

Lessons from Implementation Science
James James Cornford Cornford
Proposed Structure of the Session
• What is the problem?
• Do you have it too? Give an example.
• What is “Implementation Science”?
• Does it sound of interest to you? Why?
• An example of middle range theory: Normalisation Process Theory
• Could you make use of this theory?
• Discussion: What (if anything) can Innovation in the Food Science learn from Implementation Science?
• Take Away Actions
• For me
• For you

The implementation Problematic

• Implementation science has arisen in the context of the Wider “Evidence-based” movement
• Evidence-based Policy
• Evidence-based Practice(s)
• Implementation Science deals with a specific problem of EBP
• We have high quality scientific evidence about ‘what works’ in the lab or even in efficacy trials, but…
• …when we attempt to act on this evidence we find that implementing this knowledge is extremely difficult/impossible….
• …the ‘science to service’ gap (Ogden and Fixsen, 2014: 4)
Example: MRSA and Handwashing
• We know that effective handwashing reduces the spread of MRSA (Methicillin-resistant Staphylococcus aureus) in Hospitals.
• But we find it difficult to get patients and professionals to do it!
• “Addressing only determinants such as knowledge, awareness, action control, and facilitation is not enough to change HH [Hand Hygiene] behaviour.
• Addressing combinations of different determinants showed better results.
• This indicates that we should be more creative in the application of alternative improvement activities addressing determinants such as social influence, attitude, self-efficacy, or intention. (Huis et al., 2012: 1)


And here too?
The
“Speed”, “Stick,” “Spread” and “Scale”
Problems


• Why do innovations take so long to be incorporated into general use?
• Evidence Based Practices take on average 17 years to be incorporate into routine health care (Morris et al., 2011)
• What makes innovation Stick?
• Many innovations are implemented but participants quickly return to the old ways.
• What makes innovations Spread?
• Innovations are implemented but remain in isolated islands.
• What makes innovations Scale?
• Innovations are successfully implemented in small pilots or trials but don’t work at scale.
QUESTION 1

•Do you recognise the speed, stick, spread and scale problems? Yes/No/Maybe
•Can you briefly describe a specific case? (speed, stick, spread, scale or some combination)
Some Context

Institutions
• BMC Health Services Research (founded 2001)
• Implementation Science Journal (founded 2006 –see Eccles and Mittman, 2006)
• US Institutes of Health IS (2015)
• Centre for Implementation Science, Kings College London (2017).
• UCL….
Implementation Science
• Implementation science is “the scientific study of methods to promote the systematic uptake of research findings and other EBPs [Evidence Based Practices] into routine practice, and, hence, to improve the quality and effectiveness of health services.”(Bauer et al. 2015: 3)
• From “What works?” to “How can we make this work?”


Implementation Research
• Implementation research is the scientific study of methods to promote the systematic uptake of research findings and other evidence-based practices into routine practice, and, hence, to improve the quality and effectiveness of health services and care. This relatively new field includes the study of influences on healthcare professional and organisational behaviour (Eccles and Mittman, 2006: 1).

Implementation Studies
• “Implementation studies typically employ mixed quantitative-qualitative designs, identifying factors that impact uptake across multiple levels, including patient, provider, clinic, facility, organization, and often the broader community and policy environment. Accordingly, implementation science requires a solid grounding in theory and the involvement of transdisciplinary research teams” (Bauer et al 2015: 1 emphasis added).

Why Implementation Science
• Research Impact Agenda
• More than just papers!
• Healthcare systems Value for Money agenda
• Aging populations –declining health, co-morbidity

