
























For the 17th year in a row, U.S. News & World Report ranks Texas Children’s #1 in Texas and among the nation’s best. This honor reflects our standard of care, but our mission extends beyond rankings: to pioneering research, groundbreaking discoveries and expanding possibilities in pediatric medicine.



















Top in the nation in every specialty:
No. 1 No. 1
No. 1
No. 2
No. 2 No. 2 No. 5
No. 5 No. 5 No. 9
Cardiology & Heart Surgery
Neurology & Neurosurgery
Pulmonology & Lung Surgery
Neonatology
Nephrology (Kidney Disorders)
Urology
Diabetes & Endocrinology
Gastroenterology & GI Surgery
Orthopedics
Cancer

CHAPTER ONE
12 The Promise and Challenges of AI in Medicine
Artificial intelligence is transforming healthcare, but that doesn’t mean it’s without potential drawbacks.
40 The Midwife Solution
To save more mothers’ lives, the U.S. needs to rethink how we give birth.
42 Living Longer, Living Better
Ten science-based strategies that can help you stay healthy and vibrant late into life.
46 The Hidden Health Risks of Alcohol
Raising a glass to good health is doing just the opposite.
72 Pain and the Power of the Mind
Mind-body therapies may help you reframe awareness of pain.
78 Your Ultimate Menopause Guide
With the right lifestyle strategies and treatment, this hormonal transition can be an empowering period of life.
82 Walking Toward Better Health
Putting one foot in front of the other is a simple way to reduce your risk of certain chronic diseases.
86 Best Diets of 2025
Your goal: to find the eating plan that will work best for you.
89 Eat Your Way to Better Gut Health
What you put on your plate can help—or hurt—the well-being of your gut.
93 How to Put Together a Family Medical History
Your family’s medical past may hold the key to your future health.

Clinical excellence, breakthrough research, and world-class expertise.



For 125 years, we’ve been the established leader in treating children on the West Coast. Whether it’s for routine care or a lifesaving need, families turn to Children’s Hospital Los Angeles for the very best in pediatric care.
































The American College of Cardiology (ACC) recognizes these Health Systems for their commitment to driving preeminent hospital care for heart patients. Participating in the ACC’s proven quality care delivery and outcomes programs demonstrates their commitment to better lives for healthier tomorrows.












Wellstar Health System
University of California Health System
SSM Health Care
Adventist Health
Alabama Healthcare Holdings, LLC
Baptist Memorial Health Care Corporation
BJC HealthCare
Banner Health
Yale New Haven Health
Deaconess Health System, Inc.
Kaleida Health Buffalo
General Foundation
Memorial Health System of California
MultiCare Health System
Mayo Foundation for Medical Education and Research
The Cleveland Clinic Foundation
PorterCare Adventist Health System
Prime Healthcare Services
ScionHealth
SCL Health System
St. Luke’s University Health Network
146 Taking On Childhood Concussions
A deep dive into kids’ head injuries—from the warning signs to recovery.
152 A Parent’s Guide to Nourishing a Healthy Eater Doc-approved tips for making sure kids get the nutrition they need. 156 Navigating the Youth Mental Health
The support and guidance you need to help a child through their challenges.



Read about how U.S. News identified and ranked top hospitals in each
181 The Rankings See how nearby hospitals performed in areas of specialty care and in common procedures and conditions.
195 Caring for Whole Communities
U.S. News recognizes hospitals that treat patients from every stratum of their communities.
198 Best Regional Children’s Hospitals A region-by-region ranking based on performance in 11 specialties.
Two of our hospitals, Robert Wood Johnson University Hospital and Cooperman Barnabas Medical Center, have earned recognition as Best Regional Hospitals, ranking in the top 10 in New Jersey, and in the top 25 in the competitive Mid-Atlantic Region. Our hospitals throughout New Jersey have been recognized for quality in a variety of specialties: cardiac and cancer care, neurology and orthopedic surgery, and more. Learnmoreatrwjbh.org/usnews.
NUTRITION AND LIFESTYLE
A look at some of the most popular and best researched diets, with reviews by a panel of health experts. Discover the top plans for weight loss, diabetes management and heart health, as well as the best plant-based and menopause diets. health.usnews.com/best-diet
Stay on top of the latest health news and research, and get expert insight into trending wellness topics. health.usnews.com/wellness
INSURANCE
State-by-state ratings of insurers offering Medicare Advantage and Medicare Part D plans, plus tips on choosing one of these plans vs. original Medicare. health.usnews.com/medicare
POPULATION HEALTH
An interactive platform featuring news, analysis and county-level rankings that examine how social factors shape America’s health and well-being. usnews.com/news/healthiestcommunities
OUTPATIENT CARE
Discover the top outpatient surgery centers for a variety of procedures near you. health.usnews.com/best-ascs

We’ve evaluated nearly 5,000 hospitals on 22 common procedures and conditions, including hip replacement, knee replacement, heart bypass surgery, colon cancer surgery, diabetes and stroke, as well as 15 medical specialties from cancer care to cardiology. health.usnews.com/best-hospitals
SENIOR CARE
An analysis of government data and published ratings of more than 15,000 nursing home facilities throughout the United States. health.usnews.com/ best-nursing-homes
Which over-the-counter products do pharmacists and dermatologists prefer? To make your next trip to the drugstore easier, check out these top recommended medicine and health products, ranging from skin care to supplements. health.usnews.com/otc
PHYSICIAN SEARCH TOOL
A searchable directory of more than 750,000+ doctors. Patients can find and research doctors who have the training, certification, practical experience and hospital affiliation they want—and can see ratings based on other patients’ experience. health.usnews.com/doctors


Nationally recognized for excellence, year after year.






























El Camino Health has deep roots in the South Bay, providing compassionate care that’s part of a comprehensive, coordinated network, putting you and our community first.
Our commitment to excellence continues to earn national recognition, including being named “Best Hospital 2025–2026” by U.S. News & World Report for consecutive years. Every recognition reflects the trust our patients place in us, the honor we value most. For leading-edge primary, urgent and specialty care delivered through a personalized approach for every stage of life, choose El Camino Health.
El Camino Health. Our strength is your health.





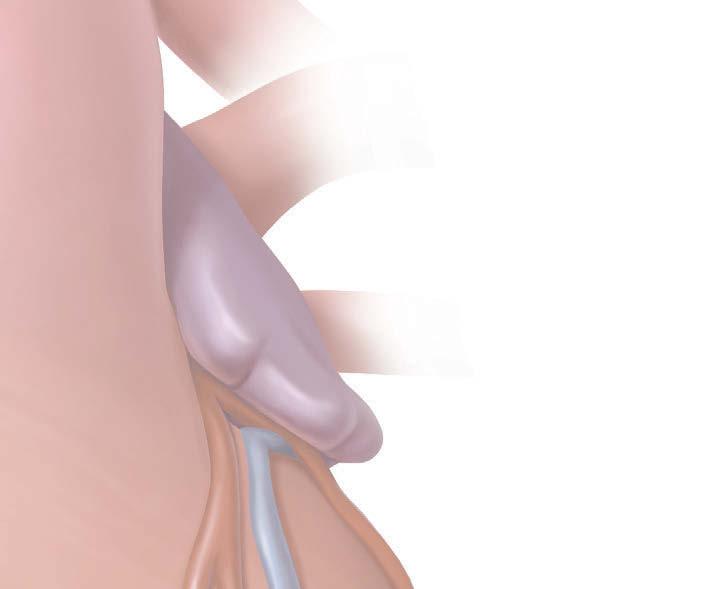
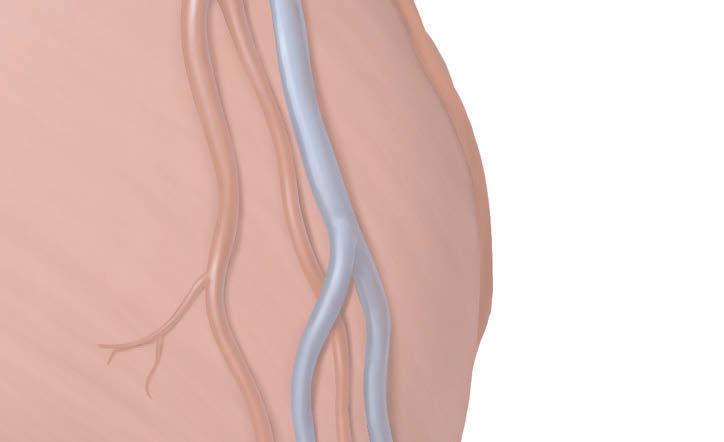
Lexi, 2 years old. Received in utero surgery for spina bifida at 25 weeks.
When Lexi was still in her mother’s womb, fetal surgeons and neurosurgeons at Nationwide Children’s Hospital repaired a spinal defect that would have a ected her ability to walk. Today, she’s a happy 2-year-old who can walk on her own.
Every day, Nationwide Children’s helps children like Lexi take a step towards a better quality of life. See









The health headlines you need to know about
The best hospital for you or a loved one depends on the type of care you need. For a rare bone condition or a lung transplant, for instance, you may need to travel to a hospital that earned a top 50 national ranking for orthopedics or pulmonology, respectively. But for a common procedure or condition like a hip replacement or COPD, you are likely to find that a hospital close to home is highly rated by U.S. News.


The quality of health care provided by hospitals to patients across the nation varies widely. U.S. News delves into various quality measures to publish rankings and ratings of hospitals that assist millions of patients annually. These patients face the prospect of surgery or specialized hospital care that can pose a risk due to such factors as age, physical condition or the type of illness. The rankings and ratings are a tool to help consumers make important health care decisions, in conjunction with advice from medical practitioners.
U.S. News’s Best Hospitals project evaluates U.S. adult hospitals annually on how they provide 37 different types of care. The rankings of 15 medical specialties use a variety of quality measures to identify the hospitals that excel at handling the most complex and difficult cases. The ratings of 22 common procedures and conditions are based entirely on objective quality indicators, such as patient outcomes and nurse staffing levels. We also publish

an Honor Roll of the hospitals that excel in many types of care, as well as rankings of general hospitals by state and major metro area.
Hospitals that earn top 50 rankings in a specialty have a gold Best Hospitals award “badge” (logo) on their U.S. News profile page, with information about how many such rankings they won. General hospitals that excel in a large number of common procedures and conditions have a silver “Best Regional Hospitals” silver badge and may be ranked in their state and/or metro area. Hospitals that place in the top 10% for a specialty but not in the top 50, or that achieve the highest possible rating for a common procedure or condition, have a High Performing Hospitals emblem on their profile page.

Hospitals that earn a badge or emblem may obtain permission, for a fee, to display the badge or emblem via websites and other media from BrandConnex, U.S. News’s licensing agent. Current and future rankings, ratings and awards are not affected by such purchases or by any other promotional fees.
• The evaluation of hospitals in your area: https:bit.ly/USN-area


• For detailed information about a specific hospital: https://bit.ly/USN-search
• About U.S. News’s hospital evaluations, including Best Children’s Hospitals and Best Hospitals for Maternity Care as well as Best Hospitals: https://bit.ly/USN-FAQ
• Detailed methodology reports about the Best Hospitals specialty rankings https://bit.ly/USN-2526 and the procedures and conditions ratings https://bit.ly/USN-ratings
• Hospitals that earn a badge or emblem may contact usnews@BrandConnex.com for information about using U.S. News Best Hospitals badges and emblems.



Artificial intelligence is transforming medicine, offering advancements in diagnostics, treatment, drug development and patient care. But that doesn’t mean it’s without potential challenges and ethical considerations to ensure responsible, effective use.
by Cheyenne Buckingham ©
rtificial intelligence, or AI, is a contentious topic in today’s world, but both health care professionals and researchers are enthusiastic about its potential to revolutionize patient care—from diagnosis and treatment to how doctors correspond with their patients.
AWhile recent advancements have catapulted AI into the spotlight, the technology isn’t new. It has been around for more than 70 years, with the first medical applications emerging in the 1970s. Since then, the technology has helped doctors diagnose conditions and identify appropriate treatments. It’s also assisted radiologists in interpreting microscopic abnormalities on imaging scans, including mammograms and other routine cancer screenings.
Fast forward to today: AI is more sophisticated than ever before, and it will only continue to become more knowledgeable. Just recently, the first AI-designed drug, Rentosertib, made its way through several clinical trials, showing promise as an effective treatment for idiopathic pulmonary fibrosis (IPF), a chronic, progressive lung disease that makes it challenging to breathe.
AI also assists scientists with drug repurposing, or identifying which readily available medications can be used—alone or in combination with others—to treat rare diseases, including certain cancers and neurological conditions. In radiology, AI offers radiologists a second set of eyes that surpass human capabilities.
Yet despite the technology’s impressive prospects, AI—much like humans—can make mistakes, which is why it’s best used (for now) as a collaborative tool for physicians and researchers. In other words, providers and scientists alike still need to keep a careful eye on its decision-making abilities.
The use cases for AI in medicine are rapidly expanding as the technology improves. In fact, your doctor likely already uses AI during your office visits.
Administrative tasks “One area that has made a big difference in patient care is ambient documentation, in which AI listens to a conversation between the doctor and the patient and produces notes in real time,” says Dr. David Westfall Bates, the co-director of the Center for Artificial Intelligence and Bioinformatics and the
Learning Healthcare System at Mass General Brigham.
In some instances, the physician can have key takeaways from the appointment and next steps drafted and ready to send by the end of the visit. “AI scribes provide some immediate quick wins, from an organizational perspective, and also decrease the epidemic of clinician burnout that we’re seeing today,” says Brenton Hill, the head of operations and general counsel for the Coalition for Health AI (CHAI)
Data suggest that tools like these can reduce a physician’s time spent documenting a patient’s electronic health record (EHR) by as much as 16%. That said, AI scribes have been known to record notes incorrectly sometimes, which is why the physician needs to review the script before logging it into the patient’s medical records or sending follow-up notes via the patient portal.
Artificial intelligence tools can also be used to generate letters and scripts for insurance companies, says Bates. Essentially, AI can help physicians execute the administrative elements of their job in a more timely and efficient manner.
Disease detection and diagnosis AI offers clinical support by aiding in diagnosis. It analyzes patterns in patient data and presents them to health care professionals to help guide informed decisions.
“AI algorithms are being tested for their ability to consolidate and analyze a variety of patients’ data, such as medical histories, lab and imaging results and genetic information, to predict when disease might arise,” says Dr. Andrew Hantel, a health services researcher, hematologic oncologist and ethics consultant at Dana-Farber Cancer Institute and Harvard Medical School. “AI can enhance interpretation of images used in diagnosis or treatment. When used by trained physicians, AI tools can improve the speed and accuracy of some diagnoses.”
For example, tools like Google’s DeepMind have successfully identified breast cancer in mammograms, explains Thomas Swalla, CEO of Dotmatics, a software company that connects science, data and decision-making.
A 2020 study found that Google’s DeepMind AI system outperformed six human radiologists when it came to identifying breast cancer on the screen, and newer research has shown similar results. This suggests that the tool can be used to help reduce false negatives and false positives.
their own unique genetic makeup, meaning how you fare on a medication could be vastly different from another person.
Using AI to make personalized treatment recommendations based on a patient’s genome can help physicians make better choices for their patients, potentially saving them the distress of having to rule out multiple medications or therapies through trial and error.
“AI algorithms have the potential to help synthesize different data sources to recommend treatments that account for genetic data, co-occurring conditions and estimated risk,” Hantel says. These algorithms are still in the testing phase, so they aren’t widely used yet in the clinical setting.
Robotics Robots can assist physicians in a variety of ways. For example, AI-powered robots are currently being tested for use in surgery to enhance precision and reduce the need for invasive procedures when possible. “Robotics can help surgeons better assess their operations in real time,” Hantel says.
Robotics can also be employed to help with logging notes in the patient portal, cleaning hospital rooms and examining images such as MRIs and X-rays.
Drug development AI is helping design life-saving drugs, such as Rentosertib. “AI-based algorithms are being used to predict the structure of different human proteins and how they interact with a variety of chemical compounds to identify promising candidates, reduce research costs and shorten the time to clinical trials,” says Hantel.
Bates adds that AI is particularly strong at reading pathology slides, which are tiny pieces of tissue placed on glass for doctors to examine under a microscope and check for signs of disease. “This is the way most cases of cancer are diagnosed,” he says.
Personalized treatments “AI will be used a lot in the future, I believe, to personalize treatments for patients,” Bates says. When treating a specific condition, such as hypertension, a doctor will likely start you on a medication that most people respond well to. But each person has
At Dotmatics, Swalla is seeing AI accelerate early-stage drug discovery by modeling and predicting how molecules will behave before they’re synthesized in the lab. “Scientific intelligence platforms, like our own Dotmatics Luma, enable scientists to simulate, iterate and analyze compound designs faster and more intelligently, reducing both time and cost across the design-make-test-decide cycle.”
The benefits of AI in medicine are far-reaching for both physicians and patients. Perhaps the most important is this: AI can help doctors support their patients more effectively and more consistently.
To start, AI holds enormous potential to reduce doctor burnout. A 2025 survey found that 54% of physicians believe AI could help ease stress and burnout, which is a notable rise from 44% in 2023. That optimism matters: doctors today are stretched thinner than ever.
Consider this: a 2022 study estimated that a primary care physician would need 26.7 hours in a sin-
gle day to deliver all guideline-recommended care to their patients. That math alone makes it clear why exhaustion and errors happen. When clinicians are expected to be superhuman, mistakes become inevitable. This is where AI steps in—not as a replacement, but as a partner. Think of it as the med student who never sleeps: it can handle all of the relentless data review, pattern recognition and administrative load that siphon precious hours away from direct patient care.
For patients, however, one of the greatest promises of AI-supported healthcare is improved access. People in underserved communities— especially rural areas—often struggle to reach high-quality care. A Pew Research Center survey found that nearly one in four rural residents reported lacking easy access to good doctors and hospitals. That gap in care can mean delayed diagnoses, and untreated conditions as well as unnecessary suffering.
At CHAI, Hill notes that patient advocacy groups are already voicing excitement about working with AI developers to close these gaps. Tools such as large language models could play a pivotal role: answering common medical questions, delivering reliable health information and guiding patients in deciding when to seek care. Imagine someone living two hours from the nearest hospital—AI could help them distinguish between a situation that truly requires an emergency room visit and one that can safely be managed at home or with a local clinic.
“There’s a large gap of data that’s made available for these developers to train on,” Hill says. Patient data protection laws, such as the Health Insurance Portability and Accountability Act (HIPAA), inhibit developers from training their algorithms on patient medical records.
In addition, hospitals and clinics in rural areas are often less likely to provide data to developers, Hill says. This means AI tools may not work well for populations they haven’t been trained on, making them less accurate or useful in those settings.
“AI models require large, high-quality datasets, but medical data is inconsistent, incomplete and fragmented across systems,” explains Hantel.
Additionally, when it comes to chronic disease management, AI tools can be an invaluable resource. Apps can help patients log their symptoms and provide real-time dietary recommendations to help them improve their health.
“AI can also aid in how medical information is conveyed to patients, especially those with lower health literacy or who speak a different language than their care team,” says Hantel. Moreover, wearable devices that use AI can continuously monitor data and flag health risks earlier, helping a patient get ahead of serious symptoms or complications.
While AI has demonstrated immense promise for improving care, it comes with its own set of drawbacks and challenges. The biggest barrier right now is the amount of training needed to get AI tools up to speed so that they can deliver reputable and safe advice to patients.
Plus, training and distributing AI models nationwide is costly, which can raise the risk of widening existing health disparities.
“Building and deploying AI systems is expensive and time-consuming, so smaller practices and resource-limited settings won’t get AI tools as quickly or broadly,” says Hantel.
AI, as of right now, isn’t immune to biases. Bates brought up a real-life example of an AI scheduling tool for chronic disease patients that predicted Black and Hispanic patients would have higher no-show rates. Based on this data, the algorithm recommended overbooking these groups of people, leading to patients spending an inordinate amount of time sitting in the waiting room even though they had an appointment that day.
And from the patient’s point of view, there are concerns around data privacy. “Increased reliance on digital data and cloud-based AI systems raises concerns about data breaches and confidentiality,” Hantel says.
AI will likely always require humans to monitor its decisions and processes. The hope for this sophisticated technology is that, one day soon, it will elevate patient care, enhance research for drug development, educate physicians and streamline administrative tasks. “However, this needs to be done in a way that is intentionally inclusive so that AI does not worsen pre-existing biases and injustice in how medicine is practiced,” Hantel says.
There may also need to be regulations on how heavily physicians rely on AI, as overdependence could diminish their clinical skills. And Hantel says that checks and balances are also important. This way, AI can’t dehumanize care or use patient and hospital data for profit rather than health as the ultimate goal.
The next few years will be pivotal. If developed and deployed responsibly, AI could transform healthcare into a system that is not only more efficient, but also more compassionate and equitable. The opportunity isn’t just to upgrade medicine—it’s to reimagine it for the better. l
Find hospitals delivering trusted heart and stroke care, guided by the American Heart Association.
For over 100 years, the American Heart Association has driven progress in heart and brain health, so high-quality care is within reach wherever you live. Today, hospitals across the country are putting that science into practice with consistent, research-based care for heart disease and stroke.
These hospitals are part of something bigger: changing the future of health for everyone, everywhere. Their efforts reflect a century of innovation and a relentless push for better health.
The new Commitment to Quality award honors hospitals achieving high performance across three or more Get With The Guidelines® programs – showcasing a system-wide commitment to real-time data, evidence-based care and teamwork across specialties.
See how the American Heart Association measures hospital performance and find trusted care near you.
This content is produced by or on behalf of our sponsor; it is not written by and does not necessarily reflect the view of U.S. News & World Report editorial staff. Learn more at mediakit.usnews.com.

These organizations are sponsors of American Heart Association’s health care quality improvement programs.









Every 34 seconds, someone in America dies of cardiovascular disease. Heart disease and stroke remain the No. 1 and No. 5 leading cause of death, respectively.
Nearly 47% of U.S. adults have high blood pressure, 72% have unhealthy weight and 57% have Type 2 diabetes or prediabetes. More than 2,800 hospitals participate in Get With The Guidelines, a 20-plus year effort to bring research-based, equitable care to heart and stroke patients. Cardiovascular diseases, including heart disease and stroke, claim more lives in the U.S. than all forms of cancer and accidental deaths – the No. 2 and No. 3 causes of death –combined.
To find out more, visit usnewsbrandfuse.com/ AmericanHeartAssociation.


ONew to 2025, the American Heart Association is recognizing hospitals across the country for their dedication to guideline-directed quality care for their stroke and cardiovascular patients. Hospitals with this designation have received silver or higher awards in three or more Get With The Guidelines modules this year.
before first hospital arrival to PCI ≤ 120 minutes for transferred STEMI patients for two or more consecutive, calendar years (Gold Plus) or one calendar year (Silver Plus), in addition to current Gold or Silver Get With The Guidelines – CAD status.
STEMI: Receiving Gold or Silver A C


