Pathways to Impact
Transforming complex data into powerful outcomes

Department of Medicine
Chair’s Report 2025




Department of Medicine
Chair’s Report 2025


“Pathways to Impact” captures the idea of taking bold steps to measure and expand the true reach of our faculty’s work, whether in patient care, research, education, or community engagement. By harnessing the power of big data and advanced analytics, we are gaining deeper insights into outcomes, quality of care, and effectiveness. We are no longer just participating in progress; we are actively shaping what medical excellence looks like in a data-driven, modern world.
This year, the Department of Medicine has embraced this charge with remarkable ambition. We’ll explore how large-scale data analysis is accelerating medical breakthroughs, as well as how genomics and artificial intelligence are delivering truly personalized care. We are also reimagining how data science is integrated into medical education, ensuring the next generation of physicians and researchers is equipped to lead in an era defined by information and insight. These efforts, spanning research, patient care, and training, demonstrate how our faculty are not only advancing medicine, but also redefining its very foundation.

As you explore this year’s annual report, you will see how our work, rooted in compassion, driven by evidence, and powered by innovation, is touching lives far beyond the clinic walls. Together, we are not only advancing medicine but redefining what it means to make an impact and heal the sick and keep them healthy.

Roy E. Weiss, MD, PhD Chief Medical Officer Ambulatory Services- UHealth
Rabbi Morris I. Esformes Endowed Chair in Medicine and Endocrinology
Kathleen & Stanley Glaser Distinguished Chair
Professor | Chairman
Department of Medicine
University of Miami Miller School of Medicine


Dr. Chung
How big data is transforming real-world medicine and who it reaches
Cecilia P. Chung, M.D., M.P.H., doesn’t just see patients. She sees patterns.
As a physician-scientist trained in rheumatology, pharmacogenomics, and pharmacoepidemiology, Dr. Chung, who is also Chief of the Division of Rheumatology and Immunology in the Department of Medicine, has harnessed the scale and scope of big data to uncover unexpected risks, refine treatments, and reach patients often excluded from conventional medical research. In her hands, numbers become insight, patterns become prevention, and research becomes care.
“Traditional randomized clinical trials are considered the gold standard, but one of their limitations is the strict inclusion and exclusion criteria,” she explains. “That means many of the patients I see in clinic might not even qualify for those trials. Big data allows us to study broader, more diverse populations, giving us results that are more generalizable.”
Dr. Chung began asking hard questions early in her career: Why do some people develop disease while others don’t? And, for those who do, why do some respond to treatment while others experience debilitating side effects? These questions still guide her work. Now, with data from electronic health records, biobanks, and population-scale claims databases at her fingertips, she’s finding answers.
Dr. Chung, left, recipient of the 2022 Henry Kunkel Early Career Investigator Award and the 2022 Leon I. Goldberg Early Investigator Award, consults with a colleague.


One of the greatest advantages of using large-scale data, Dr. Chung notes, is the ability to conduct realworld research. Where randomized clinical trials offer control, big data offers breadth. This data-informed approach can reveal how certain medications perform across age, gender, race, and certain underlying conditions, critical information clinical trials often can’t provide.
“With large datasets, we can detect differences or patterns that smaller studies might miss. It gives us the ability to study thousands of patients in a relatively short time, which can be especially valuable when evaluating drug safety or treatment effectiveness or certain patient populations,” she says.
In a study that analyzed TennCare data, Tennessee’s Medicaid program, for example, Dr. Chung and her team found that 15 percent of children under 18 had received opioid prescriptions in a given year, and in some cases even toddlers. “It was eye-opening,” she recalls. “We were seeing opioid use in children as young as two to five years old for relatively minor conditions such as dental work or minor trauma, conditions where opioids might not be medically necessary.”
That’s not the kind of finding you’d get from a clinical trial alone. It took Medicaid claims data, a broad perspective, and the willingness to ask hard questions.
For another project, Dr. Chung leveraged a large-scale biorepository that links de-identified electronic health records with genomic data. Using this resource, she and her research team studied immunosuppressant drugs, which are prescribed for autoimmune and rheumatologic conditions, cancer, kidney disease, and to prevent rejection in transplant patients. These drugs have a narrow therapeutic index –meaning the effective dose is close to the dose that can cause harmful side effects – and because they suppress the immune system, they increase the risk of infection. As a result, they require close monitoring and careful dosing.
With National Institutes of Health (NIH) funding, Dr. Chung’s team studied an immunosuppressant drug called azathioprine to identify both genetic and non-genetic factors linked to its side effects and toxicity. Initially, they noticed that people of different races were discontinuing the drug at different rates due to leukopenia, a drop in white blood cell counts. (White blood cells are a key part of the immune system,
helping the body fight infections.)
But a closer look revealed that race wasn’t the cause; the real driver was a specific genotype (a genetic trait). This genotype strongly affected white blood cell counts and led clinicians to discontinue the medication.
“The genotype was leading clinicians to stop treatment, but what we found suggests we might be undertreating some patients,” says Dr. Chung. “We’re now asking, through more extensive research, whether we should adjust the dose instead of stopping the drug entirely.”
Big data is also useful for studying how drugs interact. In everyday settings, people often take more than one medication at a time. Dr. Chung and her team examined combinations like the muscle relaxant tizanidine and the antibiotic ciprofloxacin and identified significant risks such as dangerous drops in blood pressure. In another study, they explored how differences in genes’ encoding enzymes like CYP2D6 (which helps the body break down drugs like antidepressants and heart medications) can affect how people respond to medications like codeine.
Today, as artificial intelligence (AI) helps physician-scientists sift through
“We’re in an exciting time with unprecedented opportunities,” Dr. Chung says. “It’s not a question of if, but how wisely we’ll use the data.”
massive datasets, Dr. Chung envisions a future where pharmacogenomics, the study of how a person’s genes affect their response to medications, moves from promise to practice.
“There are opportunities to bring together massive, complex datasets to better understand things like susceptibility, who is more likely to develop a condition, as well as the likelihood of a response to certain drugs. That’s why I find the pharmacogenomics aspect of research so interesting – because it’s actionable,” she adds.
Dr. Chung’s work goes far beyond the lab – it involves studying diverse patient populations in real-world settings. She also conducts research at the Miami VA Healthcare System (VA), where one of her projects assesses the safety of non-opioid treatment options for patients at high risk for heart problems.
Her drive and determination began at a young age. “People tell me I started saying I wanted to be a doctor as young as three,” she says. “And I never changed my mind.”
Born in Peru, Dr. Chung first trained as a rheumatologist at the National University of San Marcos in Lima before research opportunities led her to Canada and eventually to Vanderbilt University. At Vanderbilt, she earned a Master of Public Health and began working with large health databases linked to programs like Medicare and TennCare. Her early projects, which focused on opioid prescription patterns, hypertension, and lupus, sparked a lasting interest in population-level drug safety and why people respond differently to treatments.
Dr. Chung also mentors medical students and junior faculty. And through it all, she continues to ask big, foundational questions. Since joining the department in January 2023, she has focused on creating opportunities for students to explore academic rheumatology and research. For example, an undergraduate student spent a month with Dr. Chung and her team working on a small research project. The student later presented her work at the Florida Society of Rheumatology and connected with a senior investigator at the NIH. “The
student recently joined a training program at the NIH and now plans to become a physician-scientist,” Dr. Chung adds.
This is exactly the kind of path she hopes to support and encourage.
“Not everyone will follow this path, but it’s important to give students the chance to explore it,” Dr. Chung says. Currently, she’s mentoring two medical students and two rheumatology fellows who are learning to use real-world data to develop and answer research questions, with support from her team’s programmer. She also helps students identify the right training and opportunities to advance their goals.
Looking ahead, what excites her most is a future where genetic data is part of every patient’s record, AI spots risks before harm occurs, and care is truly personalized.
“We’re in an exciting time with unprecedented opportunities,” Dr. Chung says. “It’s not a question of if, but how wisely we’ll use the data.”
She’s committed to shaping that future, advancing it one dataset and one discovery at a time.



Dr. Imm

In the ever-evolving world of medicine, the intersection of data and education is reshaping how the next generation of physicians is trained. At the Department of Medicine, an exciting transformation is underway, one that harnesses vast amounts of data to personalize, refine, and elevate medical education like never before. This shift toward “precision education” not only enhances student success but also equips future doctors with the nuanced skills required to navigate a rapidly changing healthcare landscape.
“The fact that we’re using data – large amounts of it – to validate how we assess students is a big deal,” says Matthew Imm, M.D., Assistant Professor of Clinical Medicine, Director of Assessment and Entrustment, and Director of the Practice of Medicine Clerkship and a leader in this educational transformation.
The Miller School of Medicine’s journey toward data-driven medical education began with a realization: critical information about student learning was scattered across fragmented systems.
“For a long time, all the different pieces of information that tell us how students learn – who’s likely to succeed, what types of assessments differentiate high and low performers – were in very disparate places,” says Dr. Imm. “To use this information to develop any meaningful insights was really tough.”
Launched in August 2020, NextGenMD is an innovative, integrated training curriculum that combines early clinical exposure, case-based small-group learning, and strong longitudinal mentorship to prepare well-rounded physicians for today’s rapidly evolving medical landscape. It was developed by a task force of faculty, students, and

residents who analyzed national trends in medical education.
The curriculum is designed with flexibility in mind. The first phase resembles a traditional college experience, with large lectures complemented by interactive learning and small-group sessions, all within a structured classroom setting that includes exams and assessments. The second phase, meanwhile, shifts to a more personal, hands-on approach. Students rotate through medical specialties, actively participating in patient care. Their progress is assessed through both written exams and clinical performance evaluations.
“We’ve seen that students who struggle during the first phase often continue to struggle with those highstakes assessments later on. That’s why it’s important to identify issues early and help students develop stronger strategies from the start,” says Dr. Imm.
One key strategy has been to
leverage data analysis to enhance medical education. This data-driven approach is highly interdisciplinary, bringing together experts in health informatics, statistics, learning science, clinical education, and administrative leadership. These teams work collaboratively to design and refine systems that support students and ensure that data is used effectively.
When the school began transitioning to this innovative curriculum, it also launched a parallel effort to modernize its data infrastructure, moving from rudimentary, often paper-based systems to a unified digital platform capable of capturing and analyzing large volumes of educational data.
This transformation was more than just a technical upgrade; it represented a major cultural and operational shift.
“When I first started as a clerkship director about eight years ago, we
This chart tracks students’ academic performance over
Consistent
were literally migrating everything from paper to digital systems. Grades, evaluations, it was all in a physical format,” Dr. Imm recalls.
Today, the University has a centralized database that consolidates admissions data, academic records, learning management systems, registrar info, and enrollment statistics into a unified “data lake.” This integration enables coaches, teachers, mentors, and administrators to ask meaningful questions: Are students progressing? Is the curriculum effective?
One of the department’s key tools is the Learning Analytics Dashboard, which connects to an e-portfolio that tracks student performance over time. Launched together with the NextGenMD curriculum five years ago, it offers real-time insights into individual and class progress and helps to ensure assessments are appropriately challenging.
“It lets us see how students are doing and whether our assessments are too easy or too hard in real time by tracking average score changes between exams,” says Dr. Imm. “Having immediate access to performance data allows us to quickly adjust the curriculum or teaching methods and identify struggling students early, before problems get worse.”
Early intervention, in fact, is key to the new approach.
“We’re committed to providing the right support from the start,” explains Dr. Imm. “We don’t want to wait until a student is failing before intervening. By then, their motivation has probably
taken a hit,” says Dr. Imm. “Instead, we want to spot unproductive patterns early like study habits, behavior, or other issues, and intervene proactively.”
Personalized mentorship is a cornerstone of the curriculum, which is reflected in the role of lead clinical educators (LCEs). Each student is assigned a dedicated LCE who mentors them throughout medical school and into residency.
This type of mentorship relies heavily on data-driven insight. LCEs have visibility into student trajectories, who’s excelling, who’s plateauing, and who’s falling off, allowing timely conversations and tailored learning plans. This visibility extends beyond academics to clinical skills, tracked across multiple checkpoints including standardized patient exams. The e-portfolio visualizes this growth, giving mentors and students a clear picture of development over time.
“By viewing that data alongside academic performance, we can start to build a more holistic, 360-degree picture of each student,” says Dr. Imm. “That’s the direction we’re headed in, the ability to use integrated data not just for evaluation, but for meaningful mentorship and support.”
But it’s not just students who benefit from data; the curriculum is also reviewed closely. Medical education is complex, and without a clear structure of objectives and assessments, gaps and redundancies can emerge. To address this, the department used its Learning Management System to map each curricular objective to the institution’s learning goals. This revealed strengths and weaknesses in content coverage, leading to targeted, datadriven improvements. The next step is linking those objectives to assessments and competencies, creating a detailed performance record.
“This will eventually allow us to create a comprehensive ‘report card’ for each student, not just showing the classes they took, but tracking their
This chart shows a student’s performance across clinical skills and reasoning tasks compared to their peers. Aggregated ePortfolio data from Phases 1–3 reveal evolving strengths and weaknesses, supporting targeted coaching and early intervention.
“By viewing that data alongside academic performance, we can start to build a more holistic, 360-degree picture of each student,” says Dr. Imm.
mastery of individual competencies over time,” Dr. Imm explains.
Looking ahead, the goal is to get even more specific, not just identifying that a student is struggling, but understanding exactly where and why.
“Right now, we can say, ‘This clinical skill needs work,’ or ‘You’re underperforming in this specific area,’” Dr. Imm explains. “But in the future, we want to go even deeper – like identifying whether a student consistently struggles with a certain type of multiple-choice question or if their diagnostic reasoning falls behind their management skills.”
Dr. Imm envisions using artificial intelligence (AI) to develop personalized dashboards that students can access independently. These systems could recommend specific resources and study materials based on each student’s individual learning
gaps. “That’s the vision we’re working toward, a more dynamic, responsive support system,” he adds.
The University plans to actively pursue the integration of AI to harness its potential to enhance personalized learning. This type of initiative reflects a growing national shift toward precision education, an approach similar to precision medicine. Many leading academic medical institutions are already at the forefront of this trend, integrating electronic medical records (EMRs) with learning platforms to track and analyze students’ clinical exposure and performance in real time.
“The future of AI in medical education is to use increasing amounts of data to uncover insights into students’ clinical exposure, decisionmaking, and competencies. It’s about providing personalized, meaningful feedback,” says Dr. Imm. “We’re not there yet, but it’s a direction we’re excited to move in.”

