CONNECTING ALUMNI, FRIENDS AND COMMUNITY
JACOBS SCHOOL OF MEDICINE AND BIOMEDICAL SCIENCES UNIVERSITY AT BUFFALO

CONNECTING ALUMNI, FRIENDS AND COMMUNITY
JACOBS SCHOOL OF MEDICINE AND BIOMEDICAL SCIENCES UNIVERSITY AT BUFFALO
At the Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, our mission is clear: transforming ideas into impact, advancing science, improving health and strengthening the well-being of Western New York and beyond. We know that lasting change happens through collaboration, and we’re proud to work in partnership with our community to drive progress.
In this edition of UB Medicine, we highlight how our faculty, learners and partners are bringing that mission to life in powerful ways. Our research enterprise isn’t just one component—it’s an entire ecosystem where basic science research, clinical trials and our facilities come together to create a robust environment for discovery. This interconnected approach is what allows us to translate scientific breakthroughs into real-world solutions that make a difference in our region.
This seamless pipeline is fueled by strategic investments in our people and infrastructure. You’ll read how our new facilities are more than just bricks and mortar; they are engines of innovation that support our full research enterprise.
We are equally committed to cultivating the next generation of scientific leaders, investing in STEM-focused outreach and providing strong support for junior faculty. This momentum is reflected in our enrollment growth in undergraduate and master’s programs, learners who are choosing UB as the place to begin their journey in science and medicine.

From foundational science to the bedside, we are translating discovery into action. These efforts underscore UB’s leadership in population-focused innovation and our commitment to improving lives through research that moves from bench to bedside.
As we implement Epic—the most widely adopted electronic health record system—across our clinical sites, we’re opening new doors to accelerate research, improve care and expand our impact. This is a transformative moment for UB and for the patients and for the people we serve.
Together with our learners, faculty, and partners, we are shaping a future defined by innovation, compassion and progress. Thank you for being part of our story.
With pride and gratitude,

Allison Brashear, MD, MBA
Dean, Jacobs School of Medicine and Biomedical Sciences Vice President for Health Sciences President and CEO, UBMD Physicians’ Group
UB Medicine is published by the Jacobs School of Medicine and Biomedical Sciences at UB to inform alumni, friends and community about the school’s pivotal role in medical education, research and advanced patient care in Buffalo, Western New York and beyond.
VISIT US: medicine.buffalo.edu/alumni COVER IMAGE
A look at the many different aspects of the Jacobs School research enterprise.
Photo illustration/Cover design: Ellen Stay
Medical schools, community organizations and local leaders join forces to confront a public health crisis

How the Jacobs School’s research enterprise enables discovery and enriches health

ALLISON BRASHEAR, MD, MBA
Vice President for Health Sciences and Dean, Jacobs School of Medicine and Biomedical Sciences
President and CEO, UBMD Physicians’ Group
Jeffry Comanici
Assistant Vice President for Advancement
Editor Patrick S. Broadwater
Contributing Writers
Dawn M. Cwierley
Keith Gillogly
Ellen Goldbaum
Dirk Hoffman
Copyeditor
Ann Whitcher Gentzke
Photography
Sandra Kicman
Meredith Forrest Kulwicki
Douglas Levere
Nancy Parisi
KC Kratt
Art Direction & Design
Ellen Stay
Editorial Adviser
John J. Bodkin II, MD ’76
Affiliated Teaching Hospitals
Erie County Medical Center
Roswell Park Comprehensive Cancer Center
Veterans Affairs Western New York Healthcare System
Kaleida Health
Buffalo General Medical Center
Gates Vascular Institute
John R. Oishei Children’s Hospital Millard Fillmore Suburban Hospital
Catholic Health
Mercy Hospital of Buffalo Sisters of Charity Hospital
Correspondence, including requests to be added to or removed from the mailing list, should be sent to: Editor, UB Medicine, 955 Main Street, Buffalo, NY 14203; or email ubmedicine-news@buffalo.edu
Student numbers rise across undergraduate, master’s and PhD programs
A select collection of images from events happening at the Jacobs School over the past few months.

