CPD Past, Present and Future
The cost of PI insurance non-compliance
Final year student? Find out what to do next
Every CPD hour counts.
What happens if you don’t reach the required 60 hours?

DENTAL SPRING 2021
PAGE
4
PAGE
8
PAGE
34
PAGE
10
EDITOR
Dr Matthew Nangle
EDITORIAL TEAM
A/Prof Alex Forrest
Dr Gary Smith
Ms Lisa Rusten
Ms Jane Nettleton
PRODUCTION
Published by the Australian Dental Association (Queensland Branch)
CONTACT
22-26 Hamilton Place
Bowen Hills Qld 4006
PO Box 611, Albion Qld 4010
Phone: 07 3252 9866
Email: adaq@adaq.com.au
Website: adaq.org.au
ADVERTISING KIT
Information on advertising, deadlines and artwork specifications are available in the ADAQ Advertising Kit: adaq.org.au/advertising
GRAPHIC DESIGN LEAD
Kristen Willis, Tondo Creative
COVER ART DESIGN & GRAPHIC DESIGN SUPPORT
Emerson Domingo Jr
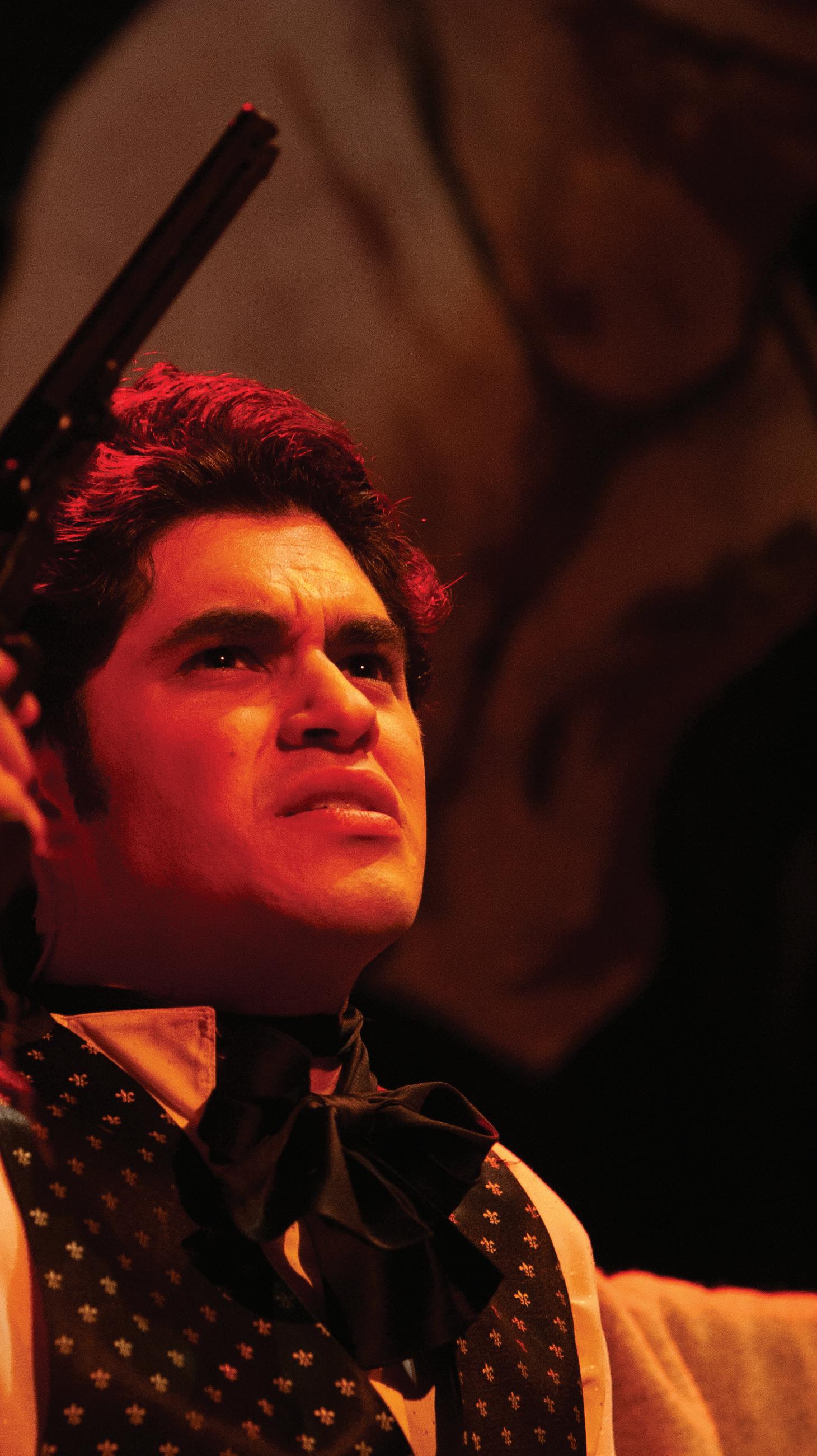
DISCLAIMER
ADAQ Dental Mirror is published for the information of Members only and is not for general distribution.
ADAQ COUNCILLORS
PRESIDENT
A/Prof Alex Forrest AO
SENIOR VICE PRESIDENT
Dr Matthew Nangle
JUNIOR VICE PRESIDENT
Dr Jay Hsing
COUNCILLORS
Dr Meglin Rathnasamy (Peninsula)
Dr Kelly Hennessy (Central)
Dr Kaye Kendall (Moreton)
Dr Sobia Zafar (Moreton)
Dr Gina Irwin (Western)
Dr David Le (Moreton)
Dr Graeme Westacott (Moreton)
Dr Tim Keys (Sunshine Coast)
FEDERAL COUNCILLORS
Dr Angie Nilsson Dr Martin Webb
IMMEDIATE PAST PRESIDENT
Dr Norah Ayad
ADAQ SUB-BRANCHES
Bundaberg Dr Paul Dever Mackay Dr Peter Monckton
Dr Joseph Nguyen (Burnett)
Dr Jay Hsing (Moreton)
Dr Keith Willis (Moreton)
Toowoomba Dr Rob Sivertsen
Ipswich Dr Andrew Wong Sunshine Coast Dr Peter Jorgensen Gold Coast Dr Gabriela Ciubuc-Batau
Kingaroy Dr Man Chun (Simon) Lee Gladstone Dr Patrick Dohring

Rockhampton Dr Kelly Hennessy
Cairns
Dr Brian James
ADAQ COMMITTEES
Dental Practice Committee
Convener: Dr Matthew Nangle
Dental History Preservation Committee
Convener: Dr Gary Smith
Oral Health Committee Convener: Dr Kaye Kendall
Conduct and Honours Committee
Convener: A/Prof Alex Forrest AO
Recent Graduates and Students Committee
Convener: Dr Malak Fouda
Volunteering in Dentistry Committee
Convener: Dr Jay Hsing
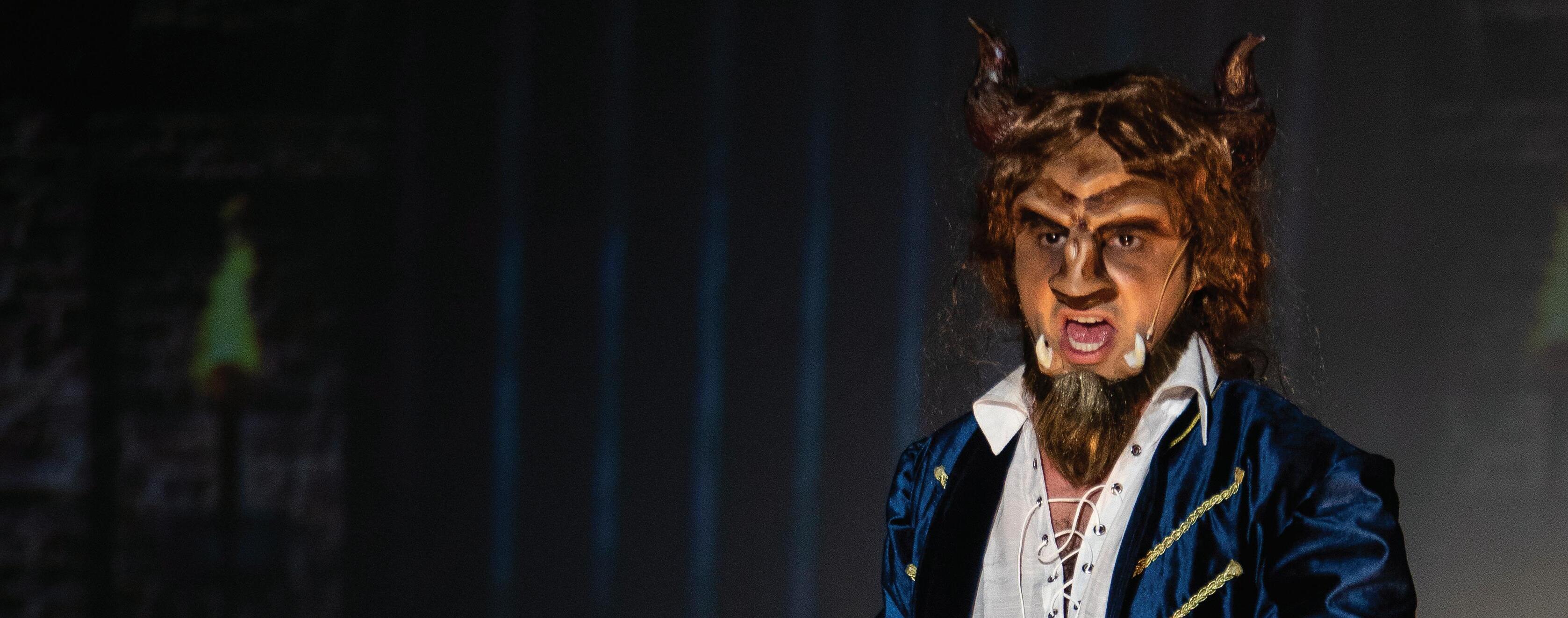
SPRING 2021 CONTENTS 04 FROM THE PRESIDENT CPD Past, Present and Future 07 CEO REPORT Council Elections 08 The cost of PI insurance noncompliance 10 CPD Non-compliance 12 The importance of up-to-date training registers 14 Digital Dentistry 20 History of dental education in Queensland 32 Q&A with the recent graduate and student dental panel 36 MEMBER SPOTLIGHT Prosthodontics, Performing, and Opening Packets
Copyright is reserved throughout. No part of this publication may be reproduced in part or whole without the written consent of the publisher. This publication is for the purpose of promoting matters of general interest to Members of the Association. The views expressed in this magazine do not necessarily reflect the views and policies of ADAQ or ADA. Publication of advertisements for products or services does not indicate endorsement by ADAQ. All material is positioned and published at the discretion of ADAQ.
FROM THE PRESIDENT CPD PAST, PRESENT AND FUTURE
A/PROF ALEX FORREST AO
ADAQ CPD is changing, you may have noticed this already over the last couple of years.
In 2019, we conducted a CPD survey and if you have read the regular CPD emails or attended a course, you will have seen that that our new offerings reflect the results of the survey.
Our CPD program is re-imagined with topics from Botulinum Toxin to orthodontics to TMJ. There are a range of courses specifically for recent graduates, OHTs and practice staff. This has been achieved under the shadow of the pandemic, in spite of the restrictions that it has caused. It reflects the commitment the new ADAQ brings to you – to be the best CPD provider in the nation. How has this come about, and where are we headed?
WHERE ARE WE HEADED?
Last year, ADAQ held its first strategic workshop during which Council considered that ADAQ’s previous Vision and Mission were no longer appropriate. We decided that ADAQ needed a rational and contemporaneous focus which should be reflected in our statements of purpose. Out of this workshop, our new Vision is “Supporting the dental profession and advancing the oral health of all Queenslanders” and our new Mission is “Working every day to be the preferred and trusted source of knowledge and information about oral health and clinical practice”. You can see that CPD becomes a major focus for ADAQ as opposed to simply being a service we provide, because it is a core part of our DNA. In keeping with our statements of purpose, we want to become the best CPD provider in Australia with topics that align to your needs. We are working towards making our CPD the best available, combining both theory and hands-on courses that do not promote equipment, materials or solutions offered by particular companies or suppliers.
ADAQ is independent, and aims to give you the best, unbiased information we can.
ADAQ is independent, and aims to give you the best, unbiased information we can, to align with our mission to become the preferred and trusted source. For this reason, we will conduct another CPD survey in 2021 and I encourage as many of you to participate in the survey as possible.
WHAT CPD CAN WE PROVIDE?
ADAQ is not a university. Other than being a Registered Training Organisation for Dental Assistants, we are not a front-line teaching institution and are not registered as such. We can’t therefore provide qualifications in the way that a university can. What we can offer is courses that allow you to update your current knowledge base and develop clinical skills in areas where you already have scope of practice. This informs the CPD that we provide to help you develop your clinical, administrative and interpersonal skills and keep up to date with progress in dentistry and its specialties.
WHAT HAS CHANGED?
Until recently the ADAQ CPD Committee’s role was to meet once a month to suggest new courses and monitor feedback from courses that has been delivered. A recurring CPD calendar existed, and new courses were slotted into vacant areas from





4 ADAQ DENTAL MIRROR SPRING 2021
year-to-year. In spite of rotation of its chair and membership, this model effectively stifled innovation because the calendar kept repeating previous courses and left relatively little room for new ones. It was obvious that change was needed.
In 2021, we introduced the CPD Advisory Panel. It is comprised of leading specialists, whose role is to vet and provide feedback to inform CPD proposals in their respective disciplines, and contribute jointly to review of multidisciplinary submissions. To translate the Advisory Panel’s advice into action, ADAQ recently appointed a full-time CPD Manager, Ms. Madonna McManus. Madonna is responsible for developing the CPD program and having a full-time person who has extensive experience within the dental industry devoted to CPD illustrates our commitment to excellence.
Since the pandemic, the CPD landscape has changed dramatically. The majority of education, regardless of the industry, is now conducted via webinars. ADAQ has been fortunate enough to run face-to-face events since August last year and we are noticing that the majority of Dentists are enjoying these events.
The challenge for us continues to be reaching our rural and remote practitioners and to combat this we will continue to offer as many courses as possible as in-person or via webinar and where possible, a range of CPD courses will be offered free-ofcharge for Members.
A new page on the ADAQ website offers a range of courses that you can complete at a time that works for you
ADAQ is introducing regular CPD events to be held on the same evening once each month between 6:30 pm and 8:00 pm. Look out for these, as they will be “bite sized” and topical. We continue to support and encourage you to attend special interest societies and study clubs.
Multi-stage courses have been introduced throughout 2021, we’ll continue to design courses to offer you information and techniques you can build on. Complex treatment often requires a multiple staged approach and we are adopting the same philosophy when it comes to building your skills, competence and knowledge in specific areas or within your career.
COUNCIL ELECTIONS ARE OPEN
MS LISA RUSTEN
ADAQ Council has spent much of the past two years working to improve the governance of the organisation, with a significant focus on the foundation document of the Association; the ADAQ Constitution.
The Constitution sets out the rules that govern the organisation and how it will operate. A fundamental part of the ADAQ Constitution is the election of Councillors who are Directors of the organisation and must meet the responsibilities of Directors as set out under the Corporations Act.
At the 2020 Annual General Meeting, Members supported key changes to the Constitution relating to the size of Council, and the terms of Councillors. These changes were important because a large Council can be unwieldy and become an impediment to robust decision making as factions within the Council can develop and those with the loudest voice can overwhelm the majority.
Ipswich City, Somerset Regional and Lockyer Valley Regional), there are now four positions available.
ADAQ has an ongoing commitment to provide not only lecture-based CPD, but also seminars and hands-on courses to practitioners outside of the South-East
A focus will be on supporting emerging specialists and introducing them to our audience. It will have a two-fold effect, where they can gain experience and visibility within the profession, and practitioners learn from those who are guaranteed to be at the leading edge of progress in their specialty and can report on new developments and techniques of interest.
corner.
ADAQ has an ongoing commitment to provide not only lecturebased CPD, but also seminars and hands-on courses to practitioners outside of the South-East corner.
ADAQ sub-branches will be instrumental in coordinating these courses and they will become ever more important in building opportunities for local Members in regional areas. The more active and vibrant the sub-branch, the greater the opportunity. A good example is the Cairns sub-branch which has partnered with ADAQ to run a conference in Cairns this September themed “Topics in the Tropics”. This is a wonderful opportunity for Members in the North to hear topics of interest and develop, share, and renew friendships.
WHAT’S NEW?
CPD is now being offered ‘On Demand’, a new page on the ADAQ website offers a range of courses that you can complete at a time that works for you. This program will continue to grow so keep checking back and see what’s available at www.adaq.org. au/ondemand. Federal ADA also holds regular online events which provide a national perspective on events and topics of importance.
In 2021, ADAQ became an accredited provider of CPD to the Royal Australian College of General Practitioners. This college has a well-developed quality assurance process which mirrors the one that ADAQ is developing. Our intent is to make sure that the CPD we offer meets or exceeds your expectations and adheres to strict quality guidelines, and this is a major focus as we move forward.
CONCLUSION
Our vision is to provide the CPD that meets the needs of the entire dental team along with other primary healthcare groups. Developing awareness of dental disease and dental care in these groups is fundamental to improving the oral health of Queenslanders.
We will know that we are achieving our goals when ADAQ becomes the first choice for your CPD needs and you don’t need to consider any other providers. We’re well on the way now, so watch this space!
Similarly, requiring all Councillors to stand for re-election at the same time risks the loss of corporate knowledge and continuity of the work of Council. While this change means that elections will now be an annual feature of the ADAQ calendar, it also means some continuity of the work of Council is preserved.
So, here we are at election time for Council once again but with some key changes;
• Instead of eight positions being available in Division 1 of Moreton (Brisbane City, Logan City, Moreton Bay, Redland City,
• Elections for Division 4 (Central – Rockhampton, Gladstone, Livingstone Shire, Mackay, Whitsunday, Banana Shire, Maranoa, Paroo Shire, Woorabinda Aboriginal Shire, Central Highlands Regional, Blackall, Barcaldine, Longreach, Boulia Shire and Isaac regional Council) and Division 8 (Gold Coast City and Scenic Rim) will not be held this year and will instead be held in 2022. The Councillors representing those areas, Dr Kelly Hennessy and Dr Norah Ayad, have agreed to continue on Council for an additional year and I would like to thank them for their commitment in agreeing to extend their current term so that the Constitutional change staggering the terms of elected Councillors can be achieved.
Nominations for Council representatives for Divisions 1,2,3,5,6 and 7 open on August 27. Nomination forms will be sent to all Members eligible to make nominations and vote and are also available on adaq.org.au/councilnominations

