Authors:
Sociological research: Adina Ghiocel-Pascu and Anamaria Dinu
Legal research: Ștefi Ionescu Research assistant: Luca Istodor

Layout & Design: Cristian-Dan Grecu
Graphic elements: Alex Petrican
Translation to English: prof. psih. ing. MA Daniela-Irina Darie



Collaborators: Iustina Ionescu, Alina Dumitriu, Diana Dragomir, Teodora Ion-Rotaru, Florin Buhuceanu, Cosmin Grădinariu, Andre Rădulescu, Ralu Baciu.
Thank you to all of the organisations, institutions and people who supported us in conducting the interviews for the sociological part of the research.
This research was made by Accept Association and ECPI- The Euroregional Center for Public Initiatives, in partnership with Sens Pozitiv, Rise Out, PRIDE Romania, Identity.Education.

Contents

I. GLOSSARY OF GRAPHIC SYMBOLS EMPLOYED IN THE RESEARCH REPORT 5
II. INTRODUCTION 9
Background to the research 9
Objectives of the research 9
Methodology of the Research 10
Stage 1 – qualitative research 10
Stage 2 – quantitative research 10
Stage 3 – legal research 12
III. SOCIOLOGICAL RESEARCH 13
Section 1: Exploring the needs of people living with HIV in accessing the health services in Romania 14
i The medical and emotional pathway of the HIV-positive patient 15
ii Challenges associated with HIV/AIDS 16
iii Coping mechanisms in the interaction with the medical system 20
iv. Circle of trust of the HIV+ person 25
v. The role of NGOs 27
vi. Health services in Romania 28
Section 2: Contextualising the lack of antiretroviral treatment 30
Section 3: Understanding discrimination, prevention, information and the interest of people living with HIV in the context of the legal framework in Romania 33
i Discrimination 34
ii Exposure of the HIV-positive status 36 iii HIV Prevention 38
iv. Impact of Covid-19 41
Section 4: Conclusions of the sociological research 43
IV. LEGAL RESEARCH
45
Section 1: General aspects 46
Section 2: Medical legal framework 55
Section 3: Social protection 65
Section 4: Education system and HIV 68
Section 5: Fight against discrimination 70
Section 6: Confidentiality 74
Section 7: Criminal incrimination 81
Section 8: Conclusions of the legal framework validated by the sociological study 88 V. RECOMMENDATIONS 90
I. Glossary of graphic symbols employed in the research report

Qualitative research stage
This symbol marks that the data in that section results from the qualitative stage of our sociological research.
Quantitative research stage
This symbol marks that the data in that section results from the quantitative stage of our sociological research.


HIV/AIDS Gay person
This symbol marks a discussion around HIV/AIDS or about people living with HIV (PLHIV). HIV stands for Human Immunodeficiency Virus. HIV attacks the immune system and gradually damages it. This means that without treatment and care, a person living with HIV is at risk of developing serious infections and cancers that a healthy immune system would ward off. Current HIV treatment works by reducing the amount of virus in the body so that the immune system can function normally. It cannot get rid of HIV completely, but with the right treatment and care, a person with HIV can expect to live a long and healthy life.

This symbol marks a discussion/mention related to a gay person, i.e. a person attracted to other people of the same gender as them (eg: a man attracted to other men, a woman attracted to other women).




Heterosexual person
This symbol marks a discussion/mention related to a heterosexual person, i.e. a person sexually and/or romantically attracted to people of a different gender than themselves (eg: a man attracted to a woman; a woman attracted to a man).
Transgender person
This symbol marks a discussion/mention related to a transgender person, or trans person. This is an umbrella term that includes those people who have a gender identity other than the sex they were assigned at birth. The term includes those individuals who feel the need, prefer, or choose, through language, terms of address, clothing, accessories, makeup, or bodily modifications, to present themselves differently from the expectations associated with their assigned gender at birth. This concept
6
includes people who have undergone medical or legal transition (people with a trans past), but also people who identify as transgender but do not transition, as well as all those who have a gender identity or gender expression that does not conform to the standard of „male” or „female”.

Drug user
This symbol marks a discussion/mention related to drug users. In this research, we focused in particular on people who use injecting drugs, as they constitute one of the categories at risk for HIV infection.
Person who practices commercial sex
This symbol marks a discussion/mention related to commercial sex workers, i.e. adults who occasionally or regularly receive money or goods in exchange for consensual sexual services or erotic performances.


Social activists
This symbol marks a discussion/mention related to social activists, namely those people who fight for the rights of disadvantaged or discriminated people, such as people living with HIV, LGBTQ+ people, Roma people etc.
Medical staff
This symbol marks a discussion/mention related to medical personnel: doctors, nurses, nurses etc.



Sources:
• Informat HIV, Asociația Sens Pozitiv: https://informathiv.ro/;
• Raportul Trans în România, Asociația Accept: https:// transinromania.ro/trans-in-romania/;
• Understanding Sex Work in an Open Society, Open Society Foundations: https://www.opensocietyfoundations.org/explainers/ understanding-sex-work-open-society
7
II. Introduction
Background to the research
“Organizing for Change” is a project aiming to support the fight against HIV/AIDS through a variety of actions targeted at MSM, TG, persons practicing commercial sex and people living with HIV.

Within this project, ACCEPT and ECPI have coordinated a sociological research in order to understand the health needs of people living with HIV and LGBTI people, the difficulties they face and the way in which the Romanian legislative framework responds to these challenges.
This report consists of three main sections:




Qualitative exploratory research aiming to highlight the health needs of people living with HIV, Quantitative research analyzing data obtained from an online questionnaire on a sample of 139 people, Legal research on the relevant legislation.




Objectives of the research
Investigating the current Status Quo on:
• information,
• education,
• prevention and
• access to health services by MSM, TG, sex workers and PLHIV.
Identifying the needs and challenges faced by these persons as well as the impact of these situations on the physical, mental and emotional health of the health service beneficiaries.
Investigation of the discriminatory perceptions and situations in the context of the access to the health services.
Reflection of the legislative framework in the daily lives of MSM, TG, sex workers and PLHIV.
9
Methodology of the Research
Stage 1: Qualitative research



Methodological design: 13 In-Depth Interviews with the interview duration of approximately 60 minutes and 2 Focus Groups with the discussion duration of approximately 120 minutes.

Target group investigated: included a mix of social actors relevant to the topic under investigation: PLHIV, HIV/AIDS activists, sexual and reproductive health and women’s rights activists and persons within the health system.


The data collected in the qualitative research is not statistically representative due to the small sample size. The role of the qualitative research was to explore and understand the challenges faced by persons living with HIV.
Stage 2: Quantitative research
The sample consisted of: 139 respondents (LGB/MSM people, persons living with HIV, persons practicing commercial sex, transgender persons, homeless persons).
• Nationwide distribution (respondents from 24 counties in 27 localities)
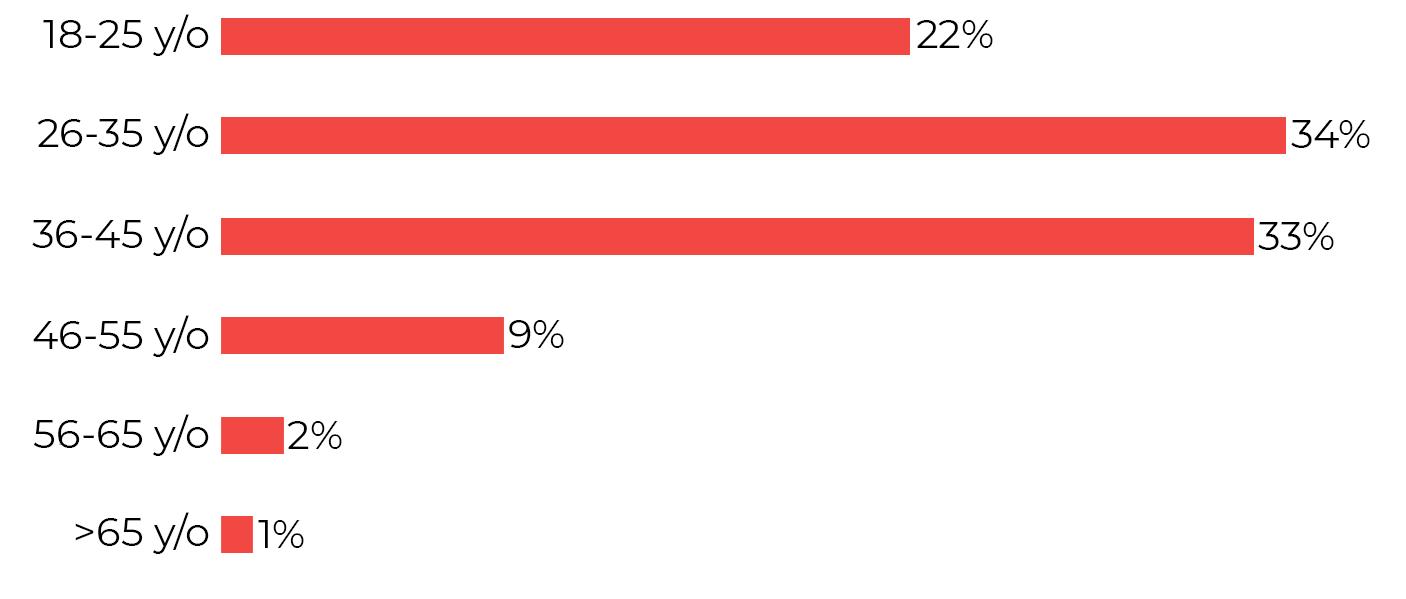
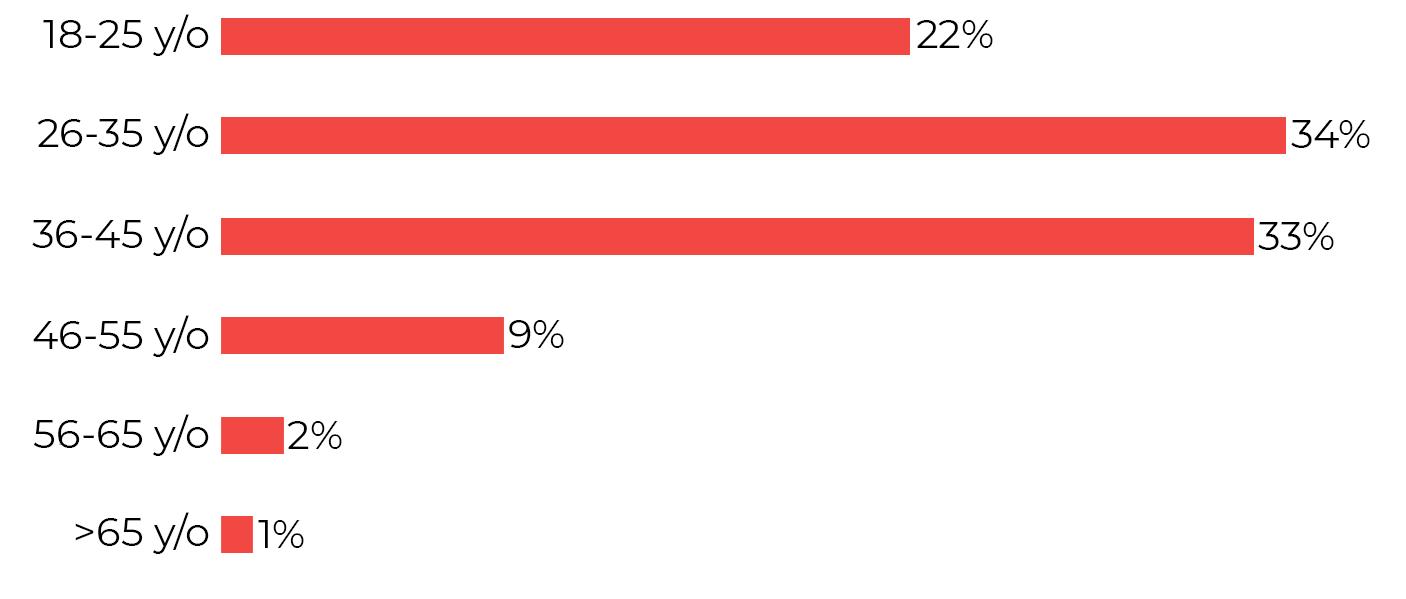
• Balanced mix by age group 18-65 (good distribution, especially in the 18-45 age range) and active-passive in employment

Sample structure in the quantitative stage
Age of the respondents How old are you?
10
Gender of the respondents
Gender

The answer to the question “Gender” was left open so that the participants could define and declare their gender identity as they wished.
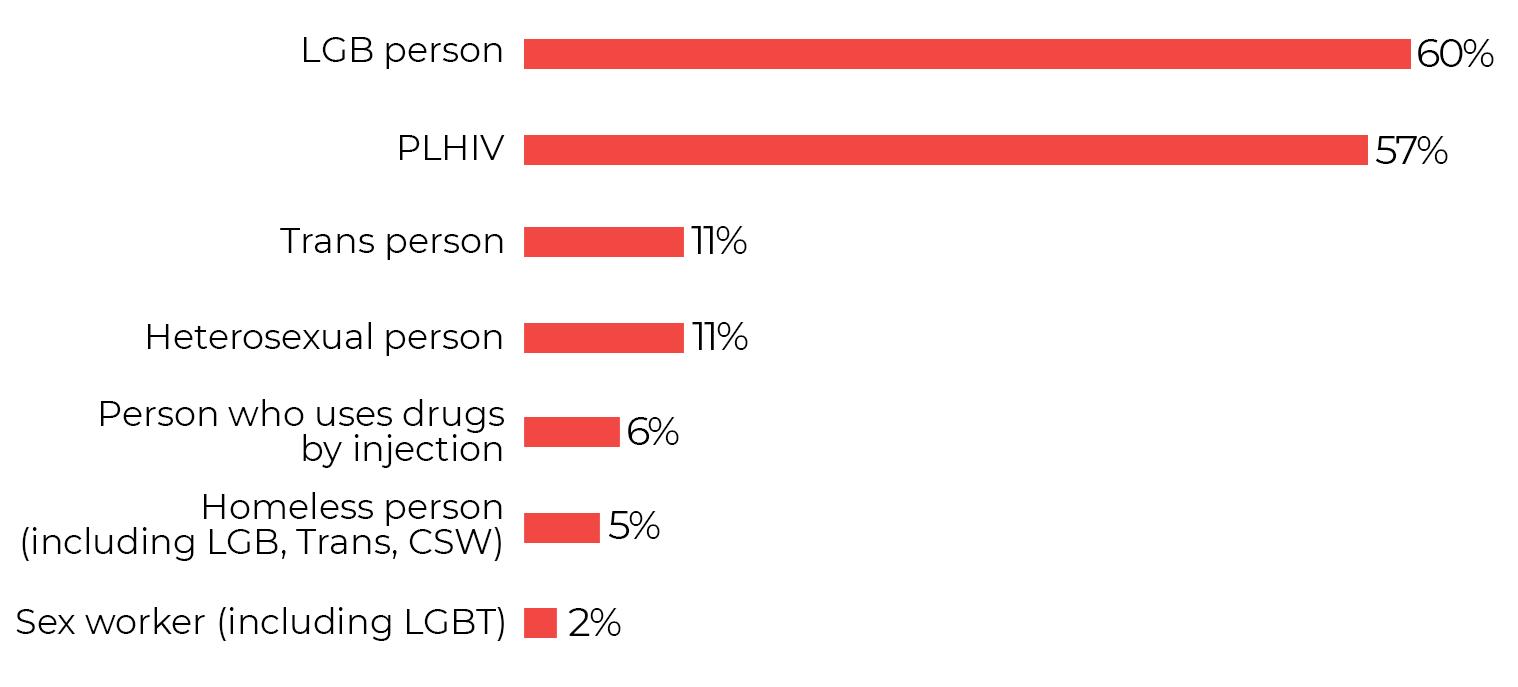
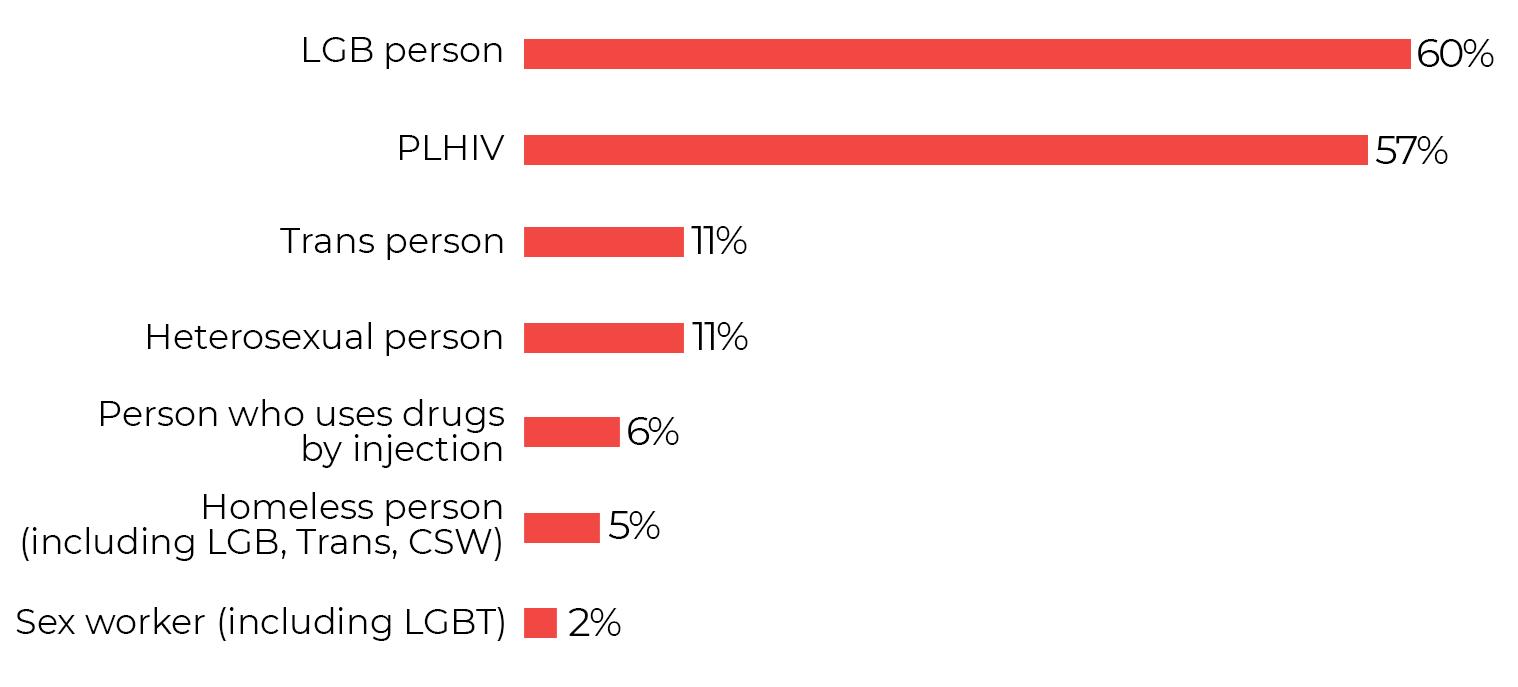
Categories of interest included in the study
Which of the following categories do you fall into?
Pre-determined sampling quota of minimum 30% HIV+ and minimum 50% LGBT in order to obtain a sample that is representative of the topic under investigation and reflective of the community of interest for this study.
In terms of the current occupation, half (53%) of respondents work full-time, 9% work part-time, and 38% do not work.

11
Occupation
In terms of level of education, the majority of respondents (87%) have at least completed the high-school courses (primary school 8%, vocational school/ technical college 4%, high school 25%, university 35%, post-graduate studies 27%), and in terms of the time of the positive HIV diagnosis, for half of the respondents it occurred within the last 5 years.