The Jacobs School had a large presence at this year’s Juneteenth parade and celebration events at Martin Luther King Jr. Park. Buffalo boasts one of the largest and oldest Juneteenth festivals in the nation.
Jian Feng, PhD, SUNY Distinguished Professor of physiology and biophysics, delivers the 2025 Stockton Kimball Lecture in the Dozoretz Auditorium. The lecture is paired with the school’s faculty and staff recognition awards ceremony each May, marking one of the final events of the academic year. Steven J. Fliesler, PhD, SUNY Distinguished Professor and Meyer H. Riwchun Endowed Chair Professor of ophthalmology, was named this year’s winner of the Stockton Kimball Award for outstanding scientific achievement and service.


Joy filled the air at the University at Buffalo’s Center for the Arts as incoming medical students donned their white coats for the first time. The event, held at the conclusion of orientation week in July, marked the ceremonial beginning of their medical careers for more than 180 new first-year medical students.
Jacobs School graduates of 2024 are a year removed from med school, but they’re still scoring high marks. According to the AAMC Resident Readiness Survey, 98.1 percent of Jacobs School alumni from the Class of 2024 are meeting or exceeding the overall expectations of their residency program. Scoring well on residency reviews is nothing new to Jacobs School graduates—our alumni consistently meet or exceed expectations at a high level, year after year—but the 98 percent mark is the school’s best result over the past five years.

As part of orientation week, Jacobs School medical students and faculty assisted local agencies with service projects across the city of Buffalo and Western New York. The projects not only helped out local nonprofits and service organizations, but the community engagement of our students is a built-in feature of the school’s new Well Beyond curriculum.

The University at Buffalo’s new Genetic Counseling Graduate Program has received accreditation from the Accreditation Council for Genetic Counseling (ACGC), the field’s national accrediting organization.
The two-year Master of Science program, which will be administered by the Office of Biomedical Education in the Jacobs School of Medicine and Biomedical Sciences at UB, will prepare students to become board-certified genetic counselors who help patients understand genetic risks and guide decision-making.
Applications to the program opened Aug. 1 and will run through Dec. 15. More information can be found at medicine. buffalo.edu/education/genetic-counseling.
The program has already received approvals from SUNY and the New York State Education Department. With the program’s start in fall 2026, UB will be the first public university in New York State to offer a master’s in genetic counseling.
“All patients in Western New York should have access to the health benefits of genetic and genomic medicine,” says Lindsey M. Alico, a board-certified genetic counselor and director of UB’s Genetic Counseling Graduate Program. The Orchard Park native joined UB in 2023 from Sarah Lawrence College, where she previously co-directed its genetic counseling program, the nation’s oldest and largest.
Laurie S. Sadler, MD, clinical associate professor of pediatrics and a clinical geneticist in Buffalo for over 30 years, is the UB program’s first medical director.
Genetic counselors don’t directly diagnose conditions or prescribe therapies. They instead offer guidance and information about inherited diseases that may affect patients and their families.
Genetic counselors help patients and providers understand the clinical implications of complex genetic test results in order to make more informed health care decisions. Expectant parents may see a genetic counselor after an abnormal
carrier screening test or ultrasound. Patients may also be referred to a genetic counselor to determine if a recently diagnosed disease has a genetic component.
“Sometimes we see someone who’s been diagnosed with cancer and has an unusual feature, like a rare type of cancer or diagnosis at a young age, and they want to know the chance that it was due to a hereditary cause,” says Alico, clinical assistant professor in the Jacobs School’s Office of Biomedical Education.
Most health care providers have received little genetics training while in school and would benefit from more support in genetic-related care, Alico says. While telehealth has improved access to genetic counselors, there’s demand for more counselors, both locally and nationally.
The idea for creating a genetic counseling degree program coincided with the 2015 launch of UB’s Genome, Environment and Microbiome Community of Excellence, or GEM, which promotes genetics, genomics and microbiome research and outreach to advance understanding of personal health issues. Jennifer A. Surtees, PhD, now the chair of the Department of Biochemistry, is GEM’s co-director and spearheaded the genetic counseling effort, shepherding the program through its curricular development and early approvals.
She worked closely with Carolyn Farrell, PhD, who directed the Clinical Genetics Service at Roswell Park
Comprehensive Cancer Center for over 15 years, and with Norma J. Nowak, PhD, professor of biochemistry and codirector of GEM.
Throughout the development process, Surtees says it was key to involve faculty from many schools—including medicine, nursing, public health, pharmacy, law, social work, education, and arts and sciences—to garner their
perspectives on genetics.
She adds that the launch of the program is a return to the region’s historical contributions to genetic and genomic research, noting UB researchers’ involvement with the Human Genome Project and achievements in neo-natal testing for PKU and for sickle cell anemia.
Applicants to genetic counseling programs participate in an admissions match overseen by the Genetic Counselor Educators Association that places them into accredited programs. Interviews will take place during the spring semester, with the first student cohort beginning classes in fall 2026. UB’s program will enroll four students initially, Alico says, but will expand to include six students per class.
Students in the program will complete 61 credits from classes taken over 21 months. In addition to completing a master’s thesis, students must complete clinical rotations with certified genetic counselors. Surtees and Alico acknowledge the commitment local genetic counselors have made to developing the master’s program and to supervising and teaching students.
Program graduates will be able to sit for the American Board of Genetic Counseling certification exam to become a Certified Genetic Counselor, a required credential to practice in most areas.
In New York State, genetic counselors do not have licensure and therefore cannot operate independently; they must be embedded within an existing hospital or practice. Thirty-five other U.S. states, however, issue licenses for genetic counselors.
UB’s new genetic counseling program was developed by (left to right) Carolyn Farrell, Lindsey M. Alico, who directs the program, Jennifer A. Surtees, and Norma J. Nowak.

