DR JAY HSING'S FINAL FROM THE PRESIDENT
DE-ESCALATION OF A PATIENT CONCERN

DR JAY HSING'S FINAL FROM THE PRESIDENT
DE-ESCALATION OF A PATIENT CONCERN

EDITOR
Dr Kelly Hennessy
EDITORIAL TEAM
Dr Jay Hsing
Dr Gary Smith
Ms Lisa Rusten
Ms Melissa Kruger
PRODUCTION
Published by the Australian Dental Association (Queensland Branch)
CONTACT
28 Hamilton Place Bowen Hills Qld 4006
PO Box 611, Albion Qld 4010 Phone: 07 3252 9866
Email: adaq@adaq.com.au
Website: adaq.org.au
ADVERTISING KIT
Information on advertising, deadlines and artwork specifications are available in the ADAQ Advertising Kit: adaq.org.au/advertising
GRAPHIC DESIGN
Jack Cartwright-Glavas
COVER ART DESIGN
Jack Cartwright-Glavas

DISCLAIMER
ADAQ Dental Mirror is published for the information of Members only and is not for general distribution. Copyright is reserved throughout. No part of this publication may be reproduced in part or whole without the written consent of the publisher. This publication is for the purpose of promoting matters of general interest to Members of the Association. The views expressed in this magazine do not necessarily reflect the views and policies of ADAQ or ADA. Publication of advertisements for products or services does not indicate endorsement by ADAQ. All material is positioned and published at the discretion of ADAQ.
PRESIDENT Dr Jay Hsing
SENIOR VICE PRESIDENT
Dr Kelly Hennessy
JUNIOR VICE PRESIDENT
Dr Paul Dever
COUNCILLORS
Dr Carl Boundy (Peninsula)
Assoc Prof Alex Forrest (Moreton)
Dr Peter Jorgensen (Sunshine Coast)
Dr Alexander McDonald (Gold Coast)
ADAQ SUB-BRANCHES
Bundaberg Dr Paul Dever
Cairns Dr Brian James
Gold Coast Dr Norah Ayad
ADAQ COMMITTEES
Awards and Honours Committee
Convener: Dr Jay Hsing
Volunteering in Dentistry Committee
Convener: Dr Jay Hsing
Dr Rachael Milford (Western)
Dr Ellen Rogers (Moreton)
Dr Grace Sha (Moreton)
Mr Glen Beckett (Skills-based)
Ipswich Dr Andrew Wong
Kingaroy Dr Man Chun (Simon) Lee
Mackay Dr Raghu Channapati

Policy, Advocacy and Advisory Committee Convener: Dr Norah Ayad
Rockhampton Dr Chloe Sturgess
Sunshine Coast Dr Peter Jorgensen
Toowoomba Dr Phoebe Fernando
As I write my final President’s Address for the Dental Mirror, I fondly reflect on the past two years, and the privilege of serving as your President. It’s been a great honour, and a challenge that I have truly enjoyed. Opportunities like this are rare, and I was driven to make the most of the time I had in leading our Association.
A positive part of my role as President is being able to acknowledge the wonderful contributions of others. I am incredibly proud of what our organisation has achieved over the past couple of years. This success is the result of a tremendous amount of hard work behind the scenes. My deepest thanks to my fellow board directors, our CEO, Lisa Rusten, and her management team, the hardworking staff at ADAQ who provide the outstanding support and services members have come to expect, and our committee and advisory panel members.
Last but not least, my heartfelt thanks to you, my fellow members, for your unwavering support and words of encouragement. Whether delivered in-person at an event, via email, or by text message, your support has been received with immense gratitude.
I am proud to lead an organisation that consistently provides outstanding support and advocacy for its members. Through strong governance, effective operational systems and prudent financial management, we have delivered essential services and member benefits while maintaining a strong balance sheet. It has been rewarding to see progress across multiple areas, some of which I will highlight below.
As we reflect on these achievements, we must also look ahead with enthusiasm. I am excited to introduce our new Strategic Plan, which builds on the ongoing support and services discussed in my Autumn and Winter remarks earlier this year. This plan will guide us over the next few years, outlining our future vision and the steps required to achieve our goals.

Turning to specific areas of progress, I am delighted that our CPD program has improved in quality and variety in recent years.
Also, a new CPD Pricing Policy was implemented earlier this year to further enhance the value of membership, allowing members to attend courses at 20% below cost price. Looking ahead, there are plans to further enhance our offerings by creating relevant and targeted continuing education courses informed by member needs across all cohorts. Our CPD program will continue to innovate and grow in the future.
Support for our affiliated study clubs and sub-branches has also been a priority. I am pleased to share that they now receive increased support, both financial and non-financial. Additionally, building positive relationships with our profession’s specialist societies has been productive. I have prioritised their promotion, resulting in the establishment of the Bite Club Directory, which has been running for two years now.

Additionally, my commitment to fostering a culture of giving back is reflected in the progress of our Volunteering in Dentistry Committee, which has its own webpage and quarterly e-newsletters. After spearheading the creation of this committee as Junior Vice President, I am thrilled to witness its efforts come to fruition by facilitating partnerships between dental charities and volunteers. Dental volunteering has been a dedication of mine for the past twenty years and holds significant personal meaning.

Another priority has been recognising the diverse needs of our members. As such, there has also been a renewed focus on supporting those in rural and regional areas. The Rural/Regional Initiative aims to better serve members outside the Southeast corner. ADAQ successfully hosted its inaugural regional event in Emerald, drawing strong participation from Emerald, Rockhampton, Barcaldine, Yeppoon, Bundaberg, Ipswich, Brisbane, and the Gold Coast. Local attendees were extremely appreciative of an event in their region. This event serves as a promising pilot for future regional support initiatives.
This year also marked the establishment of the Edward Walter Haenke Rural Practitioner Award, which honours exceptional rural and remote dentists who have significantly contributed to their community or demonstrated exemplary commitment to rural/remote oral health. Looking ahead, several initiatives are planned for regional members, including a formal panel of dental specialists for tele-advice and a regional mentoring program. Another key area of progress has been in our advocacy efforts. It’s encouraging to note ADAQ's active engagement in discussions with both state and federal governments. We represented the profession in the Queensland Government's inquiry into reducing vaping. I’m thrilled to see the introduction of new tobacco and vaping laws, which include some of the harshest penalties in Australia, following on from the inquiry. Furthermore, ADAQ was invited to Parliament House to meet with Queensland’s Health Minister, the Hon. Shannon Fentiman, to discuss approaches to improve the oral health of Queenslanders. This was followed by a joint letter to the Federal Health Minister, the Hon. Mark Butler, outlining possible reforms for improved oral health. While there remains more work ahead, I'm gratified that ADAQ is playing a significant role in these efforts.
A further significant achievement is the recently completed renovation of the ADAQ offices in Bowen Hills, which has brought a much-needed revitalisation. It is fantastic to have a building that members can be proud of and that inspires our staff to continue their great work. Importantly, the renovation ensures the building meets all fire and safety codes, provides secure access for both

Our Constitution currently requires that Council includes one Councillor from each of the eight membership divisions. Proposed changes aim to consolidate these into two divisions— South East Queensland and Regional Queensland—simplifying the election process while ensuring representation from both urban and regional areas, with four Councillors from each region. Up to four co-opted Councillors may also be appointed based on skills and experience, though they cannot serve as President.
Additionally, it is proposed that the terminology in the Constitution be updated to align with the Corporations Act 2001 (Cth) and corporate governance standards (e.g. changing Council to Board and Councillors to Directors).
In 2019, members voted to pursue registration as a charitable institution with the Australian Charities and Not-for-profits Commission as part of the ADAQ and ADAQUE merger. However, ADAQ has been unable to meet the requirements due to its status as a professional organisation, leading to the discontinuation of this pursuit. Therefore, it is recommended that the deed of amalgamation be amended to allow the merger to proceed.
These changes will be voted on at this year’s AGM on the morning of Saturday 23rd November, just before our Annual Clinic Day. The current Council unanimously supports the proposed changes and recommends that members vote in favour of each resolution.

ADA FEDERAL
While you've read about the strength and prospering of ADAQ above, I also wish to see our Federal body flourish and reach its potential. This is personally important to me because I am a proud ADA member and I believe a strong ADA enhances our profession's advocacy efforts and ensures cohesive support for all members across Australia.
Image Annual Clinic Day 2023

Achieving this goal requires fostering accountability and transparency in our Federal body’s decision-making processes and actions, particularly in light of the substantial reported financial loss of $4.8 million, across the previous two financial years, due to the 2023 FDI Congress in Sydney.
In my previous address, I alluded to communicating with the ADA Federal Board in an attempt to seek transparency. Unfortunately, despite efforts from myself and others, there has been minimal progress. I’ve requested details from the current ADA Federal Board about the FDI Congress loss, including a breakdown of income and expenses and summaries of the two reports commissioned afterward, which were funded by ADA members. I have also sought clarification on their strategic goal expenses and how members’ monies are being allocated. Regrettably, I have only received perfunctory and superficial responses.
Although ADAQ helps the Federal body collects their fees, the latter operates independently from ADAQ. This means that the ADA Federal Board is not obliged to provide any answers to ADAQ or its President. Therefore, it is incumbent upon us, as individual members, to consistently pursue the transparency we seek. We must pose questions and advocate for openness and accountability when it is lacking.

