Provider Forum

16
November 2022

te
Karakia Timatanga (opening) Whakataka te hau ki te uru Whakataka te hau ki te tonga Kia mākinakina ki uta Kia mātaratara ki tai E hī ake ana te atakura He tio, he huka, he hau hū Tīhei mauri ora! Cease the winds from the west Cease the winds from the south Let the breeze blow over the land Let the breeze blow over the ocean Let the red-tipped dawn come with a sharpened air A touch of frost, a promise of a glorious day
Whakataka
Hau
Agenda
Speaker Session
Phil Back, GM – Network Services, WBoP PHO 7 to 7.15 PM PHO Update
Dr Robert McIntosh, MD FRCP, Interventional
Cardiologist, Hauora a Toi Bay of Plenty
Tracey Cumming, Advanced Practitioner
Cardiac Physiologist, Hauora a Toi Bay of Plenty

Sonya Ginty, Physiotherapist – COTS, Hauora a
Toi Bay of Plenty
Dr Claire Isham, Clinical Director, WBoP PHO
Dr James Peckett, Clinical Advisor, WBoP PHO
7.15 to 7.40 PM Cardiac Monitoring in BOP Outpatients
7.40 to 7.55 PM COTS Programme Update
7.55 to 8.10 PM PHO Clinical Update
Dr Claire Isham, Clinical Director, WBoP PHO 8.10 to 8.20 PM CME Update
Michelle Meyer, Clinical Advisor, WBoP PHO 8.20 to 8.30 PM PHO IV Iron Programme Update
PHO Update
Phil Back
General Manager – Network Services
Western Bay of Plenty Primary Health Organisation

Context for Localities ‘Cube’

