BRITTANY C. MONTROSS
UBMD vascular surgeon discusses what she does, how the field continues to evolve with minimally invasive approaches and why she chose this particular specialty of medicine P.4


Hormone Replacement Therapy
CAN EASE MENOPAUSE SYMPTOMS
Head of NYS Smokers Quitline in WNY helps people butt out cigarettes — “More people are quitting and current smoking rates are at record lows,” he says P. 9


ORAL CONTRACEPTIVE SOON AVAILABLE WITHOUT A PRESCRIPTION
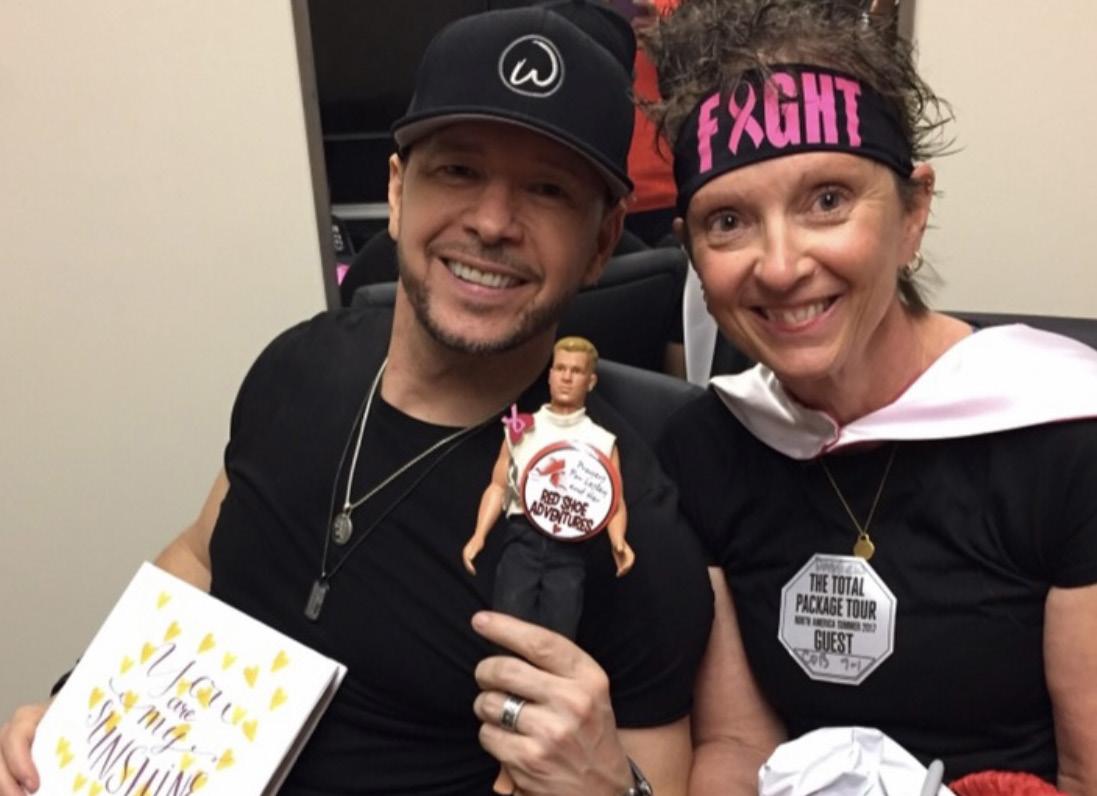
How I Beat Cancer
Cathy Nichols of Amherst has been a big advocate for women to get screened for breast cancer. Read the profile of four women who beat breast cancer.

BFOHEALTH.COM OCTOBER 2023 • ISSUE 108 FREE
P.16
Female Surgeons Bring Better Outcomes for Patients, Two Studies Show
The field of surgery has long been dominated by men, and still is today.
But two new studies show that if patients want safe, effective longterm results, picking a female surgeon might be key.
In one study involving more than 1 million Canadian surgical patients whose outcomes were followed for a year, “those treated by a female surgeon were less likely to experience death, hospital readmission or major medical complication,” wrote a team led by physician Christopher Wallis, of Mount Sinai Hospital in Toronto.
Another study — this time focused on gallstone removal, one of the most commonly performed surgeries — also found female surgeons outperforming males, on average, when it came to outcomes.
Both studies were published online Aug. 30 in JAMA Surgery.
Why the gender gap?
According to physician Martin Almquist, who wrote an accompanying editorial in the journal, it might come down to differences in attitudes toward risk-taking, the surgeon's ability to collaborate with others, and being “patient-centered” when it comes to making decisions around surgery.
In both studies, female surgeons tended to be more methodical and take longer to complete a surgery
compared to their male colleagues, the researchers noted.
“Being accurate and careful most likely beats risk-taking and speed when it comes to consistently achieving good outcomes for the patient,” concluded Almquist, a surgeon at the Skane University Hospital in Lund, Sweden.
Almquist conceded that it’s not yet proven how women outperform men in the OR.
“Perhaps personality traits more common among women contribute to better outcomes?” he said.
Regardless of the reasons, “Surely, the ideal of the surgeon as the [male] ’lonesome cowboy’ belongs to an era long gone," Almquist added.
The surgical profession remains a largely male domain, however.
For example, in the Canadian study — which looked at 25 different types of surgeries conducted between 2007 and 2019 — only about 151,000 of a total of nearly 1.2 million procedures had been conducted by women.
In the study, Wallis and his colleagues tracked 90-day and one-year outcomes for all patients.
Data was first compiled on a “composite outcome” that included deaths, hospital readmissions and/ or complications. According to the study, nearly 14% of patients treated by male surgeons experienced at
least one of these events within 90 days, compared to just 12.5% of people operated on by a woman.
At one year post-surgery, 25% of the patients of male surgeons had experienced such an event, compared to just under 21% of those treated by women. When it came to deaths, 2.4% of patients who’d been operated on by a man were deceased by one year post-surgery, compared to 1.6% of those who'd had a female surgeon.
The second study, focused on gallbladder operations, was led by physician My Blohm, a surgeon at Mora Hospital in Sweden.
It focused on more than 150,500 patients who underwent elective or emergency gallbladder surgeries between 2006 and 2019. Patient outcomes were tracked for 30 days after their procedures.
Again, the team found that female surgeons tended to spend more
time on a surgery — an average 100 minutes for an elective procedure versus an average of 89 minutes for men.
Maybe that extra time and attention paid off for patients: For elective procedures, patients operated on by male surgeons had 28% longer hospital stays and a 66% higher odds for bleeding complications, compared to patients operated on by a female surgeon, Blohm’s team reported.
So why would a surgeon’s gender matter?
“Personal characteristics and attitudes are difficult to study, but probably affect outcomes,” the Swedish group wrote.
“This study’s important finding that female surgeons may perform safer operations and operate more slowly indicates that caution might be a favorable quality," they added.

Pelvic Pain Bringing You Down?


If you are between the ages of 18-70 and have been experiencing pelvic pain for more than three months, you may be eligible to participate in an NIH-funded study to evaluate 2 evidence-based, non-drug treatments for Urologic Chronic Pelvic Pain Syndrome (UCPPS). Qualified participants, male or female, will receive a noninvasive medical examination to confirm UCPPS and 10 weeks of treatment at no cost, with few clinic visits.

Qualified participants may receive up to $225 for their time.
een the ages of 18-70 and have been experiencing more than&three months, you may be eligible to NIH funded study to evaluate 2 evidence based, nons for Urologic Chronic Pelvic Pain Syndrome (UCPPS). pants, male or female, will receive a non- invasive ation to confirm UCPPS and ten weeks of treatment at w clinic visits. Qualified participants may receive up to me
If you are between the ages of 18-70 and have been experiencin pelvic pain for more than&three months, you may be eligible to participate in an NIH funded study to evaluate 2 evidence based, drug treatments for Urologic Chronic Pelvic Pain Syndrome (UCPP Qualified participants, male or female, will receive a non- invasive medical examination to confirm UCPPS and ten weeks of treatme no cost, with few clinic visits. Qualified participants may receive $225 for their time

Health insurance is not needed to participate. Please call 716-898-6254 to learn more about this clinical study.
e is not needed to participate Please call 716-898- 6254 bout this clinical study.
Health insurance is not needed to participate Please call 716-898to learn more about this clinical study.
716-
Page 2 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • October 2023
at Buffalo - Behavioral Medicine Clinic
UB Behavioral Clinic at:
8-6254 ppic.com University at Buffalo - Behavioral Medicine C Pelvic Pain
Down?
Bringing Yo
Call the UB Behavioral Medicine Clinic at: 716898-6254 ubeppic.com

















































October 2023 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • Page 3 At ECMC, each of us—from doctors, nurses, support sta , and specialists—is focused on not just healing the community but supporting each other at every turn. Our commitment to our employees starts with a rewarding work environment and continues through to our professional development programs. Whether you’re just starting out or you’re a seasoned healthcare professional, ECMC is the perfect t to further your career. Join the ECMC family of caregivers at ECMC.EDU/CAREERS THE BEST CARE HAPPENS WHEN WE COME TOGETHER. SAVING LIVES SIDE BY SIDE EC4033 In Good Health 1/2 pg ad (Nursing) (9.5 x 6.75).indd 1 4/18/23 7:20 AM
Americans Who Are Deaf Can Now Use 988 Suicide Helpline
The U.S. government's 988 Suicide and Crisis Lifeline is expanding its reach to help more people.
The crisis line has now launched services in American Sign Language (ASL) to help callers who are deaf or hard of hearing.
The ASL services were launched in September, according to the U.S. Department of Health and Human Services.
“Individuals across America who use ASL as their primary language can now readily access the support they need during a mental health crisis,” Health and Human Services Secretary Xavier Becerra said in an agency news release. “With the introduction of 988 ASL services, we are taking a significant stride forward in providing inclusive and accessible support for the deaf and hard-of-hearing community."
The services use a videophone device that transmits video and audio. It can be reached by clicking “ASL Now” on 988lifeline.org. Callers can alternatively call 1-800273-TALK (8255) but will soon also be able to directly dial to 988 by videophone.
"After years of advocacy to ensure that 988 is available to everyone not only through voice calls, but also texting and video for sign language users, the National Association of the Deaf (NAD) is thrilled that the 988 Suicide & Crisis Lifeline is now available to use through video calls in sign language,” said NAD CEO Howard A. Rosenblum. “We encourage anyone going through a crisis or thinking about suicide to contact 988 in any way preferred -- voice, text, or sign language."
The new move is part of an ongoing effort by the HHS's Substance Abuse and Mental Health Services Administration (SAMHSA) to add accessibility to behavioral healthcare.
An earlier update added Spanish-speaking services by text and chat.
“We're talking about mental health in a way that we have not historically talked about it,” said Monica Johnson, director of the 988 & Behavioral Health Crisis Coordinating office at SAMHSA.
The 988 Suicide and Crisis Lifeline was launched last year for anyone who is experiencing a mental health crisis, emotional distress or contemplating suicide. It is an evolution from the former National Suicide Prevention Lifeline.
Making it possible to reach help by dialing only three digits was meant to make it easier to remember.
Meet Your Doctor
By Chris Motola
Q: As a vascular surgeon, what kinds of pathologies do you treat?
A: The vascular system is the arteries and veins, so we operate on arteries and veins anywhere in the body outside of the brain and outside of the heart. Things that we treat or operate on that we medically manage are peripheral arterial disease, the arteries in the legs or even in the belly. Where there are blockages people have pain when they’re walking around, wounds on their feet. So we’ll use angiogram ballooning, stenting to open up the blood vessels to give you more blood flow or to reroute blood flow around a blockage. We do abdominal aortic aneurysms, which involves the dilation and ballooning of the blood vessels, usually in the abdomen, although there can be aneurysms all over the body. If they rupture, you’re bleeding out, which is a life-threatening emergency. So we treat those, both endovascularly or open the abdomen and make repairs. We do carotid arteries in the neck, which can be a stroke risk if there are blockages there. We do a lot of work with people with kidney disease. We do venous disease, varicose veins, people with wounds on their legs as well as people who have blood clots in their legs. It can lead to leg swelling and other issues. We also treat blood vessels that lead to the gut and the kidneys.
Q: Are most of these surgeries minimally invasive?