6 7 ADAQ DENTAL MIRROR
FROM THE CEO
WELL OVER $70,000!
THE COST OF PI INSURANCE NON-COMPLIANCE
Dental practitioners have failed to appreciate the significance of complying with their insurance obligations.
INTRODUCTION
We all know Professional Indemnity (PI) insurance is required to practice dentistry in Australia. However, what does this really mean? Do you have a full understanding of the consequences of failing to hold the appropriate and continuous professional indemnity coverage?
1 EXPENSIVE MISTAKE –CASE STUDY ONE
In late July of 2020, Dr Dent contacted ADAQ after receiving a complaint which included a claim for compensation from a former patient. The complaint related to treatment completed in 2018, which involved two simple extractions and subsequent implant treatment. Crowns were placed on top of the implants and no immediate complications were reported. The implants subsequently failed due to a late-stage rejection.
Upon investigation, it became apparent Dr Dent had forgotten to renew her PI insurance which expired at 4pm on 30 June 2020. This was despite having received her renewal notice, a follow-up SMS, and a final reminder email. Due to Dr Dent’s failure to renew her insurance, she/they did not have a current PI Policy in place at the time the claim was made. Dr Dent was therefore not insured for this claim – even though the incident occurred in 2018 and at that time the treatment was performed, Dr Dent held a valid insurance policy.
Dr Dent had not appreciated that PI insurance policies operate on a claims-made basis. This means a dentist MUST hold an insurance at the time the claim is made - not at the time the treatment occurred.
patient commenced a formal personal injuries claim (PIPA claim), claiming he suffered serious tissue damage, a serious gum injury and permanent localised numbness. The matter was finally settled for $50,000.
Dr Dent was required to pay not only the settlement sum, but also the incurred legal costs, which brought the total amount paid out to well over $70,000!
Had Dr Dent prioritised the renewal of her insurance policy prior to it lapsing, she could have avoided this stressful and unnecessary financial burden of being uninsured.
2 PUBLIC (HEALTH) ENEMY NUMBER ONE –CASE STUDY TWO
Dr Bite had worked in private practice for 5 years before moving to a public health role in a government organisation. He had previously held PI insurance through a private insurance company but decided not to renew because he had “heard” that his employer provided PI insurance for its employees and therefore, he incorrectly formed the view he did not need additional PI coverage.
In August 2020, a claim was made against Dr Bite regarding treatment he performed whilst in private practice in December 2018. Dr Bite’s government insurance did not cover him for the claim and he immediately contacted ADAQ to seek assistance.
Dr Bite was advised that whilst most government employers provide indemnity, this is generally limited to treatment performed in the course of their employment.
insurance with appropriate ‘retroactive cover’. Retroactive Cover provides coverage for claims arising out of treatment performed prior to the commencement date of a current insurance policy. Most PI insurance policies (including QBE’s policy, which can be purchased through ADAQ) will provide dentists with unlimited retroactive cover.
As Dr Bite did not have retroactive cover, he was in breach of the Dental Board Registration Standard
As Dr Bite did not have retroactive cover, he was in breach of the Dental Board Registration Standard, AND he was not insured for the claim that arose out of his prior private practice. With the assistance of ADAQ, Dr Bite was able to resolve the claim amicably with his former patient and he was not required to pay any money to settle the matter.
3 A MOMENTARY LAPSE IN JUDGEMENT –CASE STUDY THREE
The end of financial year is a crazy time and is often a whirlwind of sales, promotions, tax discussions, and more sales. As such, it is easy to lose track of time and miss the 30 June deadline for renewing your PI insurance.
Several years ago, Dr Tooth, an early-career ADAQ Member, forgot to renew her PI Insurance until late July. This meant she was uninsured for a 4 week period.
Ahpra and the national boards have a nationally-consistent audit methodology which they apply to ensure compliance with the mandatory registration standards.
The following year, Dr Tooth was the subject of an Ahpra practitioner audit. During this audit, Ahpra noted the 4 week lapse of insurance. An investigation was then commenced against Dr Tooth for her failure to notify the Dental Board of this lapse AND for making a false declaration on her annual Ahpra registration renewal regarding holding appropriate insurance for the previous year. ADAQ supported Dr Tooth through the investigation process by assisting her with her submission to explain her short lapse of insurance.
Luckily for this young dentist, with the assistance of ADAQ, she was able to adequately explain her mistake and was not subjected to any penalties.
CONCLUSION
The three case studies discussed above are examples of how not understanding professional indemnity insurance has led to serious problems.
This means a dentist MUST hold an insurance a t the time the claim is made - not at the time the treatment occurred.
Dr Dent had no insurance policy in place at the time the claim was made. In other words, she was uninsured.
In this case, ADAQ assisted Dr Dent to find appropriate legal representation to assist her response to the claim. Her former
Whilst most government employers provide indemnity, this is generally limited to treatment performed in the course of their employment.
And further, a government employer will often require employees to hold their own personal professional indemnity policy in addition to their government indemnity. Most importantly, an employer’s indemnity does not cover a dentist for treatment performed outside of their employment.
The Dental Board requirement is that a dentist MUST hold PI
Dr Tooth, an early-career ADAQ Member, forgot to renew her PI Insurance until late July. This meant she was uninsured for a 4 week period.
No claims arose during this period, and despite her oversight, Dr Tooth was given unlimited retroactive cover, which covered her for all claims (even during the period she was uninsured).
As the Dr Tooth was given unlimited retroactive cover, she thought her mistake had been fixed and did not dwell on the matter further.
However, the Dental Board’s registration standard for PI insurance requires a dentist to notify Ahpra within 7 days if they do not have appropriate PI insurance in place. Also, upon a dentist’s annual Ahpra registration renewal, they are required to declare they held for the previous year. As many practitioners are aware,
Not understanding professional indemnity insurance has led to serious problems.
These also demonstrate the importance of maintaining appropriate and continuing PI Insurance coverage – even when you are working in government or not practicing. All practitioners must keep in mind:
1. PI insurance in Australia operates on a claims-made basis. This means that you MUST hold an appropriate policy at the time a claim is made. Continuity of coverage is essential. If you are not working for a period due to sickness, family commitments or travel, you still must hold insurance to cover you for this period.
2. Where an employer provides PI insurance, the practitioner is still required to take out their own PI policies to ensure they have full retroactive coverage.
3. Having Professional Indemnity Insurance is a mandatory requirement of Ahpra registration and is actively enforced through Ahpra practitioner audits.
The ADAQ Compliance, Advice, and Policy team assists you in understanding your professional indemnity insurance options and obligations, including selecting a policy appropriate for your needs. ADAQ can also assist you to obtain run-off cover, when you decide to cease practice.
 LARISSA ALDERTON Senior Advisor - ADAQ Compliance, Advice and Policy
LARISSA ALDERTON Senior Advisor - ADAQ Compliance, Advice and Policy
8 9 ADAQ DENTAL MIRROR SPRING 2021
CPD: WHAT ARE MY REQUIREMENTS AND WHAT HAPPENS IF I DON’T COMPLY?
Dental practitioners are required to complete 60 hours of CPD activities over a 3-year period. The current CPD cycle extends from 1 December 2019 to 30 November 2022. A minimum of 48 hours (80%) must be spent on clinical or scientific-based CPD activities and a maximum of 12 hours (20%) can be contributed to non-scientific CPD activities. To assist practitioners in complying with this requirement, the Dental Board of Australia has issued a Registration Standard and Guidelines. However, it does not detail mandatory CPD activities to be undertaken. Instead, it recommends dental practitioners undertake a varied range of CPD activities that they feel are in line with their learning needs.
The obligations of registered health practitioners in relation to CPD requirement is set out in the National Law (section 128):
“(1) A registered health practitioner must undertake the continuing professional development required by an approved registration standard for the health profession in which the practitioner is registered.
(2) A contravention of subsection (1) by a registered health practitioner…may constitute behaviour for which health, conduct or performance action may be taken”.
At the annual Ahpra registration renewal, all dental practitioners must declare they have met the CPD Registration Standard. If audited, you must produce a logbook which includes details of the CPD activities undertaken, the number of hours spent, and whether the activity is clinically or scientifically based. The Board may also ask for evidence of your attendance (e.g. certificate of attendance).
CASE STUDY: WHAT HAPPENS WHEN I DON’T COMPLY?
Dr Anon was contacted by Ahpra as part of its usual audit process. He was requested to provide evidence that:
1. he held appropriate professional indemnity (PI) insurance, and
2. he had met his CPD requirements for the previous three-year cycle.
Upon review of Dr Anon’s documents, Ahpra noted he had failed to meet the required number of hours for CPD. This also meant he had provided a false declaration upon the annual renewal of his Ahpra registration.
Dr Anon was asked to explain his failure to comply. However, the Dental Board did not accept Dr Anon’s reasoning. As a result, conditions were imposed on Dr Anon’s registration. These were detailed on the public register and required him to complete the outstanding CPD hours over the next 12 months - in addition to his current CPD requirements.
If Dr Anon fails to meet these conditions, Ahpra may refuse to renew his registration, preventing him from practising dentistry.
OUTCOME
After receiving the conditions, Dr Anon contacted ADAQ for assistance. ADAQ supported Dr Anon in identifying appropriate CPD activities, as well as making contact with a suitable peer who could provide one-on-one education to him when required.
To ensure Dr Anon was aware of his obligations (and would not find himself in a similar position again), ADAQ directed Dr Anon to information regarding CPD requirements. Dr Anon also received assistance to remove his conditions once the required CPD were completed.
This example shows that failure to focus on completing CPD activities within the required timeframe can lead to serious consequences. ADAQ can assist practitioners to meet these requirements, including any practitioners returning to work after an absence, or commencing work during the CPD cycle.
LARISSA ALDERTON
Senior Advisor - ADAQ Compliance, Advice and Policy
IF YOU HAVE ANY QUESTIONS REGARDING CPD REQUIREMENTS OR ANY REGULATORY NOTIFICATIONS, PLEASE CONTACT THE ADAQ COMPLIANCE, ADVICE AND POLICY TEAM ON 07 3252 9866 OR AT ASSIST@ADAQ.COM.AU
UPCOMING EVENTS









10 11 ADAQ DENTAL MIRROR SPRING 2021 TMJ: Craniofacial Pain and Dysfunction 24 SEPTEMBER FIND OUT MORE Drug Interactions Dentists Must Know 22 OCTOBER FIND OUT MORE HR: Change and Challenges for Dental Practitioners 29 SEPTEMBER FIND OUT MORE Botulinum Toxin and Intraoral Dermal Fillers 23-24 OCTOBER FIND OUT MORE Understanding Numbers Benchmarking and Practice Improvement 13 OCTOBER FIND OUT MORE Practice Accreditation Quick Start Workshop 22 OCTOBER FIND OUT MORE Periodontal Maintenance - A Team Approach 10 NOVEMBER FIND OUT MORE Advance d Oral Surger y 12 NOVEMBER FIND OUT MORE Dis aster Victim Identification 12-13 NOVEMBER FIND OUT MORE In-Office Whitening 3 DECEMBER FIND OUT MORE
THE IMPORTANCE OF UP-TO-DATE TRAINING REGISTERS FOR ALL STAFF
Continuing Professional Development for staff is important for a practice to stay compliant, competent, and – most importantly –safe.
All staff training records should be wellorganised and kept on-site. Records should contain any certificates, training dates, and attendance registers that have been signed by staff. Regardless of the format (e.g. electronic or paper), they need to be easy to retrieve for all staff members, and contain the following information:
1. who received training on a specific topic, and
2. all the topics on which staff have been trained
Regular staff meetings should be scheduled to discuss any training requirements, as well as updates to practice policies and procedures. There should be a short summary record kept for all discussions.
NEW CLINICAL STAFF
Onboarding of new clinical staff will require an induction program and should include practical implementation of practice infection control measures and work health and safety measures.
Training for existing staff will be ongoing unless it is identified in a training analysis that dental staff require immediate updates.
EXTERNAL AUDITS
In the event a practice undergoes an external audit, training records for all staff will need to be produced to the auditors. Infection control training and updates contribute heavily to annual training, and this will be reflected in your practice’s Infection Control Management Plan training section. The document includes staff training requirements, expected outcomes and records to be kept. This is an important practice document that reinforces the training needs and should be added to the staff training records.
Training for staff should include but not limited to the following:
• General orientation to the physical environment of the practice, including clean and contaminated zones
• Radiation Safety Training
• Hand Hygiene procedures
• Confidentiality of patient information
• Management of body fluid exposures
• Practice expectations and recommendations for vaccination prior to commencing work
• Environmental hygiene
• Use of PPE including policy on wearing and cleaning uniforms
• Infection control incidents
• Reporting requirements for sharps injuries and workplace incidents
• Management of waste streams and hazardous substances
• First aid procedures
• Emergency procedures for fire and medical emergencies
• Instrument reprocessing processes –cleaning and sterilisation
• Surgical technique and preparation, including scrubbing, gowning, and gloving
CREATING A TRAINING PROGRAMME
Ensuring that staff are trained and supervised are key responsibilities of the practice management. They need to determine the staff qualifications, competencies, and experience – and ensure this is adequate to deliver safe performance of the various procedures. Competency-based training for dental staff is based on training individuals for the tasks they perform in their roles in the workplace.
Another important matter to consider is the type of training required. A training needs analysis (TNA) is a review of learning and development needs within a business or organisation.
It will identify:
• the standard of performance required in the job
• what people need to know to do their jobs
• what people need to do in their jobs
• how, when, where and by whom assessment will occur.
KEY CHANGES SUMMARY: ADA INFECTION PREVENTION & CONTROL GUIDELINES (4TH EDITION)
The ADA’s Infection Control Committee has taken into consideration the most recent published evidence and recommendations around Infection Prevention and Control, following the principles of assessing risk and adapting the required protective and preventive measures.
• Key compliance points have been introduced to outline critical points.
ADA Infection Prevention and Control Guidelines - 4th Edition
It will allow managers to plan training programmes that suit staff development needs. Importantly, a budget can be prepared and time can be allocated during clinical down time to conduct the training.
• An expansion of the section on risk-based precautions.
• An update to the section on PPE, including:
• Hypoallergenic gloves
• The need for side protection on glasses
Key changes summary
Staff annual performance reviews are a great opportunity to discuss and identify individual training needs, and then develop an action plan:
• what training is to be undertaken
• who provides the training and how
• Discusses how prescription lenses that are worn for vision correction can become a suitable form of protective eyewear when the lenses are inserted in frames designed to provide a suitable level of protection to the orbital region.
The ADA’s Infection Control Committee has taken into consideration the most recent published evidence and recommendations around Infection Prevention and Control, following the principles of assessing risk and adapting the required protective and preventive measures.
• how often and where this will occur and
• what sequence the training will follow.
• Protective clothing – Discusses concept of layering, so that street clothes worn underneath do not become contaminated with material from patient treatment.
• Barriers – Includes clarification around the role of the TGA Essential Principles and the manufacturer’s instructions.
• Key compliance points have been introduced to outline critical points.
• Reinforces the need to remove burs from handpieces, and tips from ultrasonic scalers.
THE 4TH EDITION INCORPORATES
INFORMATION FROM:
The CDNA 2018 Guidelines for the Management of Health Care Workers known to be Infected with Blood-Borne Viruses. Includes updated definitions for exposure prone procedures.
The May 2019 NHMRC Australian Guidelines for the Prevention and Control of Infection in Healthcare (including bare below the elbow, surgical hand hygiene, and updates to the national Hand Hygiene Initiative).
The latest versions of Australian Standards, including AS 4381:2015 Single-use face masks for use in health care (including the difference between level 1, 2 and 3 masks); and AS 2773:2019 Ultrasonic cleaners
A dental practice should encourage professional development and the growth of its staff. Establishing clear goals will help staff with development and direction to succeed and be an integral member of the team in your practice. Further, staff will also need to be rewarded and performance recognised.
• An expansion of the section on risk-based precautions.
• An update to the section on PPE, including:
- Hypoallergenic gloves
- The need for side protection on glasses
To help your practice keep track of staff training records, you can download our continuous professional development template at bit.ly/adaq-cpd-template.
Alternatively, if your practice has gone through practice accreditation, you will have training register templates available through the accreditation hub on the ADA website.
• Protective clothing – Discusses concept of layering, so that street clothes worn underneath do not become contaminated with material from patient treatment.
ADAQ TRAINING & PRACTICE CONSULTANCY TEAM
• Barriers – Includes clarification around the role of the TGA Essential Principles and the manufacturer’s instructions.
• Flags the need for following manufacturer’s instructions regarding sterilizing piezoelectric scalers.
• Describes zones and the distribution of splatter contamination. Flags the issues with aerosols remaining in the air.
• Discusses a more structured approach to environmental cleaning and having a schedule that picks up high touch surface.
• Describes zones and the distribution of splatter contamination. Flags the issues with aerosols remaining in the air.
• Discusses a more structured approach to environmental cleaning and having a schedule that picks up high touch surface.
- Discusses how prescription lenses that are worn for vision correction can become a suitable form of protective eyewear when the lenses are inserted in frames designed to provide a suitable level of protection to the orbital region.
• Dental unit waterlines: good practice to test water on a regular basis, e.g., 6 monthly or annually. No change in target level of 200 CFU/mL. When high counts are found, the waterlines will need to undergo additional shock or sanitising treatments.
• Dental unit waterlines: good practice to test water on a regular basis, e.g., 6 monthly or annually. No change in target level of 200 CFU/mL. When high counts are found, the waterlines will need to undergo additional shock or sanitising treatments.
• Gives clarifications on the use of single use items.
• Gives clarifications on the use of single use items.
• Discusses situations where the use of orthophthalaldehyde (OPA) may be appropriate.
• Provides expanded information on the use of washerdisinfectors, and soaking before cleaning, Discusses endotoxins in rinsing water.
• Discusses situations where the use of orthophthalaldehyde (OPA) may be appropriate.
• Permits the use of specifically designed silicone rubber rings to identify instruments or instrument cassettes, that do not impede cleaning or sterilisation.
• Reinforces the need to remove burs from handpieces, and tips from ultrasonic scalers.
• Flags the need for following manufacturer’s instructions regarding sterilizing piezoelectric scalers.
• Provides expanded information on the use of washer-disinfectors, and soaking before cleaning, Discusses endotoxins in rinsing water.
• Permits the use of specifically designed silicone rubber rings to identify instruments or instrument cassettes, that do not impede cleaning or sterilisation.