Jennifer A. Surtees, PhD, professor of biochemistry in the Jacobs School of Medicine and Biomedical Sciences, has been named chair of the Department of Biochemistry, effective July 1.
“Recognized for her outstanding scientific leadership, collaborative spirit and remarkable ability to mentor and inspire, Dr. Surtees brings both scientific distinction and a genuine passion for education and community outreach to this leadership role,” says Allison Brashear, MD, MBA, UB’s vice president for health sciences and dean of the Jacobs School.
Surtees is both internationally recognized in the fields of genome stability and genetic diversity and a passionate advocate for boosting scientific literacy in the general population.

Surtees’ groundbreaking research explores how cells maintain the integrity of their genetic material, with a focus on DNA repair, replication fidelity and the regulation of nucleotide pools. Her lab investigates how disruptions in these processes contribute to cancer and neurodegenerative diseases. She is particularly wellknown for her work showing how research into altered levels of DNA building blocks may inform future cancer therapies.
“Dr. Surtees brings both scientific distinction and a genuine passion for education and community outreach to this leadership role.”
- Allison Brashear, MD, MBA
A UB faculty member since 2007, Surtees is a prolific scholar, having authored numerous peer-reviewed journal articles, book chapters and scholarly reviews. She is frequently an invited speaker at national and international scientific meetings.
During the COVID-19 pandemic, she launched collaborations with UB colleagues and the Erie County Public Health Laboratory to sequence SARS-CoV-2 genomes, helping to track variants and guide public health responses—work that continues as part of the New York State COVID Genomic Sequencing Consortium. This work was a catalyst for Surtees to assemble a broad, interdisciplinary team focused on pandemic prevention through novel environmental monitoring and building trust through community conversations and STEM outreach.
As co-director of the Genome, Environment and Microbiome (GEM) Community of Excellence, she has led efforts to develop and foster interdisciplinary research teams at UB and to promote genome and microbiome literacy at UB and in the Buffalo community, earning the Jacobs School’s Community Service Award for Excellence in Promoting Inclusion and Diversity.
Surtees earned her Bachelor of Science degree in genetics from Western University (Ontario), and her master’s and PhD in molecular and medical genetics from the University of Toronto.
Asim Khan, PhD, a nationally recognized expert in digital technologies and strategic health care information leader, has been named the University at Buffalo’s health sciences chief data and information officer, effective Sept. 2.
Khan joined UB from the Allegheny Health Network, where he served as system director of IT business intelligence and interoperability. He also serves as chief data and information officer for UBMD Physicians’ Group and as executive director of UB Information Technology HIPAA Compliance.
In his new roles, Khan works to create and implement a unified information technology strategy across UB’s health sciences and UBMD’s 17 practice plans. In order to enhance patient care, research and education, Khan focuses on driving digital transformation, improving data governance, and enabling information systems to work in unison.

