NURSING
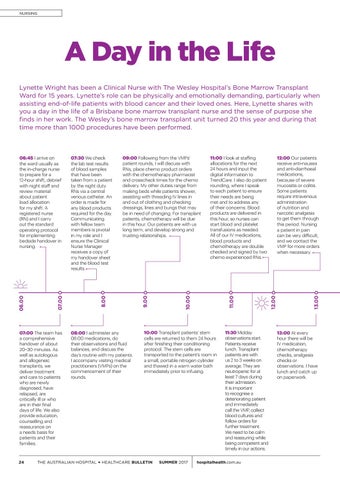
A Day in the Life Lynette Wright has been a Clinical Nurse with The Wesley Hospital’s Bone Marrow Transplant Ward for 15 years. Lynette’s role can be physically and emotionally demanding, particularly when assisting end-of-life patients with blood cancer and their loved ones. Here, Lynette shares with you a day in the life of a Brisbane bone marrow transplant nurse and the sense of purpose she finds in her work. The Wesley’s bone marrow transplant unit turned 20 this year and during that time more than 1000 procedures have been performed.
07:00 The team has a comprehensive handover of about 20–30 minutes. As well as autologous and allogeneic transplants, we deliver treatment and care to patients who are newly diagnosed, have relapsed, are critically ill or who are in their final days of life. We also provide education, counselling and reassurance on a needs basis for patients and their families.
24
08:00 I administer any 08:00 medications, do their observations and fluid balances, and discuss the day’s routine with my patients. I accompany visiting medical practitioners (VMPs) on the commencement of their rounds.
SUMMER 2017
11:30 Midday observations start. Patients receive lunch. Transplant patients are with us 2 to 3 weeks on average. They are neutropenic for at least 7 days during their admission. It is important to recognise a deteriorating patient and immediately call the VMP, collect blood cultures and follow orders for further treatment. We need to be calm and reassuring while being competent and timely in our actions.
hospitalhealth.com.au
13.00
12.00
11.00
10:00 Transplant patients’ stem cells are returned to them 24 hours after finishing their conditioning protocol. The stem cells are transported to the patient’s room in a small, portable nitrogen cylinder and thawed in a warm water bath immediately prior to infusing.
THE AUSTRALIAN HOSPITAL + HEALTHCARE BULLETIN
12:00 Our patients receive anti-nausea and anti-diarrhoeal medications, because of severe mucositis or colitis. Some patients require intravenous administration of nutrition and narcotic analgesia to get them through this period. Nursing a patient in pain can be very difficult, and we contact the VMP for more orders when necessary.
11:00 I look at staffing allocations for the next 24 hours and input the digital information to TrendCare. I also do patient rounding, where I speak to each patient to ensure their needs are being met and to address any of their concerns. Blood products are delivered in this hour, so nurses can start blood and platelet transfusions as needed. All of our IV medications, blood products and chemotherapy are double checked and signed by two chemo experienced RNs.
10.00
09:00 Following from the VMPs’ patient rounds, I will discuss with RNs, place chemo product orders with the chemotherapy pharmacist and crosscheck times for the chemo delivery. My other duties range from making beds while patients shower, assisting with threading IV lines in and out of clothing and checking dressings, lines and bungs that may be in need of changing. For transplant patients, chemotherapy will be due in this hour. Our patients are with us long term, and develop strong and trusting relationships.
9.00
07:30 We check the lab test results of blood samples that have been taken from a patient by the night duty RNs via a central venous catheter. An order is made for any blood products required for the day. Communicating with fellow team members is pivotal in my role and I ensure the Clinical Nurse Manager receives a copy of my handover sheet and the blood test results.
8.00
07.00
06.00
06:45 I arrive on the ward usually as the in-charge nurse to prepare for a 12-hour shift, debrief with night staff and review material about patient load allocation for my shift. A registered nurse (RN) and I carry out the standard operating protocol for implementing bedside handover in nursing.
13:00 At every hour there will be IV medication, chemotherapy checks, analgesia checks or observations. I have lunch and catch up on paperwork.