U N I V E R S I T Y O F M I A M I M I L L E R S C H O O L O F M E D I C I N E Y E A R I N R E V I E W | 2 0 2 0
Department of PhysicalTherapy
D E P A R T M E N T O F P H Y S I C A L T H E R A P Y
Y E A R I N R E V I E W 2 0 2 0
L e t t e r f r o m t h e C h a i r
C l i n i c a l N e w s
U M P T R e s p o n d s t o C o v i d
T h e C o v i d P A C E R P r o j e c t
T a b l e o f C o n t e n t s
D e p a r t m e n t R e c o g n i t i o n s a n d A w a r d s
I n v i t e d P r e s e n t a t i o n s
D o c t o r o f P h y s i c a l T h e r a p y P r o g r a m
U M R e s i d e n c y P r o g r a m s
P h . D . P r o g r a m U p d a t e s
R e s e a r c h N e w s
C o m m u n i t y O u t r e a c h
F a c u l t y P u b l i c a t i o n s 2 0 1 8 - 2 0 2 0
From Dr. Neva Kirk-Sanchez, Ph.D., PT
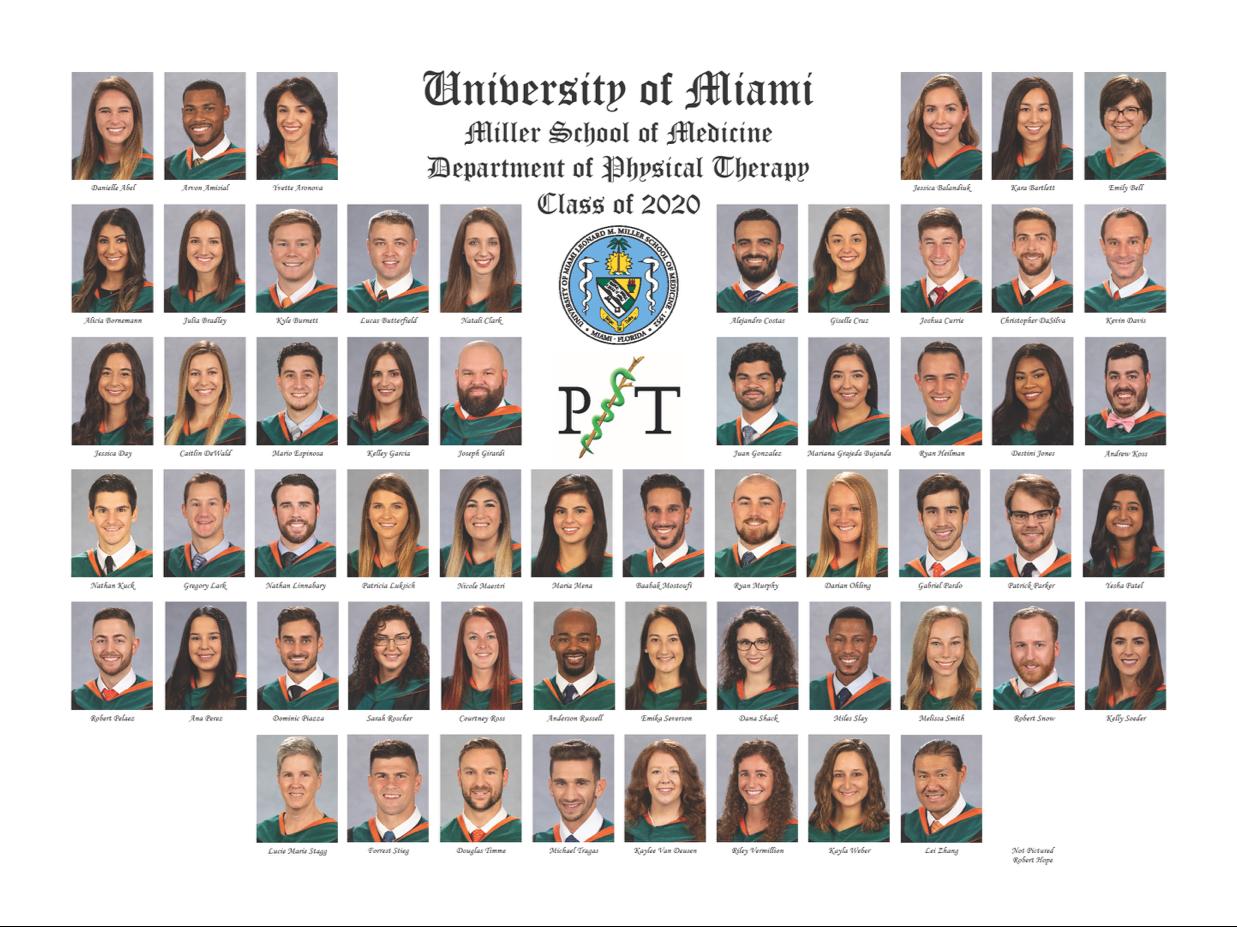
In March of 2020, our lives were put on hold as Covid-19 brought our academic and clinical operations to a halt. The pause in operations was brief, as the clinicians and residents quickly pivoted to e-visits and telehealth services, the faculty and staff converted the academic curriculum to virtual teaching, and the students adapted to a new way of learning. In May, 59 new clinicians were welcomed into the profession, and we were able to virtually celebrate the accomplishments of UMPT Class of 2020.
As Spring turned to Summer, and then to Fall, we dealt with illness and fear within our own family, but we continued to move forward. The clinics modified schedules, facilities, and policies to continue to provide the highest level of care to as many patients as possible. The faculty developed new ways to safely bring students into the classroom. Dozens of new DPT and PhD students, and residents in all specialty areas, started their professional journeys. As is customary for the UMPT family, we banded together as we endeavored to keep our mission moving forward.
As a global pandemic has asserted itself as the backdrop of 2020, the clinicians, faculty, students, and staff that make up the UMPT family have continued to march forward with flexibility, adaptability, resilience, creativity, and an incredible amount of hard work. In this year of unimaginable uncertainty, longstanding racial injustice and short-term political unrest have added further to the fear and frustration.
As is customary for the UMPT family, we banded together as we endeavored to keep our mission moving forward.
As a global pandemic has asserted itself as the backdrop of 2020, the clinicians, faculty, students, and staff that make up the UMPT family have continued to march forward with flexibility, adaptability, resilience, creativity, and an incredible amount of hard work.
Although many forces are working to divide our country and our community, I am proud to be part of this team of remarkable individuals who have shown great compassion and have held a firm moral ground in these unprecedented times.
In this first annual newsletter, we reflect on the last few years, as we look forward to the next decade. We will review the accomplishments of our clinicians, our residents, our students, and our faculty. Challenges remain, but our steadfast commitment to the patients, students, and communities we serve will continue to move us down a path of adaptability and change in 2021. I look forward with great confidence to a bright and productive future as we continue to fulfill all facets of our mission.
A YEAR IN OUR CLINICS
THE UNIVERSITY OF MIAMI PHYSICAL THERAPY CLINICS INCLUDE:


Inpatient care at UHealth Tower
5 outpatient clinics
Physical therapy service at the Sylvester Comprehensive Cancer Center Satellite clinics
THE CLINICAL TEAM TACKLES COVID-19
As with the rest of the world, Physical and Occupational Therapy at UHealth has experienced great change over the last 12 months. The year 2020 started in typical fashion with discussions and plans related to growth, new hires, and raises. However, by mid-March with tremendous teamwork and coordination, we brought our five outpatient clinics to a screeching halt in one weekend. At that time, we were not poised to be able to deliver telehealth, but continuity of patient care was crucial. All but the few remaining post-operative patient appointments were canceled indefinitely.

On extremely short notice, the clinical leadership team developed a plan for clinicians to make courtesy telephonic contact with all patients to communicate our circumstances, do a welfare check, and update home programs. This approach served as a valuable platform from which to develop billable telehealth model. By late April the strong rhythm of communication was converted to billable telehealth visits via Zoom Evaluations and follow up visits were done remotely, and some of the traditional assessment techniques that involve hands-on applications had to be forfeited. Despite this drastic pivot to virtual care, clinicians still made therapeutic connections, used their visual assessment skills, and came up with novel observations techniques such as measuring joint angles goniometrically through the camera.
Outpatients were still being served, and still benefitting from therapy services, some of them much preferring this model over the traditional challenges of commuting, parking, and waiting in full waiting rooms. The month of May saw a phased re-opening of the outpatient clinics that has continued to gather steam ever since, and telehealth volumes gradually declined, but still continue to this day Surprisingly, our specialty services of pelvic rehabilitation and neurological rehabilitation have been our most robust and sustainable telehealth service offerings.
Despite the drastic pivot to virtual care, clinicians still made therapeutic connections, used their visual assessment skills, and came up with novel observations techniques. Unlike our outpatient team, the inpatient team never saw a hiatus in service delivery, but the rhythm did slow with the initial uncertainty of the pandemic. PPE was available, but scarce, and clinicians were not allowed to treat patients without proper protection. Schedules were modified almost weekly, converted to four ten-hour days, and later to three twelve-hour days similar to the nursing schedule model. As the PPE supply stabilized, and the need for service delivery to the COVID units became overwhelming clear, a small team of PT/OT volunteers initiated direct patient care in May with tremendous impact. Since then, the COVID team has expanded, involving more of our inpatient staff.
The need for service delivery to the COVID units became overwhelming clear, a small team of PT/OT volunteers initiated direct patient care in May with tremendous impact
While the world continues to be challenged with the effects of the pandemic, we remain committed to the purpose and vision of being the Premiere Center for Therapy Services in South Florida, and beyond.
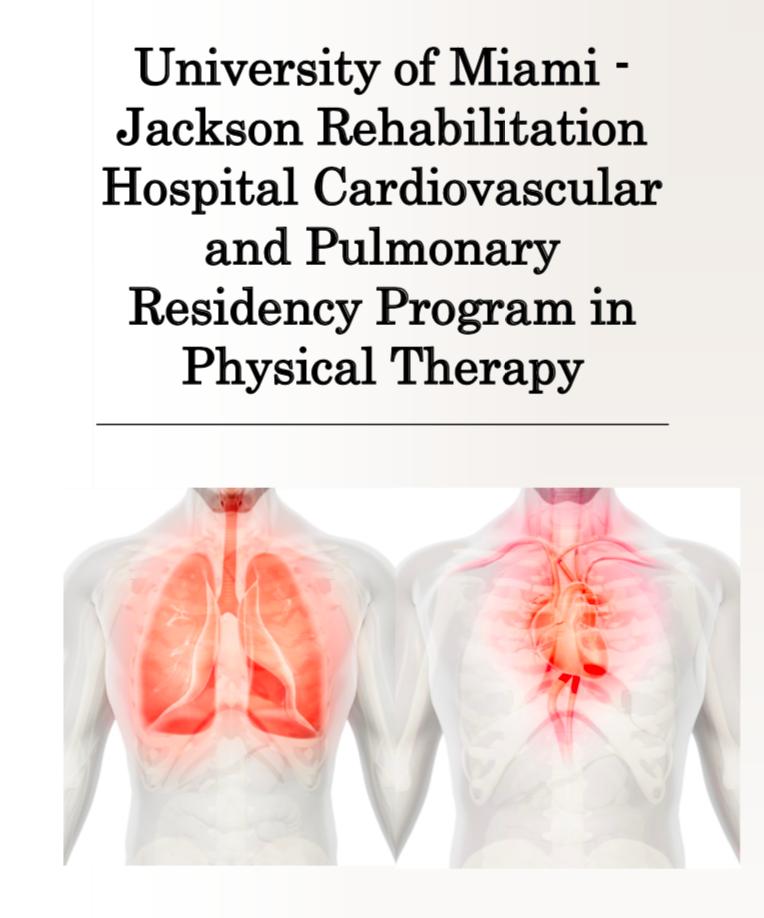
One of the highlights of this difficult time was the esprit du corps that the clinicians demonstrated. The team got to work, pivoted into new arenas of contribution and developed some research data bases. As a result, no pay-cuts or layoffs occurred throughout the pandemic. With 148 clinical team members, and another dozen on the way, the clinical enterprise continues to grow, develop and diversify This past year welcomed the brand new Cardiopulmonary Residency program to our group of other more long-standing residencies in orthopedics, geriatrics, pediatrics, sports, and neuro. Our inpatient presence at Sylvester Comprehensive Cancer Center has expanded and welcomed new full time and part time therapy staff to advance our mission in cancer care.
While the world continues to be challenged with the effects of the pandemic, we remain committed to the purpose and vision of being the Premiere Center for Therapy Services in South Florida, and beyond.
THE YEAR AT A GLIMPSE
Inpatient care
DELIVERED THERAPY SERVICES WITH NO INTERRUPTION DURING THE PANDEMIC
INTRODUCED TELEHEALTH BY APRIL, ONLY A MONTH AFTER THE SHUTDOWN BEGAN
GREW TO 148 CLINICAL TEAM MEMBERS, WITH MORE ON THE WAY
WELCOMED THE NEW CARDIOPULMONARY RESIDENCY, AND EXPANDED CARE THE SYVLVESTER COMPREHENSIVE CANCER CENTER
Outpatient care Our Clinical Team New Growth
OUR CLINIC DIRECTORS:



 TERESA GLYNN Vice Chair of Clinical Services
MARLON WONG Assistant Vice Chair of Clinical Services
CHRIS VITOLO Assistant Vice Chair of Clinical Services
MARLON PEREIRA Manager, UHealth Towers Outpatient
CHELSEA MILLER Manager, CRB Pain Clinic
TERESA GLYNN Vice Chair of Clinical Services
MARLON WONG Assistant Vice Chair of Clinical Services
CHRIS VITOLO Assistant Vice Chair of Clinical Services
MARLON PEREIRA Manager, UHealth Towers Outpatient
CHELSEA MILLER Manager, CRB Pain Clinic




 LUIS FEIGENBAUM Senior Associate Athletic Director for Performance, Health, and Wellness
NORIS PEREZ Manager, Lennar Clinic
CRISTINA PACHECO Manager, UHealth Towers Inpatient
ANNEMAY LELIS Manager, Oncology Rehab Services
RICH MANCINI Manager, Plantation Clinic
LUIS FEIGENBAUM Senior Associate Athletic Director for Performance, Health, and Wellness
NORIS PEREZ Manager, Lennar Clinic
CRISTINA PACHECO Manager, UHealth Towers Inpatient
ANNEMAY LELIS Manager, Oncology Rehab Services
RICH MANCINI Manager, Plantation Clinic



 NELSON TRETO Manager, Kendall Clinic
GAYLENE HORSFALL Manager, Hand Services
JENNIFER ZAMORA Director of Front Office Business Operations
TOM DREVYN Compliance Manager
JESSICA FIRMEZA Manager, Cardiac and Pulmonary Rehabilitation Clinic
NELSON TRETO Manager, Kendall Clinic
GAYLENE HORSFALL Manager, Hand Services
JENNIFER ZAMORA Director of Front Office Business Operations
TOM DREVYN Compliance Manager
JESSICA FIRMEZA Manager, Cardiac and Pulmonary Rehabilitation Clinic
UMPT RESPONDS TO COVID-19
It was in late April that the PT Department received a distress call from the COVID ward.
There were certain patients who simply weren’t getting better, and they couldn’t go without physical therapy any longer.
TREATING COVID PATIENTS AT THE UNIVERSITY OF MIAMI HOSPITAL
Dr. Marcus Jackovitz, PT, DPT, is an inpatient physical therapist at the University of Miami Hospital (UMH). Here, he shares a firsthand account of his experience treating COVID patients throughout the pandemic:

"The Coronavirus pandemic was a surprise to all of us - the Physical Therapy Department at University of Miami Hospital (UMH) was no exception. In the following paragraphs, I will try to outline the UMH Physical Therapy Department’s overall response to the Coronavirus pandemic from the perspective of a physical therapist. I want to underline the fact that mine is a single perspective, and there were many other therapists, clinical assistants, managers, and staff that contributed to our effort.
In March, when the reality of the pandemic was setting in, the hospital began to receive COVID patients.
Hospital administration determined that there was not enough personal protective equipment (PPE) available to send physical therapists to the COVID ward. Our role at the time was to facilitate as many discharges as possible to prepare the hospital for the impending deluge of COVID patients. We were trying to get used to changes such as wearing PPE every day. Though we were uncomfortable in the masks, gowns, and face shields, we considered ourselves lucky because we had access to N-95 masks.
It was in late April that the PT Department received a distress call from the COVID ward. There were certain patients who simply weren’t getting better, and they couldn’t go without physical therapy any longer.

