The Department of Otolaryngology/Head and Neck Surgery was again named the #1 Otolaryngology program in North Carolina. While these rankings are not what drive us, this external recognition of our excellence feels good as we strive to advance care for our patients, innovate and discover through research, and provide excellent and high-volume training for learners. With the leadership of our vice chairs, division chiefs, staff, and clinic leaders, I feel fortunate to head this group of outstanding faculty, staff, residents, and fellows.
As we look back on the last year, we are thankful that the UNC School of Medicine and UNC Hospitals are returning to normal following the tremendous disruption of COVID. However, there have been continuing challenges for clinical care, research, and education. Like all hospitals, we experienced severe staffing shortages over this last year, especially in the operating room. Additionally in the summer, several of our hearing researchers were seriously impacted by a flood in their labs followed by a prolonged period for rebuilding. Again and again, with each challenge we saw amazing resilience and dedication among our faculty, staff, and residents to meet the year’s challenges and exceed expectations for each of our missions. I stand in awe in reviewing the outstanding clinical and academic productivity that we achieved with year over year increases in clinic visits and operative case and groundbreaking and innovative research that will benefit our future patients.
This year brought transition in our education program leadership as after many years of service Program Director and Associate Program Directors, Drs. Buckmire, Shah, and Ebert stepped down transitioning to Dr. Drake in an interim role and subsequently to Drs. Thorp, Leeper, and DeMason as new Program and Associate Program Directors, respectively. We are incredibly grateful to all our education leaders for their past and current vision that has established and continues to improve a remarkable training experience for our residents. We are also incredibly grateful for an anonymous endowment that was donated to support our residents as they continue to excel.
We continue to serve the people of North Carolina by expanding access to care for patients with new clinics in Wake County. This year, we were extremely excited to initiate the
UNC Department of Otolaryngology ⁄ Head and Neck Surgery
22-23 Annual Report
construction of a mobile hearing and speech clinic that will provide much-needed service to the rural areas of our state beginning in 2024. On the research front, our faculty and learners are innovating and pushing knowledge boundaries with remarkable research discoveries, and our residents continue to be tremendously productive ranking among the highest nationally for academic output.
I hope that you enjoy this recap of Otolaryngology/Head and Neck Surgery at UNC, and that this annual report leads you to some new insights into our department and what drives these outstanding accomplishments. In concert with UNC School of Medicine, the UNC Medical Center and UNC Health, we will continue to provide the highest quality of care to patients as we innovate and advance care through research, outreach, and education.
Wendell G. Yarbrough, MD, MMHC, FACS
Thomas J. Dark Distinguished Professor and Chair
Department of Otolaryngology/Head & Neck Surgery
UNC School of Medicine







DEPARTMENT CHAIR
WENDELL G. YARBROUGH, MD, MMHC, FACS
OUTPATIENT OPERATIONS & IMROVEMENT
KEVIN D. BROWN, MD, PHD
EDUCATION
ROBERT A. BUCKMIRE, MD

INPATIENT OPERATIONS & IMROVEMENT
TREVOR G. HACKMMAN, MD, FACS
ACADEMICS & OUTREACH
BRENT A SENIOR, MD, FACS, FARS



FINANCE
AUSTIN S. ROSE, MD, MBA, FARS
RESEARCH
EMILY BUSS, PHD

FACULTY DEVELOPMENT
AMELIA F. DRAKE, MD, FACS
ADMINISTRATION (INTERIM ACA)
BLAIR ALLEN

CCIC LISA PARK, AUD
VOICE & SWALLOWING DISORDERS
ROBERT A. BUCKMIRE, MD
OTOLOGY⁄ NEUROTOLOGY & LATERAL SKULL BASE SURGERY
KEVIN D. BROWN, MD, PHD
HEAD & NECK SURGICAL ONCOLOGY
TREVOR G. HACKMAN, MD, FACS


GENERAL OTOLARYNGOLOGY
CHRISTINE E. DEMASON, MD
FACIAL PLASTIC & RECONSTRUCTIVE SURGERY

J. MADISON CLARK, MD, FACS

PEDIATRIC OTOLARYNGOLOGY
CARLTON J. ZDANSKI, MD, FAAP, FACS
RHINOLOGY, ALLERGY ENDOSCOPIC SKULL BASE SURGERY
BRENT A. SENIOR, MD, FACS, FARS

The Department of Otolaryngology strives to care for patients of all backgrounds in clinical, educational and research initiatives, as part of our mission to “improve the health of North Carolininans and others whom we serve.”
Planned projects to enhance access to care include the mobile unit to evaluate children with hearing loss. Our department also sponsors a leadership development course for women medical students. Led by Angelica Lackey and Theresa Ann Dickerson this year, the longitudinal course included lectures on “Personal Core Values” by Dr Erin Malloy of Psychiatry and “Professional Housekeeping” by Dr Alice Chuang, Associate Dean for Student Affairs.

The department also hosts a journal club which meets regularly to discuss issues of access to care as well as other workforce issues.
The LILAC (Learning in Leadership at Carolina) Longitudinal is a workshopbased leadership development program for women-identifying medical students. In March 2024, Dr Caprice Greenberg, Chair of the Department of Surgery, will speak on “Networking through Conferences “.


Another group within the department is the robust Women In Otolaryngology group, who meets on occasion to discuss issues relevant to being a woman otolaryngologist. The group includes all who wish to attend.
We are excited to announce that our new wellness liaison is Dr. Brian Jewett, who will lead wellness initiatives for the department. Dr. Jewett is a strong advocate for promoting wellness with patients, medical providers, students and trainees, and within the community. Wellness initiatives are anticipated to target all areas of wellness and well-being, and efforts will include a comprehensive and innovative approach aimed to establish our department as a strategic leader in this area.


Lisa Licht, RN, continues to shine as our staff wellness liaison. One successful initiative of hers this past year has been leading all staff in a two part compassion in the workplace training.

Ebony Walker, LPN, is also involved in department wellness by leading our staff in celebrating a variety of holidays and cultural events throughout the year.













TREVOR G. HACKMAN, MD, FACS
DIVISION CHIEF
FELLOWSHIP DIRECTOR
NATHANIEL & SHEILA HARRIS DISTINGUISHED PROFESSOR

WENDELL G. YARBROUGH, MD, MMHC, FACS
THOMAS J. DARK DISTINGUISHED PROFESSOR
JEFFERY M. BLUMBERG, MD, FACS
ASSOCIATE PROFESSOR

CATHERINE J. LUMLEY, MD
ASSISTANT PROFESSOR
TRAVIS P. SCHRANK, MD, PHD
ASSISTANT PROFESSOR
C. BLAKE SULLIVAN, MD
ASSISTANT PROFESSOR


Dr. Travis Schrank continues to explore the role of NF-kB in radiation resistance through his K08 award, and has developed a regional and national reputation for his expertise in head and neck cancer genomics, particularly HPV genomics with visiting lectureships across the country. He finishes the fiscal year with 10 publications, 4 first author.
Dr. Catherine Lumley has grown a reputation for excellence in cancer clinical care and reconstructive surgery since joining the department in 2019. She currently serves as Medical Director of the Head and Neck Oncology Clinic and leads our Head and Neck Community outreach, which supported a successful Head and Neck Cancer Awareness Screening Day