VALUES AND THE FUTURE OF THE PROFESSION
Health professionals, in their primary role of providing care to the community, should prioritise patients' interests. Over recent decades, this ideal has been eroded by the commodification of healthcare. Dentistry has not been spared. Although business owners understandably seek a return on investment, it is crucial that these considerations do not come at the expense of what is in the best interest of patients.
The vast majority of dentists are honest, hard-working, patient-focused professionals. However, concerning business practices have emerged, such as the increasing use of patients' superannuation to finance dental treatment. While this can be justified in certain cases, many members I have spoken with are concerned about its misuse. There is a genuine fear that, similar to the fallout from the Chronic Disease Dental Scheme, this revenue-generating strategy will harm our collective reputation.
Dentistry is demanding, and I believe in supporting each other as colleagues. However, ignoring questionable business practices makes us complicit and undermines the integrity of our profession. We must collectively uphold high ethical standards both with ourselves and our fellow colleagues. Preserving the trust and respect of the communities we serve is essential, not just for us but also for future generations of dentists.
It has been an honour and privilege to lead ADAQ for the past two years. I will be forever grateful for the opportunity to have served as your President. At the end of the day, nobody in any position of leadership is special or remarkable. We are all simply stewards of our profession.
Members transitioning into retirement often write to explain that is why they are discontinuing their membership, and to thank the Association. I have enjoyed engaging with them as they highlight the professional camaraderie and personal joys of their careers. As a mid-career dentist, I value their insights. I also wish earlycareer dentists and students a similarly rewarding journey.
In a recent Louis Vuitton commercial, Rafael Nadal and Roger Federer were both asked how they would like to be remembered. They both said they would much rather be remembered for what they were like as human beings than as tennis players. I think this can be applied to any profession, including dentistry.
By upholding the values of our profession and advancing the mission of our Association, I look forward to a thriving future ahead for both the dental profession and ADAQ.
Image Dr Hsing's Presidential Speech at Annual Clinic Day 2023

ADAQ CONTINUING PROFESSIONAL DEVELOPMENT TEAM
ADVANCING DENTAL EXCELLENCE THROUGH COLLABORATION
For the first time, ADAQ's Clinic Day is being held on a Saturday, we have made Clinic Day more accessible for yourself and your dental team. Join us on Saturday 23 November for a day of professional development and networking.
For this year's Annual Clinic Day, we will be advancing dental excellence through collaboration. We work in a profession where collaboration is in order to achieve predictable and meaningful results for patients. With presentations from not only leading dental professionals, but also from allied health speakers.
ADAQ Annual Clinic Day is an opportunity for dental professionals, including dentists, dental hygienists, and dental assistants, and the broader dental community to come together to learn about the latest developments and best practices in the field of dentistry.
Expressions of interest are now open and we invite all ADAQ members, their dental team and allied health professionals to join us for 2024. Take a sneak peek to what is on offer for this year's Annual Clinic Day by exploring our speaker's topic, lectures and hands-on workshops.
THE ROLE OF PATIENT-CENTRED COMMUNICATION IN ENCHANCING DENTAL TREATMENT OUTCOMES
Dr Vas has an intense passion for his work. He loves orthodontics, and his easy-going nature and good sense of humour puts his patients at ease.
Dr Vas was born in India in 1977, and as a teenager he wore braces. When he was a junior in high school he realised a career in orthodontics offered an exciting opportunity for him to combine his interests in science and mathematics.
HAVE YOU EXPRESSED YOUR INTEREST FOR ANNUAL CLINIC DAY 2024?
Hands-on workshops experience high demand, make sure you express you interest to not miss out:

The ADAQ CPD & Events team can assist you with you registering you and your dental team and other queries: events@adaq.com.au
Dr Vas completed his undergraduate education at Dr. MGR Medical University in Chennai (Madras), India. He then received a master’s degree from the University of St. Thomas in Minnesota, USA before completing his orthodontic training at the University of Sydney, where he graduated with a merit scholarship. He also obtained his membership diploma with the Royal College of Surgeons of Edinburgh in the UK through an independent examination process conducted in New Zealand.
Dr Vas continues his education and training through a variety of orthodontic courses and seminars. In addition, he lectures to specialist dental groups throughout the world and teaches handson courses.
FROM COMPLAINT TO RESOLUTION: STRATEGIES FOR THE DENTAL TEAM TO MITIGATE PATIENT CONCERNS
Larissa graduated with a Bachelor of Oral Health in Oral Health Therapy and Master of Health Management, with a focus on health care law and ethics and research.
Larissa has worked in the dental profession since 2004 with experience in private practice, the University sector and the NHS in the United Kingdom. Larissa’s academic background and clinical experience puts her in an ideal position to assist ADAQ members with patient complaints, health fund audits, regulatory notification and insurance queries.
PAEDIATRIC DENTISTRY AND ORTHODONTICS: COLLABORATIVE CARE
Dr Nymphia is a Specialist Paediatric Dentist, who provides comprehensive dental care for children of all ages, including those with complex dental, medical, special needs, injuries and decay. As a Paediatric Dentist, Dr Nymphia provides treatment to children with dental caries or decay, dental trauma, special needs and behavioural difficulties requiring management (treatment) with Nitrous Oxide sedation or happy gas, intravenous sedation or General Anaesthesia (GA).
She was appointed Clinical Associate Lecturer in the Faculty of Dentistry at the University of Sydney in 2009 and worked as part-time staff specialist at the Sydney Dental Hospital until 2011.
Her special interests include prevention of dental decay in young children, providing comprehensive dental treatment to children with Autism spectrum disorder, Attention deficit disorder and those with special needs.
Patrick himself has experienced jaw pain and locking in the past, and so is passionate in helping others who live through these experiences.
INFECTION CONTROL STANDARD - ADA GUIDELINES
This is my favourite conference to attend every year. Worthwhile and useful CPD. programs.
Moira H, Annual Clinic Day 2023
Dr Nymphia has current memberships of the Australian Dental Association, Australasian Academy of Paediatric Dentistry, Australian and New Zealand Society of Paediatric Dentistry and Royal Australasian College of Dental Surgeons.
Dr Nymphia graduated with a Bachelor of Dental Surgery from University of Otago, New Zealand in 2000. After completing the Graduate Dental Program she worked in a busy private practice in rural New Zealand in 2001, before migrating across the Tasman.
She continued working in private practice in Sydney and then Perth until 2003 after which she was appointed Junior Dental Registrar at Princess Margaret Hospital for Children in Perth. In 2005, she moved to Melbourne to pursue her passion and specialist training in Paediatric Dentistry.
She completed her Doctor of Clinical Dentistry (Paediatric Dentistry) from the University of Melbourne in 2007 and commenced part-time specialist practice in 2008.
Great way to wrap up the CPD year and to catch up and network with colleagues before the madness of Christmas sets in!
Marguerite H, Annual Clinic Day 2023
MANAGEMENT OF TEMPOROMANDIBULAR JOINT DISORDERS
Patrick Lin began his Physiotherapy journey after struggling with chronic injuries during his final year of high school athletics. It was through this arduous process that he developed a great appreciation for the complexities of human movement and effective rehabilitation.
Patrick subsequently studied Physiotherapy at the University of Queensland with the intention of further developing his skills in the generalist musculoskeletal and sports rehabilitation. Many patients he saw in general musculoskeletal practice suffered from headaches and neck pain, many of which also experienced chronic and complex symptoms. Patrick felt that without specialist training, he could not create the best outcomes for these patients, and so he sought to develop his skills with Nigel and Scott at The Headache Neck and Jaw Clinic.
He has also completed Watson Headache® Institute Level 1 Foundation Course since joining the team.
Professor Laurence Walsh AO is a specialist in special needs dentistry who is based at the University of Queensland in Brisbane, where he is an emeritus professor, having retired from UQ in 2020. Laurie has been teaching infection control and clinical microbiology for over 25 years at postgraduate level and was chief examiner in microbiology for the RACDS from 1999-2020.
Laurie has been a member of the ADA Infection Control Committee since 1998, and has been re-appointed as its chair for 2021, having previously served as chair from 2009-2014. He has contributed to various protocols, guidelines and checklists and manuals used in Australia.
Always enjoy the ADAQ clinic day… CPD plus catch up with colleagues! What more could you ask?
Venerina P, Annual Clinic Day 2023
He has presented invited courses and lectures on infection control across Australia and internationally. Laurie has written over 60 articles on infection control and in addition published over 200 journal papers on clinical microbiology. He currently serves on three committees of Standards Australia (personal protective equipment; and instrument reprocessing) and in recent years has been an adviser to the Communicable Diseases Network of Australia and the Australian Commission on Safety and Quality in Health Care.