12 ADAQ DENTAL MIRROR
The information The Management known Borne definitions procedures. The Guidelines Control (including surgical the The Standards, Single-use care level 2773:2019
Download now at ADA.ORG.AU/INFECTION-CONTROL
DIGITAL DENTISTRY
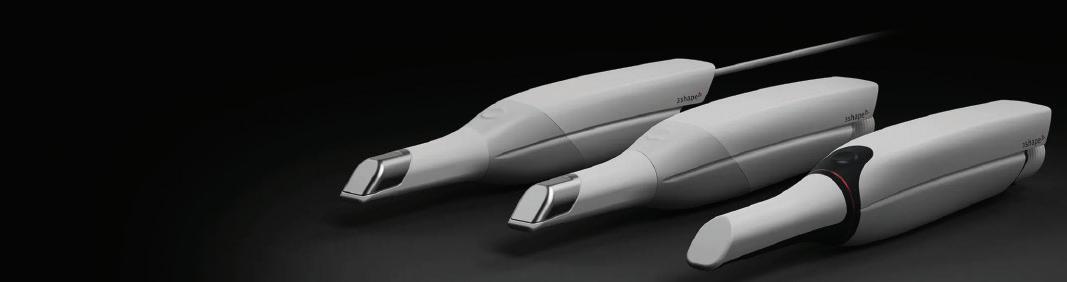
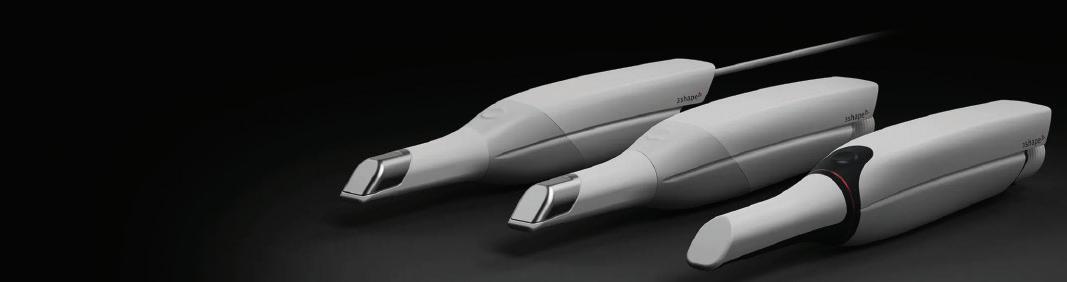
The advances of digital technologies in the field of clinical treatment planning and restorative dentistry have been significant. This has allowed many of the disciplines in these fields to be efficient, simplified, and predictable.
There is currently an explosion in the application of intra-oral scanning and additive manufacturing (3-D printing) in clinical dentistry. The dental market is showing that it will become the norm in every dental practice, in the manner similar to how rotary endodontics progressively replaced hand-file instrumentation in endodontics nearly 20 years ago! This is especially so as these technologies become more sophisticated, simplified and more importantly, affordable.
Digital impressions or optical scanning with the use of the intra-oral scanners (IOS) has enabled the acquisition of intraoral data or information with comparative levels of accuracy as conventional impression techniques.
The literature supports this accuracy of many different brands of intra oral scanners and has been shown to be similar to conventional impressions in cases of single unit restorations and fixed partial prostheses of up to 4 to 5 units.
The scanner, typically in the form of a small wand, projects a light source onto the oral structures to be scanned which is then captured or read by the imaging sensors within the IOS. The data is then processed by the scanning software, to create a virtual representation of the scanned structures.

Also, compared to traditional impression techniques, digital impressions derived from intra-oral scans have the following added advantages:
• Higher patient satisfaction and less patient discomfort as digital impressions do not involve the potential for the introduction of noxious stimuli common with conventional impression techniques
• Time-efficient – Scans can be achieved in 30 to 60 seconds with experienced operators
• Simplified Clinical Procedures – think of it like “Cut & Paste” or “Cropping digital photos” concepts
• Elimination of plaster casts – less consumables and reduced margin for further inaccuracies. Eg. Pour up problems.
• Better communication with patients – “Pictures spell a thousand words”
• Better communication with the dental technician and the interdisciplinary team
• Elimination of potential distortion of the impression material and inaccuracies of subsequent steps in the manufacturing process.
The continual development of digital technologies has also seen CAD-CAM technologies being implemented in many dental practices allowing the fabrication of indirect restorations such as crowns, inlays and onlays to be completed in a single visit. While CAD-CAM technologies such as the CEREC system has been present for many years, it is the ease of use, accuracy and reliability of the workflow that has allowed the widespread adoption of this digital system and workflow.

Another main advantage of the full digital workflow is the ability and the simplicity in accurately diagnosing and virtually planning the implant position using the digital scan and CBCT data. This in turn allows the manufacture of an accurate surgical implant guide to assist the clinician in the placement of implant fixtures under a fully guided surgical protocol, optimising the position and angulation of the fixture.

Direct light processing (DLP) and the SLA additive manufacturing technologies are currently the 2 most commonly utilised systems in restorative dentistry. Both the DLP and SLA technologies are very similar differing only in the light source. In this AM process, liquid photopolymer is exposed to light from a laser in an SLA printer or a projector in the DLP printer. The exposure results in the setting of the exposed liquid polymer, with the movement of the building platform exposing the subsequent layer of the liquid polymer to light. The additive process is repeated until the 3D object or model is built to reveal a solidified model.
The accuracy of AM is an accumulation of the several factors including; the accuracy of acquisition method, the parameters specified in the design software and the Computer Aided Manufacturing (CAM). 3D printing today, is routinely utilised in many aspects of restorative dentistry. Examples include the fabrication of surgical guides, custom trays, diagnostic models and occlusal splints.
Full digital workflows in implant treatment planning and surgical workflows in short has the following benefits:
1. Reduces the number of patient visits for the procedure
2. Provides for a simplified and predictable workflow in implant treatment planning and guided surgery
3. Provides better angulation and accuracy of placement of single and multiple implants
4. Provides confidence and increases the scope of flapless and immediate surgical implant placements
5. Increases the ability for better implant planning with the focus on a combine restorative and soft tissue driven approach in implant therapy
6. The prosthetic design process is much simpler and easier. Computer-aided manufacturing (CAM) is mainly based on two types, subtractive technologies (milling) and additive manufacturing (printing) technologies. While the use of milling technologies has been established, one of the areas in digital dentistry where significant advancements have occurred in recent times is in the field of additive manufacturing (AM) technologies or 3D printing. AM technologies have improved the connection in the digital workflow between the intraoral scanning acquisition and manufacturing processes in restorative dentistry.
Significant advancements in the AM technologies and material science have also allowed the for development of numerous restorative protocols including the fabrication of provisional indirect restorations, full arch provisional implant retained prosthesis and digital removable dentures. The continued development of digital technology in the field of additive manufacturing will inevitably occur in the near future allowing for many dental applications to be produced in-house in an affordable, efficient and simplified manner.
DR ANTHONY MAK & DR ANDREW CHIO




14 15 ADAQ DENTAL MIRROR
Figure 1. Intra-oral Scanner (image courtesy of 3Shape)
Figure 1(ii) Intra-oral Scanning
Figure 2. Cerec CAD-CAM System. (Image courtesy of Dentsply-Sirona)
Figure 3. Digital Implant Treatment Planning.
Figure 4. 3D Printed Full Arch Implant Retained Provisional Prosthesis
Printed Surgical Guide
3D Printed
Splint
Figure 5 (i). 3D
Figure 5 (ii).
Occlusal
(Image courtesy of Formlabs)
V SCAN TO LEARN MORE HEAR MORE ABOUT THIS TOPIC AT CLINIC DAY


CPD ON DEMAND
Dentists and Dental Professionals can now undertake CPD via ADAQ’s new on-demand courses

ADAQ’s CPD is transforming, over the past 12 months we’ve been working hard to deliver contemporary CPD courses for practitioners. We understand the time constraints that face busy oral health care professionals, so to assist in meeting the various needs of practitioners, ADAQ has developed online learning courses which can be accessed via the ADAQ website.
ADAQ’s new online CPD courses are designed to be a lifeline for busy dental professionals who want an easy, personalised way to undertake professional development that broadens their knowledge and skills while satisfying their registration requirements.
ONLINE LEARNING IN AUSTRALIA.
Online education in Australia has experienced a steady growth rate of 4.5% over the last 5 years. With continued advancements in technology and a widespread realisation of the efficiencies of web-based interactions, online learning is predicted to grow exponentially in the next 5 years.
ADAQ’s CPD courses are presented via the online learning platform, CANVAS. This platform allows the course creators to design and deliver relevant CPD courses that are evidence-based, personalised, interactive, and most importantly, relevant to the needs of practising dental professionals.
THE BENEFITS OF ONLINE LEARNING Accessibility
A 2020 study by the Australian Government’s Tertiary Education Quality and Standards Agency explored the experience of those undertaking online learning and professional development in Australia. The research found that the most identified positive aspect was the accessibility of online education.
Undertaking CPD online carries the benefit of being able to interact with the course material at any time. Online learners can
study at a time that suits their work and family schedules. For dentists and dental professionals, this means not having to take time away from providing patient care and not missing out on any family or recreation time. Gone are the days of running late for a face-to-face development course.
On-demand
ADAQ’s online CPD courses can be commenced at any time. There is no time travelling or waiting for a course to begin. Dental professionals can enrol and commence their CPD whenever the time is right.
Self-paced
Online professional development is perfect for those learners who wish to go slower and do small amounts when they can. There are no set timeframes for the courses and the pacing of each course is completely up to the participant.
Personal and professional excellence
The Dental Board of Australia directs registered professionals to undertake CPD that is relevant to learning needs and patient care. ADAQ is acutely aware of the CPD needs of dental professionals and works to provide online learning opportunities that apply to the realities of the profession. The courses are also designed with two priorities in mind:
1. To scaffold each learner to progress in terms of professional competency.
2. To strengthen each learner’s personal attributes that can be useful in a professional setting.
In addition to this, the courses designed by ADAQ on the CANVAS platform are structured in a way to allow each participant to demonstrate a deep understanding of the concepts being explored, and for some courses, feedback is offered to support this development.
A bright future
Online learning is an increasingly significant part of the future of education and career development. The good news is, with advancements in technology in terms of how online learning can be delivered and how it can be experienced, it has never been simpler to log on and learn. Even the most hesitant learners can find their way to online achievement. The on-demand CPD provided by ADAQ is an easy, user-friendly way to develop professionally in line with current industry best practices and provide the best patient care; And patient care is the ultimate goal of continuing professional development.
REFERENCES
1. Dental Board of Australia, Guidelines: Continuing Professional Development
2. Tertiary Education Quality and Standards Agency: Foundations for good practice: The student experience of online learning in Australian higher education during the COVID-19 pandemic


26 Nov 2021
Digital Dentistry
ADAQ’s flagship in-person eventthe networking opportunity of the year.
ADAQ.ORG.AU/CLINICDAY BRISBANE

Digital Dentistry in the General Practice
DR ANTHONY MAK

Aesthetics and Digital Dentistry
DR MICHAEL LEWIS

Clear Aligners
DR TONY WEIR

Innovation of Cone Beam and CT Imaging
DR RAAHIB DUDHIA
AND
16 ADAQ DENTAL MIRROR
SCAN TO LEARN MORE
MARK YOUR DIARIES Clinic Day is back in 2021
MORE SPEAKERS & TOPICS!
ADAQ EVENTS GALLERY
ADAQ AND BOQ BURSARY FILMING