A: A lot of these surgeries are minimally invasive. So if we use balloons and stents we’re able to do a lot of things. Over the last 20 years things have evolved from every thing being open to where we start with a minimally invasive approach for most things. We’ll try that first and then decide if an open repair would be better if we can’t do something mini mally invasively. The carotid artery we do minimally invasively with a small incision in the base of the neck, or we do it openly. It really depends on the patient’s anatomy
and features.
Q: What are the outcomes generally like for these procedures?
A: It very much depends on the patient’s condition at presentation. The outcomes with elective procedures are usually pretty good. If you have a ruptured aneurysm, it’s trickier. The generalized teaching is that if you have a ruptured aneurysm, the chance that you die before you reach the hospital is about 50%. And then it’s about 50% during the hospital stay. So we do a lot of screening and education with primaries to try to prevent them from rupturing in the first place. If we find it before it’s ruptured with imaging, the success rate is about 98%. So it’s super important to catch them. In terms of other outcomes, like treating symptoms or peripheral artery disease, and have, for example, wounds on their feet, you need an intervention to get them to heal. Other symptoms might be pain from walking around, even just around the grocery store. After our procedures they’ll be able to do those things. So outcomes there are very good in terms of both quality and quantity of life.
Q: With regard to the lower extremities, are things like wounds on the feet caused by lack of blood flow?
A: Lack of blood flow is one of the causes. If you’re diabetic, you also are at increased risk of developing wounds on your feet from both the high levels of glucose in the blood and the fact that they can’t feel their feet as well. So they might have something small that they don’t notice that develops into a wound.
But without blood flow, it’s not going to heal. So other things that put you at risk of peripheral arterial disease are things like high cholesterol, poor diet, which is huge in Buffalo. We love our chicken wings.
Q: Is Buffalo’s risk profile above the national average?
A: At the overall risk level, our rates of smoking aren’t that high compared to the South. It all kind of averages out. Smoking is another huge, very modifiable risk factor. Quitting smoking will decrease your risk of pretty much all of the diseases that
Q: What causes varicose veins?
A: Varicose veins a lot of the time are genetic. So if you have family members with varicose veins, you’re more likely to get them. Another risk factor is being on your feet a lot, so people who have a job that requires a lot of standing are at increased risk. Being overweight and not exercising can also increase venous pressure and increase your risk. It’s more common in women, but men get them too. Part of that might just be that women are more likely to present with them because they don’t like how they look. But they can be painful, they can itch. If you’re symptomatic, there are things that we can do for that too.
Q: Are they a sign of more serious pathology, or more of a nuisance?
A: They’re usually not a sign of something more serious. It’s usually a cosmetic issue, which insurance usually won’t pay for. There can be some discomfort, some itching. There is a chance that they can bleed, but that’s pretty uncommon. Even when it does, it’s not usually life-threatening, but it can be scary if it does. Along that same spectrum is chronic venous insufficiency is edema, or swelling of the legs, so having varicose veins does put you at risk for having swollen legs. From there you can have skin thickening and ulcerations. So it’s usually cosmetic, but some patients can become at risk of infection due to those wounds.
Q: What got you interested in vascular surgery?
A: I grew up in Buffalo, went to medical school here. I always thought I wanted to work with my hands, I liked anatomy, I liked fixing people and not just saying “try this medication.” I did rotations in vascular and I liked that we treat the whole patient. If they have a vascular problem they come back and see me every three, six months to a year. A lot of our patients have chronic conditions that we have to treat. I love that I get to interact with and learn about our patients. There’s a lot of interaction. And I love the surgeries that we do. There’s a lot of anatomy involved. And the minimally invasive aspect has really come around. Some of my mentors had only learned open surgery when they were in training, but they learned these new techniques well into their careers. So that was very encouraging to enter a field that’s willing to change and evolve and figure out the best way to do things for patients.
Lifelines
Name: Brittany C. Montross, M.D.

Position: Clinical assistance professor and attending vascular surgeon with the department of surgery at UBMD. Clerkship director at Jacob’s School of Medicine.
Hometown: East Aurora
Affiliations: Buffalo General Hospital, Millard Fillmore Suburban Hospital, ECMC, Niagara Falls Memorial Hospital
Organizations: American College of Surgeons; Society of Vascular Surgery; Western New York Vascular Society
Family: Husband, two children
Hobbies: Buffalo Bills fan, skiing
Page 4 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • October 2023
Brittany C. Montross, M.D.
UBMD vascular surgeon discusses what she does, how the field continues to evolve with minimally invasive approaches and why she chose this particular specialty of medicine
we treat.
Cost of a Pack of Marlboro Now Around $15
$1 cigarette tax hike projected to save 15,300 New Yorkers’ lives
Beginning Sept.1, New York state’s cigarette tax will be the highest in the nation. The $1 hike is the first cigarette tax increase since 2010 and changes the tax from $4.35 to $5.35 per pack of 20 cigarettes.
A pack of Marlboro in Upstate New York costs an average $14.50. The cost varies from region to region.
Research shows a 10% increase in tobacco prices would be expected to decrease tobacco consumption by 4% in high-income countries.
Increasing the cost of cigarettes is one of the most effective ways to pro-
mote smoking cessation and prevent youth initiation.
The American Cancer Society Cancer Action Network projects the impact of the higher tax will save 15,300 New Yorkers’ lives and prevent 14,400 youth under age 18 from becoming adults who smoke.
The latest data from the NYS Department of Health show that one in five high school-age youth uses tobacco products. New York state spends approximately $9.7 billion annually on preventable smoking-related health care costs.
Booming Sales of Legal Marijuana Linked to More Car Crashes
Emergency room visits for injuries related to driving under the influence of cannabis skyrocketed in Canada after the drug was legalized, a new study reports.
In October 2018, Canada became the second country to nationally legalize recreational or nonmedical cannabis for adult use.
While known cannabis-involved emergency department (ED) visits for traffic injuries were still rare, they grew by 475% over 13 years, with a sharper rise in accidents after legalization, the researchers found.
“Our findings highlight a concerning increase in cannabis-involvement in traffic-injury emergency visits over time, with even sharper spikes following the phases of legalization and commercialization,” said lead author Daniel Myran, a post-doctoral trainee at the Institute for Clinical Evaluative Sciences (ICES), and a family physician at the Ottawa Hospital.
“Conversely, alcohol-involvement in traffic injury ED visits did not increase over the study period, which suggests that legalization of cannabis has played an important role in rising rates," Myran said in an ICES news release.
For the study, the researchers
looked at cannabis-involved ED visits for traffic injuries between 2010 and 2021, looking for changes after the October 2018 commercialization of the legal cannabis market, which expanded products and retail stores.
The investigators reviewed data from more than 947,000 ED visits for traffic injuries in the province of Ontario. Annual rates of cannabis-involved visits surged from 0.18 visits per 1,000 total collisions in 2010 to 1.01 in 2021.
Legalizing non-medical cannabis with restrictions was associated with a 94% increase in the rate of cannabis-involved traffic injury ED visits compared to the pre-legalization period.
Later, after commercialization, which overlapped with the COVID-19 pandemic, researchers saw an even greater increase of 223% in rates compared to the pre-legalization period.
Higher rates of ED visits were seen in men, those who lived in lower-income neighborhoods and those aged 19 to 21, as well as for those who had a prior cannabis-related ED visit.
The study findings were published online Sept. 6 in JAMA Network Open.
SERVING WESTERN NEW YORK


Editor & Publisher: Wagner Dotto
Writers: Deborah J. Sergeant, Chris Motola, Jim Miller, Gwenn Voelckers, Anne Palumbo, Brenda Alesii, Ernst Lamothe Jr., Jane Schmitt, Julie Halm

Advertising: Anne Westcott, Amy Gagliano, Pam Roe

Layout & Design: Angel Campos-Toro Office Secretary: Allison Lockwood
intended
UBMD Orthopaedic & Sports Medicine is the largest orthopaedics group in Western New York, and we are still growing.



written

complement—not to take
October 2023 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • Page 5
A monthly newspaper published by Local News, Inc. Distribution: 25,500 copies throughout more than 1,500 high-traffic locations. In Good Health is published 12 times a year by Local News, Inc. © 2023 by Local News, Inc. All rights reserved. P.O. Box 550, Amherst, NY 14226 Phone: 716-332-0640 • Fax: 716-332-0779
Email: editor@bfohealth.com
•
material may be reproduced in whole or in part from
publication
lifestyle
716 Health Location Now Open 111 North Maplemere Rd., Suite 100, Williamsville, NY 14221
No
this
without the express
permission of the publisher. The information in this publication is
to
the place of—the recommendations of your health provider. Consult your physician before making major changes in your
or health care regimen.
Injuries from foot and ankle, hand and wrist to spinal conditions, joint, hip and back pain, knee, elbow, shoulder, concussion and sports medicine, our team of doctors, physical therapists, athletic trainers and other healthcare providers can help with any orthopaedic injury. We’re dedicated to being the best at making you better. Leaders in Orthopaedic Care Amherst | Buffalo | Depew | Niagara Falls | Orchard Park | Williamsville Trusted Orthopaedic Care for Bones. Joint. Muscles. Concussions. Team Doctors For: Call or visit ubortho.com 716.204.3200 Schedule an appointment today and get expert care from the largest medical group in Western New York. WESTERN NEW YORK CHAPTER We are here for you. Visit alz.org/wny or call our 24/7 Helpline at 800 272 3900
Healthcare in a Minute
By George W. Chapman
Negotiating Drug Prices
Medicare is finally flexing its purchasing power by negotiating the prices it pays for 10 drugs that treat cancer, arthritis, diabetes and heart disease. Why did it take so long?
It took the passing of the Inflation Reduction Act (I.R.A.) to authorize price negotiations of drugs with pharmaceutical companies.
So why did it take, literally, an act of Congress to negotiate drug prices, especially considering that some 80% of us are in favor of Medicare’s ability to negotiate prices?
Well, 20 years ago, then-Presi-
Big Pharma argues that negotiating prices (remember, on a whopping 10 drugs) will lower their profits and thereby negatively impact innovation.
Interestingly, drug manufacturers spend far more on stock buy backs than innovation or research and development.
Several competing drug man ufacturers sell drugs that combat diabetes, cancer, heart disease, etc. The “winner” of the price negotiation or lowest bidder could capture more if not all the market for the drug and thereby actually increase profits.
Big Pharma won’t even use the term “negotiate” as it spins this all as “big government price controls.”
If negotiating a paltry 10 drugs with Medicare will reduce profits, why then do drug manufacturers negotiate prices with just about every country (England, France, Germany, Canada, to name a few) with national or universal healthcare? It’s because those countries have not tied their hands with laws that prevent them from negotiating and employ their substantial purchasing power to keep prices down and lower costs to taxpayers to whom they have a fiduciary responsibility. It should be noted that all the countries listed have a much lower cost of care per capita than the U.S.
dent George Bush signed a law prohibiting Medicare from negotiating drug prices.
That is the penultimate (or maybe worst?) example of the absurd amount of influence Big Pharma lobbyists have on our elected officials. While negotiations are underway, Big Pharma has filed multiple lawsuits to block the government
and a lot of that can be attributed to paying far less for drugs. There is a lot of moaning from both sides of Congress about government spending. So why are we tying the government’s hands when it tries to act like a business?
from implementing this part of the I.R.A. Big Pharma should consider itself lucky to negotiate considering Medicare does NOT negotiate prices with physicians and hospitals. Medicare SETS the prices for providers of care. So much for the AMA and AHA lobbyists. There is plenty of time for the litigation to play out as the prices won’t take effect until 2026.
due to intense Big Pharma lobbying.
You would think it a slam dunk to allow Medicare to negotiate ALL drug prices. We have almost 65 million seniors on Medicare. That exceeds the total population of Canada which is about 38 million. Yet Canada, with far less purchasing power, negotiates all drug prices where it can. If we had a national health plan covering us all, Medicare would be negotiating prices on behalf of 334 million people. Medicare was about 10% ($888 billion) of the federal budget in 2021. 46% comes from general revenues, 34% from payroll taxes and 15% from beneficiary premiums. So, Medicare drug prices affect ALL of us, not just seniors.
The first 10 drugs Medicare chose to negotiate are: Eliquis blood thinner; Xarelto blood thinner, Januvia for diabetes; Jardiance for diabetes; Enbrel for rheumatoid arthritis; Imbruvica for blood cancer; Farxiga for diabetes, heart failure and kidney disease; Entresto for heart failure; Stelara for psoriasis and Crohn’s disease; and Fiasp for diabetes. These 10 drugs account for $50.5 billion or 20% of total part D costs. (Part D drugs are taken at home while Part B drugs are administered in a provider office.)

If you consider Big Pharma contributions to the campaigns of our elected officials, you’ll understand why Medicare is limited to negotiating just 10 prices and not ALL prices.
The Senate (100 members) averages about $76,000 per campaign or about $7,600,000 over the course of staggered six-year terms.
The House (435) averages about $36,000 per campaign or about $15,660,000 over the course of staggered two-year terms.
These contributions are why the Inflation Reduction Act barely passed.
Apparently, getting reelected is more important than doing the right thing.
The top 10 elected officials receiving the most money from Big Pharma are from both sides of the aisle.
Newcomer senator Raphael Warnock from Georgia leads the pack at $770,000. He has a commanding lead over the rest. In second place is Cathy Rodgers from Washington at $419,000. The next eight are: Scott Peters, California, receiving $400,000; Catherine Masto, Nevada, $382,000; Tim Scott, South Carolina, $351,000; Patty Murray, Washington, $351,000; Mark Kelly, Arizona, $350,000; our Chuck Schumer at $345,000; Brett Guthrie, Kentucky, $343,000; and Maggie Hassan, New Hampshire, $273,000.
Drug companies can easily afford to pay 1,500 lobbyists and tens of millions to campaigns to protect their profits while hospitals and nursing homes, with little to no cash to spare, struggle to stay open.
Most galling is instead of considering themselves lucky to having to negotiate only 10 drugs while Medicare sets payments to physicians and hospitals, some of the drug manufacturers have decided to sue Medicare for restraint of trade and overreach.

Business negotiations over price are commonplace. Drug companies negotiate prices with all the countries with national health insurance.
billion (with a “b”) outof-pocket last year on just the 10 drugs being negotiated.
Lower prices mean less out-ofpocket. Period.
More savings for taxpayers are on the horizon when Medicare can negotiate 15 prices in 2027-28 and then 20 after that. The severely limited number of prices that can be negotiated and the painfully slow implementation timeframe shows how difficult it was to pass the I.R.A.
No one really knows the price of a particular drug. It depends on whether you’re self-pay or covered by Medicare, Medicaid, or commercial insurance.
Commercial carriers or pharmacy benefit managers negotiate supposed discounts, but often off nebulous inflated prices quoted by the manufacturer. You never know if you’re getting a good deal. Basical ly, there just isn’t price competition among drug manufacturers as there is in most markets. Once Medicare negotiates a price, (which both par ties agree to) it should finally provide the public some price transparency.
But when Medicare flexes its muscle, they sue.
George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapmanconsulting.com.

