




































































Editorial 4
Lloyd Fisher, MD
President’s Message 5
Giles Whalen, MD
“A Partnership Can Solve Anything”- School Health Collaboration in Worcester During the Pandemic 6
Beverly Nazarian, MD
Mental Health Effects of the Pandemic on Adolescents in a Public School Setting 9
Christina A. Arpin, CAGS, LMHC
Pediatric Mental Health Through the Pandemic: A Path Forward 11
Michelle Dalal, MD
Pediatric Mental Health in the Wake of COVID-19: Identifying Solutions 13
Sonia Nagy Chimienti, MD FIDSA
On the Appalachian Trail with Dr. Tammaro: One Physician’s Action to Support the Mental Health Needs of Children and Youth 16
Sonia Nagy Chimienti, MDFIDSA
Physician as Human 17
Sarah J. Palmer, MD
PUBLISHED BY Worcester District Medical Society
321 Main Street, Worcester, MA 01608 wdms.org | mwright@wdms.org | 508-753-1579
WDMS OFFICERS
President Giles Whalen, MD
Vice President Alwyn Rapose, MD
Secretary Michelle Hadley, DO
Treasurer B. Dale Magee, MD
WDMS ADMINISTRATION
Martha Wright, MBA, Executive Director
Melissa Boucher, Administrative Assistant
Empowering Worcester Youth to Support COVID-19 Vaccination: #PostVaxLife, A Public Health Media Campaign 18
Stephenie C. Lemon, PhD Matilde “Mattie” Castiel, MD
UMass Chan Student Group “Virtual Buddies” and Its Longitudinal Mentorship for Struggling Youths
During the COVID-19 Pandemic 20
Rohit Das, BS / Thomas Drews, BS / Christian Keenan, MSE / Calvin Schaffer, BS / Fiona Splaine, BS — medical students at UMass Chan Medical School
A Pandemic’s Role on Vaccine Hesitancy in the Pediatric Population 22 Chrystina Manero, PhD, RN, CPNP-PC
Legal Consult
When is Negligence a Crime? – The Radonda Vaught Case 23
Peter Martin, Esq. Jon Barooshian, Esq.
From the Curator Perspectives From the Introduction of the Polio Vaccine 25
B. Dale Magee, MD, Curator
Society Snippets
Health Matters / WDMS Legislative Breakfast 26
WDMS Open House & Pre-Concert Reception 27
Melissa Boucher
WDMS EDITORIAL BOARD
Lisa Beittel, MBA
Sonia Chimienti, MD
Anthony L. Esposito, MD
Loyd Fisher, MD, Guest Editor
Rebecca Kowaloff, DO
Heidi Leftwich, DO
Anna Morin, PharmD
Nancy Morris, PhD, ANP
Alex Newbury, MD, Resident Representative
Thoru Pederson, PhD
Joel Popkin, MD
Alwyn Rapose, MD
Parul Sarwal, MD
Robert Sorrenti, MD
Ram Upadhyay, MD
Peter Zacharia, MD
PRODUCED BY Studio DiBella
Guiding Channels
THANK YOU TO
The Reliant Medical Group
UMass Memorial Health Care
Music Worcester
Physicians Insurance
Carr Financial
ADVERTISING
Inquiries to Martha Wright mwright@wdms.org
508-753-1579
any contributor. Statements or opinions expressed in Worcester Medicine reflect the views of the author(s) and not the official policy of the Worcester District Medical Society unless so stated. Although all advertising material is expected to conform to ethical standards, acceptance does not imply endorsement by Worcester Medicine unless stated. Material printed in Worcester Medicine is covered by copyright. No copyright is claimed to any work of the U.S. government. No part of this publication may be reproduced or transmitted in any form without written permission. For information on subscriptions, permissions, reprints and other services contact the Worcester District Medical Society.

The COVID-19 pan D em IC has been a trage D y f O r our world, our country, and our communities. The lasting impact of the pandemic will go far beyond the direct effects of the virus itself. We are fortunate that the virus has not caused a significant amount of severe disease, hospitalizations, or death in children. However, children have been asked to make many sacrifices over the past two years, mostly to ensure the safety and well-being of the adults in their lives and in the broader community. It is quite clear that the lack of in-person education, extracurricular activities, ability to socialize in typical ways, and overall disruption in their routines has led to an unprecedented rise in mental health problems among children and adolescents. We keep hearing that “children are resilient,” “they will bounce back and be fine,” and “they will adapt.” While for some this may be true, the toll that it takes and the potential long-term negative effects it has on the way they view the world and their place in it will be seen for many years to come.
The nature of much of the discourse surrounding all COVID-19 related policies, especially as they impact schools,
has provided yet another source of stress, anxiety, and trauma to our children. It has made it nearly impossible for parents to truly understand how best to manage the various risks of the virus itself and the mitigation efforts which have been necessary to lessen its impact. The messaging that our patients and their families have received has been confusing, contradictory, and unfortunately influenced by politics more than medical facts. This has made many policy decisions unnecessarily controversial.
This generation will likely be defined by the events of the past several years. Now that we are in a different phase of our fight against COVID-19, we must do what we can to heal, and our priority must be on this generation which has had so much of their young lives disrupted.
In this issue we explore the various aspects of the impact of the pandemic on our youth. There are multiple articles looking into how our children’s and adolescents’ mental health has been negatively affected. In an article by Christina Arpin, a licensed social worker and school adjustment counselor, we hear of her experiences in working in the school environment and the numerous challenges that school personnel have endured as they navigate the daily changes and challenges. Dr. Sarah Palmer, a child and adolescent psychiatry fellow, shares
her personal story of how her own health scare has impacted her training and the way she views her role in her patients’ lives. Dr. Michele Dalal, a primary care pediatrician, illustrates how the increase in mental health issues among children and adolescents grew significantly over the past two years. She explains the importance of using multiple resources and tactics to address each patient and their family’s unique needs and shares some concrete resources to address them.
A silver lining for many of us has been the ability to forge new professional relationships as a direct result of the pandemic. For me personally, participating in a multidisciplinary group consisting of school nurses, counselors, and administrators from the Worcester Public Schools (WPS) — who met on a regular basis with pediatricians in the area — was a rewarding experience. In her article, Dr. Beverly Nazarian explains how our coalition came together, what we accomplished, and how we hope to continue the collaboration in a post-pandemic world to address shared concerns and solutions that go far beyond COVID-19. A group of medical students from the UMass Chan Medical School tell their story of the unique collaboration and partnership they formed with the WPS as they set up a “Virtual Buddy” program to pair medical, nursing, and graduate students with WPS children who were struggling during the time of lockdowns and remote learning. These pairings were beneficial both to the mentee and the mentor, and some of the relationships have continued and adapted to an in-person connection.
Our Medical Society curator, Dr. Dale Magee, presents a fascinating piece of history from the archives of Worcester Medical News from the early days of the polio vaccination campaign. While we have made significant advances in vaccinology science, human nature has remained much the same. The challenges and controversies of mass vaccination efforts from them mirror what we are experiencing today. Chrystina Manero, a pediatric nurse practitioner and educator, discusses the challenges we all face with vaccine hesitance and misinformation surrounding the COVID-19 vaccination efforts and what efforts we can all take to build back public trust and confidence in vaccinations. The UMass Worcester Prevention Research Center and the Worcester Office of Health and Human Services detail the innovative program they developed, led by youths for youths, to encourage vaccination among their peers.
We have all struggled to provide the care our patients needed and continue to need during the pandemic. The rate of burnout is unprecedented which further worsens the difficulties we all face. As we move into a different phase of the ongoing efforts to control this ever changing and surprising virus, we need to consider the unique hardships that our youngest members of society have faced and the losses that they have endured. The decisions we make now and the actions we take will influence this generation for years to come. Physicians need to partner with other medical professionals as well as teachers, educational leaders, social workers, and parents to ensure we always have their needs first and foremost in our minds. +
Lloyd Fisher, MD Pediatrician and Assoc. Medical Director for Informatics, Reliant Medical Group Assistant Professor of Pediatrics, UMass Chan Medical School Immediate Past President, Mass. Chapter of the American Academy of Pediatrics Giles Whalen, MD President, WDMS
Dear COlleagues,
We are blessed that the scourge of COVID has abated – at least, the more life-threatening infectious aspects of that scourge. However, here in Worcester, and across the Commonwealth, a mental health crisis — particularly in children and adolescents — has accelerated as part of the fallout of this pandemic. The reasons for it are many, but the human consequences are appalling, and effective solutions are not so obvious or not so immediately at hand. Worcester District Medical Society has addressed the urgency of this problem at our legislative breakfast this spring with our state representatives and senators, and is committed to working with all parties to find solutions which can be practically brought to bear in as timely a fashion as possible. This particular issue of Worcester Medicine, which is so ably curated and edited by Dr. Lloyd Fisher, suggests that many solutions may well lie outside the realm of clinical medicine, away from hospital beds, emergency rooms, and medications. It admirably addresses some of the ways that we might think anew to ease this problem. In our medical world, summer is the time of new beginnings: new students, new residents, and new graduates. Everyone moves up eager for the challenges of a new start. We are grateful for this new start Dr. Fischer has provided us here, and confident in the wisdom of our concerned community who want to address this problem. Have a great summer. You may expect to hear more about what we are doing in this arena. +