ADAQ VOLUNTEER SURGERY DAY



ANXIETY CONTROL IN DENTISTRY





INTRO TO ORAL SURGERY





IMPLANT TREATMENT PLANNING


REAL WORLD ORTHODONTICS






RECENT DEVELOPMENT IN INFECTION CONTROL




18 19 ADAQ DENTAL MIRROR
HISTORY OF DENTAL EDUCATION IN QUEENSLAND
A brief retrospective on 100 years of dental education in Queensland.
A TECHNICAL PURSUIT
Dentistry shaped itself as a distinct profession in the late nineteenth century, however it was still viewed as a technical pursuit rather than a natural science and it would be for the early decades of the twentieth. This is understandable: operative and prosthetic dentistry constituted the bulk of expertise required to set up practice.
In the Jubilee History of Queensland publications of 1889 and 1910, dentistry is still listed in the manufacturing industries section, among mining and printing. Who would have thought that almost 150 years later, dentists would do actual printing, although in 3D machines!
Throughout all the Australian colonies technical education […] is made part of the educational policy of the respective governments […]
Numerous classes have been formed in mathematics, engineering, mining, assaying, analysis, chemistry, farming, dentistry photography, engraving, printing in all its departments, agriculture, etc. (p.343, Jubilee History of Qld 1889.)
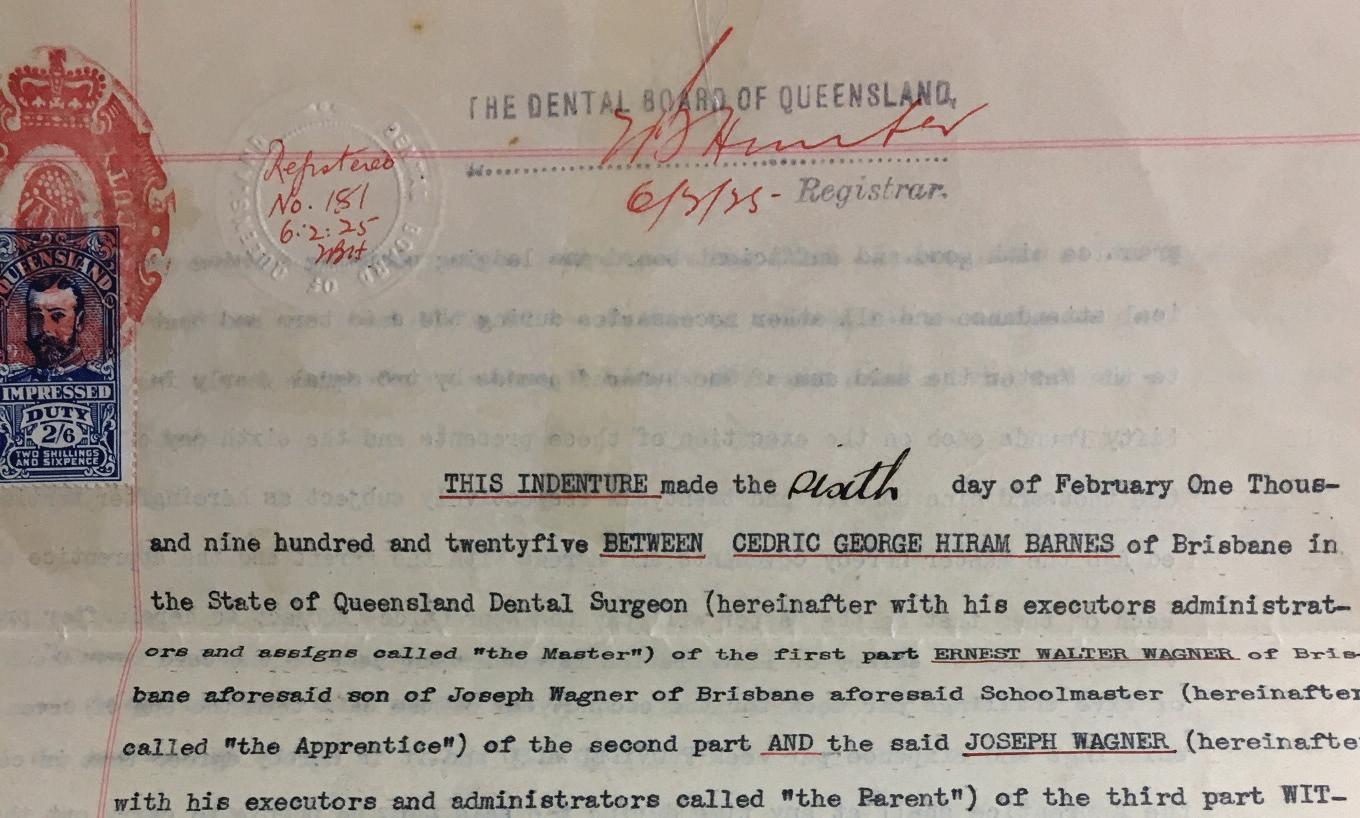
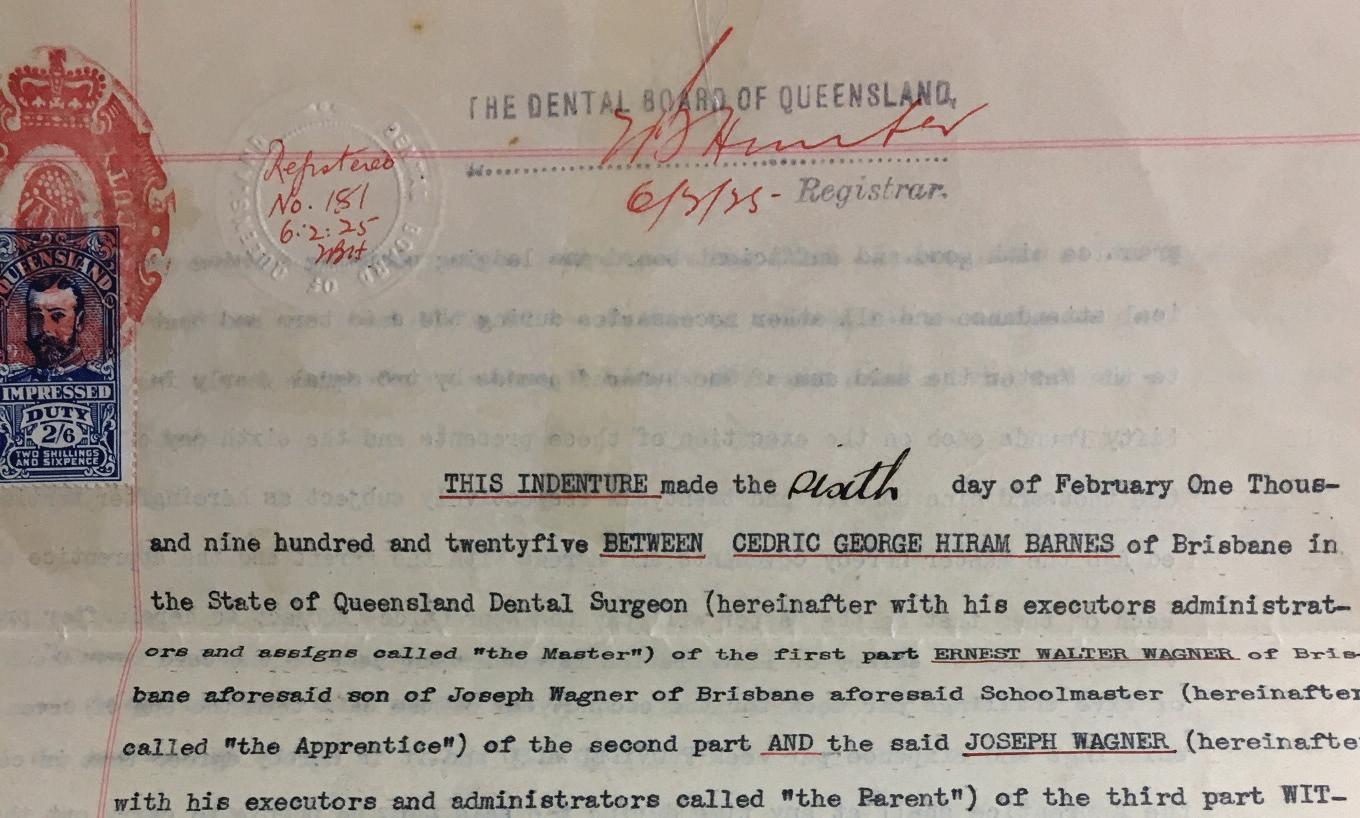
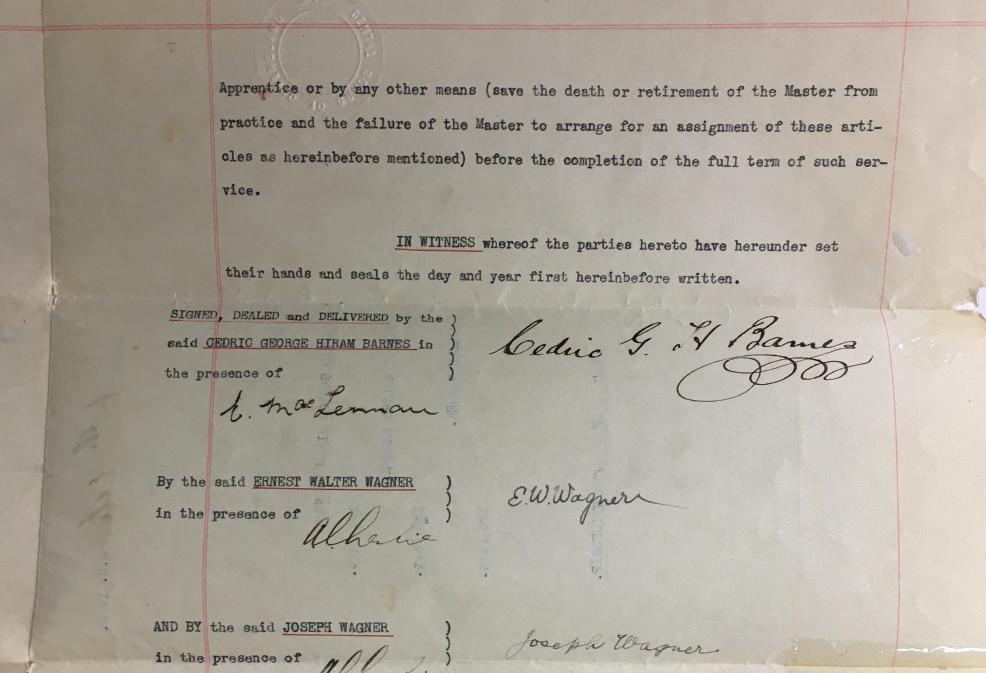
INDENTURES …FOR MAKING DENTURES!
The first formally trained dentists to set up practice in Queensland had completed their apprenticeships in Britain or the United States, where dental schools had already been established. Many were members of the Royal College of Surgeons (LDS –Licentiate of Dental Surgery).
They had enormous influence in the development of dentistry and dental schools in Queensland. For example, David R Eden, first President of the Odontological Society of Queensland, after setting up practice in Brisbane, in 1866, was master to many dentists who later became respected names in the state’s dental education and professional associations.
With modern eyes, the apprenticeship system can be easily seen as an elitist and inefficient institution that impaired the free circulation of knowledge and new techniques. However, as Bishop et al. pointed out in their 2002 paper on the development of professional ethics in dentistry: The scheme […] had a positive influence on the morality, legal identity, and professional allegiance of dentists during the ethical development of their profession in the nineteenth century.
The standard wording from surviving indentures held by the British Dental Association’s archives, reveals how the Master was expected to cultivate his pupil’s morals and social manners:
….at cards, dice or any other unlawful game he shall not play… He shall not haunt ale houses, taverns, play houses, or any other places of debauchery…
(Indenture LDBDA 1868, 06.7, cited in Bishop et al., 2002)
The curriculum was at the discretion of the Master, and only he decided whether the apprentice had reached sufficient skills to
practice on his own. However, a professional esprit du corps was evidently fostered over the generations. It matured starting late 1800s into the creation of professional associations worldwide, and later, into the structured education and practical tuition in tertiary schools.
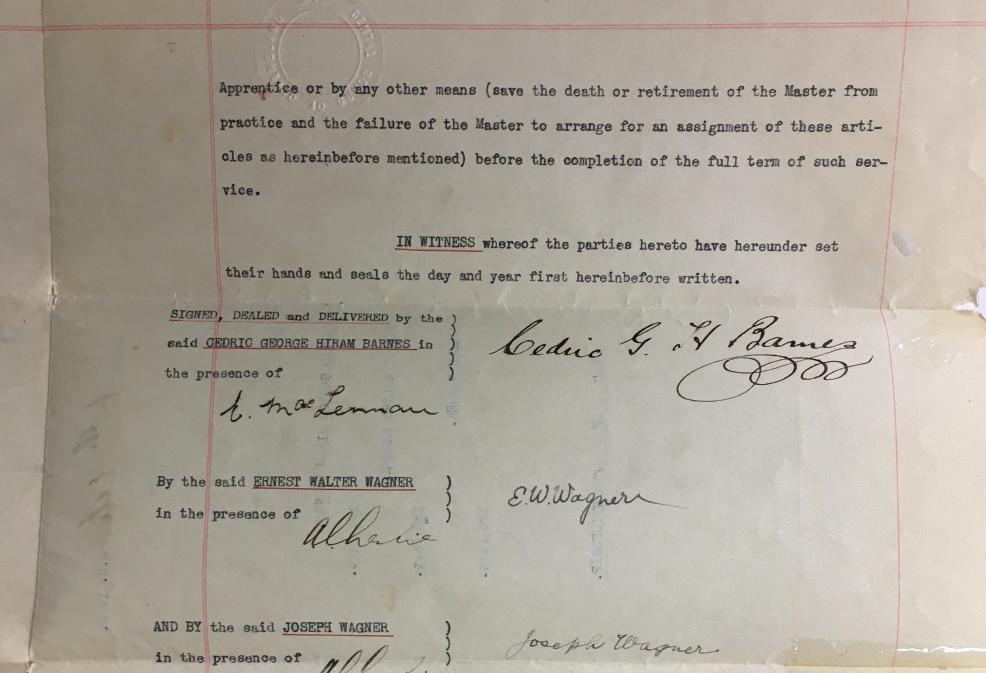
ADAQ holds a much later Deed of Apprenticeship, signed in 1925 for two years training required at the time. It documents the gradual change from the four-year apprenticeship system to a university qualification, with many students passing through a mixture of apprenticeship and service at an approved Dental Hospital or school to acquire ‘professional knowledge’.
DENTAL SCHOOL

