
FEATURING
• Navigating the Terrain of Electronic Mountain Biking Injuries
• Post-Concussion Sleep Disturbance: A Prevalent and Persistent Problem
• Tendons into the 21st Century: An ISTS Recap
VOLUME 42 ISSUE 1 2024
health
Sport
REGULARS
02
SMA Board Chair, Dr Kay Copeland, shares new developments and upcoming plans for SMA in 2024. 08

Jamie Crain discusses the new concussion guidelines and summarises this edition’s feature articles.



Do shoes or orthotics change kneecap joint loads?
Sam Kayll reviews the literature regarding the impact of shoes and orthotics on patellofemoral joint loads.

Opinions expressed throughout the magazine are the contributors’ own and do not necessarily reflect the views or policy of Sports Medicine Australia (SMA). Members and readers are advised that SMA cannot be held responsible for the accuracy of statements made in advertisements nor the quality of goods or services advertised. All materials copyright. On acceptance of an article for publication, copyright passes to the publisher.
Contents
From the Chair
Publisher Sports Medicine Australia State Netball and Hockey Centre – Parkville 10 Brens Drive Parkville VIC 3052 sma.org.au ISSN No. 2205-1244 PP No. 226480/00028 Copy Editors Archie Veera and Anelia du Plessis Marketing and Member Engagement Manager Sarah Hope Design/Typesetting Perry Watson Design Cover photograph Jacob Wackerhausen/gettyimages Content photographs Author supplied; www.gettyimages.com.au 12 Post-Concussion Sleep Disturbance: A Prevalent and Persistent Problem
and
Mountain
Injuries
Maree Cassimatis outlines the implications of sleep disturbance on individuals with concussion and provides considerations for practitioners. FEATURES 04 Shocks
Bruises –Navigating the Terrain of Electronic
Biking
Dr Gemma Ruddick analyses the injury outcomes of electronic mountain bike users. 03 From the CEO
VOLUME 42 • ISSUE 1 2024
18
Dr Jodie Dakic examines common questions about pelvic health issues experienced by exercising women.

26
Tendons into the 21st Century: The Sixth International Scientific Tendinopathy Symposium
Dr Anthony Nasser recaps session highlights from the most recent International Scientific Tendinopathy Symposium.

23
Do the feet of male and female netball players differ?
Implications for shoe fit
Maddison Kirk discusses the unique factors of male netball players’ feet and offers suggestions for improving footwear design.





29
Group-based
Frédérique Dupuis shares her assessment of the effectiveness of group-based physiotherapy interventions.

–
Pelvic health in exercising women
Are women being helped?
INTERVIEWS 32
Who Shaped SMA: Professor Garry Allison 43 Sports Trainer Spotlight: Nicola Carlish 39
Mins With: Dr Samantha McLeod 36
Medicine Around the World: Qatar
People
5
Sports
physiotherapy programs are effective in treating prevalent musculoskeletal conditions
VOLUME 42 • ISSUE 1 2024 1

FROM THE CHAIR
Reviewing SMA’s Strategic Plan in 2024 to bring
more value to members.
DR KAY COPELAND, CHAIR OF THE BOARD OF DIRECTORS (SMA), OUTLINES WHAT LIES AHEAD FOR SMA IN 2024.
Welcome to our first Sport Health for 2024.
With the year in full swing, so too is our work on bringing value to our members. The SMA Board are coming together for our planning day in April, to review our business strategy and direction, plan for improved services and more member benefits, and evaluate our ongoing business growth and sustainability. This discussion will feed the framework for the 2024-2027 SMA Strategic Plan, which will be launched later this year.
This year, we look forward to hosting our joint Conference with Australasian College of Sport and Exercise Physicians (ACSEP) at the Melbourne Cricket Ground, on October 16 – 19. Last year’s SMA Conference delegates noted the variety of multidisciplinary lectures, workshops and symposia, and excellent opportunities for networking and socialising. This year’s co-convened event with ACSEP will only add to this, offering more content, more delegates and ultimately a richer and more diverse learning experience. Early bird registrations are now open, and we look forward to seeing you there.
To increase the value we offer the sports medicine and sports science
This year, we look forward to hosting our joint Conference with ACSEP at the MCG on October 16 – 19.
many and varied disciplines that make up SMA’s membership.
Our nationally recognised training and Safer Sport programs are also expanding, with hundreds of public course session options available, including our new ‘Considerations for athletes with a disability’ course. Whether you are seeking to upskill or refresh your knowledge, we hope to see you in attendance in person or online.
disciplines we represent, SMA has started working closely with specific discipline groups to develop even more tailored learning opportunities. For starters, we’ve recently convened a Sports Doctors Special Interest Group, of five enthusiastic and committed sports doctors, who are already framing up new course offerings for our Sports Doctor members.
Alongside this, we already have a packed professional development events program scheduled. Our State Councils and Member Education Advisory Committee have strategically developed a program that offers PD opportunities to the
A major focus for many of our members this year is the upcoming Olympic and Paralympic Games to be held in Paris. Preparations are well underway for our Australian athletes and their support crews, including the health professionals who will be working hard to ensure they achieve their best result possible. If you are attending this year’s Games, we want to hear from you so that we can acknowledge and celebrate your involvement. Get in contact with the SMA team via info@sma.org.au.
I look forward to an exciting 2024 for SMA members and hope to see all of you at an SMA event this year.
 Dr Kay Copeland
Dr Kay Copeland
2 VOLUME 42 • ISSUE 1 2024 FROM THE CHAIR
 FROM THE CEO
FROM THE CEO
An exciting start to the year with new member resources.
Welcome to the first issue of Sport Health in 2024.
This year has already had a busy start with the launch of the ‘Concussion and Brain Health Position Statement 2024’ developed by the AIS in collaboration with SMA and other peak sporting organisations. The new guidelines lay out return to play and return to work/study protocols, and will help to keep our young and community-based athletes safe.
We have also launched a new online course as part of our Safer Sport offering. The ‘Considerations for Athletes with a Disability’ course has been developed in conjunction with Sport NSW and aims to provide sports trainers and first aid providers with greater awareness of the unique considerations for athletes with a disability and the considerations needed to provide specialised support across disability classifications.
The SMA online store is now open. Available for purchase are sports trainer merchandise value packages, webinar recordings, and much more. If you have any suggestions or requests for other items you would like to see made available, please let us know.
The new concussion guidelines lay out return to play and return to work/study protocols, and will help to keep our young and community-based athletes safe.
effectiveness of group-based physiotherapy programs for treating musculoskeletal conditions. With implications of concussion front of mind in recent months, Maree Cassimatis examines the occurrence of post-concussion sleep disturbance, and offers a summary of assessment tools and future research directions.
In this edition of Sport Health, we have featured a wide variety of topical articles that will appeal to the varied interests of our multidisciplinary membership base. Dr Jodie Dakic outlines commonly held concerns from exercising women regarding pelvic health and shares strategies for improving support. In addition, Frédérique Dupuis discusses the
The gear we use to participate in sport and physical activity is integral to ensuring participants remain injury free. In footwear, Sam Kayll analyses the impact of shoes and orthotics on kneecap joint loads, and Maddison Kirk investigates differences between the feet of male and female netball players and provides suggestions for improved shoe fit. With use of new automated technologies on the rise, Dr Gemma Ruddick explores the injury incidence and demography of electronic mountain biking injuries and what this means for the growing uptake of the activity.
We hope you enjoy this edition of Sport Health and find it informative and thought-provoking.
 Jamie Crain
Jamie Crain
VOLUME 42 • ISSUE 1 2024 3 F ROM THE CEO
SMA CEO JAMIE CRAIN SHARES RECENT ACTIVITIES AND UPDATES FOR SMA.
Shocks and Bruises Navigating the Terrain of Electronic Mountain Biking Injuries

ELECTRONIC MOUNTAIN BIKES HAVE BURST ONTO THE SCENE AND ARE AN INCREASINGLY COMMON SITE ON THE TRAILS. THIS IS OCCURRING DURING A TIME WHEN MOUNTAIN BIKING OVERALL IS GROWING IN POPULARITY IN AUSTRALIA AND AROUND THE WORLD. AUSPLAY STATISTICS
INDICATE THAT OVER 470,000 AUSTRALIANS PARTICIPATED IN MOUNTAIN BIKING IN 2023, WITH THE PEAK YEARS OF THE PANDEMIC BRINGING AN ADDITIONAL 180,000 INTO THE SPORT. IN 2023 IT WAS LISTED IN THE TOP 10 SPORT RELATED ACTIVITIES FOR MALES IN REGIONAL AND RURAL AREAS AND IN MALES AGED 35-54YRS.
Electronic mountain bikes (EMTBs) differ from traditional mountain bikes (MTBs) in several ways. The most obvious is the difference in overall weight. A review of popular 2023 model EMTBs weighed between 15-26kg and traditional mountain bikes usually weigh in the range of 12-16kg. The positioning of the battery also leads to a difference in weight distribution through the bike.
Anecdotally, EMTBs also attract an older demographic to the typical MTB population. Common justifications for the older demographic is that these riders may have been previously limited
4 V OLUME 42 • ISSUE 1 2024 FEATURE
DR GEMMA RUDDICK HDR Investigator Award Winner –2023 SMA ACT Research Awards

by their physical capacity and the pedal assist function of EMTBs mean they are now able to participate more fully in the sport. There is some insinuated association that these riders are also more inexperienced, however, this has not been specifically studied. Another possible reason could also be related to the higher cost of EMTBs being outside of the budget of some younger riders.
Mountain biking is a sport which carries potential risk of acute and possibly severe injury.
With the rise in popularity of EMTBs and considering the differences in bike design and rider demographics, a
study was designed to look at the injury profile of EMTB riders. All previous electric powered bicycle injury studies had not specifically examined MTBs, instead they were either unspecified or studied e-road bikes only. These studies did show that overall, there were more serious injuries by e-road bike users compared to human-powered bikes.
The study designed to address this gap in knowledge was a cross-sectional epidemiological study. It included an online voluntary survey for adult electronic mountain bike riders in the ACT and NSW who sustained an injury whilst riding at a mountain biking facility across the summer of 2022-2023.
Injury events
In most MTB injury events riders reported a combination of contributing factors. Factors can usually be divided up into different categories. Commonly cited trail and terrain factors include poor trail conditions such as muddy or slippery surfaces, obstacles such as rocks and tree roots, the technicality of the terrain and travelling downhill. Environment factors can include poor weather or pressure situations such as a race. Rider factors commonly contributing to injury events may include rider error such as incorrect form when landing a jump or riding on terrain above their skill level.
In this EMTB study, most injury events occurred during recreational rides, on moderate (blue) trails whilst travelling downhill. A point of difference between this and traditional MTB injuries was the increased frequency of injuries that occurred whilst riding uphill. With the rise in popularity of EMTBs there has been some pushback from traditional MTB riders with common complaints related to the etiquette of EMTBs passing on trails uphill. All uphill injuries, however, reported in this study were cited as a result of an obstacle and not a collision with a person.
Injury locations and types
A systematic review of MTB injury studies consistently found that the most frequent injury sites were the lower limbs, upper limbs, and clavicle. The most frequent injury types were lacerations, abrasions, and contusions. Other frequent injuries included fractures, dislocations, strains, and sprains. Concussions were reported with higher frequencies in paediatric studies, compared to adult only, or combined studies, and accounted for up to 10% of all injuries.
The results of this study found no significant difference in the location and type of injuries sustained
VOLUME 42 • ISSUE 1 2024 5 FEATURE
Photo: Dan-Edwards/ gettyImages
Shocks and Bruises Navigating the Terrain of Electronic Mountain Biking Injuries
compared to other similar MTB injury studies. The most common injury types were skin lacerations, abrasions or contusions followed by other MSK injuries including bone fractures. The most common locations for injuries were on the limbs.
Injury management and impact
Nearly half of the injuries were selfmanaged which is in line with minor skin injuries being the most common injury type. A third were managed in the emergency department and these were overwhelmingly bone fractures. Another 25% were managed by general practitioners, physiotherapists, nurse led clinics or other allied health services.
Nearly half of injuries resulted in riders unable to participate in the sport for at least seven days following the injury and nearly 60% reported moderate to severe pain. Good acute pain management plans should be considered an important factor in acute injury management and could significantly decrease injury impact not only in sport participation, but on other areas such as work or study.
Demographics
The main difference between EMTB riders in this study compared to other MTB studies was the demographic of the participants. There was an expected higher representation of riders over 40 years, with a median age of 49 years, compared to 28 years in similar traditional MTB studies.
An unexpected finding was the higher representation of female riders. The higher rate of female responses in this study could have been because they are more likely to respond to surveys, or possibly that they have a higher rate of injury. Another potential reason is that some female and new mountain bikers express a barrier to them entering the sport is that they are concerned that they will not be able to ‘keep up’. EMTBs may remove this barrier providing

an opportunity to get a more diverse demographic involved in the sport.
Summary
This first look into EMTB injuries found that they were not more severe than human powered MTB injuries and that the injury types and locations were comparable. The highlight of this study was the difference in demographics. The first point of difference is that EMTBs were noted to attract older riders, the other point of difference was the higher than expected representation of female riders.
A point of difference between this [study] and traditional MTB injuries was the increased frequency of injuries that occurred whilst riding uphill.
As we age, participation in exercise remains a significant pillar to overall mental and physical wellbeing for both males and females. In Australia, participation in sport declines with age, and women’s participation rates in sport are lower than men. EMTB’s may be a gateway to increasing participation in the sport of mountain biking by attracting a wider demographic and keeping current traditional MTB riders on their bikes for longer.
For article references, please email info@sma.org.au
Author Bio

Dr Gemma Ruddick is a General Practitioner Registrar in Canberra with an interest in sports medicine. She was awarded the 2023 SMA ACT Research Award for HDR Investigator. Her study on electronic mountain bike injuries was completed as part of her Masters in Healthcare in Remote and Extreme Environments at the University of Tasmania under the supervision of Dr Larissa Trease and Dr Sue Pearson. Gemma has previously completed research into bone stress injuries in elite athletes at the Australian Institute of Sport.
6 V OLUME 42 • ISSUE 1 2024 FEATURE
Photo: Jacob Wackerhausen/ gettyImages
Add comfort to every step
Every day, easy runs for all runners, novice or experienced, who tend to heel strike, and are looking for a high cushioned, stable neutral ride.
Updated Knit Collar & Tongue Construction
A more adaptive, supportive fit.