June 2020: three mOnths IntO the COVID-19 shutdown. Worcester Public Schools (WPS) were fully remote. The district had worked hard to equip students with laptops and Wi-Fi hot spots so they could access learning, but there were challenges. As the school year ended, those of us involved with school health were already starting to plan for school return in the fall. Around this time, the American Academy of Pediatrics (AAP) released interim guidance recommending return to school with in-person learning. Unfortunately, this release coincided with COVID-19 starting to surge in other parts of the nation as well as with fear and misinformation starting to spread in the news and social media.
As medical professionals we recognized that, although we too were learning about COVID-19, our district would require up-to-date accurate medical information to be able to make informed decisions about school reopening. With this in mind, a group of us reached out to Superintendent Maureen Binienda, offering to be a resource to the district for COVID-19 reentry planning. Shortly after, we convened the first meeting of the “Worcester Public School (WPS) Reentry Pediatrician Q & A group.” Participants included the superintendent and members of her team, the WPS nursing director and nurse leaders, and our physician group including the medical director of Worcester Department of Public Health (DPH), the WPS school physician, the president of the Massachusetts Chapter of the American Academy of Pediatrics (MCAAP), a pediatric infectious disease specialist and additional primary care pediatricians.
Our weekly virtual meetings initially focused on what we physicians were seeing in our clinics and hospitals, and fielding questions about masking, testing, or social distancing. As we began to understand each other’s perspectives and to develop trust, what started as a physician Q & A evolved into a true collaboration where we shared updates and solved problems together. Over time, our group expanded to include other key partners such as the WPS manager of social emotional learning and representatives from school-based health centers.
The pediatricians in our group were advocates for return to school and in-person learning. We shared concerns about the impact of remote learning on our patients: rising obesity, worsening sleep issues, increasing anxiety, depression, and eating disorders. We described challenges for families: lack of daycare
meant that single parents had to leave kids at home with remote learning supervised by older school-aged siblings or by grandparents struggling to navigate technology. Inadequate housing meant multiple children had to log on and learn remotely in the same crowded room.
As much as everyone wanted students back in school, our WPS partners taught us why this wasn’t simple. We learned from them about barriers to reopening, many of which were unique to large urban districts.
One barrier was transportation. Distancing requirements dictated that each school bus could transport only a fraction of the usual number of students. Existing buses already made multiple runs, and there were no extra buses, nor were there additional bus drivers. Unlike districts with more resources, many WPS families didn’t have cars or the option of driving their children to school. There was simply no way to transport all the students.
With small classrooms and a plan for six-foot distancing, only limited numbers of students could be allowed in each classroom. Older, poorly ventilated buildings proved another barrier that delayed reopening. While some Worcester schools were newer, larger, or better ventilated, WPS didn’t have the option of opening schools for some students and not others.
Nationally, urban school districts like Worcester were more likely to be fully remote than suburban or rural districts, and to have more students living in poverty. Urban districts also often have greater numbers of English language learners and students receiving special education services. These students with the highest needs often had greater difficulty learning remotely, amplifying existing disparities.
Although our district had unique challenges, WPS nurses, staff, and administration worked creatively to address them and to meet the needs of students, families, and the community.
Dr. Debra McGovern, WPS Nursing Director, shared that when buildings closed, school nurses adapted to serve the community. Early in the shutdown, they depleted their nursing offices and donated medical equipment, PPE, and cleaning supplies to shelters and the DCU field hospital. Many became contact tracing experts or staffed the afterhours COVID-19 call line, while others worked in temporary shelters set up in schools.
School nurses also worked at WPS food drop off sites, and created hygiene packs and toiletry bags for students, often
purchasing supplies on their own. They ran flu vaccine clinics and later COVID-19 vaccine clinics at every school. They set up Google classrooms instead of nursing offices, and proactively reached out to students with chronic health issues.
To keep families updated, WPS administration hosted multiple online public forums to share information and answer questions from parents and students. WPS also created technology cafes to help families troubleshoot computer issues. All WPS students received pandemic EBT cards, improving food access for families dependent on school meals. In collaboration with the Family Health Center of Worcester, WPS offered access to COVID19 testing at school for symptomatic children and staff. Concerned about student mental health, WPS implemented daily socio-emotional check-ins. If a student didn’t respond, school adjustment counselors would reach out, or even visit the home.
the Value Of COllabOratIOn:
Our collaboration allowed groups that hadn’t worked closely together in the past to learn from each other. It particularly strengthened the relationship between school nursing and educational leadership. Having everyone at the table allowed nurses to be proactive with issues rather than reactive. One nurse leader described our meetings as, “The best way to get the info dispersed and the easiest way to get it resolved. We were able to get answers and solutions very quickly compared to where we would have been without this.” This proved especially important at a time with a rapid influx of new information regarding the pandemic, as well as frequent updates to DESE and DPH guidelines.
All participants gained an appreciation for the perspectives and challenges of others that they wouldn’t have had otherwise: “.... once we collaborated, we could see what their constraints were, they could see what our constraints were, and we were able to readily fix a lot.”
Almost two years have passed since our first meeting and our group continues to meet once to twice monthly. Reflecting on our success, Superintendent Binienda noted, “A partnership can solve anything. I would never have imagined that all of us would have been together on one committee working on public health and school safety. It is a model that we shouldn’t let go of.... because we know that there is nothing stronger than working with public health and school systems to make sure that everyone stays healthy. It’s key.”
Our collaboration has been a silver lining amid the COVID-19 pandemic, and we hope it will continue. While COVID-19 is not gone, we have vaccines and a lot more knowledge. WPS students have been back in school all year and are making gains. Going forward we’d like to build upon the relationships we have created, shifting our focus from COVID-19 to other priorities such the mental health of our students, and the need to address disparities and improve child health equity in our community.
Special thanks to Maureen Binienda, Dr. Debra McGovern, Kate Perry, MSN, RN, Nicole Kazarian, MSN, RN, and Drs. Lloyd Fisher, Christina Hermos, Mary Beth Miotto, Lynda Young, and Mike Hirsh, and to all the participants in our WPS Reentry Group! +
Beverly Nazarian, MD Associate Professor, Department of Pediatrics, UMass Chan Medical School School Physician Consultant, Worcester Public Schools Beverly.nazarian@umassmemorial.org“A Partnership Can Solve Anything”School Health Collaboration in Worcester During the Covid-19 Pandemic Continued
“
.... because we know that there is nothing stronger than working with public health and school systems to make sure that everyone stays healthy. It’s key. ”


It Was the begInnIng Of the sChOOl year In september 2021, and staff already felt as depleted as we would normally experience in June. We were concerned about the students’ academic gaps from the online-learning of the previous year, as well as their overall emotional well-being. The grief, anxiety and depression that the teens experienced during the pandemic have overflowed into the classes and hallways resulting in an increase in conflicts and physical fighting. School provides structure and routine to the lives of students. Expectations for behavior and performance are familiar and understood. When schools closed, students lost that making it more difficult to adjust when they returned full time. This also took an emotional toll on teachers, counselors, nurses and administrators.
Some students need help readjusting to regular classroom routines or tasks such as taking notes, raising their hand to answer questions and remaining in school the whole day. On-line schooling afforded the option to remain in their bedrooms with the camera off still in their pajamas and playing video games or pointing their computers at the ceiling. Teachers corroborated this, saying they observed many ceiling fans as they tried to sustain their students’ attention. Some of the students reported that they hadn’t showered in days. Their reasoning was, “I can’t go anywhere so why bother?” Students who were already struggling with alcohol use and/or marijuana/cigarette use reported that their usage increased during this time. Since returning to in-person learning, a minority of students are having a difficult time completing the school day, and questioned how they ever managed to stay all day prior to the pandemic.
After over a year at home, returning to school was not like a normal year. Staff learned quickly that we couldn’t expect adolescents to adjust to this new normal quickly. They faced many challenges due to ongoing health issues, economics, social and psychological consequences of the pandemic. Households with younger children have been particularly impacted by loss of income and /or food, as well as housing insecurity. Many of our students picked up part-time jobs to contribute to the household income or babysat for their younger siblings while trying to maintain their academics. After being isolated from their peers and away from the consistent structure and routine of school, students appeared more anxious, overwhelmed, irritable and easily fatigued. Increased anxiety also presents in youth with school refusal, tardiness, difficulties with transitions and change, fears of ill-
ness for themselves and their families, somatic complaint symptoms (i.e. headaches and stomach aches), panic attacks, avoidance, obsessions and compulsions, self-harm, eating disorders, substance use, fatigue and lack of concentration (1). Instances of aggression and bullying have also increased. In this regard, personally, I have completed more risk assessments (self-harm, suicidal screenings, and threats to harm others), filed more 51A abuse/neglect reports with DCF (Department of Children and Families), and sent more students out for formal risk assessments that resulted in hospitalizations than in any other year in my 32 year career in mental health (including residential, in-home therapy, outpatient counseling and years of school counseling). My counterparts in the Southern Worcester County and Central Western areas report similar concerns.
This year, a substantial increase in counseling referrals came from parents who informed me that the outpatient counseling agencies have a 6 to 8 month wait period, where prior to the pandemic it was only a couple of weeks. School counselors, psychologists and nurses saw their caseloads and responsibilities increase significantly. Although Telehealth services for counseling were offered, most of our students chose to “pause” their outpatient counseling until they could meet with their therapist in person. “Shortly after the pandemic began more than 25% of high-school students reported worsened emotional health. . . . Private insurance data shows that mental health claims for adolescents increased sharply in 2020” (2). Adjustment Counselors are now tasked with trying to fill in the gaps in the mental health system. Many students have had to wait weeks for beds to open up in treatment facilities. I learned that most of my students that I referred for formal risk assessments waited weeks in emergency rooms and hallways for an opening as distressed parents wondered if it was worth the risk as their child was surrounded by physically ill Covid-19 and other mental health patients in crisis.
When the students returned with the Covid-19 protocols, the atmosphere in school was very different. They sat socially distanced, 6 feet apart wearing masks. It was eerily quiet and solemn like a funeral service for the first several weeks. There was no laughter in the halls, very little joking amongst the students or goofing off in their classrooms. Teachers remarked about how quiet their classes were. Our ability to understand and read nonverbal cues was reduced significantly because of the masks. They made it difficult to interpret nuances and
lead to miscommunication and misunderstanding. Once the mask mandate lifted and the majority of the students removed their masks, the hustle and bustle, laughter and the noise to which we had been accustomed returned. Teachers also noticed more students glued to their phones, wearing their earbuds constantly and appearing to be more focused on technology than pre-pandemic.
More students remarked to me that they are so tired that afterschool they take a nap for a couple of hours, go to bed by 9:00 p.m. and are still tired the next day. Many of them took naps during virtual schooling. Special needs students were particularly negatively impacted by on-line learning because in-person classrooms allow for teachers to provide more personal attention to each student’s individual needs.
Schools across the country report an increase in anxiety and disruptive behaviors. We are experiencing more verbal, physical and cyber fights following the pandemic (3). Anxiety and stress can trigger a teens “survival brain” turning a look or nudge in the hallway into a physical altercation, causing students to overreact to small issues. The APA reported the most frequently diagnosed mental health conditions in 2020 were depression, anxiety, and adjustment disorder. According to the Centers for Disease Control and Prevention, Emergency Department visits for suspected suicide attempts among adolescents jumped 31% in 2020, compared with 2019. In February and March of 2022, emergency department visits for suspected suicide attempts were 51% higher among girls aged 12-17 than during the same period in 2019 (4). “Girls and boys had similar rates of negative changes in their sleep (24% for girls vs. 21% for boys), withdrawing from family (14% vs. 13%) and aggressive behavior (8% vs. 9%) (5).
Even with the heroic efforts by teachers the continuing ongoing challenges are profound. One teacher remarked to me, “it is like having one foot in one boat (pre-Covid-19) and your other foot in another boat (post Covid-19).” They are feeling stretched and unbalanced on all sides with pressure from parents, administrators, the school community and the State. Teachers are struggling while adapting their curriculum and lesson plans back to in-person teaching.
The pandemic may subside, but its mental health effects will long linger. Although adolescence is a time of great resiliency, the pandemic has shown us that we need to do a better job teaching our students at a young age how to self-soothe, by using positive coping skills, regulating their emotions, resolving conflict, delaying gratification, and self-advocating techniques that will prepare them for future challenges that are bound to arise. Even though this has been the most stressful and exhausting year of my career, I still embrace my calling as a mental health clinician and helper to whoever may need it. +
Christina A. Arpin is a Certified School Adjustment Counselor (CAGS) and Licensed Mental Health Clinician (LMHC). She has worked at Quaboag Regional Middle-High School in Warren, MA for 24 years and has provided outpatient counseling in a community-based setting both full and part time for 15 years. The observations and views expressed are those of the author and are not intended to reflect nor express the opinions of any specific educational entity. Email: carpin@quaboagrsd.org
1. APA (2020) Stress in America, 2020 A National Mental Health Crisis. Available at https://www.a-yo.orgnews/press/ releases/stress/2020/report .
2. Fairhealth.org, The Impact of COVID-19 on Pediatric Mental Health, March 2, 2021.
3. Violence Against Educators and School Personnel: Crisis During COVID, APA-Task Force, 2022.
4. CDC, Morbidity and Mortality Weekly report, June 18, 2021/7024, 888-894.
5. Mott Children’s Hospital National Poll on Children’s health at Michigan medicine. Source-University of Michigan, News release, March 15, 2021.
“
Although adolescence is a time of great resiliency, the pandemic has shown us that we need to do a better job teaching our students at a young age how to selfsoothe . . . ”