Image 4.
The Brisbane Dental Hospital on George Street, 1917. State Library of Queensland.
Dentistry subjects listed for 1925 included Osteology, Dental Metallurgy, Practical Anatomy demo (Year 1); Radiography, Bacteriology, Orthodontia, Crown & Bridge and Cleft Palate Work, Office Management (Year 2):
Images 1 & 2 Wagner’s indenture document. 1925. ADAQ archives.
Queensland stood out among the other Australian states in that a course of study in dentistry was established before medicine, and not within the medical school as in most universities at the time.
The first university in Queensland was established in 1909. A faculty dedicated to dentistry was established in 1935 (Lumb, 1950). Before 1935, trainees went to Sydney for the medical subjects, Chemistry, Botany and Zoology. Two years of practical work followed this formal tuition.
The Brisbane Dental Hospital, established by the Odontological Society in 1908 initially for those who could not afford private treatment, introduced apprentices who completed their two-year practice there. In 1914 it was recognised as a teaching institution. Students in the final two years were assisted by dentist demonstrators on a rotating system.
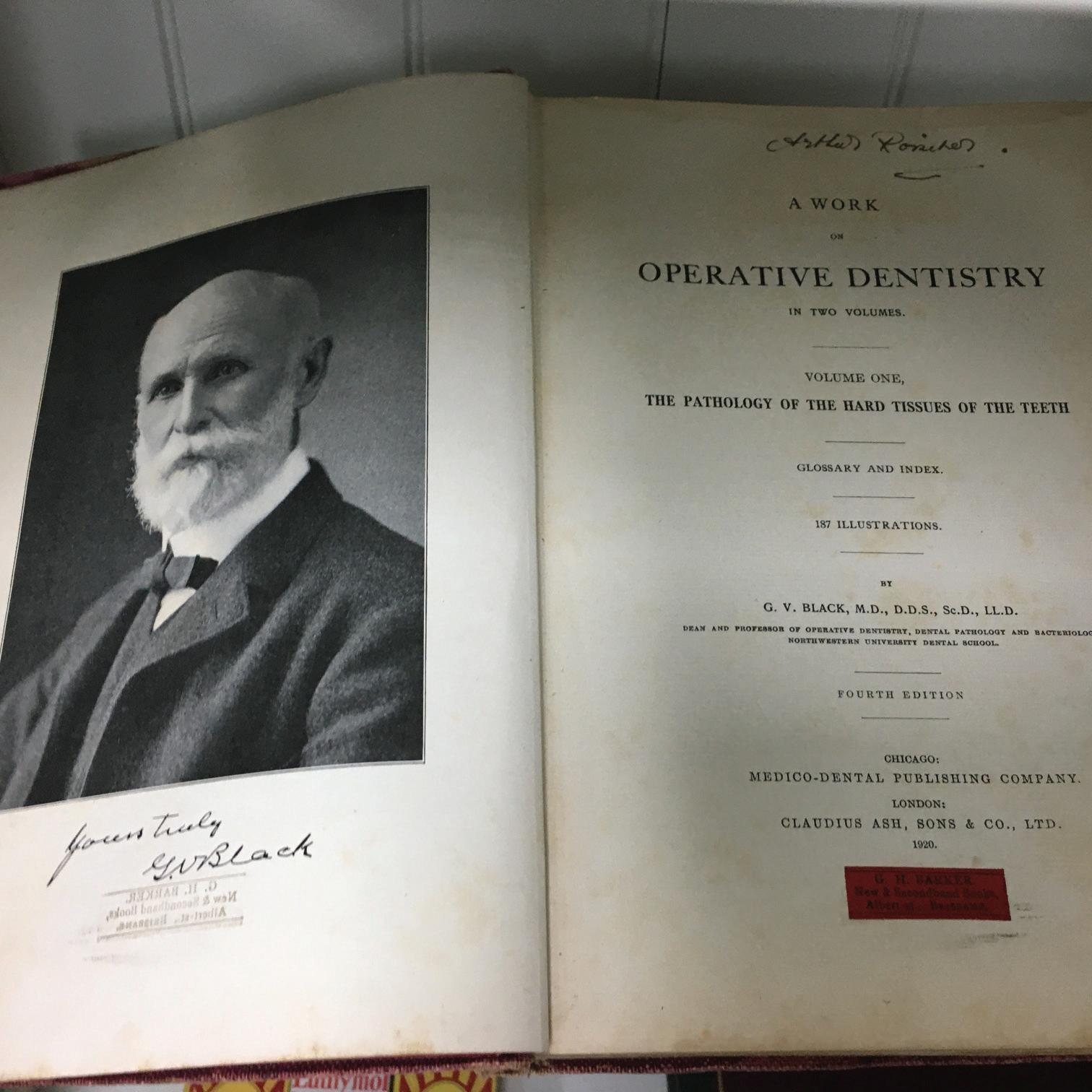
Image 5.
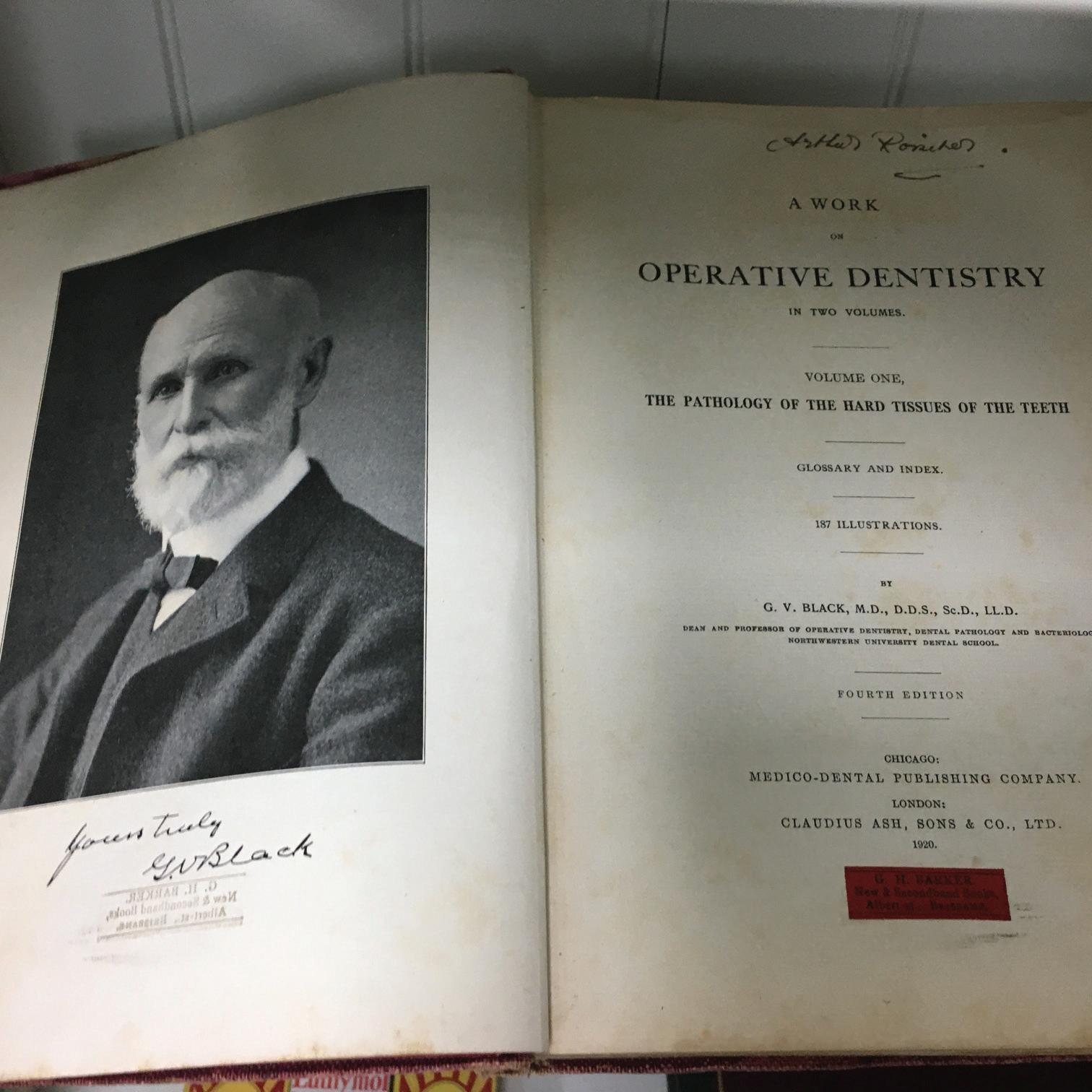
GV Black’s Operative Dentistry, 1920. The two volumes by Black were printed with yours truly and Black’s signature. ADAQ MoD. Black’s caries classification has haunted students for over 100 years
In 1926, the private apprenticeship system was entirely abolished: students would attend the College of Dentistry for the full four years and the Dental Board only dealt with registrations. The focus on technical and mechanical skills remained. In 1933, Year III students were required to perform: 18 dentures, 230 amalgam operative dentistry and 30 gold inlays, and 40 cases of periodontics (Marlay, 1979).
However, an educational shift from craftsmanship towards theory and science soon followed, and defined the second half of the twentieth century, as well as the introduction of specialist registration.
In 1962, there were 696 dentists registered in Qld, of whom 42 were also registered as specialists. (1962 Calendar of the Dental Board of Qld, ADAQ Archives).

Image 6. Gold inlay student demo on plaster, 1950s. ADAQ MoD. Students had to demonstrate their achievements in restorative dentistry.
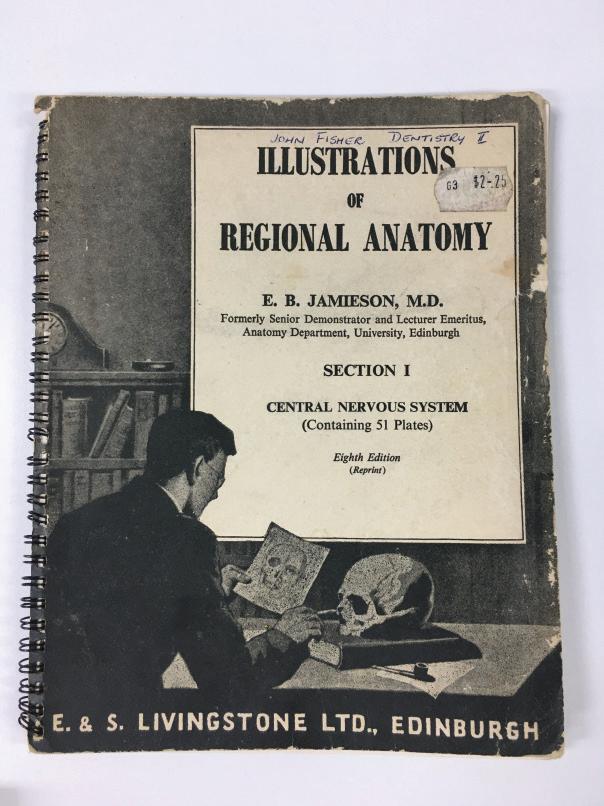
Image 7. Cover of Illustrations of Regional Anatomy textbook, 1956. ADAQ Archives.
Between 1936 and 1972, dental studies changed, with greater flexibility in clinical subjects (Zoology, no longer) and: increased emphasis on basic sciences and on preventive/community dentistry, and a decreased emphasis of (…) exodontics and prosthetic dentistry (Kruger, 1976).
MILLENNIAL DENTIST
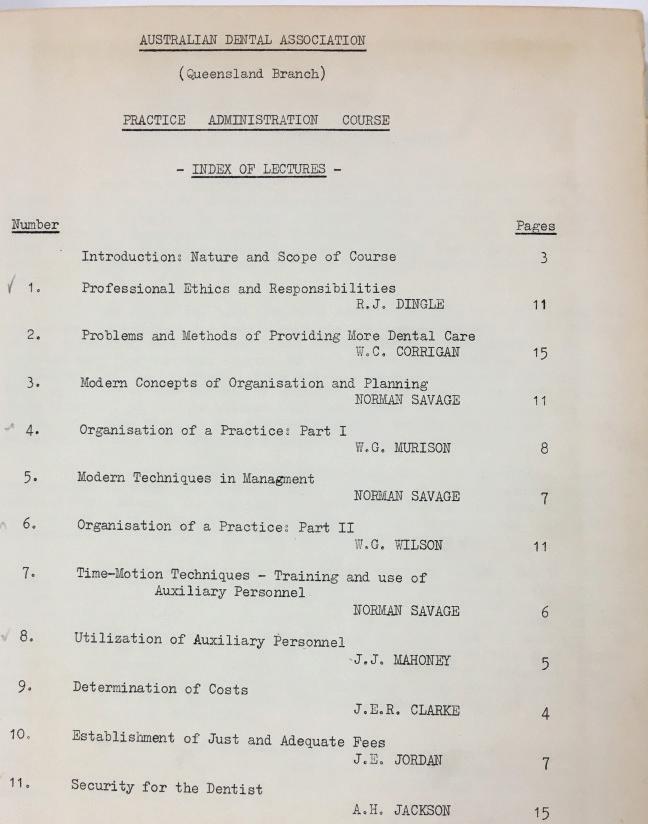
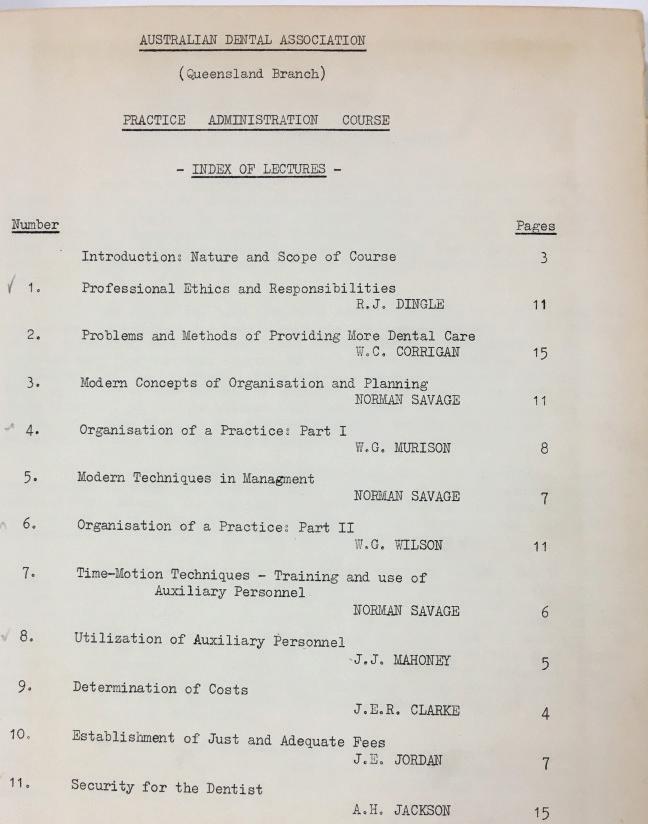
Image 9. ADAQ’s Practice administration course – contents page, 1950s. One of the ways the association helped new dentists be a success.
In 1985, in his address for the Golden Jubilee of the Dental Faculty, UQ Professor KF Adkins anticipated, somewhat prophetically, that, at the turn of the new millennium, dental students would be increasingly “accustomed to accessing
20 21 ADAQ DENTAL MIRROR
information via the video systems and programmes of computer assisted learning”. New dentists would be well trained in “the social and behavioural as well as the biological factors”; they’d study more oral medicine and less restorative dentistry.
In his predictions, however, he did miss some important developments, namely the post-1980s rise in the number of female and culturally diverse dentistry students.
TO BE TOOTH CARPENTERS: THE LIFE OF DENTISTRY STUDENTS
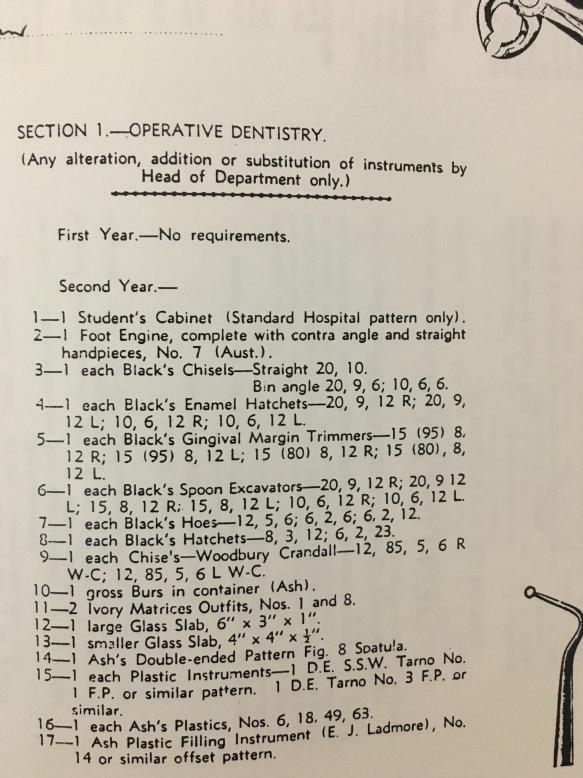

Image 11 & 12.
Image 10.
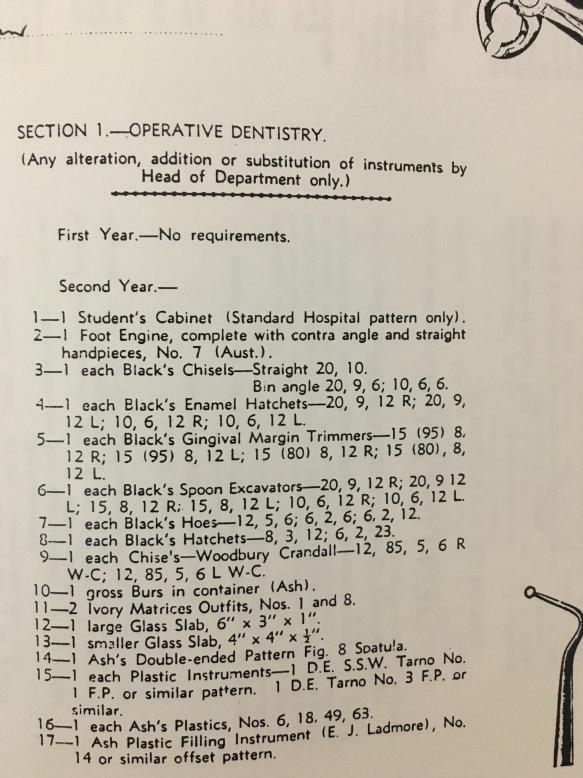
List of instruments required for operative dentistry, final years of Bachelor of Dental Science,1947-50. Source: Pearn, 1999.