Page 6 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • October 2023
5 Things You Need to Know About Asthma
By Ernst Lamothe Jr.
The lungs and airways are an important part of the respiratory system that effectively carries and stores oxygen.
A properly functioning respiratory system allows breaths to flow in and out of the lungs and into the airways. This is not always the case for individuals because some suffer from a well-known medical condition called asthma.
One in 13 people in the United States have asthma, according to the Centers for Disease Control and Prevention.
“There is a perception that asthma is not a serious disease and a failure to recognize that. [In fact] in 2021, 3,517 people died from complications of asthma,” said physician Stanley A. Schwartz, division chief of allergy, immunology and rheumatology at the University at Buffalo medical department’s internal medicine. “Currently, asthma causes approximately $56 billion in healthcare costs in the United States with hospitalizations making up a significant proportion of that cost.”
Schwartz, who is also a distinguished professor of medicine at Jacobs School of Medicine and Biomedical Sciences, discusses five components people should know about asthma.
1.Causes
Asthma appears in children and some adults who develop the medical condition later in life. Each occurrence in children and adults arises with different symptoms that are important to understand if faced
with similar symptoms.
“While there is no specific genetic basis for asthma, children born to a single parent with asthma have an increased risk of developing asthma, which increases when both parents are asthmatic,” said Schwatz.
Individuals can have situational asthma and can experience symptoms with exertion, exercise or during working hours if they have occupational exposures in the workplace. In the younger pediatric population like infants, respiratory infections are a significant cause of asthma triggers, especially viral infections such as viruses of the common cold, flu, RSV or other viruses. A major asthma trigger in individuals with a history of allergies is allergens such as pollen, pet dander, dust mites and others.
“When there are significant levels of these substances in the air and they are inhaled by patients with allergic asthma, they can trigger an attack,” Schwartz said.
2.Air quality
This year we’ve had a number of days that were labeled as poor quality. Smoke from wildfires can contain harmful particles and gases and exposure to these can cause acute respiratory symptoms especially for individuals with asthma.
“The dangerous air quality can also cause an attack. This was recently exemplified by the drifting smoke from Canadian and U.S. wildfires that caused many asthmatic patients to experience exacerbations this summer. While most but not all cases
Is It Time for a Nap or Energy Drink?
Narcolepsy treatment helps patients regulate sleep
By Deborah Jeanne Sergeant
Many people experience a “three o’clock slump” in energy, when a nap sounds really good but a cup of coffee fills the bill so they can make it through the rest of their day.
For people with narcolepsy, the urge to sleep during the daytime feels overwhelming—and can happen unexpectedly.
The condition can cause them to nod off when they do not want to sleep. A cup of coffee doesn’t help.
“It’s caused by lack of orexin, a chemical in the brain. This deficiency causes narcolepsy and not everyone who has daytime sleepiness has narcolepsy,” said Carleara Weiss,
Ph.D., registered nurse and research assistant professor at UB’s Center for Nursing Research.
Orexins are neuropeptides responsible for controlling arousing from sleep, staying awake and appetite. Without sufficient orexins, people can struggle to stay awake even when they desire wakefulness.
“The person will be working or talking with friends and just fall asleep,” Weiss said. “Or they’re driving and need to stop the car. Even if they’re typing at the computer, they have to fall asleep. Normally, we can have a cup of coffee and keep going. The person with narcolepsy can’t.”
Unwanted sleepiness is not the
of asthma are associated with allergies it is important to recognize some cases of asthma are not,” he added.
3.Misconceptions
Some people believe that asthma is just a childhood disease but in fact, it affects people of all ages. While it is more likely for this to begin in childhood, it can develop later in life. In addition, some myths about asthma treatment have caused some patients to avoid being seen or treated.
There is an incorrect conception that children with asthma will likely outgrow it. Although spontaneous remissions can occur, this is very uncommon and asthma should be considered a chronic disease that deserves lifelong treatment, said Schwartz.
Asthma guidelines are updated periodically and we encourage individuals with asthma to regularly follow up with their allergist or pulmonologist to make adjustments on their medication.
4.Handling asthma
Asthma can be managed with proper medical treatment, lifestyle and education. It is important to be in tune and recognize our symptoms and understand scenarios that can trigger asthma and this includes identifying and avoiding triggers such as allergens, smoke, pollution and respiratory infections. One should take steps to minimize exposure to these.
“For people with allergic asthma, we recommend trying to stay indoors during the allergy seasons when they have their most symptoms. Avoidance of allergens is the first step and highly recommended, such as staying away from pets to which they may be allergic,” said Schwartz.
5.Avoid smoking and unprescribed medication
Smoking is one of the worst habits for asthma and this includes active smoking as well as exposure to secondhand smoke. These can trigger asthma symptoms and make them more severe. Cigarette smoking is the No. 1 cause of preventable death in the U.S. Cigarette smoke irritates
only effect of narcolepsy. Weiss said that nightmares, hallucinations and changes in their deep sleep can also affect patients with narcolepsy.
“Many people with narcolepsy also have depression as well,” she added. “I think one important piece of narcolepsy is adjustment of lifestyle and incorporating napping. For example, they will need to take a nap or naps during the day. It’s not because they’re lazy. Physiologically, they need the naps.”
Narcolepsy type 1 includes cataplexy, when a person’s body abruptly loses muscle control in a way similar to fainting. Physician Alberto Monegro, sleep medicine specialist with UBMD Internal Medicine & UBMD Pediatrics, explained that a loss of orexin is thought to be the cause of type 1.
“Narcolepsy type 2 is thought to be caused by partial damage of orexin neurons or their projections,” Monegro said.
Monegro is a pulmonologist and critical care physician with UBMD Internal Medicine and an assistant professor with Jacobs School of Medicine and Biomedical Sciences at UB.
Physician Stanley A. Schwartz is the division chief of allergy, immunology and rheumatology at the University at Buffalo medical department’s internal medicine.
the lungs, causing redness, swelling and more mucus. Your lungs have a natural defense to keep dirt and germs out.
“Do not smoke or vape,” said Schwartz. “These bad habits not only exacerbate asthma but can cause irreversible lung damage leading to chronic obstructive pulmonary disease [COPD] which when superimposed on asthma can be very difficult to treat and could lead to premature death.
He also warns against using unprescribed treatment methods. If experiencing asthmatic symptoms, it is imperative to consult a healthcare provider, he said. In addition to medications, doctors work closely with their patients to identify and reduce interactions with triggers. In some cases, doctors may order a spirometry test to measure airflow through lungs, chest X-rays, blood tests or skin tests.
“Another issue is prolonged failure to seek medical treatment for asthma, including prolonged use of unprescribed over-the-counter drugs, which can result in irreversible damage to the lungs,” he added. “It is essential to recognize that there is no current cure for asthma, but modern therapies are highly effective and can lead to a high quality of life.”
Cataplexy is not involved with narcolepsy type 2.
Although it can be difficult for patients to receive a prompt diagnosis for narcolepsy, once they do, the proper treatments can help. Monegro said that they include alert promoting agents, stimulants, antidepressants, and the anti-cataplectic agent known as sodium oxybate.
“New medications have come to market as well such as the dopamine and norepinephrine reuptake inhibitor known as solriamfetol, and the histamine H3-receptor antagonist inverse agonist drug known as pitolisant,” he added. “Alert-promoting medications such as modafinil and armodafinil are effective in improving wakefulness. Other medications are also effective in treating narcolepsy when both excessive daytime sleepiness and cataplexy are present such as sodium oxybate, pitolisant, and atomoxetine.”
Anyone experiencing symptoms like unwanted daytime sleepiness should seek treatment from a primary care provider and, if needed, a sleep specialist.
October 2023 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • Page 7
“me time” to meditate and set my intentions for my day.
Practical tips, advice and hope for those who live alone
By Gwenn Voelckers for
October: The Perfect Time to Turn Over a New Leaf
Fall is such a special time of year. For me, it means all good things: relaxing in front of a cozy fire, making pumpkin soup on Sunday afternoons, donning my well-worn leather jacket for long walks and turning my attention to all those inside projects I neglected over the summer.
The brilliant colors, autumnal aromas and industriousness that arrive with the falling leaves really appeal to me. But this hasn’t always been the case.
After my divorce, the month of October left me feeling melancholy. I missed sharing the beauty of the season with a special someone. And I missed the sunshine as daylight waned.
Nostalgia and wistfulness would creep in and I just wanted to retreat into myself. For those who live alone, the month of October has unique challenges.
Not one to wallow in a “poor is me” state of mind, I began to develop and employ some strategies to rekindle my love of the fall season. It can be a great time to mix it up, get busy and expand your horizons.
Below are elements of my annual fall “game plan.” Take a look and see if one or more of these suggestions might add a little color to your life palette this fall:
• Tackle indoor projects: Fall is a great time to accomplish all those
nagging indoor projects on your to-do list. I have a long list and I keep it right in front of me — a daily reminder that I have plenty of home improvements to tackle, both large and small.
Too much idle time is not a friend at any time of year, but it can become downright unfriendly when gray clouds appear and the temperature drops. So, let’s get busy: organize your storage space, do some touch-up painting, update your will or clean out your inbox.
There’s nothing like being productive to beat the autumn blues.
Don’t I know it. I just finished coating my flat-roof porch with a sticky tar sealant. Confession: it was messier than it was fun, but still, I’m proud of my accomplishment. It lifted my spirits.
• Get up and get going: Staying active when there’s a chill in the air can be difficult. I can remember many a cold morning when all I wanted to do was hit the snooze button, pull up the covers and stay in bed.
As nice as sleeping in can be from time to time, I don’t recommend it as a steady diet.
In my experience, there's no better way to start your day than to wake early to start your day. In the early morning’s peace and quiet, there is glorious time to reflect and feel gratitude. I use this important
ADHD: What Parents Need to Know
About 6 million kids have been diagnosed with ADHD as of 201
Lots of children and adolescents have the condition known as ADHD, or attention-deficit/hyperactivity disorder.
What should parents know? A number of treatments exist to help with functioning, including medications approved by the U.S. Food and Drug Administration.
Typically, ADHD begins between ages 3 and 6, according to the U.S. National Institute of Mental Health. It can continue into adulthood.
People can experience one of three types of ADHD. They are predominantly inattentive, with trouble focusing, following instructions and finishing tasks; predominantly
hyperactive–impulsive, with behavior of being “constantly on the go,” talking excessively and interrupting others; and a combination of those symptoms.
An increasing number of children are being diagnosed with ADHD. About 10% of children aged 3 to 17 — or about 6 million kids — have been diagnosed with ADHD as of 2019, according to the U.S. Centers for Disease Control and Prevention.
Boys, at 13%, are more likely than girls, at 6%, to be diagnosed with ADHD.
“Boys are also more likely to have the hyperactive-impulsive type. This type of ADHD is easier to spot
As the morning brightens, my energy grows, as does my appreciation for the precious day ahead me.
• Start moving and enjoy the great outdoors: Fresh air, sunlight and even a gentle rain can be invigorating first thing in the morning. I find a sunrise walk boosts my energy and kickstarts my day. Do I always feel like layering up and taking a walk every morning? No. Do I feel better after I make the effort? Yes, without fail.
I love an unhurried solitary walk to clear my head and be mindful. But I also love a walk with my sister, Anne, or good friend, Kate, to enjoy their company and avoid the Siren song of isolation as the days grow short and get colder.
• Learn something new: Going back to school and fall go hand in hand. Who among us isn’t reminded of the nervous excitement associated with returning to school in the fall? It’s a great time to expand your intellectual horizons.
Each fall I identify a new skill or subject to learn. Last year, I researched how to divide and relocate perennials (my irises and peonies); this fall, I’m signing up to learn French on Duolingo, the free language-learning app.
Continuing education opportunities are abundant in this community and online. Check out colleges and universities, community centers, arts and cultural institutions, your local library, and workshop listings for class and workshop offerings.
• Invite people in: Over the years, I’ve discovered a few simple and manageable ways to bring people into my world and into my home. One way is to organize a gathering around a TV show or series — yes, around the TV.
For years, I invited my single friends over to watch “Downton Abbey” with me on Sunday nights. I provided the soup and salad; they provided the good company.
So, what’s your pleasure? Whether it’s football, a favorite weekly sitcom, or “Ted Lasso” on Apple TV — all of these and other TV shows can become reasons to bring friends and family together. The benefits? You’ll hone your cooking skills (boy, do I now have some great soup recipes!) and you’ll connect with people you care about.
What better way to enjoy a nice fall evening.
There are so many wonderful and meaningful strategies to enjoy the fall season and to ward off the blues that can sometimes emerge during this changing time of year. But these strategies require effort — conscious, creative effort.
If you are feeling sluggish, lonely or isolated, try a few of the strategies above. They have stood me in good stead and have reinvigorated my love for the fall season.
If you, too, are ready to turn over a new leaf, October is the perfect time!
Gwenn Voelckers is the founder and facilitator of Alone and Content empowerment workshops for women (now on hiatus) and the author of "Alone and Content: Inspiring, empowering essays to help divorced and widowed women feel whole and complete on their own" To contact Voelckers or purchase her book, visit www.aloneandcontent.com

than the quieter child who is inattentive,” said child psychiatrist Tiffany Farchione, who reviews ADHD drugs at the FDA.
Untreated ADHD can have serious consequences, the FDA warns, including falling behind in school, having difficulties with friendships and experiencing conflicts with parents.
Children with untreated ADHD also have more emergency room visits and are more likely to have self-inflicted injuries. Meanwhile, untreated adolescents are more likely to take risks.
A visit with your child's pediatrician can help determine if your child has ADHD. Also have your child's vision, hearing and anything else that might contribute to inattention checked.
Stimulants and non-stimulants are both approved by the FDA to help reduce symptoms of ADHD in children as young as age 6.
Containing various forms of methylphenidate and amphetamine,
stimulants have a calming effect on children with ADHD, Farchione said. They are thought to increase brain levels of dopamine, a neurotransmitter associated with motivation, attention and movement.
Approved non-stimulants are Strattera (atomoxetine), Intuniv (guanfacine), Kapvay (clonidine) and Qelbree (viloxazine).
Some children with ADHD also receive behavioral therapy to help manage symptoms and learn coping skills. Community support groups and schools may also provide some help.
FDA-approved medications have been tested for safety and effectiveness. Clinical trials will now look at their safety and effectiveness in children aged 4 and 5.
“We know ADHD medications are being prescribed for younger children, and we think it's essential that the data from clinical studies reflect the safety and effectiveness for this age group,” Farchione said in an FDA news release.
Page 8 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • October 2023
Live Alone & Thrive
alone
survival is measured in months.
Q: How, then, is it possible that a person who never smokes contracts lung cancer?
A: Smoking is responsible for most lung cancers, but not all. In those cases, the person may have been exposed to secondhand smoke or to radon and other toxins. The good news? Lung cancer rates are decreasing, kids are not starting to smoke, clinical advances have been achieved, and help is available through the Quitline.
Q: With all the restrictions, why is smoking still such an issue?
A: More people are quitting and current smoking rates are at record lows. But smoking has been prevalent for years, especially with the creative marketing used to promote tobacco products and cigarette smoking is still the leading cause of preventable death in the United States.
Factors to reduce cigarette smoking include things that raise the expense of smoking like the recent cigarette excise tax increase, lowering the availability of tobacco retailers, making products that are not appealing to young people, and restrictions on where one can smoke. And there is no such thing as a “smoking gene.”
Some tobacco users rationalize their smoking by thinking nothing bad will happen to them or they cite examples of people who smoked and lived to be 100.
Q: What about other forms of smoking — vaping, for example?
More American Men Now Opting for Vasectomy
Vasectomies are becoming more common in the United States, with rates surging by more than one-quarter during the past decade, a recent study reveals.
The U.S. vasectomy rate increased by 26% between 2014 and 2021, according to an analysis of commercial health claims data.
“All areas in the United States except the Northeast showed increased vasectomy rates,” said senior researcher and physician Omer Raheem. He is an assistant professor of surgery-urology with the University of Chicago School of Medicine.
Overall numbers remain low, with roughly 4% of men having undergone vasectomy, the researchers noted.
But doctors expect the demand for vasectomy will continue to increase following the 2022 Supreme Court decision that abolished the national right to abortion.
Q & A with Andrew Hyland
By Brenda Alesii
Andrew Hyland, the chairman of the department of health behavior at Roswell Park Comprehensive Cancer Center, directs the New York State Smokers Quitline.

