

Get lost, cancer. This is my seat
Unconditionally committed to keeping loved ones in our lives




Get lost, cancer. This is my seat
Unconditionally committed to keeping loved ones in our lives


2023 was a monumental year for VCU, VCU Health, and especially the VCU Massey Comprehensive Cancer Center. This was the year that our cancer center stepped into the national spotlight by becoming the 54th National Cancer Institute-designated Comprehensive Cancer Center, a prestigious status.
As a public research university and academic medical center, VCU is able to bring together advanced research — new and emerging treatments and technologies, and clinical trials — with complex care. Our advanced research and growing research volume are why VCU is ranked among the top 50 public research universities by the National Science Foundation. VCU Massey is an important part of that identity, with a significant portion of VCU’s research enterprise focused on discovering and inventing new treatments for cancer.
Our VCU Massey leadership, our teams and leaders across the enterprise and Commonwealth continue to elevate VCU’s efforts, reminding us of the critical work VCU Massey does for our students, patients and community.
VCU Health’s vision is to lead the nation in quality, affordability and impact as a trusted and preferred academic health system. I am energized by our comprehensive cancer center’s commitment to this vision and remain honored to help share our important work in this report. We are proud of all that our cancer center has accomplished and look forward to the lives improved and saved in the decades to come.
Michael Rao, Ph.D. President, VCU and VCU Health System

“We celebrate Massey’s achievement as a huge win for our entire institution, and one that will help us continue to raise the bar for excellence at VCU Health. The dedication to innovative research and education and to advancing health equity is a clear reflection of our health system’s core values.”
MARLON F. LEVY, M.D.
SENIOR VP, VCU HEALTH SCIENCES CEO, VCU HEALTH SYSTEM
2023-2024 Annual Report masseycancercenter.org
This publication was produced by the VCU Massey Comprehensive Cancer Center.
Editor Vanessa Copeland
Associate editor Grace Hummel
Design director
Terri Curtis
Contributors
Blake Belden, Amanda Kowaleski and Stephanie Mallory
To update your address or request a digital copy, email askmassey@vcu.edu.

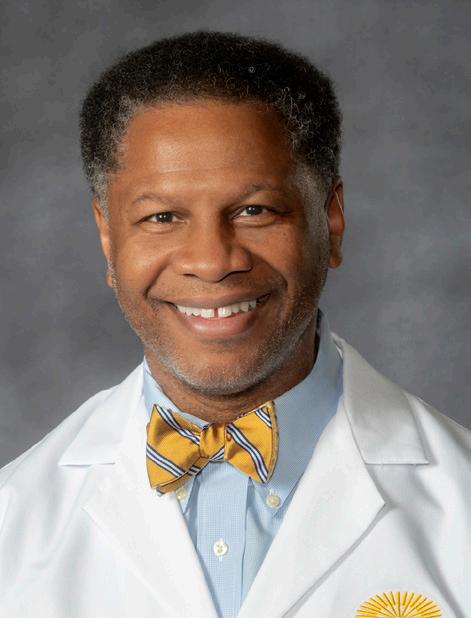
What an incredible year for VCU Massey Comprehensive Cancer Center and our community. When I joined VCU in 2019, I had one goal in mind: to lead the center in achieving designation by the National Cancer Institute (NCI) as a Comprehensive Cancer Center. In 2023, Massey was recognized with this honor from the nation’s principal authority on cancer research and training, placing us among an elite group of cancer centers influencing a new standard of care through research, education and community engagement.
This is a major step forward for our cancer center and our community, which has been an integral part of this accomplishment. This status not only elevates the caliber of research happening within the center, but positions us to optimize care for our patients and the community. At VCU Massey, we are committed to ensuring that best-in-class research and care reach everyone, holding fast to our commitment to reduce the cancer burden for Virginians.
I’m honored to showcase a glimpse of the progress we have made within our first year as a Comprehensive Cancer Center through this report and the impact these efforts are beginning to have on the broader conversation about how to treat and study cancer. We welcomed several thought leaders to visit Massey this year, including Richmond City Council Member Cynthia Newbille and Virginia Lieutenant Governor Winsome Earle-Sears, who have helped advocate for this work in the community.
The center is also being recognized on a national level for our community-centered approach and work to reduce cancer-related health disparities. I am proud to have been chair of the steering committee for the Health Disparities Cancer Progress Report, made up of top researchers from around the country, including Massey’s Katherine Y. Tossas, Ph.D., M.S., and Nolan A. Wages, Ph.D., in partnership with the American Association for Cancer Research, which highlights that, even though major strides have been made in eliminating disparities, they are still prevalent among certain populations. This intersection of social and biological factors, or what I like to call ZNA, can be just as telling as a genetic code and changes how we approach cancer’s most pressing questions.
I’m incredibly proud of our work this year and look forward to continuing our efforts to make cancer research, prevention, treatment and survivorship accessible to everyone.
Robert A. Winn, M.D. Director and Lipman Chair in Oncology, VCU Massey Comprehensive Cancer Center
Senior
Associate Dean
for Cancer Innovation, VCU School of Medicine

It is the most prestigious designation in the field of oncology — and Massey has achieved it. Now, the center is putting in the work as the first in a new generation of cancer centers with the community at its core.
At Massey, one treatment does not fit all. A rise in the number of individuals living with cancer across Virginia has catalyzed the need for new treatment options and more personalized approaches that are designed with the patient in mind.
A driving force in the field of health equity, Massey’s unwavering commitment to advancing health outcomes for all remains at the forefront of its mission. 8 11 15 23

29 35 41 45
Outreach and engagement efforts at the center promote disparities-related research, provide cancer prevention and education, enable access to cancer screening, treatment and clinical trials, and advocate for public policy.
Massey researchers are exploring cross-interactions between biological, environmental and social drivers. From DNA to ZNA, the team is uncovering new levels of influence contributing to cancer risk, incidence and disparities.
Massey experts continue to unlock new answers to cancer’s most pressing questions through clinical research, offering one of the largest selections of clinical trials in Virginia.
A recent expansion of the center’s career pathway programs is shedding light on new career paths for students while curating impactful mentorship opportunities and meaningful engagement with other trainees.
18,733
2,647
$55.8M
Total operating budget and sources

Budget breakdown by source

Budget uses by category
Research conducted across three preeminent research programs at Massey has helped VCU secure a spot among the National Science Foundation’s list of top 50 public research universities, landing at number 47 in 2023.
Select national awards and accolades
Rakesh Kukreja, Ph.D., Ph.D. Carl J. Wiggers Award American Physiological Society
Vanessa Sheppard, Ph.D. Researcher of the Year (2022) American Cancer Society
Sarah Spiegel, Ph.D. Top Female Scientist (2022) Research.com
Arnethea Sutton, Ph.D. Early Investigator Advancement Program National Cancer Institute
Robert A. Winn, M.D. President, Association of American Cancer Institutes Fellow, American Association of Cancer Research







It is the most prestigious designation in the field of oncology — and Massey has achieved it. By being named a Comprehensive Cancer Center by the National Cancer Institute (NCI), Massey has been recognized, in the NCI’s words, “for their leadership and resources, in addition to demonstrating an added depth and breadth of research, as well as substantial transdisciplinary research that bridges these scientific areas.”
At press time, there are 72 NCI-Designated Cancer Centers in the U.S. that are funded by the NCI to advance cancer research, community outreach, and oncology-related education and training. Of these 72 institutions, 58 are Comprehensive Cancer Centers — Massey and the University of Virginia Cancer Center are the only two in Virginia.
“The NCI thoroughly measured our impact on the community through outreach and engagement, while also considering our integration of cancer training and education of biomedical researchers and community health care professionals,” said Robert A. Winn, M.D., Massey director and Lipman Chair in Oncology.
According to Winn, the new comprehensive designation “allows Massey to be the first in a new generation of cancer centers that integrates the community in all of the research we do.”
The scientific field calls this approach “community-to-bench,” which means that the people who are served guide the research. According to Winn, “instead of following traditional models that keep much of the process inside a laboratory, Massey engages individuals in their communities; they are essential partners at every level of our research — design, implementation, evaluation and dissemination. The data we collect from the community helps us to refine scientific questions. We can then take medical innovations back to the community through clinical trials to serve specific needs and have a greater impact on overall health.”
Comprehensive designation offers Massey more research funding from the NCI and greater leverage when applying for other grants. The recognition also enables the center to expand its stellar team, recruiting and retaining top scientists from around the world. By doing so, the scope of Massey’s research can broaden, with new areas of expertise and methodologies to fight cancer. The designation could open more doors to collaboration with other research institutions.
Massey was among the earlier cohorts of cancer centers designated by the NCI in 1975, just four years after the creation of the NCI Cancer Centers Program. With that initial designation, Massey was already among the top 4% of the nation’s 1,500 cancer centers. When Winn started as director at Massey in December 2019, he asked, “But why stop there?” He then made achieving comprehensive status a top priority.
While the Comprehensive Cancer Center designation marks a milestone, new achievements will continue every day as Massey works toward a world without cancer. Personalized medicine is one area that is changing oncology as we know it.
“At Massey, one treatment does not fit all,” Winn said. “As our researchers continue to make advances in immunotherapy, more patients will benefit from this and other types of personalized medicine.”
As a community-to-bench center, Massey will continue to recognize the importance of location. Winn noted that “lowering cancer incidence and mortality requires not only looking at DNA but also ZNA, which is an individual’s ZIP code and neighborhood of association. Prevention programs will focus on the intersection of place and space with cancer.”
Learn more at page 35.
That approach is already proven in a new outreach effort that launched in the fall of 2023. Two “Massey on the Move” mobile health vans are now delivering cancer education and awareness to communities across central and southern Virginia. The vans also serve as an entry point for connecting with health education programs like We Can Quit and We Can Eat Well, and for accessing screening tests, diagnostic follow-up tests, cancer treatment services and state-of-the-art clinical trials.
The designation will help position Massey for even greater impact across the Commonwealth and beyond.
“We are so proud to reach this milestone — and to be leading the charge, not just in research, but in building trust and breaking down barriers between medical institutions and communities,” Winn said.
To position Massey for NCI comprehensive designation, the center embarked on a two-year fundraising campaign to generate an additional $22 million in funding. Named “Quest for Comprehensive,” the fundraising initiative focused on recruiting and retaining acclaimed scientists; increasing research and clinical trials; expanding Massey’s Molecules to Medicine program; expediting cutting-edge treatments; combating cancer health disparities; and improving cancer prevention, detection, treatment and survivorship for everyone. Thanks to that additional funding and the efforts of all stakeholders, comprehensive designation was reached in May 2023.
“Philanthropy is a critical component in building a stronger infrastructure, providing resources for our brilliant researchers, giving our community members access to lifesaving clinical trials and ultimately saving more lives,” said Becky Massey, a longtime donor and volunteer leader at the center, which bears her family name in honor of a major gift bestowed in 1983.

