Why retain dental records?
Getting informed financial consent
How to deal with workplace incidents

Looking back to how we adapted as a profession.

Why retain dental records?
Getting informed financial consent
How to deal with workplace incidents

Looking back to how we adapted as a profession.
PRESIDENT
A/Prof Alex Forrest AO
SENIOR VICE PRESIDENT
Dr Matthew Nangle
JUNIOR VICE PRESIDENT
Dr Jay Hsing
COUNCILLORS
Dr Meglin Rathnasamy (Peninsula)
Dr Kelly Hennessy (Central)
Dr Kaye Kendall (Moreton)
Dr Gina Irwin (Western)
Dr David Le (Moreton)
Dr Graeme Westacott (Moreton)
FEDERAL COUNCILLORS
Dr Angie Nilsson
Dr Martin Webb
IMMEDIATE PAST PRESIDENT
Dr Norah Ayad
ADAQ SUB-BRANCHES
Bundaberg
Dr Paul Dever
Ipswich
Dr Andrew Wong
Kingaroy Dr Jonathan Pye
ADAQ COMMITTEES
Dental Practice Committee
Convener: Dr Matthew Nangle
Dental History Preservation Committee
Convener: Dr Gary Smith
Volunteering in Dentistry Committee
Convener: Dr Jay Hsing
Mackay Dr Peter Monckton
Sunshine Coast Dr Peter Jorgensen
Gladstone Dr Patrick Dohring
Dr Joseph Nguyen (Burnett)
Dr Tim Keys (Sunshine Coast)
Oral Health Committee
Convener: Dr Kaye Kendall
Toowoomba Dr Rob Sivertsen
Gold Coast Dr Gabriela Ciubuc-Batau
Dr Sobia Zafar (Moreton)
Dr Keith Willis (Moreton)
Conduct & Honours Committee
Convener: A/Prof Alex Forrest AO
Asset Management Committee
Convener (interim): Dr Jay Hsing
Cairns Dr Karen Pettigrew
Rockhampton Dr Kelly Hennessy

Recent Graduates & Students Committee
Convener: Dr Malak Fouda
Audit Risk & Compliance
Convener (interim): Dr Martin Webb

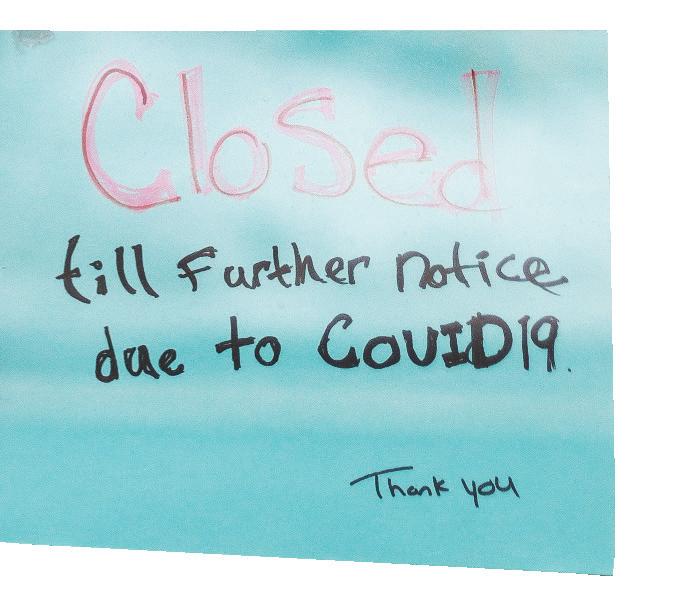
Talk of the COVID-19 virus had been swirling since late 2019 and by the time it reached Queensland on January 21, the virus had been reported in more than 170 countries with large outbreaks in Europe and the United States. On January 29, with more cases presenting daily, the Queensland Government declared a public health emergency.
Although physically distanced, we were able to come together and collaborate as an entire team daily.
When COVID-19 began to impact the Queensland community in March 2020, ADAQ’s Leadership team and President took sensible steps to help protect the staff. The decisions were made
“Although physically distanced, we were able to come together and collaborate as an entire team daily,” says Miriah Sawrey, PA to CEO.
ADAQ staff had daily meetings via Microsoft Teams so we could continue to communicate and support each other whilst also understanding the common enquiries from Members.
516 hours time spent on phone calls
2986 number of phone calls
Data between 16 Mar - 22 May 2020
Telephone support remained uninterrupted, and Members relied on ADAQ more than they ever had, with enquiries ranging from infection control to HR issues to just plain reassurance that everything would be okay.


Distributed to Members via email, social media, and ADAQ website
RESOURCES PROVIDED
Member Assistance Program
Access to wellness support resources and 24/7 counselling sessions
Financial advice and information
Prosperity Health provided a summary of information on the Federal Government’s $66 billion economic lifeline and the Queensland Government’s stimulus package.
HR Support
Information for staff and employers on JobKeeper, legislation, and fair work information and a range of FAQ’s.
ADA Guidelines
Decision trees, PPE support, Practice posters and signage
Infection Control
Updates and documentation along with videos from Prof. Laurie Walsh about COVID and what it means for the dental profession
Practice accreditation support
Free access to ADA’s practice accreditation modules and documentation
Internal approval from legal and regulatory perspective
Marketing Team would create email, set-up mailing list, and test Internal approval from legal and regulatory perspective

STAYING CONNECTED DURING COVID-19
ADAQ strived to connect with Members. We increased our digital approach – our focus was to reach Members quickly via email, website updates and social media with important updates and reminders of relevant Member services to support them both professional and personally through the pandemic.
ADAQ needed to support the Queensland Dentistry Profession as a whole , by providing information for non-members as well as members.
“ADAQ needed to support the Queensland dentistry profession as a whole,” says Teagan Criddle, ADAQ Accounts Officer. “By providing information for non-members as well as members, we could ensure there was continuity among the profession and that dentists could provide the safest possible care for the community, armed with the most up to date and accurate information.”
Through our COVID daily summary emails and webpage, we collated our support and guidance services to make it easy for Members to access the relevant information. In total we sent 33 emails during the acute phase and a further 13 to date.
To ensure accurate information was being disseminated to Members, there were frequent calls with the Chief Dental Officer, Dr Mark Brown. Internally, a six-step process was followed (see flowchart above).
While this process took a few hours, it meant that the messaging was thorough and it could be relied upon.
A decision was made by the ADAQ Council to have the COVID-19 information publicly available to support the entire profession, regardless of whether they were Members. It was important to have a united front and support the entire profession and thereby the community throughout the pandemic.
TRANSITIONING TO ONLINE LEARNING THROUGH COVID-19
600+ attendees

455 attendees
Between late June - December 2020

The pandemic forced us to cancel or postpone face-to-face events for a number of months. The ADAQ CPD and events team adapted quickly and developed a program of free educational webinars.
In late June, we returned to socially distanced face-to-face events and through until the end of the year ran 28 events with 455 attendees. Whilst CPD was not a priority for many Dental Professionals, it was critical that ADAQ was able to provide these courses for those that required this support. We continue to develop our resources by adding a video library, and on-demand CPD courses will be coming soon.
SUSTAINING THROUGH COVID-19
75% of registered QLD dentists are Members of ADAQ
Members opted for quarterly payments or deferment (17%)
Dental practitioners were on restricted practice from 24 March to 11 May 2020. During this period, many had to cancel bookings, stand staff down and close their doors. Knowing many
16 MARCH
SPECIAL REPORT
2020-21 TIMELINE
1 APRIL
Lockdown ended – ongoing mask wearing requirement until 15 April
29 MARCH 3-day lockdown announced for Greater Brisbane region.
Cancellation of all nonessential treatment and


COVID 19 Cases significantly increase within the state. Some services begin suspension (ANZAC celebrations, UQ lectures, police drink and drug driving tests)

17 MARCH
Announcement of 1B vaccination rollout for front line health professionals commencing 22 March.
18 MARCH
ADAQ put in place temporary work-fromhome arrangements for all staff, effective Monday 23 March
23 MARCH
From midday, Queensland shut down of non-essential services.


8 JANUARY 3-day lockdown announced for Greater Brisbane region.
11 JANUARY
Lockdown ended – ongoing requirement of mask wearing until 22 Jan.


practitioners were struggling, the ADAQ CEO and Council held a meeting to discuss offering relief for the upcoming membership renewals period.
It was agreed that ADAQ would introduce quarterly payments but also allow Members to defer their payments, allowing an extra three months to pay their subscriptions.
The value of Membership has never been more clearly illustrated as it was during the lockdown period. Practitioners saw the support and advice ADAQ was providing and as a result, we attracted 129 additional Members, an increase of 4%.
successfully advocated for
no increase in Federal ADA membership subscriptions
no increase in insurance premiums
option of deferred payment for 3 months
24 MARCH
Dental Practices placed on level 2 restrictions.
25 MARCH
Dental Practices placed on level 3 restrictions and Queensland state borders close.

ADAQ returned to face-to-face, socially-distanced events in late June 2020.

8 APRIL
ADAQ cancelled all faceto-face CPD events until May 31.
21 APRIL
The Prime Minister announced that restrictions would ease from Monday 27 April, with practices moving to Level 2 restrictions

27 MAY
ADAQ Face-to-face CPD events return with restrictions. Final daily summary paused due to eased restrictions.

11 MAY
Dental Practices moved to level 1 restrictions
27 APRIL

ADAQ Membership renewal period opens with no increase on subscriptions.
27 APRIL
Dental Practices moved to level 2 restrictions


ADAQ provided Members the option to defer payments for 3 months and the introduction of quarterly payments.
There were times we were on the phone for hours listening to their concerns and reassuring them.
There is no denying the impact COVID-19 has had on the profession, patients and communities. ADAQ’s mission was to be there from the beginning to provide advice, education, resources and assurance. As the old saying goes, ‘we were given lemons and together we made lemonade’.
“It was great to really connect with our Members and show them we were here to support them through difficult times,” says Davina Barker, ADAQ Education & Practice Advisor. “There were times we were on the phone for hours listening to their concerns and reassuring them. We constantly sought advice from experts to ensure our Members and the community were kept up to date.”
The pandemic is not over yet. Cases continue to arrive from overseas and the virus and its newer variants sometimes escape quarantine. Further community outbreaks can be anticipated although the risk may decrease with more widespread vaccination, and we are ready in the event of future lockdowns to continue to provide you with timely and accurate messaging and services.


The important and reliable information needed to protect us all will remain with you no matter what the situation - we have your back.
“The work that our CEO, Management Team and Staff did under the extraordinary circumstances caused by the COVID-19 pandemic saw seamless maintenance of services to our Members, and timely updates and reliable information delivered to all dentists in Queensland to help protect them, their staff and their patients,” recalls A/Prof Alex Forrest, ADAQ President 2021. “This was made possible by having protocols prepared in advance for exactly this type of situation. We continue to plan for all reasonably foreseeable contingencies to support you regardless of any emergency we may encounter, and our support with services and the important and reliable information needed to protect us all will remain with you no matter what the situation as long as we can continue to function. We have your back!”


Public health laws give certain powers to the Chief Medical Officer and DirectorGeneral of Health so they can control the spread of a pandemic.