Dr. Jeffrey Blumberg leads the UNC microvascular surgery program, and is a nationally recognized leader in reconstructive surgery, particularly the use of the scapula system for complex chimeric reconstruction in the head and neck. He serves as associate director of the head and neck fellowship and supervising physician of our APP program. This past year Dr. Blumberg led a medical mission trip to Malawi to perform a needs assessment at the UNC Lilongwe facility, with plans to return to Malawi to perform surgery and share techniques and approaches with the goal of improving patient care at the global level and furthering UNC otolaryngology’s presence and impact within the international medical community.
Dr. Christopher “Blake” Sullivan completed a tremendous first year as faculty at UNC, bringing a new skill set to the head and neck team within the clinical and research realm.
His recent NCBD review “Time to treatment patterns of head and neck cancer patients before and during the Covid-19 pandemic. “ detailed the issues surrounding time to treatment and survival across the country.
Dr. Trevor Hackman serves as division chief and fellowship director for the UNC head and neck oncology program, as well as serving on the executive committee for the salivary section of the AHNS, and as an active member of the ethics, CDMS and quality committees for the AHNS. Dr. Hackman’s research spans QI, epidemiology, simulation and translation/trial research. This past year was highlighted by publication of a study demonstrating ability for his provisionally patented novel TORS simulator to discriminate between novice and experienced robotic surgeons, for which a subsequent training validation study has been performed. Within the institution, Dr. Hackman serves as a coach, mentor, faculty for Relational Leadership at Carolina and co-chair of the Medical Staff Physician Excellence Committee.
The incredible recovery story of Mr. Bell was highlighted on UNC's media circut! His tongue was treated on a cutting edge induction clinical trial that required expertise of UNC's multidisciplinary team. Mr. Bell's response decreased the amount of surgery and allowed him to avoid radiation thrapy which will greatly improve his speech and swallowing.
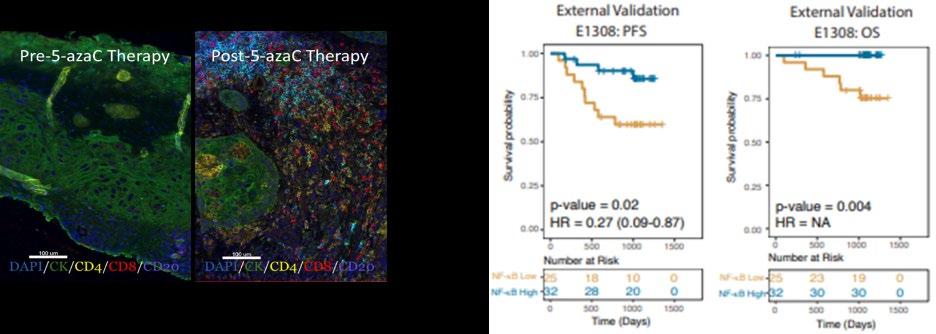
While the head and neck division actively advances research across various arenas of translational science, genomics, epidemiology, outcomes and quality improvement, this year we are especially proud of a few landmark and influential manuscripts. Dr. Wendell Yarbrough lab’s work “Non-canonical HPV carcinogenesis drives radio-sensitization of head and neck tumors” was recently published in the Proceedings of the National Cancer Institue (PNAC). This will be a landmark paper since it is the first to identify two subtypes of HPV+ Head and Neck Cancer, one with favorable and one with poor prognosis. It also describes a novel mechanism of HPV carcinogens and provides insight explaining why one subgroup has improved survival.
Also in the realm of cancer genomics, our group, led by one of our residents, Wesley Stepp MD, PhD, and K08-funded faculty, Travis Schrank, MD, PhD, published “Development of a Novel Molecular Test for Determining HPV Integration Status in HPV-Positive Oropharynx Cancers” in JAMA-OHNS, detailing the development of a novel diagnostic assay for
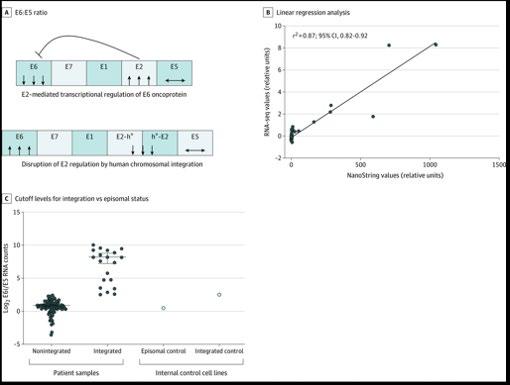
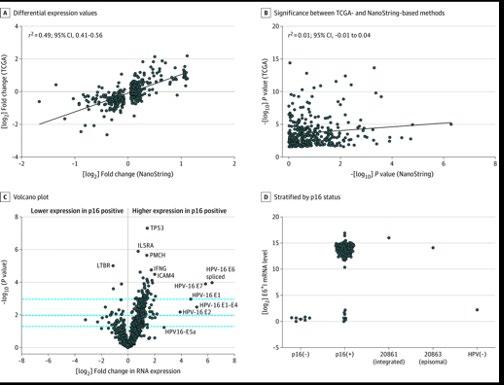
human papillomavirus–driven cancers of the oropharynx and the role viral integration could play in the process.
Additionally, our multidisciplinary cancer group has been at the national forefront pioneering neoadjuvant therapy trials for head and neck cancer since 2011, previously publishing mature 5-year outcomes for our phase 2 neoadjuvant chemo-immunotherapy “risk adaptive” transoral surgery trial led by Drs. Trevor Hackman and Jared Weiss in Oral Oncology in 2020. Our team has recently published the latest phase 2 neoadjuvant surgery trial for resectable locally advanced head and neck squamous cell carcinoma, in Cancer. This neoadjuvant trial not only redemonstrated the safety and feasibility of
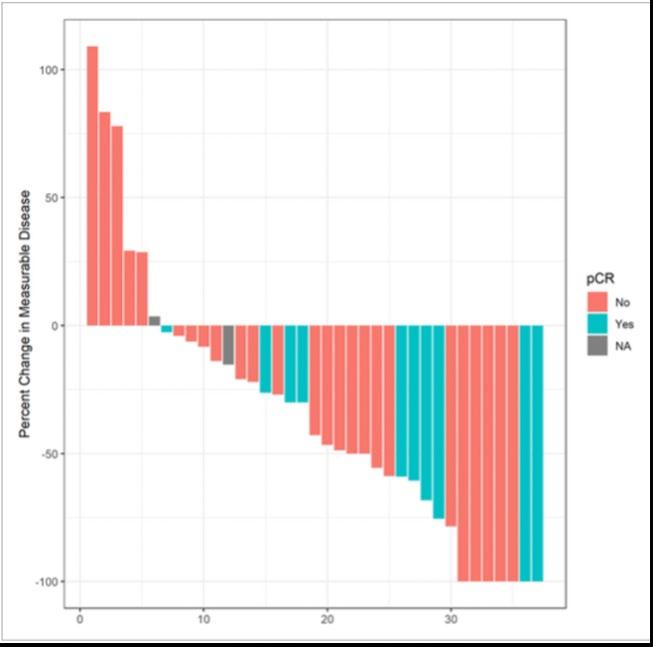
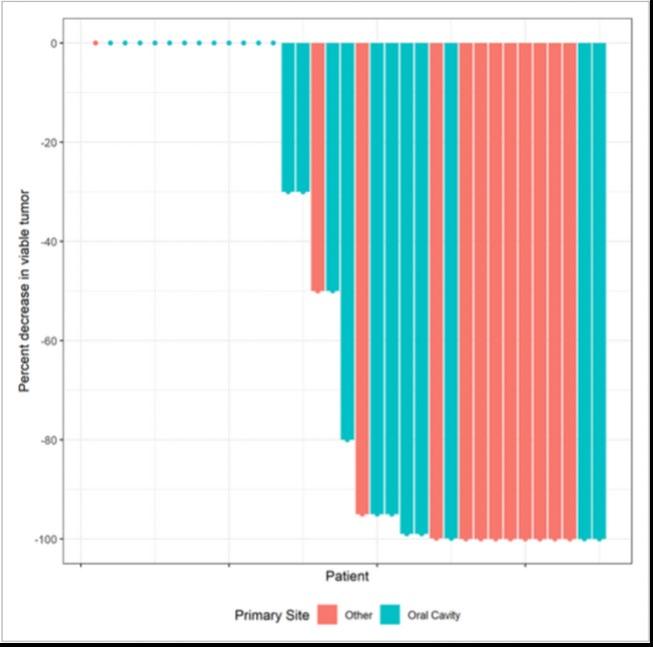
neoadjuvant chemoimmunotherapy treatment for locally advanced cancer, but also the promising treatment responses and pathologic downstaging afforded by neoadjuvant approach despite the advanced stage tumors, including those in the oral cavity.
Within the realm of epidemiology, our collaborative group recently published a landmark report “Poor oral health influences head and neck cancer patient survival: an International Head and Neck Cancer Epidemiology Consortium pooled analysis” in the Journal of the National Cancer Institute. This pooled analysis of 2500 patients from 4 studies conclusively demonstrated that “good oral health as defined by maintenance of the natural dentition and frequent dental visits appears to be associated with improved overall survival among head and neck squamous cell carcinoma patients.”
Finally, within the sphere of simulation, our group completed and published its experience with the development of a novel 3D-printed TORS simulator in Laryngoscope. Our lowcost, high fidelity simulator successfully differentiated novice from experienced and
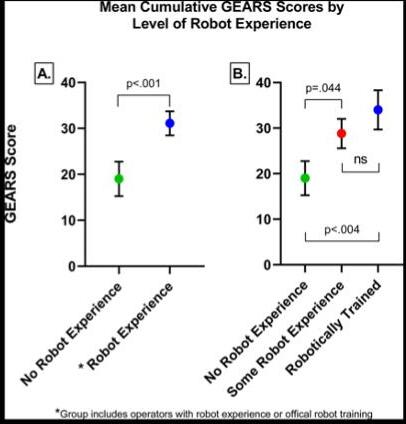
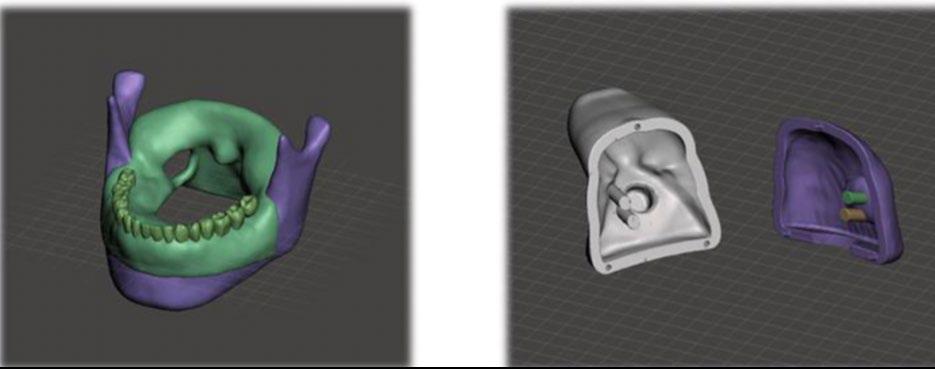
robotically trained operators of the da Vinci SI robot during simulated tonsillectomy and base of tongue resections. A subsequent validation study of this simulator as a training tool on the da Vinci SP robotic system has been completed with manuscript in preparation for submission.
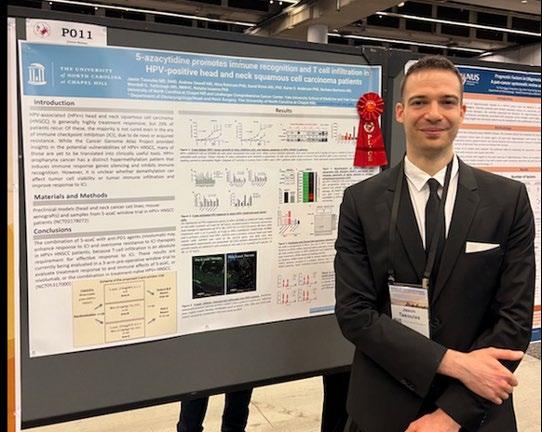
This past year saw our faculty traveling across the country and overseas for visiting lectureships and presentations. Highlights included a visiting lectureship at the World Thyroid Congress in London; Invited faculty for the Emory Microvascular Course and Invited speaker at the ENT SAAA Congress in Johannesburg, South Africa; Putney Lectureship Guest Speaker at MUSC in Charleston SC, Guest Lecturer at the ECOG-ACRIN Spring Meeting Chicago IL, and Invited Speaker for the Yale Spore, CEP/DRP Meeting New Haven CT. Finally, the UNC Head and Neck Oncology Division celebrated 12 podium and poster presentations at the International American Head and Neck Surgery Society Meeting in Montreal, capped off by a second place for best poster for our post doctoral fellow, Jason Tasoulas.
RO1 – Dissecting NF-kB pathway in HPV-associated HN Cancer
R01 – Exploring therapeutic demethylation in HPV-associated HN Cancer
UO1 – Observational study to validate HPV DNA genotyping and prognostic genomic biomarkers for diagnosis and treatment of HPV-associated HNSCC
P50 – Project 3 in HN SPORE: Overcoming Treatment Resistance in HN Cancer Multi-institutional R01 looking at the role of CRTC1/MAML2 on mucoepidermoid carcinoma cells.
In addition, Dr. Schrank was awarded a K08 and a career enhancement award. Dr. Isaeva recieved the Developmental Research Award, and the department was awarded a flash grant from the NC Biotechnology Center.
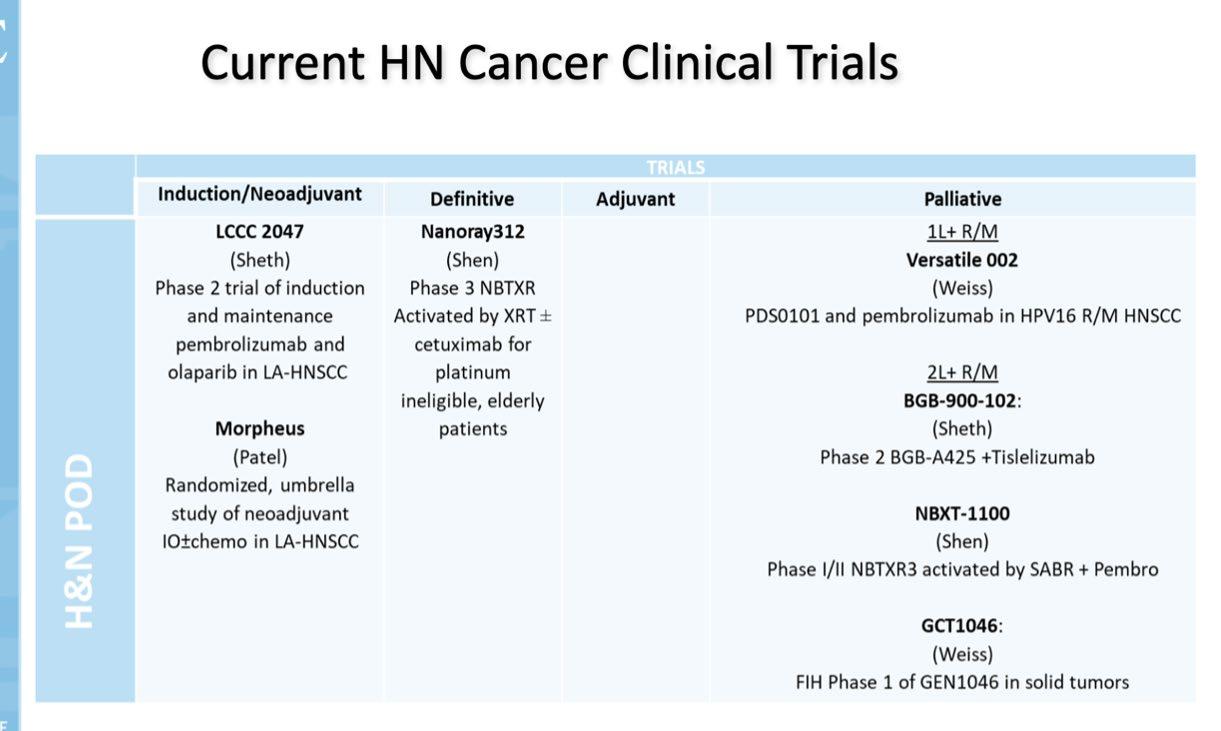
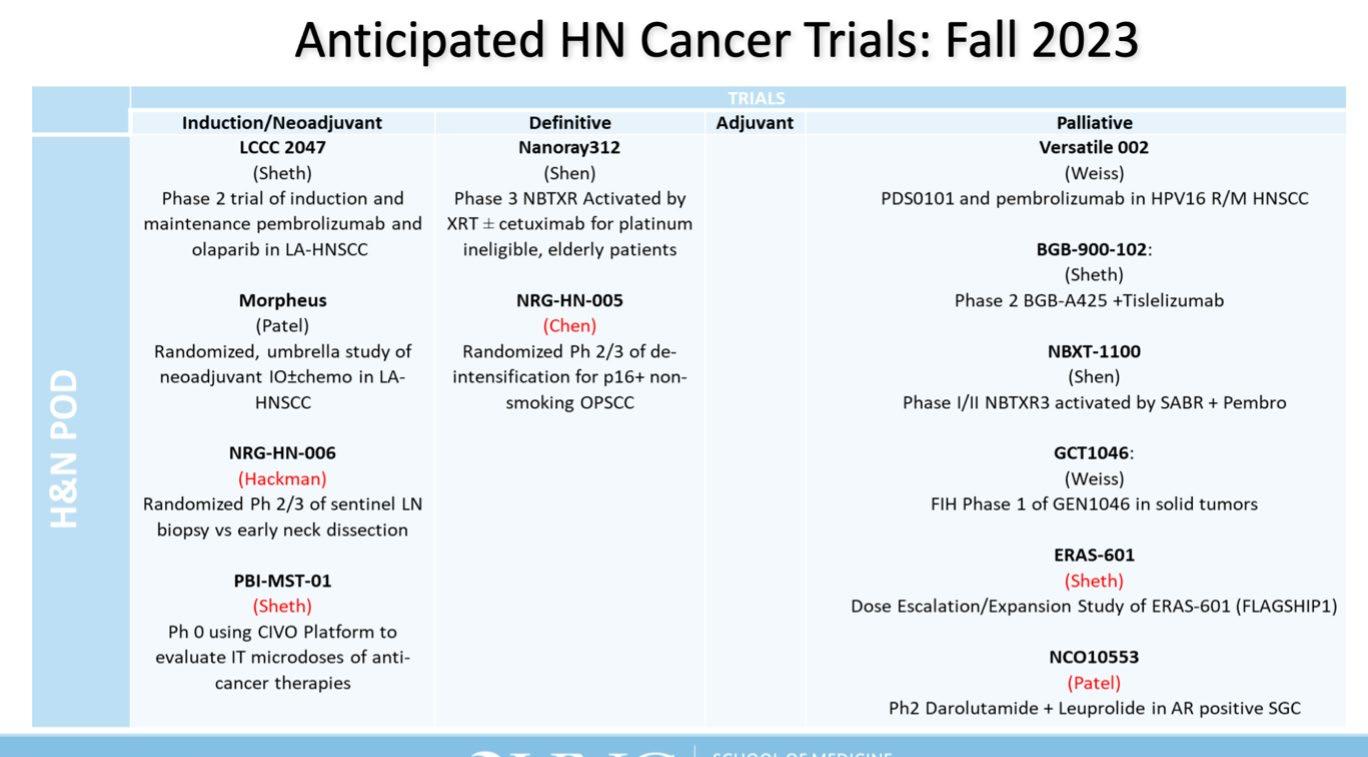
Our Multidisciplinary Head and Neck Cancer Team, composed of 6 head and neck surgeons, 3 radiation oncologists, and 4 medical oncologists/trialists, boasts a broad portfolio of in-house, industry and cooperative group clinical trials, covering the spectrum of induction/neoadjuvant therapy, definitive therapy and palliative trials.


CARLTON J. ZDANSKI, MD, FAAP, FACS
CHIEF, DIVISION OF PEDIATRIC OTOLARYNGOLOGY
HERBERT H. THORP ⁄ JULIAN T. MANN DISTINGUISHED PROFESSOR

AMELIA F. DRAKE, MD, FACS
NEWTON D. FISCHER DISTINGUISHED PROFESSOR
AUSTIN S. ROSE, MD, MBA, FARS PROFESSOR

LAUREN A. LEEPER, MD, FACS
ASSOCIATE PROFESSOR FELLOWSHIP DIRECTOR
JAIME P. DOODY, MD
ASSISTANT PROFESSOR
The Division of Pediatric Otolaryngology continues its strong dedication to research, education and clinical care here at UNC Department of Otolaryngology.
In addition to the faculty in this division, we have trained future generations of Pediatric Otolaryngologists/Head and Neck Surgeons for over a decade, representing the first Specialty Fellowship training program in the Department of Otolaryngology/Head and Neck Surgery at UNC. This year we are pleased to welcome Allison Keane, MD as our latest fellow.
Research and Education continue to thrive in the division with an ever-growing research portfolio which resulted in more than 25 presentations at national and international meetings and more than 10 scientific articles. Members of the Division are involved in numerous leadership roles on a Departmental, National, and International level.
The Division continues to serve as Co-Host of the yearly Carolina Pediatric Airway Course (CPAC), in partnership with the Medical University of South Carolina (MUSC). This course mentors’ residents and fellows from UNC, MUSC, Duke, Wake Forest, Emory, Medical College of Georgia, Eastern Virginia Medical School, and Vanderbilt on Pediatric Airway issues. This year's Visiting Professor was the legendary Mr. John Russel, MD from Trinity College in Dublin who regaled with tales of his career and Oscar Wilde.