In addition to supporting endowed professorships and chairs, the generosity of an active network of donors, corporate partners and grateful patients have propelled Massey’s growth and status as an NCI-designated Comprehensive Cancer Center by helping to build an infrastructure that supports faculty at all stages of their career.
It was a record-setting year for giving at Massey with $88 million raised in FY23. This included a prestigious $70.2 million transformational gift from the Bristol Myers Squibb Foundation to improve participation in clinical trials, driving better health outcomes with the creation of the Robert A. Winn Excellence in Clinical Trials Award Program.
With comprehensive status now achieved, Team Massey looks ahead to the future of the cancer fight and Massey’s role in improving care and outcomes for all people. “NCI designation doesn’t mean our work is done,” Becky Massey added. “It just means we’re going to start working even harder.”
Learn more at vcumassey.org/support




As part of a safety-net hospital, Massey remains committed to providing the latest cancer treatments and care to every patient that comes through the doors. But outside the walls of the medical center, patients face a multitude of other challenges — ones that don’t always show up on a medical exam.

The Healing Space is an innovative take on how mindfulness meets medicine. Opened in late 2023, the area located within the VCU Health Adult Outpatient Pavilion is a place for patients to find peace amidst the stress of cancer treatment. The space includes floor-to-ceiling, state-of-the-art video screens and was envisioned by Massey Advisory Board members and volunteer leaders Terrell Harrigan, Becky Massey and Shelly Arthur. Harrigan, along with her husband Elliott, donated funds to bring the idea to life, creating an immersive design that lends itself to mindfulness-based interventions — some of which have been shown to help with anxiety and depressive symptoms during a patient’s cancer journey.
The room is designed for patients, as well as caregivers, staff and even Massey investigators. Massey hopes the space will be used for future research efforts, offering clinicianscientists and researchers a different perspective on the needs, values and experiences individuals face when dealing with a cancer diagnosis — and how to better address those needs moving forward.
Scan the QR code to explore the Healing Space
The Children’s Tower at Children’s Hospital of Richmond (CHoR) at VCU brings innovative care to young patients in a kid-friendly environment. While it primarily serves as a location for medical treatments, the tower is filled with cheerful, calming touches that improve the patient experience. Colorful furniture, murals lining the walls, animal mascots and special family amenities add up to create a place of peace and optimism for patients and their loved ones.
The $420 million tower officially opened in April 2023. This milestone also marked the first time that inpatient and outpatient pediatric cancer care will be housed in the same city block, including a dedicated pediatric cellular immunotherapies unit.
“The conversations around a fully kid-focused children’s hospital have been taking place for many years,” CHoR president Elias Neujahr said. “With the opening of the Children’s Tower, we are able to mark the completion of a longstanding vision, one built just for kids. It truly is unlike any other.”
In the Children’s Tower’s first few months, CHoR saw double-digit growth in acute care admissions, imaging studies, emergency visits and surgeries.

Cellular Immunotherapies and Transplant (CIT) services at Massey include cutting-edge biological therapies that help harness a patient’s immune system to fight cancer. It is only in the last decade that physician-scientists have been able to utilize immunotherapy more broadly, harnessing a patient’s immune system to boost immunologic response.
The CIT program’s outpatient clinic was relocated to a new space within VCU Health’s North Hospital in 2023 to accommodate its growing portfolio of clinical trials and expanding capabilities. This new space promotes multidisciplinary collaboration, enabling better-coordinated and more convenient care, while offering more support for the high-quality research being conducted on site.
Massey was the first in Virginia certified to offer CAR-T therapy and in 2023 provided over 55 treatments using engineered T-cells from patients. All six FDA-approved CAR-T therapies currently on the market are available to patients at the center.

“Immunotherapy is an important tool in
approach to
cancer
care,”
our multi-modal
said John McCarty, M.D., director of the CIT program and a member of Massey’s Developmental Therapeutics research program. “Beyond CAR-T and BiTE therapy, Massey also offers gene therapy.”

Studies show that integrative approaches to cancer care that consider the whole patient can help ease treatment side effects and support overall well-being for cancer patients. A major pillar of overall well-being is a balanced diet, which includes vitamin-rich fruits and vegetables. But a 2023 survey assessing food insecurity conducted by the center found that more than a third of Massey’s patients do not have sufficient access to these critical foods. To help bridge this gap, Massey hosts a farm stand on campus in partnership with local nonprofit Shalom Farms to offer fresh fruits and vegetables to patients.
To further help cancer patients, Massey applied for and was awarded a large McKesson Foundation grant, which subsequently launched the In Cancer Care, Food is Medicine program. This initiative is the first of its kind in Virginia to systematically screen cancer patients for food insecurity and connect those in need with on-site, long-term resources.
Food insecurity has also been linked to obesity, which studies show can contribute to cancer risk and increased health disparity. Cities with some of the highest obesity rates in the state, such as Petersburg, Virginia, are within
the center’s catchment area. Jessica LaRose, Ph.D., and Maghboeba Mosavel, Ph.D., of Massey’s Cancer Prevention and Control research program, began using grassroots wellness coaching for Petersburg residents to evaluate the effectiveness of community-led weight management strategies. Funded by the National Institutes of Diabetes and Digestive and Kidney Diseases, the behavioral model includes training family members, friends, and those close to at-risk patients to share opportunities for lifestyle changes to help patients lose weight and improve heart health.
Building on its long-standing commitment of promoting healthy eating because of its role in preventing cancer, Massey is taking action to support more equitable food access for patients by expanding evidence-based research on the association between cancer and diet. The center is working with local and national partners, including Shalom Farms and the McKesson Foundation, to elevate patient education and support services for food insecure patients.

Scan the QR code to learn more about the Food is Medicine initiative











With nearly 450,000 cancer survivors in Virginia, new challenges are coming to light as the number of people living beyond their cancer diagnosis continues to rise. Regardless of where they are in their cancer journey, Massey’s team of clinicians and scientists are dedicated to treating the whole patient.
Insomnia is common among patients with brain cancer and significantly higher among service members, affecting nearly half of all veterans. Clinical psychologists in Massey’s Cancer Prevention and Control research program are evaluating new ways to treat insomnia in these patients. Ashlee Loughan, Ph.D., LCP, and Autumn Lanoye, Ph.D., LCP, are building on a first-of-its-kind trial conducted by Loughan’s team that uncovered promising results from Cognitive Behavioral Therapy for Insomnia, or CBT-I, in brain cancer patients. The drug-free treatment incorporates educational, behavioral and cognitive interventions to treat sleep disturbance.
The pair will expand on this work with funding awarded in 2023 from the U.S. Department of Defense, investigating the immediate benefits of CBT-I and how these benefits are maintained over time through a telehealth-based therapeutic program.
Another common side effect of cancer treatment is chemotherapy-induced peripheral neuropathy (CIPN). CIPN can cause temperature-based pain, nerve damage or numbness — often in the hands or feet. A clinical trial led by Developmental Therapeutics research program member Renato Martins, M.D., M.P.H., who serves as Chair of the Division of Hematology, Oncology & Palliative Care at VCU, and holds the Martha Anne Hatcher Distinguished Professorship in Oncology, launched early in 2023 to assess the benefits of medically-based at-home therapies based on a proposed treatment algorithm for CIPN compared to traditional treatment methods.

Massey also understands some cancer patients endure unintended, long-term negative effects of treatment. All patients with cancer who experience pain, either due to the cancer itself or as a result of the cancer treatments, deserve to have their pain adequately managed.
However, a portion of disease-free cancer survivors find themselves taking opioids to manage pain which may have resulted from cancer treatment. In some cases this can lead to opioid addiction. To help this, VCU received funding from the Virginia Opioid Abatement Authority to help educate patients and providers on the long-term harm associated with opioid use. As part of this initiative, Massey has developed a multidisciplinary clinic to help disease-free, long-term cancer survivors reduce, and when possible, stop the chronic use of opioids.
Nearly 50 cancer survivors, caregivers and advocates convened for a patient advocacy workshop in June 2023 co-hosted by Massey and the National Patient Advocate Foundation.
The event fostered dialogue between patients and providers about ways to improve access to equitable, high-quality care through innovative approaches. Mary Helen Hackney, M.D., medical director of community oncology at Massey, shared insight from the provider perspective, highlighting the importance of empowering patients and patient advocates to ask for additional resources that may help ease the burden of cancer.
“Ask your doctor, ask your nurse navigator, ask your social worker and if something changes, ask again,” Hackney said.
The group explored the challenges and tribulations cancer patients and caregivers often face, including prevalent social drivers of health such as a lack of reliable transportation, financial insecurity and mental health problems.
At Massey, survivorship services are a crucial aspect of a patient’s overall care plan and are prioritized from the beginning of treatment. Attendees expressed the benefit of support programs like chaplain services, cardio-oncology and genetic-testing, and how they can boost overall wellness during and after treatment.