Public health measures during lockdowns including border closures and interruptions to certain businesses are enacted by public health authorities in the affected jurisdictions. The public health laws give certain powers to the Chief Medical Officer and Director-General of Health so they can direct certain actions. Controlling the spread of the pandemic is exactly what these types of powers are designed to achieve.
When there is a surge in the number of cases of community transmission, all of the state and national pandemic plans call for an elevation in control measures. That is in the pandemic 101 handbook of practically every state or national government around the world, so it’s a predictable thing to see when there is clearly a surge in cases of (in this case) a particularly contagious strain of the virus. Bear in mind in this situation that the role of the ADA remains as always to support members. The ADA is not a regulator. The regulator is the guard dog, while the ADA is the guide dog. Advice from the ADA has been pivotal in creating a situation where dental services did not shut down completely during periods of lockdown.
In any pandemic, it is common to see small outbreaks which then need to be suppressed. In public health management of pandemics, this is known as “the hammer and the dance”. The hammer is the measures to suppress and eliminate cases in the community. The dance is the withdrawal of those measures in a gradated way that does not allow another outbreak to get out of control. One only has to look at the second wave in Victoria to see the consequences of a situation that has got out of control - or to look at the third wave which is currently occurring in Europe.
There is an extensive literature on aerosol transmission of COVID-19 and in July 2020, based on this evidence, the WHO
changed their official advice and emphasised the importance of aerosol based transmission in certain situations.
The ADA is not a regulator. The regulator is the guard dog, while the ADA is the guide dog.
The series of layered measures which sit within the ADA advice for the pandemic have been successful in preventing large numbers of cases of COVID-19 in Australian dentists being acquired in the workplace. Published evidence from the USA also shows that the layered measures used in the USA (which were almost the same) were also very effective.
There is a paper on COVID-19 published roughly every 14 minutes and one cannot expect the general dentist to wade through such an enormous mountain of information nor consider how best to apply all that information into the setting of a dental practice. This is where the expertise of the ADA’s Infection Control Committee comes in. It distills evidence into practical recommendationsbased around the concept of ‘as much as necessary, but as little as possible.’
The whole concept of transmission-based precautions underpins all modern infection prevention and control approaches, and indeed this is legally enshrined in the requirements in Queensland
for what must be included in a dental practice’s infection control management plan. Hence at a time when the risk is greater (which is clearly the case at the moment), more stronger control measures are needed. When the risk reduces, so does the stringency of the control measures. It’s not a difficult concept to see that the two must be related.
A final comment is that we know from research conducted right here in Brisbane that using the triplex syringe and using power dental instruments generates large amounts of particles in the size range of 1 to 2 µm, i.e., aerosols. This adds to an already large literature where there are over 80 studies as well as several recent systematic reviews (all published in 2021). Such systematic reviews represent the highest level of the pyramid of evidence-based dentistry.
DR ANGIE NILSSON
ADAQ FEDERAL COUNCILLOR
WHAT KEEPS YOU BUSY AT THE MOMENT?
There is a paper on COVID-19 published roughly every 14 minutes and one cannot expect the general dentist to wade through such an enormous mountain of information. This is where the expertise of the ADA’s Infection Control Committee comes in.
One only has to look at the situation in some other parts of the world to recognise that Australia has been quite successful in containing the spread of COVID-19. The level of disruption to everyday life experienced in this country is nothing like what has been experienced overseas. A lockdown for three days is certainly an inconvenience to the practice, but when considered in the wider context of suppression and elimination of community transmission, would be regarded by most as a justifiable measure. After all, these lessons were all learnt 100 years ago with the Spanish Flu. Those who did not make the effort to contain the spread experienced second and third waves of infection.
The virus is different, but the patterns are the same. Those who do not learn from the lessons of history are destined to repeat the errors of the past. Containment, lockdowns, physical distancing, and the wearing of masks and other items of PPE were effective in the pandemic 100 years ago. They remain effective today. Contact tracing information from Australia shows clearly that one single person with COVID-19 can be responsible for an outbreak of several hundred cases in the community.
To paraphrase the old saying, no one raindrop believes that it is responsible for the flood. EMERITUS
Me keeps me busy. I enjoy working under pressure and learning new things; between my job, PhD study, ADAQ council, house reno, and my two boys (three if you count my husband), there is always something to keep me occupied.

