

















A Publication of the Torrance Memorial Health System
3330 Lomita Blvd., Torrance, CA 90505 310-325-9110
EDITOR
Jill Biggins Gerbracht
EXECUTIVE DIRECTOR MARKETING
Erin Fiorito
PUBLISHER, CREATIVE DIRECTOR
Vincent Rios
COPY EDITOR
CONTRIBUTORS
Lisa Buffington
John Ferrari
Diane Krieger
Marissa Minderler, MS, RDN
Jared Sayers
Laura Roe Stevens
Melissa Bean Sterzick
Nancy Sokoler Steiner
PHOTOGRAPHERS
Siri Berting
Philicia Endelman
Ed McClure
Michael Neveux
Mitchell Yee
Laura L. Watts Published by Vincent Rios Creative, Inc. VincentRiosCreative.com
©2026 Torrance Memorial Medical Center. All rights reserved. Reproduction or use in whole or in part without written permission is prohibited.
This publication is for informational purposes only and should not be relied upon as medical advice. It has not been designed to replace a physician's medical assessment and medical judgment. Always consult first with your physician regarding anything related to your personal health.
As we enter 2026, Torrance Memorial Health continues to move forward with purpose honoring a proud legacy of care while embracing the innovation and partnerships that will define our next chapter.
This February marks eight years of our affiliation with Cedars-Sinai, a collaboration that has expanded access to advanced specialty care while preserving the personalized, community-based approach that has long distinguished Torrance Memorial. That commitment is especially meaningful during American Heart Month, and this issue’s feature on advancements in cardiology highlights how our teams are delivering leading-edge heart care—from new heart failure therapies to expanded women’s heart health services—all close to home.

This issue also celebrates the people who shape the fabric of our community. On our cover, we are proud to feature world surf champion Mike Purpus, whose influence extends far beyond the waves. Mike’s lifelong passion for surfing, deep friendships and commitment to the South Bay reflect the power of connection, movement and purpose—all essential elements of lifelong health and well-being.
Throughout this issue of Pulse, you’ll find stories that reflect Torrance Memorial’s comprehensive approach to care—from orthopedic and cardiology innovations to community partnerships, volunteerism and a look ahead at the continued expansion of our emergency department as we prepare for the future.
As we move confidently into our second century of service, Torrance Memorial remains steadfast in its mission: to provide exceptional, compassionate care, invest in innovation and strengthen the health of the communities we are privileged to serve.
Together, we are building the future of care—rooted in trust, guided by innovation and centered on you.
Warm regards,
Keith Hobbs President/CEO
Torrance Memorial Medical
Center
If you do not wish to receive future issues of this publication, please email publications@tmmc.com with your name and complete address as it appears on the mailing panel.

Simple steps and advanced procedures can stop heart disease before or after it starts.
Torrance Memorial is at the forefront of comprehensive weight management care, offering a full range of personalized treatments.
32 ZEST FOR LIFE: PURPUS & FRIENDS
More than a surf legend, Mike Purpus embodies the spirit of community, service and aloha in the South Bay.
36 HELPING HANDS: A MATCH MADE IN HEAVEN
The Children's Burn Foundation and Torrance Memorial partner to provide 360-degree care for South Bay pediatric burn survivors and their families.
38 OUR COMMUNITY VIPS
The founder of a substance abuse and mental health resource for school-aged children and their parents; an Eagle Scout whose South Bay butterfly habitat restoration project is part of a bigger picture.






Torrance Memorial Earns Advanced Certification for Total Hip and Knee Replacement
Torrance Memorial Medical Center has been awarded The Joint Commission’s Gold Seal of Approval® for Advanced Total Hip and Knee Replacement Certification. This prestigious recognition reflects our ongoing commitment to providing safe, high-quality patient care. The certification was granted following a rigorous on-site review conducted last August, during which a Joint Commission reviewer assessed compliance across a range of standards. These included program management, preoperative care, operating room procedures, post-anesthesia care, nursing, discharge planning, physical therapy and patient self-management support. The Gold Seal of Approval® is a symbol of excellence and a testament to the hard work, dedication and expertise of our orthopedic team and supporting staff.
U.S. News & World Report Best Hospitals for Maternity Award 2026
Torrance Memorial has been recognized as part of U.S. News & World Report’s Best Hospitals for Maternity 2026. High-quality maternity care, provided from pregnancy through birth and postpartum, is key to the long-term health of newborns and mothers. We are honored and proud to receive this accomplishment that reinforces our reputation for high-quality maternity care, excellent childbirth and postpartum care.
Torrance Memorial Designated a North American Skull Base Society Multidisciplinary Team of Distinction

The Beacon Award for Excellence is a significant milestone on the path to exceptional patient care and healthy work environments. It recognizes unit caregivers who successfully improve patient outcomes and align practices with the American Association of Critical-Care Nurses’ six Healthy Work Environment Standards. The gold-level Beacon Award for Excellence earned by 3 West PCU signifies an effective and systematic approach to policies, procedures and processes that include engagement of staff and key stakeholders; fact-based evaluation strategies for continuous process improvement; and performance measures that meet or exceed relevant benchmarks. We applaud the commitment of the caregivers on 3 West PCU for working together to meet and exceed the high standards set forth by the Beacon Award for Excellence.
The North American Skull Base Society (NASBS) Multidisciplinary Team of Distinction recognizes hospitals with exceptional, collaborative skull base surgery teams dedicated to providing comprehensive care for patients with complex skull base conditions. This designation reflects NASBS’ commitment to inclusive, multidisciplinary education and patient-centered care across a wide range of medical specialties. To earn this recognition, institutions must demonstrate a coordinated team approach that includes at least four NASBS member physicians, representing both core skull base specialties—such as neurosurgery and otolaryngology—along with allied experts from complementary disciplines. Designation as an NASBS Multidisciplinary Team of Distinction is based on established criteria and recognizes excellence in collaboration; it is not intended as a medical referral. Torrance Memorial Medical Center is proud to be designated as an NASBS Multidisciplinary Team of Distinction.
Torrance Memorial Earns Blue Distinction® Center+ Recognition
Torrance Memorial has been recognized by Anthem Blue Cross as a Blue Distinction® Center+ for Spine Surgery, an honor awarded to hospitals that demonstrate excellence in patient safety, clinical outcomes and cost-efficient care. This designation reflects the high standards met by Torrance Memorial’s spine care team, whose performance is evaluated using objective quality measures developed through the Blue Cross Blue Shield Association’s partnership with the American Academy of Orthopaedic Surgeons. Blue Distinction Center+ facilities achieve significantly lower complication and readmission rates, along with meaningful cost savings—helping patients experience safer procedures, smoother recoveries and better overall outcomes.
Written by Marissa Minderler, MS, RDN, Clinical Dietitian
Cooking may feel like a daunting task in today’s busy world, but preparing meals at home is linked to better overall health outcomes and significant cost savings. Although grocery prices have risen, a home-cooked meal still averages just $5 to $6, compared to $12 to $25 for a single restaurant meal. In fact, cooking at home just three additional days per week has been associated with annual savings of nearly $2,500 to $3,000. Beyond the financial benefits, cooking at home can also reduce calories, saturated fat and sodium intake—three key factors that strongly influence heart health. Cardiovascular disease remains the leading cause of death in the United States and affects an estimated 128 million people. While many factors contribute to the development of heart disease, nutrition plays a central and modifiable role. If you’re looking to support or improve your heart health, start with these practical nutrition and cooking tips.

1 Choose lean proteins instead of high-fat meats. Example: Use skinless chicken breast, 93% to 99% lean ground turkey, fish, tofu or beans instead of sausage, bacon or higher-fat red meat. Why: Higher-fat meats contain large amounts of saturated fat, which is known to raise LDL (“bad”) cholesterol. Lean and plantbased proteins contain significantly less saturated fat, supporting heart health without increasing cholesterol.
2 Include fish high in omega3s two or three times per week. Example: Salmon, sardines, trout, tuna. Why: Omega-3 fatty acids help lower triglycerides, reduce inflammation and support healthy blood vessel function. If you do not consume fish, add plant-based omega-3 sources daily, such as chia seeds, ground flaxseed, walnuts and hemp seeds.
3 Use olive oil instead of butter.
Example: Sauté veggies in olive oil rather than butter.
Why: Olive oil is rich in heart-protective monounsaturated fats that help raise HDL (“good”) cholesterol and lower LDL (“bad”) cholesterol. It also contains antioxidants that support vascular health.
4 Season with herbs, spices, citrus and vinegar instead of salt. Example: Garlic, paprika, rosemary, lemon juice and vinegar.
Why: Reducing sodium intake helps lower blood pressure and decreases strain on the heart. Herbs and spices add flavor without the health risks associated with excess sodium.
5 Fill half your plate with fruits and vegetables.
Example: Berries, leafy greens, tomatoes, broccoli, carrots, bell peppers and carrots.
Why: Fruits and vegetables are high in fiber, potassium and antioxidants which help lower cholesterol, regulate blood pressure, reduce inflammation and decrease the risk of certain cancers, including colon cancer.
6 Add beans and lentils.
Example: Add chickpeas to salads or swap half the meat in chili for beans. Why: Beans are rich in soluble fiber, which helps remove cholesterol from the bloodstream.
7 Choose whole grains over refined grains.
Example: Brown rice, quinoa, wholewheat pasta, oats and barley.
Why: Whole grains retain fiber and nutrients that help lower cholesterol, stabilize blood sugar and reduce the risk of cardiovascular disease.
8 Limit added sugars.
Example: Choose water or unsweetened beverages instead of soda; use fruit to sweeten oatmeal or yogurt. Why: Excess added sugar contributes to weight gain, high triglycerides and insulin resistance—all of which increase heart disease risk.
9 Opt for heart-healthy cooking methods.
Example: Bake, grill, roast, steam or air-fry foods instead of deep-frying. Why: These methods require little to no added fat and help reduce overall calorie and saturated fat intake.
Serves 2
Why it’s heart-healthy:
Chia seeds are rich in soluble fiber and plant-based omega-3s—two powerful nutrients that help lower LDL (“bad”) cholesterol and support healthy blood pressure. Light coconut milk provides creaminess with less saturated fat while keeping the recipe dairy-free. Mango adds vitamin C, antioxidants and natural sweetness.
This refreshing pudding supports smooth blood vessel function and makes a nutritious option for breakfast, a snack or even dessert.
10 Watch your portions.
Example: Use smaller plates, measure oils when cooking and pre-portion snacks instead of eating from the container.
Why: Eating appropriate portions supports weight management and helps prevent overeating, which reduces strain on the heart.
Ready to take the next step toward a healthier lifestyle? Our expert registered dietitian nutritionists are here to help. Connect with Medical Nutrition Therapy or the Diabetes Self-Management Program at the Torrance Memorial Lundquist Lurie Cardiovascular Center, 2841 Lomita Blvd., Suite 335. Call 310-8916707 or visit TorranceMemorial.org/ nutrition to explore upcoming classes, hands-on programs and personalized nutrition appointments designed to support your long-term health.
Ingredients:
• 1 cup light coconut milk or almond milk
• 3 tablespoons chia seeds
• ½ cup diced mango
• ½ teaspoon vanilla
Instructions:
Stir chia seeds into milk and vanilla. Refrigerate for at least 4 hours or overnight. Top with fresh mango before serving.