ThrOugh thIs panDemIC, there Were sO many DIsruptions to the normal routines of daily life that it became difficult to know what to expect, leading to worries and anxiety for kids and their families. Feelings of hopelessness and sadness grew, especially amongst teens, while thoughts of suicide and actual suicide attempts rose slightly from pre-pandemic times. The mental health crisis had been present before the pandemic, but through the pandemic, certain populations have experienced significantly increased mental health needs such as LGBTQ youth, youth in poverty, racial and ethnic minority youth, and youth whose families had been affected by COVID.
The combination of worries, sadness, and trauma led to increased mental health concerns that inundated emergency departments, primary care offices, and mental health clinics, and overwhelmed the existing medical system. A mental health emergency was declared with the hopes of funneling more resources to the mental health crisis — but as with any crisis, stresses grew as people began to find it difficult to access therapists and psychiatrists to meet the mental health needs of their kids.
Now, as we are two years into the pandemic, the focus needs to be redirected on the path forward. As outlined in the Surgeon General Report, Protecting Youth Mental Health (1), there are many factors which shape youth mental health including individual, family, community, environmental, and societal factors. We have an opportunity to influence each of these factors to help alleviate the mental health crisis and it starts by what we can do day to day.
First and foremost, we must listen nonjudgmentally to kids and spend time with them to understand their concerns. Studies show the presence of one stable, caring supportive relationship can change the trajectory of a child’s life (2). We can also offer training to individuals to enable them to help someone who is experiencing worsening sadness or anxiety or who is in crisis. Training for non-medical personnel can be considered through programs such as the Youth Mental Health First Aid by the National Council for Mental Wellbeing.
In the clinical setting, mental health concerns can be addressed quickly and expediently by all who provide care, from front staff and nurses to providers and behavioral health clinicians. We can ensure behavioral health screenings — such as the PSC-17, Y-PSC-17, PHQ-9, or GAD-7 — are being completed at each well child visit and, when a screen is elevated, that a comprehensive interview is completed. The United
States Preventative Services Task Force recommends screening for depression for all kids ages 12 to 18 (3) and will soon be recommending anxiety screening for kids ages 8 to 18.
Following screenings and subsequent interviews, urgent or non-urgent collaborative action plans can be developed with the families. Massachusetts has the benefit of crisis intervention teams that can be accessed if needed. If suicidal ideation is present and safety plans cannot be created, then children and teens should be sent to emergency departments for emergent evaluations. If acute needs are not present, families should be informed about the diagnosis and treatment plans. These treatment plans could include a wide range of interventions, from lifestyle interventions — like improved sleep, healthy eating, increased physical activity, stress management, avoiding risky substances like marijuana, nicotine, and alcohol, and increasing social connections — to psychotherapy and medications. The plans should also include routine follow up by behavioral therapists or primary care providers to ensure continuity of care and follow-up for progression or worsening of symptoms. Behavioral therapists can be accessed within clinics, in the community or online.
Kids and their families need the reassurance that they have a team working with them to help them through any mental health challenges. This can include teachers, counselors, family members, primary care providers, and others who are stakeholders in their well-being. Working collaboratively and individualizing treatment plans can be very effective in mental health care.
“
The mental health of kids is intricately linked to everything that occurs around them.
It takes knowledge, skill, and time to deal with mental health issues: Time is needed to talk to patients, understand concerns, make diagnoses, coordinate care, and ensure appropriate follow-up. As clinicians, we need support to ensure we can provide the best mental health care by encouraging behavioral health integration at every level and access to urgent services through programs such as the Massachusetts Children Psychiatry Access Program (MCPAP) when practices do not have resources to fully integrate behavioral health providers. Health systems need to change to allow adequate time to see patients and reimbursement for mental health visits.
Lastly, we need to advocate for our patients outside the clinical setting so that we influence the environmental and societal factors which affect youth mental health. The mental health of kids is intricately linked to everything that occurs around them. We must continue to advocate for policies such as longer recess times, longer lunch times, later school start times, access to in school counselors, and so much more.
Because mental health is a part of overall health and wellness, policies which ensure good physical health are the exact same ones that will continue to boost mental health for kids and families alike. Every small step we can take to address, approach, and advocate for improved mental health for our youth can lead to improved quality of life and reduced mental health issues as an adult. All of us can do our part to improve mental health for youth each and every day. +
Michelle Dalal, MD, Medical Director of University Health Services, Northeastern UniversityHELPFUL RESOURCES:
National Suicide Prevention Line: 1-800-273 8255
Mass Health Crisis Intervention Services
(Patients with any Insurance can Access): 1-877-382-1609
HELPFUL WEBSITES:
Massachusetts Child Psychiatry Access Program- MCPAP: https://www.mcpap.com/
Youth Mental Health First Aid: https://www.mentalhealthfirstaid.org/population-focused-modules/youth/
1. Office of the Surgeon General (OSG). Protecting Youth Mental Health: The U.S. Surgeon General’s Advisory Washington (DC): US Department of Health and Human Services; 2021.
2. National Scientific Council on the Developing Child. (2015). Supportive Relationships and Active Skill-Building Strengthen the Foundations of Resilience: Working Paper 13. http://www.developingchild.harvard.edu
3. Albert L. Siu, , on behalf of the U.S. Preventive Services Task Force , et al; on behalf of the U.S. Preventive Services Task Force .. Screening for Depression in Children and Adolescents: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med.2016;164:360-366.
“
Every small step we can take to address, approach, and advocate for improved mental health for our youth can lead to improved quality of life and reduced mental health issues as an adult. ”