Though their lungs showed signs of improvement, these patients had been so ravaged by coronavirus and the resulting weeks-long hospital stay, that they were severely deconditioned. Most of our initial patients were suffering from muscle atrophy, ICU delirium, encephalopathy, PTSD, or some combination thereof. I remember the day that my supervisor asked for volunteers to go the COVID ward. Four of us raised our hands at first. Many others joined us later.
Many of the challenges of providing physical therapy in a COVID ward were immediately apparent. The process of donning all the PPE necessary to enter the sealed off hallway was terrifying, but we had a wonderful nurse to walk us through it. Most of the patients we saw initially were ICU level patients. They were attached to all sorts of monitoring equipment, IV’s, catheters, and often ventilators. Our time in the unit had to be limited because at the time, the risk of infection with prolonged exposure was not known. This was combined with the excessive perspiration and exhaustion that resulted from wearing so much PPE while mobilizing patients requiring maximum assistance. It was not uncommon for me to change scrubs three times in one day because I had sweat through them.
Initially, we entered the COVID ward in teams of three - one physical therapist, one occupational therapist, and one clinical assistant. The team approach was crucial to our success and safety. Within a few weeks, we had rehabilitated numerous patients to the point of discharge. When one of our first COVID patients, who had been at the hospital for 2 months at this time, finally recovered to the point of discharge, we lined the hallways to say goodbye to him. It felt like we had won the pandemic. It was the end of May and we had no idea what still lay in store for us.
We were starting to think that Florida might not get as bad as New York, but then our case numbers started creeping up. We had to seal off another hallway for coronavirus patients, then a whole ward was sealed off, followed by a whole floor. It was a good thing that UMPT worked so hard to facilitate discharges in earlier months, because we needed the space badly. At one point, parts of 5 floors of the hospital were dedicated to COVID patients.

In its essence, physical therapy did not change during this time: it was always about helping people regain their functional independence. It became a lot more personal, though. I remember meeting a patient for an initial evaluation, getting to know them and learning about their lives. Two days later I would see them on a high flow nasal cannula. The next day they were intubated, and soon after lost their life.

In its essence, physical therapy did not change during this time: it was always about helping people regain their functional independence. It became a lot more personal, though.
I remember incorporating family time into therapy whenever possible. No family visits were allowed, so we used a tablet and encouraged patients to sit up while they talked to their loved ones. I will never forget the fear and sadness in the faces and voices of family members, or the despair patients felt when we couldn’t connect to their loved ones. I remember patients asking to talk to their families because they thought they were dying. It was an incredibly challenging setting in which to be a physical therapist, or even just a person, for that matter.
As the case numbers started to drop, and the hospital gained control of the surge in patients, we started to lick our wounds and assess what had happened. It was September at this point, and we were exhausted physically, mentally, and emotionally. We had learned to provide therapy in very challenging and stressful situations and how to adapt our exercise programs for people that were confined to the short leash of a high flow nasal cannula or a ventilator. We did a lot of good for a lot of people and we continue to work at it to this day. As more research comes out, we continue to refine our methods, and we won’t stop.
If there is one thing that you should know about the role of physical therapy in the coronavirus pandemic, it’s that we are an absolutely essential part of the treatment team. In the coming years, therapists that work in every setting will help coronavirus patients reclaim their mobility and their lives after coronavirus. The work to provide therapy for this population has really only begun, and we will be treating COVID survivors for a long time to come.
- Dr. Marcus Jackovitz, PT, DPT

It was an incredibly challenging setting in which to be a physical therapist, or even just a person, for that matter.
Shortly after the start of the COVID-19 pandemic, the Cardiovascular and Pulmonary Section of the APTA initiated the development of the PostAcute Covid-19 Exercise & Rehabilitation (PACER) Project.
The goal of the PACER Project was to provide online educational courses to assist physical therapists with the knowledge and skills needed to care for COVID-19 patients. A total of 16 PACER Project presentations were developed by physical therapists from the United States and abroad, and posted on Youtube and the APTA website.
Two of the PACER Project presentations were developed by Lawrence Cahalin PhD, PT who is a Clinical Professor in the Department of Physical Therapy. They included one presentation on respiratory muscle testing and training, and another presentation on the use of blood flow restriction training both of which have application to Covid19 rehabilitation.
The presentation on respiratory muscle testing and training also included Magno F. Formiga PhD, PT who completed his PhD in 2019 in the Department of Physical Therapy at the University of Miami.
T H E P A C E R P R O J E C T U M P T F A C U L T Y C O N T R I B U T E T O C O V I D - 1 9 E D U C A T I O N A L I N I T I A T I V E
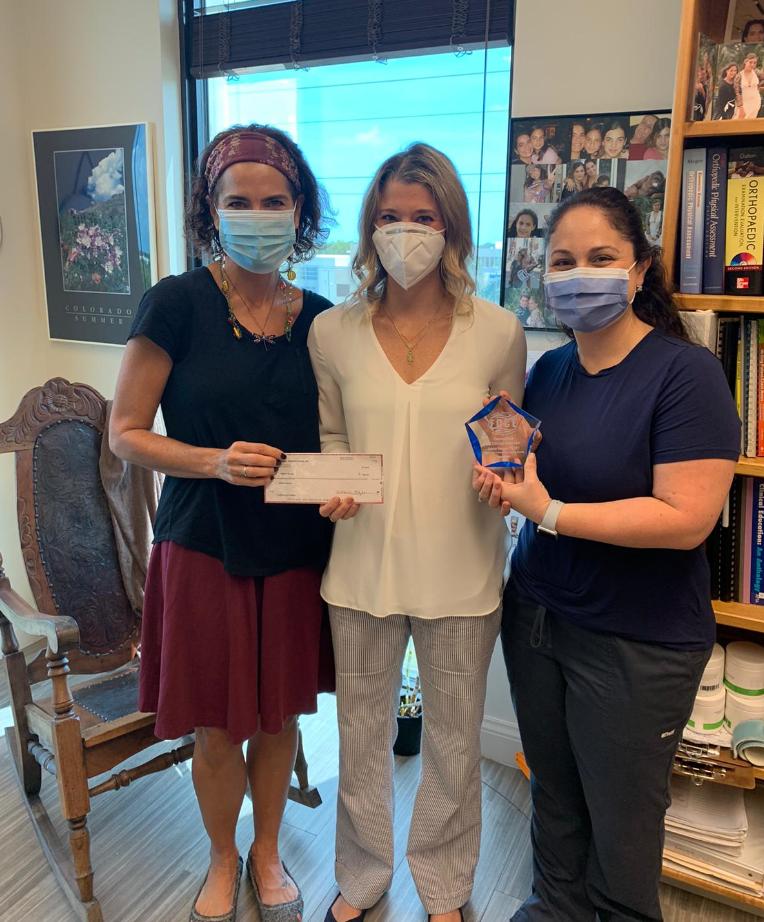
UMPT DEPARTMENTAL RECOGNITIONS



F A C U L T Y M E M B E R
Dr. Meryl Cohen, DPT, MS, FAPTA
C L I N I C I A N
Dr. Annemay Lelis, PT, DPT, CLT
2020 Teacher of the Year Award
S T A F F M E M B E R
Jean Fowler, Vice Chair of Administration
2020 FPTA award for Excellence in Academic Teaching.
Associate Editor for the Journal of Neurologic Physical Therapy, Mentored
Translational Research Scholars Program Award (KL2)
2020 Outstanding Clinical Instructor Award from the Florida Consortium of Clinical Educators

Distinguished Fellow of the National Academies of Practice, Board of Directors of the Physical Therapy Learning Institute
Lucy Blair Service Award
Associate Professor of Clinical Physical Therapy



F A C
U L T Y A W A R D S
B R Y O N S M I T H 2020 J O Y C E G O M E S - O S M A N
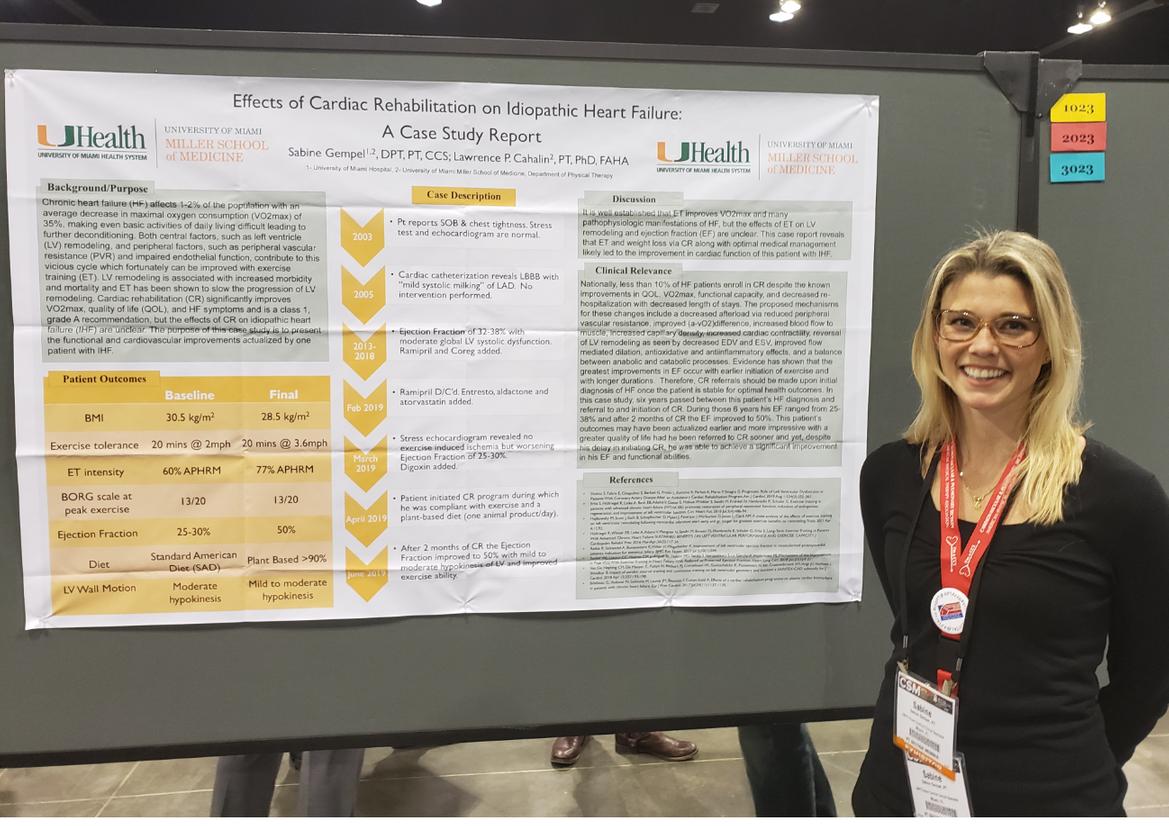
S A B I N E G E M P E L
G R E G O R Y H A R T L E Y
E L S A D R E V Y N
Z A H I L L Y S A L I N A S
B R Y O N S M I T H
F A C U L T Y R E C O G N I T I O N S
2019

M E R Y L C O H E N
R O B E R T G A I L E Y
K A T H R Y N R O A C H
C A R O L D A V I S
M I C H E L E R A Y A
O T H E R F A C U L T Y R E C O G N I T I O N S 2020
F A C U L T Y R E C O G N I T I O N S 2018