GET WITH THE GUIDELINES — STROKE, HEART FAILURE, RESUSCITATION, AFIB
Gold Plus Achievement B B
These hospitals are recognized for two or more consecutive calendar years of 85% or higher adherence on all achievement measures and 75% or higher adherence to an additional set of quality measures in heart failure and/or stroke.
Gold Achievement AN A A A
These hospitals are recognized for adherence for two or more consecutive calendar years of 85% or higher adherence on all achievement measures applicable to each program (75% or higher adherence to the identified composite score for rural measures).
Silver Plus Achievement D D
These hospitals are recognized for one calendar year of 85% or higher adherence on all achievement measures and 75% or higher adherence to an additional set of quality measures in heart failure and/or stroke.
Silver Achievement C L C L C C
These hospitals are recognized for one calendar year of 85% or higher adherence on all achievement measures applicable to each program (75% or higher adherence to the identified composite score for rural measures).
GET WITH THE GUIDELINES — CORONARY ARTERY DISEASE
STEMI: Receiving Gold Plus or Silver Plus BD
These hospitals are recognized for compliance to FMC at or
These hospitals are recognized for two or more consecutive, calendar years (Gold) or one calendar year (Silver) of 75% compliance on each performance measure and 50% on arrival to first facility to PCI ≤ 120 minutes for patients transferred for primary PCI.
STEMI: Referring Gold Plus or Silver Plus BD
These hospitals are recognized for compliance to Door In / Door Out in 30 minutes or less for transferred STEMI patients for two or more consecutive, calendar years (Gold Plus) or one calendar year (Silver Plus), in addition to current Gold or Silver Get With The Guidelines – CAD status.
STEMI: Referring Gold or Silver A C
These hospitals are recognized for two or more consecutive, calendar years (Gold) or one calendar year (Silver) of 75% or higher compliance on each performance measure.
Rural Coronary Artery Disease: NSTE_ACS NL and STEMI NL
These hospitals are recognized for one calendar year (Silver) or two calendar years (Gold) of 75% or higher adherence to the identified composite score rural measures.
NSTEMI: Gold or Silver AC
These hospitals are recognized for achieving 65% adherence to Dual Antiplatelet prescription at discharge and 85% or higher compliance on each of the four performance measures for two or more consecutive calendar years (Gold) or one calendar year (Silver).
TARGET: AORTIC STENOSISTM
Target: Aortic Stenosis™ Honor Roll K
These hospitals are recognized for 75% or higher achievement score on percentage of patients with a class I indication for aortic valve replacement who receive definitive treatment (valve replacement) within 90 days of initial diagnosis & 50% or higher achievement score on percentage of echoes with potential severe aortic stenosis who have all necessary evaluation and testing completed to clarify severity and determine whether a Class 1 indication exists.
*These hospitals received Get With The Guidelines®-Resuscitation awards from the American Heart Association for two or more patient populations.
For a searchable map of hospitals by region and across the U.S.,
Medical Center South, Montgomery
Brookwood Baptist Health, Birmingham
Brookwood Medical Center, Birmingham
Coosa Valley Medical Center, Sylacauga
Cullman Regional Medical Center, Cullman
DeKalb Regional Medical Center, Fort Payne
East Alabama Medical Center, Opelika,
Huntsville Hospital, Huntsville
Marshall Medical Centers, Guntersville
Mobile Infirmary, Mobile
North Baldwin Infirmary, Bay Minette
Northeast Alabama Regional Medical Center, Anniston
Riverview Regional Medical Center, Gadsden
Shelby Baptist Medical Center, Alabaster
Southeast Health Medical Center, Dothan
Tanner Medical Center/East Alabama, Wedowee
Thomas Hospital, Fairhope
UAB Medicine Enterprise, Birmingham
Health Providence, Mobile
USA Health University Hospital, Mobile
Whitfield Regional Hospital, Demopolis
Alaska Native Tribal Health Consortium, Anchorage
Bristol Bay Area Health Corporation, Dillingham
Peninsula Hospital, Soldotna
Memorial Hospital, Fairbanks
Scottsdale Campus,
Thunderbird Medical Center, Glendale
Deer Valley Medical Center,
HonorHealth John C. Lincoln Medical Center, Phoenix
HonorHealth Mountain Vista Medical Center, Mesa
HonorHealth Scottsdale Osborn Medical Center, Scottsdale
HonorHealth Scottsdale Shea Medical Center, Phoenix
HonorHealth Scottsdale Thompson Peak Medical Center, Scottsdale
HonorHealth Sonoran Crossing Medical Center, Phoenix
Mayo Clinic Arizona, Phoenix
St. Joseph’s Hospital and Medical Center, Phoenix
Summit Healthcare Association, Show Low
Tempe St. Luke’s Hospital, Tempe
Tucson Medical Center, Tucson
Valleywise Health Medical Center, Phoenix
Verde Valley Medical/Northern Arizona Healthcare, Cottonwood
Yuma Regional Medical Center, Yuma
Arkansas Methodist Medical Center, Paragould
Ashley County Medical Center, Crossett
Baptist Health Medical Center - Arkadelphia, Arkadelphia
Baptist Health Medical Center - Conway, Conway
Baptist Health Medical Center - Hot Spring County, Malvern
Baptist Health Medical Center - Little Rock, Little Rock
Baptist Health Medical Center-North Little Rock, Little Rock
Baptist Health-Fort Smith, Fort Smith
Baptist Memorial Hospital Crittenden, West Memphis
BAXTER HEALTH, Mountain Home
Bradley County Medical Center, Warren
CHI St. Vincent Hot Springs, Hot Springs
CHI St. Vincent Infirmary, Little Rock
CHI St. Vincent Medical Center North, Sherwood
CHI St. Vincent Morrilton, Morrilton
Chicot Memorial Medical Center, Lake Village
Conway Regional Medical Center, Conway
CrossRidge Community Hospital, Wynne
Dallas County Medical Center, Fordyce
Dardanelle Regional Medical Center, Dardanelle
Delta Memorial Hospital, Dumas
Fulton County Hospital, Salem
Great River Medical Center, Blytheville
Izard Regional Hospital, Calico Rock
Johnson Regional Medical Center, Clarksville
Lawrence Memorial Hospital, Walnut Ridge
Mena Regional Health System, Mena
Mercy Hospital Booneville, Booneville
Mercy Hospital Fort Smith, Fort Smith
Mercy Hospital Northwest Arkansas, Rogers
Mercy Hospital Paris, Paris
Mercy Hospital Waldron, Waldron
NEA Baptist Memorial Hospital, Jonesboro
North Arkansas Regional Medical Center, Harrison
Ozarks Community Hospital, Gravette
Piggott Community Hospital, Piggott
Saint Mary’s Regional Medical Center, Russellville
Siloam Springs Regional Hospital, Siloam Springs
South Arkansas Regional Hospital, El Dorado
South Mississippi County Regional Medical Center, Osceola N
St. Bernards Five Rivers Medical Center, Pocahontas
St. Bernards Medical Center, Jonesboro
Stone County Medical Center, Mountain View
UAMS Medical Center, Little Rock
Wadley Regional Medical Center at Hope, Hope
Washington Regional Medical Center, Fayetteville
White River Health System, Batesville
White River Medical Complex ER, Cherokee Village
Adventist Health - Glendale, Glendale
Adventist Health and Rideout, Marysville
Adventist Health Bakersfield, Bakersfield
Adventist Health Hanford, Hanford
Adventist Health Howard Memorial, Willits
Adventist Health Lodi Memorial, Lodi
Adventist Health Sierra Vista, San Luis Obispo
Adventist Health Simi Valley, Simi Valley
Adventist Health St. Helena, St Helena
Adventist Health Tulare, Tulare
Adventist Health Ukiah Valley, Ukiah
Adventist Health White Memorial Montebello, Montebello
Adventist Health White Memorial, Los Angeles
Alameda Hospital, Alameda
Alta Bates Summit Medical Center | Summit Campus, Oakland
Antelope Valley Medical Center, Lancaster
Arrowhead Regional Medical Center, Colton
Bear Valley Community Healthcare District, Big Bear Lake
California Hospital Medical Center, Los Angeles
California Pacific Medical Center | Davies & Van Ness Campuses, San Francisco
Cedars-Sinai Medical Center, Los Angeles
Centinela Hospital Medical Center, Inglewood
Chinese Hospital, San Francisco
Chino Valley Medical Center, Chino
CHOC Children’s Hospital, Orange
Clovis Community Medical Center, Clovis
Community Hospital of the Monterey Peninsula, Monterey
Community Memorial Hospital, Ventura
Community Regional Medical Center, Fresno
Corona Regional Medical Center, Corona
Dameron Hospital, Stockton
Desert Regional Medical Center, Palm Springs
Desert Valley Hospital, Victorville
Dignity Health - Glendale Memorial Hospital and Health Center, Glendale
Dignity Health Bakersfield Memorial Hospital, Bakersfield
Dignity Health Dominican Hospital, Santa Cruz
Dignity Health French Hospital Medical Center, San Luis Obispo
Dignity Health Marian Regional Medical Center, Santa Maria
Dignity Health Mercy Hospital of Folsom, Folsom
Dignity Health Mercy Hospitals of Bakersfield, Bakersfield
Dignity Health Mercy Medical Center Merced, Merced
GWTG – CAD
STEMI REFERRING:
B Gold Plus Referring
A Gold Referring
D Silver Plus Referring
C Silver Referring
GWTG – RURAL CAD: NSTE_ACS N Gold Achievement L Silver Achievement
GWTG – RURAL CAD: STEMI
N Gold Achievement
L Silver Achievement
Dignity Health Mercy Medical Center Redding, Redding C B
Dignity Health Northridge Hospital Medical Center, Northridge B
Dignity Health Sequoia Hospital, Redwood City B
Dignity Health Sierra Nevada Memorial Hospital, Grass Valley BN
Dignity Health St. John’s Hospital Camarillo, Camarillo B
Dignity Health St. John’s Regional Medical Center, Oxnard B
Dignity Health St Joseph’s Medical Center, Stockton D B
Dignity Health, Mercy Mt. Shasta, Mount Shasta ND
Doctors Hospital of Manteca, Manteca B
Doctors Medical Center Modesto, Modesto B
Eden Medical Center, Castro Valley B
Eisenhower Health, Rancho Mirage B K
El Camino Health, Mountain View and Los Gatos, Mountain View B
Emanate Health-Queen of the Valley Hospital, West Covina B
Emanuel Medical Center, Turlock C D
Encino Hospital Medical Center, Encino B
Enloe Medical Center, Chico B B
Fairchild Medical Center, Yreka ND
Garden Grove Hospital Medical Center, Garden Grove B B
Garfield Medical Center, Monterey Park B
Good Samaritan Hospital, San Jose B
Healdsburg Hospital, Healdsburg N
Hemet Global Medical Center, Hemet A
Henry Mayo Newhall Hospital, Valencia B
Hi Desert Medical Center, Joshua Tree N
Hoag Hospital Irvine, Irvine B
Hoag Memorial Hospital Presbyterian, Newport Beach B B
Huntington Beach Hospital, Huntington Beach B
Hospital, Pasadena B JFK Memorial Hospital, Indio
John Muir Medical Center - Concord, Concord
John Muir Medical Center - Walnut Creek, Walnut Creek O A B B
Kaiser Foundation Hospital - Antioch, Antioch B
Kaiser Foundation Hospital - Baldwin Park, Baldwin Park B
Kaiser Foundation Hospital - Downey, Downey B
Kaiser Foundation Hospital - Fontana, Fontana B
Kaiser Foundation Hospital - Fremont, Fremont
Kaiser Foundation Hospital - Fresno, Fresno
Kaiser Foundation Hospital - Los Angeles, Los Angeles
Kaiser Foundation Hospital - Manteca, Manteca
Kaiser Foundation Hospital - Modesto, Modesto
Kaiser Foundation Hospital - Moreno Valley, Moreno Valley
Kaiser Foundation Hospital - Oakland, Oakland
Kaiser Foundation Hospital - Ontario, Ontario B
Kaiser Foundation Hospital - Orange CountyAnaheim and Irvine, Anaheim B
Kaiser Foundation Hospital - Panorama City, Panorama City B
Kaiser Foundation Hospital - Redwood City, Redwood City B
Kaiser Foundation Hospital - Richmond, Richmond
Kaiser Foundation Hospital - Riverside, Riverside B
Kaiser Foundation Hospital - Roseville, Roseville D B
Kaiser Foundation Hospital - Sacramento, Sacramento
Kaiser Foundation Hospital - San Diego, San Diego
Kaiser Foundation Hospital - San Francisco, San Francisco
Kaiser Foundation Hospital - San Jose, San Jose
Kaiser Foundation Hospital - San Leandro, San Leandro B
Kaiser Foundation Hospital - San Marcos, San Marcos D
Kaiser Foundation Hospital - San Rafael, San Rafael
Kaiser Foundation Hospital - Santa Clara, Santa Clara
GWTG – CAD NSTEMI: A Gold C Silver
TARGET: AORTIC STENOSIS : K Target: Aortic StenosisTM Honor Roll
* These hospitals received Get With The Guidelines®-Resuscitation awards from the American Heart Association for two or more patient populations. O Hospitals with this designation have received silver or higher awards in three or more Get With The Guidelines modules this year.
Kaiser Foundation Hospital - Santa Rosa, Santa Rosa
Kaiser Foundation Hospital - South Bay, Harbor City
Kaiser Foundation Hospital - South Sacramento, Sacramento
Kaiser Foundation Hospital - South San Francisco, South San Francisco
Kaiser Foundation Hospital - Vacaville, Vacaville
Kaiser Foundation Hospital - Vallejo, Vallejo
Kaiser Foundation Hospital - Walnut Creek, Walnut Creek
Kaiser Foundation Hospital - West Los Angeles, Los Angeles
Kaiser Foundation Hospital - Woodland Hills, Woodland Hills
Kaiser Foundation Hospital - Zion, San Diego
Kaweah Delta Health Care District, Visalia
Keck Hospital of USC, Los Angeles
Kern County Hospital Authority, Bakersfield
La Palma Intercommunity Hospital, La Palma
Loma Linda University Children’s Hospital, Loma Linda
Loma Linda University Medical Center Murrieta, Murrieta
Loma Linda University Medical Center, Loma Linda
Lompoc Valley Medical Center, Lompoc
Long Beach Medical Center, Long Beach
Los Angeles General Medical Center, Los Angeles
Los Robles Regional Medical Center, Thousand Oaks
MarinHealth Medical Center, Greenbrae
Orange
PIH
PIH
Providence Cedars Sinai Tarzana Medical Center, Tarzana
Providence Holy Cross Medical Center, Mission Hills
Providence Little Company of Mary Medical Center - San Pedro, San Pedro
Providence Little Company of Mary Medical Center - Torrance, Torrance
Providence Petaluma Valley Hospital, Petaluma
Providence Saint John’s Health Center, Santa Monica
Providence Saint Joseph Medical Center, Burbank
Providence Santa Rosa Memorial Hospital, Santa Rosa
Providence St. Mary Medical Center, Apple Valley
GWTG – STROKE:
Gold Plus Achievement
Silver Plus Achievement
GWTG – RURAL STROKE :
Achievement
Silver Achievement
Queen of the Valley Medical Center, Napa
Redlands Community Hospital, Redlands
Regional Medical Center of San Jose, San Jose
Riverside Community Hospital, Riverside B
Riverside University Health System-Medical Center, Moreno Valley
Ronald Reagan UCLA Medical Center, Los Angeles
Saddleback Memorial Medical Center, Laguna Hills
Saint Agnes Medical Center, Fresno
Salinas Valley Health Medical Center, Salinas
San Antonio Regional Hospital, Upland
San Dimas Community Hospital, San Dimas B
San Gorgonio Memorial Hospital, Banning D
San Joaquin General Hospital, French Camp B
San Ramon Regional Medical Center, San Ramon
Santa Barbara Cottage Hospital, Santa Barbara B
Santa Clara Valley Medical Center, San Jose B
Santa Monica-UCLA Medical Center Orthopedic and Hospital, Santa Monica
Santa Ynez Valley Cottage Hospital, Solvang
Scripps Green Hospital, La Jolla
Scripps Memorial Hospital Encinitas, Encinitas
Scripps Memorial Hospital La Jolla, La Jolla B
Scripps Mercy Hospital Chula Vista, Chula Vista B
Scripps Mercy Hospital San Diego, San Diego B
Sharp Chula Vista Medical Center, Chula Vista B
Sharp Coronado Hospital, Coronado B
Sharp Grossmont Hospital, La Mesa
Sharp Memorial Hospital, San Diego
Shasta Regional Medical Center, Redding B B
Sherman Oaks Hospital, Sherman Oaks
Sierra View Medical Center, Porterville
Sonoma Valley Hospital, Sonoma
Southwest Healthcare System-Inland Valley Medical Center and Rancho Springs Medical Center, Wildomar B
St. Bernardine Medical Center, San Bernardino
St. Elizabeth’s Community Hospital, Red Bluff
St. Francis Medical Center, Lynwood
St. Joseph Hospital, Eureka, Eureka
St. Joseph Hospital, Orange
St. Jude Medical Center, Fullerton
St. Louise Regional Hospital, Gilroy
St. Mary Medical Center, Long Beach
Stanford Health Care, Stanford
Stanford Health Care Tri-Valley, Pleasanton
Stanford Medicine Childrens Health, Palo Alto
Sutter Amador Hospital, Jackson
Sutter Auburn Faith Hospital, Auburn
Sutter Davis Hospital, Davis
Sutter Delta Medical Center, Antioch
Sutter Lakeside Hospital, Lakeport
Sutter Medical Center, Sacramento, Sacramento
Sutter Roseville Medical Center, Roseville
Sutter Santa Rosa Regional Hospital, Santa Rosa
Sutter Solano Medical Center, Vallejo
Sutter Tracy Community Hospital, Tracy
Tahoe Forest Hospital, Truckee
Temecula Valley Hospital, Temecula
Torrance Memorial Medical Center, Torrance
GWTG – HEART FAILURE:
Gold Plus Achievement
Gold Achievement
Silver Plus Achievement
Silver Achievement
GWTG – RURAL HEART FAILURE:
Silver Achievement
GWTG – RESUSCITATION :
Gold Achievement
Silver Achievement
GWTG – AFIB:
Gold Achievement
Silver Achievement
GWTG – CAD STEMI RECEIVING:
Tri-City Medical Center, Oceanside
Twin Cities Community Hospital, Templeton
UC San Diego Health - East Campus, San Diego
UC San Diego Health, San Diego
UCI Health - Lakewood, Lakewood
UCI Health Fountain Valley, Fountain Valley
UCI Health-Los Alamitos, Los Alamitos
UCI Medical Center, Orange
UCLA West Valley Medical Center, West Hills
UCSF Health Saint Francis Hospital, San Francisco
UCSF Health St. Mary’s Hospital, San Francisco
University of California San Francisco (UCSF), San Francisco
University of California, Davis Medical Center, Sacramento
USC Arcadia Hospital, Arcadia
USC Norris Comprehensive Cancer Center, Los Angeles
VA Loma Linda Hospital, Loma Linda
Valley Presbyterian Hospital, Van Nuys
Ventura County Medical Center/Santa Paula Hospital, Ventura
Washington Health, Fremont
West Anaheim Medical Center, Anaheim
Wilma Chan Highland Hospital Campus, Oakland
Woodland Memorial Hospital, Woodland
CommonSpirit St. Anthony Hospital, Lakewood
CommonSpirit St. Anthony North Hospital, Westminster
CommonSpirit St. Francis Hospital, Colorado Springs
Gunnison Valley Health, Gunnison
HCA HealthONE Aurora, Aurora
HCA HealthONE Mountain Ridge, Thornton
HCA HealthONE Rose, Denver
HCA HealthONE Swedish Medical Center, Englewood
Intermountain Health Good Samaritan Hospital, Lafayette
Intermountain Health - Lutheran Hospital, Wheat Ridge
Intermountain Health Platte Valley Hospital, Brighton
Intermountain Health St. Mary’s Regional Hospital, Grand Junction
North Colorado Medical Center, Greeley
Parkview Medical Center, Pueblo
Saint Joseph Hospital, Denver
Sky Ridge Medical Center, Lone Tree
UCHealth Greeley Hospital, Greeley
UCHealth Highlands Ranch Hospital, Highlands
UCHealth Longs Peak Hospital, Longmont
UCHealth
UCHealth
UCHealth Memorial Hospital North, Colorado Springs
UCHealth Pikes Peak Regional Hospital, Woodland Park
UCHealth Poudre Valley Hospital, Fort Collins
UCHealth University of Colorado Hospital, Aurora
GWTG – CAD
STEMI REFERRING:
B Gold Plus Referring
A Gold Referring
D Silver Plus Referring
C Silver Referring
GWTG – RURAL CAD: NSTE_ACS
N Gold Achievement
L Silver Achievement
GWTG – RURAL CAD: STEMI
N Gold Achievement
L Silver Achievement
Bridgeport Hospital, Bridgeport
Charlotte Hungerford Hospital, Torrington
Connecticut Children’s Medical Center, Hartford
Danbury Hospital, part of Nuvance Health, Danbury
Day Kimball Hospital, Putnam
Greenwich Hospital, Greenwich
Griffin Hospital, Derby
Hartford Hospital, Hartford
Lawrence + Memorial Hospital, New London
Manchester Memorial Hospital, Manchester
Middlesex Hospital, Middletown
Midstate Medical Center, Meriden
Norwalk Hospital part of Nuvance Health, Norwalk
Saint Francis Hospital and Medical Center, Hartford
Sharon Hospital, Sharon
St. Vincent’s Medical Center, Bridgeport
Stamford Hospital, Stamford
The Hospital of Central Connecticut, New Britain
UCONN Health / John Dempsey Hospital, Farmington
Waterbury Hospital, Waterbury
William W. Backus Hospital, Norwich
Hospital, Windham
Bayhealth Medical Center - Kent General Hospital, Dover
Bayhealth Sussex Campus, Milford
Healthcare, Lewes
Newark
Hospital - Wilmington, Wilmington
Nanticoke, Seaford
Howard University Hospital, Washington
Georgetown University Hospital,
Advent Health Heart of Florida, Davenport
Altamonte Springs, Altamonte Springs
Apopka, Apopka
AdventHealth Carrollwood, Tampa
AdventHealth Celebration, Celebration
AdventHealth Dade City, Dade City
AdventHealth Daytona Beach, Daytona Beach
AdventHealth DeLand, DeLand
AdventHealth East Orlando, Orlando
AdventHealth Fish Memorial, Orange City
AdventHealth Kissimmee, Kissimmee
AdventHealth New Smyrna Beach, New Smyrna Beach
AdventHealth North Pinellas, Tarpon Springs
AdventHealth Ocala, Ocala
AdventHealth Orlando, Orlando
GWTG – CAD NSTEMI: A Gold C Silver
TARGET: AORTIC STENOSIS : K Target: Aortic StenosisTM Honor Roll
* These hospitals received Get With The Guidelines®-Resuscitation awards from the American Heart Association for two or more patient populations. O Hospitals with this designation have received silver or higher awards in three or more Get With The Guidelines modules this year.
AdventHealth Palm Coast Parkway, Palm Coast
AdventHealth Palm Coast, Palm Coast
AdventHealth Sebring, Sebring
AdventHealth Tampa, Tampa
AdventHealth Waterman, Tavares
AdventHealth Wesley Chapel, Wesley Chapel
AdventHealth Winter Garden, Winter Garden
AdventHealth Winter Park, Winter Park
AdventHealth Zephyrhills, Zephyrhills
Ascension St. Vincent’s St. Johns County, St Johns
Baptist Hospital of Miami, Miami
Baptist Hospital, Pensacola
Baptist Medical Center - Beaches (Baptist Health), Jacksonville Beach
Baptist Medical Center - Jacksonville (Baptist Health), Jacksonville
Baptist Medical Center - South (Baptist Health), Jacksonville
Baptist Medical Center Clay, Fleming Island
Baptist Medical Center Nassau, Fernandina Beach
Bartow Regional Medical Center, Bartow
BayCare Wesley Chapel, Wesley Chapel
Bayfront
Bethesda Hospital East, Boynton Beach
Bethesda Hospital West, Boynton Beach
Boca Raton Regional Hospital, Boca Raton
Broward Health Coral Springs, Coral Springs
Broward
Cleveland Clinic
Good Samaritan Medical Center, West Palm
Gulf Breeze Hospital, Gulf Breeze
Gulf Coast Medical Center, Fort Myers
Halifax Health - UF Health Medical Center of Deltona, Deltona
Halifax Health Medical Center of Daytona Beach, Daytona Beach
Halifax Health Medical Center of Port Orange, Port Orange
HCA FL Orange Park Hospital, Orange Park
HCA Florida Bayonet Point Hospital, Hudson
HCA Florida Blake Hospital, Bradenton
HCA Florida Brandon Hospital, Brandon
HCA Florida Citrus Hospital, Inverness
HCA Florida Englewood Hospital, Englewood
HCA Florida Fawcett Hospital, Port Charlotte
HCA Florida Fort Walton-Destin Hospital, Fort Walton
HCA Florida JFK North
GWTG – STROKE: B Gold Plus Achievement A Gold Achievement D Silver Plus Achievement C Silver Achievement
GWTG – RURAL STROKE :
Gold Achievement
Silver Achievement
HCA Florida Kendall Hospital, Miami
HCA Florida Lake Monroe Hospital, Sanford
HCA Florida Largo Hospital, Largo
HCA Florida Lawnwood Hospital, Fort Pierce
HCA Florida Memorial Hospital, Jacksonville
HCA Florida North Florida Hospital, Gainesville
HCA Florida Northside Hospital, St. Petersburg
HCA Florida Northwest Hospital, Margate
HCA Florida Oak Hill Hospital, Brooksville
HCA Florida Ocala Hospital, Ocala
HCA Florida Osceola Hospital, Kissimmee
HCA Florida Palms West Hospital, Loxahatchee B
HCA Florida Pasadena Hospital, South Pasadena D
HCA Florida Raulerson Hospital, Okeechobee N
HCA Florida Sarasota Doctors Hospital, Sarasota B
HCA Florida South Shore Hospital, Sun City Center B
HCA Florida South Tampa Hospital, Tampa B
HCA Florida St. Lucie Hospital, Port Saint Lucie B
HCA Florida St. Petersburg Hospital, Saint Petersburg B
HCA Florida Trinity Hospital, Trinity B
HCA Florida West Hospital, Pensacola B
HCA Florida West Marion Hospital, A part of HCA Florida Ocala Hospital, Ocala B
HCA Florida Westside Hospital, Plantation B
Hendry Regional Medical Center, Clewiston L L
Hialeah Hospital Primary Stroke, Hialeah
Holmes Regional Medical Center, Melbourne
Holy Cross Hospital, Fort Lauderdale
Homestead Hospital, Homestead
HSA PGH, LLC, Hialeah
Jackson Memorial Hospital, Miami
Jackson North Medical Center, North Miami Beach
Jackson South Medical Center, Miami
Johns Hopkins All Children’s Hospital, St. Petersburg
Jupiter Medical Center, Jupiter
Lakeland Regional Health Medical Center, Lakeland
Lakewood Ranch Medical Center, Bradenton
Lee Memorial Hospital, Fort Myers
Lower Keys Medical Center, Key West
Memorial Hospital, Bradenton
Mariners Hospital, Tavernier
Clinic Florida, Jacksonville
Mease Countryside Hospital, Safety Harbor
Mease Dunedin Hospital, Dunedin
Memorial Hospital Miramar, Miramar
Memorial Hospital Pembroke, Pembroke Pines
Memorial Hospital West, Pembroke Pines
Memorial Regional Hospital, Hollywood
Morton Plant Hospital, Clearwater
Morton Plant North Bay Hospital, New Port Richey
Mount Sinai Medical Center, Miami Beach
NCH Healthcare System, Naples
NCH North Naples Hospital, Naples
Nicklaus Children’s Hospital, Miami
Orlando Health - Dr. P. Phillips Hospital, Orlando
Orlando Health - Orlando Regional Medical Center, Orlando
Orlando Health - South Lake Hospital, Clermont
Orlando Health Arnold Palmer Hospital for Children, Orlando
Orlando Health Horizon West Hospital, Winter Garden
GWTG – HEART FAILURE: B Gold Plus Achievement
Gold Achievement D Silver Plus Achievement C Silver Achievement
GWTG – RURAL HEART FAILURE: L Silver Achievement
GWTG – RESUSCITATION : A Gold Achievement C Silver Achievement
GWTG – AFIB: A Gold Achievement C Silver Achievement
GWTG – CAD STEMI RECEIVING: B Gold Plus Receiving A Gold Receiving D Silver Plus Receiving
C Silver Receiving
Orlando Health Inc. - Health Central Hospital, Ocoee
Orlando Health St. Cloud Hospital, Saint Cloud
Oviedo Medical Center, Oviedo
Palm Bay Hospital, Palm Bay
Palm Beach Gardens Medical Center, Palm Beach Gardens
Physicians Regional Healthcare System, Naples
Physicians Regional Medical Center - Collier Boulevard, Naples
Sacred Heart Bay, Panama City
Sacred Heart Health System, Pensacola
Santa Rosa Medical Center, Milton
Sarasota Memorial Health Care System, Sarasota
Sarasota Memorial Hospital - Venice, North Venice
South Miami Hospital, South Miami
St. Anthony’s Hospital, St. Petersburg
St. Joseph’s Hospital - South, Riverview
St. Joseph’s Hospital, Tampa
St. Marys Medical Center, West Palm Beach
St. Vincent’s Medical Center-Clay County, Middleburg
St. Vincent’s Medical Center, Jacksonville
Steward Florida Medical Center, Fort Lauderdale
Tallahassee Memorial HealthCare, Tallahassee
Tampa General Hospital, Tampa
UF Health Flagler Hospital, Saint Augustine
UF Health Jacksonville, Jacksonville
UF Health Leesburg Hospital, Leesburg
UF Health Shands Hospital, Gainesville
UF Health Spanish Plains Hospital, The Villages
University of Miami Health System, Miami
Viera Hospital, Viera
Wellington Regional Medical Center, Wellington
Boca Medical Center, Boca Raton
Kendall Baptist Hospital, Miami
Haven Hospital, Winter Haven
Gordon, Calhoun
Atrium Health Navicent Baldwin, Milledgeville
Atrium Health Navicent The Medical Center, Macon
Candler Hospital, Savannah
Coffee Regional Medical Center, Douglas
Colquitt Regional Medical Center, Moultrie
Crisp Regional Health Services, Cordele
Doctors Hospital Augusta, Augusta
Effingham Health System, Springfield
Emory Decatur Hospital, Decatur
Emory Hillandale, Lithonia
Emory Johns Creek Hospital, Duluth
Emory Saint Joseph’s Hospital, Atlanta
Emory University Hospital Midtown, Atlanta
Emory University Hospital, Atlanta
Grady Health System, Atlanta
Hamilton Medical Center, Dalton
Houston Healthcare - Warner Robins, Warner Robins
John D. Archbold Memorial Hospital, Thomasville
GWTG – CAD
STEMI REFERRING:
B Gold Plus Referring
A Gold Referring
D Silver Plus Referring
C Silver Referring
GWTG – RURAL CAD: NSTE_ACS
N Gold Achievement
L Silver Achievement
GWTG – RURAL CAD: STEMI
N Gold Achievement
L Silver Achievement
Memorial University Medical Center, Savannah
Morgan Medical Center, Madison
Northeast Georgia Medical Center- Habersham, Demorest
Northeast Georgia Medical Center, Barrow, Winder
Northeast Georgia Medical Center, Braselton, Braselton
Northeast Georgia Medical Center, Lumpkin, Dahlonega
Northeast Georgia Medical Center, Gainesville
Northside Hospital Atlanta, Atlanta
Northside Hospital Cherokee, Canton
Northside Hospital Duluth, Duluth
Northside Hospital Forsyth, Cumming
Northside Hospital Gwinnett, Lawrenceville
Phoebe Putney Memorial Hospital, Albany
Phoebe Sumter Medical Center, Americus
Phoebe Worth Medical Center, Sylvester
Piedmont Athens Regional Medical Center, Athens
Piedmont Augusta Hospital, Augusta
Piedmont Cartersville Medical Center, Cartersville
Piedmont Columbus Midtown, Columbus
Piedmont Columbus Northside, Columbus
Piedmont Eastside Medical Center, Snellville
Piedmont Fayette Hospital, Fayetteville
Piedmont Henry Hospital, Stockbridge
Piedmont Hospital, Atlanta
Piedmont Macon Medical Center, Macon
Piedmont Mountainside Hospital, Jasper
Piedmont Newnan Hospital, Newnan
Piedmont Newton Hospital, Covington
Piedmont North Hospital, Macon
Piedmont Rockdale Hospital, Conyers
Piedmont Walton Hospital, Monroe
SGMC Health, Valdosta
Southeast Georgia Health System, Brunswick
Southern Regional Medical Center, Riverdale
St. Francis - Emory Healthcare, Columbus
St. Joseph’s Hospital, Savannah
St. Mary’s Good Samaritan Hospital, Greensboro
St. Mary’s Hospital, Athens
St. Mary’s Sacred Heart Hospital, Lavonia
Stephens County Hospital, Toccoa
Tanner Medical Center/Carrollton, Carrollton
Tanner Medical Center/Villa Rica, Villa Rica
Tift Regional Medical Center, Tifton
Union General Hospital, Blairsville
Upson Regional Medical Center, Thomaston
Wellstar Cobb Hospital, Austell
Wellstar Douglas Hospital, Douglasville
WellStar Kennestone Regional Hospital, Marietta
Wellstar MCG Health, Augusta
WellStar North Fulton Hospital, Roswell
WellStar Paulding Hospital, Hiram
WellStar Spalding Regional Hospital, Griffin
WellStar West Georgia Medical Center, LaGrange
Guam Memorial Hospital, Tamuning
Guam Regional Medical City, Dededo
GWTG – CAD NSTEMI: A Gold C Silver
TARGET: AORTIC STENOSIS : K Target: Aortic StenosisTM Honor Roll
* These hospitals received Get With The Guidelines®-Resuscitation awards from the American Heart Association for two or more patient populations. O Hospitals with this designation have received silver or higher awards in three or more Get With The Guidelines modules this year.
Adventist Health Castle, Kailua
Hilo Medical Center, Hilo
Kaiser Foundation Hospital - Moanalua, Honolulu
Kona Community Hospital, Kealakekua
Kuakini Medical Center, Honolulu
Maui Memorial Medical Center, Wailuku
North Hawaii Community Hospital, Kamuela
Pali Momi Medical Center, Aiea
Samuel Mahelona Memorial Hospital, Kapaa
Straub Benioff Medical Center, Honolulu
The Queen’s Medical Center Punchbowl, Honolulu
The Queen’s Medical Center West O’ahu, Ewa Beach
Wilcox Medical Center, Lihue
Eastern Idaho Regional Medical Center, Idaho Falls
Portneuf Medical Center, Pocatello
Saint Alphonsus Regional Medical Center, Boise
Advocate Christ Medical Center, Oak Lawn
Advocate Condell Medical Center, Libertyville
Advocate Good Samaritan Hospital, Downers Grove
Advocate Good Shepherd Hospital, Barrington
Advocate Illinois Masonic Medical Center, Chicago
Advocate Lutheran General Hospital, Park Ridge
Advocate Sherman Hospital, Elgin
Advocate South Suburban Hospital, Hazel Crest
Advocate Trinity Hospital, Chicago
Alton Memorial Hospital - BJC Healthcare, Alton
Ascension Alexian Brothers, Elk Grove Village
Ascension Saint Alexius, Hoffman Estates
Ascension Saint Joseph Chicago, Chicago
Blessing Hospital, Quincy
Carle BroMenn Medical Center, Normal
Carle Eureka Hospital, Eureka
Carle Foundation Hospital, Urbana
Carle Health Methodist Hospital, Peoria
Cook County Health, Chicago
Decatur Memorial Hospital, Decatur
Endeavor Health Edward Hospital, Naperville
Endeavor Health Elmhurst Hospital, Elmhurst
Endeavor Health Evanston Hospital, Evanston
Endeavor Health Glenbrook Hospital, Glenview
Endeavor Health Highland Park Hospital, Highland Park
Endeavor Health Northwest Community Hospital, Arlington
Endeavor Health Swedish Hospital, Chicago
Fairfield Memorial Hospital, Fairfield
FHN Memorial Hospital, Freeport
Franciscan Health Olympia Fields, Olympia Fields
Gibson Area Hospital and Health Services, Gibson City
Hamilton Memorial Hospital, McLeansboro
Herrin Hospital, Herrin
Hillsboro Area Hospital, Hillsboro
Horizon Health, Paris
Humboldt Park Health, Chicago
GWTG – STROKE:
B Gold Plus Achievement
A Gold Achievement
D Silver Plus Achievement
C Silver Achievement
GWTG – RURAL STROKE :
N Gold Achievement
L Silver Achievement
Insight Hospital & Medical Center, Chicago
Javon Bea Hospital – Riverside, Rockford
John and Mary E. Kirby Hospital, Monticello
Loyola University Medical Center, Maywood
MacNeal Hospital, Berwyn
Marshall Browning Hospital, Du Quoin
Mason District Hospital, Havana
Memorial Hospital of Carbondale, Carbondale
Memorial Hospital, Carthage
Mercy Harvard Hospital, Harvard
Mount Sinai Hospital, Chicago
Northwestern Medicine Central DuPage Hospital, Winfield
Northwestern Medicine Delnor Hospital, Geneva
Northwestern Medicine Huntley Hospital, Huntley
Northwestern Medicine Kishwaukee Hospital, Dekalb
Northwestern Medicine Lake Forest Hospital, Lake Forest
Northwestern Medicine McHenry Hospital, McHenry
Northwestern Medicine Palos Hospital, Palos Heights
Northwestern Memorial Hospital, Chicago
OSF HealthCare Little Company of Mary Medical Center, Evergreen Park
OSF HealthCare Saint Anthony’s Health Center, Alton B
OSF Saint Anthony Medical Center, Rockford
OSF Saint Francis Medical Center, Peoria
OSF St. Joseph Medical Center, Bloomington
Red Bud Regional Hospital, Red Bud
Medical Center, Chicago B
Riverside Medical Center, Kankakee B
Rush Copley Medical Center, Aurora
Rush Oak Park Hospital, Oak Park
Rush University Medical Center, Chicago
Saint Joseph Hospital - Elgin, Elgin
Saint Joseph Medical Center- Joliet, Joliet
Saint Mary of Nazareth Hospital, Chicago
Sarah Bush Lincoln Fayette County Hospital, Vandalia
Sarah Bush Lincoln Health Center, Mattoon
Silver Cross Hospital, New Lenox
Springfield Memorial Hospital, Springfield
SSM Health Good Samaritan, Mount Vernon
St. Joseph Memorial Hospital, Murphysboro
UChicago Medicine AdventHealth Bolingbrook, Bolingbrook
UChicago Medicine AdventHealth GlenOaks, Glendale Heights
UChicago Medicine AdventHealth Hinsdale, Hinsdale
UChicago Medicine AdventHealth La Grange, La Grange
UChicago Medicine, Chicago
UI Health, Chicago
Wabash General Hospital, Mount Carmel
Ascension St. Vincent Anderson, Anderson
Ascension St. Vincent Hospital, Indianapolis
Baptist Health Floyd, New Albany
Columbus Regional Hospital, Columbus
Community Heart and Vascular, Indianapolis
Community Hospital - North, Indianapolis
Community Hospital East, Indianapolis
Community Hospital of Anderson, Anderson
Community Hospital, Community Healthcare System, Munster
GWTG – HEART FAILURE:
B Gold Plus Achievement
A Gold Achievement
D Silver Plus Achievement
C Silver Achievement
GWTG – RURAL HEART FAILURE:
L Silver Achievement
GWTG – RESUSCITATION : A Gold Achievement
C Silver Achievement
GWTG – AFIB: A Gold Achievement C Silver Achievement
GWTG – CAD STEMI RECEIVING:
B Gold Plus Receiving
A Gold Receiving
D Silver Plus Receiving
C Silver Receiving
Community Howard Regional Hospital, Kokomo
Community South, Indianapolis
Deaconess Gateway Hospital, Newburgh
Deaconess Gibson Hospital, Princeton
Deaconess Hospital, Evansville
Elkhart General Hospital, Elkhart
Eskenazi Health, Indianapolis
Franciscan Health - Crown Point, Crown Point
Franciscan Health Indianapolis, Indianapolis
Franciscan Health Lafayette East, Lafayette
Franciscan Health Michigan City, Michigan City
Good Samaritan Hospital, Vincennes
Indiana University Health Arnett, Lafayette
Indiana University Health Ball Memorial Hospital, Muncie
Indiana University Health Bedford Hospital, Bedford
Indiana University Health Bloomington Hospital, Bloomington
Indiana University Health Frankfort Hospital, Frankfort
Indiana University Health Jay Hospital, Portland
Indiana University Health Methodist Hospital, Indianapolis
Indiana University Health Morgan Hospital, Martinsville
Indiana University Health North Hospital, Carmel
Indiana University Health West Hospital, Avon
Indiana University Health White Hospital, Monticello
Lutheran Hospital, Fort Wayne
Memorial Hospital and Health Care Center, Jasper
Memorial Hospital, South Bend
Methodist Hospitals, Inc., Gary
Parkview Kosciusko Hospital, Warsaw
Parkview Randallia Hospital, Fort Wayne
Parkview Regional Medical Center, Fort Wayne
Parkview Whitley Hospital, Columbia City
Reid Health Connersville, Connersville
Reid Health, Richmond
Riley Hospital for Children at Indiana University Health, Indianapolis
St. Catherine Hospital, Inc., East Chicago
St. Mary Medical Center, Hobart
Terre Haute Regional Hospital, Terre Haute
Union Hospital - Clinton, Clinton
Union Hospital, Terre Haute
Adair County Health System, Greenfield
Cass Health, Atlantic
CHI Health Mercy Hospital Council Bluffs, Council Bluffs
CHI-Iowa Corp d/b/a MercyOne Des Moines Medical Center, Des Moines
Clarinda Regional Health Center, Clarinda
Davis County Hospital and Clinics, Bloomfield
Genesis Health System- Davenport, Davenport
Greater Regional Health, Creston
Hancock County Memorial Hospital, Britt
Hegg Health Center, Rock Valley
Henry County Health Center, Mount Pleasant
Iowa Specialty Hospital Belmond, Belmond
Iowa Specialty Hospital Clarion, Clarion
Jackson County Regional Health Center, Maquoketa
Keokuk County Hospital and Clinics, Sigourney
GWTG – CAD
STEMI REFERRING:
B Gold Plus Referring
A Gold Referring
D Silver Plus Referring
C Silver Referring
GWTG – RURAL CAD: NSTE_ACS
N Gold Achievement
L Silver Achievement
GWTG – RURAL CAD: STEMI
N Gold Achievement
L Silver Achievement
Mahaska Health, Oskaloosa
Mary Greeley Medical Center, Ames
Mercy Medical Center-Cedar Rapids, Cedar Rapids
MercyOne Clinton Medical Center, Clinton
MercyOne Dubuque Medical Center, Dubuque
MercyOne North Iowa Medical Center, Mason City
MercyOne Siouxland Medical Center, Sioux City
MercyOne Waterloo Medical Center, Waterloo
Methodist Jennie Edmundson Hospital, Council Bluffs
Montgomery County Memorial Hospital, Red Oak
Myrtue Medical Center, Harlan
Pocahontas Community Hospital, Pocahontas
Sioux Center Health, Sioux Center
St. Anthony Regional Hosptial, Carroll
UnityPoint Health-Trinity Muscatine, Muscatine
University of Iowa Health Care Medical Center Downtown, Iowa City
University of Iowa Hospitals and Clinics, Iowa City
UPH Allen Hospital, Waterloo
UPH Finley Hospital, Dubuque
UPH Iowa Methodist Medical Center, Des Moines
UPH St Luke’s Hospital Cedar Rapids, Cedar Rapids
UPH St. Luke’s Sioux City, Sioux City
UPH Trinity Bettendorf, Bettendorf
UPH Trinity Regional Medical Center, Fort Dodge
AdventHealth Shawnee Mission, Shawnee Mission
AdventHealth South Overland Park, Overland Park
Amberwell Health Hiawatha, Hiawatha
Ascension Via Christi St. Francis, Wichita
Cheyenne County Hospital, Saint Francis
CommonSpirit St. Catherine Hospital Garden City, Garden City
Community HealthCare System, Onaga
Gove County Medical Center, Quinter
Hays Medical Center, Hays
Hutchinson Regional Medical Center, Hutchinson
Lawrence Memorial Hospital, Lawrence
Nemaha Valley Community Hospital, Seneca
Newman Regional Health, Emporia
North Central Kansas Medical Center, Concordia
Olathe Medical Center, Olathe
Overland Park Regional Medical Center, Overland Park
Providence Medical Center, Kansas City
Rooks County Health Center, Plainville
Saint Luke’s South Hospital, Overland Park
Salina Regional Health Center, Salina
Stormont-Vail HealthCare, Topeka
The University of Kansas Health System St. Francis Campus, Topeka
The University of Kansas Health System, Kansas City
Wesley Medical Center, Wichita
ARH Our Lady of the Way, Martin
Baptist Health Corbin, Corbin
Baptist Health Deaconess Madisonville, Madisonville
GWTG – CAD NSTEMI: A Gold C Silver
TARGET: AORTIC STENOSIS : K Target: Aortic StenosisTM Honor Roll
* These hospitals received Get With The Guidelines®-Resuscitation awards from the American Heart Association for two or more patient populations.
O Hospitals with this designation have received silver or higher awards in three or more Get With The Guidelines modules this year.
Baptist Health Hardin, Elizabethtown
Baptist Health LaGrange, LaGrange
Baptist Health Lexington Hospital, Lexington
Baptist Health Louisville, Louisville
Baptist Health Paducah, Paducah
Baptist Health Richmond, Richmond
Barbourville ARH Hospital, Barbourville
Bourbon Community Hospital, Paris
Carroll County Memorial Hospital, Carrollton
CHI Saint Joseph Health System - Saint Joseph London, London
Clark Regional Medical Center, Winchester
Deaconess Henderson Hospital, Henderson
Ephraim McDowell Fort Logan Hospital, Stanford
Ephraim McDowell James B. Haggin Hospital, Harrodsburg
Ephraim McDowell Regional Medical Center, Danville
Frankfort Regional Medical Center, Frankfort
Georgetown Community Hospital, Georgetown
Harlan ARH Hospital, Harlan
Harrison Memorial Hospital, Cynthiana
Hazard ARH Regional Medical Center, Hazard
Highlands ARH Regional Medical Center, Prestonsburg
King’s Daughters Medical Center, Ashland
Lake Cumberland Regional Hospital, Somerset
Mary Breckinridge ARH Hospital, Hyden
McDowell ARH Hospital, McDowell
Mercy Health Lourdes Hospital, Paducah
Mercy Health Marcum and Wallace Hospital, Irvine
Middlesboro ARH Hospital, Middlesboro
Morgan County ARH Hospital, West Liberty
Murray Calloway County Hospital, Murray
Norton Audubon Hospital, Louisville
Norton Brownsboro Hospital, Louisville
Norton Hospital, Louisville
Owensboro Health, Owensboro
Paintsville ARH Hospital, Paintsville
Pikeville Medical Center, Inc., Pikeville
Saint Joseph East, Lexington
Saint Joseph Hospital, Lexington
St. Elizabeth Edgewood, Edgewood
St. Elizabeth Ft. Thomas, Fort Thomas
The Medical Center at Albany, Albany
The Medical Center at Bowling Green, Bowling Green
The Medical Center at Caverna, Horse Cave
The Medical Center at Scottsville, Scottsville
TJ Health Columbia, Columbia
TJ Samson Community Hospital, Glasgow
TriStar Greenview Regional Hospital, Bowling Green
UK HealthCare, Lexington
UK St. Claire, Morehead
UofL Health - Jewish Hospital, Louisville
UofL Health - Mary & Elizabeth Hospital, Louisville
UofL Health - UofL Hospital, Louisville
Whitesburg ARH Hospital, Whitesburg
GWTG – STROKE:
GWTG – HEART FAILURE:
CHRISTUS Coushatta Health Care Center, Coushatta
CHRISTUS Ochsner St. Patrick Hospital, Lake Charles B
East Jefferson General Hospital, Metairie
Glenwood Regional Medical Center, West Monroe
Lake Charles Memorial Health System, Lake Charles
Lakeview Hospital, Covington
Leonard J. Chabert Medical Center, Houma
Manning Family Children’s, New Orleans
North Oaks Medical Center, Hammond
Ochsner Baptist, New Orleans
Ochsner Lafayette General Medical Center, Lafayette
Ochsner LSU Health Monroe, Monroe
Ochsner LSU Health Shreveport, Shreveport
Ochsner Medical Center - Kenner, Kenner
Ochsner Medical Center - New Orleans, New Orleans
Ochsner Medical Center Westbank, Terrytown, LA, Gretna
Our Lady of Lourdes Regional Medical Center, Lafayette
Our Lady of the Lake Regional Medical Center, Baton Rouge
Rapides Regional Medical Center, Alexandria
Slidell Memorial Hospital East, Slidell
Slidell Memorial Hospital Main, Slidell
St. Charles Parish Hospital, Luling
St. Frances Cabrini Hospital, Alexandria
St. Francis Medical Center, Monroe
St. James Parish Hospital, Lutcher
St. Tammany Parish Hospital, Covington
Thibodaux Regional Health System, Thibodaux
Touro, New Orleans
University Medical Center New Orleans (UMCNO), New Orleans
West Jefferson Medical Center, Marrero
Willis Knighton Pierremont, Shreveport
WK Bossier Health Center, Bossier City
Bridgton Hospital, Bridgton
Central Maine Medical Center, Lewiston
Eastern Maine Medical Center, Bangor
Houlton Regional Hospital, Houlton
Maine Medical Center, Portland
MaineGeneral Medical Center, Augusta
Pen Bay Medical Center, Rockport
Rumford Hospital, Rumford
Adventist HealthCare Shady Grove Medical Center, Rockville
Adventist HealthCare White Oak Medical Center, Silver Spring
Ascension Saint Agnes Hospital, Baltimore
Atlantic General Hospital, Berlin
CalvertHealth Medical Center, Prince Frederick
Carroll Hospital Center, Westminster
ChristianaCare - Union Hospital, Elkton
Doctors Community Medical Center, Lanham
Frederick Health Hospital, Frederick
Greater Baltimore Medical Center, Baltimore
Holy Cross Germantown Hospital, Germantown
GWTG – RESUSCITATION
GWTG – CAD
GWTG – AFIB:
GWTG – RURAL STROKE
GWTG – RURAL HEART FAILURE:
Holy Cross Hospital, Silver Spring
Johns Hopkins Bayview Medical Center, Baltimore
Johns Hopkins Howard County Medical Center, Columbia
Luminis Health Anne Arundel Medical Center, Annapolis
MedStar Franklin Square Medical Center, Baltimore
MedStar Good Samaritan Hospital, Baltimore
MedStar Harbor Hospital, Baltimore
MedStar Southern Maryland Hospital Center, Clinton
MedStar St. Mary’s Hospital, Leonardtown
MedStar Union Memorial Hospital, Baltimore
Mercy Medical Center, Baltimore
Meritus Medical Center, Hagerstown
Northwest Hospital, Randallstown
Sinai Hospital of Baltimore, Baltimore
Suburban Hospital Johns Hopkins Medicine, Bethesda
The Johns Hopkins Hospital, Baltimore
TidalHealth Peninsula Regional, Salisbury
University of Maryland Baltimore Washington Medical Center, Glen Burnie
University of Maryland Capital Region Medical Center, Largo
University of Maryland Charles Regional Medical Center, La Plata
University of Maryland Medical Center, Baltimore
University of Maryland Shore Medical Center at Easton, Easton
University of Maryland St. Joseph Medical Center, Towson
University of Maryland Upper Chesapeake Medical Center, Bel Air
UPMC Western Maryland, Cumberland
Addison Gilbert Hospital, Gloucester
Baystate Franklin Medical Center, Greenfield
Baystate Medical Center, Springfield
Baystate Wing Hospital, Palmer
Berkshire Medical Center, Pittsfield
Beth Israel Deaconess Hospital - Milton, Milton
Beth Israel Deaconess Hospital - Needham, Needham
Beth Israel Deaconess Hospital-Plymouth, Plymouth
Beth Israel Deaconess Medical Center, Boston
Beverly Hospital, Beverly
BMC-Brighton, Brighton
Boston Medical Center, Boston
Boston Medical Center - South, Brockton
Brigham and Women’s Faulkner Hospital, Boston
Brigham and Women’s Hospital, Boston
Cape Cod Hospital, Hyannis
Cooley Dickinson Hospital, Northampton
Emerson Health, Concord
Fairview Hospital, Great Barrington
Falmouth Hospital, member Cape Cod Healthcare, Falmouth
Holy Family Hospital - Haverhill, Haverhill
Holy Family Hospital - Methuen, Methuen
Holyoke Medical Center, Holyoke
Lahey Hospital & Medical Center, Burlington, Burlington
Lawrence General Hospital, Lawrence
Lowell General Hospital - Main Campus, Lowell
Massachusetts General Hospital, Boston
Melrose-Wakefield Hospital, Melrose
GWTG – CAD
STEMI REFERRING:
B Gold Plus Referring A Gold Referring D Silver Plus Referring
C Silver Referring
GWTG – RURAL CAD: NSTE_ACS
Mercy Medical Center, Springfield
MetroWest Medical Center - Framingham, Framingham
Milford Regional Medical Center, Milford
Mount Auburn Hospital, Cambridge
Newton-Wellesley Hospital, Newton
North Adams Regional Hospital, North Adams
Saint Anne’s Hospital, Fall River
Saint Vincent Hospital, Worcester
Salem Hospital, Salem B
Southcoast Health Charlton Memorial Hospital, Fall River B
Southcoast Health St. Luke’s Hospital, New Bedford B
Southcoast Health Tobey Hospital, Wareham B
Sturdy Memorial Hospital, Attleboro B
Tufts Medical Center, Boston B
UMass Memorial - Marlborough Hospital, Worcester B
UMASS Memorial HealthAlliance-Clinton Hospital, Fitchburg B
UMass Memorial Medical Center, Worcester B
Aspirus Iron River Hospital, Iron River D Beacon Kalamazoo, Kalamazoo C B
Bronson Methodist Hospital, Kalamazoo B
Chelsea Hospital, Chelsea C
Corewell Health Beaumont Grosse Pointe Hospital, Grosse Pointe B
Corewell Health Beaumont Troy Hospital, Troy B
Corewell Health Big Rapids Hospital, Big Rapids LD BN
Corewell Health Farmington Hills Hospital, Farmington Hills B
Corewell Health Gerber Hospital, Fremont L BN
Corewell Health Grand Rapids Hospitals- Blodgett, Grand Rapids B D
Corewell Health Grand Rapids Hospitals - Butterworth Hospital, Grand Rapids B B
Corewell Health Greenville Hospital, Greenville LD L
Corewell Health Lakeland Hospitals, Saint Joseph B
Corewell Health Ludington Hospital, Ludington
Corewell Health Pennock Hospital, Hastings
Corewell Health Reed City Hospital, Reed City
Corewell Health Trenton Hospital, Trenton
Corewell Health William Beaumont University Hospital, Southfield
Corewell Health Zeeland Hospital, Zeeland
Corewell Health’s Beaumont Hospital, Dearborn, Dearborn
Covenant HealthCare, Saginaw
DMC Detroit Receiving Hospital, Detroit
DMC Harper University Hospital, Detroit
DMC Huron Valley-Sinai Hospital, Commerce Township
DMC Sinai-Grace Hospital, Detroit
Eaton Rapids Medical Center, Eaton Rapids
Garden City Hospital, Garden City
Henry Ford Health - Genesys, Grand Blanc
Henry Ford Hospital and Health Network, Detroit
Henry Ford Jackson Hospital, Jackson
Henry Ford Macomb Hospital, Clinton Township
Henry Ford Providence Novi Hospital, Novi
Henry Ford Providence Southfield, Southfield B
Henry Ford Rochester Hospital, Rochester
Henry Ford St. John Hospital, Detroit
Henry Ford West Bloomfield Hospital, West Bloomfield
GWTG – CAD NSTEMI:
GWTG – RURAL CAD: STEMI
Gold Achievement
Silver Achievement
TARGET: AORTIC STENOSIS : K Target: Aortic StenosisTM Honor Roll
* These hospitals received Get With The Guidelines®-Resuscitation awards from the American Heart Association for two or more patient populations. O Hospitals with this designation have received silver or higher awards in three or more Get With The Guidelines modules this year.
Henry Ford Wyandotte Hospital, Wyandotte
Hurley Medical Center, Flint
Lake Huron Medical Center, Port Huron
Mackinac Straits Health System, Saint Ignace
McKenzie Health System, Sandusky
McLaren Bay Region, Bay City
McLaren Central Michigan, Mount Pleasant
McLaren Flint, Flint
McLaren Greater Lansing, Lansing
McLaren Lapeer Region, Lapeer
McLaren Macomb, Mount Clemens
McLaren Northern Michigan, Petoskey
McLaren Oakland, Pontiac
McLaren Port Huron Hospital, Port Huron
Memorial Healthcare, Owosso
Munson Medical Center, Traverse City
MyMichigan Medical Center - Alpena, Alpena
MyMichigan Medical Center- Gladwin, Gladwin
MyMichigan Medical Center Clare, Clare
MyMichigan Medical Center Midland, Midland
MyMichigan Medical Center Saginaw, Saginaw
MyMichigan Medical Center West Branch, West Branch
ProMedica Charles and Virginia Hickman Hospital, Adrian
ProMedica Monroe Regional Hospital, Monroe
Scheurer Health, Pigeon
Trinity Health Ann Arbor, Ypsilanti
Trinity Health Grand Rapids, Grand Rapids
Trinity Health Livonia, Livonia
Trinity Health Muskegon Hospital, Muskegon
Trinity Health Oakland, Pontiac
Trinity Health Shelby Hospital, Shelby
UMH-Sparrow, Lansing
University
Ann Arbor
Northwestern Hospital, Minneapolis
Aspirus St. Luke’s Hospital, Duluth
CentraCare St. Cloud Hospital, Saint Cloud
Essentia Health East. St. Mary’s Medical Center, Duluth
Essentia Health-St. Joseph’s Medical Center, Brainerd
Fairview Range Medical Center, Hibbing
Grand Itasca Clinic and Hospital, Grand Rapids
Hennepin Healthcare System, Inc., Minneapolis
Lakeview Memorial Hospital, Stillwater
M Health Fairview Lakes Medical Center, Wyoming
M Health Fairview Northland Medical Center, Princeton
M Health Fairview Southdale Hospital, Edina
M Health Fairview St. John’s Hospital, Maplewood
M Health Fairview University of Minnesota Medical Center, Minneapolis
Mayo Clinic Health System- Mankato, Mankato
Clinic Hospital - Rochester, Rochester
Mercy Hospital, Coon Rapids
GWTG – STROKE:
Murray County Medical Center, Slayton
North Memorial Health Hospital, Robbinsdale
Owatonna Hospital, Owatonna
Park Nicollet Methodist Hospital, Saint Louis Park
Regions Hospital, Saint Paul
United Hospital, Saint Paul
Baptist Medical Center - Attala, Kosciusko N
Baptist Medical Center Leake, Carthage L
Baptist Memorial Healthcare - Yazoo, Yazoo City
Baptist Memorial Hospital - Desoto, Southaven
Baptist Memorial Hospital - Golden Triangle, Columbus
Baptist Memorial Hospital - North Mississippi, Oxford BL
Baptist Memorial Hospital - Union County, New Albany N
Baptist Memorial Hospital Calhoun, Calhoun City
Copiah County Medical Center, Hazlehurst
Delta Health-The Medical Center, Greenville
Forrest General Hospital, Hattiesburg
Greenwood Leflore Hospital, Greenwood
Highland Community Hospital, Picayune
Jefferson Davis Community Hospital, PRENTISS
Marion General Hospital, Columbia
Memorial Health System- Gulfport, Gulfport
Merit Health Madison, Canton
Merit Health Wesley, Hattiesburg
Methodist Olive Branch Hospital, Olive Branch
Mississippi Baptist Medical Center, Jackson
North Mississippi Medical Center - Iuka, IUKA
North Mississippi Medical Center, Tupelo
Ochsner Medical Center Hancock, Bay Saint Louis
Ochsner Rush Medical Center, Meridian
Pearl River County Hospital, Poplarville
River Oaks Hospital, Jackson
S. E. Lackey Memorial Hospital, Forest
Singing River Gulfport, Gulfport
Singing River Hospital Ocean Springs, Ocean Springs
Singing River Hospital Pascagoula, Pascagoula
South Central Regional Medical Center, Laurel
St. Dominic Memorial Hospital, Jackson
Stone County Hospital, Wiggins
University of Mississippi Medical Center, Jackson
Walthall General Hospital, Tylertown
Winston Medical Center, Louisville
Barnes-Jewish Hospital, Saint Louis
Barnes-Jewish St. Peters Hospital, Saint Peters
Bates County Memorial Hospital, Butler
Belton Regional Medical Center, Belton
Boone Hospital Center, Columbia
Bothwell Regional Health Center, Sedalia
Cameron Regional Medical Center, Cameron
Capital Region Medical Center, Jefferson City
Carroll County Memorial Hospital, Carrollton
Cass Regional Medical Center, Harrisonville
Centerpoint Medical Center, Independence
GWTG – RURAL STROKE :
GWTG – HEART FAILURE:
Gold Plus Achievement
Silver Achievement
GWTG – RURAL HEART FAILURE:
GWTG – RESUSCITATION :
Gold Achievement
Silver Achievement
GWTG – AFIB:
Achievement
Achievement
Christian Hospital, St. Louis
Citizens Memorial Hospital, Bolivar
Cox Barton County Hospital, Lamar
Cox Medical Center Branson, Branson
Cox Monett Hospital, Monett
CoxHealth Medical Center South, Springfield
Freeman Health System, Joplin
Golden Valley Memorial Healthcare, Clinton
Hannibal Regional Hospital, Hannibal
Harrison County Community Hospital, Bethany
Hedrick Medical Center, Chillicothe
Lafayette Regional Health Center, Lexington
Lake Regional Health System, Osage Beach
Lee’s Summit Medical Center, Lees Summit
Liberty Hospital, Liberty
Mercy Hospital Jefferson, Crystal City
Mercy Hospital Joplin, Joplin
Mercy Hospital Lebanon, Lebanon
Mercy Hospital Lincoln, Troy
Mercy Hospital Perry, Perryville
Mercy Hospital South, Saint Louis
Mercy Hospital Southeast, Cape Girardeau
Mercy Hospital Springfield, Springfield
Mercy Hospital St. Louis, St. Louis
Mercy Hospital Washington, Washington
Missouri Baptist Medical Center, Saint Louis
Missouri Baptist Sullivan Hospital, Sullivan
Missouri Delta Medical Center, Sikeston
Mosaic Life Care d/b/a Heartland Health, Saint Joseph
Mosaic Medical Center- Albany, Albany
Mosaic Medical Center-Maryville, Maryville
NKC Health, North Kansas City
Ozarks Medical Center, West Plains
Parkland Health Center, Farmington
Phelps Health, Rolla
Poplar Bluff Regional Medical Center, Poplar Bluff
Progress West Hospital, O Fallon
Ray County Hospital and Healthcare, Richmond
Research Medical Center, Kansas City
Saint Francis Medical Center, Cape Girardeau
Saint Luke’s East Hospital, Lees Summit
Saint Luke’s Hospital of Kansas City, Kansas City
Saint Luke’s North Hospital, Kansas City
SSM Health Cardinal Glennon Children’s Hospital, St Louis
SSM Health DePaul Hospital, Bridgeton
SSM Health Saint Louis University Hospital, Saint Louis
SSM Health St. Joseph Hospital -St. Charles, Saint Charles
SSM Health St. Mary’s Hospital, St. Louis
SSM Health, St. Clare Hospital, Fenton
SSM St. Joseph Hospital Lake St. Louis, Lake St Louis
St. Joseph Medical Center, Kansas City
St. Luke’s Hospital, Chesterfield
St. Mary’s Health Center, Jefferson City
St. Mary’s Medical Center, Blue Springs
University Health Truman Medical Center, Kansas City
University of Missouri Health Care, Columbia
Washington County Memorial Hospital, Potosi
Western Missouri Medical Center, Warrensburg
Wright Memorial Hospital, Trenton
Referring
Referring
Referring
Beartooth Billings Clinic, Red Lodge
Benefis Health System, Great Falls
Billings Clinic, Billings
Bitterroot Health, Hamilton
Bozeman Health, Bozeman
Cabinet Peaks Medical Center, Libby
Logan Health Medical Center, Kalispell
Mountainview Medical Center, White Sulphur Springs
Providence St. Patrick Hospital, Missoula
Roundup Memorial Healthcare, Roundup
Ruby Valley Medical Center, Sheridan
St. James Healthcare, Butte
St. Luke Community Healthcare, Ronan
St. Peter’s Hospital, Helena
St. Vincent Healthcare, Billings
Stillwater Billings Clinic, Columbus
Wheatland Memorial Healthcare, Harlowton
Bellevue Medical Center, Bellevue
Bryan Medical Center, Lincoln
CHI Health Creighton University Medical Center Bergan Mercy, Omaha
CHI Health Good Samaritan Hospital, Kearney
CHI Health Immanuel Medical Center, Omaha
CHI Health St. Elizabeth, Lincoln
CHI Health St. Francis Medical Center, Grand Island
Columbus Community Hospital, Columbus
Cozad Community Hospital, Cozad
Crete Area Medical Center, Crete
Faith Regional Health Services, Norfolk
Gothenburg Health, Gothenburg
Great Plains Health, North Platte
Jefferson Community Health & Life, Fairbury
Jennie M. Melham Memorial Medical Center, Broken Bow
Johnson County Hospital, Tecumseh
Kearney Regional Medical Center, Kearney
Kimball Health Services, Kimball
Mary Lanning Healthcare, Hastings
Methodist Fremont Health, Fremont
Nebraska Medical Center, Omaha
Nebraska Methodist Hospital, Omaha
Regional West Medical Center, Scottsbluff
Carson Tahoe Regional Medical Center, Carson City
Centennial Hills Hospital Medical Center, Las Vegas
Dignity Health St. Rose Dominican HospitalSan Martin Campus, Las Vegas
Dignity Health St. Rose Dominican Hospital - Siena Campus, Henderson
ER at Blue Diamond, Las Vegas
ER at Cadence, Henderson
ER at McCarran NW, Reno
ER at Spanish Springs, Sparks
North Vista Hospital, North Las Vegas
* These hospitals received Get With The Guidelines®-Resuscitation awards from the American Heart Association for two or more patient populations.
O Hospitals with this designation have received silver or higher awards in three or more Get With The Guidelines modules this year.
Northern Nevada Medical Center, Sparks
Renown Regional Medical Center, Reno
Saint Mary’s Regional Medical Center, Reno
Sierra Medical Center, Reno
Southern Hills Hospital & Medical Center, Las Vegas
Summerlin Hospital Medical Center, Las Vegas
Sunrise Hospital & Medical Center, Las Vegas
University Medical Center of Southern Nevada, Las Vegas
Catholic Medical Center, Manchester
Concord Hospital - Franklin, Franklin
Concord Hospital- Laconia, Laconia
Concord Hospital, Concord
Dartmouth-Hitchcock Medical Center, Lebanon
Elliot Hospital, Manchester
Exeter Hospital, Exeter
Parkland Medical Center, Derry
Portsmouth Regional Hospital, Portsmouth
St. Joseph Hospital, Nashua
Wentworth-Douglass Hospital, Dover
AtlantiCare Regional Medical Center, Pomona
Chilton Medical Center, Pompton Plains
Barnabas Medical Center, Livingston
Heart and Lung Center, Browns Mills
Englewood Hospital and Medical Center, Englewood
Hackensack Meridian Bayshore Medical Center, Holmdel
Hackensack Meridian Health Jersey Shore University Medical Center, Neptune
Hackensack Meridian JFK University Medical Center, Edison
Hackensack Meridian Ocean University Medical Center, Brick
Hackensack Meridian Palisades Medical Center, North Bergen
Hackensack Meridian Pascack Valley Medical Center, Westwood
Hackensack Meridian Raritan Bay Medical Center, Perth Amboy
Hackensack Meridian Riverview Medical Center, Red
Hackensack Meridian Southern Ocean Medical Center, Manahawkin
Washington Township Hospital, Turnersville
Jersey City Medical Center, Jersey City
Monmouth Medical Center, Long Branch
Morristown Medical Center, Morristown
Newton Medical Center, Newton
Overlook Medical Center, Summit
Penn Medicine Princeton Medical Center, Plainsboro
Robert Wood Johnson University Hospital Somerset, Somerville
Robert Wood Johnson University Hospital, New Brunswick
Saint Clare’s Health, Denville
Saint Clare’s Hospital, Dover General, Dover
Saint Michaels Medical Center, Newark
Saint Peter’s University Hospital, New Brunswick
Shore Medical Center, Somers Point
St. Joseph’s University Medical Center, Paterson
St. Joseph’s Wayne Medical Center, Wayne
St. Luke’s Warren Hospital, Phillipsburg
St. Mary’s General Hospital, Passaic
The Valley Hospital, Ridgewood
University Hospital, Newark
Virtua Marlton Hospital, Marlton
Virtua Memorial Hospital of Burlington County, Mt. Holly
Virtua Our Lady of Lourdes Hospital, Camden
Virtua Voorhees Hospital, Voorhees
Christus St. Vincent Regional Hospital, Santa Fe
Gallup Indian Medical Center, Gallup
Lovelace Medical Center, Albuquerque
PHC-Las Cruces, Inc. dba Memorial Medical Center, Las Cruces
Presbyterian Healthcare Services, Albuquerque
Presbyterian Rust Medical Center, Rio Rancho
University of New Mexico Hospitals, Albuquerque
Albany Medical Center, Albany
Arnot Ogden Medical Center, Elmira
Auburn Community Hospital, Auburn
Bassett Medical Center, Cooperstown
BronxCare Health System, Bronx
Brookdale University Hospital Medical Center, Brooklyn
Catholic Health - Kenmore Mercy Hospital, Buffalo
Catholic Health - Mercy Hospital of Buffalo, Buffalo
Catholic Health - Mount St. Mary’s Hospital, Lewiston
Catholic Health- Sisters of Charity Hospital, Buffalo
Cayuga Medical Center, Ithaca
Cohen Children’s Medical Center, New Hyde Park
Columbia Memorial Hospital, Hudson
Crouse Hospital, Syracuse
Ellis Medicine, Schenectady
F.F. Thompson Hospital, Canandaigua
Flushing Hospital Medical Center, Flushing
Garnet Health Medical Center - Catskills, Harris
Garnet Health Medical Center, Middletown
Gates Vascular Institute / Buffalo General Medical Center, Buffalo
Geneva General Hospital, Geneva
Glen Cove Hospital, Glen Cove
Glens Falls Hospital, Glens Falls
Good Samaritan Hospital, a member of WMC Health, Suffern
Good Samaritan University Hospital, West Islip
Guthrie Corning Hospital, Corning
Guthrie Cortland Medical Center, Cortland
HealthAlliance: Broadway Campus a Member of the WMC Health Network, Kingston
Highland Hospital, Rochester
Huntington Hospital, Huntington
Interfaith Medical Center, Brooklyn
Jamaica Hospital Medical Center, Richmond Hill
Lenox Hill Hospital, New York
Lewis County Health System, Lowville
LIJ Medical Center at Forest Hills, Forest Hills
LIJ Valley Stream, Valley Stream
Long Island Jewish Medical Center, Queens
Maimonides Medical Center, Brooklyn
Maimonides Midwood Community Hospital, Brooklyn
Mather Hospital Northwell Health, Port Jefferson
Mercy Hospital, Rockville Centre
MidHudson Regional Hospital of WMC Health, Poughkeepsie
Montefiore Medical Center - Moses Campus, Bronx
Montefiore Mount Vernon Hospital, Mount Vernon
Montefiore Nyack Hospital, Nyack
Montefiore St. Luke’s Cornwall, Newburgh
Mount Sinai Brooklyn, Brooklyn
Mount Sinai Morningside, New York
Mount Sinai Queens, Astoria
Mount Sinai South Nassau, Oceanside
Mount Sinai West, New York
Nassau University Medical Center, East Meadow
NewYork-Presbyterian Brooklyn Methodist Hospital, Brooklyn
NewYork-Presbyterian Hudson Valley Hospital, Cortlandt Manor
NewYork-Presbyterian Queens, Flushing
NewYork-Presbyterian/Columbia University Medical Center, New York
NewYork-Presbyterian/Lower Manhattan Hospital, New York
NewYork-Presbyterian/The Allen Hospital, New York
NewYork-Presbyterian/Weill Cornell Medical Center, New York
NewYork-Presbyterian/Westchester, Bronxville
North Shore University Hospital, Manhasset
Northern Dutchess Hospital, Rhinebeck
Northern Westchester Hospital, Mount Kisco
NYC Health + Hospitals/Bellevue, New York
NYC Health + Hospitals/Elmhurst, Elmhurst
NYC Health + Hospitals/Harlem, New York
NYC Health + Hospitals/Jacobi, Bronx
NYC Health + Hospitals/Kings County, Brooklyn
NYC Health + Hospitals/Lincoln, Bronx
NYC Health + Hospitals/Metropolitan, New York
NYC Health + Hospitals/North Central Bronx, Bronx
NYC Health + Hospitals/Queens, Jamaica
NYC Health + Hospitals/South Brooklyn Health, Brooklyn
NYC Health + Hospitals/Woodhull, Brooklyn
NYU Langone Hospital - Brooklyn, Brooklyn
NYU Langone Hospital - Long Island, Mineola
NYU Langone Hospital - Suffolk, Patchogue
GWTG – CAD
STEMI REFERRING:
B Gold Plus Referring
A Gold Referring
D Silver Plus Referring
C Silver Referring
GWTG – RURAL CAD: NSTE_ACS N Gold Achievement L Silver Achievement
GWTG – RURAL CAD: STEMI
N Gold Achievement
L Silver Achievement
NYU Langone Hospitals, New York
Olean General Hospital, Member: Upper Allegheny Health System, Olean
Peconic Bay Medical Center Northwell Health, Riverhead
Phelps Hospital, Northwell Health, Sleepy Hollow
Plainview Hospital, Plainview
Richmond University Medical Center, Staten Island
Rochester Regional Health at Newark Wayne Community Hospital, Newark
Rochester Regional Health at Rochester General Hospital, Rochester
Rochester Regional Health at United Memorial Medical Center, Batavia
Rome Health, Rome
Saint Joseph’s Medical Center, Yonkers
Samaritan Hospital, Troy
Samaritan Medical Center, Watertown
Saratoga Hospital, Saratoga Springs
SBH Health System, Bronx
Soldiers & Sailors Memorial Hospital, Penn Yan
South Shore University Hospital, Bay Shore
St. Catherine of Siena Hospital, Smithtown
St. Charles Hospital, Port Jefferson
St. Francis Hospital and Heart Center, Roslyn
St. James Hospital, Hornell
St. John’s Episcopal Hospital, Far Rockaway
St. John’s Riverside Hospital, Yonkers
St. Joseph Hospital, Bethpage
St. Joseph’s Health, Syracuse B
St. Lawrence Health at Canton-Potsdam Hospital, Potsdam D
St. Peter’s Hospital, Albany
Staten Island University Hospital - Prince’s Bay, Staten Island
Staten Island University Hospital, Staten Island
Stony Brook Southampton Hospital, Southampton
Stony Brook University Hospital, Stony Brook
Syosset Hospital, Syosset
The Brooklyn Hospital Center, Brooklyn
The Mount Sinai Hospital, New York
UHS Wilson Medical Center, Johnson City
University Hospital at Downstate - Downstate Health Sciences University, Brooklyn
University of Vermont Healthnetwork-Champlain Valley Physician’s Hospital, Plattsburgh
Upstate University Hospital, Syracuse
UR Medicine Strong Memorial Hospital, Rochester
Vassar Brothers Medical Center, Poughkeepsie
Westchester Medical Center, Valhalla
White Plains Hospital, White Plains
Wyckoff Heights Medical Center, Brooklyn
Wynn Hospital, Utica
Alleghany Health, Sparta
Angel Medical Center, Franklin
Annie Penn Hospital, Reidsville
Atrium Health Cabarrus, Concord
Atrium Health Cleveland, Shelby
Atrium Health Kings Mountain, Kings Mountain
GWTG – CAD NSTEMI: A Gold
TARGET: AORTIC STENOSIS : K Target: Aortic StenosisTM Honor Roll
* These hospitals received Get With The Guidelines®-Resuscitation awards from the American Heart Association for two or more patient populations.
O Hospitals with this designation have received silver or higher awards in three or more Get With The Guidelines modules this year.
Atrium Health Lincoln, Lincolnton
Atrium Health Mercy, Charlotte
Atrium Health Pineville, Charlotte
Atrium Health Stanly, Albemarle
Atrium Health Union, Monroe
Atrium Health University City, Charlotte
Atrium Health Wake Forest Baptist High Point Medical Center, High Point
Atrium Health Wake Forest Baptist Lexington Medical Center, Lexington
Atrium Health Wake Forest Baptist Medical Center, Winston-Salem
Atrium Health’s Carolinas Medical Center, Charlotte
Blue Ridge Regional Hospital, Spruce Pine
Caldwell UNC Health Care, Lenoir
Cape Fear Valley Medical Center, Fayetteville
CarolinaEast Medical Center, New Bern
CaroMont Regional Medical Center, Gastonia
Carteret Health Care, Morehead City
Central Carolina Hospital, Sanford
Columbus Regional Healthcare, Whiteville
Cone Health Alamance Regional Hospital, Burlington
Duke Raleigh Hospital, Raleigh
Duke Regional Hospital, Durham
Duke University Hospital, Durham
Durham VA HealthCare System, Durham
ECU Health Beaufort Hospital - A Campus of ECU Health Medical Center, Washington
ECU Health Bertie Hospital, Windsor
ECU Health Chowan Hospital, Edenton
ECU Health Duplin Hospital, Kenansville
ECU Health Edgecombe Hospital, Tarboro
ECU Health Medical Center, Greenville
ECU Health North Hospital, Roanoke Rapids
ECU Health Roanoke-Chowan Hospital, Ahoskie
FirstHealth Montgomery Memorial Hospital, Troy
FirstHealth Moore Regional Hospital - Hoke, Raeford
FirstHealth Moore Regional Hospital - Richmond, Rockingham
FirstHealth Moore Regional Hospital, Pinehurst
Frye Regional Medical Center, Hickory
Hugh Chatham Memorial Hospital, Elkin
Iredell Memorial Hospital, Statesville
Lake Norman Regional Medical Center, Mooresville
Maria Parham Medical Center, LLC, Henderson
Mission Hospital McDowell, Marion
Mission Hospitals, Inc., Asheville
Northern Regional Hospital, Mount Airy
Novant Health Ballantyne Medical Center, Charlotte
Novant Health Brunswick Medical Center, Bolivia
Novant Health Forsyth Medical Center, Winston-Salem
Novant Health Huntersville Medical Center, Huntersville
Novant Health Kernersville Medical Center, Kernersville
Novant Health Matthews Medical Center, Matthews
Novant Health Mint Hill Medical Center, Charlotte
Novant Health New Hanover Regional Medical Center,
Novant Health Presbyterian Medical Center, Charlotte
GWTG – STROKE:
Gold Plus Achievement A Gold Achievement D Silver Plus Achievement
Silver Achievement
GWTG – RURAL STROKE :
Gold Achievement
Silver Achievement
Novant Health Rowan Medical Center, Salisbury
Novant Health Thomasville Medical Center, Thomasville
Onslow Memorial Hospital, Jacksonville D
Sentara Albemarle Medical Center, Elizabeth City N
St. Luke’s Hospital, Columbus
The Moses H Cone Memorial Hospital, Greensboro
The Outer Banks Hospital, Nags Head
UNC Health Blue Ridge, Morganton
UNC Health Johnston, Smithfield
UNC Health Lenoir, Kinston
UNC Health Nash, Rocky Mount
UNC Health Pardee, Hendersonville
UNC Health Wayne, Goldsboro
UNC Hospitals, Chapel Hill
UNC REX Healthcare, Raleigh
UNC REX Holly Springs Hospital, Holly Springs
Wake Forest Baptist Health Wilkes Medical Center, North Wilkesboro
WakeMed Health & Hospitals - Cary Campus, Cary
WakeMed Health & Hospitals - Raleigh Campus, Raleigh
Wesley Long Hospital, Greensboro
Altru Health System, Grand Forks B
Ashley Medical Center, Ashley L
CHI Lisbon Health, Lisbon
CHI Mercy Health - Valley City, Valley City
CHI St. Alexius Dickinson, Dickinson
CHI St. Alexius Health Bismarck, Bismarck
Community Memorial Hospital, Turtle Lake
Essentia Health - Fargo, Fargo
First Care Health Center, Park River
Heart of America Medical Center, Rugby
Jacobson Memorial Hospital Care Center, Elgin
Jamestown Regional Medical Center, Jamestown
Langdon Prairie Health, Langdon
Mountrail County Medical Center, Stanley
Northwood Deaconess Health Center, Northwood
Oakes Community Hospital, Oakes
Pembina County Memorial Hospital, Cavalier
Sanford Bismarck Medical Center, Bismarck
Sanford Medical Center Fargo, Fargo
Sanford Medical Center Mayvile, Mayville
SMP Health - St Kateri, Rolla
South Central Health Wishek, Wishek
Southwest Healthcare Services, Bowman
St. Andrew’s Health Center, Bottineau
Tioga Medical Center, Tioga
Towner County Medical Center, Cando
Trinity Health Kenmare Hospital, Kenmare
Trinity Health, Minot
Unity Medical Center, Grafton
West River Health Services, Hettinger
Adena Regional Medical Center, Chillicothe
Ashtabula County Medical Center, Ashtabula
GWTG – HEART FAILURE: B Gold Plus Achievement
Gold Achievement D Silver Plus Achievement C Silver Achievement
GWTG – RURAL HEART FAILURE: L Silver Achievement
GWTG – RESUSCITATION :
Gold Achievement
Silver Achievement
GWTG – AFIB: A Gold Achievement
Silver Achievement
GWTG – CAD STEMI RECEIVING:
Atrium Medical Center, Middletown
Aultman Alliance Community Hospital, Alliance
Aultman Hospital, Canton
Bethesda Butler Hospital, Hamilton
Blanchard Valley Health System, Findlay
Cincinnati Children’s, Cincinnati
Cleveland Clinic Akron General Medical Center, Akron
Cleveland Clinic Avon Hospital, Avon
Cleveland Clinic Euclid Hospital, Euclid
Cleveland Clinic Fairview Hospital, Cleveland
Cleveland Clinic Hillcrest Hospital, Mayfield Heights
Cleveland Clinic Marymount Hospital, Garfield Heights
Cleveland Clinic Medina Hospital, Medina
Cleveland Clinic Mercy Hospital, Canton
Cleveland Clinic South Pointe Hospital, Warrensville Heights
Cleveland Clinic Union Hospital, Dover
Cleveland Clinic, Cleveland
Clinton Memorial Hospital, Wilmington
Coshocton Regional Medical Center, Coshocton
East Liverpool City Hospital, East Liverpool
Firelands Regional Medical Center, Sandusky
Fisher Titus Medical Center, Norwalk
Genesis Healthcare System, Zanesville
Good Samaritan Hospital, Cincinnati
Holzer Health System, Gallipolis
Kettering Health Dayton, Dayton
Kettering Health Greene Memorial, Xenia
Kettering Health Hamilton, Hamilton
Kettering Health Main Campus, Dayton
Kettering Health Miamisburg, Miamisburg
Kettering Health Troy, Troy
Knox Community Hospital, Mount Vernon
Licking Memorial Hospital, Newark
Lima Memorial Health System, Lima
McCullough Hyde Memorial Hospital, Oxford
Mercer Health, Coldwater
Mercy Health - Anderson Hospital, Cincinnati
Mercy Health – Fairfield Hospital, Fairfield
Mercy Health - St. Elizabeth Youngstown Hospital, Youngstown
Mercy Health Clermont Hospital, Batavia
Mercy Health St. Charles Hospital, Oregon
Mercy Health West Hospital, Cincinnati
Mercy St. Vincent Medical Center, Toledo
Mercyhealth- Urbana Hospital, Urbana
Miami Valley Hospital, Dayton
Miami Valley South, Centerville
Mount Carmel Health System, Columbus
Mount Carmel St. Ann’s, Westerville
Ohio State University Wexner Medical Center, Columbus
Doctors Hospital, Columbus
OhioHealth Mansfield Hospital, Mansfield
OhioHealth
Ohiohealth Pickerington Methodist Hospital, Pickerington
Pomerene Hospital, Millersburg
ProMedica Flower Hospital, Sylvania
ProMedica Memorial Hospital, Fremont N
ProMedica Toledo Hospital, Toledo B K
Soin Medical Center, Beaver Creek B
Southwest General Health Center, Middleburg Heights O B A A B
Springfield Regional Medical Center, Springfield B
St. Rita’s Medical Center, Lima B
Summa Health System - Akron Campus, Akron B
The Christ Hospital, Cincinnati A
The Jewish Hospital Mercy Health, Cincinnati B B
The MetroHealth System, Cleveland O A B
The Ohio State University Wexner Medical Center East Hospital, Columbus B
The University of Toledo Medical Center, Toledo B B
TriHealth Bethesda North Hospital, Cincinnati B B
UC Health – University of Cincinnati Medical Center, Cincinnati B B
UC Health – West Chester Hospital, West Chester B B
UH Rainbow Babies and Children’s Hospital, Cleveland C *
University Hospitals Ahuja Medical Center, Beachwood B
University Hospitals Cleveland Medical Center, Cleveland B
University Hospitals Conneaut Medical Center, Conneaut N
University Hospitals Elyria Medical Center, Elyria B
University Hospitals Geauga Medical Center, Chardon B
University Hospitals Geneva Medical Center, Geneva BN
University Hospitals Parma Medical Center, Parma B
University Hospitals Portage Medical Center, Ravenna B
University Hospitals Samaritan Medical Center, Ashland BN
University Hospitals St. John Medical Center, Westlake B
University Hospitals Tripoint Medical Center/ University Hospitals West Medical Center, Painesville B
Upper Valley Medical Center, Troy B Western Reserve Hospital, LLC, Cuyahoga Falls
Wilson Health, Sidney
Wooster Community Hospital, Wooster
Wyandot Memorial Hospital, Upper Sandusky
Ascension St. John Medical Center, Tulsa
Cherokee Nation Health Services WW Hastings Hospital, Tahlequah
Comanche County Memorial Hospital, Lawton
Duncan Regional Hospital, Duncan
Fairview Regional Medical Center, Fairview
Hillcrest Hospital South, Tulsa
Hillcrest Medical Center, Tulsa
Integris Baptist Medical Center Portland Avenue, Oklahoma City
INTEGRIS Baptist Medical Center, Oklahoma City
INTEGRIS Southwest Medical Center, Oklahoma City
Jackson County Memorial Hospital, Altus
Memorial Hospital of Texas County, Guymon
Mercy Hospital Ada, Ada
Mercy Hospital Ardmore, Ardmore
Mercy Hospital Oklahoma City Comprehensive Stroke Center, Oklahoma City
Norman Regional Health System, Norman
Northeastern Health System, Tahlequah
Okeene Municipal Hospital, Okeene
Oklahoma State University Medical Trust dba Oklahoma State University Medical Center, Tulsa
* These hospitals received Get With The Guidelines®-Resuscitation awards from the American Heart Association for two or more patient populations. O Hospitals with this designation have received silver or higher awards in three or more Get With The Guidelines modules this year.
(OKLAHOMA CONTINUED)
OU Health University of Oklahoma Medical Center, Oklahoma City
Saint Francis Hospital Muskogee, Muskogee
Saint Francis Hospital South, Tulsa
Saint Francis Hospital Vinita, Vinita
Saint Francis Hospital, Tulsa
St. Anthony Hospital, Oklahoma City
St. Mary’s Regional Medical Center, Enid
Stillwater Medical Center, Stillwater
Asante Rogue Regional Medical Center, Medford
Asante Three Rivers Medical Center, Grants Pass
Bay Area Hospital, Coos Bay
Good Samaritan Regional Medical Center, Corvallis
Hillsboro Medical Center, Hillsboro
Kaiser Sunnyside Medical Center, Clackamas
Kaiser Westside Medical Center, Hillsboro
Legacy Emanuel Medical Center, Portland
Legacy Good Samaritan Medical Center, Portland
Legacy Meridian Park Medical Center, Tualatin
Legacy Mount Hood Medical Center, Gresham
OHSU, Portland
PeaceHealth Sacred Heart Medical Center RiverBend, Springfield
Providence Medford Medical Center, Medford
Providence Portland Medical Center, Portland
Providence St. Vincent Medical Center, Portland
Providence Willamette Falls Medical Center, Oregon City
Salem Hospital, Salem
Samaritan Albany General Hospital, Albany
Samaritan Lebanon Community Hospital, Lebanon
Samaritan North Lincoln Hospital, Lincoln City
Samaritan Pacific Communities Hospital, Newport
Santiam Hospital, Stayton
Sky Lakes Medical Center, Klamath Falls
St. Anthony Hospital, Pendleton
St. Charles Madras, Madras
St. Charles Medical Center, Bend
St. Charles Prineville, Prineville
Wallowa Memorial Hospital, Enterprise
Abington-Lansdale Hospital, Lansdale
ACMH Hospital, Kittanning
AHN Wexford Hospital, Wexford
Allegheny General Hospital, Pittsburgh
Allegheny Valley Hospital, Natrona Heights
Bryn Mawr Hospital, Bryn Mawr
Butler Memorial Hospital, Butler
Canonsburg Hospital, Canonsburg
Chester County Hospital, West Chester
Chestnut Hill Hospital, Philadelphia
Conemaugh Memorial Medical Center, Johnstown
Conemaugh Meyersdale Medical Center, Meyersdale
Conemaugh Nason Medical Center, Roaring Spring
Doylestown Hospital, Doylestown
Einstein Medical Center Montgomery, East Norriton
GWTG – STROKE:
GWTG – HEART FAILURE:
Gold Plus Achievement
Gold Achievement
Silver Plus Achievement
Silver Achievement
Evangelical Community Hospital, Lewisburg
Forbes Hospital, Monroeville
Geisinger Community Medical Center, Scranton
Geisinger Jersey Shore Hospital, Jersey Shore
Geisinger Lewistown Hospital, Lewistown
Geisinger Medical Center Muncy, Muncy
Geisinger Medical Center, Danville
Geisinger St. Luke’s Hospital, Orwigsburg
Geisinger Wyoming Valley, Wilkes Barre
Grand View Health, Sellersville
Grove City Medical Center, Grove City
Heritage Valley Beaver, Beaver
Heritage Valley Sewickley, Sewickley
Holy Redeemer Hospital, Meadowbrook
Independence Health Frick Hospital, Mount Pleasant
Independence Health Latrobe Hospital, Latrobe
Independence Health Westmoreland Hospital, Greensburg
Indiana Regional Medical Center, Indiana
Jeanes Hospital - Temple University Health System, Philadelphia
Jefferson Abington Hospital, Abington
Jefferson Einstein Philadelphia Hospital, Philadelphia
Jefferson Hospital, Clairton
Methodist Hospital, Philadelphia
Northeast, Philadelphia
Medical Center, Wynnewood
Lehigh Valley Health Network Cedar Crest, Allentown
Lehigh Valley Health Network Muhlenberg, Bethlehem
Lehigh Valley Hospital- Hazleton, Hazleton
Lehigh Valley Hospital - Schuylkill, Pottsville
Lehigh Valley Pocono, East Stroudsburg
Bucks Hospital, Bristol
LVH Hecktown Oaks, Easton
Meadville Medical Center, Meadville
Mercy Fitzgerald Hospital, Darby
Monongahela Valley Hospital, Monongahela
Nittany Medical Center, State College
Hospital, Philadelphia
Paoli Hospital, Paoli
Penn Highlands DuBois, DuBois
Penn Medicine Lancaster General Hospital, Lancaster
Penn Presbyterian Medical Center, Philadelphia
Penn State Health Hampden Medical Center, Enola
Penn State Health Holy Spirit Medical Center, Camp Hill
Penn State Health Lancaster Medical Center, Lancaster
Penn State Health Milton S. Hershey Medical Center, Hershey
Penn State Health St. Joseph Medical Center, Reading
Pennsylvania Hospital, Philadelphia
Phoenixville Hospital, Phoenixville
Pottstown Hospital, Pottstown
Reading Hospital-Tower Health, West Reading
Riddle Hospital, Media
Robert Packer Hospital, Sayre
Roxborough Memorial Hospital, Philadelphia
Saint Vincent Health System, Erie
Sharon Regional Medical Center, Sharon
St. Clair Health, Pittsburgh
St. Luke’s Allentown Campus, Allentown
St. Luke’s Carbon Campus, Lehighton
GWTG – RESUSCITATION :
Achievement
GWTG – AFIB:
Gold Achievement
GWTG – RURAL STROKE
GWTG – RURAL HEART FAILURE:
Silver Achievement
Silver Achievement
GWTG – CAD STEMI RECEIVING: B Gold Plus Receiving
Gold Receiving
Silver Plus Receiving C Silver Receiving
St. Luke’s Hospital - Anderson Campus, Easton
St. Luke’s Hospital – Easton Campus, Easton
St. Luke’s Hospital-Miners Campus, Coaldale
St. Luke’s Hospital Quakertown Campus, Quakertown
St. Luke’s Hospital Sacred Heart, Allentown
St. Luke’s Monroe Campus, Stroudsburg
St. Luke’s University Hospital, Bethlehem
St. Mary Medical Center, Langhorne
Suburban Community Hospital, Norristown
Temple University Hospital, Philadelphia
The Children’s Hospital of Philadelphia, Philadelphia
The Hospital of the University of Pennsylvania, Philadelphia
Thomas Jefferson University Hospital, Philadelphia
UPMC Altoona, Altoona
UPMC Bedford, Everett
UPMC Carlisle, Carlisle
UPMC East, Monroeville
UPMC Hamot, Erie
UPMC Hanover, Hanover
UPMC Health - Harrisburg, West Shore and Community Osteopathic, Harrisburg
UPMC Lititz, Lititz
UPMC Memorial,
UPMC
UPMC Muncy, Muncy
UPMC Northwest, Seneca
UPMC Presbyterian,
UPMC Shadyside, Pittsburgh
UPMC Somerset,
UPMC St. Margaret,
UPMC Wellsboro, Wellsboro
Warren General Hospital, Warren
Memorial Hospital, Honesdale
Waynesboro Hospital, Waynesboro
GWTG – CAD
STEMI REFERRING:
B Gold Plus Referring
A Gold Referring
D Silver Plus Referring
C Silver Referring
GWTG – RURAL CAD: NSTE_ACS
N Gold Achievement
L Silver Achievement
GWTG – RURAL CAD: STEMI
N Gold Achievement
L Silver Achievement
Aiken Regional Medical Center, Aiken
AnMed, Anderson
Beaufort Memorial Hospital, Beaufort
Bon Secours St. Francis Eastside, Greenville
Bon Secours St. Francis Hospital, Charleston
Bon Secours St. Francis-Downtown, Greenville
Carolina Pines Regional Medical Center, Hartsville
Cherokee Medical Center, Gaffney
Coastal Carolina Hospital, Hardeeville
Colleton Medical Center, Walterboro
Conway Medical Center, Conway
East Cooper Medical Center, Mount Pleasant
ER at Sweetwater - Extension of Aiken Regional Medical Centers, North Augusta
Hilton Head Hospital, Hilton Head
Lexington Medical Center, West Columbia
McLeod Health Loris, Loris
McLeod Health Seacoast, Little River
McLeod Regional Medical Center, Florence
Mount Pleasant Hospital, Mount Pleasant B
MUSC Health - Lancaster Medical Center, Lancaster N
MUSC Health, Charleston B
MUSC-Orangeburg, Orangeburg
Newberry County Memorial Hospital, Newberry L L
Pelham Medical Center, Greer
Piedmont Medical Center, Rock Hill
Prisma Health Baptist Easley Hospital, Easley
Prisma Health Baptist Hospital, Columbia B
Prisma Health Baptist Parkridge Hospital, Columbia B
Prisma Health Greenville Memorial Hospital, Greenville B
Prisma Health Greer Memorial Hospital, Greer B
Prisma Health Hillcrest Hospital, Simpsonville B
Prisma Health Laurens County Hospital, Clinton B
Prisma Health Oconee Memorial Hospital, Greenville BN
Prisma Health Richland Hospital, Columbia
Prisma Health Tuomey Hospital, Sumter
Ralph H. Johnson VA Medical Center, Charleston
Roper Hospital, Charleston
Roper St. Francis Berkeley Hospital, Summerville
Self Regional Healthcare, Greenwood
Spartanburg Regional Medical Center - Church Street Campus, Spartanburg B B
Summerville Medical Center, Summerville B
Tidelands Georgetown Memorial Hospital, Georgetown N
Tidelands Waccamaw Community Hospital, Murrells Inlet B
Trident Medical Center, North Charleston B
Union Medical Center, Union L
Avera McKennan, Sioux Falls
Monument Health Rapid City Hospital, Rapid City
Sanford USD Medical Center, Sioux Falls
Baptist Memorial Hospital Memphis, Memphis
Baptist Memorial Hospital-Carroll County, Huntingdon ND
GWTG – CAD NSTEMI: A Gold C Silver
TARGET: AORTIC STENOSIS : K Target: Aortic StenosisTM Honor Roll
* These hospitals received Get With The Guidelines®-Resuscitation awards from the American Heart Association for two or more patient populations. O Hospitals with this designation have received silver or higher awards in three or more Get With The Guidelines modules this year.
Blount Memorial Hospital, Maryville
Bristol Regional Medical Center, Bristol
CHI Memorial Hospital Chattanooga, Chattanooga
CHI Memorial Hospital Hixson, Hixson
Childrens Hospital at Erlanger, Chattanooga
Cookeville Regional Medical Center, Cookeville
Cumberland Medical Center, Crossville
East Tennessee Children’s Hospital, Knoxville
Erlanger Baroness Hospital, Chattanooga
Erlanger East Hospital, Chattanooga
Fort Sanders Regional Medical Center, Knoxville
Hawkins County Memorial Hospital, Rogersville
Highpoint Health-Riverview with Ascension Saint Thomas, Carthage
Highpoint Health - Sewanee with Ascension Saint Thomas, Sewanee
Holston Valley Medical Center, Kingsport
Jackson-Madison County General Hospital, Jackson
Johnson City Medical Center, Johnson City
LeConte Medical Center, Sevierville
Maury Regional Medical Center, Columbia
Methodist Germantown Hospital, Germantown
Methodist Medical Center, Oak Ridge
Methodist North Hospital, Memphis
Methodist South Hospital, Memphis
Methodist University Hospital, Memphis
Morristown-Hamblen Healthcare System, Morristown
Newport Medical Center, Newport
Parkridge East Hospital, Chattanooga
Parkwest Medical Center, Knoxville
Roane Medical Center, Harriman
Saint Francis Hospital, Memphis
Saint Thomas Midtown Hospital, Nashville
Saint Thomas Rutherford Hospital, Murfreesboro
Saint Thomas West Hospital, Nashville
St. Francis Hospital - Bartlett, Bartlett
Starr Regional Medical Center, Athens
Sumner Regional Medical Center, Gallatin
Tennova Healthcare Clarksville, Clarksville
Tennova LaFolletteMedical Center, La Follette
The University of Tennessee Medical Center, Knoxville
TriStar Centennial Medical Center, Brentwood
TriStar Horizon Medical Center, Dickson
TriStar Skyline Medical Center, Nashville
TriStar Southern Hills Medical Center, Nashville
TriStar Stonecrest Medical Center, Smyrna
TriStar Summit Medical Center, Hermitage
Turkey Creek Medical Center, Knoxville
Vanderbilt Tullahoma - Harton Hospital, Tullahoma
University Medical Center, Nashville
Wilson County Hospital, Lebanon
Medical Center, Franklin
AdventHealth - Central Texas, Killeen
Providence, Waco
Seton Hays, Kyle
GWTG – STROKE: B Gold Plus Achievement
A Gold Achievement
D Silver Plus Achievement
C Silver Achievement
GWTG – RURAL STROKE : N Gold Achievement L Silver Achievement
Ascension Seton Medical Center Austin, Austin
Ascension Seton Williamson, Round Rock
Baptist Health System, San Antonio B
Baptist Hospitals of Southeast Texas, Beaumont B
Baylor Scott & White - The Heart Hospital Baylor Denton, Denton A K
Baylor Scott & White All Saints Medical Center - Fort Worth, Fort Worth B
Baylor Scott & White Heart and Vascular Hospital - Dallas, Dallas B A K
Baylor Scott & White Medical Center - Brenham, Brenham N
Baylor Scott & White Medical Center - Buda, Buda D
Baylor Scott & White Medical Center - Centennial, Frisco B A B
Baylor Scott & White Medical Center - College Station, College Station B A B
Baylor Scott & White Medical Center - Grapevine, Grapevine B
Baylor Scott & White Medical Center - Hillcrest, Waco C B
Baylor Scott & White Medical Center - Irving, Irving B
Baylor Scott & White Medical Center - Lake Pointe, Rowlett
Baylor Scott & White Medical Center - Lakeway, Lakeway B B
Baylor Scott & White Medical Center - Marble Falls, Marble Falls BN
Baylor Scott & White Medical Center - McKinney, McKinney B C B
Baylor Scott & White Medical Center - Pflugerville, Pflugerville B
Baylor Scott & White Medical Center - Plano, Plano B
Baylor Scott & White Medical Center - Round Rock, Round Rock B B
Baylor Scott & White Medical Center - Taylor, Taylor N
Baylor Scott & White Medical Center - Temple, Temple B A B K
Baylor Scott & White Medical Center - Waxahachie, Waxahachie B
Baylor Scott & White The Heart Hospital - Plano, Plano B A B K
Baylor St. Luke’s Medical Center, Houston C B
Baylor University Medical Center - Dallas, Dallas B
Ben Taub Hospital, Houston O B A A B
BSA Health System, Amarillo B
Carrollton Regional Medical Center, Carrollton A A B
CHI St Luke’s Health Brazosport, Lake Jackson B
CHRISTUS Good Shepherd Health System - Longview, Longview B
CHRISTUS Good Shepherd Health System-Marshall, Marshall N
CHRISTUS Mother Frances Hospital - Sulphur Springs, Sulphur Springs BN
CHRISTUS Mother Frances Hospital - Tyler, Tyler B
Christus Mother Frances Jacksonville, Jacksonville LD
Christus Mother Frances Winnsboro, Winnsboro N
CHRISTUS Santa Rosa - New Braunfels, New Braunfels D
CHRISTUS Santa Rosa Hospital-Westover Hills, San Antonio D
Christus Santa Rosa San Marcos, San Marcos D
CHRISTUS Southeast Texas Health System-St. Elizabeth, Beaumont B
CHRISTUS Spohn Hospital - Alice, Alice N
CHRISTUS Spohn Hospital - Beeville, Beeville N
CHRISTUS Spohn Hospital - Kleberg, Kingsville N
CHRISTUS Spohn Hospital Corpus Christi - Shoreline, Corpus Christi B
Christus Spohn Hospital Corpus Christi - South, Corpus Christi B
CHRISTUS St. Michael Health System, Texarkana B
CHRISTUS St. Michael Hospital - Atlanta, Atlanta B L ND
Citizens Medical Center, Victoria A B
Coleman County Medical Center, Coleman N
Corpus Christi Medical Center, Corpus Christi D
Covenant Medical Center, Lubbock B
GWTG – HEART FAILURE:
B Gold Plus Achievement A Gold Achievement
D Silver Plus Achievement
C Silver Achievement
GWTG – RURAL HEART FAILURE:
L Silver Achievement
GWTG – RESUSCITATION : A Gold Achievement C Silver Achievement
GWTG – AFIB: A Gold Achievement C Silver Achievement
GWTG – CAD
STEMI RECEIVING: B Gold Plus Receiving A Gold Receiving
D Silver Plus Receiving
C Silver Receiving
Cuero Regional Hospital, Cuero
Dallas Regional Medical Center, Mesquite
Del Sol Medical Center, El Paso
Dell Children’s Medical Center, Austin
Dell Seton Medical Center at The University of Texas, Austin
Doctors Hospital at Renaissance, Edinburg
Glen Rose Medical Center, Glen Rose
Graham Regional Medical Center, Graham
Harlingen Medical Center, Harlingen
HCA Houston Healthcare - Clear Lake, Webster
HCA Houston Healthcare - Conroe, Conroe
HCA Houston Healthcare - Kingwood, Kingwood
HCA Houston Healthcare - Mainland, Texas City
HCA Houston Healthcare - Medical Center (Park Plaza), Houston
HCA Houston Healthcare - Northwest, Houston
HCA Houston Healthcare - Pearland, Pearland
HCA Houston Healthcare - Southeast, Pasadena
HCA Houston Healthcare Tomball, Tomball
Hendrick Medical Center South, Abilene
Hendrick Medical Center, Abilene
Houston Methodist Baytown Hospital, Baytown
Houston Methodist Clear Lake Hosptial, Houston
Houston Methodist Hospital, Houston
Houston Methodist Sugar Land Hospital, Sugar Land
Houston Methodist The Woodlands Hospital, The Woodlands
Houston Methodist West Hospital, Houston
Houston Methodist Willowbrook Hospital, Houston
Hunt Regional Healthcare, Greenville
Huntsville Memorial Hospital, Huntsville
Jasper Memorial, Jasper
JPS Health Network, Fort Worth
Knapp Medical Center, Weslaco
Las Palmas Medical Center, El Paso
Lyndon B Johnson Hospital, Houston
Lynn County Healthcare System, Tahoka
Medical City Children’s Hospital Dallas, Dallas
Medical City Frisco, Frisco
Medical City Plano, Plano
Memorial Hermann - Texas Medical Center, Houston
Memorial Hermann Cypress Hospital, Cypress
Memorial Hermann Greater Heights Hospital, Houston
Memorial Hermann Katy Hospital, Katy
Memorial Hermann Memorial City Medical Center, Houston
Memorial Hermann Northeast Hospital, Humble
Memorial Hermann Pearland Hospital, Pearland
Memorial Hermann Southeast Hospital, Houston
Memorial Hermann Southwest Hospital, Houston
Memorial Hermann Sugar Land Hospital, Sugar Land
Memorial Hermann The Woodlands, The Woodlands
Methodist Charlton Medical Center, Dallas
Methodist Dallas Medical Center, Dallas
Methodist Hospital | Metropolitan, San Antonio
Methodist Hospital | Northeast, San Antonio
Methodist Hospital | Stone Oak, San Antonio
Methodist Hospital Hill Country, Fredericksburg
Methodist Hospital, San Antonio
Methodist Mansfield Medical Center, Mansfield
Methodist Richardson Medical Center, Richardson
Midland Memorial Hospital, Midland
GWTG – CAD STEMI REFERRING: B Gold Plus Referring A Gold Referring D Silver Plus Referring
C Silver Referring GWTG – RURAL CAD: NSTE_ACS
Gold Achievement
Silver Achievement
GWTG – RURAL CAD: STEMI
Gold Achievement L Silver Achievement
Mission Regional Medical Center, Mission
Moore County Hospital District, Dumas
Nacogdoches Memorial Hospital, Nacogdoches
North Texas Medical Center, Gainesville
Northwest Texas Healthcare System, Amarillo
Palo Pinto General Hospital, Mineral Wells
Pampa Regional Medical Center, Pampa
Paris Regional Health, Paris
Parkland Health & Hospital System, Dallas
Peterson Health, Kerrville
Resolute Baptist Hospital, New Braunfels
Rio Grande Regional Hospital, McAllen
Seton Medical Center Harker Heights, Harker Heights
Shannon Medical Center, San Angelo
South Texas Health System Edinburg, Edinburg
South Texas Health System McAllen Medical Center, McAllen
St. David’s Georgetown Hospital, Georgetown
St. David’s Medical Center, Austin
St. David’s North Austin Medical Center, Austin
St. David’s Round Rock Medical Center, Round Rock
St. David’s South Austin Medical Center, Austin B
St. Joseph Health Regional Hospital, Bryan
St. Joseph Medical Center, Houston
St. Luke’s Health-Memorial Lufkin, Lufkin
St. Luke’s Health – The Woodlands Hospital, The Woodlands
Texas Health Allen, Allen
Texas Health Alliance, Fort Worth
Texas Health Arlington Memorial Hospital, Arlington
Texas Health Cleburne, Cleburne
Texas Health Dallas, Dallas
Texas Health Denton, Denton
Texas Health Fort Worth, Fort Worth
Texas Health Frisco, Frisco
Texas Health Heart & Vascular, Arlington
Texas Health HEB, Bedford
Texas Health Hospital Mansfield, Mansfield
Texas Health Huguley Hospital Fort Worth South, Burleson
Texas Health Plano, Plano
Texas Health Presbyterian Flower Mound, Flower Mound
Texas Health Southwest Fort Worth, Fort Worth
Texas Health Stephenville, Stephenville
Texoma Medical Center, Denison
The Hospitals of Providence East Campus, El Paso
The Hospitals of Providence Sierra Campus, El Paso
The Hospitals of Providence Transmountain Campus, El Paso
Titus Regional Medical Center, MT Pleasant
United Regional Healthcare System, Wichita Falls
University Hospital, San Antonio
University Medical Center of El Paso, El Paso
UT Health East Texas Carthage, Carthage
UT Health East Texas Pittsburg, Pittsburg
UT Health Henderson, Henderson
UT Health Jacksonville, Jacksonville
UT Health Quitman, Quitman
UT Health Tyler, Tyler
UTMB Health, Galveston
UTSouthwestern Medical Center, Dallas
Valley Baptist Medical Center-Brownsville, Brownsville
GWTG – CAD NSTEMI:
TARGET: AORTIC STENOSIS : K Target: Aortic StenosisTM Honor Roll
* These hospitals received Get With The Guidelines®-Resuscitation awards from the American Heart Association for two or more patient populations.
O Hospitals with this designation have received silver or higher awards in three or more Get With The Guidelines modules this year.
Valley Baptist Medical Center-Harlingen, Harlingen
Regional Medical Center, Brownsville
Ward Memorial Hospital, Monahans
Yoakum Community Hospital, Yoakum
Ashley Regional Medical Center, Vernal
CommonSpirit Holy Cross Hospital Davis, Layton
Intermountain Layton Hospital, Layton
Intermountain McKay-Dee Hospital, Ogden
Intermountain Medical Center, Murray
Intermountain St. George Regional Hospital, Saint George
Intermountain Utah Valley Hospital, Provo
Lakeview Hospital, Bountiful
Ogden Regional Medical Center, Ogden
Mark’s Hospital, Salt Lake City
Regional Hospital, Orem
Uintah Basin Medical Center, Roosevelt
Uintah Basin Medical Center, Vernal
University of Utah Health, Salt Lake City
Central Vermont Medical Center, Berlin
University of Vermont Medical Center, Burlington
Bon Secours Memorial Regional Medical Center, Mechanicsville
Bon Secours Rappahannock General Hospital, Kilmarnock
Bon Secours Richmond Community Hospital, Richmond
Bon Secours St. Francis Medical Center, Midlothian
Bon Secours St. Mary’s Hospital, Richmond
Carilion Roanoke Memorial Hospital, Roanoke
Centra Lynchburg General Hospital, Lynchburg
Chesapeake Regional Medical Center, Chesapeake
Fauquier Hospital, Warrenton
Inova Fair Oaks Hospital, Fairfax
Inova Fairfax Hospital, Falls
Inova Loudoun Hospital, Leesburg
Inova Mount Vernon Hospital, Alexandria
Mary Washington Hospital, Fredericksburg
Riverside Doctor’s Hospital Williamsburg, Williamsburg
Riverside Regional Medical Center, Newport News
Riverside Shore Memorial Hospital, Onancock
Riverside Walter Reed Hospital, Gloucester
Sentara CarePlex Hospital, Hampton
Sentara Leigh Hospital, Norfolk
Sentara Martha Jefferson Hospital, Charlottesville
Sentara Norfolk General Hospital/Sentara Heart Hospital, Norfolk
Sentara Northern Virginia Medical Center, Woodbridge
GWTG – STROKE: B Gold Plus Achievement A Gold Achievement D Silver Plus Achievement C Silver Achievement
GWTG – RURAL STROKE :
Achievement
Silver Achievement
Sentara Obici Hospital, Suffolk
Sentara Princess Anne Hospital, Virginia Beach
Sentara RMH Medical Center, Harrisonburg
Sentara Virginia Beach General Hospital, Virginia Beach
Sentara Williamsburg Regional Medical Center, Williamsburg
Southside Regional Medical Center, Petersburg
Stafford Hospital, Stafford
Twin County Regional Healthcare, Galax
University of Virginia Medical Center, Charlottesville
UVA Haymarket Medical Center, Haymarket
UVA Prince William Medical Center, Manassas
VCU Community Memorial Hospital, South Hill
VCU Health Medical Center, Richmond
Virginia Hospital Center, Arlington
Winchester Medical Center, Winchester
Columbia County Health System, Dayton
Confluence Health-Central Washington Hospital, Wenatchee
EvergreenHealth Medical Center, Kirkland
EvergreenHealth Monroe, Monroe
Harbor Regional Health Community Hospital, Aberdeen
Harborview Medical Center, Seattle
Jefferson Healthcare, Port Townsend
Kadlec Regional Medical Center, Richland
Kittitas Valley Healthcare, Ellensburg
Salmon Creek Medical Center, Vancouver B
MultiCare Allenmore Hospital, Tacoma B
MultiCare Auburn Medical Center, Auburn B
MultiCare Capital Medical Center, Olympia
MultiCare Covington Medical Center, Covington
MultiCare Deaconess Hospital, Spokane
MultiCare Good Samaritan Hospital, Puyallup
MultiCare Tacoma General Hospital, Tacoma
MultiCare Valley Hospital, Spokane Valley D
MultiCare Yakima Memorial, Yakima
Newport Hospital and Health Services, Newport
Ocean Beach Hospital, Ilwaco
Othello Community Hospital, Othello
Overlake Medical Center and Clinics, Bellevue
PeaceHealth Southwest Medical Center, Vancouver
PeaceHealth St. John Medical Center, Longview
PeaceHealth St. Joseph Medical Center, Bellingham
PeaceHealth United General Medical Center, Sedro Woolley
Providence Centralia Hospital, Centralia
Providence Holy Family Hospital, Spokane
Providence Regional Medical Center Everett, Everett
Providence Sacred Heart Medical Center, Spokane
Providence St. Peter Hospital, Olympia
Pullman Regional Hospital, Pullman
Saint Anne Hospital, Burien
Saint Anthony Hospital, Gig Harbor
Saint Clare Hospital, Lakewood
Saint Joseph Medical Center, Tacoma
Saint Michael Medical Center, Silverdale
Seattle Children’s Hospital, Seattle
Snoqualmie Valley Hospital, Snoqualmie
GWTG – HEART FAILURE: B Gold Plus Achievement A Gold Achievement D Silver Plus Achievement C Silver Achievement
GWTG – RURAL HEART FAILURE: L Silver Achievement
GWTG – RESUSCITATION : A Gold Achievement C Silver Achievement
GWTG – AFIB: A Gold Achievement C Silver Achievement
GWTG – CAD STEMI RECEIVING: B Gold Plus Receiving
Gold Receiving D Silver Plus Receiving
C Silver Receiving
St. Francis Hospital, Federal Way
Swedish Medical Center - Ballard, Seattle
Swedish Medical Center - Cherry Hill Campus, Seattle
Swedish Medical Center - Edmonds, Edmonds
Swedish Medical Center - First Hill Campus, Seattle
Swedish Medical Center - Issaquah Campus, Issaquah
Three Rivers Hospital, Brewster
Trios Health, Kennewick
TriState Health, Clarkston
University of Washington Medical Center, Seattle
UW Medicine | Valley Medical Center, Renton
VA Puget Sound Health Care System, Seattle Campus, Seattle
Virginia Mason Medical Center - Seattle, Seattle
Willapa Harbor Hospital, South Bend
Berkeley Medical Center, Martinsburg
Braxton County Memorial Hospital, Inc., Gassaway
Cabell Huntington Hospital, Huntington
CAMC General Hospital, Charleston
Camden Clark Medical Center, Parkersburg
Greenbrier Valley Medical Center, Ronceverte
Minnie Hamilton Health System, Grantsville
Mon Health Medical Center, Morgantown
Montgomery General Hospital, Montgomery
Potomac Valley Hospital, Keyser
Preston Memorial Hospital, Kingwood
Raleigh General Hospital, Beckley
St. Mary’s Medical Center, Huntington
Stonewall Jackson Memorial Hospital, Weston
Summers County ARH Hospital, Hinton
Summersville Regional Medical Center, Summersville
United Hospital Center, Bridgeport
West Virginia University Hospitals, Morgantown
Wheeling Hospital, Wheeling
WVU Medicine - St. Joseph’s Hospital, Buckhannon
Ascension All Saints Hospital, Racine
Ascension Columbia St. Mary’s Hospital Milwaukee, Milwaukee
Ascension Franklin Hospital, Franklin
Ascension NE Wisconsin- St. Elizabeth Campus, Appleton
Ascension SE Wisconsin Hospital - Elmbrook Campus, Brookfield
Ascension St. Francis Hospital, Milwaukee
Aspirus Divine Savior Hospital and Clinics, Portage
Aspirus Eagle River Hospital, Eagle River
Aspirus Langlade Hospital, Antigo
Aspirus Medford Hospital and Clinics, Medford
Aspirus Riverview Hospital & Clinics Inc., Wisconsin Rapids
Aspirus Wausau Hospital, Wausau
Aurora BayCare Medical Center, Green Bay
Aurora Lakeland Medical Center, Elkhorn
Aurora Medical Center - Grafton, Grafton
Aurora Medical Center - Kenosha, Kenosha
Aurora Medical Center- Oshkosh, Oshkosh
Aurora Medical Center Bay Area, Marinette
Aurora Medical Center Burlington, Burlington
Aurora Medical Center Manitowoc County, Two Rivers
Aurora Medical Center Sheboygan County, Sheboygan
Aurora Medical Center Summit, Summit
Aurora Mount Pleasant Medical Center, Mount Pleasant
Aurora Sinai Medical Center, Milwaukee
Aurora St. Luke’s Medical Center, Milwaukee
Aurora St. Luke’s South Shore, Cudahy
Aurora West Allis Medical Center, West Allis
Bellin Health Oconto Hospital, Oconto
Bellin Memorial Hospital, Green Bay
Beloit Memorial Hospital, Beloit
Cumberland Healthcare, Cumberland
Froedtert Hospital, Milwaukee
Froedtert Menomonee Falls Hospital, Menomonee Falls
Froedtert Pleasant Prairie Hospital, Pleasant Prairie
Froedtert West Bend Hospital, West Bend
Gundersen Boscobel Area Hospital and Clinics, Boscobel
Gundersen Lutheran Medical Center, La Crosse
Gundersen Moundview Hospital & Clinics, Friendship
Holy Family Memorial Medical Center, Manitowoc
Howard Young Medical Center, Inc., Woodruff
HSHS St. Clare Memorial Hospital, Oconto Falls
Lafayette Hospital + Clinics, Darlington
Marshfield Medical Center, Marshfield
Mayo Clinic Health System - Eau Claire, Eau Claire
Mayo Clinic Health System - La Crosse, La Crosse
Mercy Health Hospital and Medical Center Walworth, Lake Geneva
Mercy Hospital and Trauma Center, Janesville
Monroe Clinic - SSM Health, Monroe
ProHealth Care, Oconomowoc Memorial Hospital, Oconomowoc
ProHealth Care, Waukesha Memorial Hospital, Waukesha
Richland Hospital, Richland Center
SSM Health St. Clare Hospital, Baraboo
SSM Health St. Mary’s Hospital - Madison, Madison
St. Agnes Hospital, Fond Du Lac
ThedaCare Medical Center - Berlin, Berlin
ThedaCare Medical Center - New London, New London
ThedaCare Medical Center - Shawano, Shawano
ThedaCare Medical Center - Waupaca, Waupaca
ThedaCare Regional Medical Center - Appleton, Appleton
ThedaCare Regional Medical Center - Neenah, Neenah
University of Wisconsin Hospital and Clinics, Madison
UPH Meriter Hospital, Madison
Upland Hills Health, Dodgeville
UW Health East Madison Hospital, Madison
Vernon Memorial Healthcare, Inc., Viroqua
Banner Wyoming Medical Center, Casper
Cheyenne Regional Medical Center, Cheyenne
Three Rivers Health, Basin
This content is available online at https://usnewsbrandfuse.com/AmericanHeartAssociation/
GWTG – CAD
STEMI REFERRING: B Gold Plus Referring A Gold Referring
D Silver Plus Referring
C Silver Referring
GWTG – RURAL CAD: NSTE_ACS
GWTG – RURAL CAD: STEMI
Gold Achievement L Silver Achievement
GWTG – CAD NSTEMI:
Gold
Silver TARGET: AORTIC STENOSIS : K Target: Aortic StenosisTM Honor Roll
* These hospitals received Get With The Guidelines®-Resuscitation awards from the American Heart Association for two or more patient populations. O Hospitals with this designation have received silver or higher awards in three or more Get With The Guidelines modules this year.
by Avital Norman Nathman and Deborah Wage ©
IMAGINE A BUSINESS where your expenses far outpace your competitors, results are worsening and over 80% of failures are preventable. In any other sector, such a performance would trigger a crisis. Stakeholders would demand answers. The operation would either be overhauled—or collapse. So why do we continue to allow the U.S. birth industry to stumble along, despite abysmal outcomes and staggering losses?
For decades, pregnant women who survived traumatic childbirth have shared their stories, highlighting the systemic harms and challenges baked into the current birth system. Yet, year after year, the U.S. continues to underperform, especially for Black and Indigenous women. Black women, in particular, are three times more likely to die from pregnancy-related causes than white women. Their stories—of pain, of injustice, of survival—have been shared widely. But still, the system does not change.
From 2000 to 2023, the global maternal mortality rate dropped by 40%. But the United States has moved in the opposite direction. During the height of the COVID-19 pandemic, U.S. maternal deaths surged by almost 40%. A 2022 report from The Commonwealth Fund showed that the U.S. maternal mortality rate in 2020 was several times the rate in most other highly-resourced countries, at 24 deaths for every 100,000 live births on average, and 55 deaths for every 100,000 births for Black women in particular.
Contrast this with countries like the Netherlands, Australia and Japan. Not only were their maternal mortality rates dramatically lower, they continued to decline during the pandemic.
And it’s not just the outcomes that are grim—so are the costs. A routine, uncomplicated vaginal birth in the U.S. averages close to $9,000. In Australia, it’s closer to $5,000; in Germany, as low as $1,360. Cesarean deliveries here routinely cost almost $14,000, and we tend to have more of them than other similarly resourced countries.
To save more mothers’ lives, the U.S. needs to rethink how we give birth—starting with midwives.
In Australia, they’re less than $8,000. In Germany, $2,400. We are spending the most to deliver some of the worst results.
According to a 2024 CDC report, a shocking 84% of pregnancy-related deaths in the U.S. are preventable. So why is this allowed to continue? Why are we writing off these lost lives? Perhaps it has something to do with the fact that, as one maternal health insurance insider put it, “It’s simply cheaper to let women die.”
In any other industry, people would be rushing in to overhaul and fix things, yet we continue to allow potential largescale solutions to flounder. And one of the biggest solutions—the midwifery model of care—continues to lack the support it needs to flourish.
The midwifery model of care, practiced widely and successfully in other nations, remains underutilized and under-supported in the United States. A 2019 study comparing low-risk pregnant patients of midwives and obstetricians at 11 different hospitals found that midwifery patients had significantly lower intervention rates, including an approximately 30-40% lower risk of C-sections.
In states where there is improved access to midwives, there are also significantly lower rates of surgical births, preterm babies and low infant birth weight. Mid-