• Dr. Carlton Zdanski, MD continues his work on an R01 funded by the National Heart, Lung and Blood Institute related to anatomic optical coherence tomography for quantitative to predict the need for surgery in pediatric subglottic stenosis using airway elastography derived from endoscopic OCT and intraluminal pressure measurement. (R01-HL154429-0, $3,966,921)
• Dr. Amelia Drake continues her work as Co-PI on a COVID-19 grant related to retaining clinical scientists funded by the Doris Duke Charitable Foundation.
• Dr. Amelia Drake, MD continues to do meaningful and impactful work with the UNC Dental School pertaining to craniofacial microsomia including NIDCR R01 DE02951001, Craniofacial microsomia: Accelerating Research and Education (CARE), NIDCR 2R01DE022566-06A1 (Zajac PI) 2019 – 2024 Development of Stop Consonants in Children with Repaired Cleft Palate: Continuation Study.
• Dr. Carlton J. Zdanski collaborates with investigators at NCSU with PI Dr. Alon Greenbaum (R21 DC020005, 09/16/2022 – 07/31/2025 "Establishing the pig as a large animal model for studying drug delivery to the inner ear") and Dr. Nicorsur Iftimia (SBIR 10-07742-8060-46 Multimodal Optical Probe for Real-time Assessment of Airway Tissue after Injury).
• Dr. Austin Rose participates in the FastTraCS grant supported by NC TraCs as a Clinical Advisor.
• Dr. Drake continues her leadership in the American Cleft Palate-Craniofacial Association (Past President) and mentorship with Drs. Leeper and Zdanski in attendance at the Annual Meeting held in Raleigh, NC this past year.

The inaugural meeting of the international research group called CARE that studies craniofacial microsomia.
Outreach remains an ongoing commitment in the Division of Pediatric Otolaryngology/ Head and Neck Surgery despite the COVID Pandemic. Commitments include outreach to Malawi and Ecuador.
Most recently, post-COVID, Dr. Leeper has renewed efforts at Benjamin Bloom Hospital, which is the sole public Children’s Hospital in El Salvador. Dr. Leeper has been going annually since 2012 but efforts were paused in 2021 due to Covid. The team sees many patients each year whom they have taken care of since infancy (and several patients are now teenagers that return). The team works throughout the year with the Bloom Hospital staff surgeons (Dr. Pamela Bolaños, seen in this photo with Dr. Leeper and former UNC OHNS Resident Dr. Krishna Patel) who provide continuity of care for these patients as well.
The Division continues to expand its services in the Triangle. With our newest clinic location at Lake Boone Trail in Raleigh, NC, in addition to our sites of care at the Meadowmont Clinic, Carolina Crossing Clinic, the Pediatric Multi-Disciplinary Thyroid Clinic, the UNC Cleft Palate/Craniofacial Clinic, The Vascular Anomalies Clinic, and The North Carolina Children's Airway Center.

UNC Department of Otolaryngology ⁄ Head and Neck Surgery
22-23 Annual Report


J. MADISON CLARK, MD, FACS
CHIEF, DIVISION OF FACIAL PLASTIC AND RECONSTRUCTIVE SURGERY
FELLOWSHIP DIRECTOR

MATTHEW Q. MILLER, MD
ASSISTANT PROFESSOR
UNC FACIAL NERVE CENTER DIRECTOR
BRIAN S. JEWETT, MD
PROFESSOR


VIRGINIA "GINNY" DRAKE, MD
ASSISTANT PROFESSOR
NICOLE A. HUGHES, LE
ACADEMIC AESTHETICIAN

WILLIAM W. SHOCKLEY, MD, FACS
EMERITUS PROFESSOR
FOUNDING VICE CHAIR
FOUNDING CHIEF
The growth of the division has been incredible. We stand on the shoulders of a true “giant” in the field, Dr. Bill Shockley. From the time that Dr. Madison Clark joined him in 2015, the division has added 3 additional full-time FPRS faculty members in 3 consecutive years:
• Dr. Matt Miller, Director-UNC Facial Nerve Center, September 2021
See the Facial Nerve Center page for accomplishments
• Dr. Brian Jewett, September 2022
20 years at the Univ of Miami, former Division Chief and Fellowship Director
• Dr. Virginia “Ginny” Drake, September 2023
Residency-Johns Hopkins
FPRS Fellowship-Univ of Michigan
This growth has increased the breadth and depth of our scope of practice to include all aspects of Facial Plastic and Reconstructive Surgery. This has not only further enhanced our medical student, resident, and fellowship education, but we are also now fully staffed to accept referrals from our valued colleagues from across North Carolina and beyond.
Invited panelists for Body (Facial) Dysmorphic Disorder at one of the largest aesthetic conferences in the world (AMWC Monaco), March 31, 2023. From left to right: Dr. Madison Clark, Dr. Brittany Howard (Mayo Arizona, and first UNC FPRS fellow), Dr. Sabrina Fabi (San Diego, CA), Dr. Nicole Kanaris (Johannesburg, South Africa).
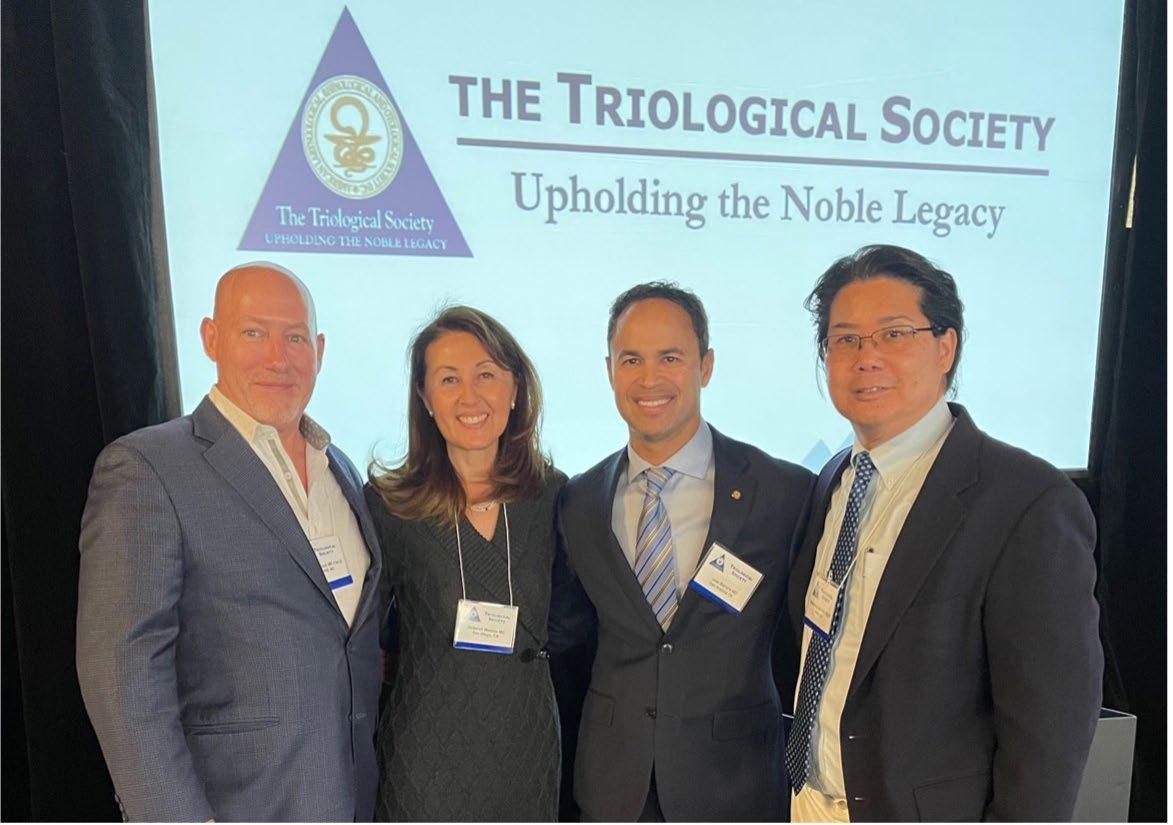
Invited panelists for Dorsal Preservation Rhinoplasty at the Combined Sections Triological Society meeting, January 27, 2023. From left to right: Dr. Madison Clark, Dr. Deborah Watson (San Diego, CA), Dr. Jose Barrera (San Antonio, TX), Dr. Brian Wong (Irvine, CA).

This 2022-23 academic year was the FPRS division’s most productive year to date, which is not surprising given the growth of the division. From the division’s 25 publications for the year, the TOP 5 PUBLICATIONS that we would like to highlight are the following:
1. O’Rourke SP and Miller MQ. Predicting Depressor Anguli Oris Excision Outcomes Using Local Muscle Block. Facial Plast Surg Aesthet Med. 2022 Nov 15. doi: 10.1089/ fpsam.2022.0282. Epub ahead of print. PMID: 36378249.
2. Varman R, Miller MQ. Microvascular Gracilis Free Flap: Single and Double Innervation. Atlas Oral Maxillofac Surg Clin North Am. 2023 Mar;31(1):33-41. doi: 10.1016/j.cxom.2022.09.005. PMID: 36754505.
3. Mims MM, Shockley WW, Clark JM. Casual Observers' Perception on the Aesthetics of the Butterfly Graft. Laryngoscope. 2023 Oct;133(10):2578-2583. doi: 10.1002/lary.30562. Epub 2023 Jan 5.PMID: 36602076
4. Kim SG, Menapace DC, Mims MM, Shockley WW, Clark JM. Age-Related Histologic and Biochemical Changes in Auricular and Nasal Cartilages. Laryngoscope. 2023 Sep 7. doi: 10.1002/lary.30990.PMID: 37676075
5. Shockley WW. Complications in Surgical Reconstruction: My View. Semin Plast Surg. 2023 Feb 9;37(1):3. doi: 10.1055/s-0043-1761300. eCollection 2023 f: 36776804
The bolded names are those medical students and fellows who have worked alongside the faculty in these projects, and they deserve special recognition. Finally, although Dr. Shockley has retired from clinical practice, he not only remains active in resident and fellow education, but he continues to be sought after for his expertise and contributions to the literature (see # 5).

Annual Fellowship Alumni Dinner, AAPRS Annual Meeting, Washington, DC. From left to right: Dr. Matt Miller, Dr. Mark Mims (Univ Oklahoma), Dr. Madison Clark, Dr. Bill Shockley, Dr. Jonas Miller (current UNC FPRS Fellow), Dr. Deanna Menapace (Mayo Florida), Dr. Jennifer Kim (Invited Speaker, Univ of Michigan), Dr. Rahul Varman (Creighton University).

Invited faculty-The Portland Rhinoplasty Course. Dr. Fausto Lopez Ulloa (Mexico City, Mexico) and Dr. Madison Clark, taking a break from teaching in the dissection lab.
The 2022-23 academic year was also the FPRS division’s most productive year to date. From the 18 national and international presentations, the TOP 5 PRESENTATIONS that we would like to highlight are the following:
1. Shockley, WW. Panel Discussion: Nasal Reconstruction: Setting the Foundation. AAFPRS. Washington DC, Oct 21,2022
2. Miller MQ. Panel Discussion: The Cross Section of Facial Rejuvenation and Reanimation. The International Federation of Otorhinolaryngological Societies; Dubai, UAE. January 2023.
3. Miller MQ. Panel Discussion: Facial Reanimation: Approach and Challenging Cases. The International Federation of Otorhinolaryngological Societies; Dubai, UAE. January 2023.
4. Clark JM. Panel Discussion: “Preservation Rhinoplasty – Or, Less Can Be More.” Triological Combined Sections Meeting. San Diego, CA, January 27, 2023
5. Clark JM. Panel Discussion: “My patient has BDD, Now What?” AMWC Monaco. March 31, 2023.
These presentations were each invited panel presentations, and they demonstrate the broad scope of expertise within the FPRS division.
Research continues to be very active in the FPRS division, with ongoing projects including clinical outcomes in facial paralysis, skin cancer reconstruction, and nasal airway obstruction. Dr. Drake is creating an IRB for skin cancer reconstruction database that will resemble the Facial Nerve database that was established by Dr. Matt Miller. Other ongoing projects include the following:
• Narrative interviews of facial paralysis patients
• Impact of race and culture on facial paralysis
• PROM readability in facial paralysis
• Periocular reanimation
• Systematic review of alar reconstruction using composite grafts
• Analysis of histology and biochemical properties of the dorsal septal articulation
• CFD analysis of the INV in DPR
$15,000 (Department Grant-Dr. Matt Miller, The Impacts of Race and Culture on the Patient Experience of Facial Paralysis)
$2000 (CMSRP, Yang Lee, mentored by Dr. Madison Clark)
• Dr. Rahul Varman graduated in June 2023, joined Creighton University School of Medicine
• Dr. Jonas Miller started July 2023, following completion of his residency at Johns Hopkins
• Dr. Tyler Rist matched for start July 2024, following completion of his residency at MUSC