WArchitectural rendering of the UHealth Tower renovation, scheduled for completion in 2026.
“When I first became Chief Medical Officer in 2014, we didn’t have a developed medical staff office or formal processes around quality and safety,” recalls Dr. Ferreira, who is CMO of Inpatient and Acute Care Services at the University of Miami Health System. “Those first few years were spent building those processes so we could function as a true academic medical center.”
At the time, her office was little more than a skeleton crew: herself, an administrative assistant, and one staff member overseeing medical staff and quality. Eleven years later, that small office has grown into a fully structured department of more than 40 professionals, all dedicated to integrating quality, safety, efficiency, and patient experience into every aspect of care.
The early years were focused on putting the right systems in place. Before standardized processes were implemented, differences in individual practice styles led to inconsistent outcomes and opportunities for improvement in patient care and experience. So Dr. Ferreira and


hen Tanira B. Ferreira, M.D., Associate Professor of Clinical Medicine, joined the University of Miami Miller School of Medicine in 2009, she found herself at an institution full of promise but lacking the robust infrastructure to effectively deliver on its academic mission.
her small team began laying the groundwork for a new system, rooted in five guiding principles that became the framework for lasting change:
Quality: All care must be evidence-based.
Safety: No patient should suffer preventable harm, such as falls, pressure ulcers, or central line infections.
Efficiency: Patients should not remain in the hospital longer than medically necessary.
Patient Experience: Patients want answers delivered clearly and consistently.
Readmissions: Patients should leave healthier, without having to return to the hospital unnecessarily.
The turning point came in 2017, when three separate entities – Bascom Palmer, Sylvester/ UMHC, and UHealth Tower – were unified under a single hospital license. Just as pivotal, the Epic electronic health record (EHR) platform was rolled out across the entire system. Prior to that, records were scattered and hard to use.
“As a pulmonary critical care physician,
“We’ve built something special; a framework that links quality, safety, efficiency, and patient experience to education, research, and clinical service,” Dr. Ferreira explains.
I’d be rounding in the intensive care unit (ICU) with three computers open: Meditech for inpatient data, Epic for emergency department (ED) and ambulatory records, PACS for imaging, plus a paper chart,” recalls Dr. Ferreira. “It was not an efficient process.”
The shift was transformative: a unified license, a single patient record system, and new hospital bylaws that required community providers to join the faculty and follow academic standards. Those who chose not to align with the new standards transitioned out of the system.
“The result was accountability,” notes Dr. Ferreira. “Care quality became consistent. Mortality rates fell. Patient experience improved. For the first time, we had a solid structure to build upon.”
With the infrastructure in place, the team turned its attention to data. By partnering with Vizient, a U.S.-based company that helps hospitals and medical centers improve quality, safety, efficiency, and cost-effectiveness, the hospital gained access to national benchmarking and quality outcomes. But Dr. Ferreira knew raw numbers alone would not be enough. It required strong physician partnership with the multiple service lines to obtain meaningful data to their specialty, so progress could be tracked.
“You can’t just give providers raw data,” she explains. “It must be

validated, meaningful, actionable, and developed with physicians at the table.”
Her team created a balanced scorecard to track mortality, readmissions, efficiency, and overall patient experience. Data moved seamlessly from frontline providers to the board, creating a single, reliable source of truth for accountability.
One clear example of that accountability came from the operating rooms. In the past, surgeons began cases at varying times, and room turnover often stretched over an hour. By standardizing start times at 7:30 a.m. and reducing turnover to 35 minutes, efficiency improved dramatically.
“Now we’re applying the same approach to cath labs, bronchoscopy, gastrointestinal, and interventional radiology suites,” she said. “It has increased capacity, improved patient flow, and strengthened accountability.”
Month by month, these scorecards reveal both progress and setbacks. January, for example, is notoriously difficult: the hospital fills up, complications rise, and mortality can spike. “One bad month takes about three months to recover,” Dr. Ferreira says. “But two bad months in a row? That’s unacceptable. The data becomes a call to action.”
Another key metric used is the Case Mix Index (CMI), which reflects the average severity and complexity of hospitalized
patients. A higher CMI indicates that a hospital is treating sicker patients who require more resources.
Risk adjustment is essential. “If a young, otherwise healthy patient dies of pneumonia, that’s very different from a terminal cancer patient with multiple complications dying of pneumonia,” Dr. Ferreira says.
To capture this information more accurately, the team refined Epic templates and improved documentation, ensuring that severity of illness was properly reflected. “The guiding principle is simple; you can only improve what you can measure,” she says.
The quality transformation journey began to take shape in 2019 with the support and guidance of Dipen J. Parekh, M.D., Chief Executive Officer and Chief Operating Officer of UHealth and Executive Vice President for Health Affairs at the University of Miami, who at the time was the Founding Director of the Desai Sethi Urology Institute and Professor and Chair of the Department of Urology, along with Kymberlee Manni, who had just been appointed hospital CEO. Then came COVID-19.
At that time, Dr. Ferreira’s team developed a predictive model that could forecast COVID inpatient census a week in advance, allowing them to run “two hospitals in one” — one for COVID patients, one for non-COVID patients. “We kept occupancy at 100% without overwhelming our capacity,” she explains.
Launched under the leadership of Dr. Ferreira and her quality team, UHealth’s Data Analytic Research Team (UHealth-DART) bridges quality improvement with rigorous scholarship.
The group meets monthly to vet proposals with the dual aim of improving care and producing peer-reviewed output. By 2020, DART had published more than 20 articles covering topics such as sepsis detection and COVID-19, contributing to nearly 40 publications in total. Their work has included leveraging Epic clinical data, developing predictive models, and standardizing care protocols. Among its studies are evaluations of the SOFA (Sequential Organ Failure Assessment) score, a tool that gauges the severity of a patient’s organ dysfunction and helps predict outcomes in critical illness.
DART researchers work alongside department faculty such as Dr. Hayley Gershengorn, from the Division of Pulmonary, Critical Care, and Sleep Medicine, who co-leads the initiative and serves as Medical Director for Quality Data Analytics.
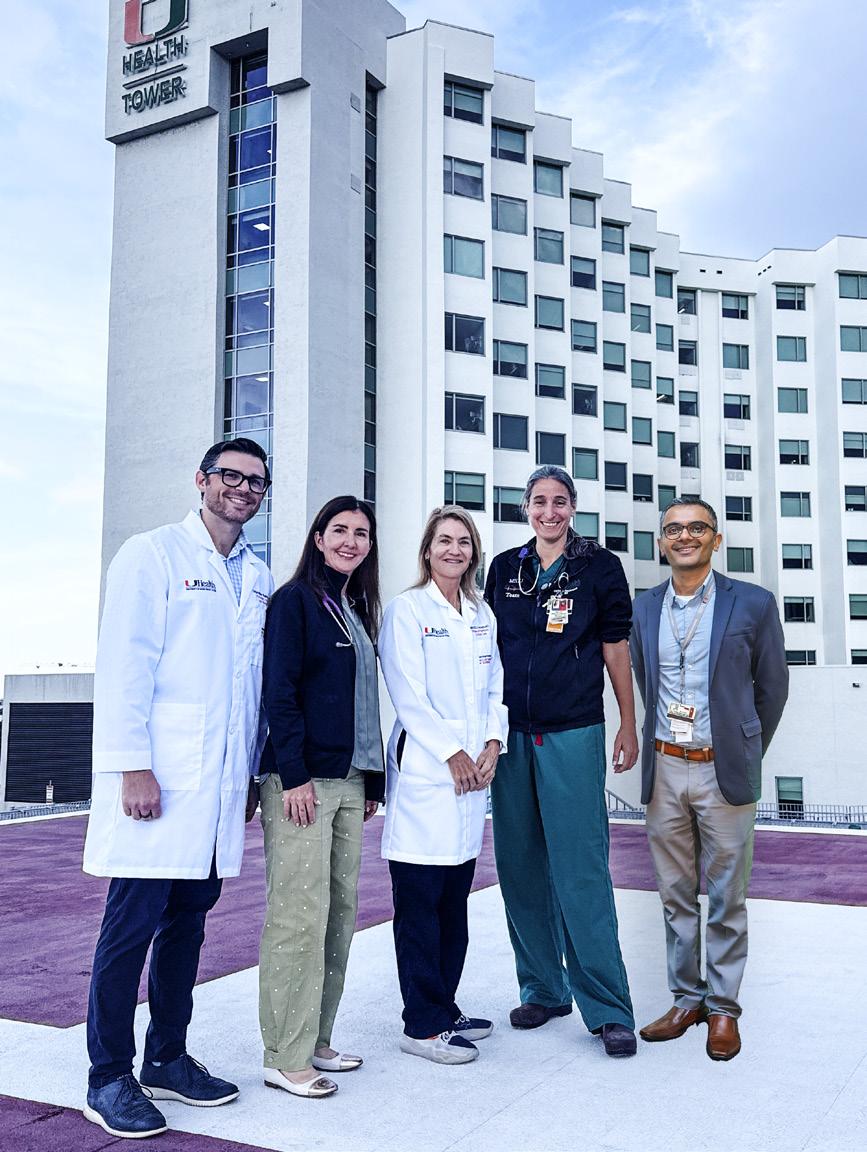
Dr. Ferreira (center) acknowledges and thanks DART team physicians Christopher Mallow, M.D., M.H.S. (far left); Marie Anne Sosa, M.D. (second from left); Hayley B. Gershengorn, M.D., (second from right); and Bhavarth Shukla, M.D., M.P.H. (far right).
The first major quality project – running two hospitals in one and a predictive COVID model – led to high-impact publications in the New England Journal of Medicine and British Medical Journal. Following this success, Dr. Ferreira and the quality team formalized their efforts as the Data Analytic Research Team (DART), aiming to connect quality improvement with academic output. (Refer to the sidebar on this page.)
“Dr. Weiss once told me: ‘Don’t forget you’re an academician,’” Dr. Ferreira recalls. “That stuck with me. Everything we do in quality must also advance research, education, and clinical care, but somehow, that work needs to be translated into peerreviewed journals and publications.”
Data isn’t just about numbers, it must improve care. Surgical and medical departments now use tailored scorecards to track outcomes and complications.
In oncology, for example, the team monitors how many patients die within 14 days of receiving chemotherapy.
“Some deaths are unavoidable, but others may be an opportunity to transition to comfort and palliative measures when no meaningful expectations for recovery are possible with aggressive care,” she says.
Because Dr. Ferreira still practices, continuing to provide ICU coverage, she witnesses firsthand how these frameworks influence care.
“It gives you an advantage,” she says. “I know what happens at the bedside. I’m right there with the staff.”
Other hospitals have taken notice. UHealth now regularly presents at Beckers and Vizient conferences, sharing scorecards, validation tools, and other effective strategies.
“A lot of hospitals are asking to speak to us,” says Dr. Ferreira. “We’ve become a resource for others.”
The next frontier will involve expanding the use of artificial intelligence (AI) and innovation to
advance safe and efficient care. AI tools are already supporting documentation validation and predicting patient outcomes, while an AI Governance Committee ensures these processes are applied responsibly.
“The future is about combining data, accountability, and innovation to continuously advance care,” she adds.
For Dr. Ferreira, this is ultimately a story of transformation – from fragmentation to framework, and from inconsistency to accountability.
“We’ve built something special; a framework that links data-driven metrics to quality, safety, efficiency, and patient experience to education, research, and clinical service. That’s the foundation of academic medicine,” Dr. Ferreira explains.
She adds: “We also aim to further expand our quality data science team, positioning it to be a conduit to advance research and quality improvement projects that align with organizational goals.”
In-Person Encounters for UHealth
30% from Department of Medicine
70% from All Other Departments
Tele-Medicine Encounters for UHealth
22% from Department of Medicine
78% from All Other Departments
Total Revenue for UHealth
18% from Department of Medicine
82% from All Other Departments












































































































































































































































Fellowships
Alex Velasquez, M.D.
Cardiology - Cardiovascular Disease
Omar Wever Pinzon, M.D.






























Cardiology – Advanced Heart Failure/ Transplant
Raul Mitrani, M.D.
Cardiology – Clinical Cardiac Electrophysiology
Michael Dyal, M.D.
Cardiology – Interventional Cardiology
Violet Lagari-Libhaber, D.O. Endocrinology
Morgan Sendzischew-Shane, M.D. Gastroenterology
Iriana Hammel, M.D. Geriatrics
Janaki Sharma, M.D. Hematology/Oncology
David Goldberg, M.D. Hepatology
Mariana Khawand-Azoulai, M.D. Hospice and Palliative Care
Jose Castro, M.D. Infectious Diseases
Zain Mithani, M.D. Nephrology
Rachel Damico, M.D., Ph.D. Pulmonary/Critical Care
Carlos Lozada, M.D. Rheumatology
Alexandre Abreu, M.D. Sleep Medicine
The Division of Cardiovascular Medicine is a national leader in patient care, innovation, and training, ranking in the top 11th percentile nationally by U.S. News & World Report and holding the highest cardiovascular program designation in South Florida. Our reputation for excellence is reflected in remarkable growth: a 40% increase in inpatient cardiovascular volume, a 30% increase in outpatient clinic visits, and significant expansion in diagnostic testing — including echocardiograms (+40%), cardiac computed tomography/ magnetic resonance imaging (CT/MRI) (+70%), and invasive procedures such as left heart catheterizations and percutaneous coronary interventions (+25%). This growth underscores both the rising regional demand for advanced cardiovascular care and the community’s trust in our exceptional quality and outcomes.
As pioneers in cardiovascular innovation, we are among the first in the nation to offer transformative therapies, including renal denervation for resistant hypertension, drugcoated balloon angioplasty, pulse field ablation for atrial fibrillation, and extravascular implantable cardioverter-defibrillator implantation. Our programs in interventional cardiology, structural heart disease, and electrophysiology consistently
employ the most advanced tools, imaging modalities, and software platforms to improve precision, safety, and patient recovery. The Structural Heart Disease Program ranks in the top 10% nationally for quality, with nearzero 30-day mortality, nearly 100% home discharges, readmission rates under 1%, and the state’s first same-day transcatheter aortic valve replacement (TAVR) discharge.
Our advanced cardiovascular imaging program is among the most sophisticated in the region, integrating state-of-the-art cardiac CT and MRI technology with artificial intelligence (AI)-driven analysis for coronary plaque assessment, fractional flow reserve from computed tomography (FFR-CT), and valve modeling. With facilities across multiple Miami-Dade locations and rapid turnaround – most results delivered in under 24 hours – our imaging services not only enhance diagnosis but also directly support complex interventions in interventional cardiology, structural heart disease, electrophysiology, and cardiovascular surgery.
In FY2025, we welcomed several outstanding physicians to our cardiovascular team, adding expertise in advanced and structural imaging, heart failure, and general non-invasive cardiology. Building on this momentum, we are actively recruiting and expect to add approximately 10 more physicians
in the coming year, further expanding our capabilities in both specialized and comprehensive cardiovascular care.
With extensive active funding, the Cardiovascular Research Program is a powerhouse of scientific discovery and innovation. Our National Institutes of Health (NIH)-funded translational science bridges fundamental discoveries to clinical applications, while a robust portfolio of clinical trials spans prevention, advanced imaging, heart failure, structural heart disease, and electrophysiology. By leveraging artificial intelligence and real-world data analytics, we accelerate the development of cuttingedge diagnostics and therapies. This integration of research, technology, and clinical excellence has positioned us as a national hub for translating breakthroughs from bench to bedside.
The University of Miami/Jackson Memorial Hospital’s Cardiovascular Fellowship Program is a premier destination for training future leaders in heart and vascular medicine, providing a robust, high-volume, and diverse clinical environment that cultivates both clinical excellence and academic leadership. Our Accreditation Council for Graduate Medical Education