Stage 3: Legal research

The legal research identified and structured the main legal milestones and the medical legal framework. In the analytical approach, the most relevant sources composing the HIV/AIDS normative framework were considered, such as: the HIV Law and its implementing rules, the Law on the rights of the patient and other rules in the medical system and on social protection, the Penal Code, the Ordinance on the prevention and sanctioning of all forms of discrimination.
This report presents the integrated results of the sociological and legal research.
The sociological research identifies and exposes the difficulties that persons living with HIV and those from the LGBT community face in accessing the health services in Romania.
The legal research is complementary to the sociological study and highlights the legal framework that should ensure the protection of HIV positive persons.
12
III. Sociological research

Section 1: Exploring the needs of people living with HIV in accessing the health services in Romania
The in-depth interviews conducted as part of the qualitative research revealed a positive correlation between the level of education of the study participants (PLHIV) and their own health management: the higher the level of education (university, master’s degree), the better PLHIV manage their own health. Persons with a high level of education were able to achieve an undetectable viral load due to increased adherence to the prescribed treatment. Thus, their health status is described with a focus on comorbidities (lipodystrophy, lung disease, endocrinological disease, etc.) rather than HIV.
In the case of persons with a low level of education who were more likely to be drug users and persons practicing commercial sex, the state of health was often described in terms of AIDS, with a poor management of the various manifestations of the disease. Adherence to treatment was very low, in one case non-existent.
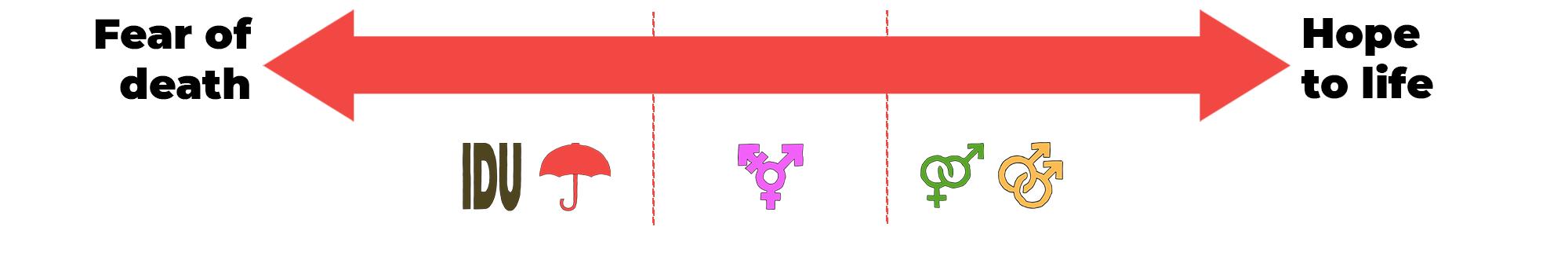
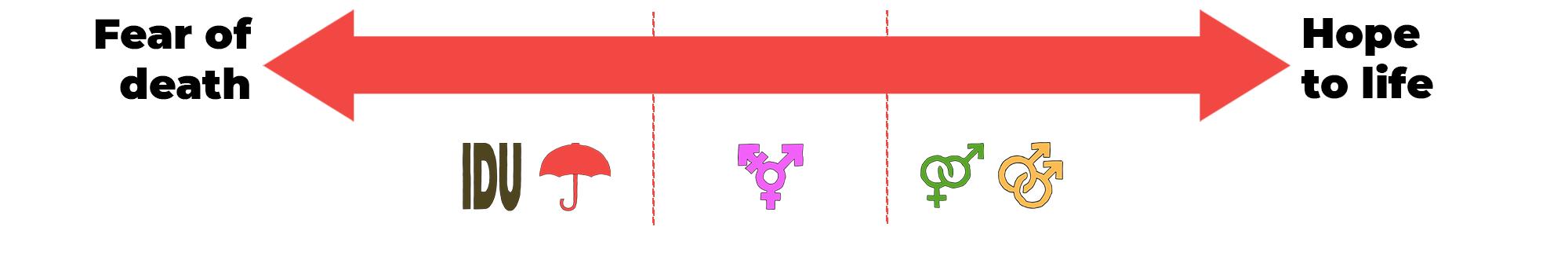
The attitude of the HIV-positive patients towards their own HIV status is generated by 2 main factors:
The drug users and the persons practicing commercial sex with low levels of education (regardless of their sexual orientation) view their HIV-positive status with a high level of negativity and resignation. The fear of death is a frequent topic in their conversations.
Low adherence to treatment is an effect of a whole vicious circle: lack of access to information makes them unaware of the importance of treatment and health professionals are reluctant to explain the long-term medical effects to these patients. Even more, these patients sometimes experience hostile behaviour from health professionals and thus end up refusing to go to hospital.
Transgender, heterosexual and highly educated gay people are rather tolerant and optimistic when it comes to being HIV+. They project a long-term future, plan for personal development and want to be actively involved in HIV and AIDS prevention and information campaigns.


14
The health professionals interviewed for the study believe that the medical progress in terms of HIV therapy has been impressive since the 1997-1998 baseline year. The treatment regimens have evolved greatly and HIV is now seen as a chronic disease that can be “compared to hypertension or diabetes”.

If I had to choose between HIV or diabetes, I would happily choose HIV. You live much more decently with HIV than with diabetes. (healthcare professional)
The medical and emotional pathway of the HIV-positive patient

The HIV-positive patient’s medical journey is accompanied by a lot of uncertainty that increases the anxiety and leads to emotional imbalances.

A state of drowsiness, muscle pain, headache, cough, fever occurs. Some patients experience very severe colds which prompt further investigations.
ELISA test (screening test) Western blot test (confirmatory test) Both tests are performed in test collection laboratories.
Following the confirmation of the Western Blot test, the patient is referred to an infectious disease physician who will take over the patient for therapeutic management and monitoring. The infectious disease physician will certify the final diagnosis

NGOs intervene at this stage and provide support.
The initiation of the treatment is performed by the infectious disease doctor. The therapeutic objective is to lower the viral load to as low as possible for long periods of time in order to restore the immune system.
After the patient has adjusted to the antiretroviral therapy and the new lifestyle, their mood improves. Adherence makes a decisive contribution to the patient’s quality of life.
Lack of treatment, especially in newly diagnosed individuals, severely impacts the balance of the HIV-positive patient and jeopardizes the previously acquired therapeutic benefit.

15
Challenges associated with HIV/AIDS
The challenges of PLHIV investigated within the qualitative research could be grouped into two main categories: direct challenges and indirect challenges generated by the presence of HIV in their lives.

Adversely affected health condition: frequent feelings of malaise, frequent chronic fatigue, nausea, muscle and joint pain, rash, fever, chills, coughing







The impact of treatment on health: multiple side effects (vomiting, drowsiness, watery stools, dental problems, etc.), the appearance of associated diseases such as candida, the therapeutic fatigue that sets in due to the fact that the treatment must be administered for life, the strictness of the treatment administration also has a strong impact on the social life of PLHIV.
Lack of treatment represents another challenge faced by PLHIV
Lack of pills is a recurring issue, HIV-positive persons face this situation every year with no explanation as to “when and how” this problem will be solved. Alternative solutions offered by the health system are:

Providing antiretroviral treatment for short periods of time: for 7-10 days; for 2 weeks; for 1 month. This alternative causes multiple lifestyle disruptions for PLHIV. They have to leave their workplace frequently to pick up their treatment. In addition, the frequent visit to the hospital brings an increased exposure of the patients and the impossibility of preserving the confidentiality of the diagnosis within the community they belong to.
Hospital visits are a source of anxiety and a constant reminder of illness for all respondents surveyed. The frequent hospital visits for treatment pick-up contribute significantly to amplifying this anxiety and to the development of a “hospital phobia” among PLHIV
16
You do realize that if I’m at the hospital every week to get my treatment, it’s almost impossible not to run into someone I know in the hallways. I most wish people didn’t know about my illness, in a small town if they do, you can say goodbye to your job, your friends... not to mention the impact it would have on my parents. (LGB HIV+ person)
Changing the therapeutic regimen with treatments that are available. Often, the therapeutic regimens recommended as substitutes are ‘outdated’ regimens containing inferior treatments in terms of the tolerability profile associated with the prescribed drug. This alternative feeds the patients’ fear of developing resistance to the therapy, thus compromising the therapeutic benefit.

Providing preferential treatment only for patients at an advanced stage of disease severity. Current protocols guiding the management of HIV-positive patients direct the health care professionals to provide immediate and nonpreferential treatment to all patients diagnosed with HIV.




I didn’t receive any treatment for the first two years after the diagnosis because my tests looked very good and the doctor said no treatment was needed. I had to have a certain CD4 and viremia value to go on treatment. Later, these protocols were changed and now the patient has to receive treatment immediately after diagnosis. (Heterosexual person, HIV+)
The emotional health adversely affected: frequent feelings of anxiety, inadequacy, depression, low self-esteem, feelings of guilt and suicidal thoughts.


Social life is severely affected: self-isolation and lack/limitation of sexual relations due to the fear of passing on the virus (especially among the less educated persons), frequent discriminatory situations leading to the rejection of HIV-positive people (avoidance and stigmatization of PLHIV, exclusion from their circle of friends, humiliation of PLHIV, difficulties in establishing long-term relationships, etc.). It is not the virus itself that is stigmatizing but the way in which the HIV+ person became infected: HIV is often associated with a depraved sexual behavior, drug abuse and a sexual orientation other than the heterosexual one.

17
I don’t understand why people are empathetic and compassionate when it comes to sick people but not when it comes to HIV+ people. You would say that we are not sick but that we should be punished for having this virus. They feel the need to blame and instigate discriminatory behaviour... as if that would make us better. (Heterosexual HIV+ person)
Exposure to potentially discriminatory situations when interacting with authorities: the medical system and the Police. Interaction with the medical system revealed situations where HIV-positive people felt humiliated and felt their right to treatment was denied. Treatment of dental problems and gynaecological conditions were listed among the most common potentially discriminatory situations.
Humiliating attitude and aggressive behaviour among the community policemen/public constables, is especially mentioned by the drug users and the commercial sex workers.
The dentist freaked out the moment I told him about my diagnosis and I saw him get all agitated around me. He started postponing my appointments and eventually told me he couldn’t see me anymore. (LGBT HIV+ person)





I think that visit to the cardiologist was the shortest consultation I’ve ever had. After I told him I was HIV positive, he immediately told me he had a lot of patients and couldn’t see me anymore. I saw him take a compress on which he had put some alcohol and touched the doorknob with that compress in his hand when he opened the door to ask me out. (HIV+ LGB person)
At the hospital they didn’t even want to give me any more pills, they said I was throwing them away so they wouldn’t give me any more. But I don’t throw them away, they paint us with the same brush and it’s not fair. And when the guards come down the street, they shout at me ”Get away from there, you AIDS-man” and they’re so scared of me you’d think I had the plague. (HIV+ drug user)
The challenges for the health professionals in managing HIV-positive patients are related to the patients’ lack of adherence to the treatment. They believe that relatively few HIV-positive patients are truly adherent (more than 90% comply with treatment) and this is due to a lack of awareness of the risks and the long-term effects of the disease.
Logistical and financial challenges that limit the public information campaigns on HIV and AIDS are also mentioned and thus a limited understanding of the disease among the general population persists.



18
At an early stage of the quantitative interview, we estimated the extent of the challenges the HIV-positive persons experience due to their current health status and how often they face them, trying to cover the challenges highlighted in the qualitative research stage:

Challenges generated by the disease stage/life with HIV (impact on overall health if you are not HIV+ but have health problems)
Challenges arising from the current treatment (side effects of the treatment)
Challenges in relation to the health system (difficulties in obtaining treatment due to the mode of distribution/absence of treatment, recurrent treatment interruptions)
Emotional challenges (psychological/emotional impact + personal life/ relationships)
Social challenges (stigmatization, discrimination, self-isolation, physical inability to take part in different activities, denial of certain health services, etc.)





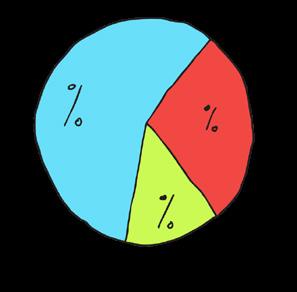
The biggest challenges were found to be emotional (58%), health-related (45%) and social (45%).
Challenges

19
The data in the conclusion above represent the cumulative percentages of codes 3=Sometimes, 4=Often, 5=Very often
*Other (34 respondents). Most mentions were related to the relationship/ interactions with the physicians and the medical staff (not very LGBT friendly, lack of empathy/ disrespect of gender identity by assuming the gender at birth is same as the current gender/ fear of coming in for regular gynaecological check-up due to the sexual orientation/ older physicians and they don’t care financial challenges and finding a job or problems at the current job (absences due to ill health, fear of not being found).
A warning signal is that because of the interaction with the public health personnel, there is a risk that some patients will stop the treatment (one patient said “The physicians treat us like animals, that’s why I didn’t take treatment at all”).


Coping mechanisms in the interaction with the medical system

Coping mechanisms used by PLHIV to cope with the interaction with the medical system in Romania
Certain PLHIV prefer to avoid the interaction of any kind with the medical system in Romania even if it means depriving themselves of the antiretroviral treatment.
There are also people who, once in the halls of hospitals, try not to disturb and stay in a shadow so as not to generate an interaction with the medical personnel.

20
When I go to pick up my treatment, I don’t lift my eyes from the ground for fear that there will be an argument. The nurses are capricious... today they ask you how you are and tomorrow they pick on you because you breathe the same air as them (LGB HIV+ person)
I stopped going to the hospital because I was going in vain. The last time I went they gave me something and put me to sleep and when I woke up I was thrown out on the street...they didn’t know anything about me. I don’t need their treatment anymore because I go there and nobody pays any attention to me (Drug user and commercial sex worker, HIV+)
There have also been instances mentioned where buying small gifts (candy, coffee, flowers, etc.) and giving them to nurses/physicians manages to de-escalate the interaction between some PLHIV and some health care professionals.
Other patients, especially those with a higher level of education, make fun of trouble and adopt self-irony as a language of communication.




There are also HIV-positive patients (those with higher levels of education) who try to live with the medical system and inform themselves in advance about the degree of tolerance and acceptability of the physicians towards PLHIV and LGBT people. ARAS supports these patients with various contacts of physicians who accept to treat LGBT HIV+ persons.
I’ve made friends with the nurses at the hospital, I always buy a box of candy and tell them I’ve come to get my ”treatment” (candy) so I bring them candy. (HIV+ heterosexual person)
I don’t want to risk running into any more doctors who tell me they’re too busy so I talk directly to ARAS and ask about doctors who agree to treat HIV+ LGBT persons. That’s how I found my dentist and it’s very ok to interact with him. (HIV+ LGBT person)

Offensive attitudes are present both among HIV+ people with a high level of education and among those with a low level of education. The revolt of the patients can be found among both profiles, but it manifests itself differently.

21
People with education + : adopt an assertive attitude and do not allow medical professionals to have discriminatory behavior or show a hostile attitude. These people know their rights and are most often supported/ guided by various NGOs in claiming their right to treatment/life.


People with education – : are often conflicted and respond with verbal aggression to hostile attitudes from medical personnel. The lack of access to informative resources, the lack of education regarding the management of one’s own emotions, as well as the repeated exposure of these patients to various discriminatory situations, lead them “to the brink of despair” and make them exhibit aggressive behaviors.
I understand that they may have hard days when they see a lot of patients (and this Covid situation has further burdened their work) but that’s not my fault. When I go to the hospital, I don’t go for love but out of need and I want to get answers to my questions, I don’t accept to leave there without answers, without treatment or feeling like taken for a ride. (HIV+ LGB person)
I get angry very easily and if somebody says something to me, I’m not at all ashamed to make a fuss... I even swore at the nurses in the hospital corridor. (LGBT person, commercial sex worker, HIV+)


The physicians interviewed for this study are somewhat reserved about the mentions of the HIV-positive patients referring to their interaction with the health services in Romania. They attribute the “dissatisfaction” of the HIV-positive persons to the therapeutic fatigue and the tense situation generated by the Coronavirus pandemic.
Social activists believe that there is “no smoke without fire” and the HIV-positive patients often have to deal with medical staff who approach them from positions of power and manage to intimidate newly diagnosed patients in particular.

In terms of accessing the health services for persons living with HIV, the most common situations are:


22
Lack of treatment/interruption of treatment (delayed stock, delayed approval of funds, incorrect estimate of the treatment needed, etc.) – 65%


Breach of confidentiality (name calling in the corridor in relation to diagnosis/treatment release, waiting in shared queues with other patients with the same diagnosis) – 48%
Treatment offered for less than 30 days – 45%
The state of health not being regularly assessed (every 6 months) through specialist investigations occurs in 39% of cases, and changing treatment according to the existing stocks without a medical reason occurs in 35% of cases.
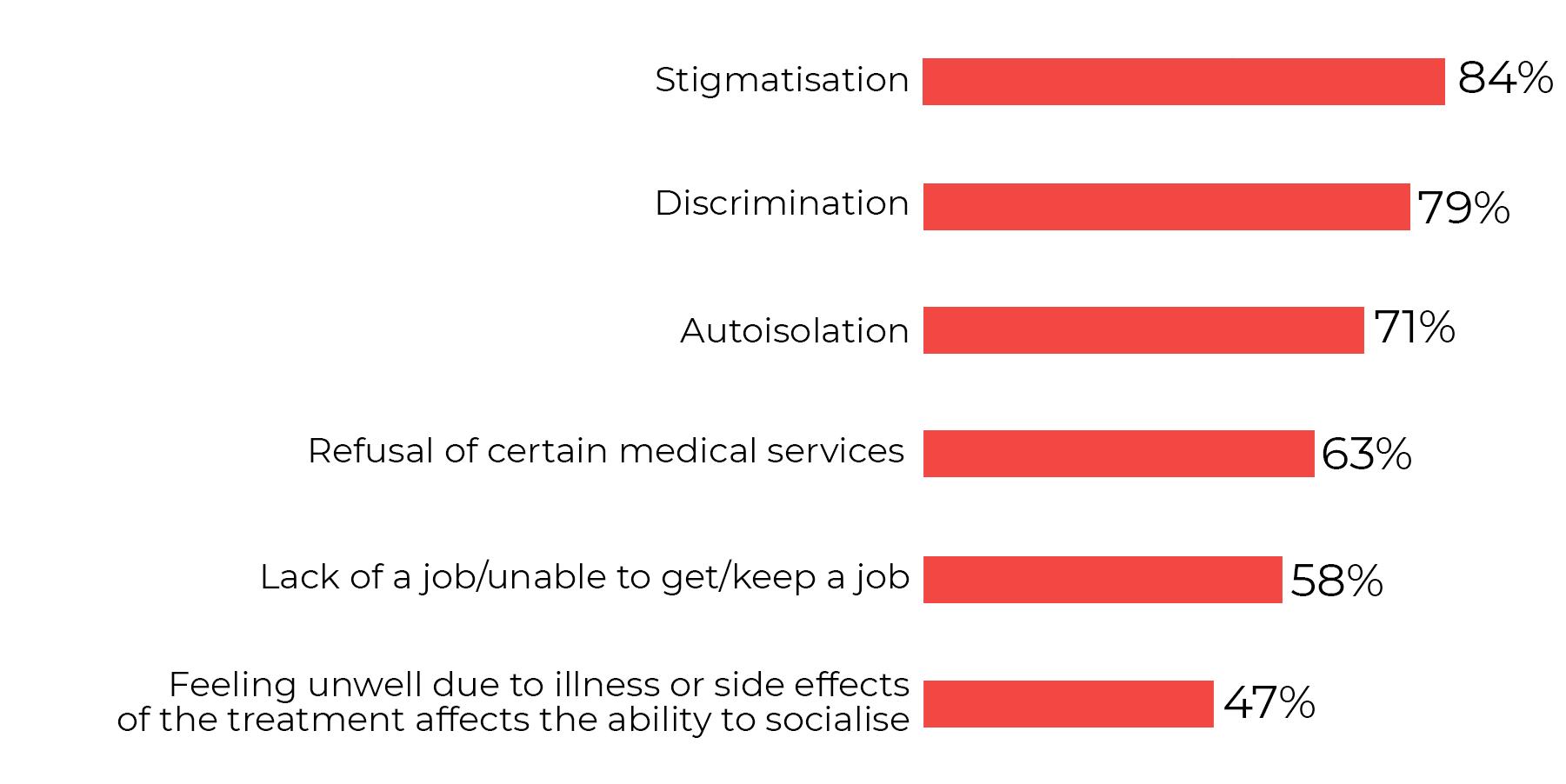
In terms of social challenges, the majority faced by the community are stigma (84%), discrimination (79%), self-isolation (71%), denial of certain medical services (63%). Also worth mentioning are challenges such as lack of a job/ inability to get/keep a job (58%) and feeling sick due to illness or the side effects of treatment affecting the ability to socialize (going out with friends, family obligations, etc.) – 47%.
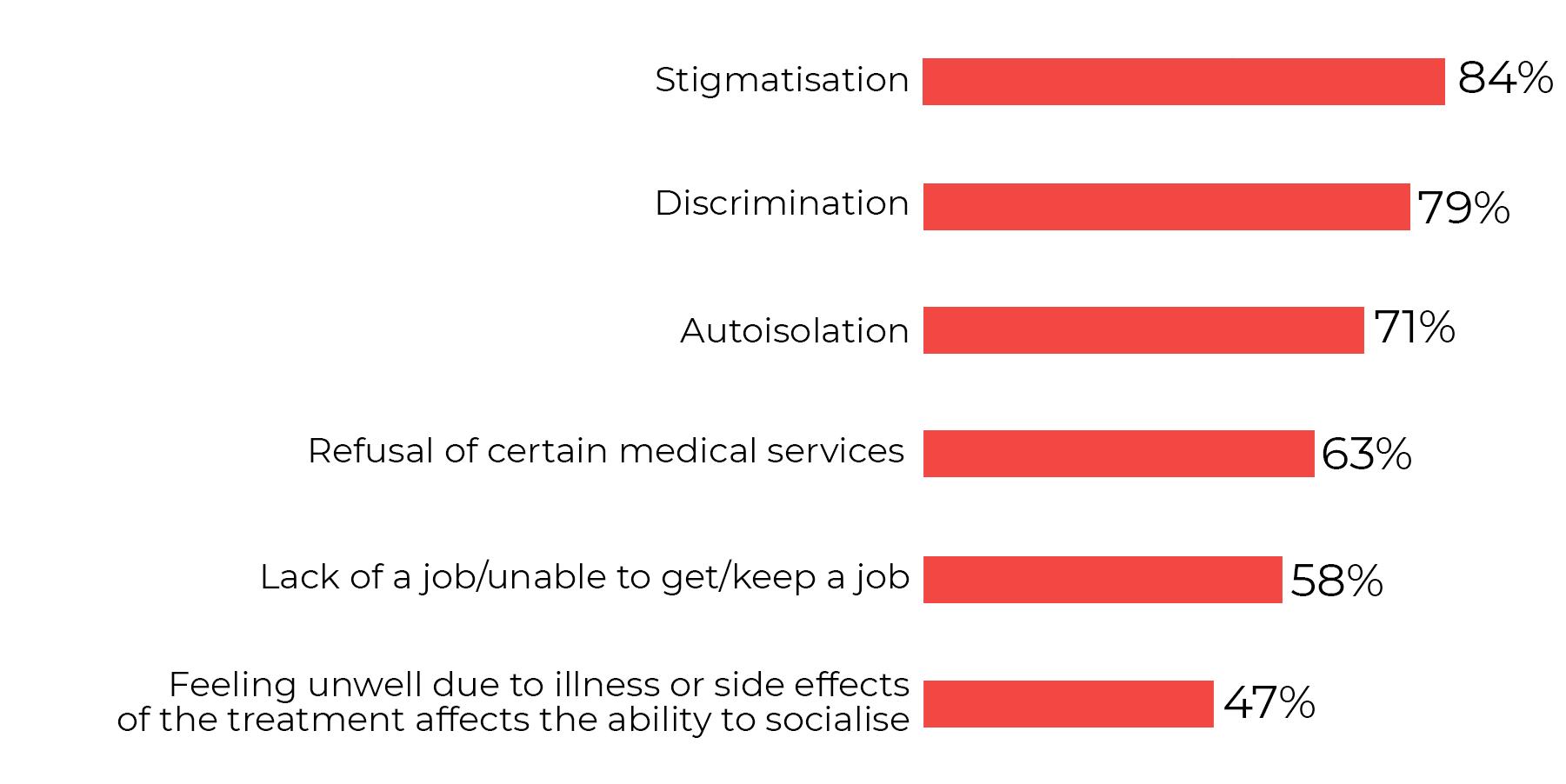
Social Challenges
The data in the conclusion above are cumulative percentages codes 3=Sometimes, 4=Often, 5=Very often

When community members were asked to think about the current needs they face and their order of importance, the order in which they should be addressed,

23
the most important was the need for social acceptance, followed by (in order of importance):


Easier access to healthcare
Acceptance from those around me (family, friends, partner, etc.)
Belonging (inclusion in a group of friends)

Easier access to treatment (receiving treatment on time)
Finding/keeping a job
Access to counselling services (counselling and support through psychotherapy)
Access to financial benefits (monthly food allowance, tax relief, etc.)