On January 1, 2022, the amerICan psyChOlOgICal Association (APA) Monitor on Psychology published its 2022 Trends Report, an outstanding 14-part report on emerging trends in mental health (1). One of the trends included was “Children’s mental health is in crisis”. This comprehensive report noted that two years into the COVID-19 pandemic, demand for mental health services amongst children and adolescents had reached “all-time highs”. Pre-pandemic data from the Centers for Disease Control (CDC) (2) indicated that almost 1 in 5 children suffered from a mental, emotional, or behavioral disorder, with only 20% receiving care for their mental health condition. Data collected in the period 2013-2019 (3) indicated that 20.9% of adolescents aged 12-17 had experienced a major depressive episode, and in 2018 and 2019, approximately 7 of 100,000 children aged 10-19 years died by suicide. The APA trends report cited a 2020 national survey coordinated by Children’s Hospital of Chicago (4) that queried 1,000 US parents about the impact of the pandemic on the mental health and well-being of their children. Seventy-one percent of the respondents indicated that the pandemic has impacted the mental health of their child, and 69% stated that the pandemic was the worst thing that had happened to their child. Data published in Morbidity and Mortality Weekly Report (MMWR) in 2020 indicated that mental health emergency department visits between March and October 2020 rose by 24% for children aged 5-11, and 31% for those aged 12-17, in comparison with data from 2019 (5). Since 2000, there has been a 4.5-fold increase in death by suicide due to ingestion in children aged 10-12 (6).
In September 2021, Dr. Arthur C. Evans, Jr., Chief Executive Officer of the APA, testified before the U.S. House of Representatives on this issue. His comprehensive written testimony, “Putting kids first: addressing COVID-19’s impact on children” (7), provided a compelling and sobering overview of the current state of mental health in our children, and highlighted ways in which we can act to help mitigate the long-term negative impact of the pandemic on the mental well-being of youth and young adults. Dr. Evans’ testimony indicated that a strategic, population health-based preventative approach would be critical to supporting children and their behavioral health needs now and beyond the pandemic. Moving away from traditional acute-care models and investing in resources that meet children where they – and their caregivers - work and play, can be effective and impactful. Specifically, increasing available mental health services in schools and in community health centers can improve access, focus on prevention rather
than crisis management, and may help to prevent some acute decompensations. Inpatient services are currently not sufficient to meet the needs of children with mental health crises; many children wait for days if not weeks in emergency departments and on inpatient wards, awaiting the specialty care that they need.
Notably, Dr. Evans emphasized the importance of schoolbased mental health services, which have long been critical resources for children experiencing distress in school settings. The disruption of daily routines as a result of COVID-19-related hybrid and remote learning has disconnected children from trusted school-based resources. This has in turn deepened the profound negative impact of the pandemic on the mental health of this vulnerable population. Staffing of school psychologists is currently insufficient to meet the increased needs resulting from the pandemic. Specifically, Dr. Evans cites data indicate that school psychologists currently serve three times the number of recommended students. Numbers of providers from other specialties who might offset the need, including counselors and social workers, are also in short supply.
Children have struggled to learn and develop on a personal and social level during this period of distancing and isolation; some may have been grappling with the loss of loved ones and navigating grief and personal trauma experienced as a result of the COVID-19 pandemic. Time away from school and structured social activities may have led to increased time spent on social media, which could have in turn exacerbated feelings of isolation, stress, and anxiety and contributed to behavioral issues. Untreated, persistent mental health challenges in children could impact success in academics and completion of educational requirements. In the long term, we may witness profound impacts on employment and socioeconomic stability due to the dual pandemics of COVID-19 and mental health.
Looking forward, and focusing on how we can intervene, Dr. Evans’ testimony advocated for the Increasing Access to Mental Health in Schools Act (H.R.3572), supporting the development of partnerships between institutions of higher education and local agencies, thereby increasing the numbers of mental health professionals in school settings. He also highlighted the Mental Health Professionals Workforce Shortage Loan Repayment Act, (H.R. 3150) authorizing a student loan repayment program to help boost numbers of mental and behavioral health professionals choosing to work in schools and in Community Health Centers. An additional potentially effective program referenced in this testimony is the Com-
additional resource for vulnerable children. Examples referenced include Yale’s RULER program (8) and Mental Health Primers (9), both of which provide curricula for educators, to cultivate emotional intelligence, recognize the warning signs of mental health crises, and help educators identify stressors and navigate the presence of anxiety and uncertainty in the classroom. Ultimately, the goals of these and similar initiatives are to decrease burnout in the K-12 setting, to support children and educators, and to potentially prevent escalation of classroom-based stress and anxiety.
Now, more than ever, in the wake of the COVID-19 pandemic, resources to support our teachers in their support of children is critical. Through the advocacy of organizations committed to the mental well-being of our children, through education and communication to break down barriers and stigma, and through the collaborative support of educators, families, and all healthcare providers, we can ensure that our children will emerge from this pandemic with the resources and support that show them that we care, and that we are invested in their long-term health and well-being, despite these profound challenges. +
Dr. Sonia Chimienti is Senior Associate Dean for Medical Education at the Geisel School of Medicine at Dartmouth, and former Vice Provost for Student Life at the TH Chan School of Medicine at the University of Massachusetts Medical School.
prehensive Mental Health in Schools Pilot Program Act (H.R. 3549). This initiative will seek to positively impact student well-being in poorly resourced schools by investing in a holistic approach to mental health programs, train ing school-based staff and educators to better support students through emotional intelligence training and trauma-informed support.
The APA 2022 Trends Report similarly highlights a variety of ways in which psychologists are working to address this crisis by focusing on schools and communities; advocating for increased school-based mental health resources, training educators to recognize crisis and trauma in children, and promoting resilience training in K-12 educators. The American Rescue Plan Act, which was passed in March 2021, provides $170 billion in school funding, which can be utilized to increase mental health services and staffing in school settings, focusing on prevention in addition to treatment. The APA 2022 Trends report highlighted a number of training programs and formal curricula in mental health that can be provided for school-based staff, to help educators build skills and serve as an
1. Abramson A, 2022 Trends Report, “Children’s mental health is in crisis”, https://www.apa.org/monitor/2022/ 01/special-childrens-mental–health#:~:text=In a 2020 survey of,to happen to their child. Accessed June 5, 2022.
2. https://www.cdc.gov/childrensmentalhealth/access.html (updated 4/27/22, accessed 6/5/22)
3. Bitsko RH, Claussen AH, Lichtstein J, et al. Surveillance of Children’s Mental Health – United States, 2013 – 2019 MMWR, 2022 / 71(Suppl-2);1–42. https://www.cdc.gov/ mmwr/volumes/71/su/su7102a1.htm
4. https://www.luriechildrens.org/en/blog/childrens-mental-health-pandemic-statistics/
5. Leeb, R. T., et al., Morbidity and Mortality Weekly Report, Vol. 69, No. 45, 2020
6. https://www.usnews.com/news/health-news/articles/ 2022-03-15/suicide-rate-is-spiking-upwards-inpreadolescent-children
7. https://www.apa.org/news/press/releases/2021/09/ covid-19-children-testimony.pdf
8. https://ycei.org/ruler
9. https://www.apa.org/ed/schools/primer
Untreated, persistent mental health challenges in children could impact success in academics and completion of educational requirements.
In the long term, we may witness profound impacts on employment and socioeconomic stability .


In th I s I ssue O f the W O r C ester D I str IC t m e DIC al Society magazine, we bring attention to the profound negative impact of the COVID-19 pandemic on the mental health of children across our nation. Amidst the sobering data presented in this issue, it is easy to despair and wonder what one person can do to combat such a significant challenge. Those of us who are not directly involved in caring for children with mental health issues feel the urgency of the situation and may wish to help. Fortunately, there is a great deal that we can do. Building awareness of mental health challenges and needs, reducing stigma through conversations and education, and advocating for resources are just a few ways in which we can contribute, regardless of our primary areas of professional focus. I recently caught up with one New England physician who is doing what he can to try to raise awareness regarding the mental health needs of children in crisis.
Dr. Dominick Tammaro, a colleague and adult medicine physician is hiking the Appalachian Trail (AT) this summer to raise awareness and funding for pediatric mental health care. As a physician and educator, Dr. Tammaro has been aware, as many of us have, of the toll that the pandemic has taken on our children and youth. Dr. Tammaro is hiking the Appalachian Trail to raise awareness of this crisis and support the work of Bradley Hospital. The first children’s psychiatric hospital in the United States, Bradley Hospital opened in 1931 through the bequest of George and Helen Bradley, whose daughter Emma who suffered from complications of encephalitis at the age of 7. The Bradley Hospital provides a variety of mental health services for children not only in New England, but nationally and internationally. It also invests in advocacy and training for members of the community. I had the opportunity to ask Dr. Tammaro about his motivation to hike the AT and to share why pediatric mental health rose to his awareness.
SNC: Dr. Tammaro, why were you compelled to raise funds for and bring awareness to this particular problem?
DT: I think that there are many areas where people are especially vulnerable, especially after two years of uncertainty, social isolation, health concerns and disruption of the social safety net. I have seen an increase in patients admitted to hospital with mental health problems as well as medical conditions complicated by the co-existence of psychiatric comorbidities. This has been front and center in my work and that of my colleagues so, when I undertook planning for my hike, I thought it a worthwhile and relevant cause.
SNC: In an ideal world, what do you hope will be an outcome from your efforts?
DT: It’s all about access in my view. That means those in need of mental health care should have the ability to (a) find and access a provider, (b) [ ensure that the provider] has the skillset and training to provide the specific post-traumatic care necessary in the current mental health crisis and (c) to do so without fear of patient stigma. That last item is a tall order based on long-standing societal prejudices, but the first two elements would make the care of individuals affected by post-COVID mental illness more effective.
SNC: Are there personal narratives or stories that your patients or friends have shared that impacted your decision to support mental health services for children?
DT: I have several friends who are involved in K-12 education as teachers, administrators, and healthcare staff. The teachers especially are uniformly observing students with high levels of anxiety and depression with the simultaneous loss of social anchors and coping skills. This is evident in classroom behaviors and loss of grade-level preparation in subject matter. Many students have lost family members or spent time with restricted contact with loved ones and are feeling disconnected from their routines and support systems. During the peak and recovery periods of the COVID pandemic, my hospital’s daily operational preparedness meetings reflected an unprecedented increase in hospitalizations of children for mental illness. In the adult wards, we likewise saw evidence of unaddressed mental health needs in young adults. I think this is a chronic issue in our country made much worse by COVID, which had major health and social impacts.
SNC: As you have made this hike on the Appalachian Trail, have you talked about this mission with people you’ve encountered, and if so, what feedback and stories have your co-hikers shared?
DT: Yes indeed. I’m not the only person utilizing a hike of this nature as a vehicle to raise awareness and funds for worthwhile causes. Several of my hiking buddies are Veterans who are raising funds to help the extraordinary rise in mental health conditions and
suicide among Veterans. Like hikers, Veterans have a close-knit community of support and recognize the mental health needs of this group. Similarly, many hike the AT at a transition point in their lives, often after some traumatic event or personal crisis. I’ve spoken to hikers who have experienced loss and personal mental health challenges who are walking through their pain and seeking restoration through nature and fellowship in the woods.
SNC: Anything else you might wish to share?
DT: Yes – my donation and YouTube pages, both listed below! Seriously, mental health conditions are often hidden just beneath the surface of our daily experiences. We should remain mindful of their existence and of the fact that many suffer in silence. Together we can assist in their proper care and recovery. +
HELPFUL RESOURCES:
My YouTube Channel (a phrase which I NEVER thought I would ever type in my life...): https://www.youtube.com/channel/UCF7PNmFf9y6a39LPYtQ3Gow
*To learn more about Bradley Hospital, please visit https://www.lifespan.org/locations/ bradley-hospital/about-bradley-hospital/ our-history.
*Dr. Tammaro’s Donation Page - Appalachian Challenge: Meeting the Mental Health Needs of Our Youth: https://giving.lifespan.org/ Bradley/appalachian-trail-fundraiser
Dr. Sonia Nagy Chimienti is Senior Associate Dean for Medical Education at the Geisel School of Medicine at Dartmouth, and former Vice Provost for Student Life at the TH Chan School of Medicine at the University of Massachusetts Medical School.
Dr. Dominick Tammaro is Vice-Chair for Education in the Department of Medicine at Rhode Island Hospital in Providence, RI. He is formerly the Internal Medicine Residency Director at the Warren Alpert Medical School at Brown University.
Tra I n I ng I n C h I l D an D a DO les C ent psychiatry has long been my goal. When it came time to construct match lists, I scrutinized curricula seeking out only programs that allowed me as much contact as possible with young people, developing personalities, the most vulnerable of our society. I had an aspirational, optimistic streak that imagined the future psychiatrist I would become. I imagined someone strong and capable, connected and sensitive, and that somehow my trajectory through fellowship would not only be one of growth but one of exponential growth in my ability to treat patients and provide relief to families.
Nothing prepared me for how training would unfold. Personal calamity, without exaggeration, landed me at 33 weeks pregnant in the Memorial ICU with sepsis due to pneumonia. It was mere months into my long-awaited entrance to child & adolescent fellowship training. I fought hard to be discharged, carefully stating my case using my degree to argue that I would know the warning signs to come back. My nurses tried to warn me: What I had been through, they said, was much more than I was acknowledging. One was even so frank as to say to me, plainly, “People come to the ICU and they die.” Apparently, I wasn’t hearing it.
I was placed on medical leave for months. The forced stillness of my body, fighting to breathe every day, sent my mind to anxious wanderings. I dared to google morbidity rates for sepsis in third trimester women. I tried to process what had happened but barely had time before my son was born. I fought to enjoy maternity leave but felt so vulnerable, so frightened, and the looming return to work was inescapable.
There’s a feature in the video game Mario Kart where, if you fall off the Rainbow Road, your character dies — but then a little angel picks it up and drops it right back where it had fallen. I had always wondered what happened at the depths of that fall, what happened to the character whose “life” was lost. This may be the anxiety that kept me from ever really enjoying video games, but this is also how I understand my return to work. The person I was before just... died... and now it is back to the races. A new version of who I am is here, rolling down Rainbow Road.
I am here, continuing on my path through child and adolescent psychiatry fellowship training in a national crisis that challenges even the most stalwart of my supervisors. As I reflect on my aspirations to become a child psychiatrist, I often feel far from being able to provide relief to families. Instead, I find myself partnering with them even more as we lament our dwindling resources, and the COVID-19 pandemic continues to take its worst out on the most vulnerable. Children suffer. I wish there were an aspirational path of exponential growth, and if it existed, I wish I were on it. At this point in training, however, I am realizing how human we all are. This work requires that we not only appreciate the humanity in our patients, but also the humanity in each other and the vulnerability that comes with that territory. +
Sarah J. Palmer, MD is a First Year Child & Adolescent Psychiatry Fellow at UMASS Chan Medical School. Email: sarahpalmer@umassmemorial.org