Rearfoot
PureGEL™
For improved softness and shock attenuation.
New Engineered Knit Upper
Softer feel and improved midfoot hold.
FF BLAST™ PLUS ECO
Premium cushioning and soft underfoot feel.
New Hybrid ASICS Grip
A combination of both ASICSGRIP™ & AHAR™ outsole rubbers provide better grip



GELNIMBUS™
26
PROFESSIONAL BUYERS PROGRAM Join the ASICS Professional Buyers Program to keep up to date with the latest ASICS performance footwear and technology and receive discount on footwear. *T&Cs apply. SCAN TO REGISTER. LEARN MORE
Do shoes or orthotics change kneecap joint loads?
SAM KAYLL 2023 ASICS SMA Conference Best Poster Winner -People’s Choice Award

Patellofemoral pain is a highly prevalent condition affecting young people through to older adults, including both active and sedentary populations. Clinical guidelines recommend exercise, and education on load, selfmanagement strategies and the nature of patellofemoral pain, as the cornerstones of patellofemoral pain treatment. However, 57% of people still report symptoms five to eight years following diagnosis, showing that current treatment is sub-optimal for this non-self-limiting condition. The persistent nature of patellofemoral pain symptoms, the poor long-term prognosis, and limited evidence on effective treatment options, means patients may also be at an increased risk of developing patellofemoral osteoarthritis compared to the general population, although this is yet to be confirmed by prospective studies.
Patellofemoral pain is defined as pain at or around the patella during activities that load the patellofemoral joint, such as running, squatting, or descending stairs. It is postulated that treatment strategies that reduce patellofemoral joint load may be efficacious for patellofemoral pain. Biomechanical foot-based interventions, such as
footwear, insoles, and foot/ankle taping or bracing, have been proposed as low-burden treatment approaches that may reduce patellofemoral joint loads and, therefore, improve symptoms.
For example, minimalist footwear (i.e., lightweight shoes with thin flexible soles that do not possess any motion control properties) can reduce knee flexion and quadriceps muscle force, thereby reducing patellofemoral joint load. Likewise, insoles with medial support, taping and bracing can reduce foot pronation, a motion theoretically linked to an increase in patellofemoral joint load via tibial and femoral internal rotation. As such, these interventions are commonly used in the clinical setting and insoles are recommended as best practice in international guidelines for managing patellofemoral pain.
Despite the biomechanical rationale and widespread use of these interventions, no study has
Photo: PeopleImages/ gettyImages 8 V OLUME 42 • ISSUE 1 2024 FEATURE
Biomechanical
foot-based interventions, such as footwear, insoles, and foot/ankle taping or bracing, have been proposed as low-burden treatment approaches
that may reduce patellofemoral joint loads.

systematically reviewed research investigating the effects of biomechanical foot-based interventions on patellofemoral joint loads. Although one recent systematic review included some studies that evaluated footbased interventions, its focus was on comparing patellofemoral joint reaction force across everyday activities, and it did not conduct a sub-group analysis of intervention effects. Thus, the specific effect(s) of biomechanical foot-based interventions on patellofemoral joint loads remains unclear.
Patellofemoral joint loads may be quantified using direct (reaction force and pressure) or surrogate (external flexion or internal extension moment) measures. Although 3D models are considered more accurate, the majority of researchers have estimated patellofemoral joint reaction force using sagittal plane 2D models that combine the knee flexion angle and moment with mathematical representations of the extensor mechanism. To calculate pressure, the reaction force is divided by the contact area obtained from previous studies. Where there are high amounts of pressure during gait, the knee moment will also be high. To fully understand the effects of interventions designed to reduce patellofemoral loads, it is thus important to consider
research that has investigated each of these direct and surrogate estimates of patellofemoral joint loads.
Therefore, we undertook a systematic review and meta-analysis aimed at evaluating the effect(s) of biomechanical foot-based interventions on patellofemoral loads during walking and/or running in adults with and without patellofemoral pain or osteoarthritis.
HOW DID WE GO ABOUT THIS?
We searched five databases for studies that assessed the effects of biomechanical foot-based
interventions (footwear, insoles, taping or bracing) on peak patellofemoral joint loads (quantified by patellofemoral joint pressure, reaction force, or knee flexion moment) during walking or running in people with patellofemoral pain or osteoarthritis.
Where there were three or more studies that were sufficiently similar, meta-analysis was performed. We assessed the risk of bias using the Cochrane Risk of Bias 2 for randomised cross-over trials and the certainty of evidence from each meta-analysis with the GRADE approach. The GRADE approach considers a range of domains, including the risk of bias, that may make the result of a meta-analysis more or less certain.
We found that minimalist footwear reduced peak patellofemoral joint loads by 7.4% on average compared to conventional footwear during walking and running combined.
We identified 33 eligible studies. There were three eligible comparisons for meta-analysis during walking and running combined: minimalist vs. conventional footwear, insoles with medial support vs. no insole, and rocker vs. non-rocker footwear. We sub-grouped each analysis by task (walking or running) and population (patellofemoral pain, healthy or patellofemoral osteoarthritis). However, some of these sub-groups were based on one or two studies and we could not draw firm conclusions.
VOLUME 42 • ISSUE 1 2024 9 FEATURE
Photo: choochart choochaikupt/ gettyImages
Do shoes or orthotics change kneecap joint loads?
WHAT DID WE FIND?
The results are summarised in Figure 1
Minimalist footwear reduces patellofemoral joint loads
We found that minimalist footwear reduced peak patellofemoral joint loads by 7.4% on average compared to conventional footwear during walking and running combined. These findings are similar to a previous systematic review and meta-analysis that found high-heeled footwear increase the knee flexion angle and moment during walking. The novel findings from our study show that even conventional footwear with a moderate heel and/or increased amounts of cushioning will increase patellofemoral joint loads when compared to minimalist footwear.
We attribute the reduction in patellofemoral joint loads observed with minimalist footwear to two primary mechanisms. Firstly, minimalist footwear reduces step length (increasing cadence). A reduction in step length brings the stance limb closer to the centre of mass,

reducing knee flexion and quadriceps demand. Studies consistently show a shorter step length in minimalist footwear; and an increased cadence reduces patellofemoral joint load. The second factor is the combination of reduced stack height, weight, and heel-to-toe drop and increased flexibility in minimalist footwear. These characteristics lower the knee flexion angle, moment, and quadriceps muscle force, resulting in a reduced patellofemoral reaction force.
After sub-grouping by task (walking or running) or population (healthy, patellofemoral pain or patellofemoral
osteoarthritis), differences in patellofemoral joint load between minimalist and conventional footwear were only evident during running (9.5% difference on average) or in participants with patellofemoral pain (albeit, only one study on runners was available). This suggests that minimalist shoes may only be effective during activities that provoke higher joint loads, such as running, or only in people with patellofemoral pain. Patellofemoral pain is particularly prevalent amongst runners, likely because patellofemoral joint loads are high over numerous loading cycles. As such, the differences in patellofemoral
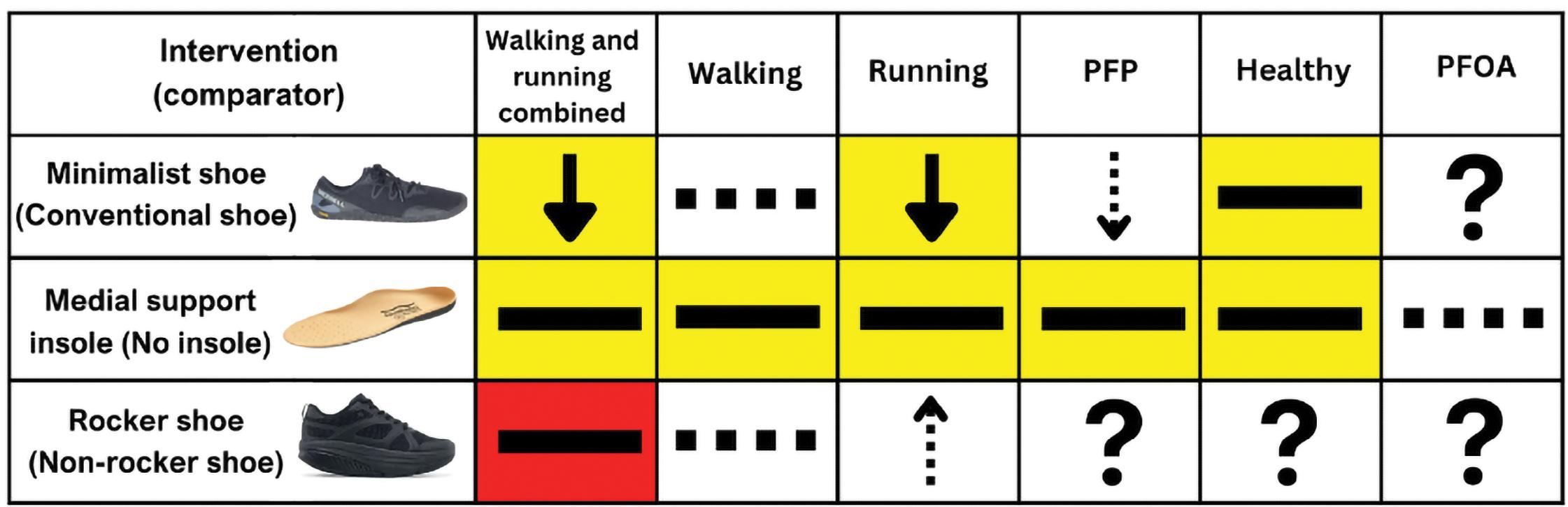




 Figure 1: Summary of results. Reduction, increase, and no difference in PFJ loads from meta-analysis; Reduction, increase, and no difference in PFJ loads based on one or two individual studies; = no data available; very low, low, moderate, and high certainty evidence according to GRADE; White = GRADE not performed due to limited studies; PFP = patellofemoral pain; PFOA = patellofemoral osteoarthritis
Figure 1: Summary of results. Reduction, increase, and no difference in PFJ loads from meta-analysis; Reduction, increase, and no difference in PFJ loads based on one or two individual studies; = no data available; very low, low, moderate, and high certainty evidence according to GRADE; White = GRADE not performed due to limited studies; PFP = patellofemoral pain; PFOA = patellofemoral osteoarthritis
10 V OLUME 42 • ISSUE 1 2024 FEATURE
Photo: AndreyPopov/ gettyImages
loads will become greater when considering cumulative load. For example, runners will experience 18.28*BW (1,462 kg for an 80kg person) less joint force in minimalist footwear (despite an increase in cadence and the number of loading cycles) compared to conventional footwear over one kilometer (based on a calculation of total force impulse [BW x stance time] x number of steps per kilometer). Therefore, clinicians may consider recommending minimalist footwear to reduce patellofemoral joint loads in runners or people with patellofemoral pain.
Medial support insoles and rockersoled footwear have no effect on patellofemoral joint loads
The results from our pooled analysis indicated that medial support insoles and rocker-soled footwear do not alter patellofemoral joint loads when compared to no insole and conventional footwear during walking, running, and walking and running combined. In contrast, two previous studies showed medial support insoles are effective for the treatment of patellofemoral pain. One was a cohort study that gave insoles to people with patellofemoral pain over a 12 week period. The other was a randomised controlled trial that compared medial support insoles to ‘wait and see’. However, when comparing flat sham insoles to medial support insoles for the treatment of patellofemoral pain and osteoarthritis, studies have found no difference in pain between groups in the immediate, medium (twelve weeks), and long-term (one year). Additionally, medial support insoles are of no additional benefit to a physiotherapy program over the short, medium, and long term, although the same study did find medial support insoles were effective compared to sham insoles at six weeks. Our finding of no load reduction with medial support insoles in combination with the above studies indicates that the pain reducing effects of insoles may largely be contextual, rather than biomechanical (medial support reducing pronation, femoral motion and patellofemoral joint pressure). Contextual effects contribute to a
[Research] suggests that minimalist shoes may only be effective during activities that provoke higher joint loads, such as running, or only in people with patellofemoral pain.
significant proportion of treatment effects in clinical practice. For example, researchers have found that contextual effects, such as a credible placebo/ sham and a positive therapeutic relationship, are responsible for around 61% of the overall effect of interventions used to treat knee osteoarthritis.
CLINICAL IMPLICATIONS
We found that minimalist footwear reduces patellofemoral joint load during running. However, it is uncertain whether these biomechanical effects translate to symptomatic benefits. For instance, a recent systematic review found that patellofemoral joint reaction force did not differ between adults
with and without patellofemoral pain during everyday activities, including running, suggesting that increased patellofemoral joint loads are not a consistent feature of patellofemoral pain. Furthermore, the relationship between patellofemoral joint load and pain is uncertain. In fact, there is evidence that pain may be more closely related to factors other than load, such as kinesophobia. Thus, even though minimalist footwear reduces patellofemoral joint loads, further research is needed to determine whether clinicians should advise patients to use minimalist footwear to manage patellofemoral pain.
CONCLUSION
Minimalist footwear may reduce peak patellofemoral joint loads slightly compared to conventional footwear during running only. Medial support insoles may not alter patellofemoral joint loads during walking or running and the evidence is very uncertain about the effect of rocker-soled shoes during walking and running combined. Clinicians aiming to reduce patellofemoral joint loads during running may consider minimalist footwear.
For article references, please email info@sma.org.au
Author Bio
Sam Kayll is a PhD Candidate at The Centre for Health Exercise and Sports Medicine at The University of Melbourne. His research is focused on the effect of foot-based interventions on knee biomechanics. He is currently investigating how patellofemoral pain and footwear changes knee biomechanics in adolescents. Alongside his research, Sam works as an osteopath at Balwyn Sports and Physiotherapy Centre in Melbourne, sits on the Victoria State Council for Sports Medicine Australia, and is on the Osteopathy Australia Educational and Advisory Committee. Sam is also involved in teaching in the Doctor of Physiotherapy program at The University of Melbourne.
VOLUME 42 • ISSUE 1 2024 11 FEATURE
Post-Concussion Sleep
A Prevalent and Persistent Problem
SLEEP DISTURBANCES ARE ONE OF THE MOST COMMONLY REPORTED COMPLAINTS AFTER CONCUSSION, WITH 30 TO 70% OF INDIVIDUALS WITH CONCUSSION ENDURING SLEEP DISTURBANCE POST-INJURY. NOT ONLY ARE SLEEP DISTURBANCES HIGHLY PREVALENT IN THE ACUTE PHASE OF CONCUSSION, BUT THEY ARE ALSO KNOWN TO PERSIST FOR YEARS THEREAFTER.
Until recently, screening for sleep wake disturbances in individuals with concussion has largely been disregarded and overlooked in the overarching management of concussion. Inadequately recognising early signs of sleep disturbance after concussion represents a missed opportunity for treatment that could play a significant role in enhancing recovery outcomes.
This article discusses how sleep disturbance may present in individuals with concussion. Available assessment tools for evaluating sleep, as well as, considerations for future research in this area are also discussed.
Concussion and Sleep
Concussion is a subset of mild traumatic brain injury (mTBI) that results in the rapid onset of temporary neurological dysfunction. Symptoms
associated with concussion are widespread, with varying frequency and severity, and can consist of disturbance to physical, cognitive,
ٚ Headache
ٚ Postural hypotension
sleep and emotional clinical health domains. Figure 1 summarises the breadth of symptoms observed in individuals with concussion.
ٚ Memory impairment
ٚ Confusion
ٚ Mental fogginess
ٚ Dizziness
ٚ Nausea and/or vomiting
ٚ Motion sensitivity Autonomic
ٚ Phonophobia
ٚ Photophobia
ٚ Convergence insufficiency
ٚ Slowed reaction time
ٚ Reduced concentration and attention span
ٚ Accommodation deficits
ٚ Headache triggered by visual activity
ٚ Balance problems
ٚ Difficulty falling and/ or staying asleep
ٚ Anxiety, depression, rumination
ٚ Limited social interaction, anhedonia, sadness
ٚ Irregular sleep/ wake patterns
MAREE CASSIMATIS 2023 SMA Research Foundation Major Grant Winner
Figure 1 Symptoms of concussion
Sleep & Mood 12 V OLUME 42 • ISSUE 1 2024 FEATURE
Cognitive Vestibular Ocular
Disturbance