Keeping my HIV status confidential

The need for acceptance and social belonging of the person living with HIV implicitly speaks to the social stigma associated with HIV and the multiple discriminatory behaviors that result from it (including in accessing the health services).
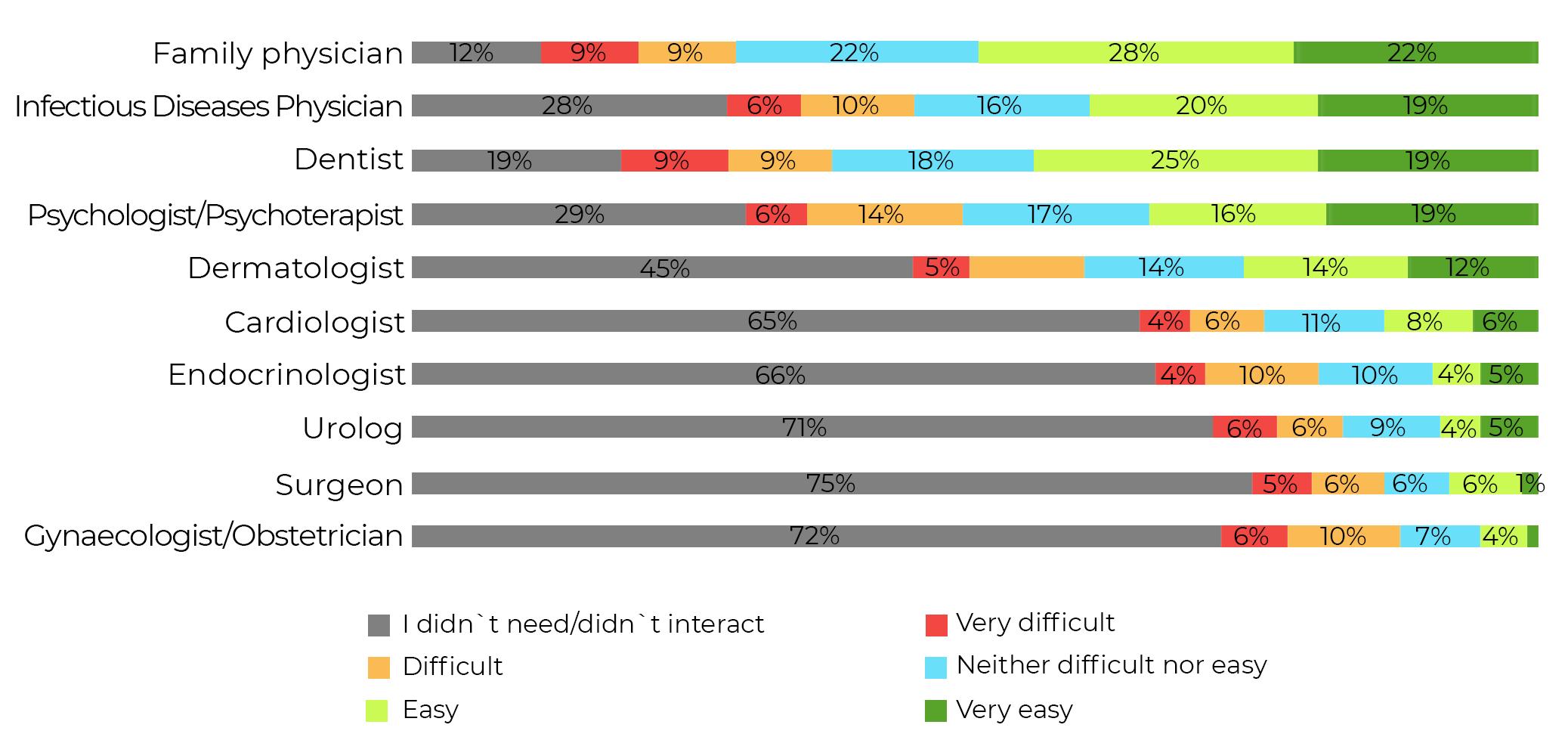
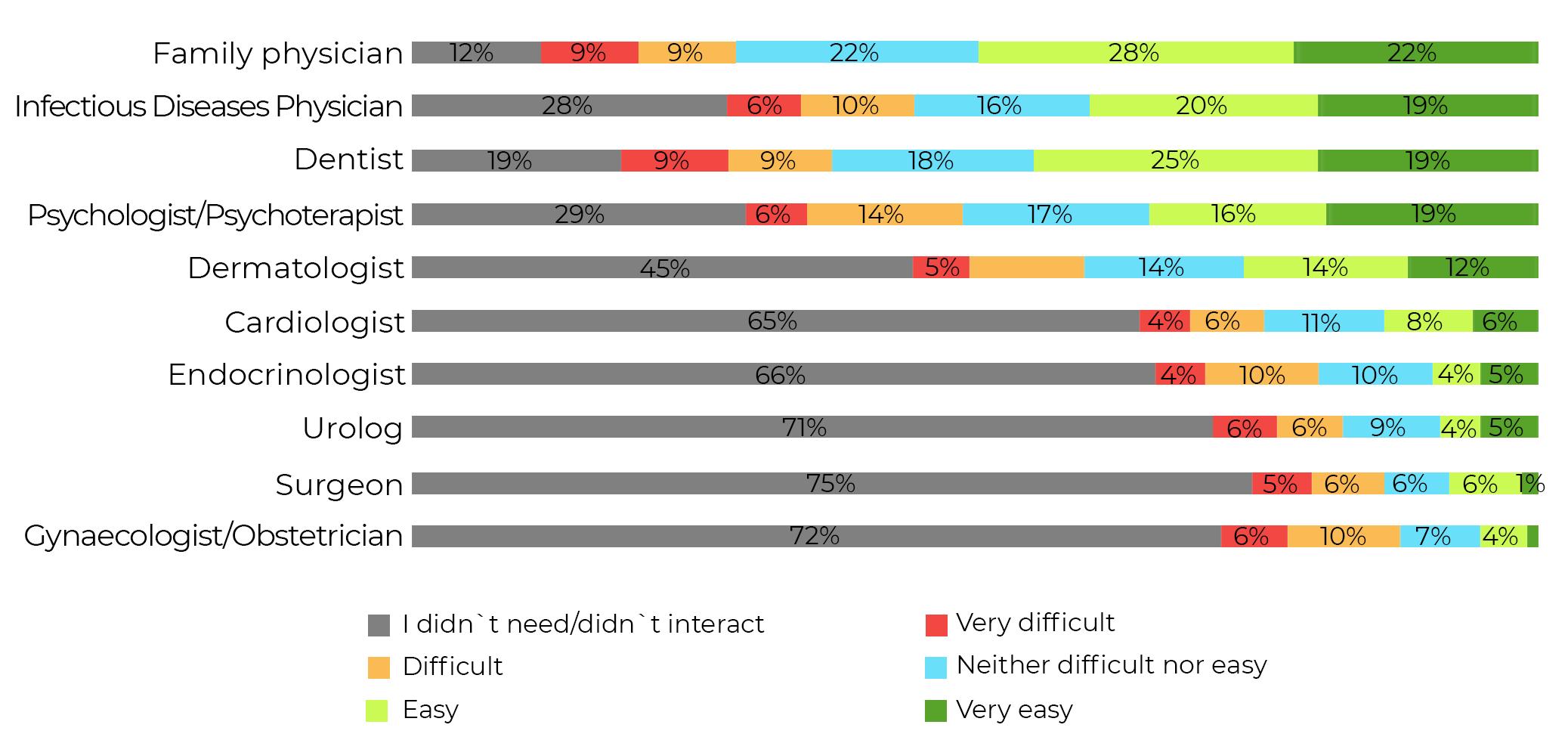
When it comes to accessing certain medical services/specialist physicians, half of the respondents have easy or very easy access to their family doctor. Other physicians accessed relatively easily are the infectious diseases physician and the dentist.
More than half of the respondents did not need or did not interact with any Cardiologist, Endocrinologist, Urologist, Surgeon or Gynaecologist
Which physicians have you interacted with so far and how easy was for you yo access that medical service?
24
According to the quantitative data, over the course of a year, the community members interacted most often with the Psychologist/Psychotherapist (on average 10 times per year, some respondents even dozens of times per year), the Family Doctor (on average 4 times per year), the Infection Doctor (3 times per year) and the Dentist (3 times per year).
Circle of trust of the person living with HIV



The qualitative research revealed that the presence of the psychotherapist is extremely important for all respondents included in the study. The positioning of the psychotherapist in the diagram of relevant people is with family members and close friends. The relationship with the psychotherapist is often described as honest, based on mutual respect and extremely helpful to PLHIV especially during the period of diagnosis and acceptance (first 6-12 months).
The relationship with the infectious disease physician is defined by the degree of professionalism of the physician (which cannot be easily assessed by the HIVpositive person) and the empathy shown towards the patient. The interaction between the HIV-positive person and the infectious physician is described as a distant relationship and contact between the patient and the physician occurs once every 6-12 months (coinciding with the time of the viremia and CD4 cell investigations).
25
An empathetic attitude on the part of the infectious disease physician and genuine interest in the patient’s problems are the two fundamental characteristics that contribute to strengthening the relationship of trust between the physician and patient.

The HIV-positive people interviewed are often anxious about interacting with the infectious disease physician; they often feel rushed, not actively listened to and unsure of the physician’s ability to recall each patient’s medical history.



I’m not sure my physician knows who I am, every time I tell him as much detail as possible so he can spot me... the problem is always time, he doesn’t have more than 5-10 minutes and things seem to be on a conveyor belt there. I would like to see that he asks me how I feel, that he actually cares about me as a person. (HIV+ LGB person)
Some HIV-positive people (especially respondents with higher levels of education) keep in touch with their infectious disease physician via text messages when needed. However, due to the pandemic context and the restrictions imposed by the authorities, some patients have not interacted with their infectious disease physician in the last 1.5 to 2 years.
In the last two years, many infectious disease physicians have been giving priority to coronavirus-infected patients and there has been a transfer of HIV-positive patients only to certain infectious disease physicians. This setup is a source of dissatisfaction both for the patients who feel “abandoned” and for the health professionals who feel they no longer have control over the therapeutic progress of their HIV patients.
Now, because of the pandemic, we have had to do some re-organisation, the vast majority of physicians are only dealing with Covid patients and we have kept only a small core of physicians dealing with the HIV patients. This nucleus consists of about 6 physicians who have to see 1500 HIV patients every month... and I no longer have direct contact with my HIV patients who I used to see every 1-3 months. (medical professional)
26
The role of NGOs
The role of the NGOs is also extremely important in the relationship dynamics of the HIV-positive person. Since the onset of the Covid-19 pandemic, the work of the NGOs has been hampered by the large number of requests received from PLHIV.

Access to the hospital was restricted and many of the questions from the HIVpositive patients were addressed directly to the relevant NGOs.
NGOs are invested with a lot of trust (both by the patients and the health professionals) when it comes to accurate, complete and always updated with relevant HIV information in the medical and social sphere
Preparing the necessary documentation to access various social benefits is another support activity offered by the NGOs in support of the HIV-positive persons
The role of emotional support, advocacy and membership of the relevant groups for the HIV-positive persons is also associated with non-governmental organisations.

The NGOs are seen as a binder between PLHIV and health professionals, often accompanying the HIV-positive patients when they first interact with health professionals
The quantitative research shows that for half of the respondents (54%) living with HIV is more of a disadvantage in accessing the health services, and 32% cannot judge whether it is a disadvantage or an advantage.
Similarly, for half of the respondents (53%), being part of the LGB/ MSM community is more of a disadvantage in accessing the health services, and 43% cannot judge whether it is in their favour or not when accessing the health services.

27
And for the majority of those from the Trans community (93%), their status is more of a disadvantage when they need to access a medical service.

Health services in Romania
On a scale of 1 to 10, the average level of satisfaction with the quality of the health services in Romania is 4.8, and the average level of trust in these services is 4.7, with the Trans persons and the persons practicing commercial sex giving the lowest scores (averages of approx. 3 and 2 respectively), the highest scores being given by drug users and homeless people (averages of 7 for quality of services and 6 for trust in these services).
The quality of care is described in terms of access to modern treatments with fewer side effects, easier administration (one pill a day) and less impact on the lifestyle of the HIV-positive persons.



PLHIV who took part in the current study believe that state-of-the-art treatments are now available in Romania. However, access to these treatments is sometimes considered to be preferential offered by the physicians especially in small towns or rural areas


I know that there are treatments with fewer side effects and that they are administered in one pill a day but my physician didn’t want to prescribe me this therapeutic scheme. ARAS encouraged me to ask for a newer (therapeutic) regimen, but the physician said he knew better. I kept hearing about the different gifts and attentions you have to give if you want to have access to better treatments. (LGB person, HIV+)
I know for sure that there are state-of-the-art treatments in Romania, but due to certain political and economic interests, some patients are still kept on outdated therapeutic schemes. I encourage everyone I talk to go and ask their physicians to reevaluate the need to change the treatment... especially when they are experiencing serious side effects. (social activist)
When it comes to personal experience with public health services, the intention to recommend the public health services in Romania to a friend is very low (average of 4.1).
28
Satisfaction scale: 1=Very dissatisfied, 10=Very satisfied
Confidence scale: 1=Not at all confident, 10=Very confident
Recommendation scale: 1=I would definitely not recommend, 10=I would definitely recommend

29
Section 2:

Contextualising the lack of antiretroviral treatment.

In terms of receiving treatment/prescription refills, this type of service is accessed on average 8 times per year, and the health monitoring tests take place on average 2 times per year (for 44 of the respondents, the tests were performed only 1 time per year, and for 15 persons, not at all).
In general, tests to monitor treatment are carried out at the request of the patient in 62% of cases or on the recommendation of the specialist/infectious disease specialist in 56% of cases.
Satisfaction with the current antiretroviral treatment is good (average 8.2, with half of the respondents giving a score of 10).
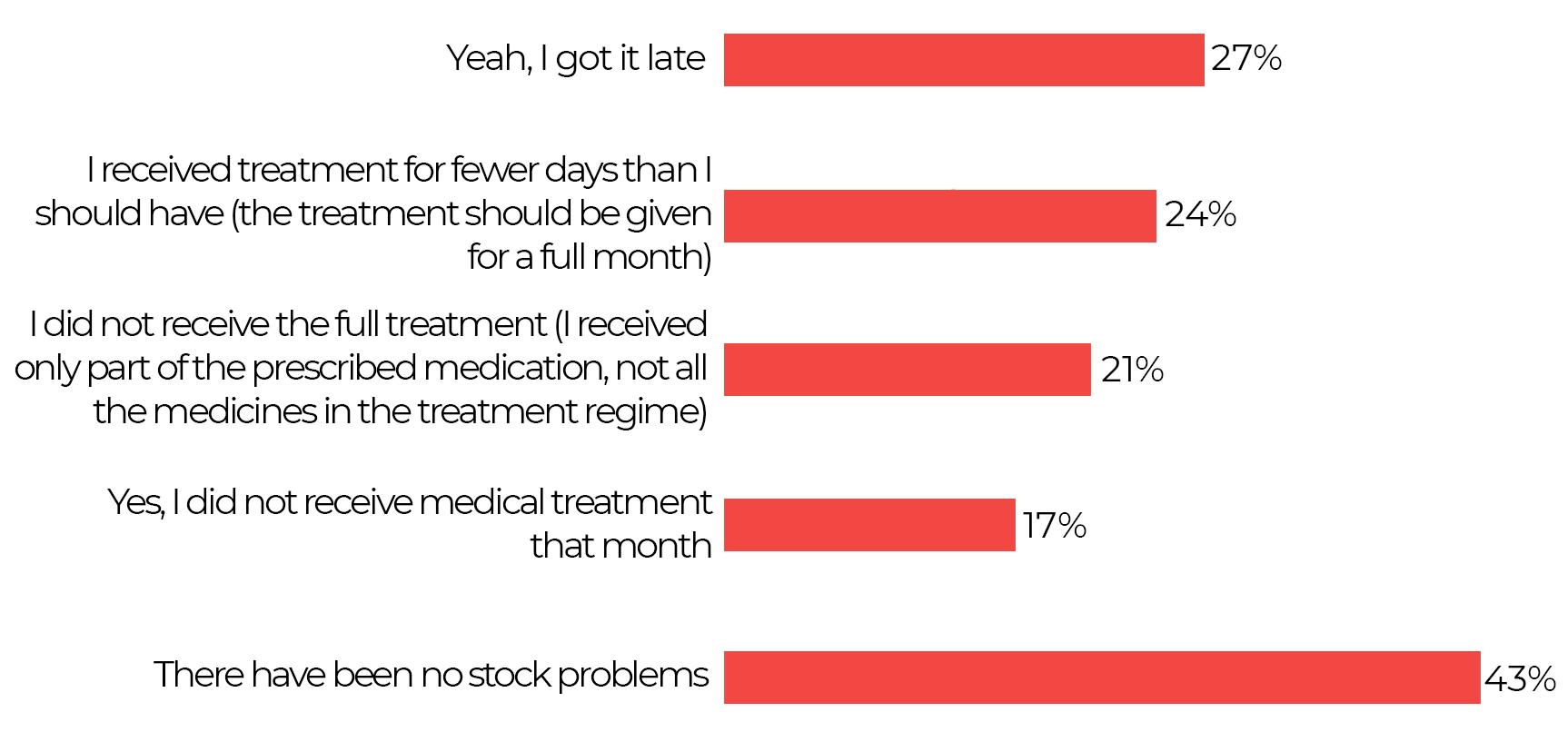
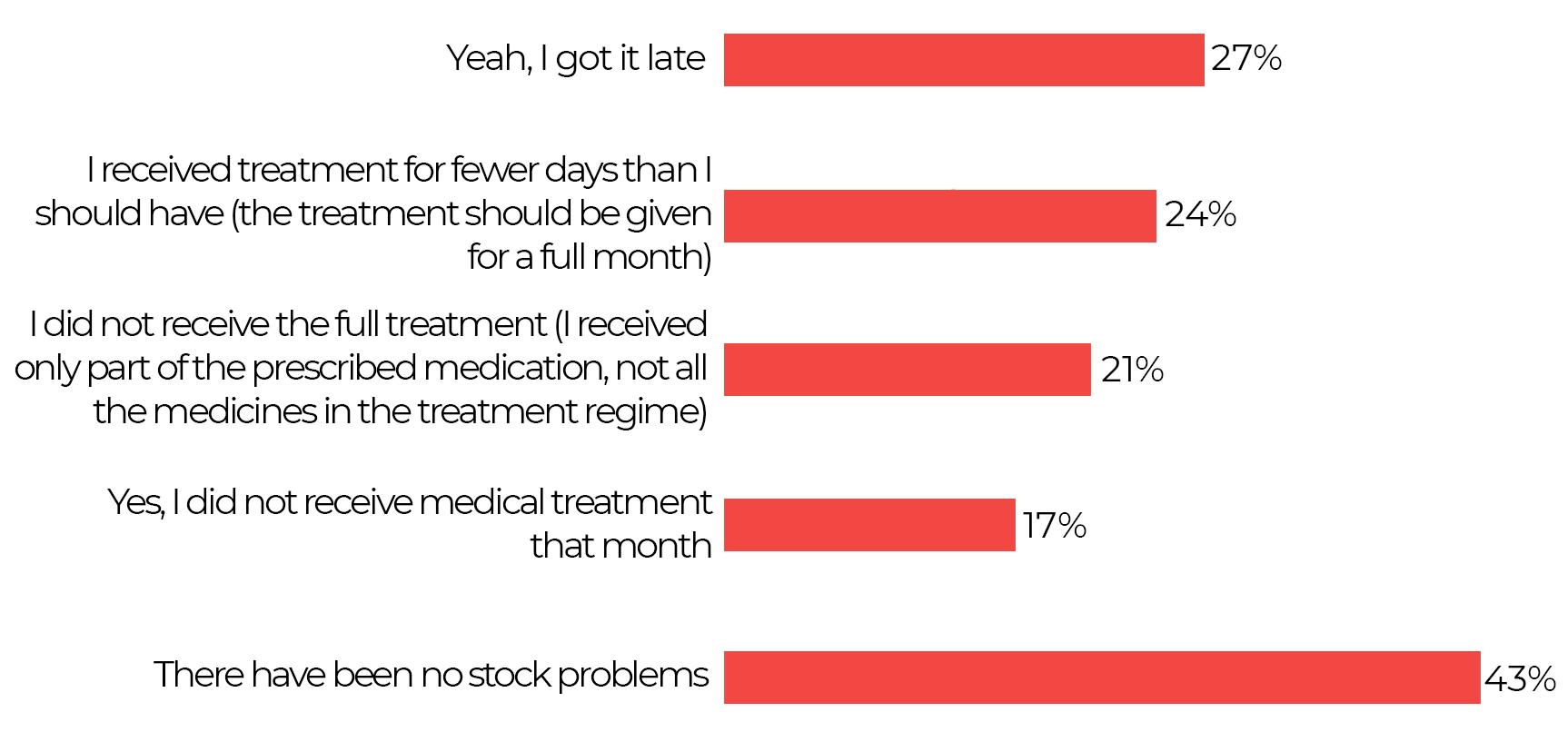
When asked if there were situations where treatment was not available, more than half of the respondents (57%) encountered problems: they received it late or for fewer days than they should have (treatment was supposed to be offered for a whole month) or they even did not receive the full treatment (they received only part of the prescribed medication, not all the drugs in the treatment schedule). In these situations, the patients have to create/build up a stockpile. 43% of respondents had no stock problems.
Availability of the treatment
30
In the pre-COVID period the patients were told on average twice a year that one or more of their medicines were missing, and in the COVID period these situations doubled in number (on average 4 times a year). n).