Cardiac Monitoring In BOP Outpatients

 Dr Rob McIntosh MD FRCP
Dr Rob McIntosh MD FRCP
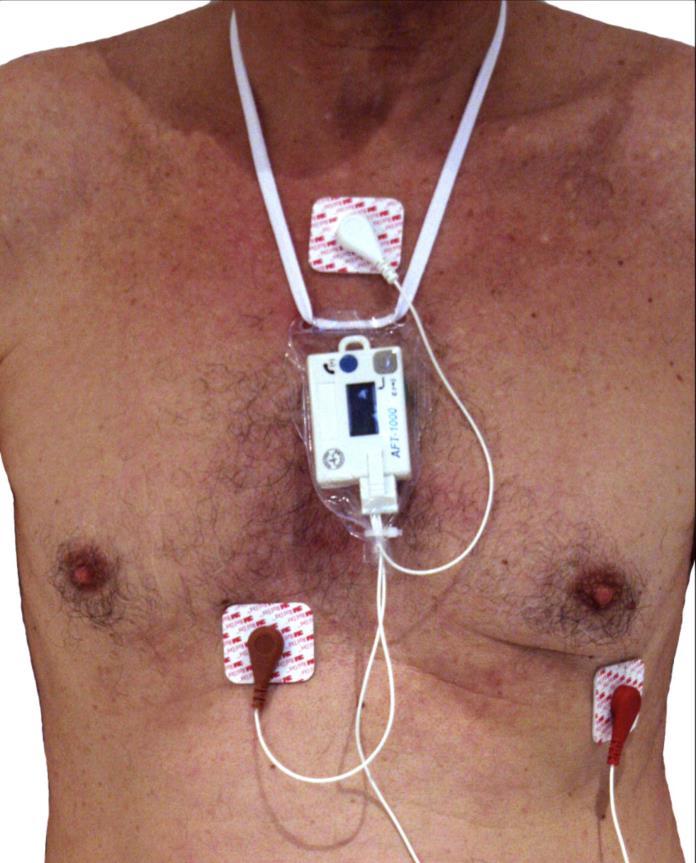
The ‘Holter Monitor’
• An ambulatory electrocardiographic system designed by Dr Norman J. Holter in 1957.
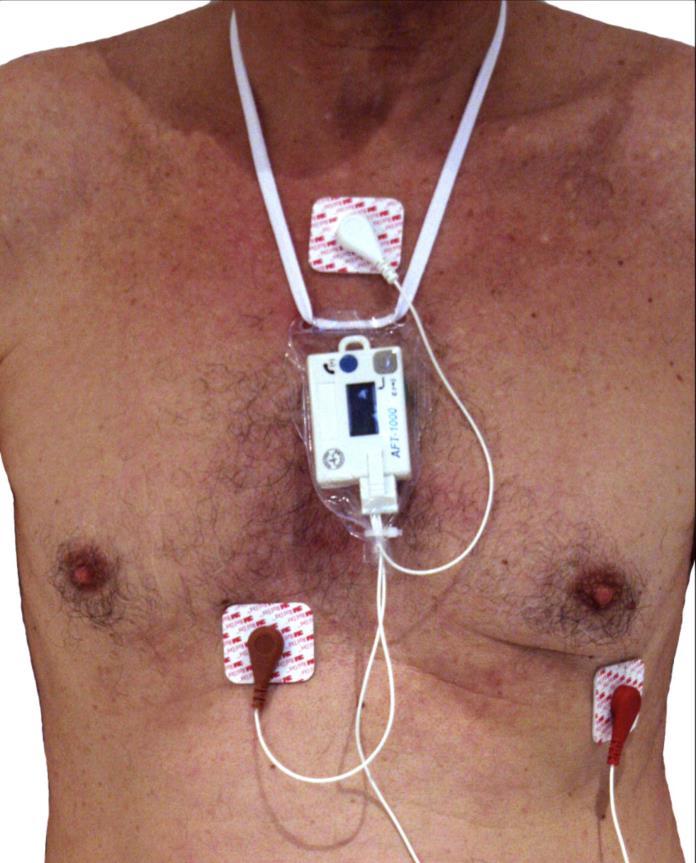
• Designed to gather electrocardiographic signals from individuals whilst they go about their daily activities. Providing ‘continuous ambulatory monitoring.’
• The first Holter monitor was about the size of a briefcase and comprised of an amplifier, tape recorder, electrodes attached to the individual's chest, playback unit and analysing unit.
• Devices can now be approximately the size of a matchbox.
Norman J Holter (1914-1983)
Common Referral
To establish the link between palpitations and abnormal heart rhythms • To diagnose the cause of syncope or near syncope • Patients with neurologic events when transient atrial fibrillation or flutter is suspected - ‘cryptogenic stroke’