Yiannis S. Chatzizisis, M.D., Ph.D.
Division Chief Professors
Simon C. Chakko, M.D. (Emeritus)
Yiannis S. Chatzizisis, M.D, Ph.D.
Eduardo J. De Marchena, M.D.
Chunming Dong, M.D.
Jeffrey Goldberger, M.D.
Joshua M. Hare, M.D.
Robert J. Myerburg, M.D. (Emeritus)
Rafael Sequeira, M.D. (Emeritus)
Professors of Clinical Medicine
Maureen H. Lowery, M.D. (Emeritus)
Claudia Martinez, M.D.
Raul Mitrani, M.D.
Research Professor
Lina Shehadeh, Ph.D.
Associate Professor
Martin S. Bilsker, M.D. (Emeritus)
Associate Professors of Clinical Medicine
Eugene J. Bauerlein, M.D.
Pedro Cox, M.D.
Michael Dyal, M.D.
Litsa K. Lambrakos, M.D.
George Marzouka, M.D.
Alan H. Schob, M.D.
Omar Wever-Pinzon, M.D.
Research Associate Professor
Wayne Balkan, Ph.D.
Assistant Professors of Clinical Medicine
Sharon N. Andrade-Bucknor, M.D.
Pedro Covas, M.D.
Joseph Esterson, M.D.
Mrudula Munagala, M.D.
Nikolaos Spilias, M.D.
Robert B. Stang, M.D.
Alex Velasquez, M.D.
(ACGME)-accredited subspecialty fellowships in interventional cardiology, electrophysiology, and advanced heart failure/transplant, along with our dedicated one-year International Interventional Structural Heart Disease Fellowship, attract global top-tier talent.
During the 2025 academic year, we trained 27 fellows across PGY4 to PGY-6 levels. With a recent program expansion, we now offer comprehensive training in general cardiology, interventional cardiology, electrophysiology, structural heart disease, heart failure, hypertension and preventive medicine, and advanced cardiovascular imaging. Fellowship growth is expected to reach 40 fellows – an increase of approximately
Research Assistant Professors
Jose Manuel Condor, Ph.D.
Martin Liu, M.D., Ph.D.
Wei Wu, Ph.D.
Shijia Zhao, Ph.D.
Staff Physicians
Beteal Ashinne, M.D.
Antonio Barquet-Leon, M.D.
Andrew Bromley, M.D.
Hoda Butrous, M.D.
George Degheim, M.D.
Murry Drescher, M.D.
Thanh Duong-Wagner, M.D.
Mehrdad Ghahramani, M.D.
David Weininger, M.D.
Zachariah P. Zachariah, M.D.
Fellows
Cardiovascular Disease
First Year
Fatemah Akbar, M.D.
Ian Ergui, M.D.
Jessica M. Gonzalez, M.D.
Khaled Harmouch, M.D.
Behdad Kavianpour, M.D.
Ashwin Kumar, D.O.
Vidit D. Majmundar, M.D.
Saurabhi M. Samant, M.D.
Zafer Sattouf, M.D.
30% – further strengthening our expertise across these disciplines.
In March 2025, we hosted our inaugural continuing medical education (CME) event, Cardiology for the Primary Care Physician. The conference welcomed 85 healthcare providers from across the country, with many more participating via live stream.
Held in Miami from January 18-20, 2025, the Miami Valves Conference, a leading global platform for innovation, collaboration, and patient-centered cardiovascular care, brought together leading interventional cardiologists, cardiac surgeons, imaging specialists, and allied health professionals from around the world. The program featured live cases, expert lectures,
Second Year
Saahil Jumkhawala, M.D.
Fabricio Malaguez Webber, M.D.
Alan Mendez Ruiz, M.D.
Nicole Parellada, M.D.
Anastasios Roumeliotis, M.D.
Julio Cesar Santana, M.D.
Andrew Sephien, M.D.
Third Year
Mohammed Ali, M.D.
Marina Byer, M.D.
Trevor I. Eisenberg, M.D.
Nayrana Griffith, M.D.
Rafael J. Hernandez, M.D.
Beatriz P. R. Rodriguez, M.D.
Francisco J. Romeo, M.D.
Advanced Cardiac Imaging
Patrina Conley Brown, D.O. Clinical Cardiac Electrophysiology
Suraj Dahal, M.D.
Phillip Rubin, M.D. Heart Failure
Gabriel Esses, D.O.
Hypertension and Preventive Cardiology
Shahzad Hassan, M.D. Interventional Cardiology
Natalie T. Dal’bo, M.D.
Angie M. Molina, M.D.
Deep B. Sangani, M.D.
interactive discussions, and hands-on training on advanced transcatheter therapies, including TAVR, mitral and tricuspid interventions, and left atrial appendage closure.
Our 2025 Heart Month Campaign was the highest-volume initiative in our division’s history, adopting a multichannel approach to increase public awareness of cardiovascular health.
UHealth’s Cardiology and Heart Surgery program was ranked No. 92 nationally in the 2024–2025 U.S. News & World Report rankings. Our program also earned “high performing” designations in key areas of cardiac care, including heart failure, heart attack, and aortic valve surgery.
The Division of Clinical Pharmacology is primarily a research division dedicated to the investigation of the effects of new pharmacological agents and disease mechanisms in humans. We are proud of our long and established record of successful research across a wide range of therapeutic areas.
Narcolepsy type 1 (NT1) is a chronic neurological sleep disorder that can be severely disruptive and often disabling. It affects approximately 1 in every 2,000 people in the United States – about 200,000 Americans – though some experts believe the prevalence may be higher due to underdiagnosis. NT1 interferes with the brain’s regulation of
sleep, leading to significant daytime problems. Common symptoms include disrupted nighttime sleep, abnormal rapid eye movement (REM) sleep, excessive daytime sleepiness, hallucinations, and cataplexy, which is sudden muscle weakness or loss of muscle control. The annual cost of medical treatment for narcolepsy is estimated at around $12,000 per patient, excluding lost wages.
The Division of Clinical Pharmacology is developing a novel, orally available molecule that targets the biochemical pathway underlying NT1. This represents the first approach designed to directly treat the pathophysiological cause of narcolepsy. The compound is
eliminated by the liver, and liver dysfunction can alter drug absorption, distribution, metabolism, and excretion. The purpose of this study is to evaluate the safety, pharmacokinetics (how the drug is processed in the body), and optimal dosing schedule of this promising compound in patients with liver disease.
The apolipoprotein L1 (APOL1) gene is expressed in multiple human organs, including the kidney. Two APOL1 variants, G1 and G2, are associated with the development and progression of chronic kidney disease (CKD). When CKD occurs in patients carrying two APOL1 variants, it is referred to as APOL1mediated kidney disease (AMKD). These variants are more common

among individuals of African ancestry, partly explaining the higher risk of CKD and progression to end-stage kidney disease in this population compared to those of non-African ancestry.
The division is collaborating on the development of an APOL1 inhibitor for the treatment of AMKD – a novel therapy with the potential to slow kidney disease progression in millions of patients. Because the compound is primarily eliminated through liver metabolism, the current study is designed to evaluate its pharmacokinetics, safety, and tolerability in participants with mild or moderate liver impairment, with the goal of establishing an appropriate dosing schedule.
The division has further developed and expanded its five-session and two-week courses aimed at incorporating clinical pharmacology principles into research and clinical practice training. The program has now been implemented across multiple levels, including medical students, residents, fellows, and faculty. Participants learn the basics of clinical pharmacokinetics followed by clinical applications. Subsequent sessions cover drug metabolism in the liver, drug interactions, the effects of organ dysfunction, and pharmacogenetics.



Richard A. Preston, M.D., M.S.P.H., M.B.A.
Division Chief
Professor of Clinical Medicine
Richard A. Preston, M.D., M.S.P.H., M.B.A.


The Division of Digestive Health and Liver Diseases has expanded its clinical practice to UHealth Doral and welcomed several new providers to staff UHealth Doral, Lennar, SoLé Mia, and the downtown campus practices. With this expansion, the division has added 11 new staff physicians and three new advanced practice providers (APPs) to the team.
The Crohn’s and Colitis Center now offers intestinal ultrasound, led by Oriana Damas, M.D., M.S.C.T.I., with support from Stephanie Ioannou, M.D., and Gabriella Raffa, M.D. This technology provides real-time, cost-effective assessment of disease activity and treatment response. The Gastrointestinal (GI) Genetics clinic has also expanded its reach, with the addition of Carolina de Varona, A.P.R.N. Ms. de Varona recently graduated from the City of Hope’s Intensive Course in GI
Genomic Cancer Risk Assessment. Sunil Amin, M.D., M.P.H., performed UM’s 100th esophageal per-oral endoscopic myotomy (POEM), a less-invasive procedure that improves quality of life for patients with achalasia.
David Goldberg, M.D., M.S.C.E., was awarded a multiple-PI, five-year R01 from the National Cancer Institute (NCI) to develop new risk models for predicting keratinocyte carcinomas in kidney and liver transplant recipients, who face an increased risk of skin cancer. This research aims to refine models to predict both incident and subsequent skin cancers, while also creating evidence-based treatment algorithms focused on immunosuppression management in these high-risk patients.
His work on the THINKER-NEXT study was recognized as a late-

breaking abstract at the 2025 World Transplant Congress. This study evaluates the safety and effectiveness of transplanting kidneys from donors with hepatitis C virus (HCV) into HCVnegative recipients. Preliminary results show a 99% HCV cure rate for the organ recipients, a major breakthrough in expanding the availability of donated organs.
Dr. Damas, Interim Director of the Crohn’s and Colitis Center, and her research team launched two clinical trials offering innovative treatment options for patients with inflammatory bowel disease (IBD). A new National Institutes of Health (NIH) R01 trial is testing an American-tailored, Mediterranean-inspired diet for patients with ulcerative colitis while also examining each patient’s microbiome and genetics to identify who responds best to dietary therapy. A second trial is designed to study diet and medicationbased weight loss for patients with Crohn’s disease.
Shria Kumar, M.D., M.S.C.E., an advanced endoscopist and cancer preventionist, has expanded primary gastric cancer prevention efforts in South Florida though a one-of-akind, community-based test-andtreat strategy for Helicobacter pylori, supported by an NRG Oncology/ NCI Community Oncology Research Program (NCORP) grant and two industry trials. Her research also investigates risk factors for early-onset colorectal cancer (CRC), including whether accelerated aging may contribute to its development in young people. Her published work is among the first large-scale analyses comparing early-onset and later-onset CRC to better understand why younger people are developing colon cancer at striking rates.
Cynthia Levy, M.D., an expert in cholestatic liver disease, serves as global PI for an interntational multi-

Daniel Sussman, M.D., M.S.P.H.
Division Chief, Interim
Professors
Jaime S. Barkin, M.D. (Emeritus)
Paul Martin, M.D. (Emeritus)
Professors of Clinical Medicine
Amar Deshpande, M.D.
Cynthia Levy, M.D.
Daniel Sussman, M.D., M.S.P.H.
Associate Professor
David Goldberg, M.D., M.S.C.E.
Associate Professors of Clinical Medicine
Sunil Amin, M.D. , M.P.H.
Jodie Barkin, M.D.
Oriana Damas, M.D., M.S.C.T.I.
Jose Garrido, M.D.
Binu John, M.D.
Patricia Jones, M.D., M.S.C.R.
David Kerman, M.D.
Assistant Professors of Clinical Medicine
Stephanie Ioannou, M.D.
Shria Kumar, M.D., M.S.C.T.I.
Eric Martin, M.D.
Jordan Orr, M.D.
center prospective observational cohort study to support drug development in adult patients with primary sclerosing cholangitis (PSC). She was also the first author of an oral presentation at the European Association for the Study of the Liver (EASL) annual meeting, and of a Journal of Hepatology manuscript on the safety and efficacy of elafibranor in PSC.
Amar Deshpande, M.D., and Daniel Sussman, M.D., M.S.P.H., collaborated with S. Barry Issenberg, M.D. (Division of General Internal Medicine), and colleagues at the University of Pennsylvania to demonstrate how large language models can be used to optimize clinical workflows across multiple platforms for colonoscopic polyp surveillance. This work was published in Gastroenterology
Several GI and liver attendings and fellows presented work at Digestive Disease Week 2025 in San Diego, CA,, covering topics including applications of artificial intelligence, pancreatic cancer screening, risk factors for earlyonset cancers, clinical trials for IBD and
Ami Panara Shukla, M.D.
Gabriel J. Perrault, M.D.
Gabriella Raffa, M.D.
Andrew Scheinberg, M.D.
Morgan Sendzischew Shane, M.D., M.S.C.T.I.
Staff Physicians
Janyll Castineira, D.O.
Fabian Emura, M.D.
Juan Gomez Cifuentes, M.D.
Mahmoud Mahfouz, M.D.
Emory Manten, M.D.
Francesca Raffa, M.D.
Grigoriy Rapoport, M.D.
Joshua Turkeltaub, M.D.
Fellows
Gastroenterology Disease Fellows
First Year
Kristen Fadel, M.D.
Neelima Gaddipati, M.D.
Shruti Kulkarni, M.D.

Miami GI Congress Co-Directors, Jodie Barkin, M.D., and Sunil Amin, M.D., M.P.H., showcase advances in gastroenterology and endoscopy at the inaugural conference.
pancreatic diseases, and outcomes from innovative procedures such as endoscopic submucosal dissection.
The division continues to demonstrate excellence in medical education at multiple levels. Morgan Sendzischew Shane, M.D., M.S.C.T.I., serves as Fellowship Program Director,
Nikita Mittal, M.D.
Muhammad Raza, M.D.
Claudia Saborit, M.D.
Second Year
Helen Bermudez, M.D.
Keri Ann Buchanan-Peart, M.D.
Jonathan Gross, M.D.
Gala Martinez Godoy Brewer, M.D.
Myra Quiroga, M.D.
Third Year
Chaitra Banala, M.D.
Nisa S. Desai, M.D.
Lauren Lee Johnson, M.D.
Rahil Harshad Shah, M.D.
Shyam Vedantam, M.D.
Transplant Hepatology Fellow
Monica Sihota, M.D.
Advanced Endoscopy Fellow
Gregory Toy, M.D. (Clinical Instructor)
shaping the next generation of gastroenterologists and thought leaders. The most recent graduating class included four fellows who advanced to academic institutions, with another pursuing an advanced endoscopy fellowship. Ami Panara Shukla, M.D., contributes as a Longitudinal Clinical Educator and Andrew Scheinberg, M.D., now leads the Phase I medical student GI module.
Jodie Barkin, M.D., and Dr. Amin codirected the division’s inaugural Miami Gastroenterology Congress, which showcased division faculty, national speakers, and a live endoscopy component for advanced GI education.
Dr. Damas co-led the American Gastroenterological Association (AGA) Southeast Regional Women in GI Workshop at the University of Miami, uniting 50 women nationwide for sessions with distinguished speakers to foster connection and career advancement.
The IBD Center hosted its annual Ins and Outs of IBD Conference in Miami, sharing key updates in IBD care.
Outpatient encounters grew from 29,500 to 42,000, reflecting both expanded access and the division’s continued commitment to delivering high-quality care. This growth was driven by the recruitment of Maria Yanez-Bello, M.D., and Tamara de Souza, M.D., along with the expansion of our advanced practice provider (APP) and nurse navigator teams.
The division expanded its clinical services with the launch of an integrated sleep-metabolic clinic and the development of specialized programs in bone health and lipidology. This multidisciplinary approach reflects the division’s commitment to transforming care delivery by fostering collaboration, enhancing efficiency, improving outcomes, and elevating the patient experience. Additionally, the Comprehensive Diabetes Center at the Lennar Foundation Medical Center earned renewal of American Diabetes Association (ADA) recognition for four years, underscoring our leadership in com-
prehensive diabetes management. The division ranks in the top 22% nationwide (U.S. News & World Report).
Endocrinology was the top participating division in the Department of Medicine’s 11th Annual Eugene J. Sayfie, M.D. Research Day, submitting 31 abstracts and winning three “Shark Tank” awards. The inaugural Diabetes Day, held in November, brought together faculty, fellows, and participants for a progam of discussions and presentations on the future of diabetes therapies, incretinbased treatments, GLP-1–related side effects, and weight-loss strategies.
Nationally and internationally, our faculty and trainees were highly visible at the ADA Scientific Sessions and ENDO 2025, contributing research on beta cell preservation, vascular regulation of islets, diabetes risk prediction, continuous ketone monitoring, and cardiometabolic health. At ENDO 2025, our six fellows
presented 13 posters showcasing their research and case studies. This achievement underscores the division’s commitment to training the next generation of academic endocrinologists.
Leaders including Joana Almaça, Ph.D., Rodolfo Galindo, M.D., Alejandro Caicedo, Ph.D., and Ernesto BernalMizrachi, M.D., continue to excel through National Institutes of Health (NIH)-funded research, innovative clinical programs, and mentorship. Dr. Galindo served as Chair of the 12th Annual Endocrine Fellows Conference on Type 1 Diabetes Care and Management, sponsored by the Endocrine Society, and also contributed to the development of the 20242025 American Diabetes Association Standards of Care guidelines. Mark Jara, M.D., was recognized for his leadership on the Endocrine Society’s Trainee and Career Development Core Committee, which supports mentorship and career growth for early-career endocrinologists.