Use the QR code for another heart-healthy recipe, the Mediterranean Bulgur, Chickpea & Herb Salad.
Torrance Memorial supports new moms, babies and entire families with expert care.
Written by Laura Roe Stevens

If ever there is a time to surrender and trust the process in life, it’s during pregnancy. But it’s not easy—especially during long, complicated or early labors. It is a vulnerable time for expectant mothers, filled with lessons on trust, inner strength, focus and the critical need for a reliable, dedicated and talented support team.
Expectant moms can rely on the labor and delivery team at Torrance Memorial Medical Center. The hospital has been designated by the Joint Commission as a Maternal Level of Care III hospital—meaning that Torrance Memorial provides exemplary care for complex maternal, fetal and obstetric conditions and has in-house specialists and intensive care.
New moms rave about Torrance Memorial’s highly qualified and dedicated physicians, labor and delivery nursing staff and devoted neonatal nurses—all trained in the latest technology and innovative approaches. They prioritize comfort, support and unparalleled care for mom, baby and the entire family.
“I don’t know what I would have done without the doctors at Torrance Memorial. They were remarkable! And I can’t say enough good things about the amazing labor and delivery and NICU nurses,” says Christina Smith, new mom of Isabella, who arrived seven weeks early on August 12, 2025, and stayed four weeks in the Level III Neonatal Care Unit (NICU).
Christina’s pregnancy had been “perfect,” she shares. She had no morning sickness and no problems handling her job as an executive for a TV show, requiring long hours on set. She felt so good that she walked 4.5 miles a day as well.
But at 29 weeks, with no prior symptoms, Christina’s blood pressure rose. She began monitoring it at home. When her blood pressure read above “178 over something,” Christina called Natalie Thorpe, Torrance Memorial clinical nursing director of Maternal Child Health Services.
“I was surprised when Natalie told me to go to L&D immediately. I was given blood pressure medication, and it came down overnight,” explains Christina.
A few weeks later, she told Matthew, her husband, that something was off. They checked, and her blood pressure was high again. She took blood pressure medication, then went to the hospital.
At Torrance Memorial her reading was normal. Instead of sending her home, however, in an
abundance of caution Aviv Herzlich, MD, decided to keep Christina overnight, saying, “Something is telling me not to let you go home tonight. If you’re fine in the morning, you can go then.”
High blood pressure during pregnancy is linked to preeclampsia, a severe condition that can risk both the mother’s and the baby’s lives. Giving birth seven or eight weeks premature is not ideal, but with today’s medical advances in neonatal care, it can be done safely.
Dr. Herzlich’s hunch proved correct. In the middle of the night Christina’s blood pressure skyrocketed, and she was put on magnesium to level it out.
When her obstetrician, Zachary Abelson, MD, came in that morning, he gave Christina the news that she would not be going back to work. “He said, ‘Oh, you’re not leaving until you have this baby. We’re going to try to get you to 34 weeks first.’ I was in shock, but then realized if I had been home when my blood pressure skyrocketed in my sleep, who knows what could have happened,” she says.
Under the care of Dr. Abelson, as well as obstetrician Ricardo Huete, MD, and Vikas Sacher, MD, a specialist in high-risk pregnancies, Christina was given blood pressure medication three times a day and steroids to strengthen baby Isabella’s lungs.
“Dr. Abelson said I had one of the most severe preeclampsia cases he has seen. It rose so high, I had an emergency C-section,” Christina says. “Thankfully Isabella was just fine. Her heart rate and breathing were unaffected.”
Tiny Isabella was cared for by Torrance Memorial’s NICU nurses, who have years of experience and a reputation for dedication and compassion. During the four weeks of NICU care, nurses also educated both mom and dad on how to care for their preemie.
“It was stressful to have our baby there every day, but the nurses gave us tips and tricks we wouldn’t have learned on our own, like how to bathe, swaddle and handle her because she was so small,” Christina explains. “They also showed us how often to do skin-toskin touch, how to hold her, how to feed her and how to get the calculations for feeding. They helped us put Isabella on a feeding and sleep schedule. At four months she was nearly sleeping through the night. I attribute this to the nurses and therapists who worked with her.”
When Christina and Isabella returned to Torrance Memorial for its annual reunion Halloween party, she said it felt like returning to visit family members because starting a family should be in the care of those who feel like home. •
For more information visit TorranceMemorial.org/medicalservices/maternity-child-health.

• Maternal Level of Care III designation for exemplary care for complex maternal, fetal and obstetric conditions.
• In-house specialists and intensive care.
• Level III NICU care, providing a NICU nurse at birth.
• Gold Standard Safe Sleep Hospital certification.
• Baby-Friendly designation by UNICEF/ World Health Organization.
• Active member of California Maternal Quality Care Collaborative, focused on improving the state’s maternity care.
• Renovated private labor and delivery suites and postpartum unit.
• Expanded education programs include prenatal yoga, lactation services, breastfeeding classes, perinatal support, C-section care, skin-to-skin practices, rooming-in and support for bonding, mental health support for postpartum, and support groups for childbirth, infant care and parenting.

Written by Nancy Sokoler Steiner | Photographed by Michael Neveux
Just as medical and nursing school students participate in hands-on clinical care as part of their schooling, the same is true for those studying to earn a Master of Health Administration (MHA). By working in real-world settings, these students become better prepared to fill their professional roles.
Torrance Memorial's president and CEO Keith Hobbs believes strongly in educating the next generation of health care administrative leaders. In fact, Hobbs has been mentoring MHA students at his workplaces since 2008. He formalized the practice by creating the Torrance Memorial MHA residency program in 2022. Each year, the hospital chooses two or three MHA residents.
“I think training MHA residents is a great way to give back and help leave a legacy of future leaders in health care,” says Hobbs. “It also creates a pipeline for filling positions that help us move our organization forward.”
Hobbs and chief operating officer Derek Berz co-lead the program and serve as the students’ preceptors—a combination of supervisor and mentor. Since the program began, 11 MHA students have completed their residencies at Torrance Memorial.
Evan Holly, one of this academic year’s three MHA residents, says, “Torrance Memorial is the perfect balance of getting high-level exposure into day-to-day operations as well as being part of a bigger health system through Cedars-Sinai. It’s been great to be privy to how senior leadership collaborates.”

Holly has worked on a variety of projects during his time at Torrance Memorial. One involved a financial comparison of two AI tools that predict heart attacks. Another resulted in having doctors and nurses do rounds together to increase communication and coordination.
He has enjoyed seeing the new emergency department come to fruition. Torrance Memorial will be the only hospital in California to have a two-story emergency department, and Holly has participated in leadership meetings addressing how to distribute resources between the two floors.
Lauren Bauer, a participant in the 2022 cohort, is one of four previous MHA residents to advance to a fulltime position with Torrance Memorial. As finance manager, Bauer’s responsibilities include overseeing the annual hospital operating budget, leading the Decision Support Finance team and participating in long-range financial planning.
When she arrived at Torrance Memorial for her MHA residency, Bauer knew she wanted to work in hospital operations but didn't know which specific area. Working with different departments and leaders allowed her to see where her skill set and preferences best matched the hospital’s needs.
She appreciated getting exposure to departments including marketing, supply chain, pharmacy and the independent physicians association. And when it came to finance, she clicked with both the leadership and the daily responsibilities of that discipline.
“I learned so much in the residency,” she says. “All the leaders, directors, executives and vice presidents were so willing to teach me and include me in their thought processes. That culture of support and investing in the next generation really made me want to stay here. The residency was my foundation, and now I’ve been able to grow each day as a Torrance Memorial team member.” •

Written by Lisa Buffington
There’s no doubt that coping with an illness, injury or hospitalization is challenging. For people who are homebound and facing a chronic illness or lengthy recovery, managing their health can feel especially overwhelming. In this situation, many people move to a skilled nursing facility for either a temporary or permanent stay. However, South Bay residents may have an alternative that allows them to remain at home.
“Torrance Memorial Home Health is a four-star patient satisfaction, Medicare-certified, Joint Commission-accredited home health care agency that cares for patients throughout the South Bay area,” says Debbie Griffin, executive director of the Home Health, Hospice and Palliative Care programs at Torrance Memorial Medical Center. “With an order from a physician, we can provide comprehensive skilled care for acute health conditions or
Torrance Memorial’s Home Health team helps patients stay safely at home by connecting them with the care and community resources they need.
exacerbations of a chronic health condition—all delivered in the comfort of the patient’s home.”
In most cases, home health services are coordinated before a patient leaves the hospital, and the first home visit occurs within 24 to 48 hours of hospital discharge. Caregivers assist with the hospital-to-home transition, closing care gaps and improving health outcomes.
“Most patients want to recover at home, so our goal is to help our patients age in place and prevent emergency department visits or rehospitalization. We teach people how to recognize the warning signs of a problem and get help early,” says Griffin.
Whether a patient needs ongoing care for a chronic condition like kidney failure, heart failure or chronic obstructive pulmonary disease, or shortterm acute care after an injury, joint replacement or surgical procedure, they can expect personalized treatment in a familiar, relaxed environment.
The team—including registered nurses and licensed vocational nurses—assesses each patient’s needs and provides intermittent care as ordered by their physician. Home health nurses also educate patients on wound care, IV infusions, ostomy care, tube feeding and more—equipping patients with the confidence and skills required to manage their care at home. The nursing team is available seven days a week with an after-hours on-call service for emergencies.
Physical therapists work with patients to improve strength, balance and mobility, while occupational therapists help patients learn strategies to assist with everyday tasks, such as cooking, bathing, using the stairs and getting dressed. Home health aides provide nonmedical assistance, such as help with bathing, dressing and grooming.
The Torrance Memorial Home Health team also includes social workers who connect patients with community resources to help them stay in their homes, such as caregiver support, private caregiving services, home medical equipment, financial support, legal assistance and more.
Torrance Memorial Home Health is also adopting technology that streamlines communication between home care professionals and providers. The team has implemented a remote monitoring
system that records blood pressure, blood oxygen, weight and glucose levels and automatically enters them into the patient’s electronic medical record (EMR). The team recently started using a new app that takes pictures of wounds, automatically measures their size and depth, and sends a PDF image to be included in EMR—allowing providers to see how the wound heals or changes over time.
“These systems allow providers to track the progress of care and help us improve patient management and outcomes,” says Griffin. “If we notice something abnormal, we take immediate action to connect the patient with their provider so they can get the care they need.”
A physician’s order is required to initiate home health care services. Patients and their families may also request an evaluation. For more information or to request home health care, call 310-784-3739. •
Kim Carlon, 68, a retired respiratory therapist from Hawthorne, was hospitalized four times in the past year. But having Torrance Memorial Home Health on her care team made a bad year better.
“I receive physical therapy, occupational therapy and nursing care at home, and I couldn’t ask for better care than I’m getting now,” says Carlon, who receives a visit from her physical therapist twice a week and from her occupational therapist and nurse once a week.
The consistent care Carlon has received has helped with her recovery. And she has developed a strong connection with her caregivers along the way.
“My team—including occupational therapists Jason and Alex; physical therapists Judy, Maggie, Aliven and Sean; and social worker Stephanie—provides what I need when I need it,” says Carlon. “I love them and appreciate everything they do for me. They are the reason why Torrance Memorial Home Health is so amazing.”
Written by Melissa Bean Sterzick
The beauty of being on a bike is seeing the world in a different way—fast and free. E-bike use is a growing trend throughout the South Bay, providing an enjoyable, affordable and eco-friendly way to get around. However, local emergency departments are seeing an increase in e-bike injuries, many of which could be prevented. Though there are risks, e-bikes are great for both recreation and transportation, and here in Southern California they can be used year-round. Kurt Hansen, MD, a Torrance Memorial emergency department physician, says e-bike riders can stay safe with the right equipment and education.
“The 100% absolute most important thing is a helmet,” Dr. Hansen says. “The head is good at getting hit. It’s strong, but when you add a motor and speed, that’s where the danger to your brain comes in.”