M E R Y L C O H E N
G R E G O R Y H A R T L E Y
R O B E R T G A I L E Y
M A R K N A S H
M I C H E L E R A Y A
U M P T R E C O G N I Z E S T H E F U L L T E A M O F
F A C U L T Y M E M B E R S
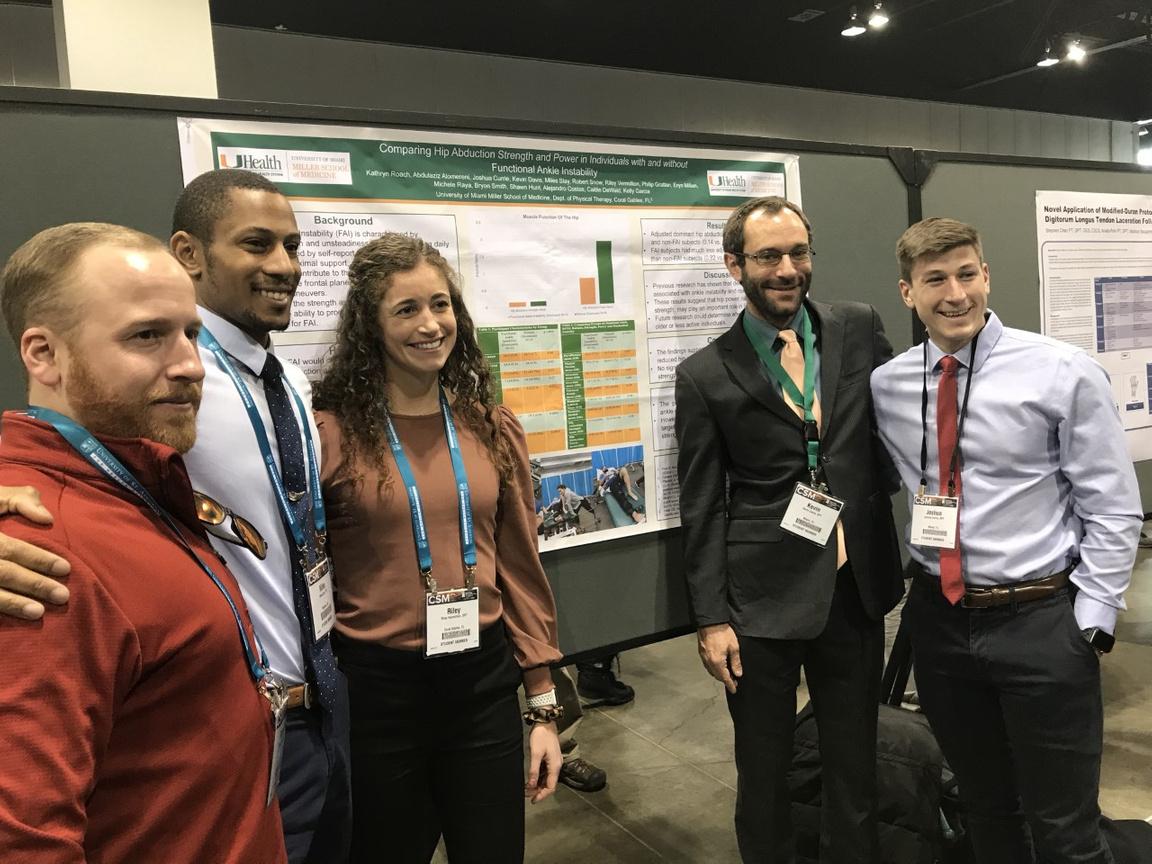
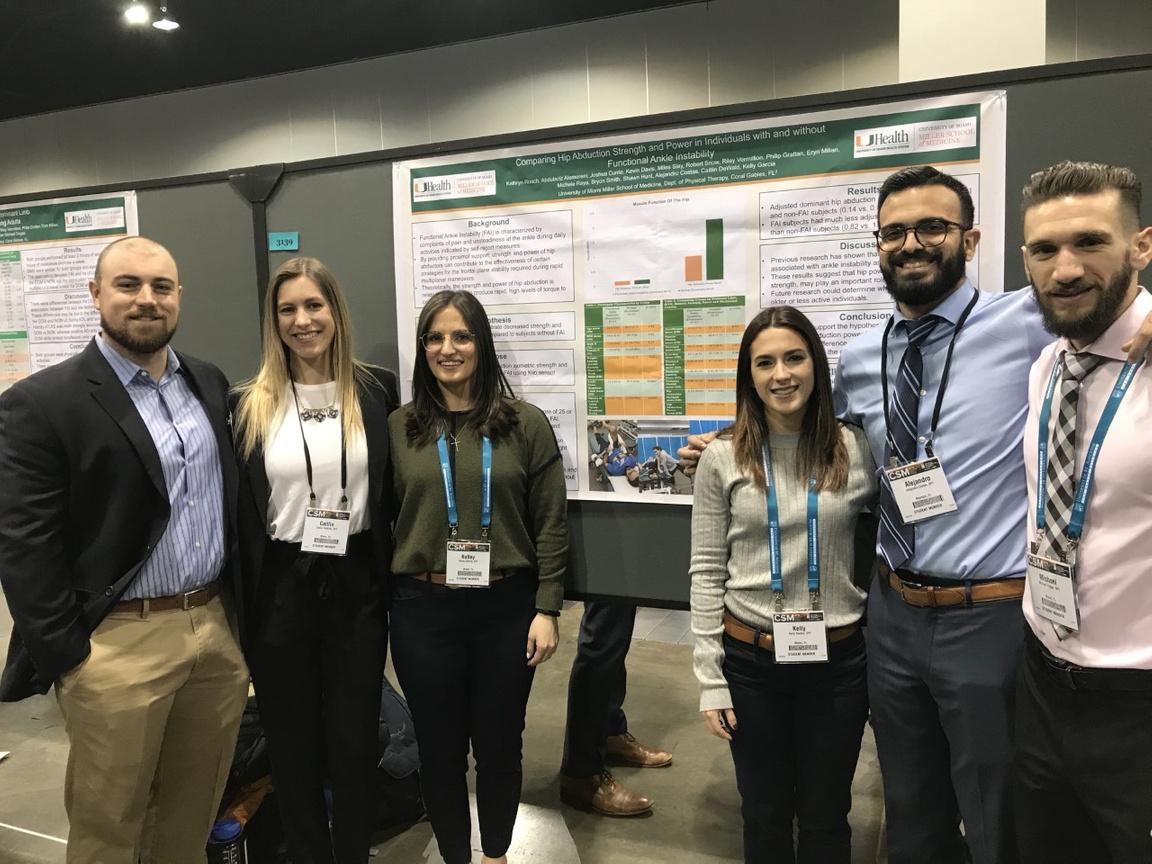
APTA COMBINED SECTIONS MEETING
IN 2020, THE UM DEPARTMENT OF PHYSICAL THERAPY PRESENTED...
35 education sessions, platform presentations, and posters, on topics including cardiopulmonary, education, sports, orthopedics, geriatrics, acute care, health policy and administration, neurology, oncology, pelvic health, and amputee rehabilitation.
NOTABLE PRESENTATIONS INCLUDED...
Lead speaker Dr. Amanda Clifton, a recent UM Pediatric Residency graduate, was joined by faculty members Dr. Moore and Dr. Cahalin, and 2nd year DPT students Yesha Patel and Giselle Cruz, to present their research: "Sternal Precautions and Prone
Positioning of Infants Following Median Sternotomy: A Nationwide Survey," published in Pediatric Physical Therapy

2 0 2 0 D e n v e r , C O
IN 2019, THE UM DEPARTMENT OF PHYSICAL THERAPY PRESENTED:
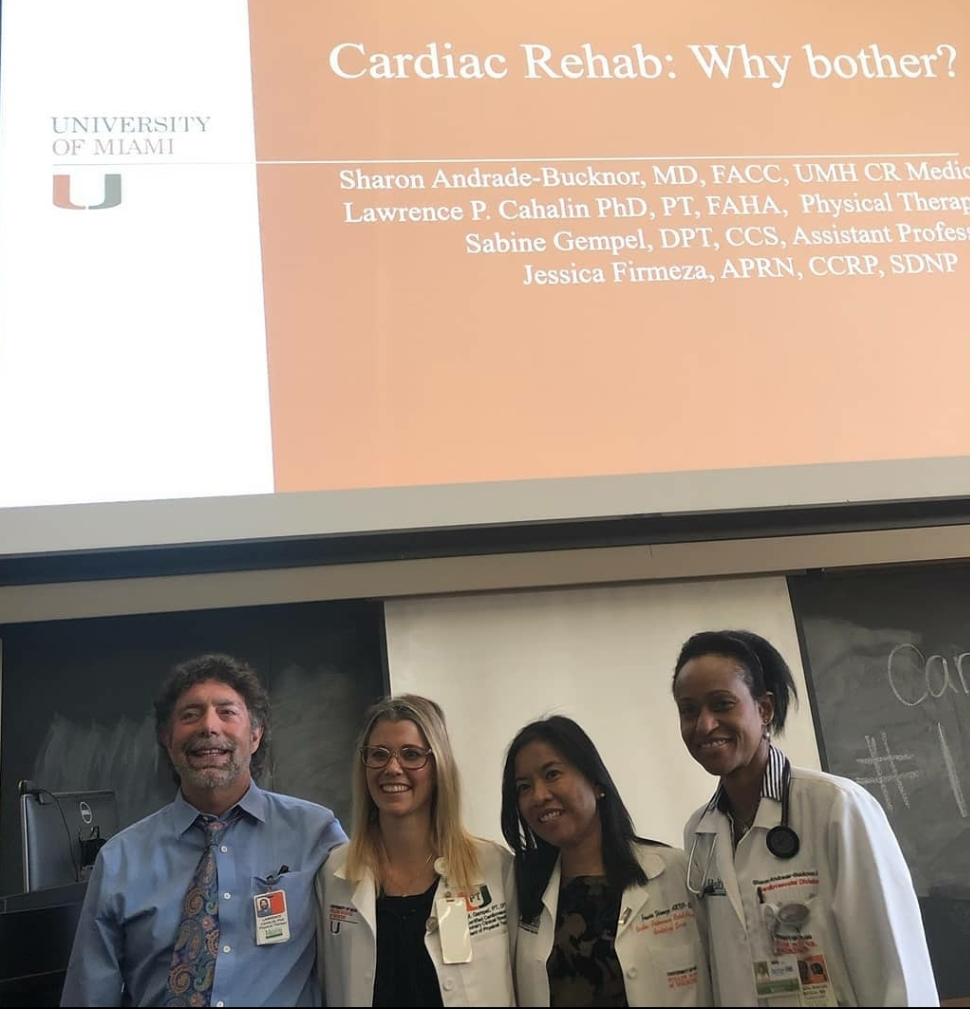


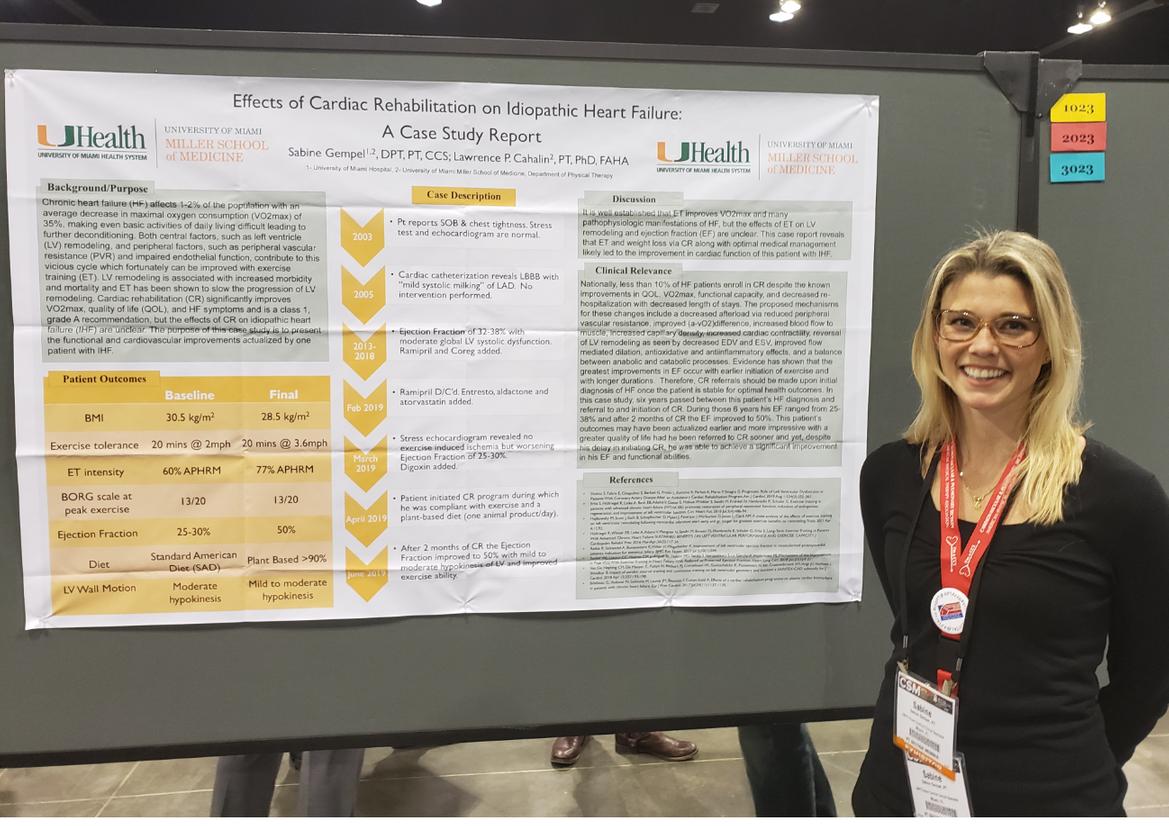
33 education sessions, platform presentations, and posters, spanning all physical therapy specialties.
IN 2018, THE UM DEPARTMENT OF PHYSICAL THERAPY PRESENTED:
42 education sessions, platform presentations, and posters, spanning all physical therapy specialties.
2 0 1 8 N e w O r l e a n s , L A 2 0 1 9 W a s h i n g t o n , D C
OTHER NATIONAL AND INTERNATIONAL PRESENTATIONS
APTA Education Leadership Conference
APTA National Student Conclave
APTA NEXT Conference
International Association for the Study of Pain (IASP) Virtual Series on Pain & Expo
Australian Orthotic and Prosthetic Association National Conference
Spinal Cord Association Annual Meeting
PRISM Conference
International Congress British Fascia Symposium
Monthly McKnight Research Meetings
4th Annual Neural Engineering Symposium
UMPT FACULTY INVITED PRESENTATIONS:
UMPT FACULTY INVITED PRESENTATIONS: 2020 2019
APTA Education Leadership Conference
National Academies of Practice Annual Meeting and Forum
World Confederation for Physical Therapy (WCPT)
American College of Surgeons Clinical Congress
UMH & Jackson's Cardiology Grand Rounds
FPTA Annual Meeting
APTA Academy of Pediatric Physical Therapy Conference
International Society of Prosthetics and Orthotics World Congress
American College of Sports Medicine (ACSM) Annual Meeting
FPTA Student Conclave
UHealth Sports Medicine Morning Conference
Academy of Physical Medicine & Rehabilitation Annual Assembly
2018 UMPT FACULTY INVITED PRESENTATIONS:
APTA Education Leadership Conference
APTA NEXT Conference
FPTA Annual Conference
International Stroke Conference Annual Meeting
Society of Student-Run Free Clinics Conference
OTWorld Congress
Australian Orthotic Prosthetic Association National Assembly
Atlantic Coast Conference Sports Medicine Association's Annual Clinical Symposium
UHealth Sports Medicine Morning Conference
The Dutch Congress of Rehabilitation Medicine
Annual Meeting of the American Spinal Injury Association
Annual Conference of the Southwest Chapter of the American College of Sports Medicine