He has been with Roswell Park since 1995, working to help people eliminate their tobacco use and ultimately make the Quitline a thing of the past. In Good Health recently spoke with Hyland, a Williamsville resident who earned his Ph.D. in epidemiology and community health from the State University of New York at Buffalo.
Q: Let’s talk numbers. How many people smoke in New York state, according to your research?
A: Throughout the state, 12% of the adult population uses cigarettes or about 1.7 million people. In Western New York, that translates to about 7% of the population, causing 1,500 deaths. In addition, 30% of all cancer deaths are attributed to smoking.
Q: What types of cancer are directly related to smoking?
A: Lung cancer is the leading cause of cancer death. In fact, lung cancer kills more than the next three combined: colon, breast and prostate. Tobacco use is a big deal. About 85% of lung cancers come from combustibles — cigarettes and cigars. Lung cancer is among the deadliest and most aggressive type of the disease;
A: Vaping products have grown significantly. Nobody thinks young people using vaping products is a good idea, and about 4% to 5% of adults in the state are e-cigarette users. These products have lower levels of toxins but are not safe.
Q: Is your Quitline a free service?
A: Yes. Our service helps anyone using a nicotine product. We can be reached seven days a week by phone or by texting QUITNOW to 333888 or chat, and at our website: www.nysmokefree.com. Our phone number: 1-866-NY-QUITS.
Q: What should one expect when calling the Quitline?
A: The caller will speak to a trained tobacco treatment specialist, who will help identify smoking triggers, key issues and determine if nicotine replacement therapy is appropriate. A large number of clients have other co-morbidities, which may make them eligible for other resources.
We offer starter kits that help reduce cravings. It is not a magic pill, however. the evidence shows it can help.
Q: Who is your typical client?
A: Most of our clients have a lower income, lower education, lack of private health insurance and experience other mental and physical health challenges. They want to quit but are facing strong headwinds. We offer a free service to help them. We receive on average 100 calls a day across the state.
Q: How is the Quitline funded?
A: We work with a $4 million annual contract with funding from the New York State Department of Health.
“After the Roe v Wade overturn, there has been a significant increase in Google searches for vasectomy, as well as an uptick in vasectomy consultations and procedures,” physician Stanton Honig, division said chief for reproductive and sexual medicine at Yale School of Medicine.
“This recent study points to the fact that men are taking more of a role in reproductive health and family planning, especially when they are finished having children,” continued Honig, who was not involved with the new research.
For the study, Raheem and his colleagues gathered health insurance claims data to calculate the annual vasectomy rate among privately insured men in the United States, aged 18 to 64.
The percentage of all male patients undergoing vasectomies in a given year increased from about 0.43% in 2014 to 0.54% in 2021, the investigators found.
The relative increases were greatest in men with no children (61%), men with an older wife (41%), single men (41%), and young men 18 to 24 (37%).
Vasectomy also remained a popular option for men with two or more children, the results showed.
Rural areas experienced greater increases in vasectomy rates than urban areas, the researchers added.
“Given the political landscape, some men are leaning in and taking more responsibility to prevent unintended pregnancy,” said physician Monica Dragoman, system director of the complex family planning division in the department of obstetrics, gynecology and reproductive science at Mount Sinai School of Medicine in New York City.
October 2023 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • Page 9
Head of NYS Smokers Quitline in WNY helps people butt out cigarettes — “More people are quitting and current smoking rates are at record lows,” he says
RDs vs CNs: What the Difference?
Careers of registered dietitian nutritionist and certified nutritionist present differences
By Deborah Jeanne Sergeant
They both would tell you to quit eating so many potato chips and start eating more veggies.
So, what’s the difference between a registered dietitian nutritionist (RD) and a certified nutritionist (CN) or a certified nutrition coach?
Some of the confusion lies in the name. A few years ago, registered dietitians began going by “registered dietitian nutritionist” or just “nutritionist” as a more consumer-friendly approach. “Dietitian” sounds restrictive. Who wants to go on a diet?
“Nutritionist” sounds like someone focused on good nutrition. Although it’s mainly marketing, the moniker update can make it difficult for some people to understand the differences between the two.

RDs typically function within a medical setting to address specific diagnoses or health goals.
“Registered dietitians are widely trained as clinicians,” said Dana Ingebretson, master’s trained registered dietitian, certified diabetes educator, certified dietitian nutritionist and chair the Wellness Department at Neighborhood Health Center in Buffalo. “We can assess a person from multiple aspects: nutritionally, psychosocially, ability to change, counseling techniques, interpreting research. A nutritionist may or may not be trained in multiple ways,
focusing more on nutrition, not in terms of assessing or being able to counsel. A lot of nutrition care is not just about food.”
One thousand supervised hours of interning and a bachelor’s degree is required to sit for the registered dietitian exam and as of January, that bar will be raised to the master’s level for new internships. Ingebretson already has a master’s degree. In addition, once the nationally recognized credential is bestowed, the registered dietitian must complete 75 credit hours of continuing education every five years.
“You won’t find a certified nutritionist working in healthcare because they can’t bill insurance companies,” Ingebretson said. “You might find one running a practice where they charge out of pocket. Someone who is a pharmacist or medical doctor might take a six-month course and get training, too. Certified nutritionists can give good, science-based information, but it’s hard to practice this alone.”
She said that programs such as the American Nutrition Association and Precision Nutrition are examples of programs that provide good training.
To become a certified nutritionist requires completing a few weeks to six months of classes on the basics of
macro and micronutrients. CNs, also sometimes called nutrition coaches, typically function within settings such as a health foods store, wellness center or, like Sean Rohrback, a gym. Rohrback owns L&S Fitness in Rochester and is a certified nutritionist through Precision Nutrition. He said he completed his coursework in a total of 18 months.
Of course, programs to become a CN or nutrition coach vary, but Rohrback said that his coursework was “a deep dive into the science of nutrition, understanding the ins and outs from scientific perspective and the psychology of working with clients. It had practical work with case studies and understanding how to apply the information to help clients attain good health. It’s not just nutrition but emotional and existential and environmental health and social health and mental. It looks at the person as a whole and how the coach can guide them to better decisions.”
He recognizes that the RD prescribes meal plans for specific ailments and diseases—duties outside of his scope—and he sticks with helping people make better nutritional choices, paired with stress reduction and physical activity.
Rohrback hopes to eventually complete coursework to become a nationally board-certified health coach. A father-to-be, Rohrback is also working on pre- and post-natal certification through Girls Gone Strong to help women in those stages of motherhood.
“What we focus on here is to help people move better and get stronger,” he said of L&S. “It’s an overall more sustainable way they can work out and be a strong leader in life and do what you want. It’s about how to help people from a movement standpoint. We help people who’ve had surgery and have done rehabilitation. We’re the next step.”
The Ross Eye team is dedicated to providing comprehensive and advanced care to all ages. Our pediatric eye specialists provide comprehensive eye exams to assess your child’s vision health, reducing the risk of their vision affecting school participation and grades.


With three locations, including a new stateof-the-art location in Orchard Park, the comprehensive eye care professionals and surgeons at the Ross Eye Institute are the team to turn for all your eye care needs.

Specializing in:
• pediatric eye care
• adult eye care: general eye health/conditions
• cataracts
• dry eye
• macular degeneration
• & more!
Page 10 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • October 2023 Career in Healthcare
ROSSEYE.COM Additional Information
SmartBites
By Anne Palumbo
The skinny on healthy eating
Helpful Tips
Select blemish-free squashes that feel heavy and firm, especially near the stem ends. Delicata’s thin, easy-to-slice skin does not need to be peeled before cooking. Also, this squash holds its shape during cooking, making it an excellent choice for stuffing and baking. As mentioned, whole delicata keep for several months if stored in a cool, dry place.
Boost Your Immune System with Delicata Squash
When I discovered delicata squash a few years ago, I couldn’t stop talking about it. I still can’t! The taste, the texture, the nutrition, the delicate skin…oh, if only it were available year-round.

The good news is, they’re in season now through November. And the even better news is, they can be stored safely for about two to three months in a cool, dry place.
But here’s the best news of all about this striped, pleasantly sweet winter squash: it’s chock full of nutrition, particularly vitamins C and A — two vitamins that boost immune system health. Right now, with flu and cold season bearing down on us, bolstering this all-important system seems wise.
Like other winter squashes, delicata is super low in fat, sodium, cholesterol and calories (only 40 per cup). And while it may have more carbs than some vegetables (10 grams per cup), it is by no means a carb-watcher’s nightmare. As a comparison: 1 cup green beans (7 grams), 1 cup corn (27 grams), 1 medium potato (35 grams), and — okay, this is not a vegetable but I couldn’t resist
— 1 soft pretzel (80 grams).
Delicata’s natural carbs are “complex” and take longer to digest, versus the “refined” carbs found in processed foods, such as sugary drinks, pastries, white bread, most snacks, and many cereals. The good fiber-rich carbs in delicata squash provide longer-lasting energy, more stable blood sugars, and fiber-driven heart protection. The bad fiber-depleted carbs in most processed foods, on the other hand, tend to cause spikes in blood sugar levels, which can trigger hunger and lead to food cravings. Numerous studies support that excessive refined-carb consumption may pave the way for health problems, such as obesity, Type 2 diabetes, and heart disease.
Unlike other hard-skin winter squash, delicata’s skin is edible, adding a nutty deliciousness to an already yummy squash. But that’s not all it adds: its skin is also rich in fiber, vitamins, minerals, and antioxidants. Antioxidants are beneficial molecules that fight free radicals, which, when elevated in your body, have been linked to heart disease, cancer, and other diseases.

Milk Alternatives Don’t Always Measure Up to Milk
PARMESAN-CRUSTED
ROASTED DELICATA SQUASH

Serves 4
1 delicata squash, washed and dried
1 tablespoon olive oil
¼ teaspoon kosher salt coarse black pepper, to taste
¼ cup grated parmesan cheese

1. Preheat oven to 425° F. Line a large baking sheet with parchment paper; set aside.
2. Trim the ends off the delicata squash, then slice the squash in half lengthwise and scoop out the seeds. Slice the seeded halves into ½-inch thick slices (half circles) and place them in a large bowl.
3. Drizzle the olive oil, salt, and pepper over the squash slices, tossing well to coat. Transfer
¼ cup whole-wheat panko breadcrumbs
1 teaspoon dried thyme
1 garlic clove, minced
1 teaspoon lemon zest (optional)
to the prepared baking sheet, arranging the slices in an even, flat layer.
4. In a small bowl, combine the parmesan, breadcrumbs, thyme, garlic, and lemon zest.
5. Sprinkle the parmesan mixture over the squash, pressing to adhere.
Roast in the center of the oven until tender and golden brown, about 25 minutes.
Anew analysis of more than 200 plant-based milk alternatives found that few contain the calcium, vitamin D and protein that can be found in cow’s milk.
Only 12% of the alternative milk products studied had comparable or greater amounts of all three nutrients, the University of Minnesota study showed.
“Our results provide evidence that many plant-based milk alternatives are not nutritionally equivalent to cow’s milk,” said Abigail Johnson, associate director of the University of Minnesota School of Public Health Nutrition Coordinating Center.
“Based on these findings, consumers should look for plant-based milk alternative products that list calcium and vitamin D as ingredients. They may also want to consider adding other sources of calcium and vitamin D to their diets.”