A helmet only works if it’s worn correctly. “Sometimes kids wear a helmet but don’t clip it under the chin. When they go flying the helmets go flying, and their heads hit the ground,” he says.
Maintaining visibility is important. Riders should wear bright clothing, use reflectors and stay in bike lanes. In many car-versus-bicycle accidents, besides head injuries, cyclists experience broken hips or a fractured pelvis. E-bike accidents also often lead to broken wrists, elbows and collarbones, and severe soft-tissue injuries. Wrist guards, kneepads and thick clothing can also help reduce injuries.
As e-bike use and popularity grow among kids and teens, Torrance Memorial emergency department physician Kurt Hansen, MD, emphasizes the importance of safe habits.
“Anyone over 16 with a driver’s license has a better sense of road safety. You understand what happens at an intersection; you understand what blind spots are,” Dr. Hansen says. “My biggest concern for riders who haven’t taken driving lessons is they don’t understand the unpredictability of traffic.”
E-bikes present a risk for pedestrians too. “If you have 80 pounds of bike with a 170-pound human on it going 20 miles an hour, it’s going to do damage. And you’re liable,” Dr. Hansen says.
Anyone on an e-bike needs to know where they can ride and how to yield, cross intersections, regulate speed and so on. Dr. Hansen has three sons, ages 7, 11 and 14. He says if he ever gives them regular access to e-bikes, they will have training first.
One option he’s considered is E-Bike Sense—a safety course that teaches kids to ride responsibly. The company’s owner and founder is Megan Lamb, a South Bay resident and former competitive cyclist.
“Every time I would see a local kid riding recklessly, my heart sank. So when my son begged me for an e-bike, I insisted on formal training. There wasn’t a safety course specifically geared toward kids,” she says. “Our training helps them consider the realities and risks of e-bikes.”
The Centers for Disease Control and Prevention reports around 40% of e-bike-related injuries involve riders under 18. Head injuries account for 60% of hospital visits involving e-bike accidents. It’s up to parents to reinforce safe use.
“Without a helmet, you can hit your head and it can change the course of your entire life trajectory,” Dr. Hansen says. “Speed is also key, so I would set some limits.”
Kids need to know their e-bikes are fun, useful and powerful. They have a responsibility to ride them carefully. An accident might mean they miss a season of their sport or a semester of school … or worse. And if they hurt someone else—a pedestrian or a friend—there can be lifelong consequences.
“Parents need to sit down with their kids and tell them, ‘Let’s be safe. Here’s what we do so the person you want to be is still there. Helmet use has to be nonnegotiable—meaning there’s no riding without a helmet.’” •
“The head is good at getting hit. It’s strong, but when you add a motor and speed, that’s where the danger to your brain comes in.”
– Kurt Hansen, MD

NEW E-BIKE SAFETY LAWS AND REGULATIONS PUT INTO ACTION IN CALIFORNIA AS OF JANUARY 1, 2026, INCLUDE:
• A provision allowing for citing parents of minors who commit offences while riding electric bicycles.
• An option for minors cited specifically for helmet violations is to clear their fines by completing a California Highway Patrolapproved safety course.
• A requirement for all electric bicycles to have either a red rear reflector or a solid or flashing red rear light that includes a built-in reflector. This must be used during all hours of operation, including daytime riding.

A milestone anniversary honors decades of volunteer service at Torrance Memorial.
Written by Nancy Sokoler Steiner
Volunteer culture is strong at Torrance Memorial.
More than 900 individuals, identifiable by their trademark blue jackets, help their community by collectively contributing more than 115,000 hours of service each year to Torrance Memorial. Most adult volunteers choose to join the Volunteer Auxiliary, an independent nonprofit that provides programming and raises
funds for the hospital—the same way a PTA supports its school.
The Volunteer Auxiliary celebrates its 75th anniversary this year. “Volunteering has been part of Torrance Memorial from the start,” says recently retired director of volunteer services, Mary Matson. “In 1951, 25 years after the hospital’s founding, six volunteers chose to formalize the Auxiliary, which exists to support the medical center.”

In January, the Torrance Memorial Auxiliary presented the hospital with a check for $245,000.
L to R: CEO Keith Hobbs, Mark Lurie, MD, Laura Schenasi, Tina Trudnowski, Melinda Richmond, Mary Wright, Michelle Di Marco
The Volunteer Auxiliary owns and operates the Gift Shop in Lundquist Tower. All Gift Shop profits, along with bake sale proceeds and membership dues, benefit patient services. Matson notes that over the years, the group has raised more than $8 million. In 2014, the Healing Garden was named in honor of the Volunteer Auxiliary.
Volunteers help in settings including the information desk in the Grand
Lobby, the surgery department waiting room and patient rooms, where they may drop by to offer snacks or company. Volunteer escorts take patients to various departments, Clowns on Rounds bring smiles to patients, and dogs and their owners provide canine comfort through the Pet Visitation Program.
Betty Broughton began volunteering in 1994 and has given more than 32,500 hours of her time. She started soon after retiring from Hughes at the suggestion of her daughter, Dianna Tyndall, clerical manager in the radiology department. She has served as president of the Volunteer Auxiliary three times and held many other roles, including secretary, treasurer and gift shop co-chair.
Today, the 87-year-old volunteers three times a week, including one day in surgical admitting. “I enjoy being with people,” she says. “And especially in surgery, patients may be scared and I try to calm their nerves.”
A self-described morning person,

Broughton works the 5 to 9 a.m. shift. “I’ve met some wonderful people and made great friends over the years,” she says. “This is a wonderful place to work.”
In 1989, Judy Sipes proposed forming the Luminaries, a service group where mothers and their teenage children volunteer together. Luminaries help on-site and raise funds through special events. The group donated $15,000 in its first year and has raised more than half a million dollars since its founding.
Children of active Luminaries join NOVAs, a high school volunteer program. They serve as patient escorts, help at special events, decorate the pediatrics ward, and make tray favors and blankets for patients, among other activities.
“There’s now a waitlist to join the NOVAs,” Sipes notes. “It’s moving for me to see how the program has continued all these years.”
She volunteers in the gift shop on Monday mornings and is the shop’s


handbag and jewelry buyer. “The hospital has been my home. I’ve had so much fun and gained as much as I have given,” says Sipes, who has attended conventions for hospital volunteers and was surprised to learn how many hospitals struggle to recruit volunteers while Torrance Memorial’s volunteer program flourishes.
“The Volunteer Auxiliary is a thriving entity and partner to Torrance Memorial,” says Matson. “It would not be the same without them.”
Following Matson’s retirement in November 2025, longtime Torrance Memorial staff member Kimberly Flores has stepped in as the new director of volunteer services and is leading the auxiliary into its 75th year and beyond. •
To learn more about volunteer opportunities visit TorranceMemorial. org/volunteer.
Top, L to R: Early days of the Torrance Memorial Auxiliary; the Auxiliary's Pet Visitation programs.
Bottom: Longtime volunteers with 22 to 48 years of service (L to R): Barbara Smith, Ruth Sve, Margaret Johnson, Jean O'Dell and Betty Broughton, who has given more than 32,000 hours of time her time to the volunteer program.

TMIPA physicians can be independent of TMPN
TMPN physicians are members of TMIPA
Together, Torrance Memorial IPA and Torrance Memorial Physician Network provide a place for everyone.
Written by John Ferrari
Imagine you’re a physician. You want to focus on practicing medicine without having to manage payroll, insurance billing or other administration. Torrance Memorial has a home for you.
Imagine you’re a different physician. You’re an entrepreneur too. You like being able to manage your own practice and employees. Torrance Memorial also has a home for you.
Now imagine you’re a patient in a managed care HMO or Medicare
Advantage plan. You’re looking for a comprehensive health care service provider. Torrance Memorial has a home for you as well.
Finally, imagine you’re a nurse, medical technologist, administrative specialist or other health care professional. You want to work with fellow professionals who share your dedication in a workplace that’s efficient and caring. Yes, Torrance Memorial has a home for you.
These homes intersect in Torrance
Memorial’s two physician groups: the Torrance Memorial Physician Network (TMPN) and Torrance Memorial Independent Practice Association (TMIPA). They may sound similar, but they were established to meet different needs, and they provide flexibility and efficiency in different areas.
TMPN and TMIPA also have a lot in common. They both help physicians practice medicine and manage their medical practice. Most importantly, they both support Torrance
Memorial Medical Center in providing outstanding comprehensive, coordinated health care.
Established in 1983, the Torrance Memorial Independent Practice Association has been around for more than 40 years. “The independent practice association concept was formed in the emerging California managed care market of the 1980s as a way for independent physicians to act as a group and provide more efficient care at a lower cost,” says Torrance Memorial senior vice president Chris Rogers.
After the enactment of the Health Maintenance Organization Act of 1973, managed care HMOs increased in popularity by reducing out-of-pocket costs for consumers—but they also reduced primary care physicians’ flexibility in responding to their patients’ health care needs. IPAs work with managed care HMO and Medicare Advantage plans to provide more responsive, point-of-service care to patients.
“Here in Torrance, we know our community better than a payer based somewhere else. We coordinate care right here in our offices at Torrance Memorial,” says Rogers.
At the same time, IPAs provide fiscal efficiencies for physicians by reducing overhead, sharing costs and increasing their ability to negotiate as a collective. HMO and Medicare Advantage plan administrators delegate to the IPA responsibility for patient administration such as payment and care management and coordination.
“We take care of those things here in TMIPA. It’s a model that benefits the managed care plans, the physicians and the patients through more efficient care. Through this delegation we have a financial interest in providing the best, most efficient care to the patient,” explains Rogers. “Administratively, we deliver better care to the patient. The IPA allows us to deliver the right
care, leading to better outcomes at a better price, more efficiently. Through our network of 877 providers, we coordinate care for more than 82,000 members across medical specialties and out into the community too. For example, we can track a patient’s need for transportation and other support services by coordinating with social workers. We stitch together what is otherwise a very fragmented health care delivery system.”
Created to improve health care efficiencies and outcomes under managed care, Torrance Memorial’s IPA includes independent physicians together under an umbrella organization, while allowing them to retain their own practices. The Torrance Memorial Physician Network, established in 2012, responds to a different trend in health care.
Torrance Memorial senior vice president Heidi Assigal explains: “The key driver to form the network was some of our more senior community physicians weren’t seeing younger doctors come into the community to practice family medicine. Newer doctors often would like to focus on medicine, not administration. As the complexity of office management has increased, there’s been less appetite among young doctors to open their own practices. Insurance and billing administration, regulation compliance and the staff needed to run an office—they’ve all increased.”
TMPN responds to that shift by giving physicians a place to practice medicine without having to also manage their practice. TMPN member physicians are all TMIPA member physicians too, but their practices are managed by Torrance Memorial. TMIPA physicians who aren’t TMPN members manage their own practices. “Some physicians still have that entrepreneurial spirit,” notes Rogers.
TMPN also gives Torrance Memorial a tool for the future. “Our initial focus
was primary care,” says Assigal, “but over the years we have added many specialties. We’re also constantly assessing where we’ll need more specialists. Neurology is one growth area, as is obstetrics. We recruit a mix of new doctors, mid-career doctors and very experienced doctors.”
“TMPN helps us plan for and manage our growth and development,” adds Torrance Memorial president and CEO Keith Hobbs. “This ongoing recruitment effort allows us to adapt to retirements, replacements, practice acquisitions and new patient growth, while strategically filling in the gaps in essential specialties and optimizing care. The expansion of the physician network also opens doors for new primary care and expanded specialty clinics, addressing the ever-growing patient demand and ensuring we meet the needs of our community.”
Growing from two offices and seven clinicians in 2012, TMPN now has about 45 clinics and office locations with about 650 staff supporting approximately 185 clinicians.
“TMPN is intended to serve Torrance Memorial’s service area—from El Segundo to San Pedro, and Gardena and Lawndale in the east,” says Assigal. “As we grow in the community, we’re growing the patient base that has the Torrance Memorial experience, and that helps make Torrance Memorial Medical Center the hospital of choice. We keep enhancing the services our physicians bring to their patients right here in the South Bay. That’s a positive experience for our patients, and Torrance Memorial rises to the top among their health care choices. That doesn’t stop with our clinicians—all of our staff are aligned with our core values, and that creates a collective pride and commitment to service excellence. Clinicians and staff bring the heart of Torrance Memorial into the community.” •