Dr Porter’s student cabinet, and particular of makeshift aspirator built with his mother’s perfume bottle. Students had to purchase all their equipment needed for operative dentistry in their first or second year, which was very expensive for some. It was customary to engrave your name in each single hand instrument to discourage theft. ADAQ MoD.
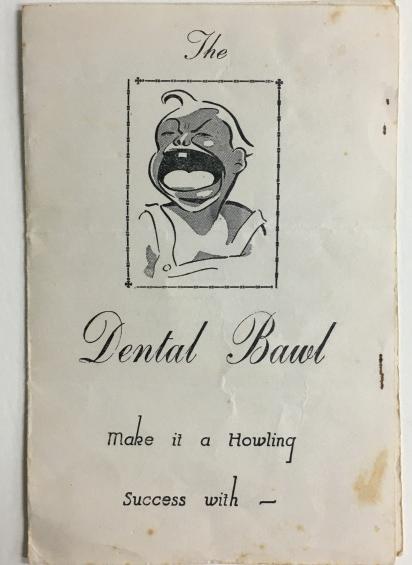
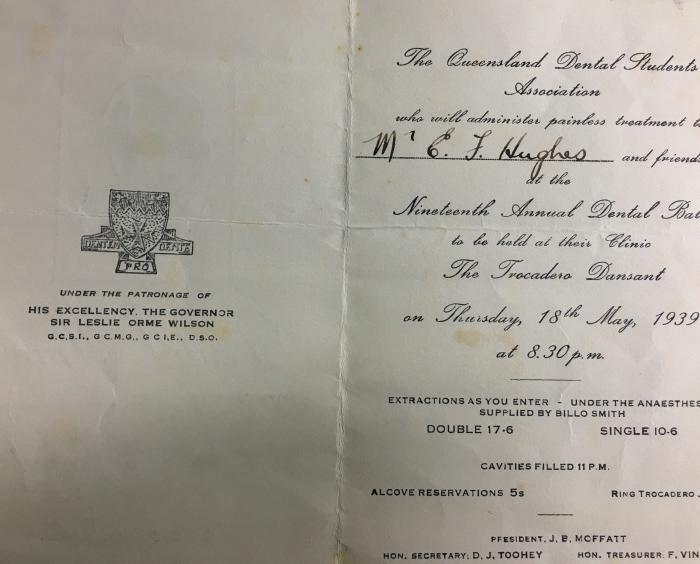
Image 13 & 14.
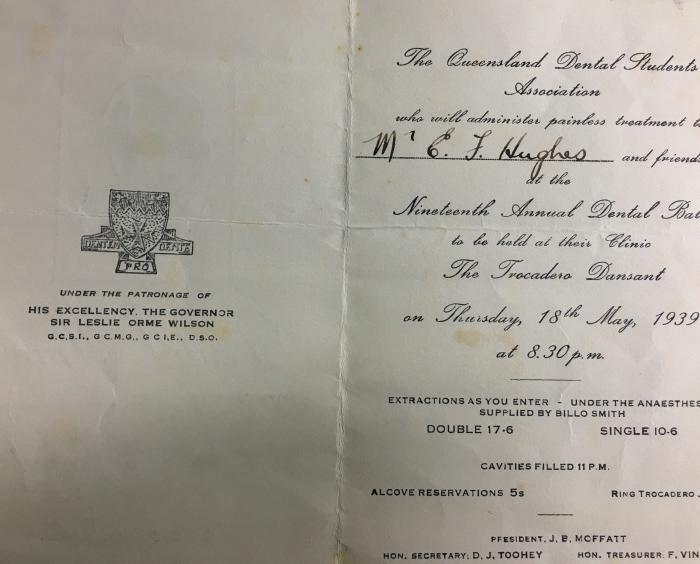
Invite to the Dental Bawl, UQ, 1939. ADAQ Archives. Classic dental humour by the Dental Students’ Association.

15.
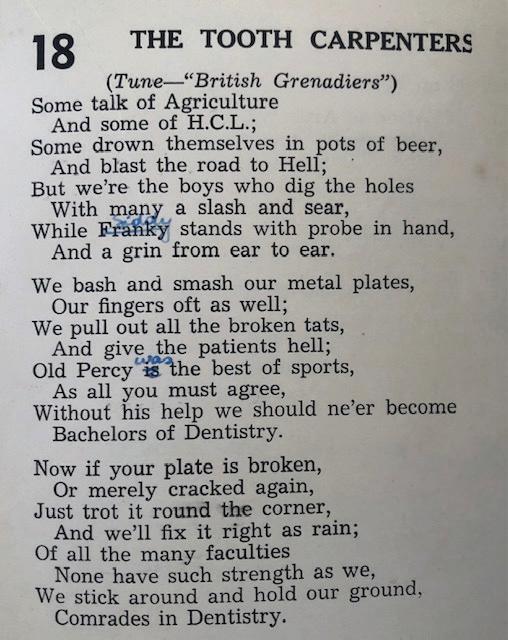
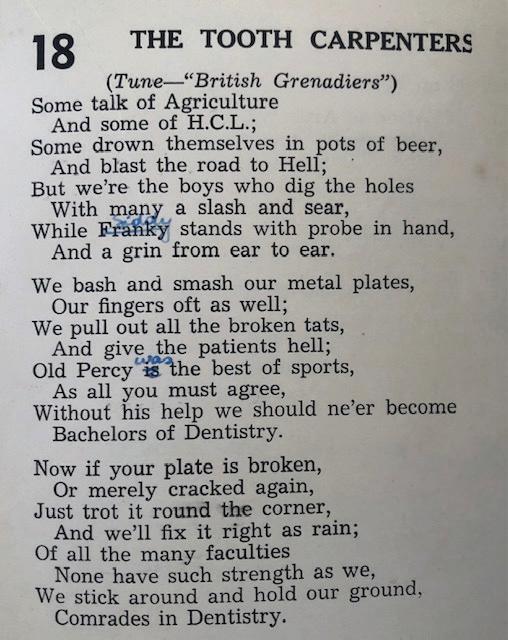
Image 16.
The Tooth Carpenters poem. Commem. Song Book, 1946. Author unknown. Courtesy of Rob McCray.

Image 17.
The Matrix Band, featuring a future Dental History committee chair and Dr Glen Croft…1979. Courtesy of Gary Smith
KEEN TO RECORD YOUR STORY AS A DENTIST IN QUEENSLAND FOR POSTERITY? GET IN CONTACT WITH THE ADAQ DENTAL HISTORY COMMITTEE: ADAQ@ADAQ.COM.AU
Continue reading about the history of dental education in Queensland (including a bibliog raphy):
ADAQ.ORG.AU/MUSEUM

22 ADAQ DENTAL MIRROR
Image
Queensland College of Dentistry, final students – 1933. Poulsen, Brisbane. ADAQ Archives.
MEDICAL EMERGENCIES AROUND ORAL PIERCINGS
The prevalence of oral piercings amongst younger individuals around the world is increasing each year. There is a lack of knowledge amongst both the public, as well as dental professionals, concerning many of the complications of oral piercings that can lead to medical emergencies.
P PATIENT/POPULATION/ PROBLEM
Dental professionals underpinning knowledge of complications and medical emergencies because of oral piercings
I INTERVENTIONS Education
C COMPARISON Knowledge
O OUTCOMES Dental Professionals improved confidence and better equipped to discuss oral piercings with patients
Dental professionals often miss key behaviours, knowledge, and attitudes toward oral health that pertain to oral piercings, It is important that such key information is given to patients who display such body modifications (King et al., 2018). A survey of oral health professionals revealed that only 24.5% felt confident in providing advice to patients on the adverse effects of oral piercings and their potential medical complications to patients. Some 52.8% felt that they needed written advice themselves to better inform their views and to address their lack of confidence on this topic.
Oral piercings have been identified as a new challenge in dentistry, their prevalence in young people can be as high as 12% (Samoilenko et al., 2019). Of body modifications that can be done, tongue piercings is the second most likely to produce medical complications, closely followed by lip piercings. Only navel piercings have higher complication rates. There are documented cases of teenagers who have died from septicaemia after oral piercings. A US-based study of some 3,494-oral piercing-related emergencies that occurred across 100 hospital emergency departments noted that 73% of patients were between the ages of 14 and 23 (King et al., 2018).
The severity of complications after oral piercing ranges from minor local complications (pain, swelling, and bleeding) through to life threatening conditions such as Ludwig’s angina, infectious endocarditis and brain abscesses (Samoilenko et al., 2019). There are long term risks from allergic reactions to metals, in the form of allergic contact dermatitis, especially from nickel or cobalt components of alloys used in piercings. While the alloys
used for oral piercings should be biologically inert, nonreactive, and compatible with human tissue (Domingo et al., 2019), this is often not the case. Metal ion particles can leach into the local environment from piercings. Corrosion and degradation of the piercing over time can drive local inflammatory responses, that add to those caused by microbial biofilms that grow on the metallic surfaces.
Lesions of the oral mucosa have been found at the sites of piercing, even in teenagers. Particles of aluminium and tin have been found within immune surveillance cells, which otherwise are tasked with detection of bacteria and other harmful organisms (Domingo et al., 2019). Local inflammatory changes can include scarring and hypertrophy. This is worse when the piercing is of poor quality.
Other major known risks of piercings include damage to teeth from trauma and abrasion. Tooth movement can also be caused.
There are many risks from improper maintenance of oral piercings. Frequent cleaning of the piercing and review of the site by both the patient and their oral health professional is important for early detection of complications. The periodic reviews should be alert for problems such as tooth wear, fractures, tooth displacement, gingival recession, and plaque deposits on the surface of the piercing. Each review should identify patient oral behaviours, as well as piercing cleaning and hygiene practices. Recordings should be made of habits developed because of the piercing.
Published data indicates that gingival recession and elevated dental caries risk are common in those with oral piercings. A comprehensive assessment of dental behaviour and oral status in 50 patients with tongue piercing versus 50 aged-matched controls found that those with tongue piercings had a worse oral status, with higher DMF scores and more recession (Ziebolz et al., 2019) (Table 1).
Risks of oral piercing are summarized in Tables 2 and 3, both of which are taken from Walsh (2008).
TABLE 1. WORSE DENTAL AND PERIODONTAL FINDINGS FOR 50 PATIENTS WITH PIERCING VERSUS CONTROLS
ORAL HEALTH PARAMETERS PIERCING CONTROLS P VALUE
DMF-T score 11.3 ± 6.5 7.6 ± 6.0 p < 0.01
Decayed teeth 1.4 ± 2.6 0.3 ± 0.9 p < 0.01
Missing teeth 1.4 ± 2.5 0.3 ± 0.8 p < 0.01
Suclus bleeding index 33.0 ± 33.0 14.7 ± 14.0 p < 0.01
Teeth with PPD ≥ 4 mm 29% 7% p < 0.01
BOP in % (mv ± sd) 24.57 ± 4.70 8.82 ± 3.07 p < 0.01
Mandibular lingual recession 0.4 ± 1.0 0.0 ± 0.2 p < 0.01
Enamel cracks 1.7 ± 2.3 0.6 ± 1.0 p < 0.01
Non-carious tooth defects
Abrasion 2.3 ± 2.4 0.1 ± 0.3 p < 0.01
Values are means and standard deviations. Adapted from Ziebolz et al. 2019.
COMMON ACUTE PROBLEMS WITH INTRA-ORAL PIERCINGS
• Pain
• Prolonged bleeding from damage to major vessels
• Tissue trauma and swelling
• Nerve injury, leading to paraesthesia
• Acute local infection
• Speech impediment
• Hypersalivation and drooling
• Taste impairment (From Walsh 2008)
LONG TERM COMPLICATIONS OF INTRA-ORAL PIERCING
• Aspiration or swallowing of the ornament
• Impairment of normal oral hygiene measures
• Obstruction of dental radiographs
• MRI imaging is contraindicated with magnetizable metals
• Hard tissue injury (tooth chipping and wear, occlusal interferences)
• Soft tissue injury (gingival and mucosal lacerations, gingival recession, mucoceles, traumatic neuromas)
• Soft tissue scarring and keloids
• Foreign body reactions
• Severe local infection leading to airway compromise (Ludwig’s angina)
• Chronic blood borne virus infection from piercing equipment (hepatitis B & C, HIV)
• Adverse reactions to metals (e.g. allergic contact dermatitis, argyria)
• Airway alterations (for uvula piercings), leading to snoring
• Problems in placing airways for intubation
• Persistent bacteraemias, with the potential for disseminated or distant infection (brain abscesses, endocarditis)
(From Walsh 2008)
In conclusion, as oral piercings increase in popularity amongst younger individuals, it is essential that all members of the profession are aware of the short and long term complications and the possible medical emergencies that can arise because of oral piercings.
Some useful resources to support oral health education on piercings are the ADA resources Lifestyle Risks and www.ada.org.au/Dental-Professionals/Policies/National-OralHealth/2-2-9-Oral-Piercing/ADAPolicies_2-2-9_OralPiercing_ V1.aspx
ADAQ TRAINING & PRACTICE CONSULTANCY TEAM, EMERITUS PROF. LAURIE WALSH AO
REFERENCES:
1. Samoilenko V et al. (2019). Oral piercing is a new challenge in the dentistry. Medičnì Perspektivi, 24(4), 133-144. DOI: 10.26641/2307-0404.2019.4.189605
2. Domingo MG et al. (2019). Oral exfoliative cytology and corrosion of metal piercings. Tissue implications. Clinical Oral Investigations, 23(4), 1895-1904. DOI: 10.1007/s00784-018-2626-4
3. King E et al. (2018). Oral piercings and their complications – how confident are we as a profession? British Dental Journal, 224, 887–895.
4. Walsh LJ. (2008) Missing the point: The risks of intra-oral piercing. Australasian Dental Practice 19(4), 156-158.
5. Ziebolz D et al. (2019). Comprehensive assessment of dental behaviour and oral status in patients with tongue piercing—results of a cross-sectional study. Clinical Oral Investigations, 24(2), 971-977. DOI: 10.1007/s00784-019-03002-y
24 25 ADAQ DENTAL MIRROR SPRING 2021

LEARN YOUR LESSONS AND BE BETTER PREPARED FOR THE NEXT LOCKDOWN(S)
History has a way of repeating itself and those that do not learn from the past are doomed to repeat their mistakes in the future. Even though it was not that long ago, I will outline the following to refresh your memory –
1 April 2021 – Brisbane comes out of a three day lockdown
30 April 2021 – India starts reporting new cases of more than 300,000 per day
27 May 2021 – Victoria starts its fourth (14 day) lockdown
19 June 2021 – NSW Bondi cluster emerges
26 June 2021 – Greater Sydney locks down
27 June 2021 – N.T. / Darwin locks down
30 June 2021 – Brisbane, Gold Coast and Sunshine Coast head into 3-4 day lockdown
Note that for 6-7 weeks from April through to mid-May we were in a state of bliss and it appeared as though the new normal had finally arrived. In the middle of April the travel bubble had opened up with New Zealand. JobKeeper had finished, unemployment fell, consumer confidence was up, as was economic activity. What could possibly go wrong? As we all know, a new strain of the Covid-19 virus emerged and Australia was woefully under vaccinated.
The State and Federal Governments will continue to provide financial assistance to those businesses and individuals affected by Covid related lockdowns and restrictions. It is essential that all businesses be prepared to apply for assistance which is relevant to them. They should be aware of the following-
1 State Government grants are issued under specific grant programs. Most dentists will have a reasonable understanding of what a research and development grant is. You apply for the grant and if you receive it then you must spend it on research and development. This is exactly the same process for a grant related to business assistance for Covid. You apply for the grant (you must meet all of the criteria) and if successful you need to spend it as directed - usually to cover business-related expenses.
2 State and Federal Government assistance is only claimable by individuals and businesses that meet the criteria set. I’ve seen applications rejected for the following reasons - the tax return, BAS or ABN has the incorrect ANZSIC code which identifies the business as something other than a dental surgery; the ABN for the contracting dentist is not registered for GST; the surgery or contracting dentist cannot prove the required decline in revenue; the dental surgery operates through a trust but the ABN registration is with the trustee company;
3 Some grants have time and quantity limits i.e. first in best dressed. Businesses need to keep abreast of announcements relating to financial assistance.
Care must be taken when applying for financial assistance to ensure that there are no adverse consequences to the future operations of the dental surgery. Assistance that was provided more than
12 months ago in the form of provision of government backed loans, deferral of payments on existing loans and deferral of rental payments did not affect your credit rating. We now find that banks are taking these into consideration when assessing the business for new lending applications.
Lastly, be mindful of changing how you operate. For ABN contracting dentists, the change to operating under a services and facilities agreement may mean that they are unable to pass a reduction in income test even though they may be receiving less commission. Practice owners should also be careful if they are considering changing their corporate structure, as they may be denied financial assistancewhich was the case in Victoria where you only automatically received the second Circuit Breaker Business Support Package if you had received the first one in the same business entity.
ABOUT THE AUTHOR

ALBERT GIGL
Albert Gigl is the founder of MW Partners, Specialist Dental Accountants. He has spent the last 15 years specialising in providing taxation advice for dentists. Contact Albert on 07 5554 6400 or albert@mwpartners.com.au for an obligation-free, confidential consultation.