WHAT DREW YOU TO A CAREER IN DENTISTRY?
I wanted to be a film score composer; my music teacher let me know fairly early on it probably wasn’t going to work out, so I looked into healthcare and being able to work with my hands. My high school work placement at a dental practice turned into a regular gig and it went from there
WHAT ARE YOU AIMING TO ACHIEVE IN YOUR TIME AS AN ADAQ COUNCILLOR?
I didn’t come into the role with specific aims; I joined to serve the members and needs of the organisation. What I hope to see is collaboration and innovation.
WHAT MOTIVATED YOU TO JOIN THE ADAQ COUNCIL AND GIVE BACK TO THE INDUSTRY?
I missed working with a council with a unified purpose; I had such an amazing experience working with the ADA Tasmanian branch councillors that I was excited to meet the Queensland crew. ADAQ have achieved amazing things with a lot of courage in the last few years; to be a part of a new chapter is a great opportunity.
WHAT DO YOU LIKE TO DO IN YOUR SPARE TIME AWAY FROM DENTISTRY?
I spend time with my family; they keep me grounded. I started skate-boarding a few years ago and have kept it up in the hope my kids still want to hang out with me as teenagers! I still play the piano; better than any yoga or massage to get the cobwebs out of my brain.
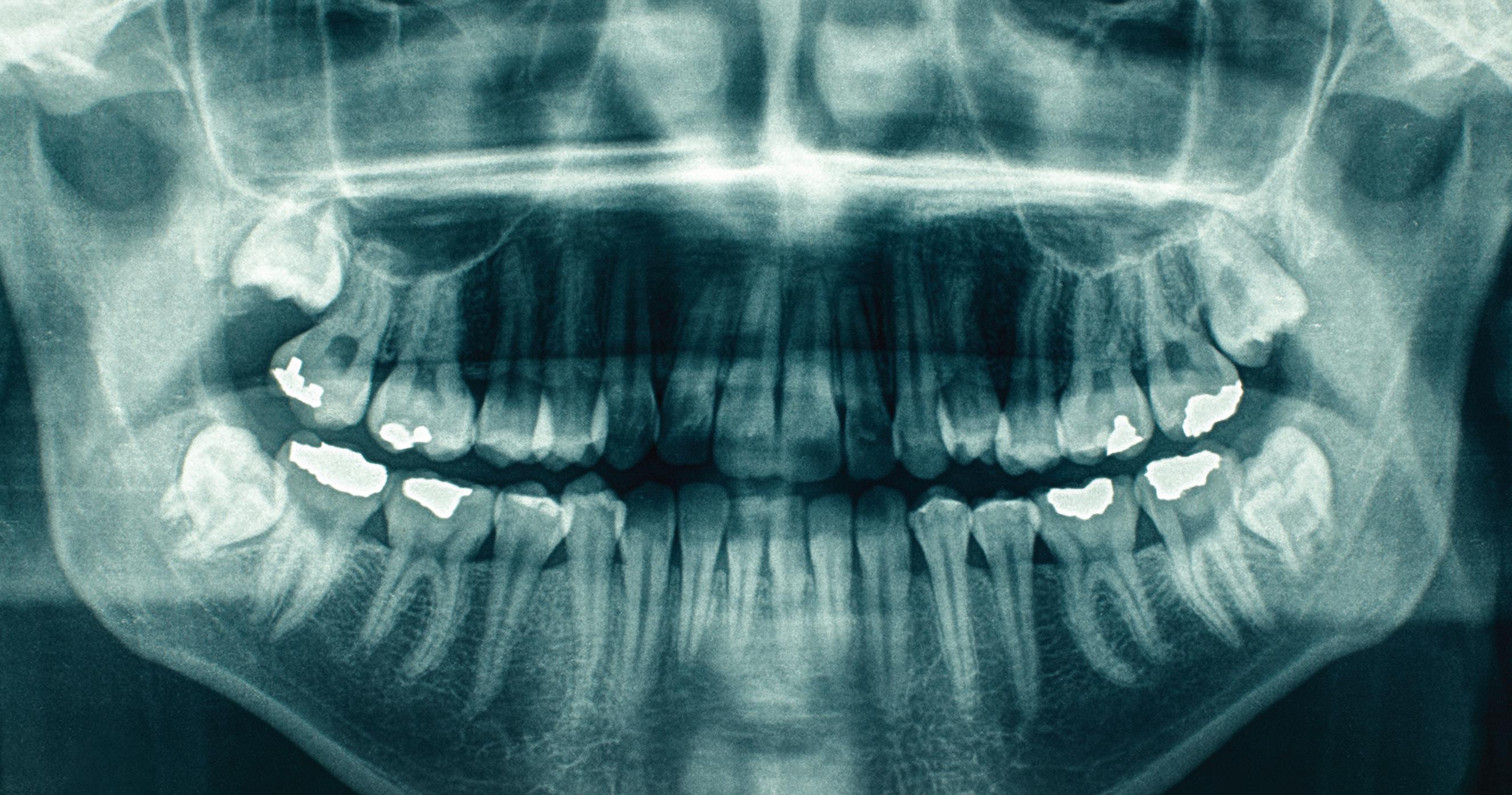
The fundamental human right to an identity is recognised through many conventions and declarations including Article 6 of the United Nations Universal Declaration of Human Rights.
As forensic odontologists, much of our work involves identifying deceased individuals. Generally, we are asked to deal with individuals who can’t be identified by simpler means such as being viewed by relatives or friends. This may be because they have died in traumatic circumstances, or perhaps they haven’t been found for some time following death, or no relatives or friends can be located. Usually they are no longer recognisable or it would be distressing for relatives to see them.
Police conduct an investigation to determine the likely identity of the deceased person, and then a scientific basis for establishing this is sought. The final evidence is considered by a Coroner, who will certify identity on the basis of the information before them. There are three disciplines that can provide an opinion on identity that will be accepted as definitive. These are DNA comparison, fingerprint comparison, and the comparison of dental features with dental records by a forensic odontologist.
DNA comparison is time-consuming and expensive, and it relies on getting a sample with which to compare the profile of the deceased person. This may involve police looking for such things as toothbrushes or other personal items that are likely to contain their DNA, but people share such things (even toothbrushes!), and so this can lead to confusing outcomes.
• Based on DNA sample known to be of the deceased (e.g. from personal items)
• Compete with criminal casework and may not be prioritized
• Based on fingerprints at a dwelling
• Requires careful interpretation to distinguish from other fingerprints
• Success depends on quality of dental records and whether they have not been destroyed by a practice
Forensic DNA profile matching also needs to compete with criminal casework and may not be prioritised. Police may have to approach relatives to seek DNA samples for familial comparison, but this is invasive and can be unwelcome at a time when family and friends are grieving. Similarly, if a missing person does not have fingerprints on file, police fingerprint specialists may look for fingerprints at the dwelling if all else fails, but once more, others may leave their prints there, so the results can require careful interpretation.
Dental comparison is useful in all these cases, but it depends on our ability to trace dental records back to one or more dental practices. It also depends on the quality of the dental records including (importantly) any images that are available, including 3D scans. We also must assume that the dental records are correctly named. There have been instances in the public dental system of different individuals using the same health care card to secure free appointments. But most importantly, the dental records must still be in existence.
The ADA Policy Statement 5.17 on dental records states that records should be retained for at least seven years after the last patient visit, of if the patient was under 18 years of age, at least until they reach the age of 25 years. This is the minimum retention period for holding dental records. The Dental Board of Australia has recently retired its Guidelines on Dental Records which contained a comparable clause to the ADA Policy. As a result, the Dental Board no longer advises any specific period for retaining records and expects you to comply with your legal obligations.
persons. Many of these individuals will have been found deceased after substantial periods of time and identifying them will be complex. It will rely heavily on DNA comparison, anthropology to build a profile of the remains, and forensic odontology. For obvious reasons, fingerprints won’t be so useful because of the state of the remains. In such cases, we do not wish to run into difficulties with dental records that have been destroyed because of their age.
One of the most significant services that we as a profession can provide is to give an identity back to those who no longer have a voice.
These days, numerous practices and clinics rely on electronic storage of dental records which enables large volumes to be stored relatively cheaply. While this brings its own unique issues (security, redundancy, and ensuring that the technology remains current and that older records remain readable with newer technologies), there are now fewer reasons to delete or destroy older records. The Queensland Health Sector (Clinical Records) Retention and Disposal Schedule for public health records explicitly states that there is no requirement for public medical records to be destroyed at the expiration of a minimum retention period. This is also true of the ADA policy statement. You don’t have to destroy records at the end of the minimum retention period and in fact you can retain records for as long as you wish.
The situation most often becomes critical for us when we are faced with an older matter in which the remains of a longdeceased person have recently been admitted to the mortuary. It is not uncommon for us to determine that dental visits were made more than ten years ago and on some occasions, the relevant records have been destroyed. If we have nothing to compare the teeth of the deceased with, we cannot advance the case. It is worth reflecting that dental records are usually destroyed long before the actual teeth themselves, and evidence of dental treatment can survive and be of assistance for decades after death.
This issue is likely to come into even greater focus as there is now a national program aimed at identifying long-term missing
This article is a plea. If you’re planning on destroying records, please think about other options.
So, this article is a plea. If you’re planning on destroying records, please think about other options such as retaining any electronic record files you have, or scanning your physical documents into electronic files. Physical records certainly take up storage space, but physical x-rays less so. Please try and keep them even if you wish to destroy the written records. Also, some dentists are now investing in 3D scanners so they can retain electronic copies of study models instead of physical copies, which again saves storage space. If you have not yet moved to electronic record storage, at a minimum, we ask that you consider at least retaining physical x-ray or photographic images as they would be extremely helpful for identification of persons who are long since deceased. Images are much more useful to us than written documents.
If you have any digital records, we now have cheap multi-terabyte storage and excellent backup options. Ask yourself if there is any need to delete these electronic records at all. If you must remove them, can they be archived and the archive transferred to new technology as it emerges? Or can they simply be retained on your current storage system? Proprietary image formats may become more difficult to access in the future as standards and technologies evolve, but this will be more of a problem for us forensic odontologists than for you, although some practices are already encountering the need to update their records or images to meet the requirements of a new software system as they refurbish. So rather than delete records, we ask that you consider all the good reasons for retaining them.
One of the most significant services that we as a profession can provide is to give an identity back to those who no longer have a voice. Your dental records can help us do that! We, and the family members of those deceased, would be very grateful for any assistance you can provide.
A/PROF ALEX FORREST AO DIRECTOR OF FORENSIC ODONTOLOGYQLD HEALTH FORENSIC & SCIENTIFIC SERFICES
Whether a dentist obtained financial consent from a patient, is a common complaint faced by dentists.
A dentist recently contacted ADAQ upon receiving an OHO notification. In this matter, the patient claimed the dentist quoted an incorrect amount for their treatment and alleged the dentist was now seeking a substantially higher amount after commencing the treatment.
In this particular case, the patient was given two separate treatment plans and a quote for each plan. The treatment options were:
Option 1: Simple adhesive restorations - $1,330
Option 2: indirect full crowns/bridge - $11,840
At the time of the initial consultation, the dentist explained the options in detail to the patient and also the risks of each treatment. The dentist also printed out the two treatment plans and quotes for the patient to take home and consider. The dentist also recorded their advice to the patient and actions in their clinical notes.
The patient took both treatment plans and quotes home to consider and subsequently advised they wished to proceed with option 2.
The patient then attended for their first appointment where considerable work was undertaken. Upon completion of this appointment, the dentist requested payment in line with option 2. It was at this point the patient raised a concern regarding costs and said they had expected to pay the lower amount.
The dentist again explained the treatment options and the quotes. The patient unfortunately did not accept this explanation and claimed they were quoted the lesser amount for option 2. In order to resolve the matter, the dentist offered to discount option 2 and also offered a payment plan. This was rejected by the patient.
Since the complaint was not related to clinical care, the OHO moved the complaint to its local resolution team. This team conducts a service akin to a free mediation service where the OHO staff facilitate communication between a practitioner and the patient with the aim of the parties reaching common ground in order to resolve the complaint.
In this instant, the dentist was invited to prepare a written response to the complaint. The dentist approached ADAQ to assist in preparing this response. ADAQ reviewed the information provided by the OHO and advised the dentist to outline the events that occurred in chronological order including providing details of their discussions with the patient. ADAQ reviewed the response and suggested a number of amendments, to assist to highlight
the steps taken by the dentist to show they gained informed financial consent and that the patient simply made a mistake.
ADAQ submitted the response to the OHO and was appointed as the dentist’s contact person so the dentist was not interrupted during the day regarding the matter. The dentist could then deal with any issues that arose at a convenient time.
ADAQ can assist with resolution of complaints, and in doing so, avoid a breakdown of professional relationships
The OHO resolution officer was able to use the written response to draw the patient’s attention to their mistake. Once the patient was made aware of their mistake, the resolution officer contacted ADAQ and asked if the dentist could provide a further discount for the option 2 treatment and complete the treatment. After negotiation on the treatment price which ADAQ facilitated for the dentist, the parties reached an amicable agreement and the treatment continued.
Both the dentist and patient were happy with the outcome.
This case highlighted the importance of obtaining not only informed consent to proposed treatments but also informed FINANCIAL consent. It also highlights that ADAQ can assist with resolution of complaints, and in doing so, avoid the situation where the professional relationship can break down.
Assistance with complaint management is just a small portion of the services available to a Member from ADAQ. We can help you through the OHO notification process, review documents and give suggestions on how to respond to regulators. We can also be your point of contact with regulators, so you can focus on your ongoing treatment of patients and deal with the complaint at a time convenient to you.
NEESHA PIERCE LLB LLM BA MANAGER - COMPLIANCE, ADVICE & POLICY ADAQ
Receiving a complaint is like being under the spotlight.
Everything is put into question. Your clinical performance. Your qualifications. Your communication. Your insurance claims history.
There is a team at ADAQ with one focus: to help Members navigate the complaints minefield.
They take every step to help you resolve complaints quickly. And if it escalates to a formal complaint to Ahpra, OHO, or your insurer, the team can guide you through this process as well.
This combined advice and insurance service means you’ll spend less time under the spotlight, and more time concentrating on your practise.
The most common ways incidents can occur – and how to prevent them from happening.

A busy dental practice can face many types of hazards, whether that be chemical, biological, physical, or ergonomic. Unfortunately, these have resulted in injuries and other workplace incidents.
As a profession, the following areas should be closely monitored: manufacturer guidelines for storage, handling of chemicals and medicaments, regular maintenance of equipment and environment, periodic review of procedures and policies.
In the clinical environment, the most common incident is sharps injury, with body fluid exposure following suit. The safe disposal of sharps is the responsibility of the clinician at point of use. Improper disposal of sharps is a breach of workplace safety and health legislation. Not only that – it may also result in staff distress. A staff member on the receiving end of an exposure may feel anxious and in distress, especially when waiting for blood test results when the source or patient is unknown. Ensure all team members, including clinicians, have appropriate training in work procedures in order to prevent this from happening.
Referral to counselling services for staff who experience anxiety as result of an occupational exposure, whether actual or perceived, can be beneficial and should be encouraged.
ADAQ receive many calls from dental practices enquiring about process for reporting of incidents and accidents. This include documentation that needs to be completed, administering first aid to staff and follow up risk management. Under Queensland
legislation, you are required to report a ‘notifiable’ workplace incident immediately after becoming aware that it has occurred. Failure to report may result in penalties.
A notifiable incident can include:
• the death of a person
• a serious injury or illness of a person or
• a dangerous incident
Further information on a notifiable incident can be found on the Safe Work Australia website. Safe Work Australia is not a regulator and cannot advise you about reporting a workplace incident. All employers must report injuries sustained by workers for which worker’s compensation may be payable by their workers compensation insurer.
If you need help in Queensland, contact Worksafe Queensland by phoning 1300 362 128 or by using the online incident notification form.
For non-notifiable incidents that do not need to be reported, it is recommended that you document, record and follow up to prevent another incident of the same nature occurring in the workplace in the future.
• Time/Date of Incident
• Location of Incident
• Name of Person Injured
• How did the Incident Occur
• What Happened
• Type of Exposure
• Was there Blood Visible on the Device
• Name of the Source Involved if Known and their Medical History if Known
• Action Taken
• Follow up Required and Additional Information
Safe Work Australia has incident report templates, fact sheets, and other documents outlining the information that must be included in your reporting. Visit safeworkaustralia.gov.au
• Stop work, clean the wound/site with soap and water, dry and cover with a waterproof dressing
• For a splash to the mouth or eyes flush with generous amounts of water or normal saline for 5 minutes, remove contact lenses prior to flushing
• For a body fluid exposure, remove clothing if necessary and wash affected area with soap and water
• Seek first aid if required, depending on the nature of the injury and/or exposure
• Send staff member for baseline tests to establish their serological status at time of exposure
• These blood tests will be essential if workcover insurance is claimed at a later date
• Testing of the source patient is recommended if known and patient is compliant with such
• Positive tests for HIV antibodies, HCV antibodies and Hep B antibodies will require follow up tests
• Follow up tests will need to be scheduled at 1-, 3- and 6-months intervals or determined by your practitioner
• Notify supervisor or mandatory reporting requirements within own organisation
• Complete incident report with all required reporting information
• Follow up the required action and additional information
• Follow up risk register and risk assessment
Step 1: Identify Hazards
Identify any hazards in the practice– any hazard that is existing and any potential hazard. Create a list of existing or potential hazards and the current control measures the practice may have in place.
Step 2: Assess the risk
The degree of risk needs to be determined once the hazards have been identified and how they can potentially cause harm or injury within the working environment.
Step 3: Control the risk
The practice should then look at processes to eliminate or reduce the risk as much as possible after assessing the risks. This can be done by using the hierarchy of control measures.
Step 4: Review
Control measures need to be reviewed once they have been implemented to determine if the measure is fit for its intended purpose.
Review is an ongoing process and when new processes are introduced into the practice we need to consider if the control measure is the most effective method.
A risk register document should be accessible and maintainable tool for regulatory compliance in the workplace. This document will be an important record of identified risks and form part of your risk management plan. It should contain the information you collate from the actions and follow up from hazards identified. This will include your descriptions of hazards and, once logged on the register, you can identify: the harm that the hazard could cause, the likelihood that the harm could occur and the level of risk.
All risk registers need to have person responsible for action, due dates, completed dates, and review follow up dates.
Your overall risk management plan should be referred to in your workplace health and safety manual in your dental practice. Risk register templates and fact sheets can be downloaded from the Safe Work Australia website.
EDUCATION AND PRACTICE ADVISOR ADAQ
1. www.safeworkaustralia.gov.au/
2. www.worksafe.qld.gov.au/
3. www.worksafe.qld.gov.au/__data/assets/pdf_ file/0019/72631/first-aid-in-the-workplace-cop-2021. pdf
4. www.worksafe.qld.gov.au/__data/assets/pdf_ file/0022/72634/how-to-manage-work-health-andsafety-risks-cop-2021.pdf
5. www.health.qld.gov.au/clinicalpractice/guidelines-procedures/diseases-infection/ infection-prevention/standard-precautions/sharpssafety/sharp-safety-program
6. www.worksafe.qld.gov.au/safety-and-prevention/ hazards/hazardous-exposures/biological-hazards/ skin-penetrating-injuries
ANTERIOR & POSTERIOR COMPOSITE RESTORATION