Simple steps and advanced procedures can stop heart disease before or after it starts.
Written by John Ferrari
Avisit to the cardiology department sounds daunting, but when you’re in coronary distress, there’s nowhere you’d rather be than Torrance Memorial’s Lundquist Lurie Cardiovascular Institute (LLCVI). Even before developing a coronary condition, the LLCVI can help keep your heart healthy and head off heart disease.
A comprehensive heart institute, the LLCVI offers the full range of specialized cardiac services, much more than a standard community hospital. LLCVI physicians, nurses and technicians have the skills and equipment to treat even the most serious heart conditions. Just as important, they have the tools to stop heart disease before it starts.
“The majority of coronary disease is preventable,” says interventional cardiologist Ankush Chhabra, MD, the institute’s medical director.
With a healthy lifestyle and early detection, diagnosis and treatment of coronary disease, 80% of premature heart attacks and strokes are preventable. Dr. Chhabra notes that the LLCVI’s cardiologists now spend more time talking with patients about prevention than about procedures. “Prevention is the most exciting and impactful part of cardiology right now.”
Chances are, you already know how to minimize your risks of suffering from a heart attack or stroke (see sidebar). But what if you find yourself with a racing heart and shortness of breath? Gripped with chest pain? Or trying to beat cancer? The LLCVI is definitely where you want to be.
If your heart skips a beat, it may be innocuous—or serious. Any abnormal heart rhythm is a form of arrhythmia, and the LLCVI can diagnose and treat the full range of arrhythmias, from benign to life-threatening.
Atrial fibrillation (A-fib), one of the most common, can lead to an increased risk of blood clot formation and stroke or heart failure. “A-fib affects about 5% of the population in the United States, and the biggest risk factor is age,” says cardiac electrophysiologist Matthew Ostrom, MD.
Dr. Ostrom specializes in ablation, a minimally invasive procedure that creates small scars to block the electrical signals responsible for A-fib and other arrhythmias. This can be accomplished through heat, cold or, more recently, pulsed field ablation—a technique using electrical pulses to precisely affect the targeted tissue.
“It’s safer and faster,” Dr. Ostrom says. “With pulsed field ablation, we don’t worry as much about damaging nearby tissue. The procedure is quicker, and patients experience a faster recovery. We don’t know exactly what causes most arrhythmias, but we do know there are multiple risk factors, including obesity, hypertension, diabetes and sleep apnea.
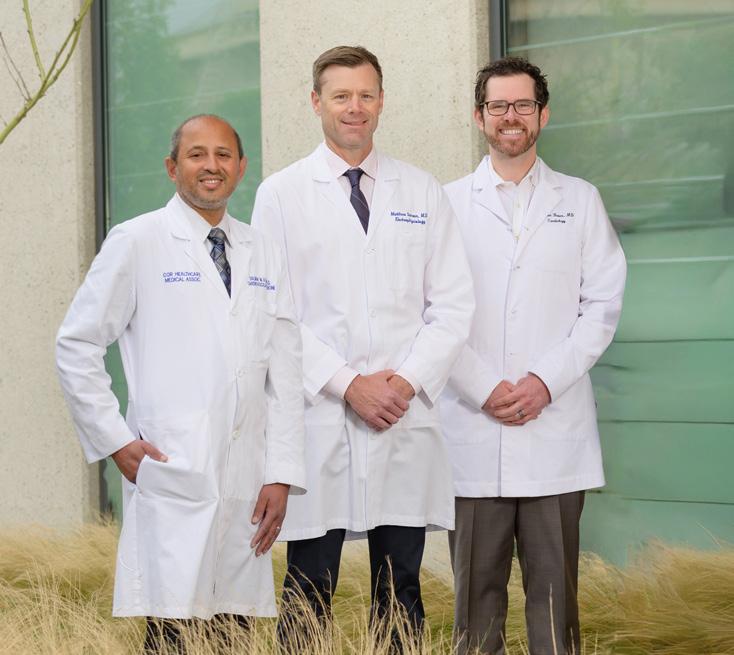
Members of the expert cardiology team at Torrance Memorial's Lundquist Lurie Cardiovascular Institute, at left (L to R): Salman Azam, MD, Matthew Ostrom, MD, Brenton Bauer, MD
Below: Ankush Chhabra, MD, the institute's medical director

A lot of these conditions could be better prevented through education and lifestyle changes.”
The same risk factors apply to heart attacks, notes interventional cardiologist Salman Azam, MD, adding that LLCVI cardiologists now focus on working with patients to prevent heart attacks, as well as helping patients recover.
“One of the most important developments in the prevention of heart attacks is Torrance Memorial’s screening program,” he explains. “I use it to focus on preventive measures, starting with lifestyle choices.”
For patients who’ve already had a heart attack, the first step is to create a picture of their heart and arteries.
“The Lundquist Lurie Cardiovascular Institute brings cardiology specialists together to review the patient’s anatomy and tailor treatment to the individual from a multispecialty perspective,” says Dr. Azam. “The ability to do that is one of the benefits of a comprehensive heart institute. We have the specialists and technology to treat the most complex coronary disease with a variety of tools, from lifestyle modifications and medication to surgery. It’s all based on what the patient needs.”
Torrance Memorial uses a multispecialty approach throughout its medical departments. One example is cardiooncology, a field combining heart and cancer care that has developed over the past decade.
Brenton Bauer, MD, director of the LLCVI’s echocardi-
ography lab, heart failure program and cardio-oncology program, notes that people with cancer face a higher risk of heart disease. Some patients share risk factors for both illnesses, while cancer treatments themselves can lead to blood clots, arrhythmias or other heart-related conditions.
Cardio-oncology encourages collaboration between cardiologists and oncologists ensuring patients receive the best care for cancer. “Treatment plans are individualized for each patient, taking into account their specific cancer and therapy,” Dr. Bauer notes. “We closely monitor patients and implement proactive strategies to reduce the risk of cardiac complications.”
The partnership between oncologist, cardiologist and patient may begin even before treatment, with prehabilitation. “We all work together to get the patient in the best shape condition possible, through cardio-pulmonary conditioning, dietary changes and other measures.”
Torrance Memorial’s physicians aren’t the only ones using a multispecialty approach. The LLCVI’s nursing staff uses a multiple-system approach to provide the best, most comprehensive care to patients as well. Designated a Magnet® hospital by the American Nurses Credentialing Center, Torrance Memorial Medical Center is recognized for providing the best in nursing care and professionalism in nursing practice.
That’s especially important in cardiology, says Peggy Crabtree, RN, the LLCVI’s director. “Cardiac nursing requires a level of expertise to understand how the heart is impacted by other systems and conditions. It’s work that requires a commitment to learning and excellence, and Torrance Memorial is really good at supporting that. Everyone on the cardiology nursing team is certified in their specialty.”
For everyone who finds themselves in the LLCVI, nurses are the first people they’ll see and the people they’ll see most often. “Cardiology is a multidisciplinary team, and our physicians really respect everyone on that team.”
Looking ahead, Dr. Chhabra is enthusiastic about plans to add a wellness center to the institute. “The main effort will be nutritional counseling and exercise physiology and we’ll go from there,” he says. “The center will also emphasize community engagement. We want to encourage healthy lifestyle habits. Now that we know how much lifestyle affects coronary health and are really focusing on that, we want people to come in to the LLCVI before they need to see us—so they don’t need to see us later.”
Torrance Memorial’s partner cardiology practice, COR Healthcare Medical Associates, is located at 2841 Lomita Blvd., Suite 100, in Torrance. Call 310-257-0508 to find a heart specialist. •
The American Heart Association has developed eight key measures for improving and maintaining cardiovascular health.
1. Eat well. Whole foods, lots of fruits and vegetables, lean protein, nuts, seeds and cooking in non-tropical oils such as olive and canola.
2. Be more active. Adults should get 2½ hours of moderate or 75 minutes of vigorous physical activity per week. Children should have 60 minutes every day, including play and structured activities.
3. Quit tobacco. Use of inhaled nicotine delivery products, particularly cigarettes, is the leading cause of preventable death in the United States.
4. Get enough sleep. Most adults need 7-9 hours of sleep each night; children need more. Adequate sleep promotes healing, improves brain function and reduces the risk for chronic diseases.
5. Manage weight. Your doctor or health care provider can help you figure out if your weight is healthy for your age and body. A healthy weight helps your brain and heart function better.
6. Control cholesterol. High levels of non-HDL, or “bad,” cholesterol can lead to heart disease.
7. Manage blood sugar. Over time, high levels of blood sugar can damage your heart, kidneys, eyes and nerves.
8. Manage blood pressure. High blood pressure can harm heart and brain health and usually has no symptoms. It can lead to serious health problems, including heart attack, stroke, dementia, heart failure, kidney disease/failure and vision loss.
Seasonal allergies strike year-round. Talk to your doctor about the best solution for you.
Written by Melissa Bean Sterzick
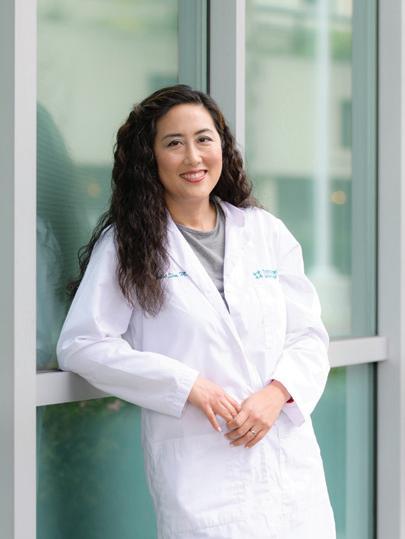
It’s not a cold. It’s not the flu. It’s seasonal allergies, brought to you by the beautiful weather, winds and foliage of the South Bay. While bugs and viruses plague the nose and throat for a week or two, seasonal allergies can last for weeks and months. Some find spring sets off their sinuses; others suffer during the winter months when the house gets stuffy. To make seasonal allergy season much less sneezy, Yuan Liu, MD, a Torrance Memorial Physician Network ear, nose and throat specialist, recommends over-the-counter meds including sinus sprays, a few simple changes around the house and possibly allergy testing.
What are the common triggers and patterns of seasonal allergies, specifically in the South Bay?
Indoor and outdoor allergens are present during every season. The most common outdoor allergens in our area include olive, oak, eucalyptus and walnut trees. Typically during the spring pollen season, these allergens are the culprits. During the summer months, grasses—including Bermuda, blue and rye—can cause allergies. Weeds such as ragweed and sagebrush can cause allergies in the fall. Indoor allergens such as dust mites, dogs, cats, cockroaches and mold affect people year-round. Windy days, especially in December and January during peak Santa Ana wind season, can worsen allergies due to the spread of allergens.
How can individuals tell the difference between allergies, colds and infections?
Allergies typically cause a runny nose, itchy and watery eyes, and sneezing, but colds from viruses (the most common) or bacteria usually cause a runny nose with throat pain, fatigue, headaches and sometimes muscle aches. Colds get worse and then better over the course of one to three weeks, whereas allergies can last a day or go on daily and indefinitely, as long as the allergens are present.
What over-the-counter treatments work best, and when should a patient consider prescription options or allergy testing?
For minor allergy symptoms, a saltwater rinse can clear the sinuses of allergens and mucus. Flonase or other nasal steroid sprays are generally effective and have minimal side effects. Over-the-counter oral antihistamines are helpful as well but are generally less effective than nasal sprays. Allergy testing is reserved for those who cannot tolerate nasal sprays or do not find them effective.
How can patients manage more severe or persistent allergies, including those affecting sleep, asthma or sinus health?
Severe allergies require allergy testing. Various tests can help identify the exact allergens—whether it's weeds, trees, grass, pollen, pet dander and so on—that trigger allergic reactions. Then the allergy treatment plan created is specific to the patient. Treatment can include daily steroid use (usually with sprays and rinses) or allergy shots. And sometimes inhalers are needed to control asthma symptoms.
When is it important to see a doctor, and what allergy services or specialists are available through Torrance Memorial Physician Network?
If over-the-counter antihistamines and nasal sprays are not helping or there are severe symptoms such as nasal blockage, facial pressure and nasal drainage, then it’s a good time to see a doctor. We have five ear, nose and throat specialists who can help, and we can usually see patients within a week, if not sooner.
Yuan Liu, MD, practices at Torrance Memorial Physician Network ENT at 23650 Crenshaw Blvd., ste.100 Torrance, CA. 90505. He can be reached at 310-891-6733.