Ernesto Bernal-Mizrachi, M.D.
Division Chief
Professors
Rodolfo Alejandro, M.D. (Emeritus)
Ernesto Bernal-Mizrachi, M.D.
Alejandro Caicedo-Vierkant, Ph.D.
Dirk Homann, M.D. (Pending Rank)
Alberto Pugliese, M.D. (Emeritus)
Jay Skyler, M.D.
Jay Sosenko, M.D.
Roy E. Weiss, M.D., Ph.D.
Professor of Clinical Medicine
Gianluca Iacobellis, M.D., Ph.D.
Research Professor
Ricardo Pastori, Ph.D.
Associate Professor
Joana Almaça, Ph.D.
Associate Professors of Clinical Medicine
Rodolfo Galindo, M.D.
Zeina Hannoush, M.D.
Violet Lagari-Libhaber, D.O.
Francesco Vendrame, M.D., Ph.D.
Research Associate Professor
Armando Mendez, Ph.D.
Assistant Professor
Rene Barro-Soria, Ph.D.
Assistant Professors of Clinical Medicine
David Baidal, M.D.
Ayse Canturk, M.D.
Tamara de Souza, M.B.B.S.
Mark Jara, M.D.
Jason Levine, D.P.M.
Diana Soliman, M.D.
Ron Varghese, M.B.B.S.
Research Assistant Professors
Ruy Andrade Louzada Neto, Ph.D.
Manuel Blandino, Ph.D.
Carlos Blaschke, M.D.
Khemraj Hirani, Ph.D.
Rahul Mittal, Ph.D.
Joana Nunes Lemos Oliveira, Ph.D.
Rayner Rodriguez-Diaz, Ph.D.
Joao Saar Werneck De Castro, Ph.D.
Staff Physicians
Ashley Engel, M.D.
Silvia Gra Menendez, M.D.
Bresta Miranda, M.D.
Julio Pita, M.D.
Anu Thekkumkattil, M.D.
Carmen Villabona, M.D.
Maria Yanez-Bello, M.D. Fellows
First Year
Monica Bodenstab, M.D.
Jessica Oliveira Pinto, M.D.
Mariana Velasquez Duran, M.D.
Nathalie Wacher Rostoker, M.D. Second Year
Crystal M. Acosta, M.D.
Marie Louise Aoun, M.D.
Karla Amelia Baez Rodriguez, M.D.
Ayoola Omobolande Olayiwola, M.D.

Endocrinology Conference 2025 – Faculty and Fellows
Group photo (left to right): Rodolfo Galindo, M.D.; Savian Renato, M.D.; Karla Baez, M.D.; Marie Louise Aoun, M.D.; Carmen Villabona, M.D.; Alejandra Razzeto, M.D. (alumni); Hery Mejia, M.D. (alumni); Miguel Jara-Palacios, M.D. (alumni) ; Mario Bustos, M.D. (alumni); Francisco Barrera Echegoyen, M.D. (alumni); Zenia Hannoush, M.D. Front row: Ayoola Omobolande Olayiwola, M.D.; Violet Lagari, D.O.

Endocrinology Conference
2025 Poster Presentations
Far left: Karla Baez, M.D., and Violet Lagari, D.O.
Immediate left: Zenia Hannoush, M.D., and Hery Mejia, M.D.
The Division of General Internal Medicine has significantly expanded its clinical practice at UHealth Doral with the addition of four new staff physicians: Yanelys Fernandez-Nosti, M.D., German Lopez, M.D., Adelaida Cueto, M.D., and Farrell Sheehan, M.D. Division faculty will also provide care at UHealth SoLé Mia. Under the leadership of Maritza Suarez, M.D., the division has implemented multiple artificial intelligence (AI) initiatives across UHealth, from

ambient AI with Suki to AI-assisted clinical documentation and in-basket messages.
Gauri Agarwal, M.D., and Ken Goodman, Ph.D., published “Can a Chatbot Be a Medical Surrogate?: The Use of Large Language Models in Medical Ethics Decision-Making” in the New England Journal of Medicine AI. Dr. Agarwal also published the first AI educational module for health profession students in the Association of American Medical Colleges’ MedEdPORTAL
Erin Marcus, M.D., M.P.H., Stefanie Brown, M.D., M.B.A., and Joan St. Onge, M.D., M.P.H., published “Residency Program Planning for Hurricanes and Beyond” in the Journal of Graduate Medical Education and presented their work at national conferences, sharing strategies for preparing residency programs for natural disasters.

Dr. Brown and Dr. St. Onge published “Integration of Behavioral Health Specialists in Residency Programs” in the Journal of Biomedical Research & Environmental Sciences.
Sonjia Kenya, Ph.D., led the 2025 cohort of the Cardiovascular Research Empowerment Workforce Program (CREW), a partnership between UM and the U.S. Virgin Islands (USVI) Department of Health, training eight undergraduate students from the USVI in research.
Division faculty were also selected for multiple oral and poster presentations at the national Society of General Internal Medicine (SGIM) meeting in May 2025.
Sarah Bland, M.D., served as Faculty Accreditation Lead for the recent Liaison Committee on Medical Education (LCME) review. The LCME granted the Miller School of Medicine full accreditation for the maximum eight-year term, an exceptional outcome that reflects the strength, dedication, and continued progress of our academic and clinical community.
Dr. St. Onge was appointed to the Accreditation Council for Graduate Medical Education (ACGME) Board of Directors in November 2024 for a three-year term and was also named to the Florida Agency for Health Care Administration’s Graduate Medical Education Committee.
Elizabeth Greig, M.D., received the Faculty Citizenship Award at the 2024 Dean Faculty Awards. As Co-Director of the Global Institute for Community Health and Development, Dr. Greig participated in the United States Naval Ship (USNS) Comfort’s most
Elizabeth Greig, M.D., provided disaster simulation training aboard the USNS Comfort.
Sabrina Taldone, M.D., M.B.A.
Division Chief
Professors
Olveen Carrasquillo, M.D., M.P.H.
Laurence Gardner, M.D.
Kenneth Goodman, Ph.D. (Emeritus)
S. Barry Issenberg, M.D.
recent humanitarian mission, fostering partnerships in medicine and patient care across the Caribbean, Central America, and South America.
S. Barry Issenberg, M.D., served as President of the Society for Simulation in Health Care.
Dr. Kenya received a proclamation from the City of Miami, presented by Mayors Daniella Levine Cava and Francis Suarez.
Dr. Agarwal and her interdisciplinary team received the UM Provost Award for Excellence in Collaborative Teaching for their AI in Healthcare curriculum for first-year medical students.
Division faculty at the national Society of General Internal Medicine (SGIM) meeting in May 2025.
Left to right: Dr. Suarez, Dr. Alex Mechaber, Dr. Hilit Mechaber, Dr. Brown, Dr. Kenya, Dr. Snow, Dr. Suarez Zarate, Dr. Taldone, Dr. Carrasquillo, and Dr. Clauss at the national SGIM meeting.
Professors of Clinical Medicine
Panagiota Caralis, M.D., J.D.
Daniel Lichtstein, M.D. (Emeritus)
Erin Marcus, M.D., M.P.H.
Joan St. Onge, M.D., M.P.H.
Ross Scalese, M.D.
Professor of Professional Practice
Sonjia Kenya, Ph.D.
Associate Professor
Mark Gelbard, M.D. (Emeritus)
Associate Professors of Clinical Medicine
Gauri Agarwal, M.D.
Yvonne Diaz, M.D.
Hilit Mechaber, M.D.
Paul Mendez, M.D.
Maritza Suarez, M.D.
Sabrina Taldone, M.D., M.B.A.
Frederick Williams, M.D.
Assistant Professors of Clinical Medicine
Levy Amar, M.D.
Howard Anapol, MD
Sarah Bland, M.D.
Stephanie Clauss, D.O.
Gregory Coleman M.D.
Janelle Cuervo, D.O.
Nemer Dabage-Forzoli, M.D.
Janelis Gonzalez, M.D.
Elizabeth Greig, M.D.
Lilliam Guzman M.D.
Brian Hagenlocker, M.D.
Melanie Helfman, M.D.
Margarita Llinas M.D.
Cristina Pravia, M.D.
Anita Sikha, M.D.
Katelin Snow, M.D.
Jacobo Wajner M.D.
Staff Physicians
Alexandra Calandriello, M.D.
Manuela Calvo, M.D.
Adria Cruz Labrada, M.D.
Adelaida Cueto, M.D.
Nisha Dabir, M.D.
Ana de Diego, M.D.
Neelesh Dewan, M.D.
Yanelys Fernandez-Nosti, M.D.
Grettel Garcia, M.D.
Janella Leon, D.O.
German Lopez, M.D.
Marie Normil, M.D.
Hiram Rodriguez, M.D.
Farrell Sheehan, M.D.

The Division of Geriatrics and Palliative Medicine continues to expand its team and services to better meet the needs of patients with serious illness. The geriatrics team added two new faculty members and a nurse navigator, while palliative medicine welcomed two Advanced Practice Registered Nurses (APRNs) and a nurse navigator.
A new palliative care clinic at UHealth Doral has also opened, joining an established network of services at UHealth Tower and other clinical sites. These expansions increase access to specialized, compassionate care that is focused on symptom management, comfort, and support for patients and families during complex health journeys.
Michael Huber, M.D., advanced his research on clinical, policy, and
legislative variation in the care of seriously ill patients with critical illness, publishing in multiple journals, including Chest and JAMA Health Forum
Dr. Huber received a Faculty Appreciation Award, and Mariana Khawand-Azoulai, M.D., received a Mentorship Award from the University of Miami/Jackson Memorial Hospital. As Director of the Hospice and Palliative Medicine Fellowship, Dr. Khawand-Azoulai introduced new curricula on bereavement and serious illness communication and supported a grant-funded educational initiative to train community health workers.
UHealth’s Geriatrics Program earned recognition as “high performing” by U.S. News & World Report – a
designation reserved for hospital specialties ranked in the top 10% nationwide. The program received a Geriatrics Scorecard rating of 62.3 out of 100, underscoring its commitment to excellence in the care of older adults. These milestones highlight UHealth’s continued leadership in delivering compassionate, high-quality care across a wide range of specialties.
Dr. Khawand-Azoulai was named a fellow of the American Academy of Hospice and Palliative Medicine, recognizing her leadership and contributions to the field. She continues to lead the UHealth inpatient palliative care service and collaborates with institutional leaders on quality initiatives to improve care for seriously ill patients.





Marcio Rotta Soares, M.D.
Division Chief
Professors
Stuti Dang, M.D.
Silvina Levis, M.D. (Emeritus)
Research Professor
Guy Howard, Ph.D.
Research Associate Professor
Carlos Perez-Stable, Ph.D.
Assistant Professors of Clinical Medicine
Iriana Hammel, M.D.
Michael Huber, M.D.
Mariana Khawand-Azoulai, M.D.
Luis Samos-Gutierrez, M.D.
Julia Sanchez, M.D.
Marcio Soares, M.D.
Khin Zaw, M.D.
Fellows
Geriatric Medicine
Marilia Monte Carrilho Da Silva, M.D.
Angela Castillo Diaz, M.D.
Carlos Dominguez, M.D.
Sofia Economidou, M.D.
Arielle Gallardo, M.D.
Ram Prakash Thirugnansambandam, M.D.
Hospice and Palliative Care Medicine
Toluwami Adebayo, M.D.
Khaled El Khatib, M.D.
Julie Kanter, M.D.
Juliet Kimathi, M.D.
Nandita Saharan, M.D.
The Division of Hematology continues to redefine how and where expert care is delivered across South Florida. The opening of UHealth Doral in 2024 and UHealth SoLé Mia in October 2025 extends our reach into growing communities, providing convenient access to advanced hematologic care. These expansions, combined with the recruitment of new faculty and advanced practice providers, reflect a strategic effort to meet increasing patient demand while maintaining a focus on innovative, patient-centered care. New outpatient clinics include


those that focus on cutaneous lymphomas, clonal hematopoiesis, and bone marrow failure conditions.
Over the past five years, the number of distinct hematology patients has grown by 54% (compound annual growth rate of 9%), while total visits and procedures have grown by 61% (compound annual growth rate of 9%). This year, inpatient volumes increased by 5% and 477 patients enrolled across 83 active clinical trials – 267 in interventional treatment studies, representing a 21% increase from FY24. Notably, 54% of participants came from traditionally underrepresented minority groups, underscoring our commitment to inclusive research and equitable access to experimental therapies.
Izidore Lossos, M.D., received the 2024 Excellence in Clinical Service Award for his leadership and dedication to meaningful patient outcomes, exemplifying our commitment to clinical excellence.
Our faculty are not only published in leading high-impact journals but also play an active role in shaping the future of hematology research, clinical trial design, regulatory frameworks, and standards of care. Their leadership is redefining how therapies are developed, evaluated, and implemented.
In FY25, our faculty authored 69 peer-reviewed publications, 33% of which appeared in journals with impact factors above 10, including top journals in hematology, oncology, and general medicine.
Juan Alderuccio, M.D., led a pivotal investigator-initiated trial at the University of Miami Sylvester Comprehensive Cancer Center that was featured at the American Society of Hematology (ASH) Annual Meeting, published in Lancet Haematology, and incorporated into the National
Comprehensive Cancer Network (NCCN) guidelines as a new standard of care for lymphoma.
Since 2022, Mikkael Sekeres, M.D., M.S., has collaborated with the U.S. Food and Drug Administration (FDA) to advance drug development pathways for myelodysplastic syndromes (MDS). His March 2025 Blood Advances publication, developed with FDA input, outlines strategies to better align trial design with regulatory standards. A companion article in Blood, coauthored with Stephen Nimer, M.D., and Justin Taylor, M.D., proposes more inclusive, phase-appropriate eligibility criteria for MDS trials, with recommendations intended to guide future regulatory approvals.
Dr. Lossos continues to redefine lymphoma classification, contributing to the World Health Organization’s 2025 publication on mantle cell lymphoma.
Dr. Nimer, collaborating with Dr. Taylor and Terrence Bradley, M.D., identified the role of phosphorylated CARM1 in proliferation of hematologic malignancies.
Dr. Taylor earned a National Institutes of Health (NIH) R01 grant to investigate resistance to Bruton’s tyrosine kinase (BTK) inhibitors in chronic lymphocytic leukemia (CLL), ranking in the top 1% of NIH submissions. His lab’s discovery that BTK kinase-dead resistance mutations can be overcome by targeted protein degradation earned national recognition, advancing to the Final Four in STAT News’ 2024 March Madness biomedical innovation competition. He also was elected to the American Society for Clinical Investigation (ASCI) and received the Award for Outstanding Basic/Translational Research in December 2024.
Jonathan Schatz, M.D., secured a Department of Defense grant to study B-cell lymphoma biology and immune system interactions.