To stratify the risk of sudden cardiac death
To evaluate transient episodes of cardiac arrhythmia or myocardial ischemia • To evaluate prognosis • To monitor the efficacy and safety of pharmacological or non-pharmacological therapies • To detect proarrhythmic responses to antiarrhythmic therapy in patients at high risk
To analyse the function of pacemakers or other implantable devices
Holter Monitoring
Indications •
•
•
•
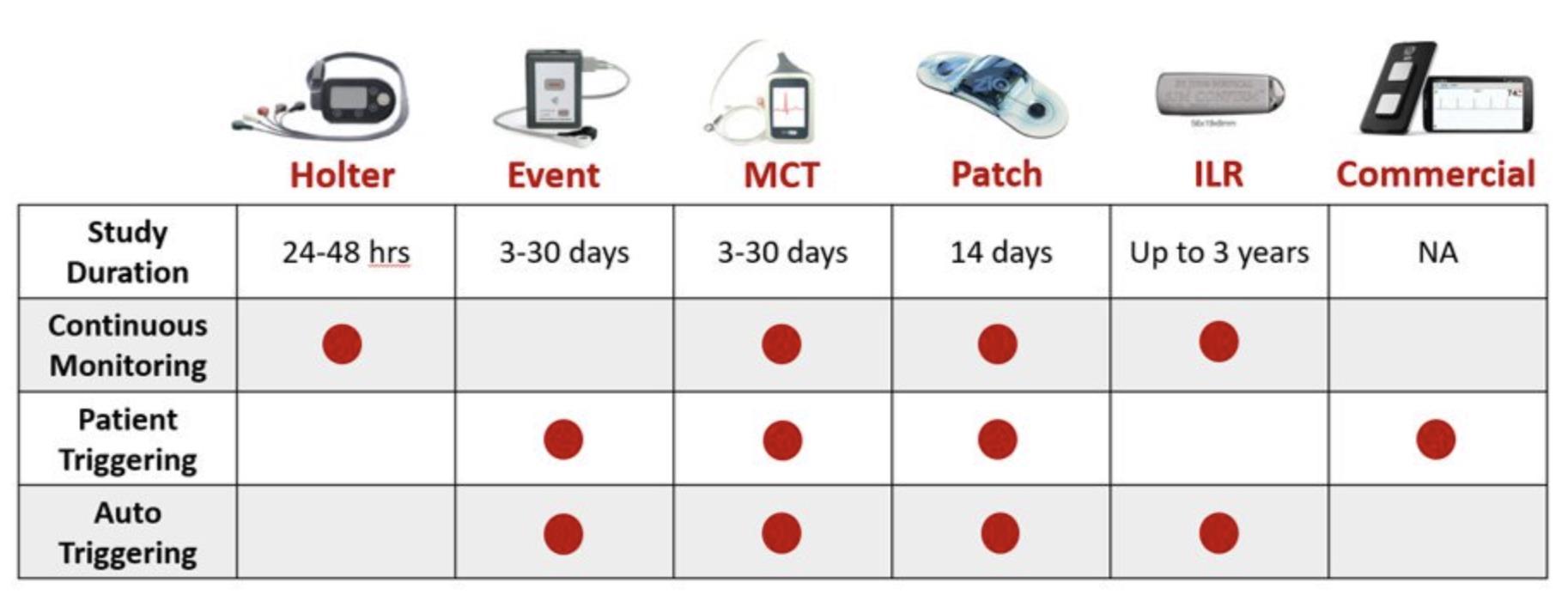
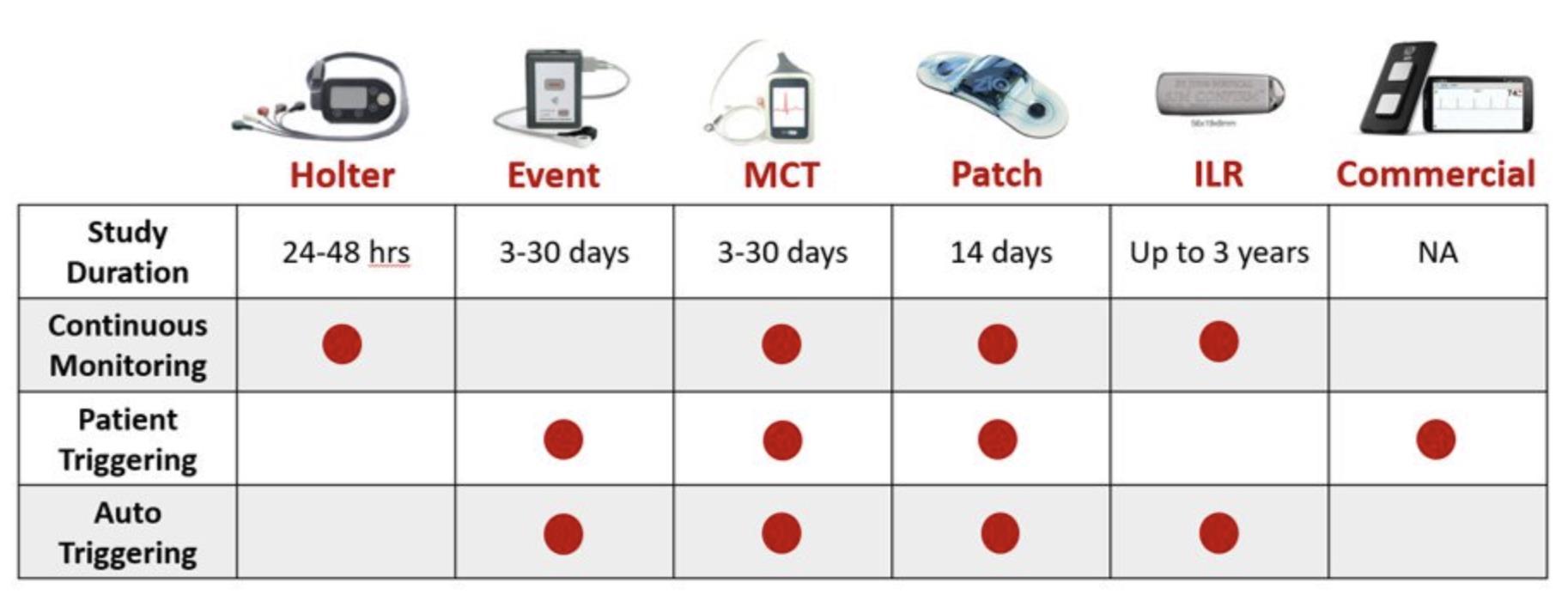
MCT: Mobile Cardiac Telemetry. ILR: Implantable loop recorder.
Monitor Options…
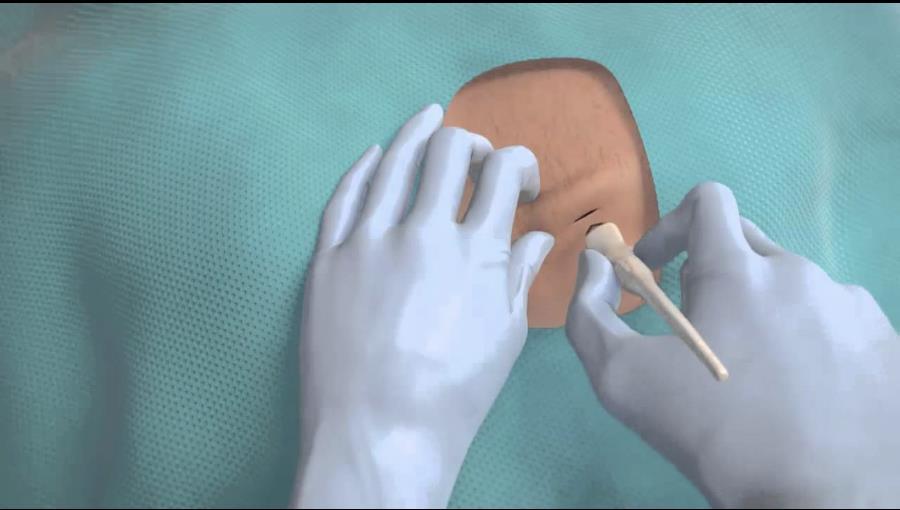
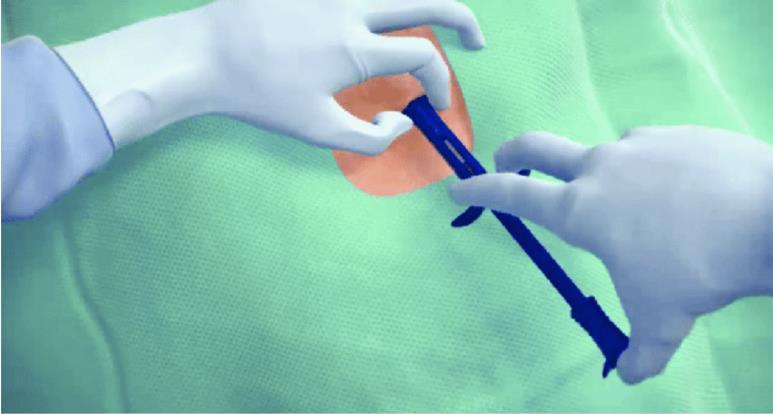
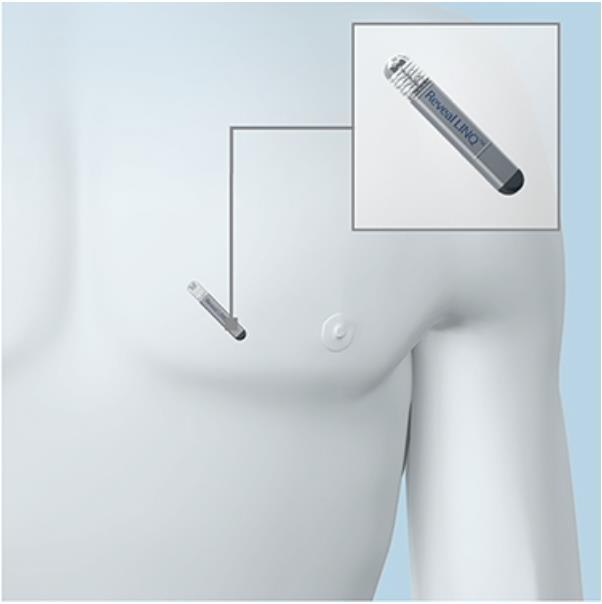
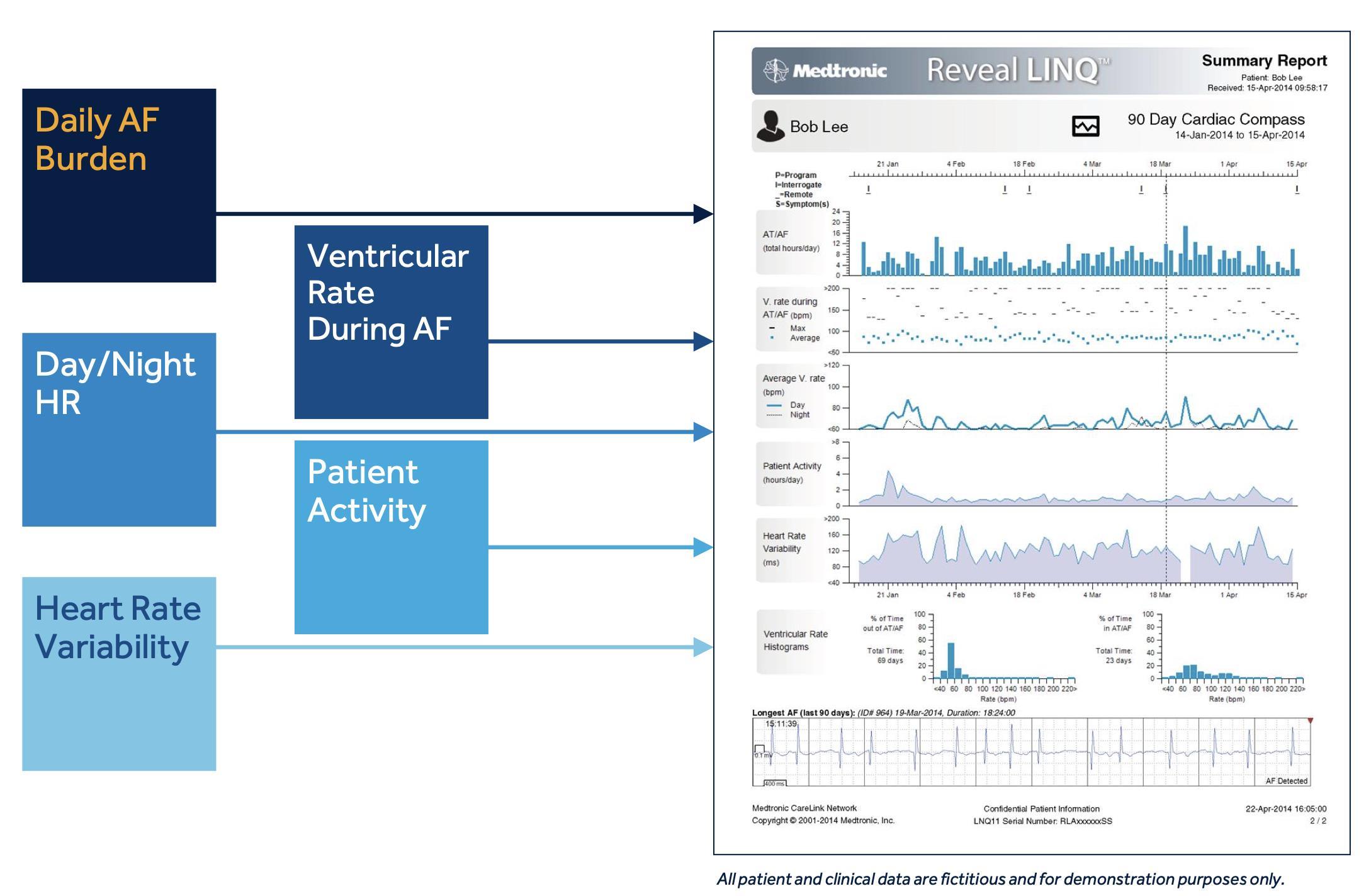
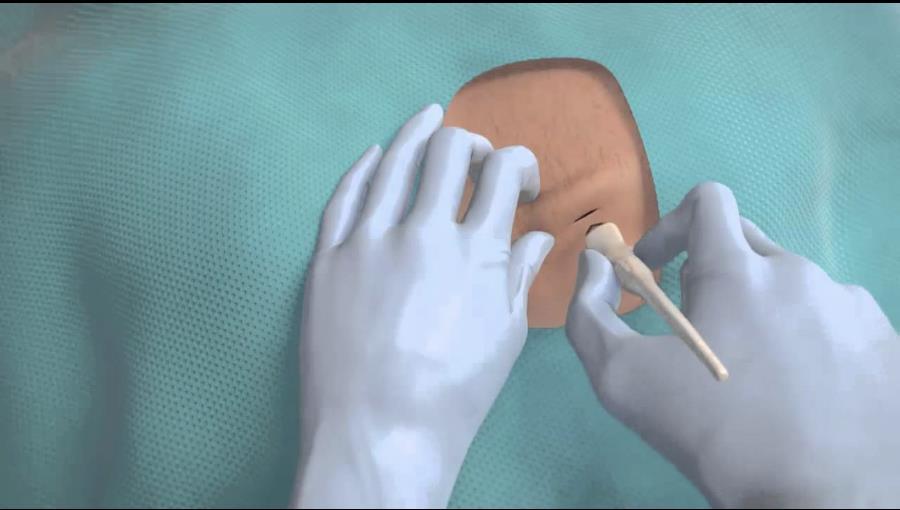
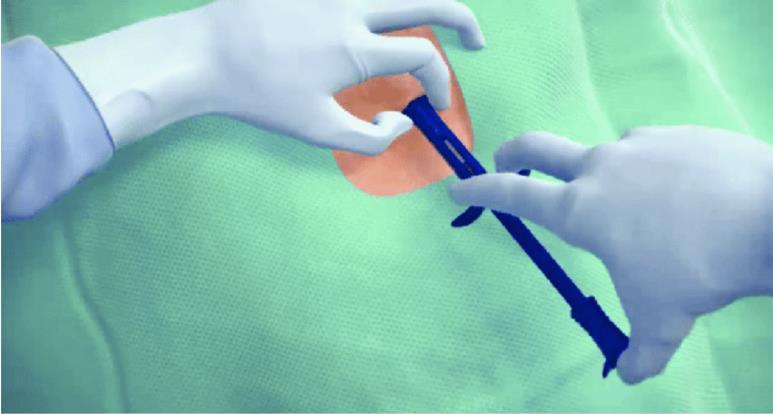
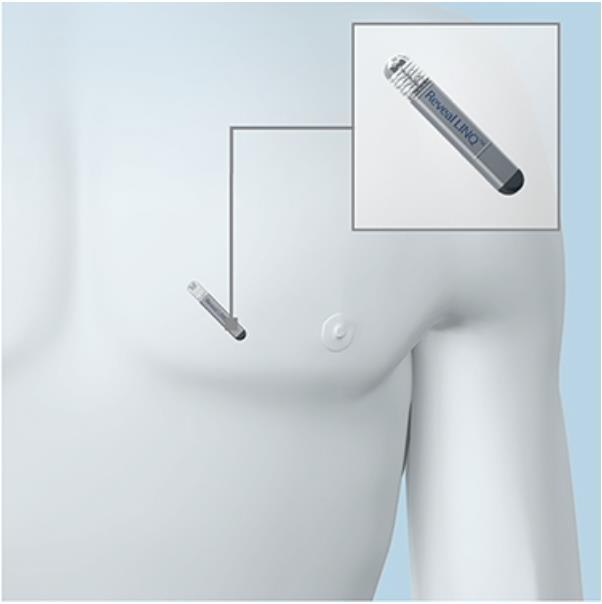
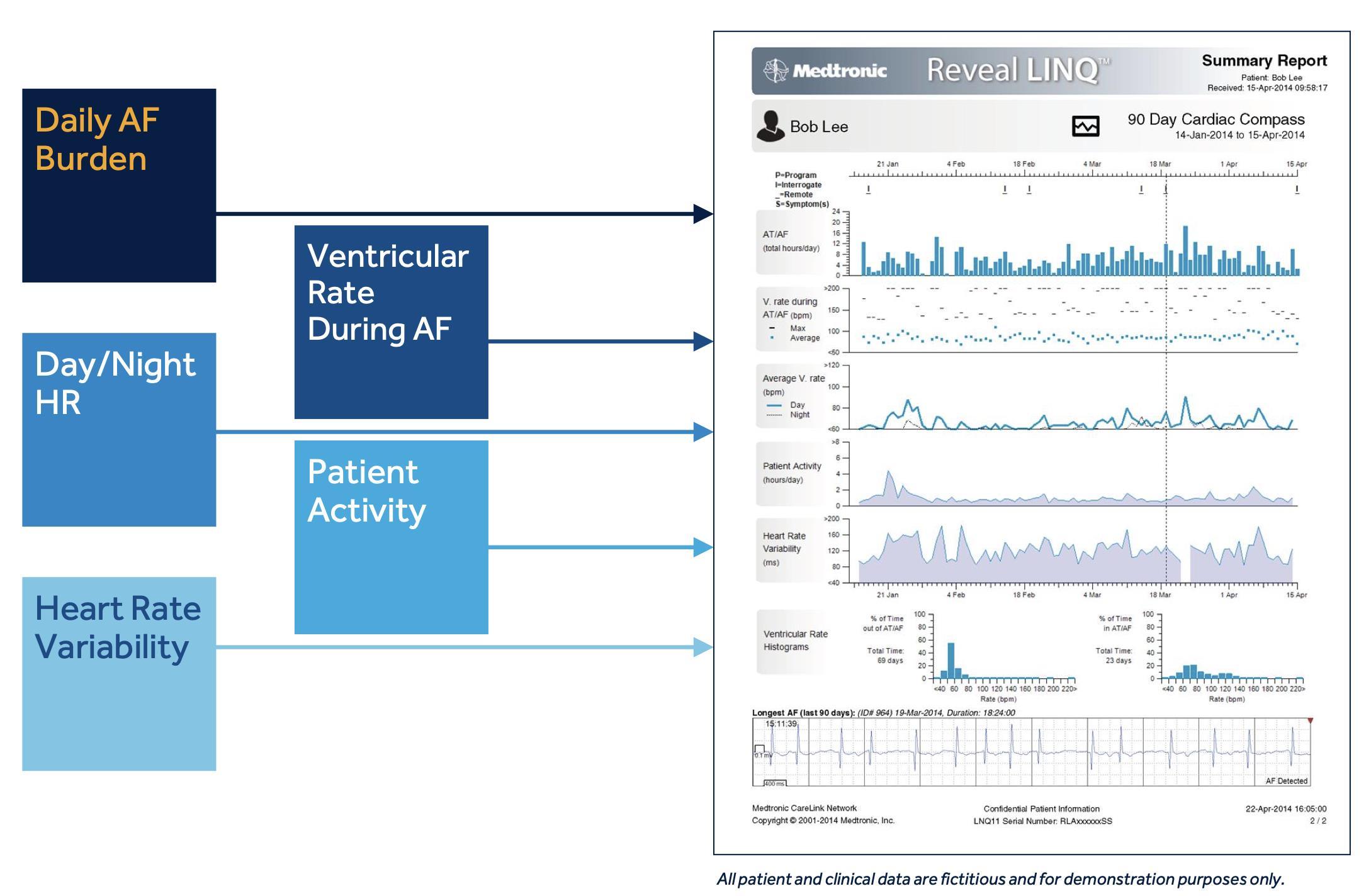
Implantable Loop Recorder (ILR)