wives have been consistently shown to provide better quality care and attention and improve mortality rates, so why are they still seen as a “cottage industry” in the U.S.?
While the overall big business of birth is flailing, midwives are on the ground in their communities and making improvements. Nowhere is this more important than areas where perinatal care is few and far between, particularly in the South, which is home to the nation’s highest maternal mortality rates.
In southeastern Florida, the Southern Birth Justice Network operates a Mobile Midwife Clinic to bring care directly to expectant mothers. And in Alabama, the state with the highest maternal mortality rate, midwife Stephanie Mitchell created the state’s first midwife-led, freestanding birth center, offering a radically more supportive, accessible model of care. These aren’t fringe efforts. They’re lifelines.
Despite the knowledge that midwives are crucial to addressing this crisis, right now in the U.S., OB-GYNs outnumber midwives three
to one. In New Zealand—a country with one of the lowest maternal mortality rates globally—there are 46 midwives for every eight OB-GYNs attending a live birth. The difference is stark. The outcomes, even more so.
If our current system were a monopoly, it would be guilty of suppressing competition and innovation to the detriment of public health. It is not ser ving families. It is not protecting mothers. It is not saving lives.
The numbers are damning and the solutions are known, so the question remains: how many more women must die, be harmed or carry lifelong trauma before the U.S. embraces change?
Midwifery isn’t a silver bullet, but it is a proven, powerful part of the solution. To combat this crisis, we must welcome all hands on deck. The lives of our mothers—and the future they carry—depend on it. l
Longevity is the new buzzword in the wellness world. Want in? These ten science-based strategies can help you stay healthy and vibrant late into life.
by Heidi Godman and Vanessa Caceres ©
NUMBERS MATTER to Jan Sirota, a retired investment banker who lives in Sarasota, Florida. He recently celebrated 12 years of marriage, cycles 40 miles a day and races cars at 150 miles per hour in High Performance Driver Education events.
The number that doesn’t seem to matter? His age. Now 76, he says age is “irrelevant to me. There’s no reason to say that I’ll slow down because I’m getting older.”
Sirota isn’t the only one embracing longevity. In a world where aging is no longer viewed as an inevitable decline but instead a chapter to be optimized, more and more businesses and experts are focusing on helping people live longer, healthier lives. From Silicon Valley biohackers to supplement startups and global wellness brands, companies are jumping headfirst into the booming longevity movement.
This trend is being fueled by a growing understanding of aging as a biological process—one that might be slowed or even modified. Scientists now study aging with the same rigor once reserved for disease. And while the fountain of youth remains elusive, growing evidence suggests that lifestyle, diet and targeted interventions can meaningfully extend healthspan.
“Certainly genetics play a part in this, and then of course luck,” says Dr. Patricia Harris, clinical chief of the division of geriatrics at the David Geffen School of Medicine at UCLA. “However, I don’t want anyone to think we can’t fight destiny a little bit.”
Some physical and social changes are unavoidable with age. Muscle and bone mass decline. So do sex hormone levels, kidney function, mental sharpness and reaction time. Chronic illnesses such as cardiovascular disease or Type 2 diabetes may also develop as we get older.
And the social toll can be equally impactful. Retirement, adult children leaving home or the loss of close friends or a spouse can lead to isolation, loneliness and even depression—setting off a downward spiral.
“Loneliness is one of the biggest problems I see,” Harris says. “It leads to depression and a loss of motivation to manage health. People become sicker and frailer, which keeps them from getting out and socializing. It increases the risk for an early death.”
Longevity is measured in lifespan, or how long a person lives. But simply extending life without preserving quality is no longer the goal. Instead, the conversation is shifting to healthspan, or the number of years a person lives free of chronic illness, cognitive decline and physical dependency. It’s about adding life to your years, not just years to your life.
In the U.S., we’ve got room for improvement: The average American spends 12.4 years burdened by disease or disability before death. Is it possible to close that gap? Longevity-focused companies claim it is. From high-end supplements and personalized wearables to full-scale clinics offering $50,000 wellness plans, there’s no shortage of ways to invest in your future self.
But living longer doesn’t need to cost a fortune— and it’s not about getting lucky with your DNA. Genetics only account for about 25% of longevity. The rest? It’s lifestyle. Experts say that simple, consistent changes can yield powerful, lasting benefits. Read on for some of the top to focus on.
Research is increasingly demonstrating that the way you take care of yourself today may have a big effect on your health later in life. While there’s no magic formula, these science- and expert-backed strategies can boost your chances of living a healthy, long life.
1
“Time and again, studies show true benefits of not smoking, keeping weight down and keeping major health conditions like high blood pressure, heart disease or diabetes well controlled,” says Harris. If you haven’t already talked about ways you can improve your personal health numbers, book an appointment to have that conversation with your doctor. (Turns out, more people need to! Only 30% of Americans say they have discussed ways to age well and live longer with their doctor.)
Studies have shown that eating a healthy diet in midlife is associated with better health in our older years. “A Mediterranean-style diet is associated with longevity around the globe,” says Dr. Saket Saxena, a geriatrician at Cleveland Clinic. This includes a fair
amount of fruits, vegetables, legumes, seeds, nuts, olive oil and whole grains while keeping sugar, sweetened drinks, refined carbs, red meat and processed meats to a minimum.
One reason why the diet may help the aging process: It lowers inflammation markers and optimizes gut health. And the payoff of tweaking what’s on your plate is impressive: One study found that following a diet like this could extend lifespan by about 10 years.
Exercise reduces stress levels in our bodies, circulates oxygen to all tissues (which is good for the brain!) and builds up strength, so you’re at less risk for frailty and life-threatening falls, explains Harris. Plus, studies have linked midlife fitness with reduced odds for developing chronic disease (like Alzheimer’s disease, stroke and diabetes) later in life.
How much exercise do you need? The standard recommendation is 150 minutes per week of moderate intensity exercise, such as playing a game of tennis, gardening or walking briskly. But if that’s daunting, Harris says to consider that a goal to work toward, not an absolute. “If you get out and walk regularly for three minutes when you hadn’t been walking at all, that’s a real accomplishment.”
Research shows people who get seven to eight hours of sleep a day, go to bed as early as possible and get good quality sleep have longer healthspans than those who don’t. Consistency is also important. Going to bed at roughly the same time every night (so your circadian clock isn’t constantly disrupted) promotes healthy functioning into old age.
By staying socially active and connected to friends and loved ones, you may increase your lifespan and healthspan by about three years. It helps fight loneliness, depression and isolation. If you’re far from loved ones, join a club or volunteer to meet new friends. “The number of social interactions in a day or week improves life expectancy, even in people with heart disease and colon cancer,” Harris says. “It doesn’t have to be a best friend. It can be someone in a coffee shop or the person at the cash register in the grocery store.”
We can’t all race cars like Sirota, but we can try a new hobby, learn another language or take a class at a local college. Some universities allow retirees to audit classes for free, whether in-person or online. “Staying mentally active in some way staves off dementia,” Harris says. “It has to be something that continues to engage your brain as you get older.”
“Hearing impairment can lead to a decline in socialization and mental stimulation. This can have an impact on activity, leading to depression and isolation, which can cause functional decline and reduce longevity,” says Saxena. In fact, the risk of premature death is almost 25% lower for those who use hearing aids compared with people who never use them.
Chronic stress actually ages you from the inside out. Part of that is due to the fact that this ongoing stress raises inflammation throughout the body.
“People with higher levels of inflammation have a more limited life expectancy,” Harris says. To ease stress, try meditating or doing stress-relieving exercises like yoga or tai chi. The good news? Your “biological age” can actually reverse when you reduce stress. Whether it’s travel, games, walks or a chat with friends, find what calms you—and stick with it.
Greater purpose in life has been linked with a lower risk of stroke, better sleep, healthier weight, higher physical activity levels and lower inflammation in some people. It’s also associated with a reduced risk of cognitive decline and Alzheimer’s disease.
Sirota, who is passing on his business experience to enterprising high schoolers, says this approach to life just makes him feel good. “It gives me incredible joy to help kids,” he says. You can live with purpose by volunteering, helping a family member or doing anything that gives you meaning.
“Extended UV radiation exposure over a lifetime can cause so much DNA damage that it hastens cell aging throughout the body,” says Dr. S. Manjula Jegasothy, an aesthetic dermatologist and clinical associate professor of dermatology at the University of Miami’s Miller School of Medicine and founder of the Miami Skin Institute.
UV exposure also increases the risk of skin cancer. And from an appearance standpoint, UV exposure ages the skin. To stay safe, limit your time in the sun (especially between 10 a.m. and 2 p.m.), wear protective clothing and apply a broad-spectrum sunscreen with an SPF of 15 or higher regularly l
IT MAY NOT LOOK LIKE MUCH , but one move could reveal a lot about your long-term health. Called the sit-rise test, this (seemingly!) simple challenge asks you to lower yourself to the floor, then stand back up without bracing on your hands, knees, arms or any other support.
In a 12-year study, researchers found that adults who could perform the test unaided had markedly lower risks of early death, especially from heart-related causes, than those who needed help getting up.
Why? This single move checks multiple boxes tied to healthy aging: strength, balance, flexibility and coordination.
The test is easy to try at home—just make sure you’re in a clear, safe space. Can you do it? Whether the answer is yes, no or almost, the insight it offers is worth noting. Think of it as a quick, at-home check-in on your mobility—and a motivator to keep building strength and stability as you age.
Average life expectancy for women in the U.S. 81.1 Years For men, about 5.3 years less. 75.8 Years
The “healthspan gap”: the difference between total lifespan and years lived in good health. 12.4 Years
LIFESTYLE THAT MATTERS
Portion of longevity determined by genes; the rest is shaped by lifestyle and environment.