In 2023 Massey launched the CancerIQ survey which evaluates the eligibility of patients for genetic testing. The center has since screened over 2,000 patients to identify those eligible for genetic testing. The survey not only helps inform who should consider testing and triages patients by risk, but also improves access to genetic testing at large by increasing care team capacities and compliance.
Clinical leaders at Massey offer insight into the newly rolled-out Cancer Service Line (CSL) and how the change will help better serve patients across the Commonwealth.

Kandace McGuire, M.D., FACS
Senior Medical Director, Cancer Service Line and Interim SVP, Cancer Service Line
Q. Providing high-quality, accessible care to patients from all backgrounds is a top priority for Massey. How will the CSL affect the quality of cancer care?
A. The CSL brings together multiple disciplines including hematologists, medical and radiation oncologists, cancer surgeons, nurses and other support staff to provide patientcentered, team-based cancer care. This approach allows us to leverage the latest scientific advances and offer the treatments of tomorrow through clinical trials. It also allows us to be nimble and responsive while meeting our patients where they are, when they need it most — whether that is at Massey or in the community.

Paymon Bagheri, FACHE, FACMPE, CECM, CHFM, CPPS, CPHQ, CSM
Senior Operations Director, Cancer Service Line
Q. Health care is complex, particularly within a matrix-based cancer center like Massey. What strategies are being implemented to enhance care delivery?
A. Within the CSL, there are several key actions we are taking to enhance care delivery. We are focused on achieving clinical integration across the entire VCU Health System to optimize efficiency so we can serve and support more patients. In addition, we continue to harness emerging technologies and data tools that enable us to provide better care. These strategies will have a domino effect enhancing physician and staff engagement and providing evidence-based patient care with better outcomes.
Kim Keller, RN, MSN, OCN
Senior Clinical Research & Quality Assurance Director, Cancer Service Line
Q. As part of an academic medical center, Massey’s mission is rooted in research. How are clinical teams working in tandem with physician-researchers to deliver the latest cancer advancements?
A. We are in the process of becoming American Society of Clinical Oncology (ASCO) Certified, a quality initiative which
ensures the development of a collaborative, multidisciplinary treatment plan for every patient. Because innovative care remains the foundational pillar of our patient care delivery strategy, our care teams believe a clinical trial should be considered as a first option for treatment at every stage of a patient’s cancer journey.
Learn more about ASCO Certified: Patient-Centered Cancer Care Standards
Jessica Gray, MS, RN, BMTCN
Senior Nursing Director, Cancer Service Line
Q. Nursing is an essential patient touchpoint and often a driving factor of patient satisfaction. How is the CSL ensuring nursing excellence?
A. Our commitment to nursing excellence begins with a comprehensive orientation and oncology-focused training for each of our oncology nurses and continues throughout their careers. When patients receive care in the hospital or at any of our outpatient settings, our care teams remain in constant communication to ensure a seamless experience for them. Patients are also screened for personal and social factors which could impact their journey and are connected to navigation and other supportive services to help make their journey a bit easier.

Paula Fracasso,
M.D., Ph.D., FACP Senior Advisor, Cancer Service Line
Q. Massey is now an NCI-designated Comprehensive Cancer Center. How is the CSL helping to elevate Massey’s research priorities and community approach through a patient-centered care model?
A. Incorporating CSLs into NCI-designated comprehensive cancer centers aligns with the NCI’s expectations of fostering innovation and excellence in both research and care delivery for all patients with cancer. While the organizational structures may differ from one cancer center to the next, the goal remains the same: to collaboratively align value-based, patient-centered care in our communities with cancer research at Massey.


Massey is driving more equitable patient outcomes through the work of its researchers, physicians and staff. By improving care delivery and leveraging data sciences, the center’s local impact is resonating nationwide, paving the way for broader health advancement for all.
A pilot project from the National Comprehensive Cancer Network® (NCCN®) is moving cancer care providers to the top of the class. This project is based on work from the Elevating Cancer Equity initiative, a joint program from NCCN®, the American Cancer Society Cancer Action Network, and the National Minority Quality Forum and co-created by Massey director, Robert A. Winn, M.D. The Elevating Cancer Equity working group’s Health Equity Report Card was developed to offer actionable recommendations to reduce racial disparities in access to cancer care.
This tool is now being piloted at five leading academic cancer centers to assess the feasibility of implementing the Health Equity Report Card, focusing on its ability to measure and report on equitable care practices across four main areas: community engagement, accessibility of care and social drivers of health, addressing bias in care delivery, and quality and comprehensiveness of care.
“Your ZIP code and the neighborhood where you live impact many aspects of health, including cancer onset and outcome; beyond that, we know there is also implicit and explicit bias in care delivery,” Winn said.
The Health Equity Report Card is also being adapted to meet the needs of community-based organizations as part of the Alliance for Equity in Cancer Care. The multi-site initiative is funded by the Merck Foundation and led by Massey in partnership with the VCU Center on Health Advancement, who collectively serve as the Alliance National Program Office.

Catchment area data is a critical resource and helps inform nearly every aspect of cancer center operations. However, harnessing that data and analyzing its impact remains a challenge. By its very definition, data is the collection of facts and statistics used for reference. This information not only guides patient care decisions, but also cancer disparities research and outreach activities for at-risk communities. So, how can this information be better utilized to collectively improve data access and health outcomes? Enter Massey.
In late 2023, the center hosted the first-ever Catchment Area Data Conference – Beyond Definition, in Richmond, VA. The event brought together nearly 300 scientific minds from across the nation to discuss best practices in cancer health data collection, dissemination and utilization while exploring policies and methodologies to advance cancer center catchment area analytics. With representation from more than 50 NCI-designated centers, the transformative event was the first to bridge oncology data sciences, technology-based health solutions and innovative community engagement strategies to help streamline the use of and access to catchment area data.

The event boasted keynote presentations from national leaders, data-driven software workshops, and a poster session showcasing the latest advancements in cancer research and data analytics. As a result, more than a dozen research articles were published in the Journal of Preventive Oncology and Epidemiology, including a comprehensive editorial by Massey director Robert A. Winn, M.D., and Katherine Y. Tossas, Ph.D., M.S., director of catchment area data analytics at Massey, assistant professor of social and behavioral sciences and Harrison Endowed Scholar at the VCU School of Public Health.
Experience the News Center recap at vcumassey.org/cadanews

Cancer remains a critical global health challenge as the second leading cause of death worldwide. In 2023, Massey established the Global Oncology Program Office to help reduce global cancer disparities through leading-edge research collaborations across the cancer continuum, workforce development and sustainable international partnerships that foster community outreach and engagement.
Under the joint leadership of Khalid Matin, M.D., and Katherine Tossas, Ph.D., M.S., the office aims to extend Massey’s impact beyond its catchment area by fostering bilateral partnerships with countries dedicated to addressing cancer health disparities through innovative and disruptive solutions. Serving as a hub for global collaboration, the program facilitates partnerships with institutions and communities worldwide, leveraging Massey’s unique community-to-bench approach to tackle the complex challenges of cancer across different populations.
With a focus on mutual learning and innovation, the program aligns Massey’s expertise with global efforts, initially targeting collaborations in Cuba and Africa, where unique cancer prevention strategies like vaccines have been pioneered. By integrating local innovations with Massey’s resources and research, the Global Oncology Program seeks to advance cancer prevention, diagnosis and treatment while addressing shared burdens such as lung, breast and colorectal cancers.
This initiative underscores Massey’s commitment to reducing the global burden of cancer by creating more effective strategies that transcend geographic boundaries and elevate the impact of cancer research worldwide. Through these global partnerships, Massey is poised to lead transformative change and set new standards for global oncology collaboration.

In his role as director of the Alliance for Equity in Cancer Care initiative, Winn offers insight into a recent shift in terminology around social determinants — or drivers — of health.
Q. You’ve helped introduce new terminology for social determinants of health to social drivers of health. Why the change?
A. These terms are often used interchangeably, but by the very nature of the word, social determinants of health are predetermined or fixed. Social drivers are similar in that they affect health outcomes; however these influences aren’t treated as finite. It’s why we do what we do. Every day, we are working to move the needle towards ensuring a more accessible health care system for everyone.
Q. These factors are crucial in understanding and evaluating health disparities. What steps can be taken to bring more awareness to these contributors?
A. There is an important intersection between place and space, one that is largely misunderstood in health care. Collaboration with traditional “non-health” sectors such as transportation, education and housing is a way to bring more awareness to issues — including housing insecurity and food deserts — and how these factors relate to one’s ability to not just access but also to receive quality, patientcentered care. Initiatives like the Alliance are a great example of evaluating barriers to care from multiple perspectives. Only then can you effectively evaluate where there are gaps and identify solutions to begin closing them.
Q. How can health care professionals and patient navigators incorporate this language into practice to better address social drivers of health?
A. The adoption of new terminology is a critical part of ensuring health literacy for our patients and is just as important as implementing new technological approaches or practice guidelines. We must empower our communities and patients to advocate for themselves and be confident and engaged in their treatment; patients should feel like they are in the driver’s seat.
Learn more about the Alliance at equityincancercare.org




Massey’s community activities and outreach efforts are designed to help reduce the cancer burden. But, to serve the community, we must actively learn from it, which sometimes means going outside our comfort zone. On wheels or online, Massey is showing up when it matters most.