Current BOP DHB waiting lists for non-invasive cardiac diagnostic tests • Waiting lists for cardiac diagnostics –• Tauranga • Whakatāne • Modality Modality ‘Urgent’ Referral ‘Routine’ Referral Total Holter 84 244 328 Event Monitor 19 28 47 Echo 79 1858 1937 Modality ‘Urgent’ Referral ‘Routine’ Referral Total Holter 12 29 41 Event Monitor 2 5 7 Echo 27 276 303 BOP DHB Totals Awaiting Rhythm Monitoring: 423 Awaiting Echo: 2,240
Available resources (non-invasive)
• 22 Holter monitors: 15 TGA (3 dedicated to stroke team), 7 WKA
• 3 Event monitors (TGA only)
• 5 Echo machines: 4 TGA, 1 WKA (soon to be 2)
• 2 full day-physiologist sessions for rhythm analysis (all based at TGA) plus ad hoc extra hours available as overtime.
• TGA: 2 full-day echo sessions (for outpatients) occurring on most weekdays, 1 inpatient list. The portable machine is made available for cath-lab cover.
• WKA: Weekdays, full day echo session (mixed inpatient/outpatient)
Approximate Real World Turnover
• Under current processes a single Holter monitor can perform a maximum of 2-3 studies a week (delays in turnover, appointment availability, 48hr sessions requested, late returns, COVID absences, weekends etc).
• Rhythm analysis following monitor return can take anywhere from 15 min to several hours depending on complexity.
• We are currently processing ~90 OPA rhythm studies a month
• A whole day echo OP list (with reporting) allows for ~7 patients to be scanned per sonographer-day.
• Echo is heavily burdened with inpatient requests (40-50% of scans).
• ~450 echos are completed each month (~225 OPA).
Typical Outpatient Waiting Times… • Rhythm monitor – Urgent 3-6 Months • Rhythm monitor – Routine 9-12 Months • Echo – Urgent 2 Months • Echo – Routine >12 Months Average wait times for routine referrals have increased from around 3months in 2011-2015 to 9-12 months (and climbing) at the current time.
to reducing wait-times and improving service efficiency
Strict referral vetting and test appropriateness cross-checking.
Avoid repeating recordings unnecessarily – Inpatients will have had recorded telemetry – daily analysis and recording is uploaded to MCP for all to see.
More efficient use of existing resources… less hardware down-time, less time between patient turnovers.
Buy more kit, organise more analysis sessions...
Holter $3750 per unit, costs are approximately $511 for processing each study.
Echocardiogram $272,342 per machine.
Use of 3rd party monitors with analysis support: ‘MyPatch’ or ‘Zio’.
Outsource echo lists to the private sector.
Encourage patients to use commercially available rhythm monitors / wearable monitors.
Potential approaches
•
•
•
•
•
•
•
•
•
Vetting and Appropriateness Criteria
The diagnostic sensitivity of a Holter depends very strongly on
clinical history (age, cardiac history, presence of risk factors/family cardiac history).
12 lead ECG findings – has one been done?
frequency of symptoms – less than
–
The nature of the symptoms reported also often differentiates between commonly benign and more significant underlying pathologies… • ‘Skipped beat’ or ‘isolated thud’ – ectopic beats • Pounding or rapid palpitation – SVTs, AF, Ventricular arrhythmias.
•
•
•
•
daily
24hr Holter largely ineffective. •
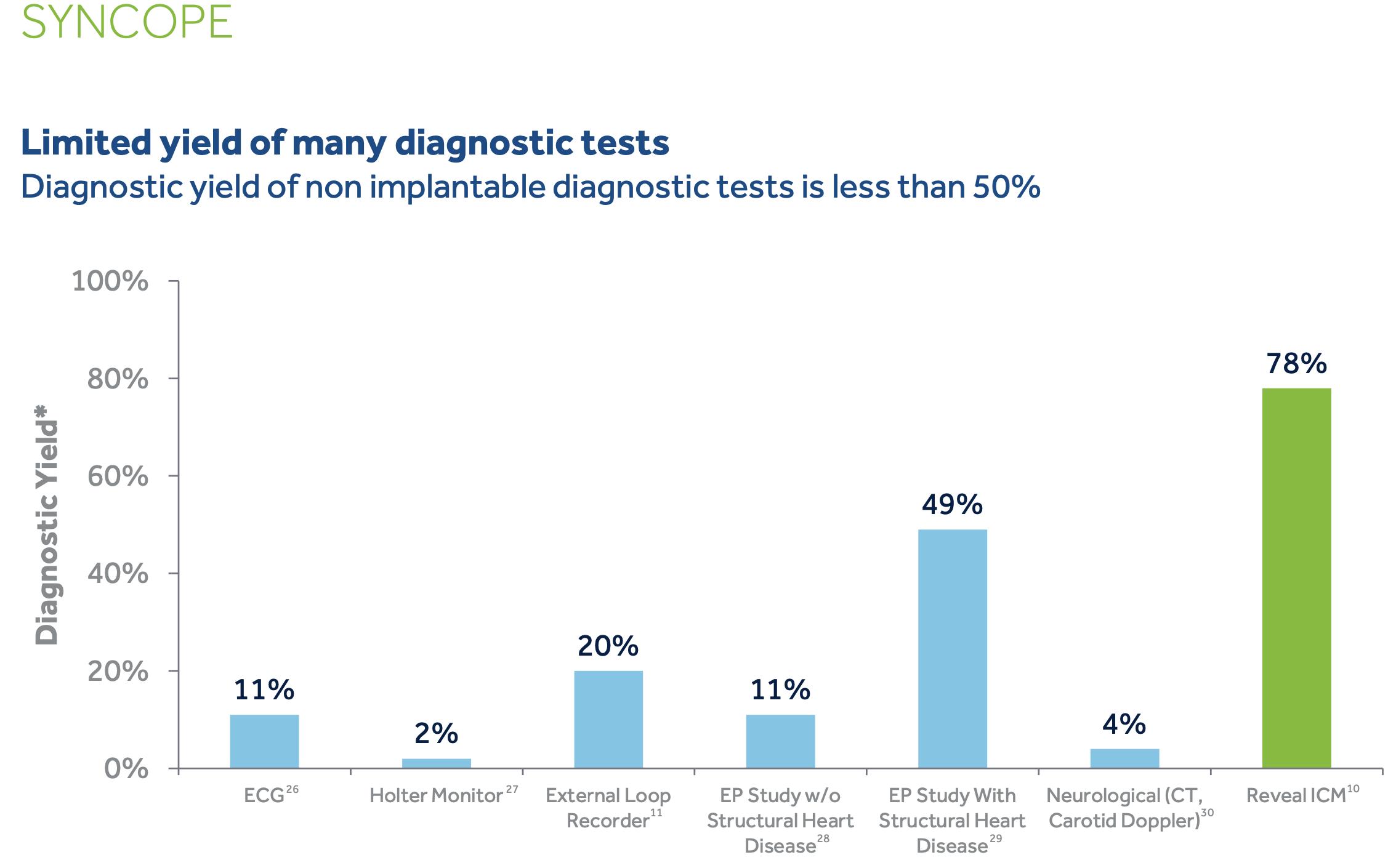
Vetting – Consider sensitivity of rhythm monitoring methods
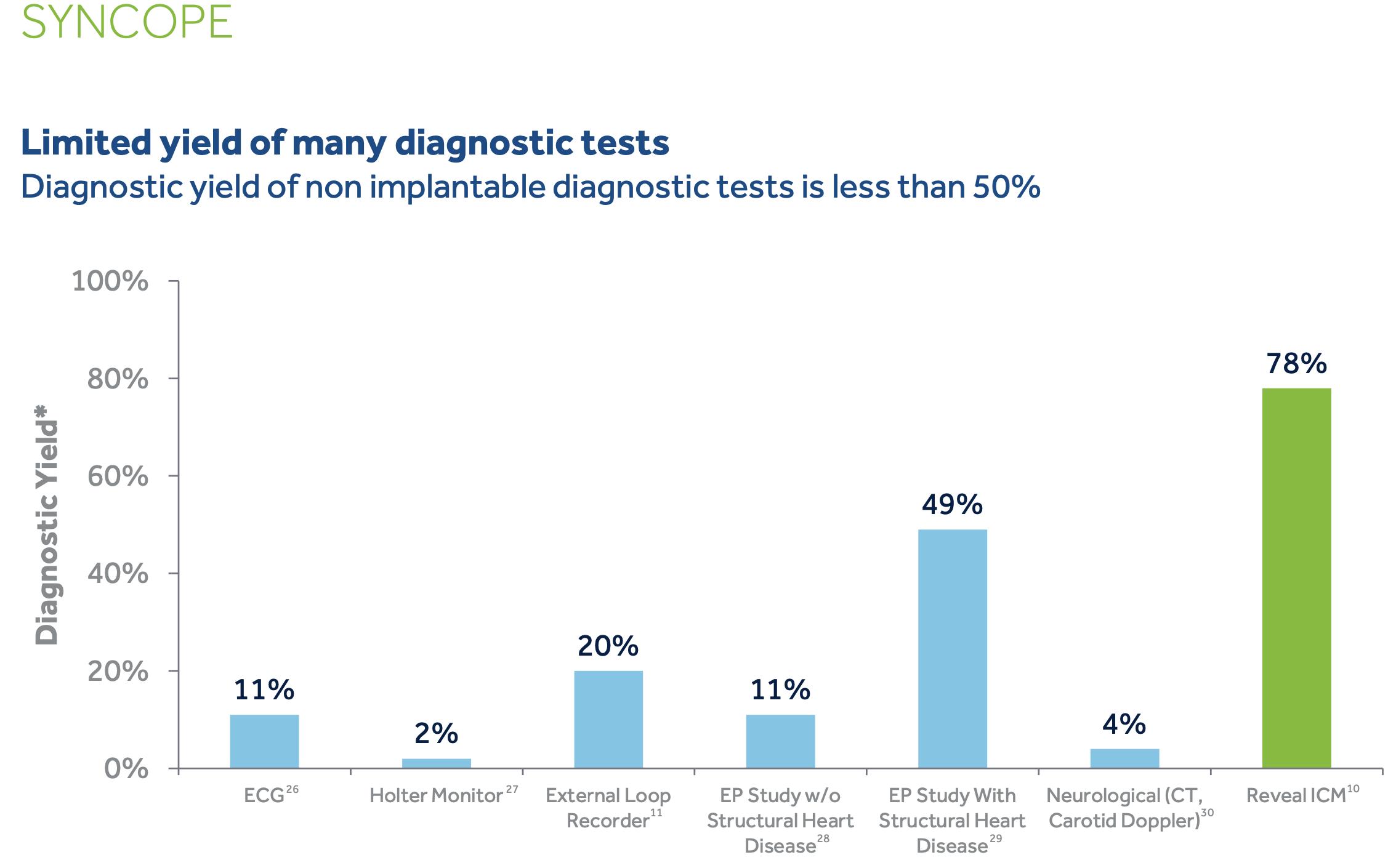
• In a mixed population referred for investigation of potential arrhythmia, 24Hr Holter monitoring has a low diagnostic yield due to the short recording period and the often paroxysmal nature of arrhythmias (diagnostic pick up ~9%).
• Longer periods of recording lead to enhanced diagnostic sensitivity e.g. for a 14-day patch monitor, reported rates of detection of arrhythmia at days 3, 7, and 14 was 28%, 47%, and 66%.
• Implanted loop recorders may lead to further improvements in diagnostic sensitivity
• BUT – longer recording / ILRs = more resource use, more expense, lower turnover, and for ILR – potentially unnecessary invasive procedures.
Loop recorders for everyone?
Vetting Summary
• Patients without a 12 lead ECG or comprehensive history accompanying their referral should not be wait-listed for a 24hr-Holter.
• Patients with low symptom frequency and no significant cardiac risk factors should not be listed for routine Holter monitoring due to the low diagnostic yield. An alternate path should be recommended/considered.
• Young usually well patients, with a normal ECG and no concerning historical features should be reassured in the first instance (especially if transient palpitation has occurred in the context of other recent illness/COVID vaccine). They are likely to be experiencing benign ectopic beats.