• Limits of Quality Improvement, Information Dissemination and Translational Medicine approaches
• QI limited to incremental improvements of existing practices
• Dissemination limited to communication
• Translational Medicine narrowly clinical focus
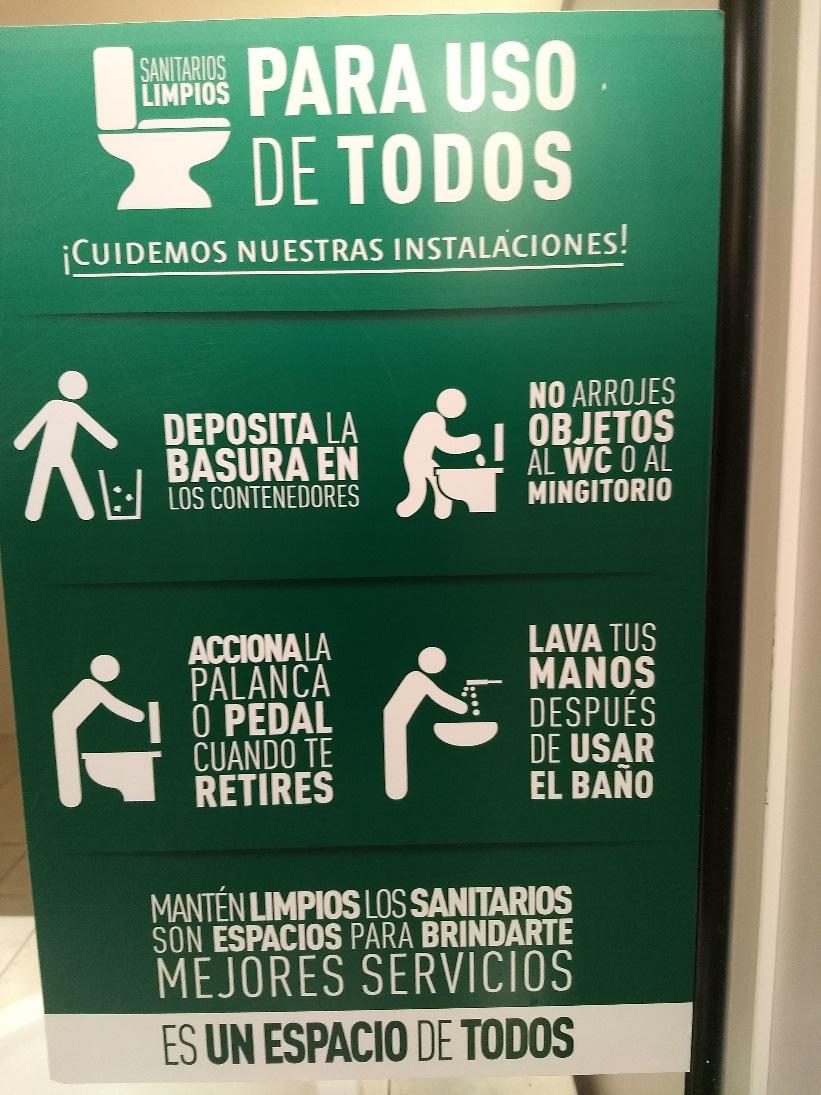
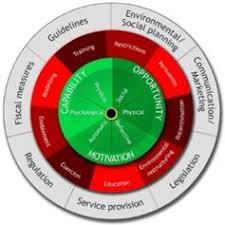
Behavioural Science
• Emphasis on changing behaviour of
• Patients
• Providers
• Links to behavioural science
• Behavioural Economics (e.g., Kahneman, 2011)
• MINDSPACE (Cabinet Office/IoG, 2010)
• COM-B (Competence, Opportunity, Motivation Behaviour Change) –e.g., Michieet al. 2014
Messenger (we are heavily influenced by who communicates information)
Incentives (our responses to incentives are shaped by predictable mental shortcuts such as strongly avoiding losses)

Norms (we are strongly influenced by what others do
Defaults we „go with the flow‟ of pre-set options)
Salience (our attention is drawn to what is novel and seems relevant to us)
Priming (our acts are often influenced by sub-conscious cues)
Affect (our emotional associations can powerfully shape our actions)
Commitments (we seek to be consistent with our public promises, and reciprocate acts)
Ego (we act in ways that make us feel better about ourselves)
Evolution
• Implementation Science 1.0
• Descriptive studies of Gaps and Barriers to implementation
• e.g., Health Foundation (2015) What’s Getting in the Way? Barriers to Improvement in the NHS
• Implementation Science 2.0
• Testing strategies and approaches to implementation
• e.g, most articles in IS
• Implementation Science 3.0
• Developing Generalizable Theory of Implementation
• e.g, Normalisation Process Theory (May and Finch 2009; May 2013)

e.g., CFIR
(Damschroederet al.,
2009)

• Consolidated Framework for Implementation Research
• 39 Constructs across 5 Domains
• Intervention (e.g., complexity, trialability, cost)
• Inner setting (e.g., leadership engagement, implementation climate)
• Outer setting (e.g., peer pressure, policy, patient needs)
• Characteristics of Individuals (e.g., knowledge and beliefs, self-efficacy)
• Process (e.g., planning, executing, engaging)