Khan will oversee implementation of the Epic electronic medical record across UBMD and its practice plans, a key initiative to enable a unified electronic health record system across UBMD, Kaleida Health and the Erie County Medical Center.
He also leads the university’s information security team and the Jacobs School of Medicine and Biomedical Sciences’ Office of Medical Computing, working to align IT strategies with institutional goals and regulatory requirements.
“UB is uniquely positioned as a leader in technology, research and education, and I’m thrilled to direct a digital strategy that will help keep the university at the forefront of health sciences innovation,” Khan says.
Khan joined UB with more than 20 years of experience in health care information systems. At Allegheny Health Network, Khan directed enterprise-wide data and digital services.
His previous work has involved the development of clinical data repositories, advanced analytics and reporting systems, artificial intelligence (AI) automation in clinical workflows, and other large-scale digital health initiatives. His research interests include federated health care data governance, shared data platforms and AI.
Khan holds a PhD in computer and information science and has also received master’s degrees in information quality, project management, and engineering management, and a bachelor’s degree in electrical and electronics engineering. He is an alumnus of the University of Arkansas at Little Rock and George Washington University. Khan has served as adjunct faculty at Colorado State University Global and the University of Arkansas at Little Rock.
After a combined four decades guiding their respective departments, two longtime chairs step aside
James D. Reynolds, MD ’78, earned his undergrad and medical degrees from the University at Buffalo and returned to join the Jacobs School faculty in 1988. Nine years later, he would become chair of the school’s Department of Ophthalmology, a position he would hold for nearly three decades.
John E. Tomaszewski, MD, a Philadelphia native, built a distinguished 30-plus-year career at the University of Pennsylvania before moving to Buffalo to become chair of the Department of Pathology and Anatomical Sciences in 2011.
Their roads to leadership positions at the Jacobs School were certainly dissimilar, but upon their recent retirements as chair of their respective departments, they leave with a shared legacy of respect, admiration and success.
“We extend our deepest gratitude for the service of both Dr. Reynolds and Dr. Tomaszewski. Their decades of exceptional leadership and their contributions to their respective fields have had a profound impact on the Jacobs School and have shaped and inspired the journeys of countless students, researchers, faculty, and staff,” said Allison Brashear, MD, MBA, dean of the Jacobs School and vice president for health sciences at UB. “We wish them both all the best in their well-deserved retirements.”

A renowned pathologist, researcher, educator, mentor and friend to many, John E. Tomaszewski, MD, stepped down from his role as Peter A. Nickerson, PhD, Professor and Chair of the Department of Pathology and Anatomical Sciences on July 1. His extensive research career has illuminated translational genitourinary pathology and led to new quantitative image analysis tools for digital pathology and predictive modeling of disease and therapy response. A SUNY Distinguished Professor, he played a pivotal part establishing and running the region’s most extensive COVID-19 testing program during the pandemic. Known for his steadfast leadership, Tomaszewski will stay on as interim chair during the search for the department’s new leader.
Academic degrees: Doctor of Medicine, University of Pennsylvania, 1977; Bachelor of Arts in biology, LaSalle College, 1973.
Publishing numbers: Peer-reviewed manuscripts: 346; book chapters: 25; abstracts: 71; reviews: 5; and editorials: 3.
Most meaningful awards: The David B.P. Goodman Award, University of Pennsylvania Department of Pathology and Laboratory Medicine Service and Citizenship Award, 2010; Mastership Award, American Society for Clinical Pathology, 2014; SUNY Distinguished Professor, 2017; Peter A. Nickerson, PhD, Professor and Chair, 2017; Gold Foundation Champions of Humanistic Care Award, 2021; Dean’s Award, Jacobs School of Medicine and Biomedical Sciences, 2016 and 2025.
One piece of advice for aspiring physicianscientists: Find a big bunch of the very best mentors in your field and communicate with your mentors clearly and regularly.
Favorite UB memories: Planning and openings of the new downtown medical campus buildings, especially the new Jacobs School of Medicine and Biomedical Sciences at High and Main Streets. Being honored as the inaugural Peter A Nickerson, PhD, Professor and Chair of Pathology and Anatomical Sciences.
How you would like to be remembered by your UB colleagues: Fully committed to the missions of education, research and practice in pathology and laboratory medicine and in anatomy. Building a graduate (PhD and MS) program in computational cell biology, anatomy, and pathology. Establishing early and continuous laboratory testing for SARSCoV-2 in Western New York during the COVID-19 pandemic.
Best thing about Buffalo: The lakes and the falls. The generosity and kindness of the people of Buffalo. THE BILLS.
First thing you plan to do in retirement: My wife Jane and I look forward to spending our days with our four children, their spouses, and our 11 grandchildren.

