
12 minute read
Hypersomatotropism Why my cat is so resistant to insulin
Hypersomatotropism
Why my cat is so resistant to insulin
By Teresa Budge
Dip Animal Health Technology, RVT AVN and AVNAT Continuing Professional Development
Hypersomatotropism is where the pituitary gland is excessively producing growth hormone (GH). GH is the hormone responsible for tissue growth and cell reproduction and regeneration. It consists of a long, single chain of amino acids called a polypeptide, and is produced in the cells of the anterior pituitary gland. Excessive GH production then leads to an increase in production of insulin growth factor 1 (IGF-1). IGF-1 is mainly produced in the liver. They both follow the same trend in the blood; if one is increased, the other follows suit.1
THE PITUITARY GLAND The pituitary gland is an integral part of the body. Located at the base of the brain, it regulates multiple hormones in the body. There are two main parts to the pituitary gland: the adenohypophysis (anterior pituitary) and the neurohypophysis (posterior pituitary). Each side controls its own certain hormones; however, together they control the production of seven major hormones in the body. The first five are controlled by the adenohypophysis2 and the last two are controlled by the neurohypophysis. 1. adrenocorticotropic hormone (ACTH), which stimulates the adrenal glands to produce cortisol 2.thyroid stimulating hormone (TSH), which stimulates the thyroid gland to produce thyroxin 3.growth hormone (GH), which regulates muscle and bone growth 4.follicle stimulating hormone (FSH)/ luteinising hormone (LH), which together aid in follicular growth and ovulation 5.prolactin (PRL), which enables milk production in mammals 6.oxytocin (OXY), which plays key parts in reproduction and social behaviour 7.antidiuretic hormone (ADH), which regulates the water balance in the body. It tells the kidneys when to release water (via urine) and when to retain it. This helps maintain blood pressure, fluid volume of the blood vessels and sodium concentrations.
PRESENTATION AND DIAGNOSIS Cats can present to the veterinary hospital with a vast range of clinical signs. Cats in early stages of disease still have excessive GH being produced. Even before diabetes has been diagnosed, the patient may present with weight gain and signs of excess GH production, such as polyphagia (increased appetite), polydipsia (increased thirst) and polyuria (increased urination).3 There may be a period after diabetes is diagnosed where insulin requirements are considered relatively normal (1–3 international units (IU) per cat).1 There will eventually be a notable pattern of poor response to insulin requiring over 3 IU per kilogram and still resulting in persistent hyperglycaemia (normal range 4.5–7 mmol/L). A cat with hypersomatotropism will usually be overproducing growth hormone for a period of months before they develop the symptoms of acromegaly, which is the condition seen when this occurs. A cat with acromegaly will usually have a diabetes mellitus (DM) diagnosis beforehand, though DM can sometimes present after the acromegaly diagnosis.4 It occurs predominantly in male cats over 8 years of age (can range from 4–17 years).1 The symptoms may also not be very noticeable at first as they can develop slowly. Clinical signs of chronic, increased
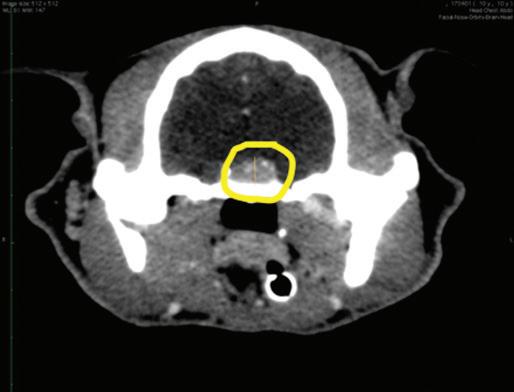


levels of IGF-1 are prognathia inferior (enlarged mandible), enlarged or clubbed paws, degenerative arthropathy, a stertor or snore due to thickening of the oropharyngeal tissue, cardiac changes such as myocardial hypertrophy (enlargement and thickening of the heart muscle) and often organomegaly (enlarged liver, spleen, kidneys or even thyroid).1 A physical exam is always the best place to start. Start by getting a baseline heart rate, respiratory rate and effort, temperature, and weight. In a patient that is having historical weight gain (extra muscle and bone growth due to increased IGF-1 levels) despite poorly controlled diabetes, acromegaly should be considered. A systolic heart murmur can also be a clinical sign of acromegaly (due to the heart wall thickening). Collecting and submitting a complete blood panel is also helpful to identify any additional, concurrent issues. A patient with acromegaly and concurrent unregulated diabetes will usually have serum abnormalities such as hyperglycaemia (high glucose), hyponatraemia (low sodium) and hypochloraemia (low chloride), hyperkalaemia (high potassium), and some elevated liver enzymes such as total bilirubin (Tbil), alanine amino transferase (ALT) and alkaline phosphatase (ALKP). In the absence of underlying haematological disease, only the occasional mild increase in haematocrit was seen on a complete blood count.5 There are a few places that run validated immunoassays for IGF-1 testing. Royal Veterinary College in the UK and the Diagnostic Centre at Michigan State University are two. Conveniently, Idexx Laboratory here in Australia now has IGF-1 testing available. They will send samples to the RVC in the UK for testing. Otherwise, samples can be submitted straight from the consulting vet clinic to the RVC. Results greater than 1000 ng/mL (normal is < 795 ng/mL6) is abnormal and considered a marker for hypersomatotropism.7 