Question 2

•Does this kind of approach sound relevant and interesting to you?
•Can you identify an opportunity to use of deploy some of the theories and tools developed by IS?
Normalisation Process Theory (NPT)
• Developed over a long period by Carl May and a wide range of collaborators (especially Tracey Finch)
• Building on much classic and modern sociology (diffusion theory, symbolic interactionists, STS etc.)
• A ‘middle range theory of Normalisation Processes that provides an explanatory framework for investigating the routine embedding of material practices in their social contexts’ (May and Finch 2009: 536)
• ‘It begins with the question what is the work?’ (May and Finch 2009: 538)



NPT Implementation
• Implementation =
• Embedding (making practices routine)
• Integration (sustaining routine practices)
• NPT is a reflexive theory!
• May, in particular, has put a lot of thought into how NPT can itself be “normalised” and implemented
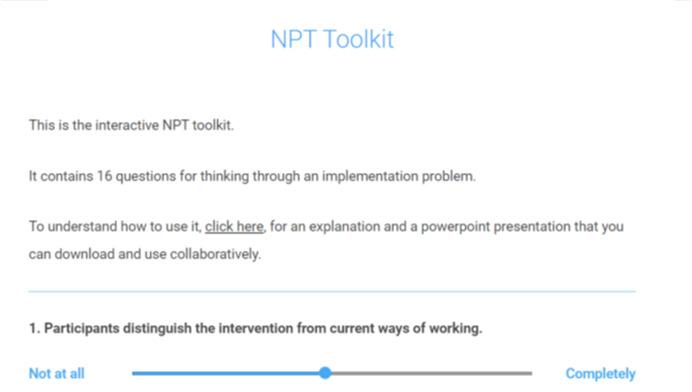
• See http://www.normalizationprocess. org/

NPT Starting points
• Material Practices become routinely embedded in social contexts as the result of people working, individually and collectively to implement them
• The work of implementation is operationalised through four generative mechansims (Coherence; cognitive participation; collective action; reflexive monitoring)
• The production and reproduction of material practice requires continuous investments by agents in ensembles of action that carry forward in time and space (May and Finch, 2009: 540)


The Theoretical Propositions
• Coherence
• Embedding is dependent on the work that defines and organizes a practice as a cognitive and behavioural ensemble
• Embedding work is shaped by factors that promote or inhibit actors’ apprehension of a practice as meaningful
• The production and reproduction of coherence in a practice requires that actors collectively invest meaning on it
• Cognitive Participation
• Embedding is dependent on work that defines and organizes the actors implicated in a practice
• Embedding work is shaped by factors that promote or inhibit actors’ participation
• The production and reproduction of a practice requires that actors collectively investment commitment in it
• Collective Action
• Embedding is dependent on work that defines and operationalizes a practice
• Embedding work is shaped by factors that promote or inhibit actors’ enacting it
• The production and reproduction of a practice requires that actors collectively invest effort in it
• Reflexive Monitoring


• Embedding is dependent on work that defines and organizes the everyday understanding of practice
• Embedding work is shaped by factors that promote or inhibit appraisal
• The production and reproduction of a practice requires that actors collectively invest in its understanding
Simplifying
• X.1 define mechanism
• Organises as an ensemble, actors, practice, understanding
• X.2 define components of a mechanism
• Meaningful, participation, enactment, appraisal
• X.3 define actors’ investments in a mechanism
• Meaning, Commitment, Effort, Understanding
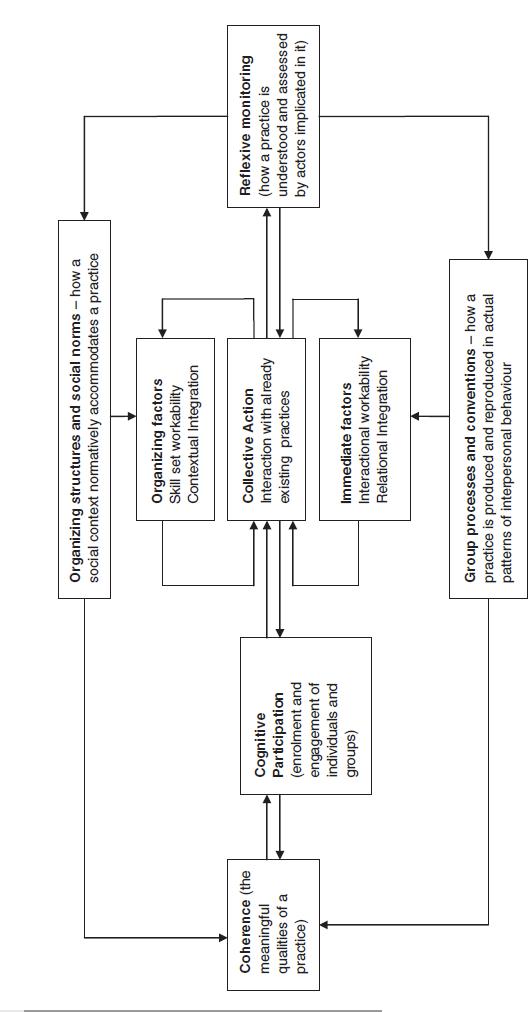