EFFECTIVE RECORD KEEPING


ADAQ TRAINING RADIOLOGY PRAC





INTERMEDIATE ORAL SURGERY







MANAGING THE WORN DENTITION



Advances in microbiology and pathology had ushered a revolution in surgical practices that eventually trickled down to dentistry, helping to make this field a recognised health profession by imitating the sterile look of surgical suites.
By the early 1900s, an understanding of germ theory became essential to professional practice in dentistry. The ‘sterile look’ replaced the stuffiness of previous surgical offices and became associated with modernity and progress (Glenner). The only acceptable materials were readily cleaned and shiny looking. Metal cabinets replaced wooden counterparts. Linoleum replaced rugs under the chair, the latter also losing its prickly plush or velvet.
Nickel-plated units were initially common in the 1910s but were gradually superseded by metal furniture with a paint finish, first black then ivory white, which remained the standard for decades. Beautifully carved ivory or ebony handles on instruments lost favour as easily scrubbed steel presented on sanitary glass trays became the standard.
For dentists, adopting aseptic practices meant visually distinguishing themselves from their not-so remote charlatan past — a ‘visual emancipation’, a show that their skills and knowledge were on par with those of a medical doctor. The sterile surgery was perceived more as a business strategy than a clinical necessity.
During the 1920s, a special sterilising room was often built [by those who could afford it] to be in full view of the arriving patients. This ostensibly confirmed the dentist’s prestige and ability to care for their patients. Ritter Dental Manufacturing Company When Is a Dentist A Success? (1920) highlighted the psychological role of the sterilising room, rather than its functional one. Ritter’s emphasis is obvious: in the 29-page booklet, four detailed illustrations of this area take a sizeable chunk of the limited space available (Image 6-8).
By 1939, the ostentatiousness and duplicity of the ‘sterilising room’ fashion was clearly mocked, as Bremner’s Story of Dentistry attests: “in fact, this elaborate outfit, with its shining boilers and shimmering glass jars was seldom used; for the small sterilizer in the laboratory was more convenient. The sole purpose of the sterilizing room was to impress patients”.
Cost and time were perceived barriers to application of sound infection control routines (Fulford & Stankiewicz). Boiling dental instruments remained the main way of disinfection in dentistry (Miller 1891) for decades, with more expensive equipment such as autoclaves shunned, until prices dropped (Nield). Water boilers were operated in Australian dental practices up until the 1980s.

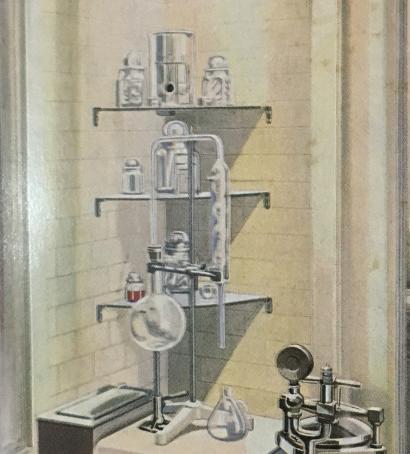
Image 6-8.
Ritter manufacturing Co. When is a dentist a success? 1920. ADAQ Archives.
The British Dental Trade Association’s 1979 Introduction to Dentistry describes three steriliser types in use at the time: autoclaves, hot-air sterilisers, and water boilers. An Australian 1969 Dental Assistant’s manual also mentions Gamma radiation sterilisation and ultra-violet lights, chemical vapours as well as ultrasonic vibration. The use of the new sterile paper packages (patented in the 1950s) and of disposable pre-sterilised instruments are recommended to increase efficiency and reduce breaks to the ‘sterile chain’.
Needles and small items were sterilised for reuse in a little barrel device. Disassembly of high-speed handpieces was tedious, bins overflowed with disposables plastics, and chairs corroded fast with harsh cleaning.
However, basic protection measures such as wearing gloves continued to be disputed or ignored (Schlich) well into the second half of the 20th century. In the dental surgery, chair assistants were often the only ones to wear rubber gloves and some recall being instructed to just wash them at the sink and reuse. Some dentists stood by a popular expression at the time that ‘you only wear gloves to eat lunch!”.



Unfortunately, pandemics aside, the next generation of health professionals will be unlucky enough to deal with another problem: spiralling antibiotic-resistant infections (Schlich).
Whatever the challenges ahead, we can be thankful to have come after those IC pioneers who did a lot of the guess work, and provided tools and knowledge to fight infection. What’s left for modern dentists is to use them correctly.
For further reading on IC history, see Helen Nield’s article online:
Nield, H. A short history of infection control in dentistry. BDJ Team 7, 12–15 (2020). https://doi.org/10.1038/s41407-020-0402-1
REFERENCES AND FURTHER READING
1. Australian Dental Association Queensland Branch. The Australian Dental Mirror. A Reflection of Professional Activities. Issue XV. May 1947
2. Bremner,K. (1939). The Story of Dentistry from the Dawn of Civilisation to the Present. Dental Items of Interest Publishing Co
As late as 1990, in his humorous book Nothing but the Tooth, WA dentist Neil Burman, jokes on his decision to finally: “… bite the latex bullet and make gloves part of my professional life”, and complains that: “[…] this powder covers mouth mirrors with a haze reminiscent of an Alaskan snowstorm, making identification of hard oral tissues somewhat haphazard. The glove material is composite friendly […] in other words composite fillings would prefer to stick to the glove than any tooth surface”.
The current pandemic is an unwelcome but essential reminder of the importance of IC and PPE, and of ease and consequence of cross-infection. For our younger dentists, this would be the first major outbreak affecting their practice closely, since the 1980s HIV and hepatitis epidemics, or the Creutzfeldt-Jakob disease (‘mad cow’) disease scare of the 1990s.
Older Members will remember the 1985 joint statement issued swiftly by ADAQ, the School of Dentistry and the Dental Board on HIV spread, which recommended what are now standard precautions (glasses, gloves, masks) be made mandatory for all dental practitioners in Queensland, a position soon adopted federally. Or they may remember being vaccinated for hepatitis: a member of our committee recalls being the first person in Bundaberg to be immunised against Hepatitis B. His GP’s advice was: “Sure about this? You may get AIDS”!
3. British Dental Trade Association (1979). Introduction to Dentistry
4. Burman, Neil (1990). Nothing but the Tooth. Northbridge, W.A: Merry Molar Publishing. Pp 62-63
5. Certification Committee of the Dental Assistants ‘Association of Australia. Dental Assistants’ Manual 1969
6. Fossume, FLA Plea for More Thorough Dental Asepsis. The Dental Cosmos: a monthly record of dental science [Volume 47, Issue 6, June, 1905, pp. 672-674]
7. Freiberg J. A. (2017). The mythos of laudable pus along with an explanation for its origin. Journal of community hospital internal medicine perspectives, 7(3), 196–198. https://doi.org/10.1080/20009666.2017.1343077
8. Fulford M.R., Stankiewicz N.R. (2020) A History of Infection Control. In: Infection Control in Primary Dental Care. BDJ Clinician’s Guides. Springer, Cham. https://doi. org/10.1007/978-3-030-16307-5_
9. Glenner, RA (1984). The Dental Office: A pictorial History. Montana: Pictorial Histories Publishing Company
10. Nield, H. A short history of infection control in dentistry. BDJ Team 7, 12–15 (2020). https://doi.org/10.1038/s41407-020-0402-1
11. Nutton, V. (1990). The Reception of Fracastoro’s Theory of Contagion: The Seed That Fell among Thorns? Osiris, 6, 196-234. Retrieved January 31, 2021, from http://www.jstor.org/stable/301787
12. Pesapane F, Marcelli S, Nazzaro G. Hieronymii Fracastorii: the Italian scientist who described the “French disease”. An Bras Dermatol. 2015;90(5):684-6.
13. Patrick, Ross (1987). A history of health & medicine in Queensland, 1824-1960. St. Lucia, University of Queensland Press
14. Redaelli, P., Visocchi, V. Agostino Bassi precursor of comparative mycopathology. Mycopathologia 2, 37–42 (1940). https://doi.org/10.1007/BF00450241
15. Ring, Malvin E (1992). Dentistry. An Illustrated History. New York: Abradale Press Inc.
16. Ritter Dental Manufacturing Co (1920). When Is A Dentist A Success?. New York: Ritter Dental Manufacturing Co. Inc. Publishers.
17. Ruggi (1924) Ricordi della mia vita.
18. Schlich T. (2015). Why were surgical gloves not used earlier?. Lancet (London, England), 386(10000), 1234–1235. https://doi.org/10.1016/S0140-6736(15)00271-8
19. S.S.White Dental MFG CO. SSWhite General Catalog of Dental Supplies1932
20. Strasser B. &Schlich T. (2020). A history of the medical mask and the rise of throwaway culture. Lancet (London, England), 396(10243), 19-20. https://www. thelancet.com/journals/lancet/article/PIIS0140-6736(20)31207-1/fulltext
21. Traité de la peste: recueilli des meilleurs auteurs anciens et modernes, et enrichi de remarques et observations théoriques et pratiques (1721).Switzerland: chez Philippe Planche.
22. The three pictures and the associated text have been adapted from The Dental History Calendars (1997, 1998, 1999) by Wolfgang O. Funk held in ADAQ collection
“The practice has got so busy since we started using HealthEngine, we’ve hired a new dentist and two more staff members. This is our new dentist’s third day with us, and she’s already fully booked!”
When Practice Manager Karen Stringfellow made the move to Smile Bright Dental in Sunnybank Hills in early 2018, it was already a busy and wellestablished practice (over 22 years), with a steady trickle of word-of-mouth referrals. But Karen and the practice owner, Dr Dennis Chang, were keen to get more new patients and grow the practice.
They’d tried Facebook with little success. They’d got a good organic dental SEO strategy, but they were missing out on online bookings from all that web traffic. Smile Bright Dental changed that overnight with HealthEngine.
“Our practice wasn’t offering online bookings when I arrived. And after doing a little more research on HealthEngine, I soon discovered that no other local practice was either. Here was a hole in the market, and I wanted to fill it with us!” said Karen.
It’s predominantly an Asian community surrounding the practice, and Karen identified an opportunity to tap into the local online market of young mums and young professionals.
“They’re the kind of people who want to be able to book appointments online, after hours, at their convenience. And there are quite a few who are also booking on behalf of their aging parents, who struggle with the language barrier and don’t want to call the practice.”
Signing up for a paid featured listing instantly put Smile Bright Dental at the top of the HealthEngine search results for dental practices in Sunnybank Hills, giving them an advantage as the only featured local practice.
“New patients immediately started coming in via HealthEngine. And these aren’t people who book once and disappear,” says Karen. “They might initially just be looking for the first available appointment that’s closest to them, at the time they need it. But we always make sure they get the best patient experience while they’re here, so they come back.”
HealthEngine has played an integral part in helping the practice enhance the patient experience too. By calming the phones down on the front desk, it’s freed up time for the staff to give patients the best experience when they walk through the door. Karen and her team have also been very strategic with their dental marketing strategy. They’re regularly sharing the link to book via HealthEngine with their existing patients, making sure everyone knows they have the added convenience of booking online at any time.
“HealthEngine has taken our dental marketing to a whole new level. We’re seeing an average of 55 patient bookings a month and an ROI of 144%. And just to give you a comparison, our SEO is delivering an average of about 30 patient bookings a month and an ROI of about 98%. Seriously, nothing has been as good as HealthEngine.
But success isn’t just about the numbers for the Smile Bright Dental team. It’s about the positive words in their online reviews too.
“It’s extremely competitive out there. Patients are very savvy these days and online reviews really matter,” said Karen.
“Since we’ve been concentrating on our patient care, our online reviews have
gone through the roof! And some of the patient reviews we get on HealthEngine are so lovely, heartfelt and beautiful, we’ve started putting them in the dental files so our dentists get to see them. It’s good for them to know what people like and really value about them and their service.”
The practice has got so busy now, they’ve hired a new dentist and two more staff members.
“This is our new dentist’s third day with us and she’s already fully booked,” said Karen.
Now the team is looking for ways to create some space in their books, so they can keep bookings available on HealthEngine.
“It’s amazing how rapidly dental marketing has changed. I first started using HealthEngine about four or five years ago, when I was managing other practices,” said Karen. “Back then, most patients were still choosing to ring the practice to book an appointment. But there’s been a big shift to online in the last couple of years, and I’ve seen HealthEngine gain a huge amount of traction.
“As more and more patients are now expecting to be able to book their appointments online, you’ve got to be there in that space, or you’ll get left behind.”
HealthEngine offers a powerful dental marketing platform that instantly connects you to Australia’s largest patient network.
FILL YOUR BOOKS. PRACTICES.
HEALTHENGINE.COM.AU