Other options – The Patch? • ‘MyPatch’ – Negotiations ongoing with BOP DHB. • System is in current use at Waikato and Nelson DHBs. • Rhythm analysis is provided by the third party company. Turnover <24hr compared to 10days. • Potential for a ‘non-contact’ diagnostic service facilitated by couriers. • Basic cost $150 per patient 24Hr recording. Can be worn for up to 14 days at small additional cost. • Benefits - potential savings of multiple $1000’s per month and markedly improved turnover times. • Risks - loss of own monitor capacity, potential future price hikes, confidentiality of data.



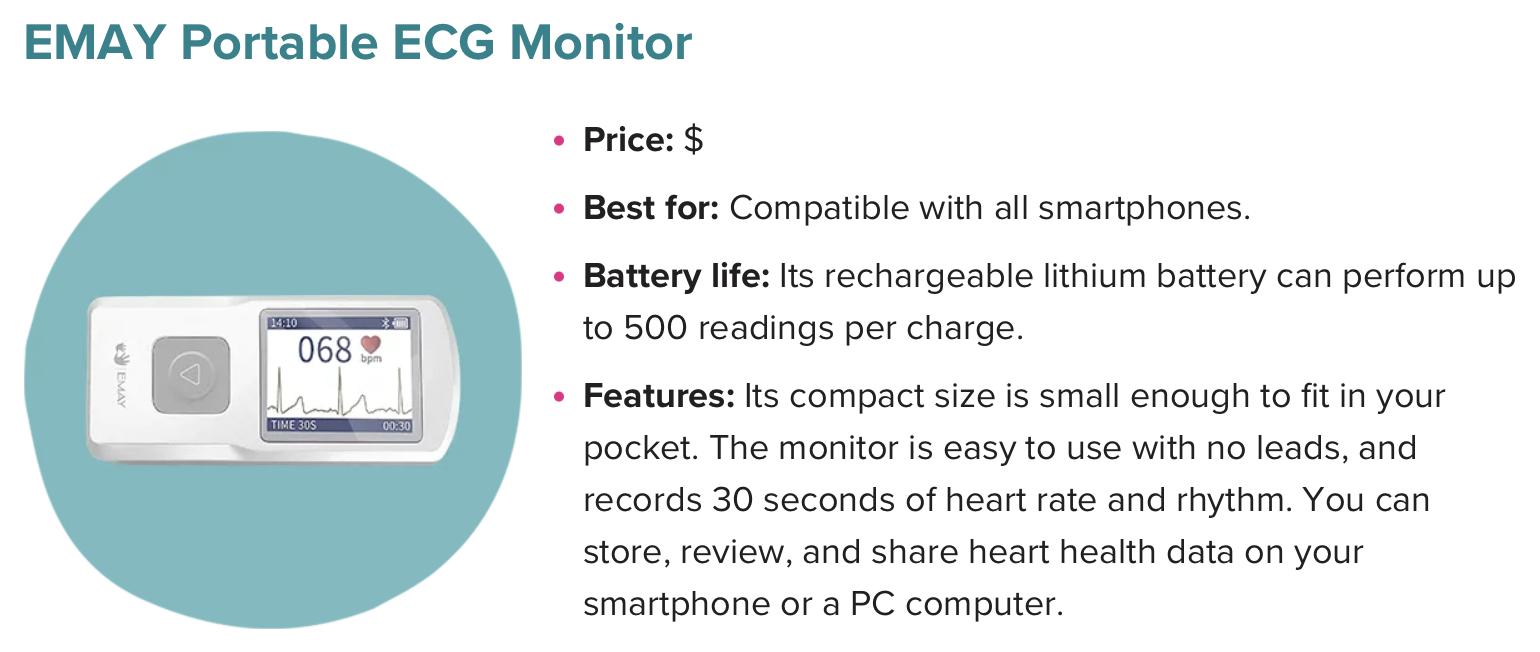
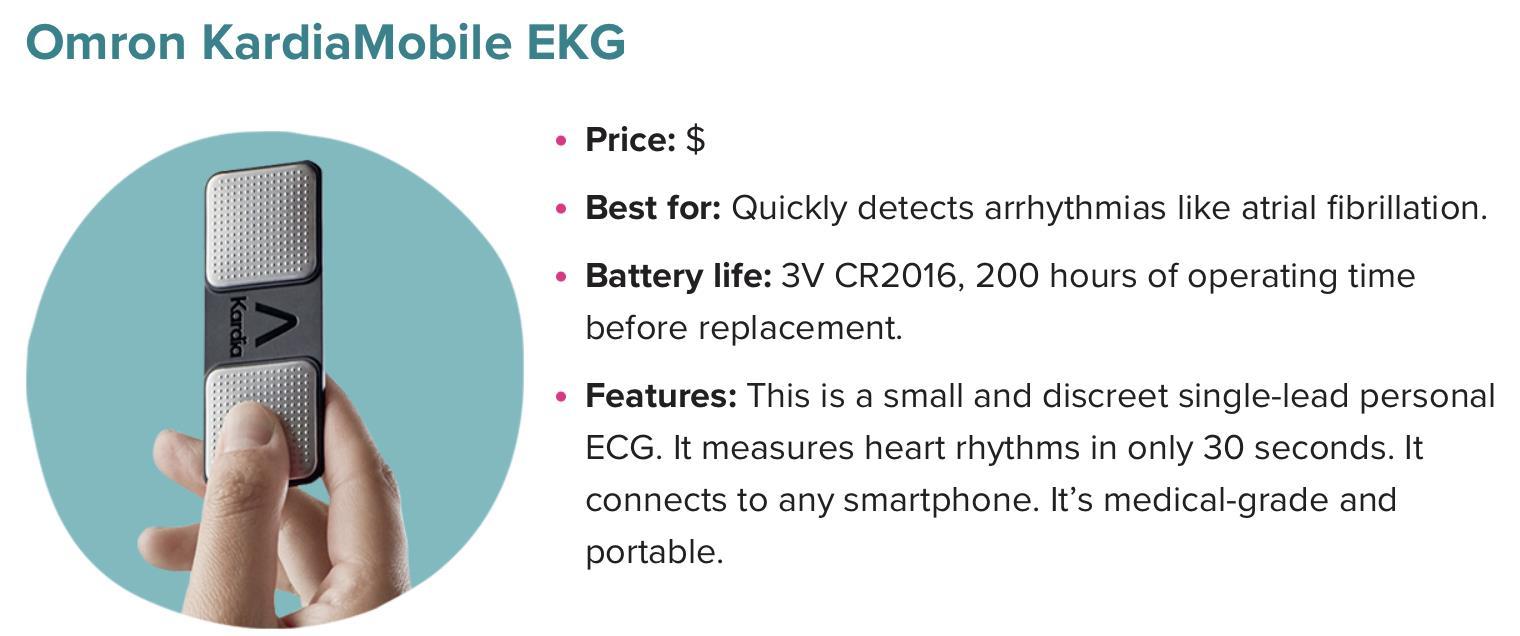
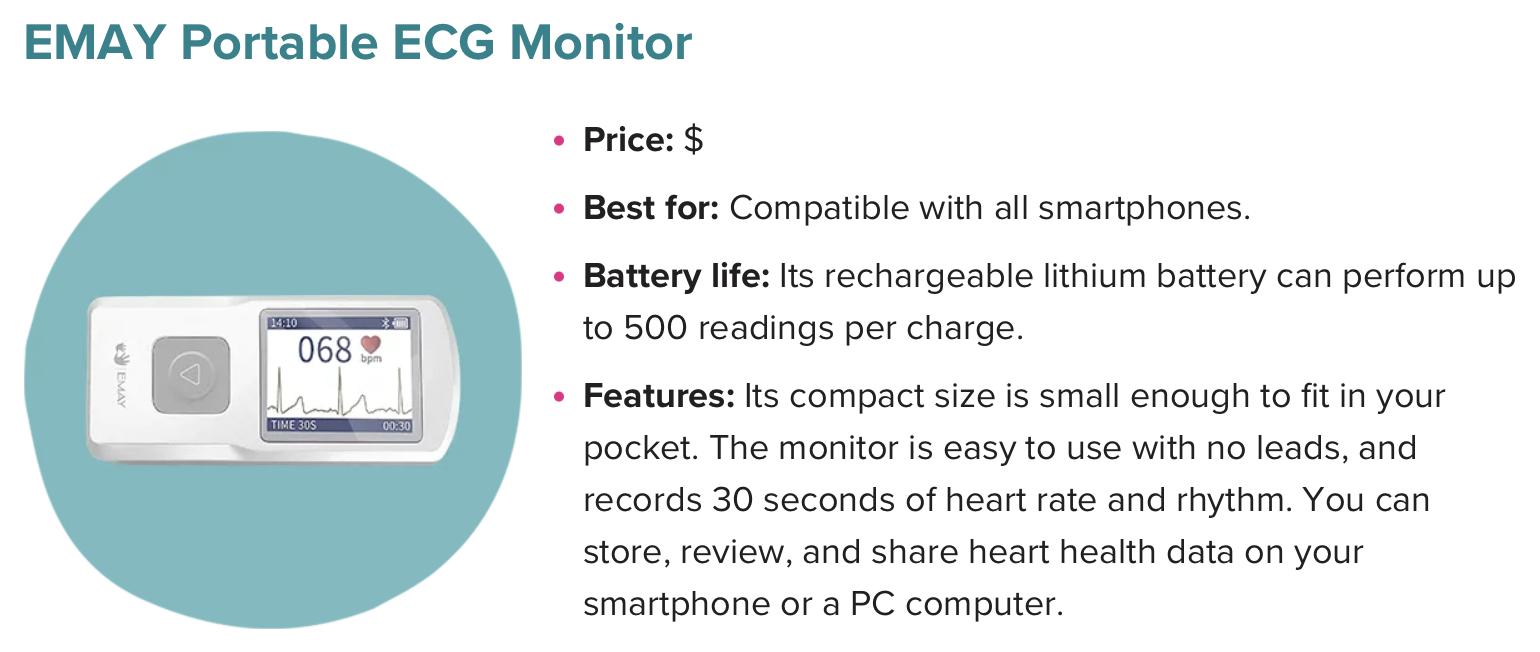
Wearable health tech/Commercial monitors For Patient Led Monitoring • It is critical to differentiate between heart rate monitors vs Devices that can record an ECG rhythm strip. • Heart rate monitors can be very inaccurate, particularly with ectopic beats when they often inappropriately diagnose bradycardia. They can be useful in identifying prolonged inappropriate high heart rates e.g. AF. • Wearable devices that can collect an exportable ECG strip • Apple Watch (series 4 and above) • Fitbit Sense or Charge 5 • Samsung Galaxy Watch 3 • Small portable devices that can collect ECGs independently or paired with a smart phone • EMAY Portable ECG monitor • Omron KardiaMobile EKG • Wellue Portable EKG monitor
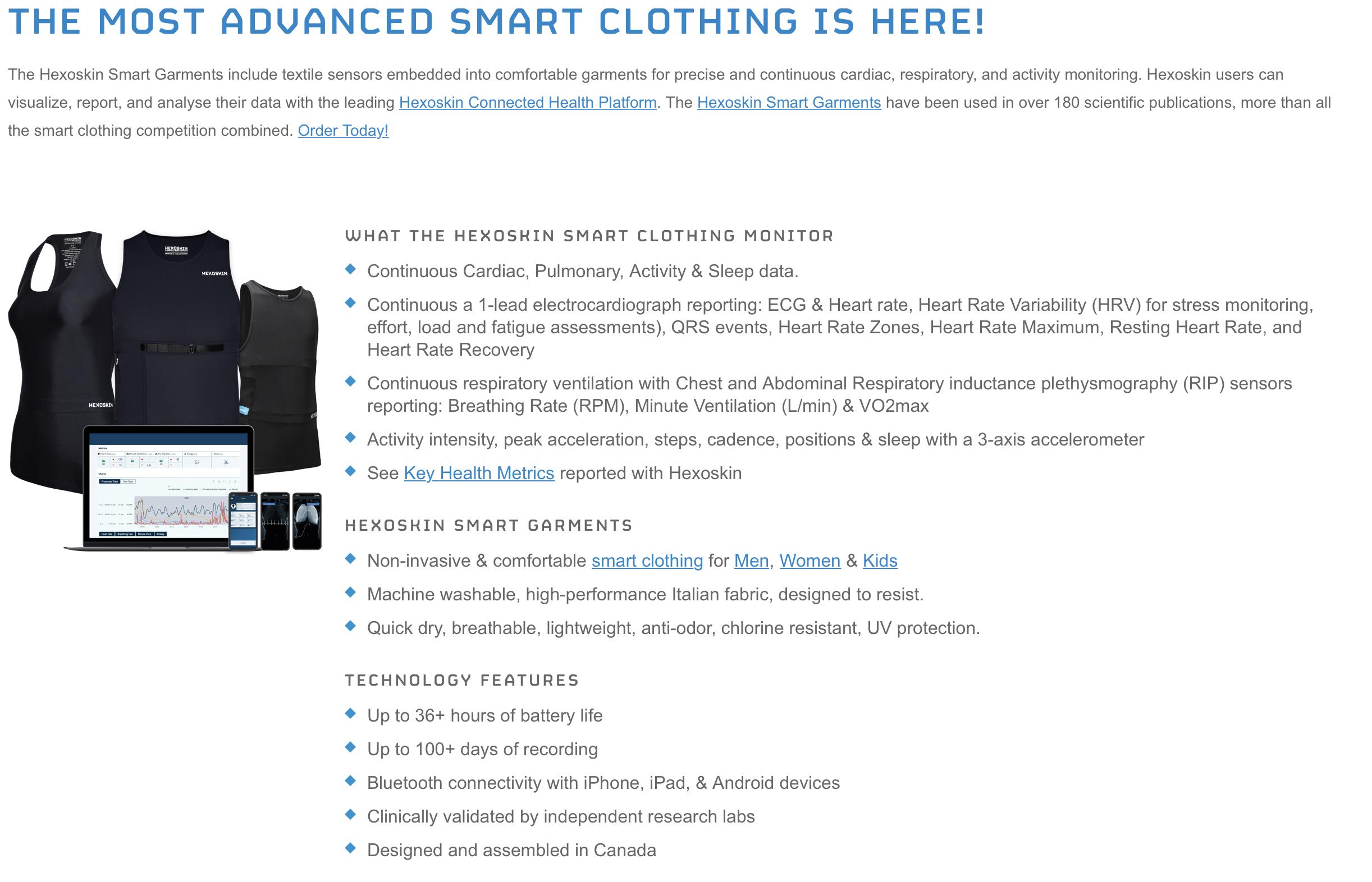




