REMOTE NURSING
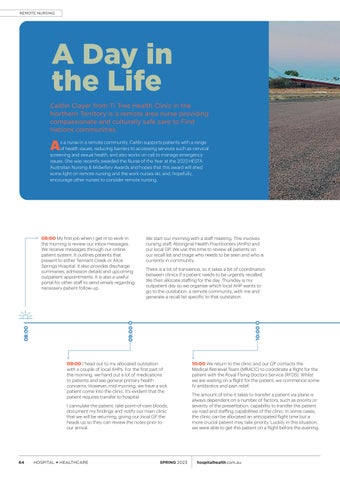
A Day in the Life Caitlin Clayer from Ti Tree Health Clinic in the Northern Territory is a remote area nurse providing compassionate and culturally safe care to First Nations communities.
A
s a nurse in a remote community, Caitlin supports patients with a range of health issues, reducing barriers to accessing services such as cervical screening and sexual health, and also works on call to manage emergency issues. She was recently awarded the Nurse of the Year at the 2023 HESTA Australian Nursing & Midwifery Awards and hopes that this award will shed some light on remote nursing and the work nurses do, and, hopefully, encourage other nurses to consider remote nursing.
We start our morning with a staff meeting. This involves nursing staff, Aboriginal Health Practitioners (AHPs) and our local GP. We use this time to review all patients on our recall list and triage who needs to be seen and who is currently in community. There is a lot of transience, so it takes a bit of coordination between clinics if a patient needs to be urgently recalled. We then allocate staffing for the day. Thursday is my outpatient day so we organise which local AHP wants to go to the outstation, a remote community, with me and generate a recall list specific to that outstation.
10:00
09:00
08:00
08:00 My first job when I get in to work in the morning is review our inbox messages. We receive messages through our online patient system. It outlines patients that present to either Tennant Creek or Alice Springs Hospital. It also provides discharge summaries, admission details and upcoming outpatient appointments. It is also a useful portal for other staff to send emails regarding necessary patient follow-up.
09:00 I head out to my allocated outstation with a couple of local AHPs. For the first part of the morning, we hand out a lot of medications to patients and see general primary health concerns. However, mid-morning, we have a sick patient come into the clinic. It’s evident that the patient requires transfer to hospital. I cannulate the patient, take point-of-care bloods, document my findings and notify our main clinic that we will be returning, giving our local GP the heads up so they can review the notes prior to our arrival.
64
HOSPITAL + HEALTHCARE
SPRING 2023
10:00 We return to the clinic and our GP contacts the Medical Retrieval Team (MRACC) to coordinate a flight for the patient with the Royal Flying Doctors Service (RFDS). Whilst we are waiting on a flight for the patient, we commence some IV antibiotics and pain relief. The amount of time it takes to transfer a patient via plane is always dependent on a number of factors, such as priority or severity of the presentation, capability to transfer the patient via road and staffing capabilities of the clinic. In some cases, the clinic can be allocated an anticipated flight time but a more crucial patient may take priority. Luckily in this situation, we were able to get this patient on a flight before the evening.
hospitalhealth.com.au