VaCCInatIng yOuth anD famIlIes In WOrCester fOr COVID-19 is a vital part of the public health response to the pandemic. According to the City of Worcester Division of Public Health surveillance using new census population totals (1), 33% of children 5-11 years, 62% of youth 12-15 years, and 53% of youth 16-19 years are fully vaccinated with two doses. Rates for boosters, which are now available to everyone aged 5 and up, remain sub-optimal.
Since the COVID-19 vaccines were approved, Worcester’s Office of Health and Human Services and the Division of Public Health have worked tirelessly to provide access to the vaccines through Vaccine Equity Clinics held in trusted and accessible community locations, such as the Worcester Public Library, community agencies, places of worship, and stores. The UMass Worcester Prevention Research Center (PRC), funded by the Centers for Disease Control and Prevention at UMass Chan Medical School, has partnered to support these Vaccine Equity Clinics through a public health media campaign promoting COVID-19 vaccine confidence and uptake among youth and families.
WOrCester
the
The Worcester Youth Vaccine Ambassador public health media campaign is a local initiative to promote vaccine confidence among youth and families. The campaign is guided by social cognitive theory (2) and youth empowerment (3) theories that suggest that people are influenced to change their health behavior by hearing stories and motivations of people who are influential to them. #PostVaxLife promotes vaccination through youth and families sharing personal motivations, with an emphasis on addressing racial and ethnic disparities in COVID-19 and COVID-19 vaccinations through diverse voices.
UMass Worcester PRC and Worcester’s Office of Health and Human Services facilitated the campaign, but it was led by, and for, youth. The Youth Vaccine Ambassadors were influential youth living in Worcester. The goal was to amplify the voices of our talented youth by giving them a platform to share why they got vaccinated. These motivations formed the foundation of the vaccination promotion media campaign to encourage and inspire others to get vaccinated. Together, these youth created the #PostVaxLife hashtag and logo and used them to share vaccine information on social media as a way to build vaccine con-
fidence in the city of Worcester. This hashtag, #PostVaxLife, was meaningful to the youth, highlighting their desire to get back to the things that they enjoy doing again.
There were different reasons why youth decided to get vaccinated. Isabella, one youth ambassador said, “I got vaccinated to protect my friends and family. After getting vaccinated I was able to enjoy my life better and feel safer.”
In the campaign materials, youth ambassador Jean shared, “I’m vaccinated for my mom, for my dad, for my grandmother...for myself. I love them, so I want to protect them. Protect yours.”
When asked why they got vaccinated, another one of our local youth vaccine ambassadors, Morgan, said, “I got the vaccine because my mom and little brother suffer from autoimmune diseases. I wanted to keep me and my family healthy, so far, we have been. #PostVaxLife.”
This public health campaign highlights Worcester’s goal to increase youth vaccinations by using youth as trusted messen-


“
. . . people are influenced to change their health behavior by hearing stories and motivations of people who are influential to them. ”
gers to share their own motivational stories and through those narratives and storytelling.
The campaign created video public service announcements (PSAs), posters, and fliers featuring the Youth Vaccine Ambassadors. Each public health message featured the ambassador’s story, locations to access the COVID-19 vaccine, and websites with more information. These vaccine confidence messages were shared and distributed through three social media platforms, mass media outlets (TV and radio), flyers, posters, billboards, and Worcester Regional Transit Authority bus ads. In partnership with youth-serving agencies, the Youth Vaccine Ambassadors also promoted Vaccine Equity Clinics held at trusted agencies to increase the access of the vaccine for local youth and families.
To complement the campaign materials, our team created COVID-19 vaccine fact sheets based upon questions that local families have asked, sought endorsement by local health systems, and translated them into nine languages. Materials associated with this public health campaign, including PSAs and COVID-19 vaccine fact sheets are available at the UMass Worcester Prevention Research Center website (www.umassmedmed.edu).
To evaluate the impact of participating in the campaign on youths themselves, we conducted interviews with three participants, who all reported very positive experiences. One youth ambassador said, “At the first vaccine event, nobody wanted to get the vaccine but after I shared my vaccine story and gave them my reason why, I saw at least six people get up and go to get their vaccine. Being an outlet in that way was super cool.”
When asked if they’d participate in a campaign like this again, one youth said, “Of course, for sure. I definitely would. I’m really glad I was a part of this push.”
Following the success of sharing personal vaccine stories, our team expanded the model to feature family voices. Through
a collaboration with Girls Inc. of Worcester, local families created PSAs, billboards, and bus signs, featuring their own motivations to reach a #PostVaxLife by being vaccinated with the COVID-19 vaccine. Our work is now expanding to support local pediatricians in their efforts to talk to vaccine-hesitant parents, and family vaccine ambassadors to talk with friends and family in neighborhoods with low vaccination rates. As the pandemic continues and youth vaccine rates lag, creating new strategies to integrate youth into these efforts will continue to be vital.
This work is funded by the Centers for Disease Control and Prevention and is a product of a Prevention Research Center (Agreement #6U48DP006381-03-01). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention. +
REFERENCES:
1. City of Worcester Division of Public Health. 5/27/2022. Worcester Weekly Vaccination Report.
2. Bandura A. Self-efficacy: The Exercise of Control. New York: WH Freeman and Company; 1997.
3. Zimmerman MA. Empowerment theory. In: Rappaport J, Seidman E, eds. Handbook of Community Psychology. U.S.: Springer; 2000:43-63.
Stephenie C. Lemon, PhD, is Director of the UMass Worcester Prevention Research Center, and professor and chief of Preventive and Behavioral Medicine at UMass Chan Medical School. Email: Stephenie.lemon@umassmed.edu.
Matilde “Mattie” Castiel, MD, is commissioner of Health and Human services for the City of Worcester and associate professor of medicine at UMass Chan Medical School. Email: CastielM@ worcesterma.gov.
This public health campaign highlights Worcester’s goal to increase youth vaccinations by using youth as trusted messengers to share their own motivational stories and through those narratives and storytelling.