First, identify the allergen. Different avoidance measures work for different allergens. For indoor allergies like dust mites, use an air purifier, wash bedding regularly, and get rid of carpets and rugs. For outdoor allergies, keep allergens out by closing windows and run an air purifier in the house. When outdoors, a well-sealed mask can be very helpful. In addition, rinsing with a gentle saline solution can clear allergens and decrease inflammation in the nasal passages.
“Surgery and medications are tools, but diet and nutrition are essential to achieving the best possible outcomes.”
— registered dietitian Noel Le, RDN, CNSC
Torrance Memorial is at the forefront of comprehensive weight management care, offering a full range of personalized treatments.
Written by Lisa Buffington I Photographed by Mitchell Yee
Over the past 20 years, weight management advice and treatment options have evolved. Today the experts at Torrance Memorial Medical Center use the latest tools and strategies to deliver personalized, comprehensive weight management care.
Torrance Memorial takes a multidisciplinary approach to weight management that supports patients at every stage of their journeys. This includes helping patients safely manage GLP-1 prescriptions, connecting them with nutrition and lifestyle support services and, when appropriate, offering access to surgical weight loss options— often with guidance from their primary care provider.
Torrance Memorial Physician Network family medicine physician Soohan Mansuri, MD, says it’s now easier than ever for patients to access a range of weight management options. “Primary care providers are often a patient’s first stop on their weight management journey. At Torrance Memorial, we work closely across
specialties to ensure patients have coordinated access to medical, nutritional and surgical weight loss options, along with support navigating insurance requirements for GLP-1 medications.”
As the use of GLP-1 weight loss medications continues to grow, it's crucial for patients who are considering using weight management medications to consult with their primary care provider first, advises Dr. Mansuri. Although GLP-1s may be available from other online or in-person sources, a primary care provider has access to valuable health and medication history that can help determine whether GLP-1s are likely to be safe and effective.
Primary care providers can refer patients to a range of local weight management programs and services—including Torrance Memorial’s in-person or online fitness classes such as yoga, strength training, Pilates, line dancing and more (see class listing on page 46). Hosted in a health care setting and online, these classes are perfect for those who may not feel comfortable hitting



Scan the QR code to register for Torrance Memorial fitness classes.
a crowded gym or who need help getting started following an extended break from physical activity.
Whether a patient chooses medication, lifestyle changes or weight loss surgery, nutrition is a crucial ingredient in the recipe for prolonged weight management success.
“Surgery and medications are tools, but diet and nutrition are essential to achieving the best possible outcomes,” says registered dietitian Noel Le, RDN,
CNSC, who specializes in working with bariatric surgery patients. “Our pre-op classes, one-on-one counseling sessions and post-op support groups give patients the foundation and skill set they need to take ownership of their health and address psychological, emotional and lifestyle factors that impact diet.”
Torrance Memorial’s team of registered dietitians also developed the CORE4 Weight Management Program, which promotes lasting results through hands-on support and education in nutrition, physical activity and behavior modification.

Torrance Memorial bariatric surgeon
Houman Solomon, MD, with patient and Torrance Memorial Physician Network nurse practitioner
Esmerelda Guerrero, who lost 145 pounds after gastric bypass surgery in 2021.
Lisa Araujo, a Torrance Memorial laboratory technician who lost more than 150 pounds after gastric bypass surgery in 2009, has firsthand experience with the evolution of weight-management care. More importantly, despite numerous changes in treatment options and approaches over the years, the support she received from her bariatric surgeon, Houman Solomon, MD, and the Torrance Memorial team has remained consistent.
“Before surgery, no matter what I tried, I couldn’t keep the weight off,” says Araujo. “After my surgery, I’ve been able to maintain my weight loss for 16 years by keeping my eye on the prize—and with the help of Dr. Solomon and my team, who make it so easy to reach out and are always there to listen and help me find solutions.”
When she experienced weight gain several years after her initial procedure, Araujo was prescribed Ozempic, a GLP-1 medication, to help manage “food noise” and promote fullness—demonstrating how bariatric surgery and medications can work hand in hand.
Torrance Memorial nurse practitioner Esmeralda Guerrero, FNP, also underwent bariatric surgery performed by Dr. Solomon. Her experience with weightmanagement care at Torrance Memorial now enables her to offer valuable advice to her patients.
“When I first met Dr. Solomon, I weighed 318 pounds. After struggling for years, I was so relieved when he told me that I had a metabolic problem and I needed a metabolic solution,” says Guerrero, who lost 145 pounds after gastric bypass surgery in 2021. “After my experience, I tell my patients that if you want to dig a ditch, you want to use the best tool available. If you have a lot of weight to lose and are living with weight-related chronic conditions, bariatric surgery is like using a tractor,
medication is akin to using a shovel, and diet and exercise are like trying to dig a ditch using your hands. It’s exciting to have better tools available now.”
According to Dr. Solomon, many people don’t realize that obesity is a complex medical and psychosocial issue—and the solution often involves combining multiple treatment options to achieve optimal results.
“Surgery is an effective, long-lasting weight management solution, and medications can be effective for the right candidates. But we also offer mental health, social, exercise and nutrition support for our patients,” says Dr. Solomon, a general surgeon who is board-certified in medical and surgical weight loss. “At Torrance Memorial, we have all the tools at our disposal, and we try to tailor our treatment approach to our patients and guide them to make choices that will help them meet their short- and long-term health goals.”
Regardless of where a patient is on their weight-management journey, they can find the support and treatment options they need at Torrance Memorial.
“Our approach is comprehensive, and we stay connected to our patients for life—because when it comes to weight management, the solution isn’t one-size-fits-all,” says Dr. Solomon.
If you have questions about weight management, Torrance Memorial experts have the answers. Scan the QR code to learn more about our weight-management services or request a consultation with one of our experts. •

More than a surf legend, Mike Purpus embodies the spirit of community, service and aloha in the South Bay.
Written by Jared Sayers | Photographed by Michael Neveux
Surfing is not soccer. It’s not basketball nor football. For better or worse, it’s one of those obscure pursuits that is far more singular than collective—a deeply personal experience, unique to the individual. Yet despite that singularity in the water, on land there’s a much more collective dynamic … and it can be spotted a mile away. It’s like a secret society of those with gills and those without. As my friend Joey Lombardo likes to say, the surf community is a tribal one.
Those with gills will already know this man, but many of you may not: Mike Purpus. Born and raised in Hermosa Beach, he is one of the world’s gifts to surfing. He grew up during a unique era, right between the longboard transition and the shortboard revolution. Unconventional and magnetic, his surfing mirrored his larger-than-life personality. On land and in many tribal circles, he’s a cosmic warrior of sorts.
His résumé includes a second-place finish at the 1972 Makaha International Championships; competing in the World Surfing Championships in 1968, 1970 and 1972; a five-time invitee to the Duke Kahanamoku Invitational; and being the first star on the Hermosa Beach Surfers’ Walk of Fame. To this day, he remains the oldest competitor in the South Bay Boardriders Surf Series.
But upon closer examination, there’s something a little different about Purp.
As we prepared for this story, he walked me through his Redondo home, showing me trophies, achievements, photos and memorabilia. Yet there was something else in the room— something unseen. Something that hung in the air and settled over the dusty trophies and faded nylon carpet.
As he chatted about this story or that, this trophy or that achievement, there was a magnetism to him. It was layered with humor. That humor was layered with joy. And that joy was layered with something magnetic and hard to put a finger on—rooted in service. It communicated something along the lines of: You’re my friend. Welcome to my home. I’m so stoked you’re here.
Did you know that across various tribal communities—from Hawaiian to Tongan, Zulu, Navajo and beyond—chiefs have traditionally led through service? In return, the tribe takes care of the chief, allowing the chief to continue to take care of the tribe. This mutual responsibility creates long-term stability and places leadership at the center of the communal well-being.
Fun fact: Purp hasn’t had a driver’s license since 1980. So how does he get where he needs to go? Nonchalantly, he says, “I have friends.”
Today, his good friend Steve Littrell gives him a ride wherever Purp needs to go: doctor appointments, grocery store runs, you name it. Steve is the wheels. And it should be said, Steve
lives in Lakewood—not around the corner.
Did you know that many societies and tribal communities throughout history didn’t collapse due to outside enemies or sudden disasters? They collapsed because leadership at the top stopped working. When chiefs became status-driven rather than stewardship-driven—turning power into something symbolic and competitive— it created internal conflict, often leading to abandonment, social destabilization and, ultimately, population collapse.
Purp chooses people. And the people choose Purp. It’s been that way his whole life. As his good friend Dan Merkel says, “Mike freely gives others the aloha spirit.”
Alo means presence, face or shared space. Hā means breath or life force. Together, aloha means “the sharing of breath”—a recognition of mutual existence and connection. That is exactly what Mike has and gives away freely.
And I’m pretty sure that’s what I felt in Purp’s home that day. You know it when you feel it. A commodity that’s becoming harder and harder to come by in the lonewolf, entrepreneurial, influencer economy we find ourselves in. Money can’t buy it. But boy oh boy do people want it. Just a little unsure how to access it.
Purp stewards it freely. And in return, the tribe takes care of its chief.
Thank you, Mike Purpus, for your aloha. For the stories. For the laughs. For the radical performance in and out of the water—but most of all, for your stewardship of the things money can’t buy. Your aloha is woven into the very fabric of the South Bay’s communal identity, and for that, the tribe thanks you. •