 ALDEN PRIDGEN SPEECH PATHOLOGIST
ALDEN PRIDGEN SPEECH PATHOLOGIST
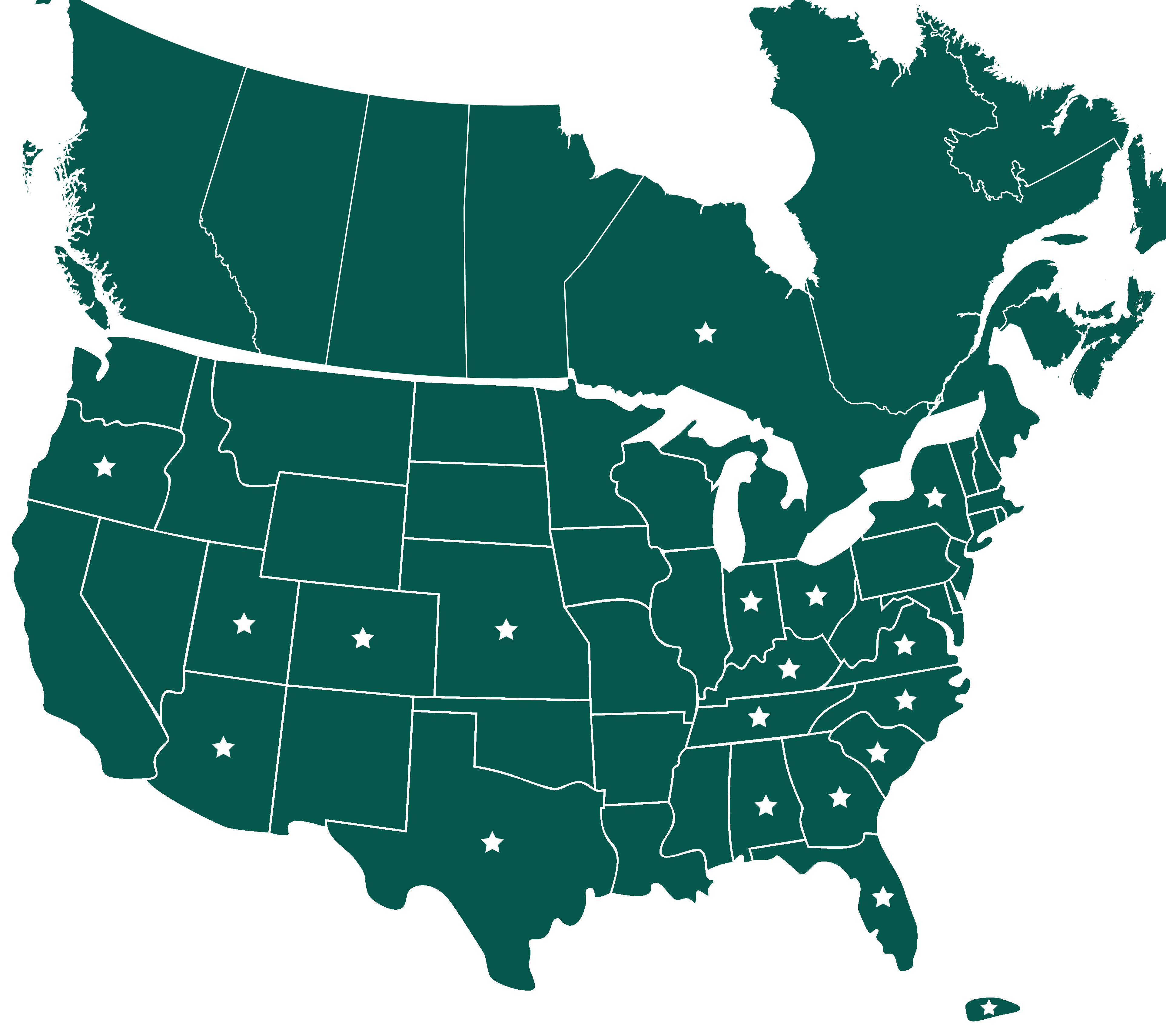
The UNC Facial Nerve Center had a year of tremendous growth in 2022-2023. Alden Pridgen joined the team as the second facial nerve therapist, working alongside Heather Davis Cuevas. Dr. Virginia Drake was recruited to the Division of Facial Plastic and Reconstructive Surgery, after completing her residency at Johns Hopkins and fellowship at the University of Michigan. She starts in September and will work alongside Dr. Miller in evaluating and treating patients with facial paralysis. The UNC Facial Nerve Center has expanded its national and international presence, treating more than 500 patients from 17 US states, two Canadian provinces, and Puerto Rico. The Facial Nerve Center continues to help shape the way patients with facial paralysis are cared for around the world by presenting its work in publications and presentations. Dr. Miller was invited to give three podium presentations on facial reanimation surgery at the International Federation of Otolaryngology Societies (IFOS) World Congress in Dubai.
• Miller MQ, Hadlock TA. Commentary on: “Chemodenervation Algorithm: Functional and Aesthetic Considerations for Facial Harmony in Patients with Post-Facial Paralysis Synkinesis. Facial Plast Surg Aesthet Med. Epub ahead of print 2023 May 15.
• O’Rourke SP and Miller MQ. Predicting Depressor Anguli Oris Excision Outcomes
Using Local Muscle Block. Facial Plast Surg Aesthet Med. 2022 Nov 15. doi: 10.1089/ fpsam.2022.0282. Epub ahead of print. PMID: 36378249.
• Varman R, Miller MQ. Microvascular Gracilis Free Flap: Single and Double Innervation. Atlas Oral Maxillofac Surg Clin North Am. 2023 Mar;31(1):33-41. doi: 10.1016/j. cxom.2022.09.005. PMID: 36754505.
• Miller MQ. The Crossection of Facial Rejuvenation and Reanimation. The International Federation of Otorhinolaryngological Societies; January 2023; Dubai, UAE.
• Miller MQ. Facial Reanimation: Approach and Challenging Cases. The International Federation of Otorhinolaryngological Societies; January 2023; Dubai, UAE.
• O’Rourke SP, Miller MQ. Predicting depressor anguli oris excision outcomes using local muscle block. 13th International Symposium of Facial Plastic Surgery; October 2022; National Harbor, MD.
• Dr. Miller gave an invited lecture to the Wake Forest Department of OtolaryngologyHead and Neck Surgery on facial reanimation surgery
• Dr. Abdulmalik Ismail visited the UNC Facial Nerve Center in May 2023 to learn about management of facial paralysis
• Dr. Miller and one of his patients were featured on a UNC Health Talk, Innovative Procedures Allow Bell’s Palsy Patient to Smile Again, in September 2022
• Dr. Miller was the invited expert for a British Medical Journal podcast on Bell’s palsy in November 2022
• Dr. Miller was awarded a UNC Department of Otolaryngology/Head and Neck Surgery Small Research Grant, The Impacts of Race and Culture on the Patient Experience of Facial Paralysis, Awarded $15,000 in January 2023.
The Facial Nerve Center has now evaluated and treated more than 500 patients from the following states/territories and Canadian provinces:
North Carolina, South Carolina, Virginia, Georgia, Tennessee, Arizona, Texas, Kansas, Ohio, New York, Kentucky, Utah, Halifax– NS Canada, Toronto– Canada, Florida, Oregon, Puerto Rico, Alabama, Colorado, Indiana
UNC Department of Otolaryngology ⁄ Head and Neck Surgery
22-23 Annual Report

BRENT A. SENIOR, MD, FACS, FARS
DIVISION CHIEF
HAROLD C. PILLSBURY, III DISTINGUISHED PROFESSOR

CHARLES S. EBERT, JR., MD, MPH, FARS, FAAOA, FACS
FELLOWSHIP CO-DIRECTOR
MEDICAL DIRECTOR OF OTOLARYNGIC ALLERGY SERVICES PROFESSOR
BRIAN D. THORP, MD, FACS, FARS
FELLOWSHIP CO-DIRECTOR
ASSOCIATE PROFESSOR


CHRISTINE KLATT-CROMWELL, MD
ASSOCIATE PROFESSOR
ADAM J. KIMPLE, MD, PHD, FACS, FARS
ASSOCIATE PROFESSOR
DIRECTOR OF RHINOLOGY RESEARCH

MEGHAN NORRIS, MS, MSPAS, PA-C
PHYSICIAN ASSISTANT
Dr. Senior was honored to provide the David W. Kennedy Lecture at the Annual Meeting of the American Rhinologic Society in Nashville on “Global Outreach in Otolaryngology: Lessons Learned in a Quarter Century in Vietnam.” He was also pleased to be able to return to Vietnam after a COVID imposed recess, joined by the current Rhinology fellow, Scott Hardison, MD, and one of Rhinology's international fellows, Kazuhiro Omura, MD. He directed the “Rhinology PreCourse” for the Meeting of the ASEAN ORL Society in Hanoi. He continues as President of the International Rhinologic Society and Vice President of Development and Strategy for the American Rhinologic Society.

Brent Senior, MD, presented the Kennedy Lecture at the Annual Meeting of the American Rhinologic Society, Nashville.


Dr. Ebert continued his societal leadership being named President of the American Academy of Otolaryngic Allergy Foundation while also contributing as Associate Editor for the major consensus document: “International Consensus on Allergy and Rhinology: Allergic Rhinitis 2023,” published in The International Forum of Allergy and Rhinology. He was asked to be a member of the NIH Workshop on Allergic Fungal Sinusitis, and in support of his university, he was pleased to be named to the UNC Faculty Council.

Dr. Thorp was excited to be named Program Director for the UNC Department of Otolaryngology/Head and Neck Surgery Residency Program, taking over from longtime director, Robert Buckmire. He continues his outstanding leadership of the PreCourse for the North American Skull Base Society. He also served as Panelist for Joint AHNS/ ARS/NASBS Sinonasal Malignancies Program as well as Moderator for Sinonasal Malignancies Expert Panel at COSM. He also serves as an at-Large Member of the Medical School Executive Committee. But he is quick to point out that his greatest achievement this year was the birth of Iris Larson Thorp to him and his wife Lindsay!

Dr. Kimple continues as a coinvestigator and the lead Otolaryngologist on the Genetic Disorders of Mucociliary Clearance Consortium an NIH sponsored Rare Disease Clinical Research Network which has a 5 year grant for $7.5 million from the National Center for Advancing Translational Sciences and National Heart Lung Blood Institute.

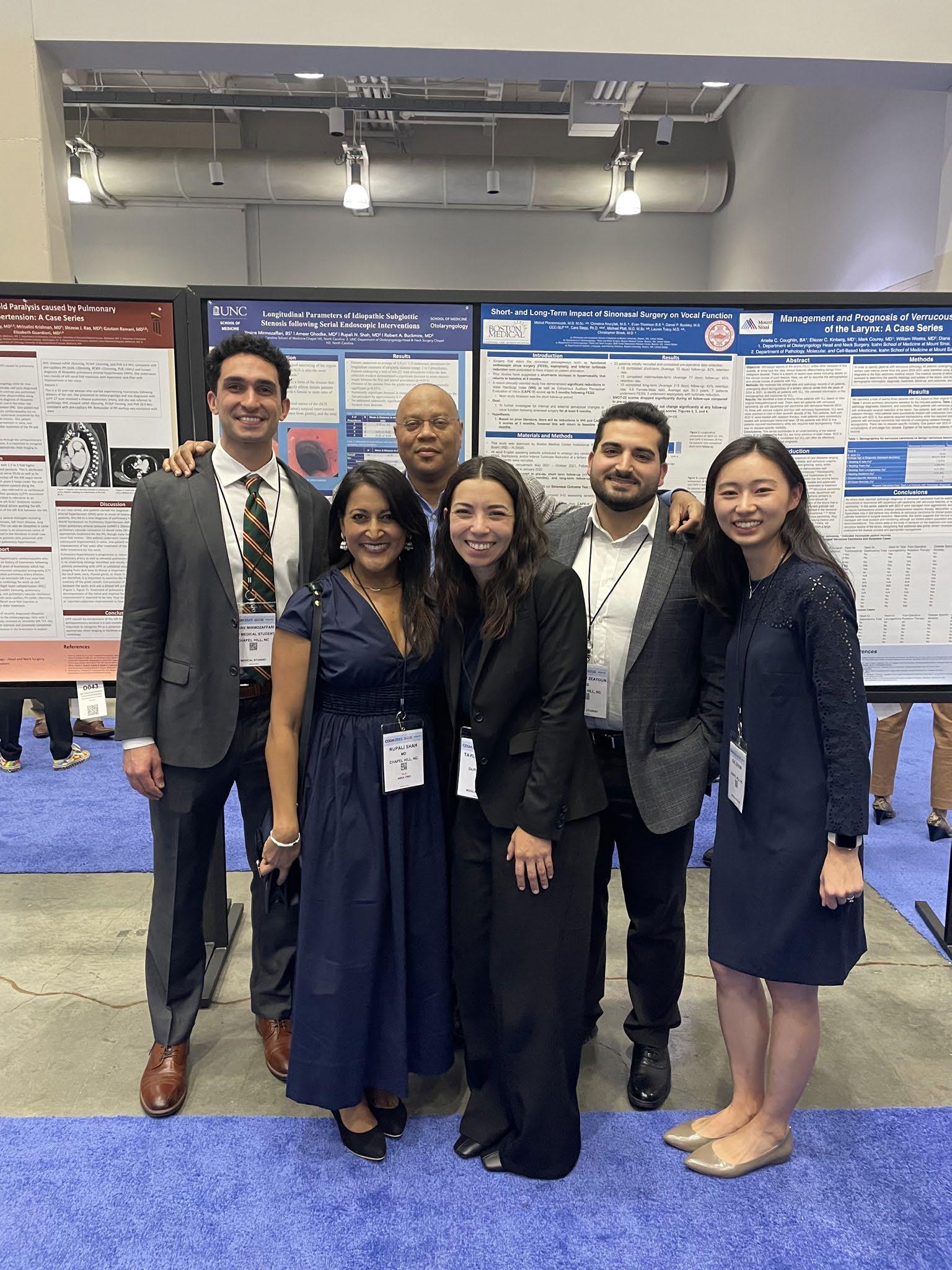
He also leads as a co-Principal investigator on a multinational, $3.5-million project funded through the Chan Zuckerberg Initiative to map crucial cellular roles in human health and disease. As Director of Rhinology Research, he is most proud of the 20 manuscripts published by the division that had a mentored student, resident or international fellow as the lead author.

Some of the members of the Rhinology, Allergy, and Endoscopic Skull Base Surgery Research Team, 2023.
In addition to her busy rhinology/skull base practice, Dr. Klatt-Cromwell has been very busy in a variety of UNC and UNC Health leadership courses, including “Relational Leadership” and “Clinical Leadership.” She has been a coauthor on a series of published papers on those areas, and most recently she was named to the UNC Lineberger Equity Council Executive Committee.

Illustration from “Cranial Nerve Zero: What the Rhinologist Needs to Know” was featured on the cover of IFAR in its October 2023 edition. First author, Ibtisam Mohammad, MD is a visiting surgeon in the division from Turkey.