Both calcium and vitamin D were
identified in the 2020-2025 Dietary Guidelines for Americans as nutrients of public health concern for underconsumption.
“We know from our dietary assessments for nutrition studies that consumers are choosing more plantbased milk alternatives,” Johnson said in a news release from the American Society for Nutrition.
Only 28 plant-based alternatives had similar or more calcium, vitamin D and protein as dairy milk, the study found.
“Our findings point to a need to ensure that consumers are aware that many plant-based milk alternative products in the marketplace today are not nutritionally equivalent to cow’s milk,” Johnson said. “Product labeling requirements and dietary guidance to the public are among the approaches that may be helpful in alerting and educating consumers.”
October 2023 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • Page 11
to officials.
While many patients come to Roswell Park from the Western New York region, many also come from across the country seeking care. Last year, Roswell Park treated patients from a total of 42 states as well as one foreign country.
Bills quarterback Jim Kelley, who has sought various treatments there since being diagnosed with cancer of the upper jaw in 2013 and since experiencing multiple recurrences.
Cancer Centers in Buffalo Attract
According to the North American Association of Central Cancer Registries, based on data collected between 2016 and 2020, New York state is one of the top 10 states for invasive cancer incidence rates, with other states in that group including New Jersey, Kentucky, Iowa, and West Virginia.
Local, Out-of-State
Patients
Roswell Park and Erie County Medical Center offer a wide range of treatments for cancer, including a number of clinical trials
 By Julie Halm
By Julie Halm
Nobody ever wants to hear the words, “it’s cancer.” When they do, however, there are critical choices to be made, including where a person chooses to seek treatment.
Here in Western New York, there are several options for patients should they receive that news, which is delivered to just shy of 115,000 New York state residents on an annual basis, according to the New York State Department of Health’s Cancer Registry and Cancer Statistics.
According to that same source, “cancer is the second most common chronic disease in New York state and is second only to heart disease as the leading cause of death.”
Roswell Park Comprehensive Cancer Center declares in its very name exactly the patients which it aims to treat, and they do so at great volume on an annual basis.
According to the most recent vital statistics, measuring the center’s last fiscal year running from April 1, 2022 to March 31, 2023, the facility, which has a total of 157 beds, had a total number of 49,105 patients under active care, according to statistics published by the center. In addition to more established treatments, Roswell Park currently has 193 active cancer-related clinical trials assessing some new therapy or approach — and another 40-plus set to open within the next 6 months, according
The most prevalent cancers found in patients very based on age, ethnicity, gender and other factors, which can impact where those diagnosed chose to seek their treatments. According to the North American Association of Central Cancer Registries, the most commonly diagnosed cancers in North American men are, in order of prevalence, prostate; lung and bronchus; colon and rectum; bladder; and melanoma of the skin. There is some alignment among North American women with the top five by gender being, in order, breast, lung and bronchus; colon and rectum; uterus corpus and uterus NOS; and melanoma of the skin.
Regardless of the diagnosis, residents of the Western New York region and those considering coming to this area for treatment are not limited in their choices.
The Erie County Medical Center also offers a variety of treatments for patients with cancer at the Center for Cancer Care, including specialties in head and neck, plastic and reconstructive surgery, dental and medical oncology, maxillofacial prosthetics, and breast oncology, according to the organization’s website.
While many cancer patients have chosen to be treated at ECMC, among the most famous is former Buffalo
Just last year, the Commission on Cancer, a program of the American College of Surgeons, granted the Buffalo hospital a three-year accreditation, meaning that it has met 34 COC quality care standards and will be evaluated every three years to determine if the facility “Maintain(s) levels of excellence in the delivery of comprehensive patient-centered care.”
ECMC is also a member of the Great Lakes Cancer Care Collaborative.
Perhaps with these qualifications in mind, 2,433 new cancer patients were treated at the Center for Cancer Care ECMC in 2022 and 2023.
That tally includes a variety of treatments ranging from chemotherapy, surgical interventions and those seeking second opinions regarding their care. Of those individuals, several traveled considerable distances to seek care at ECMC, including three patients from Ontario, Canada, 15 patients from out of state and 26 who came from other parts of New York outside of the Western New York region.
Like Roswell Park, ECMC is also participating in clinical trials, with 12 clinical research projects in total at the facility at this time.
Unlike Roswell Park, ECMC treats a wide range of patients, including those seeking emergency and trauma care, bariatric surgery, behavioral health services, and orthopedic and sports medicine, among other things.
Whether a cancer patient hails from the city or its surrounding suburbs, out of state or even out of the country, they have several options right here in Buffalo.
AI Assisted Mammograms
Study: Radiologist using artificial intelligence detected
than
only by radiologists without AI help
By Deborah Jeanne Sergeant
Astudy published by Swedish researchers in August indicates that artificial intelligence (AI) can safely augment and even improve radiologists’ work in detecting breast cancer.
The study is the first trial that compares AI-assisted mammogram readings with human-only mammogram readings.
The radiologist using AI detected 20% more cancers than those read only by two radiologists without AI help.
Using AI didn’t appear to increase the number of false positive mammograms, which is when an abnormality is noted but not actually present.
In addition to greater efficacy, using AI also reduces the work hours needed to read mammograms by 44% because AI replaces the work of one radiologist (some hospitals require that two radiologists are required to read each mammogram). This can be particularly helpful in health systems with few radiologists, such as in rural areas.
According to the American College of Radiology, 82% the 20,970 radiologists providing patient care are age 45 and older and 53% are 55 and older. The demand for radiologists is
rising as the aging Baby Boomers require more care. The Bureau of Labor Statistics states that the need for new radiologists is expected to rise by 6%, “faster than average” between 2022 and 2032 compared with all other occupations. Enlisting the help of AI can help mitigate this rise in demand.
“Early research appears to show that AI-assisted mammograms may be an important tool to help radiologists detect breast cancer,” said Susan Brown, registered nurse and senior director of health information and publications at Susan G. Komen headquarters in Dallas. “It is hoped that AI-assisted mammograms will increase accuracy and efficiency.”
Brown noted that false positives and false negatives could be an issue with AI-read mammograms but hopes that additional research will confirm the early studies on AI assisted mammograms.
Nancy Wayne, marketing administrator at Rochester-based Elizabeth Wende Breast Care, wants to see additional research to show that AI plus a radiologist is just as good as two radiologists.
“AI is a wonderful tool,” she noted. “We’re still early on in the development of AI. There are multiple products out there currently. We’re

Page 12 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • October 2023
Women’s Health / Breast Cancer Awareness
20% more cancers
those read
→
Women’s Health / Breast Cancer Awareness Understanding the Stages of Breast Cancer:
0, 1, 2, 3 and 4
Adiagnosis of breast cancer comes with many tough questions, but one of the biggest is what stage your cancer is.
Millions of women struggle with such questions every year: Breast cancer is the most common cancer in women in the United States, with the sole exception of skin cancers, according to the American Cancer Society. It accounts for roughly onethird of all new female cancers each year.
Once you receive a breast cancer diagnosis, your doctor will determine the stage of your particular cancer using the results of your diagnostic tests. Knowing the specific stage of your cancer helps determine the best treatment options for you, as well as your expected survival rate.
The most common tool physicians use to stage breast cancer is the American Joint Committee on Cancer’s (AJCC) TNM system. T stands for the size of the tumor, N for whether the cancer has moved into lymph nodes, and M indicates whether the cancer has spread to other places in the body. Numbers or letters after T, N and M provide more details about each factor. Higher numbers mean the cancer is more advanced.
According to the American Society of Clinical Oncology (ASCO), breast cancer stages are broken down into five levels: Stages 0, 1, 2, 3 and 4. Below you will find expert guidance on each of the stages, along with the associated five-year relative survival rate.
Stage 0 breast cancer
In stage zero (0) breast cancer, also called noninvasive or in situ cancer, the disease is only in the ducts of the breast and has not spread to the surrounding breast tissue (Tis, N0, M0).
Stage 0 breast cancer survival rate is 99%.
Stage 1 breast cancer
Stage IA: In this stage, the tumor is small, but has invaded the breast tissue. There is none in the lymph nodes (T1, N0, M0).
Stage IB: The cancer has spread to the lymph nodes and is larger than 0.2 mm but less than 2 mm. Either there is no sign of a tumor in the breast, or it is 20 mm or smaller (T0 or T1, N1mi, M0).
Stage 1 breast cancer survival rate is 86% (Stage IB) to 99% (Stage IA).
Stage 2 breast cancer
Stage IIA:
• While no evidence of a tumor is found in the breast, the cancer has spread to one to three axillary (under arm) lymph nodes. The cancer hasn’t spread to other parts of the body (T0, N1, M0).
• A tumor of 20 mm or less is found in the breast, and the cancer is in one to three axillary lymph nodes (T1, N1, M0).
• While the tumor is larger (greater than 20 mm but not more than 50 mm), it has not spread to the
axillary lymph nodes (T2, N0, M0).
Stage IIB:
• The tumor is greater than 20 mm but not larger than 50 mm. It is also found in one to three axillary lymph nodes (T2, N1, M0).
• The tumor is larger than 50 mm but none is found in the axillary lymph nodes (T3, N0, M0).
Stage 2 breast cancer survival rate is 86% to 99%, depending on whether it has spread to the lymph nodes.
Stage 3 breast cancer
Stage IIIA: This stage involves a tumor of any size which has spread to four to nine axillary lymph nodes or to internal mammary lymph nodes, but has not spread to other parts of the body (T0, T1, T2, or T3; N2; M0). This stage may also have a tumor larger than 50 mm which has spread to one to three axillary lymph nodes (T3, N1, M0).
Stage IIIB: The tumor has invaded the chest wall or has caused ulceration or swelling of the breast. There may or may not be cancer in as many as 9 axillary or internal mammary lymph nodes. It hasn’t spread
to other parts of the body (T4; N0, N1 or N2; M0). It also may have been diagnosed as inflammatory breast cancer.
Stage IIIC: Any sized tumor that has invaded 10 or more axillary lymph nodes, the internal mammary lymph nodes, and/or lymph nodes under the collarbone. It has not spread to other parts of the body (any T, N3, M0).
Stage 3 breast cancer survival rate is 86%.
Stage 4 breast cancer
This stage involves a tumor of any size. The cancer has spread to other organs, including the bones, brain, liver, lungs, distant lymph nodes or into the chest wall (any T, any N, M1). Metastatic breast cancer found when cancer is first diagnosed only occurs about 6% of the time and may be called de novo metastatic breast cancer. Usually, metastatic breast cancer isn’t found until after a previous diagnosis and treatment of early-stage breast cancer.
Stage 4 breast cancer survival rate is 30%.
still not quite able to say one product fits all. There are multiple companies with proprietary products. We’re hopeful where at some point the AI has to fulfill certain criteria to be appropriate. I’m not sure at this point we’re there. It is promising.”
“AI is everything in imaging,” said Avice O’Connell, director of the UR Medicine breast imaging program. “But it’s not going to take our jobs. AI is something we’ve been using for more than 20 years in mammography. In 1998 the first computer aided detection the computer-scanned images and highlighted things that could be cancer. There’s still that kind of computer-aided detection. There are usually four marks on every exam, so a human still has to look at it. It’s just an aid to make sure we’re not missing things.”
O’Connell views AI as a means to screen the “easy” cases more quickly so radiologists can pay more attention to more challenging cases. But in either, a human must be involved; AI is only a tool but doesn’t make any decisions about health.
“The patient makes the ultimate decision whether or not to have the biopsy,” O’Connell said. “We’d still follow up the patient in six months.”
O’Connell sees machine learning
Susan Brown, is a registered nurse and senior director of health information and publications at Susan G. Komen. “It is hoped that AI-assisted mammograms will increase accuracy and efficiency.”

as the next threshold of mammography advancement, meaning that AI technology reads more and more mammograms; it becomes more skilled at catching abnormal findings. She also thinks that AI-assisted mammography will help in areas of the world where few specialists exist.

“The vast majority of breast imaging around the world is not read by breast experts,” she said. “AI has huge value in every country.”
YOUR SUPPORT
Enjoy reading In Good Health newspaper? The paper is free to you but very expensive to produce and distribute. Keep the publication going. Consider supporting the publication. If you are a reader, please become a paid subscriber. If you’re a nonprofit, a medical practice or organization, consider advertising in the paper. You will get a great deal of exposure since the paper is everywhere for the entire month. We will even design your ad at no charge.
For more information, send an email to editor@BFOhealthnews.com — Type “Support” on the subject line.
October 2023 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • Page 13
→
Health / Breast Cancer Awareness
How I Beat Cancer...
Patty Wieczorek of Amherst
Get screened for breast cancer: There’s really no excuse
By Julie Halm
Patty Wieczorek wasn’t experiencing any symptoms of breast cancer at the age of 48. She had no family history of breast cancer, either. But she still went regularly for screenings — something she says that all women should do.
The practicality of that advice proved itself when at that age, at a regular screening, Wieczorek learned that she had ductal carcinoma in situ in one of her breasts. While not the news that anyone wants to hear, the meaning of the medical lingo is that the problematic cells have not spread outside of the duct.
According to the Breast Cancer Research Foundation, this particular form of cancer has a 98% survival rate at the 10-year mark.
Wieczorek is not one to panic easily, she said, referring to herself as a very practical person. She also
noted that her husband is an epidemiologist and her son is an OB-GNY, so she is plenty used to being in the world of healthcare.
“My attitude was ‘OK, now what’s next? Let’s get ‘er done,” she said. What was next was surgery. She underwent a total of four to make sure her margins were clear and then underwent radiation to complete her treatment.
For the next 10 years, she contin
‘Catching the Cancer Early Was the Biggest Thing’
By Jane Schmitt
Codds of surviving breast cancer greatly increase when the disease is diagnosed and treated in the beginning stages.
In fact, the Amer ican Cancer Society describes early detection as central to its goal “to en sure every one has an opportunity to prevent, detect, treat and survive cancer.”
“I’ve always been a true believer that if you have something ailing you, get it checked out before it gets worse,” said Nichols, an Amherst woman whose own cancer journey began in mid-2021 when her annual screening revealed irregulari ties in her left breast.

Now done with treatment, she’s
ued to undergo routine screenings, urging her two adult daughters to do the same.
Although she felt calm and pragmatic about her own journey, a mother never stops worrying about her own children, she noted.
“It’s concerning, it really is,” she said. “It’s very important for the first generation after me to get screened regularly. Your girls are considered high risk because your mother had it.”
She and her daughters have also undergone genetic testing and Wieczorek said that she is encouraged by the ongoing advancements in that process as well.