A typical pattern of sleep disturbance may involve a report of excessive sleepiness within the first week of injury, followed by difficulty falling and/ or staying asleep in the subsequent weeks after injury.
VOLUME 42 • ISSUE 1 2024 13 FEATURE
Photo: AVAVA/ gettyImages
Sleep is a critical factor in brain healing after a concussive injury. Sufficient sleep duration, quality and timing may be important factors for neuroplastic recovery following concussion. Furthermore, the risk of sporting injuries, including sportrelated concussion, is heightened when athletes are sleep deprived or have poor sleep quality.
The type and onset of sleep disturbance can differ significantly among individuals with concussion. A typical pattern of sleep disturbance may involve a report of excessive sleepiness within the first week of injury, followed by difficulty falling and/ or staying asleep in the subsequent weeks after injury. The initial period of excessive sleepiness may signify the ideal environment required for the brain to restore neurometabolic homeostasis. However, 2 to 3 weeks after concussion, the individual with sleep disturbance often experiences trouble with initiating sleep or maintaining sleep, which in turn may be promoting daytime fatigue.
The underlying mechanism of sleep problems in individuals with concussion is not fully understood. Sleep disturbance following traumatic brain injury has been associated with decreased melatonin production, the occurrence of psychiatric
comorbidities, including anxiety and depression, and impaired hypocretin levels, which may be notable factors contributing to sleep disturbance in this population. Importantly, a higher incidence of sleep disturbance is reported to occur in individuals with concussion/mTBI compared to individuals with moderate to severe traumatic brain injury. One theory suggested for this may be due to the role of awareness, whereby patients with more severe injuries may not have as much awareness of their sleep difficulty. It has also been theorised that individuals with concussion return to daily and work schedules sooner, even though they are not completely recovered, which subsequently results in sleep disturbance persisting for longer in this population group.
Sleep disturbance can exacerbate postconcussion symptom burden, worsen mood, impair cognitive function and the potential for recovery. Patients with poor sleep quality following concussion have been shown to have greater functional impairment 6 months post-injury compared to those without sleep disturbance following injury. This suggests that early identification of sleep disturbance may detect individuals at-risk of adverse concussion recovery outcomes and poor prognosis.

Common Types of Sleep Disturbance After Concussion
The most common sleep-related symptom after concussion is difficulty with sleep initiation and/or sleep maintenance (insomnia). Others with concussion may experience excessive daytime sleepiness, hypersomnia or circadian rhythm disturbance.
Insomnia
Insomnia symptoms consist of trouble falling asleep, trouble staying asleep and early morning awakenings, which can result in daytime fatigue, sleepiness, mood disruption and functional deficits. In adults with mTBI, the prevalence of clinically diagnosed insomnia is 4 to 5 times higher than the general population, and symptoms associated with insomnia are found to occur in 70% of mTBI-affected individuals. One study on children and adolescents with sport-related concussion found that ‘trouble falling asleep’ was reported in 45% of their patient cohort.
Excessive Daytime Sleepiness and Hypersomnia
Excessive daytime sleepiness is characterised by an irrepressible need to sleep that results in an inability to maintain wakefulness or alertness during frequent episodes of the day. A clinical challenge is identif ying
Patients with poor sleep quality following concussion have been shown to have greater functional impairment 6 months post-injury compared to those without sleep disturbance following injury.
14 VOLUME 42 • ISSUE 1 2024 FEATURE
Photo: gorodenkoff/ gettyImages
Abbreviations: ESS, Epworth Sleepiness Scale; ISI, Insomnia Severity Index; mTBI, Mild Traumatic Brain Injury; PSQI, Pittsburgh Sleep Quality Index.
whether excessive daytime sleepiness may have contributions from other sleep disorders, such as insomnia or circadian rhythm disruption, or whether excessive daytime sleepiness is due to an underlying hypersomnolence syndrome. In patients with traumatic brain injury, there is a correlation between injury severity and hypersomnia, with hypersomnia being more prevalent following moderate to severe traumatic brain injury than in those with mTBI.
Circadian Rhythm Disorders
initiating sleep, maintaining sleep and waking at standard wake times may be misinterpreted as insomnia instead of circadian rhythm sleep disruption. One study identified circadian rhythm disruption in 36% of patients with mTBI who were reporting insomnia symptoms.
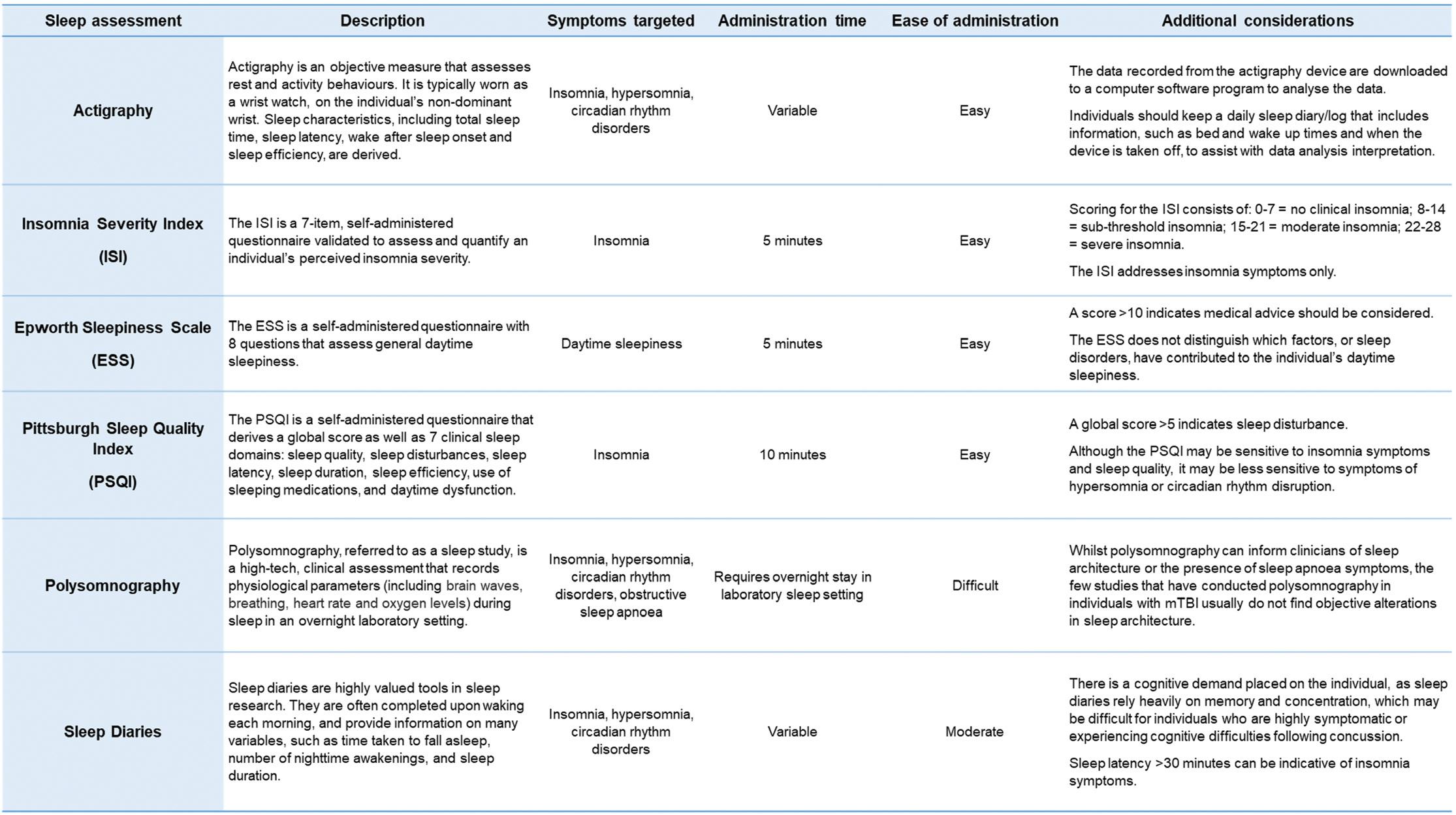
Assessment of Sleep After Concussion
when selecting a suitable assessment tool to monitor sleep behaviour after concussion. These include:
1. How often you will be seeing the patient. Will you see them once or will they return for follow-up appointments?
2. The length of time you have to assess sleep during each appointment.
Sleep disturbance after concussion can be associated with changes in the timing and rhythm of sleep, whereby the body’s biological sleepwake schedule is out of sync with the desired 24-hour environmental schedule. This mismatch is associated with altered rhythm and timing of melatonin secretion and body temperature. The most commonly identified circadian rhythm disorder following concussion is delayed sleep phase syndrome. Circadian rhythm disorders can be misconstrued as insomnia, as complaints of difficulty
It is important for clinicians to assess both nighttime and daytime sleep behaviour, as nighttime sleeping difficulties may be the underlying source of daytime sleepiness, or alternatively, sleep patterns may be linked to a 24-hour circadian shift.
Specific assessment of sleep behaviour in individuals with concussion is often scarce. Current assessments commonly utilised in concussion settings may only briefly enquire about sleep behaviour, such as by asking one or two sleep questions that form part of a larger symptom checklist.
There are some practical considerations to take into account
3. The length of time you have to score and interpret sleep assessment data.
4. The cost of assessment tools, and whether free and low-cost assessments are preferred or more expensive, technologically advanced options are available to you or the patient.
If you are seeing the patient at one point in time, you may choose to administer a few short, validated sleep questionnaires to assess insomnia and daytime sleepiness. In the event of seeing the patient on several occasions throughout the course of their recovery, Table 1
Summary of sleep assessment tools
VOLUME 42 • ISSUE 1 2024 1 5 FEATURE
you may choose to administer both sleep questionnaires and continuous sleep measures, such as a sleep diary or actigraphy monitoring.
Table 1 presents a summary of sleep assessment tools that can be used in individuals with concussion. These sleep assessments vary in cost, availability and administration time to provide clinicians with options to more carefully and comprehensively evaluate sleep in individuals with concussion. The sleep assessments presented were chosen to address the more common types of sleep disturbance observed in those with concussion (insomnia, excessive daytime sleepiness, hypersomnia, and circadian rhythm disorders). There are a number of other commonly used sleep assessments that are also available to clinicians.
Sleep Disturbance in Paediatric Concussion
The paediatric population is a vulnerable group at risk of concussion, with one in five children having experienced a concussion by the age of 10 years old. Although the majority of children and adolescents recover from a concussion within one month, as many as 30% will still experience persistent post-concussion symptoms greater than 4 weeks.
There are unique considerations relating to adolescence and sleep. Adolescence is a period characterised by significant changes, both in growth and development. These changes are especially important in relation to brain function and sleep cycles. Adolescents undergo adaptations to their circadian rhythms as they progress
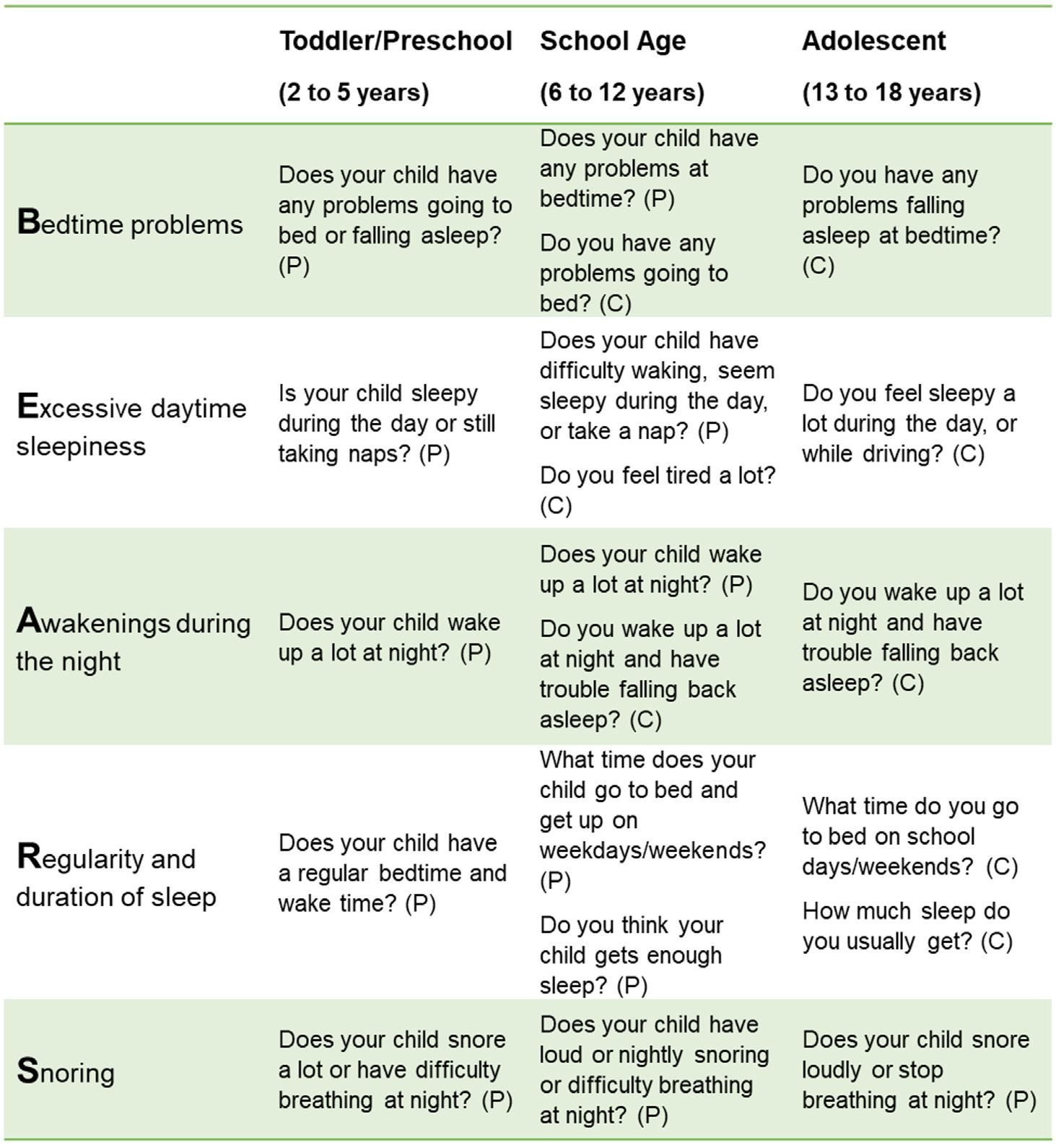
Abbreviations: (C) = child, (P) = parent
Source: Mindell JA, Owens JA. A Clinical Guide to Pediatric Sleep, Diagnosis and Management of Sleep Problems. Philadelphia, PA: Lippincott Williams & Wilkins; 2003.
from childhood to adulthood. There have been studies that demonstrate adolescents and young adults have a biological predisposition for a delayed circadian phase. Therefore, it can be difficult to determine if sleep disturbance found in adolescents with concussion is pre-morbid or as a result of the injury itself. It is also possible that concussion may exacerbate such a pre-morbid tendency.
Studies that have assessed sleep disturbance in paediatric patients with concussion predominantly rely on subjective measures. An observational study conducted in children and adolescents, aged 6 to 18 years old, revealed that sleep disturbance following concussion was associated with poorer outcomes, including exacerbated postconcussion symptom burden and worsened neurocognitive function. A systematic review investigating the consequences of sleep disturbances in paediatric traumatic brain injury conveyed that sleep disturbance was associated with fatigue and poor quality of life following injury.
Obtaining sufficient sleep throughout childhood plays a pivotal role in optimising somatic health, academic performance, and psychosocial wellbeing in the developing brain. This highlights the need to screen for and monitor sleep disturbance in children and adolescents with concussion to mitigate the risk of long-term health consequences.
Table 2 displays the BEARS sleep screening tool, which is a useful resource designed to screen for sleep disturbance in toddlers, preschoolers, school-aged children and adolescents. The resource provides the clinician with structured questions about sleep disturbance that have been modified across developmental age groups.
Research and Clinical Directions
Considering the high prevalence and long-term sequelae of postconcussion sleep disturbance, sleep needs to be routinely assessed in individuals with concussion. The use of standardised and validated sleep
Table 2
The BEARS sleep screening tool
16 VOLUME 42 • ISSUE 1 2024 FEATURE
assessment tools is encouraged. If available, combining subjective measures with objective measures will strengthen the assessment of sleep disturbance in this population group and improve the veracity of findings in future research studies.
Further research is needed in the paediatric population to investigate the implications of sleep disturbance in children and adolescents across the concussion recovery continuum, and elucidate how disruptions in sleep post-injury impact cognitive and psychological development in the developing brain. Moreover, there is a lack of evidence-based treatment options for sleep disturbance following concussion. Some studies have explored potential treatment options for sleep disturbance in traumatic brain injury populations, including sleep hygiene education, cognitive behavioural therapy, and melatonin supplementation. However, there is a paucity of robust studies exploring these therapies in concussion specific cohorts.
Take Home Points
ٚ Sleep disturbance is commonly reported following concussion.
ٚ Types of sleep disturbance identified in individuals with concussion include insomnia, excessive daytime sleepiness, hypersomnia and circadian rhythm disruption.
ٚ Post-concussion sleep disturbance may compromise an individual’s recovery from injury and return to pre-injury activities.
ٚ Routine sleep screening following concussion will improve early identification of those experiencing sleep disturbance during their recovery.
ٚ Further research is needed in the paediatric population to determine the impact of sleep disturbance on the concussion recovery continuum in the developing brain.
For article references, please email info@sma.org.au

