Dr. Valerie Gorman Be proactive in your healthcare
Dr.
Valerie Gorman MD, FACS
I am dedicated to offering my patients an advanced, personalized and targeted approach to breast surgery and the treatment of breast cancer.


By AUDREA MEDINA Managing Editor
“Find a problem and fix it.” That personal philosophy led Dr. Valerie Gorman into the surgical field where she discovered she also liked the idea of maintaining a long-term relationship with her patients. This is why she decided to specialize in breast cancer surgery.
“In my field, I get to walk with a patient through a very difficult time, help them fix a problem, and then continue to check in with them through the years. I get to know them, and their families, well.”
During her 20-year career, Dr. Gorman has seen changes in the way breast cancer is discovered, treated, and reduced.
Cancer treatment no longer comes in a one-size-fits-all plan. When she first began her career, both chemotherapy and radiation were primary in the plan of attack. It’s different now.
Dr. Gorman explains, “Chemotherapy, though, for example, may actually not respond to certain tumors, and because of the new advances in testing, I can tell my patients that they don’t have to have it because there’s a better option to target their specific type of tumor.” Sometimes lumpectomies, mastectomies, and prescription drugs can eradicate a tumor without the need for more aggressive forms of treatment.
Each plan is personalized and individual, and Dr. Gorman shares that much of the plan incorporates the patient’s goals. She talks patients through their fears and concerns, like whether chemo worked for a family member, how the patient feels about it, and also considers things like post-surgical cosmetic reconstructive goals. She also educates her patients on recidivism rates and which treatment options could best reduce risk further down the line.
She shared, “Some patients may not want chemotherapy, but when they realize that it will reduce the risk of recurrence in five or 10 years, they’ll decide this See GORMAN, Page 7


Catching it early ... Jamie Van Eyck’s journey through breast cancer
By AUDREA MEDINA
Managing Editor
When doctors told Jamie Van Eyck she had breast cancer, she was stunned. “You go from doing just fine one moment to realizing you’re going to need surgery,” she said. “It’s very scary and overwhelming.”
Van Eyck, a professor at Baylor University, had been diligent about scheduling annual mammograms since turning 40. Her mother had insisted on it, reminding her daughters never to skip a year. For four years, every scan had come back normal. Then, at age 44, her doctors noticed calcifications scattered across her left breast. A second mammogram, followed by an ultrasound and biopsy, confirmed the diagnosis: ductal carcinoma in situ (DCIS), a common but serious early form of breast cancer located in the milk ducts.
The words left her reeling. “Suddenly you have all these paths in front of you—finding the right doctor, scheduling surgeries, educating yourself as much as possible,” Van Eyck said. “It’s a lot to take in.”
In Waco, where she lives, Van Eyck quickly met with a breast surgeon, reconstructive surgeon, and oncologist. She settled on Dr. Valerie Gorman, a breast surgeon in her area, but friends urged her to seek out specialists in Dallas, too. That’s how she found Dr. Jason Potter, a reconstructive surgeon and was very pleased with the level of care she received from each. “Dr. Gorman was marvelous,” Van Eyck said. “She explained what to expect and gave me the statistics for different
choices. That information helped me make the decision that was right for me.”
For Van Eyck, that decision was to undergo a double mastectomy. “Some women choose the more minimal surgery, others want everything removed,” she explained. “It’s overwhelming because you want to be told what to do, but there isn’t one right answer.”
Surgeons removed both breasts in November 2023. Lab results later showed the cancer had stayed contained, with only one small invasive spot. Thankfully, her lymph nodes were unaffected, meaning Van Eyck avoided chemotherapy and radiation. “If I had waited a few more months, that invasive spot might have grown,” she said. “Catching it early made all the difference.”
By June 2024, her reconstruction surgery was complete. Alongside recovery, Van Eyck began taking Tamoxifen, a medication that reduces estrogen absorption. Because her cancer was estrogen-fed, the drug lowers her risk of recurrence. “It comes with menopause-like side effects, but I’ve been fortunate,” she said.
Emotionally, Van Eyck describes two phases: the anxious buildup to surgery and the relief that followed. “Leading up to it, I had a ton of anxiety,” she said. “But once the mastectomy was over, I felt good. When the lab results came back and confirmed everything was removed, that was the best possible outcome.”
Follow-up visits with her surgeon were frequent at first—every three months, then every six. Today, she sees her doctor once a year. With no breast tissue remaining, mammograms are