Key revisions have been made to this latest edition of the Infection Prevention Control Guidelines based on the evolving knowledge base in this area.
DAVINA BARKER, LYNNE MCLEAN & MARICEL MOSS
It is important that every registered Dental Practitioner and all members of the Dental Team familiarise themselves with new elements and update their practice policies accordingly.
During December 2023, Standards Australia released the Reprocessing of reusable medical devices and other devices in health and non-health related facilities, AS 5369:2023. This standard specifies the requirements and practices necessary for the effective and safe reprocessing, storage, handling and transportation of reusable medical devices and other devices used in human health care and other treatments.
The Australian Dental Association Infection Prevention Control Guidelines are informed by the following key reference documents and their updates:
• Australian Guidelines for the Prevention and Control of Infection in Healthcare (NHMRC 2019)
• AS 5369:2023 reprocessing of reusable medical devices and other devices in health and non – related facilities
• National Hand Hygiene Initiative
• Australian National Guidelines for the management of Healthcare Workers Living with Blood Borne Viruses Who Perform Exposure Prone Procedures and Healthcare Workers who Perform Exposure Prone Procedures at Risk of Exposure to Blood Borne Viruses (CDNA 2019)
We have put together the following list to assist you in meeting your practice obligations.
The reprocessing area must be appropriate in layout and size for the volume of reusable medical devices (RMDs) being reprocessed. Part of the dental facility must be designated as the reprocessing area for RMDs (including cleaning, packaging and sterilising) and must not be used for any other purpose. Ideally, this should be a dedicated room that is physically separate from the treatment room(s).
If that is not possible because of limited space, in line with the principle of segregation, reprocessing should occur well clear of the contaminated zone, in an area that is partitioned off, with good workflow processes established, and where there is minimal risk of aerosol contamination of the reprocessing area.
Use of physical segregation (such as dividers or partitions) becomes important in such situations, to ensure proper segregation. Such physical segregation is an important consideration in the design of reprocessing areas.
Segregation requirements also mean that where reprocessing work and patient care occur in the same room or physical space

Segregation partitions between the dirty and clean parts of the reprocessing area, e.g. between packaging and sterilising. These could include solid walls, glass walls, dividers or partitions, dividers made of polycarbonate or Perspex™, the use of passthrough equipment (e.g. washer-disinfectors and steam sterilisers that pass the load through solid walls), or sufficient physical separation (spatial segregation) to prevent clean areas or processed RMDs being compromised.
The practice must develop a process map (workflow diagram) showing how RMDs and other items progress through reprocessing. This must be designed to ensure that within the reprocessing area of the practice, the risk of cross-contamination is effectively managed, in accordance with a completed risk assessment. (AS 5369, p. 40) (ADA Infection Control Guidelines 5th Edition page 38).

ACCESS STANDARDS
AUSTRALIA'S 5369:2023
With Bowie-Dick type tests, ensure that the brand and type of the B-D type test used matches the chamber size of the steam steriliser (noting that small sterilisers have a chamber size of less than 60 litres, under EN 13060). The steriliser manufacturer may recommend particular products for the Bowie-Dick type test.
Once the mandatory daily Bowie-Dick type test has been completed (and passed), the next point in the process is the question of whether to then undertake a further test, using a process challenge device (PCD).
The answer to this reflects two considerations. These two aspects apply to both small and large steam sterilisers, in terms of the optional use of PCDs under AS 5369
The first of these is the information stated in the steam steriliser IFU. The steriliser manufacturer may recommend using a particular type of PCD at a certain frequency (e.g. daily) and may even recommend a particular brand and product for that purpose. The manual will then also specify which cycle to select when running the PCD test and will describe where to place the PCD test device in the chamber.
The second consideration is a local risk assessment. If a practice only sterilises solid instruments in their pre-vacuum steam steriliser, an optional PCD test is not indicated, since solid items do not create major issues for air removal and steam penetration. On the other hand, if the practice is regularly sterilising RMDs with a lumen (e.g. handpieces), the hollow regions of these make air removal and steam penetration more challenging. In that case, the practice should follow the process below for deciding on the use of a PCD, based on a local risk assessment, whenever dental handpieces and other hollow items are being sterilised.
The approach is as follows:
1. Identify the hollow/lumened items that are being sterilised, and note how often this occurs (e.g. daily, weekly). Examples include:
High-speed air turbine handpiece
Low-speed restorative handpiece
Surgical handpiece
Piezoelectric ultrasonic scaler body or piezo-surgery handpiece
Metal large or small diameter suction tip
Metal triplex tip
2. When hollow items are being sterilised every day, the practice could consider performing a PCD test that conforms to ISO 11140.6 (i.e. poses a challenge that is equivalent to the reference hollow device) every day, prior to a live load with hollow items.
3. When hollow items are being sterilised only occasionally (i.e. not every day) the practice could consider performing a PCD test that conforms to ISO 11140.6 on the day, prior to a live load with hollow items.



4. If surgical handpieces being sterilised, they must be packaged into a sterile barrier system and steam sterilised using a B cycle. An appropriate PCD test that conforms to ISO 11140.6 should be done on that day prior to a live load with surgical handpieces.
5. If unwrapped high-speed air turbine handpieces or low speed restorative handpieces are being sterilised in a compact cassette steriliser with S cycles, follow the steriliser manufacturer IFU. The practice could consider using the manufacturer’s particular PCD test on that day prior to a live load with handpieces. It is essential to follow the loading information in the IFU exactly, to position the handpieces in the cassette for sterilisation. (AS 5369)-(8.7 - table 8.2), (Clause 8.7.4) (ADA Infection Control Guidelines 5th Edition page 50)
Learn more with the ADA webinars on the infection preventsion guidelines, free for ADA members:

AS 5369: 2023 requires dental practices and services to have in place a system for batch control identification that links steriliser cycle batch information of a critical item that has been sterilised, with an individual patient procedure.
The batch number then connects the patient procedure to a particular steam steriliser cycle, and thus to the records which document:
The specific steam steriliser that was used
The date (and time) that sterilisation was undertaken
The load contents
The type of sterilising cycle used
The identification of the loading operator
The cycle information from physical indicators (e.g. on data or printouts)
Results of checking chemical indicators
Results of checking packages for conformity (intact SBS, intact seals, no damp or wet packages)
The identification of the unloading operator who released the load for use.
BCI also plays and important role when there is back-to-base and offsite reprocessing, since it connects patient records to the records of sterile stock processed by those external suppliers.




The key actions in BCI can be summarised as follows:
Maintaining a comprehensive log of steam steriliser cycles, with data entry at the time of loading the chamber. An operating logbook must be maintained for every steam steriliser, which records the data for each cycle. This record book must be kept for at least 7 years after the last entry, unless a longer period is stated in the facility’s local policy or required under jurisdictional regulations.
Record batch numbers so that cycles with critical instruments can be identified.
Apply batch code information onto packages, either manually or with a labelling gun;
Check packages after sterilising for correct sterilisation outcomes.
Complete the sign-off that releases the cycle contents, based on physical and chemical indicator results;
Operators are to enter batch codes into patient records for all surgical procedures where critical items are used. The clinician is responsible for ensuring that batch codes for packages of sterile items are transferred into the patient’s records for the relevant procedure.
Because BCI can refer to instrument packs or sets, as well as to individual instruments, there is logic in simplifying the inventory of instruments used for surgical procedures, specifically how these are packaged into sets (rather than single instruments). It is likely to be more efficient to combine several critical instruments into a set, rather than to keep each instrument in its own separate package. AS 5369- (6.4.2), (2.5.3),( 2.6.3.2) (ADA Infection Control Guidelines 5th Ed page 45-47)
Water
Water for rinsing -assessing hardness
Water softening
Options for water for steam sterilisation
Water for final rinsing
Measurement of endotoxins and how to follow a risk-based approach
Water treatment systems for high quality water
Ventilation
Types of air conditioning
Directional flow
Air changes per hour
Measuring air exchange rates
Impact on sterile stock shelf life
Using local exhaust ventilation
When loading the autoclave are pouches placed plastic side or paper side up on the trays?
With regard to positioning non-packaged RMDs and packages of RMDs in the chamber of a steam steriliser, when a B cycle is run, the superior efficiency of air removal from paper-plastic pouches by multiple vacuum cycles is such that the arrangement of these (plastic facing up, facing down, or on the side) does not greatly affect air removal. The main considerations are that, for items laying horizontally, paper down is preferred, to avoid water condensation droplets dampening the paper. Most steam sterilisers have angled or vertical racks. These racks are ideal for small pouches as they prevent droplet pooling, and also improve loading efficiency and steam penetration through the load. Hence, the manufacturer’s loading instructions should be followed, and where not specified, the preference is for plastic side up/paper side down.
Is it mandatory to use a washer-disinfector to reprocess regular dental instruments (rather than an ultrasonic cleaner or manual cleaning)?
Mechanical cleaning of instruments (RMDs) can be carried out in washer-disinfectors or by using ultrasonic cleaners. Mechanical cleaning is preferred to manual cleaning as it is more efficient and reduces the risk of exposure to blood, and the risk of penetrating skin injuries from sharp or pointed instruments. The use of washer-disinfectors is not mandatory unless using RMDs that are expressly required to undergo an instrument washing and thermal disinfection process. However, washer-disinfectors are more efficient at pre-sterilisation cleaning than both ultrasonic cleaners and manual cleaning.
Mechanical cleaners used in dental practices may be washer disinfectors (which also provide thermal disinfection), ultrasonic cleaners or combination units which perform both. Not all instruments are suited to thermal disinfection or ultrasonic cleaners, so careful attention should be paid to the manufacturer’s instructions to determine the appropriate management of RMDs.
Do I need to keep the chemical indicators from the autoclave? Chemical indicators are designed to be read at the end of a cycle, and the result obtained is compared with the reference colour change chart provided by the manufacturer.
Once checked, chemical indicators must be discarded. There is no requirement to keep and store these indicators. The colour change chemistry used within chemical indicators is not intended to provide results of archival quality if these indicators are stored for several years.