UM DPT PROGRAM UPDATES

ADAPTING OUR CURRICULUM TO COVID

S i n c e M a r c h 2 0 2 0 , w e h a v e s e e n d r a s t i c c h a n g e s i n t h e
m a n n e r i n w h i c h w e d e l i v e r o u r c u r r i c u l u m . O n
M a r c h 6 , t h e D P T 1 a n d D P T 2 s t u d e n t s p r e s e n t e d a f a n t a s t i c H u r r i c a n e C h a l l e n g e f o r M i a m i - D a d e S c h o o l
C h i l d r e n w i t h s p e c i a l n e e d s . O n t h a t h i g h n o t e , t h e y l e f t f o r a m u c h - n e e d e d S p r i n g B r e a k . I n t h e m e a n t i m e , t h e C o v i d - 1 9 v i r u s w a s g a i n i n g m o m e n t u m
i n S o u t h F l o r i d a . F a c u l t y a n d s t a f f s t o c k e d u p o n m a s k s a n d h a n d s a n i t i z e r s a s t h e v i r u s e x p l o d e d i n t h e c o m m u n i t y .
A f e w d a y s l a t e r , P r e s i d e n t F r e n k a n n o u n c e d t h a t a l l c l a s s e s w o u l d p i v o t t o 1 0 0 % o n l i n e , p r o h i b i t i n g a n y i n - p e r s o n c l a s s e s a n d e x t e n d i n g S p r i n g B r e a k t o a l l o w f a c u l t y t i m e t o p r e p a r e f o r a n a l l - v i r t u a l e n v i r o n m e n t . A f e w d a y s l a t e r , t h e C l a s s o f 2 0 2 0 w a s r e m o v e d f r o m t h e c l i n i c a l e n v i r o n m e n t , a n d t h e C l i n i c a l e d u c a t i o n t e a m g o t t o w o r k t o s e e k g u i d a n c e f r o m o u r p r o f e s s i o n a l o r g a n i z a t i o n s t o n a v i g a t e t h e i m p a c t o f t h e s e c h a n g e s o n c o m p l e t i n g c l i n i c a l e x p e r i e n c e s . W i t h m u c h w o r r y a n d h a r d w o r k , w e w o r k e d t o e n s u r e t h a t e a c h a n d e v e r y o n e o f o u r g r a d u a t e s w a s r e a d y f o r p r a c t i c e . I n M a y , w i t h g r e a t f a n f a r e , w e c e l e b r a t e d t h e g r a d u a t i o n

o f 5 9 n e w p h y s i c a l t h e r a p i s t s w i t h a

j o y f u l Z O O M g r a d u a t i o n a w a r d s
c e r e m o n y !
M e a n w h i l e , t h e f a c u l t y q u i c k l y m o d i f i e d s y l l a b i , a n d m o v e d a l l
l e c t u r e m a t e r i a l f o r w a r d , c o n v e r t e d
t o v i r t u a l f o r m a t . M o s t f a c u l t y h a d n e v e r u s e d Z o o m o r
B l a c k b o a r d C o l l a b o r a t e , a n d t h e l e a r n i n g c u r v e w a s s t e e p ! L a b s w e r e p u s h e d i n t o t h e f u t u r e , a s w e m i s t a k e n l y t h o u g h t t h a t w e w o u l d
b e b a c k t o n o r m a l i n a f e w w e e k s . R e a l i z i n g t h a t t h e s e c h a n g e s w o u l d
b e l o n g - t e r m a n d e x t e n d a t l e a s t i n t o S u m m e r , w e d e v e l o p e d a p l a n t o c o n t i n u e o u r h a n d s - o n l a b e x p e r i e n c e s s a f e l y .
B y t h e S u m m e r , a n e w c l a s s o f 6 2 s t u d e n t s j o i n e d t h e f a m i l y w i t h a v i r t u a l o r i e n t a t i o n a n d a s h i f t i n t h e c u r r i c u l u m . P e r m i s s i o n w a s g r a n t e d f r o m t h e P r o v o s t a n d
P r e s i d e n t t o h o l d i n - p e r s o n l a b s w i t h 1 0 t o a r o o m , w i t h m a s k s a n d s h i e l d s , p r e s c r i b e d r o o m a n d b u i l d i n g f l o w , r e g u l a r t e s t i n g a n d s c r e e n i n g .
A v i r t u a l W h i t e C o a t C e r e m o n y c e l e b r a t e d t h e r e a d i n e s s o f t h e C l a s s o f 2 0 2 2 t o m o v e i n t o t h e c l i n i c . O u r a g i n g a u d i o v i s u a l s y s t e m w a s r i g g e d a n d m a n i p u l a t e d t o a l l o w s t r e a m i n g b e t w e e n h a l f - f u l l c l a s s r o o m s . S t a f f d e v e l o p e d p l a n s t o e n s u r e t h a t a l l p r o t o c o l s w e r e m e t , a n d t h e t e a m p u l l e d t o g e t h e r t o m a k e s u r e t h e l e a r n i n g c o n t i n u e d .

S u m m e r t u r n e d t o F a l l , t h e i c a l E d u c a t i o n t e a m w o r r i e d s t u d e n t s w o u l d n o t b e a b l e t o p l e t e t h e i r i n t e r n s h i p s , b u t a c u l o u s l y , o u r c o m m u n i t y n e r s a n d t h e c l i n i c a l e d u c a t i o n m e n s u r e d t h a t a l l 1 2 0 s t u d e n t s e p l a c e d i n t h e c l i n i c ! B y t h e o f F a l l , a l m o s t a l l s t u d e n t s e o n t r a c k a n d r e a d y f o r a l o n g d a y B r e a k .
F a s t f o r w a r d t o t h e S p r i n g s e m e s t e r . S t u d e n t s , f a c u l t y , a n d s t a f f h a v e a l l p u l l e d t o g e t h e r t o m a n a g e t h e “ n e w n o r m a l ” i n w h i c h w e f i n d o u r s e l v e s . T h e f a c u l t y h a s g a i n e d n e w s k i l l s i n v i r t u a l t e a c h i n g , s t u d e n t s h a v e a d j u s t e d t o v i r t u a l l e a r n i n g , c l a s s r o o m s h a v e b e e n u p g r a d e d t o g r e a t l y e n h a n c e t h e s t u d e n t a n d f a c u l t y e x p e r i e n c e , a n d w e h a v e a l l l e a r n e d h o w t o f u n c t i o n t h r o u g h m a s k s a n d s h i e l d s .
W e c o n t i n u e t o f e e l t h e t h i n g s t h a t w e h a v e l o s t : t h e S a i l i n g C o u r s e , t h e L A G O c l i n i c , t h e H u r r i c a n e C h a l l e n g e . B u t w e h a v e l e a r n e d s o m u c h , w e h a v e f o c u s e d a n d p r i o r i t i z e d , w e h a v e m a d e t h e v e r y b e s t o f t h e s i t u a t i o n w e a r e i n , a n d f i n a l l y w e s e e s o m e l i g h t o n t h e h o r i z o n .
V a c c i n e s a r e c o m i n g , t h e l e a r n i n g c o n t i n u e s , n e w c o u r s e s h a v e b e e n d e v e l o p e d , a n d o l d c o u r s e s h a v e b e e n r e i m a g i n e d . A s w e f a l l i n t o a “ n e w n o r m a l , " w e w i l l i n e v i t a b l y b e a b l e t o c o m e t o g e t h e r a g a i n p h y s i c a l l y , b u t w i t h n e w s a f e g u a r d s a n d p r o t o c o l s i n p l a c e . W e w i l l h o l d o n t o t h e p o s i t i v e s t h a t h a v e c o m e f r o m t h i s e x p e r i e n c e , a n d w e w i l l c e l e b r a t e t h e l e a r n i n g t h a t c o n t i n u e s a s w e c r e a t e a n e w w a y t o s u p p o r t e a c h o t h e r . K u d o s a n d g r a t i t u d e t o t h e e n t i r e U M P T f a m i l y f o r n a v i g a t i n g t h i s j o u r n e y t o g e t h e r .
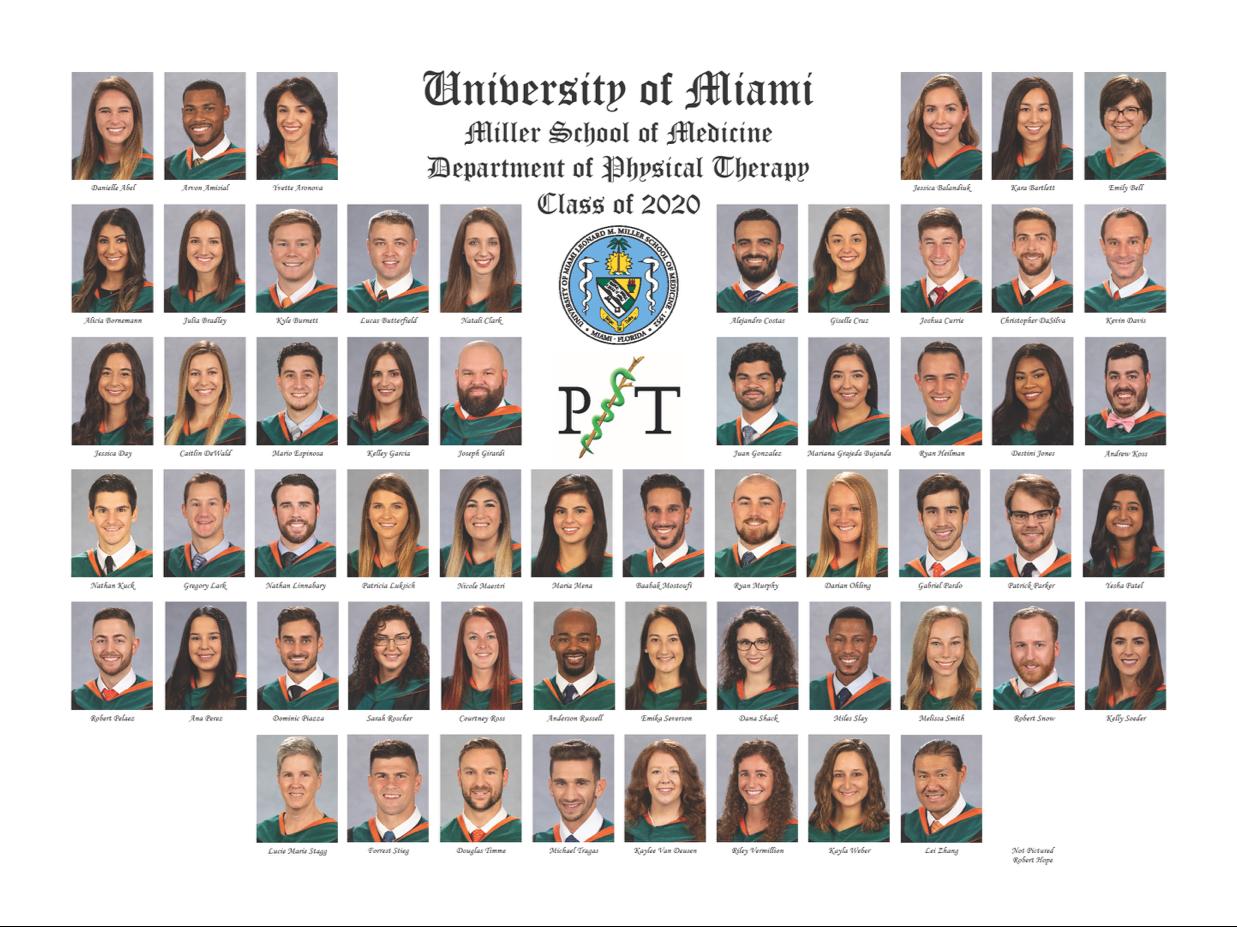
C O N G R A T U L A T I O N S C L A S S O F 2 0 2 0 ! T H E C L A S S O F 2 0 2 1 T H A N K S T H E F A C U L T Y F O R T H E I R S U P P O R T , A D A P T A B I L I T Y , A N D L E A D E R S H I P D U R I N G T H E P A N D E M I C






C L I N I C A L E X C E L L E N C E A W A R D
D r L u c i e M a r i e S t a g g
S T U D E N T L E A D E R S H I P A W A R D
C L A S S O F 2 0 2 0 A W A R D R E C I
E
A C A D E M I C E X C E L L E N C E A W A R D
. E m i l y B e l l D r . C h r i s t o p h e r D a S i l v a D r . E m i k a S e v e r s o n C H A I R ' S A W A R D D r . J u a n G o n z a l e z D r . B a a b a k M o s t o u f i
D r K a y l a W e b e r
P I
N T S
D r
S H E R R I H A Y E S S T U D E N T




S C H O L A R S H I P A W A R D
E X C E L L E N C E I N T H E R A P E U T I C
P R E S E N C E A W A R D
D r . F o r r e s t S t i e g
L I N D A C R A N E M E M O R I A L
S C H O L A R S H I P
D r . A n a P e r e z
R U B L E Y / R O B E R T S S E R V I C E S C H O L A R S H I P
D r . M e l i s s a S m i t h

D r . A l i c i a B o r n e m a n n
S T E V E N J . R O S E S C H O L A R S H I P
D r L u c i e M a r i e S t a g g
Project: Modifiable variables that contribute to walking speed in people with a lower limb amputation.