Coping with the lack of treatment has generated anxiety and fear among the HIV-positive persons (especially among newly diagnosed patients in the last 1-2 years) and there are various ways in which these patients try to acquire a reserve stock in order to avoid such future stresses: go to pick up their monthly treatment 2-3 days earlier and thus manage to save a few pills each month they try to buy a refill bottle from other countries but the cost is prohibitive for most of the respondents surveyed they try to borrow or buy from other HIV-positive persons if the treatment regimens are similar in desperate situations, they turn to Alina Dumitriu (Sens Pozitiv) for help in getting the treatment
Interviewees from the health system see the gaps in the provision of antiretroviral treatment as a consequence of the turmoil created by the Coronavirus pandemic. Basically, the whole medical system focused on treating Covid patients and they had priority over the chronically ill. The strategy of the medical system was decoded as one of ‘survival’ being highly reactive to the large number of Covid cases.
Since Covid-19, all we’ve done is survive and we’ve focused less on the quality of survival. We hope to get back to better times. (healthcare professional)


The representatives of the non-governmental organizations which were involved in this study are of the opinion that this “pill crisis” is not only rooted in a mismanagement of the logistical implications generated by the pandemic context, but is linked to an underbudgeting of the national HIV plan in the context of the non-existence of the National Strategy for Surveillance, Control and Prevention of HIV/ AIDS. The recurrence of the “pill crisis” occurs year after year and is not an isolated event generated by Covid-19, but accentuated during the


31
pandemic. Every year, the signing of the budget amendment is usually delayed and thus the whole logistical circuit suffers, and the stocks of treatment needed by the HIV-positive people are significantly reduced.

There is also the perception that the more social actors are involved in the decision making, the more diluted the responsibility will be and the final decision will be repeatedly delayed.

It’s no use that it falls under the responsibility of the Minister of Health because it has no power if it has no money to allocate to these treatments. Antiretroviral treatment is free for all HIV-positive patients and yet there are long periods when they do not have access to the treatment. The responsibility for providing this treatment should be in the hands of those who have the power of financial decision, those who sign the initial budgets and their amendments. (social activist)
The quality of life at this moment for the HIV-positive patients, with the current treatment, taking into account the services provided by the Romanian public health system, was evaluated at an average level (average of 6.4, on a scale from 1 to 10, where 1=very bad, 10=very good). The persons who practice commercial sex tend to have a significantly lower quality of life.
32
3: Understanding discrimination,

The main sources of information used to stay informed about HIV or other diagnosis (prevention, disease, health status) are the Internet/search engines (Google, etc.), NGOs, the Internet – specialized websites and the specialist (the specialist being a source used significantly more by the heterosexual persons).

Information sources - HIV/other diagnostics

Regarding the sources of information used to stay up to date with the information about the treatment and the health services, the preferred ones are the Internet, the specialist physician and the family doctor (especially the LGB persons tend to access the various sources more, compared to Trans persons, sex workers, drug users).
Specialized Internet sites, NGOs and Social Media are sources of information used to a significantly greater extent by Sex Workers to keep up to date with information related to HIV or other diagnosis. The Psychologist/Psychotherapist
33
Section
prevention, information and the interest of the persons living with HIV in the context of the legal framework in Romania
and the persons with the same diagnosis are sources of information that are significantly more used by the persons aged 18-25 when they need information about treatment and medical services.

The fact that the Internet is the main source of information accessed shows the need for effective national information campaigns to encourage people to access official sources, and at the same time to understand which sources are relevant in order to access accurate, up-to-date and useful information. The fact that the NGOs are at the top of the list of preferred sources could facilitate a close collaboration between the NGOs, the state and the health professionals.

Discrimination
1 Intersectionality = “analytical tool for studying, understanding, and addressing the ways in which sex and gender intersect with other personal characteristics/identities and how these intersections contribute to unique experiences of discrimination.” (https://ec.europa.eu/info/sites/ default/files/a_union_of_equality_eu_action_plan_against_racism_2020_-2025_ro.pdf )

34
The anxiety regarding the access to health services by PLHIV is strongly rooted in the “Intersectionality” 1 of different social identities that can generate discriminatory behaviors among the health professionals. The lower
Surse de informare - tratament și servicii
the educational level of the HIV positive persons investigated and the more overlapping social identities (sexual orientation, ethnicity, socio-economic status, etc.), the more they will experience fear of the interaction with the health professionals.

There is a preconception that the attitude of the health professionals is rather distant, authoritarian and lacking empathy towards the patients in hospitals. When a highly socially stigmatising pathology (HIV+) and a sexual orientation other than the heterosexual one also plays a role, the risk of discrimination and aggressive behaviour (verbal, emotional) increases significantly.
...he/she shouted after me ”Mister” like it was the first time he/she had seen me and I was dressed just like I am now, in girl clothes and I have long hair and I was wearing make-up. They just don’t want to respect that I feel like a woman and they always talk dirty and I get reprimanded when I go for my treatment. (LGBT person, sex worker, HIV+)
I went to the hospital in my home town with a friend who had been bitten by a bee and was feeling sick and we went to the emergency room and when the nurse came in, he told her he was HIV positive and she shouted across the corridor to another nurse ”Be careful, he’s an AIDS-person, don’t touch him... you can tell from far away that he has AIDS”. (LGB person, HIV+)
When discussing the legal framework which assesses/manages cases of discrimination, 6 out of 10 respondents are aware of this type of information, but only 12% of respondents have also taken such steps when they/ someone else in the community has been discriminated against.

Do you know information about the legal framework that assesses/deals with cases of discrimination?


35
For cases of discrimination of any kind (gender, race, etc.), people in the community prefer to turn to anti-discrimination NGOs in 54% of cases, or to the CNCD = National Council for Combating Discrimination in 42% of cases.

Although they know which authorities can help them report a discriminatory behaviour, most HIV-positive persons prefer not to do so for fear of exposure. Most often they seek help from the NGOs and ask them for legal support to solve their problems, without agreeing to come forward and file a formal complaint.
The vast majority of respondents, almost 80%, believe that the incrimination2 of HIV transmission makes access to HIV testing/treatment services more difficult/ influential.

Exposure of HIV-positive status
There are three factors that determine the exposure of HIV-positive status especially when accessing health services. Most respondents interviewed declare their HIV+ status out of concern for their own health status as well as the health status of others.
2. Article 354 of the Criminal Code: “(1) The transmission, by any means, of acquired immunodeficiency syndrome – AIDS – by a person who knows that he/she suffers from this disease shall be punished by imprisonment from 3 to 10 years.”

36
Who do you turn to in cases of discrimination of any kind (gender, race etc.)?
Legal framework: Few people living with HIV see the legal framework as the main motivating factor for declaring their HIV+ status. Some respondents consider it a legal obligation to declare their HIV-positive status though, others consider it <slightly abusive> because their confidentiality is violated and once declared, they risk hostile attitudes.

Care for others: even though there are well-established protocols for the protection of health professionals (wearing masks, surgical gloves, etc.), certain HIV-positive persons feel the need to draw the attention of the health professionals so that they can protect themselves properly.
In couple relationships, even when the HIV-positive person is undetectable (i.e. the virus is not transmissible), they still feel the need to share this information with their partner as a sign of respect and care for their relationship.


Caring for oneself: the declaration of HIV-positive status is often initiated by patients in order to ensure that the physician will take this diagnosis into account when conducting clinical investigations and recommending treatment. There are multiple drug interactions that HIV-positive patients fear could have a negative impact on their health. Most are of the opinion that this exposure of the HIV+ diagnosis brings the risk of hostile/discriminatory behaviors but prefer to choose the <most manageable evil>.
The medical professionals investigated are of the opinion that this diagnostic confidentiality is not violated because there are now well-established protocols by which the physician can have access to the patient’s medical history in order to treat him/her: during the consultation, the physician will ask the patient what other treatments he/she is currently taking and, depending on his/her answer, he/she will know exactly which treatment to prescribe in order to avoid drug interactions that may be harmful to the patient.
We have very clear protocols that guide us to ask the patient what other treatments they are currently undergoing. Depending on the patient’s answer, we will also find out about the HIV+ diagnosis immediately without forcing the patient to reveal this to us. In this way, we will be able to immediately recommend a treatment that does not interfere with the patient’s current treatment”. (healthcare professional)
Social activists believe that there is a clear protocol regarding the protection of healthcare professionals when interacting with their patients: physicians, nurses and any healthcare professional must take
37
all protective measures as if the patient in front of them might have an infectious disease. Some of those interviewed believe that HIV-positive patients should not be asked if they are HIV+ in order to avoid exposure to potential discriminatory behaviour.

The physician must behave as if all their patients are possible carriers of HIV, hepatitis, etc. They must wear gloves, a mask and have a whole protocol which if they follow, they will be perfectly safe. I don’t understand why the patient has to declare whether they have HIV or not... this is a violation of the confidentiality of the diagnosis and then the patient risks hostile or aggressive behaviour. (social activist)
HIV Prevention
Both PLHIV interviewed and the social activists involved in this study are of the opinion that ”HIV prevention” in Romania is an almost non-existent topic and this initiative is rather left to the NGOs.

In the context in which Romania has been lacking for several years a national strategy for the surveillance, control and prevention of HIV/AIDS cases to be approved by the Government, the subject of prevention is not widely addressed.
Health professionals support initiatives that address HIV prevention in Romania but believe that these initiatives should be coordinated at ministerial/government level so that there is alignment and consistency in the information provided to the general public.
They believe that prevention can only be achieved through integrated public information and education campaigns on HIV and AIDS.
NGO efforts in this direction are conditional on the availability of their own resources. There is very little testing capacity among hospitals and the testing services provided by NGOs are insufficient.

The Semper Musica Association is mentioned as an example of ”good practice” because it has managed to implement various actions in high schools to discuss the topic of HIV and methods of prevention in the spread of this virus.

8 out of 10 respondents have heard about PrEP (pre-exposure prophylaxis to HIV infection), the vast majority (97%) consider that the introduction of PrEP in

38
Romania is important, and almost unanimously (99%) the community members who were included in the survey consider that it is important that this protocol is communicated and explained within the community (for 92% of them it is even very important, and especially for HIV positive and LGB persons).


PrEP involves the use of an HIV/antiretroviral drug by an HIV-negative person to prevent HIV infection. The anti-HIV drugs in PrEP stop the replication of the virus in case of sexual contact with an HIV-positive person. Access to PrEP and information about this prophylactic measure can positively impact the intimate and social lives of the persons living with HIV.
Moreover, 94% of respondents say that it would be useful to organise a national campaign to promote this protocol.
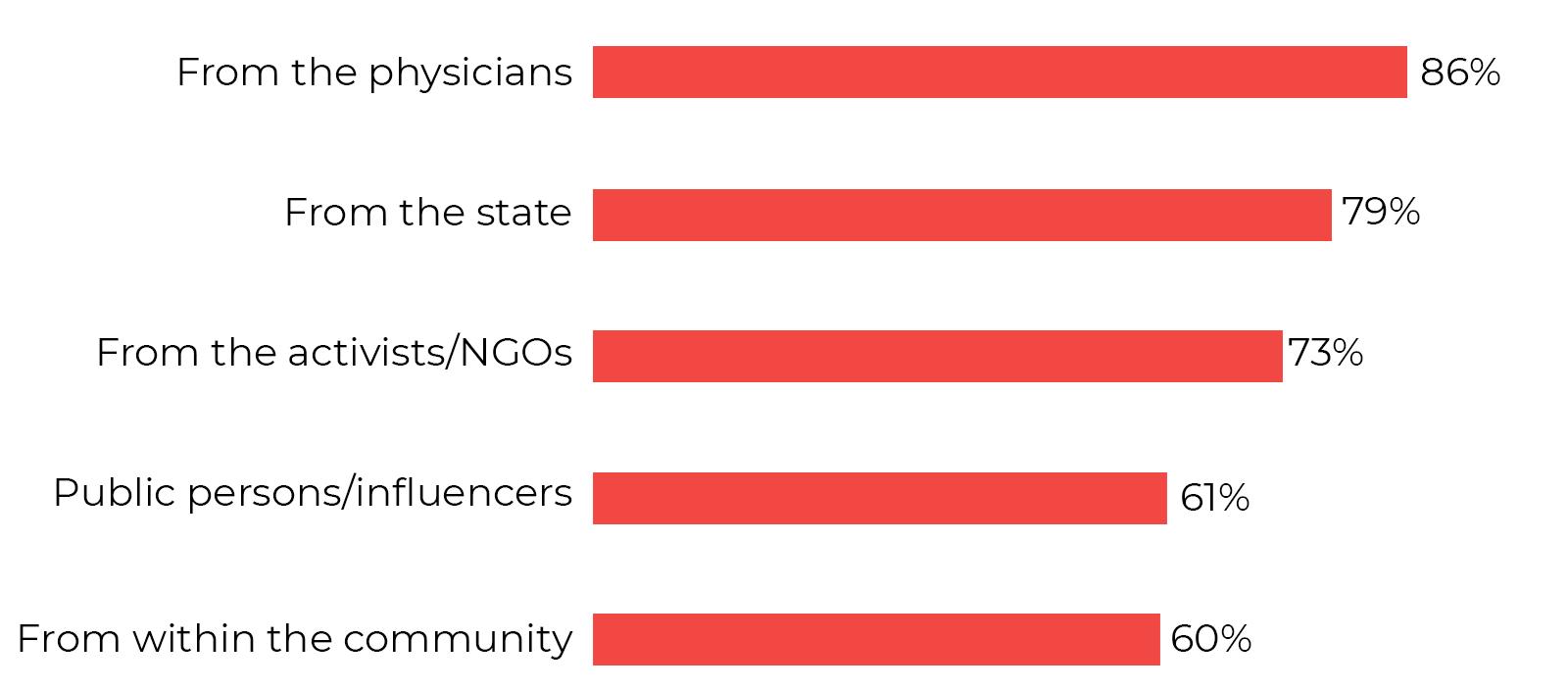
The respondents believe that this information about PrEP should come mainly from physicians and the state, and that the activists/NGOs would come third in this ranking.
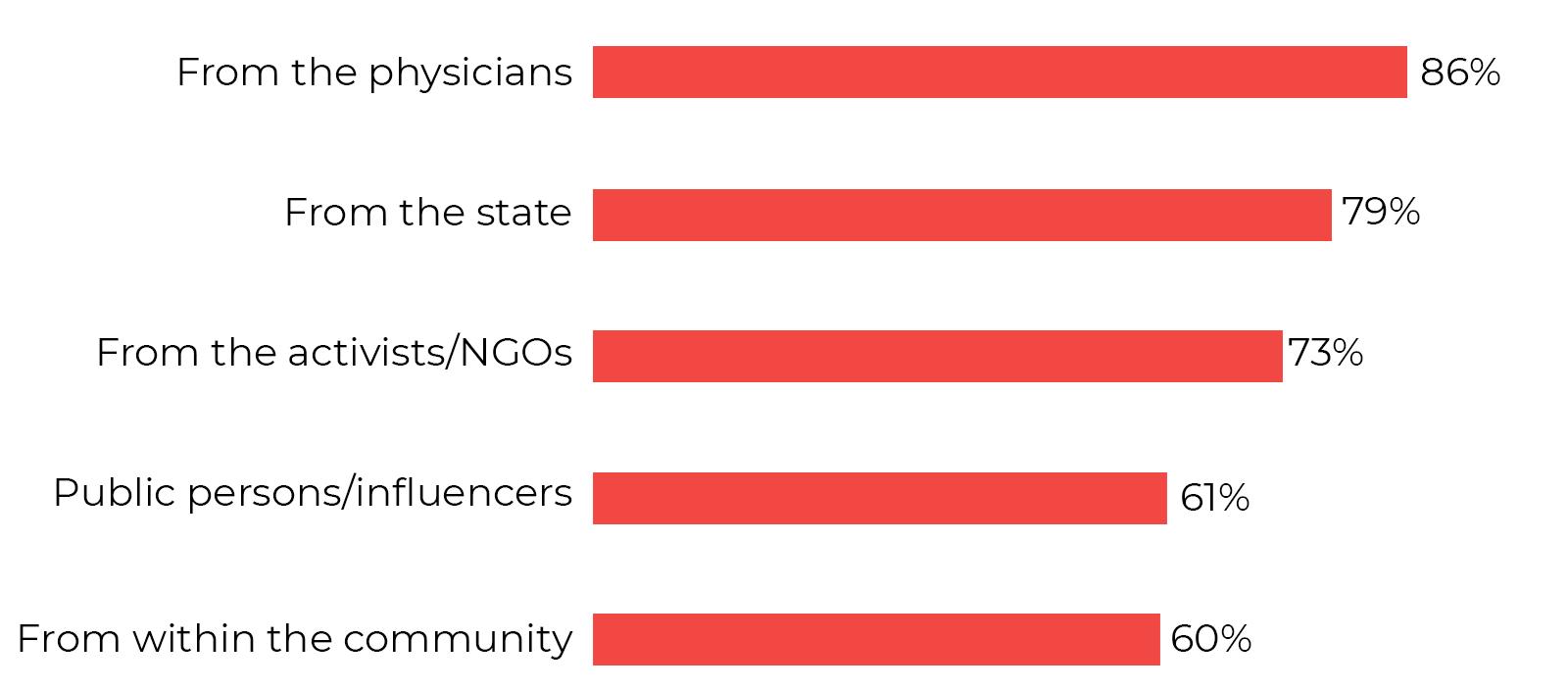
From whom should information about PrEP come
In the Top 3 biggest problems faced by the Romanians, the respondents included access to health care, access to education and access to equality, without any restriction of status, race, gender, etc. (non-discriminatory access to work, access to public and private services, etc.). Access to legal advice (particularly important for LGB persons and those aged 18-25) and access to free expression follow in the ranking. Access to equality is particularly important for PLHIV and persons who use drugs
39
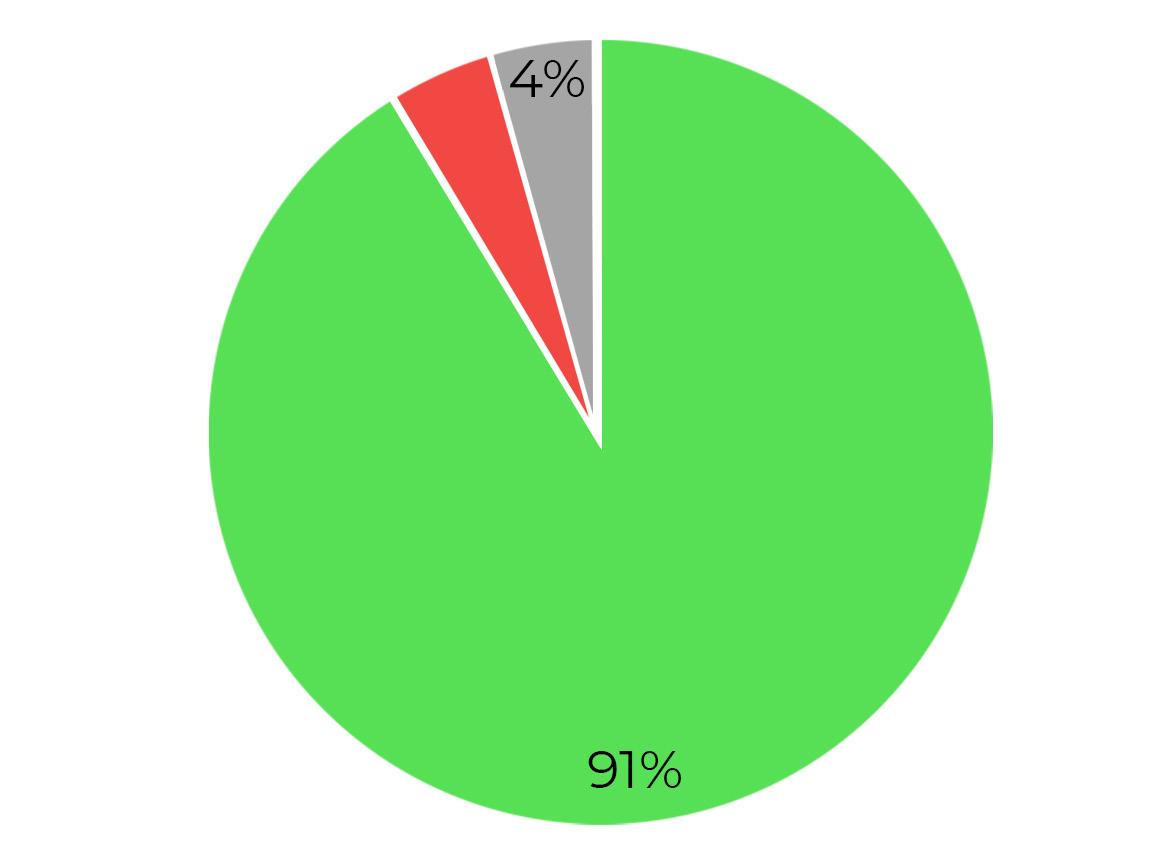
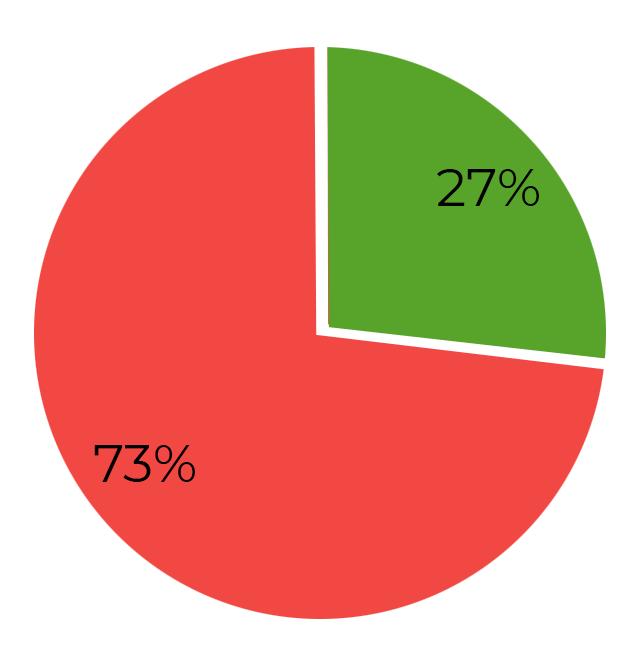
Regarding sex education/health education in schools, 73% of the respondents did not have access to this type of education in school.
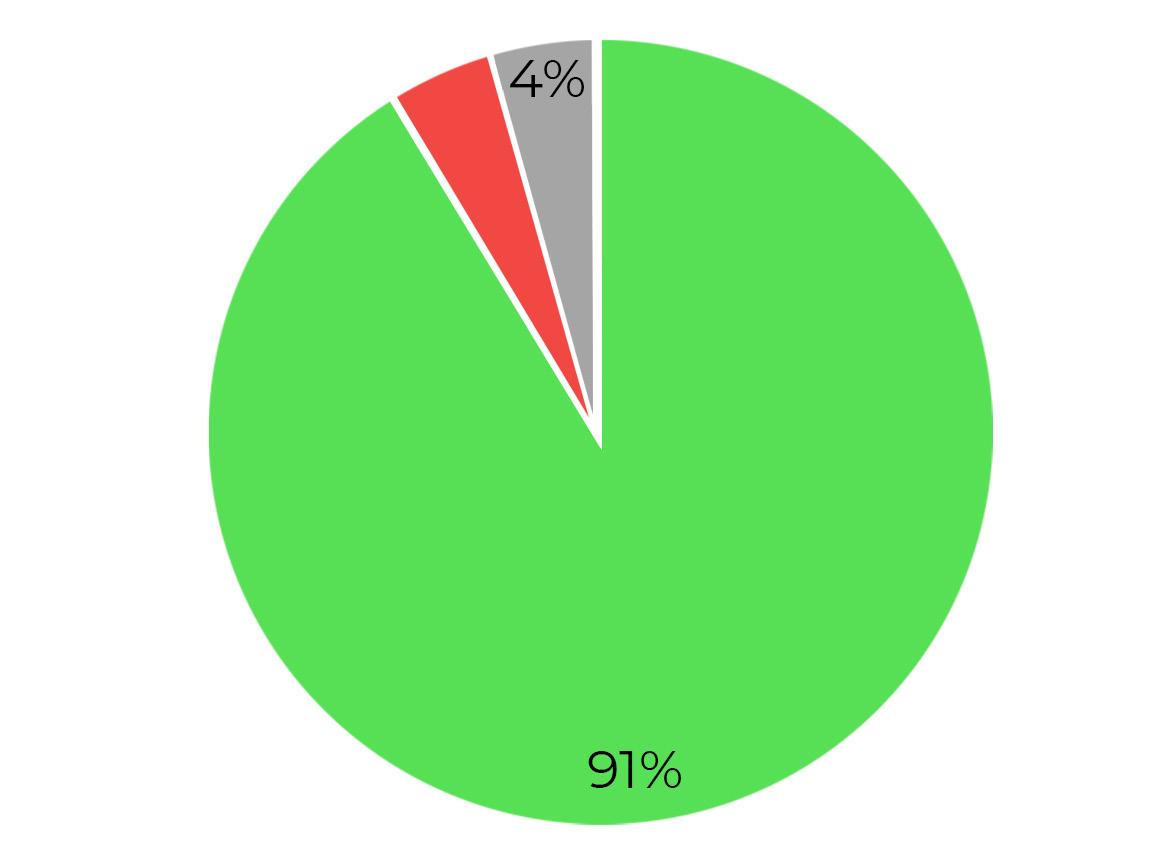