“Before, they used to only look at the BRCA1 and BRCA2 genes,” she said. “Now they look at 17 different genes.”
Despite the initial optimism of
The diagnosis was ductal carcinoma in situ, or DCIS.
“I was shocked. There was a moment of ‘Are you kidding me?’ I would never have known because there were no physical signs, no symptoms. There was no lump that I felt,” said Nichols, 51. “Imaging caught it. Had they not caught it, what could have happened?”
Thus began a journey that so many others have gone on, with a referral to an oncologist followed by more tests, then surgeries and a treatment plan that included chemotherapy. Next was radiation therapy, which her doctor ordered five days a week for four weeks.
“Luckily, I didn’t have any nausea. I had an appetite, but everything tasted different because of the medications,” she said. “I hadn’t had a Big Mac in decades and one Saturday my husband took our son swimming and he called me on the way home to see if I needed anything. It was probably the first day of treatment and I said, ‘I need a Big Mac!’ So my loving husband got me one.”
Spreading the message
Nichols was determined to not let the cancer diagnosis affect her and her family more than was necessary.
“My mindset was, ‘I’m going to get through this.’ There are people who have gone through worse and had bigger surgeries and lived through it,” she said. “I wanted to keep my daily life as normal as possible.”
That wasn’t easy, however. And she had her share of low points.
“After my second surgery, I came home and sat on the couch and started to cry. My husband asked what
her prognosis, a decade later, Wieczorek would learn that her cancer had returned and this time, she was not a candidate for the measures doctors had taken the first time.
“So at that point, once you’ve gotten radiation, it’s over with and you can’t do radiation again on that particular breast so then you end up having a mastectomy,” she said.
Through the second diagnosis, which came about five years ago, Wieczorek said that she maintained the attitude and outlook she had the first time.

“My whole philosophy, when it came back, was like, ‘OK, now what?’” she said. “I didn’t fear dying.”
That kind of courage, though goes hand in hand with taking pragmatic steps to prevent the situation from becoming worse than it need be, including getting screened regularly. While she firmly pushes her own daughters to get screened, Wieczorek said that she also encourages other women to do the same, noting that for most, the cost of screenings is covered by insurance as a part of regular preventative care.
“There really is no excuse,” she said. “Just make the appointment.”
was the matter and I said, ‘This just sucks.’ He said, ‘That’s OK, just let it out.’ Ten minutes later, I was good,” Nichols said. “I just needed that ‘woe is me’ moment.”
When the cancer treatments caused her hair to come out in clumps, her hairdresser shaved her head. Her husband, Joe, showed his support by shaving his head, too.
“He really stepped up. He wanted to do everything — the laundry, the meals. It was almost too much for me sometimes because I’m kind of a control freak,” Nichols said. “The days I was in bed, just exhausted and feeling lousy, he was fabulous — so doting. If I needed anything, he was always right there. But if I needed to be left alone, he left me alone.”
She turned to social media to post treatment updates and encourage others to pay attention to their health and wellness. Inspiring people to take action and get screened was a priority, fueled by her own experience and something special she had created at home.
“One thing that helped me through it was what I call my Inspiration Wall. So many people sent me cards, notes, little gifts and pick-meups. I took all of those and put them on a wall that we walk by multiple times a day,” she said.
Now she is firmly focused on the future, with a post-treatment regimen that includes six-month checks via mammograms and ultrasounds. And she continues to spread the message that early detection of cancer can save lives.
“After my first surgery, I went out for girls’ night with three friends. One was a cancer survivor. The other two were delayed on their mammograms. They made their appointments the next day,” she said.
Page 14 • – Buffalo & WNY’s Healthcare Newspaper • October 2023 Women’s
Cathy Nichols of Amherst has been a big advocate for women to get screened for breast cancer
How I Beat Cancer...
Janice Hetrick of Lancaster
Donnie dolls and foot races – how one woman handles her cancer
By Julie Halm
In 2012, Janice Hetrick’s mother was diagnosed with breast cancer.

As a result, for a time, she went to get mammograms every six months, until her insurance company said that they were no longer necessary at that interval and they wouldn’t be covering the cost every six months any further. It was within the next six months — and three years to the month after her mother’s own diagnosis — that Hetrick heard, “it’s cancer.”
She and her mother had different types of breast cancer and as the mother of two daughters, Hetrick wanted to get genetic testing done. She said that because she was older than 50, her insurance declined to cover that cost.
Roswell Park Comprehensive Cancer Center would later offer, however, because among Hetrick’s mother, father, herself and three brothers, only one brother was cancer free.
When her own breast cancer was found, it was on the left side and involved her lymph nodes. Hetrick, a former nurse at St. Joseph Campus in Cheektowaga, said that she elected
to take what she felt were the best next steps, which included a double mastectomy.
“It was up to me and when they said lymph nodes, I’m a nurse, I’m not going to mess around,” she said.
One of the hardest parts of her journey was telling her own mother about the diagnosis, she said, adding that her mother felt guilt over the situation. When her own mother was diagnosed, Hetrick’s family decided to do a mud run event, which involves racing and doing physical tasks in muddy conditions, as the name implies.
“It happened to start raining that day and my mom was at the finish line because she was undergoing chemo, and she’s crying because we all finished and we’re all full of mud and so I decided to start doing all of these races for her, so I did like 43 of these races between 2012 and 2015,” said Hetrick. Her own diagnosis would not stop that momentum either. “When I was diagnosed, the day before my surgery, I rapelled the Niagara Casino, and then a week after my double mastectomy I did the Tough Mudder and then after I
Melinda Easter of Williamsville Not your mother’s breast cancer
By Julie Halm
There was once an Oldsmobile commercial which referred to its newer, improved vehicles as “Not your father’s Oldsmobile.”
So when Melinda Easter was diagnosed with breast cancer, like her mother before her, one of the pos itive thoughts she hung on to was, “this is not my moth er’s breast cancer.”
Easter was 48 — the same age as her mother was — when she was diagnosed in 2002. Despite the family history, she said that she had never worried too much and just went for her regular mammograms.
“It’s not that I didn’t think about it, I just didn’t worry about it,” she said.
Her first diagnosis was on her
right side and it was invasive ductal cancer. She knew that there would be treatments and perhaps struggles ahead, but she took solace in knowing that her journey would not look like her moth-
“It’s just the progress that they’ve made and that made me feel really good,” she said. “What my mother suffered through, it was awful, but she forged the way so that I didn’t have to.”
Easter underwent a surgical biopsy, then a lumpectomy and because the margins were never clear, she eventually underwent a Just two years later, she began experiencing discharge from her left breast, what she called a “dead
finished chem and radiation a week later I did a marathon in Florida.”
She has also done numerous biking events, including one crossstate in support of her mom and from diagnosis to present has done more that 350-foot races.
It was during one of those races shortly after a surgery, that participants were supposed to go in a creek. A friend asked what she might have in her car to represent her going into the creek and the best bet was a Donnie Wahlberg doll left behind by one of her grandkids from a recent camping trip. It became a running theme from then on, “wherever I go, Donnie
giveaway.” This time, however, the cancer was lobular and completely unrelated to her first battle. She underwent chemotherapy as well as her second mastectomy.
Although the second round of breast cancer was not a recurrence, she would later find a lump on the left side of her chest which as a recurrence from the first, causing her to undergo chemotherapy, surgery and radiation, which she said was the one treatment she always wanted to avoid.
Easter said that the series of diagnosis, despite the positive attitude she tried to have, became at points, exhausting. This was especially the case after she was later diagnosed with unrelated lung cancer.
When the third breast cancer diagnosis came, she said she could almost understand because she wasn’t necessarily following all of the medical advice that was given to her, but between her third bout of breast cancer and the lung cancer diagnosis, she had been following medical advice to a T and adding other healthy habits to her routine.
“I did at first, did the protocol. Where I went off was after the second breast cancer, I finished with chemo and then you crash through menopause and the doctor said, ‘We’re going to prescribe you anastrozole, an aromatase inhibitor’ and I thought, ‘Are you kidding me? It’s
goes,” said Hetrick. Since then, she has gotten to meet Wahlberg and had Donnie dolls signed by the New Kids on the Block founding member. Other women who receive a breast cancer diagnosis might not choose a Donnie doll as one of their coping tools, but Hetrick said that she would give others the same advice she gave her own brother when he received a pancreatic and liver cancer diagnosis.
“Don’t just sit there, if you want to get up and go for a bike ride, get up and go for a bike ride. You can’t let cancer control you,” she said. “You have to control it.”
just going to weaken my bones and all of the bad things you hear,’” she said. “I just had a bad attitude and was tired.”
Eventually, she did wind up taking the medication and did great with it, which has helped her form some of the advice she would give to other women who find themselves in her shoes.
Although she has no daughters, Easter does have granddaughters and said she would tell them that they should follow the medical protocols and balance those with more holistic things.
Easter has taken up yoga, learned about nutrition and sought therapy during her journey. She also says that the power of friendship and community to get you through the hard times. A former music teacher, she still hangs onto CDs made for her by friends during that time as well as the cards that came in from her students.
“It’s buoyant, the love of friends,” she said.
While it’s understandable that Easter might worry about her granddaughters one day receiving the diagnosis that she and own mother did, she said she takes comfort in the thought that medical advances by that time will make any potential diagnosis for them, not their grandmother’s breast cancer.
October 2023 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • Page 15 Women’s Health
/ Breast Cancer Awareness
Women’s Health / Breast Cancer Awareness
Hormone Replacement Therapy Can Ease

Menopause Symptoms
As if night sweats, mood swings, mid-section weight gain, low libido and vaginal dryness weren’t bad enough — menopause can also raise the risk of cardiovascular disease, autoimmune disorders and osteoporosis. Is hormone replacement therapy an option?
By Deborah Jeanne Sergeant
Ever since prescribing hormones for menopausal symptoms — known as hormone replacement therapy — was correlated with increased risk of blood clots, stroke and cancer, fewer doctors have offered hormone replacement as an option.
However, James Woods, OBGYN with URMC, said that the real problem is a lack of understanding the biology behind menopause.
“You don’t need to fear menopause,” Woods said. “Your quality of life can be maintained with proper management. You just need people who understand this biology. You improve the overall health with the patient. We need specific things to be dealt with. Some women come in weeping or fearful. All they’ve been told is to ‘live with it; it’s just part of getting older.’ Or ‘It’s good news; you can’t get pregnant. Or ‘Hormones are bad; stay away from them.’”
He views menopause as not just one year without menses but a 10- to 20-year window where a woman transitions into the post-menopausal state. Each month from puberty until the early 40s, the ovaries produce high levels of estradiol at mid-cycle, when the woman’s body ovulates.
“That provides enormous positive effects,” Woods said.
Those include estradiol’s anti-inflammatory properties and its ability to boost dopamine and other “happy hormones.” But around age 40, when ovaries start to show some age, those positive effects begin to decline and by age 51 on average, women begin menopause. Since measuring estradiol levels isn’t part of a typical exam, it’s not obvious during that 10-year window that anything’s changing until other symptoms show up.
The old way of addressing menopause through hormones was high doses of estrogen-only therapy. However, estradiol is one type of estrogen. Just treating women with a dose one-tenth of what their ovaries would naturally produce offers benefits. Research from the National Institutes of Health show that estradiol helps protect bones and may improve cardiac function.
Woods said that the correlation between hormone therapy and breast cancer arose from a study with an oral product, Premarin with a synthetic, Provera, which resulted in fewer than one in 1,000 in the control group compared with the placebo group. But another part of the study using only Premarin showed a slight reduction of breast cancer.
“That has been maintained for 20 years,” Woods said. “Women carry a concept of ‘hormones cause breast cancer.’ It’s a statement that has to be broken down.”
These days, oral estrogen isn’t as commonly prescribed because more targeted delivery methods exist, like a patch or cream. Oral medication is filtered by the liver, which can raise the risk of blood clots.
Maintaining hormone levels can help reduce inflammation and promotes the body’s ability to support bone density. Woods explained that in younger women, the bones are in a constant state of building new cells and breaking down old cells. But an inflammatory response of the body disrupts that process so the bones become softer.
Hot flashes are more than a nuisance. Woods said that they can indicate a higher cardiovascular risk. The hypothalamus in the brain signals the body to develop at puberty.
“Right next to that group of two neurons is the heat center,” Woods said. “When you’re younger, you didn’t realize you have half a degree that your body temperature could fluctuate and it would send a signal that you’re hot. You lose that half a degree and it sends a signal to the brain that you’re hot.”
The body sweats as a response to get that heated blood near the surface of the skin to cool.
“It’s a cardiovascular risk,” Woods said. “If it’s not treated and stopped, those women will be at more risk of cardiovascular damage and death. It’s not just an inconvenience.”
Weight gain also affects many women between 45 and 65. Woods said that the lack of estradiol causes inflammation of the lining of the intestines and upsets gut bacteria. In turn, the body’s metabolism slows down so that it stores more fat, increasing risk of cardiovascular disease, diabetes and more.
Depression and anxiety can also increase the risk of cardiovascular disease. These mental health struggles can stem from health issues, as well as what Woods calls the “chronic stress window” of caring for aging parents, working full time at the busiest part of her career, and bearing the majority of household chores and child rearing responsibilities.
“At that stage many women realize life didn’t work out,” Woods said. “Domestic violence, divorce and kids who could be in trouble add to the stress.”
Woods said that compared with women of the same age who lack these stressors; their immune system is different from those subjected to chronic stress.
He said that the best time to begin hormone replacement is around 48, as the levels begin to dip and before inflammatory damage begins. Woods also counsels about other, non-hormonal treatments that may help.
“The story about the risks of HRT have been confusing for both women and their medical providers over the last 20 years after the press around the Women’s Health Initiative study in the early 2000s leading to a generation of patients and clinicians terrified about HRT generally,” said physician Pebble Kranz, assistant professor of clinical family medicine and obstetrics and gynecology at University of Rochester and medical director of the Rochester Center for Sexual Wellness. “We now know that many of the findings from that study need to be evaluated in context and with more nuance.
“For most people younger than 65, HRT is not harmful and can be beneficial regarding heart, bone, sleep, mental and sexual health. Meanwhile, the current guidelines are that HRT should be used for bothersome symptoms of menopause — hot flashes, sleep disruption, vaginal symptoms and others — not for prevention of health issues of aging. As with so much in medicine, the benefits and risks of HRT should be an individualized conversation with a qualified healthcare provider,” Kranz said.
She wishes more providers would seek more up-to-date information about menopause care from organization such as The Menopause Society.
Samantha Sassone, doctorate of nursing practice, adult nurse practitioner and clinical director at Vitalize Medical & Aesthetics in Rochester specializes in HRT. She said that treating menopausal symptoms should be an individualized approach, starting with a physical and comprehensive blood work.
“Everyone is not on the same prescription,” she said. “We base it on their chief complaint, like more libido, or stopping the hot flashes or mood swings. We can tailor it to their specific needs.”
Patients receiving estradiol do so through pellets placed under the skin every four months. Sassone said they’re well tolerated and avoid the issues associated with patches and creams, such as the cream rubbing off on others or the patches falling off.
Patients receiving pellets must have a recent negative mammogram and PAP smear results and they receive follow-up appointments to keep tabs on their health.
Patients also receive follow-up appointments within six to eight weeks, including lab work and again in six months and thereafter annually.
Another of the ways Sassone treats menopausal symptoms is through peptide therapy, which mimics the pituitary gland to generate human growth hormone. This “whole body therapy” boosts mood, collagen production, muscle recovery, better sleep, libido and hair, skin and nail health.
“Each woman is different,” Sassone said. “Sometimes, it’s used for a couple of years to help them get through the symptoms. Some like the way they feel and it’s long-term.”
Page 16 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • October 2023
Pebble Kranz
Oral Contraceptive Soon Available Without a Prescription
Opill offers a 98% rate of effectiveness in preventing conception. It’s expected to hit the market in early 2024
By Deborah Jeanne Sergeant
The FDA recently approved Opill (norgestrel) as an over-thecounter oral contraceptive. It’s expected to be available early 2024, according to news reports.
Typically, oral contraceptives require a physician’s exam and prescription. Opill was first approved with a prescription in 1973. When taken as directed — one pill daily at the same time each day — Opill offers a 98% rate of effectiveness in preventing conception.
“This is so exciting,” said physician Elana Tal, UBMD Obstetrics & Gynecology, clinical assistant professor, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo. “It could potentially be a big game changer.”
Tal said that unlike oral contraceptives that contain estrogen and progestin, Opill is safe for people who smoke or who have a history of blood clots, stroke or bleeding disorders.
The FDA’s website states that women who have or who have had breast cancer shouldn’t take Opill. Other contraindications include women who are pregnant or who think they might be pregnant, along with another birth control pill, vaginal ring, patch, implant, injection or an intra uterine device, or as an emergency contraceptive, also known as a morning-after pill. Men should also not take Opill.
Dual-hormone contraceptives typically warn that it’s not recommended for women 35-plus. However, Opill has no such contraindication. Its safety has been established for women as young as 15. However, sale of Opill will not be limited by age.
Opill has the typical oral contraceptive side effects. The FDA listed irregular bleeding, breast tenderness, headaches, nausea, dizziness, ab-

