CHAPTER 4: MAKING IT HAPPEN
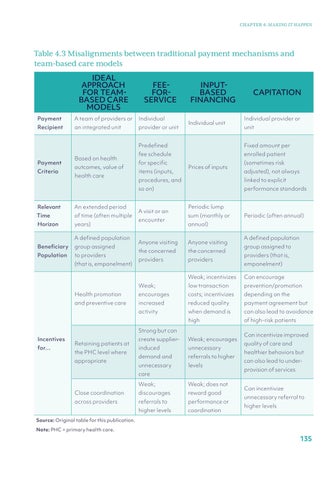
Table 4.3 Misalignments between traditional payment mechanisms and team-based care models IDEAL APPROACH FOR TEAMBASED CARE MODELS
FEE- FORSERVICE
Payment
A team of providers or
Individual
Recipient
an integrated unit
provider or unit
Payment Criteria
Based on health outcomes, value of health care
Relevant
An extended period
Time
of time (often multiple
Horizon
years) A defined population
Beneficiary
group assigned
Population
to providers (that is, empanelment)
INPUTBASED FINANCING Individual unit
for…
Individual provider or unit
Predefined
Fixed amount per
fee schedule
enrolled patient
for specific items (inputs,
Prices of inputs
(sometimes risk adjusted), not always
procedures, and
linked to explicit
so on)
performance standards
A visit or an encounter
Periodic lump sum (monthly or
Periodic (often annual)
annual)
Anyone visiting
Anyone visiting
the concerned
the concerned
providers
providers
A defined population group assigned to providers (that is, empanelment)
Weak; incentivizes
Can encourage
Weak;
low transaction
prevention/promotion
Health promotion
encourages
costs; incentivizes
depending on the
and preventive care
increased
reduced quality
payment agreement but
activity
when demand is
can also lead to avoidance
high
of high-risk patients
Strong but can Incentives
CAPITATION
Retaining patients at the PHC level where appropriate
create supplier-
Weak; encourages
induced
unnecessary
demand and
referrals to higher
unnecessary
levels
care Weak;
Weak; does not
Close coordination
discourages
reward good
across providers
referrals to
performance or
higher levels
coordination
Can incentivize improved quality of care and healthier behaviors but can also lead to underprovision of services Can incentivize unnecessary referral to higher levels
Source: Original table for this publication. Note: PHC = primary health care.
135