Some of the US delegation to ASEAN ORL Meeting in Hanoi, Vietnam including UNC Otolaryngologists Austin Rose, MD, and Brent Senior, MD, and former resident, Harold Pine, MD, and international fellow, Kazuhiro Omura, MD
UNC Department of Otolaryngology ⁄ Head and Neck Surgery 22-23 Annual
UNC Rhinology, Allergy, and Endoscopic Skull Base Surgery Fellow, Scott Hardison, MD, lecturing at the ASEAN ORL Meeting Rhinology Precourse, in Hanoi, Vietnam

• Adam Kimple – Co-I “Characterizing the upper airway manifestations in Primary Ciliary Dyskinesia and Primary Immunodeficiencies”, a $7.5 million from the National Center for Advancing Translational Sciences and National Heart Lung Blood Institute
• Adam Kimple – Co-PI $3.5 million Chan Zuckerberg Award Mapping the Pediatric Inhalation Interface: Nose, Mouth, and Airways
RESEARCH AND PUBLICATIONS from the Division in the last year focused on 4 primary areas:
• Continuing its tradition of leadership in the fields of Rhinology, Allergy, and Endoscopic Skull Base Surgery, members of the division served as contributors and editors for several international and national guidelines papers including:
a. Consensus criteria for chronic rhinosinusitis disease control an international Delphi Study. (Rhinology)
b. International consensus statement on allergy and rhinology: Sinonasal tumors. (International Forum of Allergy & Rhinology)
c. Multicenter Survival Analysis and Application of an Olfactory Neuroblastoma Staging Modification Incorporating Hyams Grade. (JAMA Otolaryngol Head Neck Surg)
d. EPOS/EUFOREA update on indication and evaluation of Biologics in Chronic Rhinosinusitis with Nasal Polyps 2023. (Rhinology)
e. The EUFOREA pocket guide for chronic rhinosinusitis. (Rhinology)
f. ICARS: Allergic Rhinitis 2023
• The division continues to provide cutting-edge and world-leading research in the area of sinus disease in patients with genetic disorders of mucociliary clearance including cystic fibrosis and primary ciliary dyskinesia:
a. Sinonasal quality of life in primary ciliary dyskinesia.
b. Mucolytic treatment of chronic rhinosinusitis in a murine model of primary ciliary dyskinesia
c. Primary ciliary dyskinesia: An update on contemporary diagnosis.
d. Factors that predict pursuing sinus surgery in the era of effective modulator therapy
• Partnering with colleagues in other labs at UNC including the EPA, members of the division published unique clinical and translational research that helps us to better understand the basic mechanisms of sinusitis and how certain medications impact the course of disease. While additional work helps in understanding how our astronauts’ nose and sinuses are impacted by lunar dust while on the moon.
a. In Vivo Fluticasone Absorption in Surgical Patients.
b. Nasal biomarkers of immune function differ based on smoking and respiratory disease statusc.
c. Site-specific detection and differential levels of immune mediators in the sinonasal mucosa.
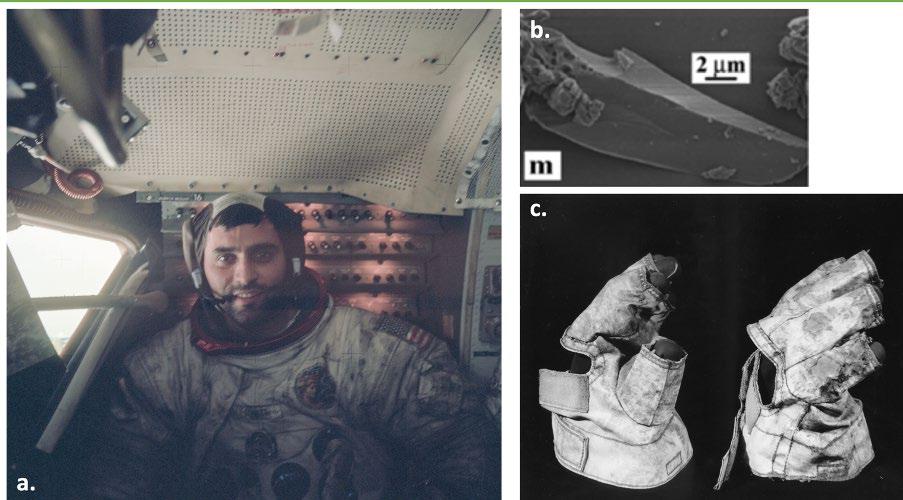
d. Lunar dust: A unique nasal irritant forgotten by history.
a) Lunar dust seen on the spacesuit in the Apollo module
b) micrograph of the sharp shards unique to lunar dust
c) dust adherent to the gloves of an Apollo astronaut
• Research from the division also helped to shed light on residency education in otolaryngology/head and neck surgery, including the extent of racial bias in letters of recommendation for residency, as well as the special needs of left-handed trainees.
a. Racial and Ethnic Bias in Letters of Recommendation and Personal Statements for Application to Otolaryngology Residency
b. "Left on their own": Left-handedness among rhinologists and otolaryngology trainees.
9
MENTORED STUDENTS AND INTERNATIONAL FELLOWS
• Taylor Stacks UNC Medical Student - Holderness Fellow 2022-23
• Meredith Lamb – Campbell Medical Student 2022 -23
• Sulgi Kim – UNC Medical Student 2022 - 23
• Aurelia Monk – UNC Medical Student – Holderness 2023-23
• Nick Melott – Des Moines University College of Osteopathic Medicine Summer 2023
• Anysa Fernandez – UNC Medical Studeent - Castillo Scholar, Summer 2023
• Shreyas Payti – Stoneybrook School of Medicine – Summer 2023
• Ibtisam Mohammed, MD – Visiting Research Fellow, Gazi University, Ankara, Turkey
• Kazuhiro Omura, MD –Visiting Research Fellow, Jikei University, Tokyo, Japan

KEVIN D. BROWN, MD, PHD
DIVISION CHIEF
JOSEPH P. RIDDLE DISTINGUISHED PROFESSOR

MATTHEW M. DEDMON, MD, PHD
MEDICAL DIRECTOR OF AUDIOLOGY
ASSISTANT PROFESSOR
A. MORGAN SELLECK, MD
FELLOWSHIP CO-DIRECTOR
ASSISTANT PROFESSOR
NICHOLAS THOMPSON, MD
ASSISTANT PROFESSOR
KAYLA WILKERSON, DNP, FNP-BC, RN
OTOLOGY NURSE PRACTITIONER
Neurotology welcomed Dr. Nicholas Thompson as a faculty member this year! Dr. Thompson joins the Neurotology team with the honor of having been awarded the Fellow Teaching Award, by UNC Department of Otolaryngology-Head & Neck Surgery upon his completion of his fellowship. He has had a busy start to his tenure at UNC by co-authoring 7 publications for the division and presenting at 7 separate meetings for neurotology. Most notably, however, Dr. Thompson and Dr. Dedmon worked together on a Clinical Trial: ‘ClinicalTrials.gov Identifier: NCT05441540 - Internal Jugular Vein Compression Collar for Novel Symptomatic Treatment of Venous Pulsatile Tinnitus,’ This was a prospective trial that evaluated the use of a wearable compression collar for 20 patients who had pulsatile tinnitus. They found a significant improvement in symptom intensity and burden of illness with a median symptomatic relief of 50%. Overall, it seemed that the collars offered good acute symptom relief for patient with venous pulsatile tinnitus.
In the 2022-2023 fiscal year, Dr. Selleck was part of the AAOHNS Otology and Neurotology Education Committee, the Hearing Committee, and the WIO Leadership Development and Mentorship Committee. She was awarded “Faculty Teacher of the Year” voted on by the residents. Dr. Selleck aided in the education of our residents and medical students by giving talks about “Balance Problems and Facial Nerve Considerations” and “Vestibular Anatomy and Physiology,” and also leading a small group discussion on “ENT Cases.” She completed xRead in FLEX through ONEC and got IRB approval for the MED-EL pediatric Bone Bridge Study.
Dr. Dedmon attended the 20th Hearing and Structure Preservation International Meeting as a member of their Program Committee, and also attended the 2nd Annual International Fall Cochlear Implant Meeting as a member of their Scientific Committee. Along with being on these international committees, Dr. Dedmon was the course director for the Temporal Bone Course held annually for our residents.
Dr. Brown was the Scientific Director and Host for the 20th Hearing and Structure Preservation Workshop, and also the Course Director for the 2nd Annual International Fall Cochlear Implant Meeting. He wrote position statements for cochlear implantation in adults and children with single-sided deafness for AAO-HNS, and was also an Honor Award Recipient from the Academy to recognize his volunteer service over the last five years. In 2022, Dr. Brown’s article titled, “Benefits of cochlear implantation in childhood unilateral hearing loss,” was the top downloaded article in the Laryngoscope.
• “UNC Otolaryngology Internal Research Grant Dedmon and Grose (Co-PI) 3/2021-7/2023 $40,0000 - 10% "Concurrent recording of the electrically-evoked compound action potential and the auditory brainstem response in cochlear implant users"
• ClinicalTrials.gov Identifier: NCT05441540 - Internal Jugular Vein Compression Collar for Novel Symptomatic Treatment of Venous Pulsatile Tinnitus
• Pivotal, prospective, multi-centre, randomised control, blinded study evaluating the efficacy of a dexamethasone eluting Slim Modiolar electrode (CI632D) in the reduction of fibrosis as compared to a standard Slim Modiolar electrode (CI632) in a newly implanted adult population with bilateral, post-linguistic, moderate to profound sensorineural hearing loss.
• Post-approval, prospective, nonrandomized, single arm multicenter investigation to evaluate the safety and effectiveness of cochlear implantation in children and adults with unilateral hearing loss/single-sided deafness.
• Neural Prediction to Enhance Language Outcomes in Children with Cochlear Implant (R01) – Dr. Kevin Brown Site PI
• Cochlear Implantation in Infants and Toddlers with Single-Sided Deafness
• Clinical Utility of Residual Hearing in the Cochlear Implant Ear (Multisite U01) – Dr. Kevin Brown Site PI
• Place-based mapping in electric-acoustic stimulation listeners (R21) – Dr. Kevin Brown Co-Site PI
• Expanded Indications in the MED-EL Pediatric Cochlear Implant Population 22

Drs. Dillon and Dedmon with our newest Neurotology Fellow, Dr. Ben Johnson!
From Left: Dr. Meg Dillon, Dr. Ben Johnson, and Dr. Matthew Dedmon



DIVISION CHIEF
ASSOCIATE PROFESSOR

DORIS
ASSISTANT PROFESSOR
The Division of General Otolaryngology has had a productive year. Both Drs. DeMason and Lin continue to grow UNC Otolaryngology's footprint in Chatham County. Dr. Lin also runs a rural otolaryngology elective for medical students. Dr. DeMason continued in her role as the Director of Medical Student Education for the department and this past year became one of the residency’s Associate Program Directors. Dr. DeMason was promoted to associate professor and she did her 50th hypoglossal nerve implantation this year.
The division continues to be involved with many research projects. Dr. Lin published an article on tinnitus and the COVID-19 vaccination which was featured on Forbes.com. Dr. DeMason has been involved with many research projects that have been published this past year on underrepresented groups in academic otolaryngology. Dr. DeMason was also on multiple panels at the AAOA and AAO-HNS meetings in Nashville this past September. Drs DeMason and Lin received a research grant evaluating the department’s diversity, equity and inclusion journal club. The division plans to continue expanding their educational and research efforts over the next few years.

ROBERT A. BUCKMIRE, MD
DIVISION CHIEF
MARCH FLOYD RIDDLE DISTINGUISHED PROFESSOR

RUPALI (PALI) N. SHAH, MD
PROFESSOR

Dr. Shah was an invited speaker/ panelist at the American Bronch-Esophagological Association Annual Meeting on the topic of: “Action Items for the Unhappy Physician or How to Stay That Way for Happy Physicians.” She has additionally been selected to serve on the UNC School of Medicine Diversity & Inclusion Council- advisory board to the Vice Dean for Diversity, Equity, and Inclusion (Nate Thomas). She has been promoted to full professor in the last academic year, and received the inaugural “American Laryngological Association Post-Graduate Member Best Paper Award at the 2022 ALA/ COSM meeting in May 2022.

Dr. Buckmire was elected to the American Laryngological Association Council and currently serves as the Treasurer of this professional organization.
For the 7th consecutive year, members of the Voice and Swallowing Division mentored a student who won a Carolina Medical Student Research Program grant ($4500) - a competitive research grant program for 1st year medical students.
• Comparative treatment outcomes for idiopathic subglottic stenosis: 5-year update. (North American Airway Collaboative. Laryngoscope. 2022 Oct 26. Doi: 10.1002/lary.30449)
• Impact of serial intralesional steroid injections on idiopathic subglottic stenosis (North American Airway Collaboative Otolaryngol Head Neck Surg. 2023 Jan 19. Doi: 10.1002/ohn.190
These two publications represent a historic collaboration of laryngologists across the country, combined to achieve the statistical power necessary to study a rare disease, subglottic stenosis. We participate in the North American Airway Collaborative (NoAAC) -which was conceived and designed to combine, collate and analyze data from laryngologist with a busy airway practices across the country. These publications represent the latest outcome of this collaboration, made possible by these Herculean organizational efforts.
• "Rank equity Index Unveils Lack of Parity in Faculty Advancement in Academic Otolaryngology.” Oral Presentation, Triological Society at COSM. May 2023. Boston, MA. (Kim S, Russel SM, Stack TJ, Frank-Ito DO, Farzal Z, Ebert CS, Buckmire RA, Demason CE, Shah, RN.).
• "Finding the Leaks in the Pipeline for Underrepresented Racial Minorities in Otolaryngology.” Poster Presentation, Triological Society Combined Sections meeting. Jan 2023, Coronado, CA. (Russel SM, Farzal Z, Shah RN, Ebert CE, Buckmire RA, Demason CE, Frank-Ito DO)
Over the last several years, we have assembled a Medical Education Study Group what has grown to be multi-institutional (Duke and UNC), that assembles many faculty involved in the administration of residency education, primary research faculty, a research-track resident with a speciality in public health, and medical students. The broad focus of this group was to better study and elucidate the means by which we currently select, educate, and propagate otolaryngology residents. Our recent publications have focused on how an individuals demographics (race and sex) affect matriculation into Otolaryngology residency and promotion through the ranks of academic Otolaryngology. These two recent national presentations represent recent output of this vibrant collaborative research collective.
• Can the remote use of a peak flow meter predict severity of subglottic stenosis and surgical timing?
Laryngoscope. 2023 Mar 133(3):628633. (Park M, Tie K, Davis H, Hall J, Buckmire RA, Shah RN)