From Petersburg to South Hill and beyond, Massey’s Community Outreach & Engagement team is the center’s boots on the ground delivering cancer education, prevention and screening, and care coordination to communities across central and southern Virginia.
A pair of mobile health vans were added to the team in 2023, to help educate individuals on lifestyle behaviors and riskreducing activities like smoking cessation, healthy eating as well as programming to promote cancer prevention and early detection. Serving as an entry point for the community, the vans have already covered over 8,000 miles, connecting Massey with more than 1,500 Virginians.
Massey also believes in empowering individuals to take control of their health. Two new programs, We Can Take Action and We Can Eat Well, were introduced in 2023 and built on the success of Massey’s smoking cessation program, We Can Quit. The programs combine personalized coaching and group-based
sessions to help participants reduce their cancer risk. From goal setting to grocery store tours, the two programs reached 450 community members.
Community Outreach & Engagement also supports patient navigation. Navigation helps guide patients through the entire cancer journey, including screening, diagnostic testing, treatment, clinical trials and survivorship. These services also assist patients in overcoming barriers to care, including social drivers of health. As Massey’s footprint expands statewide, the center is working to ensure patients screened in the community have access to appropriate follow-up care. To date, Massey has helped nearly 150 patients navigate the complexities of cancer care and challenges resulting from social drivers of health.
The vans also have another tie to the community: Richmond artists Sir James Thornhill and Hamilton Glass, who created the artwork featured on the vans to reflect Massey’s involvement and commitment to the community.
In partnership with the Petersburg Public Library, Massey opened the Petersburg Resource Center, which provides cancer education and cancer prevention for residents in the Tri-Cities area.
Massey’s first navigation to breast cancer screening event was held in partnership with Central Virginia Health Services (Charles City), the Chickahominy Tribal Center and Sentara Health. A second event was held in October, 2023.
July 2023
Allies in Health for Underserved Groups was launched by Massey, bringing together aligned serviceoriented partners, resource providers, FQHCs, free clinics and nonprofits operating in the Colonial Heights, Hopewell and Petersburg areas.
September 2023
Two mobile vans funded through The Dominion Energy Charitable Foundation are launched into the community to offer cancer education and prevention services to at-risk communities. Educational materials were supported by Bank of America.
November 2023
As part of a larger social media effort, Massey launched a Facebook campaign in six target localities to inform and educate residents on colorectal cancer and screening options. The campaign was viewed by nearly 200,000 individuals.
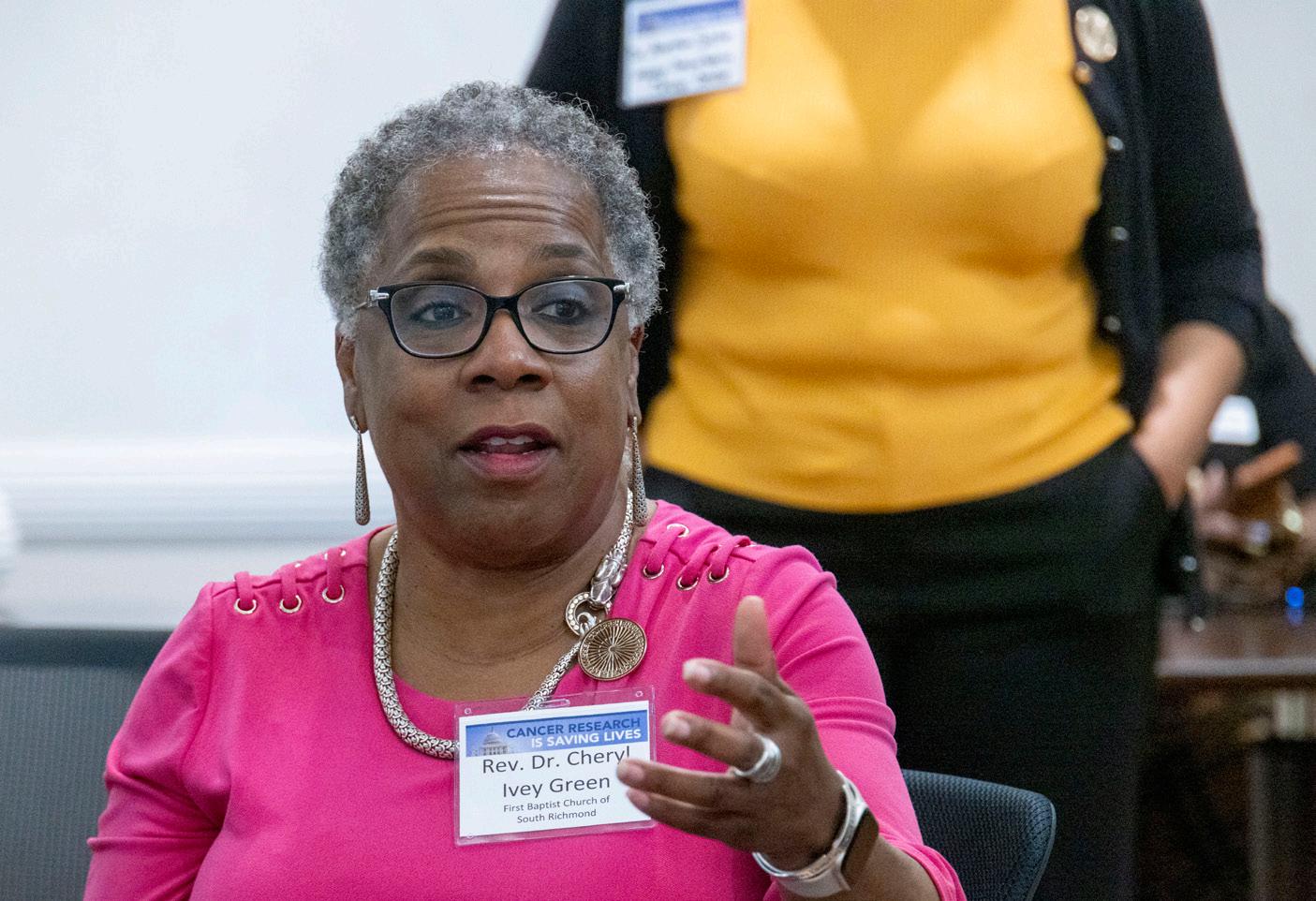
Since 2020, Facts & Faith Fridays has served as a critical touchpoint between Massey and the faith-based community. Massey welcomes leading health care and topical experts to join the conversation each month. The virtual discussion gives the public first-hand insight into various topics from the Cancer Moonshot and clinical trials to community health.
Notable experts like Francis Collins, M.D., Ph.D., the former director of the National Institutes of Health and then-scientific advisor to the president, joined a Facts & Faith Fridays session to speak on national initiatives like the Cancer Moonshot and efforts to move this goal forward. Topics included multi-cancer early detection tests, a focus on building back cancer screenings that took a hit during the COVID-19 pandemic and more engagement of community members in scientific research.
Former Richmond Mayor Levar Stoney also joined the ranks of Facts & Faith Fridays guests in 2023. Stoney spoke on lessons learned from the COVID-19 pandemic, as well as a resiliency developed by the city’s workforce and operations as a result. Understanding the correlation between one’s physical environment and health outcomes, he also emphasized the need for more affordable housing to support the pace of the city’s growth.
In August 2023, Facts & Faith Fridays leaders partnered with First Baptist Church of South Richmond to physically offer clinical trials education by way of Massey’s mobile vans. The event not only informed the public about the benefits of clinical trials, but gave attendees an opportunity to participate in a cancer screening trial involving a simple blood test. For example, in just 45 minutes, Rev. Cheryl Ivey Green, D. Min., was able to participate in a clinical trial that could change the way cancer is diagnosed and treated for generations to come.
Regardless of the topic, Massey remains a safe space for open dialogue as a means to enhancing the lives of people in our communities.
It’s no surprise that Massey is at the top of its game when it comes to community collaboration. Built around the center’s community-to-bench model, the voice of our patients and constituents echoes throughout everything Massey does. From research priorities to statewide collaborations, Massey practices what we preach.

When Massey heard tribal citizens in Charles City County suspected a cancer hot spot among the Chickahominy Tribe, the cancer center stepped in. The Chickahominy TRUTH (Trust, Research, Understand, Teach, Heal) Project aims to better understand structural and individual-level contributors to cancer risk. In partnership with Chickahominy Tribal Leadership, Massey conducted household interviews, water testing and a community survey to gain insight into the perceived cancer risks of Charles City County residents. Under the leadership of Katherine Tossas, Ph.D., M.S., and Maria Thomson, Ph.D., the team completed nearly 700 surveys, with 66% of respondents impacted by cancer. The survey highlighted significant perceptions of health and environmental influences, including social drivers of health such as food insecurity (19%), pollution exposure (71%) and health care mistrust (47%), emphasizing the complex factors impacting cancer prevention and screening behaviors.