Author Bio

Maree Cassimatis is an Accredited Exercise Physiologist with clinical experience working within the areas of chronic disease management, musculoskeletal rehabilitation, and preventive health medicine. Maree is currently a PhD candidate at the University of Sydney. Her PhD thesis is investigating the effects of concussion on sleep, and the implications of sleep disturbance on recovery outcomes in children and adolescents recuperating from concussion. Throughout her candidature, Maree has worked in close affiliation with the Kids Concussion Service at the Children’s Hospital Institute of Sports Medicine, examining various aspects of concussion aftercare, including early recognition, timely intervention, exercise prescription to aid recovery and tailored treatment plans.
VOLUME 42 • ISSUE 1 2024 17 FEATURE
Photo: AnnaStills/ gettyImages
Pelvic Health in Exercising Women
Are women being helped?
DR JODIE DAKIC 2023 Wendy Ey Award for Best Paper –Women in Sport
What is the ‘pelvic floor’ – and what can ‘go wrong’?
The pelvic floor is comprised of passive components: ligaments, fascia, connective tissue and active components: the pelvic floor muscles, which are located at the base of the pelvic cavity. The pelvic floor provides structural support for the pelvic organs. Any change to the function or integrity of these structures can result in development of a pelvic floor disorder.
Why do pelvic floor symptoms occur during sport?
Pelvic floor disorders encompass a spectrum of conditions involving dysfunctions of the bladder and bowel, pelvic organ prolapse, and pelvic pain. During sport, increased intra-abdominal pressure (IAP) during exertion, along with ground reaction forces (GRF), transfers downward forces to the pelvic floor. Pelvic floor muscles contract to counteract these forces, but for some women, the pressure can overwhelm the pelvic floor support, leading to symptoms. Jumping, running, lifting and tackling are common activities that may provoke symptoms.
The pelvic floor muscle can also have increased tone or difficulty relaxing, which may contribute to symptoms such as pelvic pain, sexual dysfunction, urinary symptoms or difficulty emptying the bowel or bladder.

What pelvic floor symptoms do female athletes experience?
There are a broad range of pelvic floor disorders and associated symptoms that female athletes may experience including:
ٚ Urinary incontinence – leaking urine (loss of bladder control)
ٚ Anal incontinence – leaking wind or stool (loss of bowel control)
ٚ Pelvic organ prolapse – feeling of a dragging, pulling, bulging or pressure in the pelvis
ٚ Urinary urgency/frequency – needing to rush to the toilet often and/or a strong/constant urge to urinate
ٚ Pain in the pelvic region
ٚ Painful sex
ٚ Difficulty emptying the bladder or bowel.
How common are pelvic floor symptoms in female athletes?
Pelvic floor symptoms are highly prevalent in female athletes. One in three female athletes experience urinary incontinence (leaking urine) including up to 80% of those engaging in high-impact sports such as gymnastics. Approximately, one in two women who participate in teamball sports report leaking urine. The likelihood of experiencing urinary incontinence is three time greater in elite athletes than recreational athletes. More research across a broad range of sports, into the prevalence
18 VOLUME 42 • ISSUE 1 2024 FEATURE
A recent study by our research group found that one in two exercising women stopped playing a sport when they experienced pelvic floor symptoms.

of other pelvic floor disorders is required. Approximately 80% of power/weightlifter and gymnasts report accidental leakage of wind or stool during sport. Up to one in four weightlifters and 7% of triathlete report symptoms of pelvic organ prolapse. There is limited data on the prevalence of pelvic pain in female athletes, however in a recent mixedsport study, 45% of athletes report pain during sexual intercourse.
Do pelvic floor symptoms occur in younger women and those who have not had children?
Pregnancy and childbirth are a common risk-period for women to develop pelvic floor symptoms. However, women of all ages experience symptoms, including those that have not given birth. A recent systematic review found that one in two young, adolescent, female athletes (<19 years) reported leaking urine during sport. The perimenopausal and menopausal years are another life stage where women commonly develop pelvic floor symptoms. It is important to understand that pelvic floor symptoms effect women of all ages.
What impact do pelvic floor symptoms have on health and performance?
A recent study by our research group (n=4556 symptomatic, Australian women) found that one in two exercising women stopped playing a sport when they experienced pelvic floor symptoms. We also found that one in three young, symptomatic women (18-25 years) stopped a form of sport due to their symptoms. Exercising women also reported substantial impact on training and performance. In order to avoid provoking symptoms they reduced training load, intensity or avoided high-impact activities. Elite gymnasts have reported leaking urine caused them to lose concentration during routines. In a recent qualitative study, we found that pelvic floor symptoms impacted on women’s

social well-being and enjoyment of participation in sport. Women reported embarrassment, anxiety that their symptoms may become known to others, and avoidance of group training sessions. They experienced distress when required to wear fitted or light/bright uniforms which made concealing leakage or continence underwear and pads challenging. Restricting fluid intake to avoid leakage was another coping strategy commonly used, placing exercising women at risk of dehydration.
Do female athletes commonly tell anyone within sports or exercise settings about their symptoms?
Women are often reluctant to discuss their pelvic floor symptoms with anyone. We discovered that amongst symptomatic women in our large survey study (n=4556), a majority had not told anyone within their sport or exercise setting that they were experiencing symptoms. The reasons for not telling included embarrassment and a lack of pelvic health knowledge or education. Women did not know who to tell or what treatment options were available to them. In studies across a variety of elite sports settings, less than 10% had told someone within their performance support team. Providing
Photo: Thanumporn Thongkongkaew/ gettyImages
VOLUME 42 • ISSUE 1 2024 19 FEATURE
Photo: SciePro/ gettyImages
Pelvic Health in Exercising Women
Are women being helped?
education to female athletes on pelvic health can facilitate their ability to seek help and disclose symptoms.
Are we currently screening for pelvic floor symptoms within Australian sports and exercise settings?
We recently investigated the pelvic floor screening practice of Australian professionals working with exercising women (n=636) i.e. physiotherapists, personal trainers, doctors, coaches and exercise physiologists/scientists. We found that at risk-groups of women are not commonly being screened for pelvic floor symptoms. Despite the child-bearing years being a common period for pelvic floor symptom onset, one in two professionals do not screen for PF symptoms in pregnant or post-natal women. Even lower rates of screening were occurring in menopausal women and young high-impact athletes, all of whom have a high rate of experiencing pelvic floor symptoms during sport.
How can we make pelvic floor screening safe and acceptable in sports settings?
Pelvic floor symptoms are personal in nature and so it is crucial to consider the method for screening prior to