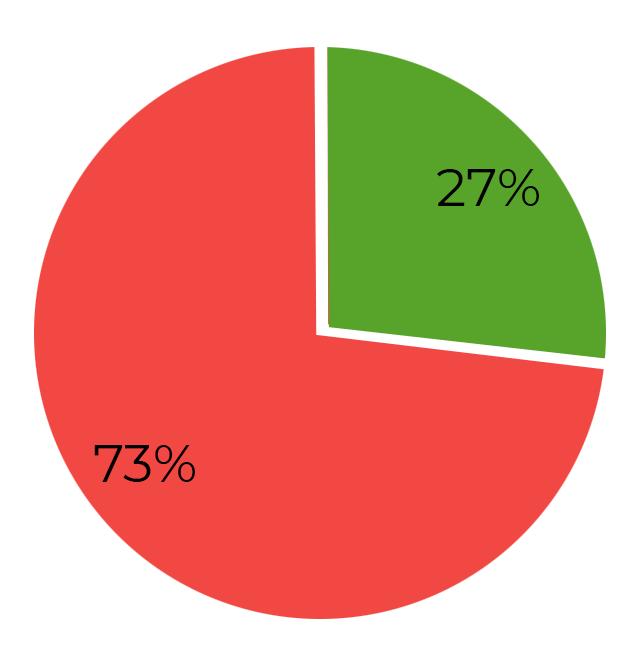
Have you had access to sex education/health education in school?

91% of the respondents believe that sex education/health education definitely contributes to a healthier population.
Do you think that the access to sex education/health education is necessary/ contributes to a better health of the population?
40
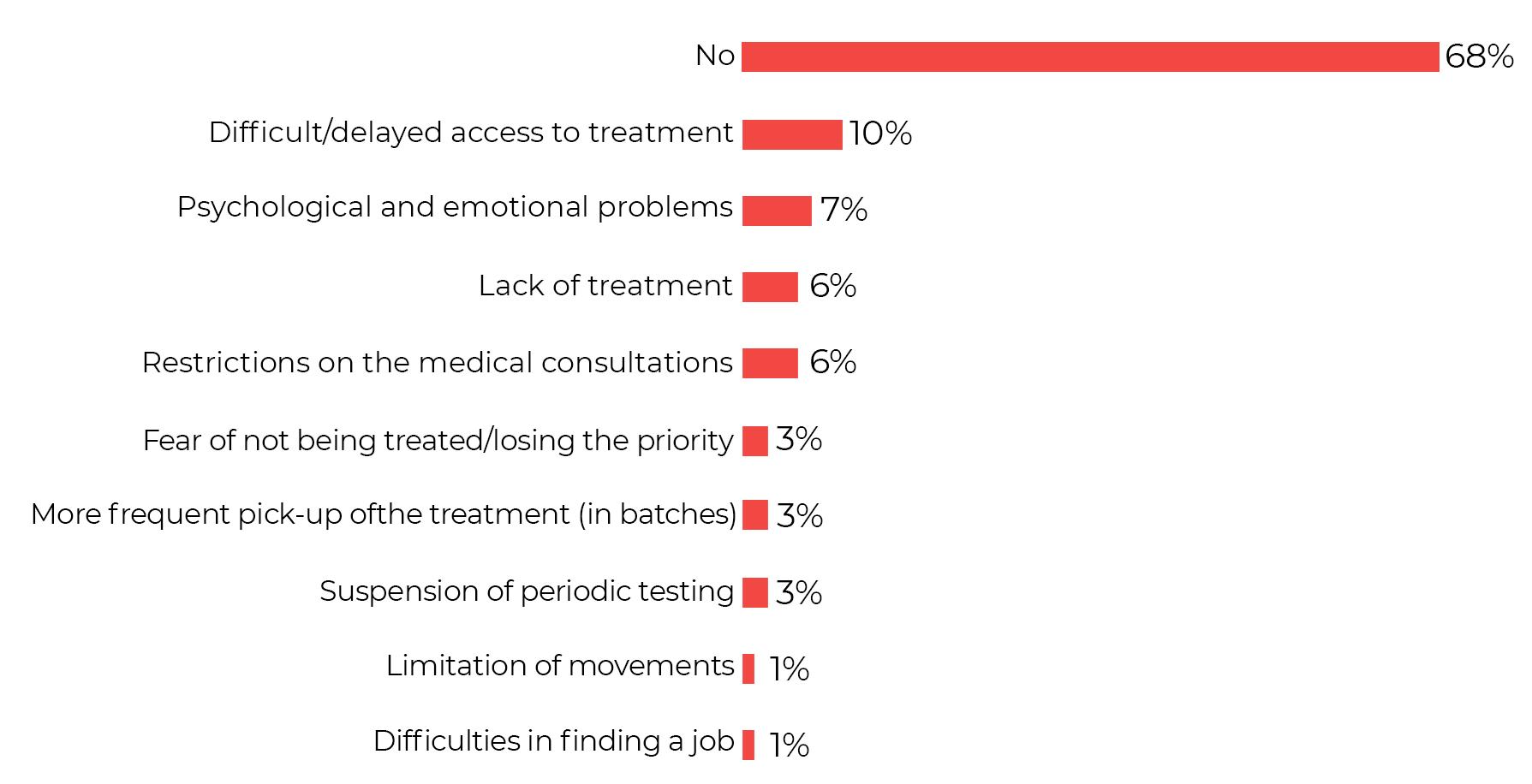
Impact of Covid-19
The impact of the COVID pandemic was felt mainly through restricted access to the health services (hospital, doctor, tests), the medical system was blocked and the lack of organisation was felt. Patients were also affected by the hampered/ delayed access to treatment. Some patients lacked proper communication with health professionals, some feared the way in which COVID could impact HIVpositive persons, they needed psychotherapy more often, chronic diseases were sometimes neglected by the specialists, exacerbations occurred following the COVID infection.
An interesting response was the opinion of one patient: “It seemed to me that the GP didn’t consult as often anymore, but just gave referral notes.”


Psychologically, PLHIV lived with the fear of getting sick, anxiety, a sense of unpredictability, putting off everything that could be put off.
Certain patients felt a positive impact, through the respect for confidentiality (e.g., no more shouting of names in the corridor) or by receiving treatment for 3 months and having an easier access to doctors through online consultations.
What impact/implication have you experienced as a result of the COVID pandemic in terms of access to healthcare?

41
Other implications experienced as a result of the COVID pandemic, related to HIV patient status, were:

Psychological and emotional problems (fear, insecurity, social marginalization)
Lack of treatment (“Lack of specific drugs was motivated by the diversion of funds to fight COVID”)
Restriction of medical consultations (difficult access especially to specialist physicians)
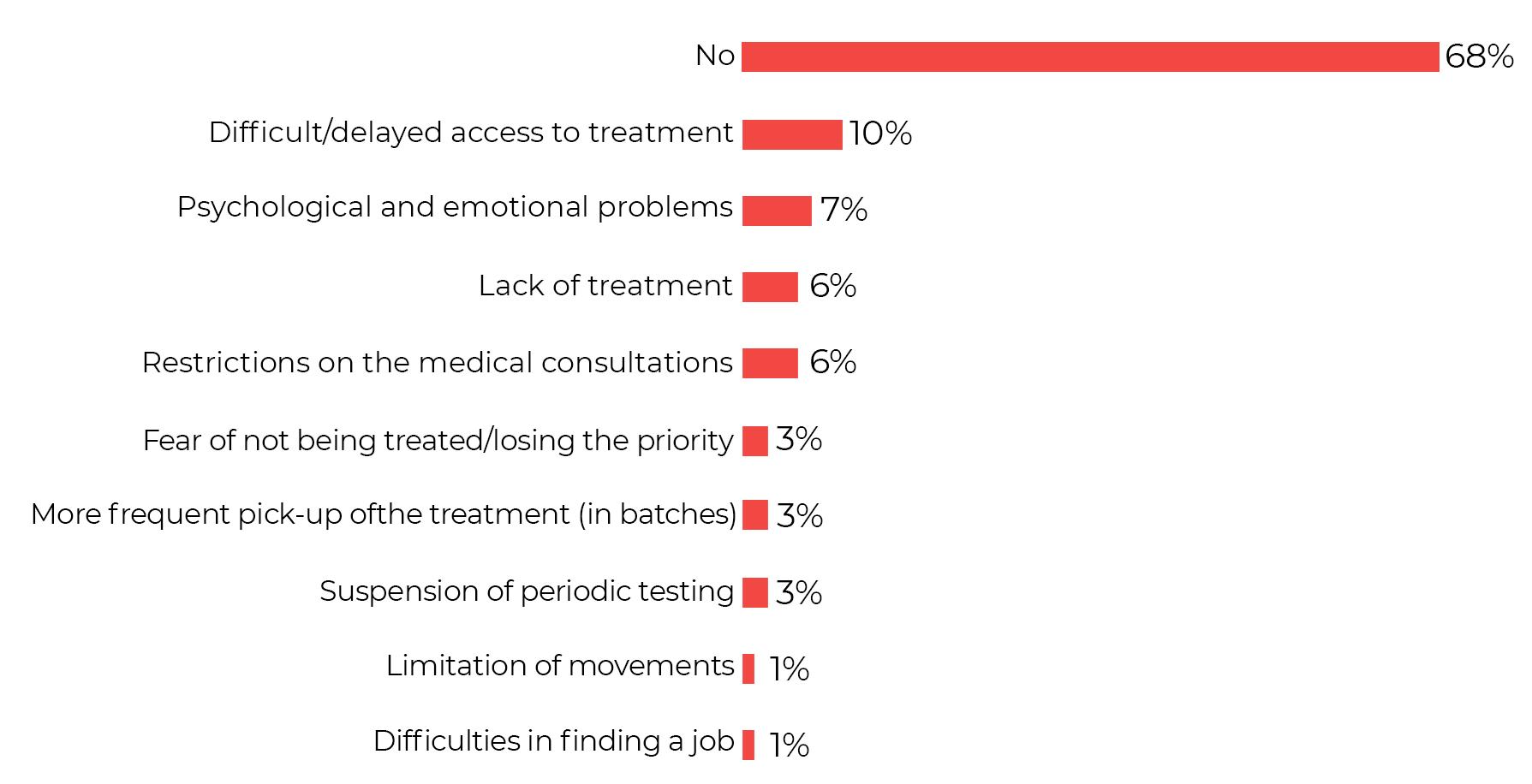
Fear of not being treated/no longer having priority (“initially the anticovid vaccine eligibility database does not communicate the HIV patient eligibility”)



Were there any other implications, felt in the aftermath of the COVID pandemic, related to your status as an HIV patient?

42
Section 4: Conclusions of the sociological research
The main fear and difficulty of PLHIV resides in the social stigma (84%) that feeds the discriminatory behavior (79%) among the general population and specifically even among the health professionals.
Discrimination arises as an effect of the intersectionality of different social identities and HIV-positive status: HIV/AIDS has a strong social stigma associated with it, on top of which overlaps the sexual identity, socio-professional status, ethnicity, etc. The more overlapping social identities there are, the greater the risk of discriminatory behavior.
Although aware of the existence of certain rules and laws aimed at protecting people living with HIV, PLHIV prefer not to seek help from the authorities because they fear public exposure. They often turn to the NGOs (54%) for help and guidance
The respondents surveyed believe that there are inconsistencies in the way these laws are implemented in practice and there is no effective control procedure to redress the discriminatory and illegal behavior.
Life with HIV is an overwhelming emotional rollercoaster and the difficulty in managing it does not come from the medical challenges associated with HIV, but rather, from the social and emotional ones: rejection, lack of belonging, feelings of loneliness, anxiety, depression, guilt projected by others onto persons living with HIV and internalized by them, etc.
The HIV-positive person’s circle of trust is limited and the specialist physician is often not invested with a priority support role. Family, friends, NGOs and the psychotherapist are part of the emotional support team accompanying the HIV+ patient’s journey.

The involvement of the NGOs in the dynamics of the relationship between HIVpositive patients and the health system is very important because the social activists are invested with the role of ”Patient Navigator”3 .
3.The navigator is the person who helps the patients to understand and accept their illness, explains the therapeutic pathway, helps them with their medical file, accompanies them to medical check-ups and explains the results of the medical investigations; tries to motivate the patient by presenting success stories and offering emotional support.

43
There are discrepancies between the experiences of PLHIV and the statements of health professionals when discussing the lack of treatment:

he HIV-positive patients notice a recurrence of the lack of treatment and often become anxious because they feel their lives are in danger; their emotional burden is high and fear dominates the health professionals speak more about the lack of financial resources and logistical gaps that have been further affected due to the pandemic situation; emotional burden is rather reserved and optimistic about the future
With the support of NGOs, most patients have identified possible solutions they can turn to when they do not receive full treatment. These emergency solutions are not made available to the patients by the state authorities, but are the result of the individual efforts of the patients and various social activists involved in the fight against HIV/AIDS.
In terms of the currently available therapies, most treatments are perceived as modern, effective and with high tolerability profiles. However, access to these modern therapies is still difficult, especially outside Bucharest, and it is the patients who have to insist on more easily administered treatment regimens with fewer side effects.
The HIV/AIDS information and prevention campaigns are considered important and necessary by all participants in the study. Currently, there is no centralized effort in Romania towards HIV/AIDS prevention. The state authorities have difficulties in implementing large-scale education and information campaigns and the NGOs have financial limitations because their efforts are self-sustained without external support.
The context of the Covid-19 pandemic has destabilised the medical routine of the HIV-positive patients, who have encountered multiple difficulties in accessing the medical services and the availability of antiretroviral treatment.