The Virginia’s Firefighter Cancer Support Network (FCSN) and the Richmond Professional Firefighter Association reached out to Massey to help mitigate cancer risk among Virginia’s 500+ registered fire departments. Known carcinogens, which can cling to personal protective equipment, expose firefighters to an increased risk, as the chemicals can cause cellular changes that can lead to cancer. In response, Massey researchers are developing a cancer registry that will offer insight into the health needs of firefighters and inform better strategies for providing education and prevention resources to those in the fire service. These efforts are being led by Bernard Fuemmeler, Ph.D., M.P.H., associate director for population science and Gordon D. Ginder, M.D., Chair in Cancer Research, along with Cancer Prevention and Control research members Jim Burch, Ph.D., and Chrisa Arcan, Ph.D. The FCSN also received Massey’s Seed to Harvest community grant in 2023.



Cancer Champs or Champions, Massey’s group of community research advocates, is another vital connection to the community. Champions are trained to foster dialogue between Massey investigators and the community to help identify research priorities and community needs. In partnership with Capital Area Health Education Center, Project Nana and Virginia Community Health Worker Association, Massey provided tailored cancer research training to over 100 community members, 33% of whom are cancer survivors. The specialized training in cancer research, self-efficacy and health literacy skills equips trainees with resources to educate other individuals and organizations and prepares them to be integral members of research teams.
At the state level, Massey convened health district directors and leaders from the Virginia Department of Health across all 35 health districts for an inaugural cancer summit in 2023. The first-ofits-kind summit emphasized the importance of collaboration not just at the community level but the state level. During a legislative panel featuring Del. Delores McQuinn, Rep. Jennifer McClellan and Rep. Rob Wittman, attendees were urged to advocate for the health of their districts, noting that cancer is an issue that touches every person in Virginia and deserves the attention given during the summit.
According to the American Cancer Society, the LGBQTIA+ community may be at an increased risk for getting cancer. Nearly 50 years ago, Massey’s founding director Walter Lawrence Jr., M.D., helped establish the center’s vision of ensuring optimal health outcomes for all. Massey continues to uphold this commitment today — inside and outside the cancer center walls — by strengthening partnerships with the LGBQTIA+ community.
Massey introduced a new LGBTQIA+ focused employee resource group in 2023: Massey Pride. The collaborative was largely driven by the center’s work within the queer community and is led by staff from various units and departments across the center. Massey was also a first-time sponsor of the 2023 PrideFest celebration, the largest LGBTQIA+ event in the Commonwealth. With attendance in the tens of thousands, Massey used its increased profile to hold hundreds of one-on-one conversations with community members related to prevention and disparities, in addition to facilitating connections to services like We CAN Quit, Massey’s tobacco cessation program, and navigation to screening.
Us Giving Richmond Connections (UGRC), Inc., a 2023 recipient of Massey’s Seed to Harvest community grant, led a “Let’s Talk About Cancer” series, which reached over 100 community members with support from the center. Based on requests from the organization, Massey navigators coordinated with health system partners to facilitate breast screening for a dozen individuals at UGRC’s annual “Day of Purpose” in July of 2023.


As scientists uncover more details about social and biological factors and their influence on cancer disparities, Massey researchers are investigating the full landscape of biosocial determinants of cancer to improve health outcomes for all.
Social drivers of health include factors such as income, education and environment, as well as a person’s ZNA, or ZIP code and neighborhood of association. Biological determinants of health are individual characteristics that are inherited or linked to genes, such as ancestry or physical activity and personal health conditions. Understanding how social and biological factors cooperate to drive cancer can help researchers develop better strategies to reduce disparities.

Increasing evidence shows that neighborhood disadvantage — a lack of adequate economic and community resources within a geographic area — and negative environmental exposures are directly associated with higher rates of cancer and worse outcomes. Contributing factors can include pollution, access to food, home property value, crime rates, poverty level and stress. Robert A. Winn, M.D., and colleagues continue to champion the need for scientists to better understand how neighborhood factors influence the biological stress response as a means to inform specific needs of different communities to improve cancer outcomes and reduce disparities.
While previous research has identified links between cancer incidence and environmental exposures around the time of diagnosis, cancer risk in different populations has not been investigated through a long-term assessment of combined exposures over time. To address this gap, David Wheeler, Ph.D., was awarded a $1.7 million grant from the National Cancer Institute (NCI) to examine neighborhood exposures over decades using statistical models and analysis. This work could inform evidence-based policies to restructure neighborhoods to limit factors that lead to disparities in breast, colorectal and lung cancers. These efforts are now being led by Robert Perera, Ph.D.
Certain populations experience higher exposure to environmental pollutants. Black people in the U.S. develop liver cancer at nearly double the rate of white people, in part due to liver damage caused by pollution. Richard Sterling, M.D., is a collaborator on an NCI grant-funded initiative to study the genetic and environmental factors that influence this imbalance in cancer rates. This is part of an effort to implement effective cancer prevention and intervention strategies, including the utilization of an assessment score that can alert patients and providers to risk for liver disease.

In honor of our cherished colleague David Charles Wheeler, who fought bravely throughout his battle with brain cancer, Massey recognizes Dr. Wheeler’s contributions to the cancer center and VCU at large. His work serves as a profound reminder of our mission to eradicate cancer, and we do so in recognition of his legacy.

While there are a number of social and environmental factors that contribute to cancer disparities, there are also a variety of biological and genetic factors that lead to disproportionate cancer rates in different populations. Scientists at Massey are persistent in their pursuit to understand the biological and genetic variations that are individual to different tumors in an attempt to develop more effective prevention and treatment strategies.
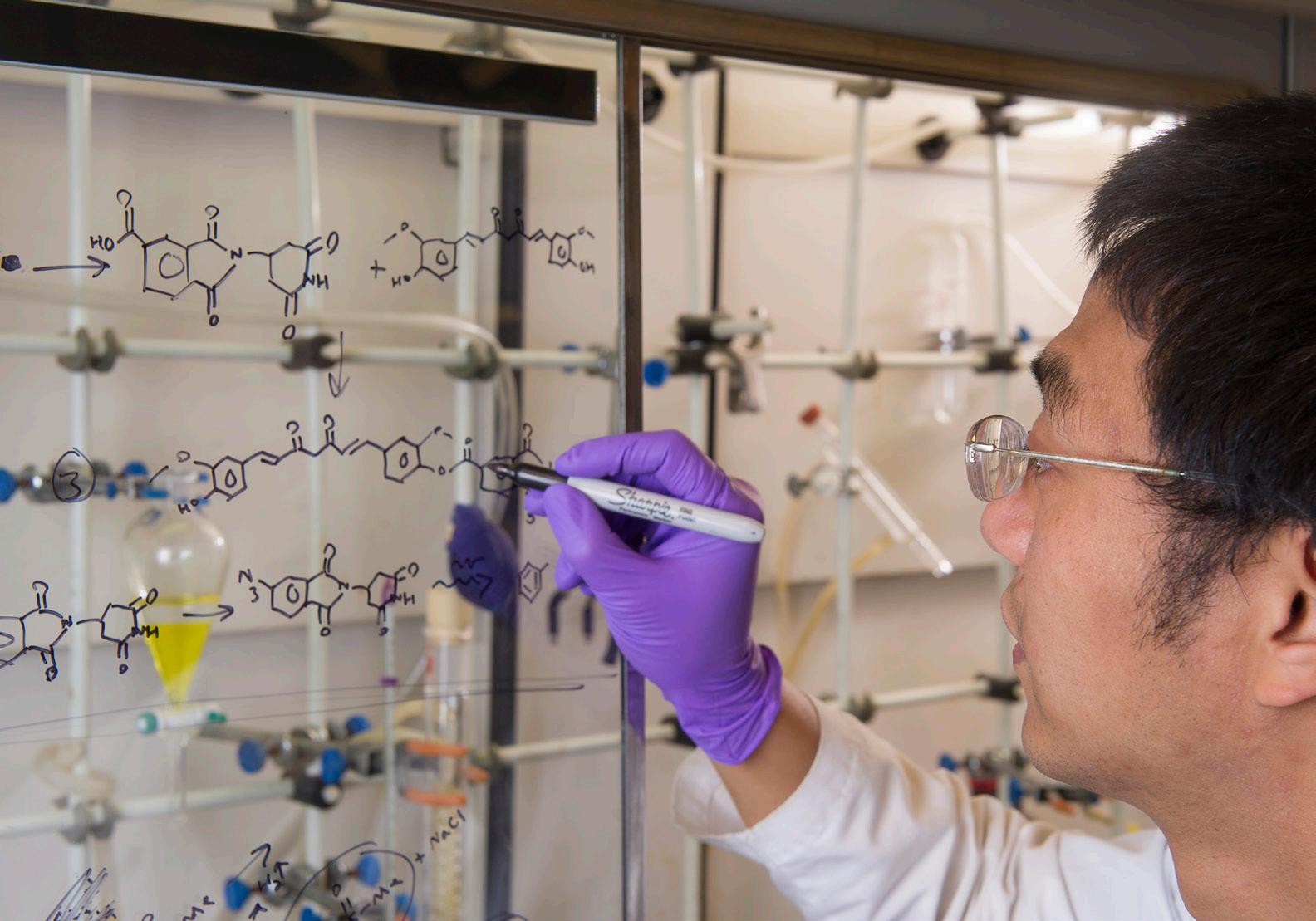
Biomarkers offer a way to examine how a person’s particular genes and proteins influence cancer development, and they are increasingly informing advances in personalized care. Some cancer treatments, including targeted therapies and immunotherapies, may only be effective for patients with specific biomarkers.
Micro-RNAs (miRNAs) are promising biomarkers for cancer staging, diagnosis, outcomes and treatments.
Soma Dhakal, Ph.D., holds grant funding from the NCI to develop a single-molecule detection platform, as well as a microfluidic chip, to enable a fast analysis of miRNAs within multiple breast cancer samples in under one hour. This research could inform entirely new approaches to clinical cancer assessment, diagnosis and personalized treatment.