Torrance Memorial and the Children’s Burn Foundation partner to provide 360-degree care for South Bay pediatric burn survivors and their families.
Written by Laura Roe Stevens
Burns are the fifth-leading cause of unintentional injury-related death for infants, children and teens under age 19 in America. In fact, more than 300 infants, children and adolescents die each year—while 80,000 are treated in emergency departments for burn injuries, according to the Centers for Disease Control and Prevention.
Torrance Memorial Medical Center’s partnership with the Children’s Burn Foundation provides topnotch medical care and rehabilitation while also easing financial and emotional strain for families as they navigate the road to recovery.
“Most people don’t realize the tremendous and long-lasting stress families experience when a child has a burn injury,” says Tanya Sorkin, chief program officer for the Children’s Burn Foundation, a Sherman Oaks-based nonprofit organization that provides financial, emotional and psychological assistance to burn survivors and their families.
“Many children require multiple surgeries; some aren’t fully covered by insurance. Parents need to be by their child’s side at the hospital, and this can require much time off work.”
Sorkin explains that hospital case workers let her team know if families of a pediatric burn patient become rent- or food-insecure, or if any siblings of the burn survivor need caregiving, transportation or emotional support during this time.
“It’s easy for a situation to spiral, and that’s where we can come in. We can provide gas cards, support groups, rent assistance and can even assist with co-payments for surgeries that a child requires that are not covered by insurance,” Sorkin adds.
Families of pediatric burn patients breathe easier when they come to Torrance Memorial, as they are guaranteed the highest quality of medical care by exceptionally trained and experienced physicians and staff who utilize the latest technology for reconstructive surgery and rehabilitation. The partnership with the Children’s Burn Foundation is especially meaningful for the long-standing relationships that physicians and staff build with the families, explains Matthew Reiss, MD, director of the Torrance Memorial Burn Center.
For instance, Dr. Reiss says, the foundation helped a local family whose lives were forever changed after their ADU burned down in 2024.

The Children's Burn Foundation helps young burn survivors and their families thrive through support, care and connection.
The fire killed the father, severely burned the mother and burned 60% of their 6-year-old daughter’s body. She was treated by Dr. Reiss and his team.
Another son with special needs lost a leg, and the 21-year-old son, who had not been home at the time of the fire, was left in charge to manage family care and the funeral for his father.
“It was traumatizing. And although the mother was out of the hospital earlier than her daughter, she was devastated and depressed and still had her own injuries,” explains Dr. Reiss. “The older son was the decision-maker and took care of the family. He received a lot of help from the Children’s Burn Foundation. The youngest needed multiple surgeries, including a tracheostomy, and they all had significant rehabilitation needs.”
Both Sorkin and Dr. Reiss reiterate how uplifting the services of the Children’s Burn Foundation are, as pediatric burn patients and families move from despair and pain into support, confidence and more ease. They get to know the families well and build long-lasting relationships. Each year, both Torrance Memorial Burn Center and the Children’s Burn Foundation host annual holiday parties where new and old families reunite year after year.
“It’s an incredible feeling to help a child recover from significant injuries, and to see families return for our annual holiday party,” says Dr. Reiss. “It’s my favorite part of the job and time of the year, as families return 20 to 30 years later! I get to see them doing well, and it feels great to know it’s due

to our care and the assistance that the Children’s Burn Foundation provides.”
Dr. Reiss admits that every time a child and family rush into the emergency department with significant burns, it’s hard. He holds on to the success stories and lets the family know they will be one too.
Tanya Sorkin, chief program officer for the Children's Burn Foundation, and Matthew Reiss, MD, director of the Torrance Memorial Burn Center, at an annual holiday family reunion party last December.

“When a child and family come in, I’m helping them through the most trying time in their lives. I tell them: ‘OK, this is hard right now, but I know in time I’ll see you dancing at our Christmas party. You’ll get through this. I’ve seen it.’ And it’s a wonderful feeling.” •
AT-A-GLANCE:
4,000
Helps 4,000 pediatric burn survivors and their families internationally each year.
1,000
Assists 1,000 local families annually with financial and psychological support.
200,000
Provides burn prevention education programs to 200,000 people every year, including teachers, parents, caregivers and students at elementary, middle and high schools.

parents with trusted resources, education and community support across the South Bay.
Laura Short McIntire founded a substance abuse and mental health resource for school-aged children and their parents.
Written by Nancy Sokoler Steiner I Photographed by Michael Neveux
The day after Laura Short McIntire attended a community meeting to brainstorm ways of addressing youth binge drinking and substance use, she proposed a new approach to prevention. Her concept was a scalable model that would connect parents with free online resources, shared personal stories, expert advice and in-person education events aimed at reducing stigma and helping youth thrive.
The principal of LSM Communications, McIntire has a background in strategic planning and communications. And her consulting work for the Thelma McMillen Recovery Center at Torrance Memorial gave her insight into substance abuse issues. (The center is the South Bay's only hospitalbased outpatient alcohol and drug treatment facility and offers programs for both adults and teens.)
McIntire’s concept struck a chord, so she and her LSM Communications team created South Bay Families Connected (SBFC). Implemented as a pilot project at Mira Costa High School in 2015, SBFC now partners with more than 100 South Bay schools.
SBFC’s website, southbayfamiliesconnected.org, offers original videos of teens and parents sharing their experiences, informative blogs and vetted resources addressing issues ranging from managing tech and social media in healthy ways to grief and loss and mindful parenting.
“It’s a place to find trusted resources on a wide variety of youth wellness issues,” McIntire says. “Administrators and school counselors like having a trusted landing place to send people.”
School administrators and members of the parent and youth advisory committees make suggestions about topics and content to add. “It’s all been incredibly positive and synergistic,” McIntire says.
In addition to free parent education events, SBFC holds a monthly Families Connected Parent Chat in partnership with Beach Cities Health District and the Thelma McMillen Recovery Center. The free support group, open to parents from all participating schools, is led by McIntire and Moe Gelbart, MD, Torrance Memorial’s director of behavioral health.
“The Parent Chat has been a wonderful resource for me as we navigated elementary school, middle school and high school and all the unique challenges each of those stages brings into our lives,” says one parent participant. “It's a wonderful space where I feel safe to share concerns and challenges, seek advice from peers and get reassurance that I’m not alone.”
Prior to launching SBFC, McIntire held positions in the health care management consulting division of Ernst & Young, Providence Saint Joseph Medical Center and Cedars-Sinai Cancer.
She notes that SBFC would not be a nonprofit today if it weren’t for the tireless efforts of Ellen Rosenberg, former Manhattan Beach Unified School District member and SBFC’s first board president, and Charlotte Gesten, former board COO. Today Ann Marie Whitney heads the board with support from key officers Ann Lundy and Naya Elle James.
“I’m grateful I was invited to the table and had the ability to build something the community has embraced, but our success has been made possible by our numerous school and community partners and the dedication of our board members and volunteers,” she says. “It’s my privilege to be in a position to connect, listen and collaborate.” •

Brady Barrett’s butterfly habitat restoration project hints at his career goals.
Written by Nancy Sokoler Steiner I Photographed by Michael Neveux
When it came time to plan his Eagle Scout project, Brady Barrett chose to focus on rescuing a small blue insect about the size of a thumbnail. More specifically, he partnered with the South Bay Parkland Conservancy to help restore the native habitat of the El Segundo blue butterfly, a species that came close to extinction just a few decades ago.
“My grandparents and my dad are from El Segundo, so I was familiar with the restoration effort,” says Barrett, a senior at St. John Bosco High School in Bellflower. Working with the conservancy and the city of Redondo Beach, he identified an area in Czuleger Park to clean up and then plant buckwheat and other native species. The area is now part of a wildlife corridor that will eventually stretch from El Segundo to the Palos Verdes Esplanade and through the Hermosa Beach Greenbelt.
“There were some empty dirt patches that had become covered with dog poop and other trash, so the residents weren’t happy and it wasn’t hospitable to the butterflies,” Barrett explains.
The project took place over two weekends and involved 28 volunteers. The first weekend involved clearing the debris

and preparing the soil for new plants. Planting happened the second weekend.
Scouts who wish to earn the rank of Eagle, the highest rank within scouting, must carry out a service project. Only 4% of scouts reach this rank, which also requires earning 21 merit badges and holding leadership positions within the troop. The process generally takes at least six years to complete. Barrett has met all the requirements.
Scouting is not Barrett’s only experience serving his community. He also participated in Torrance Memorial Medical Center’s High School Volunteer Program. This entails committing to regular volunteer service as a hospital escort for a period of 13 months and draws many more applicants than positions available. Escorts assist with various tasks, including transporting patients by wheelchair, delivering specimens to the lab, and conveying medical charts and supplies around the hospital.
“It’s my goal to become a surgeon, so this was a great way to get a feel for the hospital environment,” he says. “The experience at Torrance Memorial has 100% reinforced my goal.”
Barrett attends a specialized biomedical program at his high school. It offers classes, such as molecular biology, typically encountered only in university settings. To further his medical experience, he attended a high school program at Children’s Hospital Los Angeles, where he was able to shadow physicians and learn more about different fields of medicine.
“I think my experience at Torrance Memorial helped me get selected for this program,” he says.
Ever mindful of his career goals, Barrett applied and was accepted for a high school summer fellowship at The Lundquist Institute for Biomedical Innovation at Harbor-UCLA Medical Center. It involved hands-on training with institute faculty in their labs, conducting an intensive research project and presenting his findings.
Whether protecting tiny butterflies, interacting with hospital patients or doing research, Barrett seems drawn to curing and restoring. •