Computed tomography, or CT, is recommended to assess the brain to identify a mass or growth of the pituitary gland. This helps in diagnosis of hypersomatotropism and is helpful when planning a radiation or surgical approach for treatment. HOW DO WE TREAT HYPERSOMATOTROPISM? There are a few different treatment options available for a cat with a pituitary mass causing an increased GH production. The two main recognised ways to treat this condition are by radiation therapy and surgery.7 Radiation therapy involves the use of a linear accelerator (commonly referred to as a LINAC), which delivers high doses of energy or electrons as a beam targeting a patient’s tumour with the intent to shrink it. The more conventional and safer approach is definitive radiotherapy (DR). Definitive radiotherapy delivers radiation in the safest way, as it splits up a large dose into multiple small ones. The patient needs to undergo 20 radiation treatments, Monday to Friday over 4 weeks, each one requiring a short general anaesthetic. A newer protocol starting to be used is stereotactic radiotherapy (SRT). This approach delivers 3 large doses over 1 week, each also requiring a general anaesthetic. With the availability of newer planning capabilities and delivery techniques, SRT has good
Continued from previous page
safety margins, though because of the large doses there is still a risk of harmful radiation effects on the surrounding normal brain tissue. Overall, the mean survival rate of a patient undergoing SRT is longer than the survival rate of one undergoing DR, whether it is due to less anaesthesia time or that SRT delivers doses more effective to pituitary tumours.8 Radiotherapy generally has few side effects but is not usually successful in decreasing the level of GH and therefore IGF-1 being produced. While increased insulin sensitivity and possibly even diabetic remission can be seen with radiotherapy, the clinical manifestations (arthropathies, myocardial changes, etc.) associated with increased IGF-1 levels can take years if at all to rectify.1 The surgical approach, called a hypophysectomy, removes the pituitary tumour and gland in one go due to the small size. The patient is anaesthetised during the procedure and placed into sternal recumbency with the head held up by a surgical head frame. The rigid head frame is needed to keep the patient as still as possible. The pituitary gland with tumour may only measure a few millimetres in diameter and can be extremely close to important nerves and arteries. The site is then accessed through the soft palate in the mouth. Surgery is the best option for curing acromegaly. It is considered the optimal approach with a much higher incidence of diabetic remission and decrease of IGF-1 and GH levels, as most cats (60–80%) have much better diabetic control or go into diabetic remission within one month.7 Surgical success is dependent on the size of the tumour as well as the experience of the surgery and postoperative care teams. Success rates with an established team (neurosurgeons, surgical nurses, internal medics, and nurses, criticalists and ICU nurses) are 90–96% (4–10% mortality rate)7; they help see the patient through to discharge and beyond. It is good practice to place a multiple lumen central venous catheter into the cat before proceeding to surgery. It will allow for easy access for serial blood glucose monitoring in theatre and will help with all the blood collections needed for the first few days postoperatively without compromising peripheral veins with multiple blood draws. MEDICATIONS AND FLUIDS REQUIRED There are several fluids and medications a hypophysectomy patient needs to receive while in theatre and postoperatively. Cats undergoing hypophysectomies usually have some degree of heart disease due to the thickening of the heart from the increased GH production. For this reason, fluid rates need to be conservative during surgery, preferably not going above 4 millilitres per kilogram per hour (mL/kg/hr). Pain management: A fentanyl constant rate infusion (CRI) is recommended intraoperatively for pain relief. This should be delivered at an undiluted concentration of 50 micrograms per millilitre (ug/mL) to allow for smaller volumes to be delivered. Fluids: The patient should be on a fluid drip of compound sodium lactate (Hartmann’s) during surgery and an appropriate isotonic (0.9% NaCl/ Hartmann’s) or hypotonic (0.45% NaCl or glucose 5%) fluid postoperatively. The electrolyte levels of sodium and potassium postoperatively will dictate which IV fluid is chosen. It is expected, once the pituitary gland is removed, that the cat will become hypernatremic (increased sodium levels) due to the lack of ADH being produced by the neurohypophysis (posterior pituitary).9 Insulin: An actrapid (regular insulin) CRI will need to be started to help keep control of the cat’s hyperglycaemia. A special, highly concentrated dose of 11 international units per kilogram (normal is 1.1 iu/kg) is added to a 240 mL bag of regular 0.9% sodium chloride. The infusion is then adjusted as needed in response to the blood glucose, only needing to run at low rates to keep our fluid volumes low. Cortisone: Since the adrenals will no longer be receiving any ACTH stimulus from the pituitary signalling them to release cortisol, a hydrocortisone sodium succinate (HSS) CRI will need to be started as soon as the

