CHAPTER 2: CHALLENGES FOR HEALTH SYSTEMS: COVID-19 AND BEYOND
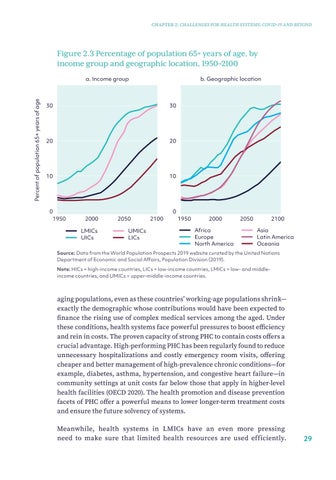
Figure 2.3 Percentage of population 65+ years of age, by income group and geographic location, 1950–2100
Percent of population 65+ years of age
a. Income group
b. Geographic location
30
30
20
20
10
10
0 1950
0 2000 LMICs UICs
2050 UMICs LICs
2100
1950
2000 Africa Europe North America
2050
2100 Asia Latin America Oceania
Source: Data from the World Population Prospects 2019 website curated by the United Nations Department of Economic and Social Affairs, Population Division (2019). Note: HICs = high-income countries, LICs = low-income countries, LMICs = low- and middleincome countries, and UMICs = upper-middle-income countries.
aging populations, even as these countries’ working-age populations shrink— exactly the demographic whose contributions would have been expected to finance the rising use of complex medical services among the aged. Under these conditions, health systems face powerful pressures to boost efficiency and rein in costs. The proven capacity of strong PHC to contain costs offers a crucial advantage. High-performing PHC has been regularly found to reduce unnecessary hospitalizations and costly emergency room visits, offering cheaper and better management of high-prevalence chronic conditions—for example, diabetes, asthma, hypertension, and congestive heart failure—in community settings at unit costs far below those that apply in higher-level health facilities (OECD 2020). The health promotion and disease prevention facets of PHC offer a powerful means to lower longer-term treatment costs and ensure the future solvency of systems. Meanwhile, health systems in LMICs have an even more pressing need to make sure that limited health resources are used efficiently.
29