Advisors: Robert Gailey, Ignacio Gaunaurd, Anat Kristal

A P T A M I N O R I T Y S C H O L A R S H I P A W A R D D r . B r i a n a S a d e S c o t t C l a s s o f 2 0 1 9 D r . J u a n G o n z a l e z C l a s s o f 2 0 2 0 D r . A l i c i a B o r n e m a n n C l a s s o f 2 0 2 0 S T E V E N J . R O S E S T U D E N T R E S E A R C H A W A R D D r . N a t a l i C l a r k D r . E m i k a S e v e r s o n D r . F o r r e s t S t i e g




W E L C O M E C L A S S O F 2 0 2 3 ! C L I N I C A L I N S T R U C T O R E X C E L L E N C E A W A R D 2 0 2 0
D r J u l i a n R i v e r a
D r S e a n B r i m a c o m b e
UM RESIDENCY PROGRAMS
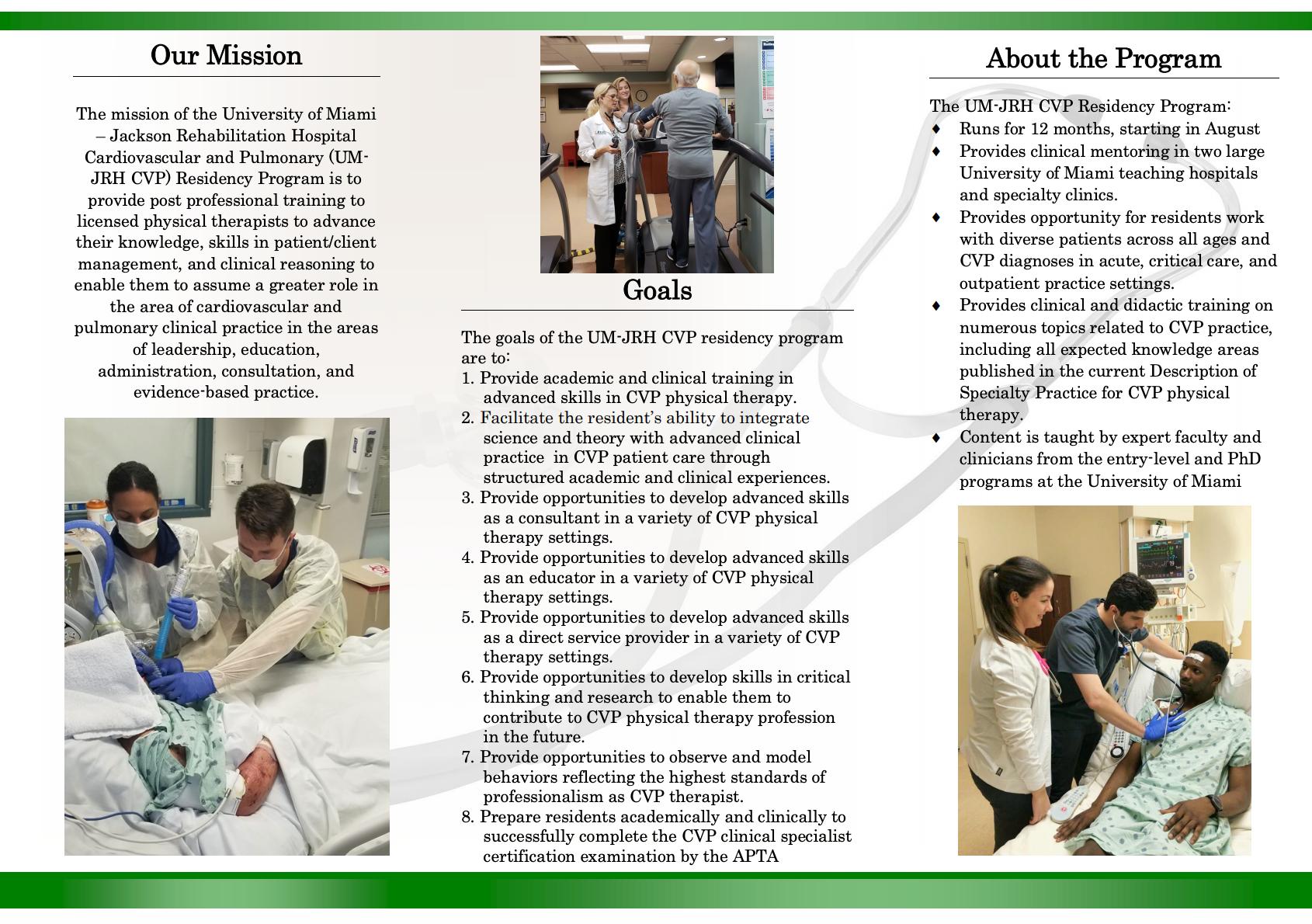
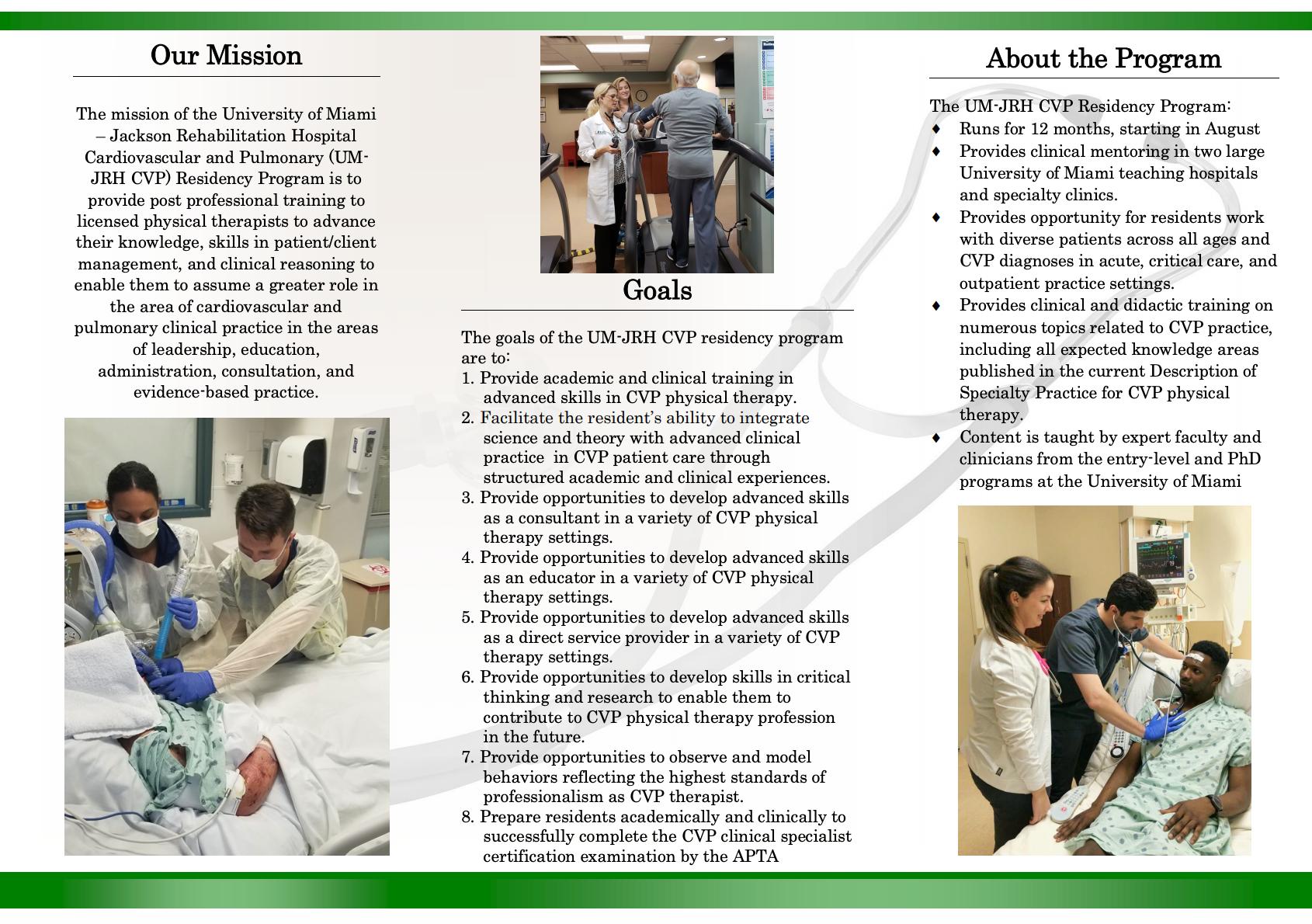
INTRODUCING... OUR NEW CARDIOPULMONARY RESIDENCY 2020-2021!










@umptortho @umptsports @umneuropt
GERIATRICS CARDIOPULMONARY ORTHOPEDICS NEUROLOGY PEDIATRICS SPORTS D i r e c t o r : D r . J e n n i f e r C a b r e r a D i r e c t o r : D r . J a m e s M o o r e D i r e c t o r : D r . M a t t C a r a h e r D i r e c t o r : D r . M e r y l C o h e n D i r e c t o r : D r . M a r l o n W o n g D i r e c t o r : D r . L u i s F e i g e n b a u m @umptcardio @um nchptpeds @umscrhgeript
OUR RESIDENCIES INCLUDE...
LEARN MORE ABOUT OUR RESIDENCIES:
WELCOMING OUR 2020-21 RESIDENTS