Mikkael A. Sekeres, M.D., M.S.
Division Chief
Professors
John Byrnes, M.D.
Izidore Lossos, M.D.
Craig Moskowitz, M.D.
Stephen Nimer, M.D.
Joseph Rosenblatt, M.D.
Mikkael Sekeres, M.D., M.S.
Professor of Clinical Medicine
Juan Carlos Ramos, M.D.
Jonathan Schatz, M.D.
Gerald Soff, M.D.
Research Professor
Ramiro Verdun, Ph.D.
Associate Professor
Justin Taylor, M.D.
Associate Professors of Clinical Medicine
Juan Alderuccio, M.D.
Alvaro Alencar, M.D.
Justin Watts, M.D.
Assistant Professors of Clinical Medicine
Ney Alves, M.D.
Terrence Bradley, M.D.
Diana Byrnes, M.D.
Roberto Cano, M.D.
The division continues to shape the future of hematology through mentorship, education, and leadership across national and international platforms. Faculty mentor learners at all levels and contribute globally through lectures, collaborations, and committee service.
Dr. Nimer received the 2024 ASH Mentor Award in recognition of his lasting impact on training and developing physician-scientists. Sangeetha Venugopal, M.D., was named a 2024 Scholar by the ASH Clinical Research Training Institute. Asaad Trabolsi, M.D., earned top honors in the “Shark Tank” competition at the Department of Medicine’s 11th Annual Eugene J. Sayfie, M.D. Research Day.
In addition to educating the next generation of learners – spanning undergraduate, medical school, residency, and fellowship training –our educational reach extends globally, with faculty chairing conferences and
Namrata Chandhok, M.D.
Jonathan Cohen, M.D.
Jibran Durrani, M.D.
Thomas Harrington, M.D.
Thomas Earl Platé IV, M.D.
Georgios Pongas, M.D.
Michele Stanchina, D.O.
Asaad Trabolsi, M.D.
Sangeetha Venugopal, M.D.
Steven Weiss, M.D.
Research Assistant Professors
Xiaoyu Jiang, Ph.D.
Jun Sun, Ph.D.
Yu Zhang, M.D.
Staff Physicians
Diogenes Alayon, M.D.
Mayda Arias, M.D.
Erika Correa, M.D.
Douglas Faig, M.D.
David Lessen, M.D.
Ashley Rose, M.D.
Daniel Tannenbaum, M.D.
delivering key lectures across Europe, Israel, Latin America, Central America, and North America.
Justin Watts, M.D., Maria Figueroa, M.D. (from the Department of Biochemistry and Molecular Biology), and Dr. Sekeres co-chaired the Miami Leukemia Biennial Conference; Alvaro Alencar, M.D., co-chaired the Simpósio Internacional de Onco-Hematologia (SINTOMA) in Brazil; and Dr. Sekeres co-chaired the AAMDSIF Bone Marrow Failure Summit, organized by the Aplastic Anemia and MDS International Foundation.
Beyond teaching, our faculty hold key leadership roles that are shaping the future of hematology: Dr. Nimer chairs the MDS Foundation Board; Dr. Sekeres chairs the ASH Treatment of Older Adults with Acute Myeloid Leukemia (AML) guidelines and serves as Associate Editor of the Journal of Clinical Oncology; Dr. Figueroa is Deputy Editor-in-Chief of Blood Neoplasia; and Dr. Alencar leads a National Cancer Institute (NCI)-
Fellows
First Year
Valentina Ardila, M.D.
Jose Forero, M.D.
Dan M. Kaplan, M.D.
Asad Rauf, M.D.
Second Year
Akshee Batra, M.D.
Robert Briski, M.D.
Michael Durante, M.D., Ph.D.
Samantha El Warrak, M.D.
Ernest Philon, D.O.
Daniel Tuerff, M.D.
Third Year
Ali Al Sbihi, M.D.
Palash Asawa, M.D.
Chinmay Jani, M.D.
Traci King, M.D.
Amrit Paudel, M.D.
sponsored cooperative group trial. In addition, hematology faculty also hold committee and leadership positions on seven ASH committees, as well as on committees within the American Society of Clinical Oncology (ASCO) and the American Association for Cancer Research (AACR).
Taylor, M.D. with mentee Allison Cool, winner of the best overall award for her poster “Understanding Resistance to Bruton’s Tyrosine Kinase Degraders” in the Basic and Translational Research category at the Department of Medicine’s 11th Annual Eugene J. Sayfie, M.D. Research Day.
This year, we embraced bold steps to measure, expand, and truly understand the reach of our work across patient care, research, education, and community engagement. Our pursuit of redefined impact is evident in every corner of our work, whether it is improving patient flow, refining care delivery models, or creating equitable pathways for better health outcomes. By integrating real-time analytics into our decision-making, we are translating data into meaningful change for our patients, learners, and community. Our hospitalists have resumed staffing the Jackson Memorial Hospital Resident Procedures Team, ensuring hands-on procedural training and mentorship for the next generation of hospitalists. The division initiated a monthly morbidity and mortality conference to review complex patient cases, fostering open dialogue and sharing of insights and evidence-based best practices among our providers. We also developed new inpatient teams to provide coordinated co-management services in partnership with specialists, enhancing multidisciplinary collaboration and patient care.
Our faculty provided critical coverage for the Jackson Resident Procedures Team, supporting hands-on training and ensuring that learners receive high-quality procedural experience in a safe, supervised environment.
We also proudly represented the division at the Society of Hospital Medicine Conference in Las Vegas, Nevada, where we shared our innovations, engaged with national leaders, and brought back best practices to strengthen our clinical, academic, and operational initiatives. These experiences enhance professional development while
reinforcing our commitment to being at the forefront of hospital medicine on a national stage.
In FY25, our division successfully onboarded 18 new hospitalists, integrating them seamlessly into our team and strengthening our ability to deliver exceptional care to the diverse patient population we serve across South Florida and beyond. This growth reflects more than an increase in numbers; it represents a strategic investment in expanding our reach and deepening our expertise.



Marcio Rotta Soares, M.D.
Division Chief
Associate Professors of Clinical Medicine
Armen Henderson, M.D.
Efren Manjarrez, M.D.


Assistant Professors of Clinical Medicine
Candido Anaya, M.D.
Rafael Enrique Hernandez Oquet, M.D.
Joshua Laban, M.D.
Ahmed Luqman, M.D.
Vijay Mehta, M.D.
Maria Antonietta Mosetti, M.D.
Andrew Para, M.D.
Sayari Patel, M.D.
Sebastian Suarez Zarate, M.D.
Kyle Sutherland, M.D.
Pulkit Taunk, M.D.
Rachel Werne, M.D.
Harry Wine, M.D.
Staff Physicians
Alberto R. Arancibia, M.D.
Scott Berger, M.D.
Erica Corredera, M.D.
Nia Feaster, M.D.
Daniel Franco, M.D.
Rafael Garces, M.D.
Lucas Lages, M.D.


During the Hospitalist Day celebration, Division Chief Marcio Soares, M.D., presented awards to Liana Woodley-Pearson, M.D. (top left), Hospitalist of the Year; Carla Molliner, PA-C (top right), APP Rookie of the Year; Pulkit Taunk, M.D. (bottom left), Innovator of the Year; and Laura Traini-Mongelli, D.N.P., A.P.R.N. (bottom right), Hospital Educator of the Year.
Roselande Marcellon, M.D.
Taaha Mendha, M.D.
Hermes Milanes, D.O.
Samantha Milanes, D.O.
Bipte Modi, M.D.
Deepak Mummidavarapu, M.D.
Aldo Pavon Canseco, M.D.
Yelyzaveta Prysyazhnyuk, M.D.
Reubender Randhawa, M.D.
Zakia Rauf, M.D.
Michael Rodriguez, M.D.
Allan Rubinfeld, M.D.
Ayesha Saad, M.B.B.S.
Jonathan Salter, M.D.
Ankita Saxena, M.D.
Juan Serralles Allongo, M.D.
Pamela Trotter, M.D.
Gilberto Velazco, M.D.
Liana Woodley-Pearson, M.D.
Jessica Zuleta, M.D.
and
sharing their posters at the Department of Medicine’s 11th Annual Eugene J. Sayfie, M.D. Research Day.
Our division has experienced rapid growth in our clinical enterprise. We have focused on recruiting top talent and strengthening leadership roles within the Miller School of Medicine.
This year, Shaoli Chaudhuri, M.D., joined our faculty as Assistant Professor of Clinical Medicine. She pursued resident and fellowship training at Columbia University Medical Center and Mount Sinai Hospital, where she distinguished herself through rigorous clinical practice and a commitment to advancing medical knowledge. Dr. Chaudhuri joins our growing general infectious diseases and continuity care service lines.
Our General Infectious Diseases (ID) practice within the Multidisciplinary Clinic at the University of Miami Hospital and Clinics delivered care to more than 2,600 patients this year, reflecting our commitment to comprehensive, patient-centered services. With more than 6,000 clinical encounters to date, we are expanding our team by adding two new faculty members to meet growing demand and uphold our high standards of care.
Our HIV care service line also demonstrated significant growth, achieving over 2,500 patient encounters—a 7% increase from the previous year. This expansion reflects our commitment to delivering consistent, ongoing care while adapting to the changing needs of our patients.
Notably, Dushyantha Jayaweera, M.D., who has served as a dedicated faculty member for more than 30 years, was honored with the 2025 Department of Medicine’s Humanism in Medicine Award in recognition of his exceptional contributions and commitment to patient care and community service.
Our division spearheads innovative research initiatives that generate meaningful impact within our field and beyond.
Susanne Doblecki-Lewis, M.D., M.S.P.H., Division Chief, received a $3.6 million, multi-year R01 to explore effective social network strategies for HIV prevention across Miami-Dade County. Dr. Doblecki-Lewis evaluates

and leverages the influence of trusted relationships to increase HIV self-testing and knowledge about HIV treatment and prevention.
Ricardo Franco, M.D., received a grant from the Center for Disease Analysis Foundation (CDAF) to systematically locate diagnosed-butuntreated (DBU) individuals for hepatitis infections and to connect these patients to care. The Re-Link Project aims to provide evidence of practical and costeffective practices to reduce hepatitis B and C rates in the community.
Maria Alcaide, M.D., has demonstrated outstanding leadership as both a clinician and researcher, providing scientific and administrative oversight for numerous multidisciplinary studies addressing HIV and other emerging infections in the US and internationally. She has served as principal investigator on multiple National Institutes of Health (NIH)-funded projects. This year, Dr. Alcaide was appointed Interim Vice Provost for Research and Scholarship, reflecting her continued commitment to advancing research excellence. Additionally, she received

UHealth Director of Infection Control and Antimicrobial Stewardship Bhavarth Shukla, M.D., with Tanira Ferreira, M.D., C.M.O. of UMHC, at the 2025 Scientific Meeting on Candida auris, June 2025.

Susanne Doblecki-Lewis, M.D., M.S.P.H.
Division Chief
Professors
Maria Alcaide, M.D.
Gordon Dickinson, M.D. (Emeritus)
Margaret Fischl, M.D.
Michael Kolber, M.D.
Mario Stevenson, Ph.D.
Hansel Tookes, M.D.
Professors of Clinical Medicine
Lilian Abbo, M.D.
Gio Baracco, M.D.
Jose Castro, M.D.
Susanne Doblecki-Lewis, M.D., M.S.P.H.
Dushyantha Jayaweera, M.D.
Paola Lichtenberger, M.D.
Michele Morris, M.D.
Allan Rodriguez, M.D.
Associate Professors of Clinical Medicine
Shweta Anjan, M.D.
Folusakin Ayoade, M.D.
the 2025 Andrew Schally Distinguished Investigator Award.
In Fall 2024, we opened the Infectious Diseases Research Unit (IDRU) in the Converge Miami Building, a milestone that advances our research mission. This state-of-the-art, 3,000-square-foot facility expands our capacity for federally funded clinical and implementation science research, as well as clinical trials serving MiamiDade County.
Our American College of Graduate Medical Education (ACGME)accredited Infectious Diseases Fellowship Program prepares the next generation of scholars, educators, and clinicians. Led by Paola Lichtenberger, M.D., and Jose Castro, M.D., it trains 10 general ID fellows and two transplant ID fellows each year. We are advancing innovation through the 2025 Miami ID Symposium, five fellow presentations at IDWeek, and a new monthly conference with the Department of Orthopedics on complex bone and joint infections.
Laura Beauchamps, M.D.
Catherine Boulanger, M.D.
Jose Camargo Galvis, M.D.
Ricardo Fonseca Franco, M.D.
Yoichiro Natori, M.D.
Isabella Rosa-Cunha, M.D.
David Serota, M.D.
Bhavarth Shukla, M.D.
Jacques Simkins-Cohen, M.D.
Candice Sternberg, M.D.
Stephen Symes, M.D.
Assistant Professors of Clinical Medicine
Julia Bini Viotti, M.D.
Shaoli Chaudhuri, M.D.
Teresa Chueng, M.D.
Michael Gelman, M.D.
Chris Mark Lopez, M.D.
Alexis Powell, M.D.
Mohammed Raja, M.D.
Antoine Salloum, M.D.
Aasith Villavicencio Paz, M.D.
Research Assistant Professor Mark Sharkey, Ph.D. Fellows
First Year
Maha Albukhari, M.D.
Heli Gandhi, M.B.B.S .
Lynda Ostermann, M.D.
Nasser Rizvi, M.D.
Raymond Smith, M.B.B.S.
Second Year
Madiha Ahmed, M.D.
Jason Victor Chavez, M.D.
Tara Herrera, M.D.
Deborah Jimenez, M.D.
Sudiksha Sethia, M.B.B.S Infectious Diseases Transplant Fellows
Maryam Abul, M.B.B.Ch
Joseph Berger, M.D.
Michelle Gonzalez, M.D.