This is particularly relevant to Class 5 and 6 indicators, which use sophisticated multi-step chemical reactions. When indicators are stored in record books, acid released from the paper of the record book can permeate into the indicator and cause colour changes. Thus, do not keep ANY chemical indicators (Classes 1 through to 6) as part of the records of the practice.
What daily steam steriliser (autoclave) tests am I required to do?
Always consult the manufacturer’s instructions. In general, if using the most common type of steriliser (a small pre-vacuum steriliser which runs B cycles), you will need to run, as a minimum:
Vacuum leak rate test: This is normally performed daily (weekly in the case of sterilisers that have air detectors).
Bowie-Dick type test: This is run each day immediately after the vacuum leak rate test and before processing any RMDs. For larger steam sterilisers (chamber capacity above 60 litres), follow the manufacturer’s IFU regarding the types of tests that are required.
Refer to the section on PCDs for detailed information on the selection and use of PCDs. This discusses using a PCD when that is described in the steam steriliser IFU. It also discusses using a PCD when indicated by a local risk assessment, e.g. when restorative handpieces or other hollow items are being sterilised.
At ADAQ, we recognise that the entire dental team plays a critical role in providing quality oral care. If you are a Dental Prosthetist, Oral Health Therapist, Dental Hygienist, Dental Technician, Practice Manager, or Dental Assistant, we welcome you to ADAQ Dental Team Access. Here, you can gain access to relevant ADAQ services and resources.
The TPC team provides practices with support and consultancy services through a team of skilled professionals with extensive experience in infection control, practice accreditation, and practice management.
To find out how the ADAQ TPC team can help you, contact consultancy@adaq.com.au

To be eligible for Dental Team Access, you must be employed within a practice where a dentist is a financial member of ADAQ. If you are a dental technician or prosthetist, you must have the support of a nominated dentist who is a financial member of ADAQ.
Dental Team Access offers numerous benefits, including:
• Discounted rates on all CPD courses
• Regular communications and information from ADAQ
• Access to the ADAQ Dental Community closed Facebook Group
• Access to the Dental Mirror, a quarterly online magazine
• Access to an online wellness portal
• PI/PL insurance at favorable prices* Insurance assistance including claims management, legal assistance and dispute resolution is only available if their practicting member dentist holds an insurance policy with ADAQ.
• Access to infection control resources

There is no annual fee for ADAQ access for the dental team.
Applying is simple. Complete the form at the provided link, and our Membership Services team will reach out to you within 2-3 business days to provide your access details (login/password). Sign up today and start enjoying the benefits of Dental Team Access!
For more information, visit the Dental Team Access webpage, www.adaq.org.au/DentalTeam

Dental practices, like many other small businesses, are not immune to financial challenges. Factors such as fluctuating patient numbers, increasing overhead costs, and evolving industry standards can place significant pressure on a dental practice's financial stability.
When faced with these challenges, restructuring and turnaround strategies become crucial. Here we explore how dental practices navigate financial difficulties and achieve long-term stability and growth.
Restructuring in a dental practice involves making significant changes to its financial and operational structure to improve efficiency, profitability, and sustainability.
Common reasons necessitating the need for a structure review include:
• Declining Revenue: Decreased patient volume or lack of repeat patients.
• Rising Costs: Increased expenses for supplies, equipment, or personnel eating into profitability.
• Operational Inefficiencies: Ineffective processes or outdated technology hindering performance.
• Debt Issues: High levels of debt or poor cash flow management may threaten the practice's viability.
The first step in any restructuring effort is a thorough financial assessment. This involves a review of the financial statements and analysing key metrics to understand the current state of the practice.
The Important areas to review are:
1. Profit and Loss Statement (Income Statement): This statement provides insights into revenue, expenses, and overall profitability. Identifying trends in income and expenses can help pinpoint areas requiring adjustment.
2. Balance Sheet: Analysing assets, liabilities, and equity helps determine the practice’s financial health and liquidity. It is crucial to assess whether the practice has sufficient assets to cover liabilities.
3. Cash Flow Statement: Understanding cash flow patterns is vital for managing day-to-day operations and ensuring there is enough liquidity to meet obligations.
4. Key Performance Indicators (KPIs): Metrics such as revenue per patient, revenue per hour per dentist, the practices booking percentage, and overhead percentages in relation to patient fee income provide valuable insights into the practice’s performance.
Restructuring in a dental practice involves making a significant changes to its financial and operational structure to improve efficiency, profitability, and sustainability
Once the financial assessment is complete, the next step is to develop a restructuring plan. This plan should address both operational and financial aspects of the practice.
Analyse Expenses: Identify areas where costs can be reduced without compromising patient care. For example, renegotiating supplier contracts or reducing discretionary spending can help lower expenses.
Optimise Staffing: Evaluate staffing levels and roles to ensure they align with patient needs. Cross-training staff and implementing efficient scheduling can improve productivity and reduce staff costs.
Fee Adjustments: Review and adjust fee structures to reflect the value of services provided. Ensure that fees are competitive and aligned with industry standards.
Increase Patient Volume: Implement marketing strategies to attract new patients and retain existing ones. Offering promotions or expanding services can also boost revenue.
Technology Upgrades: Invest in modern technology and practice management software to streamline operations and improve patient experience, including a clinical analytics add-in that will provide you with useful data and areas of focus.
Process Improvement: Evaluate and refine clinical and administrative processes to enhance efficiency and reduce waste.
Restructure Debt: Negotiate with lenders to restructure existing debt to obtain a cheaper interest rate. This may involve extending payment terms or consolidating loans to reduce monthly payments.
Improve Cash Flow: Implement strategies to improve cash flow, such as offering discounts for early payment or tightening credit policies.
Successful implementation of a restructuring plan requires careful consideration, execution and ongoing monitoring. Key steps in the implementation process include:
Communicate Change: Clearly communicate the restructuring plan to staff, patients, and other stakeholders. Transparency helps build trust and ensures everyone is aligned with the new direction.
Monitor Progress: Regularly review financial and operational performance against the goals outlined in the restructuring plan. Use KPIs and financial reports to track progress and adjust as required.
Adjust as Needed: Be prepared to make further adjustments to the plan based on performance data and changing circumstances. Flexibility is essential for navigating the complexities of a turnaround.
Seek Professional Advice: Engage with financial advisors, accountants, or consultants who specialise in the dental industry. Their expertise can provide valuable insights and support throughout the restructuring process.
Accounting plays a critical role in the restructuring and turnaround process. Accurate financial reporting and analysis are essential for making informed decisions and measuring progress. Regular and accurate bookkeeping is critical to ensure that the information to hand is up to date, so that timely and informed decisions can be made.
Financial Forecasting: Develop financial forecasts to project future performance based on the restructuring plan. Forecasts help anticipate cash flow needs and identify potential financial challenges.
9 Budgeting: Create a detailed budget that aligns with the restructuring plan. A well-structured budget provides a roadmap for managing expenses and allocating resources effectively.
9 Performance Tracking: Use accounting systems to track financial performance and compare it against benchmarks. Regular performance reviews help identify areas of concern and opportunities for improvement.
9 Tax Considerations: Be mindful of tax implications related to restructuring activities. For example, changes in revenue or expense patterns may affect tax liabilities. Consult with tax professionals to ensure compliance and optimise tax outcomes.

Restructuring and turnaround efforts in dental practices require a comprehensive approach that integrates both financial and operational strategies. By conducting a thorough financial assessment, developing a robust restructuring plan, and leveraging accounting information, dental practices can address financial challenges and position themselves for long-term success. Effective communication, ongoing monitoring, and professional guidance are key to navigating the complexities of restructuring and achieving a successful turnaround. Ultimately, with the right strategies and support, dental practices can enhance their financial stability, improve operational efficiency, and continue to provide high-quality care to their patients.
William Buck’s Business Advisory team are Australia’s leading advisor to dental practitioners, helping you improve value and align personal and business objectives.
For a confidential, complimentary consultation to discuss how we can assist with aligning your business with you personal and financial goals, please contact your local William Buck Business advisory specialist.