and processed foods alter biology in populations at high risk of certain cancers, such as Black men and prostate cancer. The study, which is being conducted in collaboration with Victoria Findlay, Ph.D., could lead to the implementation of new strategies to limit the accumulation of cancer-causing metabolites in at-risk populations.
Growing evidence also points to the effects of diet on biological changes that lead to the growth of tumors in different populations. David Turner, Ph.D., holds more than $2 million in grant funding from the NCI to analyze how metabolized sugar, fat
Genetic differences by race are known to amplify cancer inequities. For example, Black women have different vaginal microbiomes than their white counterparts, and they are disproportionately affected by lesions that will likely evolve into cervical cancer. Katherine Y. Tossas, Ph.D., M.S., leads an initiative, funded by The V Foundation for Cancer Research, to determine if racially distinct genetic pathways contribute to precancerous lesions, and if the vaginal microbiome could be a target for improved cervical cancer screenings. This project will uncover information that can inform the creation of targeted interventions to improve the health outcomes for all women.
Research also indicates that gender differences affect cancer progression and the immune response. Joseph Landry, Ph.D., led an NCI-funded effort to identify immune differences between males and females that impact lung cancer growth and their ability to respond to treatment options. They determined that a specific genetic pathway plays an important role in regulating the immune response and could help inform the development of future lung cancer therapies.

Resources that accurately reflect the patient population — including cancer models from varging individuals — is an essential tool for understanding, and ultimately combatting, cancer disparities. Massey researchers have launched the United for Health Equity - Living PDX Program to create new patient-derived xenograft (PDX) models of cancer, with a focus on underrepresented populations with breast and pancreatic cancers to more accurately represent the patient population in Massey’s catchment area.
The NCI-funded U54 was awarded to Chuck Harrell, Ph.D., and Jose Trevino, M.D., who serves as Chair of the Division of Surgical Oncology and previously held the Walter Lawrence Jr. Distinguished Professorship in Oncology. Alongside collaborators Jennifer Koblinski, Ph.D., Jinze Liu, Ph.D., and Mikhail Dozmorov, Ph.D., the pair are co-leading the development and implementation of the program. Successfully generated PDXs will undergo intensive scientific analysis to better understand how ancestry contributes to genetics and affects response to targeted cancer therapeutics. The team-based project will also generate preliminary data to support future clinical trials at Massey.
Massey’s 2021-2025 Strategic Plan set the course for cancer research with a focus on four priority cancer types: breast, lung, colorectal and prostate cancers.
Breast cancer
Despite declining breast cancer deaths in the U.S., Black women have a 41% higher death rate than white women. Victoria Findlay, Ph.D., and David Turner, Ph.D., led a study in collaboration with the Medical University of South Carolina, identifying that the reduction of the protein Cav1 — a novel biomarker for poor outcomes in breast cancer — could serve as a potential driver of breast cancer disparities. The study was published in Frontiers in Immunology and points to a specific cellular mechanism that is associated with the loss of Cav1 and aggressive disease growth in breast tumor cells.
Cancer Biology research program member Jiong
Li, Ph.D., was among a team of scientists who published work in Nature Communications revealing a new strategy for overcoming drug resistance in lung cancer. Findings indicate that a specific protein, LRPPRC, binds to RNA and controls the cellular response to standard treatment options for lung cancer, and the researchers suggest that a new combination strategy could be an effective solution for overcoming resistance to current treatments.
Basic research scientist Can Senkal, Ph.D., and his collaborators discovered a previously unknown interaction between proteins that control energy production in colon cancer tumors. The study was published in Cell Reports and highlights the novel Hsp27 and CerS1 interaction that could be targeted by small molecules to eliminate cancer cells.
Research from Paul B. Fisher, M.Ph., Ph.D., and Swadesh K. Das, Ph.D., determined that a particular gene — MDA-9/Syntenin-1/SDCBP — is the ringleader behind a molecular domino effect driving prostate cancer growth and metastasis. Published in the Proceedings of the National Academy of Sciences, the study examined the role of the MDA-9 gene in prostate cancer and how this gene communicates with surrounding cells and tissue in the tumor microenvironment. Future research is ongoing to investigate novel MDA-9 small molecule inhibitors as potential combination therapies for early stage and advanced prostate bone cancer using clinical tumor samples and animal models. The aim is to translate laboratory results into the clinic to treat patients with prostate cancer.
Scan the QR code to explore Massey’s 20212025 Strategic Plan


Massey continues to offer one of the largest selections of clinical trials for adults and pediatrics in Virginia for enabling our investigators to participate in practicechanging clinical science every day. Over the last few years, Massey has continued an upward trend toward record-breaking numbers of clinical trial accruals at the cancer center.




As a part of the North American Star Consortium (NASC), Massey is a national collaborator on efforts to identify promising new treatments for all cancer patients. NASC is a partnership between five leading cancer centers in the country and one of only nine NCI-funded Experimental Therapeutics Clinical Trials Networks. This consortium informs, develops and leads paradigm-shifting clinical trials ensuring the accrual of participants that reflects the national population. Led by Steven Grant, M.D., Massey’s involvement in this initiative helped advance the understanding of the efficacy of different treatment options for cancer, including acute myeloid leukemia. The consortium also serves as a springboard for early-stage investigators like Keri Maher, D.O., who was instrumental in these analyses.
Over the last year, physician-scientists at Massey have translated scientific discoveries from their laboratories into action. Through research and clinical trials, Massey investigators are directly advancing the national practice and understanding of breast cancer care.
Breast cancer affects one in eight women in the U.S. Higher levels of cancer-fighting immune cells in breast tumors are associated with a better response to chemotherapy and overall improved outcomes in patients. Through a phase 2 clinical trial led by Harry Bear, M.D., Ph.D., a team of Massey scientists identified a combination of drugs (a chemotherapy known as decitabine and an immunotherapy called pembrolizumab) that, when given as a first-stop treatment before the standard of care for triple-negative breast cancer, enhanced patients’ immune response and made their breast tumors more vulnerable to chemotherapy administered prior to surgery or radiation.
Leading specialists at Massey are also shaping the future of radiation treatment for breast cancer in the U.S. Moderate hypofractionated radiation is a form of radiation therapy administered in higher doses over a shorter period than standard radiation therapy, offering more convenient and shorter treatment times for patients. However, the unknown risk of lymphedema — tissue swelling caused by the buildup of lymphatic fluid — associated with this form of treatment in lymph node-positive breast cancer has limited its universal clinical use. A phase 2 trial, conducted by Douglas Arthur, M.D., chair of the Department of Radiation Oncology, and collaborators Alfredo Urdaneta, M.D., Todd Adams, M.D., and Nitai Mukhopadhyay, Ph.D., set out to evaluate this risk. Findings indicated that there is not sufficient evidence of increased lymphedema risk, endorsing this beneficial treatment option in the clinic for patients with node-positive breast cancer.
Accelerated partial-breast irradiation is a form of radiation therapy where a higher dose is targeted only to the part of the breast where cancer is present over a shorter period of time than standard whole-breast radiation. Bridget Quinn, M.D., Ph.D., led another phase 2 trial at Massey that seeks to determine the safety of using multiple catheters to deliver accelerated partial-breast irradiation through radioactive implants placed directly inside the breast tumors. These implants provide a concentrated dose of radiation over a two-day period. If proven effective, this could significantly reduce radiation treatment regimens for many breast cancer patients.
For more than 30 years, Massey has played a significant role in facilitating the development of communitybased oncology clinical trial partnerships through its Minority/Underserved NCI Community Oncology Research Program (MU-NCORP).
MU-NCORP has been an important part of Massey’s history, and its expansion of clinical trial offerings statewide provides cancer patients access to prevention, early detection and treatment clinical trials, as well as cancer care delivery research closer to home.
Through specialized support for investigators at community sites in the development and ongoing management of a quality clinical trials program, Massey is increasing clinical research opportunities for communities outside the greater Richmond area. The statewide network also provides access to innovative cancer trials through membership to all four adult National Clinical Trials Network groups, Children’s Oncology Group and two NCORP Research Bases.
Massey is one of only 14 MU-NCORPs in the country, and is actively partnering with 10 health systems and oncology medical practices throughout the Commonwealth.