UM PH.D PROGRAMS
SPOTLIGHT ON: DR. ANNE PALERMO
Dr. Anne Palermo, PT, DPT, Ph.D. recently completed her doctoral studies in the University of Miami Department of Physical Therapy. Her dissertation work investigated the impact of spinal cord injury on respiratory function and balance.
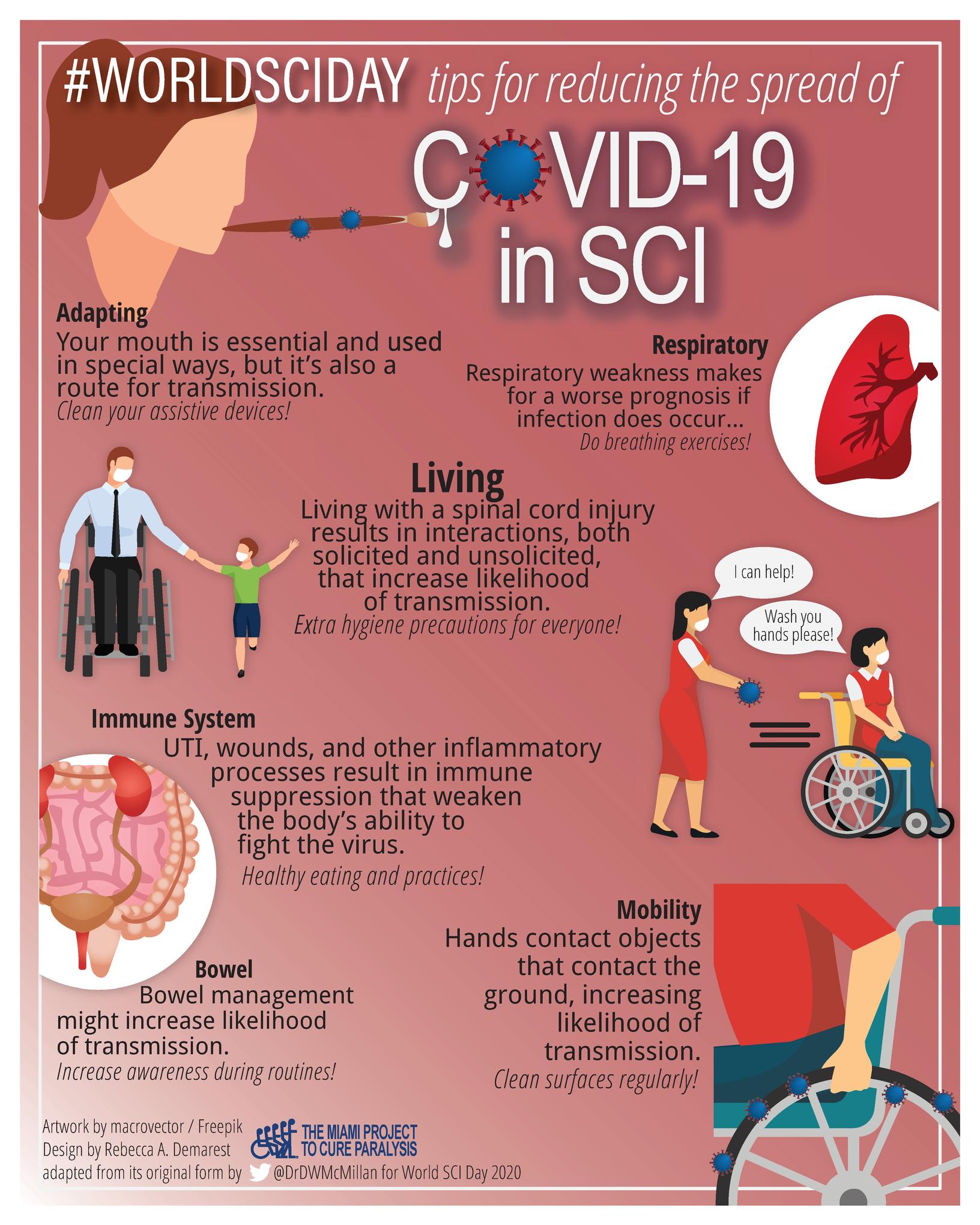
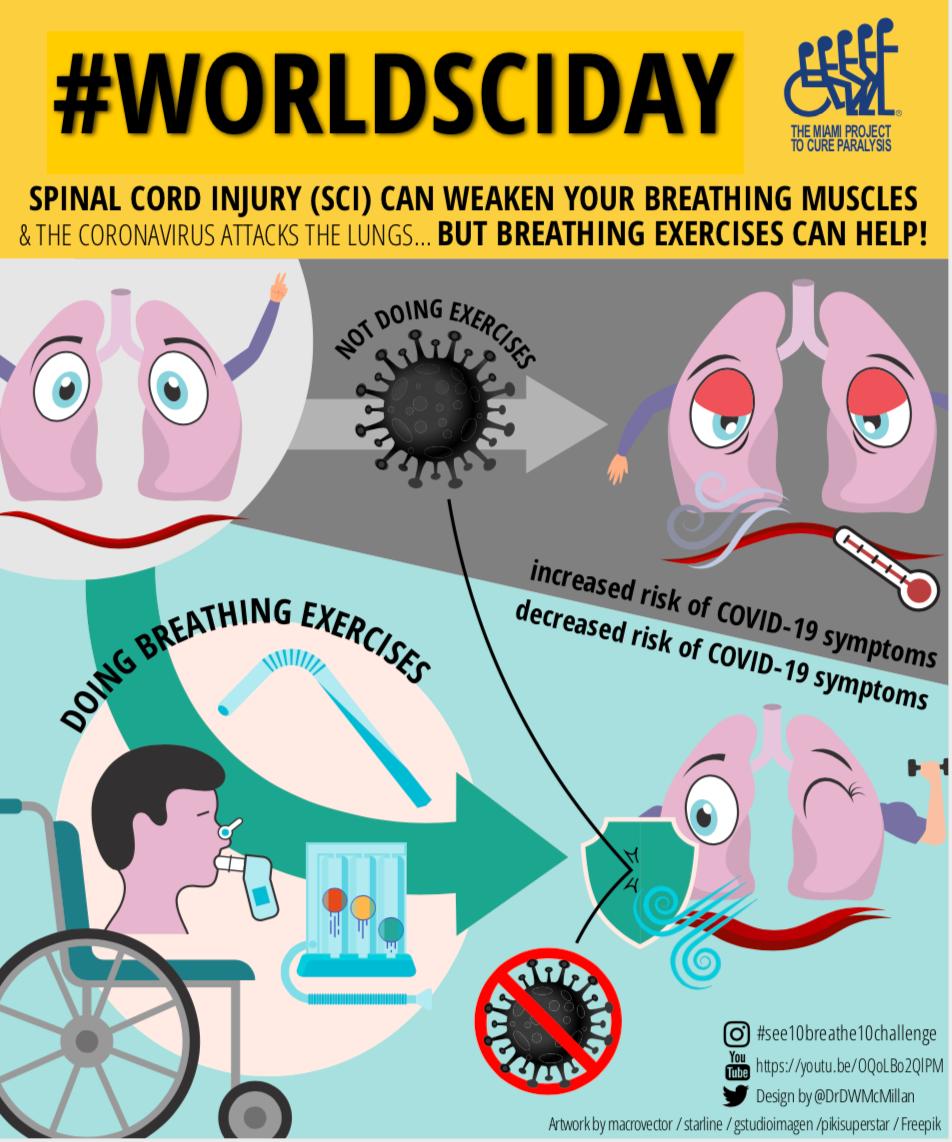
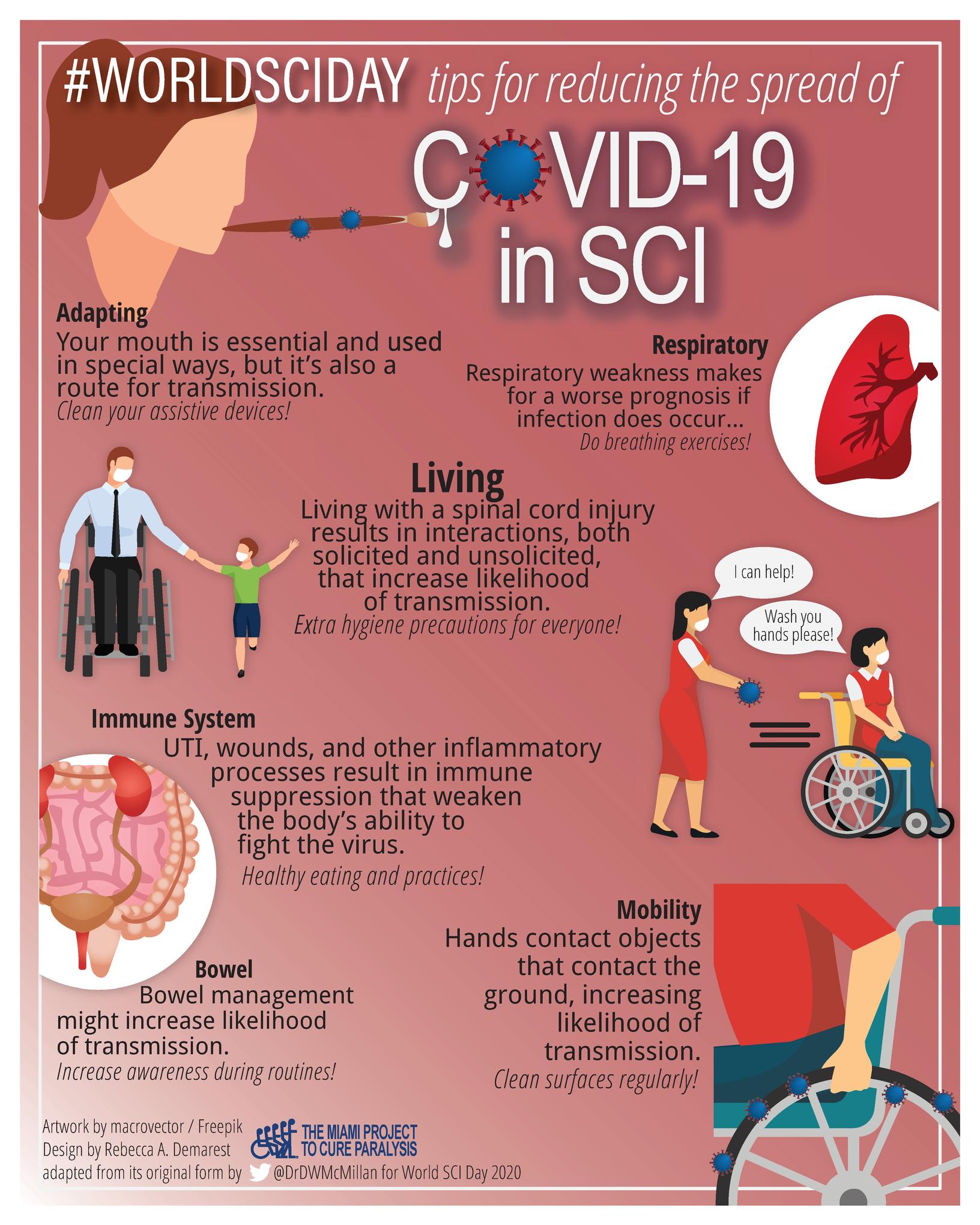
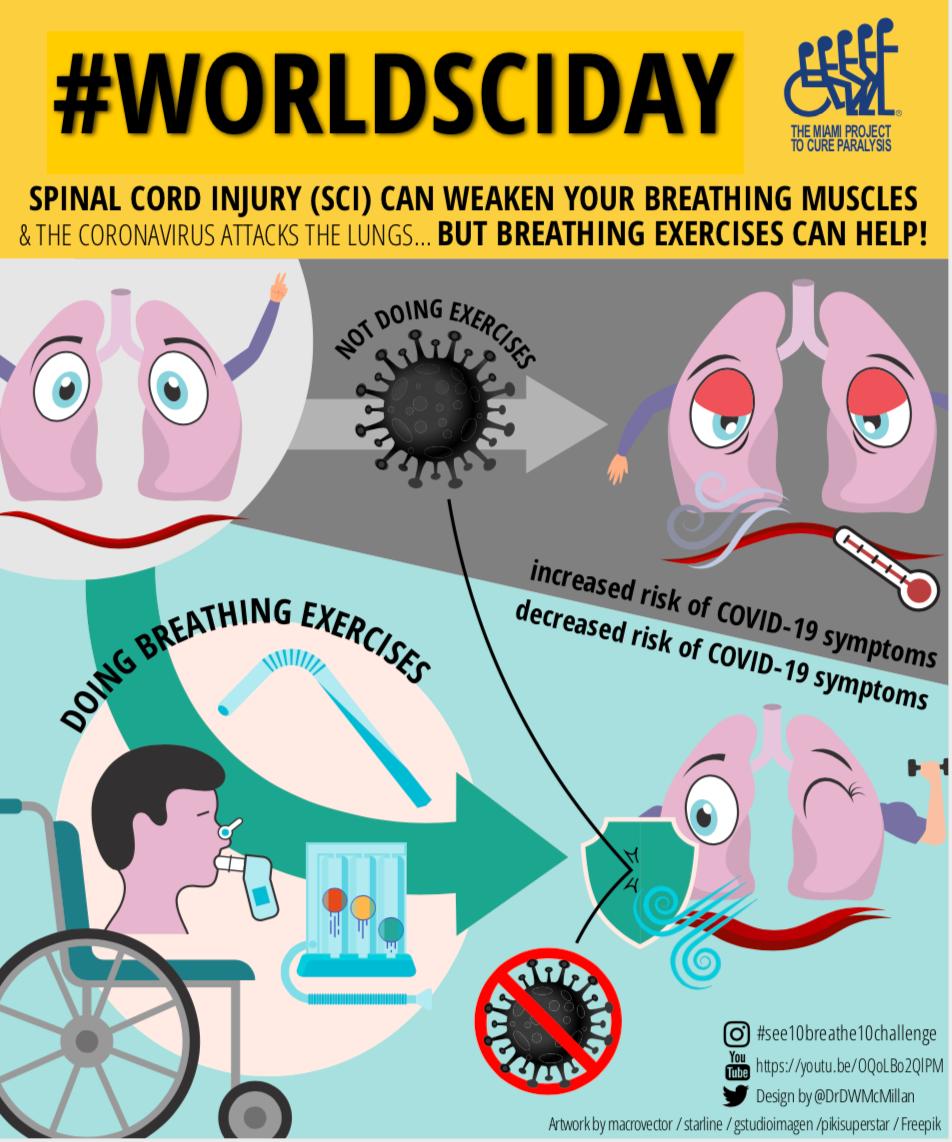
Along with other researchers at The Miami Project to Cure Paralysis, Dr. Palermo was able to disseminate information on respiratory muscles and their relevance to COVID-19 for both SCI clinicians and SCI patients.
For this work, Dr. Palermo was featured in the article "Strengthen Your Lungs Against COVID-19 Symptoms". She also created educational videos in English and Spanish for the #See10Breathe10 Challenge on the topic of respiratory muscle therapy for SCI.
Dr. Palermo also completed an intervention study sponsored via the Promotion of Doctoral Studies II Award (PODS-II) from the Foundation for Physical Therapy Research (FPTR). This grant application was awarded the Mary Lou Barnes Award for receiving being the highest rated application in Neurology.
In the “World SCI Day Poster Contest” hosted by the International Spinal Cord Society, Dr. Palermo contributed to both the 1st place and 3rd place posters, pictured above, on the topic of respiratory health for individuals with SCI
OUR 2019-2020 PH.D GRADUATES
PH.D PUBLICATIONS 2018-2020
2020 MANUSCRIPTS:
Romm MJ, Soyeon A, Fiebert I, Cahalin LP A Meta-analysis of Therapeutic Pain Neuroscience Education, Using Dosage and Treatment Format as Moderator Variables Pain Practice (In Press)
Romm MJ, Soyeon A, Fiebert I, Cahalin LP A Meta-analysis of Group-Based Pain Management Programs: Overall Effect on Quality of Life and Other Chronic Pain Outcome Measures with an Exploration into Moderator Variables that Influence the Efficacy of Such Intervention. Pain Medicine (In Press).
DeLuca ND, Vajta-Gomez JP, Vital I, Cahalin LP, Campos M. The Impact of Yoga on Inspiratory Muscle Performance in Veterans with COPD: A Pilot Study. International J Yoga Therapy (In Press).
Formiga MF, Dosbaba F, Hartman M, Batalik L, Plutinsky M, Brat K, Ludka O, Cahalin LP. Novel versus traditional inspiratory muscle training regimens as homebased, stand-alone therapies in COPD: protocol for a randomized controlled trial Int J Chron Obstruct Pulmon Dis 2020;15:2147-2155
Formiga MF, Fay R, Hutchinson S, Locandro N, Ceballos A, Lesh A, Buscheck J, Meanor J, Owens J, Cahalin LP Effect of Aerobic Exercise Training with and without Blood Flow Restriction on Aerobic Capacity in Healthy Young Adults: A MetaAnalysis Int J Sports Phys Ther 2020;15(2):175-187
Lucarevic J, Schubert M, Clemens S, Applegate B, Bennett C, Gaunaurd I, Gailey R The Relationship Between Vestibular Sensory Integration and Prosthetic Mobility in Community Ambulators with Unilateral Lower Limb Amputation. Phys Ther (In Press)


Palermo AE, Cahalin LP, Garcia KL, Nash MS. Psychometric Testing and Clinical Utility of a Modified Version of the Function in Sitting Test for Individuals With Chronic Spinal Cord Injury. Arch Phys Med Rehabil. 2020 Jul 13:S00039993(20)30428-7. doi: 10.1016/j.apmr.2020.06.014.
 Dr. Magno Formiga, PT, Ph.D.
Dr. Anne Palermo, PT, Ph.D.
Dr. Robyn Rice, PT, Ph.D.
Dr. Magno Formiga, PT, Ph.D.
Dr. Anne Palermo, PT, Ph.D.
Dr. Robyn Rice, PT, Ph.D.
2019 MANUSCRIPTS:
Formiga MF, Vital I, Urdaneta G, Masters B, Herrera J, Campos MA, Cahalin LP Higher serum levels of systemic inflammatory markers are linked to greater inspiratory muscle dysfunction in COPD Clin Respi J 2019 13(4):247-255
Formiga MF, Vital I, Urdaneta G, Campos MA, Cahalin LP Beyond inspiratory muscle strength: clinical utility of single-breath work capacity assessment in veterans with COPD. Respir Med, 2019. 147:13-18.
Formiga, M.F.; Urdaneta, G.; Vital, I.; Balestrini, K.; Cahalin, L.P.; Campos, M.A. (in press). The BODE Index and Inspiratory Muscle Performance in COPD - Clinical Findings and Implications. SAGE Open Medicine. November 2018.
Clemens S, Klute G, Kirk-Sanchez N, Raya M, Gaunaurd I, GaileyR. TemporalSpatial Values during 180º step turn in people with unilateral lower limb amputation. Gait Posture. 63:276-281, 2018.
2018 MANUSCRIPTS:
Formiga M, Roach K, Vital I, Urdaneta G, Balestrini K, Caleron-Candelario R, Campos M, Cahalin L Reliability and validity of the Test of Incremental Respiratory Endurance measures of inspiratory muscle performance in COPD International Journal of COPD 2018: 13 1569-1576
Formiga, M F ; Urdaneta, G ; Vital, I ; Balestrini, K ; Cahalin, L P ; Campos, M A (in press) The BODE Index and Inspiratory Muscle Performance in COPD - Clinical Findings and Implications SAGE Open Medicine November 2018
Clemens, S. M., Gailey, R. S., Bennett, C. L., Pasquina, P. F., Kirk-Sanchez, N. J., Gaunaurd, I. (2018). The Component Timed-Up-and-Go Test: The utility and psychometric properties of using a mobile application to determine prosthetic mobility in people with lower limb amputations. Clinical Rehabilitation, 32(3), 388-397.
OUR CURRENT PH.D STUDENTS
STUDENTS: CANDIDATES:
Sulaiman Alanazi
Shatha Aldraiwiesh
Abdulaziz Alomereni
Danylo Lucio Ferreira Cabral
Juan Gonzalez
Marangela Prysiazny Obispo
Julia Rapicavoli
Marnin Romm
Andrea Wood
Nicole De Luca
Anat Kristal
Jennifer Lucarevic
Tamira Bartholomew Prince
Jordyn Rice
ONGOING RESEARCH GRANTS
THE FUNCTIONAL OUTCOMES RESEARCH EVALUATION (F.O.R.E.) CENTER
The University of Miami Functional Outcomes Research and Evaluation (F.O.R.E.) Center is a state-of-the-art clinical based research facility with a team of investigators that includes physical therapists, physicians, music engineers, computer programmers, and biomedical engineers.