Jamie Van Eyck with husband, Jose, and children, Josephine and James.
no longer part of her routine, but she remains vigilant with self-exams and checkups.
Looking back, Van Eyck sees her story as a lesson in vigilance. “My whole goal after being diagnosed was to tell as many people as I can: this is real, and early detection matters,” she said. She stresses that family history is not the only factor. “One in eight women will develop breast cancer. More and more women are being diagnosed without any family history. Early detection is your best defense against harsher treatments and better ensures a healthy, cancer-free life.” She also wants women to know about the lesser-known warning signs of breast cancer. Some, she said, are subtle changes that are easily dismissed but should be taken seriously. Women typically begin getting mam-

mograms at age 40, but many will develop breast cancer in their 30s and even 20s. Knowing these early warning signs, Van Eyck emphasizes, is especially important for younger women who are not yet receiving annual screenings.
Her advice is simple but urgent: get yearly mammograms, even if you’re afraid or think you’re not at risk. “These exams are covered by insurance. To not take advantage of that is a real risk for women,” Van Eyck said. “If I hadn’t stayed on schedule, my outcome might have been very different.”
Nearly two years after her diagnosis, Van Eyck describes herself as grateful—for her doctors, for the timing, and for the outcome. “I feel very fortunate and blessed to have caught it early and to have had such wonderful care,” she said. “It really is a blessing from God.”
Courtesy photo
The Silent Struggle Men with Breast Cancer
By JAEDYN STAPLETON
Sun Staff Writer