Massey has seen tremendous growth in our career pathway programs, particularly those designed for students and trainees who are less exposed to career opportunities in the biomedical sciences. In 2023, Massey investigators were engaged with 563 students and trainees, 21% of whom were Black, Native American and/or Latine, and 67% who identified as female.
DEVANAND SARKAR, MBBS, PH.D.
ASSOCIATE DIRECTOR, RESEARCH TRAINING & EDUCATION
HARRISON FOUNDATION DISTINGUISHED PROFESSORSHIP IN CANCER RESEARCH

Massey’s innovative career pathway program for cancer-focused research education and training has seen substantial growth in the last year. Led by the Office of Cancer Research Training & Education Coordination, four new programs have been introduced since 2022, offering exciting opportunities for students and trainees across the Commonwealth.
With funding from a Cancer Center Support Grant supplement, Massey’s Office of Research Development launched additional resources to support investigators navigating the complex research funding landscape. Training navigators at the center help identify scientists at any career stage from three minority-serving institutions — VCU, Virginia State University and the University of Puerto Rico Comprehensive Cancer Center — who are interested in developing NCI proposals. Since the award, Massey has engaged nearly 40 trainees and facilitated a dozen research submissions.
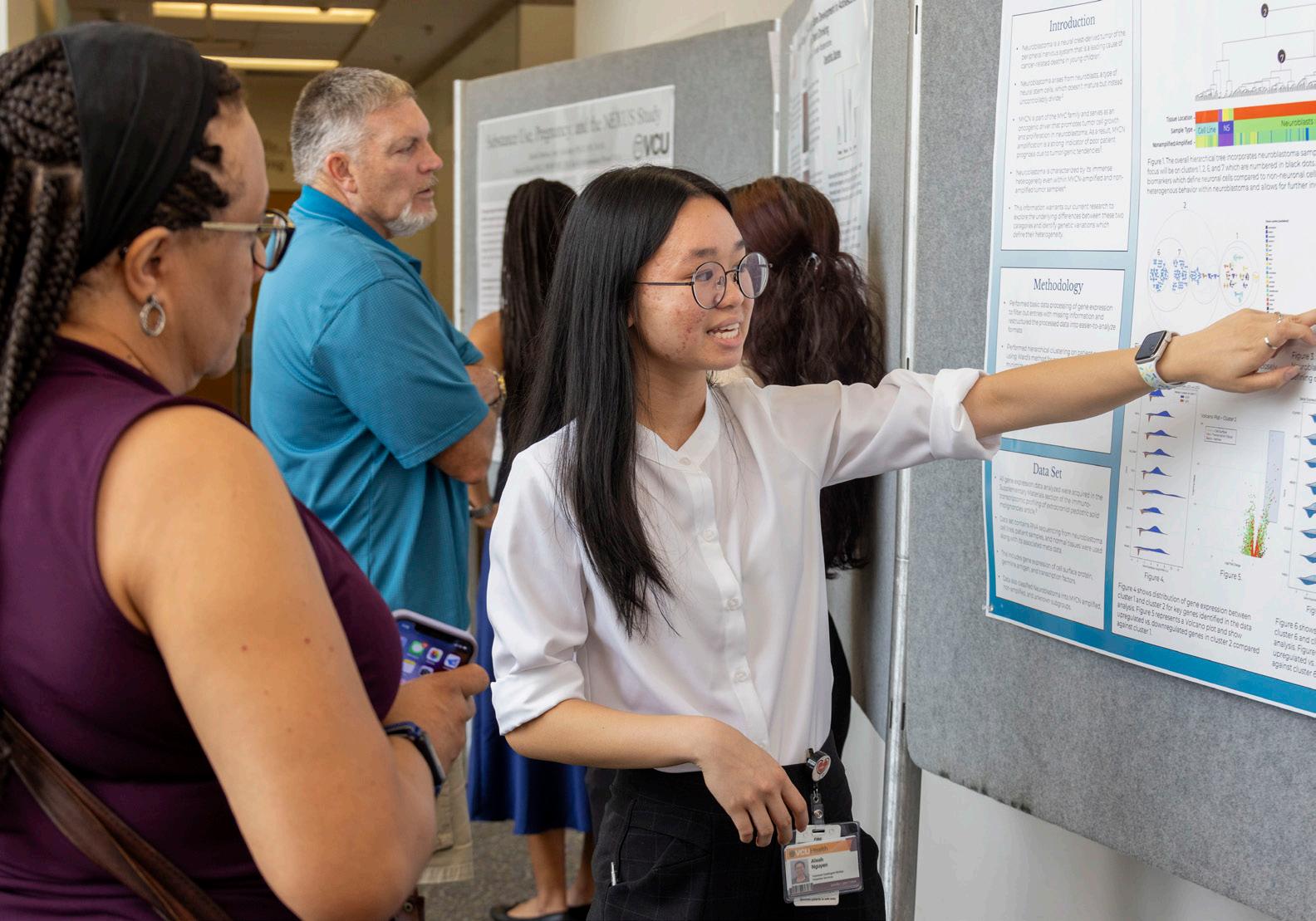
In 2023, the center also hosted its first Student Summer Research Symposium, where more than 25 students showcased their research, presenting scientific posters and sharing experiences with Massey leaders, mentors and other trainees. Massey’s recently expanded portfolio of career pathway programs includes the American Cancer Society-funded Cancer-focused Undergraduate Research Experience (CURE) and the National Cancer Institute-funded Integrative Training in Cancer Biology program.
Learn more about Massey’s career pathway programs

In partnership with the American Cancer Society, Massey hosts undergraduate students historically underrepresented in medicine for an immersive summer internship at the center’s downtown Richmond campus. CURE’s inaugural 2023 cohort of four students were paired with Massey mentors across basic, clinical and population sciences. Under the leadership of David Gewirtz, Ph.D., CURE offers hands-on research and provides real-world insight into oncology-focused career opportunities beyond the classroom.
One in the cohort, Sandra Makar, interned in the laboratory of Paula Bos, Ph.D., as a CURE student the summer before her senior year at VCU. Makar was initially drawn to the opportunity as a way to gain more experience prior to pursuing a Ph.D. in cancer research. Ten weeks later, she completed an independent research project on Treg cells and stem cells in the mammary gland. Makar went on to present her work at the American Association of Cancer Research annual meeting, one of the largest oncology research conferences in the world, where she received an honorable mention recognition (one of 10) among 100 student presentations.
Scan the QR code to watch the CURE video

Cancer biology training programs are inherently designed around basic, laboratory-based science. But at Massey, everything starts with the community. Massey’s most recent NCI-funded T32 integrative training program for pre- and postdoctoral trainees is designed to bring community engagement to the benchside — incorporating non-biological factors driving cancer disparities into the scientific questions and leveraging community input into the design, implementation and dissemination of basic cancer research. The Integrative Training in Cancer Biology program’s initial cohort of six trainees kicked off their training by meeting with cancer champion mentors to gain insight into ways to interact with the community from a research perspective.
Matthew Fernandez, a Ph.D. student at Massey and the VCU School of Pharmacy, was named as a recipient of the 2023 AACR Minority Scholar in Cancer Research Award. The award program intends to increase the scientific knowledge base of minority scientists and to encourage them to pursue careers in cancer research. During the annual meeting, Fernandez presented his research in the area of nanomedicine, which is focused on improving chemotherapy efficacy for triple-negative breast cancer with macrophage-targeted immunotherapy. Fernandez hopes the work will enhance the standard of care by reprogramming the breast tumor to a pro-inflammatory phenotype.
“This award means a lot to me because it shows that my laboratory is doing good work and making strides toward improving patient outcomes for those diagnosed with triplenegative breast cancer,” Fernandez said. “It feels good to represent the Hispanic community.”
Fernandez is co-mentored by Sandro R.P. da Rocha, Ph.D., professor of pharmaceutics and director for Pharmaceutical Engineering at the School of Pharmacy and a member of Massey’s Developmental Therapeutics research program, and Douglas H. Sweet, Ph.D., chair of Pharmaceutics and E. Claiborne Robins Distinguished Professor at the VCU School of Pharmacy.