44
IV. Legal research
Section 1: General aspects


1.1 General aspects
The general legal framework applicable to the situation of the persons living with HIV and the fight against the spread of the virus is based on Law 584 of 29 October 2002 on measures to prevent the spread of AIDS in Romania and to protect the persons infected with HIV or suffering from AIDS (“HIV Law”) and its implementing regulation of 24 November 2004 (“HIV Law Implementing Regulation”). The two laws generally concern the division of tasks between various governmental bodies and state institutions, but also include a number of provisions concerning the rights and obligations of the persons living with HIV and issues of confidentiality in the medical and professional sphere. The HIV Law regulates the process of developing National Strategies for the Surveillance, Control and Prevention of HIV/AIDS (“National Strategies”). According to an earlier form of the HIV Law and the still in force form of the Regulation on the Implementation of the HIV Law, the National Strategies should be developed by the National Commission for the Surveillance, Control and Prevention of HIV/AIDS (“National HIV Commission”).1
A system of legislation for ensuring THE access to medical treatment is in place, starting with Law 95/2006 on health reform (“Health Law”), which includes the HIV/AIDS-specific treatment within the intervention areas of national public health programs (“National Public Health Programmes”). These national health programs are key to providing the necessary funding for free access to the appropriate treatment – they are drawn up periodically by the Ministry of Health with the participation of the National Health Insurance Fund. In the field of HIV/AIDS, there is a separate national program called the National Programme for HIV/AIDS Prevention, Surveillance and Control. An important role in regulating the access to medicines is played by the technical norms for the implementation of national public health programs (“Technical Norms for the Implementation of National Programmes”). There is also Law 46/2003 on
1. The legal situation of the National HIV Commission is unclear given the abrogation of Article 4 of the HIV Law, but the other references and powers of the Commission remain in force. These issues are discussed in Chapter 2.5 below

46
patients’ rights, a normative act which establishes the rights of the beneficiaries of health services.
In terms of social protection, the persons living with HIV or AIDS receive a monthly food allowance – the methodology for granting this is established by the order of the Minister of Labour and Social Solidarity and the amount is set by government decision. Currently in force is the Methodology for granting the monthly food allowance to adults and children infected with HIV or AIDS and for controlling its use by those entitled to it, approved by Order no. 223/2006 (“Methodology for granting the food allowance”) and its amount is currently established by Order 1177/2003 approving the amount of the monthly food allowance for persons infected with HIV or AIDS (“GD on Food Allowances”). In the case of children for whom special protection measures have been established, the sum of the amounts due under Law 272/2004 on the protection and promotion of the rights of the child (“Law on Child Protection”) is increased by 50% in the case of children infected with HIV or AIDS.
Romania’s anti-discrimination legislation, specifically Ordinance No 137 of 31 August 2000 on the prevention and sanctioning of all forms of discrimination (“Anti-Discrimination Law”), explicitly states HIV status as a characteristic in relation to which discrimination is sanctioned.
In the area of criminal law prosecution, Romania continues to criminalise the “transmission of AIDS” through the offence of “transmission of acquired immune deficiency syndrome” in Article 354 of the Criminal Code. At the same time, the Criminal Code provides as an aggravating circumstance the commission of other offences for reasons related to HIV/AIDS infection and establishes the restriction of the exercise of the rights of persons infected with HIV/AIDS as a separate ground for the offence of abuse of office.
1.2 HIV law and main legal milestonese
From a formal point of view, the HIV Law sets out the main coordinates of the Romanian state’s response to the spread of the virus and the protection of PLHIV:
(i) Assignment of ministries and public authorities – designates the main State authorities with responsibilities in this area, in particular2:


2. The current names of the relevant entities at the time of drafting this material are used

47
Ministry of Health
Ministry of Labour and Social Solidarity – under which the Authority for the Protection of Persons with Disabilities (also designated) operates








Ministry of Family, Youth and Equal Opportunities – under which the Authority for the Protection of Children’s Rights and Adoption operates


Ministry of Education
The following are also designated:
National Health Insurance House
Romanian College of Physicians
Romanian College of Pharmacists
County and Bucharest Public Health Directorates
Hospitals (public or private) and schools (public or private).
(i) Establishment of the National HIV Commission – the original version of the HIV Law established the National HIV Commission, an inter-ministerial body to plan and monitor the implementation of the Government’s HIV/ AIDS policy.

(ii) Establishment of formal measures and objectives – the law establishes two categories of measures:








Measures of preventing the transmission of HIV infection – which generically include:
Educating the population on how HIV is transmitted
Mandatory provision of the necessary precautions and means in all health facilities
Mandatory provision of means to prevent mother-to-child transmission of HIV infection
Obligation for all mass media to promote the use of condoms free of charge on a quarterly basis to prevent sexual transmission of HIV infection
The provision by the employers of the post-exposure prophylaxis free of charge
Social protection measures – which follow the two main coordinates: Unrestricted and unconditional right to work and non-discriminatory career advancement

Respect for the right to education

48
In concrete terms, however, while the HIV Law establishes the right to a monthly food allowance, the amount of which is set by government decision.
(iii) Regulation of confidentiality relationships – the law sets out the principles of the right to confidentiality and the obligation of the employers, officials and employees of the health networks to respect this right. On the other hand, the law establishes the obligation of the patients to inform the health care personnel of their HIV status.
(iv) Financing the prevention activities and protection measures – the law states that the budget of each relevant ministry must include a separate chapter for financing prevention, education and social protection activities. At the same time, the law establishes that therapeutic and health care activities shall be carried out from the budget of the Ministry of Health free of charge
1.3
Allocation of tasks to authorities according to the HIV Law Enforcement Regulation
The HIV Law Enforcement Regulation is the legal instrument that sets out the government institutions with responsibilities for the HIV Law enforcement.

The table below illustrates a number of actions and tasks prescribed by the legislation in which the various authorities are charged with duties:
Duties
Preparation or, where appropriate, participation in the preparation of draft legislation governing:
a) measures to prevent HIV transmission;
(b) social protection measures for persons infected with HIV or AIDS;
(c) confidentiality of data relating to HIVinfected persons;


Responsible authority3
Ministry of Health Ministry of Labour, Social Solidarity and the Family Ministry of Education and Research Ministry of National Defence Ministry of Administration and Interior Ministry of Justice
3. The names in the tables are based on the names in the legislation - their powers have been transferred through successive takeovers of portfolios by the current authorities.

49
d) appropriate treatment of HIV-infected persons eligible for treatment;
(e) specialist training and the development of medical research in this field;
(f) financing of activities for the prevention of HIV transmission and treatment of PLHIV, as well as social protection measures for the affected persons.
Elaboration and proposal to the Government for the approval of the National HIV/AIDS Strategy
Ministry of Transport, Construction and Tourism
General Secretariat of the Government Chancellery of the Prime Minister
Development of the national HIV/AIDS prevention, surveillance and control programme and measures to reduce the social impact of HIV/AIDS cases.
National Commission for HIV/AIDS Surveillance, Control and Prevention Ministries and institutions with responsibilities in the field and/or with their own health network

Carrying out research in order to determine the groups at risk
Ministry of Health, in collaboration with:
Ministry of Labour, Social Solidarity and the Family, Ministry of Education and Research, National Youth Authority, National Agency for Sport, National Authority for Child Protection and Adoption, National Authority for Persons with Disabilities, National Health Insurance House, Romanian College of Physicians, Romanian College of Pharmacists
50
Informing the population and training the medical and auxiliary personnel on universal precautions and means to prevent HIV transmission
Informing the population and training the medical and auxiliary personnel on universal precautions and means to prevent HIV transmission
Mandatory means of preventing motherto-child transmission of HIV infection, including:
- measures of ensuring the free counselling and testing of pregnant women
- provision of antiretroviral treatment for pregnant women infected with HIV or AIDS
- clinical and laboratory monitoring of newborn babies born to mothers infected with HIV or AIDS, - and any other measures necessary for lowering the risk of mother-to-child transmission of HIV infection
Ministry of Health Ministry of Health Ministry of Health
Development of a list of professions and activities at risk of occupational exposure to HIV infection

Monitoring of compliance with the obligation of all health facilities and physicians, regardless of their form of organization, to admit and provide medical care for HIV/AIDS-infected patients and
Ministry of Health Ministry of Labour, Social Solidarity and the Family
Ministry of Health National Commission for HIV/AIDS Surveillance, Control and Prevention
51
take appropriate action against those guilty of non-compliance with this obligation
Activities aimed at ensuring the continuous training of health workers in the field of HIV infection
Ensuring the appropriate level of amounts allocated from the budget of the Single National Health Insurance Fund for specific medicines and healthcare materials to be acquired for this purpose and carrying out their acquisition
Ministry of Health
Ensuring, monitoring and controlling the use of amounts allocated from the budget of the Single National Health Insurance Fund, monitoring, controlling and analysing the physical and efficiency indicators during the implementation of the programmes
Providing information every six months to the Health Committees of the Senate and Chamber of Deputies on the indicators of the sub-programmes for the prevention and control of HIV/AIDS, the way in which the specific therapy and of the associated infections have been provided
National Health Insurance House
Monitoring compliance with the right to work of PLHIV or suffering from AIDS
National Health Insurance House and the county health insurance funds

Ministry of Health
Ministry of Labour, Social Solidarity and the Family, through the Labour Inspectorate
52
Providing free of charge to persons infected with HIV or suffering from AIDS all information and professional counselling services, including job search according to the stage of the disease, according to the law
Informing the employers about the rights and obligations of the employees infected with HIV or suffering from AIDS and their obligation not to discriminate on grounds of health
County and Bucharest Employment Agencies
Educating the employees on the right to free post-exposure prophylaxis
Ensuring the payment of monthly food allowances to adults and children infected with HIV or suffering from AIDS who are hospitalized, institutionalized and in state outpatient clinics, in accordance with the methodology approved by order of the Minister of Labour, Social Solidarity and the Family
Ministry of Labour, Social Solidarity and the Family, together with Ministry of Health,
Conducting annual sociological research aimed at monitoring the number of recipients of monthly food allowances, their family and social situation and will advance proposals for the development of new social protection programmes and measures
Dissemination of educational and information programmes on HIV prevention and appropriate behaviour towards persons living with AIDS in all state
Ministry of Labour, Social Solidarity and the Family Ministry of Labour, Social Solidarity and the Family
Ministry of Labour, Social Solidarity and the Family
Ministry of Education and Research, together with:

53
and private school establishments and free, universal and unconditional access to this information for all young persons attending a level of education.
Ministry of Labour, Social Solidarity and the Family, National Youth Authority, National Agency for Sport, National Authority for Child Protection and Adoption,

National Authority for Persons with Disabilities
Ensuring the introduction into the curriculum, differentiated by school cycles, of a health education programme, including, inter alia, a separate chapter on HIV/AIDS, as well as the introduction into the teacher training/continuing education system of general knowledge on HIV/AIDS, the protection of the affected persons and the behaviour towards them and the development of extra-curricular and extra-school activities, and ensuring the monitoring of the implementation of these programmes
Promotion in the educational establishments of the development of an appropriate attitude towards persons infected with HIV or suffering from AIDS in order to eliminate their marginalisation and discrimination and to create a tolerant environment towards them.
Ministry of Education and Research
Ministry of Education and Research, through the county school inspectorates
54
Section 2: Medical legal framework
2.1
Ensuring the universal provision of treatment
The universal access to treatment for persons living with AIDS was introduced in 2001 and the programme has been recognised as a model in the region3. The HIV law currently provides that specific antiretroviral medication and HIV/AIDSrelated diseases are established free of charge4. The HIV Law also stipulates that the financing of therapeutic and health care activities shall be provided from the budget of the Ministry of Health or, where appropriate, the National Health Insurance Fund5
The Health Law includes a number of activities of public hospitals that can be financed from the state budget and these include HIV/AIDS programmes6 Specifically, the subject matter and funding mechanisms are determined by: National Public Health Programmes developed periodically by the Ministry of Health with the participation of the National Health Insurance House – in this case the National HIV/AIDS Prevention, Surveillance and Control Programme; and Technical Norms for the Implementation of National Programmes issued by the Ministry of Health
At the time of writing, the technical rules in force are those of 30 March 2017, established for the years 2017 and 2018, their applicability being extended successively – according to the last extension, they remain in force until the end of the month in which 60 days after the date of entry into force of the state budget law for the year 2022 will have passed7
This system of rules is complemented by:
Government Decision No 720/2008 approving the list of international common names of medicines available to the insured persons, with or without personal contribution, on prescription, under the social health insurance system, as well as the international common names of medicines available under the national health programmes; and
Order of the Minister of Health and of the President of the National Health Insurance House No 1.605/875/2014 approving the method of calculation, the





3. UNAIDS Country Progress Report on AIDS – Reporting Period January 2015 – December 2015

4 Article 10 of HIV Law

5 Article 16 (2) of HIV Law
6 Article 193 (2) (h) of Health Law
7. Article II of the Order of the Minister of Health No 1087/2017
55
list of trade names and the settlement prices of medicines to be granted to the patients under national health programmes and the methodology for their calculation.
2.2 Distribution of medicines exclusively in hospital pharmacies
According to the rules in force8, in contrast to the previous regulations9, the medicines for the outpatient treatment of HIV/AIDS patients are distributed through the closed-circuit pharmacies of the health units through which these programmes are implemented, on the basis of a prescription/medical order10 As such, medicines cannot be obtained free of charge through the private pharmacy networks and the beneficiaries have the only option of purchasing medicines in the relevant hospital pharmacies.
This issue – the need to obtain medicines in hospital networks, which often involves the access to wards, or queuing designated for persons living with HIV –has been identified as a source of anxiety for the beneficiaries, jeopardising the legal right to the confidentiality of the medical status.

At the same time, the exclusive reimbursement of the closed-regime medicines makes the infected persons vulnerable to the malfunctioning of the public medicine supply system.
The norms establishing these rules do not benefit from recitals or explanatory memoranda explaining the reasons for the dispensing of medicines by the closed-circuit pharmacies.
2.3 Difficulties in accessing the treatment

Although in terms of primary laws, access to the medicines should be free of charge, in reality, Romania has experienced a substantial crisis in the recent years
8. Article 14 of the 2022 Technical Standards for the implementation of national public health programmes
9 The 2008 technical rules stipulated that the medicines could be dispensed both through the open-circuit pharmacies in contractual relations with the health insurance companies and through the closed-circuit pharmacies of the health units, ensuring an optimal access to treatment.
10 The rules state that in the context of the SARS-CoV-2 pandemic, the prescription period for HIV/AIDS and tuberculosis patients can be up to 90/91/92 days, as appropriate.

56
in terms of the availability of the necessary medicines. The main problem seems to be the mobilisation of resources needed to effectively implement the national programmes regarding the access to antiretroviral medicines.
The main causes of this commonly identified crisis are, on the one hand, the insufficient allocation of funds to supply the hospitals with the necessary drugs, but also the fact that the existing financial allocations do not support changes in treatment regimens or in relation to the increasing number of patients.
However, the insufficient attention paid to this aspect in the budget programmes is consistently blamed on the long absence of a National HIV Strategy in the Romanian system.
2.4 Discrimination in the healthcare system and the issue of confidentiality in HIV Law
Discrimination in the healthcare field continues to substantially affect the community of persons living with HIV. The problems identified include issues such as the refusal of medical personnel to provide specialist care, or negative changes in behaviour resulting from the disclosure of the HIV status.
The patient’s obligation to inform the treating physician
The HIV Law establishes that patients are obliged to inform their treating physician, including the dentist, of their HIV status when they know it11. The HIV Law does not establish a penalty for the breach of this obligation, but provides that if (i) a “voluntary” transmission of the infection occurs, (ii) the patient was aware of his or her HIV positive status, and (iii) the transmission occurred for reasons attributable to the patient, then the patient is liable “according to the law” – it is plausibly understood that the reference is to tort liability in the Civil Code but also to the offence of transmission of immune deficiency syndrome in the Criminal Code which is explored in more detail in section [7] below on the criminalisation of HIV/ AIDS transmission.
It is debatable to what extent the patient’s obligation to inform the treating physician of his/her HIV status is justified. From the perspective of the health
11. Article 8 (3) of HIV Law


57
system, there are arguments concerning the need for the physician: (i) to know the full history of the patient’s conditions in order to prescribe the appropriate treatment; and (ii) to be able to take the appropriate personal protective measures to avoid a potential exposure that could lead to the transmission of the infection.
On the other hand, this obligation seems to trigger in the real life the premises of an act of discrimination and to expose the patient to the risk of not obtaining the medical treatment at all. As for the above arguments: (i) regardless of the condition, it is advisable for the physician to know the patient’s complete history, but the legislator did not feel the need to establish a general legal obligation in this respect, and (ii) regardless of the condition, the medical professional ethics require the physician to take the necessary precautions to avoid contracting any infection (e.g., by using masks or gloves).
In reality, however, it seems that this obligation to inform seems to be reserved for HIV/AIDS status, without any distinct medical justification in relation to other medical conditions, and its existence seems to be a tribute to an era when the legislative system developed in response to the AIDS epidemic did not rationally take into account the scientific reality of how the virus can be transmitted.
The physician’s obligation to provide care
The HIV Law states that the health facilities and the physicians, regardless of their specialty, are obliged to admit and provide medical care in the specialty they represent, according to the pathology presented by the patient. On the other hand, the HIV Law does not establish or refer to any sanction for breach of this obligation.
At the same time, the breach of this obligation could constitute a contravention under the anti-discrimination legislation.
Article 10
Discrimination of a natural person, a group of persons or a legal entity, on account of their belonging or the belonging of their management to a race,

58
Ordinance No 137/2000 on preventing and sanctioning all forms of discrimination
nationality, ethnic group, religion, social or disfavoured category, on account of their beliefs, age, sex or sexual orientation, shall constitute contravention, if the deed does not fall under the incidence of criminal law, by means of :
a) refusal to grant administrative and juridical public services;
b) denying the access of a person or group of persons to health public services –choice of a family doctor, medical assistance, health insurance, emergency care or other health services; (...) h) the refusal to grant a person or group of persons certain rights or facilities
The National Council for Combating the Discrimination, the body competent to investigate and sanction such acts, has the prerogative to award sanctions of between RON 1,000 and 30,000 if the discrimination targets an individual and between 2,000 and 100,000 lei if the discrimination targets a group of persons or a community.
In addition to this, regarding the practice of refusing treatment, the offence of abuse of office provided for in the Criminal Code should also be considered.
Criminal Code
Article 297 – Abuse in office
(1) The action of the public servant who, while exercising their professional responsibilities, fails to implement an act or implements it faultily1 thus causing damage or violating the legitimate rights or interests of a natural or a legal entity, shall be punishable by no less than 2 and no more than 7 years of imprisonment and the ban from exercising the right to hold a public office.
1. By a decision of the Constitutional Court, it was established that this paragraph is not contrary to the Constitution except in so far as “implements it faultily” is interpreted as “implements it in violation of the law” - Decision 405/2016 [A/R] on the exception of unconstitutionality of the provisions of Article 246 of the Criminal Code of 1969, Article 297 para. (1) of the Criminal Code and Article 13^2 of Law No 78/2000 on the prevention, detection and punishment of corruption

59
(2) The same punishment applies to the action of a public servant who, while exercising their professional responsibilities, limits the exercise of a right of a person or creates for the latter a situation of inferiority on grounds of race, nationality, ethnic origin, language, religion, gender, sexual orientation, political membership, wealth, age, disability, chronic non-transmissible disease or HIV/AIDS infection.
The classification of physicians as civil servants is an issue that has raised a range of controversies in Romania, with the Romanian College of Physicians arguing that the classification is “objectionable” and “unfair”.12 Instead, the consistent position of the High Court of Cassation and Justice seems to confirm13 that, at least from a criminal point of view, a physician employed under a contract of employment in a hospital in the public health system is a civil servant.
The revision of the legal regime of


the

obligation to disclose the HIV status
In countries such as the UK or France the patient is not obliged to inform the physician of their HIV status. However, this legal situation does not prevent the health systems and the public communication associated with HIV/AIDS status from highlighting and promoting the extent to which, although not mandatory, it is always recommended that the physician be informed of the patient’s medical status.
2.5 National HIV/AIDS Commission
The HIV legislation currently in force formally assigns an important role to the National HIV Commission. In addition to its role in developing the National HIV/ AIDS Strategy, the Commission also has a role in: monitoring the compliance of the health facilities with their obligations under the HIV Law14; establishing a methodology under which employers must provide postexposure prophylaxis free of charge15; and
12. Hotnews, 18 August 2015 – https://www.hotnews.ro/stiri-esential-20364270-colegiul-medicilor-din-romania-solutiile-inaltei-curti-cazul-hotararilor-prin-care-medicul-este-asimilat-functionarului-public-criticabile.htm
13. Decision of HCCJ (High Court of Cassation and Justice) from 3 December 2014 and published in the Official Gazette of 13 January 2015; HCCJ Decision of 4 June 2015 and published in the Official Gazette of 5 August 2015
14 . Regulation for the Implementation of the HIV Law
15. Article 6 (h) of HIV Law

60
development of standards for inpatient and outpatient diagnosis, treatment and therapy monitoring under the coordination of the regional HIV/AIDS centres16


At the date of this material, the above methodology and standards developed by the National HIV Commission have not been identified from the research. Also, as discussed in the next section, a National HIV/AIDS Strategy has not been adopted in Romania for over a decade.


The activity and operation of the National HIV/AIDS Commission is also regulated by Government Decision No 330/2003 (“GD on the National Commission”) which includes a number of more detailed tasks, including: evaluating the HIV/AIDS legislation and proposing the necessary legislation implementation of special actions and measures for persons affected by discrimination on grounds of HIV/AIDS proposing to the Government in the state budget the necessary funds for the implementation of the National Strategy
The National HIV/AIDS Commission does not have its own website (although it is mandatory according to the GD on the National Commission) that allows monitoring its work, publishing activity reports or any other evidence of its tasks.



In the summer of 2021, a draft Government Decision was published to replace the present GD on the National Commission with a similar text, but with some modifications such as: removing the commission from the authority of the Prime Minister and transferring it to the Ministry of Health the elimination of working groups of specialists by areas of activity the abolition of the obligation to respond to requests from the population under Law 544/2001

At the time of writing of this material, this decision has not been adopted.
In the autumn of 2021, by Ordinance 18/2021, the Romanian Government repealed Article 4 of the HIV Law which provided for the establishment of the National HIV/AIDS Commission, but all other provisions and references to the role and prerogatives of the Commission mentioned above remained in force. In the Note of justification of the ordinance, the explanation for the approval is that the 16. Article 11 of HIV Law
61
measure was necessary in view of “the legal framework for the establishment, by Government Decision, of the National Intersectoral Commission for the Control of Tuberculosis and the HIV/AIDS infection, in order to coordinate at national level all measures for the control of tuberculosis, HIV/AIDS infection and related diseases, to avoid confusion in the application of legal norms, for legislative accuracy, considering the fact that the 2 structures have similar attributions.”
From a legal point of view, the consequences of this repeal are unclear since, on the one hand, the paragraph providing for the establishment of the commission has been deleted but, on the other hand, no legal text has been adopted providing for its abolition and, at the same time, all other provisions referring to the commission are still in force. An interpretation according to which the commission would be abolished would lead to the conclusion that a significant component of the HIV/ AIDS legislation would become ineffective and, in the absence of a replacement entity, all the activities assigned to the commission by the HIV Law would cease to be prescribed by law in their entirety.
As such, the adopted text of the law has led to a climate of legal uncertainty surrounding a structure intended to provide an essential mechanism for the inter-institutional cooperation in the HIV/AIDS area within the health system.
Ordinance 18/2021 has been the subject of a complaint of unconstitutionality lodged by the People’s Advocate which is still pending at the time of the drafting of this material.