asking. In a recent mixed-methods study conducted by our team, women made several recommendations for safe ways to start a conversation on pelvic health. Prior to asking direct questions on pelvic floor symptoms, women preferred that professionals demonstrate knowledge on the topic, explain why they are asking, what help may be provided and who will have access to their answers. Integrating questions into pre-existing general health and pre-exercise questions can help normalise the topic. Seeking consent to ask the questions, demonstrating comfort and knowledge on the topic and considering the timing and privacy of the screening are also important considerations.
What can be done in sports setting to improve the management of pelvic floor disorders?
such as pelvic floor physiotherapists can allow for referral, provision of education sessions and collaborative management with the aim of enhancing sport performance and participation. Uniform designs that allow a pad to be worn or leakage hidden should also be considered.
Cautions to consider with pelvic floor screening
In community dwelling women, there is highquality evidence that exercises for the pelvic floor muscles are effective at curing or reducing the symptoms of incontinence and pelvic organ-prolapse.
Sports settings can create pelvic health safe environments by creating an open and respectful environment, led by positive role models and advocates (support staff or peers). Both professionals and women requested that professional development on pelvic health be provided to those working closely with exercising women, so that they can better support those experiencing symptoms. Building referral networks and relationships with professionals with specialised knowledge of pelvic floor disorders
Considering the sensitive nature of pelvic floor symptoms, it’s important for professionals to show cultural sensitivity and recognize that for some, discussing pelvic floor symptoms may evoke emotional reactions, particularly in those with a history of trauma or challenging childbirth experiences. Some suggested ways to address this include: offering women the choice of who they would prefer to talk to and gauging their comfort levels during discussions. Referral network for those experiencing distress should be considered prior to screening. It is important to remember that pelvic floor symptoms may occur due to more serious underlying health conditions and that referral to an appropriate medical professional is initiated where indicated.
What factors put female athletes at risk of developing pelvic floor symptoms?
We know that the load of pregnancy and childbirth places women at risk
Photo: gpointstudio/ gettyImages
FEATURE
of developing a pelvic floor disorder. Beyond this, there is limited research into what places female athletes at risk of developing pelvic floor symptoms. Factors such as generalised hypermobility, disordered eating/ low-energy availability and training volume have been investigated without conclusive evidence thus far. Further research is needed before we can screen for athletes at risk of developing symptoms.
Management of pelvic floor symptoms in athletes?
In community dwelling women, there is high-quality evidence that exercises for the pelvic floor muscles are effective at curing or reducing the symptoms of incontinence and pelvic organ-prolapse. There is a need for high-quality clinical research trials, to prove the effectiveness in women who experience symptoms during high-load sports. Preliminary studies in small populations, including a pilot RCT, have shown promising results. Many women may have some difficulty consciously contracting or relaxing the pelvic floor muscles. Therefore, pelvic floor muscle training, delivered under professional supervision to ensure a correct technique and exercise prescription dosage is the current gold-standard. However, pelvic floor muscle training delivered as part of a general group-exercise session or via online platforms may also be effective for many women. For women performing self-taught pelvic floor muscle training without symptom improvement, individual consultation is encouraged. A physiotherapist with a special interest in the pelvic floor can provide individualised assessment and treatment of pelvic health and work collaboratively with sports and exercise professionals to ensure multidisciplinary athlete care. Other pelvic health management strategies may include bladder retraining, fluid/dietary modifications, exercise modification, assessment of the lumbo-pelvic complex, pessary device to support the pelvic organs and pain education.
What’s next for providing better pelvic health support for female athletes?
Pelvic health is an underrecognised and under-resourced area of sports medicine. Key focus areas for the future are to:
1. Raise awareness that female athletes experience a broad range of pelvic floor symptoms that impact their participation and performance
2. Provide education on pelvic health to female athletes so they can understand their symptoms, be aware of who to go to for help and know that non-surgical treatment options are available
3. Provide training for professionals on how to screen for pelvic floor symptoms and provide education, referral and management within their scope of practice. Educate on how to conduct safe and sensitive screening integrated into existing pre-exercise and general health surveillance processes
4. Conduct research to investigate riskfactors for symptom development, causes of pelvic floor disorders in nulliparous young women and evidence-based management of pelvic floor disorders for those participating in high-impact and heavy lifting sports
For article references, please email info@sma.org.au
Author Bio

Dr Jodie Dakic is a Senior Lecturer in the Department of Physiotherapy at Monash University, with over 20 years of clinical experience as a practising physiotherapist in the fields of elite sports physiotherapy and women’s health. Jodie has a strong track record of conducting research into pelvic health in exercising women and injury epidemiology/prevention. She has been CI-A of several funded projects, resulting in numerous peer-reviewed articles and presentation at national and international conferences. Dr Dakic was the winner of the Wendy Ey Women in Sport Award at the 2023 Sports Medicine Australia Conference. She is an invited member of the global Hologic Women’s Tennis Association Women’s Health Task Force and the Australian Institute of Sports Female Performance Health Initiative Research Reference Group. Jodie is passionate about raising awareness of pelvic health in female athletes and has developed and delivered pelvic health educational workshops, online modules and infographics with key stakeholders such as the Australian Institute of Sport, AFLW and Play Like a Girl.
VOLUME 42 • ISSUE 1 2024 2 1 FEATURE
Journal of Science and Medicine in Sport and sister journal JSAMS Plus
Official journals of Sports Medicine Australia
New Topic
Cornerstone reviews now highlighted on jsams.org, scan QR code to access. Note that there are more papers in the pipeline www.jsams.org/content/cornerstone-reviews
Did you know…
“Pensar en Movimiento” (Thinking in Movement), a scientific online journal (edited by Luis Fernando Aragon-Vargas from the University of Costa Rica) is now publishing selected JSAMS papers. For more information see editorial from Vol 27, issue 1 https://doi.org/10.1016/j.jsams.2024.01.001
JSAMS Plus
Has now simplified the submission process ensuring that uploading a paper to the system is easier and faster than before. Please check the Guide for Authors
Special issues
Published: 24th International Congress on Snowsports Trauma and Safety –The biennial meeting of the International Society for Snowsports Safety (ISSS)
Guest editors: Irving S. Scher, Jeremy Witchalls, Tracey Dickson Call
Lead
for papers: Exercise Oncology
Editor: Dr David Mizrahi
Papers will be published open access without APCs. Deadline
Guest Editors: Prof Rob Newton, ECU, WA, Australia; Dr Carolina Sandler, Western Sydney University, Sydney, Australia and Dr Erika Rees-Punia, American Cancer Society, GA, USA
date 30TH April 2024

Do the feet of male and female netball players differ?
Implications for shoe fit
MADDISON KIRK 2023 ASICS SMA Conference
John Sutton Award for Best Paper – Sports and Exercise Science
In netball, foot-related issues are a common problem, affecting a staggering 85% of netball players during a season - with blisters, ankle sprains, calluses and bruised toenails being the most common issues. Netball-specific shoes have the potential to play a vital role in protecting and supporting players’ feet during the sport’s high-impact and multi-directional movements and, in turn, decrease these common foot-related issues. Our recent survey of 2,925 netball players, however, has revealed that both male and female netball players are dissatisfied with the fit and functionality of current netball-specific shoes, with a notable proportion of men expressing concerns about how their shoes fit, particularly regarding width and length.
To achieve their desired function, netball-specific shoes must fit players’ feet correctly. To fit well, the interior space within a shoe must match the size and shape of the foot it encases. Manufacturers build shoes around a three-dimensional structure known as a ‘last’ to achieve this match between the shoe and foot. Traditionally, manufacturers have made women’s athletic shoes using a smaller version of a men’s last, with all dimensions proportionally scaled down according to foot length. However, if women’s

feet differ in shape relative to men’s, this would be inappropriate and could lead to poorly fitted shoes for women. It would be equally unacceptable for a man’s shoe to be designed as a scaled-up version of a woman’s last. As netball has traditionally been a femalecentric sport, many footwear options are available to women, allowing female netball players to select a shoe model that best suits their foot shape and playing circumstances. However, despite the recent 88.4% increase in men playing netball in Australia, only one netball-specific shoe model is currently marketed explicitly for men.
FEATURE
Photo: s-c-s/ gettyImages
VOLUME 42 • ISSUE 1 2024 23
Photo: RobertoDavid/ gettyImages
Do the feet of male and female netball players differ?
Implications for shoe fit
Researchers have consistently reported that male and female feet differ in size relative to stature and shape. Therefore, men’s feet are unlikely to be scaled-up versions of female feet but instead differ in several shape characteristics. The path to reducing foot-related problems and pain and improving the satisfaction of netball players regarding their shoes lies in understanding the dimensions and morphology of the feet of both male and female netball players.
To better understand the size and shape of netball players’ feet, our research team from the University of Wollongong, led by Maddison Kirk, travelled across Australia to threedimensionally scan the feet of 251 male and 251 female sub-elite and
Researchers have consistently reported that male and female feet differ in size relative to stature and shape.
elite netball players. After analysing each scan, the unique results revealed that the size and shape of netball players’ feet differed significantly between sexes. Male netball players had significantly larger absolute and normalised foot measurements compared to their female counterparts, notably at the ball of the foot, heel and instep. Even when we normalised the measurements to height, men had
longer feet by approximately 0.24% of height and wider feet by 0.22% of height than women. These results mean that for a male and female netball player, both 170 cm tall, the male netball player would have a foot approximately 4.1 mm longer and 3.7 mm wider than the female netball player. The feet of netball players were also shown to be classified into one of five foot types, which we called (i) Extra long-and-wide, (ii) Long-andwide, (iii) Flat, (iv) Tapered, and (v) Short-and-narrow. Females were more likely to have Tapered and Short-andnarrow foot types, and males were more likely to have Extra long-andwide and Long-and-wide foot types.
Given the significant sex differences in foot shape revealed in our study
 Photo: m-gucci/ gettyImages
Photo: m-gucci/ gettyImages
24 VOLUME 42 • ISSUE 1 2024 FEATURE
and previous research, netball-specific shoes designed for females are unlikely to fit the feet of male netball players. Therefore, manufacturers should build netball-specific shoes around lasts that reflect the differences between men and women in foot size and shape highlighted in this study. The results from this research have practical implications for clinicians, researchers, and footwear manufacturers, as summarised below.
Implications for netball shoe design
ٚ Female netball players’ shoe sizes ranged from EU 34 to EU 45, and male netball players’ shoe sizes ranged from EU 37 to EU 53. However, the largest netball-specific shoe size currently available to males is an EU 50.5 (US 15), suggesting that the available sizes do not cater for all male’s feet. Netballspecific shoes, particularly those manufactured for males, should be available in larger sizes to reflect the foot length of this cohort.
ٚ Male netball players have significantly broader foot and heel widths than

female netball players. The average foot width varied up to 5.9 mm for a given foot length between males and females. Netball-specific shoes available on the market today are only manufactured in two width sizes – “B – standard” or “D – wide”, with the one netballspecific shoe designed explicitly for males available only in standard width. A range of shoe models with varying widths, including narrow and extra wide options, should be available to all netball players.
ٚ A female netball-specific shoe is likely too narrow and not high enough for most males at the instep and toe
box. We suggest that multiple sex and size-related foot dimensions, such as foot height and width measures, be considered during the grading process of netball-specific footwear to accommodate the range of foot types of netball players.
Ensuring netball-specific shoes match the shape of both male and female netball players’ feet will help optimise shoe fit and comfort and likely reduce foot-related problems and pain associated with ill-fitting footwear.
For article references, please email info@sma.org.au
Author Bio
Male netball players had significantly larger absolute and normalised foot measurements compared to their female counterparts, notably at the ball of the foot, heel and instep.

Maddison Kirk is a PhD candidate in the Biomechanics Research laboratory at the University of Wollongong. Recently, Maddison submitted her PhD thesis entitled “Improving footwear for male netball players”. Her primary research interests are footwear, lower limb injury prevention, structure and function of the foot and improving performance, specifically within netball. She received the John Sutton Award for Best Paper in Sports and Exercise Science and presented in the Best of the Best session at the 2023 ASICS SMA Conference.
VOLUME 42 • ISSUE 1 2024 25 FEATURE
Photo: luckyraccoon/ gettyImages
Tendons into the 21st
The Sixth International Scientific Tendinopathy Symposium
Between the 9th and the 11th of November 2023, hundreds of healthcare professionals flew from around the globe to gather in the picturesque city of Valencia, Spain to attend the International Scientific Tendinopathy Symposium. The Symposium is a multidisciplinary forum where professionals discuss…you guessed it, everything related to tendon injuries. This primarily includes basic science, diagnostics and clinical management. The first edition of the symposium was held in Umeå, Sweden in 2010, with other venues including Oxford and Vancouver. The sixth edition of the conference was held in the iconic technology hub, the Ciudad de las Artes y las Ciencias (City of Arts and Sciences). The modern architecture of the hub juxtaposed against the charming streets of the old town, just a short walk away, provided an idyllic setting. In typical fashion, the symposium drew celebrities of the tendinopathy research world to share their latest insights on tendon pain. The theme of the symposium was Tendons into the 21st century.
Day one commenced with preconference workshops led by two internationally renowned Australian researchers, Professor Jill Cook and Associate Professor Tania Pizzari. Professor Cook conducted a clinically focused workshop on the differential diagnosis of Achilles tendinopathy, while Associate Professor Pizzari addressed considerations for managing upper limb tendinopathy.
Following the pre-conference workshops, the early afternoon began with a welcome address from the organizing committee, which included Australian researcher Dr Ebonie Rio. This was succeeded by the first keynote
session, delivered by distinguished academic rheumatologist, Professor Dennis McGonagle. His session provided valuable insights from decades of research concerning the basic anatomy and changes that occur at the enthesis (bone tendon junction) in different pathologies. This included a discussion about the similarities and differences between tendinopathy and enthesitis, a feature of spondyloarthritis.
The day concluded with another noteworthy keynote session presented by Associate Professor Karin Silbernagel from Delaware University. She advocated for healthcare practitioners to consider tendinopathy as a disease rather than a single, isolated injury. This session prompted attendees to consider broader approaches to managing tendinopathy. The day concluded with welcome drinks and a tasting of local cuisine.
Day two began with keynote sessions by Dr Chavaunne Thorpe, discussing the role of the interfascicular matrix in tendon health, and Associate Professor Tania Pizzari, focusing on rotator cuff tendinopathy. Dr Pizzari emphasized crucial differences for clinicians in rehabilitating rotator cuff tendinopathy compared to lower limb tendons like the Achilles and Patellar tendons, one such being the degree of pain tolerated during rehabilitation.
A highlight of the afternoon was a comprehensive overview of the management of Achilles tendinopathy presented by Sports Physician and Associate Professor Robert-Jan de Vos from Erasmus University in the Netherlands. This presentation challenged the audience by posing provocative questions related to the evidence supporting different interventions, including exercise as
an isolated treatment and injection therapies, and provided the audience with key gaps in the evidence that must be addressed. The afternoon concluded with a comprehensive session on tendon rehabilitation led by Dr Igor Sancho. Delegates then hungrily proceeded to the conference dinner, commencing at the local dinner time of 9 pm!
The final day started with an update from representatives of the gluteal tendinopathy research group, headed by Dr Alison Grimaldi and Associate Professor Angie Fearon. This update shared the methodical process taken to understand just how robust current measurement tools are, that are used to evaluate this condition. Other notable sessions included Dr Myles Murphy’s introduction to a new outcome measure that can
Besides the obvious highlight of visiting the picturesque city of Valencia, I liked the intimate nature of the conference and that the sessions were delivered from a broad international audience – this made you feel like you were hearing the very latest research from a range of perspectives.
-Symposium attendee
26 V OLUME 42 • ISSUE 1 2024 SPECIAL FEATURE
Century
be used to capture the severity of Achilles tendinopathy and Dr Alison Grimaldi’s presentation on factors that mediate treatment effects of gluteal tendinopathy. The latter was voted the best paper by a senior researcher.
The sixth edition of the International Scientific Tendinopathy Symposium was a resounding success, bringing together experts and clinicians from around the world to share the latest research. Over the course of three days, attendees enjoyed an array of workshops, keynote sessions, and presentations covering various aspects of tendinopathy, from basic science to diagnostics and rehabilitation strategies. The relaxed nature of the conference fostered the exchange of ideas, with the idyllic setting of Valencia adding to the overall experience.
Author Bio

Dr Anthony Nasser is an APA Titled Sports and Exercise Physiotherapist with a special interest in hip pain. Anthony completed his PhD through La Trobe University which focused on the assessment and treatment of hip-related tendinopathy. Since completing his PhD, Anthony has continued to conduct research in this area. He has been involved in teaching musculoskeletal physiotherapy at several leading universities and is currently employed as a Senior Lecturer at the University of Technology, Sydney in the Graduate School of Health. Anthony is a member of SMA’s NSW State Council and Sport Health Working Group.