Every October, the world turns pink. Ribbons line storefronts, walks are organized, and stories of brave women fill our feeds. We think of mothers, daughters, sisters, and wives. But hidden behind the sea of pink is a truth that rarely gets spoken; men get breast cancer too.
It’s a truth that shocks most people. Breast cancer is seen as a “women’s disease,” but thousands of men are diagnosed every year. Most never saw it coming. They didn’t know the signs. They didn’t think it was possible. And because of that, many are diagnosed late – when treatment is harder and the fight is steeper. Imagine it: you find a lump on your chest, but you brush it off. You tell yourself it’s nothing because breast cancer isn’t something men get. Weeks turn into months, until suddenly it’s not nothing. It’s cancer, and now you’re fighting for your life against a disease you never thought would touch you.
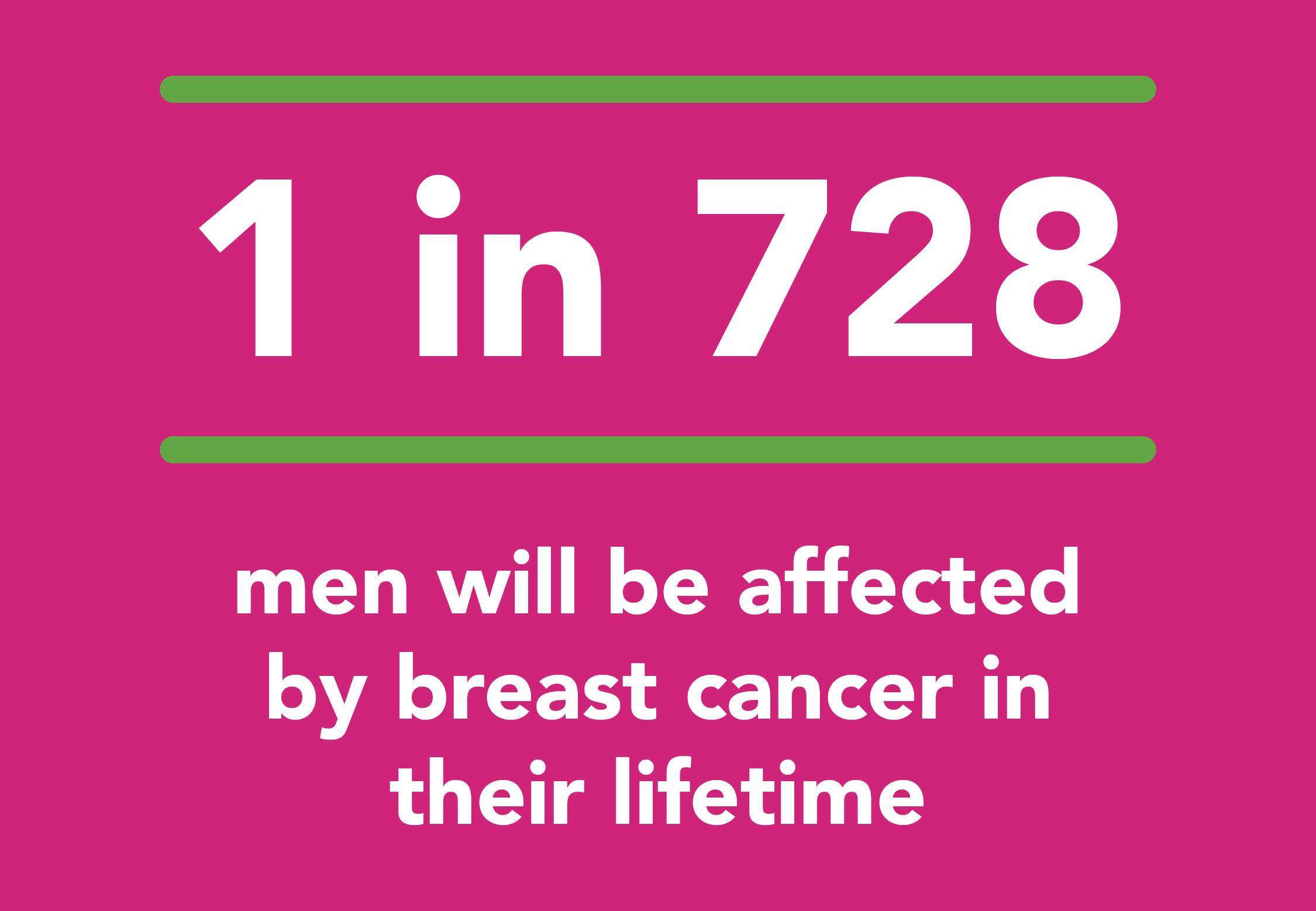
For the men who live through it, the battle is more than physical. It’s lonely. It’s isolating. It’s a diagnosis that often comes with silence, embarrassment, and even shame. Breast cancer walks, support groups, awareness campaigns – almost all of them are designed with women in mind. Men are left wondering where they fir in, or if anyone will ever understand their story. But awareness matters. Awareness saves lives. Male breast cancer may be rare – about 1 in 726 men will face it in their lifetime – but rare doesn’t mean impossible. And the truth is, when it is caught early, survival rates improve dramatically. So, this October, when you see pink, remember that breast cancer doesn’t just touch woman and silence can cost lives. The more we speak, the more we see, the more we save. Pink may be the color of the month, but the fight belongs to all of us.

How does it happen? What Causes Breast Cancer?