dominal pain, increased appetite and bloating.
The FDA encourages women to discuss Opill with a healthcare provider or pharmacist if they currently take a prescription for drugs to treat seizures, tuberculosis, HIV AIDS, pulmonary hypertension or take an over-the-counter supplement containing St. John’s wort. Opill may interact with these drugs or become less effective. Opill can also affect the efficacy of emergency contraceptives.
Tal views Opill as a way for patients who want contraceptives but are between doctors or insurance plans.
“There are six million new pregnancies in the US a year, about half of which are unintended,” Tal said. “As access to reproductive healthcare and high-quality maternity care becomes difficult for people to access, what a game changer this could be, especially for the most disenfranchised among us.”
Although Opill will be available without seeing a doctor, PAP smears and routine care are still important.
The Centers for Disease Control and Prevention states on its website that “all women are at risk for gynecologic cancers and risk increases with age.” It’s vital that women seek preventative exams on the schedule their care provider recommends, even if they use Opill.
“Oral contraceptives are one of the many methods of family planning,” said Kafuli Agbemenu, registered nurse with UB School of Nursing and Women’s Reproductive Health Researcher. “With Opill, a contraceptive can be accessed in a timely fashion, without the delay of finding a healthcare provider, scheduling and attending a medical appointment, needing insurance to fill a prescription and actual availability of the contraceptive at an affordable
cost. All these are even more challenging for younger people or those living in rural areas with limited access to healthcare providers. Opill will also enhance health equity by potentially increasing contraceptive access to underserved populations. Additionally, considering recent access to reproductive health services changes, an over-the-counter contraceptive will contribute to empowerment and bodily autonomy.”
She said that barriers to healthcare include geographic access, affordability, stigma, privacy and adherence.
Women taking Opill should take it for seven days prior to relying on it for contraception to better ensure its effectiveness. For many years, doctors have routinely prescribed oral contraceptives for controlling patient’s abnormal bleeding, period pain and other similar issues. But the FDA has not approved Opill for these uses. It’s vital that women seek a provider’s care for such symptoms and not try to self-diagnose and hope Opill will take care of it.
The active ingredient in Opill concerns the Rev. Jim Harden, CEO of CompassCare, which offers reproductive counseling and sexually transmitted infection testing and treatment services in Rochester, Buffalo and Albany and statewide via telehealth.
“Peer reviewed medical articles and the World Health Organization state that this exposure to steroidal contraception increases risks of cancer,” Harden said.
Harden writes extensively on medical ethics. His book “Ethical Theory and Pertinent Standards in Women’s Reproductive Health” was endorsed by the late Edmund D. Pellegrino, a physician and former chair of the President’s Council on Bioethics; senior research scholar at the Kennedy Institute of Ethics; and professor emeritus of Medicine and Medical Ethics at Georgetown University.
Hardin noted the National Institutes of Health’s statement about progestin-only oral contraceptives as “at least comparable to the risk of combined oral contraceptives” which the NIH said “increase the risk of breast cancer” as a “group 1 carcinogen for breast cancer, as well as for cervical and liver cancer.”
The FDA’s website states that “each Opill tablet contains 0.075 mg. of a single active steroid ingredient, norgestrel, a totally synthetic progestin.”
Harden believes that the side effects of Opill have not been clearly communicated to patients and that once it’s available without a prescription, many women, particularly younger women, will take it without reading any of the package warnings or without knowledge of it side effects.
“It appears this drug is wildly unsafe under normal circumstances, say nothing of giving access without physician oversight,” he said. “Once this is available over the counter, you’re eliminating the safety net that is so important to medicine.”
He believes that over-the-counter access to Opill would mean that women may try to take Opill off-label as emergency contraceptives, a use for which Opill has no FDA approval.
Colt Wasserman, a physician, views Opill as lowering barriers for people who face barriers in obtaining contraceptives.
“It provides another way of obtaining contraceptives,” he said. “I feel really excited for patients.”
Wasserman is chief medical officer for Planned Parenthood of Western and Central New York, which includes offices in Rochester, Canandaigua, Batavia, Buffalo, Niagara Falls and Syracuse.

Every county’s health department offers free condoms, as do many other organizations. However, Wasserman feels that “contraception is not a one-size-fits-all decision. It’s really important for each patient to have a lot of different resources to plan their future. I’m excited about barrier methods and condoms being widely available, but an over-thecounter contraceptive is only going to increase the number of choices people have.”
The cost for Opill is not yet known. If it follows the pattern of emergency contraception, which costs about $88, then Opill would not reduce barriers to contraception for people with a low income.
Opill will likely not have an age minimum for purchasing it. Youth who are too young to buy over-thecounter cough syrup will be able to purchase Opill once it’s available in the first quarter of 2024. As for concerns about teens taking Opill without parental supervision, Wasserman doesn’t see a problem.
“We know that teenagers and youth can understand how to use contraception safely and effectively,” he said. “Requiring some kind of ID proof of age can disproportionally affect those who don’t have access to an ID. When this was issued, it was decided to make it generally available.”
He also does not believe that greater availability of contraception will increase the rates of teens becoming sexually active. Wasserman wants parents to try to maintain open conversations about matters such as sex and “establish themselves as safe people in their youth’s lives to be able to provide guidance,” he said.
October 2023 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • Page 17 Women’s Health / Breast Cancer Awareness
“It could potentially be a big game changer,” said physician Elana Tal at UBMD Obstetrics & Gynecology, referring to Opill, the new over-thecounter oral contraceptive approved by the FDA.
Women’s Health / Breast Cancer Awareness
Breast Cancer
‘Over-diagnosed’
Among Older Women
Study: Some women over 70, if diagnosed with breast cancer, need to weigh if pursuing treatment is the right course
By Deborah Jeanne Sergeant
Arecent study of 54,635 women ages 70-plus by Yale School of Medicine indicates that 31% of women ages 70-74 and 47% of those 75-84 were possibly “over-diagnosed” with breast cancer.

The term means that they were found to have a kind of breast cancer that is slow growing and that treatment would likely not extend their lives or improve their quality of life.
In fact, pursuing treatment such as lumpectomy, mastectomy or chemotherapy would dramatically decrease quality of life.
“There is no exact age at which women should stop getting mammograms,” said Susan Brown, registered nurse, senior director of Health Information and Publications at Susan G. Komen headquarters in Dallas. “Breast cancer risk increases with age and mammography doesn’t appear to be less effective in women 70 and older. However, there are risks of mammography in older women, including over-diagnosis and over-treatment, when a cancer that would not have caused problems if untreated is treated and the person is subjected to side effects without receiving any real benefit from the treatment.”
Many major health organizations recommend women ages 70 and older continue to get regular mammograms as long as they are in good health and could benefit from treatment if breast cancer were found.
She added that poor health may cause some women may stop routine breast cancer screening, as would the presence of other health issues that would take precedent. The organiza-
tion’s stance is that women should be able to access regular screening mammograms as long as they and their providers think they should. When to stop mammography— and when to start—relies upon many health factors.
Robert Smith, vice president of Early Cancer Detection Science for the American Cancer Society, said that women at high risk may start with annual mammograms earlier than other women, typically around age 30.
“Some women with a first-degree relative like a mother or a sister who was diagnosed at a young age have been advised to begin screening ten years before the age that relative was when she was diagnosed,” Smith said. “Women who receive regular mammograms are more likely to have breast cancer diagnosed earlier, less likely to need aggressive treatments, and more likely to be cured. However, mammograms are not infallible; they may miss some cancers, and even when issues are found in an initial screen, further testing may be needed to confirm the presence of cancer.”
Those who are 55 and older may choose to switch to every other year. But Smith said those who are 75 or older can continue annual screening as long as they remain in good health and expect to live at least another 10 years.
At Rochester-based Elizabeth Wende Breast Care, there’s not age cutoff for mammogram for patients who want them.
“At age 25, we sit down and talk about risk factors like family histo-
A Year After Launch, OTC Hearing Aids Aren’t Catching On With U.S. Consumers
It’s now been possible to buy a hearing aid over-the-counter for nearly a year, but few Americans are doing so.
More education is needed about just who these over-the-counter (OTC) hearing aids can help, according to the American Speech-Language-Hearing Association (ASHA). It polled more than 2,200 Americans about the issue in late June and early July.
Just 2% of respondents aged 40
and older who have hearing difficulties said they had purchased an OTC hearing device, the poll showed.
In all, 4% said they were likely to purchase an OTC hearing aid in the next year.
About 56% of respondents said their hearing wasn’t the best. Only 8% had been treated.
Many said their hearing difficulties weren’t “bad enough” to warrant care, the ASHA found.
About 48% of respondents with
ry, genetic mutations, and if they’re Black or other minorities or Ashkenazi Jewish and therefore higher risk,” said Nancy Wayne, marketing administrator. “We want to offer screening opportunities earlier than 40 as needed for the higher risk women who may have a genetic mutation or who’ve had breast cancer already or have had radiation to the chest wall at a young age.”
But even for women with no history of breast cancer in their family and with no issues, Wayne said that a first mammogram by 40 is recommended.
“There’s more to it than dying,” said Avice O’Connell, director of the UR Medicine Breast Imaging program. “There are people who ignore their cancers and it’s ulcerating through their skin and dripping. You also want them to stay comfortable. It depends on the age and health of the woman coming in. In England and Ireland, they don’t do mammograms after age 70. You’d have to pay for it yourself. It’s so much easier to take out a cancer the size of a bean or grape. You can take it out and monitor without radiation or chemotherapy.”
Although the medical protocol isn’t to ignore breast cancer, the approach is different.
“We may not want to go all out like they’re 35,” O’Connell said. “If someone’s educated and informed enough, they should make that decision. There’s nothing wrong with monitoring. Screening picks it up long before you feel it. If it is not growing, you could keep following it.”
Allison Magnuson, a breast cancer oncologist with URMC, looks at
untreated hearing difficulties let their symptoms persist for more than two years. Nearly one-third of folks with hearing difficulties said their quality of life had been adversely affected.
“Hearing problems aren’t uniform. They vary and, thus, so does treatment,” Janice Trent, vice president for audiology practice at the ASHA, said in an association news release. “The longer one waits to act, the greater and more costly problems can become.”
That’s why ASHA urges the public to seek a comprehensive hearing evaluation from a certified audiologist before purchasing an OTC device or taking some other step.
“Insurance providers cover these evaluations, which ensure that care is appropriate and effective,” Trent said.
ASHA noted that a recent study found that using hearing aids can significantly reduce cognitive
age as only a number—and only one aspect of the patient’s health profile.
“The number really doesn’t mean a lot,” she said. We need to step back and look at overall health status and what is their remaining life expectancy. There’s a lot of variability.”
Someone in her early 70s may have numerous comorbidities and maintenance drugs. Or she could be spry, active, eating well and in good health with no issues. That’s what Magnuson refers to as “physiological aging, not chronological aging.”
“Any type of diagnosis or treatment really has to be put into the context of someone’s overall life expectancy and health status,” she said. “A medical condition that arises for someone with a shorter lifespan, it may not bother them. An indolent, slower growing cancer may not manifest into a problem in their lifetime.”
Some older women with numerous other medical problems and a new breast cancer diagnosis may enjoy a better quality of life with medication that can help slow the growth of the cancer.
Magnuson thinks that patients should discuss their providers their overall health and life expectancy when considering mammograms and if a lump is discovered.
“If side effects outweigh the benefits, we talk about this,” Magnuson said. “Talk with your doctor about your preferences. Everyone thinks differently and makes decision differently. It’s about having that conversation with your doctor about any decision. The doctor can guide you on pros and cons, but only the patient knows what’s in their own values and what value they put on those pros and cons.”
(“thinking”) decline.
OTC devices are intended for people aged 18 and up who have mild to moderate hearing loss. They’re not meant for children.
Advertising about the devices isn’t always helpful, according to ASHA, which noted an inaccurate comparison between OTC hearing aids and reading glasses. The hearing aids do not simply increase sound volume. Hearing can be damaged if an OTC is over-amplified, the association warned.
“Hearing health must be a priority, not something that is taken lightly, neglected, or treated inappropriately or without clear and complete information,” Trent said. “We will continue to educate the public and professionals about OTCs as well as [about] the importance of hearing health and taking prompt action when hearing difficulties arise.”
Page 18 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • October 2023
By Jim Miller