VOLUME 42 • ISSUE 1 2024 2 7 SPECIAL FEATURE
Photo: SeanPavonePhoto/ gettyImages

CONCUSSION MANAGEMENT
An introductory overview of concussion recognition and management to help you better understand this sporting injury.
Learn about the signs and symptoms, identifying a potentially concussed athlete, managing a suspected concussion and the latest return to play guidelines.

Scan tocheckoutthe fullcourseprogram
CONSIDERATIONS FOR ATHLETES WITH A DISABILITY
Looks at a range of considerations to be made when working with athletes with a disability, both universal and specific for those with a physical, intellectual or sensory disability.
Learn about communication and rapport building, athlete pre-screening, environmental considerations, and much more.

Scan
fullcourseprogram
Both online courses have been developed to support medical practitioners, first responders, coaches, sports trainers, athletes, parents, officials and clubs.
tocheckoutthe
Group-based physiotherapy programs
are effective in treating prevalent musculoskeletal conditions.
FRÉDÉRIQUE DUPUIS (2023 ASICS SMA Conference Best Poster Winner – Clinical Sports Medicine) AND JEAN-SÉBASTIEN ROY
Musculoskeletal disorders are a prevalent cause of pain and impose a significant economic burden worldwide. Conservative management, such as physiotherapy, has gained recognition as the primary therapeutic approach. However, the widespread occurrence of musculoskeletal disorders has raised substantial concerns regarding the accessibility of physiotherapy services in healthcare systems. Access is currently limited by long waiting times, which have been shown to worsen disability for individuals dealing with musculoskeletal disorders. For organisations with limited resources, there is a need for innovative and effective interventions to optimize the use of resources and increase access to physiotherapy services.
A systematic review was conducted to identify effective strategies to improve access to outpatient rehabilitation services, and several options were outlined. These strategies included the modification of referral management (for example, implementing selfreferral), extending and modifying the roles of service providers (for example, physiotherapists conducting orthopaedic triage), and changing the model of care delivery. The latter is the focus of this article.
Traditionally, physiotherapy interventions are delivered on a one-on-one basis. This model is predominantly used in both public and
private services. However, changing the one-on-one usual physiotherapy care to a group-based intervention has been shown to reduce waiting time in the context of cardiac rehabilitation without affecting treatment outcomes. Groupintervention can alleviate waiting times by allowing the treatment of multiples individuals at the same time. For organization with limited resources and treating populations with a high prevalence of musculoskeletal injuries, the implementation of groupbased physiotherapy programs might be particularly relevant.
Group-intervention can alleviate waiting times by allowing the treatment of multiples individuals at the same time.

VOLUME 42 • ISSUE 1 2024 2 9 FEATURE
Photo: Sunlight19/ gettyImages
Group-based physiotherapy programs are effective in treating prevalent musculoskeletal conditions.
The effectiveness of group-based physiotherapy programs has previously been evaluated, primarily in public outpatient physiotherapy services, among patients with chronic back, neck, and shoulder pain. Results from several RCTs suggest that they are as effective as usual one-onone physiotherapy care in reducing pain and disability. Additional benefits such as cost-effectiveness and enhanced motivation with peer support were also outlined.
However, there are still gaps in the literature regarding the effectiveness of group-based physiotherapy interventions. Most previous studies were conducted in outpatient public physiotherapy facilities, focusing on the treatment of the general population with chronic musculoskeletal pain. The existing literature provides limited insights into the effectiveness of group-based programs for individuals exposed to high levels of training and physical work. Occupations characterized by high demands, such as athletes or military members, pose unique challenge for recovery and rehabilitation. It is conceivable that the effectiveness of group-based physiotherapy programs may be different within such populations.
Group-based physiotherapy programs have been criticized for their nonpersonalized aspect, potentially limiting their effectiveness in population with specialized and extensive engagement in physical training. Some evidence suggests that personalized intervention, such as one-on-one physiotherapy care tailored to the specific needs, requirements, and goals of each patient, leads to better outcomes than standardized

group-based interventions. Indeed, most of the group interventions described in the literature are currently implemented with a standardized approach, where all participants in the group complete the same pre-defined exercise program. This highlights a limitation of group-based interventions, potentially overlooking the complexities of real-world clinical practice and characteristics of specialized populations.
To fill the gaps in the literature, our recent pragmatic randomized trial compared personalized group-based physiotherapy interventions to the usual one-on-one physiotherapy care in military members of the Canadian Armed Forces. The significant amount of physical training and demanding nature of military occupations make
musculoskeletal disorders the main cause of medical leaves and restricted duties. The high prevalence of musculoskeletal disorders and limited resources led to an insufficient number of physiotherapists to care for patients within an appropriate timeframe in one of the largest garrisons. Three groupbased physiotherapy programs were developed to address this issue. These programs include several exercise stations, where all exercises have multiples degrees of difficulty. The Lumbar Program specifically focuses on the management of nonspecific low back pain, the Upper Extremity Program targets rotator cuff-related shoulder pain injuries, and the Lower Extremity Program has been designed to manage patellofemoral pain syndrome and ankle sprains.
The existing literature provides limited insights into the effectiveness of group-based programs for individuals exposed to high levels of training and physical work.
Although conducted in a group setting, these programs were designed with a personalized approach, where exercises to be performed are carefully chosen based on the clinical evaluation of each patient. An initial evaluation determines the treatment plan, taking into consideration the patient’s clinical needs and capacities, and the severity of the condition. During a typical group session, each participant brings its treatment plan and performs his own prescription of exercises, supervised, and guided by the therapist. Multiple time slots are offered to the patients each week, and the group size can vary between three and twenty participants.
30 VOLUME 42 • ISSUE 1 2024 FEATURE
Photo: PeopleImages/ gettyImages
Our results (n=120) suggest that there is no difference between the effectiveness of the group-based physiotherapy programs (n=61) and the usual one-on-one physiotherapy care (n=59) in the treatment of low back pain, rotator cuff-related shoulder pain, patellofemoral pain syndrome, and ankle sprains. All participants showed statistically and clinically significant improvement in disability and pain intensity at 6, 12 and 26-weeks after the beginning of the interventions.
Another gap in the literature concerns the evaluation of patient satisfaction with participation in group-based physiotherapy interventions. Delivering a new mode of physiotherapy intervention could impact patients’ satisfaction, firstly because it may not align the patient’s initial expectations. Also, offering a group intervention is likely to have distinct characteristics from the usual interventions, such as less one-onone time with the professional, as well as fewer time slots. Satisfaction was assessed in this pragmatic trial, evaluating both satisfaction with the treatment received and satisfaction with outcomes (current symptoms state after discharge).
There was no difference between the groups regarding patients’ satisfaction. At the end of the intervention, fortysix percent (46%) of the participants in the one-on-one physiotherapy group and fifty-six percent (56%) of the participants in the group intervention answered they were satisfied with their current symptoms state after discharge. Regarding satisfaction with the intervention received, eighty percent (80%) of participants in both groups answered they were satisfied or very satisfied.
These results are in line with previous literature evaluating group-based physiotherapy interventions. They provide compelling evidence that group-based physiotherapy programs present a valuable and well-received alternative to conventional care for various musculoskeletal conditions, particularly among individuals who engage in high levels of training and
Our results suggest that there is no difference between the effectiveness of the group-based physiotherapy programs and the usual one-on-one physiotherapy care.
physical work. In addition, our study showed the possibility of personalizing group-based interventions. This model of care holds significant relevance for organizations with limited human and financial resources, such as sports organizations and outpatient rehabilitation services. While simultaneously catering to multiple patients, it offers greater accessibility compared to oneon-one physiotherapy care.
For article references, please email info@sma.org.au

Author Bio

Frédérique Dupuis is a physiotherapist working at the sports medicine clinic
Le PEPS de l’Université Laval, in Canada. She is a PhD candidate at the Centre for Interdisciplinary Research in Rehabilitation and Social Integration (CIRRIS), a research center affiliated to Laval University in Quebec, Canada. Her thesis focusses on the rehabilitation of musculoskeletal disorders, improving access to care and cost-utility analysis of rehabilitation interventions. She also has an interest in understanding the underlying mechanisms of musculoskeletal pain, with a specific focus on the impact of physiotherapy interventions on musculoskeletal structures. She has been awarded the Clinical Sports Medicine Poster Award at the 2023 ASICS SMA Conference.
VOLUME 42 • ISSUE 1 2024 31 FEATURE
Photo: PeopleImages/ gettyImages
People Who Shaped SMA
Professor
Garry Allison
What motivated you to pursue a career in sports medicine?
I won a scholarship to Sydney University for physical education and became passionate about water polo, representing NSW at various levels. Moving to Western Australia to pursue the national team, I transitioned to coaching and later became the WAIS coach for the U20 team and the men’s and women’s teams. When with WAIS I completed a master’s research degree at UWA in biomechanics and isokinetic resistance training for water polo and specifically aspects of throwing. I realized I could be a qualified sports coach, trainer, or pursue physiotherapy, leading me to choose the latter.
As a sports physiotherapist, what led you to become involved in the neuroscience space?
During the last 2 years of my physiotherapy studies, I accepted a position in the Honours research program. Everyone thought I’d go down the Sports pathway, but I already had a Master’s degree in this area so I chose to diversified my research to focus on a more disabled population, particularly spinal cord injury patients. This occurred because the Physio School was on the same campus as the Rehabilitation hospital and across the oval was the SCI rehabilitation unit. The choice was opportunistic yet changed my life. Applying my expertise in biomechanics and motor control from elite athlete research, I delved into neurological rehabilitation programs, providing insights into motor control aspects of the diaphragm in
spinal stiffness and stability, which ultimately influenced my core stability research. Understanding the motor control factors that differentiated between a Push and a Throw of a water polo ball opened up a whole level of motor control understanding that translated to other exercise rehabilitation programs.
How did you first become involved with organisations such as Autism CRC, Children’s Research Strategic Council, and the National Drug Research Institute?
After teaching at Curtin and a stint at UWA’s Department of Surgery, I returned to Curtin in a Neuroscience and Trauma Physiotherapy role. Seeking more leadership opportunities, I accepted the Dean of Research for Health Sciences, expanding my involvement in internal centres, institutes, and national and international partnerships. I learnt a lot in these committee roles and undertook additional training in company risk and governance. These roles were part of the promotion, but I was enthusiastic and was an active participant in these leadership and committee roles. These experiences influenced my research by developing implementation plans for rehabilitation programs in primary healthcare and hospital outpatients. Cost utility and work force management became my interest in health systems and services. In reflection, it was not much different from coaching or managing a large list in a WAFL club by a person who never played AFL, in a club that had won the

32 VOLUME 42 • ISSUE 1 2024 PEOPLE WHO SHAPED SMA

SMA’s multidisciplinary focus on Sports Medicine, incorporating high-level knowledge and international conferences, has profoundly impacted my career.
wooden spoon in all grades three years running. I served for 12 years, 6 grand finals and we broke a 25-year drought. The diversity of these experiences has been the foundation of me fulfilling my current role as Associate Deputy Vice Chancellor of Research Excellence.
How and when did you first join SMA?
I joined the Physiotherapy Association in the late 80s, eventually transitioning to the sports physiotherapy interest group. Having completed my biomechanics at the University of Western Australia, my involvement with key figures in Sports Medicine Australia began through collaborative research programs. I can’t pinpoint the exact date, likely the late 80s or early 90s. I joined the SMA conference committee around the same time that I was the inaugural Australian Research Fellow at the Australian Institute of Sport. Following that, I managed the judging at the conference for multiple years before moving on to the board to contribute my leadership and governance skills.
How has being involved with SMA helped you in your career?
Simply put, SMA’s multidisciplinary focus on Sports Medicine, incorporating high-level knowledge and international speakers at conferences, has profoundly impacted my career. The exposure allows professionals to discuss topics at a higher level and step outside professional silos. SMA’s diverse membership with a common interest
VOLUME 42 • ISSUE 1 2024 33 PEOPLE WHO SHAPED SMA
Garry Allison Professor
in Sports Medicine and physical activity and exercise, rather than a subgroup within a single profession, has broadened my interests, experiences, and network. While I remain a member of my specific profession, SMA has diversified my professional outlook, connecting me with individuals from various backgrounds, enriching my research endeavours. SMA has opened the doors for better collaborations outside my original professional boundaries.
What is your advice for those starting their career in sports medicine?
My advice is to have a specific focus on a profession, cultivating general and soft skills along with strong values and commitment. Never compromise on values, as they constitute your core

brand. Once established, particularly in academia, research, or consultation services, build your brand as the “go-to person” for a particular skill set—be it a methodology, cohort, population, or pathology. Listen to understand the language of other professionals and translate this knowledge across domains. Many seeds of innovations are
planted at the intersection of different knowledge domains. Long-term career progression involves scaling your activities initially but ultimately being trusted, collaborating, and possessing specialist skills that add value, make you a prime candidate for promotion or partnership and also increases the possibility of job satisfaction.