 Rohit Das, BS, Thomas Drews, BS, Christian Keenan, MSE, Calvin Schaffer, BS, and Fiona Splaine, BS, medical students at UMass Chan Medical School
Rohit Das, BS, Thomas Drews, BS, Christian Keenan, MSE, Calvin Schaffer, BS, and Fiona Splaine, BS, medical students at UMass Chan Medical School

YOuth mental health aCrOss the unIteD states Was declining years before the pandemic even began. Persistent feelings of sadness or hopelessness increased 40% among high school students from 2009-2019, while pediatric emergency department visits for mental health disorders rose by 60% and self-harm visits by 329% between 2007-2016 (1, 2). Then the COVID-19 pandemic hit. In addition to the ongoing mental health crisis, youths were experiencing social isolation in unprecedented numbers, resulting in overwhelming situations in both the medical and school systems across the country, as well as right here in Worcester.
To address this problem, a multidisciplinary team of physicians at the University of Massachusetts Chan School of Medicine (UMass Chan) had the idea to foster a sense of connectedness and belonging through a “virtual buddy” system. “By setting up a network of our students to call the Worcester Public School (WPS) students who were struggling, we could provide support, fellowship, and kindness when COVID-19 was creating the most uncertain of times,” recounts Dr. Michael Hirsh, medical director for the Worcester Department of Public Health (DPH) and a program advisor. The initiative would match WPS students with medical, nursing, and graduate students from the UMass Chan community to form longitudinal relationships. Our UMass Chan student-led team was recruited from pre-existing mentorship volunteer groups to spearhead the Virtual Buddy initiative and do our part to help combat youth mental health challenges.
Establishing effective communication with WPS staff was crucial because they understood the intricate details and nuances of the challenges their students faced on a daily basis. “Our goal was to create an intervention that started with the schools, since the schools know the kids best,” noted Dr. Brian Skehan, child psychiatrist and early project advisor. Through Maura
Mahoney, WPS Manager of Social Emotional Learning, we were connected with Lauren Colwell, an adjustment counselor at University Park Campus school, who became our main point of contact. Together, we created a program that would best serve students struggling with isolation and mental health. With the program structure in place, we began outreach to engage the UMass student body and recruit the “mentors.” Before mentors could be paired with a buddy, they participated in a training session led by pediatrician and WPS school physician Dr. Bev Nazarian and child psychiatry fellow Dr. Arielle Graham. The aims of the training were to emphasize the need for stronger support networks in the youth population affected by COVID19, teach the mentors how to empower these students, and inform mentors of the protocols and available resources in the event of an emergency. Mentors were also encouraged to attend Youth Mental Health First Aid Workshops, led by Colwell and fellow adjustment counselor Juliamy Saraiva, which “teaches a 5-step action plan for how to help young people in both crisis and non-crisis situations.”
While every student in the WPS system may have struggled with the isolation and anxiety that the pandemic caused, some were disproportionately affected. Those students, as

“
I really love this program as it pairs you with someone that likes the things you like and gives you someone to talk about your problems with.
”
identified by their school adjustment counselors, were referred to the program. Both the mentors and WPS students filled out a form to indicate their hobbies, favorite movies/shows, and experiences. Over 25 matches were made over the one year span, some of which are still in communication today. After being matched, the pairs interacted remotely via phone calls, Zoom sessions, or multiplayer online video games. Each pairs’ activity was reported in a Google form log, which provided a description of the interaction, so that Colwell could be up to date on each pair. As time went on and distancing restrictions loosened, pairs were encouraged to meet in person, provided the students’ families were informed and agreeable.
The impact of this program can be seen in the response of the students involved. One of these students, Owen, states, “There are days when I just don’t feel like talking much and there are days when I want to, but that happens very rarely with this program. I really love this program as it pairs you with someone that likes the things you like and gives you someone to talk about your problems with.” The longitudinal relationship helps give students a safe space to express themselves while also taking a step back from the stressors that they face every day. While the program is centered around the mental health of the WPS students, it has helped the mentors as well.
One of the mentors, Thomas, states “Talking to my buddy is always a highlight of my week. Chatting about Star Wars or video games is a nice reprieve from the constant stressors of medical school.” Additionally, mentors learned how important a holistic approach is to addressing complex topics such as youth mental health; treatment and prevention start far outside the walls of a doctor’s office or hospital.
Although the program had a positive impact, there were challenges as well. Time constraints came up for some mentors, who were unable to follow through after the initial pairing. Over time, mentors and students both navigated new academic transitions, and meetings for some pairs became more infrequent, while others lost touch altogether. Additionally, there was a greater need for mentors who are non-native English speakers, but unfortunately most of the mentors were not fluent in other languages and were unable to accommodate this need. These problems will be addressed before the start of the upcoming school year.
The social deprivation that this pandemic has created is unlike anything that has been seen before and has amplified a previously growing youth mental health crisis. Regardless of when the pandemic ends, there will always be students that are disproportionately socially isolated and are deserving of a friend and mentor. With that in mind, there will always be a place for Virtual Buddies and the goal is to keep this support system strong for these deserving students.
We would like to thank Dr. Skehan, Dr. Hirsh, Dr. Nazarian, Dr. Graham, Lauren Colwell, Juliamy Saraiva, and all others involved in helping to make this program a reality. None of this would have been possible without them.
Rohit Das, BS, Thomas Drews, BS, Christian Keenan, MSE, and Fiona Splaine, BS are 3rd year medical students and Calvin Schaffer, BS is a 4th year medical student
Rohit Das, email: rohit.das@umassmed.edu
Thomas Drews, email: thomas.drews@umassmed.edu
Christian Keenan, email: christian.keenan@umassmed.edu
Calvin Schaffer, email: calvin.schaffer@umassmed.edu
Fiona Splaine, email: fiona.splaine@umassmed.edu
1. Centers for Disease Control and Prevention. (2022, March 31). New CDC data illuminate youth mental health threats during the COVID-19 pandemic. Centers for Disease Control and Prevention. Retrieved May 15, 2022, from https://www.cdc.gov/media/releases/2022/p0331youth-mental-health-covid-19.html#:~:text=According to the new data,hopeless during the past year.
2. Lo, C. B., Bridge, J. A., Shi, J., Ludwig, L., & Stanley, R. M. (2020). Children’s Mental Health Emergency Department Visits: 2007–2016. Pediatrics, 145(6). https://doi. org/10.1542/peds.2019-1536
“
. . . there will always be students that are disproportionately socially isolated and are deserving of a friend and mentor. ”

The COVID-19 pan D em IC has D era I le D r O ut I ne vaccine delivery services to children and adolescents, leaving them at risk for vaccine-preventable diseases. Vaccination is a measure of a community’s health, and we must do better. When routine vaccinations are not prioritized, our patients and community are vulnerable to sporadic outbreaks of vaccine preventable illness. COVID-19 has had a substantial impact on routine childhood vaccination. The World Health Organization reported Tdap immunization rates have decreased for the first time in nearly 28 years (1). This is thought to be caused by factors related to the COVID-19 pandemic including decreased number of in-person healthcare encounters, newfound vaccine hesitancy, and misinformative social media campaigns related to vaccinations. Pediatric nurses, health care providers, and medical homes are in a unique position to impact this phenomenon while considering the role of atraumatic care and effective communication.
We have seen a decrease in the number of in-person health care encounters over the past two years. Initially this was related to fear of COVID-19 exposure in clinic settings and now is more likely a feature of convenience. Immunizations cannot be administered at virtual visits leading to a delay of routine vaccination of children of all ages.
Newfound vaccine hesitancy is related to the spread of immunization inaccuracies surrounding the development and distribution of the COVID-19 vaccine. This, combined with widespread increasing rates of vaccine hesitancy, the reluctance or refusal to vaccinate despite the availability of vaccines, has the potential to seriously impact community health (2).
Misinformation campaigns are powerful. False claims about vaccinations undoubtedly undermine public trust. Data gathering often precedes decision making. When large quantities of easily accessible data are inaccurate, false, or misleading, vaccine hesitancy is encouraged. Unlike traditional media campaigns, social media offers users the ability to create, and disseminate, content rapidly without editorial oversight. This has increased the frequency of exposure to mistruths, and the sheer number of misinformation campaigns far outweighs the ability of a healthcare professional to correct mistruths and interrupt these campaigns via in-person consultation. This is particularly impactful for people with low health literacy, anyone with difficulty accessing data addressing alterative views, and people without access to a trusted healthcare provider. In these cases, mistruths become reality and contribute to vaccine hesitancy and refusal.
The process of educating, vaccinating, and interrupting the
spread of mistruths should happen at all healthcare encounters, including episodic and mental health visits. This is especially true and relevant since many healthcare encounters were missed due to the pandemic. Each in-person healthcare encounter should be an opportunity for education and ideally vaccination. Sharing objective information and creating a non-judgmental environment that prioritizes shared decision making with caregivers and children is critical to effective communication about vaccines and to dispel the anti-vaccine myths.
Pediatric nurses and pediatricians are embedded within the community. Yet, as it relates to their profession, they tend to take a passive role when interfacing with social media. Eighty-five thousand new anti-SARS-CoV-2 vaccine Facebook accounts and 60 million followers of these accounts emerged over the course of the post-vaccine era of the COVID-19 pandemic (3). Fewer than 60% of HCPs use social media for professional purposes and most interactions are passive (3). Nurses are the most trusted profession in the world for the twentieth year in a row (4). It is the responsibility of nurses and other HCPs to engage with social media to dispel myths and spread scientific facts. Connection with the community, in this case via social media, can enhance trust, rapport, and relationships via education. These factors can be impactful when considering vaccine hesitancy of all kinds.
Relationships between nurses and families begin with infant vaccines and are fostered within medical homes. Medical homes provide comprehensive care by establishing partnerships with families, the community, specialty care, family support, and education. The approach, education provided, rapport with the parent, and trust of the child are formed early on for pediatric patients. In some cases, this rapport and trust have been established for a family in the context of older siblings or even by the parents themselves as patients. Pediatric nurses and providers can greatly influence a family, based on their credentials and rapport, when making recommendations, sharing fact-based information, supporting, and educating families. This relationship is a bridge to close the anti-vaccination chasm as it relates to the COVID-19 vaccine and other childhood immunizations that were missed and/or are currently due.
Consistently incorporating principles of atraumatic care into routine vaccine administration facilitates ongoing vaccination. For example, distraction tools such as the “shot blocker,” can decrease the patient’s perception of pain during injections. Frequently, fear of injections, post-injection soreness, fear of syncope, or general health care anxiety are barriers to a patient’s desire and agreement to get vaccinated. This can also contribute
to a caregiver’s willingness to consent in the moment versus delaying vaccination to another healthcare encounter. Addressing and controlling for these factors in the pediatric setting by educating the patient and their family on the pain management and distraction tools available and on symptomatic management of post-vaccine symptoms as well as incorporating developmentally appropriate anxiety mitigation techniques into routine vaccine protocol have the potential to impact overall vaccine hesitancy. This, in conjunction with offering routine and recommended vaccinations at each healthcare encounter, encouraging in-person health maintenance visits, as well as communicating with families via an electronic health record portal about immunization gaps, can help restore our community vaccination rates post-pandemic.
Effective communication, atraumatic care, engagement with social media, and considering each healthcare encounter an opportunity to vaccinate are critical tools as we battle vaccine hesitancy. Pediatric nurses and physicians have a professional responsibility to use strategies to enhance COVID-19 and pediatric routine vaccination hesitancy. +
Chrystina Manero, PhD, RN, CPNP-PC, Assistant Professor – UMass Chan Medical School and Tan Chingfen Graduate School of Nursing
1. Olusanya OA, Bednarczyk RA, Davis RL, Shaban-Nejad A. Addressing Parental Vaccine Hesitancy and Other Barriers to Childhood/ Adolescent Vaccination Uptake During the Coronavirus (COVID-19) Pandemic. Frontiers in Immunology. 2021;12.
2. Akbar R. Ten threats to global health in 2019. World Health Organization. 2019.
3. Hernandez RG, Hagen L, Walker K, O’Leary H, Lengacher C. The COVID-19 vaccine social media infodemic: healthcare providers’ missed dose in addressing misinformation and vaccine hesitancy. Hum Vaccin Immunother. 2021;17(9):29622964.
4. Saad L. US ethics ratings rise for medical workers and teachers. Gallup, Inc. 2020.


