conditions commonly encountered at the community pharmacy setting. It was a wonderful event that was well-attended and is hopefully the start of more interdisciplinary events.
Rockingham Dental recently hosted a successful Dental Rescue Day, treating 13 patients on the day, and offering to adopt four patients for ongoing treatment. Thank you so much to volunteer dentists, Drs Vilas Menon, Hari Menon, Zena Ibrahim and Jude Ferando, and their hard-working practice team. There is a dire need in the Rockingham and Peel region for volunteers like Rockingham Dental Centre. If your practice would like to find out more about hosting an ADHF Dental Rescue Day, contact Andrea Paterson at adminwa@adhf.org.au

CHAT international volunteer dental missions are back this year, and volunteers are wanted for trips in September and November.
If you would like to help make a difference in rural areas of southern Vietnam, consider volunteering for the following trips to Vietnam:
September 16-23
November 18-25
Join us at the General Meeting with a special presentation from prosthodontist, Dr Sundar Varadharajan ‘Desperate times call for desperate measures; restorative solutions for compromised implant placement’.

ADA House
54-58 Havelock St West Perth
6.15pm Eat and Meet
7.15pm Meeting Followed by Lecture
RSVP to adawa.com.au/membership/rsvp
For details about the trips or more information with CHAT, contact secretary@chatinc.org.au adawa.com.au

We wish to inform our members of the sad passing of one of our former Council members.
Dr May joined Council in 1994 and served as a Councillor up until the end of 2000. Dr May was the Chair of the House and Social Committee from his start until 2000. He was instrumental in the move from Altona Street to our current premises at ADA House in Havelock Street. Dr May also served on the UCDEC Committee in 1997 – and the Emergency Dental Practice Arrangement Committee for 1998-2000.
Dr May will be fondly remembered by the members and staff of the ADAWA, and we send our condolences to his family and loved ones.
We also wish to inform our members of the sad passing of orthodontist, Dr Peter Heagney, who was an ADAWA member for over 50 years.
Dr Heagney served as the President of the University Dental Students Society and also served on the ADA (WA Branch) Post Graduate Education Committee and the Constitution and Ethics Community. He was a gracious mentor to dental students. Dr Heagney passed away after a long illness. We send out condolences to his family and loved ones.
Dr Jessica Kong - new addition to the team

Victoria Park Orthodontics is delighted to announce Specialist Orthodontist Dr Jessica Kong has joined Dr Frank Furfaro, Dr Angela Ross and Dr Christophe Duigou in our modern and newly expanded specialist orthodontic practice. Dr Jessica Kong is now accepting referrals for all aspects of orthodontic care, from early interceptive treatment to adult orthodontics.
We are pleased to announce that Specialist Periodontist Dr Anchalee Jennings-Lowe has joined Vision Periodontics. She is accepting referrals for all aspects of periodontics and implant surgery.

T +61 9361 0022
E reception@vicparkortho.com.au
A Level 1, 734 Albany Hwy, East Victoria Park 6101
W vicparkortho.com.au
Dr Fleur Creeper is excited to be returning to practice in her new periodontal studio. She looks forward to supporting your patients with their periodontal needs and is gratefully accepting referrals.
T (08) 6430 0333
E admin@visionperiodontics.com.au

A Unit 1/26 Charles Street, South Perth
W visionperiodontics.com.au
T (08) 6184 4754
E hello@thegumstudio.com

A 252 Stirling Street, Perth
W thegumstudio.com
Dr Laura Leask - new addition to the team

Smile Time Orthodontics are pleased to welcome Dr Laura Leask to the specialist team.


FREMANTLE
T (08) 9335 4031
E Fremantle@smiletime.com.au
A 45 Quarry Street, Fremantle
MT HAWTHORN
T (08) 9443 6188
E Fremantle@smiletime.com.au
A Unit 2/187 Scarborough Bch Rd, Mt Hawthorn
W smiletime.com.au
adawa.com.au
Save

At
That’s why our commercial property loans give you the ability to borrow up to 100% of the purchase price of your practice premises. What’s more, for a limited time you can save up to $2,500 on valuation fees when you choose to finance your commercial property purchase with us.^
We’ve been helping dental professionals secure their practice premises for over 30 years. Now let us help you. Visit