In June 2022, a proposal for a National HIV/AIDS Strategy was published as having been developed by the National HIV/AIDS Commission, a sign that the Government does not interpret the repeal of Article 4 as abolishing the Commission either.
Taking into account the important role that this Commission continues to play in the HIV/AIDS legislative framework, the lack of clarity regarding its organisation and functioning as well as the absence of activity reports illustrating the fulfilment of the roles assigned by law to this commission are regrettable.
2.6 The problem of implementing the National Strategy
According to the Regulation on the Implementation of the HIV Law, the National HIV Commission is in charge of elaborating and proposing for the approval of the
62
Government the National HIV/AIDS Strategy. The ministries and institutions with responsibilities in this field and/or with their own health network are also responsible for developing the National Programme for the prevention, surveillance and control of HIV/AIDS infection, as well as measures to reduce the social impact of HIV/AIDS cases.
However, the last National HIV/AIDS Strategy was adopted for the period 20042007, and only for the 2019-2021 period a draft for the National Strategic Plan for the Surveillance, Control and Prevention of the HIV/AIDS infections was published (which, from our verifications, was never adopted).

The existence of a National Strategy is essential for allocating money for prevention, but also for treatment, so that the persons living with HIV/AIDS can benefit from treatment without interruption.
After all this time of absence, a proposal for a National HIV/AIDS Strategy was published in June 2022 which, at the time of the preparation of this material, has not yet been adopted.
2.7 Food allowances in health care facilities
According to GD no. 429/2008 on the level of food allowances for the collective consumption in public health units, the level of food allowances in the public health units is 17.6 lei/day for adults and 16.5 lei/day for children
In May 2022, a number of amendments to Law 95/2006 on health care reform were adopted, introducing the following new paragraphs to Article 229 of the law:
Law No 95/2006 on health care reform
Article 229 (...)
“(5) The amount of the food allowance in public health units is set by order of the Minister of Health, is updated annually in line with the inflation rate and cannot be less than 22 lei/day of hospitalization. The expenses related to the

63
food allowance in public health units are covered by transfers from the State budget, through the budget of the Ministry of Health, to the budget of the Single National Health Insurance Fund.
(6) The food allowance may be supplemented by a decision of the administrative board of the health unit, provided that sources of financing other than the amounts from the contracts concluded with the health insurance companies and from the state budget are identified.”

Also in May 2022, the Ministry of Health adopted Order of the MH 1488/2022 for the establishment of the amount of the food allowance in public health units issued by the Ministry of Health (MH), according to which the amount of the food allowance is 33 lei per day of hospitalization (or 990 lei/month). By comparison, the value of the minimum consumption basket for a decent living17 has been set at 2708 lei for a single adult in 2021.
17. Special Report concerning the respect for the right to work and occupational social protection, Bucharest 2022 – According to the report, in the absence of official data, the analysis of the minimum consumption basket for a decent living is based on a study by Friedrich Ebert Foundation Romania and Syndex Romania on 5 November 2021
64
Section 3: Social protection

3.1 Monthly food allowances
According to Article 7 (4) of the HIV Law,18 the Government must approve an amount for the monthly food allowance to ensure the effectiveness of antiretroviral treatment applicable to: “inpatients and institutionalised patients, as well as outpatients.” The research shows that there is still an unchanged normative act (Government Decision No 1177/2003 approving the amount of the monthly food allowance payable to persons infected with HIV or AIDS) which, citing Article 7(4) of the HIV Law, sets the level of the monthly food allowance payable to adults at 7.7 lei/day for adults and 5.7 lei/day for children
According to the Methodology for Granting the Food Allowance, the payment of the monthly food allowance is carried out by the county labour and social protection directorates, respectively of the Bucharest municipality and can be made: (a) by postal order; (b) in a personal account; (c) in another form of payment specified in the application by the adult beneficiary or the child’s legal representative; (d) in a special account opened for this purpose by the general directorates of social assistance and child protection of the counties or districts of the municipality of Bucharest or the authorized private body – for children entrusted or placed in care by a public social assistance institution or authorized private body.
The extremely low levels of the allowance provided for above remained unchanged at the time of writing. On the website of the Ministry of Labour and Social Solidarity a draft Government Decision was published from 13 July 2022 to amend GD 1177/2003. According to the substantiation note of this text, the objective is to correlate with Law no. 95/2006, and the note also refers to MH Order 1488/2022 (both mentioned in section 2.7 above). Unfortunately, however, the proposed text is extremely unclear, stating only: the amount of the monthly allowance “shall be increased on the same date as the amount of the food allowance for the public health units, according to Article 229 of Law No 95/2006 on health reform”
18. Article 7 (4) of the HIV Law: “Monthly food allowances shall be granted for adequate nutrition for both inpatients and institutionalized patients, as well as for the outpatients, to ensure effectiveness in the treatment with antiretroviral drugs, in an amount approved by Government decision.”


65
– without specifying the amount by which this amount is increased. It is of course recommended that this text be clarified by the time it is adopted.



3.2 Wage increases associated with HIV/AIDS status
According to a Romanian Government Decision from 2018,19 the personnel paid from the public funds (according to Law 153/2017), employed with a severe or serious degree of disability, receive a bonus of 15% of the basic salary (HIV/AIDS status is recognized as a type of disability under Law 448/2006 on the protection and promotion of the rights of persons with disabilities).
Also, according to Law 448/2006, the above personnel who have in their care and protection an adult person with severe or accentuated disability, infected with HIV or suffering from AIDS, receive a bonus of 25% calculated on the basic salary.
3.3 Other measures of social protection
According to the legislation mentioned above, the Ministry of Labour has a number of legal obligations regarding the situation of the persons living with HIV:
Monitoring the compliance with the right to work of the persons living with HIV or AIDS
From the research carried out, we did not identify a monitoring report published by the Ministry of Labour in relation to this monitoring, or a dedicated centre for complaints associated with the non-compliance with the right to work on the grounds of HIV/AIDS
Provision free of charge for the persons infected with HIV or AIDS of all information and professional counselling services, including job search according to the stage of the disease, under the conditions of the law
From the research carried out, we did not identify any prepared material, or an information centre opened by the Ministry of Labour that is accessible free of charge and dedicated to information and professional counselling for PLHIV
19. Decision 751/2018 for the determination of the categories of persons with disabilities who benefit from an increase of 15% of the basic salary/functional salary/employment allowance
66
Informing the employers about the rights and obligations of the employees with HIV infection or suffering from AIDS and the obligation non-discrimination against them on the basis of health
From the research carried out, we did not identify any measures at general level whereby the employers are publicly informed about the obligations associated with the employees infected with HIV or suffering from AIDS.
ensuring the education of the employees on the right to free post-exposure prophylaxis

From the research carried out, we did not identify any measures at a general level whereby the employers are educated on the above.
Performing annual sociological research to monitor the number of recipients of monthly food allowances, their family and social situation and advance proposals for the development of new social protection programmes and measures
No such published research was found in the verifications undertaken.
67
Section 4: Education system and HIV

The Ministry of Education is in charge of:
Dissemination of educational and information programmes on the prevention of the transmission of HIV infection and of the appropriate behaviour towards the persons living with AIDS in all state and private educational institutions and provision free of charge of universal and unconditional access to this information to all young persons attending a form of education.
Ensuring the introduction into the curriculum, differentiated by school cycle, of a health education programme, including, inter alia, a separate chapter on HIV/ AIDS, as well as the introduction into the teacher training/continuing education system of general knowledge on HIV/AIDS, the protection of affected persons and behaviour towards them and the development of extra-curricular and extraschool activities. The Ministry will ensure the monitoring of the implementation of these programmes.
Promotion in the educational institutions of the development of an appropriate attitude towards the persons living with HIV and AIDS in order to eliminate their marginalisation and discrimination and to create a tolerant environment towards them.
However, as the quantitative study shows, 73% of respondents did not have access to sex education/health education in schools. In the production of this material, we could not identify concrete measures taken by the Ministry of Education to fulfil these tasks. Failure to comply with these legal obligations leads to maintaining or even increasing the level of social stigma and misinformation about people living with HIV.
In this context, it is important to mention the legislative initiative tacitly approved by the Senate in 2022 on the modification and completion of Law 272/2004 on the protection and promotion of the child’s rights.20 The legislative draft includes provisions restricting the dissemination of information on “the popularisation of homosexuality” in the family but also in any other environment, including educational institutions, research environments, the internet, the media, etc.
This initiative is open to criticism from numerous perspectives, including certain legal ones, given the unconstitutional nature of certain limitations on freedom of expression, the right to privacy and the right to free speech.
20 http://www.cdep.ro/pls/proiecte/upl_pck2015.proiect?idp=19747




68
However, particularly in the context of the fight against the spread of HIV and the improvement of the quality of life of the persons living with HIV, these kinds of provisions have a devastating effect in that they risk outlawing any prevention and outreach campaigns aimed at groups vulnerable to HIV/AIDS.

69
Section 5: Fight against discrimination
5.1 Legal instruments to protect against discrimination
The Anti-Discrimination Law is the main legal instrument for sanctioning the discriminatory behaviour, explicitly providing for the status of HIV infection as a characteristic in relation to which discrimination is sanctioned.

According to the Anti-Discrimination Law, the following acts (to the extent that they are not covered by the criminal law) towards persons living with HIV constitute offences:
Article 10 (...)
a) refusal to grant administrative and juridical public services;
b) denying the access of a person or group of persons to health public services – choice of a family doctor, medical assistance, health insurance, emergency services or other health services;
c) refusal to sell or rent a plot of land or building for housing purposes;

d) refusal to grant a bank credit or to conclude any kind of contract;

e) denying the access of a person or group of persons to the services provided by theatres, cinemas, libraries, museums and exhibitions;
f) denying the access of a person or group of persons to the services provided by shops, hotels, restaurants, bars, discotheques or any other service providers, whether they are in public or private property;
g) denying the access of a person or group of persons to the services provided by public transportation companies – by plane, ship, train, subway, bus, trolley-bus, tram car, taxi or by any other means of transport;
h) the refusal to grant a person or group of persons certain rights or facilities
70
The Criminal Code also establishes a number of indirect protections such as: providing for aggravating circumstances in the case of any offence committed on account of HIV/AIDS infection21;


the enshrinement of a variant of the offence of abuse of official duty for the act of a civil servant who restricts a right or creates a situation of inferiority on the grounds of HIV/AIDS infection22; the adoption in 2022 of an amendment to the Criminal Code offence of incitement to violence, hatred or discrimination, which explicitly provides for the category of HIV/AIDS infection
Criminal Code
Article 369: Incitement to violence, hatred or discrimination
Incitement of the public, by any means, to violence, hatred or discrimination against a category of persons or against a person on the grounds that they belong to a particular category of persons defined on the basis of race, nationality, ethnicity, language, religion, gender, sexual orientation, political opinion or affiliation, property, social origin, age, disability, chronic non-contagious disease or HIV/AIDS infection, considered by the offender as a cause of inferiority of one person in relation to others, shall be punishable by imprisonment for a term of 6 months to 3 years or a fine.
Also, the Regulation on the Implementation of the HIV Law establishes that the persons infected with HIV or suffering from AIDS have the right23 to nondiscriminatory treatment in terms of the right to education, the right to work, the right to professional promotion and social protection, according to the national legislation on the prevention and sanctioning of all forms of discrimination and according to the international conventions, covenants and treaties to which Romania is party.
The National Council for Combating Discrimination (“NCCD”) is responsible for monitoring and sanctioning the acts of discrimination.

The Anti-Discrimination Law sets out sanctions applicable to the perpetration of the offences set out, which may include:
21. Article 77 (h) of the Penal Code.
22. Article 297 (b) of the Penal Code.
23. Article 3 of the HIV Law

71
1 Fines – from RON 1,000 to RON 30,000 (if the discrimination targets a natural person) and from RON 2,000 to RON 100,000 (if the discrimination targets a group of persons or a community); and

2. The obligation to publish in the media a summary of the decision on the fact-finding decision or the judgement on the perpetration of the offence

5.2 The work of the NCCD in relation to HIV discrimination
According to the responses to requests for information to the NCCD advanced in preparation of this material, from 2003 to November 2021, the NCCD found no more than 23 contraventions, of which only 6 were resolved with a fine. The maximum fine imposed by the NCCD being RON 5,000, individually. This number represents 26% of the investigation files opened during this period.
The cases brought to the attention of the NCCD tend to fall predominantly in two categories: either cases alleging discrimination in the workplace or cases alleging discrimination in relation to the provision of a medical service.
An analysis of the NCCD decisions shows that the number of cases where the liability is established is very small compared to the number of complaints that end up being settled by the NCCD College.
Many of the rejections appear to be based on technical issues such as lack of standing, lack of jurisdiction or lateness.
Most dismissals seem to be based on the absence of a causal link between the claimed act and the existence of a prejudice against HIV status. For example, judgement No 401/2020 analyzed the situation of a petitioner who claimed that on presenting himself in the emergency room of a hospital, he was taken in by a physician who, on learning that the patient was living with HIV, was subsequently refused the medical services and requested that the go to another hospital for surgery. However, the NCCD College established that the physician had in fact refused the medical procedure on the grounds that it was not necessary according to the medical tests. Thus they did not establish a causal link between the criterion invoked by the petitioner, that of HIV infection, and the facts complained of.
72
Another recurring case is the case of the publications or posts on social media containing a language considered offensive or discriminatory. For example, in Decision No 24/2021, the NCCD College assessed a case concerning a post with the text: “Revolting! An HIV-positive bastard scratched a policeman on duty on Sunday evening. The assailant told the lawman he wanted to give him the disease too... Now comes the shocking part! The prosecutors investigating the case have decided that the AIDS-sick psychopath cannot be remanded in custody. The reason: he suffers from several chronic illnesses, including diabetes! I don’t know who the prosecutor on the case is, but I’ll find out just to tell him it’s... (I’ll let you each fill in the blanks)”
The NCCD College held that the action falls within the limits of the right of free expression of individuals.
Unfortunately, this position of the College illustrates that the authority does not consider itself competent to intervene in relation to the devastating effect that the exposure in the public space of this type of message has on the stigmatisation of the persons living with HIV.

73
Section 6: Confidentiality
6.1 Disclosure of HIV status – is there an obligation to disclose?

Apart from the aspects regarding the information of the treating of HIV Act, discussed above, there is no general obligation to disclose the HIV status.
On the other hand, the legal framework in Romania makes it difficult for a person living with HIV to choose not to disclose his or her HIV status, or to effectively benefit from the protection of confidentiality of this information.
The decision not to disclose could be subject to an analysis in a potential criminal liability investigation into the transmission of the virus.
As discussed in more detail below, HIV transmission is still criminalised, with unclear wording in the law as to the extent to which unintentional transmission can be punished. It is also unclear to what extent the disclosure of HIV status can be a defence or mitigating circumstance in a case of involuntary transmission.
At the same time, the general provisions on civil liability in tort may be applicable in the case of damage caused by a potential HIV transmission, so that even if the conditions of criminal liability were not met, the requirements of civil liability may still be met. Here again, there are no provisions determining the extent to which the disclosure or non-disclosure may be taken into account in establishing a liability.
The existence of such a legal regime in the absence of explicit enshrinement may (at least in practice) expose the persons living with HIV to an increased risk of repression in the event of HIV transmission due to the non-disclosure of HIV status – although the increased risk is not based on an explicit legal basis.
Aspects associated with the employment relations

The persons subject to labour legislation are required to obtain a medical certificate stating that the person concerned is fit to perform that type of work 24 According to the Labour Code, failure to comply with this obligation renders the

74
24
Article 27 of the Labour Code
individual employment contract null and void. The Labour Code stipulates that specific medical tests may also be required for employment in the fields of health, catering, education and other fields laid down by law.
Occupations and fields in which the HIV testing is mandatory, or may be mandatory at the request of the occupational health physician, upon employment or periodically - according to Government Decision No 355/2007 on the workers’ health surveillance:
Pharmaceutical industry
Hairdressing, barbering, massage, cosmetics (manicure and pedicure) establishments
Elementary health care personnel, nursing personnel, personnel caring for the handicapped persons and foster carers
Senior and middle health personnel
In other areas, the decision not to disclose does not enjoy the same protection as, for example, the pregnancy – the Labour Code prohibits requesting pregnancy tests at the time of employment, but does not prohibit any other tests. Moreover:
(a) the occupational medical examination is compulsory;
(b) the HIV Law provides the obligation to announce the HIV status to the attending physician, when known25; and

(c) the worker’s general obligations to communicate and cooperate with the employer and/or designated workers on matters that may endanger the health of workers.26
25. Article 8 (3) of HIV Law
26. Article 23 of Law 319/2006 on safety and health at work
75
As such, these provisions jeopardise the freedom of the persons living with HIV to choose not to disclose their HIV status, and there are arguments for maintaining the disclosure of this status to the occupational health physician (even if HIV testing is not mandatory in the relevant employment sector).
In view of the above, in order to develop a protective legislative framework for the right of the persons living with HIV to be able to protect the confidentiality of this information, it is recommended that this right be expressly established in legislation for the persons living with HIV.
6.2 Protection of confidentiality
Privacy protection in general legal texts
The right to protection of confidentiality of HIV status is enshrined in fundamental legal texts, starting with Article 8 of the European Convention on Human Rights and Article 26 of the Romanian Constitution on the protection of intimate, family and private life.
The General Data Protection Regulation (GDPR)27 prohibits the processing of personal data revealing health data without the consent of the individual, but there are a number of exceptions.
GDPR Article 9(2)(b)


Exception to the prohibition to process personal data revealing health data
Processing is necessary for the purposes of carrying out the obligations and exercising specific rights of the controller or of the data subject in the field of employment and social security and social protection law in so far as it is authorised by Union or Member State law or a collective agreement pursuant to Member State law providing for appropriate safeguards for the fundamental rights and the interests of the data subject
27. Article 9 of Regulation (EU) 2016/679 of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data and repealing Directive 95/46/EC (General Data Protection Regulation)
76
9(2)(c)
Processing is necessary to protect the vital interests of the data subject or of another natural person where the data subject is physically or legally incapable of giving consent
9(2)(h)
Processing is necessary for the purposes of preventive or occupational medicine, for the assessment of the working capacity of the employee, medical diagnosis, the provision of health or social care or treatment or the management of health or social care systems and services on the basis of Union or Member State law or pursuant to contract with a health professional and subject to the conditions and safeguards referred to in paragraph 3
9(2)(i)

9(2)(j)
Processing is necessary for reasons of public interest in the area of public health, such as protecting against serious cross-border threats to health or ensuring high standards of quality and safety of health care and of medicinal products or medical devices, on the basis of Union or Member State law which provides for suitable and specific measures to safeguard the rights and freedoms of the data subject, in particular professional secrecy
Processing is necessary for archiving purposes in the public interest, scientific or historical research purposes or statistical purposes in accordance with Article 89(1) based on Union or Member State law which shall be proportionate to the aim pursued, respect the essence of the right to data protection and provide for suitable and specific measures to safeguard the fundamental rights and the interests of the data subject
Criminal Code
Disclosure of private life information such as the HIV status is also criminalised by the criminal law in Article 227 of the Criminal Code, according to which the unlawful disclosure of data or information concerning a person’s private life, which is likely to cause harm to a person, by a person who has become aware of it by virtue of
77
their profession or office and who is under an obligation to keep it confidential, is punishable by imprisonment from 3 months to 3 years or a fine.

The Patients’ Rights Law
Law No 46/21 January 2003 on patients’ rights enshrines the right to confidentiality of medical information, which establishes28 that all information on the patient’s condition, investigation results, diagnosis, prognosis, treatment, personal data are confidential even after the patient’s death and cannot be disclosed without the patient’s consent or an express legal provision. However, consent is no longer required for disclosure if the information is needed by other accredited healthcare providers involved in the patient’s treatment.
The same law states that any interference in the patient’s private or family life is prohibited – but exceptions are made in cases where: such interference positively influences the diagnosis, treatment or care provided, with the consent of the patient; or where the patient poses a danger to him/herself or to public health.
HIV Law

According to HIV Law,29 The confidentiality of data regarding the persons living with HIV or suffering from AIDS is mandatory for: (a) employees of the health network; (b) employers of these persons; (c) public officials who have access to these data. However, the HIV law does not establish a sanction for the noncompliance with these obligations.
Disclosure by the occupational physician

As stated above, the Romanian law does not appear to have mechanisms to protect a person living with HIV in the event of a decision not to disclose their status to the occupational health physician (there are even arguments that there is a legal obligation for such disclosure). Normally, the occupational health physician is bound by the professional secrecy promoted by the medical code of
28. Article 21 of Law No 46/21 January 2003 29. Article 8
78
ethics and the results of medical examinations of employees are communicated to the employers only in terms of fitness or unfitness.30
Unfortunately, however, the law explicitly provides for an exception to this obligation with regard to “infectious and parasitic diseases with risk of transmission in the community.”