How Seniors Can Save on Prescription Drug Costs

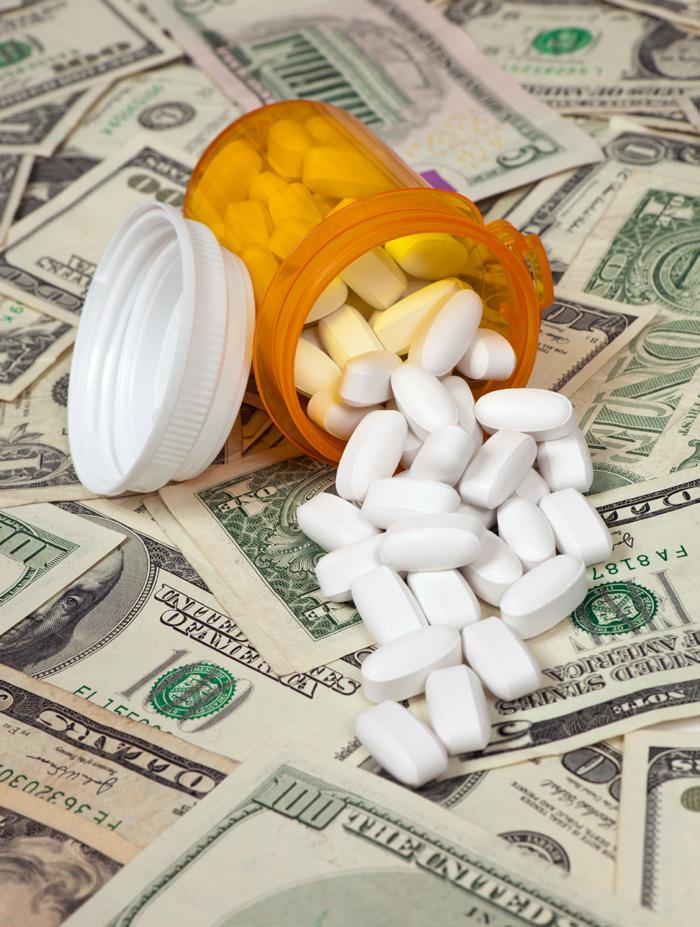
Dear Savvy Senior,
I take several medications for multiple health conditions and the prices keep going up, even with my Medicare prescription drug insurance. Can you recommend any tips that can help cut my costs?

Tapped Out Tina
Dear Tina,
The high cost of prescription drugs is an ongoing problem that stings everyone, but it usually affects seniors more because they have a greater need for medications and because Medicare doesn’t cover all their drug costs.


While the Inflation Reduction Act, that was signed into law last year, will help seniors save on their medications by negotiating lower drug prices and capping out-of-pocket spending at $2,000, it will be a few years before the law is fully enacted. In the meantime, here are some different strategies that can help reduce your costs so you can afford what you need.
• Talk to your doctor: A good first step is to review your medications once a year with your doctor to find out if any of them can be stopped or reduced. If you’re taking any brandname drugs check to see if they are available in a cheaper generic form. Also, for any drugs you’re taking long-term ask your doctor for a cheaper three or six-month prescription, versus a one month. And find out if any of the pills you’re taking can be cut in half. Pill splitting allows you to get two months’ worth of medicine for the price of one. If you do this, you’ll need to get a prescription for twice the dosage you need.
• Review your insurance: Carefully review your drug coverage during the open enrollment period, which runs Oct. 15 – Dec. 7 for Medicare beneficiaries. Make sure all your regular medications are covered in the plan’s formulary; that your current pharmacy is in the plan’s network; and that your plan covers additional medication coverage in the gap. To shop and compare Medicare prescription drug plans go to Medicare. gov/plan-compare.
• Pay cash: Not using insurance for prescriptions seems counterintuitive, but in some cases, it may save you money. For example, many chain pharmacies and big-box stores like Walmart and Costco have their own prescription savings programs that may be lower than your insurance copayment. Or you can use coupons through GoodRx.com or RxSaver. com that can save you up to 80% off
the list price of generic and some brand-name drugs in certain pharmacies.
• Shop online: You can also save on regularly used medications by having them sent to you from a mail-order pharmacy. Check with your health insurer or regular pharmacy to see whether it will get you a better deal. If not, check online pharmacies like CostPlusDrugs.com or HoneybeeHealth.com. With these, you may spend less in some cases than you might with insurance.
• Buy from Canada: Because prescription drugs are often much cheaper north of the border, many Americans have chosen this option for years. While this is technically illegal in most states, the Food and Drug Administration generally does not stop people from doing it. If you want to explore this option use PharmacyChecker.com, an online tool that will help you identify reputable Canadian and international online pharmacies.
• Get more help: If your income is limited, you may also be able to get help through Medicare’s Extra Help program (Medicare.gov/basics/ costs/help/drug-costs), your state pharmaceutical assistance program (Medicare.gov/plan-compare/#/ pharmaceutical-assistance-program/ states) or patient assistance programs (Medicare.gov/pharmaceutical-assistance-program). Visit each website to see if you’re eligible and to apply.
October 2023 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • Page 19
Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.
SEND US YOUR FEEDBACK AND GET A FREE SUBSCRIPTION! NAME ADDRESS WHAT DO YOU LIKE ABOUT IN GOOD HEALTH NEWSPAPER? CITY/TOWN STATE ZIP Yes! Send me six free issues of In Good Health to the above address, beginning with the upcoming issue. P.O. Box 550, Amherst, NY 14226 Disclaimer: your comments may be used for marketing purposes. WHERE DID YOU PICK UP THE PAPER? 100 Amherst Villa Road / Buffalo, NY 14225-1432 716.626.5808 / / MERCYFLIGHT.ORG GREAT PLACE TO WORK: WHY MERCY FLIGHT EMS IS A • DYNAMIC PEOPLE • EXCITING LEARNING OPPORTUNITIES • MERCY FLIGHT GIVES BACK TO THE COMMUNITY • FLEXIBLE SCHEDULING AVAILABLE • COMPETITIVE COMPENSATION AND BENEFITS • DEVELOP YOUR EMS CAREER WITH MERCY FLIGHT • STATE-OF-THE-ART EQUIPMENT Mercy Flight, Inc. is an equal opportunity employer and a proud supporter of the WNY community. JOIN OUR TEAM Apply today at mercyflight.org/join-our-team We have immediate opportunites for full-time and part-time positions with the Mercy Flight EMS team for Dispatcher, Certified First Responder, EMTB, A/EMT, A/EMT-CC and EMT-Paramedic candidates. Pay rates are commensurate with experience, starting at: CFR Drivers $15.65/hr EMT-Basic $17.85/hr A/EMT $18.85/hr A/EMT-CC $23.50/hr EMT-Paramedic $24.50/hr Dispatcher $18.40/hr • 401(k) with 3.5% Employer Match for all employees • Wide variety of health and welfare benefits available for full-time employees
Surviving domestic abuse requires not only escaping the reach of the perpetrator to achieve physical safety, but also recovering emotionally and mentally.

Marcy Abramsky, licensed clinical social worker and owner of InspireAmind in Williamsville, said that survivors of domestic violence often feel an anxious adrenaline surge immediately after leaving.
“It’s like you’ve just robbed a bank and whatever just happened will catch up with you,” she said. “This mixed feeling of fear and yet the rush of what you think you want. You feel totally confused about what happiness is to you.”
Once the basic, immediate needs of housing and financial resources are met, it’s important to seek emotional support through counseling and group support. At that point, “you can begin to really consider the fact that you are now safe,” Abramsky said. “This support also helps you to accept the reality of what you lived through versus your new safety. As part of the healing process, you should look at your resources, self-awareness and transformation of your perspective. Find resources within your family, friends or new peer group for support. Connect to people start to be authentic and share your true experiences without fear of judgment.”
For a long time, the survivors have been forced to deny their own thoughts, wishes, and needs to fulfill the perpetrator. Some survivors were dominated by an abuser so long that
Domestic Abuse Recovery
By Deborah Jeanne Sergeant
they no longer know how to make decisions or even what they want anymore, from choices as trivial as what to eat for dinner to choices as important as who to date. This can place them in danger of becoming trapped in another abusive relationship again.
Perpetrators purposefully craft their version of reality around the survivor by cutting them off socially, denying them their victims their rights and individuality and enforcing—with consequences—the abuser’s point of view.
“Gain awareness and perspectives--sexually, intellectually, emotionally and financially--and take in the new information about who you really are,” Abramsky said. “Update and reprogram yourself by working to evaluate that who you are isn’t what your abuser made you think. It is your new perspective and awareness of your strengths, value and happiness.”
Perpetrators do more than hit. Abuse can also include intentional and persistent mental, emotional, spiritual and sexual abuse. Mental abuse includes intimidation, mind games, gaslighting and manipulation. Emotional abuse can take the form of “love bombing” followed by withdrawal, threats, cruelty and completely withholding love and affection. Spiritual abusers may restrict or force participation in particular worship and spiritual expression and use ever-shifting “rules” about spiritual practice to control the victim. Sexual abuse involves using sexual
practice for manipulating the victim, such as forcing or withholding intimacy or demanding unwanted types of sexual activity. The foundation of all abuse is consistently using means to control and dominate the other person.
In addition to the brainwashing aspects of abuse, survivors suffer the loss of their relationship (difficult though it was) and often their home, pets, work, friends and possessions. Numerous areas of their lives change in a flash when they leave.
Jill Woodruff, board-certified art therapist and licensed mental health counselor in private practice in Dansville, likens it to the processing required for grief and loss. The stages are not necessarily linear, and it takes time to work through it, as victims have been conditioned to live under the perpetrator’s control over every area of their lives for months and typically years. Before diving into another romantic relationship, it’s vital to recover first.
“Always with mental health, there’s no right answer as to how anyone is supposed to feel,” Woodruff said. “Give people time and space to feel. Hold a space for them and give them time.”
Woodruff advises survivors to stay in one-on-one therapy as long as possible.
“That gives you someone outside your own head giving you input,” she said. “Find a group to participate in to feel validated.”
Caring friends can also help provide support in rebuilding a sense
of self-worth and confidence. Oftentimes, survivors are more gracious to others than themselves.
“Ask yourself, ‘What would a healthy relationship look like if I saw it for someone else?’” Woodruff posed. “Your own lens is skewed by abuse. Providing reflective distance for ourselves can help us see what’s healthy for someone else is also healthy for ourselves.”
This strategy can help build better skills for navigating relationships, whether friendships or romantic relationships. Survivors need to learn how to set personal boundaries that are neither too permissive nor too restrictive.
Most abusers damage the survivor’s relationships with others as isolating the victim helps keep the abuse secret and prevent supportive friends and loved ones from helping. Becoming involved in group settings with a hobby or other activity can help rebuild friendships and build new friendships.
“Get involved in a supportive community setting with a hobby or something that feels good and is unconditional and supportive,” Woodruff said.
This can be a good time to pick up a beloved hobby that was dropped or to try something completely new. Some people find that practicing martial arts provides a supportive community of new friends, a physical activity that is both mentally and physically engaging, and practical skills that can boost their confidence.
Page 20 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • October 2023
Experts say when immediate needs of housing and financial resources are met, it’s important for victims to seek emotional support through counseling and group support






































































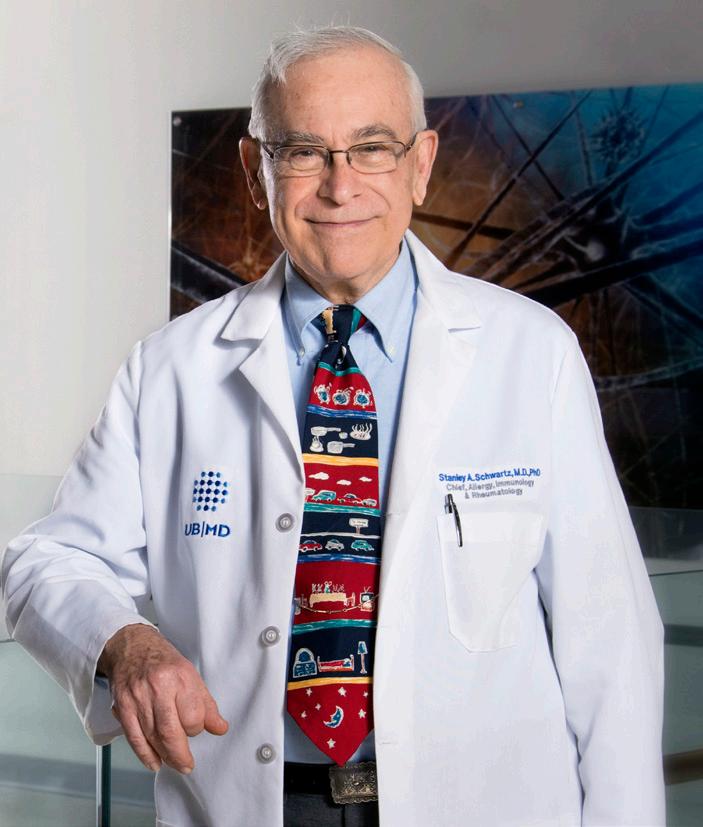











 By Julie Halm
By Julie Halm