Strengths and pitfalls of patient-led ECG monitoring. Strengths • Long term monitoring period • Primarily symptomatic recordings • Enthusiastic patient involvement • Frees hospital resources Weaknesses • No good for syncope/asymptomatic arrhythmia! • Analysis/administration time (which may be considerable) may not be remunerated. • Cost of device is currently born by patient – potential for access inequalities. • There may be a noticeable lack of filtration between receiving clinician and patient • Obsessive and compulsive patients / anxiety disorders • Poor quality ECG traces
To Summarise
• Please bear with us when it comes to waiting times for cardiac diagnostic tests. We are working on it!
• Be judicious in choosing whom to refer for both rhythm monitoring or echocardiography.
• Consider whether either simple reassurance of potentially a patientled rhythm monitoring strategy might be the best option for your patient.
• Watch this space for arrival of Patch-based monitoring.
Acknowledgements
• Michelle Bayles – Team leader for clinical physiology • Data provision, ongoing service management and development. • Tracey Cumming – Senior cardiac physiologist • Community service development • Cardiac physiology team – a persevering bunch! • Generally working hard to get through it all and still smiling. THANK YOU!
Community Orthopaedic Triage Service Update(s)
 16th
2022 Sonya Ginty, COTS Physiotherapist
16th
2022 Sonya Ginty, COTS Physiotherapist
November
What is COTS?
•
Physiotherapy led Orthopaedic assessment clinic • Bay wide, community locality service • Pilot to project to business as usual • Recognition of need for nonsurgical management pathways

referrals • Triage all non-acute referrals from all sources to Orthopaedics • Exception HSC & Fractures • eGrading • Improved communication
Orthopaedic
October 2022 535 non-acute referrals received ➢ 50% ALL spines ➢ 60% of ALL hips & knees 12% expedite requests September 2022 624 non-acute referrals received ➢ 50% ALL spines ➢ 60% of ALL hips & knees 11% expedite requests Orthopaedic Referral Statistics
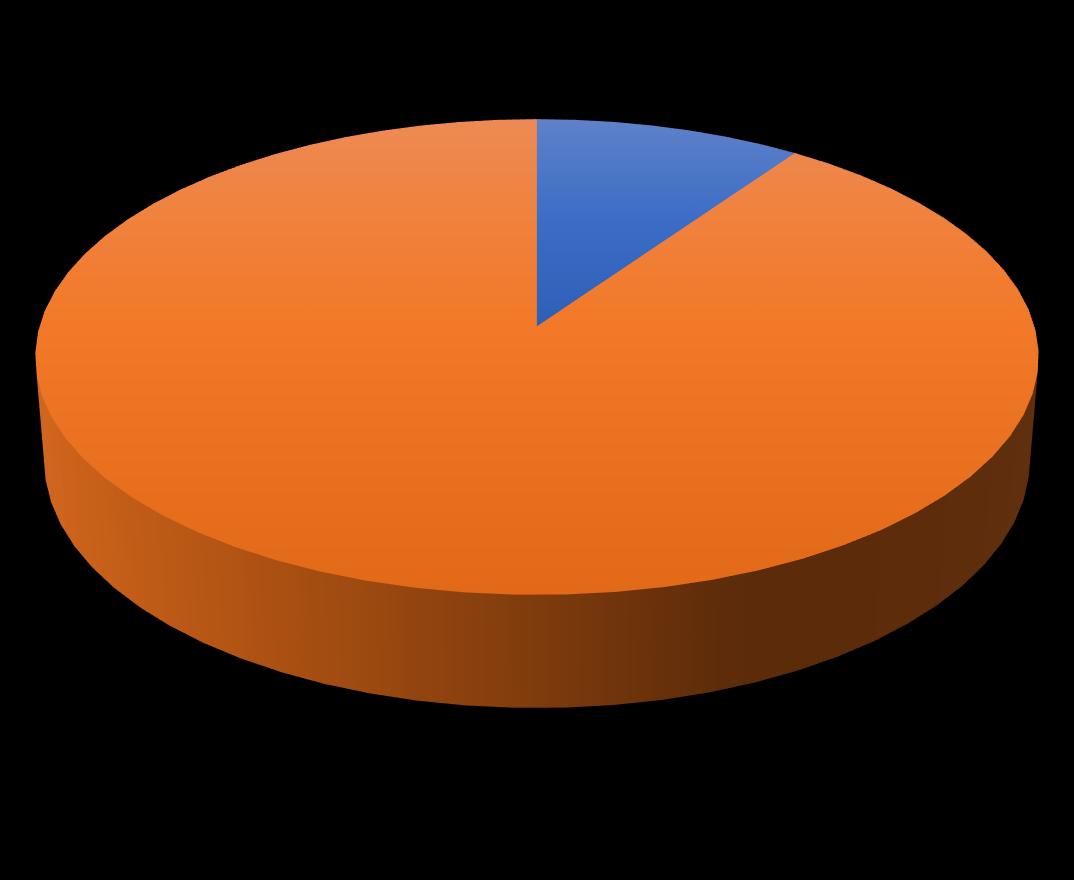
• Current wait 15 days for COTS assessment • Communication typically within 1 week • 70%
appointment
•
Patient journey
of patients seen in Physiotherapy led Orthopaedic clinics, managed independent of need for Specialist
• 30% referred to FSA clinic(s)
> 6-month wait for routine assessment • Can fast track based on clinical urgency • MRI pilot – direct access for imaging at time of COTS assessment, level playing field
management OA & AWA 15% of patients referred to AWA 10-week combined education & exercise for patients with OA hip & knee Private provider throughout BOP Access is via Orthopaedics, COTS or MSK Physiotherapy Limited funded places but acknowledgement that primary care access would be helpful in future Thank you for sending those earlier in their journey!
Non-surgical
Patient Satisfaction Survey