Come and discover the real i DENT ity of the profession in Queensland – ADAQ’s own dental cabinet of curiosities!
We’re living in the past here at the ADAQ Museum of Dentistry (MoD). Step into an early 1900s dental surgery, with genuine equipment and furniture from those years. View ornate footpedal drills, early x-ray equipment, a beautiful swan-armed dental chair from the 1870s and many examples of beautiful – and barbaric – extraction keys.
Learn more about the history of denture making and casting of crowns, including the ‘Five dentures’ showcasing the evolution of techniques from the 1600s: the display that spurred the modern Committee’s effort to initiate work to make the collection available to the public and build a permanent museum exhibition.
A Museum of Dentistry for Queensland has been in the works since the foundation of the Odontological Society of Queensland, which had in its objects the ‘formation of a Library and Museum’ in their Constitution; a reference to the preservation of the history of dentistry remains one of ADAQ’s objectives. The 1985 Australian Congress held in Brisbane showcased a wonderful historical display, in collaboration with the University of Queensland. Many of the items in our collection were originally in that display.
As the collection grew to thousands of instruments and archival documents in 2018, the Council appointed a Dental History Preservation Committee to organise a permanent display. Over the last couple of years, the Committee and ADAQ staff have been working to organise, restore, research and catalogue. This work is ongoing, but now we’re preparing to show it all off.

The Committee continues to research and sieve through archives to prepare future exhibitions. However, we would like to collect some feedback to make sure we’re steering in the right direction. Therefore, we would like to invite you to an exhibition preview before we open to the public.
Saturday mornings from June until July 2021. By appointment only and numbers are limited. Please contact Alessandra Boi for information at adaq@adaq. com.au or call 07 3252 9866.
All members, their families, dental students and practice teams are welcome to come and have a peek; but…there’s a catch. When you arrive, we will ask you to choose an object or two that you especially like, or hate, and write a few lines on: what it means to you, what you know about it, why it resonates or piqued your interest. Your thoughts may form part of the public exhibition’s text.
A special thank you to all members who have donated so that we can continue to build our fantastic collection, and everyone who has been involved so far!
Alexandra Coombs, Harry Akers, Robert McCray, Michael Foley, Richard Olive, Gary Smith; with Alessandra Boi (ADAQ Staff).

Superannuation planning should not be left until the last day in June and there are consequences for getting it wrong.
June is here, and it’s time to consider what you can do to reduce your taxable income / tax liability. One of these deductions which often gets left until the last moment is maximising (personal) superannuation contributions. With almost 1.5 million people requesting COVID-19 early release of super during the 2020 calendar year, it is now time to consider replenishing or topping up your super balance if you can afford to do so. The maximum amount of concessional (tax-deductible) super contributions allowed each year is $25,000 inclusive of any 9.5% super guarantee/employer contributions. A further $100,000 in non-concessional (non tax-deductible) super can also be contributed in any one year. Anyone under 65 years of age can also bring forward the next two years of non-concessional contributions making a total of $300,000.
If you are an employee receiving 9.5% from your employer or a contracting dentist that has already made some personal super contributions during the year, you are able to top up your super to a maximum of $25,000 before 30th June 2021. It is more important than ever this year to check with your superannuation fund to determine exactly how much has been deposited due to the Superannuation Amnesty in 2020 which saw many employers correcting past errors. Additionally your June 2020 contribution was most likely deposited in July 2020 –so even though the contribution relates to an earlier year, it will be counted in the year it is actually received by the super fund. Personal super contributions must also be received by the super fund on or before 30 June 2021 in order to be tax deductible. With 30 June 2021 falling on a Wednesday this year - my advice is to make your contribution no later than Friday, 25 June 2021 to ensure it is receipted by the super fund in the current year. Before you can claim a tax deduction for your personal super contributions,
you must provide your super fund with a notice of intent to claim a tax deduction and also receive acknowledgement from them confirming your ability to claim before you lodge your tax return.
From 1 July 2018 it is possible to catch up on prior year’s shortfall in super contributions. If your contributions in 2018/19 or 2019/20 were below $25,000 then you are able to catch up on the shortfall in 2021. To be eligible you must have a current super balance of less than $500,000 and you must make the full $25,000 contribution in 2021 before you are able to catch up on some or all of your shortfall. If you have not made any contributions in the past few years then you can potentially contribute up to $75,000 prior to 30 June 2021. The catch up provisions are for a maximum of five years and it is always the oldest shortfall which is caught up first.
High income earners with taxable income over $250,000 will become liable for Div. 293 tax on your concessional super contributions. It is only the super contributions which are in excess of $250,000 that are subject to the additional 15% contributions tax. The maximum tax is therefore $25,000 X 15% = $3750. This amount can be paid by the dentist from their personal funds or from their accumulated balance in their super fund. Most dentists opt for paying the tax themselves to ensure that they maintain the highest balance possible in their super fund. There are also additional charges on any contributions which either exceed your concessional contribution cap ($25,000) or your non concessional contribution cap ($100,000). These additional charges (taxes) are either at your marginal tax rate or 47%. It is therefore not advisable to exceed your contribution under any circumstances.
Employee contributions are required to be paid every three months and within 28 days of the end of the quarter. This usually means that the employee super contributions for the months of April, May and June 2021 will be paid in July 2021. If they are paid in July 2021 then they are not tax deductible until the 2021/22 financial year. As an employer, consider paying super the same day your last June pay cycle ends, to get the tax deduction in the current year. Otherwise, consider paying the April and May contributions in June 2021.
The benefit of making tax-deductible super contributions is not just the immediate reduction in tax payable but also the much more important and long lasting benefit of providing a sound financial foundation for your retirement.

Albert Gigl is the founder of MW Partners, Specialist Dental Accountants. He has spent the last 15 years specialising in providing taxation advice for dentists. Contact Albert on 07 5554 6400 or albert@ mwpartners.com.au for an obligation-free, confidential consultation on pre-June 30 tax planning strategies.