26 ADAQ DENTAL MIRROR
CASUAL
CONVERSION UPDATE AND REMINDER
In March 2021, the Fair Work Amendment (Supporting Australia’s Jobs and Economic Recovery) Bill 2021 ( Bill ) passed Parliament. The Bill introduced several changes to casual employment, including providing a statutory mechanism for casual conversion.
Prior to these changes, there was no universal entitlement to casual conversion, rather, employees covered by a modern award (such as the Health Professionals and Support Services Award 2020) (HPSS Award) were able to request casual conversion
If they met the eligibility criteria outlined in the award. Now, the Fair Work Act 2009 (FW Act) requires employers to proactively offer casual conversion to eligible employees. This applies to all employees in the practice, not just those covered by a modern award.
There is a transitional period which ends on 27 September 2020 to allow employers time to make assessments as to whether they need to offer casual conversion. Practices must therefore determine who is eligible, and make offers of conversion prior to this date.
WHO NEEDS TO MAKE AN OFFER?
The changes apply to national system employers, which are those that fall under the national workplace relations laws. Practices operating as sole traders, unincorporated partnerships, unincorporated trusts and incorporated associations that are not trading or financial corporations in Western Australia are covered by the Western Australia State System instead, and are therefore not covered by the changes implemented in the Bill.
Small businesses, meaning practices with less than 15 employees, are also excluded from needing to make an offer. Employees employed in a small business retain the right to request casual conversion, however the administrative burden of having to actively offer conversion is removed.
Practices with 15 or more employees are required to make offers of casual conversion to eligible employees.
WHO IS AN ELIGIBLE EMPLOYEE?
The Bill defines an eligible employee as someone who:
• has been employed by the employer for a period of 12 months beginning the day the employment started; and
• during at least the last 6 months of that period, the employee has worked a regular pattern of hours on an ongoing basis which, without significant adjustment, the employee could continue to work as a full time employee or a part time employee (as the case may be).
If employees meet the above criteria, an offer of casual conversion must be made within 21 days of the employee reaching their 12 month anniversary, unless an exemption applies.
WHEN CAN A PRACTICE CHOOSE NOT TO MAKE AN OFFER?
There are also certain instances in which a practice with more than 15 employees is not required to offer conversion. This includes where a reasonable business ground exists. These include:
• the employee’s position will cease to exist in the next 12 months;
• the hours of work which the employee is required to perform will be significantly reduced;
• there will be a significant change in either or both of the following:
• the days on which the employee’s hours of work are required to be performed;
• the times at which the employee’s hours of work are required to be performed which cannot be accommodated within the days/times the employee is available to work
• making an offer of conversion would not comply with a recruitment or selection process required by law.
If a practice elects not to make an offer of casual conversion, it must still notify the employee of its decision in writing.
MAKING AN OFFER
When making an offer of casual conversion, practices must ensure the following criteria are met:
• The offer must be in writing; and
• Be an offer for the employee to convert to either part-time or full time employment (consistent with their hours of work during the relevant period); and
• Be provided to the employee within 21 days after they reach their 12-month anniversary.
Before making the offer in writing, the practice will need to meet with the employee and discuss the specific details of the offer.
Once an offer is made, the employee has 21 days to accept the offer in writing. If the employee does not respond, it is taken that they have rejected the offer.
NEXT STEPS:
Given the transitional period comes to an end on 27 September 2021, practices should be proactive and ensure that, if required, they undertake assessments of casual employees to assess eligibility, and make offers to eligible employees before this date.
For further information on this article, please contact ADA HR Advisory Service on 1300 232 462.
HOW TO INCENTIVISE PERFORMANCE IN THE PRACTICE
Incentivising performance is a key strategy for practices to implement to create and nurture a mutually beneficial relationship between employer and employee. Providing employees with rewards to recognise performance, whether financial or otherwise, is a proven constructive approach to building workplace rapport and job satisfaction.

Incentivising performance is a key strategy for practices to implement to create and nurture a mutually beneficial relationship between employer and employee. Providing employees with rewards to recognise performance, whether financial or otherwise, is a proven constructive approach to building workplace rapport and job satisfaction.
TANGIBLE INCENTIVES
Bonus schemes are perhaps the most conventional and wellknown workplace incentives. Creating a link between hard work and being a team player, with the possibility of receiving a heftier paycheck, is an almost sure-fire way to improve employee performance within the workplace. Offering additional payments and bonuses to employees creates an achievable goal and encourages them to endeavour to be better.
For example, offering employees an additional day of annual leave or paid time off at the discretion of the employer, in recognition of them going above and beyond for the practice, gives employees an incentive to strive to be their best. Alternatively, practices may implement a bonus structure, which may entitle an employee to receive a bonus payment for meeting or exceeding key targets within a defined period.
INTANGIBLE INCENTIVES
Nonetheless, incentive arrangements don’t have to be financial to be effective. In fact, studies have shown non-monetary rewards can be more effective than monetary ones. This is because tangible, or monetary rewards are an extrinsic motivation. That is, it motivates people to work for the reward. Non-financial rewards
focus on intrinsic motivation, which triggers internal behaviours and can promote better performance.
Having inexpensive or non-monetary incentives in place within the practice can bring out the best in employees without compromising the practice’s financial position. This may include implementing a feedback system, in which employee’s performance is recognised and displayed, a handwritten note or even an employee of the month poster. Both private and public recognition of employees’ hard work reminds them that they are a valued member of the Practice and that their contributions are appreciated.
Rewarding employees for their efforts helps build a bond between management and the employee and helps to incentive performance. To incentivise performance, and maintain high performance within the practice, requires the practice to provide continuous incentives. If a practice is inconsistent, and only rewards outcomes, rather than positive behaviours, employees are less likely to be incentivised to perform.
Non-monetary incentives can take form in any way the practice sees fit. However, one thing is for sure – recognising employees’ diligence and hard work, and consequently incentivising performance, works for the collective benefit of the practice.
For further information or assistance in relation to this article, please do not hesitate to contact the ADA HR Advisory Service on 1300 232 462.
28 29 ADAQ DENTAL MIRROR SPRING 2021
GOODWILL EXPLAINED
ADAQ COUNCIL NOMINATIONS
Nominations are sought for Members of the Australian Dental Association (Queensland Branch) (ADAQ) to join Council as representatives of the following divisions:
• No 1 Division – Moreton
• No 2 Division – Burnett
• No 3 Division – Western
• No 5 Division – Northern
• No 6 Division – Peninsula
• No 7 Division – Sunshine Coast
The position of Divisional Councillor Representative is for a period of two (2) years commencing from the conclusion of the Annual General Meeting (AGM) that will be held on 25 November 2021.
HOW TO NOMINATE
• Nominees may submit a statement of support for their nomination
• Nominations must be in writing
• Signed, fully completed and scanned nominations should be emailed to councilelections@adaq.com.au or posted to PO Box 611, Albion, Qld, 4010.
• Posted nominations must be received by 12 noon AEST on Friday 24 September 2021
• Nominations may be withdrawn at any time within 72 hours from noon Friday 24 September 2021.
DEADLINES
Nominations open: Friday 27 August 2021
Nominations close: 12 noon AEST on Friday 24 September 2021
NEED HELP OR HAVE QUESTIONS?
Please call ADAQ and speak with Miriah Sawrey on (07) 3252 9866 or email ea@adaq.com.au
By growing, investing in, and managing your practice, you’re inherently building goodwill, but what is goodwill and what else could you be doing to increase the value of your practice?
Ask any dentist what’s valuable about their practice and the first things that will spring to mind are intangible. After all, if you’ve spent years building a practice that your patients and employees love coming to, that goodwill is far more valuable than the sum of all the equipment and assets you’ve acquired over time. Goodwill is at the core of well-established practices, but how do you build it and how can you put a cash value on it?
Finance providers certainly value goodwill and do try to determine a cash value for it. Goodwill is the value of your practice, excluding the property, equipment and other physical assets.
Goodwill is an intangible asset, unlike a property or piece of equipment, and represents the reputation of the business and brand you have created, including consistent good service and strong employee relations. Goodwill is made up of the established number of patients, as well as the products and the services you offer. It also includes all those non-physical assets that belong to a practice such as the practice’s IP information, phone numbers, websites, and so on. The value put on goodwill can also vary depending on the industry, and the size of the practice.
There are three general steps a practice owner can take to build goodwill as an asset. Firstly, provide a consistently exceptional client service and build an ongoing relationship with your patients—this is an easy one to do as it is something all practices aspire to anyway. This will build advocacy for your practice through word of mouth and referrals. Secondly, invest in marketing and patient management/retention to build up your data base and attract new patients. This will support the advocacy generated from delivering great experiences. And thirdly, hire the right staff to look after your patients. Having the right team makes patients feel at ease and make them feel cared for. Those three steps will have the largest impact on building goodwill.
“A number of our medical and dental clients started out with nothing aside from their qualification,” says BOQ Specialist’s finance consultant Michelle O’Connor. “The hard work is getting their practice going and building goodwill. That’s why when a vendor is looking to sell, you will often hear that they’re selling what they’ve built up over 25 or 30 years.”
GOODWILL HUNTING
Building goodwill takes time and effort, and is unique to each individual practice. That’s why goodwill isn’t only valued on your active patient numbers. You must look at the value placed on the services offered to those patients and the value your patients place on them. In short, it’s complicated.
One of the other complicating factors in valuing goodwill is who is buying the practice. If a practice sells to a corporate group, other conditions may affect the sale price. These might include ongoing performance, and the current owner staying on for a period of time. If an independent practitioner buys the practice, it could be sold with no conditions for the current owner to stay on.
“Let’s say the buyer already works in that practice as an associate,” Michelle O’Connor explains. “The current owner is looking to retire, and they’ve worked out a succession plan. The price may differ because if the buyer is already working in the practice, as they have probably already built up their own patient base. We have some benchmark numbers of where we estimate it is placed and look back on historical sales to help value the practice. Credit officers in banks also have access to that kind of information.”
This is where the deep industry knowledge of BOQ Specialist comes in to play. They have decades of specialist experience in the dental professions so they understand not only how practices work, but also where the real value lies.
So, if you’re thinking about taking the next step in practice ownership, speak to one of BOQ Specialist’s local finance consultants on 1300 160 160 or visit boqspecialist.com.au/ goodwill to find out how we can tailor a finance solution for you.
31 ADAQ DENTAL MIRROR SPRING 2021
30
LEARN MORE AND
AT ADAQ.ORG.AU/COUNCILNOMINATIONS
NOMINATE
Disclaimer – The issuer and credit provider of these products and services is BOQ Specialist – a division of Bank of Queensland Limited ABN 32 009 656 740 AFSL and Australian credit licence no. 244616 (“BOQ Specialist”). Terms, conditions, fees, charges, eligibility and lending criteria apply.
situation,
BOQ Specialist
not offering financial, tax
legal advice.
obtain independent
tax and
advice as
felis fusce. Tortor ac parturien.
Any information is of a general nature only. We have not taken into account your objectives, financial
or needs when preparing it. Before acting on this information, you should consider if it is appropriate for your situation.
is
or
You should
financial,
legal
appropriate.parturient
BOQSPECIALIST.COM.AU/GOODWILL
Q&A WITH THE MEMBERS OF THE RECENT GRADUATE AND STUDENT COMMITTEE
The second half of 5th year for dentistry students can be incredibly stressful and exciting, not knowing what the next chapter after university holds.

ADAQ has a specific committee called The Recent Graduates & Students (RG&S) committee to help support you through the transition from student to practitioner.
Read on for our responses to some of the most commonly asked questions! We hope they help you prepare for the next chapter.
HOW LONG DID IT TAKE YOU TO FIND A JOB POST-GRADUATION?
This answer varies a lot depending on who you ask. Everyone is different, I would say, start writing your resume in the second half of final year, around August/September time. Have it ready to go in case a great job advertisement catches your eye.
Most practices start to advertise a position starting from September. The ads really start to increase near October and November. Remember, the practices need to advertise, then hold interviews and then they will offer you a position. This whole process usually takes around a few months. The position is usually advertised for an end of January start time, to ensure all your documents are ready (your registration, your provider number, your prescriber number). For the majority of people, from when you start applying, it takes a few months to land your ideal job. Majority of us sat at least 4-5 interviews.
WHERE DO YOU LOOK TO FIND A JOB?
The ADA jobs board, is great, you can filter search to find the type of job you want i.e. part time or full time and in the location that
you want. Also knowing that the advertised practice is aware of ADA provides comfort in its reputation. Seek and Indeed are also other avenues people have found jobs through. There are multiple Facebook groups such as “DPR” and “Australian Dentists” is also a new avenue a lot of practices are advertising on.
Networking is probably the main one; if you go to your local study club and express an interest in finding work, they may be able to connect you with a colleague. Asking your clinical and pre-clinical demonstrators will also assist you greatly. Even going to your local dental practice and discussing with them your interest and observing them will help go a long way
WHAT ARE YOU ENJOYING THE MOST ABOUT BEING A QUALIFIED DENTIST?
Definitely it would be meeting new patients, being able to treatment plan independently. Building a network with specialists and other dental colleagues.
Completing treatment successfully and knowing you have helped your patients and have overcome challenges.
Other dentists find the reward in being able to change your patients’ perception of dentistry, that it is not scary, and it is a great service. Being a family dentist and seeing your patients every 6months building that rapport.
WHAT DID YOU STRUGGLE WITH THE MOST WHEN YOU FIRST STARTED WORKING IN A DENTAL PRACTICE?
Confidence, a lot of graduates struggle with confidence. Knowing that a more experienced clinician can complete the same treatment quicker and maybe even better. However, a way to overcome this is to ensure you work at a supportive practice. You don’t want any time pressures on the first few years out.
Life vs Work balance, this is essential but can be very tricky to find the balance first starting out. It can be very tempting to just keep taking more hours, working longer and harder. However, this can lead to burn-out very quickly, dentistry is a great career and if practiced right and a good balance is found, it can allow for many activities alongside work and a healthy balanced life.
HOW HAVE YOU GONE ABOUT ENSURING YOU HAVE MENTORS/SUPPORT IN A CLINICAL SETTING?
From the time of searching for your job, you need to ensure your employer is willing to provide mentorship. This will often be advertised but it is important to ask them what type of mentorship they provide, for example, will there be dedicated days or after clinic time to go through cases together. It is also important to ask your employer if they have hired new graduates before and what their expectations are, you want to ensure your
UPCOMING EVENTS FOR STUDENTS & RECENT GRADUATES
Item Numbers, Communication, and Conundrums
9 SEPTEMBER
VIVA Prep Session for University Students
26 SEPTEMBER
Preparing you for the Profession
6 OCTOBER
employer is willing to teach you and understands the steep learning curve.
If having hands-on mentorship is difficult, then definitely try finding the right CPD for you. ADAQ provides a large variety of online CPD for free and hold CPD events for hands-on clinical skill improvement.
Observing other dentists or specialists in your area will help you a lot also! They can become excellent mentors.
WHAT IS YOUR ONE TOP TIP FOR GRADUATING STUDENTS?
Enjoy it! Finally! After all these years of studying, you have graduated, this is a massive achievement. It can be very overwhelming being a new graduate, however just know that there is so much support out there for you and everyone starts off as a new graduate!
Have some clear goals for yourself, start with simple goals or making your basic dental skills excellent. Such as perfecting your fillings. Take lots of pictures and go over your cases, selfreflecting is a great tool to help you improve your skills.
Make sure you keep your activities, hobbies this helps with making sure you have good mental and physical health.
SCAN TO LEARN MORE

SCAN TO LEARN MORE

SCAN TO LEARN MORE

ABOUT THE AUTHOR

DR MALAK FOUDA
Malak is the convener of the ADAQ Recent Graduates & Students Committee. If you have any other questions you would like answered, you can contact her anytime on rgs@adaq.com.au
32 33 ADAQ DENTAL MIRROR SPRING 2021
A DIFFERENT SENSE OF ADVENTURE
Inspired by a passion for rural and remote dentistry, a shared sense of adventure and the use of top-notch equipment, dentist Dr Garret Robles and his wife Mary Ann Robles have built two unique, complimentary dental practices to keep their sense of adventure alive.



“The farthest north we’ve taken our ‘pod’ or ‘tooth shuttle’ as kids call it, was in Normanton, responding to an invitation by North West Remote Health; and the furthest west is at a cattle station.”
“MYTOOTHDOCTOR was initially established so that POD clients in the Outback would have their own dental home in Townsville,” explains Dr Garret. “Now we have invested heavily in special care equipment, and MYTOOTHDOCTOR is the first and only private practice in Australia with its own bariatric and wheelchair tilt platform,” he says. “This equipment enables us to carry out procedures on wheelchair-bound patients without having to transfer them to a dental chair. The patient can be comfortably treated in his or her own wheelchair, with the platform allowing us to tilt the patient safely to an optimum ergonomic position for sit-down four-handed dentistry.”
Apart from children and special care patients, MYTOOTHDOCTOR also treats families and elderly patients with traumatic dental experiences. The team employs a full range of nonpharmacologic behaviour management techniques and for more complex work, dental rehabilitation is performed under general anaesthetic at the Mater Hospital.
To meet an increasing demand for their unique dental services, POD and MYTOOTHDOCTOR have expanded their team with two dentists and six support staff. The company prides itself for having staff who understand the dynamic nature of its business and are willing to take on the challenges of rural and remote dentistry.