• 6- week data collection regarding satisfaction including assessment of cultural needs • > 80% patients gave positive feedback • Relates to their experience of wait times, location, understanding of service, quality of care received • Felt confident in the clinicians knowledge
decision
and their involvement in
making & management plan

1. Exploring spinal pathway 2. Anaesthetic team on preoptimization & identification earlier in patient journey 3. Hand pathway 4. Online resource/Webpage Future direction:

Contact us with feedback, comments or questions?
catherine.willis@bopdhb.govt.nz COTS.clinic@bopdhb.govt.nz
PHO Clinical Update

Dr Claire Isham, Clinical Director, WBOP PHO Dr James Peckett, Clinical Advisor, WBOP PHO
Covid Update: Evusheld
309 eligible patients in WBOP. 152 patients with Heamatology who will administer Evusheld at the hospital. 138 patients to be managed by primary care, spread across most WBOP practices.
Practices will be provided with their patient list via the PHO portal tomorrow
Specialist services will send letters to the 138 patients early next week
Patients will be advised to contact their general practice for assessment and administration.
Evusheld Claiming guide available on PHO Covid page includes links to eligibility criteria, administration process and resources, clinical information, as well as the claiming process.
https://portal.wboppho.org.nz/images/documents/Evusheld_claiming_guide_22.pdf
CARE Children’s Asthma Study
• MRINZ are running a trial to look at whether AIR therapy is superior to the current management strategy of separate SABA and ICS inhalers in 5 - 15-year-olds, and are asking for GP support to recruit
• CARE study - 1 page summary by WBOP PHO – Issuu
• To assist with recruitment practices can do their own query, build, and mail merge with up to $500 reimbursement, or the research team can do this from the practice.
• Contact Atalie.Colman@mrinz.ac.nz if you would like to contribute

DECIDE.org.nz National Abortion Telehealth Service

• 0800 DECIDE www.decide.org.nz
• Offers free confidential contact with trained specialists. They can also connect people to abortion providers in their area or arrange an early medical abortion (EMA) over the phone.
ACC claims for maternal birth injuries
• From 1 October 2022 our accident cover includes specific injuries birthing parents can experience from the beginning of labour through to delivery of the pēpi/baby.
• That means those who give birth from 1 October 2022 onwards and who have a covered injury can access the appropriate support, treatment, and care through the Accident Compensation Scheme to help their recovery and return to independence.
• Maternal birth injuries (acc.co.nz)
General update on what can be found on the WHOP
PHO Portal
Mental health resources Covid resources Programme information
Special Ukraine Policy

health assessment
resource for
Special
Visa
Please contact your Network Liaison for claiming information
Primary & Community Care Cyber Security Maturity Assessment – closes 25 November Assessment for Micro-Small primary & community care provider
CSMAms@22 Assessment for Medium-Large primary & community care provider
CSMAml@22
Visa Holders From 17 October 2022, persons from Ukraine holding a 2022 Special Ukraine Visa are eligible for a one-off initial 45-minute
fully funded by Te Whatu Ora – Health New Zealand. Health Pathways
2022
Ukraine
Holders Final 13 Oct 2022 by WBOP PHO – Issuu
NSTeam@wboppho.org.nz
Link: https://tewhatuora.jotform.com/222777366131963 Password:
Link: https://tewhatuora.jotform.com/222815804606960 Password:

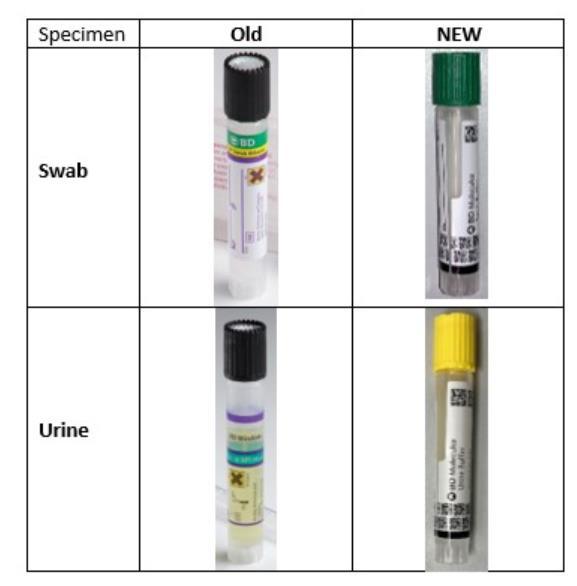
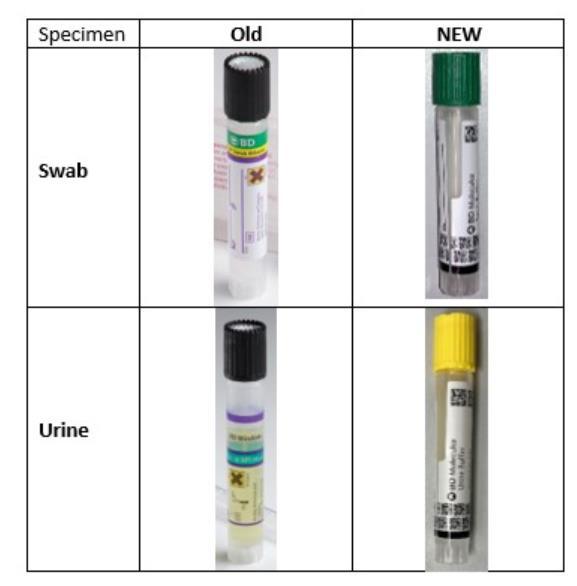
STI Collection Kit Change – Pathlab • Clinicians must transition to the new STI kits/tubes by Friday 18th November. Any of the old black cap STI tubes received from Monday the 21st November will result in a recollect request as the old Viper XTR instruments will be turned off and these tubes are not compatible with the new BD COR instrument. STI Collection Kit Change | News (pathlab.co.nz)
CME Update
Dr Claire Isham Clinical Director
Western Bay of Plenty Primary Health Organisation



CME/CNE Update 2023
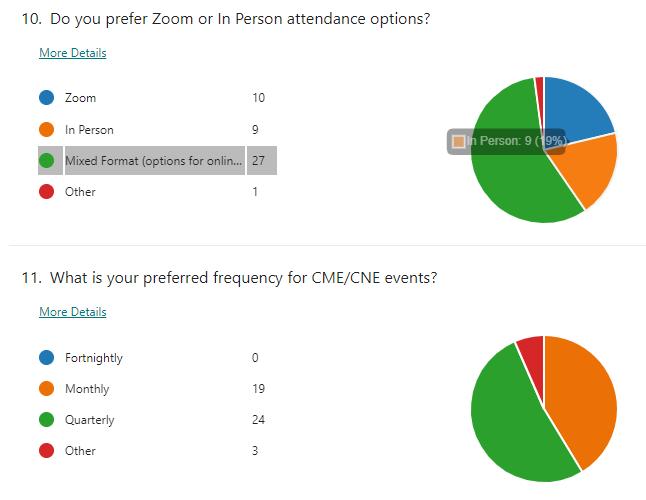
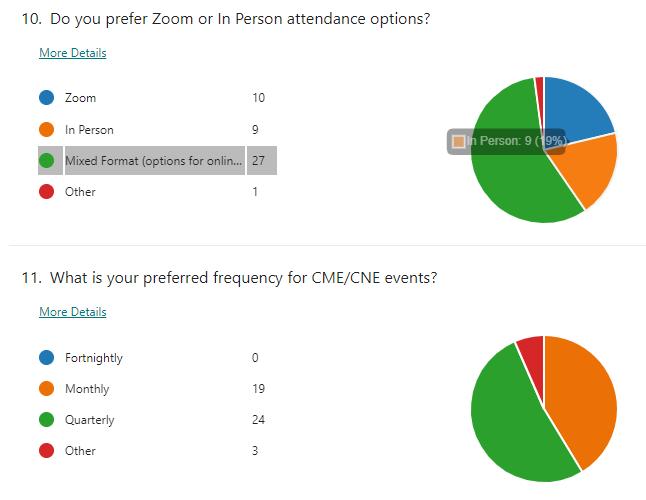
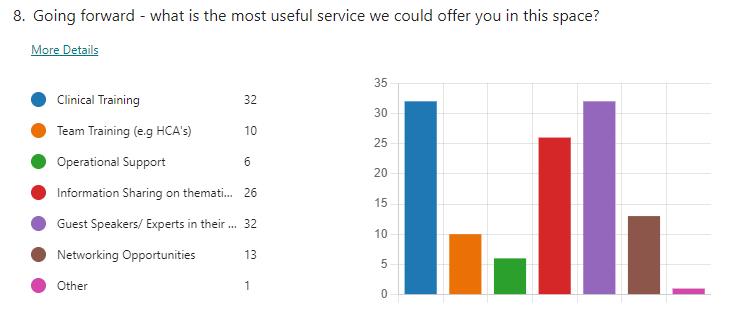
General update • Thank you to everyone who completed the survey • 47 Respondents, including 21 nurses (45%) • The PHO was successful in it’s recent RNZCGP CME audit
• CME/CNE is valued, with responders overwhelmingly in support of the continuation with the current CME offered in both formats, face-to-face and via Zoom, with the added benefit of the zoom recordings being made available after events.