The end of financial year is a common time for many individuals and businesses to review their general insurances. This year, arguably more so than at any time before, it is important to comprehensively review your insurance whether you self-manage the process or work with an adviser.
So why is it particularly important this year, and what should you do to ensure you achieve the best outcome? This article explores three factors linked to the hardening insurance market to help Members understand the current market environment
There has been a perfect storm of events which have challenged insurer’s profitability, and these have resulted in a hardening insurance market. In the past 18 months most businesses have been impacted by not only COVID-19 but several natural catastrophes, bushfires, floods etc.
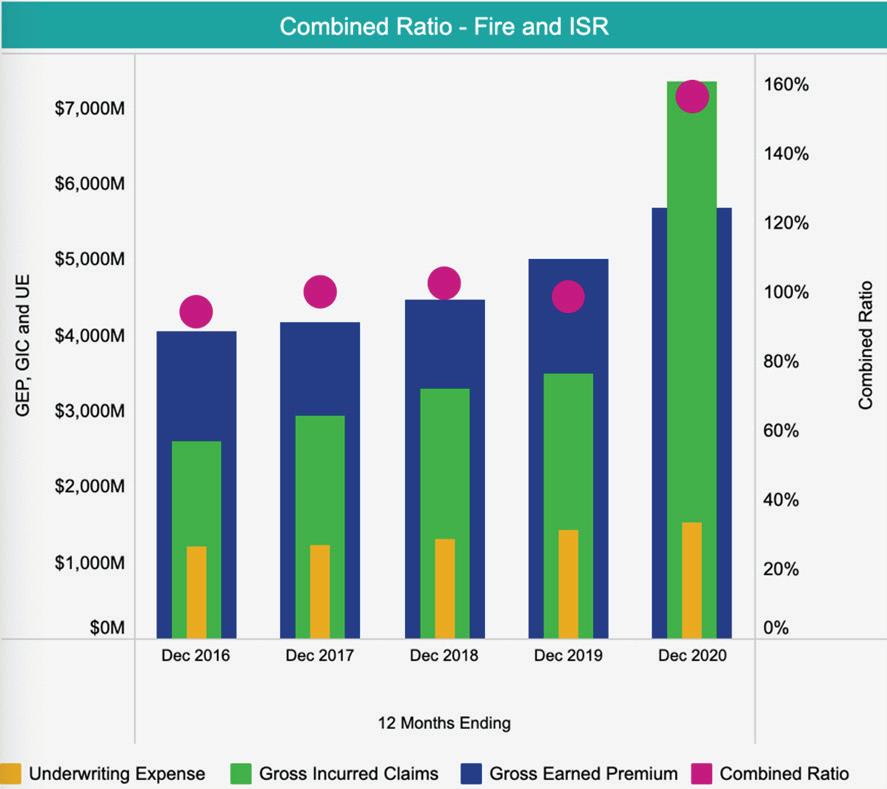
Source: KPMG GI Insights Dashboard 2021
Property insurance, as the name suggests, relates to physical buildings and contents as well as to business interruption or loss of business profit due to insured damage.
The 2019 Australian Bushfires resulted in $2.2 Billion of claims costs incurred in the first half of the 2020 financial year. This represented Australia’s third largest bushfire event since 1967. Immediately following was an East Coast low which hit QLD and NSW and resulted in further insured loss of $989 Million.
As a result of the fifth year (in 2020) where the industry combined ratio for Australian
Property Insurers was at or above 100%, resulting in pay outs of approximately $1.6M (figure 1)in claims costs and administration expenses for every dollar in premium received.
This sector includes Professional Indemnity, Medical Malpractice and Directors’ & Officers’ Liability insurance. Long running factors such as the growth in class actions, building industry certification issues, legal costs from enquiries such as the Royal Commission into aged care and banking, and the uncertainty of the financial impacts to the economy of COVID-19 are impacting this sector.
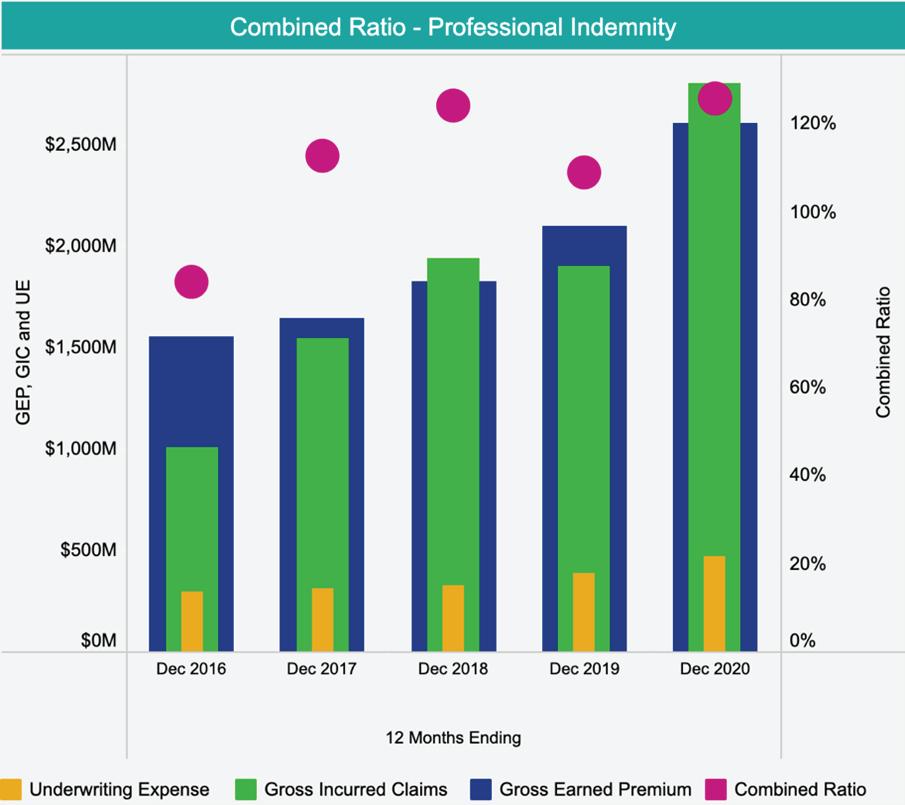
Source: KPMG GI Insights Dashboard 2021
For Australian Financial Lines insurers the combined ratio has been above 100% for four of the last five years as shown in figure 2. The recent Marsh Global Insurance Market Index for Q1 2021 reports that pricing in the Pacific region grew 48% in the quarter, and that this represented the 15th consecutive quarter of double digit premium increases.
Before we tie this all together, it is worth noting that what happens overseas also has an impact on the domestic market. Many insurers have reduced how many clients they insure and the sums insured
they provide. This reduction in capacity (supply) is resulting in a magnification of premium increases.
Lloyds of London is regarded as the world’s leading insurance market. Within its 2018 Lloyd’s Performance Management Directive, a review labelled ‘Decile 10’ showed that 62% of Lloyd’s syndicates (underwriters) that wrote nonUSA Financial Lines insurance made an aggregate loss over the previous six years, making it the second least profitable class at Lloyd’s in that time. Syndicates within the Lloyds market were therefore mandated to provide written business plans on how they intend to remediate and return each class to profit. Several syndicates decided to completely exit the Financial Lines market in late 2019 and early 2020. In addition, many reduced capacity with some estimates saying that overall, Financial Lines capacity halved in that time.
All these factors have led to the current marketplace of increasing premiums, reduced policy limits, higher excesses and reduced policy coverage. The same pressures exist beyond the two product sectors discussed, and this is the essence of a hardening insurance market.
To position yourself for the best outcome, we recommend ensuring you check the information your insurer or adviser has is accurate and up to date. Engage as early as you can as insurers are asking more questions than ever before. Any uncertainty the insurer has will increase the price at best, or at worst it may mean that you struggle to get insurance.
If the Mediprotect team can be of any assistance, we welcome the opportunity to work with you.
DAVID HANSEN NATIONAL MANAGER - MEDIPROTECT INSURANCE SOLUTIONS
Workplace policies are the best way for practices to control appearances in the workplace. A well-rounded uniform policy, which stipulates what is and what is not acceptable in relation to piercings and tattoos and in relation to personal hygiene, is useful to set the standard.
Generally, the requirements in the policy must be reasonable, for example, a policy may prohibit an employee from showing tattoos with offensive symbols, or large, obvious facial piercings, but it would likely be unreasonable to prohibit an employee from having any piercings or tattoos at all. If an employee then breached the policy, the practice could address it as a disciplinary matter.
deposited onto the facial skin. Hence, facial piercings which cannot be covered by either supplied PPE or an approved waterproof covering are not acceptable. The current mandate from NHMRC infection control guidelines and Hand Hygiene Australia for “bare below the elbow” addresses the wearing of jewellery on the fingers, hands and wrists, and the use of false fingernails from the standpoint of infection control as a uniformly applied international best practice. This is another example of where the practical elements of wearing such items can directly impact on occupational health.
Whilst practices may introduce workplace policies which govern an employee’s appearance in the workplace, it is important to ensure that the policy is not discriminatory.
Under the Fair Work Act 2009 (Cth) (‘Act’) the following attributes are protected, meaning an employee cannot be treated differently, or have adverse action taken against them for having a protected attribute. These include:
• Race
• Colour
• Sex
It is important to ensure that employee appearance policies are not discriminatory.
Using the available evidence to support a position is important when framing local policies. For example, there is a significant literature regarding the health risks of piercings including metal allergies, local infections and scarring. Facial piercings make the facial skin harder to clean, increases the risk of acquiring unwanted infection for the staff member concerned, and this poses a challenge as many dental procedures (including using a triplex syringe) generate large amounts of splashing and some of that will be
Likewise, there is an extensive literature around adverse oral health impacts from lip and tongue piercings (e.g. tongue and lip piercings are associated with the risk of gingival recession, and tongue piercings are associated with tooth fractures), so a staff member wearing those in a clinical setting runs counter to contemporary best practice in oral health, and may give confusing messages to patients who are being told why they should not wear these.
Practices can also regulate employee appearances from a Workplace Health and Safety perspective. In particular, large piercings and jewellery may cause a risk to health and safety as masks or other equipment may get stuck on the piercing and cause an injury. Employers may therefore consider requiring that employees do not wear large jewellery in piercings, or remove all facial piercings before attending work.
• Sexual Orientation
• Age
• Physical or mental disability
• Marital status
• Family or caring responsibilities
• Pregnancy
• Religion
• Political Opinion
• National extraction; and
• Social origin.
Practices should be mindful that in some cases, piercings and tattoos may be cultural or religious and therefore may be protected under the Act.
Practices should remember that prospective employees are also protected from discrimination under the Act. As such, the Practice should communicate its expectations regarding personal appearance early in the recruitment process and ensure that employment related decisions are not made based on a protected attribute.
Two unmissable, inperson events coming later this year.
We are excited to announce that ADAQ is bringing back in-person conferences!
17-18 Sept 2021
A two-day regional symposium in beautiful, sunny Cairns.
DETAILS COMING SOON

26 Nov 2021
Digital Dentistry Clinic Day
ADAQ’s flagship in-person eventthe networking opportunity of the year.
DETAILS COMING SOON
 BRISBANE
CAIRNS
BRISBANE
CAIRNS
Supplier promotions and Government initiatives can make investing in new equipment an attractive option.
Running a dental practice can be challenging– especially if you’re concerned that your equipment may not be up to scratch.
While the decision to upgrade your dental equipment is a big one, if it improves the level of patient care, productivity and profitability, it may be worth considering the investment. Being savvy about when you buy is key, says Senior Finance Specialist Luke Truscott from BOQ Specialist. “Upgrading equipment can be an investment, but you can make savings if you do it at the right time, or take advantage of Government incentives,” he explains.
Here are some strategies which might make buying or upgrading your equipment easier.
A big drawcard for dentists—especially those considering capital investment—is the annual ADX trade show held by the Australian Dental Industry Association. This event has the latest innovations, technologies and techniques for dentists. “It’s packed with suppliers and exhibitors showcasing the new equipment or new technology they may be bringing out,” says Luke, “and there are usually a lot of ‘limited time only’ or ‘show only’ promotions and specials that dentists can take advantage of.”
Taking advantage of the Government’s instant asset write-off scheme could also help you with capital expenditures—and may result in a lower tax bill to boot.
“When the scheme started, if you were an eligible business owner with less than $10 million in turnover, you could purchase a piece of equipment costing under $150,000 and immediately write that asset off, instead of depreciating the asset over a period of years,” says Luke.
“If you purchased a piece of dental equipment for $100,000, for example, the instant asset write-off scheme would allow you to take a tax deduction for the full cost of the asset in that year, rather than over a number of years,” he explains. “This effectively lowers your taxable income earlier and means you’re not going to pay as much tax in that year.”
However, an extended version of the scheme (known as the temporary full expensing incentive) has meant that since 6 October 2020, the instant asset write-off threshold of $150,000 doesn’t apply so there’s no cap on asset purchases. This incentive is also available until 30 June 2023. “To tap into this initiative, you just need to have an aggregate turnover of under $5 billion, which covers almost all dentists” adds Luke.
Another scheme that dentists may wish to look into when financing equipment or upgrades is Phase Two of the Government’s SME Guarantee Scheme, which aims to provide small and medium enterprises (SMEs) with access to a range of funding to help them adapt to their new operating environment, or invest in their business for the future.
“Under the Scheme, a client can use the loan for a broad range of business purposes, including purchasing a bigticket item — a piece of capital equipment such as a CBCT system or CAD/CAM technology, or something that perhaps they couldn’t purchase before. The Government guarantees 50% of the loan, so the benefit to the dentist is that they receive a lower interest rate on the loan. This Scheme ends on 30 June 2021 and eligibility criteria is applicable.”
Dentists considering equipment upgrades may wonder which method is best for purchasing equipment—buying it outright, or financing it with a chattel mortgage facility?
“A lot of dentists use a chattel mortgage facility to finance their equipment purchases, so they can leverage off Government initiatives such as the temporary tax incentive. Also, under a chattel mortgage, they’re the actual owner of the equipment. Because of that, they can instantly write off the asset and claim GST benefits.”
You can still take advantage of the instant asset write-off option if you buy outright, he adds. “However, you’re not leveraging the low interest rate environment available at the moment, and financing those bigticket items also enables you to use your cash for other expenses or investments”.
There have been so many advancements in technology and dental innovations in recent years, and patients are looking for dental clinics that offer quality, cuttingedge treatments that save them time, says Luke.
“Plus, having up-to-date infection controls, especially post-COVID, shows you’re committed to having a safe environment for patients,” he adds, “Investing in updated equipment could mean you’re potentially one of the first in your area to offer that technology to your patients.”
Before upgrading any of your dental equipment, you may wish talk to your accountant and a financial advisor for advice on your particular circumstances. CONTACT
We all know that the generosity effect is good for our wellbeing. Being kind and showing support for others is as good for the giver as it is for the receiver. This also plays out in the workplace when we are generous with our time and support to others.