The number of Americans who say they have discussed longevity with their doctor. Let’s bump up that number—talk to your physician about what you can do to age well at your next appointment.














Staying socially active and connected to friends and loved ones may increase lifespan and healthspan by about three years.




Volunteering 100 hours per year or more is linked to a lower risk of premature death compared to their peers who did not volunteer.


150–300 MINUTES/WEEK
Recommended amount of moderate-intensity exercise for longevity. 7–8 HOURS IDEAL NIGHTLY SLEEP to reduce risk of early death. 25%
A lack of social connection can increase the risk for premature death as much as smoking up to 15 cigarettes a day. NURSING HOME? of Americans 50+ who would like to stay in their homes as they age 75%




of consumers have purchased healthy aging products or services
$455.4 BILLION
The estimated global anti-aging market size by 2030 of Americans take vitamins or supplements specifically for longevity. 58% 70%
Raising a glass to good health is doing just the opposite.
by Chuck Ingoglia, president and CEO of the National Council for Mental Wellbeing, and Johna Burdeos ©
WHETHER IT’S A CASUAL GLASS OF WINE at dinner or a weekend cocktail with friends, alcohol is a big part of how many of us relax, socialize and unwind. But as new research and health advisories emerge, it’s becoming increasingly clear that the effects of alcohol on our health may be far more serious than we’ve been led to believe, and we may want to rethink our happy hour habit.
In early 2025, then-U.S. Surgeon General Vivek Murthy raised the alarm about alcohol’s link to at least seven kinds of cancer and called for a new health warning on alcoholic beverages. It might be the most consequential public health report since the surgeon general warned about the dangers of cigarettes in 1964.
Why did Murthy’s warning come now? About 178,000 people in the U.S. died from excessive drinking in 2021, compared with 138,000 in 2016, according to the most recent data from the Centers for Disease Control and Prevention. That increase of nearly 30% makes alcohol one of the leading causes of preventable death in this country.
So how much is really too much? And is it true that red wine is actually

good for your heart? Let’s unpack the facts, the myths and the new science that could change how you think about drinking—for good.
Alcohol and
What the Experts Say
You’ve likely already heard that alcohol is linked to liver disease. But what some people don’t realize is that drinking alcohol is associated with many other health

risks. In fact, alcohol is classified as a Group 1 carcinogen—or something that can cause cancer.
According to Dr. Michael Siegel, a professor at Tufts University School of Medicine, alcohol isn’t just a carcinogen, it’s a strong one: “It is in the same category as asbestos, benzene, arsenic, radiation, tobacco, vinyl chloride and plutonium.”
You don’t have to be a heavy drinker to raise your risk of cancer. The U.S. Surgeon General’s advisory says that even one drink a day or less can increase the likelihood of developing certain cancers, including breast (in women), colorectal, esophageal, liver, mouth, throat and voice box.
Why is that? When you drink alcohol, your body breaks it down into a chemical called acetaldehyde, which is a known carcinogen, explains Dr. Nishan Tchekmedyian, deputy physician-in-chief at City of Hope in Orange County, California. “Acetaldehyde can damage DNA and may lead to tumor growth, as well as cell and liver damage.”
And there are other ways that alcohol causes cancer: It produces harmful molecules that increase inflammation and changes hormone levels, including estrogen, which can increase the risk of
breast cancer. Additionally, alcohol can absorb toxic chemicals, like tobacco smoke, making it easier for them to enter the body and increase the risk of mouth and throat cancers.
Drinking doesn’t just raise your cancer risk—it impacts nearly every system in your body:
• Brain: Alcohol disrupts brain communication, affecting your mood, behavior, thinking and coordination. It can kill or damage brain cells, and while acute injury may not be harmful, repeated daily consumption can lead to neurological impairment, explains Siegel.
• Heart: Drinking heavily over time or on one occasion can damage the heart, leading to issues like weakened heart muscles, irregular heartbeat, high blood pressure and stroke.
• Liver Alcohol causes liver injury, which is reversible and


temporary, but not if you continue to drink large amounts chronically, says Siegel. Heavy drinking can lead to long-term liver-related conditions like fatty liver, alcoholic hepatitis, fibrosis and cirrhosis.
• Digestive System: Drinking can weaken the gut lining and disrupt healthy gut bacteria. Alcohol affects the pancreas by triggering toxic substances that may lead to pancreatitis, a painful condition that causes swelling and impairs digestion.
• Immune System: Alcohol weakens your immune system, says Dr. Raj Dasgupta, associate program director of internal medicine at Huntington Health Hospital in California. Chronic drinkers have a higher risk of infections like pneumonia and tuberculosis, but even one episode of heavy drinking can lower immunity for up to 24 hours.
• Mental Health: Alcohol increases your risk for mental health issues like anxiety and depression. It also raises the risk of dependency, accidents and strained relationships over time, adds Dasgupta.


First, some people should avoid alcohol altogether. This includes: those under the age of 21, pregnant women, individuals taking medications that interact with alcohol, those who experience facial flushing or dizziness with alcohol and people with health conditions like high blood pressure and diabetes.












You’ve probably heard that red wine is “heart healthy” because of antioxidants like resveratrol. But that claim is far murkier than it seems. “Cancer risk factors don’t discriminate between types of alcoholic beverages,” says Dr. Tchekmedyian. Even if red wine has antioxidants, the alcohol it contains still increases your cancer risk. Plus, you can get the same antioxidants from foods like grapes, peanuts, blueberries and spinach—without the health risks.
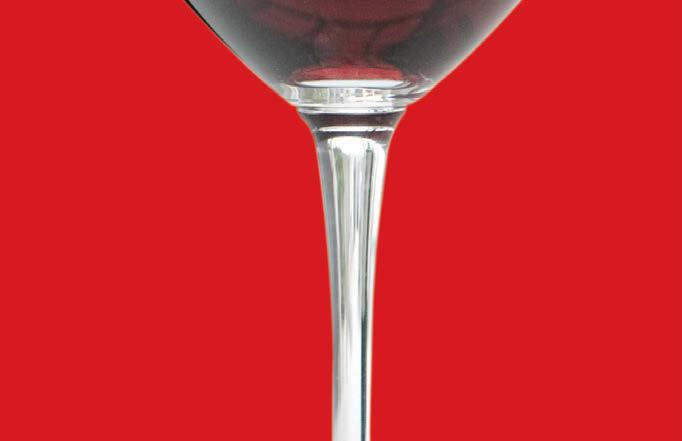





For healthy adults who choose to drink and do not fall into these groups, the U.S. Dietary Guidelines suggest that risks may be minimized by limiting intake to one drink or less per day for women and two drinks or less per day for men. This difference exists because women generally process alcohol differently, leading to higher blood alcohol levels and increased health risks, even with less alcohol, explains Dasgupta.
However, Dasgupta points out that “no type of alcohol is truly ‘healthy,’ but some choices are less risky than others.” Drinks with lower alcohol content and fewer sugars or additives might reduce certain risks, but “drinking less overall is what really matters.”
Still, the guideline is no longer tenable, according to Siegel, given the finding that moderate drinking increases cancer risk. “The new recommendation will likely be for people to avoid alcohol to reduce cancer risk.”
If you or someone you love has struggled to cut back on drinking, know that you are not alone. Nearly
29 million Americans live with what’s known as alcohol use disorder (AUD)—a medical condition where someone can’t control their drinking, even when it causes problems at work, in relationships or to their health.
And here’s something most people don’t realize: there are FDA-approved medications that can help. Three drugs are specifically approved to treat AUD are naltrexone (which reduces cravings and blocks the “reward” feeling from alcohol), acamprosate (which eases cravings and helps people maintain abstinence) and disulfiram (which causes unpleasant reactions like flushing and nausea if alcohol is consumed). Other medications like gabapentin and topiramate, originally used for conditions like seizures, also show promise.
Recently, even popular weight-loss drugs like Ozempic and Wegovy have been studied for alcohol reduction. One study found that people taking semaglutide, the active ingredient in both drugs, drank significantly less and even reduced cigarette use.
So why aren’t more people getting help? Experts believe there’s still a strong bias toward abstinence-only or counseling-based recovery. But just like you wouldn’t treat diabetes without insulin, many believe willpower isn’t enough to overcome a condition, and medication should be part of the conversation for treating alcohol misuse.
You don’t have to hit “rock bottom” to take a second look at your drinking habits. If you’ve noticed any of the following, it might be time to reassess: If you’re drinking more or longer than you planned; thinking about drinking constantly; drinking even though it causes problems at work or home; feeling anxious or low when you’re not drinking; or needing more alcohol to feel the same effect.
The good news? Any reduction helps. As Dr. Dasgupta puts it: “The truth is, any reduction in drinking can have positive effects on your health. And if you choose not to drink at all, that’s not just okay; it’s a really healthy choice.”

The current U.S. Dietary Guidelines suggest up to one drink per day for women and up to two drinks per day for men. But what does that look like? In the U.S., a standard drink contains 0.6 ounces of pure alcohol, which equals: 5 oz


As more people become aware of the risks associated with drinking, many are rethinking alcohol’s role in their lives altogether. Enter the growing non-alcoholic movement, a cultural shift that’s turning “sober curious” into a mainstream lifestyle. Drinking less has become popular among younger generations especially, with one survey reporting that 61% of Gen Z and 49% of millennials are trying to drink less.
From zero-proof spirits and craft non-alcoholic beers to sophisticated mocktail menus at high-end restaurants, the options for those choosing to skip alcohol have never been more appealing—or more socially acceptable. “Experimenting with these alternatives can make going alcohol-free feel fun rather than restrictive,” says Millie Gooch, founder of the sober community Sober Girls Society. “You still get the ritual of a nice drink without any of the downsides, which makes social events feel just as celebratory.”
Social media has amplified this message, with influencers and everyday people sharing their “sober journeys,” reframing sobriety not as deprivation but as self-care. And alcohol-free challenges like Dry January and Sober October have helped normalize experimentation, giving people permission to step back and reflect on their relationship with drinking—without pressure or stigma.
Ultimately, the non-alcoholic movement isn’t just about what’s in your glass—it’s about redefining celebration, connection and wellbeing in ways that don’t compromise your health. l
If you’re concerned about your drinking or want to explore treatment options, you can reach out to the Substance Abuse and Mental Health Services Administration hotline (1-800-662HELP), Alcoholics Anonymous (aa.org) or SMART Recovery peer support groups (smartrecovery.org).








As the global professional organization for the entire cardiovascular care team, the American College of Cardiology (ACC) is committed to supporting patients, caregivers and health care professionals by ensuring the highest quality care is delivered to every patient, every time.




ACC Accreditation Services™






ACC Accreditation Services is helping hospitals and health systems improve cardiovascular care processes and patient outcomes to achieve the highest standard of cardiac care. All of the essential components of true process improvement are embedded in ACC’s accreditation programs.

NCDR® (National Cardiovascular Data Registry)
ACC’s suite of NCDR registries is helping hospitals, health systems, centers and practices by providing data-driven insights, analysis and research to inform clinical and operational decisions, allowing the cardiovascular care team to perform at the highest level and to deliver optimal care to every patient, every time.
MedAxiom
MedAxiom, a member-driven network powered by data, is the premier source for cardiovascular organizational performance solutions.






















Registry
The following pages list more than 2,000 hospitals, centers and health systems that rely on ACC’s NCDR and Accreditation Services. Patients and caregivers can trust hospitals and centers that participate in the NCDR, receive the ACC’s Accreditation seal of approval, and are recognized with the Chest Pain – MI Registry™ Performance Achievement Award and the HeartCARE Center™ Award for delivering the best cardiovascular patient care.
The following pages list more than 2,000 hospitals, centers and health systems that rely on ACC’s NCDR and Accreditation Services. Patients and caregivers can trust hospitals and centers that participate in the NCDR, receive the ACC’s Accreditation seal of approval, and are recognized with the Chest Pain – MI Registry™ Performance Achievement Award and the HeartCARE Center™ Award for delivering the best cardiovascular patient care.


Cardiac Cath Lab Accreditation
CardiacCathLabAccreditation




CCChestPainCenterCerti fication

Helps facilities implement all the pre-, peri- and post-procedures that are essential for safe care and efficient scheduling of patients through the cath lab.
Helps fac ilities implement all the pre-, peri- and post-procedures that are essential for safe care and cient sc heduling of patients ough the c at h lab.


™yrtsigeR
CC Chest Pain Center Certification Supports Critical Access Hospitals and FreeStanding EDs in employing scientifically sound quality initiatives and best practices.
HF Heart Failure Accreditation
HFHeartFailureAccreditation
Supports Critical Access Hospitals and FreeStanding EDs in employing sc ienti fically sound quality initiatives and best practices.
EP Electrophysiology Accreditation
EPElectrophysiologyAccreditation
Ensures that requisite protocols, processes and systems are established in the care of patients with heart failure.
Ensures that requisite protocols, processes and systems are established in the care of patients with heart failure.
TV Transcatheter Valve Certification
TVTranscatheterValveCerti fication

Chest Pain Center Accreditation
ChestPainCenterAccreditation



Focuses on efficient and effective emergency care of acute coronary syndrome (ACS) patients in the hospital setting.

Focuses on ef ficient and effective emergency care of acute coronary syndrome (ACS) patients in the spital setting.


Incorporates the most recently compiled guidelines and expert consensus statements to produce the best possible care for the EP patient.
Incorporates the most recentl y compiled guidelines and expert cons ensus statements to produce the best possible care for the EP patient.
Helps hospital’s multidisciplinary teams meet standards for formalized and shared decision-making in performance of transcatheter valve replacement and repair procedures.
Helps hospital’s mult idisciplinary teams meet standards for for malized and shared decision- making in performance of transc at heter valve replacement and repair procedures.