This publication represents a line of research inquiry that has grown out of our need to serially and efficiently follow our airway patients despite barriers such as distance, means, and even pandemic. The study, initiated during the Covid pandemic, was designed to determine the utility of a simple peak flow meter for following subglottic stenosis patients remotely, and predict their need for operative intervention. Following on this research,
this means of follow up, has become our standard for serially monitoring our patient cohort with this challenging, and frequently recurring disease process. This research project was distinguished by winning both the inaugural American Laryngological Association Post-Graduate Member Best Paper Award (Dr. Shah) and the Deborah C. O'Leary UNC School of Medicine Student Research Award..
The current research within the division is focused in several areas:
• Medical Education (as described above)
• Technological advancement in Laryngology procedures and post-procedural data collection
a. Novel mechanisms for Remote real-time data collection in post-procedural patients Dr. Shah is the PI on a project based around the creation of a novel data collection App (Encore). This application, designed and created in house was designed to optimize the collection of both real-time voice data, (voice recordings) and, patient reported outcome measures (PROMs), commonly used in Laryngology practices for the purpose of gauging the longitudinal impact of clinical interventions.
b. Novel image guided simulation/training model for intralaryngeal injection
Using a 3-D printed larynx and an image guidance system, we have developed a simulated training device to assist in teaching in trans-cervical intralaryngeal botox injection. This simulator offers real-time feedback regarding the accuracy and consistency of needle placement during this technique (currently) performed through a blind, anatomical needle placement. With the assistance of a postgraduate researcher, Abdullah Zeatoun and a current medical student researcher, Zane Kaiser our existing Brainlab image guidance system has been re-purposed for this research.
The balance of the research within the division focuses upon evaluation of the efficacy of specific management strategies for vexing clinical entities, including glottic and subglottic stenosis, as well as in-office vocal fold augmentation.
12 MENTORED STUDENTS AND RESIDENTS
6 MENTORED RESIDENTS
6 MENTORED STUDENTS


LISA PARK, AUD
DIVISION CHIEF
ASSOCIATE PROFESSOR

ERIKA GAGNON, AUD, CCC-A
CLINIC MANAGER - AUDIOLOGY
ASSISTANT PROFESSOR
JENNIFER WOODARD, AUD, CCC-A
ASSISTANT PROFESSOR


MELISSA AUCHTER, AUD, CCC-A
ASSISTANT PROFESSOR
DAKOTA SHARP, AUD, CCC-A
ASSISTANT PROFESSOR
UNC Department of Otolaryngology ⁄ Head and Neck Surgery
22-23 Annual Report


LILLIAN HENDERSON, MSP, CCC-SLP, LSLS CERT. AVT
CLINIC MANAGER - SPEECH
ASSISTANT PROFESSOR

SANDRA HANCOCK, MS, CCC-SLP, LSLS CERT. AVT
ASSISTANT PROFESSOR
CHRISTINE KRAMER, MS, CCC-SLP, LSLS CERT. AVED
ASSISTANT PROFESSOR

ERIN THOMPSON, MS, CCC-SLP, LSLS CERT. AVT
ASSISTANT PROFESSOR


In their first year as a division, the faculty at the Children’s Cochlear Implant Center at UNC have been busy making their mark. The clinic got a bit of a facelift with some new furniture, murals by multi-talented audiologist Dr. Jennifer Woodard, and the ever-growing activation handprint wall. The faculty mentored several students. In the clinic, mentees included 4th year audiology externs Malia Henderson and Ricardo Vallejo, speech and language student Anna Bradshaw, and graduate students from the Division of Speech and Hearing within Allied Health. In research, faculty provided support to audiology students Shannon Culbertson, Victoria Sweeney, Sydney Mingle and ENT residents Drs. Kayla Hicks and Teresa Vos. The annual Summer Institute continued, where our speech and language pathologists coach and mentor prospective Auditory Verbal Therapists in working with children who are deaf or hard of hearing. Our faculty have also been supporting the mission of the university by teaching in classrooms at UNC and when invited to other universities. The team has been gearing up for the launch of the Mobile Speech and Hearing Unit, set to hit the road in early 2024. It is currently being built to provide hearing testing, technology fitting and care, and speech/language services to children around the state. The goal of the unit is to make top-notch UNC hearing care accessible to all of the children in North Carolina.
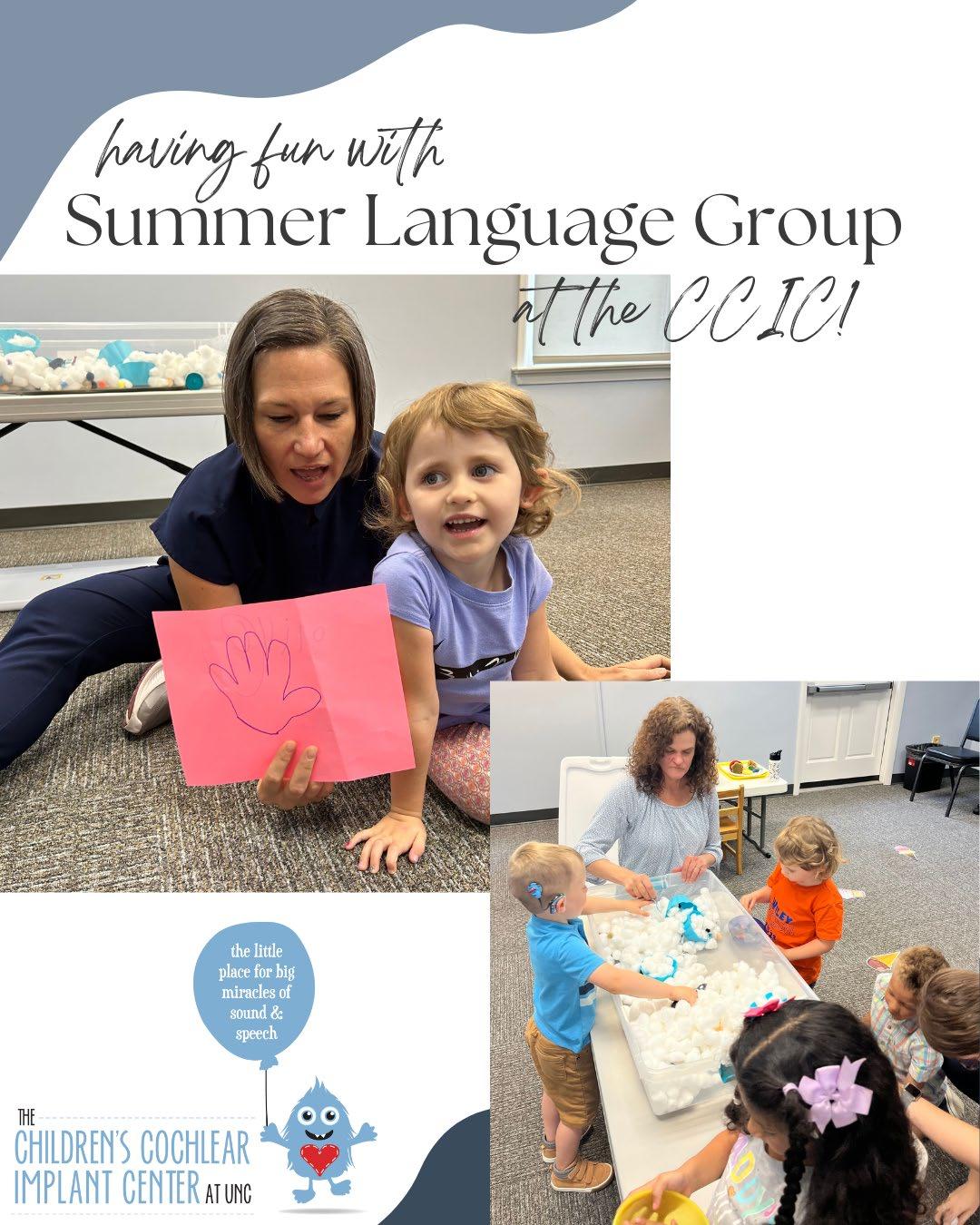
1. This past summer, the CCIC’s conference room became a Listening and Spoken Language preschool classroom for a small group of preschoolers. These children, who are deaf or hard-of-hearing, had not been able to access summer services from their school systems. Clinical faculty, Chrissy Kramer and Sandra Hancock, led this small group focusing on speech, language, vocabulary, and listening goals around summer themes. Our faculty trained a Medical University of South Carolina (MUSC) graduate clinician on performing group therapy with this patient population.
2. Dr. Dakota Sharp started On The Ear: An Audiology Podcast back in 2020 with two goals in mind: create an accessible continuing education option for clinicians and
students, and pursue his own passion for lifelong learning. Since then, with over 40 episodes so far, he has interviewed experts across the spectrum of communication sciences and disorders, including UNC Faculty members Dr. Lisa Park (Episode 6: Expanding Candidacy for Pediatric Cochlear Implants) and Dr. Meg Dillon (Episode 41: The Evolution of Cochlear Implants for Single Sided Deafness). In 2023 the podcast reached 35,000 downloads, with episodes eligible for continuing education credit for professionals and some Au.D. programs integrating the content into their curriculum.
3. Sandra Hancock, M.S., CCC-SLP, LSLS Cert. AVT traveled to Nepal in May with The Global Foundation for Children with Hearing Loss, launching a multi-year pediatric program in Nepal. With help from grantors, the GFCHL is partnering with CHEERS Hospital in Kathmandu to develop local expertise in pediatric audiology and auditory-verbal therapy for young children with hearing loss learning to listen and speak. Sandra was on a team of three speech-pathologists, and two audiologists, providing training to professionals & Community Ear Health workers from Kathmandu & surrounding areas. Sandra describes the experience as an exciting opportunity to share knowledge & expertise with service providers who are eager to learn, in an area where options for children with hearing loss are extremely limited. The goal of the GFCHL is to change that!


4. Erin Thompson, M.S., CCC-SLP, LSLS Cert. AVT was honored when she was invited by MED-EL corporation to attend and present at the 19th Annual National Conference of the Cochlear Implant Group of India (CIGICON) in November of 2022 in New Delhi, India. This year’s theme was, “Expanding Horizons – Maximizing Outcomes.” Ms. Thompson shared UNC’s research on data logging and hearing hours percentage. She gave an invited podium

presentation entitled – “Cochlear Implant Wear Time and its Direct Impact on Spoken Language Outcomes: Wear Time Data and It’s Use in a Clinical Co-Treat Model.” Ms. Thompson shared the research published by Drs. Lisa Park, Kevin Brown, Erika Gagnon, and Ms. Thompson. She was also invited to collaborate and present as part of a panel of teachers, audiologists, and speech-pathologists to review the current literature and prepare evidence-based guidelines for the long-term scholastic performance of pediatric cochlear implant users. The experience was enriched by the many opportunities to foster new professional relationships as well as be emersed in a vibrant, beautiful culture and community.
5. In July 2023, Erika Gagnon completed her second 4-year term serving as the Representative for Cochlear Implants on the North Carolina Governor’s Council for the Deaf and Hard of Hearing. This group advises the NC Department of Health and Human Services and the Department of Public Instruction on matters and services relating to deaf and hard-of-hearing individuals. During her terms, Erika attended quarterly meetings covering topics ranging from: interpreter services, Medicaid Expansion, Covid-19 Pandemic and many more. In November of 2022, Erika planned the meeting agenda and presented on pediatric cochlear implants. The meeting also included presentations from Dr. Kevin Brown highlighting the medical aspects of cochlear implantation and a panel of cochlear implant recipients and parents.
1. Park LR, Gagnon EB, Dillon MT. 2023. Factors that influence outcomes and device use for pediatric cochlear implant recipients with unilateral hearing loss. Front Hum Neurosci. 17 [Published Online Ahead of Print]. DOI: 10.3389/fnhum.2023.1141065
a. The goal of this paper was to identify factors that are related to how well children with unilateral hearing loss perform with a cochlear implant. The amount of time the child wears the device was the most influential factor. Children are less likely to wear their device as they approach their teen years. This paper provides information to help better outcomes for children with unilateral hearing loss who receive a cochlear implant.
2. Park LR, Dillon, MT, Buss E, Brown KD. 2023. Two-year outcomes of cochlear implant use for children with unilateral hearing loss: Benefits and comparison to children
with normal hearing. Ear Hear. [Published Online Ahead of Print] DOI: 10.1097/ AUD.0000000000001353.
a. This paper presented the culmination of a two-year clinical trial investigating cochlear implantation in children with unilateral hearing loss. This prospective study was the first of its kind and has set the mark for test methods, candidacy, and expectations in this population. The authors found that cochlear implantation can help children with unilateral hearing loss hear better in quiet and in noise and to localize sound. They also found quality of life improvements in the children.
3. Culbertson SR, Dillon MT, Richter ME, Brown KD, Anderson M, Hancock S, Park LR. 2022. Influence of age at cochlear implant activation on auditory skill development. J Speech Hear Res. 65(9):3539-3547. DOI: 10.1044/2022_JSLHR-22-00039
a. Before a child learns to talk, they have to learn to hear. Using data collected in the clinic on auditory milestones, the authors found that deaf children who receive cochlear implants before 9 months of age are able to catch up to their peers with typical hearing. This retrospective study was written by graduate student Shannon Culbertson and supported by faculty research, neurotology, audiology, and speech.
4. Anderson M, Dedmon MM, Thompson NJ, Park LR, Brown KD, Dillon MT. 2022. Frequency mapping of a pre-curved electrode array in the internal auditory canal for a pediatric cochlear implant recipient. Otol Neurotol. 43(7): e726-e729. doi: 10.1097/ MAO.0000000000003570
a. Sometimes our faculty inherit new patients who keep them on their toes. This paper reports on one of those children. When Dr. Melissa Anderson noted that something was out of the ordinary, Dr. Matthew Dedmon followed through and ordered imaging. There the authors found that the cochlear implant was not where it should be and was compromising the child’s hearing. Dr. Margaret Dillon, Director of Cochlear Implant Research, joined the care team. The three professionals worked together to find a unique programming method that significantly improved the child’s understanding of speech.
5. Sweeney V, Dillon M, Park LR, Brown K. 2022. Don’t Defer, Please Refer! Cochlear Implantation Candidacy as Part of the Hearing Health Care Continuum. The Hearing Journal. October 2022 Issue. 8-9.
a. Pediatric cochlear implant candidacy is ever changing and expanding. It can be difficult for clinicians who don’t work with implants routinely to keep up with current trends. One thing that stays true is the importance of early implantation. This article by graduate student Victoria Sweeney summarized what current pediatric cochlear implant candidacy looks like and stressed the importance of early referral. The authors
hope that this paper supports the growing trend to see cochlear implants as another technology option on the hearing healthcare continuum.
1. Gagnon EB & Park, LR. 2022. Datalogging: Collective Trends and Outcomes from a Large Pediatric Cochlear Implant Center. Podium Presentation at Fall CI Meeting, Santa Rosa Beach, FL. November 7-9.
a. In November 2022, members of the Children’s Cochlear Implant Center at UNC attended the first annual Fall Cochlear Implant Meeting in Santa Rosa Beach, Florida. This meeting was a great success and allowed for interdisciplinary presentations and dialogue. Dr. Erika Gagnon’s presentation