Where On a sCale Of risky behavior does criminal culpability arise?
The case of nurse RaDonda Vaught in Tennessee has given rise to much recent discussion of this question. This nurse was convicted of “criminally negligent homicide” because of a patient death resulting from the nurse’s medication error. She lost her nursing license and has been sentenced to three years’ probation. This matter highlights the complexity of hospital safety systems and the multiple demands on nursing staff. It also raises the question of whether this outcome under Tennessee law could occur here in Massachusetts.
An outline of the events that led to this outcome is short and simple, but a description of the many errors and failures that contributed to it is complex. The day before Christmas, 2017, Charlene Murphey checked into Vanderbilt University Medical Center with a subdural hematoma. By the day after Christmas, she is ready to be discharged, but before she was to leave the hospital, she was to be given a PET scan. She advised a radiology tech that she was anxious and asked for medication. Nurse Vaught was asked to administer Versed, an anti-anxiety medication, but she obtained from the automatic dispensing cabinet (ADC) and administered to Murphey Vecuronium, a paralytic agent. Vaught did not monitor the patient during the PET scan, after which Murphey was found to be unresponsive. She died on December 27, 2017 after being disconnected from a breathing machine.
A root cause analysis of this incident reveals a tangled web of errors, omissions, oversights and inefficiencies that contributed to this tragedy. Just a few of the more significant include the following:
Vaught was the “Help-All Nurse” in the Neuro-ICU at the time, was precepting a new-graduate RN and was preparing to go with the preceptee to the emergency room to conduct a swallowing study when she was asked to help out in the radiology department. Neither Murphey’s primary nurse nor any of the radiology RN’s had time to administer the anti-anxiety medication and Vaught’s assistance was sought in order that the test not be cancelled. The picture painted here is of over-stressed and over-committed nursing staff under pressure to act quickly.
Neither the primary nurse nor Vaught routinely administer Versed. Presumably due to this lack of familiarity, Vaught did not realize that Versed is a liquid and Vecuronium is in powder form. In any event, Vaught did not read the warnings on the front of the label, but concentrated on reading the reconstitution directions on the back of the label. This was undoubtedly negligent of Vaught.
The hospital had begun the process of changing the interface between the ADC and the electronic health record in November of 2017. As a result, nurses were commonly overriding certain functions in order to ensure timely care. Medications are retrieved from the ADC by typing in the first
sure timely care. Medications are retrieved from the ADC by typing in the first two letters, which generates a list of possible drugs; in this case, Vecuronium appeared at the top of the list. Vecuronium is not segregated from other drugs in the ADC nor does selection of that drug trigger special screen warnings. Normally barcode scanning is done to confirm the appropriateness of the medication to be administered to a given patient, but Vaught cannot locate any barcode scanning equipment in the radiology department when she arrives in that department to assist Murphey. Had hospital systems been working properly and readily available, designed safety features may have prevented this error.
Because the nursing staff assumed Versed was being administered to Murphey, they agreed that in-person monitoring her during the PET scan was unnecessary. The holding area where Murphey awaited the PET scan was equipped with a surveillance camera. Either form of monitoring, if conducted properly, might have alerted staff to Murphey’s condition before she suffered irreversible brain damage.
Shortly after the incident, Vaught was fired by Vanderbilt University Medical Center. Initially Murphey’s death was reported as resulting from natural causes, the error was not reported to regulators, and the hospital reached a settlement with Murphey’s family. Anonymous tipsters to both state and federal agencies resulted in investigations of both Vaught and the hospital, resulting in Vaught’s indictment and a hospital “plan of correction.” Eventually Vaught lost her nursing license; the Tennessee Board of Nursing found she was guilty of unprofessional conduct, failure to maintain an accurate record of patient care and abandonment of a patient requiring nursing care. The Board sought up to $60,000 in costs in addition to licensure discipline.
Given the number of factors leading to Murphey’s death, not all of which were within Vaught’s control, and the undisputedly unintentional nature of Vaught’s actions, one might think that professional discipline and correction of hospital policies and procedures might have been the end of the story. Why wasn’t it, and could a similar case in Massachusetts lead to a similar criminal proceeding?
The answer is likely yes. Tennessee’s adoption of a criminal negligence homicide statute was enacted in 1989 and replaced the crime of involuntary manslaughter. The Tennessee legislature recognized that culpability for deaths resulting from criminal negligence was not new and had long recognized culpability for such deaths under its involuntary manslaughter statute. In Roe v. State, 210 Tenn. 282, 358 S.W.2d 308, 314 (1962), the Tennessee Supreme Court stated, “Where one unintentionally causes another’s death by conduct not amounting to a felony [malum prohibitum] and not malum in se, but which constitutes gross and culpable negligence, he is guilty of involuntary manslaughter.”
Massachusetts has not yet codified criminal negligence statute, beyond those statutes directed at homicides caused by negligent
or impaired operation of a motor vehicle, but the manslaughter statute would likely provide a basis for criminal liability for conduct similar to RaDonda Vaught’s. To find an accused guilty of involuntary manslaughter in Massachusetts, the prosecution must prove that the accused 1) caused the victim’s death; 2) that the accused intended the conduct that caused the victim’s death; and 3) that the accused’s conduct was wanton or reckless.
According to Massachusetts’ Model Jury Instructions, wanton or reckless conduct is conduct that creates a high degree of likelihood that substantial harm will result to another. It is conduct involving a grave risk of harm to another that a person undertakes with indifference to or disregard of the consequences of such conduct. Whether conduct is wanton or reckless depends either on what the defendant knew or how a reasonable person would have acted knowing what the defendant knew.
Because neither Vaught nor Murphey’s primary nurse were experienced in administering versed, it is reasonable to conclude that Vaught would not have known that versed was a liquid and vecuronium is in powder form. To secure a dose of either drug Vaught would have begun typing the name of the drug to be dispensed into the ADC – clearly more could be done here. The question is whether, under the circumstances as a trained nurse, Vaught should somehow have known that she was about to administer vecuronium instead of versed. Was it somehow reckless of her to fail to ignore the pressures of being part of an over-stressed and over-committed nursing staff and take extra time to verify what she was doing? Unfortunately, that question often gets answered by those who may not appreciate the circumstances and pressures of someone in Vaught’s position.
The Massachusetts SJC recognized the difficulty in defining wanton and reckless conduct sufficient to sustain a conviction for involuntary manslaughter when it said, in Sandler v. Commonwealth, 419 Mass. 334 at 337 (1995) that “This court’s recognition of a fictional or constructive intention and this court’s representation that wanton or reckless conduct is different in kind from negligence do not much help in differentiating neatly between negligent conduct (including grossly negligent conduct) and reckless conduct. These concepts emphasize, however, the requirement that reckless conduct must be based on a high degree of risk that death or serious bodily injury will result from a defendant’s action or inaction when under a duty to act.”
Most would agree that there is a high risk of death or serious bodily injury when administering the wrong medication, the question is whether, under the circumstances, doing so was reckless. A jury deciding this case under Massachusetts law could certainly find RaDonda Vaught guilty. The hope, however, is that prosecutors would use their discretion when making a charging decision and focus on whether it was the nurse or the facility that created the problem. +