Class Schedule for 3105 Lomita Blvd., Torrance
Register online or call 310-517-4711 to enroll. $80 ($72 for ADVANTAGE members) for 8-week series; $40 ($36) for 4-week series. Prenatal yoga is $88 for 8-week series.
ALL CLASSES ARE HYBRID (IN-PERSON & ZOOM) UNLESS OTHERWISE NOTED
BONES FOR LIFE WITH JOY *NEW CLASS (IN-PERSON ONLY)
March 9–April 27; May 11–June 29
July 13–August 31
September 14–November 2
Monday, 12:30 to 1:30 p.m. Feldenkrais exercises support bones through gentle, weight-bearing exercises requiring no strain or pain. Improve posture and bone health.
CHAIR YOGA FOR BONE HEALTH WITH DEBI
March 11–April 29; May 13–July 1
July 15–September 2
September 16–November 4
Wednesday, 11:15 a.m. to 12:15 p.m. For those with osteopenia or osteoporosis. Strengthen muscles and bones, improve posture and balance, fall prevention, breath work. All levels.
CHAIR YOGA FOR STRENGTH AND BALANCE WITH SHARMONE (IN-PERSON ONLY)
March 9–April 27; May 11–June 29; July 13–August 3 (4 weeks only); September 14–November 2 Monday, 2 to 3 p.m.
March 12–April 30; May 14–July 2; July 16–August 6 (4 weeks only); September 17–November 5; Thursday, 2 to 3 p.m.
Use a chair in seated and standing poses to improve strength and balance.
ESSENTRICS FULL–BODY STRETCH WITH AI (IN-PERSON ONLY)
March 9–April 27; May 11–June 29;
July 13–August 31; September 14–November 2
Monday, 11 to 11:50 a.m.
March 13–May 1; May 15–July 3; July 17 –September 4; September 18–November 6
Friday, 11 to 11:50 a.m.
A gentle, full-body stretch to activate muscles, free joints and increase mobility. Bring a yoga mat.
INTEGRATED YOGA WITH ROBIN
March 11–April 29; May 13–July 1; July 15–September 2; September 16–November 4
Wednesday, 7 to 8 p.m.
Breath work, postures and meditation, such as yoga nidra.
LINE DANCING: THE NEXT STEP WITH SHARON
March 11–April 29 (no class 4/22; makeup on 5/6); May 13–July 1; July 15–August 5 (4 weeks only); September 16–November 4
Wednesday, 3:15 to 4:15 p.m.
Learn high beginner/improver line dances, complex steps. Previous line dancing experience required.
LINE DANCING BEYOND “COUNTRY” WITH SHARON
March 11–April 29 (no class 4/22; makeup on 5/6); May 13–July 1; July 15–August 5 (4 weeks only); September 16–November 4 Wednesday, 4:30 to 5:30 p.m.
Learn Country Western favorites, chacha, mambo, tango and samba in line dancing style. No partner needed.
MAT/FLOOR PILATES WITH KAREN (IN-PERSON ONLY)
March 10–April 28; May 12–June 30; July 14–September 1; September 15–November 3
Tuesday, 4 to 4:50 p.m.
All-levels class strengthens core muscles to improve balance. Moderate fitness level. Bring a mat.
MUSCLE STRENGTHENING: BEGINNING & INTERMEDIATE WITH RANDY (ZOOM ONLY)
March 10–April 28; May 12–June 30; July 14–September 1; September 15–November 3
Tuesday, 11 to 11:50 a.m.
March 13–May 1; May 15–July 3; July 17 –September 4; September 18–November 6
Friday, 11 to 11:50 a.m.
Strengthen your upper and lower body using flexible exercise bands.
STRETCHING FOR BETTER BALANCE WITH RANDY (ZOOM ONLY)
March 10–April 28; May 12–June 30; July 14–September 1; September 15–November 3
Tuesday, 10 to 10:45 a.m.
March 13–May 1; May 15–July 3; July 17 –September 4; September 18–November 6
Friday, 10 to 10:45 a.m.
Increase flexibility and mobility to help prevent injuries.
BEGINNING TAI CHI WITH RICHARD (ZOOM ONLY)
March 10–April 28; May 12–June 30; July 14–September 1; September 15–November 3
Tuesday, 2 to 3 p.m.
Intro to the form of this Chinese exercise that inspires well-being.
INTERMEDIATE TAI CHI WITH RICHARD (ZOOM ONLY)
March 11–April 29; May 13–July 1; July 15–September 2; September 16–November 4
Wednesday, 2 to 3 p.m.
Learn how to complete the form.
ADVANCED TAI CHI WITH RICHARD (ZOOM ONLY)
March 11–April 29; May 13–July 1; July 15–September 2; September 16–November 4
Wednesday, 3:15 to 4:15 p.m.
Go deeper into refining movement,
leading to improved health and mental focus.
YOGA BASICS WITH LAURA (ZOOM ONLY)
March 9–April 27; May 11–June 29; July 13–August 31; September 14–November 2
Monday, 4 to 5 p.m.
Gentle yoga poses on the floor and standing; breath work and meditation.
YOGA THERAPY FOR OSTEOPOROSIS WITH DEBI
March 10–April 28; May 12–June 30; July 14–September 1; September 15–November 3
Tuesday, 11 a.m. to 12:15 p.m.
Poses and breath work stimulate bone growth and increase strength, range of motion, posture and balance. Floor, chair and standing poses. Bring a mat.
YOGA FOR WELLNESS WITH DEBI
March 11–April 29; May 13–July 1; July 15–September 2; September 16–
November 4
Wednesday, 9:30 to 10:45 a.m.
Correct posture; increase strength, flexibility and range of motion.
Class Schedule for Malaga Cove, 2550 Via Tejon, Palos Verdes Estates
ALIGN THE SPINE WITH JOY
March 9–April 27; May 11–June 29; July 13–August 31; September 14–November 2, Monday, 9 to 10 a.m.
These Feldenkrais Method lessons help posture without pain or strain. Bring an exercise mat, hand and bath towel.
BONES FOR LIFE WITH JOY
March 9–April 27; May 11–June 29; July 13–August 31; September 14–November 2
Monday, 3:30 to 4:30 p.m.
These Feldenkrais Method exercises help support bones through gentle, weightbearing exercises—no strain or pain. Improve posture and bone health.
CHAIR EXERCISE: BEGINNING & INTERMEDIATE WITH PAM
March 10–April 28; May 12–June 30; July 14–September 1; September 15–November 3
Tuesday, 9 to 10 a.m.
Improve strength and balance using a chair. Bring exercise band and light hand weights (optional).
EXERCISE TO THE OLDIES WITH PAM
March 10–April 28; May 12–June 30; July 14–September 1; September 15–November 3
Tuesday, 10:15 to 11:15 a.m.
Standing and floor exercises to promote endurance and flexibility. Bring a mat, light hand weights and a "can-do" attitude!
ESSENTRICS® STRENGTH: FULL BODY STRETCH *NEW CLASS
March 8–April 26; May 10–June 28; July 12–August 30; September 13–November 1
Sunday, 9 to 9:50 a.m.
Strengthening/stretching to develop a toned, pain-free body. Includes floor exercise. Bring yoga mat.
ESSENTRICS® FULL–BODY STRETCH WITH AI
March 11–April 29; May 13–July 1; July 15–September 2; September 16–November 4
Wednesday, 11 to 11:50 a.m.
A gentle, full-body stretch to activate muscles, free joints and increase mobility. Bring a yoga mat.
YOQI® QIGONG FLOW & SOUND BATH
*NEW CLASS
March 8–April 26; May 10–June 28; July 12–August 30; September 13–November 1
Sunday, 10:30 to 11:40 a.m.
Gentle, slow movements, breath work, self-massage, sound bath meditation. All levels. Bring yoga mat. Blanket/pillow and eye pillow optional.
MUSCLE STRENGTHENING: BEGINNING & INTERMEDIATE WITH RANDY
March 9–April 27; May 11–June 29; July 13–August 31; September 14–November 2
Monday, 11:30 a.m. to 12:15 p.m.
Learn correct, safe techniques for strengthening your upper and lower body using a chair and flexible exercise bands.
MUSCLE STRENGTHENING:
INTERMEDIATE WITH RANDY
March 12–April 30; May 14–July 2; July 16–September 3; September 17–November 5
Thursday, 11:30 a.m. to 12:15 p.m.
Learn correct, safe techniques for strengthening your upper and lower body using a chair, flexible exercise bands and hand weights.
STRETCH & SOUND BATH MEDITATION WITH AI
March 11–April 29
May 13–July 1
July 15–September 2
September 16–November 4
Wednesday, 9:30 to 10:20 a.m.
March 14–May 2
May 16–July 4
July 18–September 5
September 19–November 7
Saturday, 12:30 to 1:20 p.m.
Gentle stretches, breath work, sounds and vibrations from various sound bath instruments. Bring a yoga mat, blanket, and pillow.
YOGA FOR STRESS REDUCTION WITH DEBI
March 14–May 2
May 16–July 4
July 18–September 5
September 19–November 7
Saturday, 9:30 to 10:45 a.m.
Gentle yoga poses on the floor, seated and standing to increase flexibility, strengthen the body and improve balance. Breath work and meditation reduce stress.
Don’t