Datalogging: Collective Trends and Outcomes from a Large Pediatric Cochlear Implant Center revealed trends and barriers to pediatric cochlear implant use and continues to highlight the Hearing Hour Percentage, an objective metric for cochlear implant wear time. Wear time is an important factor in outcomes with cochlear implants, Dr. Gagnon, along with coauthors Drs. Lisa Park, Jennifer Woodard, Margaret Richter, Caitlin Sapp, Shannon Culbertson, Margaret Dillon, Meredith Rooth, and Ms. Lillian Henderson, are currently working to publish the outcomes of this research.
2. Park L, Leeper L, Gagnon E, Henderson L. The CI Team Talks. Institute for Cochlear Implant Training. May 15, 2023.
a. This past May the Institute for Cochlear Implant Training (ICIT) invited Drs. Gagnon, Leeper, Park, and Ms. Henderson to speak on the importance of a multidisciplinary team to maximize the potential of cochlear implant recipients. ICIT is an online didactic platform focusing on training surgeons, audiologists, speech language pathologists, and Teachers of the Deaf on cochlear implantation. The UNC team
was the final presentation for the Auditory-Verbal Practice Course consisting of 31 speech language pathologists and Teachers of the Deaf.
3. Fathima S, Joy J, Preto A, Soloman U, Thompson E. 2022. Guidelines for Long Term Scholastic Performance in Pediatric CI Users. Panel at the 19th Cochlear Implant Group of India Conference. New Delhi, India. November 4-6, 2022.

a. Ms. Erin Thompson was invited to be part of a nine-person, interdisciplinary panel at part of the 19th Annual National Conference of the Cochlear Implant Group of India (CIGICON) in November 2022 in New Delhi, India. This panel was composed of teachers, PhDs, Audiologists, Educators, and Speech-Language Pathologists from across the globe. The panel met virtually and in person in advance of the conference before presenting material and answering questions to help professionals create a framework for children with hearing loss in India. They covered topics including: optimal audition, speech perception, speech production, phonological processing, executive function, emergent literacy, cognition, language - syntax/semantics/discourse as well as complex needs of a child, in an attempt to help create Scholastic Guidelines for use with children who are deaf or hard of hearing in India. This brainstorming event was just the start of a complex and continued goal to use research and knowledge from different cultures to support India as a whole.
4. Park LR. 2023. Unilateral hearing loss in children: Cochlear implantation and the benefits of bilateral hearing. Keynote presentation at the 2023 AG Bell Global Listening and Spoken Language Virtual Symposium. June 28-29.
a. Dr. Lisa Park was invited to give her first international keynote talk at the AG Bell Spoken Language Symposium. This meeting has gone and stayed virtual since the pandemic to reach more professionals around the globe. Dr. Park was honored to present data from the Children with Unilateral Hearing Loss (CUHL) clinical trial and dispel some of the myths surrounding cochlear implantation.
5. Park LR, Dillon MT, Gagnon, EB, Eskridge H, Anderson M, Dedmon, M. (2022). A team approach to better hearing: Using interdisciplinary care to solve challenging cases. Hear-n-Now Fall Conference. Durham, NC. October 14th, 2022.
a. During the CCIC’s annual fall Hear-n-Now Conference, a multidisciplinary team of department professionals presented three complex cases, highlighting the importance of working together to provide best patient care. The presenters included two
clinical audiologists, two research audiologists, an otologist, and a speech-language pathologist. The cases presented included a young boy with device misplacement, a complex auditory neuropathy case, and a difficult mapping example for a child with a rare disease. All three cases presented highlighted the importance of collaboration between the different team members. The talk was presented as a panel with each team member contributing their viewpoint and focusing on how different perspectives were integrated to help reach the best potential outcomes for the families. Following the presentation, the attendees asked several questions not only related to the presented cases but also regarding other complex cases.

The faculty at the Children’s Cochlear Implant Center believe that it is our duty to impact knowledge about cochlear implantation in children. As one of the largest pediatric programs in the world, there is a lot to contribute. This year, faculty have been working on retrospective studies looking at factors that influence cochlear implant use and factors that lead a family to either choose or reject a cochlear implant. Cochlear nerve deficiency and outcomes continue to be a topic of interest for the faculty at the CCIC. The faculty have been collaborating with UNC Health audiologists on studies related to auditory dosage and Individualized Education Plans (IEPs). There are intra-institutional studies with professionals from Lurie Children’s Hospital and Vanderbilt University. Division Chief Dr. Lisa Park spends most of her time working with the cochlear implant research team, which helps translate findings from clincal trials related to expanding cochlear implant candidacy into clinical practice.
223 SERVED THROUGH THE CCCDP GRANT PROGRAM
2,517 AUDIOLOGY APPOINTMENTS
264 SPEECH AND LANGUAGE EVALUATIONS



EMILY BUSS, PHD
CHIEF, DIVISION OF AUDITORY RESEARCH PROFESSOR

PAUL B. MANIS, PHD
CHIEF, DIVISION OF RESEARCH TRAINING AND EDUCATION PROFESSOR
MARGARET T. DILLON, AUD, PHD
DIRECTOR OF CLINICAL RESEARCH
ASSOCIATE PROFESSOR
JOHN H. GROSE, PHD PROFESSOR
DOUGLAS C. FITZPATRICK, PHD
ASSOCIATE PROFESSOR

LISA PARK, AUD
ASSOCIATE PROFESSOR


KENDALL A. HUTSON, PHD ASSISTANT PROFESSOR

MEREDITH ANDERSON ROOTH, AUD ASSISTANT PROFESSOR
MICHAEL KASTEN, PHD ASSISTANT PROFESSOR


NATALIA ISAEVA, PHD ASSISTANT PROFESSOR
MARGARET RICHTER, AUD RESEARCH INSTRUCTOR
4.2M GRANT MONEY AWARDED
THEMANIS LAB published a paper using of a combination of serial-blockface electron microscopy and computational modeling to characterize the auditory nerve inputs and patterns of connectivity onto one major cell type, the bushy cell. These patterns affect how the central auditory neurons integrate information from the cochlea and achieve better timing precision than present in the cochlea. Such timing is needed for understanding speech and for identifying the location of sounds around us. This line of work also identified new anatomical structures associated with the central auditory neurons. These studies are at the forefront of “connectomics”, the study of detailed and precise connectivity between neurons in the brain and was recently published in eLife. A new block of tissue that includes an understudied part of the cochlear nucleus thought to be involved in how we hear sounds in a loud environment has been prepared and is currently under study. This work is part of a collaborative project between UNC, University of South Florida, and University of California at San Diego.
[Spirou, Kersting, Carr, Razzaq, Pinto, Dawson, Ellisman & Manis (2023) High-resolution volumetric imaging constrains compartmental models to explore synaptic integration and temporal processing by cochlear nucleus globular bushy cells, Elife:12:e83393.]
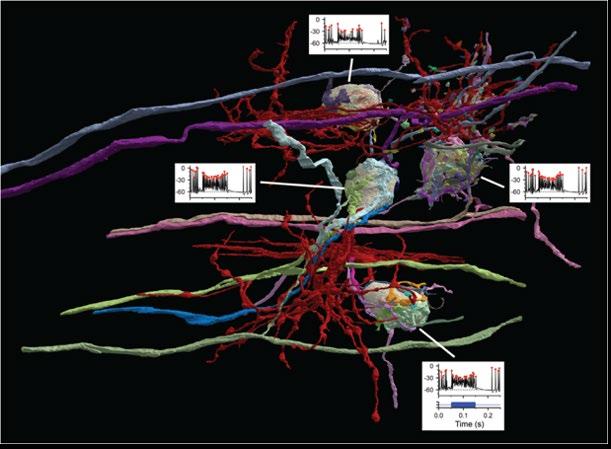
Image of 4 “bushy” neurons from the mouse cochlear nucleus with the auditory nerve fibers and synaptic endings that innervate them, reconstructed from serial-blockface electron microscopic sections. Insets are computed responses of each of the neurons to tone pips. From: Spirou… Ellisman and Manis, High-resolution volumetric imaging constrains compartmental models to explore synaptic integration and temporal processing by cochlear nucleus globular bushy cells. eLife 83393, 2023.
THE HEAD AND NECK ONCOLOGY LAB reported analysis of transcriptional data from 104 HPV+ (Human papillomavirus) HNSCC (head and neck squamous cell carcinoma) tumors together with two publicly available sources to identify highly robust transcriptional programs (modules). We found a single module that naturally subclassifies HPV+ HNSCC tumors based on a bimodal pattern of gene expression, clusters all atypical features of HPV+ HNSCC biology into a single subclass, and predicts patient outcome in four independent cohorts. The subclass-defining gene set was strongly correlated with Nuclear factor kappa B (NF-kB) target expression. Tumors with high expression of this NF-
kB module were rarely associated with activating PIK3CA alterations or viral integration, and also expressed higher levels of HPHPV E2 and had decreased APOBEC mutagenesis. Instead, they harbored inactivating alterations of key regulators of NF-kB, TNF receptor associated factor 3 (TRAF3), and cylindromatosis (CYLD), as well as retinoblastoma protein (RB1). HPV+ HNSCC cells in culture with experimental depletion of TRAF3 or CYLD displayed increased expression of the subclass-defining genes, as well as robust radio-sensitization, thus recapitulating both the tumor transcriptional state and improved treatment response observed in patients. Across all gene sets investigated, methylation to expression correlations were the strongest for the subclass-defining, NF-kB-related genes. Increased tumor-infiltrating CD4+ T cells and increased Estrogen receptors alpha (ERα) expression were identified in NF-kB active tumors. Based on the relatively high rates of cure in HPV+ HNSCC, deintensification of therapy to reduce treatment-related morbidity is being studied at many institutions. Tumor subclassification based on oncogenic subtypes may help guide the selection of therapeutic intensity or modality for patients with HPV+ HNSCC.
[Schrank, Kothari, Weir, Stepp, Rehmani, Liu, Wang, Sewell, Li, Tasoulas, Kim, Yarbrough, Xie, Flamand, Marur, Hayward, Wu, Burtness, Anderson, Baldwin, Yarbrough, & Issaeva (2023) Noncanonical HPV carcinogenesis drives radiosensitization of head and neck tumors, Proc Natl Acad Sci U S A.;120(32):e2216532120.]
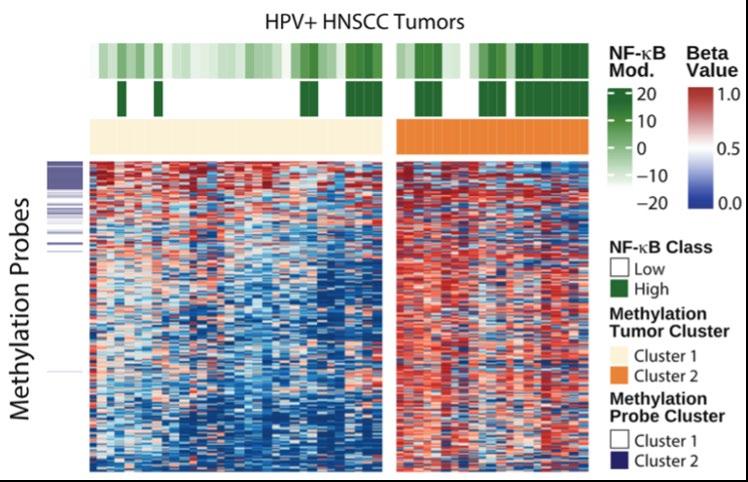
Heatmap of methylation probe intensities for HPV+ HNSCC tumors in TCGA organized by consensus clustering (k = 2). Green color scale—NF-kB (sky blue) module principal component analysis (PCA) scores. Dark green—denotes high expression of the NF-kB (sky blue) module. Tan—tumors assigned to methylation cluster 1. Orange—tumors assigned to methylation cluster 2. Warm colors—higher beta-values (more methylated). Cool colors—lower betavalues (less methylated). From: Schrank et al.(2023) Noncanonical HPV carcinogenesis drives radiosensitization of head and neck tumors, Proc Natl Acad Sci U S A.;120(32):e2216532120.
THE AUDITORY PHYSIOLOGY LAB has been studying cochlear synaptopathy using electrocochleagraphy. Cochlear synaptopathy is the loss of synapses between the inner hair cells and the auditory nerve despite survival of sensory hair cells. The
findings of extensive cochlear synaptopathy in animals after moderate noise exposures challenged the long-held view that hair cells are the cochlear elements most sensitive to insults that lead to hearing loss. However, cochlear synaptopathy has been difficult to identify in humans. This study applied novel algorithms to determine hair cell and neural contributions to electrocochleographic (ECochG) recordings from the round window of animal and human subjects. Gerbils with normal hearing provided training and test sets for a deep learning algorithm to detect the presence of neural responses to low frequency sounds, and an analytic model was used to quantify the proportion of neural and hair cell contributions to the ECochG response. The capacity to detect cochlear synaptopathy was validated in normal hearing and noise-exposed animals by using neurotoxins to reduce or eliminate the neural contributions. When the analytical methods were applied to human surgical subjects with access to the round window, the neural contribution resembled the partial cochlear synaptopathy present after neurotoxin application in animals. This result demonstrates the presence of viable hair cells not connected to auditory nerve fibers in human subjects with substantial hearing loss and indicates that efforts to regenerate nerve fibers may find a ready cochlear substrate for innervation and resumption of function.
[Haggerty, Hutson, Riggs, Brown, Pillsbury, Adunka, Buchman, & Fitzpatrick (2023). Assessment of cochlear synaptopathy by electrocochleography to low frequencies in a preclinical model and human subjects. Front Neurol.;14:1104574.]
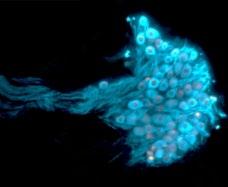
“Ganglion”, Dr. Kendall Hutson
Winner of the 2022 “Art in Science” Award at University Research Week.
Spiral ganglion cells in a mouse cochlea (the end organ for hearing) immunolabeled with antibodies to TuJ1 and Pou4F1, then imaged using light sheet fluorescent microscopy. Axons of these cells form the auditory nerve which carries information about sounds from the cochlea to the brain. Clusters of ganglion cells respond to a specific range of tones, and each cell is tuned to a specific quality of a tone based on its intensity (loudness). TuJ1 (blue) marks all ganglion cell bodies, while Pou4f1 (pink) marks the nucleus of cells tuned for loud sounds.
THE HEARING RESEARCH LAB has a longstanding program of research evaluating speech perception in challenging situations, including when multiple people are talking. A recent study conducted in collaboration with Case Western Reserve University and Iowa University characterized the effects of short-term audibility and differences in target and masker location (or perceived location) on the horizontal plane for sentence recognition in two-talker speech. Thirty young adults with normal hearing (NH) participated. Speech reception thresholds and keyword recognition at a fixed signal-to-noise ratio (SNR) were measured in each spatial condition. Short-term audibility for each keyword was quantified using a glimpsing model. Results revealed that speech-in-speech recognition depended on the proportion of audible glimpses available in the target + masker keyword stimulus in each spatial condition, even across stimuli presented at a fixed global SNR. Short-term audibility requirements were greater for colocated than spatially separated speech-inspeech recognition, and keyword recognition improved more rapidly as a function of increases in target audibility with spatial separation. Results indicate that spatial cues enhance glimpsing efficiency in competing speech for young adults with NH and provide a quantitative framework for estimating IM for speech-in-speech recognition in different spatial configurations.
[Wasiuk, Calandruccio, Oleson, & Buss (2023) Predicting speech-in-speech recognition: Short-term audibility and spatial separation, J Acoust Soc Am.;154(3):1827-1837]
THE COCHLEAR IMPLANT CLINICAL RESEARCH LAB published a paper investigating the incidence of electrode contacts within the functional acoustic hearing region in cochlear implant (CI) recipients and to assess its influence on speech recognition for electric-acoustic stimulation (EAS) users. This study included data for 105 CI recipients with functional acoustic hearing preservation (≤80 dB HL at 250 Hz) who received a 24-, 28-, or 31.5-mm lateral wall electrode array. Angular insertion depth (AID) of individual contacts was determined from imaging. Unaided acoustic thresholds and AID were used to calculate the proximity of contacts to the functional acoustic hearing region. The association between proximity values and speech recognition in quiet and noise for EAS users at 6 months post-activation was reviewed. Sixty percent of cases had one or more contacts within the functional acoustic hearing region. Proximity was not significantly associated with speech recognition in quiet. Better performance in noise was observed for cases with close correspondence between the most apical contact and the upper edge of residual hearing, with poorer results for increasing proximity values in either the basal or apical direction (r14 = 0.48, p = 0.043; r18 = -0.41, p = 0.045, respectively).
This study concluded that there was a high incidence of electrode contacts within the functional acoustic hearing region, which is not accounted for with default mapping procedures. The variability in outcomes across EAS users with default maps may be due in part to electric-on-acoustic interference, electric frequency-to-place mismatch, and/or failure to stimulate regions intermediate between the most apical electrode contact and the functional acoustic hearing region.
[Nix, Thompson, Brown, Dedmon, Selleck, Overton, Canfarotta, & Dillon (2023) Incidence of Cochlear Implant Electrode Contacts in the Functional Acoustic Hearing Region and the Influence on Speech Recognition with Electric-Acoustic Stimulation, Otol Neurotol.: Online ahead of print.]