The Romanian legal framework seems to basically create the context in which the employer will have access to the HIV status of its employees regardless of whether or not the employee consents. In order to protect against discrimination and the rights of the persons living with HIV (including the right to decide whether or not to disclose this status to their employers) it is recommended that this exception be removed or qualified so that a person’s HIV status is not disclosed to the employer.
Cases of disclosure in court
In our study we identified situations where persons living with HIV sought to pursue tort liability (and compensation) for disclosures of HIV status by the public authorities.
In a case,31 the plaintiff was able to obtain approximately 10,000 euros from the City Hall of District 1 as a compensation for the non-material damage caused as a result of the fact that their name, address, PIN32 and the name of the plaintiff’s illness were displayed on the City Hall’s website. The Court held that, although the quantification of a moral damage is not subject to legal criteria for its determination, the moral damage is determined by assessment, following the application of criteria relating to the negative consequences suffered by the person concerned, physically, mentally and emotionally, the importance of the values damaged, criteria which must be subject to the connotation of the reasonable assessment, on a fair basis, so as not to lead to unjust enrichment of the person claiming the moral damages.
30. Article 33 of Law No 418 of 18 October 2004 on the specific professional status of occupational medicine physicians
31. Civil judgment no. 4301 of 16.03.2009 pronounced by the Court of District 1
32. Personal Identification Number
79
In another case33, the claimant was unable to obtain compensation because, on the statement of the account published by his bank, under the heading of payments received from a County Agency for Payments and Social Inspection (CAPSI), the phrase “HIV-AIDS food allowance” appeared. According to the address issued by the bank, the phrase indicated was taken over by the payment orders issued by the CAPSI as the authorising officer of the payment. The court rejected the claimant’s application, citing, inter alia, that the bank employee is bound by confidentiality obligations and there was no evidence that the claimant personally knew any of the bank’s employees, as well as the fact that it was not proven that any other person had access to the statement. The court rejected the argument that the town in question is small and people know each other, pointing out that it is a town with a population of over 100,000. The court also opined in its reasoning that “it is difficult to believe that a bank clerk actually reads the details of every bank transaction on the account.”

These cases show, on the one hand, that Romanian courts can establish moral damages for acts of disclosure of the HIV status by the authorities.
On the other hand, there is a significant margin of appreciation for the courts in establishing the existence of harm and determining the extent of any damages. Unfortunately, however, it is inadvisable for a legal system to allow for judicial discretion in the context of the rights of minorities or others vulnerable to social bias (including court bias).
Moreover, the second court did not hold that the disclosure itself and the danger that strangers or persons known to the plaintiff might learn of the plaintiff’s HIV status is sufficient to establish moral damages.
33. Judgment of 20 March 2015 and 396/2015.
80
Section 7: Criminal incrimination
7.1 Existing criminal law regulation
In Romania, the offence called “Transmission of Acquired Immunodeficiency Syndrome” (“TAIS”), regulated by Article 354 of the Criminal Code is currently in force Câteva observații generale pe marginea incriminării existente:



Criminal Code
Article 354 - Transmission of the acquired immunodeficiency syndrome (AIDS)
(1) Transmission by any means of the acquired immunodeficiency syndromeAIDS - by a person who knows that he or she suffers from this disease shall be punishable by imprisonment for a term of 3 to 10 years.
(2) Transmission by any means of the acquired immunodeficiency syndrome - AIDS by a person other than the person referred to in paragraph 1 shall be punishable by a term of imprisonment of 5 to 12 years.
(3) If, by the acts referred to in paragraph (1) and paragraph (2), the death of the victim has occurred, the penalty shall be imprisonment for a term of 7 to 15 years.
(4) In case the act referred to in paragraph (2) has been committed with negligence, the punishment shall be imprisonment from 6 months to 3 years, and if it has caused the death of the victim, the punishment shall be imprisonment from 2 to 7 years.
(5) The attempt at the offences referred to in paragraph (1) and paragraph (2) shall be punishable
Some general remarks on the existing criminalisation:
As it refers to AIDS and not HIV, according to the fundamental principles of criminal law, the article should be inapplicable
The incriminating text refers to the transmission of the acquired immune deficiency syndrome (AIDS) and not to the transmission of HIV. From a medical

81
point of view, the acquired immunodeficiency syndrome itself is not likely to be transmitted, as it is a medical condition that can be acquired by a person as a result of HIV infection. As such, in line with the legal principle that the criminal law is strictly interpretative, this offence should be rendered ineffective because of its weak wording.
The principle that the criminal law is of strict interpretation is universally recognised in the criminal law doctrine, but is also found in the case law of the High Court of Cassation and Justice34, and also has a legal basis in the Criminal Code, being a consequence of the rule that no penalty may be established and applied outside its general limits.35 There is also a large body of case law of the European Court of Human Rights which either enshrines or uses this principle.36
However, as we will see below, in Romania there are prosecutions and convictions based on this offence, which is a sign that the prosecutors and the courts interpret the text of the incrimination “constructively,” which is not allowed in the criminal law.


The legal doctrine relating to this article also seemed to support such an interpretation, without taking into account the issues discussed above.37
The legal doctrine relating to this article also seemed to support such an interpretation, without taking into account the issues discussed above.
Difficulties in interpreting/applying harsher punishment in case of guilt?
The law sets a harsher penalty for the intentional transmission of AIDS by a person other than a person who knows they have the disease. The question arises, what types of persons might fit this description?
(i) Persons who are infected with the AIDS virus but don’t “know they have the disease”

34. For example, Decision No 18/3.06.2019 or Decision No 22/4.05.2022
35. Article 2 (3) of the Criminal Code
36. Coëme and others against Belgium, point 145; Del Río Prada against Spain (MC), point 80, Bașkaya and Okçuoğlu against Turkey
37. DOBRINOIU Vasile, colectiv, Noul Cod penal comentat din 01-oct-2012, Universul Juridic: “Urmarea imediată a infracțiunii presupune transmiterea SIDA, mai exact a infecției cu HIV.” (DOBRINOIU Vasile, collective, New Criminal Code commented from 01-Oct-2012, Universul Juridic: “The immediate consequence of the offence involves the transmission of AIDS, specifically HIV infection.”)
82
If this is the intended interpretation, however, it makes no sense for this category of persons to be punished more severely than a person who is aware that he/she suffers from this disease. Moreover, according to the Romanian criminal law38 no act may constitute a criminal offence unless committed with a form of guilt prescribed by the law.
The only forms of guilt39 are:
- intention: a situation where a person either (a) foresees the result of his or her act and intends it to occur by committing that act, or (b) foresees the result of his or her act and, although not intending it, accepts the possibility of its occurrence
It is clear that intent cannot be applicable in the case of persons referred to in (i) above, because, being unaware of their AIDS status, it is not possible for them to foresee the result of the transmission of this disease.

- guilt: a situation where a person either (a) foresees the result of their act but does not accept it, baselessly assuming that it will not occur; or (b) does not foresee the result of his/her act, although they should and could have foreseen it.

Again, the guilt in (a) cannot in any circumstances be applicable, leaving only the category in (b) which, however, presupposes that a person, on the one hand, is not suffering from AIDS, but at the same time, “should and could” have foreseen that they are suffering from AIDS.


(ii) Persons who do not suffer from AIDS but still transmit it
The hypothesis could be applicable, for example, to persons who could, with a form of guilt prescribed by law, have access to an infected material (e.g., blood, seminal fluid) and apply it to another person (e.g., on an open wound).
Disproportionate punishment compared to other particularly serious crimes
The penalties provided for are totally disproportionate to other offences with much more serious consequences, such as, for example:
manslaughter (Article 190 of the Criminal Code), which, in the non-aggravated form, carries a prison sentence of 1 to 5 years (or 2 to 7 years in the aggravated form) sexual intercourse with a minor (Article 220 of the Criminal Code) is punishable by 1 to 5 years’ imprisonment; sexual assault (Article 219 of the Criminal Code) is punishable by 2 to 7 years’ imprisonment;
38. Article 16 of the Criminal Code

39. In addition to intent and culpability, there is also the question of guilt of the overriding intent (when the act consisting of an intentional action or inaction produces a more serious result, which is due to the culpability of the perpetrator) – this hypothesis, however, is applicable to the same considerations as intent and culpability.

83
trafficking in human beings (art. 210 of the Criminal Code) is punishable by 3 to 10 years’ imprisonment;
rape (art. 218) is punishable by 5 to 10 years’ imprisonment.
In terms of the consequences for the victim of a TAIS offence, the application of this sentencing regime seems to suggest that contracting HIV (because as we have shown above, AIDS itself is not likely to be transmissible) is comparable in severity to being sexually assaulted, raped, trafficked or even killed. The seriousness and severity of contracting is undeniable, but equating it with the consequences of other crimes ignores the fact that, thanks to the scientific developments in the applicable treatment, HIV no longer has such serious consequences.
7.2 Criminal prosecution
According to the information provided by the Public Prosecutor’s Office, in the framework of the research carried out for the production of this material from 1997 to mid-2021, criminal proceedings were initiated in 333 cases, of which 298 cases were resolved by the lack of sending to trial, and in 35 cases, the solution was to send to trial the persons investigated.
According to the information provided by the Ministry of Justice, between January 1st 2015 and March 21st 2021, 10 cases were tried on the merits of the Romanian courts, the main subject of which was the perpetration of the TAIS offence, and between 1 January 2016 and 31 March 2021, 11 cases with TAIS as a secondary subject.
In the period 1 January 2016 – 31 March 2021, 8 persons were definitively convicted for TAIS of which 3 were sentenced to imprisonment (one of them was sentenced to more than 10 years in prison.
The content of these files was not available during the research carried out and the documentation obtained does not illustrate in what proportion the different variants of the offences in the paragraphs of the Criminal Code are considered.
On the one hand, the ratio of the number of cases of initiation of the criminal proceedings to the number of cases sent to trial is similar to the general average at the level of the Public Ministry.40 On the other hand, the fact that on a general



40. According to the Activity Report 2020 of the Public Ministry, the ratio of the number of initiations of prosecution to the number of cases sent to trial is approximately 15%.

84
level, the ratio between investigation and sending to trial is so low, shows that the selection of the social situations likely to be incriminated should be carried out with particular care.

7.3 Decriminalisation

This section includes an analysis of some of the main issues justifying the decriminalisation of TAIS as a separate offence and the repeal of Article 354 of the Criminal Code
The premises of criminalisation in the criminal justice system
From a legal point of view, there is no rule as to which acts will be subject to criminalisation and which acts, despite the fact that they may be considered reprehensible by society, will not be criminalised. This decision is taken sovereignly by the Parliament, generally through a combination of political considerations (i.e. the extent to which the criminalisation leads to a positive response from the society) and criminological considerations (i.e. the extent to which the criminalisation leads to the removal of the social danger and the reduction of the criminalised phenomenon).
In terms of political considerations, the society’s reaction to changes in public policy on HIV certainly depends on the quality of information in the public domain. In the 1980s and 1990s, the lack of understanding of the phenomenon and the perceived seriousness of the risks of a new disease paved the political way for the criminalisation of the HIV transmission – also a natural reaction of the states to compensate for the lack of effectiveness in the general effort to combat the spread of the virus.
The criminological considerations, on the other hand, can be analysed somewhat more concretely in relation to the two essential principles behind the criminalisation of an act:
1. What is the social danger of that act?
2. To what extent is the criminalisation justified in terms of reducing the incidence of the reprehensible conduct?
85
Din ambele puncte de vedere, contextul actual este extrem de diferit față de cel din 1996, când incriminarea TSID a fost adoptată pentru prima dată în sistemul penal românesc
From both points of view, the current context is very different from that of 1996, when the criminalisation of TAIS was first adopted in the Romanian criminal justice system.
From the perspective of the social danger, over time, there have been significant improvements in the treatments available in the cases of HIV infection, so that any perception of “HIV infection is a death sentence” is deeply misplaced.

At the same time, it is observable that over a period of more than 25 years that the criminalisation has no impact on the rate of HIV infection in society. Moreover, it is observable that there is a major discrepancy between the number of cases in which a prosecution was initiated under the TAIS offence (in the period analysed according to the analysis in section 6.2 above – 333 cases) and the number of cases in which the prosecution was resolved with referral for trial (35).
As such, not only has the social danger associated with the HIV infection diminished considerably, but the 25-year history of criminalisation of the virus has not illustrated the criminal justice system’s ability to detect the existence of a pronounced social risk – in simple terms, there is no evidence that the act of HIVinfected people voluntarily transmitting the infection has a worrying prevalence in the Romanian society.
UNAIDS studies and guidance41 point to a number of issues to be considered when designing the legal regime associated with the HIV/AIDS status:
• The legal regime should take into account the current reality of the transmission: HIV infection is a serious and chronic medical condition, but it has become manageable with the modern treatments available so that an infected person can generally lead a normal life;
• The general and broad wording in the incriminating texts risks undermining the scientific facts of the HIV transmission, as it does not take into account that certain circumstances of contact (such as touching, kissing, non-penetrative or oral sex) are not real situations of exposure to HIV and may lead to unjustified incriminating circumstances;
41. UNAIDS: Ending overly broad criminalization of HIV non-disclosure, exposure and transmission: Critical scientific, medical and legal considerations | Guidance Note 2013 (https://www. unaids.org/sites/default/files/media_asset/20130530_Guidance_Ending_Criminalisation_0.pdf)
86
• Given that there is scientific and medical evidence that the risk of HIV transmission can be significantly reduced by the use of condoms – and because these behaviours should be encouraged by the public health policy messages and HIV prevention strategies – condom use, or nonpenetrative or oral sex, should be considered recognised as legitimate defences to any potential criminalisation
Alternatives to criminalisation
This material is not intended to minimise the reprehensible nature of the act of voluntarily infecting another person with HIV. Any analysis of the arguments for repealing the TAIS offence must highlight the alternatives available to punish this behaviour.
Title I of the Criminal Code is peppered with offenses that can serve as a basis for prosecution of the same acts criminalized by the TAIS offense – notably, the offense in Section 194 of the Criminal Code referring to any act that “impairs the health of a person, ”the seriousness of which is assessed by days of medical care of “more than 90 days.”
Moreover, in the case of a prosecution for an act of voluntary infection with a virus other than HIV, the Public Ministry is already obliged to prosecute based on the offences that already exist in the Criminal Code, the above showing that there is no reason why HIV should have a special status.
Discriminatory criminal policy
The criminalisation of HIV transmission is an excellent example of a situation that illustrates the ability of the legal system to act in a discriminatory manner –applying a different treatment (i.e. a distinct legal framework) to the intentional transmission of HIV from any other act of violence or harm that may have consequences of a similar gravity.
A variety of negative effects of this situation can be formulated, such as:

• perpetuating the perception that the persons living with HIV are a distinct danger in society that needs to be countered by special measures
• the “demonisation” in the media of the few cases of voluntary HIV infection, focusing on this component of the reprehensible act as distinct from the general reprehensibility of the acts for which the respective persons are prosecuted
• providing tools in the criminal justice system to individualise and characterise HIV-infected persons, with the risk of increasing the circumstances of abuse against the infected persons.
87
Section 8: Conclusions of the legal framework validated by the sociological study






Conclusions
The Romanian legal framework has characteristics designed to provide a formal protection for the persons living with HIV/AIDS. It includes: legal provisions designed to ensure the free access to treatment; mechanisms for granting allowances and other social benefits; protection of confidentiality; protection against discrimination; obligations of the public authorities in relation to the information and education of society and the protection of the persons living with HIV against prejudices.

Regarding free access to treatment, the sociological study shows that in practice there are significant problems in ensuring the quality and continuity of the treatment. The legal provisions regarding the free access to treatment are not sufficient in practice, and an administrative and budgetary system is needed to support the practical implementation of this objective. In this respect, the absence of a national HIV/AIDS plan (despite the legal provisions requesting the obligation of its implementation) has been identified as one of the causes leading to the difficulties regarding the access to medicines in the recent period.
Although there are social support mechanisms, the amounts of benefits are generally modest. The quantitative study shows that 38% of the persons are unemployed (well above the national unemployment rate), which is explainable in the context of a social category still at high risk of discrimination in employment. However, the legal provisions aimed at ensuring the right of HIV-positive persons not to disclose their status to their employer have lacunae that may lead to situations of disclosure.
At a formal level, the protection of the confidentiality of one’s HIV status is enshrined either directly or indirectly in the law. However, there are significant exceptions to these rules. The most important exceptions are for medical personnel, towards whom there is still a legal obligation to disclose HIV status. This obligation to disclose appears to be unjustified in the context that 63% of the

88
respondents report being denied certain medical services because of their HIV/ AIDS status.
Physicians also have confidentiality obligations, but the qualitative study shows that almost half of the respondents identified situations where confidentiality was breached, such as calling out names in the hallway in relation to diagnosis or treatment release, waiting in shared queues with other patients with the same diagnosis

In this context, despite the existence of the provisions against discrimination based on HIV status, 84% of respondents reported experiencing stigma and 79% discrimination. The overwhelming majority of cases which come before the NCCD College are not resolved by sanctions, and difficulties are very often encountered in the ability to prove the causal link between the act being complained of and the HIV/AIDS status of the plaintiff.
Authorities such as the Ministry of Education and the Ministry of Labour have significant prerogatives in educating the population and in assessing, monitoring and mitigating the prejudices in the field of HIV/AIDS and their impact on the lives of the HIV-positive persons. The HIV/AIDS legislation sets concrete tasks and targets in this regard, many of which could not be confirmed in the analysis conducted in this study.
89
V. Recommendations

Next steps…


The first step in change is knowledge and this can be gained by facilitating the access to current and accurate information communicated by relevant persons who benefit from a capital of trust among the general public.
•
Reducing the social stigma associated with HIV:


Increasing the awareness and understanding of HIV and desensitising the general public to the subject so that the social stigma attached to HIV could be reduced/ removed
Information campaigns: HIV is not AIDS and Undetectable=Untransmittable (U=U) in order to balance the general perception of this disease and place it among the “usual, manageable” chronic diseases; information campaigns to be supported and publicly promoted by relevant medical figures (medical opinion leaders who can bring extra confidence to the information content)
Support, both emotional and in the access to care and treatment for the patients living with HIV:
Providing emotional support (national psychotherapeutic support programmes) to PLHIV, especially at the time of learning and accepting the diagnosis of HIV infection
•

Increasing the diagnosis rate by organising information campaigns about the free testing points

A better management of the funds allocated to the treatment needed by the HIV-




91
positive persons so that there are no more gaps in the provision of treatment; organisation of a reserve fund for 3-6 months in hospitals and its monitoring in order to avoid the lack of treatment
The establishment of clear legal instruments, accompanied by control mechanisms, for the procurement and distribution of antiretroviral treatment by the public authorities, to give substance to the legal requirements regarding the provision of free access to this treatment



Mentoring and guidance provided by the state institutions and/or NGOs in navigating new HIV-positive patients through the entire medical investigation pathway and connecting them with the existing support groups (”Patient Navigator” service)
Reducing/eliminating discriminatory behaviours:
Providing information/educational support to the health professionals on the risks and methods of HIV transmission. A great part of the medical personnel adopts a hostile attitude towards the HIV-positive persons because they fear for their own health and prefer to refuse the treatment rather than interact with these patients. Encouraging all social actors to adopt empathetic approaches towards the HIVpositive persons
Qualifying or completely removing the obligation to disclose HIV/AIDS status to the physicians, given the high extent of refusal by the medical personnel to treat persons living with HIV
Establishment of a legal regime to ensure that the authorities are sanctioned in cases of disclosure of HIV/AIDS status by the public authorities, regardless of the extent to which the disclosure has actually caused harm

Analysis of the additional legal instruments to guide the NCCD towards achieving an effective protection in cases of discrimination, so that the principles of “freedom of expression” or the high standards of proving a “causal link” to the act of discrimination are not barriers to protecting the persons living with HIV from discrimination
Establishment of clear legal instruments, accompanied by control mechanisms, regarding the purchase and distribution of antiretroviral treatment by the public authorities, in order to give substance to the legal requirements to ensure free access to this treatment






Rejection of the legislative initiative to amend and supplement Law 272/2004 on the protection and promotion of the rights of the child, which may have the effect of outlawing any prevention and communication campaigns aimed at groups vulnerable to HIV/AIDS

Abrogation of Article 354 of the Criminal Code which criminalises the transmission of HIV, or at least its qualification and its significant circumstancing in order to reduce the legal uncertainties resulting from the poor wording of the article, the risks of abuse and to finally reflect the realities and the scientific and social changes that have occurred since this article was adopted

92
Although motivated by common goals, NGOs seem unable to align and support each other in a unified effort to encourage and accelerate the development and approval of the National Strategy for the Surveillance, Control and Prevention of HIV/AIDS and the continued provision of antiretroviral treatment for the persons living with HIV
Introduction of mechanisms to expand students’ access to health education programmes opposable to the Ministry of Education, as an effective method of implementing their right to health and education
Establishment of an obligation for the competent authorities to involve NGOs in the necessary intersectoral mechanisms and to identify means of contracting them to perform activities in the HIV/AIDS field









Establishment of an effective mechanism for monitoring the fulfilment of the obligations of the authorities such as the Ministry of Education and the Ministry of Labour and Social Solidarity under the HIV Law – including the obligation of these authorities to publish in a publicly accessible form the activities carried out in accordance with these obligations
Close cooperation between local authorities and NGOs is needed in order to carry out prevention campaigns that can be launched with information and education sessions for the general public. The involvement of the associations of patients living with HIV is also a valuable resource that can be used in information campaigns. The choice of the information channels must take into account the target audience: the internet, the media and the NGOs relevant to the topic represent easily accessible sources of information
Establishment of an obligation for the competent authorities to involve organisations of groups of persons affected by HIV/AIDS in the necessary intersectoral mechanisms and to identify ways of contracting them to perform activities in the HIV/AIDS field
Clarification of the legal status of the HIV/AIDS Commission and establishment of a mechanism to monitor its work (especially in relation to the development of national plans, given their importance in the effective provision of access to treatment)
93
Defining the common goal and aligning the efforts of all social actors (NGOs, state authorities, patient associations, general public) to increase the effectiveness of their actions:

94