individuals we take responsibility for working through issues the best we are able to) notice if you are unintentionally projecting a message of judgement or criticism that may be contributing to others not seeking input.
We all know that the generosity effect is good for our wellbeing. Being kind and showing support for others is as good for the giver as it is for the receiver. This also plays out in the workplace when we are generous with our time and support to others.
Importantly, generosity in the workplace is pivotal and core to building psychological safety. Supporting employees to seek input when they find themselves stuck relies upon a workplace culture that is open to accept difference and vulnerability. We often think of generosity in terms of donations and physical support, however being generous in how we make time to support and assist others in problem solving is pivotal to the wellbeing of each of us and to our workplaces. Creating an environment where you and your team can confidently seek advice, ideas and problem solve solutions is core to being a psychologically safe workplace.
Importantly, generosity in the workplace is pivotal and core to building psychological safety. Supporting employees to seek input when they find themselves stuck relies upon a workplace culture that is open to accept difference and vulnerability. We often think of generosity in terms of donations and physical support, however being generous in how we make time to support and assist others in problem solving is pivotal to the wellbeing of each of us and to our workplaces. Creating an environment where you and your team can confidently seek advice, ideas and problem solve solutions is core to being a psychologically safe workplace.
It is often in the sharing of challenges that we create a workplace environment that is more satisfying, positive, and creative. COVID19 has required us to be adaptable and solve new problems, and we have often had to call on others and get input to be more creative in our problem solving. Let’s build on what we have learnt from COVID-19 and continue to be more collaborative and creative in our workplaces. The need to be able to connect and be open with our peers with workplace challenges, continues to be as important as ever.
It is often in the sharing of challenges that we create a workplace environment that is more satisfying, positive, and creative. Covid has required us to be adaptable and solve new problems, and we have often had to call on others and get input to be more creative in our problem solving. Let’s build on what we have learnt from Covid and continue to be more collaborative and creative in our workplaces. The need to be able to connect and be open with our peers with workplace challenges, continues to be as important as ever.
When employees discuss work challenges with leaders and peers, it can provide an opportunity to strengthen trust and connection in the workplace. Stronger and more connected teams typically create more positive outcomes in a more time efficient manner.
When employees discuss work challenges with leaders and peers, it can provide an opportunity to strengthen trust and connection in the workplace. Stronger and more connected teams typically create more positive outcomes in a more time efficient manner. We have great capacity to problem solve as individuals and we are also wired to problem solve together when having trouble. Feeling more connected when collaborating in problem solving permits the “survival” part of our brains to rest while permitting the problem-solving area of the brain to be activated. This assists us to think more clearly, be able to incorporate more information when developing outcomes and to be more creative.
Know your own values and biases towards help seeking behaviours. For those who have the stiff upper lip approach to managing issues on our own (and it is certainly important as
We have great capacity to problem solve as individuals and we are also wired to problem solve together when having trouble. Feeling more connected when collaborating in problem solving permits the “survival” part of our brains to rest while permitting the problem-solving area of the brain to be activated. This assists us to think more clearly, be able to incorporate more information when developing outcomes and to be more creative.
Be a role model. Ask for input from those you work with. This is also important for managers to lead by example and to set the expectation of what is and what is not acceptable or desirable in the workplace. Make a habit of asking others about how they are going and if there is anything you can assist with.
Normalise input from others as a positive and important part of problem solving. Structure opportunities into meetings where team members discuss not only what is going well but also areas where others can add ideas or provide alternative information and possible solutions.
KNOW YOUR OWN VALUES AND BIASES TOWARDS HELP SEEKING BEHAVIOURS. For those who have the stiff upper lip approach to managing issues on our own (and it is certainly important as individuals we take responsibility for working through issues the best we are able to) notice if you are unintentionally projecting a message of judgement or criticism that may be contributing to others not seeking input.
Make time to prioritise checking in with others. Research suggests that help is only provided when people feel confident to ask for support. Make time available to let people know it is ok to ask you for assistance. Giving time and permission for this to occur will provide opportunity for people to put their hand up for support. Have an attitude of positivity towards help seeking requests. View requests for assistance as constructive steps towards solution finding. Acknowledge that it takes courage to seek input and demonstrate vulnerability.
BE A ROLE MODEL. Ask for input from those you work with. This is also important for managers to lead by example and to set the expectation of what is and what is not acceptable or desirable in the workplace. Make a habit of asking others about how they are going and if there is anything you can assist with.
NORMALISE INPUT FROM OTHERS AS A POSITIVE AND IMPORTANT PART OF PROBLEM SOLVING. Structure opportunities into meetings where team members discuss not only what is going well but also areas where others can add ideas or provide alternative information and possible solutions.
Remember that the best outcomes typically occur when problem solving has included multiple viewpoints and ways of thinking in the process. Welcome different perspectives.
MAKE TIME TO PRIORITISE CHECKING IN WITH OTHERS. Research suggests that help is only provided when people feel confident to ask for support. Make time available to let people know it is ok to ask you for assistance. Giving time and permission for this to occur will provide opportunity for people to put their hand up for support.
If you would like support and would like to talk with a professional, please feel welcome to contact your member assistance support line 1300 326 350 or visit adaq.org.au/MAP
HAVE AN ATTITUDE OF POSITIVITY TOWARDS HELP SEEKING REQUESTS. View requests for assistance as constructive steps towards solution finding. Acknowledge that it takes courage to seek input and demonstrate vulnerability.
REMEMBER THAT THE BEST OUTCOMES TYPICALLY OCCUR WHEN PROBLEM SOLVING HAS INCLUDED MULTIPLE VIEWPOINTS and ways of thinking in the process. Welcome different perspectives.
ADAQ.ORG.AU/MAP
If you would like support and would like to talk with a professional, please feel welcome to contact your member assistance
Bernie will be remembered as idealistic and determined, uncompromising towards himself and others.
Bernard Homan was born in Brisbane on 16 April 1933, the only surviving child of George and Vera. His memories of growing up in the inner western suburbs of Brisbane included flattening pennies on the Ashgrove tramlines and keeping a pet cockatoo. He went to secondary school at Gregory Terrace and won a Commonwealth Scholarship to university. He graduated from the University of Queensland as a Bachelor of Dental Science with First Class Honours in 1955.
Over the next decade Bernie continued at The University of Queensland School of Dentistry, serving on the teaching staff along with his undergraduate classmate Ken Adkins, who introduced him to his future wife Judith. They married in 1959 and had 3 sons. He completed a Masters degree in periodontics but his interest was always public health dentistry.
Bernie was appointed as a Senior Lecturer in Community Dentistry from 1967 to 1991. The older generation of University of Queensland dental graduates will remember Bernie’s passionate advocacy for adjusted water fluoridation and preventive dentistry. As his family noted in his eulogy, there was no grey in Bernie’s spectrum, just black and white!
Bernie joined ADAQ as a student Member in February 1953 transitioning to active membership on graduation. Perhaps his most recognised role in ADA was as Chair of the Scientific Committee for the 1985 Australian Dental Congress, held in the recently completed and previously untried Performing Arts Centre in South Brisbane. He was replaced by his Vice-Chair,
Don O’Donoghue in the last year of the build up to the Congress following diagnosis of and treatment for a melanoma. He thus avoided having to deal with untried projection equipment, which burned up several lecturers’ precious one-off Kodachrome slides.
Perhaps his most recognised role in ADA was as Chair of the Scientific Committee for the 1985 Australian Dental Congress
He was a pioneer in Queensland in community dentistry and served on the Queensland Health Education Council (1966-76). As an Oral Epidemiologist, Queensland Department of Health, in 1971 Bernie conducted an oral health survey in Far North Queensland and the Torres Strait Islands. Four years later he was appointed as an Oral Epidemiologist, Department of Health, Northern Territory for a periodontal survey at Bamyili and Yirrkala Aboriginal Communities.
Bernie’s commitment and vision led to a number of international appointments: a Visiting Fulbright Scholarship at the Department

of Community Dentistry, University of Kentucky College of Dentistry where he studied dentistry within Health Maintenance Organisations (1972-3); a consultancy 1978 at the Pan American Health Organisation to the Department of Health, Education and Welfare, USA; an advisory role to the Delivery Systems Branch, Division of Dentistry, USPHS; Chair (1979-81 and 1981-84) of the Asian-Pacific Dental Federation Committee on Public Dental Health; and the Visiting Professor (1987) Department of Dental Ecology and Health Services Research Centre, University of North Carolina at Chapel Hill USA to study Quality Assurance in Oral Health Delivery Systems.
Screening Examination Sub-committee, Expert panel in dentistry, Committee on Overseas Professional Qualifications, Australian Department of Immigration and Ethnic Affairs (1980-82). This sub-committee and its functions were later subsumed into the Australian Dental Council. Bernie also served as a member of the National Health and Medical Research Council Working Group on Effectiveness of Water Fluoridation (1989-91) and on the NHMRC Expert Panel on Dental Care for the Older Adult (1989-90).
He pushed for a risk-based protocol and directed the public dental services towards practices that we now recognise as minimum intervention dentistry.
Bernie also had a role in redirecting oral health care in the Australian Defence Force (ADF). He was commissioned into the Army Reserve (ARES) as a Consultant in Community Dentistry at Army Office with the rank of Lieutenant Colonel (from 1979). He reoriented the ADF focus on treating oral diseases and preparing troops for deployment to prevention and dental fitness across the board. His consultancy coincided with the move towards and eventual introduction of annual readiness requirements for all personnel in the ADF. To meet the annual requirements all service personnel of all ranks had to be tested and passed competent at weapons, physically fit, medically fit and dentally fit. This reform remains in place today. He was promoted to Colonel and posted as the Colonel Consultant – Dental at 1 Military District until his retirement from the Army in 1991. His appointment as the Honorary Dental Surgeon to the Governor-General (1985-87) recognised this distinguished service.
His academic career extended into many domains: an examiner in Public Health and Preventive Dentistry for the Royal Australasian College of Dental Surgeons (1988-91) and a member of the
He was a pioneer who made a difference.
Bernie left academia in 1991 to take up an appointment as the Director, Oral Health, Queensland Health Branch(1991-95). In this role he challenged the existing mantras of preventive dentistry including that children needed an examination, scaling and cleaning and topical fluoride every 6 months. He pushed for a risk based protocol and directed the public dental services towards practices that we now recognise as minimum intervention dentistry. From this position he was seconded as the Director assisting the Chief Health Officer of Queensland Health 1995-97. This was a difficult period to have this role. It coincided with the Soorley Lord Mayoralty of Brisbane and the Lord Mayor’s Task Force on Water Fluoridation, the report of which did not find in favour of water fluoridation at that particular time. He was also appointed to the Dental Board of Queensland for two terms (1991-97).
Those who worked with Bernie will remember him as idealistic and determined, uncompromising towards himself and others. He was a pioneer who made a difference. He also made time for his family and we extend our condolences to Judith, Peter, Chris and Michael and their families.
ADA PRESIDENT, 2015
ADAQ PRESIDENT, 1985