This patient is a bilateral cochlear implant recipient, participating in a study investigating speech recognition and spatial hearing outcomes with place-based maps. In his words: "The CI is a transformative technology that has, without exaggeration, given me back my marriage, my friends and my music. I want to help Dr. Dillon and her team as they refine place-based mapping. I'm hopeful that these techniques will eventually become available for all CI patients, that acclimation to CIs will be accelerated and outcomes will improve for everyone."
Drs. Evan Nix, Matt Dedmon, Meg Dillon and Kevin Brown (left to right). Dr. Nix (PGY2) shared data from his research rotation on outcomes for CI patients with hearing preservation at the 58th Annual American Neurotology Society Spring Meeting.
TRAINEES



Stacey Kane (AuD) is completing her PhD work on hearing in children with Auditory Neuropathy.
Jason Tasoulas is a postdoctoral fellow studying in the Laboratory for Head and Neck Oncology.

Monica Folkerts is a postdoctoral fellow in the Hearing Research Lab.
Reginald Edwards is a PhD student in the Manis Lab.

Aditi Kothari is a PhD student in the Laboratory for Head and Neck Oncology. Her work focuses on HPV associated head and neck squamous cell carcinomas.
24
2 FELLOWS
10 GRADUATE STUDENTS (AUD)
1 MEDICAL STUDENT
2 POSTDOCTORAL FELLOWS (PHD)
3 RESIDENTS
3 GRADUATE STUDENTS (PHD)
2 UNDERGRADUATES
• The Manis lab identified of a subset of spiral ganglion cells thought to be involved in noise-induced and age-related hearing loss. This work used a combination of fluorescence methods in surface preparations and light-sheet imaging was done initially by Tessa Ropp, PhD, and subsequently refined by Ken Hutson, PhD.
• Drs. Dillon and Park won the Readers’ Choice award for Ear and Hearing’s most downloaded articles of 2022 with their position statements on the management of cochlear implantation in adults and children with single-sided deafness.
• We are expanding our CI research capacity with a 3rd research location in the new Cary clinic, and with the hiring of a 5th Research Audiologist.

Reginald Edwards testing a Zeiss 980 laser scanning confocal microscope. Also shown are Garrick Koermer and Christina Moore.
Members of the Head and Neck Oncology Laboratory.

UNC Department of Otolaryngology ⁄ Head and Neck Surgery 22-23 Annual Report

BRIAN D. THORP, MD, FACS, FARS RESIDENCY PROGRAM DIRECTOR

LAUREN A. LEEPER, MD, FACS
ASSOCIATE RESIDENCY PROGRAM DIRECTOR
CHRISTINE E. DEMASON, MD
ASSOCIATE RESIDENCY PROGRAM DIRECTOR

ELLEN DOUTT RESIDENCY PROGRAM COORDINATOR

Joseph Conduff, MD PGY5

Michael Canfarotta, MD PGY6 - Research Track

Todd Lambert, MD, MS PGY3

Ameer Ghodke, MD PGY2

Sarah Russel, MD PGY3 - Research Track

Cameron Worden, MD PGY2 - Research Track

John Crenshaw, MD PGY5

Elizabeth Ritter, MD PGY4

Eric Lee, MD PGY3

Habib Khoury, MD PGY2
John Henrich, MD PGY1

Zainab Farzal, MD, MPH PGY7 - Research Track

Wesley Stepp, MD, PhD PGY4

Heidi Martini-Stoica, MD, PhD PGY3

Evan Nix, MD PGY3

Scott Lamm, MD PGY1

Kathryn Kudlaty, MD PGY5

Teresa Vos, MD PGY4
Andrew Prince, MD PGY5 - Research Track

Kayla (Hicks) White, MD PGY3

Saima Wase, MD PGY1
As the first chairman of the Division of Otolaryngology/Head and Neck Surgery, Dr. Newton D. Fischer’s enduring emphasis on medical students and resident education, as well as research continues to shape the philosophy of the Department, specifically through the Annual Newton D. Fischer Conference!















Our ENT administrative team was instrumental in the Department of Otolaryngology’s many accomplishments and successes in FY23! In the first full post-COVID fiscal year with travel restrictions lifted, our all-star team successfully coordinated, booked, and reimbursed over 100 travels, both foreign and domestic, for over 60 different faculty, fellows, residents, staff, scholars, and students. This team was also crucial to the academic achievements of ENT across five different fellowship programs, including Head and Neck, Plastics, Neurotology, Rhinology, and Pediatrics. Our fellowship coordinators helped onboard FY23 fellows and supported them in a variety of ways throughout the year, while also leading the planning and coordination of interviews and applicant selection to find our future fellows of these programs.
Our residency coordinator, Ellen Doutt, was a vital part of continued ENT residency success as she supported a transition to a new team of residency leadership in ENT, while also leading the onboarding of another new class of residents. Throughout the year, Ellen is in constant communication with every one of our residents, pointing our future Otolaryngologist’s in the right direction every step of the way throughout each of their unique years in the program.
All in all, throughout the many leadership changes in our department over this past year our admin team was a constant and true backbone of our department. This team’s resourcefulness, work ethic, and dedication is second to none.
Our Public Communications Specialist, Grace Senior, led countless projects throughout the year, handling everything from our daily social media content across multiple platforms, to the coordination of the ENT events we know and love such as the ENT Zoo Day and Holiday Party to bring us all together! What a great asset to our team and department!
We also want to give a special shoutout and thanks to both Trey Webster (Accountant) and Carla Alston-Horton (Accounting Technician/AP) for their dedication to ENT. While technically employed by the Finance Shared Services, both Trey and Carla have been with ENT for 3+ years each at this point and are dedicated to ENT as though it truly was their permanent department. We are so grateful for their time and service over these past several years and throughout many changes.



• First Annual All Staff Retreat January 2023: included learning about the 5 dynamics as part of Relational Leadership at Carolina, Team Building activities and a Shared Service Project for Feed the Kids.
• Outpatient Clinic Expansion in Wake County: H & N Raleigh and Cary Clinic in late 2023.
• Schedule Build Optimization project in collaboration with UNC CASI team to implement best practices with our clinician’s templates with the goal to improve patient access.
• Focus on Team Communication and Collaboration: monthly staff celebrations (often a collaboration between Ebony Walker, Grace Senior and Ashlee Lo), monthly share out of Press Ganey positive comments, monthly share out of actions taken from staff SAFE reports, weekly email updates to staff from clinic leadership, two staff lunch & learns led by Lisa Licht on Compassion in the Workplace, huddle updates from staff specific to their work in specific divisions with providers.
• Clinical and Surgical patient confirmation calls to reduce late cancellations and no shows.
• Hannah Eskridge, Clinical Director
• Joshua Deal, Nurse Manager, All Facial Plastics Clinics
• Ashton Fields, Clinic Manager, Wake County Clinics
• Tabitha Thomas, Clinic Manager, Head & Neck Clinic in Medical Center
• Lillian Henderson, Speech Manager, Children's Cochlear Implant Center
• Erika Gagnon, Audiology Manager, Children's Cochlear Implant Center
• Michelle Solano, Clinic Manager Front Desk and Clinic Scheduling
• Ali Turner, Admin Supervisor , Surgery Scheduling
LEADING DEPARTMENT IN UNC IN

• Mortality Index (0.43)
• Length of Stay Index (1.3)
• Readmissions Rate (6.5%)
• > 4000 cases FY23
DEPARTMENT QUALITY IMPROVEMENT PROJECTS
• Length of Stay Reduction
a. JP Drain Project - Created to optimize outpatient Surgery
b. Nasogastic Tube Project - Created to optimize earlier safe discharge
c. G-tube Nomogram Study - Working to develop predictive nomogram
• Patient Education
a. Develop Pre-Op Educational Content / Pamphlet
b. Transition to online content
c. Pre-Op APP phone consultation
With consistent leadership of our advanced practice providers, Hannah Eadie and Courtney Hitpas, the otolaryngology service line has maintained inpatient HCAHP scores above 88% in the last fiscal year despite battling the continued constraints to staffing shortage and bedspace capacity post-pandemic.
• Length of stay < 6 days with LOS index <1.3
• Mortality rate of 0.43
• Readmission rate of 6.5%
• Exemplary observed Morbidity rate of 2.6% (NSQIP)
• Optimization of Enhanced Recovery After Surgery Pathway (ERAS) for HN surgery patients, results of which were recently published. As a multidisciplinary effort between Anesthesia, Otolaryngology, Pain Management, Speech/language Pathology, an ERAS pathway was developed for patients undergoing laryngectomy or partial glossectomy with flap reconstruction, as this population of patients typically require complex post operative care, average a LOS of >7 days and share similar perioperative morbidities and risks. Current work underway, lead by our APPs, to optimize and revamp the pathway. Murr AT, Sweeney C, Lenze NR, Farquhar DR, Hackman TG Implementation and Outcomes of ERAS Protocol for Major Oncologic Head and Neck Surgery. Laryngoscope. 2023 Jul 19. doi: 10.1002/lary.30904. Online ahead of print. PMID: 37466306
• Opiod Driven QI Projects
a. Implementation and Optimization of Comprehensive Inpatient Multimodal Pain Management Protocol (protocol and publication references below)
b. A multidisciplinary working group including anesthesia, chronic pain, otolaryngology, pharmacy and nursing researched and designed a multimodal pain management regiment for both inpatient and outpatient procedures during the height of the opioid pandemic.
• Readmission Nomogram Project to help identify at risk patients for readmission
a. Retrospective project study evaluating otolaryngology readmissions over a 5-year period at UNC. Patient demographics, co-morbidities, risk factors, perioperative data were analyzed
to determine factors associated with readmission. Among 365 discharges, 21 patients had unplanned readmissions within 30 days. On univariable analysis, acute myocardial infarction, number of total comorbidities, prior chemotherapy/radiation, active smoking, airway surgery, and enteral feeding, and on multivariable analysis, prior chemotherapy/radiation and active smoking were identified as significant readmission risk factors. Readmission risk increased from 2.43% to 7.48% and 41.67% with the addition of each risk factor.
• Outpatient JP drain management project. Purpose of this project is to safely and more efficiently discharge select patients home with JP drains after surgery, and thereby open up bedspace for new patients. Patients are educated preoperative on the expectation of discharge home POD#1 with JP drains, including management of the drain, with the intention of drain removal in the outpatient setting.
• Enteric feeding optimization project for inpatients after major HN surgery. Retrospective project looking at the utilization of gastrostomy tubes after major head and neck surgery, including free flap reconstruction, including days to oral diet, date of g-tube placement and length of stay. The intent of the project is to identify patient populations at high risk for g-tube placement needs, so as to allow for either 1) earlier g-tube placement in the post operative setting or 2) arrangement for discharge home with NGT, and thereby expedite discharge of the patient home to reduce LOS and open up virtual bedspace for new patients.
• Patient Education Project. Educational content developed for patient and family perioperative education, initially delivered in clinic to the patient at the first encounter, and then follow up phone visit with our APP to review the upcoming surgery, operative course and perioperative plan.

22-23 Annual Report



With the worst of the COVID-19 pandemic (hopefully) in our rear-view mirrors, over this last year the UNC Department of Otolaryngology/Head and Neck Surgery has started to enjoy gathering again in earnest! With trips to the NC Zoo, Museum of Life and Science, sporting events, graduation events, and holiday parties, faculty, staff, friends, and family got to enjoy each other in the setting of some of North Carolina’s most special places and events. While we never thought that lack of contact was good, most of us never realized how bad it was! But now, we gather, we share, we renew relationships, and as such we build each other up. We care for each other, and make care-giving for you and the people of North Carolina, better.
From our family to yours, please enjoy this cornucopia of gatherings with our UNC Department of Otolaryngology/Head and Neck Surgery over the last year!