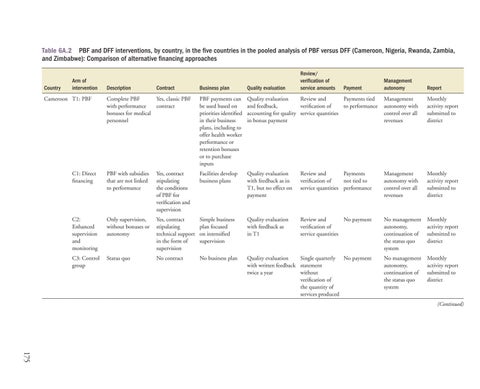
Table 6A.2 PBF and DFF interventions, by country, in the five countries in the pooled analysis of PBF versus DFF (Cameroon, Nigeria, Rwanda, Zambia, and Zimbabwe): Comparison of alternative financing approaches
Country
Arm of intervention
Management autonomy
Report
Quality evaluation Review and Payments tied and feedback, verification of to performance accounting for quality service quantities in bonus payment
Management autonomy with control over all revenues
Monthly activity report submitted to district
Facilities develop business plans
Quality evaluation with feedback as in T1, but no effect on payment
Review and Payments verification of not tied to service quantities performance
Management autonomy with control over all revenues
Monthly activity report submitted to district
Yes, contract stipulating technical support in the form of supervision
Simple business plan focused on intensified supervision
Quality evaluation with feedback as in T1
Review and No payment verification of service quantities
No management autonomy, continuation of the status quo system
Monthly activity report submitted to district
No contract
No business plan
Quality evaluation Single quarterly No payment with written feedback statement twice a year without verification of the quantity of services produced
No management autonomy, continuation of the status quo system
Monthly activity report submitted to district
Business plan
Quality evaluation
Complete PBF Yes, classic PBF with performance contract bonuses for medical personnel
PBF payments can be used based on priorities identified in their business plans, including to offer health worker performance or retention bonuses or to purchase inputs
C1: Direct financing
PBF with subsidies that are not linked to performance
Yes, contract stipulating the conditions of PBF for verification and supervision
C2: Enhanced supervision and monitoring
Only supervision, without bonuses or autonomy
C3: Control group
Status quo
Cameroon T1: PBF
Description
Review/ verification of service amounts
Contract
Payment
(Continued)
175