Michael Rao, Ph.D. President, VCU and VCU Health System
Marlon Levy, M.D., M.B.A. Senior Vice President, VCU Health Sciences CEO, VCU Health System
P. Srirama Rao, Ph.D. Vice President, Research & Innovation at VCU
John McCurley, M.D., MHA* Interim President, VCU Medical Center
Michael Elliott, PharmD, MSHA, FACHE Chief Operating Officer, VCU Health System
Arturo Saavedra, M.D., Ph.D., M.B.A. Executive Vice President for Medical Affairs, VCU Health System Dean, VCU School of Medicine
F. Gerard Moeller, M.D. Director, Wright Center for Clinical & Translational Research at VCU
Elias Neujahr, M.H.A., M.B.A. President, Children’s Hospital of Richmond at VCU
*Effective early 2025, Jim Willis assumed the position of interim president for VCU Medical Center.
MASSEY SENIOR LEADERSHIP
Robert A. Winn, M.D. Director, VCU Massey Comprehensive Cancer Center
Paula M. Fracasso, M.D., Ph.D., FACP Deputy Director, VCU Massey Comprehensive Cancer Center
Paul Fawcett, Ph.D. Associate Director, Shared Resources
Bernard F. Fuemmeler, Ph.D., M.P.H.
Associate Director, Population Sciences
Steven Grant, M.D. Associate Director, Translational Research
Michelle K. Lin, M.B.A Associate Director, Administration
Khalid Matin, M.D., FACP Associate Director, Global Oncology
Andrew S. Poklepovic, M.D. Associate Director, Clinical Research
Devanand Sarkar, MBBS, Ph.D. Associate Director, Research Training & Education
Saïd Sebti, Ph.D. Associate Director, Basic Research
Katherine Y. Tossas, Ph.D.* Interim Associate Co-Director, Community Outreach & Engagement
David P. Turner, Ph.D. Interim Associate Co-Director, Community Outreach & Engagement
*Effective early 2025, Katherine Tossas assumed the position of Associate CoDirector, Global Oncology
RESEARCH PROGRAM LEADERSHIP
CANCER BIOLOGY
Azeddine Atfi, Ph.D.
Paula D. Bos, Ph.D.
DEVELOPMENTAL THERAPEUTICS
Anthony C. Faber, Ph.D.*
Steven Grant, M.D.
Xiang-Yang “Shawn” Wang, Ph.D.
CANCER PREVENTION & CONTROL
Victoria J. Findlay, Ph.D.
Oxana G. Palesh, Ph.D., M.P.H.
*Effective late 2024, Anthony Faber stepped down from his role as program co-leader.
FAITH-BASED LEADERSHIP
FOUNDING MEMBERS
Rudene Mercer Haynes, J.D. Partner, Hunton Andrews Kurth, LLP
Rev. F. Todd Gray Pastor, Fifth Street Baptist Church
Robert A. Winn, M.D. Director, VCU Massey Comprehensive Cancer Center
STUDENT REPRESENTATIVES
Maryam Amir Student, VCU
Malk Eldessouky Student, VCU
OreOluwa Comfort Aluko Winn CIPP Research Scholar, VCU Medical School
Kevin Babu
Student, VCU Medical School
MEMBERS
Jessica Young Brown, Ph.D., LCP
Resident Therapist, Facts & Faith Fridays
Rev. Marvin Gilliam, Jr. Pastor, The Mount Carmel Baptist Church
Rev. Dr. Cheryl Ivey Green
Executive Minister, The First Baptist Church of South Richmond
Dr. Dwight C. Jones
Senior Pastor, The First Baptist Church of South Richmond
Rev. Rachel Pierce Faith Liaison & Engagement Coordinator, VCU Massey Comprehensive Cancer Center
Rev. Dr. Herbert Ponder Pastor, Mount Tabor Baptist Church
Rev. Dr. Jerome C. Ross Pastor, Providence Park Baptist Church
Rev. Dr. Tyron Williams Pastor, Mount Olive Baptist Church
Arnethea Sutton, Ph.D. Assistant Professor, Kinesiology & Health Sciences
DIRECTOR’S CABINET
Father Shay Auerbach Jesuit Priest, Sacred Heart Catholic
Karen Wilson
Senior Vice President, Bank of America
L.D. Britt, M.D.
Vice Dean of Clinical Affairs, Eastern Virginia Medical School
Tracy Douglas-Wheeler
CEO, Virginia Community Healthcare Association
Bryan Ennis
Vice President of Customer Experience Centers, CarMax
Lindsey Johnson
Representative, Chickahominy Tribe
Amy Williams
Former Vice Chair, Philanthropic Board
L. Michael Gracik, Jr., CPA
Immediate Past Chair, Massey Advisory Board
Rudene Mercer Haynes, J.D. Partner, Hunton Andrews Kurth, LLP
Ben Barani
Former Chair, Massey Alliance Young Professionals Board
Riguey King
Vice President of Community Impact, American Cancer Society
James Millner
Program Director of VA Pride, Diversity Richmond
Rev. Tyrone E. Nelson
Vice Chairman, Henrico County Board of Supervisors
Kevin D. Smith
Director of Legal Operations, Dominion Energy
Rev. Leo Whitaker
Executive Minister, Baptist General Convention of Virginia
Anne Whittemore Chair, Massey Advisory Board
RECRUITMENTS (FY23)
Elizabeth Barrows, M.D. Assistant Professor, Internal Medicine
Jonathan Berkman, M.D. Assistant Professor, Internal Medicine
Mariza Daras, M.D. Chief, Division of Neuro-Oncology Associate Professor, Neurology
Ruchi J. Desai, M.D. Assistant Professor, Internal Medicine
Bruce Hough, M.D. Assistant Professor, Internal Medicine
Emily N. Kinsey, M.D. Assistant Professor, Internal Medicine
Autumn M. Lanoye, Ph.D. Assistant Professor, Internal Medicine
John W. Melson, M.D. Assistant Professor, Internal Medicine
Carrie A. Miller, Ph.D.
Assistant Professor, Family Medicine & Population Health
Emmanuel Skordalakes, Ph.D. Associate Professor, Pharmacology & Toxicology
Douglas W. Arthur, M.D.
Florence and Hyman Meyers Chair in Radiation Oncology
Charles V. Clevenger, M.D., Ph.D.
Carolyn Wingate Hyde Endowed Chair in Cancer Research
Paul Dent, Ph.D. Universal Corporation Chair in Cancer Cell Signaling
Anthony C. Faber, Ph.D.
Natalie N. and John R. Congdon, Sr. Endowed Chair in Cancer Research
Paul B. Fisher, M.Ph., Ph.D.
Thelma Newmeyer Corman Endowed Chair in Oncology Research
Paula M. Fracasso, M.D., Ph.D., FACP
Dianne Nunnally Hoppes Endowed Chair in Cancer Research
Bernard F. Fuemmeler, Ph.D., M.P.H.
Gordon D. Ginder M.D. Chair in Cancer Research
Gordon D. Ginder, M.D. Massey Club Chair
Steven Grant, M.D.
Shirley Carter and Sture Gordon Olsson Chair in Cancer Research
Suyun Huang, M.D., Ph.D.
Paul M. Corman M.D. Chair in Cancer Research
Joseph H. Laver, M.D. Children’s Hospital of Richmond Endowed Chair in Pediatric Cancer Research
Patrick Nana-Sinkam, M.D.
Linda Grandis Blatt Endowed Chair in Cancer Research
Oxana G. Palesh, Ph.D., M.P.H.
Massey Cancer Center Chair in Cancer Research
Saïd Sebti, Ph.D.
Lacy Family Chair in Cancer Research
Vanessa B. Sheppard, Ph.D.
Theresa A. Thomas Memorial Foundation Chair in Cancer Prevention and Control
Sarah Spiegel, Ph.D.
Mann T. and Sara D. Lowry Chair in Oncology
Robert A. Winn, M.D.
Jeannette and Eric Lipman Chair in Oncology
Yuesheng Zhang, M.D., Ph.D.
Harrigan Haw Luck Families Chair in Cancer Research
Azeddine Atfi, Ph.D.
Mary Anderson Harrison Distinguished Professorship in Cancer Research
Laurence J. DiNardo, M.D.
Darlene and George P. Emerson Jr. Professorship in Cancer Research
Susan Hong, M.D., M.P.H., FACP
RGC Professorship for Cancer Research
Renato G. Martins, M.D., M.P.H.
Martha Anne Hatcher
Distinguished Professorship in Oncology
Leslie M. Randall, M.D.*
Dianne Harris Wright Professorship for the Division Director of Gynecologic Oncology at MCV-VCU
Dianne Harris Wright Professorship for OB-GYN Oncology Research
Devanand Sarkar, MBBS, Ph.D. Harrison Foundation Distinguished Professorship in Cancer Research
Jose G. Trevino, M.D., FACS
Walter Lawrence Jr. Distinguished Professorship in Oncology
Xiang-Yang “Shawn” Wang, Ph.D.
Harry and Judy Wason Distinguished Professorship
Jolene J. Windle, Ph.D. Irene Shaw Grigg Distinguished Professorship in Genetics Research
ACTIVE CANDIDATE SEARCH
Judith Talley Secor Chair
Massey Alliance Scholar
Wook-Jin “Eddie” Chae, Ph.D.
Sun Jung “Sunny” Kim, Ph.D., M.S., M.A.
Can Senkal, Ph.D.
Katherine Tossas, Ph.D., M.S.
*Following departure of chair holder, active candidate search in progress at time of publication
OFFICERS
Anne Marie Whittemore Chair
Rebecca C. Massey Vice Chair
MEMBERS
Shelly Arthur
O’Conor G. Ashby II
Ann H. Austin
Roger L. Boevé
Jean Ann Bolling
Ellen T. Bonbright
Judy S. Brown
Charles L. Cabell
Theodore L. Chandler Jr.
Judith T. Clough
John Congdon Jr.
Sarah B. Cossé
Brian Davis
Preston Dillard
James K. Donaldson
George P. Emerson Jr.
Josh Goldschmidt
Elizabeth S. Gorman
Ann Parker H. Gottwald
L. Michael Gracik Jr.
A. William Hamill
Terrell Luck Harrigan
Rudene Mercer Haynes, J.D.
Connie Hom
Eucharia Jackson
Tracey W. Jameson
Joseph R. Jenkins
Martin Johnson
Deborah J. Johnston
Linwood A. Lacy Jr.
John B. Lewis
Michelle Logan
David A. Lyons
Aaron McClung
Patricia Merrill
Henry R. Miller
Elizabeth B. Minter
Brandon Moore
James T. Napier
Mary Harvard Nolde
Carl E. Omohundro Jr.
Kathryn H. Pearson
Catherine Plotkin
Anna W. Reed
Jennifer Ronga
Helen J. Ryan
Frances Santarella
Dr. Travis L. Shaw
Karen Shudtz
Vickie M. Snead
Judith Forehand Starkey
Elizabeth H. Thornton
Christina E. Todd
Amanda Tornabene
Robert G. Whitten
Amy McDaniel Williams
EMERITUS MEMBERS
William G. Broaddus
Charles F. Crone
James E. Farnham**
Alice T. Goodwin
Adrienne Maxwell
Matthew G. Thompson
Judith Harris Turbeville
EX-OFFICIO MEMBERS
Benjamin Barani
Tara E. Daudani
Dorothy Erlanger
Lisa S. Goodwin
Julia Hammond
Mary Lawson
Joey McCaffrey
Katherine Schroth
MASSEY ALLIANCE YOUNG PROFESSIONAL BOARD (FY23)
LEADERSHIP
Benjamin Barani President
Katherine Schroth President-Elect
Michael G. Hofmeister Immediate Past President
MEMBERS
Dr. Kyle Adams
Heather Brown
Brigid Bucci
Timothy C. Cavazos
Ernest J. Chamberlain
Robert Daniel Halloran
Phebe Jenkins
Mark Lynch
Justin Maitland
Taylor Mickel
George E. Moore IV
Yann E. Reichelt
Andrew Russo
Nicholas J. Shedd
David S. Stabler III
**Deceased
William Stallings
Paul Staples
Laurenso Williams