The division hosted its inaugural Scientific Meeting on Candida auris Symposium at the University of Miami Shalala Center, led by Bhavarth Shukla, M.D., Associate Professor of Clinical Medicine and Director of Infection Control and Antimicrobial Stewardship at UHealth. The event brought together leading scholars, clinicians, and learners to share insights and discuss the latest advances in C. auris, an emerging fungal pathogen challenging hospitals worldwide.
We also welcomed the Bisno family for the Bisno Endowed Speaker Series, with Madeleine W. Cunningham, Ph.D., from the University of Oklahoma Health Sciences Center, presenting on the sequelae of Group A streptococcal infections. In honor of Thomas Hoffman, M.D., and Kenneth Ratzan, M.D., Sandra Nelson, M.D., of Massachusetts General Hospital and past president of the Musculoskeletal Infection Society, spoke on the evolving challenges of periprosthetic joint infections.
The Division of Internal MedicinePediatrics continues to redefine impact by integrating community engagement into every aspect of its mission: deliver high-quality care while promoting community health.
Faculty-led initiatives included Stronger than the Storm, a hurricane preparedness event for families of children with complex medical needs, held in Miami and Culebra, Puerto Rico. Led by Kendra Van Kirk, M.D., Anjali Saxena, M.D., and Chadwick
Flowers, M.D., this effort was conducted in partnership with Holtz Children’s Hospital Pedi Pals and Golden Hearts PPEC, and included registration with Miami-Dade County’s Emergency and Evacuation Assistance Program.
Dr. Van Kirk also collaborated with the Overtown Youth Center to provide sports physicals and screenings for underserved youth. Additionally, the division partnered with Honeycomb House to educate families and conduct mental health screenings in Liberty City and Little Haiti, with a focus on


teen dating violence prevention and hurricane readiness.
Tiffani Houston, M.D., is leading a maternal health study in collaboration with UHealth Obstetrics and Honeycomb House, investigating the relationship between environmental exposure, the vaginal microbiome, and pre-eclampsia. Her team is working to identify early disease markers among women living near bisphenol A (BPA) contamination sites, with the goal


of developing screening tools that address maternal health inequities.
Through the Global Institute, Dr. Gonzalez leads resilience-building efforts in Guánica, Puerto Rico, a community affected by environmental contamination. In collaboration with Naresh Kumar, Ph.D., of the Department of Public Health Sciences and the Environmental Protection Agency (EPA), her research supports health initiatives, education campaigns, and policy change. This summer, students from Guánica visited Miami to participate in science and art activities with local marine biologists and researchers.
Under the leadership of Bryan Leyva, M.D., the four-year Med-Peds LEAD Program continues to prepare residents to become leaders in health equity. The program emphasizes leadership, advocacy, and health systems skills
through mentorship and hands-on projects.
Tobenna Ubu, M.D., inspired local elementary school students by participating in Howard Drive Career Day, modeling leadership and community engagement. Jonathan Tolentino, M.D., advanced LGBTQ+ advocacy through educational outreach, including podcasts and campus initiatives.
Stefanie Brown, M.D., M.B.A., and Madeline Mlynczak, M.D., played a pivotal role in launching the inaugural meeting of the newly formed Association of Med-Peds Physicians, helping to shape the national vision for the specialty. Through these efforts, the division continues to build bridges between patients, communities, and future physician-leaders by advancing health equity both locally and nationally.


Stefanie Brown, M.D., M.B.A. Division Chief
Associate Professors of Clinical Medicine
Stefanie Brown, M.D., M.B.A.
Victor Cueto, M.D.
Jonathan Tolentino, M.D.
Assistant Professors of Clinical Medicine
Christina DeBenedictus, M.D.
Chadwick Flowers, M.D.
Samantha Gonzalez, M.D.
Tiffani Houston, M.D.
Matthew Imm, M.D.
Bryan Leyva, M.D.
Anjali Saxena, M.D.
Kendra Van Kirk, M.D.
Staff Physicians
Madeline Mlynczak, M.D.
Tobenna Ubu, M.D.

discussing hurricane preparedness with families in Little Haiti, Miami.
The Division of Medical Oncology is proud to highlight many exciting accomplishments, changes, and initiatives in clinical care during FY2025. These achievements are driven by our dedicated providers who work tirelessly for our communities and take bold steps to expand access and innovation.
The division grew significantly with the addition of three new clinical providers: Cindy Pabon, M.D., Priscilla Barreto-Coelho, M.D., and Emanuela Palmerini, M.D., Ph.D. In addition, clinical services were expanded to Sylvester Comprehensive Cancer Center’s Kenneth C. Griffin Cancer Research Building.
The division continues to maintain strong research funding. Lynn Feun, M.D., and his team secured funding for a Phase II, single-arm study of tebentafusp combined with radioembolization in the treatment of metastatic uveal melanoma (sponsored by Immunocore) as well as for the Sylvester Comprehensive
Cancer Center Clinical Trial Acceleration Grant evaluating regorafenib and yttrium-90 (Y-90) radioembolization for unresectable hepatocellular carcinoma.
In the past year alone, more than 150 clinical trials were opened at the Plantation location, bringing innovative treatment options closer to where patients live. This commitment has already led to more than 80 patients enrolling in studies at the Plantation site, reinforcing Sylvester’s mission to reduce the burden of cancer. As Jonathan Trent, M.D., Ph.D., noted: “Clinical trials are the backbone of advancing cancer treatment, offering patients access to the most innovative therapies available.”
Richa Dawar, M.D., and Gilberto Lopes, M.D., M.B.A., F.A.S.C.O., led the first-ever randomized trial comparing different platforms for liquid biopsy in advanced non-small cell lung cancer. Results showed that adding circulating tumor ribonucleic acid (RNA) increased detection of treatment-targeted fusions by 30%, establishing a new standard in liquid biopsy for lung cancer.
In September, Erin Kobetz, Ph.D.,

M.P.H., announced a new community partnership with ZERO Prostate Cancer, a national nonprofit dedicated to ending prostate cancer and supporting those affected by the disease. ZERO’s work in research and patient support aligns closely with our mission to bring meaningful change to our community.
Under the leadership of Dionysios Watson, M.D., Ph.D., the Bayik and Watson laboratories now mentor three Ph.D. students, one M.D./Ph.D. student, and three postdoctoral fellows. During FY25, Dr. Watson also hosted more than 10 undergraduate, graduate, and medical students for research rotations.
Carmen Calfa, M.D., launched a new initiative where a team of clinical colleagues actively engages with the community – both in person and via social media – on topics such as cancer prevention, genetics, research, clinical trials, and survivorship. A key feature of this effort is a weekly Instagram Live series co-hosted by Dr. Calfa and Tracy Millgram, founder of BRCA Strong. Tracy Crane, Ph.D., R.D.N.,

and Dr. Calfa alternate hosting duties, regularly inviting Sylvester scientists to participate as guests. Dr. Kobetz’s team has also been actively involved in supporting this initiative.
As a board member of the Union for International Cancer Control (UICC), Dr. Lopes led the proposal and successful adoption of a landmark resolution on lung health at the 78th World Health Assembly (WHA) in May 2025. Titled “Promoting and Prioritizing an Integrated Lung Health Approach,” the resolution highlights the urgent need to address respiratory diseases and their major risk factors, including air pollution and tobacco use. It seeks to strengthen national and global efforts to prevent, diagnose, and manage common lung conditions such as asthma, chronic obstructive pulmonary disease (COPD), lung cancer, pneumonia, and tuberculosis.
Leonel Hernandez-Aya, M.D., was promoted to Associate Professor of Clinical Medicine.
Jaime Merchan, M.D., successfully opened the new Experimental Therapeutics Clinic at the Griffin Clinical Research Building, now home to the Phase I Program. He also secured a successful renewal of the K12 Calabresi Career Development Award from the National Cancer Institute.

Faculty, staff and learners on a team outing.

Gilberto Lopes, M.D., M.B.A., F.A.S.C.O.
Division Chief
Professors
Bach Ardalan, M.D.
Pasquale Benedetto, M.D.
Lynn Feun, M.D.
Erin Kobetz, Ph.D.
Marc Lippman, M.D. (Emeritus)
Jaime Merchan, M.D.
Stephen Richman, M.D. (Emeritus)
Jonathan Trent, M.D., Ph.D.
Professors of Clinical Medicine
Marijo Bilusic, M.D., Ph.D.
Gina D’Amato, M.D.
Peter Hosein, M.D.
Judith Hurley, M.D.
Gilberto Lopes, M.D.
Jose Lutzky, M.D.
Research Professors
Emanuela Palmerini, M.D., Ph.D.
Niramol Savaraj, M.D.
Associate Professor
Tracy Crane, Ph.D.
Associate Professors of Clinical Medicine
Carmen Calfa, M.D.
Aman Chauhan, M.D.
Leonel Hernandez-Aya, M.D.
Chukwuemeka Ikpeazu, M.D.
Alejandra Perez, M.D.
Catherine Welsh, M.D.
Research Associate Professor
Natasha Solle, Ph.D.
Assistant Professor
Dionysios Watson, M.D.
Assistant Professors of Clinical Medicine
Priscila Barreto Coelho, M.D.
Emily Jonczak, M.D.
Lawrence Negret, M.D.
Coral Olazagasti, M.D.
Cindy Pabon, M.D.
Agustin Pimentel, M.D.
Pearl Seo, M.D.
Janaki Sharma, M.D.
Gretel Terrero, M.D.
Frances Valdes-Albini, M.D.
Luis Villa, M.D.
Research Assistant Professor
Akina Natori, M.D.
Instructor
Rui Gong, Ph.D.
Staff Physicians
Steven Bialick, M.D.
Marcelo Blaya, M.D.
Richa Dawar, M.D.
Milena Elimelakh, M.D.
Nkiruka Ezenwajiaku, M.D.
Elisa Krill Jackson, M.D.
Vinay Minocha, M.D.
Raja Mudad, M.D.
Joseph Pizzolato, M.D.
Estelamari Rodriguez, M.D.
Rakesh Singal, M.D.
Jose Carlos Suarez, M.D.
Fellows
First Year
Valentina Ardilla M.D.
Derek Essegian, M.D.
Jose Forero, M.D., Ph.D.
Dan M. Kaplan, M.D.
Asad Rauf, M.D.
Second Year
Akshee Batra, M.D.
Robert Briski, M.D.
Michael Durante, M.D.
Samantha El Warrak, M.D.
Ernest Philon III, D.O.
Daniel Tuerff, M.D.
Third Year
Ali Al Sbihi, M.D.
Palash Asawa, M.D.
Chinmay Jani, M.D.
Traci King, M.D.
Amrit Paudel, M.D.
The Division of Myeloma has solidified its position as one of the nation’s top three programs in multiple myeloma, distinguished by excellence in clinical care, innovative therapies, and a strong research-clinical interface. The division delivers comprehensive, patientcentered care and is recognized for expertise in modern chemotherapyfree combination therapies based on novel small molecules, as well as immune-based treatments including bi-specific and tri-specific antibodies, chimeric antigen receptor (CAR) T-cell therapy and emerging messenger ribonucleic acid (mRNA)-based strategies.
In 2025, more than 36,000 individuals were diagnosed with multiple myeloma in the U.S., with

Florida reporting the highest number of new cases – over 3,700. Given the availability of many new and effective therapies but no established cure, prevalence continues to rise. In 2025, more than 180,000 individuals were living with the disease in the U.S., including more than 18,000 in Florida.
In addition to advancing treatment innovation and maintaining excellence in care, the division prioritizes easy patient access. Currently, Dickran Kazandjian, M.D., and C. Ola Landgren, M.D., Ph.D., practice at the Lennar Foundation Medical Center in Coral Gables, while Ben Diamond, M.D., Abhishek Pandey, M.D., and James Hoffman, M.D., see patients at the new Griffin Clinical Research Building and at Sylvester Comprehensive Cancer Center in downtown Miami. Dr. Hoffman also maintains a clinic in Deerfield. In fall 2025, the division will expand its clinical footprint north of Miami, with Gil Hevroni, M.D., opening a clinic at UHealth Doral and Rafat Abonour, M.D., opening a clinic at UHealth SoLé Mia.
Throughout the year, the Sylvester Myeloma Institute leads several well-attended lecture programs and conferences for physicians. All content is developed by Institute faculty and lectures cover both science and clinical care.
Last summer, the division launched a freestanding inpatient service at UHealth Tower, ensuring the same level of specialist care for multiple myeloma patients in both outpatient and inpatient settings. Outpatient faculty, together with laboratory-based physician-scientist David Coffey, M.D., provide coverage for the inpatient myeloma service alongside myelomadedicated inpatient advanced practice registered nurses (APRNs). These expansions reflect the growing demand for myeloma specialist care, particularly in Florida.
The division maintains a cuttingedge research program through the Sylvester Myeloma Institute, led by world-renowned physician-scientist and founding director Dr. Landgren. The Institute serves as the hub for myeloma-focused research at the University of Miami, built on the core values of excellence, innovation, and teamwork. Its mission is to accelerate breakthroughs in multiple myeloma through advanced clinical trials, translational research, computational innovation, and precision medicine – while training the next generation of leaders, fostering wellness, and delivering world-class patient care.

Research efforts include Dr. Landgren, internationally recognized for pioneering translational research and curativeintent therapeutic approaches; Dr. Kazandjian, leading investigatorinitiated trials and early-phase drug development; Dr. Hoffman, directing innovative clinical trials in light-chain amyloidosis and other plasma cell disorders; Dr. Diamond, conducting genomic studies uncovering molecular drivers of resistance; Dr. Coffey, exploring how the immune system contributes to sustained MRD negativity; Abhishek Pandey, M.D., a Sylvester K12 Scholar (2025–2027), launching computational oncology studies examining microbiota, immunity, and diet to optimize patient outcomes; and Brian Walker, Ph.D., who joined the faculty in spring 2025, bringing internationally recognized expertise in genomics, epigenetics, and functional biology to develop novel therapeutic strategies targeting tumor signaling pathways.
The Sylvester Myeloma Institute provides patients with access to Phase I and Phase II clinical trials of firstin-class therapies, while selectively participating in pivotal Phase III trials to influence global standards of care. Currently, the division has more than 25 open clinical trials for patients with multiple myeloma, available at all our
clinical sites to ensure broad access to the latest treatments.
The program also emphasizes survivorship and quality of life. In collaboration with Sylvester’s Cancer Control Program, it integrates wellness, nutrition, mental health, and lifestyle interventions into myeloma care, reflecting a holistic, patient-centered philosophy.
Additionally, the division is building an Artifical Intelligence (AI)/ Computational Myeloma Core to integrate predictive modeling into clinical decision-making and expand collaborations with industry partners in smart monitoring and data analytics. These initiatives further establish Miami as a global hub for myeloma innovation.
Education remains central to the division’s mission. Our Advanced Clinical Myeloma Fellowship and Computational/Translational Fellowship programs provide specialized training for the next generation of myeloma leaders. Plans are also underway to launch an International Myeloma Scholars Program to foster global training exchanges and collaboration.
The division and the Myeloma Institute continue to host annual international symposia in Miami, bringing together leading experts in

C. Ola Landgren, M.D., Ph.D. Division Chief
Professor
C. Ola Landgren, M.D., Ph.D.
Brian Walker, Ph.D. (Pending Rank)
Professor of Clinical Medicine
Rafat Abonour, M.D.
Dickran Kazandjian, M.D.
Associate Professor of Clinical Medicine
James Hoffman, M.D.
Assistant Professors of Clinical Medicine
David Coffey, M.D.
Benjamin Diamond, M.D.
Gil Hevroni, M.D.
Abhishek Pandey, M.D.
myeloma research, precision medicine, and clinical care. Faculty also actively mentor fellows, Ph.D. students, and postdoctoral trainees, providing them with robust exposure to both patient care and high-impact research.