Survey Feedback
Frequency
continue with Monthly events so we can deliver a variety of subjects across the year
• There is a preference for Evening events (35/58 responses) •
–
Survey feedback continued
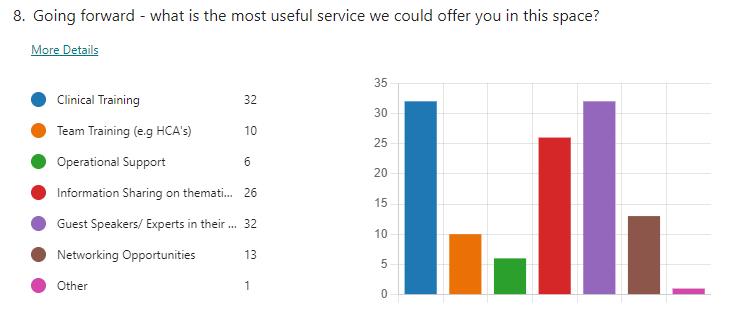
• Content - All topics identified through this survey are now on our planning list • Survey participants commented positively on having access to relevant and essential clinical training and guest speakers or experts from various fields of the profession.

Next Steps

Next Steps
• Developing a CPD Framework which will include Core Education, Education opportunities aligned with Foundation Programme and Professional Accreditation requirements as well as other topics identified by the Network.
• Further strengthening our focus on providing quality CME by providing our presenters with a new set of guidelines to ensure participants of CME/CNE get the most out of each session.
• Following feedback , we are reviewing how events are communicated and advertised across the networks PHO Newsletter, Portal Calendar, Social Media, direct email
• Expanding opportunities for learning opportunities to include nonclinical roles in GP practice.

IV Iron Programme
Review of activity and Programme updates July 2021 to June 2022

➢ Review uptake and utilisation of the programme following initiation in July 2021

Recap of Programme Programme purpose • Safe effective treatment of iron deficiency anaemia in primary care • Early correction avoiding clinical consequences • Reduce demand on Medical Day Stay Unit (MDSU) Funded under Acute Demand Service Agreement 400/annum (Allocation=300p.a WBoP & 100p.a EBoP)
https://schedule.pharmac.govt.nz/2022/11/01/SA1840.pdf
https://pharmac.govt.nz/news-and-resources/consultations-and-decisions/iron-infusions-in-the-

Target population/Eligibility ➢ > 14 years Meets Pharmacy SA criteria for Ferric Carboxymaltase (Ferinject®) AND CSC Holder OR High Needs (Māori, Pacific or Quintile 5) OR Already receiving IV iron in MDSU
Pharmac
community 2/

Review July 2021- June 2022 Identified Use By: ➢ethnicity, age, gender ➢Those already under MDSU ➢Referral source ➢IV Iron indication- new dx or existing MDSU patient Identified overutilisation of funding allocation in WBoP ➢Total Claims WBOP (incl 3 NMO) 317 ➢17 over annual agreement

Cont…….. ➢WBoP- 2 practices NOT claiming 1 has buddy system due to lack of staff avail / skills / space 1 doing high numbers of self-funded ➢NMO minimal numbers
Review does not quantify the self-funded infusions given in primary care where patient meets SA criteria but not the PHO IV Iron criteria
➢

June 2021- July 2022
0 20 40 60 80 100 120 140 5-14yr 15-24 25-44yr 45-64yr 65+yr Utilisation by Age Range: ➢ Highest utilisation >25 44yrs 171 (54.4%) 90 (28.7%) 15 (4.8%) 38 (12.1%) 0 50 100 150 200 250 300 350 NZ Euro Maori Pacific Other Utilisation by Ethnicity: ➢ Programme has a specific High needs eligibility
IV Iron Claiming Data
Utilisation by Gender

➢Prominent female use as expected with 83.3% utilisation 51 (16.2%) 263 (83.8%) 0 50 100 150 200 250 300 Male Female


Referrer to programme ➢Majority Primary Care 87.58% Primary Care 275(87.58%) Secondary 38(12.1%) Other 1(0%) Request Initiator Primary Care Secondary Other
Of those pts referred to programme by secondary care…….
Secondary initiation utilisation by age

Majority European ➢ >65yrs
0 5 10 15 20 25
15-24 25-44 45-64 65+
NZ European: 23 Māori: 4 Other: 7 22
➢

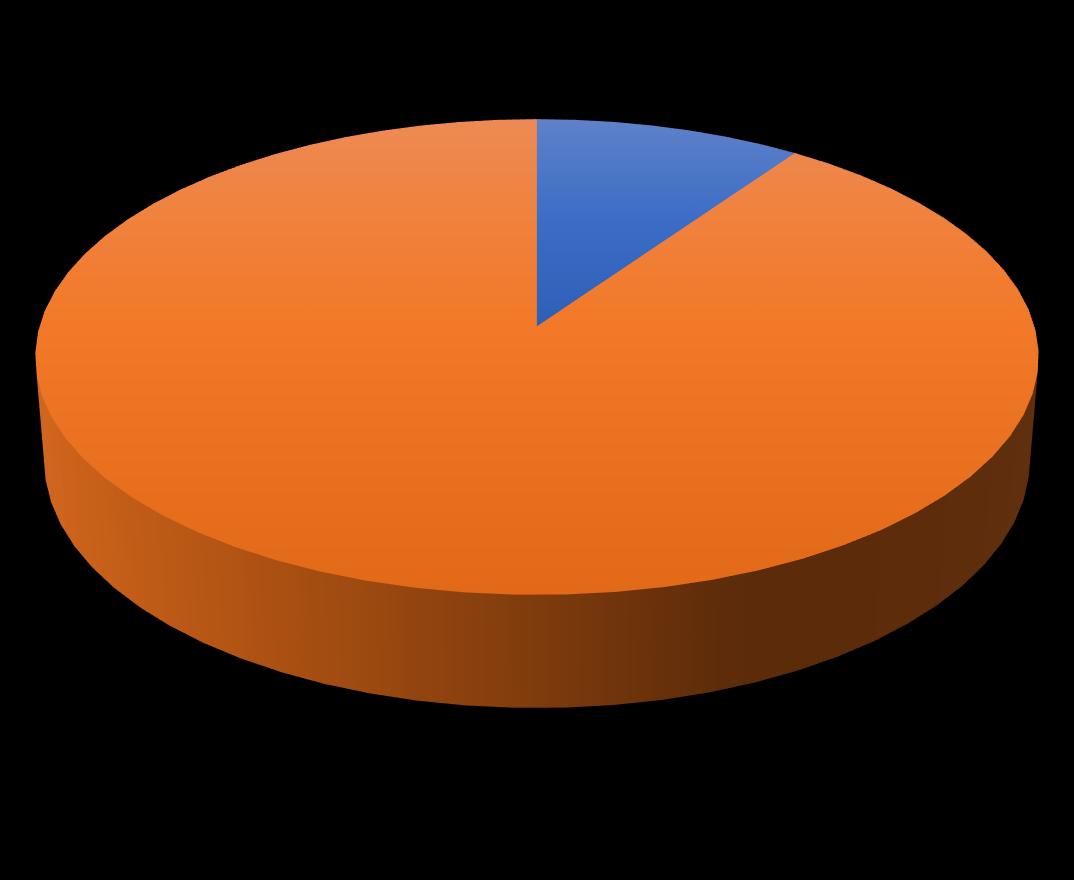
Receiving IV iron through MDSU ➢<10% ➢26 European ➢4 Other YES 30, 9.55% NO 284, 90.45% Yes No

Changes to programme ➢Amendments identified at bottom of document ▪ Option of IV iron bolus (undiluted) injection ▪ Dose guide included if Hb >140 ▪ Contraindications updated ▪ Changes to monitoring requirements pre during/post IV iron ▪ New Referral Process document into MDSU Must include details ▪ Baseline + Optional Blood tests ▪ No foetal monitoring required ▪ Ph/send Bpac ‘advice’ to obstetrician re administration during preg ▪ Repeat Hb and iron 6-12 weeks post in at risk pts ▪ Details for pts to contact pre assessment clinic if pre procedure administration ▪ Patient observed for first 5 mins of administration ▪ Updated Ferinject® drug data sheet ▪ New patient resource

Moving Forward ➢New document created for secondary care team- service/eligibility ➢Work on increasing capacity of programme ➢Review current agreement with Planning and Funding Hauora a Toi BOP re eligibility and funding ➢Work with Hauora a Toi BOP/Renal team-update Bpac referral form ➢Continue to work on collation of all Ferinject® scripts to identify numbers self funding
Resources
➢PHO Portal
https://portal.wboppho.org.nz/iron-infusionResources/
➢MidlandHealth pathways
https://midland.communityhealthpathways.o rg/288018.htm

➢Pharmac

https://schedule.pharmac.govt.nz/2022/11/0 1/SA1840.pdf
https://pharmac.govt.nz/news-andresources/consultations-and-decisions/ironinfusions-in-the-community-2/
Kia tau
Karakia whakamutunga (closing)
Kia tau kia tātou katoa Te āio, te aroha me te marutau Tīhei Mauri Ora
May peace, love and safety Be upon us all Let there be life

Thank you for joining us!










 Dr Rob McIntosh MD FRCP
Dr Rob McIntosh MD FRCP












 16th
2022 Sonya Ginty, COTS Physiotherapist
16th
2022 Sonya Ginty, COTS Physiotherapist