AFib Ablation Registry™








E EP Device Implant Registry™
Q CPCAytilauQ™krowteN
Q ACPC Quality Network™

ablation procedures) Assesses the valence, demographics, acute management and outcomes of (AFib) catheter ablation procedures.
(Catheter-based atrial fibrillation ablation procedures) Assesses the prevalence, demographics, acute management and outcomes of patients undergoing atrial fibrillation (AFib) catheter ablation procedures.
(Implantable cardioverter defibrillator and pacemaker procedures)
and pacemaker procedures)
A quality program designed for data collection and collaboration among congenital heart disease centers to improve the quality of care for patients.
A quality program designed for data collection and collaboration among congenital heart disease centers to improve the quality of care for patients.


yrtsigeRICPhtaC®
CathPCI Registry®





(Diagnostic cardiac catheterization and percutaneous coronary intervention)

Assesses the characteristics, treatments and outcomes of cardiovascular disease patients who receive diagnostic catheterization and/or PCI procedures.
(Diagnostic cardiac catheterization and percutaneous coronary intervention) Assesses the characteristics, treatments and outcomes of rdiovascular disease patients who receive diagnostic catheterization and/or PCI procedures.
CP Chest Pain — MI Registry™
CPChestPain—MIRegistry™
(Acute myocardial infarction treatment)
Is a risk-adjusted, outcomes-based quality improvement program for all patient s with chest pain.
(Acute myocardial infarction treatment) Is a risk-adjusted, outcomes-based quality improvement program for all patients with chest pain.
CVCVASCRegistrySuite™
CV CV ASC Registry Suite™
(Procedures performed in ambulatory surgery centers and o ce-based labs) O er big-picture reviews, at-aglance assessments and patient-level drilldowns on procedures such as diagnostic catheterization, PCI, and
(Procedures performed in ambulatory surgery centers and office-based labs) Offer big-picture reviews, at-aglance assessments and patient-level drilldowns on procedures such as diagnostic catheterization, PCI, and defibrillator and pacemaker implants.
Establishes a national standard for understanding patient characteristics, treatments, outcomes, device safety and the overall quality of care for ICD/ CRT-D and select novel pacemaker procedures.
Establishes a national standard for understanding patient characteristics, treatments, outcomes, device safety and the overall quality of care for ICD/ CRT-D and select novel pacemaker procedures.
IM IMPACT Registry®
IMIMPACTRegistry®
(Pediatric and adult congenital treatment procedures) Assesses the prevalence, demographics, management and outcomes of pediatric and adult congenital heart disease patients who undergo diagnostic catheterizations and catheter-based interventions.
(Pediatric and adult congenital treatment procedures) Assesses the prevalence, demographics, management and outcomes of pediatric and adult congenital heart disease patients who undergo diagnostic catheterizations and catheter-based interventions.
tsehCniaP—™yrtsigeR
Chest Pain — MI Registry™
Performance Achievement Award
PerformanceAchievementAward gnitapicitrap slatipsoh sezingoceR
Chest Pain – MI Registr y that have demonstrated sustained, top-level performance in quality of care and adherence to guideline recommendations.
Recognizes hospitals participating in Chest Pain – MI Registry that have demonstrated sustained, top-level performance in quality of care and adherence to guideline recommendations.
Platinum
L LAAO Registry™
LLAAORegistry™
T CCA/STSTVT™yrtsigeR
Gold
(Left atrial appendage occlusion procedures) Captures data on left atrial appendage occlusion (LAAO) procedures to assess real-world procedural outcomes, short and long-term safety, and comparative effectiveness.
(Left atrial appendage occlusion procedures) Captures data on left atrial appendage occlusion (LAAO) procedures to assess real-world procedural outcomes, short and long-term safety, and comparative e ectiveness.
T STS/ACC TVT Registry™
(Transcatheter valve therapy procedures) Monitors patient safety and real-world outcomes related to transcatheter valve replacement and repair procedures – plus emerging treatments for valve disease patients.
(Transcatheter valve therapy procedures) Monitors patient safety and real-world outcomes related to transcatheter valve replacement and repair procedures – plus emerging treatments for valve disease patients.
Silver
Silver
HeartCARECenter™
HeartCARE Center™
Recognizes hospitals that have demonstrated a commitment to world-class cardiovascular care through comprehensive process improvement, accredit at ion, professional excellence, and community engagement.
Recognizes hospitals that have demonstrated a commitment to world-class cardiovascular care through comprehensive process improvement, disease and procedure-specific accreditation, professional excellence, and community engagement.
Hospitals are listed by state and then by level of engagement with the ACC’s quality and process improvement programs.
Hospitals are listed by state and then by level of engagement with the ACC’s quality and process improvement programs.
Baptist Health
UAB St. Vincent’s
Abrazo Arizona Heart Hospital
Abrazo Arrowhead Campus
Canyon Vista Medical Center
Carondelet St. Mary’s Hospital
Mayo Clinic Arizona
Northwest Medical Center Houghton
Western Arizona Regional Medical Center
Yavapai Regional Medical Center
Yuma Regional Medical Center
Abrazo Central Campus
Abrazo Scottsdale Campus
Abrazo West Campus
Banner Boswell Medical Center......................
Banner Desert Medical Center
Banner Heart Hospital
Banner University Medical Center
Banner University Medical Center
HonorHealth – Deer Valley Medical Center
Valley View Medical Center
Banner Estrella Medical Center
Carondelet St. Joseph’s Hospital
Cobre Valley Regional Medical Center
– Scottsdale Osborn
Regional Medical Center
Children’s Hospital
Valley
CHI St. Vincent Infirmary
Health Fort Smith
Health System of
Marian Regional Medical Center
Mills-Peninsula Medical Center
NorthBay Medical Center.................
Palomar Medical Center ..................
Saint Agnes Medical Center
UC Irvine Health .................................
Adventist Health St. Helena
Cedars-Sinai Health Systems
Community Hospital of the Monterey Peninsula
Community Medical Center – Clovis
Community Memorial Hospital
Desert Regional Medical Center
Dignity Health St. Joseph’s
Center
Emanate Health Medical Center
French Hospital Medical Center
Fresno Community Hospital and Medical Center ...............................
Fresno Heart and Surgical
Kaweah Health
Keck Medical Center of
Los Robles Hospital & Medical Center
MemorialCare Long Beach
Providence St. Joseph
Salinas Valley Health
Hospital ....................................
Sharp Memorial Hospital
Shasta Regional Medical
St. John’s Regional
Adventist Health Glendale
Henry Mayo Newhall
John Muir Medical Center
Kaiser Permanente Fontana
Kaiser Permanente Los Angeles Medical Center
Kaiser Permanente San Francisco Medical Center
Kaiser Permanente Santa Clara Medical Center
Lucile Packard Children’s Hospital at Stanford University ..................................
Marin Health Medical Center
MemorialCare Orange Coast Medical Center
MemorialCare Saddleback Medical Center
Northridge Hospital Medical Center
PIH Health Good Samaritan Hospital
Providence Mission Hospital Medical Center
Providence Saint John’s Health Center
San Antonio Regional Hospital
Santa Barbara Cottage Hospital
Santa Rosa Memorial Hospital ..................
Scripps Memorial Hospital – La Jolla
Scripps Mercy Hospital – San Diego
Sharp Chula Vista Medical Center
Sharp Grossmont Hospital .........................
Sutter Santa Rosa Regional Hospital .......
UCLA West Valley Medical Center
White Memorial Medical Center
Adventist Health Sonora...................................
Children’s Hospital of Orange County
Dignity Health Dominican Hospital
Glendale Memorial Hospital and Health Center ..............................................
John F. Kennedy Memorial Hospital
Kaiser Permanente Downey
Center
Kaiser Permanente Irvine Medical Center....
Kaiser Permanente Oakland
Center
Kaiser Permanente Orange County-Anaheim
Center
Lakewood Regional Medical Center
Martin Luther King Jr. Community
Palmdale Regional Medical Center
PIH Health Whittier Hospital ............................
Providence Little Company of Mary Medical Center ....................................
Providence Saint Joseph Medical Center
Providence St. Jude Medical Center
Rady Children’s Hospital – San


















Intermountain Health St.
CommonSpirit St. Anthony
Hospital
Intermountain Health
Good Samaritan Hospital
Intermountain Health Platte Valley Hospital
UCHealth
Avista
Francis Hospital
Bayhealth Hospital,
Campus
Beebe Healthcare...................................
Nemours Children’s Health
St. Francis Hospital
Bayhealth Hospital, Sussex Campus
TidalHealth Nanticoke
George Washington University Hospital
MedStar Washington
AdventHealth
Cleveland Clinic
Indian River Hospital
AdventHealth Carrollwood
AdventHealth Heart of Florida
AdventHealth Sebring
AdventHealth Wesley Chapel
AdventHealth Zephyrhills
AdventHealth Dade City
AdventHealth North Pinellas
Manatee Memorial Hospital
Memorial Regional Hospital
South Broward Hospital
St. Joseph’s & St. Joseph’s
Children’s Hospitals
Tallahassee Memorial
Health Jacksonville
HCA Florida West Hospital
Lakeland Regional Health
Center
Morton Plant Hospital
of Central
University of CT Health Center John Dempsey Hospital
Orlando
Health Medical Center
HCA
Jupiter
Lakewood
Mount
Palmetto General
Santa
Tampa
Tampa General Hospital
Tampa General Hospital
UF
Bartow
Broward
Florida Medical Center, a Campus of North
HCA
HCA
HCA
Jackson
Johns
Lower
HCA Florida St. Lucie
HCA Florida Trinity
Heart & Vascular Ambulatory
Jackson West Medical
Lee Health – Golisano Children’s Hospital
Memorial Hospital West/South Broward
Nemours Children’s Hospital
North Shore Medical Center
Bay Hospital ....................................................
Sarasota Memorial Hospital
South Lake Hospital ................................................
South Miami Ambulatory Surgery Center
St. Cloud Regional Medical Center
UCF Lake Nona Medical Center ..........................
West Kendall Baptist Hospital ..............................
Wolfson Children’s Hospital
GEORGIA
Hamilton Medical
Wellstar MCG
Piedmont Augusta ..................
St. Joseph’s Hospital
Memorial Health University
Center
Atrium Health Navicent
The Medical Center ................................
Emory University Hospital Midtown
Northeast Georgia Health System
Phoebe Putney Memorial Hospital
South Georgia Medical Center
Southern Regional Medical Center......
St. Mary’s Health Care Systems
Wellstar Kennestone Regional
Center
Coffee Regional Medical Center
Emory Saint Joseph’s Hospital
Emory University
HCA Houston Healthcare
Robins


















St. Luke’s Magic
Riverside
OSF
Rush-Copley
OSF HealthCare
Rush Oak Park Hospital ................................
Rush University Medical Center
Saint Joseph Medical Center Joliet
UChicago Medicine AdventHealth
Hinsdale
Advocate Condell Medical Center
Advocate Good Shepherd Hospital
Anderson Hospital
Ascension Saint Mary Hospital........................
Deaconess Regional Healthcare
Genesis Medical Center, Silvis ........................
Gottlieb Memorial Hospital .............................
John H. Stroger Jr. Hospital of Cook County ..................................................
Lurie Children’s Hospital of Chicago
Mount Sinai Hospital..........................................
Sarah Bush Lincoln Health Center
Silver Cross Hospital ..........................................
UW Health SwedishAmerican Hospital
Advocate Children’s Hospital Oak Lawn
Advocate South Suburban Hospital
Trinity Hospital ......................................
OSF
Mercyhealth Javon Bea
Northwestern Memorial
Memorial Hospital........................................
Health Saint Francis Hospital of
Coordinated care for post-discharge heart failure treatment is essential to your quality of life. That’s why we advocate the Partner in Care approach. Find health care facilities, outpatient clinics and medical practices that are committed to the best patient outcomes and display these ACC Heart Failure Accreditation seals.
Hackensack University Medical Center
Hackensack, NJ
Outpatient Services Partner: JSUMC Advanced Heart Failure Center Neptune City, NJ
JFK University Medical Center Edison, NJ
Outpatient Services Partner: JFK Cardiovascular Clinic
AdventHealth Tampa Tampa, FL
Outpatient Services Partner: Florida Hospital Physician Group
Augusta Health Fishersville, VA
Outpatient Services Partner: Augusta Health Heart Failure Clinic
Baptist Health Paducah Paducah, KY
Outpatient Services Partner: Baptist Health Paducah Heart Failure Clinic
CHI St. Luke’s Health Memorial Lufkin Lufkin, TX
Outpatient Services Partner: The Heart Institute of East Texas
East Jefferson General Hospital Metairie, LA
Outpatient Services Partner: East Jefferson Heart Clinic

King’s Daughters Medical Center Ashland, KY
Outpatient Services Partner: King’s Daughters Structural and Heart Failure Clinic
Methodist Le Bonheur Germantown Hospital Germantown, TN
Outpatient Services Partner: Sutherland Cardiology Clinic
Methodist University Hospital Memphis, TN
Outpatient Services Partner: University of TN Medical Group Cardiology – Methodist University
Novant Health New Hanover Regional Center Wilmington, NC
United Regional Health Care System Wichita Falls, TX
Outpatient Services Partner: United Regional Health Care System
Lutheran Hospital of Indiana Fort Wayne, IN
Outpatient Services Partner: Lutheran Hospital Advanced Heart Failure Clinic
Trinity Health Ann Arbor Hospital Ann Arbor, MI
Outpatient Services Partner: Trinity Health Michigan Heart
Outpatient Services Partner: Novant Health Heart & Vascular Institute – Wilmington Main
Spartanburg Medical Center Spartanburg, SC
Outpatient Services Partners: Heart Failure Clinic Cherokee Medical Center Gaffney, SC
Heart Failure Clinic Pelham Medical Center
Greer, SC
Heart Failure Clinic Spartanburg Medical Center
Spartanburg, SC
Heart Failure Clinic Union Medical Center Union, SC
Billings Clinic Billings, MT
Outpatient Services Partner: Billings Clinic Heart Failure and Recovery Clinic
Loma Linda University Medical Center Loma Linda, CA
Outpatient Services Partner: International Heart Institute Outpatient Clinic
Renown Medical Center Reno, NV
Outpatient Services Partner: Heart Failure Program at Renown





















Medical
Mercy Health Lourdes Hospital
Norton Hospital
Saint Joseph East
Baptist Health Corbin
Baptist Health Hardin
Ephraim McDowell
Regional Medical Center
Saint Elizabeth Healthcare
Edgewood
Saint Joseph London
St. Claire Regional Medical Center
Clark Regional Medical Center
Harrison Memorial Hospital
Lake Cumberland Regional Hospital
Meadowview Regional Medical Center
Norton Brownsboro Hospital
Owensboro Health Regional Hospital
T.J. Regional Health
University of Louisville Health –
South Hospital
Baptist Health Deaconess Madisonville,
Baptist Health Richmond
Frankfort Regional Medical Center................
Greenview Regional Hospital
Highlands ARH Regional Medical Center
Murray Calloway County Hospital
Norton Women’s and Children’s Hospital
Sts. Mary & Elizabeth Hospital
Bluegrass Community Hospital
Ephraim McDowell Fort Logan Hospital
Ephraim McDowell James B. Haggin Hospital..
Fleming County Hospital
Georgetown Community Hospital
Hazard ARH Regional Medical Center
Jackson Purchase Medical Center
Norton Children’s Hospital
View Hospital
The Medical Center at Russellville
Three Rivers Medical Center
of Louisville Hospital
UofL Health Shelbyville Hospital
LOUISIANA CHRISTUS Ochsner
University of
Corewell Health, Grand
Marquette
Trinity Health
McLaren Greater Lansing
MyMichigan Medical
Midland
Trinity Health Muskegon
Henry Ford Macomb Hospital
McLaren Bay Region ..............................
McLaren Flint ...........................................
McLaren Macomb ..................................
McLaren Northern Michigan
Trinity Health Oakland Hospital
Ascension Genesys Hospital .....................
Ascension Providence Hospital
Southfield
Ascension St. John Hospital ......................
Borgess Medical Center .............................
Bronson Methodist Hospital......................
Corewell Health, Dearborn ........................
Corewell Health, Lakeland Hospitals
St. Joseph Hospital ......................................
Corewell Health, Royal Oak .......................
Corewell Health, Troy ..................................
Covenant Healthcare
Harper University Hospital .........................
Henry Ford Health ........................................
Henry Ford Jackson Hospital
McLaren Port Huron Hospital ....................
Michigan Medicine
Munson Medical Center .............................
MyMichigan Medical Center Saginaw
University of Michigan Health – Sparrow
University of Michigan Health – West ......
Ascension Providence Rochester
City Hospital
Hospital
Regional Hospital
MyMichigan Medical Center Alpena
Trinity Health Grand Rapids Hospital
Trinity Health Livonia Hospital.........................
Ascension


















Progress West Healthcare
SSM Health Cardinal Glennon
Children’s Medical
SSM Health St. Clare Hospital
Fenton
SSM Health St. Mary’s Hospital – St. Louis
SSM St. Joseph Hospital – St. Charles
SSM St. Joseph Hospital West
St. Louis Children’s Hospital
St. Luke’s Des Peres Hospital
Intermountain Health St. Vincent
Hospital
Medical Center
Health
Children’s Mercy Kansas
Citizens Memorial Hospital
Saint Luke’s East Hospital
Luke’s Northland Hospital
SSM Health DePaul Hospital – St.
SSM Health St. Mary’s Hospital –
City
Cooperman
St. Francis Hospital and
New York-Presbyterian
New York-Presbyterian
Weill Cornell Medical Center
St. Joseph’s Hospital ....................
Cayuga Medical Center at Ithaca
Stony Brook University Hospital
Vassar Brothers Medical Center
Westchester County Health Care Corp. .............................
Wyckoff Heights Medical Center
Bassett Medical Center.........................
Buffalo General Medical Center,
Gates Vascular Institute..........................
Garnet Health ..........................................
Good Samaritan Hospital .....................
Jamaica Hospital Medical Center .......
Mercy Hospital of Buffalo .....................
Montefiore Medical Center..................
Mount Sinai Hospital Morningside ....
New York-Presbyterian Brooklyn
Methodist Hospital.................................
New York-Presbyterian Columbia
University Irving Medical Center
NYU Langone Health – Tisch Hospital
UPMC Chautauqua .................................
Upstate Medical University, SUNY .....
Albany Medical Center Hospital...............
Arnot Ogden Medical Center ...................
Ellis Hospital...................................................
Good Samaritan University Hospital
Maimonides Medical Center Division of Cardiology
New York-Presbyterian Westchester .......
Northwell Health Lenox Hill Hospital.......
Northwell Health North Shore
University Hospital .......................................
Northwell Health Staten Island Hospital
NYU Langone Hospital – Long Island
Richmond University Medical Center.......
Rochester Regional Health System
South Shore University Hospital ...............
St. Peter’s Hospital........................................


















Trinity Medical Center
Cleveland Clinic Mercy Hospital.........
Lima Memorial Health System..............
Marietta Memorial Hospital
Mercy Health St. Rita’s Medical Center
Miami Valley Hospital
Mount Carmel East ................................
Saint Elizabeth Youngstown Hospital
Springfield Regional Medical Center
The Christ Hospital Health Network
Adena Regional Medical Center
Blanchard Valley Hospital............................
Genesis Hospital...........................................
Good Samaritan Hospital
Grant Medical Center ..................................
Kettering Health Dayton
Kettering Health Main Campus.................
Community Hospital ..........................
Lake West Medical Center
Mercy Health Fairfield Hospital
OhioHealth Mansfield Hospital
Riverside Methodist Hospital
The Ohio State University Wexner
Center
Hospitals
Center
University Hospitals Elyria
Center
The American College of Cardiology (ACC) thanks Emergency Medical Service (EMS) professionals for your vital role in caring for patients, including those with heart attacks and other heart-related emergencies. We are especially proud of the EMS agencies that partner with the ACC through our Accredited and Certified Chest Pain Centers and Chest Pain – MI Registry™ to advance our mission of transforming cardiovascular care and improving heart health for all. Your dedication helps ensure the best possible outcome for every patient, no matter where an emergency occurs.
Adair County Ambulance District
Northeast Regional Medical Center
American Medical Response, Inc.
Eastern New Mexico Medical Center
Anderson County Emergency Medical Services –
Anderson County EMS
AnMed
Atrium Health Floyd EMS
Atrium Health Floyd Medical Center
Bath Township Fire Department
Lima Memorial Health System
Beacon Hose Company #1
Waterbury Hospital
Bi-County Ambulance
Adventist Health and Rideout
Broken Arrow Fire Department EMS
Hillcrest Hospital South
Brownsville EMS
Valley Regional Medical Center
Brownsville Fire Department
Valley Baptist Medical Center Brownsville
Cabell County EMS
St. Mary’s Medical Center
Carroll County Fire-Rescue
Twin County Regional Hospital
Cathedral City Fire Department
Desert Regional Medical Center
City of Henderson Fire Department
St. Rose Dominican Hospital Siena Campus
City of Russellville Office –
Russellville Fire Department
Saint Mary’s Regional Health System
Denison Fire Rescue
Texoma Medical Center
East Baton Rouge Parish
Our Lady of the Lake Regional MC
Galax-Grayson Emergency Medical Services
Twin County Regional Hospital
Germantown Fire Department
Methodist Le Bonheur Germantown
Global Medical Response/AMR –
Lifeguard Ambulance Services
HCA Florida West Hospital
Good Fellowship Ambulance
& EMS Training Institute Inc.
Chester County Hospital – Penn Medicine
Harrison County EMS
Harrison Memorial Hospital
KAMP Central Ambulance Services
Mon Health Preston Memorial Hospital
Lawrence County Ambulance Services –
Lawrence County EMS
Southern Tennessee Regional Health Systems –
Lawrenceburg
Lee County EMS
Carolina Pines Regional Medical Center
Leon County Emergency Medical Services
Tallahassee Memorial HealthCare
Lima Fire Department
Lima Memorial Health System
Medic Ambulance Services
NorthBay Medical Center
Mercy EMS
UP Health System Portage
Mercy Regional EMS
Baptist Health Paducah

Ambulance Authority – Central EMS
Fayetteville, AR
Washington Regional Medical Center
Metro EMS
Little Rock, AR
University of Arkansas For Medical Sciences
Unity Health White County Medical Center
CHI St. Vincent Infirmary
Montgomery County Fire & Rescue Service
Adventist HealthCare Shady Grove Medical Center
Morgan County Ambulance Service
Centura St. Elizabeth Hospital – Colorado Plains MC
Murrieta Fire & Rescue
Loma Linda University MC – Murrieta
Normal Fire Department
Carle BroMenn Medical Center
Norton Adult Transport/Norton Healthcare, Inc.
Norton Women’s & Children’s Hospital
Oakwood Fire and Rescue
Clinch Valley Medical Center
Pafford Medical Services
Saline Memorial Hospital
Pleasure Ridge Park Fire Protection District
Sts. Mary and Elizabeth Hospital
Ponca City Fire Department
AllianceHealth Ponca City
Pope County Arkansas –
Pope County Emergency Medical Services
Saint Mary’s Regional Health System
Porter Health Services LLC – Northwest Health EMS
Northwest Health Porter
Riverside Ambulance
Riverside Medical Center
Rural Metro of TN LP – American Medical Response
Prisma Health Blount Medical Center
Shreveport Fire Department
CHRISTUS Ochsner St. Patrick Hospital
Willis Knighton Health
CHRISTUS Highland Medical Center
Terra Alta Community Ambulance Squad, Inc.
Mon Health Preston Memorial Hospital
Town of Richlands – Richlands Fire Rescue
Clinch Valley Medical Center
West Feliciana Parish Hospital
Emergency Medical Services
West Feliciana Hospital
Whitesboro Fire Department
Texoma Medical Center
Winchester Fire and EMS
Winchester Medical Center
WVU Medicine – Camden Clark
WVU Medicine Camden Clark Medical Center
Baptist Health Medical Center – North Little Rock
Baptist Medical Center – Little Rock
Palm Beach Gardens Fire and Rescue
Palm Beach, FL
Jessamine County EMS
Nicholasville, KY
Baptist Health Lexington
Saint Joseph East
Saint Joseph Hospital
Professional Ambulance and Oxygen Services
Cambridge, MA
Powell Emergency Medical Service
Deer Lodge, MT
Union EMS
Monroe, NC
Atrium Health Pineville
Atrium Health Carolinas Medical Center
Novant Health Matthews Medical Center
Novant Health Presbyterian Medical Center
Iredell County EMS
Statesville, NC
Novant Health Huntersville Medical Center
Frye Regional Medical Center
Atrium Health Wake Forest Baptist Medical Center
Catawba Valley Medical Center
Atrium Health Carolinas Medical Center
Novant Health Presbyterian Medical Center
Atrium Health Cabarrus
City of Cleveland Ambulance Service
Cleveland, OH
Fairview Hospital
The MetroHealth System
EmergyCare Erie, PA
UPMC Passavant Hospital
Saint Vincent Health Center
UPMC Hamot
Meadville Medical Center
Sharon Regional Health System
Western Berks Ambulance Association
West Lawn, PA
Penn State Health St. Joseph
City of Sugar Land Fire – EMS
Sugar Land, TX
Houston Methodist Sugar Land Hospital
City of Pharr EMS
Pharr, TX
Doctors Hospital at Renaissance
Rio Grande Regional Hospital
McAllen Heart Hospital
Kanawha County EMS
Charleston, WV
Charleston Area Medical Center, Inc
St.
Mercy Fitzgerald Hospital
Penn State Health St. Joseph Medical Center
Hospital.......................
St. Luke’s University Health
The Guthrie Clinic
UPMC Passavant
UPMC Presbyterian
Westmoreland Regional Hospital
Allegheny General Hospital.................
Forbes Hospital
Geisinger Medical Center
Lehigh Valley Health Network
Lehigh Valley Health Network
Muhlenberg
Nazareth Hospital
Penn Medicine Lancaster
General Health
Penn State Hershey Medical Center
Saint Vincent Hospital
St. Clair Health
Temple University Hospital
UPMC Hanover
UPMC Memorial.......................................
UPMC Shadyside
UPMC West Shore
UPMC Williamsport................................
Wellspan York Hospital
Abington Memorial Hospital
Regional Medical Center
Hospital
Torresdale Hospital
Medical Center
Lehigh Valley Hospital – Pocono

Maury Regional Medical Center
Bristol Regional Medical Center
Cookeville Regional Medical
Methodist Hospital Germantown
Parkridge Medical Center
Prisma Health Blount
Hospital ....................................
Saint Francis Hospital .............................
Tennova Healthcare – Turkey Creek Medical Center
Vanderbilt Tullahoma –
Harton Hospital.........................................
Ascension Saint Thomas Hospital West..
Highpoint Health Sumner
With Ascension Saint Thomas ....................
Highpoint Health Winchester
With Ascension Saint Thomas
Memphis Hospital South .............................
Methodist Hospital North ...........................
St. Francis Bartlett ........................................
Tennova Healthcare – North Knoxville
Medical Center
TriStar Centennial Medical Center ...........
West Tennessee Healthcare Dyersburg Hospital.......................................
Ascension Saint Thomas Hospital Midtown
Bradley Medical Center ....................................
Emergency Room at Sumner Station.............
NorthCrest Medical Center .............................
Medical Center .................................
Regional Medical Center
Memorial

















Woodland Heights Medical Center
Ascension Providence Waco
Baptist Medical Center
Baylor Scott & White Medical Center
Baylor Scott & White Medical Center
Baylor Scott & White The Heart Hospital Plano
BSA Hospital, LLC
CHRISTUS Good Shepherd Medical Center
CHRISTUS Santa Rosa Hospital
New Braunfels
CHRISTUS Santa Rosa Hospital
Westover Hills
Corpus Christi Medical Center
North Central Baptist Hospital
Northeast Baptist Hospital
Seton Medical Center
Harker Heights
St. David’s South Austin Medical Center
St. Luke’s The Vintage Hospital
Tarrant County Hospital District
Texas Health Harris Methodist
Hospital Fort Worth
The University of Texas Medical Branch
Clear Lake Campus
University of Texas Medical Branch at Galveston
Ascension Seton Medical Center Austin
Baylor Scott & White All Saints Medical Center
Baylor Scott & White Medical Center
College Station
Baylor Scott & White Medical Center
Irving
Baylor Scott & White Medical Center
Lakeway
Houston Methodist
Memorial Hermann Memorial City Medical
Memorial Hermann Southeast Hospital
Memorial Hermann Southwest Hospital
Memorial Hermann The Woodlands
AdventHealth
Baylor Scott & White
The Heart Hospital Fort
Corpus Christi Medical Center
Baylor Scott & White The Heart Hospital
McKinney
CHI St Luke’s Sugar Land Hospital............
CHI St. Joseph Health Regional Hospital
CHI St. Luke’s Patients Medical Center
CHRISTUS San Marcos
Citizens Medical Center
Dallas Regional Medical Center.................
HCA Houston Healthcare West
Heart Hospital of Austin
Houston Methodist Baytown Hospital
Houston Methodist Clear Lake Hospital
Laredo Medical Center
Longview Regional Medical Center
Medical City Denton
Medical City Fort Worth
Memorial Hermann Northeast Hospital
Methodist Dallas Medical Center
Methodist Richardson Medical Center
Mission Trail Baptist Hospital
Palestine Regional Medical Center
Paris Regional Medical Center
Parkland Health & Hospital Systems
Resolute Health Hospital
Round Rock
Medical
Medical

Intermountain
Ogden
Timpanogos
Castleview
The University of Vermont
Carilion Roanoke
Hospital
Centra Lynchburg
General Hospital.................
Winchester Medical Center, Inc.
Inova Schar Heart and Vascular
Medical Campus.....................
VCU-Medical College of Virginia
Augusta Health
Chesapeake Regional
Center
LewisGale Medical Center
Sentara Norfolk
General Hospital...........................
Sentara Rockingham
Hospital ........................
SOVAH Health – Danville
VHC Health.....................................
CJW Medical Center ........................
Mary Washington Healthcare.........
Riverside Regional
Center
University of Virginia
Center
Bon Secours Memorial Regional Medical Center
Bon Secours Mercy Health
St. Mary’s Hospital ..................................
Inova Schar Heart and Vascular
Inova Alexandria Hospital
Inova Schar Heart and Vascular
Inova Loudoun Hospital
Johnston Memorial Hospital

























Take charge of your well-being and set yourself up for a healthier future




































































Mind-body therapies help you reframe awareness of pain, so you can learn to use your mind to control the discomfort.
by Jake Panasevich, E-RYT and Stacey Colino, ACE-CHC, MS
I©
N 2015, Lesley Paterson broke her shoulder during a practice run the day before the Costa Rica XTERRA triathlon. The injury caused her to lose the ability to use her arm. Not only did Paterson compete in the race, but she also crossed the finish line as the winner. Furthermore, the now five-time world champion triathlete battles with debilitating, chronic Lyme disease. She attributes her ability to persevere, despite experiencing mental and physical pain, to the power of her mind.
“It’s a mindset you develop across years and years,” says Paterson, who now works as an Oscar- and BAFTA-winning screenwriter and producer. “It’s something both you’re born with and you develop and cultivate. I’ve dealt with pain my whole life, or rather sought it out.”
Paterson’s ability to navigate pain by leveraging her thoughts is also backed by research. For decades, scientists, doctors and health professionals have researched the mind-body connection, or the way that our thoughts and emotions affect our physical health.
Ellen Langer, a professor of psychology at Harvard University and author of The Mindful Body: Thinking Our Way to Chronic Health, is renowned for her groundbreaking research on the connection between mind and body. In 1979, she conducted the pivotal “counterclockwise” study, in which elderly men were immersed in a retreat and lived as if they were 20 years younger. As a result, the men grew “younger” in
health-related measurements
“We had elderly men live there a week as if they were their younger selves. For example, they spoke of the past in the present tense,” Langer says. “In a period of time, less than a week, their vision, hearing, memory and strength all improved and they looked noticeably younger, without any medical intervention.”
This study is part of a larger body of research that illustrates what Langer calls “mind-body unity.” Other studies have shown that participants’ perceptions of time can accelerate healing and reduce fatigue, underscoring the interplay between mental states and physical well-being.
When Paterson broke her shoulder, she went through a mental, stepwise approach to continue her race, despite the pain she was experiencing.
“I had broken a shoulder. Of course I’m going to feel pain, but it’s something that you’ve trained your mindset to deal with,” Paterson says. “You break it down into small sections. You say, ‘I’m going to do the swim with one arm. If I get through that, and it’s okay, then we move onto the bike. If I manage to make it a mile on the bike, great.’”
Not only did this attitude help Paterson win the race, but it could have helped her manage her pain. Langer says that being
MANAGING chronic pain involves more than just addressing the physical symptoms; it requires a holistic approach that incorporates both the mind and body. Here are five effective ways to utilize mindbody techniques for managing chronic pain:
1 MINDFULNESS MEDITATION This practice involves focusing the mind on the present moment without judgment. For chronic pain sufferers, mindfulness meditation can help cultivate awareness of pain sensations without becoming overwhelmed by them. By observing pain without reacting emotionally, individuals can reduce the stress and anxiety often associated with chronic pain and, as a result, decrease the perception of pain intensity.
2 YOGA AND STRETCHING Specific yoga poses and stretches can target areas of the body affected by chronic pain, such as the back, neck or joints. The controlled movements and emphasis on deep breathing can reduce muscle tension, improve circulation and release endorphins, which are natural painkillers. Yoga also supports pain management by encouraging mindfulness and body awareness.
3 BIOFEEDBACK The technique uses electronic monitoring equipment to teach individuals how to control physiological processes such as heart rate, muscle tension and skin temperature. By learning to modify these responses through relaxation techniques, visualization or deep breathing, individuals can reduce pain levels and improve their sense of control over their condition.
4 COGNITIVE BEHAVIORAL THERAPY
CBT is a therapeutic approach that helps individuals identify and change negative thought patterns and behaviors. When applied to chronic pain management, CBT aims to modify the way patients perceive and respond to pain. Techniques such as cognitive restructuring (challenging negative beliefs about pain)
and relaxation training can help patients regain a sense of control and reduce the impact of pain on their daily lives. CBT also addresses factors such as depression and anxiety, which commonly accompany chronic pain and can exacerbate symptoms.
5 PROGRESSIVE MUSCLE RELAXATION
PMR involves tensing and then relaxing muscle groups in a systematic manner. This process helps release physical tension and promotes relaxation throughout the body. By practicing PMR regularly, people can learn to recognize and reduce muscle tension patterns that contribute to their pain. PMR is often combined with deep breathing exercises or guided imagery to enhance its effectiveness in managing pain and promoting overall relaxation.
mindful about making decisions leads to less pain and stress and, therefore, better overall health. This approach aligns with the idea that focusing on specific, achievable goals can empower individuals to overcome challenges. Research indicates that instead of telling someone to “try” a task, encouraging them to “do” it results in significantly better performance.
“Instead of wasting your time trying to make the right decision, make the decision right,” Langer says. “The stress from making decisions comes from the fear of not making the right decision. You can’t know what the right decision is because things are always changing. They look different from different perspectives. Make it work.”
Langer believes that being decisive in the language we use for terms like cancer remission also has a profound effect on the outcome. She says that remission has the built-in expectation that the patient is going to continue to be sick, or the disease will eventually return. This can be stressful. Instead, she suggests it’s reasonable for those in remission to see themselves as cured for potentially better results.
“In some sense, you get what you expect,” Langer explains. “Every single thought has an effect on our bodies. Every movement has an effect on our thoughts. It’s all very subtle.”
A broken shoulder isn’t the only physical hurdle that Paterson has had to navigate. She first noticed signs of chronic Lyme disease in 2011. Since then, she’s experienced symptoms ranging in severity such as stomach problems, depression, anxiety and fatigue. She had to take off a full season from competing to work with functional medicine doctors.
“I’ve been through massive highs, massive lows and everything in between,” Paterson says. “It’s always believing that you can be better. That you can find something to progress.”
This mindset could have helped Paterson with pain management. Langer says that research on Parkinson’s disease, multiple sclerosis, arthritis and other chronic pain conditions shows that people find great relief by becoming aware that their pain is on a spectrum. Once
someone realizes their pain doesn’t only get worse but feels better at times, it is crucial to consider why it improves. This is an exercise in mindfulness and helps those who are suffering to stay hopeful and seek out solutions.
Paterson’s symptoms of Lyme disease manifest both mentally and physically, and the two are always interconnected.
According to Tom Walters, a board-certified orthopedic physical therapist and author of Rehab Science: How to Overcome Pain and Heal from Injury, navigating pain is both an exercise in therapy and physical movements.
“Often there’s a fear-avoidance scenario, where you have pain and you get scared to do certain movements because you’re worried it’s going to injure you,” Walters says. “Not being able to do those causes depression. Then you move less, and create more pain. A lot of people get caught in that cycle with both anxiety and depression.”
has an effect on our
Walters says that your mental health can negatively affect the pain you experience and that everyone has unique experiences with pain. He suggests that if someone is experiencing discomfort for more than three to six months, they may want to consider how their thoughts and emotions could be having an effect.
“There’s some research citing that depression is a stronger predictor of chronic back pain than any physical characteristic,” Walters says. “The mental side is definitely tied to physical pain and injuries.”
These days, Paterson continues to pursue her passions as a triathlete, and alongside her screenwriting and producing, these pursuits help to keep her motivated. They also help her navigate painful moments and actively seek out new challenges to conquer.
“I truly believe that mind work is the essence of success in life,” Paterson says. “I put myself in difficult situations and embrace any kind of failures as a way to grow, learn about myself and get better.” l
AN ESTIMATED 52 million adults in the U.S. have chronic pain, which, by definition, lasts for three or more months, according to the Centers for Disease Control and Prevention. Living with it is far from easy.
As a result, navigating conversations with people suffering from chronic pain can be tricky and delicate. There are questions and statements that may seem innocuous, but to those who live with chronic pain day in and day out, they may be upsetting.
That’s why it’s important to be thoughtful about how we talk to people whose life is marked by chronic pain. Here, what not to tell someone with chronic pain— and what to say instead.
“YOU DON’T LOOK LIKE YOU’RE IN PAIN.”
While you might see this as a compliment, it could be interpreted as disbelief that the person is actually feeling as bad as they do or a suggestion that their pain isn’t real.
One way or another, “it invalidates the person’s experience,” says Meghan Beier, an assistant professor of physical medicine and rehabilitation at Johns Hopkins University School of Medicine. This is especially problematic because people with chronic pain often feel unheard, unseen and misunderstood.
Given that you can’t tell how someone feels like by looking at them, it’s better to ask questions like: “How are you feeling today?” “How can I be supportive?” or “How are you feeling compared to how you usually feel?”

“HAVE YOU TRIED _______?”
Whether the blank is filled with a suggestion to try a specific medication, dietary change or alternative remedy, such as acupuncture, these recommendations are rarely appreciated, experts say.
“A lot of times people try to give solutions rather than listening or showing compassion or empathy to the person with chronic pain,” says Ranak Trivedi, an associate professor of psychiatry and behavioral sciences at Stanford University.
As a result, the suggestions can feel patronizing. A better approach, Trivedi says, is to ask which pain treatments or strategies the person has tried that helped.
“IT MUST BE NICE TO GET SOME TIME OFF OF WORK.”
This phrase is frequently used when someone with chronic pain takes sick days or leave, but it can come across as insensitive, as they are likely struggling and not enjoying their time off.
In situations like this, it’s best to acknowledge that they’re in pain
and ask if there are things you can do that might help them feel a little better, such as spending time outside, says Espinola. In that case, you could offer to go with them or help in a specific way by saying something like, “I’m going to the grocery store. Can I get you anything for dinner?”
“I GUESS YOU’RE GOING TO HAVE TO TOUGHEN UP.”
Some people show the sensitivity of a drill sergeant when dealing with those in pain. Telling someone, “We all experience pain,” “Buck up,” or even, “Put on a happy face” sends the message that their pain is insignificant.
Instead, it’s important to practice empathy, compassion and respect to show your support. You could say: “I’m impressed by how well you’re handling this.”
“AT LEAST IT’S NOT CANCER.”
With a statement like this, you’re essentially comparing the person’s pain with cancer, a life-threatening disease. “What you are really saying is ‘I am judging your health condition against something I find to be really scary,’ rather than validating that the person is suffering,” Trivedi says. “People often don’t realize how much someone with chronic pain is suffering.”
Ultimately, it’s important to avoid “compare and despair” moments, Beier says. It’s an unhelpful thinking style, and it could inadvertently add to the person’s distress. Instead, she adds, it’s better to focus on what the person is telling you and be supportive.
Procedures & Conditions
Hospital Data Insights is an analytics platform from U.S. News & World Report based on the data underpinning the Best Hospitals rankings.
Transform Insights Into Action
•Explore elements to help improve patient care
•Promote brand awareness
• Inform resource allocation
•Discover performance drivers
For more information or to request a free customized demo of your data, get in touch.
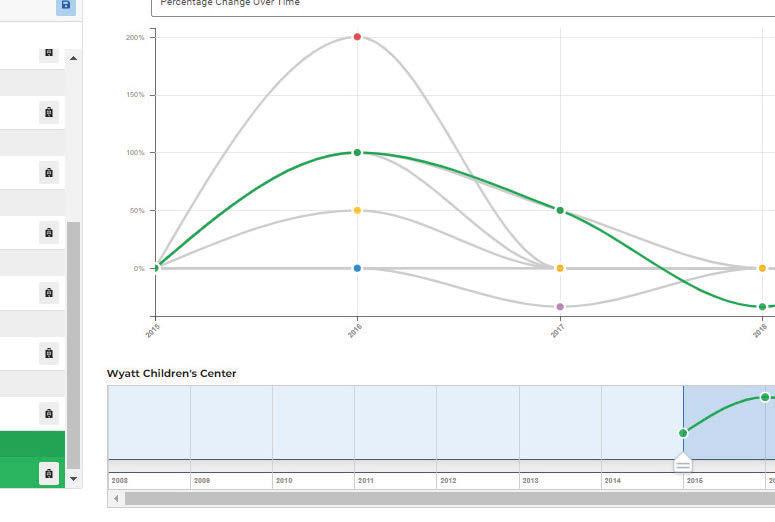
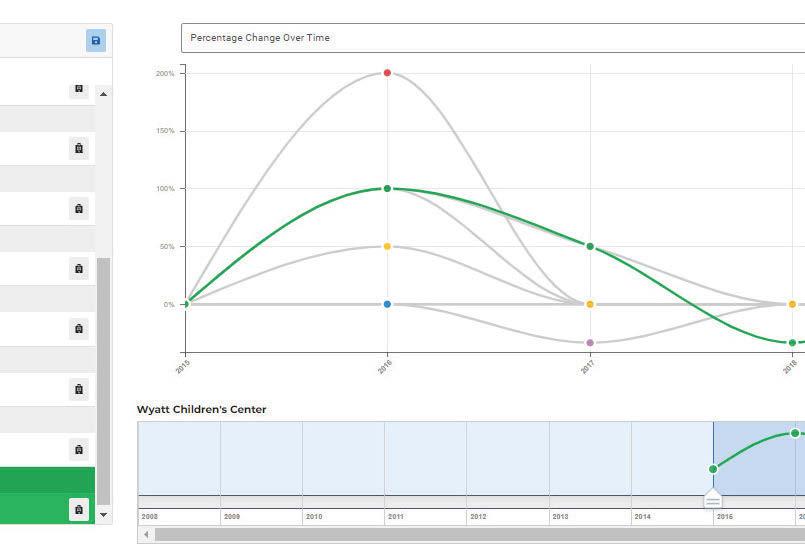
3,500+ hospitals
31+ million data points
5,000+ metrics
25 years of data
hdi.usnews.com
hdi@usnews.com (202) 955-2171
The symptoms may surprise you, but with the right lifestyle strategies and treatment, this hormonal transition can be an empowering period (pun intended) of your life.
by Christine Comizio, MPH ©
HOT FLASHES in the middle of a big meeting. A sleepless night that leaves you dragging all day. A sudden wave of anxiety that seems to come out of nowhere. If you’re in your 40s or 50s and noticing changes like these, you’re not imagining things—you’re likely moving through one of life’s biggest (and least talked about) transitions: menopause.
This natural shift happens to every woman, but it doesn’t always get the attention it deserves. In fact, many women are caught off guard by the wide range of physical and emotional changes that come with this stage, often wondering if stress, an undiagnosed health condition or something else entirely is to blame.
Because conversations about menopause have historically been pushed aside, it can feel isolating—even though more than half the population will experience it. The good news? You don’t have to just “grin and bear it.” With the right knowledge and tools, you can take charge of this stage of life, ease the symptoms that come with it and feel like yourself again—or even better.
Read on to learn about what happens during menopause, its surprising symptoms and the treatments and lifestyle changes that can help you thrive during this new chapter.

Menopause doesn’t happen overnight. In fact, while the average age for menopause is 51, the transition often starts years earlier with perimenopause, the lead-up to menopause that typically begins in a woman’s 40s (although quite a few women experience it in their 30s). Perimenopause can last anywhere from a few months to 10 years—and no two women experience it quite the same way.
During this phase, your ovaries start to slow the production of estrogen and progesterone, the key hormones that regulate your cycle and support everything from bone health to mood. This shift can cause irregular periods, mood changes, hot flashes and other symptoms.
For some women, periods may become heavier or lighter than usual, and cycles may shorten or lengthen unpredictably.