By JAEDYN STAPLETON Sun Staff Writer
Every October, pink ribbons appear everywhere – on storefronts, football fields, even coffee cups. They’re reminders of the women and families touched by breast cancer, and symbols of hope for a cure. But behind the ribbon is a question that scientists are still working to fully answer: what actually causes breast cancer?
The honest truth is, there isn’t a single cause. Instead, breast cancer develops from a mix of factors – some we inherit, some connected to our hormones, and others tied to lifestyle choices. And sometimes, it comes down to changes in our DNA that happen for reasons we still don’t completely understand.
When Genes Go Wrong
Our bodies are built on instructions written in DNA, passed down from our parents. Within that DNA are genes that act like managers – some encourage cells to grow and divide, while others put on the brakes when growth gets out of control.
But when those genes are damaged or “mutated,” things can go wrong. For example:
• Oncogenes are like a stuck accelerator pedal, telling cells to keep dividing when they shouldn’t.
• Tumor suppressor genes are supposed to hit the brakes, but when they stop working, cancer cells can multiply unchecked.
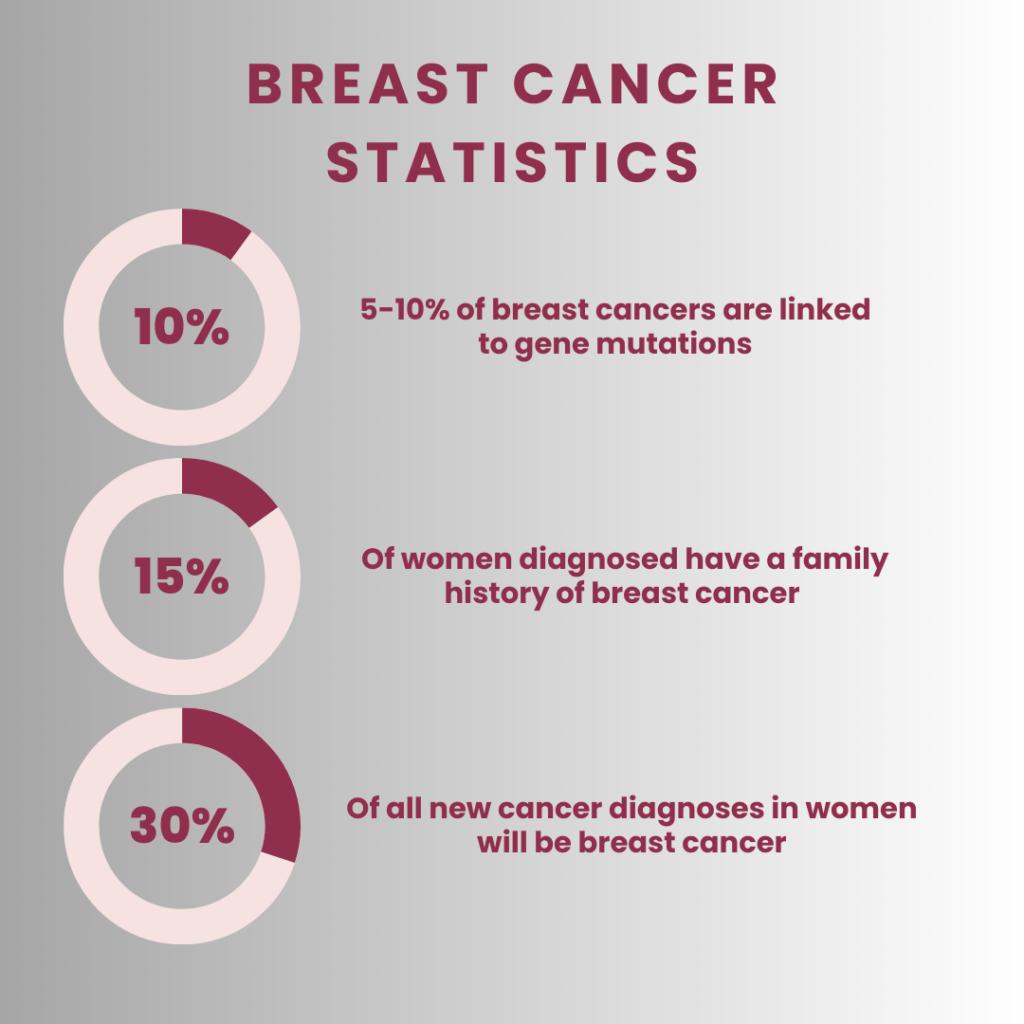
Some mutations are inherited, like the well-known BRCA1 and BRCA2 genes. Women who carry changes in these genes face a much higher lifetime risk of breast and ovarian cancer. But here’s something surprising: according to the American Cancer Society, only about 10% of breast cancers are linked to inherited mutations.
See CAUSES, Page 8