The Keys Family, the Dental Community and Periodontal World lost one of its standard bearers recently after a Purgatory of 16 months suffering from the relentless condition of Motor Neurone Disease. To have afflicted such an accomplished athlete was a double blow to him and his dear friends and wide circle of Marathon Runners, David being awarded a University Blue as a member for 5 years in the Queensland Marathon Team, with a PB of 2hrs 32mins.
He had indefatigable enthusiasm for life, rising to the top in everything he attempted.
David commenced St Joseph’s College, Gregory Terrace in 1957 coming over from St Thomas’s, Camp Hill. He was welcomed with a punch in the arm by the class ‘leader of the pack’, who received as good as he gave. From that moment we bonded like glue and remained a tight bunch of friends for the next 64 years. He was the reason I chose Dentistry when receiving the surprising news I’d won a Commonwealth Scholarship. “Why Dentistry, David?” “My Brother, John has been one for two years and owns a new Holden.” We graduated in 1966, when he then worked for John in Toowoomba. We sailed with him to London, did the FDS Primaries together, sharing a house with our wives Lyn and Ingrid.
Rebecca (now a Melbourne Lawyer) and Matthew (now a Specialist in Pain Management) were born in England and the family returned in 1971, when David took up a Teaching post in Periodontics at UQ Dental School, subsequently becoming a Registered Periodontist in 1972 completing his PhD (UQ) in 1979. We eventually shared rooms on Wickham Terrace, most mornings starting with a 20km run from the City to UQ and back. David and Lyn’s third child Peter died tragically of cancer aged 3.
To complement his love of sports he completed a Bachelor of Human Movements Degree at UQ, majoring in Cricket and Tennis. There was nothing David did by halves: he had indefatigable enthusiasm for life, rising to the top in everything he attempted: as President of Australian Society of Periodontology (Qld) for two terms, President of The Cricketers’ Club for 3 years, and President of the Easts Rugby Union Club. He married his second wife, Sandy, in 1983. She bore him 3 children, James, Tim (both Dentists, Tim a Paedodontist) and Belle (a Sonographer). Sandy remained his rock until the end. David served as President of the Gregory Terrace Old Boys’ Association for 2 years. He remained a serving member (part-time) in the RAAF Reserve for 37 years, rising to Group Captain and had 4 years as the Director of Health Reserves and 2 years and as Chair of the Medical Defence Unit responsible for all Medical Reservists in the Qld Navy, Army and Airforce.
Our Moreton Island Fishing trips were an annual highlight. When asked one day how long the barge trip took, he responded, “Two pies and a six-pack.” If only he could have caught beach worms! We made do with Tailor.
His tragic diagnosis was followed by a slow descent over 18 months during which time Sandy was his lifeline. His close mates of old gathered regularly to take him out of TriCare for coffee until the end. Not once did he complain or utter a negative expression. He remained unbelievably stoic to the end. David’s coffin was draped with his cloak of the Equestrian Order of the Holy Sepulchre of Jerusalem in which Order he was promoted to Knight Commander in 2011, together with the Flag of the RAAF. He will be sorely missed by family and friends but will remain very much alive in our hearts and memories.
KHS, MD (UW), BDSC (UQ), MB BS (UQ), FRACDS, FRACDS(OMS), FFDRCSI, FACOMS, FICD.
ORAL AND MAXILLOFACIAL SURGEON (RET’D). ADJUNCT
ASSOCIATE PROFESSOR, UNIVERSITY OF QUEENSLAND MEDICAL SCHOOL
Stay informed of opportunities and announcements exclusive to the ADAQ community
Dr Matthew Voltz and Dr Alistair Reid would like to welcome Dr Joel Tuckett to Brisbane OMS. Dr Joel Tuckett has commenced practice with us in March 2021 and is happy to accept referrals covering all aspects of Oral & Maxillofacial Surgery.
Contact Brisbane Dental Specialist Centre
• Unit 4/80 Hope Street, South Brisbane.
• Phone: 3844 4400
• Email: mail@oralsurgery.com.au
• oralsurgery.com.au/online-referral/

Perio Care is pleased to announce that Dr Amro Farag, BDSc MDSc(Perio) PhD DClinDent(Perio), Periodontist joined the practice in March 2021. Amro comes with experience in the treatment of advanced periodontal disease, periodontal regenerative surgery and implant dentistry. Amro is a lecturer of periodontics and dental implantology at the University of Queensland and is the current treasurer of the Australian Society of Periodontology (Queensland branch).
For more information
Appointments can be made through our Chermside practice on (07) 3350 4344.
Dr Arabelle Clayden, Oral Medicine Specialist, is pleased to announce that she has recommenced oral medicine practice at Dent8 Dental, 4 Frederick Street, Taringa 4068, Brisbane.
For referrals and all enquiries
Please contact the practice info@dent8.net.au or (07) 3871 3035
We are looking for a full-time Dentist to join our growing private practice located in rural Darwin. This is a great opportunity to experience our tropical lifestyle, excellent fishing and camping locations, whilst working within a modern, well-equipped dental practice performing all aspects of general dentistry including wisdom tooth extractions and paediatric dentistry.
The successful applicant:
• Has excellent communication skills with patients
• Is open-minded, empathetic and understanding
• Is confident in all forms of restorative dentistry and emergency care
• Has a minimum 1 year experience working as a Dentist in Australia, with high clinical skills and standards.
For more information
• Phone: (08) 8988 5050
• Email: reception@humptydoodental.com.au

To assist ADA members in celebrating Dental Health Week 2021 and to educate local children about the importance of oral health, Colgate-Palmolive is providing ADA members with the opportunity to order three Bright Smiles, Bright Futures oral-health education kits to support your DHW initiatives.
ADA members have the option to order both dental professional kits and teacher kits. To receive the teacher kit/s, ADA members should submit an order form providing details of the preschool, school, or community group they will be visiting.
Order forms will be made available on 1 June on the Dental Health Week website (dentalhealthweek.com.au).
Simply download, complete the form, and submit it by COB Wednesday 16 June, for delivery in time for Dental Health Week in August.
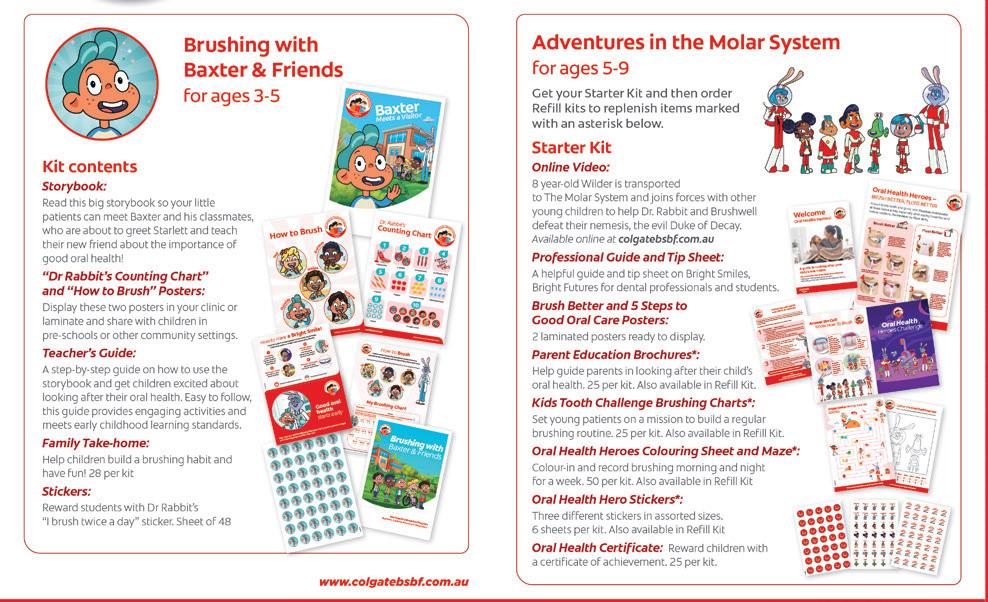
Preschool Kit
• Comprehensive Teacher’s Guide for Preschool Classrooms
• Storybook: Baxter Meets a Visitor
• Emergent Reader
• Two-sided activity poster (Dr Rabbit Counting & How to Brush)
• 28 parents’ take-home brochures
• Brush Twice a Day stickers (48)
• Handwashing resources including a soft handsoap pump
Note: Preschool and Dental Professional kits do not come with toothbrushes or toothpastes.
• Comprehensive Teacher’s Guide (Lesson Plans)
• Storybook: Back from the Molar System: The Search for Toofus
• Two-sided wall poster (How to Brush & Smart Food Choices)
• Stickers
• 32 take-home packs with brushing chart, toothpaste & toothbrush in every kit




Assisting with us
Cert III and Cert IV Dental Assistant training courses available.
Developed by experienced dental experts
Self-paced learning, start anytime
Qualified trainers, one-to-one support
State-of-the-art hands-on training facilities

Pay no establishment fees on your new equipment or fit-out purchase this EOFY*
If you’re considering new equipment or fit-out for your practice this EOFY, we have a little surprise for you. Simply finance your new equipment or fit-out purchase with us by 30 June 2021 and you will save $495 on establishment fees
Now is a great time to take advantage of competitive EOFY pricing and generous government tax concessions on business related assets and we would love to help. We’ve worked with many dental professionals over the years providing finance to help them scale to great heights. Now, let us help you.
Visit boqspecialist.com.au/eofy or speak to your local finance specialist on 1300 160 160.
BOQ Specialist. The bank for dental professionals