These changes can sometimes feel disruptive or even alarming, especially if you don’t realize they’re part of the transition.
Before menopause, your ovaries release eggs during ovulation each month and produce most of your body’s estrogen. But as you move through this transition, estrogen production gradually declines—and that’s what drives many of the changes you may feel.
Estrogen is a powerful hormone with effects far beyond reproduction. It helps protect bone density, supports the cardiovascular system, influences metabolism and even plays a role in keeping your skin plump and hydrated. When levels drop, it’s no wonder the ripple effects impact so many areas of health—and are felt across so many different parts of your body!
As estrogen levels continue to fall, menstrual periods eventually stop. Then, once you’ve gone 12 months without a period, you’ve officially reached menopause. After that comes postmenopause, the years that follow. By this time, hormone levels stabilize, but for some women, certain symptoms may linger or come and go.
It’s important to know that menopause can also arrive earlier than expected. If it happens before age 45, it’s known as early menopause; before 40, it’s called premature menopause. Menopause can also come on suddenly due to surgery that removes your ovaries or uterus, cancer

treatments like chemotherapy or radiation or certain medications that lower estrogen levels.
When you think of menopause, hot flashes might be the first thing that comes to mind—and while they’re certainly common, the list of possible symptoms goes well beyond that. The hormonal shifts that happen during this transition can affect your body and mind in ways that might catch you off guard.
Many women experience hot flashes and night sweats, sudden waves of heat that can leave you flushed and drenched (often at the most inconvenient times.) Sleep disturbances are also common, whether it’s trouble falling asleep, staying asleep or waking up drenched from a night sweat.
Cognitive changes, often described as “brain fog,” can make it harder to concentrate or remember things. Some women report that they feel forgetful or struggle to focus at work or at home.
You may experience mood swings or feelings of
anxiety or irritability that seem to appear out of nowhere. Additionally, vaginal dryness and painful sex may develop, along with urinary symptoms, like needing to go more often or more urgently.
You might also notice your metabolism slowing down. Weight gain, especially around the middle, can feel frustratingly hard to avoid, even if habits haven’t changed.
On top of all of this, joint stiffness, low libido, hair and skin changes (think dry, flaky skin and thinning strands) and severe fatigue can add to the mix, making daily life feel more challenging. And then there are other downright odd symptoms like itchy ears and burning mouth. Some women even report tingling in their hands and feet and changes in taste and body odor—all lesser-known but very real effects of hormonal change.
It’s important to remember that no two menopause experiences are alike. Some women sail through this phase with minimal symptoms, while others find that these changes impact their everyday lives in significant and disruptive ways. And while some symptoms may fade within months, others can persist for years after your last period.
That’s why it’s so valuable to seek out resources, whether that’s a supportive healthcare provider, a trusted friend group or evidence-based information online. The more you know, the more empowered you’ll feel to manage this transition on your own terms—and even view it as a time of renewal rather than decline.
The good news is that you don’t have to just power through. Today, there are many ways to ease menopause symptoms, and most women find that a combination of strategies works best.
Hormone Replacement Therapy For those dealing with hot flashes and night sweats, hormone replacement therapy (HRT) remains the most effective option. HRT works by replenishing estrogen, and sometimes progesterone, to help balance the hormonal changes that cause many of menopause’s most disruptive symptoms.
“Hormone replacement therapy is most effective within five years of onset of menopause because after five years, a woman tends to lose her estrogen receptors,” says Dr. G. Thomas Ruiz, OB-GYN and lead physician at MemorialCare Orange Coast Medical Center in Fountain Valley, California.
There are two main types of hormone therapy. Systemic HRT—which can be taken as a pill, patch, cream, gel or spray—helps address whole-body symptoms like hot flashes, sleep disturbances and mood swings. For women who still have a uterus, estrogen is typically combined with progesterone or progestin to protect the uterine lining.
Local HRT, on the other hand, is applied directly to the vaginal area and doesn’t enter the bloodstream. It delivers low-dose estrogen to the vaginal tissue and is especially useful for easing dryness or urinary discomfort.
How long a woman stays on HRT can vary, and regular check-ins are important to reassess whether the
IN 2002, the Women’s Health Initiative (WHI) study made headlines when it reported that hormone replacement therapy (HRT) increased the chance of breast cancer and other health risks for women. Almost overnight, millions stopped taking it, and doctors became cautious about prescribing it. But here’s what’s important to know:
The WHI research painted an incomplete picture. Most of the women in the study were over 60—well past the typical age of menopause—and many had other health conditions that increased their risks. The findings didn’t reflect the experience of younger women who start HRT closer to the onset of menopause.
Estrogen isn’t linked to breast cancer. In fact, newer research shows that estrogen-only HRT can lower the risk of breast cancer in women who have had a hysterectomy.
The benefits often outweigh the risks. For women who begin HRT in their 40s or 50s—within about 10 years of menopause—HRT has been shown to help protect heart health, support bone strength and improve quality of life when used appropriately and under a doctor’s care.
HRT isn’t one-size-fits-all. If you’re considering it, talk with your doctor about your personal health history, timing and goals so you can make an informed choice that’s right for you.

treatment is still needed. Some women decide to stay on it for just a few years, while others may find such great symptom relief that they prefer not to stop using it. Local vaginal therapy can often be used safely for any duration, depending on symptoms.
However, hormone therapy isn’t the right fit for everyone. Women with a history of hormone-sensitive cancers, blood clots or heart or liver problems may need to explore other options. Navigating these decisions means being your own advocate, says Dr. Octavia Cannon, a provider at Alliance Obstetrics and Gynecology in East Lansing, Michigan and a member of the Board of Directors for the American Medical Women’s Association. “If she’s not able to advocate for herself, that’s when she may need to bring someone with her—a friend, sister or partner—to try to describe the things that she’s been going through,” says Cannon.
Nonhormonal Options Not interested in HRT? You’re not out of luck. Certain medications such as antidepressants (SSRIs and SNRIs) at low doses can ease hot flashes and mood swings. “It’s generally half the dose,” Cannon notes. “However, I often see patients who say, ‘I just feel better. I feel less anxious. I feel my mood is better,’ and they want to go on the full dose, which is absolutely fine.” Supplements may also benefit some women. Every treatment plan is unique. Work with your doctor to choose what fits your needs and medical history.
Changes in your daily routine can go a long way toward easing menopause symptoms and helping you feel more like yourself. Many women find that simple adjustments—from what they eat to how they move— can make hot flashes, sleep issues and mood swings more manageable. One of the first steps is paying attention to what triggers your symptoms. For example, hot flashes can be set off by things like alcohol, certain foods and drinks, warm rooms or even stress. Learning to spot your personal triggers makes it easier to avoid or minimize them. “Don’t
underestimate how caffeine, spicy foods and not drinking enough water every day can affect symptoms,” says Cannon.
What you eat matters too. A balanced diet rich in calcium and vitamin D helps support bone health, which becomes especially important after menopause. Experts recommend about 1,500 milligrams of calcium per day for postmenopausal women. Foods like milk, yogurt, leafy greens, almonds and fortified products can help you meet your needs, and getting 15 minutes of sun exposure a day may give you a vitamin D boost. (For more on the best menopause diets, see page 88.)
Staying active is another key piece of the puzzle. Regular exercise—walking, swimming, dancing, yoga or strength training—can help with hot flashes, improve mood and protect against bone loss.
Shut-eye can also become harder to come by during menopause, so focusing on good sleep hygiene is essential. That might mean keeping your bedroom cool and dark, sticking to a regular bedtime and avoiding screens or caffeine before bed.
Finally, don’t underestimate the power of talking about your experience. Sharing what you’re going through—whether with your doctor, partner or friends and family—can help you feel supported and understood while also helping to squash the stigma around menopause. As Cannon encourages, “Start talking to your daughter who’s 25 about what you’re going through at 55—not to complain, but to inform her.” l
NAVIGATING menopause is easier when you go into your doctor’s office prepared. And if your doctor seems dismissive or pushes back on treatment options, don’t hesitate to seek a second opinion —you deserve to feel heard and supported. (Tip: If you’re feeling overwhelmed, bring a partner, friend or family member to help you ask questions and take notes.)
Here are some smart, supportive questions to help you get the care that fits your needs:
• Could my symptoms be due to menopause, or should we check for other conditions?

• What are my options for managing hot flashes, sleep issues or mood swings?
• Is hormone therapy a good fit for me? What are the benefits and risks in my case?
• If HRT isn’t recommended, what nonhormonal treatments could help?
• How can I help to protect my bone and heart health both during and after menopause?
• Are there lifestyle changes you’d suggest for easing my symptoms?
• How often should we check in to reassess my treatment plan?
Putting one foot in front of the other is a simple way to reduce your risk of chronic disease.
by Cedric X. Bryant, PhD, FACSM ©
ALKING is something almost everyone does every day. It doesn’t require fancy equipment, expensive membership or hours of free time. Yet despite how easy it is, many of us aren’t doing it nearly enough. Sitting too much and moving too little has become the norm for many people. But adding more steps to your daily life is one of the most powerful things you can do to improve your health. In fact, walking just a little more each day can help protect you from a slew of chronic diseases while also improving your quality of life.
Let’s take a closer look at the benefits of walking, how many steps are right for you and simple ways to get moving—one foot at a time.
Research shows that walking just 30 minutes a day, five days per week—or about 150 minutes a week in total—can offer enormous health benefits. It supports mental health by reducing stress, easing anxiety and helping to manage depression. Many people also report sleeping better when they walk more during the day. And walking doesn’t only help with how you feel—it also reduces your risk of disease. Studies have found that consistent walking can help prevent heart disease, type 2 diabetes and even some cancers.
Even if you already exercise at the gym or take fitness classes, walking adds another layer of protection. It can help with balance, flexibility and the kind of movement that supports your everyday tasks. Better yet, the benefits begin almost immediately. A brisk walk can lift your mood, give you a burst of energy and help you think more clearly.

You’ve probably heard that 10,000 steps a day is the magic number for good health. While it’s a good target for many people, it’s not the only number that matters.
A mile is roughly 2,000 steps, so walking 10,000 steps means you’re covering about five miles a day. That’s a great goal, but it’s more important to focus on improving your current habits rather than hitting a big number right away.
If you’re currently walking about 4,000 steps a day, increasing your steps by just 20 percent each week is a realistic way to improve your health. For example, aim for 4,800 steps next week, and then 5,800 the week after that. Small increases add up over time and are more likely to become permanent habits.

You also don’t need to carve out a large chunk of time to fit in your daily steps. Even just five minutes of walking every hour can help reduce the health risks that come from too much sitting. So whether you’re walking across the parking lot, around your house or through the grocery store, every step truly does count.
Incorporating walking into your daily life is simpler than it may seem, but making it a lasting habit takes patience and consistency. Many people believe it takes 21 days to form a new habit. While that might hold true for simple behaviors, more complex routines (like regular exercise) usually take longer. In fact, research suggests that sticking with an activity like daily walking can often take several months—or even up to almost a year—before it truly becomes second nature. So if you struggle at first, you’re not alone.
The key is to fold walking into your natural rhythm.
Treat it like any other important appointment. Block out time on your calendar the way you would for a meeting or a doctor’s visit. Giving your walks a set place in your schedule not only helps you follow through—it signals to others (and yourself) that your health is a priority.
Making walking enjoyable also increases the chances you’ll stick with it. That might mean queuing up your favorite playlist or podcast, choosing a route with beautiful scenery or inviting a friend along for the conversation. When walking becomes something you look forward to, rather than just another task, it’s more likely to stick.
Of course, becoming someone who walks every day—or someone who moves more in general—doesn’t happen overnight. It’s a gradual shift, built from small, repeated choices. If you’re just starting out, ease into it. Begin with short walks a few times a week and let your routine grow naturally over time. Walking may be the focus, but it doesn’t have to be the only form of



YOU DON’T need to carve out hours of free time to walk more. With a few smart strategies, you can turn everyday moments into opportunities for movement. Here are 10 ways to add more steps into your daily life:
1 Keep your walking shoes within reach. Stash a comfortable pair of walking shoes in your car, by your desk or near the front door. That way, when you find yourself with a few free minutes—whether between meetings or before an appointment—you can easily head out for a refreshing 10-minute stroll. These mini-breaks not only add steps but also help clear your mind.
2 Invite someone to join you. Walking with a friend, coworker or family member makes movement feel less like a chore and more like quality time. A midday walk with a colleague can boost creativity and productivity, while a post-dinner stroll with a loved one offers a chance to connect—and sneak in more steps.
3 Move while your child is at practice. Instead of staying seated in the car or on the sidelines during your child’s activities, take a few laps around the field, gym or nearby neighborhood. It’s a sim-



ple way to stay active while setting a positive example.
4 Use a fitness tracker to stay accountable. Wearable devices like pedometers, smartwatches and fitness rings can help you track your activity and set realistic goals. Whether you’re aiming for 10,000 steps or simply trying to do more than yesterday, having data at your fingertips can be a powerful motivator. Even reaching 7,000 steps a day can meaningfully lower your risk for heart disease and early death.
5 Choose the long way around. Look for chances to add extra steps into your routine. Walk to a restroom on another floor, take a longer route to your coworker’s desk or loop the block before grabbing the mail. These small choices add up without requiring extra time in your day.
6 Park once and walk. When running errands, pick a central parking spot and walk to each store instead of driving between them. If your shopping bags get heavy, drop them off at the car and continue on. This simple change can increase your daily steps while saving on gas and reducing stress.
7 Walk part of your commute. If you drive to work, consider parking a






few blocks away. If you take public transit, get off one stop early. Even five to ten minutes of walking at the start or end of your commute can lift your mood, energize your morning or help you wind down after a long day.
8 Switch up your scenery. Variety makes walking more enjoyable. Try starting your walks from different places—like a friend’s house, a local park or your office—and explore new routes. Changing up the view can make each walk feel like a fresh experience.
9 Turn calls into walking time. Meetings and phone calls don’t always have to be seated. When appropriate, take work meetings on the go or walk around the house while on long calls. You can also turn evening phone chats with friends or family into “walk and talk” sessions—adding movement while deepening connection.
10 Make it a game. Friendly competition can inspire consistency. Challenge your friends, coworkers or family members to a walking goal using a free app to track steps or minutes. Whether it’s teambased or individual, the shared effort and bragging rights can keep everyone moving.
movement you enjoy. Dancing in your kitchen, swimming laps, gardening or biking through the neighborhood all count. What matters most is that you’re moving your body in ways that feel good and fit your life.
Understanding your personal reason for wanting to move more can also help you stay motivated. Maybe you want to feel more energized during the day, find an outlet to help manage stress or go on hikes with your kids. Whatever your “why,” keep it in mind—it’s your anchor. On days when you aren’t feeling in the mood to lace up your sneakers, focusing on your “why” can help inspire you to stick with it.
If you’re still struggling to make walking a habit, social
support can also make a difference. Walk with a friend, join a neighborhood walking group or connect with others through a shared step challenge. Accountability and shared motivation often make movement more enjoyable—and more consistent.
Above all, stay positive and patient. If you miss a walk, don’t see it as failure. Just get back to it the next day. Progress doesn’t require perfection and life is busy and unpredictable, so adjust as needed. If mornings are packed, try walking after dinner. The best time to walk is the one that works for your life. Remember: Habits don’t form overnight, but every walk you take brings you closer to a healthier, more active lifestyle. Step by step, you’re building a routine that supports your well-being—and that’s something worth sticking with. l
FITNESS TRACKERS have evolved far beyond step counters. Many now measure heart rate, track sleep, monitor stress and log your body temperature. But no matter how advanced the technology, your tracker is only helpful if you use it consistently—and use it well. Follow these eight tips to get the most out of your device.
• Wear your tracker daily. Wearing it regularly builds awareness and reinforces your health goals. Keeping it charged and ready to go is key, so try plugging it in during routine moments, like while you shower or eat breakfast.
• Set it up properly. Be sure to input your details—age, weight, height and fitness level—accurately. This helps your tracker provide more personalized data, whether it’s step count, heart rate zones or calories burned.
• Be realistic. Set goals that match where you are now, not where you think you should be. If you’re walking 5,000 steps a day, jumping to 10,000 overnight may be more frustrating than moti -

vating. Gradually increase your targets and build from there.
• Make it fun. Many trackers let you join social challenges or form groups with friends and family. These can offer accountability and a boost of motivation on days when you might otherwise skip your walk.
• Don’t stop at counting steps. Explore other features your device offers—such as sleep tracking, GPS mapping for outdoor workouts or syncing with nutrition and hydration apps. The more complete your health picture, the better your progress can be.
• Watch for trends over time. For instance, if your sleep quality dips
after late-night workouts, you might consider exercising earlier in the day. Use the data as a guide, not a judgment.
• Use prompts. Set reminders that support your routine, like prompts to move every hour or go to bed at the same time each night. These small nudges can help you stay consistent without feeling overwhelmed.
• Be kind to yourself. A missed step goal doesn’t mean failure—it simply means tomorrow is a new chance to try again. Your fitness tracker is a tool to support your journey, not a scorecard. Focus on progress, and let that be enough.
Your goal: to find the plan that will work for you.
by Gretel Schueller ©
N ANY GIVEN DAY, millions of people in the U.S. are trying to lose weight. More than half of Americans reported that they followed a specific eating pattern or diet at some point in the past year, according to the International Food Information Council’s 2024 Food & Health Survey.
OYet, only 20% of dieters will be able to keep their weight off for 12 months. The truth is, dieting is hard. Many fad diets don’t work, and some can even threaten your health. And digging through mounds of information to decipher whether a particular plan lives up to the hype can be overwhelming.
U.S. News Best Diets 2025 cuts through the diet chatter to identify the plans that are most likely to help you reach your goals—whether that’s losing weight, managing a health condition (like high blood pressure or diabetes) or simply wanting to eat healthier. Then, you can decide, in consultation with your doctor or other health professional, which diet is best for you.
Now in its 15th year, U.S. News Best Diets has released its rankings for 38 popular diets across 21 categories based on various criteria, from their healthiness to the likelihood of their helping you lose weight. Many diets, like WeightWatchers, are household names, while others—like the DASH (dietary approaches to stop hypertension) and MIND diets —should be. And for 2025, the health team added 13 new ranked diets, including the menopause diet, Whole30 diet, acid reflux diet, BRAT diet and gluten-free diet.
The focus of healthy eating has evolved beyond weight loss, encompassing overall well-being and chronic disease prevention. So for 2025, U.S. News added 12 new Best Diets categories for evaluation, all focused on specific health and lifestyle needs. We mined medical journals, government reports and other resources and interviewed leading health and nutrition experts to create in-depth profiles for each diet. You can find these at health.usnews.com/bestdiets.
We’re not going to tell you what diet you should be on, but we can help lead you to a winner—the best diet for you.
Our Best Diets panelists consists of 69 experts, including medical doctors, registered dietitian nutritionists, nutritional epidemiologists and weight loss researchers who are leaders in their field. They thoroughly evaluated all 38 diets.
We worked with The Harris Poll to devise the methodology used in this year’s rankings. When considering Best Diets Overall, panelists considered: nutritional completeness; health risks and benefits; long-term sustainability; and evidence-based effectiveness.
Panelists considered each diet’s strengths and weaknesses and the specific goals each diet might be most effective at addressing, which they shared in openended responses. The Best Diets panelists also shared aspects of each diet they particularly liked or disliked and provided advice for those considering the plan. The latest rankings, which feature everything from the Mediterranean diet to the popular keto diet, can help you find the top plan for you. For the full rankings, go to health.usnews.com/bestdiets. l
Whatever your reason for wanting to change your diet, one of these science-backed plans will help you find success.
These plans minimize the symptoms of menopause, such as weight gain, hot flashes and bone density declines.
These eating plans were found to be the most effective at managing blood sugar levels for people with diabetes.
These are the best dietary choices to protect and preserve cognitive function for a healthy brain and sharper mind.
These diets facilitate weight loss at a healthy rate of one to two pounds a week and maintain it for the long term.
These diets fulfill the short-term goal of losing weight quickly (in three months or less), even if it’s not sustainable for the long term.
These healthy, plant-based diets range from entirely vegan to those that allow for a flexible mix of plant-forward foods.
These
When it comes to supporting mental well-being and mood, these diets came out on top.
These diets are for people who want to improve heart health, from helping control blood pressure to reducing cholesterol.


If your digestive health is a priority, these foods should be consumed in moderation.
1 SUGARY FOODS AND DRINKS Excess sugar is one of the worst offenders for gut health. A 2018 study in the journal Nutrients found that mice who were fed a diet high in excess sugar experienced an alteration in the makeup of their gut microbiome as well as increased gut permeability (also known as leaky gut) and increased inflammation. This in turn increased rates of fatty liver disease.
2 ARTIFICIAL SWEETENERS If sugar is harmful to gut health, artificial sweeteners should help you avoid that problem, right? Not so fast. Artificial sweeteners (like stevia, aspartame, sucralose and saccharin) are also some of the biggest culprits when it comes to poor gut health. An array of artificial sweeteners pass through the body undigested, which means they can negatively affect the microflora in your gut, says Lisa Jones, a registered dietitian based in Philadelphia.
3 ALCOHOLIC BEVERAGES Drinking more than the recommended amount of alcohol (two drinks or less a day for men and one drink or less daily for women) can harm your gut microbiome, Jones says. Research published in the journal Gut Microbes in 2020 suggests that drinking alcohol excessively is also associated with dysbiosis, which occurs when the bacteria in your gastrointestinal tract—including your intestines—become unbalanced.
4 FRIED FOODS Saturated fat, a key feature of fried foods, is hard on the gut, making these foods more difficult for your body to digest compared to fresh fruits and

vegetables, Jones says. “The oils that may be used to fry the food are rich in saturated and trans fats, which can bother your gut,” she explains. This can lead to diarrhea, gas and stomach pain.
5 RED MEAT While they might be delicious off the grill on a hot summer day, fatty meats like burgers, sausages and hot dogs can all be problematic. “Diets high in red meat and fats are especially bad for gut health,” says Kim Kulp, a registered dietitian nutritionist specializing in gut health and the owner of Gut Health Connection in the San Francisco Bay Area. “When gut microbes feed on red meat, they release an enzyme that can lead to inflammation.”
6 SALTY FOODS Salty foods can also be detrimental to gut health, notes Dr. Edward Salko, a practicing emergency physician in Kennewick, Washington and the medical director of Personalabs, a direct-to-consumer lab testing and telehealth company based in Fort Myers, Florida. “Salty foods cause bloating, fluid retention, headaches and high blood pressure,” he explains, adding that they can also disrupt protein digestion, which can alter how the gut microbiome functions.
7 ULTRA-PROCESSED FOODS Ultra-processed foods tend to be high in additives, salt and excess sugar, all of which aren’t great for gut health. They’re also typically low in dietary fiber, which is an important micronutrient for maintaining gut regularity and feeding the beneficial bacteria in our gut. Highly processed foods include bacon, ham, pate and sausage; cakes and cookies; processed lunch meats; and soft drinks.
The best thing to do for your digestive system is focus on a varied, nutritious diet. “Having diversity in your diet can improve the gut microbiota and allow more of the good bacteria to flourish,” explains Amber Core, a registered dietitian at the Ohio State University Wexner Medical Center in Columbus. This is especially important if you are taking antibiotics, which can disrupt your gut health and upset the balance of healthy microbes in your gut. Here, three types of gut-happy foods to fill your plate with.
1 PROBIOTIC FOODS Probiotics are live, health-promoting microbes, mainly bacteria and yeast. Examples of probiotics include lactobacillus (found in fermented foods, such as yogurt), bifidobacterium (found in some dairy products) and saccharomyces boulardii (a type of yeast that’s often found in probiotic supplements).
While probiotics can be sourced from supplements, many (but not all) fermented foods are teaming with probiotics, which can help populate the gut with beneficial microbes. Examples of fermented foods that are rich sources of probiotics include raw sauerkraut, yogurt, kimchi, miso, kefir and kombucha. Make sure to look for a label stating that the product contains live and active cultures. You should also be able to find the full probiotic name on the label.
2 PREBIOTIC FOODS Prebiotics, on the other hand, are plant fibers that the healthy bacteria in the gut feed on. When healthy gut bacteria break down prebiotics, they get energy for themselves. This increases their chance of survival in the gut. A diet high in prebiotic foods improves

digestion, supports the immune system and helps with the absorption of nutrients. Prebiotic-rich foods include certain fruits (bananas, raspberries, apples and kiwis); leeks, onions and garlic; beans and legumes; barley and oats; potatoes; asparagus; and flaxseeds.
3 HIGH-FIBER FOODS Good bacteria also love to chomp down on fiber. Fiber is a type of nondigestible carbohydrate that passes through the body without breaking down into its constituent parts. It helps your body regulate how to use sugar and can keep hunger and blood sugar levels in check.
Good sources of fiber include leafy greens, such as spinach and kale; cruciferous vegetables, such as Brussels sprouts, cauliflower and broccoli; beans, peas, lentils and other legumes; apples, pears, grapes and other fresh fruits; prunes, raisins and other dried fruits; avocados; root vegetables, such as potatoes, carrots and beets; whole grains, such as oats, quinoa, brown rice and whole-wheat bread; popcorn; dates; and nuts and seeds.
The foods that support gut health generally support overall health, but if you’re having stomach problems, you shouldn’t try to self-treat with food or supplements. Make an appointment to see your doctor if you have significant abdominal pain that occurs frequently or lasts more than a day, unexplained weight loss, changes in bowel habits, blood in your stool or a family history of gastrointestinal illnesses. Together, you can decide on the best treatment course to help your gut and your overall health. l


THERE CAN BE many, sometimes subtle, signs that your gut isn’t in balance, including these nine clues.
1 FREQUENT STOMACH UPSET
If your stomach often feels upset or you frequently have gas or bloating, that could be a sign that your gut health isn’t optimal.
2 INTOLERANCE OF CERTAIN FOODS
Feeling unwell after eating a specific food could point to an intolerance of that item or a component of it, which could be a sign of a problem in the gut.
3 INTENSE CRAVINGS
Do you suddenly have intense cravings for a specific food? Any changes in cravings could be a sign that your gut needs something to help bring it back into balance.
4 UNINTENDED WEIGHT FLUCTUATIONS
Gaining or losing weight without meaning to could point to an underlying issue in the gut. If your gut isn’t functioning optimally, your body may not be absorbing the nutrients it needs, leading to weight changes and potential nutritional deficiencies. You should talk to a health care provider any time your weight changes significantly.
5 SKIN IRRITATIONS OR AUTOIMMUNE DISORDERS
Your specific blend of gut microbiota can affect how well your immune system functions. As a result, a problem with your digestive health can show up as rashes, skin irritations, an autoimmune disor-

der, such as Crohn’s disease, or a thyroid problem.
6 MIGRAINES OR FREQUENT HEADACHES
If you get a lot of headaches or experience migraines, the problem may be related as much to your gut as to your head. There seems to be a direct line of communication between the gut and the brain, and a disruption in one could lead to problems in the other.
7 DIFFICULTY SLEEPING OR EXCESSIVE FATIGUE
If you don’t have a reason to feel more tired than usual, your lack of energy might be related to your gut. Your circadian rhythm—the sleepwake cycle that means you feel tired at night and alert during the day—is regulated in the brain, which is connected to the gut.
8 IRRITABILITY OR OTHER MOOD CHANGES
Mood changes can be related to a broad range of problems, but it might be worth looking at your diet and your gastrointestinal health for an underlying cause. With your brain and brain chemistry tied to your gut microbiome, a problem there could lead to mood instability as well as potential shifts in your mental health.
9 CHANGES IN BATHROOM HABITS
Having trouble going—or going too often? Both constipation and diarrhea can be signs of problems with your gut health. While it’s not uncommon to experience constipation or diarrhea from time to time, if you develop chronic symptoms or can’t seem to find another reason to explain why it’s occurring, your gut microbiome could be to blame.
Your family’s medical past may hold the key to your future health. Learn how to build a complete history and use it to personalize your prevention plan.
by Barbara Sadick ©
UNDERSTANDING your family’s health history can be one of the most powerful tools for protecting your own well-being. By identifying medical patterns and inherited traits, you and your doctor can create a personalized healthcare plan, possibly preventing serious conditions before they start.
That’s exactly what Betsy Adler set out to do. After learning that several of her first cousins had battled cancer—and that three male cousins had died from various forms of the disease—Adler decided to take action. She consulted a genetic counselor, who guided
her through the process of gathering and analyzing her family’s health data. A blood test soon followed, checking for inherited gene mutations that could increase her risk for certain cancers.
“Knowing what medical conditions run in your family can give you a heads-up on medical problems you may be at risk for, and from there you and your doctor can work to ensure your treatment is personalized to target certain risks and to possibly prevent them from occurring,” says Dr. Wendy Chung, a geneticist and chief of the


department of pediatrics at Boston Children’s Hospital.
So what exactly goes into a family medical history— and why does it matter? Let’s take a closer look.
While lifestyle and environmental factors have the heaviest influence on our health, genetics also play a role. We inherit two copies of each gene, one from each parent. These genes determine traits like eye color and height, but they also influence our likelihood of developing certain illnesses.
Some conditions, such as sickle cell anemia, cystic fibrosis and particular forms of cancer, are caused by genetic mutations. Most families have at least one member who has faced a chronic illness like cancer, heart disease or diabetes.
But relying on family anecdotes isn’t enough. Collecting accurate medical information allows you and your physician to identify hereditary risks, consider early or
more frequent screenings, decide whether genetic testing is warranted and develop a targeted prevention or treatment plan. Although you can’t change your genes, you can adjust your lifestyle and environment. For example, if heart disease or diabetes runs in your family, improving your diet and increasing physical activity can lower your risk. If there’s a pattern of breast or ovarian cancer, particularly in families of Ashkenazi Jewish descent, your doctor may recommend testing for BRCA gene mutations.
Just like Adler, who underwent testing for 71 genetic markers, you too can take proactive steps. “As more genetic tests become available, more people are taking them to investigate their family history of diseases,” says Chung. “The more we discover about genetic medical histories, the more personalized your medical care should become.”
A family medical history typically includes chronic illnesses, past treatments and medications, ethnic background, environmental exposures and lifestyle factors such as diet, exercise, alcohol use
Lifestyle and environment have the heaviest influence on health.
MANY HEALTH conditions tend to run in families. If a close relative has been diagnosed with one of the following, you may be at higher risk: Heart Disease & High Blood Pressure: A family history of early heart disease or hypertension raises your risk. Lifestyle changes like improving your diet, exercising, reducing stress and quitting smoking can help.
regular exercise and weight management are key preventive steps. Breast, Ovarian & Colorectal Cancers: Genetic mutations such as BRCA or patterns like multiple early-onset cancers in the family may signal increased risk. Early screening and genetic testing can be lifesaving.
detected early through newborn screening. Carrier testing is available for those with a family history or from higher-risk ethnic groups.

Asthma & Allergies: Asthma often runs in families, especially when allergies are also present. Avoiding known triggers may reduce flare-ups. Diabetes: If a parent has diabetes, your risk is higher. A healthy diet,





Tay-Sachs Disease: Most common in Ashkenazi Jewish, French-Canadian, Cajun and Amish populations, Tay-Sachs can be identified through carrier screening before or during pregnancy.
Obesity: Genes influence appetite, metabolism and body fat distribution, but environment plays a big role too. Healthy habits can counteract inherited tendencies.





Single Gene Disorders: Conditions like Huntington’s disease, Marfan syndrome, and Duchenne muscular dystrophy are rare but often hereditary. If they appear in your family, seek genetic counseling. Sickle Cell Disease & Cystic Fibrosis: These inherited disorders can be





















Arthritis: Some types, especially osteoarthritis, may run in families. Symptoms can be managed with medication, physical therapy and weight management.

















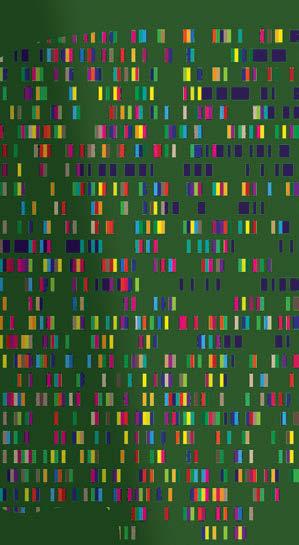








GENETIC COUNSELING is a process that helps individuals understand how inherited diseases and conditions might affect them or their families. It’s often the first step when your family medical history raises red flags. Knowing what the process involves—and whether it could be right for you— can help you take the next step with confidence.
Who should consider genetic counseling? You might benefit from genetic counseling if:
• Se veral close relatives have had the same or related types of cancer
• A relative was diagnosed with a genetic condition like cystic fibrosis or Huntington’s disease
• A family member had a disease at an unusually young age
• You’re planning to start a family and have concerns about inherited conditions
What can I expect? A session typically involves a trained genetic counselor reviewing your personal and family health history and assessing your risk for inherited conditions. They should also:
• Create a detailed family health tree
• Discuss whether genetic testing might be appropriate for you
• Explain possible outcomes and what they mean for your health
• Help you make informed decisions about prevention, screening or treatment options
How can I start? Ask your doctor for a referral, or check with major hospitals and cancer centers. Many have dedicated genetic counseling services.
and smoking habits. This history isn’t fixed—it should evolve over time as new information comes to light and additional family members are diagnosed.
To start building your family history, talk to relatives on both sides of your family. Begin with your parents, siblings and children, then expand to grandparents, aunts and uncles, nieces and nephews and cousins. The more distant the relative, the less directly their health may affect you, but broader patterns can still be informative.
“Once you’ve collected family medical history, it can be a clear way to determine whether you and your family need to worry about certain medical conditions,” says Adam Buchanan, a genetic counselor and chair of the department of genomic health at Geisinger Health. “You may see obvious patterns.”
As you gather information, focus on each relative’s relationship to you, date of birth, ethnic background and gender. Record their current age or, if deceased, their age and cause of death. Include any illnesses or chronic conditions they had, when they were diagnosed, any surgeries or hospital stays and any medications they were prescribed. Details about smoking, drinking, diet, exercise, mental health and pregnancy complications can also provide insight into risk patterns.
Don’t worry if you don’t have every piece of information at the start. Even partial details can be valuable. To streamline the process, consider using digital tools or apps designed for family health tracking, which make it easier to organize information and share it securely with healthcare providers. Keeping a binder of written notes or even simple charts can also be effective, especially if multiple relatives are planning to contribute information.
If you are adopted and do not have access to your biological family’s medical history, reach out to the adoption agency if possible, or contact your birth relatives directly if appropriate.
Once your family health information is gathered, reviewing it with your doctor can help you identify potential red flags. If a particular disease shows up repeatedly among your relatives, especially if it appears earlier than expected, it could indicate a genetic risk. A family history of multiple related cancers— such as colon, uterine and ovarian cancer—might suggest an inherited syndrome like Lynch syndrome.
These are signs that more frequent checkups or earlier screenings may be recommended. Your doctor might also advise genetic counseling or testing. What’s important is that you don’t wait—act on the information you have.
A well-documented family medical history is more than just a collection of facts. It’s a tool that can guide healthcare decisions for you and your loved ones. Most doctors are trained to spot patterns that may not be obvious to patients, and those insights could be critical.
“You should want to know your family’s medical history to keep you and your relatives healthy,” says Dr. Chung. “It’s one of the best ways to get ahead of anything that might be coming your way.” l

The 20 hospitals recognized on the Honor Roll excel in treating patients with complex diagnoses as well as those with relatively routine needs. Selection for the Honor Roll is based on points, which hospitals received for strong rankings and ratings. Hospitals that earned at least 311 out of 555 possible points made this year’s list. Each hospital on the 2025-2026 Best Hospitals Honor Roll, listed below in alphabetical order, is nationally ranked in 10 or more of the 15 Best Hospitals specialties and is rated “high performing” in most of 22 common procedures and conditions (see Page 179 and health.usnews.com/best-hospitals).
AdventHealth Orlando, Fla.
Brigham and Women’s Hospital, Boston
Cedars-Sinai Medical Center, Los Angeles
Cleveland Clinic
Hackensack U. Med. Ctr. at Hackensack Meridian Hlth., Hackensack, N.J.
Hosps. of U. of Pennsylvania-Penn Presbyterian, Philadelphia
Houston Methodist Hospital
Johns Hopkins Hospital, Baltimore
Massachusetts General Hospital, Boston
Mayo Clinic-Arizona, Phoenix
Mayo Clinic-Rochester, Minn.
Mount Sinai Hospital, New York
New York-Presbyterian Hospital-Columbia and Cornell
Northwestern Medicine-Northwestern Memorial Hospital, Chicago
NYU Langone Hospitals, New York
Rush University Medical Center, Chicago
Stanford Health Care-Stanford Hospital, Palo Alto, Calif.
UCLA Medical Center, Los Angeles
UCSF Health-UCSF Medical Center, San Francisco
University of Michigan Health-Ann Arbor

How we identified 152 outstanding hospitals in 15 specialties
by Ben Harder ©
FOR MORE THAN three decades, the mission of the U.S. News & World Report Best Hospitals rankings has been to help guide patients, in consultation with their doctors, to the appropriate place when they need a high level of specialty care. These are patients whose surgery or condition is complex, or whose advanced age, physical infirmity or existing medical condition limits their options.
Such people account for a small fraction of hospital patients, but they add up to millions of individuals—and many hospitals may not be able to meet their needs. A hospital ranked by U.S. News in cancer, say, is likely to have the expertise and capability to enroll an elderly patient with a metastatic tumor into a clinical trial for an unproven but innovative treatment.
Some community hospitals can also provide access to such experimental therapies. But not all.
The following pages offer hospital rankings in 15 different specialties, from cancer to urology. Of more than 4,000 hospitals evaluated by U.S. News this year, only 152 performed well enough to be ranked in any specialty.
In 12 of these 15 specialties, analysis of objective data from the federal government and other sources generated the main factors determining whether a hospital was ranked. To capture medical experts’ opinions, we also factored in results from annual surveys of specialist physicians who were asked to name hospitals they consider best in their specialty at handling difficult cases.
Hospitals in the other three specialties (ophthalmology, psychiatry and rheumatology) were ranked solely on the basis
Cedars-Sinai is proud to be ranked #1 in California*, #1 in Los Angeles* and named to U.S. News & World Report’s
Cedars-Sinai is proud to be ranked #1 in California*, #1 in Los Angeles* and named to U.S. News & World Report’s
Cedars-Sinai is proud to be ranked #1 in California*, #1 in Los Angeles* and named to U.S. News & World Report’s
Cedars-Sinai is proud to be ranked #1 in California*, #1 in Los Angeles* and named to U.S. News & World Report’s
“Best Hospitals 2025-26” Honor Roll for the 10th consecutive year. We’re incredibly grateful to all of our employees and the communities we serve for helping us to achieve this vital milestone.
“Best Hospitals 2025-26” Honor Roll for the 10th consecutive year. We’re incredibly grateful to all of our employees and the communities we serve for helping us to achieve this vital milestone.
“Best Hospitals 2025-26” Honor Roll for the 10th consecutive year. We’re incredibly grateful to all of our employees and the communities we serve for helping us to achieve this vital milestone.
“Best Hospitals 2025-26” Honor Roll for the 10th consecutive year. We’re incredibly grateful to all of our employees and the communities we serve for helping us to achieve this vital milestone.
Cedars-Sinai specialties ranked in the top 10 nationally:
Cedars-Sinai specialties ranked in the top 10 nationally:
Cedars-Sinai specialties ranked in the top 10 nationally:
Cedars-Sinai specialties ranked in the top 10 nationally:
Gastroenterology & GI Surgery (#2)
Gastroenterology & GI Surgery (#2)
Gastroenterology & GI Surgery (#2)
Gastroenterology & GI Surgery (#2)
Orthopedics (#5)
Orthopedics (#5)
Orthopedics (#5)
Orthopedics (#5)
Pulmonology & Lung Surgery (#5)
Pulmonology & Lung Surgery (#5)
Pulmonology & Lung Surgery (#5)
Pulmonology & Lung Surgery (#5)
Cardiology, Heart & Vascular Surgery (#6)
Cardiology, Heart & Vascular Surgery (#6)
Cardiology, Heart & Vascular Surgery (#6)
Cardiology, Heart & Vascular Surgery (#6)
Obstetrics & Gynecology (#8, tied)
Obstetrics & Gynecology (#8, tied)
Obstetrics & Gynecology (#8, tied)
Obstetrics & Gynecology (#8, tied)
Diabetes & Endocrinology (#9)
Diabetes & Endocrinology (#9)
Diabetes & Endocrinology (#9)
Diabetes & Endocrinology (#9)
*Tied for #1 rankings
*Tied for #1 rankings
*Tied for #1 rankings
*Tied for #1 rankings

No hospital is best for every patient.
of the annual physician surveys, because reliable objective data aren’t available for those areas of care.
Based on input from experts and medical studies, we have revised the ranking methodologies over time to make the rankings even more useful to consumers.
Beyond the specialty rankings, a set of 22 hospital ratings gives patients information about which hospitals excel in specific procedures, such as hip replacement, or in caring for patients with certain conditions, such as heart attack. This year, two new ratings assess hospitals’ performance in treating heart arrhythmias such as atrial fibrillation and in safely implanting pacemakers. Hospital perfor-
mance in these procedures and conditions can be found in the Best Regional Hospitals rankings (Page 179), designed to help consumers identify hospitals with expertise in numerous areas of care. If you want to learn more, additional detail is available at health.usnews.com/best-hospitals.
To be considered for ranking in most specialties, a hospital had to meet any of four criteria. It had to either: be a teaching hospital; be affiliated with a medical school; have at least 200 beds; or have at least 100 beds and offer at least four out of eight advanced medical technologies.
The hospitals next had to meet a volume requirement in each specialty—a minimum number of Medicare inpatients from 2021 to 2023 who received certain procedures and treatment for specific conditions. A hospital that fell short was still eligible if nominated in the specialty by at least 1% of physicians responding to the expert opinion survey.
At the end of the process, 2,269 hospitals remained candidates for ranking in at least one specialty. Each received a U.S. News score of 0 to 100 based on the four elements, described below. Then, in most specialties, the top 50 hospitals were ranked. Scores and data for the rest are at usnews.com. The four elements and their weights in most specialties are: Patient outcomes (45%): Success at keeping patients alive and getting them home was judged by the proportion of Medicare inpatients with certain conditions in 2021, 2022 and 2023 who died within 30 days of hospital admission or were discharged to another health care facility. Both of these rates were adjusted to account for the severity of patients’ illnesses and the complexity of their care as well as risk-elevating factors such as advanced age, obesity, high blood pressure and poverty (as reflected by whether they received Medicaid).
A widely used approach to so-called risk adjustment was employed to adjust each patient’s risk in calculating odds of a good outcome. To avoid penalizing institutions receiving the sickest patients, we excluded patients transferred in from another hospital from our analysis. A score of 5 indicates the best chance of survival or discharge to home (and 1 the worst) relative to other hospitals.
In three specialties where same-day (a.k.a. outpatient) surgery is common, a third outcome—potentially preventable complications following outpatient surgery—also factored in the rankings.
Patient experience (5%): Most hospitals are required to assess patients’ satisfaction with their experience using a survey known as the Hospital Consumer Assessment of Healthcare Providers and Systems, or HCAHPS. The score reflects how many patients had a positive overall experience during hospitalization.
Other care-related indicators (35%): The balance of patients per nurse and the hospital’s number of patients—an indicator of its degree of experience in a specialty—are examples of these factors.
Expert opinion (12 - 15%): Specialists were asked to name up to five hospitals that they consider best in their area of expertise for patients with the most difficult medical problems. In the 2025 survey alone, responses were tallied from more than 26,000 physicians.
The figures shown in the tables under “% of specialists recommending hospital” are the average percentages of specialists in 2023, 2024 and 2025 who recommended a hospital. In rehabilitation, expert opinion carried a weight of 30%. In the three specialties based entirely on expert opinion, a hospital had to be cited by at least 5% of responding physicians in the last three years of U.S. News surveys in order to be ranked.
Transparency (3%): In four specialties, hospitals are rewarded for participating in nationwide programs that measure their performance and opting to transparently share results with the public.
If you’ve consulted past editions of this U.S. News Best Hospitals guidebook, you may notice that a particular hospital you’re considering has risen or fallen in the rankings. A decline shouldn’t automatically be interpreted as a decline in performance; rather, it may be because of changes to the methodology or because other hospitals improved.
The bottom line is that no hospital— no matter how excellent—is best for every single patient. You’ll want to add your own fact-gathering to ours and consult with your doctor or other health professional as you weigh your options for where to go to get your care. l
CARF: Accredited by the Commission on Accreditation of Rehabilitation Facilities International as of March 5, 2025.
Completion of care rate: How often a hospital avoids needing to transfer patients to an acute-care hospital during their rehabilitation.
Discharge to home score: Reflects proportion of patients who, at discharge, went home rather than to a nursing home or other facility.
FACT accreditation level: Hospital meets Foundation for the Accreditation of Cellular Therapy standards as of Feb. 13, 2025 for harvesting and transplanting stem cells from a patient’s own bone marrow and tissue (level 1) and from a donor (level 2) to treat cancer.
Flu vaccination rate: Percentage of hospital’s staff who received a seasonal flu vaccine.
NAEC epilepsy center: Designated by the National Association of Epilepsy Centers as of April 8, 2025 as a regional or national referral facility (level 4) for staffing, technology and training in epilepsy care.
NCI cancer center: Designated by the National Cancer Institute as of Feb. 13, 2025 as a clinical or comprehensive cancer hospital.
NIA Alzheimer’s center: Designated by the National Institute on Aging as of June 2, 2025 as an Alzheimer’s Disease Center, indicating high quality of research and clinical care.
Number of patients: Except in rehabilitation, estimated number of Medicare patients in 2021, 2022 and 2023 who received certain high-level care as defined by U.S. News. Based on an adjustment to the number of such patients with traditional Medicare insurance. In obstetrics and gynecology and ear, nose and throat, inpatients and outpatients were included; in other specialties, only inpatients. In geriatrics, only patients ages 75 and older were included. In rehabilitation, only patients treated in 2023 were included.
A Nurse Magnet hospital: Recognized by the American Nurses Credentialing Center as of April 30, 2025 for nursing excellence. Nurse staffing score: Relative balance of nonsupervisory registered nurses (inpatient and outpatient) to average daily number of all patients. Inpatient staffing receives greater weight. Agency and temporary nurses are not counted.
Outpatient outcome score: Reflects proportion of patients who experienced a
potentially preventable complication following outpatient surgery.
Patient experience: Percentage of patients who responded positively to a survey about overall quality of their stay.
Patient services score: Number of services offered out of the number considered important to quality (such as genetic testing in cancer and an Alzheimer’s center in geriatrics).
% of specialists recommending hospital: Percentage of physicians responding to U.S. News surveys in 2023, 2024 and 2025 who named the hospital as among the best in their specialty for especially challenging cases and procedures, setting aside location and cost.
Transparency score: Indicates whether the hospital publicly reports its performance through the American College of Cardiology, the American Heart Association and the Society of Thoracic Surgeons (in cardiology and heart surgery), the American Heart Association (in neurology and neurosurgery) or the Society of Thoracic Surgeons (in pulmonology and lung surgery), and whether the hospital completed a U.S. News survey about maternity care (in obstetrics & gynecology).
Rank: Based on U.S. News score except in ophthalmology, psychiatry and rheumatology, where specialist recommendations determined rank.
Readmission prevention rate: How often a hospital keeps patients from being readmitted to an acute-care hospital within the 30 days following discharge.
Successful discharge rate: How often patients go directly home from this hospital and remain at home, rather than requiring further institutional care.
Survival score: Reflects patient survival rate in the specialty within 30 days of admission.
Technology score: Reflects availability of technologies considered important to a high quality of care, such as PET/CT scanner in pulmonology and diagnostic radioisotope services in urology.
Trauma center: Indicates a Level 1 or 2 trauma center. Such a center can care properly for the most severe injuries.
U.S. News score: Summary of quality of hospital inpatient care. In most specialties, survival is worth 36%, discharge to home 9%, operational quality data such as nurse staffing and patient volume 35%, specialists’ recommendations 15% and patient experience 5%.