The physICIans Of the WOrCester DIstrICt shOWeD remarkable insight in dealing with the emotion surrounding the polio epidemic of the 1950’s and the development of a vaccine.
In 1955, shortly after release of the vaccine, the “Cutter Incident” occurred in which, due to defective manufacturing, live virus was included in the inactivated virus vaccine. Over 40,000 cases of polio resulted, including cases of paralysis and death. The inoculations were in April, 1955.
In response Worcester Medical News published the following in May,1955:
“To one who has watched the development of immunization against contagious diseases during the last 55 years, certain definite conclusions have been formulated which he wishes to put on record.
The writer remembers the antagonism that was still alive in the early 1900s against smallpox vaccination. This was continued into the late 1920s by uninformed and regular practitioners of medicine. He was also active in organizing the campaign for the prevention of diphtheria in the city. With all similar immunizing procedures, successful and unsuccessful, there were many bugs which only trial could correct. This happened in the toxin-antitoxin that was first used to immunize against Diphtheria which was so prevalent before the 1920s. The adoption of this wonderful procedure was slow and many imperfections were gradually removed so that today we have a safe method which has nearly banished that dread disease from the community. It has gone into history as one of the great victories of medical science over disease. Immunization against Scarlet Fever had its problems also, but they were overcome by experience. Happily, with the advent of antibiotics, Scarlet Fever ceased to be a problem.
And now we have the Salk vaccine which is destined to be a wonderful addition to the physicians’ armamentarium against that frightening disease, poliomyelitis, and which has been received with greater acclaim after only a few months trial. There will be many bugs in its development. Who is to blame for the hysteria which demanded that mass production of this vaccine before all safeguards could be established? Here is one man’s opinion:
1st: The Polio Foundation for the value of publicity and its beneficial effect on their campaign for funds grabbed the opportunity with great fanfare.
2nd: The great bacteriological laboratories that were eager to be the first to present their vaccine to the public.
3rd: The public press who overplayed the value of the vaccine before it was properly safeguarded.
4th: The pharmaceutical house which gave free close circuit TV report of the evaluation of the test last summer.
5th: The medical profession who were so easily stampeded into getting the first release of the vaccine.”
Yet, after what was felt to be adequate proof of safety, the WDMS not only supported the vaccine, but worked to immunize as many as possible in the community (funds from this project provided the seed money for the WDMS Scholarship Fund.
The challenges of building trust and meeting the needs of Public Health were illustrated in this editorial from Worcester Medical News from October, 1959:
“Local newspaper reports that the board of health of a nearby town was taken to task and sort of slapped on the wrist by the district chapter of the National Foundation because four children in one family who had not received the Salk vaccine came down with polio.
Rather than be overly critical, it would be well for this chapter to intensify its efforts in the discussion of education, urging more and more people, over and over again, to take advantage of these inoculations. In this particular case, it is known that the mother was urged to take advantage of these inoculations not only through ordinary channels of publicity, but also by private physicians. Furthermore, according to available records, this particular town has done an outstanding job of immunizing the population.
We should not use slapdown methods to get these people to take inoculations. Because of ignorance, indolence, misdirection or misinterpretation of information, or “fear of the needle“ there will always be an irreducible minimum who will refuse these injections, unless we can have a law which will compel Salk injection similar to that for a smallpox vaccination. Even then, there would be a few individuals who would deviously circumventive law.
At this rating, Worcester has not had a single case of polio in 1959. Perhaps that may be due to good fortune, but more likely to our immunization program. Through the efforts of our medical society, private physicians, and the department of public health, 92% of all school children, 90+ percent of preschool children, 60+ percent of all adults under 40 years have received three or more polio inoculations. Furthermore, additional clinics are set up to take care of the stragglers so that the maximum number of people will be immunized. Worcester can indeed be proud of this record.”
Wisdom from our forefathers. Human nature, it seems, has not changed. +
Health Matters is a television program produced in collaboration with The Worcester District Medical Society and WCCA TV in Worcester. Offering valuable information on disease prevention, treatment options, current public health issues and more, Health Matters is produced in a ½ hour interview format and the program airs on WCCA TV Cable Channel 194: Wednesday- Noon and 7:30 pm, Thursday– 7:00 pm and Friday – 9:30 am.
To view episodes of Health Matters: Click Here or visit our Website: www.wdms.org


Lifestyle Medicine ~ Guest Dr. Michelle Dalal
Addiction Medicine ~ Guest: Meghan Wood
Equity and Diversity in Health Care ~ Guest: Dr. Manjul Shukla
Life as a Medical Student During COVID ~ Guest: Trent Taros
Child Health Equity Center ~ Guests: Dr. Arvin Garg and Alison LeBlanc
Presciption CPR ~ Guest: Dr. Joseph Sabato
Gun Violience ~ Guest: Dr. Peter McConarty
Medical Robotics ~ Guest: Professor Loris Fechera
Tobacco: A Public Health Perspective ~ Guest: Cherry Tangri
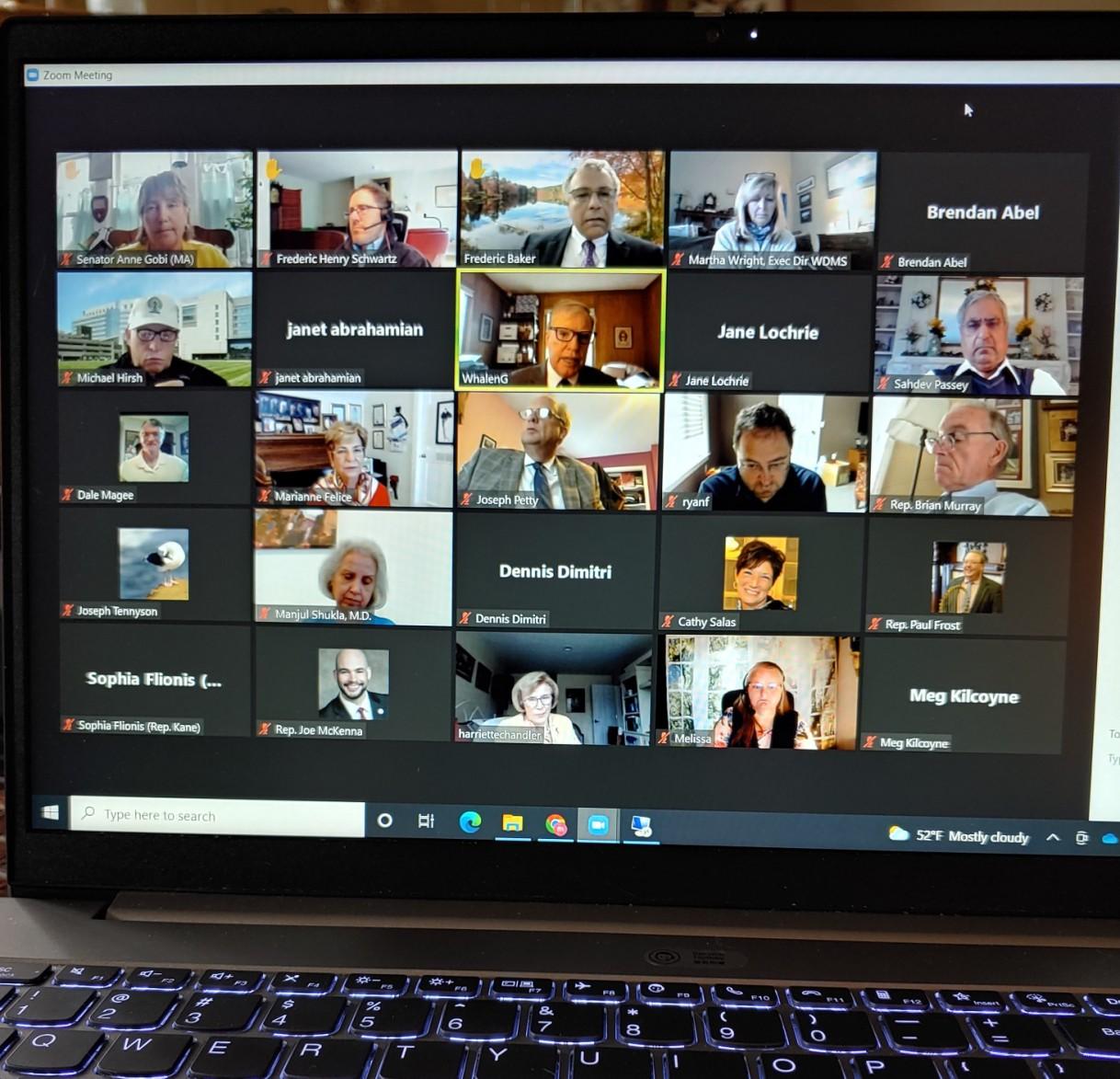
If you have an idea for a topic or guest, or wish to be a guest, please contact MBoucher@wdms.org or call 508-753-1579.
Each year, WDMS members meet with Legislators to discuss and collaborate on important, current issues affecting our community and patients. Typically in person, our annual Legislative Breakfast was held virtually on May 6, 2022. In attendance were 35 Physician Members, State and local Senators, Representatives and their Aides and the main topics of discussion were Pediatric Mental Health and The No Surprise Billing Act. Reports and testimony were compelling and areas for improvement were identified. Thank you to those who attended our meeting. Your commitment, work and support is very much appreciated.



Held on Saturday, May 7, 2022
On May 7, 2022, we hosted an Open House Reception and DeeDee Bridgewater concert, sponsored by Music Worcester. Ms. Bridgewater is an American jazz singer with an all -female band, consisting of a bass player, pianist and drummer. She is a three-time Grammy Award-winning singer-songwriter, as well as a Tony Awardwinning stage actress. Prior to the concert, we opened the doors to our newly decorated office, including medical photographs and prints, a newly restored archive ledger book and unveiling of the Dr. Joseph Sargent portrait. The portrait was restored by Mr. Gerry Scher who keeps Mechanics Hall pristine. Thank you Dr. Magee, for your research and presentation. We hope to see you all again at our next Open House.

 Dale Magee, MD WDMS Curator
Martha Wright, MBA WDMS Executive Director
Unveiling of the Dr. Joseph Sargent Portrait
The Dee Dee Bridgewater Quartet
Dale Magee, MD WDMS Curator
Martha Wright, MBA WDMS Executive Director
Unveiling of the Dr. Joseph Sargent Portrait
The Dee Dee Bridgewater Quartet