The Katz Family Division of Nephrology and Hypertension continues to expand access to expert kidney care across South Florida, adding services at UHealth Doral and soon at UHealth SoLé Mia and Kendall. Our new Cardio-Renal Clinic at UHealth Tower delivers integrated care for patients with both heart and kidney conditions. The division offers comprehensive services for glomerular diseases, hypertension, polycystic kidney disease (PKD), nephrolithiasis, and transplantation, and is home to Florida’s only American Hospital Association (AHA)-certified Comprehensive Hypertension Center.
Under the leadership of Christopher Naranjo, D.O., the PKD Foundation Center of Excellence maintained its national designation and expanded community outreach. Key initiatives include launching an autosomal dominant polycystic kidney disease (ADPKD) registry, joining the ABBVCLS-628 trial, and partnering with the PKD-Free Alliance to broaden access to genetic testing and in vitro fertilization (IVF).
Under the leadership of Adriana Dejman, M.D., the division’s Home Dialysis Program remains the largest
peritoneal dialysis (PD) program in South Florida, with top-quartile urgentstart performance and embedded PD catheter placement. UM continues to exceed regional and national averages in home dialysis penetration (16.7%), PD starts (20.8%), and urgent starts (25.6%), underscoring our commitment to early intervention and patient choice.
From FY23 to FY25, new patient wait times dropped by 55%, while outpatient visits rose 11% and new visits increased 17% – a direct reflection of expanded clinics and our commitment to timely, accessible care.
Supported by the Katz Family Drug Discovery Center, faculty lead innovative projects such as a Phase I/II trial of REJUVXL™ cell therapy for chronic kidney disease (CKD), led by Yelena Drexler, M.D., and Alessia Fornoni, M.D., Ph.D. At the Department of Medicine’s 11th Annual Eugene J. Sayfie, M.D. Research Day, M.D./Ph.D. student Antonio Fontanella won the Clinical Vignette category, and Marco Ladino Avellaneda, M.D., received the 2025 Mentor Award.
Dr. Fornoni was elected Councilor of the American Society of Nephrology (ASN) and appointed Assistant Dean for

Research Training and Development as well as Director of UM’s Research Innovation and Scholarly Engagement (RISE) program. Sandra Merscher, Ph.D., and Alla Mitrofanova, Ph.D., continue to publish high-impact research and present internationally, advancing the understanding of glomerular disease, lipid metabolism, and podocyte biology.
Gabriel Contreras, M.D., M.P.H., collaborated on three peer-reviewed publications in high-impact journals –Lancet Rheumatology, The Journal of Rheumatology, and Lupus – serving as first author on two.
With Accreditation Council for Graduate Medical Education (ACGME) approval to expand to six fellows annually, our program – led by Zain Mithani, M.D., Dr. Drexler, and Dr. Ladino Avellaneda – has enriched training through Neph Madness Physiology Month, board review initiatives, Objective Structured Clinical Examinations (OSCE) Week, and innovative rotations. The Miami VA Healthcare System dialysis rotation, directed by Dr. Ladino Avellaneda, is progressing toward becoming the first AHA-certified Hypertension Center in the VA system nationwide.

Marie Anne Sosa, M.D., M.B.A.
Division Chief, Interim
Professors
Alessia Fornoni, M.D., Ph.D.
David Roth, M.D.
Under the slogan “For the Love of Kidneys: UMiami Walks Together,” TeamUM raised over $8,000 at the 2025 National Kidney Foundation Walk, earning the Community Award.
Patient Elizabeth Ramirez became the first person to undergo a fully robotic kidney/pancreas transplant at the Miami Transplant Institute.
Professors of Clinical Medicine
Gabriel Contreras, M.D.
Warren Kupin, M.D.
Mariella Ortigosa-Goggins, M.D.
Research Professor
Sandra Merscher, Ph.D.
Associate Professors of Clinical Medicine
Yelena Drexler, M.D.
Juan Duque, M.D.
Marco Ladino Avellaneda, M.D.
Adela Mattiazzi, M.D.
Zain Mithani, M.D.
Jair Munoz Mendoza, M.D.
Marie Anne Sosa, M.D.
Assistant Professors of Clinical Medicine
Shawn Alonso, D.O.
Franco Cabeza, M.D.
Adriana Dejman, M.D.
Gretchen Marrero, M.D.
Vinodh Mechery, M.D.
Christopher Naranjo, D.O.
Marie Anne Sosa, M.D., M.B.A., received both the 2025 Longitudinal Clinical Educator Award and the Faculty Mentor Award. Dr. Drexler was promoted to Associate Professor of Clinical Medicine, and Mariella Ortigosa-Goggins, M.D., was promoted to Professor of Clinical Medicine. Honored by graduating fellows, Dr. Naranjo was named Instructor of the
Javier Pagan, M.D.
Research Assistant Professor
Tali Elfassy, Ph.D.
Alla Mitrofanova, Ph.D.
Staff Physicians
Yanetsy Olivera Arencibia, M.D.
Fernando Pedraza Taborda, M.D. Fellows
First Year
Brooke Alexander, D.O.
Omar Asad, M.D.
Anna Feliszek, M.D.
Mihad Omer, M.D.
Aakash Padodora, M.D.
Second Year
Fabian Altamirano, M.D.
Elias Kima, M.D.
Saramarina Sanchez, M.D.
Satesh Saroop, D.O.
Glenda Sosa, M.D.
Eduardo A. Villa, M.D.
Year, while Vinodh Mechery, M.D., was recognized as Attending of the Year. Dr. Ladino Avellaneda was honored as an Overall Star in the Patient Experience Provider Recognition Program.
Warren Kupin, M.D., received the Miller School Medical Student Teaching Excellence Award for his outstanding contributions to medical education.

The Division of Pulmonary, Critical Care, and Sleep Medicine is at the forefront of harnessing big data to improve patient care, drive quality initiatives, and advance research. At a time when the ability to capture, analyze, and interpret vast datasets is reshaping medicine, our faculty are applying resources ranging from real-time intensive care unit (ICU) dashboards to large-scale genetic and proteomic databases. These efforts enable precision care today while laying the groundwork for tomorrow’s breakthroughs.
At the center of this work is the Data Analytic Research Team (DART), launched in late 2019 under the leadership of Tanira Ferreira, M.D., Chief Medical Officer, as part of UHealth Tower’s commitment to excellence in quality and safety. DART is now a cornerstone of the division’s big datadriven initiatives, fostering collaborations across hospital operations, clinical practice, and research.
DART advances patient care by uniting quality improvement with scholarship. Christopher Mallow,
M.D., in partnership with DART, has led the design of provider-specific ICU dashboards that benchmark key performance indicators—such as case mix index, length of stay, mortality, procedural volume, and intermediate care utilization—against peer groups. These dashboards deliver real-time feedback, enabling leaders to spot outliers and direct improvement efforts. Building on this success, Dr. Mallow is now developing ICU-specific dashboards that incorporate patient safety indicators, giving medical directors actionable tools to drive targeted quality initiatives.
Hayley Gershengorn, M.D., (Editorin-Chief, Chest Critical Care), has also leveraged DART’s infrastructure to conduct large-scale health services research. Using national hospital datasets, multi-system electronic health records (EHRs), and staffing surveys, she has examined variation in early rehabilitation among more than a million mechanically ventilated patients, assessed whether patientto-clinician workload ratios affect ICU mortality, and applied advanced

statistical techniques to define ICU staffing models nationwide. Her research extends to antimicrobial stewardship—showing that methicillinresistant Staphylococcus aureus (MRSA) nasal swab practices can shorten antibiotic courses in nearly 700,000 sepsis admissions—and to meta-research, including evaluations of double-blind peer review across thousands of manuscripts.
DART’s next leap forward will come from building the infrastructure to support even more complex and integrated analyses.
In partnership with the University of Miami’s Information Technology Department (UMIT), the division is developing a division-wide data farm capable of storing more than 100 terabytes of information.
This platform will unify diverse data sources –from advanced imaging such as single-photon emission computed tomography (SPECT), to national datasets like the National Health and Nutrition Examination Survey (NHANES), Osteoporotic Fractures in Men Study (MrOS), and the Sleep Heart Health Study, to local pulmonary function tests and sleep study results. A


Naresh Punjabi, M.D., Ph.D.
Division Chief
Professors
Franco D’Alessio, M.D.
Rachel Damico, M.D., Ph.D.
Robert M. Jackson, M.D.
Naresh Punjabi, M.D., Ph.D.
Roland M. Schein, M.D.
Adam Wanner, M.D.
Professors of Clinical Medicine
Michael A. Campos, M.D.
Alejandro Chediak, M.D.
Hayley B. Gershengorn, M.D.
Daniel H. Kett, M.D.
Andrew Quartin, M.D.
Shirin Shafazand, M.D.
Associate Professors
Trishul Siddharthan, M.D.
Associate Professors of Clinical Medicine
Alexandre Abreu, M.D.
Sixto Arias, M.D.
Elio Donna, M.D.
Tanira Ferreira, M.D.
Gregory Holt, M.D., Ph.D.
Diane Lim, M.D.
Christopher Mallow, M.D.
Andres Pelaez Freidel, M.D.
Juan Salgado, M.D. (Pending Rank)
Maria Tupayachi Ortiz, M.D.
Assistant Professors of Clinical Medicine
Brian Adkinson, M.D.
Saramaria AfanadorCastiblanco, M.D.
Kori Ascher, D.O.
Jonathan Auerbach, M.D.
Yaroslav Buryk, M.D.
Jorge Cabrera, D.O.
Oveimar De La Cruz, M.D.
Lisa Domaradzki, M.D.
Lesley Farquharson, M.D.
Hannah Ferenchick, M.D.
Juan Cesar Fernandez Castillo, M.D.
Brian Garnet, M.D.
Sergey Gerasim, M.D.
key asset will be a comprehensive sleep physiology archive, containing over a decade of overnight recordings from 10,000+ patients, capturing rich signals for research and innovation.
Even before launch, it has delivered benefits, supporting projects such as a National Institutes of Health (NIH) F32 award to Dipan Karmali, M.D., to study cardiopulmonary health in resourcelimited settings.
This robust data ecosystem will also power research programs operating at the molecular and genetic level.
Trishul Siddharthan, M.D., and Franco D’Alessio, M.D., are leading NIH-funded studies combining genetic, proteomic, and clinical data from more than 750,000 participants to define
Daniel Gorman, M.D.
Adhiraj Gosine, M.D.
Eric Lang, M.D.
Yoslay Perez, M.D.
Andrea Shioleno, M.D.
Waleed Sneij, M.D.
Rene Rico Tresgallo, M.D.
Susan Vehar, M.D.
Martin Zak, M.D.
Research Assistant Professor
Phabiola Herrera Aldana, M.D.
Jose Herrera Alvarez, Ph.D.
Instructors
MaryKathryn Hurst, D.O.
Dipan Karmali, M.D.
Romy Rodriguez Ortega, M.D.
Staff Physicians
Sama Al-Bayati, M.D.
Ankur Aneja, M.D.
Hyasil Gonsalves-Barriero, M.D.
Gregory Millio, M.D.
Ryan Mocerino, M.D.
Hemal Parekh, M.D.
Bianca Sarmento, M.D.
Jeffrey Scott, D.O.
Jeany Villamizar, M.D.
Fellows
Pulmonary Critical Care Medicine
First Year
Mohamed Alghizzawi, M.D.
Alexandria Clarke, D.O.
a genetically and immunologically distinct type 2 inflammation (T2-high) chronic obstructive pulmonary disease (COPD) endotype.
By developing a pathway-specific polygenic risk score focused on key T2 signaling genes, paired with highthroughput cytokine profiling from deeply characterized COPD cohorts, their work is mapping how inherited risk interacts with inflammatory biology to influence outcomes.
The data farm will provide the computational capacity, secure storage, and integrated datasets needed to expand this research, enabling cross-linkages with imaging, environmental exposures, and longitudinal clinical data.
Abraham Leiser, M.D.
Abaigael Madden, M.D.
Victor Perez, M.D.
Mariam Qazi, D.O.
Gizem Reyhanoglu, D.O.
Hassan Shakir, M.D., M.B.B.S.
Carlos Valladares, M.D.
Ibrahim Zahid, M.B.B.S.
Second Year
Nulma Carguill, M.D.
Kareem Eid, M.D.
Fredy Huertero, M.D.
Claudia Marcano, M.D.
Deborah Mi, M.D.
Yaisa Moreno Hernandez, M.D.
Katarina Pitka, M.D.
Third Year
Felipe De Andrade Arnaud, M.D.
Farhad Ghamsari, M.D.
Matthew Edward Hodge, D.O.
Eduardo A. Lopez Gonzalez, M.D.
Kelly O’Boyle, M.D.
Lauren Michele Pascual, M.D.
Guil Rozenbaum Lerner, M.D.
Lee Seifer, M.D.
Sleep Medicine
Ivan Escalona Puig, M.D.
Emma Lipshultz, M.D.
Ila Snigdha, D.O.
The division is committed to training the next generation of physicians and scientists in applying big data to advance clinical care and research. Through hands-on participation in projects such as ICU dashboards and large-scale data analyses, trainees gain experience with cutting-edge tools and methodologies. By integrating real-time clinical data with research and quality improvement initiatives, the division is creating a rich learning environment that equips future leaders to navigate and shape the evolving landscape of data-driven medicine.
The Division of Rheumatology and Immunology experienced significant growth this year with the addition of Alexis Katz, D.O., who joined as a staff physician in October, expanding our outreach to Boca Raton and Coral Springs. New faculty members Jose P. Garcia, M.D., and Ami Purohit, M.D., will further strengthen our presence in Kendall, Coral Gables (Lennar), and at our newest location, UHealth SoLé Mia.
In FY25, Cecilia Chung, M.D., M.P.H., and her lab team led innovative research using big data and real-world evidence to improve outcomes for patients with rheumatic diseases. Funded by agencies such as the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and the U.S. Department of Veterans Affairs (VA), her research explores drug
safety, pharmacogenomics (how genes influence response to drugs), cardiovascular risk, and environmental factors linked to conditions including rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE).
Over the past year, Dr. Chung and her team of research staff, rheumatology fellows, and medical students published numerous peerreviewed articles and presented their work at major conferences, including ACR Convergence, the annual meeting of the American College of Rheumatology (ACR).
This past year, our fellows and residents continued to excel in education, scholarship, and professional

development. Many presented research at prominent conferences, reflecting the depth and quality of work within our division. At the ACR Convergence meeting, first-year fellows and third-year residents delivered multiple poster presentations highlighting innovative clinical research with practical applications in rheumatology. Their work received strong recognition from peers and national leaders in the field. At the Florida Society of Rheumatology meeting, residents and fellows presented clinical research and case
studies and participated in interactive workshops, showcasing their academic rigor while fostering collaboration and networking within the state’s rheumatology community.
Carlos Lozada, M.D., was honored with the Pan-American Spirit Award at the Pan-American League of Associations for Rheumatology (PANLAR) annual meeting and is slated to receive a prestigious American College of Rheumatology (ACR) award at ACR Convergence 2025 in Chicago.

Left to right: Biology undergraduate student Daniela Chavez; resident Jose Cano, M.D.; fellow Sachalee Campbell, M.D.; and Dr. Chung at ACR Convergence 2024.