UCSF MEDICAL CENTER, RANKED NO. 7


(CONTINUED)

van den Brink, M.D., Ph.D. President, City of Hope Los Angeles and City of Hope National Medical Center

Our cancer breakthroughs bring hope to millions every year.







ON PAGE 112)
“I technically died, and here I am. I’m incredibly lucky. I could not have been in better hands.”
—Guy Monseair, City Island Rowing Coach
“We had an immediate critical decision to make in the race to save Guy’s life. We decided to proceed with emergent quadruple coronary artery bypass surgery despite Guy’s swollen and weak heart resulting from his acute heart attack and cardiac arrest. There are very few health systems in the country with the knowledge base and the skill that we have at Montefiore Einstein for managing these kinds of complex life-threatening conditions.”

—Robert Michler, MD
Surgeon-in-Chief and Chair, Surgery and Cardiothoracic and Vascular Surgery Montefiore Einstein
See Guy’s story at montefiore.org/guy
Adventist HealthCare
Shady Grove Medical Center
Rockville, MD
Kevin Richman, MS, AACC
Dennis Friedman, MD, FACC Bayhealth Hospital, Kent Campus Dover, DE
Benjamin Louis Collins, MBA, BSN, RN, AACC
Roberto Scaffidi, MD, FACC
Bayshore Medical Center Holmdel, NJ
Cristina Chonko, AGPCNP-BC, AACC
Shaddy Younan, MD, FACC
CentraState Medical Center Freehold, NJ
Amy Quinlan, DNP, MBA, APN, RCIS, AACC
Robert Kayser, MD, MBA, FACC
ChristianaCare Christiana Hospital Health Services Newark, DE
Jennifer Oldham, MSN, RN, CEN, AACC
Neil Wimmer, MD, MSc, FACC
Conemaugh Memorial Medical Center Johnstown, PA
Sarah Vasilko, PA-C, AACC
Dinesh Sharma, MD, FACC Cooper University Hospital Camden, NJ
Tamara Wolf, MSN, RN, AACC
Phillip Koren, MD, FACC
Hackensack University Medical Center Hackensack, NJ
Tammy Russo, ACNP, AACC
Vaidya J. Pranaychandra, MD, FACC
Inspira Medical Center – Vineland Vineland, NJ
Tricia Crowe, MSN, RN, AACC
Andrew P. Zinn, MD, FACC
Inspira Medical Center – Mullica Hill
Mullica Hill, NJ
Bryan Gill, CVRN-BC, RN, AACC
Ashfaque Unwala, MD, FACC
The American College of Cardiology proudly recognizes hospitals and health care facilities that achieve the HeartCARE Center distinction, along with the CV champions whose leadership makes this achievement possible. This accomplishment is supported by the dedication of physicians and care team members, including credentialed Fellows and Associates of the ACC. To further highlight this honor, the HeartCARE Center award is featured in hospital profiles on the Find Your Heart a Home tool at CardioSmart.org
Jefferson Einstein Philadelphia Hospital Philadelphia, PA
Yolanda Nixon, ACNP-BC, CRNP, MSN, AACC
Sumeet K. Mainigi, MD, FACC
Jersey Shore University Medical Center Neptune, NJ
Jennifer Heck-Kanellidis, DNP, APN-C, HNP, BSN, RN, AACC
Brett Sealove, MD, FACC
JFK University Medical Center
Edison, NJ
Charyl Asuncion, AGPCNP-BC, MSN, AACC
Saleem Husain, MD, FACC
Lahey Hospital and Medical Center
Burlington, MA
Janice Morrissette, BSN, RN, AACC
Frederic S. Resnic, MD, FACC
Lawrence General Hospital Lawrence, MA
Kathy Caredeo, RN, BSN, MSN, AACC
Sunit Mukherjee, MD, FACC
Ocean University Medical Center Brick, NJ
Jennifer Heck-Kanellidis, DNP, APN-C, HNP, BSN, RN, AACC
Ali Moosvi, MD, FACC
Penn Medicine Chester County Hospital West Chester, PA
Ralph Smith, RN, BSN, AACC
Timothy Boyek, MD, FACC
Regional Hospital of Scranton Scranton, PA
Debra Jadick, NP, AACC
Thomas Dzwonczyk, MD, FACC Riverview Medical Center Red Bank, NJ
Elvira Baquerizo, MSN, MBA, APN, NP-C, CCRN, AACC
Ravi Diwan, MD, FACC
Southern Ocean Medical Center Manahawkin, NJ
Jennifer Heck-Kanellidis, DNP, APN-C, HNP, BSN, RN, AACC
Mahesh K. Tekriwal, MD, FACC
St. Francis Hospital and Heart Center
Roslyn, NY
Kristin Michele Pasquarello, MPAS, PA-C, AACC
Thomas W. Pappas, MD, FACC
UPMC Altoona Altoona, PA
Kristi Montrella, ACNP-BC, AACC
George Jabbour, MD, FACC
Wynn Hospital Utica, NY
Stephanie Mathias, BSN, RN, CCRN, AACC
Hugh MacIsaac, MD, FACC
SOUTH
AdventHealth Carrollwood Tampa, FL
Tracy Berg, ARNP, AACC
Humberto Coto, MD, FACC
AdventHealth Dade City Dade City, FL
Deborah Moore, MSN, RCIS, RN, AACC
Aung Tun, MBBS, FACC
AdventHealth Heart of Florida Davenport, FL
Tracy Bruck, DNP, EdS, MSN, RN, CHFN, AACC
Prem Srinivas Subramaniyam, MBBS, FACC
AdventHealth North Pinellas Tarpon Springs, FL
Belinda Michelle Spahn, BSN, CCRN, AACC
Norman S. Abbott, MD, FACC
AdventHealth Ocala Ocala, FL
Lynn Smith, RN, MBA, MHA, AACC
Robert L. Feldman, MD, FACC
AdventHealth Sebring Sebring, FL
Yesica Torres, BSN, RN, CHFN, AACC
Deepti Bhandare, MD, FACC
AdventHealth Tampa, Pepin Heart Institute Tampa, FL
Tracie Hughes, BSN, RN, CCRN-K, AACC
Charles R. Lambert, MD, PhD, MBA, FACC
Please visit CVQuality.ACC.org/HCC to learn how your facility can achieve ACC’s HeartCARE Center recognition.
AdventHealth Wesley Chapel
Wesley Chapel, FL
Allison K. Sutton, APRN, FNP-C, AACC
Asad Sawar, MBBS, FACC
AdventHealth Zephyrhills Zephyrhills, FL
Deborah Moore, MSN, RCIS, RN, AACC
Aung Tun, MBBS, FACC
Augusta Health Fishersville, VA
Willie Roden, MBA, BSN, RN, FACHE, AACC
Kenneth S. Sternberg, DO, FACC
Baptist Health Lexington Lexington, KY
Christopher Bell, APRN, AACC
Azhar Aslam, MD, FACC
Baptist Health Paducah Paducah, KY
Blair Lane Brockman, NP, AACC
Craig J. Beavers, PharmD, FACC
Baptist Memorial Hospital – DeSoto Southaven, MS
Amanda Sesti, MHA, BSN, RN, AACC
Arie Szatkowski, MD, FACC
Baylor St. Luke’s Medical Center Houston, TX
Seth Stephens, ACNP-BC, APRN, CPHQ, DNP, AACC
Emerson C. Perin, MD, FACC
Carilion Roanoke Memorial Hospital Roanoke, VA
Sheree Emore, MSN, FNP-BC, AACC
Gregory Dehmer, MD, MACC
CarolinaEast Medical Center
New Bern, NC
Laura Peters, BS, RT, AACC
Alex Kirby, MD, FACC
CHRISTUS Mother Frances Hospital Tyler, TX
Christine Mendoza, CCRN, BSN, CCRN-CMC, CSC, AACC
Clyde Fagg Sanford, MD, FACC
CHRISTUS Ochsner St. Patrick Hospital Lake Charles, LA
Anna C. Landry, NP, AACC
Michael C. Turner, MD, FACC
CHRISTUS St. Frances Cabrini Hospital Alexandria, LA
Erika D. McCormick, BSN, RN, CCRN, AACC Reymond Meadaa, MD, FACC
Cleveland Clinic Indian River Hospital Vero Beach, FL
Kimberly Nance, RN, BSN, CPHQ, AACC
James Wudel, MD, FACC
East Jefferson General Hospital Metairie, LA
Nicole Jones, MN, APRN, ACNS-BC, CCNS, CHFN, AACC
Ala Mohsen, MBBS, FACC
Frye Regional Medical Center Hickory, NC
Seth A. Call, PA-C, AACC
John Andrew Morrison, MD, FACC
Hamilton Medical Center Dalton, GA
Rachel Lynnette Bennett, BSN, RN, CEN, AACC
Ahsan Achtchi, DO, FACC Hillcrest Hospital South Tulsa, OK
Brian Smith, MS, RCIS, RT, ARRT, AACC
Stanley Kyle Zimmerman, MD, FACC
Jackson–Madison County General Hospital Jackson, TN
Dylan Wilson, BCPS, PharmD, AACC
John W. Baker, MD, FACC
King’s Daughters Medical Center Ashland, KY
Kristy Turley, APRN, AACC
Jerry White, DO, FACC
Lexington Medical Center
West Columbia, SC
Dawn C. Crumpton, BSN, RN, AACC
Robert M. Malanuk, MD, FACC
Medical Center Hospital
Odessa, TX
Rene Rodriguez, DNP, RN, AACC
Manohar Angirekula, MBBS, FACC
Memorial Hermann Texas Medical Center
Houston, TX
Sarah Johnson, MSN, APRN, ACNP-BC, AACC
Richard W. Smalling, MC, PhD, FACC
Memorial Regional Hospital
Hollywood, FL
Grace Corona, MSN, BSN, RN, AACC
Ralph Levy, MD, FACC
Methodist Hospital Texsan
San Antonio, TX
Michael K. Hendricks, MBA, RN, AACC
Obinna G. Isiguzo, MBBS, FACC
Methodist Le Bonheur Germantown Hospital
Germantown, TN
John Signa, BS, CVT, MBA, RTR, AACC
Brian Borkowski, MD, FACC
Methodist University Hospital Memphis, TN
Leesa J. Wright, RN, AACC
Oluwaseun Akinseye, MD, FACC
Mon Health Medical Center
Morgantown, WV
Elizabeth Carpenter, CCRN, AACC
Bradford E. Warden, MD, FACC
Norton Audubon
Louisville, KY
Robert T. Rogers, APRN, AACC
Manish Sharma, MD, FACC
Novant New Hanover
Regional Medical Center
Wilmington, NC
Megan A. Whitley-Herrington, PA-C, AACC
John Rommel, MD, FACC
Our Lady of The Lake Regional Medical Center
Baton Rouge, LA
Dawn Denicola, FNP-C, AACC
Denzil Moraes, MD, MB, BCh, FACC
Spartanburg Medical Center
Spartanburg, SC
Jennifer T. Smith, MSN, RN, CVN, AACC
Nalin Srivastava, MD, FACC
St. Luke’s Health Memorial Hospital
Lufkin, TX
Jamie Huckabee, FNP-C, AACC
Ravinder R. Bachireddy, MD, FACC
St. Mary’s Medical Center
Huntington, WV
Shari Wiley, APRN-BC, FNP, CHFN, AACC
Daniel Snavely, MD, FACC
Tallahassee Memorial HealthCare
Tallahassee, FL
Caitlin Ubilla, BSN, RN, CV-BC, AACC
Thomas Noel, MD, FACC
Texoma Medical Center
Denison, TX
Lisa Smith, MSN, RN, NE-BC, AACC
Scott Turner, DO, FACC
The Hospitals of Providence Sierra Campus
El Paso, TX
Laura Ann Wilson, AGACNP-BC, CCK, AACC
Edward R. Assi, DO, FACC
United Regional Healthcare System
Wichita Falls, TX
Hilary Wolf, PA-C, BS, MPAS, AACC
Fardin Djafari, MD, FACC
UT Health East Texas
Tyler, TX
Francisco Rivera, ACNP, FNP, AACC
Ajay Pachika, MD, FACC
Woodland Heights Medical Center
Lufkin, TX
Richard Fennell, BSN, CCRN, AACC
Vivek Mangla, MD, FACC
WVU Medicine Camden Clark Medical Center
Parkersburg, WV
Kristina S. Brooks, DNP, AACC
David Gnegy, MD, FACC
MIDWEST
Bryan Medical Center
Lincoln, NE
Sarah Schroeder, PhD, ACNP-BC, AACC
John Allen Steuter, MD, FACC
Corewell Health Grand Rapids Hospital
Grand Rapids, MI
John J. Mulder, MPAS, AACC
Ryan Madder, MD, FACC
Lutheran Hospital
Fort Wayne, IN
Megan Trotter, FNP-C, AACC
Vijay Chilakamarri, MD, FACC
Riverside Medical Center
Kankakee, IL
Cheryl Rogers, NP, CCRN, AGPCNP-BC, CHFN, MSA, AACC
Tarun Jain, MD, FACC
Adventist Health and Rideout Hospital
Marysville, CA
Eric Cooper, BSN, MPA, NE-BC, RN-BC, AACC
Babek Sanei-Fard, MD, FACC
Adventist Health Bakersfield
Bakersfield, CA
Diwata Somera, MSN, RN, CCRN-CMC, AACC
Viral Mehta, MD, FACC
Billings Clinic
Billings, MT
Joslyn Thompson, NP-C, AACC
Claudia Lama Von Buchwald, MD, FACC
Eisenhower Health Medical Center
Rancho Mirage, CA
Sheenah Fernandez, CCRN, MSN, RN, AACC
Philip Patel, MD, FACC
El Camino Health
Mountain View, CA
Kaye Jaramillo, CNS, AACC
Chad Rammohan, MD, FACC
Loma Linda University Medical Center
Loma Linda, CA
Denise Petersen, DNP, FNP-BC, CHFN, AACC
Liset Stoletniy, MD, FACC
Medical Center of Aurora
Aurora, CO
Karen Welter, ACNS-BC, AACC
Christopher Paul Porterfield, MD, FACC
National Jewish Hospital/ Intermountain Health Saint Joseph Hospital
Denver, CO
Dawn Eckler, MSN, NP-C, AACC
Jake Chanin, MD, FACC
Renown Regional Medical Center Reno, NV
Jocelyn Anderson, MMS, PA-C, AACC
Troy Wiedenbeck, MD, FACC
Saint Mary’s Regional Medical Center Reno, NV
Jeremy T. Shea, BSN, CVRN-BC, RN, AACC
Frank Carrea, MD, FACC
ThedaCare Regional Medical Center
Appleton, WI
Dessia Laxton, AGACNP-BC, AACC
Ameer Kabour, MD, MBA, FACC
UCHealth Memorial Hospital Central Colorado Springs, CO
Dawn G. Lovejoy, BSN, RN, AACC
Chris Michael Manhart, DO, FACC

50
50

EVERY MONTH, MILLIONS OF PATIENTS SEARCH FOR TOP DOCTORS AND HOSPITALS ON U.S. NEWS & WORLD REPORT. WE HELP MAKE SURE THEY FIND — AND CHOOSE — YOU.
LET’S TALK ABOUT HOW WE CAN GET YOU MORE PATIENTS.
SCAN THE QR CODE BELOW TO LEARN MORE.




At Montefiore Einstein’s new Comprehensive Brain Health Center.

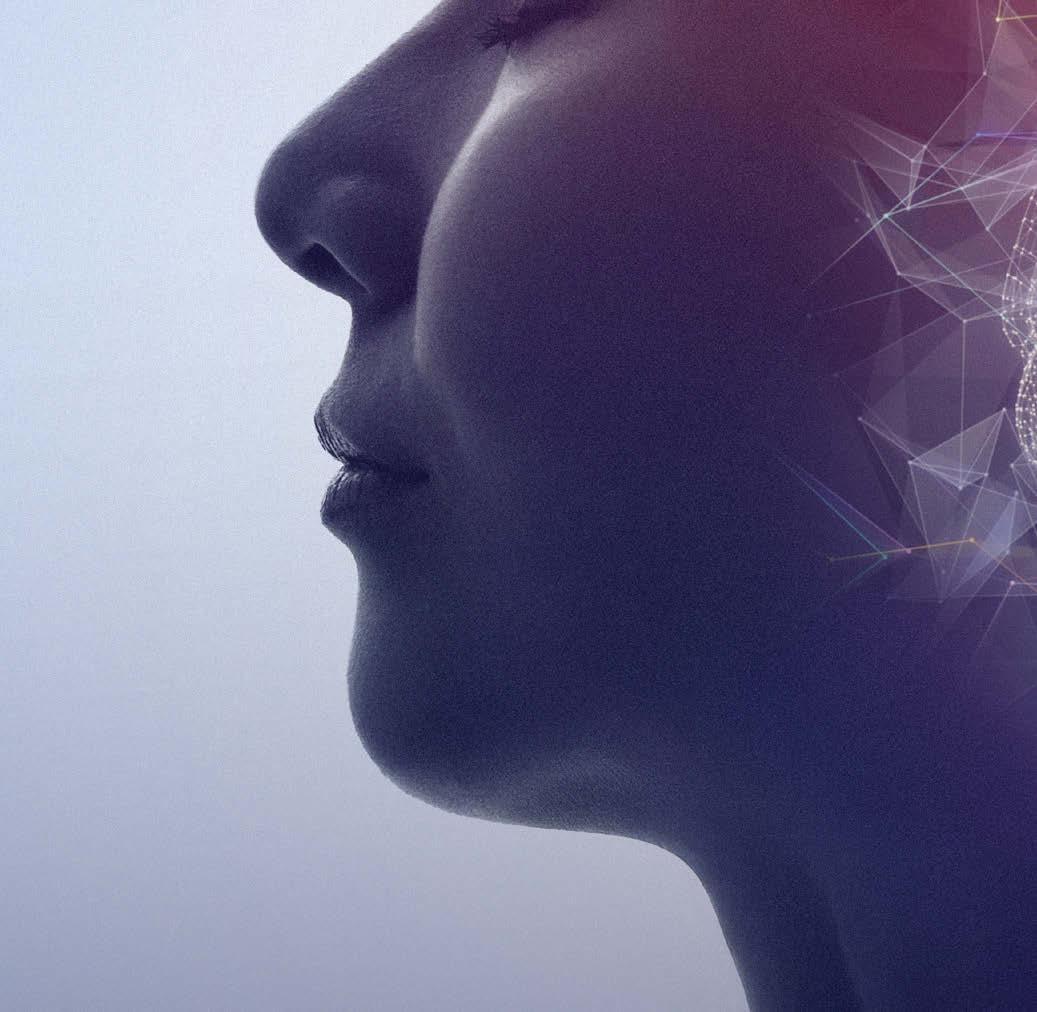





21


At RWJBarnabas Health, we believe that caring for women’s health starts with caring about women. All the more reason we’re proud to share that our hospitals received U.S. News & World Report’s highest rating for best maternity hospitals. This nationwide distinction shows our dedication to the very highest quality in maternity care. Visitrwjbh.org/maternity
CommunityMedicalCenter
MonmouthMedicalCenter

NewarkBethIsraelMedicalCenter
RobertWoodJohnsonUniversityHospital
RobertWoodJohnson UniversityHospitalSomerset
TrinitasRegionalMedicalCenter







MAYO CLINIC-ROCHESTER, RANKED NO. 3





















46
47
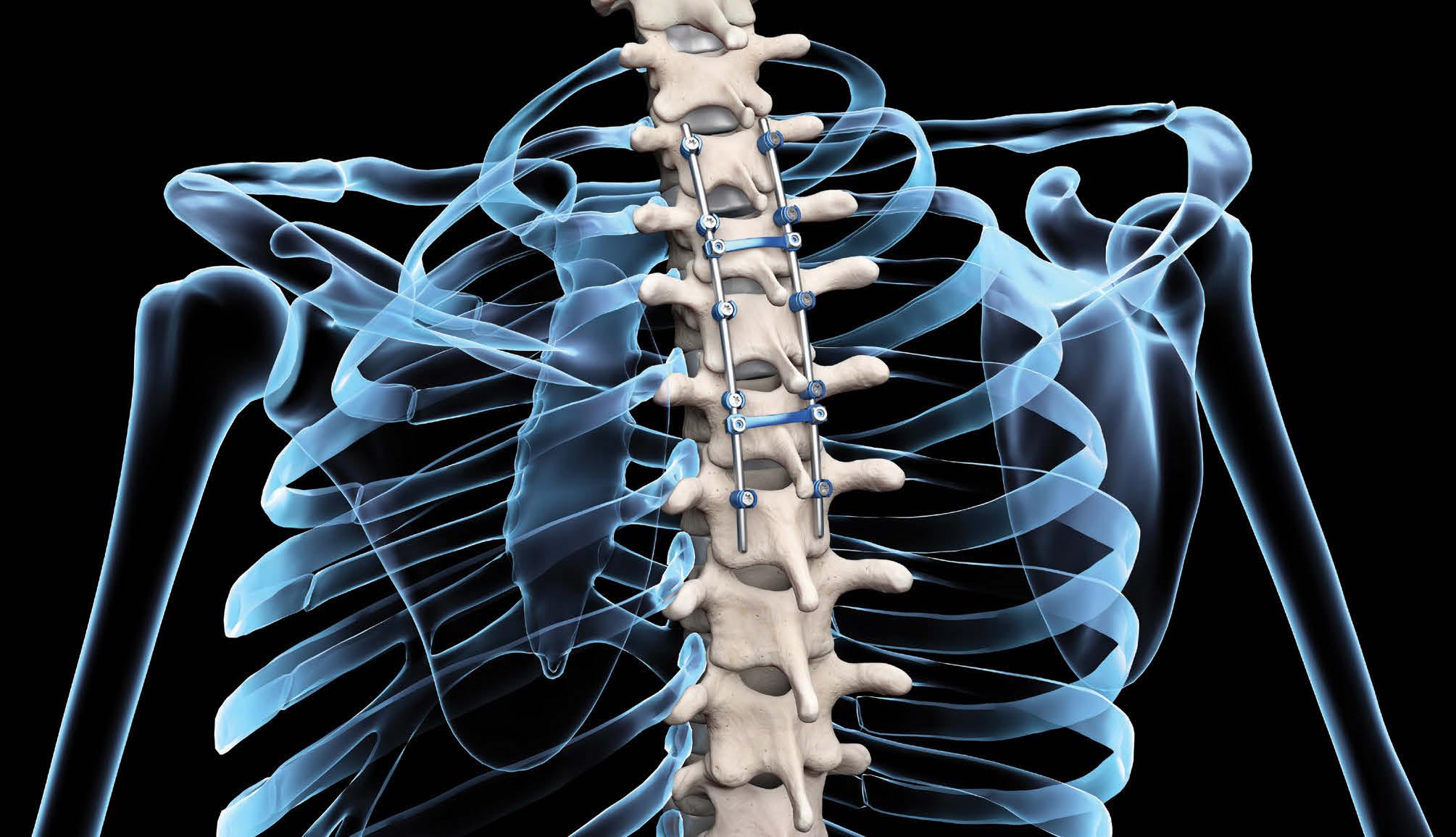


The American Orthopaedic Association applauds the following institutions for their achievements and participation in the Own the Bone® quality improvement program:
AdventHealth Orthopedic Institute, Central Florida Division - Orlando, FL
Advocate Christ Medical Center - Oak Lawn, IL
Allegheny Health Network (AHN)Jefferson Hospital - Jefferson Hills, PA
* Alliance Medical Group / Waterbury HEALTHWaterbury, CT
Allina Health-Buffalo Hospital - Buffalo, MN
* Astera Health - Wadena, MN
Atrium Health MSKI Fracture Prevention Program - Charlotte, NC
Atrium Health Wake Forest Baptist Medical Center with Advocate Health - Winston Salem, NC
Baptist Orthopedic Hospital at Mission TrailSan Antonio, TX
Baton Rouge Orthopaedic Clinic - Baton Rouge, LA
Berkshire Medical Center - Pittsfield, MA
Bryan Medical Center - Lincoln, NE
Cedars-Sinai Medical Center - Los Angeles, CA
* CentraCare St. Cloud Hospital - St. Cloud, MN
Cleveland Clinic Akron General Osteoporosis and Bone Health Center - Akron, OH
Coastal Orthopedic & Spine InstituteCamarillo, CA
Connecticut Orthopedic Institute's Bone Health Program at St. Vincent's Medical Center - Bridgeport, CT
Cooper Bone and Joint Institute - Camden, NJ
Firelands Physician Group - Sandusky Orthopedics and Pain ManagementSandusky, OH
Froedtert & the Medical College of WisconsinMilwaukee, WI
Grady Health System - Atlanta, GA
* Great Falls Clinic- Bone Health - Great Falls, MT
Hartford HealthCare Bone and Joint InstituteHartford, CT
Henry Ford Hospital - Detroit, MI
Hoag Orthopedic Institute - Irvine, CA
Huntington Hospital - Northwell HealthHuntington, NY
Johnson City Medical Center Hospital (Ballad Health) - Johnson City, TN
JPS Health Network - Fort Worth, TX
Lahey Hospital and Medical CenterBurlington, MA
* Lake Cumberland Orthopedics and Surgical Podiatry - Somerset, KY
Institutions are recognized for at least 75% compliance on at least 5 of the 10 recommended secondary fracture prevention measures over the last year.
Lexington Medical Center - West Columbia, SC
Loyola Medicine - Maywood, IL
Luminis Health - Annapolis, MD
MaineGeneral Orthopaedics - Augusta, ME
Marshfield Clinic Health System - Marshfield, WI
Medical University of South CarolinaCharleston, SC
Memorial Regional Hospital - Hollywood, FL
Mendelson Orthopedic Specialists -
A Synergy Health Partners Practice - Livonia, MI
Mount Sinai South Nassau - Oceanside, NY
Nephrology Associates, SC - Waukesha, WI
NMC Health Orthopedics & Sports SpecialistsNewton, KS
North Central Baptist Hospital - San Antonio, TX
Norton Women's and Children's HospitalLouisville, KY
NYU Langone Hospital- Long Island - Mineola, NY
NYU Langone Orthopedic Hospital - New York, NY
OhioHealth Orthopedic & Sports Medicine
Physicians - Mansfield Hospital - Columbus, OH
Orthopaedic Associates of MichiganGrand Rapids, MI
^Orthopedic Associates of SW Ohio - Dayton, OH
^Park Nicollet Methodist Hospital/TRIA
Orthopaedic Center - Minneapolis, MN
^Prisma Health-Upstate - Greenville, SC
ProHealth Care Oconomowoc Memorial Hospital - Oconomowoc, WI
ProHealth Care Waukesha Memorial HospitalWaukesha, WI
ProMedica Toledo Hospital - Toledo, OH
Regions Hospital - St. Paul, MN
* Reno Orthopedic Center - Reno, NV
Resolute Baptist Hospital - New Braunfels, TX
* Saint Alphonsus Orthopedics & Sports
Medicine- Boise - Boise, ID
^Sanford Medical Center - Fargo - Fargo, ND
Sauk Prairie Healthcare - Prairie du Sac, WI
South Texas Fracture Prevention ClinicSan Antonio, TX
Spartanburg Regional Healthcare SystemSpartanburg, SC
SSM Health Dean Medical Group OrthopedicsMadison, WI
St. Luke's Health System Osteoporosis and Bone Health Program - Boise, ID
St. Peter's Health - Helena, MT
* Steamboat Orthopaedic and Spine InstituteSteamboat Springs, CO
Tahoe Forest Health System - Truckee, CA
Tallahassee Memorial HealthCareTallahassee, FL
The Bone and Joint Center - Albany, NY
The Bone and Joint Center at AdventHealth Zephyrhills - Zephyrhills, FL
The Centers for Advanced Orthopaedics, Mid-Maryland Musculoskeletal Institute (MMI) - Frederick, MD
The Methodist Hospitals, Ortho Spine CenterMerrillville, IN
The Ohio State University Wexner Medical Center - Columbus, OH
^The Queen's Medical Center - Honolulu, HI
The University of Texas at AustinUT Health Austin - Austin, TX
* The University of Texas Medical BranchGalveston, TX
TSAOG Orthopaedics and SpineSan Antonio, TX
University Hospital - San Antonio, TX
University of Chicago - Chicago, IL
University of Cincinnati - Cincinnati, OH
University of Iowa Health Care Department of Orthopaedics - Iowa City, IA
* University of Miami Health SystemOrthopaedic Department - Miami, FL
University of Missouri-Columbia Department of Orthopaedic Surgery - Columbia, MO
^University of Texas Southwestern Medical Center- Dallas, TX
University of Wisconsin Hospitals and ClinicsMadison, WI
UT Health East Texas Orthopedic and Sports Medicine Institute - Tyler, TX
VCU Orthopedics - Richmond, VA
Virtua Voorhees Hospital - Voorhees, NJ
WVU Medicine - Wheeling HospitalWheeling, WV
^WVU Medicine Department of OrthopaedicsMorgantown, WV
^Yale New Haven Hospital Fragility Hip Fracture Program - New Haven, CT
Blanchard Valley Orthopedics & Sports Medicine - Findlay, OH
Bozeman Health - Bozeman, MT
Clear Lake Bone Institute - Webster, TX
Enloe Health - Chico, CA
Excelsior Orthopaedics - Amherst, NY
Fremont Orthopaedics - Lander, WY
Mount Sinai Health System
Department of Orthopedic SurgeryNew York, NY
NeuroSpine Center of WisconsinAppleton, WI
OrthoCincy Orthopaedics and Sports Medicine - Edgewood, KY
OrthoMichigan - Flint, MI
University of Rochester/ Strong Memorial HospitalRochester, NY
University of Utah HealthSalt Lake City, UT

4




49
50


1
5
50
The best hospital for you or a loved one depends on the type of care you need. For a rare bone condition or a lung transplant, for instance, you may need to travel to a hospital that earned a top 50 national ranking for orthopedics or pulmonology, respectively. But for a common procedure or condition like a hip replacement or COPD, you are likely to find that a hospital close to home is highly rated by U.S. News.


The quality of health care provided by hospitals to patients across the nation varies widely. U.S. News delves into various quality measures to publish rankings and ratings of hospitals that assist millions of patients annually. These patients face the prospect of surgery or specialized hospital care that can pose a risk due to such factors as age, physical condition or the type of illness. The rankings and ratings are a tool to help consumers make important health care decisions, in conjunction with advice from medical practitioners.
U.S. News’s Best Hospitals project evaluates U.S. adult hospitals annually on how they provide 37 different types of care. The rankings of 15 medical specialties use a variety of quality measures to identify the hospitals that excel at handling the most complex and difficult cases. The ratings of 22 common procedures and conditions are based entirely on objective quality indicators, such as patient outcomes and nurse staffing levels. We also publish

an Honor Roll of the hospitals that excel in many types of care, as well as rankings of general hospitals by state and major metro area.
Hospitals that earn top 50 rankings in a specialty have a gold Best Hospitals award “badge” (logo) on their U.S. News profile page, with information about how many such rankings they won. General hospitals that excel in a large number of common procedures and conditions have a silver “Best Regional Hospitals” silver badge and may be ranked in their state and/or metro area. Hospitals that place in the top 10% for a specialty but not in the top 50, or that achieve the highest possible rating for a common procedure or condition, have a High Performing Hospitals emblem on their profile page.

Hospitals that earn a badge or emblem may obtain permission, for a fee, to display the badge or emblem via websites and other media from BrandConnex, U.S. News’s licensing agent. Current and future rankings, ratings and awards are not affected by such purchases or by any other promotional fees.
• The evaluation of hospitals in your area: https:bit.ly/USN-area


• For detailed information about a specific hospital: https://bit.ly/USN-search
• About U.S. News’s hospital evaluations, including Best Children’s Hospitals and Best Hospitals for Maternity Care as well as Best Hospitals: https://bit.ly/USN-FAQ
• Detailed methodology reports about the Best Hospitals specialty rankings https://bit.ly/USN-2526 and the procedures and conditions ratings https://bit.ly/USN-ratings
• Hospitals that earn a badge or emblem may contact usnews@BrandConnex.com for information about using U.S. News Best Hospitals badges and emblems.
5
15



These hospitals are among the best in their specialty for particularly challenging patients, in the view of at least 5% of medical specialists surveyed by U.S. News over the past three years.
1
2 Wills Eye Hospital, Thomas Jefferson U. Hospitals, Philadelphia
3 Wilmer Eye Institute, Johns Hopkins Hospital, Baltimore 19.0%
4 Mass Eye and Ear, Massachusetts General Hospital, Boston
5
6
9

U.S. News’ ratings identified 353 centers that excel—here they are.
When it comes to maternity care for uncomplicated pregnancies, the best hospitals achieve safe outcomes, offer sound care without performing unnecessary interventions and support patients who choose to breastfeed. The hospitals listed here excel in these respects. To identify them, we surveyed maternity centers across the nation and obtained detailed data from more than 800. As always, we recommend consulting with your doctor when deciding which hospital to use.
continued
Kaiser Permanente Baldwin Park Medical Center, Baldwin Park
Kaiser Permanente Downey Medical Center, Downey
Kaiser Permanente Fontana & Ontario Medical Centers, Fontana V.
Panorama
Permanente Riverside Medical Center, Riverside
Kaiser
Visalia
Loma Linda University Medical Center-Murrieta
Lucile Packard Children’s Hospital Stanford, Palo Alto
Miller Children’s & Women’s Hospital Long
Sutter
Tahoe Forest Hospital District, Truckee
UCHealth Highlands Ranch Hospital, Highlands Ranch
continued
Endeavor Health Elmhurst Hospital, Elmhurst
Endeavor Health NorthShore Hospitals, Evanston
Endeavor Health Swedish Hospital, Chicago
Endeavor Health Northwest Community Hospital, Arlington Heights
Northwestern Medicine Central DuPage Hospital, Winfield
Northwestern Medicine Delnor Hospital, Geneva
Northwestern Medicine-McHenry, Huntley, Woodstock Hospitals, McHenry
Northwestern Medicine-Northwestern Memorial Hospital, Chicago
SIH Memorial Hospital of Carbondale
of Chicago Medical Center
Health Floyd, New Albany
Clark Memorial Hospital, Jeffersonville
Indiana University Health Bloomington Hospital, Bloomington
Corewell Health Gerber Hospital, Fremont
Corewell Health Trenton Hospital, Trenton
Corewell Health Farmington Hills Hospital, Farmington Hills
Corewell Health Grand Rapids Hospitals-Blodgett & Butterworth, Grand
Henry Ford Jackson Hospital, Jackson
Henry Ford West Bloomfield Hospital, West Bloomfield
Henry Ford Wyandotte Hospital, Wyandotte
What parents need to know about protecting their kids’ physical and mental well-being






A helmet isn’t always enough to protect your child. Take a deep dive into kids’ head injuries—from warning signs to recovery.
by Annika Urban ©
E’VE COME a long way from the days of brushing off a blow to the head as “just a bump” or letting kids jump back into the game while still dazed. But concussions are still a serious and surprisingly common issue among children.
WMore than 2 million kids age 17 and under in the U.S. experience a concussion each year, according to the Centers for Disease Control and Prevention. While sports are often the culprit, these injuries can also happen on playgrounds, during car accidents, or even result from a fall at home.
So what should parents know? Here’s your guide to understanding, identifying and managing concussions in kids—plus how to help prevent them in the first place.
A concussion is a traumatic brain injury caused by a blow or jolt to the head that disrupts a person’s normal brain function. While concussions occur frequently during sports, children can sustain them in any setting, including from car
and playground accidents or a fall from heights. When someone experiences a concussion, the sudden movement injures the brain, says Dr. Mathew Stokes, the director of the Neuro-Concussion Clinic at Children’s Health in Dallas, Texas and an associate professor at UT Southwestern Medical Center. The injury causes changes to nerve cells and how they send messages to each other.

Experts describe a concussion as a “software” injury because structurally, the brain looks the same on imaging tests. “But there’s a functional change in how the brain is signaling, what it’s doing that can translate into different types of symptoms,” says Stokes.
Only about 10% of concussions involve loss of consciousness, so don’t count on a child “blacking out” as the key sign, says Dr. Cynthia LaBella, the medical director of the Institute for Sports Medicine at the Ann & Robert H. Lurie Children’s Hospital of Chicago and a professor of pediatrics at Northwestern University’s Feinberg School of Medicine.
Because the brain controls so many different functions, symptoms can vary widely. They may include headaches, dizziness, nausea, sensitivity to light or noise, brain fog or

feeling “out of it “ and seizures or repeated vomiting (all of which require medical care).
“A blow to the head and any set of symptoms can signal a possible concussion,” says Gerard Gioia, director of the Safe Concussion Outcome, Recovery & Education (SCORE) Program at Children’s National Hospital in Washington D.C. “A good way to detect a suspected concussion is to use our free smartphone app, called ‘SCORE 4 BrainHealth.’ It guides the user through signs and symptoms and helps to cover the bases, especially if the more common symptoms like headache, dizziness and fatigue are not present initially.”
In some kids, however, symptoms may be more subtle—or nonexistent. And acting in a way that’s uncharacteristic of their personality can also be a sign that a child has sustained a con-
cussion. “Kids may not report any symptoms, but they just aren’t acting like their usual self,” says LaBella. ”Maybe the kid is usually pretty enthusiastic, and suddenly they become very sullen and quiet, or vice versa; a kid who’s usually pretty quiet all of a sudden starts jabbering a lot.”
There’s no single test to diagnose a concussion. Instead, doctors will generally perform neurological exams and cognitive testing to determine whether a child might have a concussion. They will also take detailed medical histories
of the patients and their family members. Conditions like ADHD, anxiety, depression or migraines—even if not previously diagnosed— can influence symptoms and recovery. Knowing this helps doctors personalize treatment.
As for imaging tests like CT scans or MRIs? They’re not typically used unless there’s concern about a skull fracture or brain bleed. “MRI is often used later on, when we’re trying to understand other factors that are playing into this person’s unusual or atypical or prolonged recovery,” explains Gioia.
More advanced tools for diagnosing a concussion may be on the horizon. Promising blood tests are being developed, including one FDA-approved test that measures proteins released by the brain into the blood— but these are currently focused on adult patients. A multi-institutional study called CARE4Kids is exploring whether bloodwork and brain imaging can help predict which children are more likely to experience longterm symptoms.
There is a major risk in sending a child back into the game after a concussion. “They could get that second impact on top of the concussion, which could result in a very severe or catastrophic injury like brain swelling or brain bleed,” explains LaBella.
Moreover, children that sit out of the game rather than continuing to play generally recover better. “You will have a faster recovery if you pull yourself out and rest right away,” says LaBella. “If you continue to play the rest of the game or the rest of the practice with a concussion, you may avoid getting another hit, but end up worsening your symptoms—and that’s going to prolong recovery.”
The best concussion care starts with prevention. Experts agree that the first line of defense in preventing childhood concussions is improved sports technique, including knowing how to fall and strengthening of neck and core muscles.
Enforcing rules that better protect players during competition is also needed. Gioia has been working with a group of experts around the country to produce a “developmental readiness model” that could eventually provide guidance, based on a child’s development. “This information will better guide a family—beyond just age alone—as to which sports and at which level the youth athlete is developmentally ready to learn and play successfully,” says Giola. “We are starting with youth football in determining the right fit for any given player as to whether they are ready to participate in flag, modified tackle or full tackle game. We want kids to have maximal fun and enjoyment while reducing injury risk because of misplacement.”
As for helmets, it’s a common misconception that they can protect kids and adults against concussions.“Helmets were designed, especially in football, to prevent more severe head injuries, particularly skull fractures and intracranial bleeds,” says LaBella.
Stokes points out that in places where there are no restrictions on kids and impact in sports, children at the age of 6 and 7 are playing football in helmets that cause their heads to wobble. At that age, children don’t have the neck strength to hold up their head in a heavy helmet, much less to stabilize their head when it takes a blow or during a hard fall, he says.
Following the rule “when in doubt, sit it out” can be life-changing. If a child has sustained a blow to the head or whiplash, it is always safer to assume they have a concussion than to ignore signs and symptoms or write them off as “just a headache.”
While you may have heard that the best way to manage a concussion is to sit in a quiet, dark room, typically this is not the case. Instead, researchers and doctors are seeing positive results from what they call active rehabilitation. “This is a gradual treatment process that takes the person’s specific symptoms into account and gradually returns them to their everyday routines while still managing their symptoms,” says Giola. “There’s been some very good data to show how this improves recovery in kids.”
Stokes explains that for a child who’s been participating in sports regularly, completely cutting out activity can be harmful to their mental and emotional health. “If you take a kid who’s an athlete—whose life is based on playing sports—and you shut them down for two, three weeks, you’ve created a kid who’s now losing their physical conditioning and is starting to develop anxiety and depression because they’re not participating,” he says.
Lifestyle is an important component of active rehabilitation. It’s recommended that during recovery, kids should aim to sleep well at night and avoid day naps, eat three meals a day, stay hydrated and manage stress as much as possible.
Schools also play a pivotal role in a child’s post-concussion recovery. “The school as a partner is very important,”
says Giola. “We have found that students who are out of school for lengthy periods of time do not do as well as students who return to school. But it’s important to provide the student with support.”
Gioia has worked to develop the “STAMP,” which stands for symptom-targeted academic management plan and can help schools be partners in aiding a student’s recovery by recommending specific plans based on a child’s symptoms. “Having a specified person to help guide and monitor the child, such as the guidance counselor, school nurse, athletic
trainer, school psychologist or administrator, is very important,” explains Giola.
The good news? While there are many steps parents and coaches can take to help minimize the chance of a concussion, you shouldn’t panic if your child does take a blow to the head. Experts agree that concussion care is evolving—and improving. With early recognition, thoughtful care and a customized step-by-step plan that maps out their gradual return to full activities, most children recover fully from concussions with no long-term effects. l
ACCORDING TO THE CENTERS FOR DISEASE CONTROL AND PREVENTION (CDC), THESE ARE THE TOP 10 SPORTS WITH THE HIGHEST RATES OF CONCUSSION AMONG YOUNG ATHLETES:
• 63% of concussions in high school football are due to tackling.
• I n sports like soccer and basketball, girls are more likely to suffer sports-related concussions than boys.
• 51% of concussions in girls’ basketball are due to collisions with another athlete.