Diagrammatically

One tiny example: Telecare
• Can I work it? Is it worth it?

• Key barriers to telecare integration were uncertainties about coherent and sustainable service and business models; lack of coordination across social and primary care boundaries, lack of financial or other incentives to include telecare within primary care services; a lack of a sense of continuity with previous service provision and self-care work undertaken by patients; and general uncertainty about the adequacy of telecare systems. These problems led to poor integration of policy and practice.
• Slow and uneven implementation and integration do not stem from problems of adoption. They result from incomplete understanding of the role of telecare systems and subsequent adaption and embeddedness to context, and uncertainties about the best way to develop, coordinate, and sustain services that assist with chronic disease management. Interventions are therefore needed that (i) reduce uncertainty about the ownership of implementation processes and that lock together health and social care agencies; and (ii) ensure user centred rather than biomedical/service-centred models of care. (May et al., 2011)
Questions 3

•What, if anything, can food science and agri-tech learn from implementation science in healthcare?
• Take away points for you?
• Take away points for me?
Limitations: health care as CAS Cynefin

Obvious
• Sense, categorise and respond
• Best practice Complicated
• Sense, analyse respond
• Good Practice Complex
• Probe sense respond
• Emergent Practice Chaotic
• Act sense respond
• Novel Practice

Lessons from IS

• Focus on implementation as a subject of equal value to medical science has been valuable
• But still nothing like the volume of funding (IS = c. 1-5% of Biomedical Research)
• Cross-disciplinary multi-level approach has been really valuable
• But this is costly and time consuming and is always a fragile alliance
• Implementation science as a reflexive practice
• Can it explain itself?
• Pre-evaluating implementations and rejecting due to poor implementation plans will save resource
• But need robust and accountable procedures for this
• The increasing challenge of assessing implementation in a “complex adaptive system” where outcomes are indeterminate
• Implementation as process of “cultivation” and “steering” rather than “fixing” or “re-engineering”
• Remember not just “What works?” but “Can we make it work?”
Cultivation or engineering?



References

• Bauer, M.S., Damschroder,L., Hagedorn,H., Smith,J. &Kilbourne, A.M. (2015) An introduction to implementation science for the non-specialist BMC Psychology 3, Articlenumber:32.
• Cabinet Office/Institute of Government (2010) MINDSPACE Influencing behaviour through public policy. London: Cabinet Office.
• Damschroder, L. J., Aron, D. C., Keith, R.E., Kirsh, S.R., Alexander, J.A. and Lowery, J. C. (2009) Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Science, 4(1): 50ff.
• Eccles, M.P. and Mittman, B. S. (2006) Welcome to Implementation Science, Implementation Science 1, Articlenumber:1.
• Health Foundation (2015) What’s Getting in the Way? Barriers to Improvement in the NHS. Evidence Scan, February.
• Huis, A. et al. (2012) Systematic review of hand hygiene improvement strategies: a behavioural approach, Implementation Science, 7(94).
• Kahneman, D. (2011) Thinking Fast and Slow. New York: Farrar, Straus and Giroux
• May, C., Finch, T., Cornford, J. et al. (2011) Integrating telecare for chronic disease management in the community: What needs to be done? BMC Health Services Research, 11(131).
• May, C. and Finch, T. (2009) Implementing, Embedding and Integrating practices: An Outline of Normalisation Process Theory, Sociology, 43(3):535554.
• Michie, S., Atkins, L. and West, R. (2014) The Behaviour Change Wheel A Guide to Designing Interventions. Silverback.
• Morris, Z. S. , Wooding S. and Grant, J. (2011) The answer is 17 years what is the question? Understanding lags in translationalresearch, Journal of the Royal Society of Medicine, 104: 510-20.
• Ogden, T., and Fixsen, D. L. (2014) Implementation science: A brief overview and a look ahead. ZeitschriftfürPsychologie, 222(1), 4-11.