The F.O.R.E. Center's most recent development is a mobile health application known as the Rehabilitative Lower-limb Orthopedic Analysis Device(ReLOAD), which transmits directly to mobile devices such as tablets and phone systems. Currently the F.O.R.E. center has four ongoing research projects using this technology to help military service members, veterans, student athletes and civilian patients.
ReLOAD is designed to provide clinicians with the ability to administer outcome measures, prescribe evidence-based rehabilitation programs, communicate with patients and obtain real-time data from their patients as they exercise at home.
CaneSense™ is another application developed at the F.O.R.E. Center that quantifies balance and agility capabilities of athletes and soldiers prior to injury, creating a baseline of performance, so if an injury were to occur, clinicians would have objective data to guide their rehabilitation and readiness to return to sport.


The F.O.R.E. Center’s collaboration with the University of Washington, (led by Dr. Ignacio Gaunaurd) is focused on new measures of mobility being developed. The Prosthetic Limb Users Survey of Mobility-High Activity (PLUSM-HA) is designed to quantify service members and other people with limb loss ability to participate in high-level mobility activities.

The F O R E Center, plans for 2021 include a one year pilot of ReLOAD in six VAs across the USA and WRNMMC to demonstrate the clinical value of mobile health and evidence-based rehabilitation.

D r I g n a c i o G a u n a u r d , P h . D , P T , M S P T P r i n c i p a l I n v e s t i g a t o r The KIIO D r . R o b e r t G a i l e y , P h . D , P T , D i r e c t o r o f U M F O R E C e n t e r
NEUROMOTOR REHABILITATION LABORATORY


UMDPT faculty member Dr. Joyce Gomes-Osman, PT, Ph.D is the Director of the Neuromotor Plasticity Laboratory, located within the Department of Physical Therapy and The Christine E. Lynn Rehabilitation Center. The research studies conducted by Dr. Gomes-Osman's team are driven to answer research questions that can impact people’s ability to live more functional and independent lives.
A central piece of Dr. Gomes-Osman's work is the concept of neuroplasticity.
Neuroplasticity is the driving mechanism that enables functional improvements from neurorehabilitation, and it is also a vital mechanism for maintaining functional independence and cognitive brain health as we age. Dr. Gomes-Osman's team uses innovative neurophysiological assessments using non-invasive brain stimulation in the form of transcranial magnetic stimulation (TMS) to measure mechanisms of neuroplasticity in clinical populations. She has studied neurorehabilitation and neuroplasticity in individuals with neurologic conditions such as spinal cord injury and stroke, and those at risk for developing age-related cognitive decline.
An important focus of Dr. Gomes-Osman's work is characterizing the "active ingredients" of physical exercise as it pertains to maintaining mental sharpness in aging adults. Her long-term goal is to use such information to delineate individualized exercise programs to promote cognitive brain health in aging. Dr. Gomes-Osman's work has been supported by the Evelyn F McKnight Brain Institute and is currently supported by the Miami Mentored Translational Research Scholars Program Award (KL2) from the Clinical and Translational Science Institute (CTSI) at the University of Miami.
In this exciting project entitled "Assessing cognitive improvements, brain neuroplasticity, and the role of genetic factors after aerobic exercise in sedentary adults," Dr. Gomes-Osman's team is assessing the mechanisms underlying cognitive benefits from a 2-month exercise program in sedentary aging adults utilizing TMS neuroplasticity assessments, physical fitness testing, and examining key genetic factors. Dr. Gomes-Osman's work has been featured in many media outlets including The Boston Globe, The Times, CBS News, Medscape, Healthline, and was featured in the Time Magazine article "Here’s How Much Exercise You Need to Keep Your Brain Healthy."
THE DEPARTMENT OF DEFENSE KIIO PROJECT
The research project "Development and Validation of a Cost-Effective Protocol for Objective Quantification of Muscle/Tendon Function in Chronic Tendinopathy" received funding from the US Department of Defense. This project is a collaboration between Kiio Inc, of Madison, WI, the University of Wisconsin and the University of Miami. Faculty-member, Kathryn Roach, PT, Ph.D is the project methodologist and principal investigator for the University of Miami. In 2020 the UMPT was added as a data collection site and Eryn Milian, PT, PhD is directing this aspect of the project with the assistance of Phil Grattan, DPT and Michele Raya, PT, PhD..
The purpose of this project is to develop and validate a novel assessment protocol, The Comprehensive Tendinopathy Assessment Protocol (CTAP) in order to improve the clinical management of Service Members with chronic tendinopathies. The CTAP has the advantage of collecting information on muscle performance with lightweight, portable sensors and a software interface developed by Kiio Inc, rather than the expensive and fixed location devices now most commonly used. It is hoped that the CTAP will ultimately provide a cost effective and accessible method for identifying changes in muscle function resulting from interventions including physical therapy. Having a valid method for measuring muscle function in individuals with tendinopathy will greatly facilitate decisions concerning discharge from care and return to strenuous activity. The findings from this study will potentially benefit clinicians as well as both military service members and civilians with tendinopathy.
L O C A L A N D G L O B A L
O U T R E A C H ( L . A . G . O )
C L I N I C
T h e L A G O p r o B o n o c l i n i c i s d e d i c a t e d t o h e l p i n g u n d e r s e r v e d c o m m u n i t i e s t h r o u g h o u t t h e M i a m i - D a d e c o u n t y . O u r d o c t o r a l p h y s i c a l t h e r a p y s t u d e n t s v o l u n t e e r t h e i r t i m e , u n d e r t h e s u p e r v i s i o n o f l i c e n s e d p h y s i c a l t h e r a p y p r o f e s s o r s a n d r e s i d e n t s , t o p r o v i d e i n t e r v e n t i o n s t o t h o s e w h o a r e u n a b l e t o a f f o r d
h e a l t h c a r e . O u r m i s s i o n i s t o c r e a t e a h e a l t h i e r a n d m o r e f u n c t i o n a l c o m m u n i t y , o n e p a t i e n t a t a t i m e .

D . O . C . S . H E A L T H F A I R S
U M ’ s D e p a r t m e n t o f C o m m u n i t y S e r v i c e ’ s ( D O C S ) m i s s i o n i s t o p r o v i d e q u a l i t y h e a l t h c a r e t o u n d e r s e r v e d p o p u l a t i o n s i n S o u t h F l o r i d a . T h e U M D e p a r t m e n t o f P h y s i c a l T h e r a p y i s v i t a l t o t h i s m i s s i o n t h r o u g h i t s c o l l a b o r a t i o n w i t h v a r i o u s h e a l t h f a i r s a c r o s s t h e S o u t h F l o r i d a a r e a
T h e U M D P T p r o g r a m p e r f o r m s f a l l r i s k a s s e s s m e n t s a t a s p e c i f i c s t a t i o n o f t h e
D O C S h e a l t h f a i r s , t o h e l p p a t i e n t s e v a l u a t e a n d m i t i g a t e t h e i r r i s k o f f a l l i n g .
P a t i e n t s a r e p r o v i d e d w i t h r e f e r r a l s t o o u r L A G O p r o - b o n o o r S a n J u a n B a s c o c l i n i c s a s n e e d e d , a n d a r e g i v e n e d u c a t i o n a l m a t e r i a l s a b o u t f a l l p r e v e n t i o n a n d r e c o v e r y a s w e l l t o h e l p i m p r o v e t h e i r q u a l i t y o f l i f e


UMPT SUPPORTS OUR COMMUNITY
H U R R I C A N E C H A L L E N G E
2 0 2 0
T h i s y e a r , U M P T c e l e b r a t e d t h e 3 2 n d a n n u a l H u r r i c a n e C h a l l e n g e , a d a y w h e n t h e D P T s t u d e n t s o r g a n i z e a f i e l d t r i p f o r c h i l d r e n w i t h d i s a b i l i t i e s f r o m 1 1 M i a m i - D a d e C o u n t y p u b l i c s c h o o l s I n 2 0 2 0 , U M P T s t u d e n t s r a i s e d $ 8 0 0 0 t o p l a n a n d f u n d t h i s y e a r ' s " B o r n t o B e W i l d " t h e m e d e v e n t , w h i c h p r o v i d e d a d a y o f f u n f o r o v e r 2 0 0 s t u d e n t s . R e a d m o r e a b o u t t h e e v e n t h e r e .