 People Who Shaped SMA
People Who Shaped SMA
PEOPLE WHO SHAPED SMA






S OLDINOVER30COUN T SEIR
Sports Medicine In Qatar

IN QATAR, THE SMALL PENINSULA IN THE LARGER ARABIAN PENINSULA, THERE ARE AROUND 10 THOUSAND PHYSICIANS FROM ALL MEDICAL BRANCHES WORKING IN THE COUNTRY. ONLY FIVE HUNDRED OF THEM ARE QATARI DOCTORS, WHICH MAKES AROUND 5% OF THEIR TOTAL NUMBER. THIS IS NOT ENTIRELY SURPRISING WHEN WE LOOK AT THE DEMOGRAPHY OF QATAR, WHERE LOCAL CITIZENS MAKE NO MORE THAN 30% OF THE GENERAL POPULATION.
From the information above, it might be predicted what does Sports Medicine, the relatively new specialization worldwide, look like in Qatar in terms of its volume. In fact, it’s not as small as one might imagine. It is difficult to discuss Sports Medicine in Qatar without using the word “Aspetar” and without mentioning it all the time. Aspetar is a specialized orthopaedic and sports medicine hospital, opened in 2007 to be the first of its kind in the Middle East. It is safe to say that sports medicine in Qatar was born at Aspetar, and that Aspetar represents sports medicine in the country to a great extent that it is hard to mention one without pointing to another. Sports medicine before Aspetar was practiced in small, limited
36 VOLUME 42 • ISSUE 1 2024 SPORTS MEDICINE AROUND THE WORLD

centres and individually, mostly by orthopaedic surgeons, team doctors and some other specialties. Shortly after it started operations, Aspetar became one of the remarkable sports medicine centres not only in the region but also in the world.
This is partly due to the high-end sports medicine facilities that meet any athlete’s expectations, but also thanks to the high-quality international sports medicine practitioners from all over the world who have contributed to the hospital since its beginning and through to the current time.
What makes it even more difficult to look for sports medicine services in Qatar outside of Aspetar is that Aspetar has established a national sports
medicine program. The role of this program is to link team doctors and sports medicine services in all sport clubs and federations in the country centrally to Aspetar. This creates a great and unique advantage as team doctors and physiotherapists are employed and supervised by a sports medicine hospital, and not by the club or the federation. In other words, they report directly to sports medicine specialists and not to the team manager or the coach, which altogether highly supports medical decisions to be on the athlete well-being side. Although Aspetar is the main hub for sports medicine in Qatar today, sports physicians can still be found in other places such as army medical services and private medical centres.
In the last decade, Aspetar’s name has been frequently observed at almost all sports medicine events in the world thanks to the research and publications done by Aspetar experts, the Aspetar sports medicine journal, and the clinical and rehabilitation services
It is difficult to discuss sports medicine in Qatar without mentioning Aspetar.
provided to elite international athletes. This is supported by remarkable accreditations the hospital gained shortly after opening its doors such as FIFA Medical Centre of Excellence, International Olympic Committee Research Centre, AFC Medical Centre of Excellence, amongst others.
This national and international blooming of Aspetar, followed by the increasing interest in sports by
 Photo: Leonid Andronov/ gettyImages
Photo: Leonid Andronov/ gettyImages
VOLUME 42 • ISSUE 1 2024 37 SPORTS MEDICINE AROUND THE WORLD
Photo: bennymarty/ gettyImages
Sports Medicine In Qatar

the local population, and the world championships hosted by Qatar in the last few years in different sports such as: artistic gymnastic, athletics, swimming, cycling, and most recently the FIFA Men’s World Cup, has made sports medicine more attractive to the local doctors, and the first generation of Qatari sports physicians has started to grow. However, as mentioned in the first lines of this article, Qatari doctors, of all specialties, are probably still less than the number of attendees in a room of one of the big sports medicine conferences in the world!
Hence it is not surprising to know that out of around sixty working sports medicine physicians in Qatar, less than one handful are Qataris. If we look also at the production of Qatari doctors, we can identify two resources. There are only two medical schools in Qatar of which one is private, and the other is under Qatar University, which is currently only eight years old with a six-year study program. This means that only two cohorts have graduated from this college so far. Therefore, most of the current Qatari doctors have graduated from abroad. This is the other and bigger resource so far, but the formula is expected
to change when the local medical schools become more established.
It is worth mentioning that in both medical schools in Qatar, students receive sports medicine training through some clinical rounds at Aspetar or as musculoskeletal workshops and lectures, also with the help of Aspetar doctors. Speaking about sports medicine training at Aspetar, this is also applicable to family medicine and rheumatology residents in the country. Also, Aspetar has received, and is still receiving international sports physicians in clinical fellowships.
As we can conclude from other
Author Bio

articles in this series, sports medicine specialization is still not well established worldwide, and it can be found in limited places around the world unlike other medical specializations. Qatar is not an exception to that. Although sports medicine is well represented in the country, the specialization is not yet there. However, a sports medicine fellowship program is in its final stages of preparation and will be launched soon. In addition, while writing these lines, a process of establishing a sports medicine association is in place. The biggest challenge is that there is the very limited number of local sports physicians, but they are motivated enough to create a sports medicine community in the country.
Dr Omar Al Sayrafi Sports medicine specialist, Aspetar Hospital, Qatar
IOC Sports Medicine Diploma
IOC Certificate in Drugs in Sport Chair of TUE Committee at Qatar Anti-Doping Committee
38 V OLUME 42 • ISSUE 1 2024 SPORTS MEDICINE AROUND THE WORLD
Photo: ali suliman/ gettyImages
5 minutes with
Dr Samantha McLeod
Can you tell us a bit about your background?
I had a career visitor, a psychologist, come to my school when I was in Year Nine and I thought I wanted to work with kids. I later did placements in physio, in teaching and lots of things but found that I was attracted to the atypical kids, whether they were quiet or noisy or troubled kids. I found out that’s what a psychologist does. I knew there were so many fields I wanted to work in, including the child and adolescent space, sport and health. I was an elite basketball player until I was in my 30s; so I was very familiar with the demands of high performance sport. I had played National League and represented the state and country so I always knew that sport might be involved somewhere, but I wasn’t sure that I only wanted to do sports psychology because it felt so close to home and similar to what I’d done previously in my own career. I couldn’t decide whether I wanted to do psychology or medicine. At some point, I looked at medicine. I was interested in all the biology and the physiology of medicine, but more about the psychology of the person and that kind of interaction. So that’s what led me to look at that. At the time there were no health psychology courses. My lecturer, who was a professor at LaTrobe University, designed the first health psychology course in Australia. At that time, the subjects were very medicine oriented but with understanding from a biopsychosocial perspective, so I loved that. Then the only course in Australia in Sports Psych was at Ballarat

Uni and I lived in Melbourne. I was prepared to go but when I spoke the Professor at La Trobe University, he said he was developing a sports psychology course at LaTrobe as well and I could train in both simultaneously. I was lucky because in the end, he ran all these extra classes after hours of all the sports psychology units for anyone who joined the health psychology program as a grad dip. He put us through all the interventions, and he took us
out in the field because he worked with the Australian cricketers and with Australian Judo and AFL. Later, I decided I wanted to do a PhD and that went across the two areas of sport and health psychology which married the medical aspects that I liked. Inevitably, I thought sports medicine was where my niche really was from growing up playing elite sport but also being more interested in the whole human, not just the performance psychology bit.
VOLUME 42 • ISSUE 1 2024 39 5 MINS WITH
Dr Samantha McLeod
What motivated you to pursue a dual qualification in Sport and Exercise Psychology and Clinical Health Psychology?
At first, I didn’t really even know the difference because there’s two different types of health psychology. There’s health psych where you go into promotion, people who do the quit program and the big government programs. Then there’s the branch that they say is clinical psych, which is doing interventions and working with individuals or groups. I always knew I loved the one-on-one space because you could do deeper work with a person. That’s why I tended to go down that clinical path. Even when I was playing, I was a point guard in basketball teams and I was often the captain. I was the team maker, so I could see how psychology had so much to do with how people were performing, their confidence, and how they reacted to injury and would catastrophize about everything. So, I knew that if I could work with athletes that were in high performance, but in the space of injury, illness, their whole psychology, then hopefully we’d make them well rounded humans and they

wouldn’t be so tragically devastated when they couldn’t play their sport, which is what happens. Their athletic identity is tied up so much in their sport and they don’t really have a wellrounded self-concept. My mission in life is to help people have self-belief. A lot of athletes and professional athletes I knew that were around me didn’t and I found that incredible when they had achieved so much in their lives yet they still didn’t really think they were worthwhile. That seems like a crime in a big sports system. That’s why I wanted to combine them both in that sports psych space.

You have previously worked with the Australian Institute of Sport, Richmond Football Club, and the International Basketball Federation. What led you to becoming involved in the high-performance sector?
Like anyone who was previously an elite sports person, I thought I was going to end up as a PE teacher. I think you go searching for where in sport you could function, and the way I work, I think psychology was the perfect place for me to end up. Early in my psychology career, I started off in my own sport of basketball and worked with a lot of different teams. I’ve done nearly everything in my own sport now. I’ve worked with domestic clubs and National League clubs. I’ve worked with the National Team, state teams. In disability space, I’ve worked with the Australian deaf and Victoria deaf teams and the Gliders. I did everything I could possibly do in that sport and I still didn’t feel like I was having the impact that I really wanted to, to help athletes with mental health problems or with chronic conditions to reach their full potential. For me getting these other positions, going to the AFL where I might have a greater spread across 44 athletes that could make a difference in their lives. With FIBA, I got approached by Peter Harcourt to form a mental health committee with a psychiatrist to globally help the doctors treat mental health for athletes traveling with teams. So, I started to think
5 minutes with 40 VOLUME 42 • ISSUE 1 2024 5 MINS WITH
about how I could get to the masses, how can we actually change sport and reach peak performance so that athletes weren’t limited by things that I didn’t think they should be limited by. I still do all of that. At the AIS my work is supervising the psychologists who run the national programs in the country, so there’s five of us that supervise those sport psychologists. That’s me helping them to be better practitioners and help more athletes, teams and sports organizations. That’s me getting to the masses. So, all of those positions, I’ll probably hold for quite a while because I don’t feel like I’ve got to the level of creating the kind of change I am aiming for yet.
Can you describe a career highlight that made you proud of what you do?
This was a hard one. When I first came to Richmond, they do this thing where every new person has to get up and do what they call the Triple H and they ask what your highlights, hardships and heroes are. I said to them, for me, I’ve achieved so much in my own sporting career. I don’t really look at achievements such as “I went to the Olympics, I did work with the Opals” as the best moments of my career. To me, I feel so privileged

with what people trust me with on a day-to-day basis. Every day I have people in my clinic, and it’s made a difference to their life and they’ve got a little bit happier or a little bit more focused or they’re performing better. I think that kind of work that I do is similar to how people talk about end-of-life care. It’s such a privilege. To me, there are so many highlights in the people that have transformed their lives. No personal achievement like going or being selected for something could override that.
What are your aspirations as a current Board Member of SMA?
I feel like it has been a life goal for me to get on this board because it’s always been on my mind ever since I finished my PhD. I think I was one of the first sports psychologist members of SMA and it took years to try and get any other sports psychologists to come into the Sports Medicine Australia mix. That has been my mission to try and do that. We’ve tried a couple of times. I feel like we are now in a better place to do that. I feel like sports psychology is underrepresented in that allied health and medical model on the board and even in the conferences. In everything, taking the psychology out of somebody and thinking that you’re going to get success doesn’t make any sense to me. I knew I had to wait for the right time. I strategically dropped some things in my career so that when this opportunity became available, I could put myself forward and I had the time to do it. Thankfully, Kay is here as Chair. We worked at Alphington Sports Medicine Clinic together for a short period of time where we overlapped, and I really wanted to work with her again and as well as Gregory Kolt. He was at LaTrobe doing his PhD with the same supervisor as me at the same time. I didn’t want to miss that era of people on the board. My mission really is to get sports medicine treating the athlete holistically, and to help athletes achieve their potential which means they can’t be limited by mental health or chronic illness or injury. We need to release that potential and I think

in a system of sport with all those resources, there should be no excuse. When I see suicide rates of athletes going through the roof, I think this is why I’ve asserted myself in a position like this so we can change that.
What is the best piece of advice you have received in your career? There are so many people that have been mentors to me, but I think rather than them saying something, I think what all of them did was they threw me in the deep end. If someone believed in me, they just took me and inserted me into something and said, “See what you can do with that.” Even if I was nervous, and when I didn’t know what the hell I was doing, they allowed me to discover what I actually have, and they were there to support me. I think I do that as a group practice owner. I have a lot of staff and I supervise a lot of young psychologists and I do a similar thing for them. I believe you don’t know how competent you are until you’re challenged. I think that’s part of my elite sporting career. I knew that but I needed people to believe in me in my psych career, and then I discovered it and once I discovered it, I felt like I had transferable skills. Everything I learned in sport, I put it into my career, and I try to instill that in the people that I supervise now and in my group practice.
VOLUME 42 • ISSUE 1 2024 41 5 MINS WITH

Nicola Carlish Sports Trainer Spotlight
How did you first become involved in sports training?
I started as part of some work that I did through university. I was in my third year of uni when I first started doing sports trainer work. It was the end of one of our subjects where we had the opportunity to get our level one certification whilst finishing off one of our courses. I had a chat with one of our guest lecturers at
the time, Gary Johnson, and he had a couple opportunities for people to come through and start working as sports trainers. It was something that I thought was the first step I could do to put my foot in the door and start to get a little bit of extra knowledge base, being that I work as an exercise physiologist as well now. That was an intro step to being able to have more hands-on management, to see what

it’s like within the rehab and acute injury management space, and to get a feel for what it was like working with different sporting teams. So, I was definitely thinking let’s try and get some practical experience and let’s see how we can start to get involved with different things that weren’t just doing the theoretical side of the work I was doing at the time.