At the core of every dental practice is a dedication to patient care and wellbeing. Recognising that patients may arrive with a range of anxieties or concerns allows us to create a more supportive and empathetic environment.
These concerns could include anxiety about procedures, fear of pain, past negative experiences, or worries about costs. Addressing these feelings with compassion and clear information can greatly enhance their experience. By focusing on their needs, especially during challenging moments, we can foster a more positive and reassuring atmosphere.
WHAT HAPPENS IN THE BRAIN WHEN PATIENTS FEEL OVERWHELMED?
When someone feels overwhelmed, anxious, or distressed, their brain experiences significant changes. The brain’s “fight or flight” response, managed by the amygdala, becomes activated. This response triggers the release of stress hormones like cortisol and adrenaline, preparing the body to react to perceived threats. The amygdala functions like an alarm system, signalling the brain and body to prepare for action when it detects something stressful. This can lead to physical symptoms such as increased heart rate, rapid breathing, and muscle tension, alongside emotional responses like fear or frustration. Meanwhile, the prefrontal cortex, responsible for decision-making and higher-order thinking, may become less active under stress, making it harder for individuals to think clearly or make rational decisions.
To support patients during these times, dental professionals can create an environment that emphasises safety and calm, which may help reduce stress responses and enable patients to process information more effectively.
UNDERSTANDING AND RESPONDING TO PATIENTS EXPERIENCING DISTRESS
When patients experience strong emotions such as anxiety or anger, dental teams play a key role in helping to ease these feelings and create a more comfortable experience. Here are some strategies tailored to support patients who may be feeling distressed:
Supporting Patients Experiencing Anxiety
9 Create a Calming Environment: The atmosphere of the practice sets the tone for a patient’s visit. A calm waiting area with soothing colours, comfortable seating, and minimal noise can be very effective. Soft, neutral decor and calming imagery reduce sensory overload, which often heightens anxiety. Offering amenities like water, reading materials, or access to nature themed videos can also contribute to a peaceful environment.

9 Implement Anxiety-Reduction Techniques: Providing patients with tools to manage anxiety can be very beneficial. Techniques like encouraging the patient to breathe deeply and slowly —where patients inhale slowly through their nose and exhale through their mouth—can calm the nervous system. Noise-cancelling headphones with calming music or nature sounds can also help patients relax. Allowing patients to bring a companion for support or to have a familiar item, like a stress ball or fidget tool, during their visit can further enhance their comfort.
9 Communicate Clearly and Reassuringly: Clear communication is essential. Explaining procedures step-by-step in simple, non-technical terms, and reassuring patients that their comfort is a priority, can significantly reduce anxiety. Describing what sensations to expect (e.g., “You might feel a slight vibration”) can alleviate fear of the unknown. Providing opportunities for patients to signal if they need a break and encouraging them to ask questions at any time promotes a sense of control and reassurance.
9 Personalised Care and Flexibility: A personalised approach recognises that each patient is unique. Some may prefer longer appointment times to discuss concerns without feeling rushed, while others might find comfort in shorter, more frequent visits to gradually build trust. Allowing patients to choose music or adjust lighting in treatment rooms can also give them a sense of control and help reduce anxiety.
9 Maintain a Calm and Open Stance: A calm demeanour and open body language can convey a willingness to listen and support patients who may feel angry. Open, relaxed postures, such as keeping hands visible and making gentle eye contact, can help set a positive tone. A calm and steady voice can help ease tension, as patients often mirror the emotional cues of those around them.
9 Validate and Acknowledge their Feelings: Patients experiencing anger often feel unheard or misunderstood. Acknowledging their feelings with empathetic statements like, “I can see how this situation might be upsetting for you,” can help them feel understood. Listening without interruption or immediately jumping to solve the problem allows patients to express themselves fully, which can be very calming.
9 Collaborate to Find Solutions: After acknowledging their feelings, working together to find a solution can be empowering. Asking open ended questions like, “How can we make this better for you today?” allows patients to voice their specific concerns. Offering practical solutions, such as rescheduling appointments, adjusting treatment plans, or discussing financial options, can help rebuild trust and improve the patient experience.
9 Establish Clear Boundaries: While empathy is important, maintaining a safe and respectful environment is essential.

Gently stating what is acceptable can help guide interactions toward a positive outcome. For example, “I’m here to help you, and I’d like us to have a calm conversation so we can find a solution together” focuses on creating a respectful and supportive dialogue.
Proactively addressing common triggers can help prevent situations where patients may feel anxious or angry. Here are some practical tips to enhance prevention efforts:
When patients experience strong emotions such as anxiety or anger, dental teams play a key role in helping to ease these feelings and create a more comfortable experience.
Streamline Appointment Scheduling and Reduce Wait Times: Efficient scheduling can help minimise wait times, reducing patient anxiety and frustration. Implementing an effective appointment system that keeps things running smoothly. Using reminders, and promptly informing patients of any delays with an estimated wait time can set clear expectations.
Consistent and Clear Communication: Preventing misunderstandings can significantly enhance the patient experience. Clearly outlining what patients can expect during their visit, including procedures, costs, and preparatory steps, helps build trust.
Using simple language and providing visual aids can clarify complex information. Following up after procedures with care instructions and contact details for further questions ensures continuity of care.
Create a Welcoming Atmosphere: First impressions matter, so a friendly greeting, a clean and comfortable waiting area, and a respectful tone from the entire team can positively influence a patient’s perception of the practice. Training all team members in customer service skills that emphasise patience, empathy, and helpfulness creates a cohesive, supportive environment.
Offer Feedback Opportunities: Inviting feedback from patients helps practices continually improve. Using surveys or comment cards to gather insights into what’s working well and what could be enhanced shows patients that their opinions are valued, promoting a sense of being heard and respected.
Empower Patients with Choices: Empowering patients with options can reduce feelings of helplessness. Allowing them to make decisions, such as choosing appointment times, pain management options, or specific treatments, fosters a sense of involvement in their care, making them more comfortable and less anxious.
The ability to effectively manage patient concerns is closely linked to the wellbeing of the team. Supporting patients can be emotionally demanding, so it’s important for dental teams to engage in regular self-care. Practical self-care strategies can help maintain resilience and enable team members to provide the best care for patients:
Take Regular Breaks: Short, frequent breaks throughout the day can help team members recharge and prevent burnout. Stepping outside, taking a brief walk, or practicing deep breathing exercises during breaks can refresh energy levels and improve focus.
Practice Stress Management Techniques: Incorporating stress management into daily routines, such as mindfulness, meditation, or stretching, can enhance emotional resilience. Encouraging team members to take a few moments to centre themselves before or after seeing patients can contribute to a calmer, more focused work environment.
Maintain a Healthy Work-Life Balance: Supporting the team in setting boundaries between work and personal time is essential for their wellbeing. Encouraging a balanced work-life relationship helps team members feel refreshed and ready to support their patients effectively.
Promote a Supportive Team Environment: Fostering a workplace culture where team members feel comfortable discussing challenges and seeking support builds a sense of community. Regular team check-ins, open communication, and peer support groups help reduce feelings of isolation and promote a supportive environment.
Encourage Continuing Education and Training: Offering opportunities for professional growth can be a form of self-care for the team. Training in stress management, communication skills, and patient de-escalation techniques equips the team with valuable tools and boosts their confidence and job satisfaction.
Recognise and Celebrate Efforts: Recognition and celebration of team achievements can boost morale and motivation. Acknowledging hard work and successes, whether it’s effectively managing a challenging patient interaction or consistently providing excellent care, fosters a positive work environment.
By equipping dental teams with strategies to address patient concerns thoughtfully and proactively, practices can significantly enhance the overall patient experience. Focusing on clear communication, personalised care, and creating a calm environment helps ensure that patients feel supported, heard, and respected. When both patients and the team are well cared for, dental practices can create a positive, stress-free environment that benefits everyone involved.