No matter what age recognizing the signs and symptoms and responding can save a life!
if you think you are having a heart attack. DON’T DELAY CALL 911
Chest pressure, squeezing, aching, or burning
Pain that travels down one or both arms
Sudden dizziness
Excessive fatigue or weakness
Anxiety
Cold sweat
Discomfort in back, neck, shoulder, or jaw
Shortness of breath
Nausea or vomiting


Aby Jennifer Hyland, RD, CSP, LD ©
S A PARENT, chances are you’ve asked yourself (more than once): Is my kid eating enough? Are they actually getting the nutrients they need? Growing like they should? These are totally normal questions—especially if you’re dealing with a picky eater. Between the mealtime standoffs and the avalanche of advice online, it’s no wonder it can all start to feel like a lot
But don’t worry—you’re not alone. This guide answers the top questions parents have about feeding their kids and offers practical tips to help raise healthy, happy eaters.
Knowing whether your child is consuming enough food is about more than just counting calories. It’s about ensuring they’re getting the right balance of nutrients that will support their growth and development. Here are a few practical ways to evaluate whether your child is eating enough:
l Appetite and meal patterns: A well-nourished child can typically go a few hours between meals without constant hunger. If your kiddo is asking for snacks all the time or seems extra hungry late at night, they might not be eating enough during the day. Aim for meals and snacks every three hours or so.
l Bowel movements: Not-so-fun but super telling. If your child isn’t urinating regularly or is constipated, it could signal a lack of fluids, fiber or food in general.
l Physical signs: Watch for ongoing fatigue, lightheadedness, thinning hair, brittle nails or bruising. These might indicate a nutrient deficiency or low overall calorie intake. If you’re concerned, talk to your pediatrician.
What should be on a preschooler’s plate?
Keep it simple and colorful. Each meal should include at least three different food groups—ideally:
l Protein: Serve up chicken, eggs, beans, tofu or other protein faves.
l Carbohydrates: Whole grain bread and crackers, pasta and potatoes, for example.
l Fruits and vegetables: Have fun with trying new produce!
l A dairy or calcium-rich food: Milk, yogurt and cheese are go-tos.
Don’t forget healthy fats. Kids need fats for brain development and fullness. Add olive oil, avocado, nut butters or full-fat dairy into meals when you can.
How many snacks should I offer throughout the day?
Aim for two snacks—one between breakfast and lunch, and one between lunch and dinner.
l Choose snacks with protein and fiber (like fruit with cheese, hummus and veggies or whole grain crackers with nut butter) to keep your child fuller longer.
l If your child is always asking for snacks, it could be a sign they’re not getting enough at mealtime. Look at their plate and check for a balance of protein, carbs, fat and fiber.
What should I do if my child refuses to finish their meal?
Resist the urge to pressure them. Studies suggest that focusing attention on eating a certain amount of food may promote overeating and result in a lower sensitivity to the amount of calories consumed. In other words, encouraging children to eat more may teach them to overeat.
Instead, let your child have a say in what they eat by offering them a choice, which helps them have a sense of control. Opportunities to make food decisions help build your child’s autonomy and independence, which may result in better cooperation around food and eating. Try asking, “Would you like carrots or cucumbers?” or “Do you want yogurt or cheese with your snack?” This gives your child some control without overwhelming them.
Determining the right portion size for your child doesn’t have to be a guessing game, and there's no single answer. The key is balance, not perfection. That said, here are a few tips:

l General guidelines: To put together a balanced meal, fill about a quarter of the plate with protein, a quarter with whole grains and the remaining half with fruits and vegetables. This gives a good starting point for meal planning.
l Let your child guide the way: Instead of focusing on exact portion sizes, allow your child’s hunger cues to guide how much they eat. Children are good at listening to their bodies, so let them decide when they’re full.
l Use age-based recommendations: Websites like choosemyplate.gov offer portion size recommendations based on your child’s age. But remember, these are just guidelines—your child’s appetite and needs may vary. You can meet with a registered dietitian for specific recommendations for your child.
How much should my child be drinking?
Hydration often flies under the radar, but it’s just as important as food. Hydration needs vary by age, activity level and climate, but use this advice as a guide.
l Water: Kids ages 2 to 5 should drink one to five cups of water a day, depending on activity and weather. Offer water with and between meals.
l Milk: Two to three cups per day is a good target. Choose
whole or 2% milk unless your pediatrician says otherwise.
l Limit sugary drinks: Juice and sweetened beverages can displace essential fluids and nutrients (and overconsumption can increase the risk of weight gain, type 2 diabetes and more). Stick to water and milk most of the time.
How can I get my kid to eat more fruits and veggies?
It’s no surprise that many kids fall short here. According to the Centers for Disease Control and Prevention, about 50% of kids ages 1 to 5 don’t eat a daily vegetable. Try these five strategies to turn things around:
1 Offer a variety: It is important to expose kids to a variety of foods starting in infancy (when developmentally appropriate at 6 months). There is no literature to support that starting with vegetables will make them less picky. But there is evidence that continued exposure to foods, even if the kids don’t appear to like them, helps develop a more long-term, positive relationship with eating all different flavors and types of foods.
2 Serve pr oduce with each meal: It sounds obvious, but kids can’t learn to like something if they aren’t exposed to it. Try
putting a fruit and a vegetable on the plate every single meal. Your tot may not eat it, and that’s okay. Just continue to offer veggie and fruit choices. And serve them in various ways: with different seasonings and dips, say, or use different cooking methods, like air fried or grilled. It can take multiple exposures sometimes for kids to learn to like a food.
3 S tart with small portions: Especially for younger kids, trying new foods can be overwhelming. If the family is eating broccoli, put one piece on your child’s plate. Then they can have more if they want it. But this is much more manageable than walking up to the table and seeing a large portion of a potentially scary new food.
4 M odel healthy eating: Positive role modeling is hugely important in getting kids to eat. If you aren’t eating the foods yourself, you can't expect your child to chow down on them. Even if you're picky and dislike certain vegetables, say, you should try to put on a good show and set an example of what healthy eating looks like for your children.
5 Mak e it fun: To make eating produce enjoyable for the whole family, have a blind taste test with your children and try a new-to-you fruit or veg. Or take your child to the grocery store or farmer’s market and let them pick out fruits and vegetables themselves. Reminder: You can be honest if you haven’t “learned to like” something yet.
How can I stop the daily food fights?
Picky eating, power struggles, food refusal—we get it. Here’s how to bring peace to the dinner table:
l Offer structure, not pressure: Stick to regular meals and snacks, but let your child decide how much to eat.
l Let your tot join in: Use cookie cutters to make silly shapes out of sandwiches or cheese slices together, or involve your child in preparing meals. The more they’re engaged in making the meal, the more likely they are to enjoy it.
l Use positive reinforcement: Make a point to acknowledge the small victories—like when your child tries a new veggie or drinks a full glass of water. A little celebration goes a long way in encouraging healthy habits! l

First and foremost, know that you’re not alone. These seven resources can provide the support and guidance you need to help your child through their challenges.
by Annika Urban ©

IN AN IDEA WORLD , mental health would be a fundamental part of every child’s health care. But in reality, far too many children miss out on this crucial component—even as mental health challenges among America’s youth continue to grow.
Today, an estimated one in five children in the U.S.—or 20%—experience a mental health disorder. These often include anxiety, depression, ADHD and behavioral challenges, says Kimberly Hoagwood, professor emeritus in the department of child and adolescent psychiatry at the New York University Grossman School of Medicine and NYU Langone’s Hassenfeld Children’s Hospital.
As children transition into young adulthood, the numbers don’t improve. Among individuals ages 18 to 25, one in three report struggling with a mental health condition. “These numbers have gone up, despite all that we know,” Hoagwood says. Suicide, now the third leading cause of death among young people ages 15 to 24, remains a pressing concern.
While these statistics can be overwhelming, Hoagwood and other experts emphasize that help is available—and you don’t have to face it alone. Here are seven resources to get you started.
When in doubt, start with your child’s primary care physician or pediatrician. Research shows that 81% of parents who are concerned about their child’s mental health have turned to their pediatrician for advice. “It is their business to understand the mental health liability of

Always take your child to the ER or contact 911 or 988 in urgent situations or if you believe they are at risk of harming themselves or others.
a child. And they can channel you into the other places where care can be acquired,” says Dr. John Constantino, a board-certified child and adolescent psychiatrist, as well as the chief of Behavioral and Mental Health at Children’s Healthcare of Atlanta. If you don’t have an appointment lined up and your child isn’t in crisis, you may be able to reach out through your health portal. Need more immediate help? Call your pediatrician’s office, explain your child’s situation and ask for advice.
Many schools offer resources for students struggling with mental health challenges. While school counselors and resource of-

ficers aren’t licensed mental health professionals, they are often well-connected to specialists, support groups and other valuable resources.
“Ask your school counselor, nurse or your teacher for guidance,” says Dr. James Norcross, a professor of psychiatry, chief of both the Texas Child Mental Health Consortium Programs and the Division of Child and Adolescent Psychiatry at UT Southwestern Medical Center and division director of psychiatry at Children’s Health in Dallas. They can also connect your child to in-school resources like yoga, mindfulness clubs and extracurricular activities that can benefit mental health.
If your child has trouble accessing in-person care, telemedicine is a valuable alternative. Virtual mental health services can be affordable or even free, depending on your insurance and provider.
One example is the Texas Child Health Access Through Telemedicine (TCHATT)
program, which provides free telemedicine services to students. “The program allows us to provide care through virtual means to schools, and the referrals come from the schools themselves,” says Norcross. For many children, the comfort of receiving care at home, rather than in an office, can be a welcome option.
With all of these great resources, don’t forget the power of recommendations and advice from trusted friends and family. Dr. Ron-Li Liaw, mental health in-chief and chair of the Pediatric Mental Health Institute at Children’s Hospital Colorado, calls this “crowdsourcing.”
From conversations with neighbors to Facebook groups, you’ll find recommendations for resources and professionals. It’s important to do your homework, though. Especially when considering recommendations from social media, Liaw emphasized the importance of double checking them against “other national resources that have been vetted for quality.”
Many online platforms can provide valuable information and connect you with local professionals. For example, the National Alliance on Mental Illness (NAMI), Mental Health America and Active Minds offer educational resources, symptom checklists and ways to locate providers. These platforms can also connect parents with support groups and offer webinars, podcasts and videos to help guide you.
For non-urgent but still critical situations, the 988 mental health crisis helpline is available 24/7. You can call or text for immediate support, and trained professionals will help you navigate the situation and provide resources. It’s also an option for teens who may feel more comfortable texting than speaking on the phone.
However, keep in mind that the 988 helpline cannot prescribe medications or provide long-term therapy. It’s an immediate support resource to help connect you to the right ongoing care.
Just like you’d go to the ER for a broken bone or another injury, your local children’s or general hospital is the place to go if your child is experiencing a mental health crisis.
Local children’s hospitals are equipped to handle mental health crises and can provide immediate care and referrals. “Go to the emergency room if it’s a crisis, even if it’s after hours,” says Norcross. Emergency rooms can assess your child’s condition, offer stabilization and refer you to the appropriate specialists. l

U.S. News evaluated 84 hospitals for their care of children and teens in mental and behavioral health conditions such as autism, anxiety, depression, eating disorders, ADHD, gender dysphoria, bipolar, schizophrenia, language and learning disorders and substance abuse and addiction. To learn more, go to http://www.usnews.com/ kids-behavioral-health.
Hospital Data Insights is an analytics platform from U.S. News & World Report based on the data underpinning the Best Hospitals rankings.
Why Hospital Data Insights?
Transform Insights Into Action
•Explore elements to help improve patient care
•Promote brand awareness
• Inform resource allocation
•Discover performance drivers
For more information or to request a free customized demo of your data, get in touch.
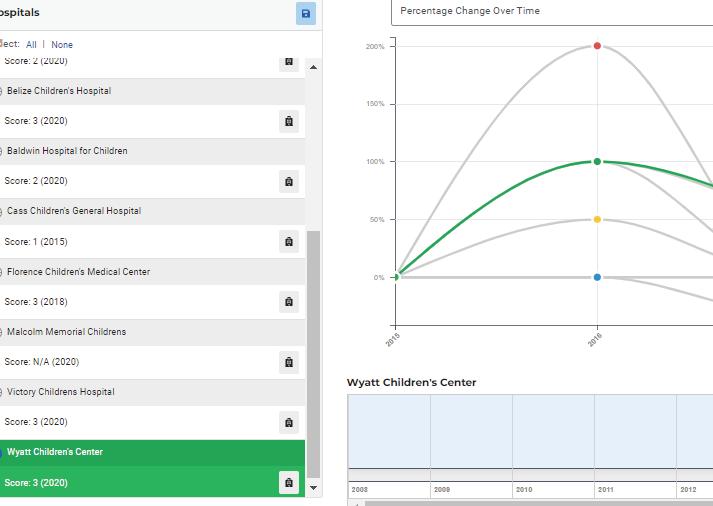
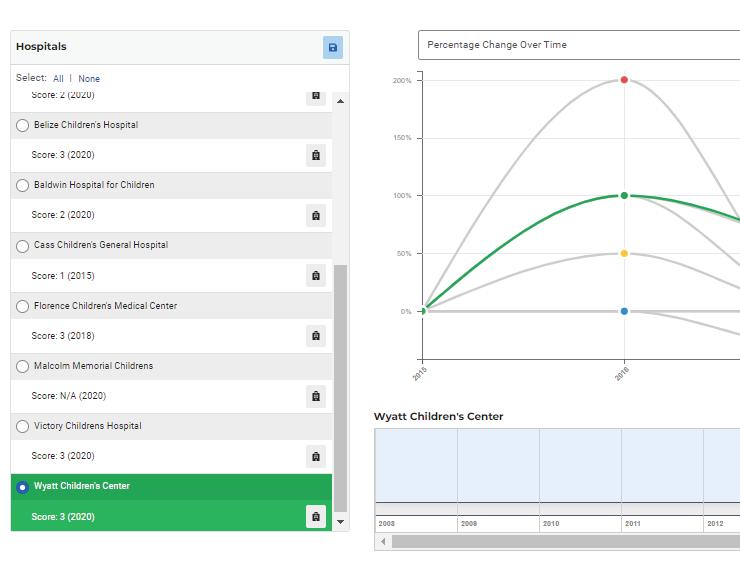
custom visualizations
This elite list showcases hospitals with unusual breadth of excellence in pediatric specialty care. For each specialty, each hospital that ranked among the top 50 earned points toward the Honor Roll: 25 points for ranking No. 1, 24 points for No. 2 and so on; hospitals ranked among the top 50 but not in the top 20 received 5 points. The 10 hospitals with the most points define the Honor Roll.
Boston Children's Hospital
Children's Hospital Colorado, Aurora
Children's Hospital Los Angeles
Children's Hospital of Philadelphia
Children's National Hospital, Washington, D.C.
Cincinnati Children's, Cincinnati
Nationwide Children's Hospital, Columbus, Ohio
Rady Children's Hospital, San Diego
Seattle Children's Hospital
Texas Children's Hospital, Houston
2025-26










How we identified 89 outstanding children’s hospitals
by Ben Harder ©
HERE SHOULD anxious parents take a newborn with a life-threatening heart defect, or find ongoing care for a child with failing kidneys or lung-clogging cystic fibrosis? A local hospital’s pediatric department might be perfectly capable of managing ear infections, allergies, flu and other common childhood ailments. But it may not have the expertise to treat severely ill kids. That’s where children’s hospitals come in. There are approximately 200 hospitals in the country that either exclusively treat pediatric patients or possess a
Wpediatric department that functions like a self-contained children’s hospital. Even within that group, some centers are better than others. U.S. News created the Best Children’s Hospitals rankings to help parents, in consultation with their doctors, find those best suited to their child.
The 2025-2026 rankings highlight top children’s centers in 11 specialties: behavioral health, cancer, cardiology and heart surgery, diabetes and endocrinology, gastroenterology and gastrointestinal surgery, neonatology, nephrology, neurology and neurosurgery, orthopedics, pulmonology and lung surgery and urology. This year, 89 hospitals ranked in at least

summary measures appear in the ranking tables on the following pages; more can be found at health.usnews. com/childrenshospitals, which also features data on dozens of additional children’s hospitals.
Almost all of the medical data used in these rankings were obtained by asking hospitals to complete a lengthy online data-collection process. This year, 108 hospitals surveyed by U.S. News provided enough data to be evaluated.
RTI International, a North Carolina-based research firm, oversaw data collection and produced the rankings. Collaborating with RTI staff, scores of pediatric experts serving in working groups helped design the data-collection survey.
Whether and how high an institution was ranked depended on three elements: its clinical outcomes (such as survival and surgical complications), its delivery of care (such as adhering to safe and effective practices) and its resources (such as staffing and technology). Each element contributed onethird of a hospital’s overall score in most specialties. A detailed FAQ about the rankings is available at health.usnews. com/aboutchildrens. Here are the basics:
one specialty, and 10 were named to the Honor Roll for scoring near the top in most or all specialties. Regional rankings for each of seven multi-state regions (Page 198) list hospitals according to the number of specialties in which they were among the best. Judging the excellence of children’s hospitals is challenging, and no single metric or ranking should be viewed as a definitive guide. U.S. News gathered hundreds of data points on each hospital to determine its strengths and weaknesses. Many
Clinical Outcomes These reveal a hospital’s success at keeping kids alive after their treatment, protecting them from infections and complications and improving their quality of life. While tough to measure, outcomes tend to matter most to both families and doctors.
Delivery of Care How well a hospital handles day-to-day care was determined in part by compliance with accepted “best practices,” such as performing neuropsychological evaluation of patients with certain cancers. Another factor: U.S. News surveyed pediatric specialists, asking them to identify up to 10 hospitals they consider best in their area of expertise for kids with complex medical problems.
Resources Surgical volume, nursepatient ratio, clinics and programs for conditions such as asthma and dozens of other measures were considered.
A Nurse Magnet hospital: Hospital recognized by American Nurses Credentialing Center as meeting standards for nursing excellence.
Infection prevention score, ICU: Ability to prevent central-line bloodstream infections in intensive care units.
Infection prevention score, overall: Ability to prevent infections through measures such as hand hygiene and vaccination.
No. of best practices: How well hospital adheres to recommended ways of diagnosing and treating patients, such as documenting blood sugar levels for a high percentage of outpatients (diabetes and endocrinology) and conducting hip exams with ultrasound specialists (orthopedics).
Nurse-patient ratio: Balance of fulltime registered nurses to inpatients.
Patient volume score: Relative number of patients in past year with specified disorders. % of specialists recommending hospital:
Percentage of physician specialists surveyed in 2023, 2024 and 2025 who named hospital among best for very challenging patients.
Procedure volume score: Relative number of tests and nonsurgical procedures in the past one, two or three years, such as implanting radioactive seeds in a cancerous thyroid (diabetes and endocrinology) and using an endoscope for diagnosis (gastroenterology). Surgical procedures are included in orthopedics.
Surgery volume score: Relative number of patients who had specified surgical procedures in past year.
Surgical complications prevention score:
Ability to prevent surgery-related complications and readmissions within 30 days (neurology and neurosurgery, orthopedics, urology).
U.S. News score: 0 to 100 summary of overall performance in specialty.
NA: Not applicable; the service is not provided by hospital.
NR: Indicates that data is not reported or unavailable.
Bone marrow transplant survival score:
Survival of stem cell recipients at 100 days. Five-year survival score: Survival five years after treatment for acute lymphoblastic leukemia, acute myeloid leukemia and neuroblastoma.
Palliative care score: How well program meets specified training and staffing standards for children with terminal or life-limiting conditions, and number of cancer patients referred to program.
CARDIOLOGY & HEART SURGERY
Catheter procedure volume score: Relative number of specified catheter-based procedures in past year, such as inserting stents and treating heart rhythm problems. Length of stay after surgery score: Success in minimizing how long certain congenital heart patients spend in the hospital for care related to their heart condition.
Norwood/hybrid surgery survival score: Survival at one year after the first in a series of reconstructive surgeries, evaluated over past four years.
Risk-adjusted surgical survival score: Survival in the hospital and 30 days from discharge after congenital heart surgery, adjusted for operative and patient risk, evaluated over past four years.
DIABETES & ENDOCRINOLOGY
Diabetes management score: Ability to prevent serious problems in children with Type 1 diabetes and to keep blood sugar levels in check.
Thyroid management score: Relative proportions of children treated for underactive thyroid who test normal and of infants who begin treatment by 3 weeks of age.
Liver transplant survival score: One- and three-year survival after liver transplant. Nonsurgical procedure volume score: Relative number of tests and noninvasive procedures. Selected treatments success score: Shown, for example, by high remission rates for inflammatory bowel disease and few complications from endoscopic procedures.
NEONATOLOGY
Infection prevention score, NICU: Ability to prevent central-line bloodstream infections in neonatal ICU.
Keeping breathing tube in place score: Ability to minimize inappropriate breathingtube removal in intubated infants.
Leaves NICU on breast milk score: Relative percentage of infants discharged from NICU receiving some nutrition from breast milk.
NICU temperature management score: Success in managing NICU patients’ temperature at the time of admission and postoperatively.
NEPHROLOGY
Biopsy complications prevention score: Ability to minimize complications after kidney biopsy.
Dialysis management score: Relative proportion of dialysis patients in past two years who tested normal.
Infection prevention score, dialysis: Ability to minimize dialysis-related infection.
Kidney transplant survival score: Based on patient survival and functioning kidney at one and three years.
NEUROLOGY & NEUROSURGERY
Epilepsy management score: Ability to treat children with epilepsy.
Surgical survival score: Survival at 30 days after complex surgery and procedures, such as those involving brain tumors, epilepsy and head trauma.
ORTHOPEDICS
Fracture repair score: A bility to treat complex leg and forearm fractures efficiently.
PULMONOLOGY & LUNG SURGERY
Asthma inpatient care score: Ability to minimize asthmatic children’s asthma-related deaths, length of stay and readmissions. Cystic fibrosis management score: Ability to improve lung function and nutritional status.
Lung transplant survival score: Reflects number of transplants in past two years, one-year survival and recognition by United Network for Organ Sharing.
UROLOGY
Minimally invasive volume score: Relative number of patients in past year who had specified nonsurgical procedures.
Testicular torsion care score: P romptness of emergency surgery to correct twisted spermatic cord.

Children’s Medical Center Dallas

Children’s Medical Center Dallas, part of Children’s HealthSM, is consistently named one of the best pediatric hospitals in the nation, and ranked in all eligible specialties by U.S. News & World Report. From our innovative CAR T-cell therapies to our advanced organ transplant program, we continue to make life better for children.
Learn about our nationally ranked care at childrens.com/excellence


“When I was 3, I was diagnosed with a rare kidney disease. My life saving journey with Montefiore Einstein included a kidney transplant at age 8. They saved my life and now I stand with them to bring awareness to pediatric kidney disease.”


The Children’s Hospital at Montefiore Einstein has been at the forefront of advancing treatments for kidney disease in children for over 50 years.
See Alisha’s life saving journey at montefioreeinstein.org/Alisha





2025-26
179 Great Care Near Home: Read about how U.S. News identified and ranked the top hospitals state by state.
1 81 The Rankings: See how district hospitals performed in areas of specialty care and in common procedures and conditions.
195 Caring for Whole Communities: U.S. News has recognized hospitals that care for patients from underserved communities.
198 Best Regional Children’s Hospitals: Explore a region-by-region ranking based on performance in 11 specialties.
How we identified and ranked the top hospitals state by state
by Ben Harder ©
IF YOU’RE LIKE MOST people who face hospitalization, you’d likely prefer to stay close to home. Not only is going to a local hospital more convenient, but it could help you avoid a hefty bill for out-ofnetwork care. Additionally, friends and family may be able to visit you if you go to a nearby hospital, and that support can be incredibly important during your recovery. Plus, getting follow-up care from the same medical team will be more practical if you don’t need to travel a great distance.
The U.S. News & World Report Best Regional Hospitals listings showcase about 500 hospitals in the country that offer high-quality care across a range of clinical services. These services include both complex, highly specialized care for the sickest patients—the focus of the Best Hospitals specialty rankings (see Page 100)—and safe, effective treatment for those whose medical needs are more commonplace, such as patients seeking hip or knee replacement surgery for age-related arthritis. The 2025-2026 Best Regional Hospitals rankings, found in their entirety at health.usnews.com/bestregionalhospitals, offer readers in most parts of the country a number of high-quality choices near home.
These evaluations are based on ratings of how well hospitals handle 22 relatively common procedures and conditions in addition to their performance in 11 specialties.* The 22 procedures and conditions are: colon cancer surgery; gynecological cancer surgery; lung cancer surgery; prostate cancer surgery; leukemia, lymphoma and myeloma; heart arrhythmia; heart attack; heart failure; heart
*Cancer; cardiology, heart and vascular surgery; diabetes and endocrinology; ear, nose and throat; gastroenterology and GI surgery; geriatrics; obstetrics and gynecology; neurology and neurosurgery; orthopedics; pulmonology and lung surgery; urology
bypass surgery; heart valve surgery; pacemaker implantation; transcatheter aortic valve replacement; abdominal aortic aneurysm repair; stroke; back surgery; hip replacement; knee replacement; hip fracture; diabetes; kidney failure; pneumonia; and chronic obstructive pulmonary disease. Hospitals are assigned a rating of “high performing,” “as expected” or “evaluated” in each area in which they treated enough patients to be evaluated.
Recognition as a Best Regional Hospital means a hospital earned at least eight “high performing” ratings across the procedures and conditions and met certain other criteria. To learn more, check out the FAQ at health.usnews.com/best-hospitals.
The Best Regional Hospitals appear ranked by state on the following pages. Hospitals are numerically ordered according to the following rules:
1. Hospitals on the Honor Roll (see Page 98) were ranked No. 1 in their state. In states with more than one Honor Roll hospital, all were tied at No. 1.
2. All other hospitals received two points for each of the 11 specialties in which they were ranked among the top 50 and one



point for each of those specialties and each procedure or condition in which it was rated high performing. The two heart valve procedures were treated as one procedure for scoring purposes.
3. A hospital lost one point for each procedure or condition in which it was rated “evaluated.” Again, the valve procedures were scored together.
Based on the same rules, hospitals in major metropolitan areas also were ranked against other top hospitals in the metropolis. Our website displays these rankings for 95 metro areas with approximately 500,000 or more residents.
To help consumers outside the biggest urban centers who are searching for high-
quality care, our website also lists top hospitals in more than 100 U.S. News-defined regions, such as Kentucky’s Bluegrass Region, the Ozarks in Arkansas and the Florida Panhandle.
Our goal with the state and metro area rankings is to identify general medical-surgical hospitals that provide both breadth and quality, so only hospitals that deliver a wide range of clinical services for adults were considered for the Best Regional Hospitals rankings.
Maternal and pediatric care did not factor into these rankings. Hospitals are separately evaluated in maternity care (Page 136), and children’s hospitals are separately ranked by region (Page 198) based on their performance across the 11 children’s specialties (Page 162). How a hospital performed in ophthalmology, psychiatry, rehabilitation and rheumatology did not factor into the Best Regional Hospitals rankings, either. While these four specialties are undeniably important, many hospitals treat few, if any, inpatients in these specialty areas.
Additionally, specialty hospitals such as dedicated cancer centers, surgical hospitals and rehabilitation facilities were not considered for the regional rankings.
Of course, a local hospital doesn’t make sense for every patient. Where you live, the type of care you need, your insurance coverage and other factors will all play a role in determining which type of hospital is preferable for your treatment. That’s why when choosing a hospital, it’s important to consult with your physician or other health professional and talk with family and friends about the hospitals that you’re comparing. Then you can combine your own research with ours to find the best possible care. l
To help patients identify top hospitals near home, the table below compares hospitals across 15 areas of complex specialty care that comprise the Best Hospitals rankings (Page 100) plus 22 procedures and conditions.






















NATIONALLYRANKED LEUKEMIA& LYMPHOMA*GYNECOLOGICALCANCER SURGERY COLONCANCER SURGERY LUNGCANCER SURGERY PROSTATECANCER SURGERYHEARTARRHYTHMIA HEARTATTACKHEARTFAILUREHEARTBYPASS SURGERY HEARTVALVE SURGERY TAVR† ABDOMINALAORTIC ANEURYSM PACEMAKER IMPLANTATION STROKEBACKSURGERYHIPREPLACEMENTKNEEREPLACEMENTHIPFRACTUREDIABETESKIDNEYFAILUREPNEUMONIACOPD‡


































































*Also includes myeloma. †TAVR: Transcatheter aortic valve replacement. ‡COPD: Chronic obstructive pulmonary disease.

















**MedStar Washington Hospital Center is ranked No. 2 and both MedStar Georgetown University Hospital and Johns Hopkins Medicine-Sibley Memorial Hospital are ranked No. 5 (tied) in the Washington, D.C., metro area rankings, which include hospitals in and around the District of Columbia. These three hospitals in D.C. are presented here alphabetically. A footnote indicates that another hospital’s results are included, that the hospital has a different name in one or more areas of care, or both. 6U. of Colorado Cancer Ctr.-UCHealth U. of Colorado Hosp., National Jewish Health 7Smilow Cancer Hospital at Yale New Haven 8MedStar Heart & Vascular Inst. at MedStar Washington Hosp. Ctr. 9Florida Orthopaedic Institute at Tampa General Hospital 10Baptist Health Miami Cancer Institute at Baptist Hospital, Baptist Hlth. Miami Cardiac & Vascular Inst. at Baptist Hosp., Baptist Health Miami Neuroscience Institute at Baptist Hosp., Baptist Health Orthopedic Care at
Hospital 11Sylvester Comp. Cancer Ctr.-U. of Miami Hosp. & Clinics, Desai
























































































1







































includes myeloma.















































Hackensack University Medical Center:
Top 20 nationally
#1* in NY-NJ metro area *Tied
#1 adult & children’s hospitals in NJ
The only nationally ranked cancer center in NJ at John Theurer Cancer Center
• • • • Specialties ranked among the best in the nation for clinical excellence in: Urology
• • • •
Orthopedics
Pulmonology
Diabetes & Endocrinology
Neurology

Geriatrics
Ear, Nose & Throat •
Cardiology, Heart & Vascular Surgery Cancer
Gastroenterology & GI Surgery

Jersey Shore University Medical Center: JFK Johnson Rehabilitation Institute: Top 20 in NY-NJ metro area
Pulmonology & Lung Surgery •
Geriatrics
Top 5 in NJ • • Among the nation’s best physical rehabilitation hospitals • Nationally High Performing in: Cardiology, Heart & Vascular Surgery

































































































*Also includes myeloma. †TAVR: Transcatheter aortic valve replacement. ‡COPD: Chronic obstructive pulmonary disease. A footnote indicates that another hospital’s results are included, that the hospital




or




















37Thomas Jefferson U. Hosps.Sidney Kimmel Comp. Cancer Ctr.-Jefferson Hlth., Thomas Jefferson U. Hosps.-Vickie & Jack Farber Inst. for Neuroscience-Jefferson Hlth., Rothman Orthopaedics at Thomas Jefferson U. Hosps.-Jefferson Hlth., Thomas Jefferson U. Hosps.-Jane & Leonard Korman Respiratory Inst.-Jefferson Hlth.













1



















































*Also includes myeloma. †TAVR: Transcatheter aortic valve replacement. ‡COPD: Chronic obstructive pulmonary disease. A footnote indicates that another hospital’s results are included, that the

































For the second year in a row, U.S. News has recognized hospitals that treat patients from every stratum of their communities.
by Tavia Binger and Ben Harder ©
Patients with high social needs often face significant obstacles in accessing top-quality healthcare services. At the same time, hospitals that care for a larger proportion of more vulnerable patients are faced with challenges, such as lower reimbursement from certain insurers, which can limit their ability to provide much-needed services to their communities. Yet some hospitals break the mold by demonstrating excellence in quality while also caring for numerous patients from vulnerable communities.
To recognize such hospitals, U.S. News developed a methodology defining the 2025-2026 Best Regional Hospitals for Community Access. The result is this list of 76 hospitals. Hospitals on this list were recognized for excellent performance in both quality and measures related to access to care for historically underserved communities, as described below.

At least 40% of Medicare inpatient visits involved patients living in more socioeconomically deprived neighborhoods. The socioeconomic deprivation of neighborhoods was assessed using Area Deprivation Index data obtained from the Neighborhood Atlas. Both national percentiles, which compare neighborhoods to others in the country, and state deciles, which compare neighborhoods only to others within the same state, were considered. Neighborhoods with national ADI values above 70 (on a scale where 100 indicates the greatest deprivation), or state ADI values above 7 (on a 1-to-10 scale), were classified as more socioeconomically deprived for this analysis. A hospital could meet this criterion if at least 40% of its Medicare patients lived in deprived neighborhoods, according to either state or national ADI.
A sizable Medicaid population. A hospital met this requirement if at least 30% of its patients were insured by Medicaid, or if it achieved the highest category (“Higher than other hospitals”) on a measure of representation of low-income patients, which was based on Medicaid data.
For the access component of this methodology, we identified hospitals that served a higher proportion of three historically underserved communities: people living in more socioeconomically deprived neighborhoods, Medicaid beneficiaries and racial and ethnic minorities. For the quality component, we identified hospitals that were awarded the Best Regional Hospitals recognition.
Hospitals received this recognition if they ranked among the Best Regional Hospitals (see Page 179) and met at least two of the following three criteria:
A patient population that reflects the racial and ethnic diversity of the surrounding community. A hospital met this requirement if at least 20% of its Medicare inpatients receiving elective care were from racial or ethnic minorities, or if it treated a nontrivial Medicare population from one or more of five racial/ethnic minority groups and achieved the highest category (“Comparable to or higher than the community”) for corresponding representation measure(s) published by U.S. News. l
These 76 institutions provide excellent care for underserved communities.
• AHN Forbes Hospital, Monroeville, Pa.
• Advocate Christ Medical Center, Oak Lawn, Ill.
• Advocate Trinity Hospital, Chicago,
• Albany Medical Center, Albany, N.Y.
• Asante Rogue Regional Medical Center, Medford, Ore.
• Ascension Alexian Brothers Hospital, Elk Grove Village, Ill.
• Ascension St. John Medical Center, Tulsa, Okla.
• Banner-University Medical Center Phoenix
• Banner-University Medical Center Tucson, Ariz.
• Barnes-Jewish Hospital, St. Louis
• Bronson Methodist Hospital, Kalamazoo, Mich.
• Cape Fear Valley Medical Center, Fayetteville, N.C.
• Christian Hospital, St. Louis
• Cooper University Health Care-Camden, N.J.
• Corewell Health Dearborn Hospital, Dearborn, Mich.
• CoxHealth Springfield, Mo.
• Dartmouth Hitchcock Medical Center, Lebanon, N.H.
• ECU Health Medical Center, Greenville, N.C.
• Eastern Maine Medical Center, Bangor
• Genesis Healthcare System-Zanesville, Ohio
• Grand Strand Regional Medical Center, Myrtle Beach, S.C.
• HCA Florida Kendall Hospital, Miami
• HCA Houston Healthcare Clear Lake, Webster
• Henry Ford Hospital, Detroit
• Hillcrest Medical Center, Tulsa, Okla.
• Indiana University Health Medical Center, Indianapolis
• Inova Alexandria Hospital, Alexandria, Va.
• Kaiser Permanente Fontana and Ontario Medical Centers, Fontana, Calif.
• Kaiser Permanente South Sacramento Medical Center, Sacramento, Calif.
• Kettering Health Main Campus, Kettering, Ohio
• Lexington Medical Center, West Columbia, S.C.
• Loma Linda University Medical Center, Loma Linda, Calif.
• Long Island Jewish Med. Ctr. at Northwell Health, New Hyde Park, N.Y.
• M Health Fairview University of Minnesota Medical Center, Minneapolis
• Maimonides Medical Center, Brooklyn, N.Y.
• Memorial Medical Center-Modesto, Calif.
• MemorialCare Orange Coast Medical Center, Fountain Valley, Calif.
• Mercy Hospital Fort Smith, Ark.
• Mercy San Juan Medical Center, Carmichael, Calif.
• Methodist Hospitals of Memphis, Tenn.
• MetroHealth Medical Center, Cleveland
• Montefiore Medical Center, Bronx, N.Y.
• Mount Sinai Hospital, New York
• Nebraska Medicine-Nebraska Medical Center, Omaha
• New York-Presbyterian Hospital-Columbia and Cornell
• New York-Presbyterian Queens Hospital, Flushing
• Ochsner Lafayette General Medical Center, Lafayette, La.
• OhioHealth Grant Medical Center, Columbus
• Park Nicollet Methodist Hospital, St. Louis Park
• Prisma Health Richland Hospital, Columbia, S.C.
• Sanford Medical Center Bismarck, N.D.
• Scripps Mercy Hospital, San Diego
• Sharp Chula Vista Medical Center, Chula Vista, Calif.
• South Texas Health System-Edinburg
• Southcoast Hosps.-Fall River, New Bedford & Wareham, Mass.
• St. Agnes Medical Center, Fresno, Calif.
• St. David’s North Austin Medical Center, Texas
• St. Francis Hospital-Tulsa, Okla.
• Stony Brook University Hospital, Stony Brook, N.Y.
• Stormont Vail Hospital, Topeka, Kan.
• Sutter Medical Center-Sacramento, Calif.
• Temple University Hospital, Philadelphia
• Texoma Medical Center, Denison, Texas,
• TidalHealth Peninsula Regional, Salisbury, Md.
• UC Davis Medical Center, Sacramento, Calif.
• UC Irvine Medical Center, Orange, Calif.
• UMass Memorial Medical Center, Worcester, Mass.
• UNC Hospitals, Chapel Hill, N.C.
• UPMC Presbyterian Shadyside, Pittsburgh
• University of Alabama at Birmingham Hospital, Birmingham
• University of Chicago Medical Center
• University of Iowa Health Care Medical Center, Iowa City
• University of Kentucky Albert B. Chandler Hospital, Lexington
• WakeMed Raleigh Campus, Raleigh, N.C.
• Wesley Healthcare Center, Wichita, Kan.
• Yale New Haven Hospital, New Haven, Conn.













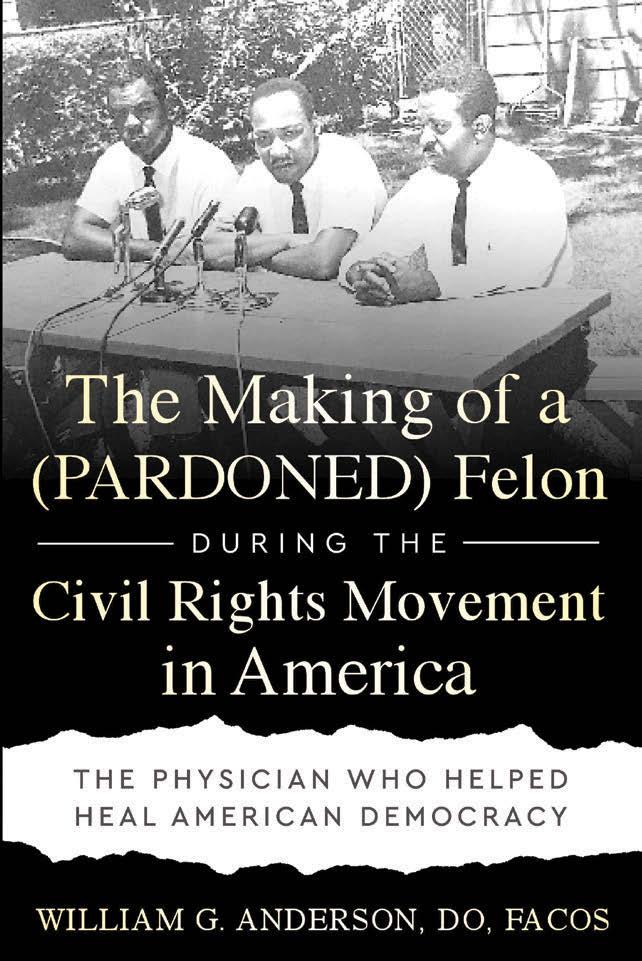
For good reasons, parents of kids who need specialty care tend to seek a hospital close to home, usually within the state where they live or in a neighboring state. Designed to help families identify top pediatric centers near home, the region-by-region rankings below compare children’s hospitals on overall performance across 11 pediatric specialties.

Yale New Haven Children’s Hospital, New Haven, Conn.
( - ) indicates hospital is not nationally ranked.
A footnote indicates that another hospital’s results are included, that the hospital has a different name in one or more areas of care, or both. 1Dana-Farber/Boston Children’s Cancer and Blood Disorders Center 2UPMC Children’s and Western Psychiatric Hospitals; UPMC Children’s Hospital of Pittsburgh-Shriners Hospitals for Children Erie 3Johns Hopkins Children’s Center-Kennedy Krieger Institute 4Virginia Congenital Cardiac Collaborative 5Rutgers Cancer Institute; RWJBarnabas Children’s Health; RWJBarnabas Children’s Health
l NATIONALLY RANKED
11 UF Health Shands Children’s Hospital, Gainesville, Fla.
Nemours Children’s Hospital-Florida, Orlando
16 Holtz Children’s Hospital at the University of Miami-Jackson Memorial Medical Center
17 AdventHealth for Children, Orlando, Fla.
6MUSC Children’s Heart Program of South Carolina 7Wolfson Children’s
Heart
Children’s and Kentucky Children’s Hospital Joint Heart Program 9Ann and Robert H. Lurie Children’s Hospital-Prentice Women’s Hospital 10Mayo Clinic-Children’s Minnesota Cardiovascular Collaborative 11St. Louis Children’s HospitalWashington University/Shriners Children’s St. Louis 12Cincinnati Children’s and Kentucky Children’s Hospital Joint Heart Program; Kentucky Children’s Hospital-Shriners Hospitals for Children 13M Health Fairview Masonic Children’s Hospital-Children’s Minnesota 14Advocate Children’s Heart Institute 15Intermountain Primary Children’s HospitalShriners Hospitals for Children-University of Utah
1 Texas Children’s Hospital, Houston
2 Children’s Medical Center Dallas16
3 Dell Children’s Medical Center, Austin, Texas
4 Cook Children’s Medical Center, Fort Worth, Texas
4 Phoenix Children’s Hospital
6 Children’s Memorial Hermann Hospital, Houston17
7 Oklahoma Children’s Hospital OU Health, Oklahoma City
4 Lucile Packard
9 Loma Linda University Children’s Hospital, Loma Linda, Calif.
( - ) indicates hospital is not nationally ranked.
A footnote indicates that another hospital’s results are included, that the hospital has a different name in one or more areas of care, or both.
16Children’s Medical Center Dallas-Scottish Rite for Children 17Children’s Memorial Hermann Hospital/Dunn Behavioral Science Center at UTHealth Houston
18UCLA Mattel Children’s & CHOC Joint Heart Program 19UC Davis Children’s Hospital/Shriners Children’s Northern California