VOLUME 42 • ISSUE 1 2024 4 3 SPORTS TRAINER SPOTLIGHT
Nicola Carlish
How long have you been an SMA sports trainer?
Since 2016, so I’m coming up on eight years now which seems wild to think about.
What has been a highlight of your journey as sports trainer so far?
It was really hard to narrow down what would be one highlight as I’ve come
through because it’s been a great experience to be able to meet with lots of people and be involved with different sports and be involved in a lot of different communities. It’s not just about being there on game day and doing what’s needed to be there with a lot of the teams I’ve worked with. It’s being involved in their community and being part of the day-in, day-out

and doing the things that need to be done to make sure your players are on the field. Being part of the support staff, but also the support staff being assistive with each other, I think has been a massive part of the journey, which I’ve seen roll over a number of times in different spaces, has been the opportunity to communicate with athletes at different levels within their sporting journey and being able to be that first line of contact to help them get the support they need. Whether it’s a physical issue or whether or not there’s other stuff going on, that they know that coming to their trainer they’ll have a safe space where they can talk. It doesn’t necessarily mean it fixes everything because we can’t do everything, but at least they know that they can come to this space and get the help that they need to go see someone or to get something fixed or to start talking to people about different areas. I think that experience and that continuous opportunity within the space of being a sports trainer has been a highlight for me every time.
How has being part of SMA helped your career so far?
The opportunity for both networking and for professional development has actually been a lot bigger of an impact than what I thought it was. Having SMA around has helped to be a lot more specific in terms of the knowledge and upskilling around our on-field work that we need to do and being more prepared for a lot of those situations where we don’t necessarily have the other support. I think people forget sometimes as sports trainers that we are generally there by ourselves. It’s not every club that’s going to have yourself and then a physio and then a doctor. You might have some circumstances where you have all of that support and then there’s other situations where it’s just going to be you by yourself trying to figure out what’s happening. So, I think
Sports Trainer Spotlight 44 VOLUME 42 • ISSUE 1 2024 SPORTS TRAINER SPOTLIGHT

having that continuous opportunity for upskilling through SMA has definitely helped to be able to keep an eye on things where we need to and keep us in touch with the issues that we might be exposed to so that we know what to do in those particular situations.
What is your advice to people wanting to get started as a sports trainer?
For those who are getting started, I’d say don’t be afraid to start with shadowing someone. I think it’s a very underrated approach. A lot of people believe that once you do your level one course that you should just go straight in and be able to do everything yourself and be able to do any coverage that you see where there might not be another trainer. I really would empower people to make sure that they’re seeking out someone who has a couple years of experience or go work under a couple level two trainers where they’re able to. I know it can be challenging at times but find someone to mentor you so that you’re not doing everything by yourself, because there are situations as sports trainers where you may get stuck in positions that you wouldn’t normally think to be in, or you wouldn’t
My advice to new trainers is to find someone to mentor you so that you’re not doing everything by yourself.
think you’d have to be exposed to. It’s good to have someone to fall back on in that situation, even if they’re not necessarily there next to you, that you can communicate to, to make sure that you’ve got everything covered or that you can actually make sure that you’ve readjusted and created the skill set that you need moving forward as well.

VOLUME 42 • ISSUE 1 2024 45 SPORTS TRAINER SPOTLIGHT


#SMAACSEP2024
















 Dr Kay Copeland
Dr Kay Copeland
 FROM THE CEO
FROM THE CEO
 Jamie Crain
Jamie Crain











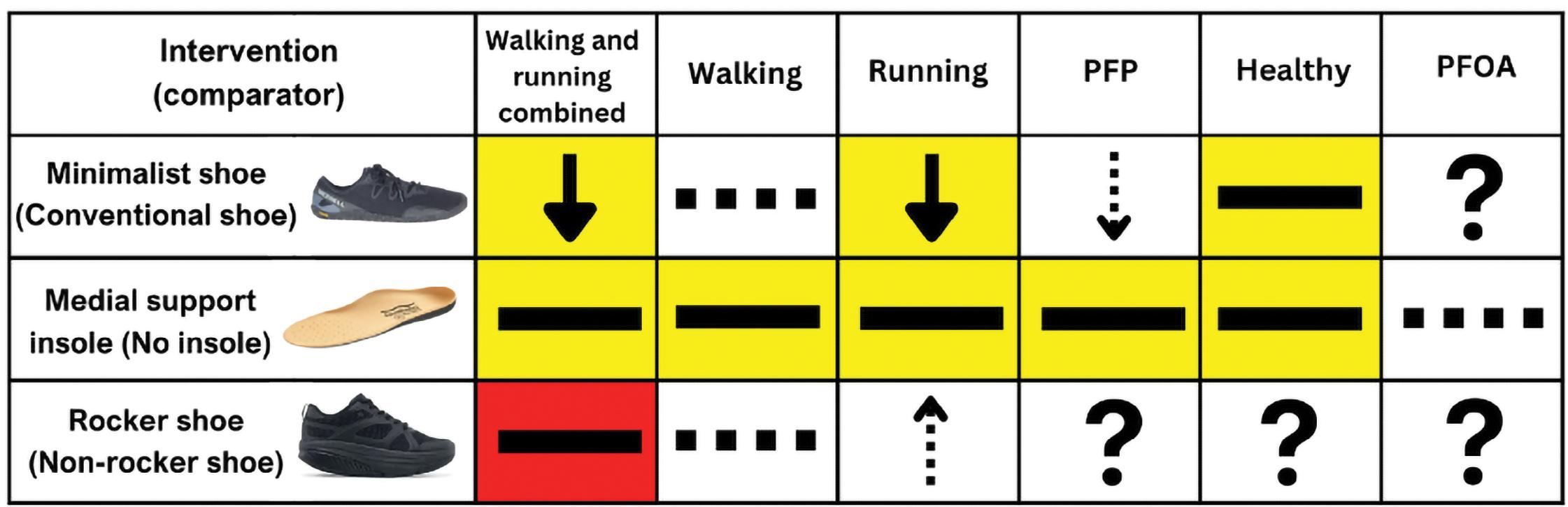


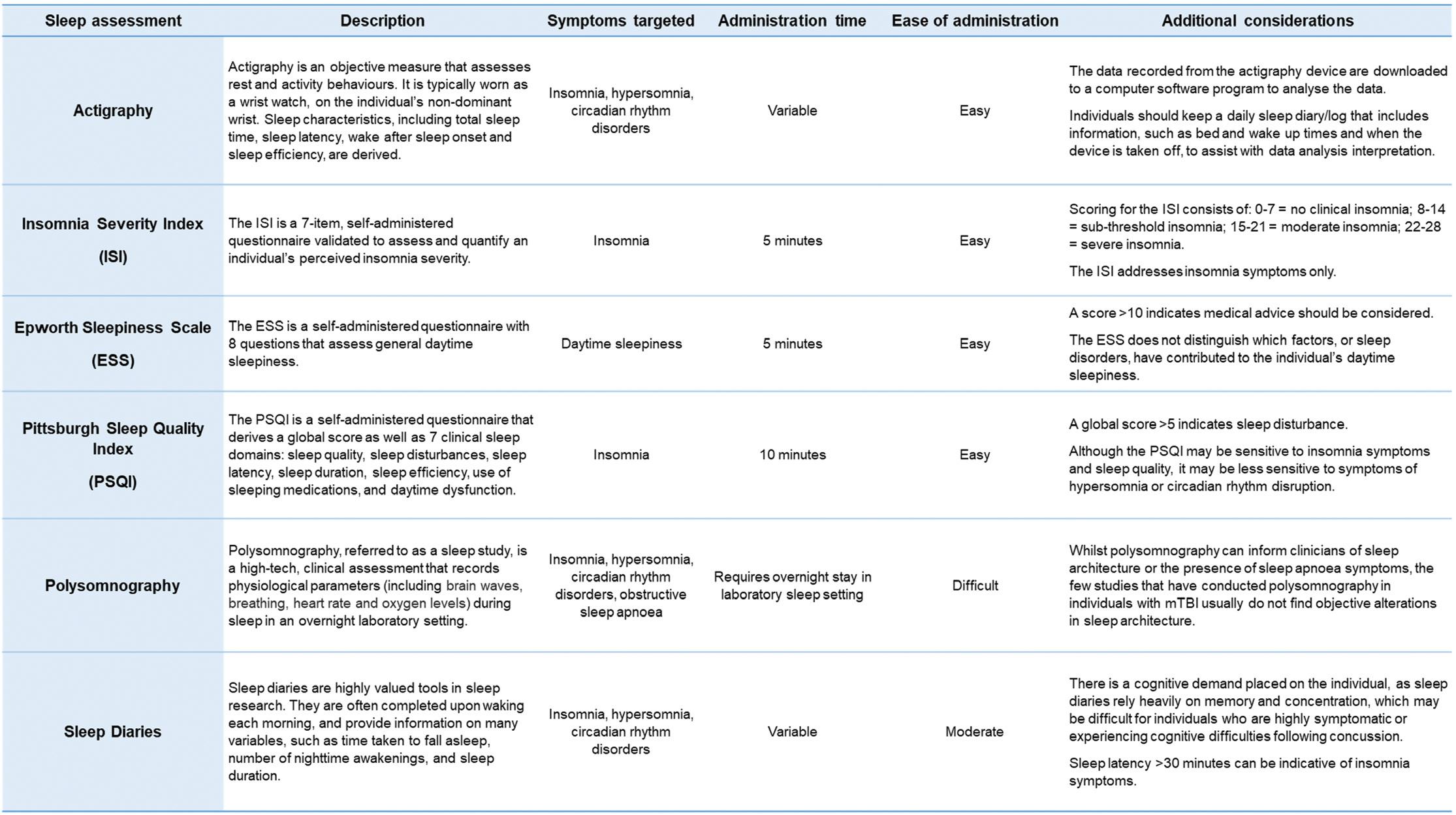
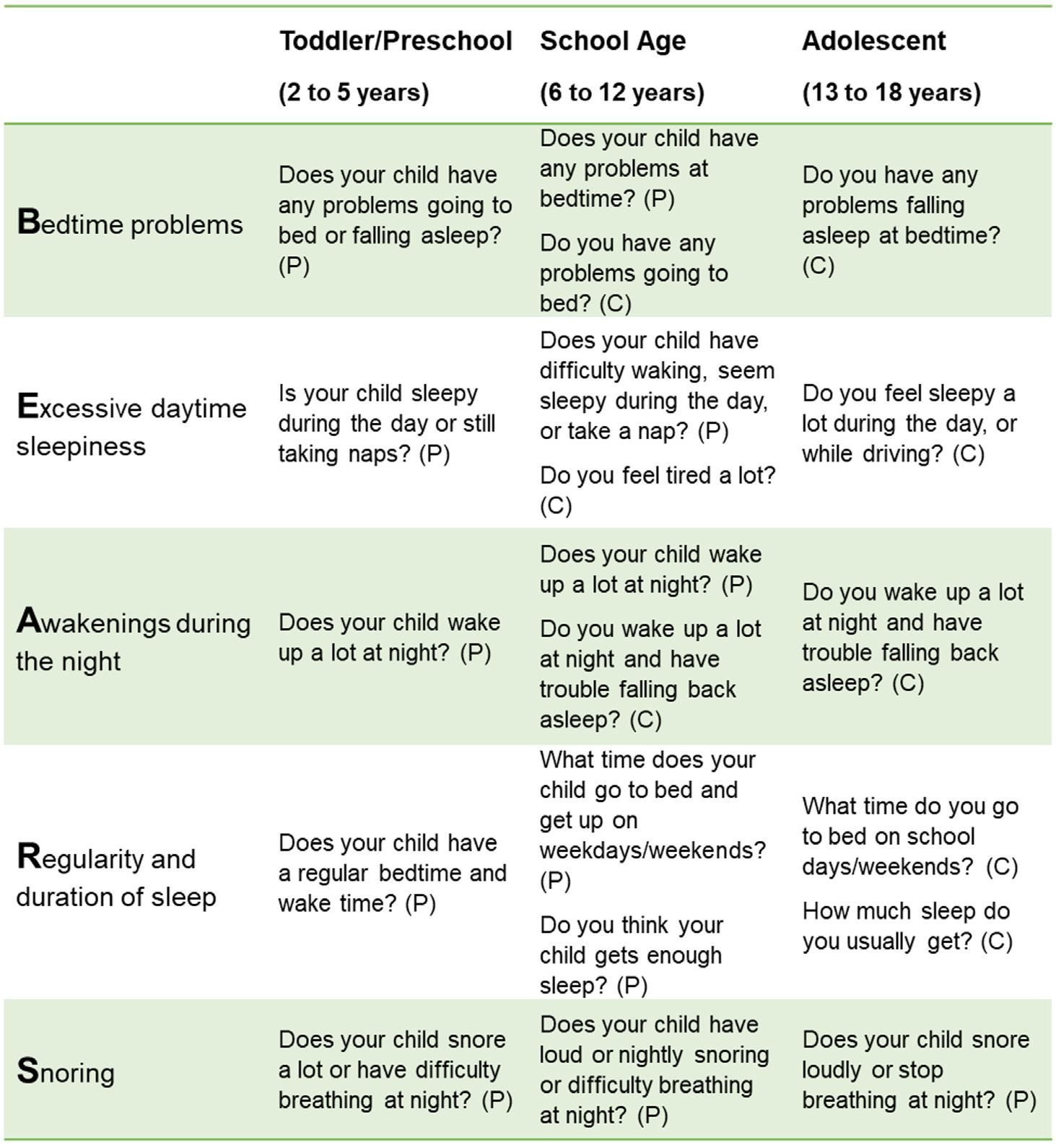








 Photo: m-gucci/ gettyImages
Photo: m-gucci/ gettyImages















 People Who Shaped SMA
People Who Shaped SMA








 Photo: Leonid Andronov/ gettyImages
Photo: Leonid Andronov/ gettyImages