The patient can be comfortably treated in his or her own wheelchair, with the platform allowing us to tilt the patient safely to an optimum ergonomic position for sitdown four-handed dentistry.
DR GARRET ROBLES
FEW dentists could list “the beauty of the outback skyline and sunsets” as one of the best parts of their job, but for Dr Garret Robles, travelling the outback is part of his 9-5.
Dr Garret and his wife Dr Mary Ann Palma-Robles, a senior visiting academic from the University of Wollongong and James Cook University, established Project Outback Dental (POD) almost two years ago, followed by paediatric and special care dental practice MYTOOTHDOCTOR six months later.
POD is North Queensland’s only private mobile dental surgery servicing rural and remote north and central west Queensland. The agile, off-road dental van is professionally fitted with complete dental equipment available in city surgeries. POD also has a state of the art self-contained mobile dental chair able to be deployed in any remote location; and a portable digital dental unit to treat patients with special needs at home, in hospital wards, and aged care facilities.
We travel Queensland’s Overlanders Way regularly from Townsville to Julia Creek , and to Outreach Service locations of the Townsville Aboriginal and Islander Health Service (TAIHS) says Dr Garret.
It was whilst teaching at JCU two years ago that Dr Garret was inspired by the university’s focus in rural and remote dentistry and envisioned having his own private dental van – providing affordable, quality and consistent services in the outback.
Dr Duane Perera completed his Doctor of Dental Surgery from the University of Melbourne and has a special interest in minor oral surgery and endodontics, while Dr Joel Abraham is a Townsville local who completed his Bachelor of Dental Surgery from JCU where he had broad clinical experience in indigenous oral health and dental public health. Both dentists have strong foundations in conservative and preventative dentistry. Dr Duane and Dr Joel described their first Outback experiences as delivering a muchneeded service that is both eye-opening and rewarding.
“When people ask why we decided to become Outback Dentists despite its many difficulties, I always keep in mind one of Robert Frost’s most misinterpreted poems,” shares Dr Garret. “We did not choose to be an Outback tooth doctor because it is a road less travelled. It is the road we have taken to respond to our different sense of adventure – one that demonstrates a distinctive purpose and passion.”
Writing and photography was supplied courtesy of DUO Magazine

35 ADAQ DENTAL MIRROR SPRING 2021
Back row, left to right: Lesley MacManus, Michelle Keys, Heather Holden, Dr Joel Abraham, Dr Duane Perera Front row, left to right: Bria Rose Cusack, Carley Mauger, Rosalind Kennedy, Mary Ann Robles, Nathaniel Layug, Dr Garret Robles
MEMBER SPOTLIGHT
PROSTHODONTICS, PERFORMING, AND OPENING PACKETS
our first flop and we lost the entire production investment. It was the first time I had experienced failure and thought it was a good time to specialise as it seems like a bit more of a sure thing than theatre (again I should have checked my facts!).
ARE YOU ALSO AN ARTIST ON PAPER?
I was very good at sculpture and drawing cause I grew up around it, but I was not passionate about it. I only ever did art as a means to an end….like set building for a show I wanted to put on, or to get into dentistry.
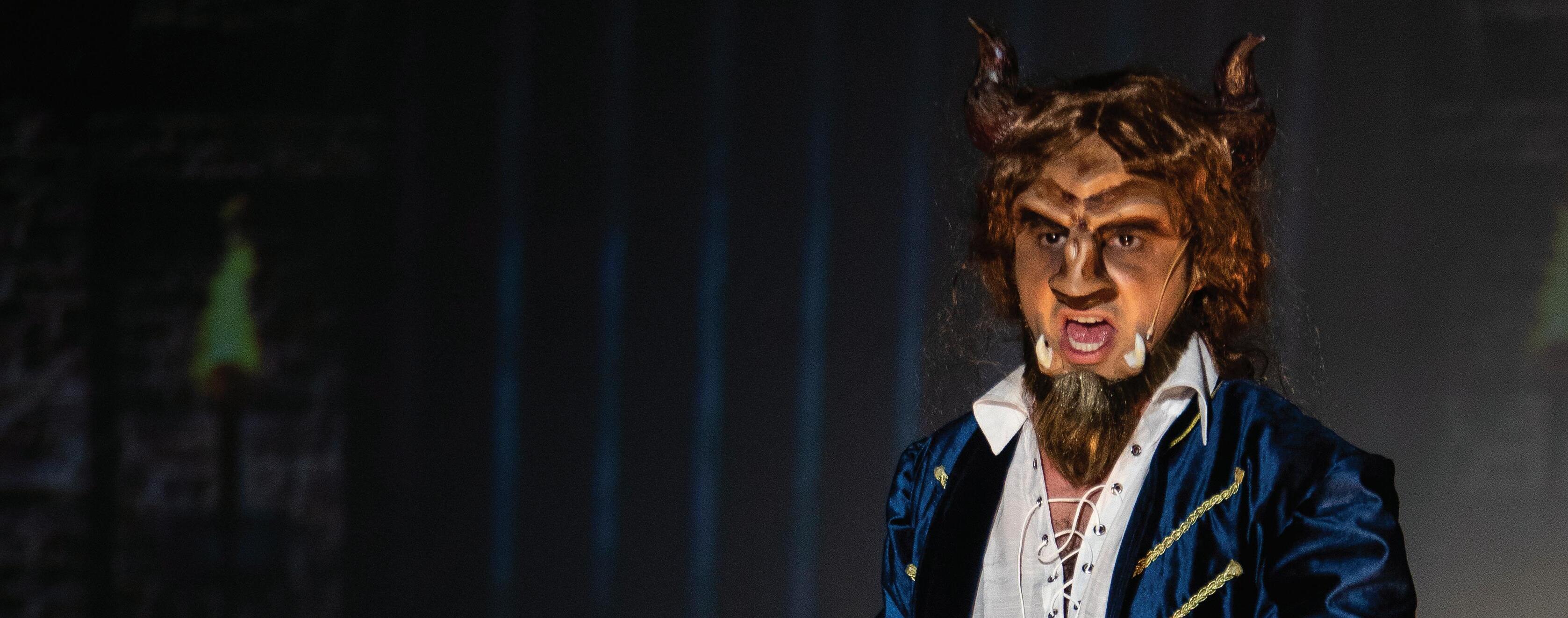

HOW DID YOUR DENTAL CAREER JOURNEY START?
My parents are puppeteers and my childhood was spent driving from puppet show to puppet show in a car without air conditioning. So we grew up in this creative and artistic environment. Despite my artistic leaning when it came time for their three children to go into the work force, there was a strong push for us to go into a profession. One of my friend’s father was a dentist and during work experience I went to his practice to watch him work. The surgery smelt clean and fresh, the air was conditioned and he spend the entire day opening packets of stuff!. We NEVER got to open packets at home and that sealed
the deal. As embarrassing as this is, the decision had nothing to do with patient care and everything to do with working conditions. …to this day I still love opening a good packet!
WHAT MADE YOU DECIDE TO CHOOSE PROS?
Don’t get me wrong…prosthodontics really suits me, but the decision was made on very flimsy criteria. I knew nothing about prosthodontics other than they cut crowns, and someone told me the head prosthodontist at Sydney dental hospital earns a salary of a million dollars a year! I should have checked my facts!
The year before specialising I was running a theatre company. After a lot of success in the Sydney theatrical scene we finally had
I come from a long line of artists. My dad and great uncle were puppeteers, my grandmother was an art teacher, and apparently her sister in law was wife to Jackson Pollock.
A funny story - When I was in grade 9 we had to choose our elective subjects. I wanted to do commerce as I felt it would get me closer to that air-conditioned office of my dreams, however my dad literally forced me to do art instead of commerce. I remember him saying “it will be easy for you”. Ironically when I opened the paper to see our HSC results, I was first in the state in visual art. But I haven’t done it since. I’m not interested in art - I like piano, acting and singing. Art was a means to an end.
Another funny story…when my granduncle stayed with Jackson Pollock and his wife in New York, on leaving Jackson offered my granduncle a few paintings as a parting gift. My granduncle told him “he wouldn’t hang them in the toilet. If he had only taken those paintings with him I don’t think any of us would be working now”…I hear “Blue poles” is valued at over 350 million….
WHAT BROUGHT YOU TO ACTING?
Dad listened to musicals in his spare time so they were always playing in the background. For some reason I just found I could sing when I was ten. My primary school worked this out too and they used to tour me round to various venues, singing bastardised tunes from “Phantom of the Opera” and “Oliver”.
When I was older I thought performing would be a good way of finding a girlfriend. This was a less successful venture. Perhaps if I had invested the same time and money in a personal trainer….
DID YOU EVER CONSIDER ACTING AS A FULL TIME ROLE?
Never. It never even crossed my mind that you could do this as a living. I was brought up with very traditional values and expectations - You grow up, you get a job, you buy a house and you get married….our family was very academic and it never occurred to me to go to acting school.
THIS YEAR YOU DID BEAUTY AND THE BEAST, TWO YEARS SOUTH PACIFIC, WHAT’S NEXT?
Sweeney Todd has just been announced so I am keen to enter the barbering trade!
IN THE RECENT PRODUCTION OF BEAUTY AND THE BEAST YOU SHARED THE STAGE WITH YOUR WIFE BELINDA?
This is how we met. Belinda auditioned for a production of “Urinetown” I directed. She threatened to leave multiple times during the rehearsal period and was strikingly beautiful. She had just graduated a degree in performance and thought I was an egocentric idiot (she is to this day, a very perceptive person)….
Apart from my wife, musical theatre never reeled in the ladies quite like I hoped. As a young man I had several girlfriends along the way but I never acquired them from seeing me on stage.
Who would have thought seeing a young man - singing his heart out to the tunes of Andrew Lloyd Webber - wouldn’t be the turn on of the century! It’s one of life’s quandaries - I bet Ghandi – spent a lot of time on that one…..
HAVE YOU EVER CONSIDERED WRITING YOUR OWN THEATRE PLAY?
No. I don’t have time or talent to do everything. I used to write shows when I was a kid but that was before I had performance opportunities.
DO YOU THINK YOU WILL REVISIT THAT LATER?
Nope - I know what makes me happy and I just like to sing. I was good at art and I know how to make puppets but they don’t feed my soul. Performing on stage is very special, and community theatre is a wonderful place to meet terrific people. The cast is always so nice to me and I try to be gracious back.
INTERVIEW BY MADONNA MCMANUS
ADAQ CPD Manager
INTERESTED IN HEARING MICHAEL SPEAK ON DENTISTRY?
Join us at Clinic Day this November, where he will discuss the latest in Aesthetics and Digital Dentistry.

36 37 ADAQ DENTAL MIRROR SPRING 2021
How Dr Michael Lewis found his specialisation (both in dentistry and the arts).
SCAN TO LEARN MORE
CLASSIFIEDS
Stay informed of opportunities and announcements exclusive to the ADAQ community
WANT THE BEST DENTURES IN MELBOURNE SERVICES?
We cover all your family dental needs. And gives the utmost importance to the client’s care and hygiene. We offer prosthetic and cosmetic dental solutions throughout Australia. our qualified and professional team offers a large network of dentists. We build a strong relationship with our clients to make sure that they get the best possible outcome. to get the best services of dental labs Melbourne and to learn more about our services you can call us at 1300 790 602 or visit https://anbdentalab.com/denturesmelbourne/
GENERAL ANAESTHETIC SERVICES BRISBANE SOUTHSIDE
Dr Anthony Speed, in association with anaesthetists from the Wesley Anaesthetic Group, wishes to advise that they can facilitate treatment for patients requiring general anaesthesia in our outpatient facility. This is particularly useful for patients who have no private hospital insurance. With an extensive range of experience, the team is willing to undertake wisdom tooth removal, place implants and perform routine restorative dentistry on all age groups including children aged 3 and above (individual case assessment), special needs patients, and dementia sufferers who are not medically compromised. Additionally we are now able to offer Cerec single visit crowns so that the patient does not have to return for subsequent cementation.
If this service can be of assistance to some of your patients who are unable to receive treatment under local anaesthesia, please phone the reception staff on 3397 1339 for further information.
USED A-DEC 500 DENTAL CHAIRS FOR SALE
Setting up a new practice or replacing an old chair? Queensland Dental Services (QDS) has good, regularly serviced, used A-dec 500 dental chairs, at one third the price of new ones. QDS is a dealer for Acteon, W&H, Carestream X-ray and CBCT, NSK, Cattani, and Stern Weber
CONTACT
Brian Gardiner on 0488 072 332 (briang@qds.net.au) for assistance setting up a new surgery, or if you are purchasing a new A-dec 500 dental chair, QDS can make it happen. QDS will install and service your new A-dec equipment, repair your NSK or W&H handpieces (in Brisbane), and perform X-ray Compliance and Validation of your W&H Lisa sterilisers, all at competitive prices. Phone Brian now on 0488 072 332 to secure your new (used) A-dec equipment.
ITERO SCANNER ELEMENT 5D LITE WITH CART
Brand new Still in carton. Just arrived Retails for $51,999 + GST Will Sell for $44,999 +GST
CONTACT
Email: smilestyle@me.com
MEET THE STAFF
MS MADONNA MCMANUS
ADAQ CPD MANAGER
WHAT’S A DAY LIKE IN YOUR ROLE?

Exciting. I work with Leigh O’Leary seeking out the very best to present engaging lectures and hands on experiences for the profession. We have a great pool of expertise on offer right here in Queensland which is very fortunate whilst we navigate our way through Covid times. But we are also looking beyond our border to bring additional speakers in 2022.
TELL US ABOUT YOUR CAREER SO FAR.
It is long so I shall I will keep it brief – I began as a Dental Assistant for Dr Stan Walsh, a former patriarch of the ADA back before gloves and masks were used. I spent 16 years in sales with Heraeus Kulzer where I drove the length of the state to visit all practices. After the birth of our son I came to ADAQ, followed by some time in my husband’s business then on to Straumann for 5 ½ years. Those 5 ½ years introduced me to value of quality education for our clinicians and I am passionate about quality CPD.

WHAT DO YOU LIKE BEST ABOUT WORKING AT ADAQ?
There is a fresh energy here at ADAQ, the excitement of building something special for the profession in CPD. And the undercover carpark.
WHEN YOU ARE NOT AT ADAQ, WHAT DO YOU LIKE DOING?
I love to feel the earth under my feet, be it in my own garden or even better, walking along the beach. But we are slowly renovating our home, so painting is my new hobby.
FUN FACTS
FAVOURITE FOOD? Corned silverside with mashed potato always warms me when I need comfort but day to day, I am a huge fan of my husband’s curries.
FAVOURITE SONG? Everything from J.J Cale’s version of Cocaine, (I can’t stay in my seat when I hear it) to different genres across decades. I also love a good musical. Let’s just say my taste is eclectic.
FAVOURITE FILM? I could watch Dead Poets Society over and over and still want to stand on the desk when Mr Keating comes to the classroom.
Study Dental
Assisting with us
Cert III and Cert IV Dental Assistant training courses available. Developed by experienced dental experts
Qualified trainers, oneto-one support
Self-paced learning, start anytime
State-of-the-art handson training facilities

38 ADAQ DENTAL MIRROR
RTO 30621

Turn the goodwill of a practice today into a loan for tomorrow
Our extensive experience lending to dentists means we understand the value of your profession – and we’re able to lend up to 100% of the purchase price of an existing practice, using goodwill as security rather than your home.*
Like you, we recognise the time it takes to build that goodwill. That’s why we take into account the sustainability of the practice and the value of intangible assets such as people, patients and intellectual property.
At BOQ Specialist, we back you and your business, giving you flexibility and support over the long term.
Learn more at boqspecialist.com.au/goodwill or speak to your local finance specialist on 1300 131 141.


BOQ Specialist. The bank for dental professionals *Subject to credit approval. The issuer of these products and services is BOQ Specialist - a division of Bank of Queensland Limited ABN 32 009 656 740 AFSL no. 244616 (“BOQ Specialist”). Terms and conditions, fees and charges and lending and eligibility criteria apply. Any information is of a general nature only. We have not taken into account your objectives, financial situation, or needs when preparing it. Before acting on this information you should consider if it is appropriate for your situation. You should obtain and consider the relevant terms and conditions from boqspecialist.com.au before making any decision about whether to acquire the product. BOQ Specialist is not offering financial, tax or legal advice. You should obtain independent financial, tax and legal advice as appropriate. We reserve the right to cease offering these products at any time without notice.








 LARISSA ALDERTON Senior Advisor - ADAQ Compliance, Advice and Policy
LARISSA ALDERTON Senior Advisor - ADAQ Compliance, Advice and Policy