THE ADAQ MEMBER ASSISTANCE PROGRAM CAN BE ACCESSED AT ADAQ.ORG.AU/MAP TO DISCUSS SUPPORT FOR YOUR EMPLOYEES OR FOR INDIVIDUALS TO ARRANGE SUPPORTIVE COUNSELLING.
DR PAUL DEVER ADAQ JUNIOR VICE PRESIDENT
This issue, the spotlight is on Dr Paul Dever, our Junior Vice President, orthodontist and owner of multiple regional practices across Queensland.
CAN YOU INTRODUCE YOURSELF AND A BRIEF HISTORY OF YOUR PROFESSIONAL CAREER?
Hi, I’m Paul! I am currently our ADAQ Councillor for the Burnett Region. I also wear a couple of other hats – I am the current ADAQ Junior Vice President, Chair of the Asset Management Committee and the inaugural ADAQ representative on the newly formed ADA Federal Board Nominations Committee – responsible for selecting board members for our federal body. I completed a Bachelor of Science through UQ majoring in biomedical science and developmental biology before undertaking my dental training at the University of Sydney. In 2012 I completed my specialist orthodontic training through the University of Melbourne. I currently live in Bundaberg and have satellite practices in Hervey Bay and Maryborough.
WHAT MOTIVATED YOU TO JOIN THE ADAQ COUNCIL?
I’m going to be totally honest here, I kind of ‘fell into’ the role when our illustrious past president, Dr Adrian Frick’s time on council came to a close. Nobody in our region was jumping out of their seats to replace Adrian. For people not familiar with the Burnett region, it is quite sizeable covering nearly 50,000km2 and representing a population of around 340,000. I put my hand up because I felt it was important for me to contribute to discussions on the oral health issues (among others) affecting our regional community. As a specialist working across the geographic region, I also prioritise the support our oral health care providers require when delivering services in regional Queensland.
COULD YOU SHARE WHY YOU CHOSE TO PURSUE A CAREER IN DENTISTRY, AND LATER SPECIALISE IN ORTHODONTICS?
It’s a bit of a soppy story, but I had a wonderful orthodontist when I was an adolescent patient (I won’t embarrass him by mentioning him by name, but he knows who he is…). He inspired me that orthodontics is an enjoyable and rewarding career. If I’m honest again, I wasn’t ‘taken’ by a lot of the other procedures in general dentistry. I really enjoyed the patient interactions and the ‘help’ I could provide to my general dental patients, especially nervous ones. I believe this personal mental block has help me to empathise and connect with other practitioners who are struggling with the day-to-day issues of practising clinical dentistry.
HOW DID YOUR BACKGROUND IN BIOMEDICAL SCIENCE AND DEVELOPMENTAL BIOLOGY INFLUENCE YOUR JOURNEY INTO DENTISTRY AND ORTHODONTICS?
At that point in time, the way to gain entry to the Bachelor of Dental Science program at the University of Queensland was by completing 12 months of a Bachelor of Science degree and then ‘moving across’ into second year BDSc. Unfortunately, I pursued other priorities and didn’t make the cut for dentistry. I continued my BSc and was fortunate to gain entry two years later to the University of Sydney’s post-graduate dental program.
Probably the biggest challenge I faced during specialist training was the fact that I was slightly older than my colleagues and ‘at a different stage of life
DID YOU FACE ANY CHALLENGES WHILE TRANSITIONING FROM GENERAL DENTAL PRACTICE TO SPECIALISING IN ORTHODONTICS, ESPECIALLY DURING YOUR TIME IN MELBOURNE?
Probably the biggest challenge I faced during specialist training was the fact that I was slightly older than my colleagues and ‘at a different stage of life’. Yesmin and I moved to Melbourne with a 13-month-old daughter and we welcomed our second child during my second year of specialist training. I have a great deal of respect for anyone who completes a tertiary degree, but those who manage that achievement with a young family deserve an extra pat on the back.
AS SOMEONE WITH EXPERIENCE IN RUNNING MULTIPLE ORTHODONTIC PRACTICES ACROSS REGIONAL QUEENSLAND, WHAT STRATEGIES HAVE YOU FOUND MOST EFFECTIVE IN BUILDING AND MAINTAINING A RESPECTED RAPPORT WITH YOUR PATIENTS?
I am acutely aware that one of my strengths is that I am a ‘people person’. I can relate to, and easily converse with someone from any walk of life. I believe that one of the fundamental tests of character (that I challenge everyone to try every day!) is put yourself in the other person’s position. It sounds corny, but I try to treat everyone in my dental chair as if they were my mother, wife or one of my kids. If you aim to treat every patient as your nearest and dearest, you can’t go wrong. This is incredibly hard to do sometimes.
But patients can sense and pick up on your efforts and intentions. Even if things go awry, as they sometimes do, if you are approaching a situation from the right mindset reasonable people will appreciate your best intentions.
GIVEN YOUR ADVOCACY FOR EQUAL ACCESS TO DENTAL SERVICES IN REGIONAL AREAS, WHAT INITIATIVES OR CHANGES DO YOU BELIEVE ARE MOST CRUCIAL FOR IMPROVING SERVICE PROVISION IN THESE REGIONS AND HAVE YOU BEEN INVOLVED IN ANY?
This is a really hard question to answer. Regional Queensland is crying out for every type of worker. I speak to parents/patients/ business owners every day and nearly all of them are looking for staff. From tyre fitters to anaesthetists to primary school teachers to hairdressers, we need more qualified people out in the country. I think the regions need to get smarter about ‘selling’ themselves. Make it hard for people to not want to live there. Highlight features like the cost of housing is more affordable, there’s a better work-life balance due to reduced commute times and the vast number of leisure activities available when work is done. The second thing our regions need to do is focus on drawing the local kids back to their region after they have completed their training in the bigger centres.
I believe that one of the fundamental tests of character (that I challenge everyone to try every day!) is put yourself in the other person’s position.

COULD YOU DESCRIBE SOME OF THE KEY INSIGHTS OR LESSONS YOU'VE LEARNED FROM LECTURING LOCALLY AND INTERNATIONALLY ON ORTHODONTIC TOPICS?
One thing I don’t think we give ourselves enough credit for across Australia and Queensland is the high level of dental education we have. We are blessed with talented clinicians and brilliant researchers who are beacons that the rest of the world turns to. I have been extremely humbled by the calibre of the Australian speakers on the couple of occasions that I have been invited to lecture internationally. I was fortunate to run a workshop in Barcelona in 2019. At that conference, the American’s and European’s were on the edge of their seats, trying to extract every last little morsel of information from the Aussie speakers. We need to be proud of this and celebrate the talented people we have around us driving us to be better.
WHAT ADVICE WOULD YOU GIVE TO YOUNG DENTISTS OR ORTHODONTISTS ASPIRING TO BUILD SUCCESSFUL CAREERS IN REGIONAL AREAS LIKE QUEENSLAND?
The world is your oyster. You will never have to worry about running out of work. The patient’s really appreciate you and what you do for them. In the smaller centres, you become an integral member of the local community. Everyone knows who you are –they smile and say G’day when you are out at the shops. Overall, I believe that the lifestyle is more relaxed and less stressful than living in the bigger centres. The rewards are here for the taking, come out and make them yours!
One thing I don’t think we give ourselves enough credit for across Australia and Queensland is the high level of dental education we have. We are blessed with talented clinicians and brilliant researchers who are beacons that the rest of the world turns to.
The patient’s really appreciate you and what you do for them. In the smaller centres, you become an integral member of the local community. Everyone knows who you are – they smile and say G’day when you are out at the shops.