S H A K E - A - L E G S A I L I N G
E L E C T I V E
T h e I n t e g r a t e d S p o r t s a n d L e i s u r e e l e c t i v e h a s b e e n o n e o f U M P T s m o s t p o p u l a r e l e c t i v e c o u r s e s i n c e f i r s t p a r t n e r i n g w i t h S h a k e - A - L e g M i a m i ’ s ( S A L M ) i n 1 9 9 6 . U s i n g s a i l i n g a s a n e d u c a t i o n a l m e d i u m , U M s t u d e n t s l e a r n c o m m u n i c a t i o n s k i l l s a n d h o w t o p r o v i d e a p p r o p r i a t e a s s i s t a n c e T h e y a l s o d e v e l o p a d m i r a t i o n f o r e l i t e s k i p p e r s w i t h d i s a b i l i t i e s a t S A L M , t h e w o r l d ’ s p r e m i e r w a t e r s p o r t s f a c i l i t y . A f t e r g r a d u a t i o n m a n y s t u d e n t s h a v e g o n e o n t o d e v e l o p , p r o m o t e o r w o r k w i t h c o m m u n i t y p r o g r a m s f o r c h i l d r e n , a t h l e t e s , m i l i t a r y v e t e r a n s a n d p e o p l e w i t h d i s a b i l i t i e s . R e a d m o r e h e r e
M A R Q U E T T E C H A L L E N G E
I n 1 9 8 9 , t h e p h y s i c a l t h e r a p y s t u d e n t s o f M a r q u e t t e U n i v e r s i t y i n W i s c o n s i n i s s u e d a c h a l l e n g e t o a l l o t h e r p h y s i c a l t h e r a p y s t u d e n t s a c r o s s t h e n a t i o n t o r a i s e f u n d s f o r p h y s i c a l t h e r a p y r e s e a r c h . T h e M a r q u e t t e C h a l l e n g e d u r i n g t h e i n a u g u r a l y e a r w a s w o n b y U M P T ! F o r t h e n e x t 1 3 y e a r s , t h e U n i v e r s i t y o f M i a m i e i t h e r w o n t h e C h a l l e n g e o r w a s C o - S p o n s o r o f t h e C h a l l e n g e . S i n c e 1 9 8 9 , t h e U M P T s t u d e n t s h a v e r a i s e d o v e r $ 3 0 0 , 0 0 0 f o r c l i n i c a l r e s e a r c h a n d t h e F o u n d a t i o n f o r P h y s i c a l T h e r a p y , m a k i n g t h e m p a r t o f t h e " C h a m p i o n S o c i e t y "
FACULTY PUBLICATIONS
MANUSCRIPTS: 2020
Agrawal V, Gaunaurd I, Kim KJ, Bennett C, Gailey R A Comparison of the Center of Pressure Trajectory Between Dynamic Response Prosthetic Feet Having Different Ankle Designs JPO J Prosthetics Orthot 2020
Asken BM, Houck ZM, Schmidt JD, Bauer RM, Broglio SP, McCrea MA, McAllister TW, Clugston JR A Normative Reference vs Baseline Testing Compromise for ImPACT: The CARE Consortium Multiple Variable Prediction (CARE-MVP) Norms Sports Med 2020 Aug;50(8):1533-1547
Brett BL, Breedlove K, McAllister TW, Broglio SP, McCrea MA, Hoy AMR, Hazzard JB Jr, Kelly LA, Port N, Putukian M, Pasquina P, Jackson J, McGinty G, O'Donnell P, Cameron KL, Houston MN, Giza C, Benjamin HJ, Buckley T, Clugston JR, Schmidt JD, Feigenbaum LA, Mihalik JP, Guskiewicz K, Anderson S, Master CL, Collins MW, Kontos AP, Chrisman SPD, Brooks MA, Rowson S, Miles CM, Susmarski A. Investigating the Range of Symptom Endorsement at Initiation of a Graduated Returnto-Play Protocol After Concussion and Duration of the Protocol: A Study From the National Collegiate Athletic Association-Department of Defense Concussion, Assessment, Research, and Education (CARE) Consortium. Am J Sports Med. 2020 May;48(6):14761484 doi: 10 1177/0363546520913252 Epub 2020 Apr 16 PubMed PMID: 32298132
Caccese JB, Bodt BA, Iverson GL, Kaminski TW, Bryk K, Oldham J, Broglio SP, McCrea M, McAllister T, Buckley TA Estimated Age of First Exposure to Contact Sports and Neurocognitive, Psychological, and Physical Outcomes in Healthy NCAA Collegiate Athletes: A Cohort Study Sports Med 2020 Jul;50(7):1377-1392
Caccese JB, Houck Z, Kaminski TW, Clugston JR, Iverson GL, Bryk KN, Oldham JR, Pasquina PF, Broglio SP, McAllister TW, McCrea M, Hoy AMR, Hazzard JB Jr, Kelly LA, Ortega JD, Port N, Putukian M, Langford TD, Giza CC, Goldman JT, Benjamin HJ, Schmidt JD, Feigenbaum LA, Eckner JT, Mihalik JP, Miles JD, Anderson S, Master CL, Collins MW, Kontos AP, Chrisman SPD, Brooks A, Jackson JC, McGinty G, Cameron KL, Susmarski A, O'Donnell PG, Duma S, Rowson S, Miles CM, Bullers CT, Dykhuizen BH, Lintner L, Buckley TA. Estimated age of first exposure to American football and outcome from concussion. Neurology. 2020 Sep 9;.
Clifton A, Cruz G, Patel Y, Cahalin LP, Moore JG. Sternal Precautions and Prone Positioning of Infants Following Median Sternotomy: A Nationwide Survey. Pediatr Phys Ther 2020;32(4):339-345.
da Silva FMF, Cipriano G, Lima ACGB, Andrade JML, Nakano EY, Chiappa GR, Cahalin LP, Cipriano GFB Maximal Dynamic Inspiratory Pressure Evaluation in Heart
Failure: A Comprehensive Reliability and Agreement Study Phys Ther 2020 Sep 17:pzaa165
Lučarević J, Gaunaurd I, Clemens S, et al The Relationship Between Vestibular Sensory Integration and Prosthetic Mobility in Community Ambulators With Unilateral Lower Limb Amputation Phys Ther 2020;100(8):1333-1342
Kim KJ, Gailey R, Agrawal V, et al Quantification of Agility Testing with Inertial Sensors after a Knee Injury Med Sci Sports Exerc 2020;52(1):244-251
Gailey R, Gaunaurd I, Raya M, Kirk-Sanchez N, Prieto-Sanchez LM, Roach K. Effectiveness of an Evidence-Based Amputee Rehabilitation Program: A Pilot Randomized Controlled Trial. Phys Ther. 2020.
Gailey R, Clemens S, Sorensen J, Kirk-Sanchez N, Gaunaurd I, Raya M, Klute G, Pasquinia P Variables that influence basic prosthetic mobility in people with nonvascular lower limb amputation PM R 12(2):130-39 2020
Gaunaurd I, Gailey R, Springer B, et al The Effectiveness of the DoD/VA Mobile Device Outcomes-Based Rehabilitation Program for High Functioning Service Members and Veterans with Lower Limb Amputation Mil Med 2020;185(Suppl 1):480-489
Gaunaurd I, Kristal A, Horn A, Krueger C, Muro O, Rosenberg AE, Gruben K, KirkSanchez NJ, Pasquina P, Gailey RS (2020) The Utility of the 2-Minute Walk Test as a Measure of Mobility in People With Lower Limb Amputation Archives of physical medicine and rehabilitation. 2020;101(7):1183-89.
Gusman L, et al. National Consortium of Clinical Educators, A consortium of the American Council of Academic Physical Therapy and Clinical Education Special Interest Group, A special interest group of the Academy of Physical Therapy Education, May 2020, Final Report from the Clinical Education Placement Process Task Force. [Manuscript-online] Available at: American Council of Academic Physical Therapy, ACAPT, Clinical Education Resource Page, https://acapt.org/resources/clinicaleducation October 28, 2020.
López-López L, Rodríguez-Torres JR, Cahalin LP, Cabrera-Martos I, Torres Sánchez I, Valenza MC Ventilatory Impairments Associated with Parkinson's Disease: A Systematic Review and Meta-Analysis Respiration 2021;1-9
Palermo A, Cahalin LP, Nash MS A Case for Inspiratory Muscle Training in SCI: Potential Role as a Preventative Tool in Infectious Respiratory Diseases Like COVID19 Spinal Cord Series and Cases 2020;6(1):87 doi: 10 1038/s41394-020-00337-7
Rodríguez-Torres J, López-López L, Cabrera-Martos I, Quero-Valenzuela F, Cahalin LP, Cebrià-I-Iranzo MDÀ, Valenza MC Inpatient Step Counts, Symptom Severity, and Perceived Health Status After Lung Resection Surgery Cancer Nurs 2020 Mar 24
Ruiz J, Feigenbaum L, Best TM. The Thoracic Spine in the Overhead Athlete. Curr Sports Med Rep. 2020;19(1):11-16.
Schmidt JD, Rawlins MLW, Lynall RC, D'Lauro C, Clugston JR, McAllister TW, McCrea M, Broglio SP. Medical Disqualification Following Concussion in Collegiate Student-Athletes: Findings from the CARE Consortium. Sports Med. 2020 Oct;50(10):1843-1855.
Shoemaker MJ, Cahalin LP, Dias KJ, Heick JD, Davenport TE, Severin R, Collins SM. On "Going beyond clinical practice guidelines." Jette AM. Phys Ther. 2020;100:1-2.
Phys Ther 2020 May 7:pzaa090
Formiga MF, Fay R, Hutchinson S, et al Effect of Aerobic Exercise Training with and without Blood Flow Restriction on Aerobic Capacity in Healthy Young Adults: A MetaAnalysis [published correction appears in Int J Sports Phys Ther 2020 May;15(3):486]
Int J Sports Phys Ther 2020;15(2):175-187
Gailey R, Clemens S, Sorensen J, et al Variables that Influence Basic Prosthetic Mobility in People With Non-Vascular Lower Limb Amputation PM R 2020;12(2):130-
Wong ML, Fleming L, Robayo LE, Widerström-Noga E. Utility of the Neuropathic Pain Symptom Inventory in people with spinal cord injury. Spinal Cord. 2020;58(1):35-42.
139
2019 MANUSCRIPTS:
El-Ansary D, LaPier TK, Adams J, et al. An evidence-based perspective on movement and activity following median sternotomy. [published ahead of print September 2, 2019]. Phys Ther J.
Ricard PEH, Cahalin LP. Cardiovascular and Pulmonary Research: The Year (2018) in Review. Cardiopulm Phys Ther J. 2019;30:106-114.
Rodríguez-Torres J, López-López L, Cabrera-Martos I, Valenza-Demet G, Cahalin LP, Valenza MC. Sarcopenia in patients with malignant pleural effusion: impact on symptoms, health status, and response to hospitalization [published ahead of print April 3, 2019] Support Care Cancer
Costa IP, Politti F, Cahalin LP, et al Acute Effects Using Light-Emitting Diode Therapy (LEDT) for Muscle Function during Isometric Exercise in Asthma Patients: A Pilot Study Biomed Res Int 2019;2019:7501870
Thomaz SR, Cipriano G Jr, Formiga MF, et al Effect of electrical stimulation on muscle atrophy and spasticity in patients with spinal cord injury - a systematic review with metaanalysis Spinal Cord 2019;57(4):258-266
Cahalin LP Ventilation, Respiration, Skeletal Muscle, and More – What, a Link? Cardiopulm Phys Ther J. 2019;30(1):2-4.
Moore JG, Cahalin LP. Commentary on "The Effect of Inspiratory Muscle Training on Duchenne Muscular Dystrophy: A Meta-analysis". Pediatr Phys Ther. 2019;31(4):330.
Stemper BD, Shah AS, Harezlak J, et al. Repetitive Head Impact Exposure in College Football Following an NCAA Rule Change to Eliminate Two-A-Day Preseason Practices: A Study from the NCAA-DoD CARE Consortium. Annals of Biomedical Engineering. 2019;47(10):2073-2085.
Feigenbaum LA, Kim KJ, Gaunaurd IA, et al. Post-Concussive CHanges in Balance and Postural Stability Measured with CaneSense TM and the Balance Error Scoring System (BESS) in Division I Collegiate Football Players: A Case Series Int J Sports Phys Ther 2019;14(2):296-307
Anderson DK, Furze JA, Moore JG Moving Toward Excellence in Pediatric Physical Therapy Education: A Scoping Review Pediatr Phys Ther 2019;31(1):95-113
Wong ML, Tibbett J, Adedolapo T, Widerstrom-Noga E The Graph-DCK Scale: A Measure of Dorsal Column Function After Spinal Cord Injury Spinal Cord 2019;57(5):412-418
Gailey R, Kristal A, Lucarevic J, Harris S, Applegate B, Gaunaurd I The development and internal consistency of the comprehensive lower limb amputee socket survey in active lower limb amputees. Prosthet Orthot Int. 2019;43(1):80-87.
Osborne R, Hartley G. Professional engagement: A consensus definition and key indicator behaviors for physical therapists. Physical Therapy Journal of Policy, Administration and Leadership. 2019;19(2):5-12.
Hartley G, Roach KE, Harrington KL, McNally S. Program-level factors influencing positive graduate outcomes of physical therapy residency programs. Phys Ther. 2019;99(2):173-182.
Darnall BD, Juurlink D, Kerns RD, et al. Commentary: International stakeholder community of pain experts and leaders call for an urgent action on forced opioid tapering. Pain Med. 2019:20(3):429-433
Gailey RS, Kristal A, Lucarevic J, Harris S, Applegate B, Gaunaurd I The development and internal consistency of the comprehensive lower-limb amputee socket survey (CLASS) in active lower limb amputees Prosthet Orthot Int 2019;43(1):80-87
2018
Broglio SP, Hareziak J, Katz B, et al. Acute Sport Concussion Assessment Optimization: A Prospective Assessment from the CARE Consortium. Sports Medicine. 2019;49(12):1977-
1987
Feigenbaum LA, Kim KJ, Gaunaurd I, et al Post-Concussive Changes in Balance and Postural Stability Measured with CaneSense and the Balance Error Scoring System (BESS) in Division I Collegiate Football Players Int J Sports Phys Ther 2019;14(2):296-307
McCrea M, Broglio S, McAllister T, et al Return to play and risk of repeat concussion in collegiate football players: comparative analysis from the NCAA Concussion Study (19992001) and CARE Consortium (2014-2017) [published ahead of print April 29, 2019] British Journal of Sports Medicine
Gaunaurd I, Kim KJ, Feigenbaum LA, et al Construct validation of lower limb segmental excursion as a measure of potential risk for lower limb injury in Division I women's basketball players. Journal of Biomechanics. 2019;84:252-256.
Caccesse JB, DeWolf RM, Kaminski TW, et al. Estimated Age of First Exposure to American Football and Neurocognitive Performance Amongst NCAA Male StudentAthletes: A Cohort Study. Sport Med. 2019;49(3):477-487.
Kim KJ, Agrawal V, Gaunaurd I, et al. Quantification of Agility Testing with Inertial Sensors following a Knee Injury. [published ahead of print July 10, 2019]. Med Sci Sports Exerc
MANUSCRIPTS:
Gomes-Osman J, Cabral DF, Morris TP, et al Exercise for cognitive brain health in aging: A systematic review for an evaluation of dose Neurol Clin Pract 2018;8(3):257-265
Spagnuolo G, Faria CDCM, da Silva BA, Ovando AC, Gomes-Osman J, Swarowsky A. Are functional mobility tests responsive to group physical therapy intervention in individuals with Parkinson's disease?. NeuroRehabilitation. 2018;42(4):465-472.
Estes, S., Iddings, J., Ray, S., Kirk-Sanchez, N. J., Edelle, F.-F. (in press). Comparison of single-session dose response effects of whole body vibration on spasticity and walking speed in persons with spinal cord injury. Neurotherapeutics.
Eltoukhy, M., Kuenze, C., Oh, J., Milian, E., Butler, L., Signorile, J. Concurrent Validity of Depth Sensing Cameras for Non-Contact ACL Injury Screening during Side-Cut Maneuvers in Adolescent Athletes: A Preliminary Study Journal of Applied Biomechanics, 2018
Kim KJ, Agrawal V, Bennett C, Gaunaurd I, Feigenbaum L, Gailey R Measurement of lower limb segmental excursion using inertial sensors during single limb stance J Biomech 2018;71:151-158
Schmidt JD, Rizzone K, Hoffman NL, et al Age at First Concussion Influences the Number of Subsequent Concussions Pediatr Neurol 2018;81:19-24
Allseits E, Kim KJ, Bennett C, Gailey R, Gaunaurd I, Agrawal V A Novel Method for Estimating Knee Angle Using Two Leg-Mounted Gyroscopes for Continuous Monitoring with Mobile Health Devices. Sensors (Basel). 2018;18(9):2759. Published 2018 Aug 22.
Gomes-Osman J, Indahlastari A, Fried PJ, et al. Non-invasive Brain Stimulation: Probing Intracortical Circuits and Improving Cognition in the Aging Brain. Front Aging Neurosci. 2018;10:177. Published 2018 Jun 8.
Allseits E, Agrawal V, Lučarević J, Gailey R, Gaunaurd I, Bennett C. A Practical Step Length Algorithm using Lower Limb Angular Velocities. Journal of Biomechanics. January, 66(3). 137-144. 2018.
Wong, M L ; Formiga, M F ; Owens, J ; Asken, T ; Cahalin, L P Safety of Blood Flow Restricted Exercise in Hypertension - A Meta-Analysis and Systematic Review with Potential Applications in Orthopedic Care Techniques in Orthopaedics 2018;33:80-88
Peres Costa I, Fernandes Silva MG, Santos Alves VLD, Aletti F, Stirbulov R, Costa D, Cahalin LP, Arena R, Sampaio LMM Reliability of the shuttle walk test with controlled incremental velocity in patients with difficult-to-control asthma J Cardiopulm Rehabil Prev 2018;38(1):54-57

Weber ML, Dean JL, Hoffman NL, et at Feigenbaum, LA Influences of Mental Illness, Current Psychological State, and Concussion History on Baseline Concussion Assessment Performance. Am J Sports Med. 2018 Apr 1: 363546518765145.

Asken, B. M., Bauer, R. M., Guskiewicz, K. M., McCrea, M. A., Schmidt, J. D., Giza, C. C., Snyder, A. R., Houck, Z. M., Kontos, A. P., McAllister, T. W., Broglio, S. P., Clugston, J. R., Anderson, S., Bazarian, J., Brooks, A., Buckley, T., Chrisman, S., Collins, M., DiFiori, J., Duma, S., Dykhuizen, B., Eckner, J. T., Feigenbaum, L. A., Hoy, A., Kelly, L., Langford, T. D., Lintner, L., McGinty, G., Mihalik, J., Miles, C., Ortega, J., Port, N., Putukian, M., Rowson, S., Svoboda, S. (2018). Immediate Removal From Activity After Sport-Related Concussion Is Associated With Shorter Clinical Recovery and Less Severe Symptoms in Collegiate Student-Athletes The American journal of sports medicine, 363546518757984

WE LOOK FORWARD TO 2021!











 TERESA GLYNN Vice Chair of Clinical Services
MARLON WONG Assistant Vice Chair of Clinical Services
CHRIS VITOLO Assistant Vice Chair of Clinical Services
MARLON PEREIRA Manager, UHealth Towers Outpatient
CHELSEA MILLER Manager, CRB Pain Clinic
TERESA GLYNN Vice Chair of Clinical Services
MARLON WONG Assistant Vice Chair of Clinical Services
CHRIS VITOLO Assistant Vice Chair of Clinical Services
MARLON PEREIRA Manager, UHealth Towers Outpatient
CHELSEA MILLER Manager, CRB Pain Clinic




 LUIS FEIGENBAUM Senior Associate Athletic Director for Performance, Health, and Wellness
NORIS PEREZ Manager, Lennar Clinic
CRISTINA PACHECO Manager, UHealth Towers Inpatient
ANNEMAY LELIS Manager, Oncology Rehab Services
RICH MANCINI Manager, Plantation Clinic
LUIS FEIGENBAUM Senior Associate Athletic Director for Performance, Health, and Wellness
NORIS PEREZ Manager, Lennar Clinic
CRISTINA PACHECO Manager, UHealth Towers Inpatient
ANNEMAY LELIS Manager, Oncology Rehab Services
RICH MANCINI Manager, Plantation Clinic



 NELSON TRETO Manager, Kendall Clinic
GAYLENE HORSFALL Manager, Hand Services
JENNIFER ZAMORA Director of Front Office Business Operations
TOM DREVYN Compliance Manager
JESSICA FIRMEZA Manager, Cardiac and Pulmonary Rehabilitation Clinic
NELSON TRETO Manager, Kendall Clinic
GAYLENE HORSFALL Manager, Hand Services
JENNIFER ZAMORA Director of Front Office Business Operations
TOM DREVYN Compliance Manager
JESSICA FIRMEZA Manager, Cardiac and Pulmonary Rehabilitation Clinic