Cecilia P. Chung, M.D., M.P.H.
Division Chief
Professor
Cecilia Chung, M.D., M.P.H.
Professor of Clinical Medicine
Carlos J. Lozada, M.D.
Associate Professor of Clinical Medicine
Elaine C. Tozman, M.D.
Assistant Professors of Clinical Medicine
Maria F. Carpintero, M.D.
Kelly Corbitt, D.O.
Jose P. Garcia, M.D.
Research Assistant Professors
Estefania Quesada-Masachs, M.D., Ph.D.
Staff Physicians
Alexis Katz, D.O.
Fellows
First Year
Kevin Cai-Zhen, M.D.
Sachalee Campbell, M.D.
Second Year
Aakriti Alisha Arora, M.D.
Maria Intriago Williams, M.D.
Estefania QuesadaMasachs, M.D., Ph.D., presenting at Grand Rounds.
The Division of Transplantation and Cellular Therapy has continued to thrive over the past year, with faculty leading investigator-initiated and multi-site clinical trials, publishing in high-impact journals, securing competitive grant funding, and launching new patient initiatives.
This year, we again broke last year’s record by treating more patients with transplantation and cellular therapy than ever before. Cara Benjamin, Ph.D., Director of the Division’s Cellular Therapy Laboratory (CTL), successfully secured renewed accreditation from the Foundation for the Accreditation of Cellular Therapy (FACT) for the CTL. In addition, the clinical Transplant and Cellular Therapy Program earned a separate three-year FACT accreditation.
Under a pilot spearheaded by Denise Pereira, M.D., we reached a major milestone by treating our first chimeric antigen receptor (CAR) T-cell therapy patients in the outpatient
setting – an achievement made possible by the opening of our new outpatient acute treatment unit at Sylvester Comprehensive Cancer Center. We also expanded patient access beyond the main campus, with new clinics at Lennar, Doral, and Plantation.
Reflecting our active efforts to extend the benefits of cellular therapy to new indications, Lazaros Lekakis, M.D., treated Miami’s first autoimmune disease patient with CAR-T cells under a clinical trial. In addition, Amer Beitinjaneh, M.D., launched the BEAT MS trial, studying autologous stem cell transplantation versus standard-ofcare therapy for patients with relapsing multiple sclerosis.
This has been a remarkably productive year for our division. Our 11 faculty members published in leading journals including Journal of Clinical Oncology, Blood, Nature, Lancet, Lancet Hematology, Lancet Oncology, Nature Cancer, JAMA Oncology, Journal
of Clinical Investigation, Science Immunology, and the New England Journal of Medicine.
Division Chief Damian Green, M.D,. had two senior author publications in Blood reporting findings from firstin-human clinical trials of a B-cell maturation antigen (BCMA) CAR-T cell therapy that he helped to develop. Jay Spiegel, M.D., was co–first author on a Journal of Clinical Oncology paper from the U.S. Lymphoma CAR-T Consortium on standard-of-care axicabtagene ciloleucel for large B-cell lymphoma. He also opened an investigatorinitiated trial combining pirtobrutinib with brexucabtagene autoleucel in mantle cell lymphoma and, in collaboration with Dr. Lekakis, secured competitive Bankhead Coley funding to expand a promising trial integrating mosunetuzumab and polatuzumab with CD-19 CAR-T therapy.
Antonio Jimenez Jimenez, M.D., continues to play a national leadership role in matched unrelated donor transplantation. He has served as Network Transplant Center Chair on

three major multi-center clinical trials –ACCELERATE, ACCESS, and OPTIMIZE
– designed to improve outcomes for patients undergoing allogeneic stem cell transplantation. His focus on reducing toxicity associated with unrelated donor transplant is improving access to this life-saving procedure not only in South Florida but across the nation and internationally. His impact is reflected in his role as senior author on the multicenter Phase II ACCESS trial, published in the Journal of Clinical Oncology.
Meanwhile, Noa Holtzman, M.D., is advancing novel natural killer (NK) cell therapeutics through K12 grant support, and Trent Wang, D.O., is integrating innovative digital applications into R01-supported research to improve transplant outcomes. Dr. Beitinjaneh is running a Phase I CD4 CAR-T trial for patients with chronic myeloid leukemia (CML).
In the laboratory, Dr. Green, Erden Atilla, M.D., and Pinar Ataca-Atilla, M.D., are investigating mechanisms of resistance to cellular therapy and developing new therapeutics for acute myeloid leukemia (AML), multiple myeloma, and lymphoma. These efforts, supported by multiple National Institutes of Health (NIH) and foundational grants, highlight the division’s robust research portfolio.
Our faculty also presented data at major international conferences and delivered invited lectures across the globe, including Brazil, South Africa, Spain, Italy, and Turkey.
Finally, the entire clinical team collaborated with Maria Rueda-Lara, M.D. (Department of Psychiatry and Behavioral Sciences), to report on psychosocial correlates of failure to complete stem cell transplant in the diverse South Florida population.
We continue to train University of Miami Miller School of Medicine internal medicine residents and hematology/oncology fellows through both our inpatient service and outpatient clinics. In addition, Dr. Green, Dr. Benjamin, Dr. Atilla, and Dr. Ataca-Atilla provide laboratory research training for learners across the spectrum, including doctoral, medical, undergraduate, and even high school students. Mark Goodman, M.D., contributed as a NextGenMD facilitator, and Dr. Beitinjaneh leads our official TCT collaboration supporting fellows rotating from Broward Health Hematology Oncology and the Cleveland Clinic.
Beyond our commitment to trainees, the division has also engaged in a wide range of community and peer education events. These include lectures to diverse audiences such as the Ukrainian Ministry of Health, visiting Brazilian clinicians, the South African Clinical Hematology Society, Papanicolaou Corps for Cancer supporters, the Woman’s Cancer Association, the Bone Marrow Transplant Infonet, and the Society for Immunotherapy of Cancer (SITC) Advances in Cancer Immunotherapy Program, where we addressed longterm toxicities after CAR-T therapy.

Damian J. Green, M.D.
Division Chief
Professor
Damian Green, M.D. (Pending Rank)
Professors of Clinical Medicine
Amer Beitinjaneh, M.D.
Lazaros J. Lekakis, M.D.
Associate Professors of Clinical Medicine
Cara Benjamin, Ph.D.
Mark S. Goodman, M.D
Antonio M. Jimenez, M.D.
Denise L. Pereira, M.D.
Trent Wang, D.O.
Research Associate Professor
Eric Wieder, Ph.D.
Assistant Professors of Clinical Medicine
Noa Holtzman, M.D.
Jay Spiegel, M.D.
Research Assistant Professors
Pinar Ataca Atilla, M.D.
Erden Atilla, M.D.

1. UHealth Palm Beach Gardens 3401 PGA Boulevard, Suite 400 Palm Beach Gardens, FL 33410
2. UHealth Downtown West Palm Beach 185 Banyan Boulevard, Suite 200 West Palm Beach, FL 33401
3. UHealth Concierge Medicine Palm Beach 218 Royal Palm Way Palm Beach, FL 33480
4. UHealth Boca Raton 1489 W. Palmetto Park Road, Suite 400 Boca Raton, FL 33486
5. UHealth Fort Lauderdale 4800 N.E. 20 Terrace, Suite 201, Building C Fort Lauderdale, FL 33308
6. UHealth Plantation 8100 S.W. 10 Street Plantation, FL 33324
7. UHealth SoLé Mia 2111 SoLé Mia Way North Miami, FL 33181
8. UHealth Miami Beach 1045 5th Street, Suites 303 and 305 Miami Beach, FL 33139
9. UHealth Fisher Island 41214 Fisher Island Drive Miami, FL 33109
10. UHealth Jackson 1400 N.W. 12 Avenue Miami, FL 33136
11. UHealth Doral 8375 N.W. 53 Terrace Doral, FL 33166
12. UHealth LeJeune 351 N.W. 42 Avenue Miami, FL 33126
13. Lennar Foundation Medical Center 5555 Ponce de Leon Boulevard Coral Gables, FL 33146
14. UHealth Kendall 8932 S.W. 97 Avenue Miami, FL 33176
15. UHealth Pinecrest (Coming Soon) 13251 S. Dixie Highway Pinecrest, FL 33156
16. UHealth Palmetto Bay 15155 S.W. 97 Avenue, Suites 100 and 240 Palmetto Bay, FL 33176
1. Sylvester Coral Springs 8170 Royal Palm Boulevard, 1st Floor Coral Springs, FL 33065
2. Sylvester Deerfield Beach 1192 E. Newport Center Drive Deerfield Beach, FL 33442
3. Sylvester Fort Lauderdale 5700 N. Federal Highway, Suite 5 Fort Lauderdale, FL 33308
4. Sylvester Plantation 8100 S.W. 10 Street, 1st Floor Plantation, FL 33324
5. Sylvester Hollywood 3850 Hollywood Boulevard, Suite 1B Hollywood, FL 33021
6. Sylvester Aventura 2801 N.E. 213 Street, Suite 1101 Aventura, FL 33180
7. Sylvester Miami 1475 N.W. 12 Avenue, 1st Floor Miami, FL 33136
8. Sylvester Doral 8375 N.W. 53 Terrace Doral, FL 33166
9. Sylvester Kendall 8932 S.W. 97 Avenue Miami, FL 33176
10. Sylvester Naples 2390 9th Street North Naples, FL 34103
Bascom Palmer Eye Institute Locations in Miami-Dade, Broward, Palm
and Collier Counties
1. Bascom Palm Beach Gardens 7101 Fairway Drive Palm Beach Gardens, FL 33418
2. Bascom Plantation 8100 S.W. 10 Street, 3rd Floor Plantation, FL 33324
3. Bascom Palmer Eye Institute 900 N.W. 17 Street Miami, FL 33136
4. Bascom/Lennar Foundation Medical Center 5555 Ponce de Leon Boulevard Coral Gables, FL 33146
5. Bascom Naples 3880 Tamiami Trail North Naples, FL 334103
by
Top Divisions by Gift Dollars
Gifts by Designation
Top Divisions by Number of Donors
Julie and Martin Franklin said it “feels right” to commemorate the work of Julie’s father with a donation to the school he loved.
No matter how old you are, the loss of your father is something that changes your life forever.
The passing of Ronald Hinds, M.D., who was both a father and a noted orthopedic surgeon, is making an enormous difference at the University of Miami Miller School of Medicine through the establishment of an endowment in his memory.
The Julie and Martin Franklin Family Foundation has made a gift of $3.75 million to create the Dr. Ronald B. Hinds Department of Medicine Endowed Chair. A beloved orthopedic surgeon in Miami, Dr. Hinds passed away a year ago at the age of 89.
“I wanted to do something to honor my father, and it feels right to pay tribute to him and his memory at the University of Miami,” explained Julie Franklin, who grew up in Miami. “My

father loved Miami and the University and, to me and my husband Martin, the two are tied together like the roots of a tree from which all the branches grow.”
The newly established Dr. Ronald B. Hinds Department of Medicine Endowed Chair will support the research pursuits of a senior faculty member in the Department of Medicine at the Miller School.
“The incredibly generous gift from Julie and Martin Franklin will ensure in perpetuity the finest in scholarship and clinical accomplishment in the Department of Medicine,” said Roy Weiss, M.D., Ph.D., professor and chair of medicine, the Rabbi Morris I. Esformes Endowed Chair in Medicine and Endocrinology, and the Kathleen & Stanley Glaser Distinguished Chair at the Miller School. “The leader who will occupy this endowed chair will set the pace for excellence not only in this generation but for generations to come. He or she will be the role model clinician setting the highest of standards for all our faculty.”




born in the U.K. and is now a Miamibased businessman, the gift is a way to honor his late father-in-law and say thank you.
Dr. Bernal-Mizrachi
“We are very grateful to Dr. Roy Weiss for the first-class care he provided to me when I needed it,” said Franklin, who serves as chairman of Nomad Foods Limited, Element Solutions, Inc. and APi Group. “We know how important research is to move medicine forward, and we are delighted to support those efforts.”
For Julie and her mother, Miriam, the endowment honors a man who meant so much to so many.
Ernesto Bernal-Mizrachi, M.D., chief of the Division of Endocrinology at the Miller School, was recently appointed as the inaugural holder of the prestigious endowed chair.
For Sir Martin Franklin, who was
“My father was adored and beloved by all. He loved working with and helping people. He was as special as they come,” said Julie.
“My husband says it best: ‘He may have been short in stature, but after his passing, I realized how larger than life he really was.’”
“My father loved Miami and the University, and to me and my husband Martin, the two are tied together like the roots of a tree from which all the branches grow.”
University of Miami Leadership
Joseph J. Echevarria
President
Dipen J. Parekh, M.D. C.E.O. of UHealth, and E.V.P. for Health Affairs, University of Miami C.O.O. of UHealth
Henri R. Ford, M.D., M.H.A. Dean and Chief Academic Officer
Department Leadership
Roy E. Weiss, M.D., Ph.D. Chair
Anna Carol Herman-Giddens, R.N., B.S.N. Senior Administrative Officer
Rachel Damico, M.D., Ph.D. Vice Chair of Faculty Development and Diversity
Michael Kolber, M.D., Ph.D. Vice Chair for Clinical Affairs
Amar Deshpande, M.D. Vice Chair for Education
Ernesto Bernal-Mizrachi, M.D. Vice Chair for Research
Khemraj Hirani, Ph.D., M.B.A. Associate Vice Chair for Research Regulatory Compliance
Alejandro Chediak, M.D. CMO for DOM
Carlos Prieto Assistant Vice President, Clinical Operations
Rolando J. Briceno, M.B.A. Executive Director, Clinical Operations
Francisco Rodriguez
Executive Director, Clinical Operations
Ivelisse Rodriguez Executive Director, Finance
Laura J. Pinzón, M.B.A. Director, Administrative Operations
Lily Ferrer, M.B.A., C.R.A. Senior Director, Sponsored Research
Ali Ismail
Senior Director, Department Planning & Operations
Jannet Yern, B.S.A. Executive Director, Employee & Student Health Services
Yiannis S. Chatzizisis, M.D., M.P.H. Cardiovascular Medicine
Richard A. Preston, M.D., M.S.P.H., M.B.A. Clinical Pharmacology
Ernesto Bernal-Mizrachi, M.D. Endocrinology, Diabetes and Metabolism
Daniel A. Sussman, M.D., M.S.P.H (Interim)
Digestive Health and Liver Diseases
Sabrina Taldone, M.D., M.B.A General Internal Medicine
Marcio Soares, M.D. Geriatrics and Palliative Medicine
Mikkael A. Sekeres, M.D., M.S. Hematology
Marcio Soares, M.D. Hospital Medicine
Stefanie Brown, M.D., M.B.A. Internal Medicine-Pediatrics

Susanne Doblecki-Lewis, M.D., M.S.P.H. Infectious Diseases
Gilberto de Lima Lopes Junior, M.D., M.B.A. Medical Oncology
C. Ola Landgren, M.D., Ph.D. Myeloma
Marie Anne Sosa, M.D. (Interim) Katz Family Division of Nephrology and Hypertension
Naresh M. Punjabi, M.D., Ph.D. Pulmonary, Critical Care and Sleep Medicine
Cecilia Chung, M.D., M.P.H. Rheumatology and Immunology
Damian Green, M.D. Transplantation and Cellular Therapy
Division Administration
Aisa Campo Cardiovascular Medicine
Michelle Monteagudo Clinical Pharmacology
Cristina Calderon-Parra Endocrinology, Diabetes and Metabolism
Carol Cottrell
Digestive Health and Liver Diseases
Joanne Alonso, M.B.A. General Internal Medicine
Austin Ambrose Geriatrics and Palliative Medicine
Angelique “Gigi” Lima Hematology
Austin Ambrose Hospital Medicine
Gabriela Vargas Infectious Diseases
Joanne Alonso, M.B.A. Internal Medicine-Pediatrics
Monica Medero Medical Oncology
Nessreen Mestari Myeloma
Christina Villanueva Katz Family Division of Nephrology and Hypertension
Alexander Alvarez
Pulmonary, Critical Care and Sleep Medicine
Lisa Deschapell Rheumatology and Immunology
Nessreen Mestari
Transplantation and Cellular Therapy