Dr. Jamie Kagihara, 40
Hometown: Aiea neighborhood of Honolulu
South Bay community: Hollyglen neighborhood of Hawthorne
Education: BA in biology from USC, 2008; MD, 2012, and internal medicine residency, 2015, from the University of Hawaii; pulmonary and critical care fellowships from USC Keck, 2018
Side gig: Balloon garland creator at Chulypopping, @chulypopping
A critical care pulmonologist’s side gig involves inflating thousands of party balloons.
Written by Diane Krieger I Photographed by Siri Berting
It’s a Thursday evening in mid-December, and Jamie Kagihara, MD, is fast-walking home from a neighborhood park where she just finished making a festive balloon garland for Hollyglen’s annual Santa parade.
Dr. Kagihara—or Dr. Balloons, as she’s known in this cozy neighborhood of Hawthorne—is an exceptionally energetic physician. A board-certified critical care pulmonologist, she lives at a breathless pace. Between her medical practice, parenting and many volunteer roles in her community, Dr. Kagihara’s lungs get plenty of exercise even without blowing up balloons. (Full disclosure: She mostly uses an electric pump.)
Dr. Kagihara started making balloon decorations three years ago. She got the idea after pricing professionally made garlands for her son’s birthday party. Sticker shock prompted her to make her own, learning from YouTube videos. She’d always been creative—before balloons, it had been photography and scrapbooking. Friends started asking her to create garlands for their parties. Before long, she started charging for her services—keeping her price well below the commercial rates that had so incensed her. She partnered with Torrance Memorial ICU nurse Emily Lee, and the hospital became one of their clients.
Business is brisk. Dr. Kagihara pumps air several nights a week, creating everything from dainty balloon bouquets to sweeping garlands.
A proud Sansei (third-generation Japanese American) from Honolulu, Dr. Kagihara grew up ocean-swimming and surfing. Her interest in lungs started with a healthy appreciation for the importance of holding one’s breath when tumbled by epic waves off Waikiki Beach.
A self-described “huge tomboy,” she played varsity volleyball and softball at the prestigious Punahou School in Honolulu. She attended USC for college, went back to Hawaii for her medical education and residency, and returned to USC for fellowships in pulmonology and critical care.
Medicine runs in the family. Her father, Lance Kagihara, MD, is a much-beloved internist, and younger sisters Jodi Kagihara, MD, and Jaclyn Kagihara, MD, specialize in hematology-oncology and interventional gastroenterology,
respectively. They all practice in Honolulu.
Jamie settled on pulmonary critical care because “in chaotic situations, I can be calm and make quick decisions. I think it stems from growing up in the Aloha state—having a cool, grounded mind,” she says.
When she joined Torrance Memorial in 2018, she was the hospital’s first dedicated intensivist. During the pandemic, she was one of seven pulmonologists pulling 12-hour shifts to care for the hospital’s sickest patients.
Heavenly Hollyglen
While she misses O‘ahu, Dr. Kagihara has laid roots in the South Bay. Weekends revolve around her two young sons’ activities: baseball, soccer, basketball.
“My kids are my everything,” she says. “They do Kumon, jujitsu and they’re learning to speak Mandarin.”
Her husband, Bryan Chu, keeps the family on track, managing their finances, shuttling the kids to after-school activities and volunteering at their school. A brand marketer with recruiting giant Robert Half, he works remotely from home.
“Bryan is amazing,” Dr. Kagihara says, heaping praise on her spouse. “He wakes up before me, and he’ll make hot breakfast for everybody. Then we walk to school or meet up with neighbors and ride together on bikes.”
Dr. Kagihara wears many hats in the family-friendly neighborhood nestled between Rosecrans Avenue and El Segundo Boulevard just north of Costco. She serves on the Citizens’ Bond Oversight Committee of the Wiseburn Unified School District and is a member of her sons’ elementary school site council and an active PTA member.
“Can I emphasize how great this community is? The people in Hollyglen have become our chosen family,” she says. “I want to be involved and contribute to the community in any way possible.”
She brings the same enthusiasm and energy to Torrance Memorial, where she chairs the critical care committee. The first pulmonologist to practice at the El Segundo office, she works long hours seeing patients in the wards and outpatient clinics.
But when the day is finally done, Dr. Kagihara trades the committees and clinical rounds for something airier, answering to the title of Dr. Balloons. •
October 3
The ninth annual YPPA Casino Night was an incredible success, raising $141,000 in support of the expansion of Torrance Memorial’s emergency department. More than 150 guests gathered at Shade Hotel Redondo Beach for a high-energy evening of blackjack, roulette, poker and craps—all united by a shared commitment to exceptional health care close to home. To stay involved and learn more about upcoming YPPA events, visit TorranceMemorial.org/YPPA.
Photographed by Ed McClure











8. Lauren Bauer, Kimberly Brown
9. Juliana Rios, Vincent Rios
10. Mona Madani, MD, Lisa Cook, MD, Mahsa Madani MD, Keanu Haghighi
11. Vimal Murthy, MD, Tram Tong, Julie Meyer-Silvino, Greg Heyes
12. Terri Zajec
13. Jamie McKinnell, MD, Heidi Hoffman, MD
14. Chris Reekie, Iris Reekie, Michael Zislis, Elisa Anhalt, MD, Doug Laurin, Nadine Bobit, Tonny Lee, MD
15. Pooja Kumar, MD, Lauren Estabrook, Lindsay Colker, Sejal Penkar, Khushboo Sareen, Lindsay Ashcraft, Seema Dhir




October 20
Torrance Memorial Ambassadors gathered at the California Surf Club for an evening honoring the strong partnership between the hospital’s medical experts and philanthropic community. Moderated by Kurt Hansen, MD, co-medical director of the Lundquist Leach Emergency Department, the physician panel included Dilrukshie Cooray, MD, rheumatology; Jeffrey Kim, MD, neurology; Soohan Mansuri, MD, family medicine; and Alexander Mejia, MD, gynecology. The speakers gave expert insight on timely topics including brain health and aging, bone health and advances in GLP-1 weight management. The event celebrated philanthropy and the community’s commitment to exceptional healthcare close to home.
Photographed by Ed McClure











December 2
The holiday season kicked off at the Festival Fashion Show by Nordstrom, part of Torrance Memorial’s 42nd annual Holiday Festival held on the hospital's campus. Guests enjoyed runway presentations, boutique shopping and a festive luncheon, with proceeds benefiting Torrance Memorial's emergency department expansion campaign.
Photographed
by
Ed McClure




1. Jackie Geiger, Kathy Santarosa, Carla Zanino
2. Denise Pellegrino, Maura Mitzuguchi, Cindy Sutherland, Celine Ott, Sandra Wang, Dora Ngan, Monica Masuda, Jennifer Chang, Jackie Wang, Michele Dee, Wan-Ping Yu, Jessica Tsai, DDS, Samantha Jean, Zandria Sia, Dede Hsu
3. Ellen Baker, MD, Alexandra Grossman, MD, Gretchen Lent, MD, Mina Diaz, Christina Ham, Melissa Benoit
4. Cindy Hagelstein, Terry Hohm
5. Myra Quesada, Suzanne Sussman, Jenny Ha, Cami Evans, Karen Sinfield, Joy Theodora, Dolly Narang, Tina Funiciello, Anya Khomut, Beth Bowen
6. Laura Schenasi, Song Klein, Nadine Bobit, Helaine Lopes




7. Renee Berliner, Kathleen Parks, Teri Hogan, Nadine Bobit, Karen Melideo
8. Chris Carreon, Elisa Chen, MD, Lora Cohn, Leena Gupta, Deveena Chandra, Kay Sheth (seated), Stephanie Coale, Lori Sherman, Vandana Sheth, Bharti Sheth
9. Michelle Tangeman, Alexandra Rogers, Justine Gregorio, Kaylynn Gregorio, Sophia Neveu, Carissa Ellis (standing), Annsley Marshall, Maria Sass, Nadia Carson, Delaney Brown (seated)
10. Stacey Markulis, Jana Stills, Ellen LaBonte, Erin Hansen.



11. Cindy Kaplan, Roxanne Mirahashmi, Teri Young, Godrat Golkar, Linda Golkar
12. Heidi Mackenbach, Julie Sanders, Sandra Sanders, Brenda Okuma
13. Timme Gunderlock, Jordon Wells, Santa Claus, Stacey Markulis, Diana Brandt, Jana Stills, Robin Smith, Barbara Bentley, Ellen LaBonte
14. Valerie Adlam, Lisa Noski, Andrea Sala, Elizabeth Burdiak, Jennifer Morgan (standing), Charlotte Adlam, Elaine McRae (seated)
15. Mary Keener, Karen Mohr, Minda Schechter, Betsy Bailey (back), Karen Gottleib, Judith Gassner, Hilary Zachry, Cristin Rigg, Libby Slane




December 5
The 42nd annual Holiday Festival Gala at Torrance Memorial was a night to remember, raising $2.1 million to support the hospital’s emergency department expansion. Held in a 23,000-squarefoot tent, the evening featured gourmet dining, premier and silent auctions, and 32 stunning holiday trees. The highlight of the evening was a transformative gift from Melanie and Richard Lundquist. We extend our heartfelt thanks to our donors, community, leaders and attendees for making this evening a resounding success. Save the date for next year’s gala and continue supporting the future of exceptional health care in our community.
Photographed by Ed McClure & Philicia Endelman






5. Laura Schenasi, Mary Tu
6. Sandii Minshull, London Theodora, Ava Mackenna, Jaden Theodora, Pat Theodora
7. Mark Lurie, MD, Zac Gray, MD, Amanda Clauson, MD, Kurt Hansen, MD, Erin Hansen, Brandy Van Zitter, Brian Miura, MD, Rhea Mathews, MD, Elisa Anhalt, MD, Stephanie Tang, DO, Tonny Lee, MD, Margaret Hsiau, MD, Brett Lorber, MD, Brian Lee
8. Twanna Rogers, Tim Rogers







9. Jack Baker, Ayne Baker, Nicholas Maddox
10. Darrin DelConte, Michelle DelConte, Eileen Mahoney, Jim Mahoney
11. Jerry Marcil, Pat Theodora, Carol Marcil, Lori O’Hern, Tom O’Hern
12. Steve Wright, Mary Wright, Heidi Assigal, Gerhard Eberhart
13. Brandon Halvorsen, Greg Halvorsen, Laurie Inadomi-Halvorsen, Ryan Halvorsen
14. Ralph Simmons, Priscilla Hunt, Brenda Nowotka
15. Lori Baldwin, Dave Baldwin, Janice Tecimer, Timur Tecimer
16. Philippe Neveu, Sophia Neveu, Jenn Hohm, Brandon Hohm



Torrance Memorial Medical Center is making strong progress on a major expansion of its emergency department (ED)—an investment designed to better serve the South Bay community now and into the future. The two-story ED expansion is well underway and is expected to open in spring 2027.
As construction continues, the vision for the expanded ED is beginning to take shape. On the second floor, framing is in progress, transforming floor plans into visible patient rooms and care areas. At the same time, essential behind-the-scenes infrastructure is being installed, including upgraded electrical and data systems, plumbing, fire sprinklers and a modern pneumatic tube system. These improvements will support safe, efficient operations once the new space opens.
A critical component of the project is enhancing the triage experience, which plays a vital role in emergency care. Construction to expand the number of triage bays began last fall and is expected to be completed this spring. This improvement will allow patients to be assessed more quickly upon arrival, helping streamline care during busy periods. During construction, the

ED remains fully operational using a temporary triage area located adjacent to the waiting room.
On the first floor, steel framing for a new reception desk has been installed, creating a more welcoming and organized arrival experience for patients and families. Meanwhile, the second floor continues to take shape with framed patient rooms and clearly defined care pods designed to support privacy, safety and efficient patient flow.
The expansion also includes important upgrades for staff. The former Neonatal Intensive Care Unit on 3 Tower is being converted into dedicated ED staff support areas, providing space for care teams to collaborate, recharge and
prepare—an essential part of delivering exceptional patient care.
Construction activity is occurring primarily during early morning hours, and some noise is expected as work continues in multiple areas of the hospital. Torrance Memorial is committed to proactive communication and thoughtful planning to minimize disruption while ensuring patient comfort and safety.
When completed, the expanded ED will significantly enhance Torrance Memorial’s ability to care for patients in emergency situations—offering more space, improved efficiency and advanced technology to meet the evolving needs of the community. •
The expanded emergency care facility, expected to open in early 2027, will feature:
• More than 80 treatment spaces, including dedicated behavioral health rooms—double the department’s current capacity.
• A modular, open-concept design with flexible spaces that can adapt to changing patient and staff needs.
• Glass-partitioned rooms to enhance visibility, safety, security and privacy.
• A waiting room with two separate patient areas.
• Enhanced technology to improve efficiency, communication and patient safety.