Fluid pumps – Courtesy of A Lam. Small Animal Specialist Hospital Kenny, P et al. Efficacy of hypophysectomy for the treatment of hypersomatotropism. Journal of Veterinary Internal Medicine. 2021:16080

pituitary is reached. This CRI is diluted to a 1 milligram per millilitre (mg/mL) concentration. Without any cortisol in the body, the patient can develop hypotension, weakness, inappropriate mentation and even seizures and death. All these infusions need to be running no higher than a combined 4 ml/kg/hr. The fentanyl CRI can be discontinued once awake and buprenorphine started. The Actrapid CRI will continue for a few days postoperatively until the cat can be transitioned back onto their subcutaneous insulin (most commonly for cats it would be the long-acting insulin glargine, though some may be on another type). Sublingual (under the tongue) or subconjunctival (under the conjunctiva of the eye) synthetic diuretic hormone (called Vasopressin or DDAVP) will need to be administered for the rest of the cat’s life (in most cases three times daily). The hydrocortisone CRI should be continued until the cat is eating well and can be transitioned to oral cortisone. Oral cortisone and oral thyroxine (since no more TSH will be produced) will be lifelong medications for the cat as well.
NURSING CARE There are multiple areas in the process of diagnosis, treatment and postoperative care where nurses can put their skills to good use. Diagnosis of this condition requires blood collection and sample submission to both local and international laboratories. Accurate recording of patient health statuses is required (weight monitoring, auscultation of any new heart murmurs) and is something that the nurse can keep on top of. For preoperative planning, working with the veterinarian to calculate appropriate fluid and medication rates as well as working with an anaesthesiologist to create an appropriate anaesthetic plan for the patient. Postoperatively, a hypophysectomy patient will need intensive care. Recovery in the ICU for multiple days is required. If available, placing a Freestyle Libre glucose sensor can be helpful for less invasive monitoring of the cat’s glucose levels as well. Blood glucose readings will fluctuate postoperatively, and electrolyte levels (sodium, potassium and chloride) will be greatly affected due to the loss of antidiuretic hormone production from the neurohypophysis..9 These will be monitored quite closely for the first 5–7 days by the intensive care nursing and veterinary teams and fluid plans can be altered accordingly. Postoperatively, cats should be offered food as soon as they are up and walking around. Nurses can offer a variety of soft, warmed cat foods to tempt the patient into eating. Anti-nausea drugs such as maropitant and ondansetron can be used to combat any nausea and mirtazapine can be administered as an appetite stimulant. Nurses should take care when tableting a postoperative hypophysectomy patient as the surgical site is on the roof of the mouth and fingers or pill poppers can damage the site. Urine outputs should be monitored closely, without using a urinary catheter. This can be done by weighing the clean litter and box before offering it to the cat, then reweighing it after urination. Unfortunately, this is only accurate if the cat doesn’t kick litter out of the box or doesn’t do a bowel movement in it. Monitoring urine output is important as when there is a lack of ADH (or Vasopressin) being produced by the neurohypophysis, the urine becomes excessively dilute, and the animal becomes polyuric. If the patient isn’t getting appropriate replacement of water or IV fluids, they become hypernatremic.10 Care for a central line, or jugular catheter, includes close monitoring for slipping or swelling, and at least every 8 to 12-hour inspections of the site. Any unused ports need to be flushed with small amounts of saline every 4 hours to keep patent. Proper flushing techniques and sampling techniques need to be adhered to so that it is kept as aseptic as possible and no air is introduced into the lines. Mentation status should be monitored closely for dullness, ataxia, head pressing, or other signs of intracranial pressure post-surgery. The blood glucose levels should be monitored quite closely for the first several days in case the cat quickly develops a sudden sensitivity to insulin and becomes hypoglycaemic, especially if they are not eating well. The hope is the cat will start to go into diabetic remission over the first week to month post-surgery. The nursing team can counsel the owners of the cat on what to watch for in the event of hypoglycaemia, such as dullness, weakness, or even partial or full seizures. These are some of the things owners probably are not used to looking out for, since they have had an insulin resistant cat for so long. After discharge, weekly to fortnightly rechecks may be required while medication doses are being stabilised or altered. Once on a stable dose of medications, every three months should be adequate for rechecks, to continue monitoring the cat’s electrolyte levels and general wellbeing post hypophysectomy.