Cert III and Cert IV Dental Assistant training courses available.
Developed by experienced dental experts
Self-paced learning, start anytime Qualified trainers, one-to-one support State-of-the-art hands-on training facilities
In the 1940s and early 1950s, there was a flurry of research on ammoniated dentifrices.
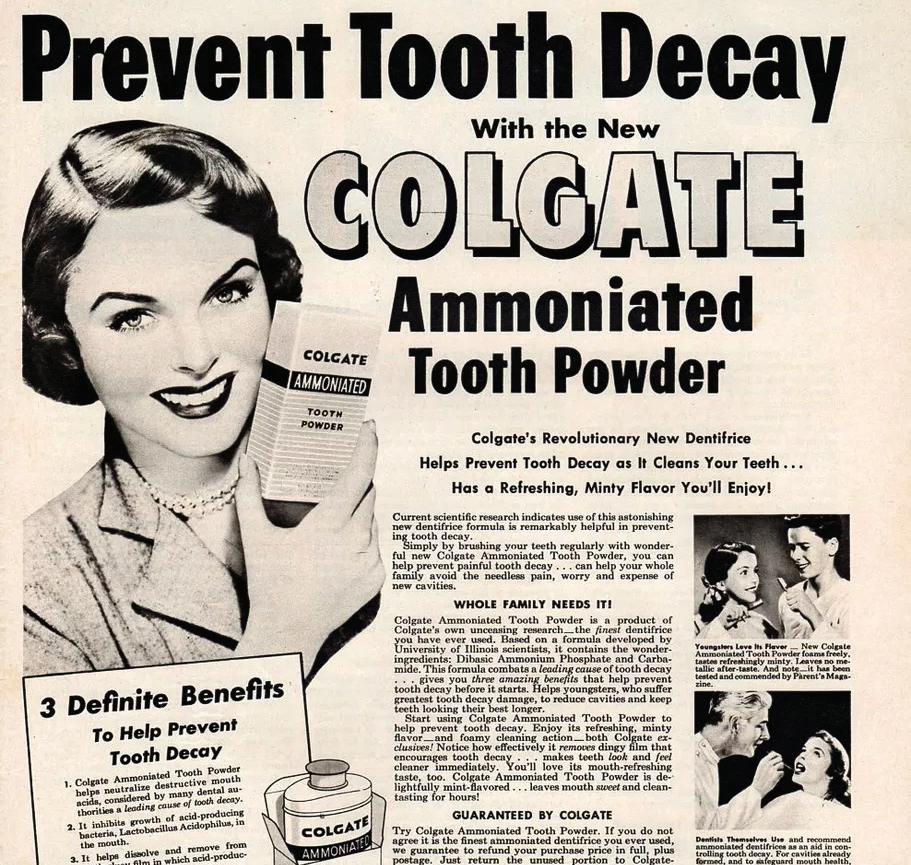
In those years, researchers at the University of Illinois led by Robert G Kesel (1903-1988), and endodontist, published preliminary findings that caries reduction would occur with the ‘consistent use of dentifrices and mouth rinses containing ammonium phosphate and urea’.
Based on this research, an ammoniated tooth powder formula was patented in the US and marketed in 1949 as ‘AMUROL’. An example of this is in the National Museum of American History’s collection. The early formulae of these dentifrice contained 5 per cent dibasic ammonium phosphate and 3 per cent urea.
In Australia, Ivorite was distributed by Clinton-Williams Pharmaceuticals and later Riley-Williams pharmaceutical wholesalers (685 Heidelberg Road, Alphington Vic). It was available in powder and paste version. ‘Ammonium therapy’ was heavily marketed in 1949 as especially suitable for children to avoid future dental issues. Ivorite contains urea peroxide (carbamide) and dibasic ammonium phosphate, which were purported to inhibit acid-forming bacteria which cause tooth decay.
Carbamide peroxide is still used today in over-the-counter teeth whitening products and other cosmetics. Urea is also present in many dermatological preparations
While evidence killed the ammonia-urea against caries research idea pretty quickly, RG Kesel went on to publish research on prevention and control of dental decay, including an interesting article in 1965 on the detrimental effect of soft drinks on dental health.
One of our members, Dr K. Powell, recently donated some items to the ADAQ Museum of Dentistry, originating from earlier dental facilities at the Enoggera Army Base, Brisbane. The donation includes a bottle of Ivorite powder. It is 11.5 cm tall, 4 cm wide at base, with clear glass and a black plastic screw lid. The label is unfortunately stained with what looks like ink, but the instructions are still visible.
Along with a selection of other objects from our museum, this tooth cleanser bottle may feature in an upcoming exhibition at the Museum of Brisbane. The Precious exhibition will bring together thousands of remarkable items from public and private collections across Brisbane. Keep an eye out for it when it opens in November 2024! Precious - Museum of Brisbane | MoB
The early formulae of these dentifrice contained 5 per cent dibasic ammonium phosphate and 3 per cent urea.
For example, a whole page was dedicated to the ‘amazing new discovery’ in the Daily Mirror newspaper on Wednesday 3 August 1949 (p.16). The new toothpaste was hailed as “the revolutionary way to prevent tooth decay… promises to make history” happened worldwide in the mid-1940s, from the earlier cosmetic claims (white teeth equal attractiveness, freshness of breath) to medical and hygiene purposes (bacteria killing, preventing tooth decay).
Ammoniated dentifrices’ efficacy claims were never fully endorsed by the dental profession, and safety concerns grew quickly. Thankfully, by the mid-1950s, fluoride toothpastes became the standard product, and the only one endorsed by the dental profession. Most other types of dentifrices fell gradually out of favour, including the ammoniated ones.
The use of urea and ammonia compounds for oral hygiene and care was well known in antiquity, and is traceable all the way back to the habits of ancient Romans. It seems women in particular used children’s urine as a whitener and cleanser.
1. KESEL RG. The Effectiveness of Dentifrices, Mouthwashes, and Ammonia-Urea Compounds in the Control of Dental Caries. Journal of Dental Research. 1948;27(2):244-258. doi: 10.1177/00220345480270022001
2. KESEL R. “Ammoniated Dentifrice,” U.S. Patent 2,622,058 (Dec. 16, 1952), assigned to the University of Illinois Foundation. 1498416055956365106-02622058 (storage. googleapis.com)
3. KESEL RG. Effect Of Soft Drinks On Dental Health. Illinois Dental Journal. 1965 Jun;34:370-372. PMID: 14313270.
4. DAVIES GN, KING RM. The effectiveness of an ammonium ion tooth powder in the control of dental caries. J Dent Res. 1952 Dec;31(6):775. doi: 10.1177/00220345520310060701. PMID: 13022832. https://pubmed.ncbi.nlm.nih. gov/13022832/
5. SEGRAVE K. America Brushes Up: The Use and Marketing of Toothpaste and Toothbrushes in the Twentieth Century. Jefferson, N.C.: McFarland & Co., 2010.
WHERE CAN I FIND MORE DENTAL HISTORY?
Visit the ADAQ Museum of Dentistry (MoD) website.
Thankfully, by the mid-1950s, fluoride toothpastes became the standard product, and the only one endorsed by the dental profession.

To organise a visit of the Museum of Dentistry or donate, email adaq@adaq.com.au
With 20% off the cost price of ADAQ courses for members, explore popular courses at the recently renovated ADAQ CPD and Training Centre at Bowen Hills, Brisbane. Scan the QR Code to learn more and register before it's too late.
of Minimal


OrthdonticsIs there any evidence out there?




















ZOE DEREK & LARISSA ALDERTON | ADAQ COMPLIANCE AND ADVISORY SERVICES
Within dentistry, many dentists find it stressful to handle difficult conversations with their patients. Whether it's due to the emotional vulnerability of an anxious patient, an adverse event or the unyielding complaint of a patient with unreasonable expectations – you are not alone.
The ADAQ Compliance and Advisory Services team assist our members with patient complaints every day. We aim to guide and support you through the process to hopefully find a resolution to the issue. We understand new graduates are placed into practice well equipped to clinically assess and provide dental care to patients, but often haven’t yet been exposed to effective communication in challenging situations. This also applies to experienced practitioners facing these circumdstances for the first time.
Having a patient raise concerns about their care can be a disheartening experience for any dentist, but it is often not a reflection on the care provided. Concerns being raised can be due to many different reasons that we will explore further below, to assist you with how to react, and what to do if this happens to you. It's important to remember that feedback and reflection can only help you improve going forward and not to take it personally or let emotions cloud your judgement when responding to the concerns.
INFORMED CONSENT & RECORD KEEPING
Following the provision of accurate and relevant information about the treatment and the alternative options available to them; and
With adequate knowledge and understanding of the benefits and material risks of the proposed treatment relevant to the person who is having the treatment or procedure.
Dental practitioners are required by the Dental Board's Code of Conduct to obtain informed consent from their patients before providing care to them.
Informed financial consent is an important but separate consent process. Patients are also consumers and where they are required to pay for health services, the price should also be given and consented to before commencing treatment.
Valid informed consent is achieved through effective communication with the patient or guardian, education, and a shared decision-making process.
The consent process should be documented and recorded in the clinical treatment notes. Documenting your consent process and any conversations had with your patient is integral to not only the patient’s continuity of care, but also your own protection from liability or potential regulatory action. As dental records are considered a legal document, if it’s not documented – ‘it didn’t

One area that we see many complaints arise from, is lack of informed consent. When the patient was not fully informed of all their options or wasn’t aware of the potential outcomes including treatment failure specific to their individual case, they can feel that something has gone wrong even if this was an inherent and seemingly obvious risk.
Having a robust informed consent process and including written consent forms for more complex treatment helps to protect you when things go wrong but also assists with avoiding potential ramifications of a complication as well.
Regardless of who the patient is, how they have reacted or what the concern raised is, it is important to try not to take it personally, and to put yourself into the patient’s shoes to understand where these concerns have come from. For example: Do they feel they have not been fully informed? Have they questioned the treatment provided because of past experiences? Do they have unreasonable expectations?
1. Reach out for support from peers and your PI provider: Senior colleagues and peers can provide valuable insight into how to handle these situations and provide you with feedback on how the treatment was managed, and their recommendations to resolve the concerns based on their own experiences. Contacting your PI provider to discuss the situation for assistance to resolve it can also assist to try to stop any situations from escalating further as well. As part of your ADAQ membership and PI insurance, we offer our advisory services to provide you with recommendations. This can include general advice, assistance with a response to the patient or make a PI insurance claim on your behalf, dependant on your initial preference and situation.
2. Acknowledge the complaint, demand or issue: To address the complaint in the first instance, there are a few ways to consider managing this and the approach will be dependent on your position on the matter and preference specific to the circumstances. We recommend you acknowledge the patient’s complaint or demand regardless of your position, however, and remain empathetic and respectful throughout.
As dental records are considered a legal document, if it's not documented'it didn't happen'.
If you feel you can’t respond to the concerns immediately, letting the patient know that the concerns have been received and giving them a date of when you will get back to them, will help them to feel heard and that their concerns are being taken seriously.
3. Consider the approach you wish to take:
Every situation and request from a patient will be different. Some patients simply wish to have their complaint addressed and to be assured by the practitioner, others are angered by the situation and may make demands of you. You might consider whether one of the following options suits your position:
• Provide no refund – If the patient has requested a refund, you can advise the patient that you are not in a position to provide a refund and your reasoning as to why. Keep in mind, some patients may not be satisfied with this and make further demand for refund or compensation or make a ‘formal’ complaint about you.
• Offer a refund – You can offer a refund to the patient for either the full or partial costs of the treatment costs incurred out of your own pocket as a gesture of goodwill on an ‘ex gratia basis’ and to resolve the matter in its entirety. We recommend discussing this with the ADAQ Compliance and Advisory Services team and/or your PI provider before making an offer to a patient.
• Lodge as a claim with your professional indemnity insurer - For demands for compensation for loss and damage suffered by the patient outside of a refund, including for the cost of rectification of work required to be undertaken by the patient, you may consider lodging as an insurance claim (claims are accepted by the insurer on a case-by-case basis, please discuss this with ADAQ for more details around the policy wording, coverage and process).
We are happy to review our member’s responses to the patient and make any suggestions and amendments to assist you. When responding to concerns, using wording such as ‘I am sorry for your experience’ and ‘I am sorry to hear you feel this way’ is appropriate to show empathy, and also ensure that you are not opening yourself to liability. We are also happy to speak with a patient on your behalf if they are agreeable and if this is of assistance to you.
Principle 4 of the shared code of conduct is as follows: Basing relationships on respect, trust and effective communication enables practitioners to work in partnership with patients.
When a patient becomes aggravated and unreasonable, or you feel that there has been a breakdown in trust and/or communication, it may be appropriate to cease the treating relationship between yourself and the patient.
9 You are ensuring the continuity of care for the patient by facilitating their transfer to another clinic. This is done by offering the prompt transfer of the patient's dental records, offering them referral to another practitioner or specialist, and making it clear of your recommendation to them moving forward and how urgently they require ongoing care.
9 If you are not comfortable with speaking to the patient any further and wish to cease communication all together, we can assist to liaise between yourself and the patient with consent from both parties. This can assist to deescalate the situation and remove the emotional aspects of the communication.