By JAEDYN STAPLETON Sun Staff Writer
For many, cancer is an abstract fear, a disease seen on television, in headlines, or quietly endured by friends and family. But for Deborah Leatherwood, it became painfully personal. When her sister-in-law was diagnosed with ovarian cancer, the devastating news shook her world. “I knew about ovarian cancer in theory,” she recalls, “but I didn’t know anything about the signs, the severity, or how deadly it really is. You don’t hear about it.”
In the months that followed, Deborah witnessed the immense toll ovarian cancer takes not just on patients, but on families navigating a healthcare system that often leaves them adrift. Her sister-in-law passed away just eleven months after her diagnosis, a loss that spurred Deborah into action. Out of grief and determination, she founded what is now the Leatherwood Foundation, a nonprofit dedicated to raising awareness, funding research, and providing direct support to those affected by gynecologic cancers.
The Leatherwood Foundation’s Call to Help... From Struggle to Strength


“Our goal is simple,” Deborah says. “Knowledge saves lives. And right now, there is too little knowledge and too few resources for people battling ovarian and other gynecologic cancers.”
Gynecologic cancers – including ovarian, cervical, and uterine cancers –are among the deadliest for women, yet they remain largely absent from mainstream awareness campaigns. Breast cancer dominates the conversation with its pink ribbons and high-profile fundraising drives, but ovarian cancer suffers in silence. “If you don’t have knowledge,” Deborah emphasizes, “how are you going to survive?”
The Leatherwood Foundation confronts this gap head-on. From grassroots fundraising to patient advocacy, Deborah and her team help families navigate resources, treatments, and financial aid programs. They fund grants directly to patients forced to make impossible choices: chemotherapy or groceries.
See LEATHERWOOD, Page 8


GORMAN
Continued from Page 2
is the best option and determine that it’s worth putting up with the effects of not feeling 100% during the course of that treatment.”
Dr. Gorman acknowledges it is important for patients to be invested in the process by joining with her team in decision-making. This collaboration gives the patient a measure of autonomy and control. It’s a whole-person approach to health care during what is an uncertain and often frightening time.
“They’re learning a whole new vocabulary with new terms and new meanings, and this is while they’re having to make hard decisions about things they’re just beginning to understand.”
Dr. Gorman, according to one of her patients, Jamie Van Eyck, did an excellent job explaining her options and helping her pick the treatment plan.
“Dr. Gorman explained everything to me where I understood and felt ready to make the best decision for my health.”
Occasionally, it happens where there is an unplanned boon for the patient.
“One of the unexpected benefits in the post-surgical reconstruction process,” stated Dr. Gorman, “is that a woman might have wanted a breast reduction for many years, and in certain cases, this can become her reali-
ty. It is encouraging to see how excited some of these women are when they come back to see me for a check-up and talk about it.”
Primarily, Dr. Gorman wants women to understand the risks as well as the facts about breast cancer. 85% of American women who get what she calls “sporadic breast cancer” have no genetic predisposition.
“I have patients come in all the time telling me they have no history of breast cancer in their families, they eat right, exercise, don’t drink or smoke, and are blown away that they have a cancerous tumor.”
Only 15% of women who get breast cancer are genetically predisposed, so Dr. Gorman stresses that women must reduce their risks by being proactive in their own healthcare.
She added that most insurance companies cover the cost of a yearly mammogram, and for those who do not have insurance, many places offer reduced-price or free screenings.
In and around Ellis County, Hope Health, Baylor Scott & White, as well as Texas Breast and Cervical Cancer Services offer assistance for these types of screenings.
“Reduce the risk of breast cancer by doing all of those healthy things like eating right and exercising,” ends Dr. Gorman, “but be proactive in getting those mammograms. Early detection is key to early treatment.”

Early warning signs of breast cancer can include:
Changes in the breast:
• A new lump or thickening
• A change in the size or shape of the breast
• Dimpling or puckering of the skin
• Thickening or hardening of the breast tissue
Nipple Changes:
• Nipple discharge, especially bloody or clear
• Nipple inversion (turning inward)
• Scaliness, redness, or irritation around the nipple
Other Symptoms:
• Pain or tenderness in the breast
• Swelling in the armpit
• Skin changes, such as redness, warmth, or swelling
• Unexplained weight loss
• Fatigue


LEATHERWOOD
Continued from Page 6
“We don’t put a cap on what we can help with,” Deborah explains. “We do as much as we can and then help direct them to other resources.”
Beyond financial support, the foundation creates community connections and hope through events like their annual “When Pink and Teal Collide” fundraiser, featuring local performers and charity auctions. Each dollar raised supports both patient grants and scholarships, with every action intentional and every dollar stretched to its maximum.
The stories fueling Deborah’s work are deeply human. Women like Kendall, unable to see the full arc of their young lives without facing loss, and women like Angie, navigating health struggles and a confusing insurance system, highlight the urgent need for advocacy and guidance. “It’s unacceptable that America only sees pink,” Deborah says. “All cancers

deserve the same awareness and support. Knowledge is the most powerful thing we can give.”
The foundation also funds research through partnerships with organizations like the Ovarian Cancer Research Alliance, helping drive studies that could lead to earlier detection and better outcomes. For Deborah, research is not optional. It is essential. “If you don’t have research, you’ll never have a cure for anything,” she says.
Deborah’s work is both practical and deeply spiritual. She sees it as a calling to honor the memory of those lost and empower the living. “These are God’s children,” she says. “I will do everything I can to help them. We can’t cure cancer just yet, but we can give people hope, resources, and the chance to fight.”

Through perseverance, faith, and community collaboration, the Leatherwood Foundation has become more than a nonprofit – it is a lifeline, a beacon of
awareness, and a voice advocating for the silent cancers too often overlooked. Deborah leaves a simple but powerful message: knowledge saves lives, awareness empowers, and no one should face cancer alone.
CAUSES
Continued from Page 5
Most breast cancers, about 90%, result from acquired mutations. These are changes that develop during a person’s lifetime, sometimes from environmental exposures like radiation or harmful chemicals, and sometimes simply by chance.
The Role of Hormones and Lifestyle
Hormones, particularly estrogen and progesterone, also influence breast cancer risk. That’s why factors like early menstruation, late menopause, or never having children can affect chances of developing breast cancer. Researchers are still piecing together exactly how hormones fuel cancer growth, but the connection is clear. Lifestyle matters too. Choices around diet, exercise, alcohol, and weight don’t guarantee or prevent a diagnosis, but they can tip the balance toward lowering or raising risk.
What Research Is Teaching Us
Thanks to advances in science, women with inherited mutations now have tools that previous generations didn’t. Genetic testing, for example, can help identify high-risk women who may choose more frequent screenings or preventive steps. Scientists are also studying smaller, less obvious genetic changes that – combined with lifestyle and hormonal influences – may explain why breast cancer runs in some families even without BRCA mutations.
Why It Matters
When you strip away the science, here’s the heart of it: breast cancer doesn’t happen for just one reason. It often takes a combination of genetic changes, hormones, and lifestyle factors working together. And while we can’t always control the “why,” research gives us better ways to detect cancer early, when treatment is most effective. This October, as we honor survivors, remember those we’ve lost, and support ongoing research, it’s worth pausing to reflect: every discovery, every new insight, brings us one step closer to prevention, better treatments, and someday, hopefully, a cure.
*Information gathered directly from the American Cancer Society. What Causes Breast Cancer? | American Cancer Society