Most experienced dentists have been in your shoes before and there is nothing to be ashamed of.

Reach out to peers for support and discuss with any mentors you might have. Most experienced dentists will have been in your shoes before and there is nothing to be ashamed of.
We are here to support you and appreciate that these situations can be incredibly stressful especially when faced with the situation for the first time.
We also encourage you to seek support in regard to your wellbeing. As part of our commitment to members we have partnered with Workplace Wellness Australia to provide you with a range of wellness services called the Member Assistance Program (MAP), which you can access at www.adaq.org.au/MAP
Read more on page on 19 to better understand how to deal with similar situations that were discussed earlier.

If you have a patient complaint you wish to discuss further, have any questions around informed consent or wish to discuss any general queries – the Compliance and Advisory Services team are here for you.
Ahpra provide information on when a conern has been made against a practitioner.

The ADAQ Compliance and Advisory Services team can also provide general advice and assist with queries around patient complaints: assist@adaq.com.au
The Compliance and Advisory Services Team consists of clinical and compliance professionals who understand your profession.
You can rely on their expertise and experience to help you make sense of complaints, health funds, and other compliance matters, another benefit of ADAQ membership.

The ADA Dental Health Foundation coordinates and provides the delivery of pro bono dental treatment to disadvantaged members of the community.
The Foundation accepts referrals to the Volunteer Dental Programs for clients who are being supported by a registered charity or not-for-profit organisation. Our volunteer dentists provide their time, expertise and practice facilities at no cost to eligible patients. We asked existing volunteer Dr Nelson Bayer about why they choose to volunteer with the ADA Dental Health Foundation.
WHY DID YOU DECIDE TO VOLUNTEER WITH THE ADA DENTAL HEALTH FOUNDATION?
As a dentist, I understand the importance of oral health in overall well-being. By volunteering my skills and expertise, I have the opportunity to positively impact the lives of individuals who may not have access to regular dental care.
This sense of fulfillment and the gratitude expressed by those I help, contribute to my own sense of wellbeing and desire to contribute to positive societal change.
By volunteering my skills and expertise, I have the opportunity to positively impact the lives of individuals who may not have access to regular dental care.
I registered for the Rebuilding Smiles Program with the ADA Dental Health Foundation to help work towards ending domestic violence. I recognise the importance of raising awareness, providing support services, and advocating for policies that protect survivors and prevent future incidents of abuse.
Engaging in altruistic activities such as volunteering has been shown to lower stress levels and improve mental health. As a busy professional, taking time to give back to my community through volunteering allows me to step away from the demands of my practice and focus on something meaningful, and practice gratitude.
As a dentist, I am thankful for the opportunities and privileges that my profession has afforded me. The ADA Dental Health Foundation has given me the chance to give back to the community that has supported me throughout my career.
The process in volunteering for the ADA Dental Health Foundation has been very easy, mostly thanks to the exceptional organisation of the State Coordinator and our Practice Manager. All communication has been clear, direct, and most helpful. The team at Valley Dental have all expressed their satisfaction in participating in the program and share the same sense of fulfilment in rebuilding smiles.
We look forward to participating in the program again in the future and highly recommend it to fellow ADA members.
The ADA Dental Health Foundation seeks to improve the dental health of Australians who cannot easily access or afford dental care.
Your involvement is crucial to the success of our program. Our initiatives thrive on the philanthropic spirit of dental practitioners like you.
If you are considering contributing to the ADA Dental Health Foundation by volunteering your time and expertise to provide a patient with a course of treatment please take a moment to visit our website and complete the form and your State Coordinator will contact you with further information.
The ADA Dental Health Foundation has given me the chance to give back to the community that has supported me throughout my career.

LEARN MORE ABOUT THE ADA DHF AND HOW YOU CAN HELP

Stay informed of opportunities and announcements exclusive to the ADAQ community

Dr Anthony Speed, in association with anaesthetists from the Wesley Anaesthetic Group, wishes to advise that he can facilitate treatment for patients requiring general anaesthesia in our outpatient facility at Holland Park. This is particularly useful for patients who have no private hospital insurance.
With an extensive range of experience, the team is willing to undertake wisdom tooth removal, implant placement and perform routine restorative dentistry on all age groups including children aged 3 and above.
Anxiety sufferers, local anaesthetic problems, severe gag reflex sufferers, special needs patients, and dementia sufferers have all been successfully treated over the years.
Additionally, we are now able to offer Cerec single visit crowns so that the patient does not have to return for subsequent cementation. Patients who are medically compromised can be treated at St Andrew’s Private Hospital by arrangement.
If this service can be of assistance to some of your patients, please phone the reception staff on (07) 3397 1339 for further information. Referral booklets are available on request.
Used A-dec 500 Chair Packages for sale.
• 12 months warranty on A-dec parts
• Excellent condition
• Refurbished by QDS technicians
• Options available
• Inspect at Morningside showroom
• Great value for money
• Installation and on-going service available
CONTACT
Brian Gardiner 0488 072 332 or sales@qds.net.au

TMJ Clinics Australia is offering a unique opportunity to join our multidisciplinary clinic and earn while you learn on a part-time basis.
No TMJ experience is required! We will teach you how to assess, diagnose and treat TMJ patients to become an experienced TMJ clinician.
This is an excellent opportunity particularly for dentists considering specialty training. If TMJ is something of interest to you, please feel free to reach out to Christina for further information
CONTACT
Christina Sadler - Operations Manager
Email: admin@tmjclinics.com.au
ALICIA CLARK
MEMBERSHIP SERVICES COORDINATOR
WHAT’S A DAY LIKE IN YOUR ROLE?

I am the Membership Coordinator in the Membership and Marketing Team with a key focus on the ADAQ Insurance Scheme. Alongside Darren Tredgett, we look after the dayto-day membership and insurance inquires.
TELL US ABOUT YOUR CAREER SO FAR
I started my career in a financial planning office managing new business insurance and investments. The principal advisor’s late father was a dentist, so the office paid homage to him with antique dental equipment throughout. I could never have imagined 20 years later I would be working alongside the Museum of Dentistry.
I continued in the world of superannuation and UK pension transfers for a few years before changing direction and moving into health regulation.
I worked at the Dental Council in New Zealand for 11 years as Deputy Registrar managing a team across registration, recertification, and professional standards.
WHAT DO YOU LIKE BEST ABOUT WORKING AT ADAQ?
There was something comforting about the familiar, from my early days in insurance to my time with the Dental Council, this role was a natural transition to life in Australia – It was meant to be.
Now 18 months on, the people keep me here, my team are a truly great bunch of people.
WHEN YOU ARE NOT AT ADAQ, WHAT DO YOU LIKE DOING?
The move to Australia was about chasing sunshine and achieving a better lifestyle for my family so, where better than the sunshine state. My weekends are spent exploring SEQ from morning markets and walking along the river to utilising our numerous annual passes.

We understand that a highly personalised service is what dental professionals need.
At BOQ Specialist, we offer a full range of finance products and services, tailored to your professional and personal needs no matter where you are in your career. With over 30 years of experience in dental finance, our focus is on building long-term relationships with our clients so that you can make financial decisions that are right for you.
Talk to your local finance specialist about our current offers and rates today on 1300 160 160 or visit boqspecialist.com.au