An active clinician-scholar for more than 40 years caring for all types of pediatric eye diseases, James D. Reynolds, MD ’78, retired July 1 as the Jerald and Ester Bovino Professor and Chair of ophthalmology. Much of his work has been seminal, especially in the field of ROP (retinopathy of prematurity), where he has been funded almost continuously by the NIH and industry for more than 25 years in ROP clinical trials. His 2002 paper on evidence-based ROP screening guidelines remains the standard to this day. “It has been a great run for me. My own career has been meaningful in so many ways, and the department has blossomed beyond any expectations,” he says.
Academic degrees: Doctor of Medicine, University at Buffalo, 1978; Bachelor of Arts in biology, University at Buffalo, 1974.
Publishing numbers: peer-reviewed articles: 81; non-peer-reviewed articles: 20; chapters: 9; and editorials: 2.
Most meaningful awards: The Al Biglan Medal awarded by my fellowship alma mater, the University of Pittsburgh, for excellence in the field of ophthalmology.
Research project/ discovery you are most proud of: Leading the NIH-funded LIGHT ROP trial and publishing the results in the New England Journal of Medicine and my work as one of the six world experts who led the RAINBOW trial that set the standard in Europe for ROP anti-VEGF treatment that was published in The Lancet.
One piece of advice for aspiring physicianscientists: Always say yes! This attitude leads to many expected and unexpected career advancements.
Favorite UB memories: The grand opening of the Ira G. Ross Eye Institute on the Buffalo Niagara Medical Campus in 2007; achieving top third status of ophthalmology programs at the NIH; and of course, ALL the people who helped me along the way.
How you would like to be remembered by your UB colleagues: As an honest hard worker who led by example and consensus, always supportive of my students, faculty and staff while maintaining a fierce sense of personal honor and always putting the patient first, regardless of circumstance.
Best thing about Buffalo: I would have to boil it down to the people. They are the salt of the earth, as my country family used to say. They have made the best patients in the world.
First thing you plan to do in retirement: I have already started my two first things: spending time with grandchildren and finding more work.
“We extend our deepest gratitude for the service of both Dr. Reynolds and Dr. Tomaszewski. Their decades of exceptional leadership and their contributions to their respective fields have had a profound impact on the Jacobs School and have shaped and inspired the journeys of countless students, researchers, faculty and staff.”
- Allison Brashear, MD, MBA

A prominent collection of community leaders and alumni have joined the Jacobs School, helping to steer and support the school as its new Dean’s Advisory Council. Members of the council serve the school in the core areas of advocacy and community engagement. Chaired by Jerry Jacobs, Jr. and Cindy Abbott Letro, the Dean’s Advisory Council meets several times per year and acts as an advisory board for Dean Allison Brashear, MD, MBA, and school leadership. Members of the council are appointed to threeyear terms.
“I’m
deeply grateful for the support of the alumni and business leaders who serve on the Dean’s Council. Their leadership, contributions and insight are invaluable resources to us and play a vital role in advancing the mission of
the Jacobs School.”
- Allison Brashear, MD, MBA
The council launched in 2024. Scott Bieler, CEO and President of West Herr Auto Group, served on the council during the 2024-25 term. Current members include:

Cappuccino works at Roswell Park Comprehensive Cancer Center specializing in the surgical management of breast cancer and is an associate professor at the Jacobs School. She serves on the admissions committee at the Jacobs School and also serves as faculty advisor of CuMIN, the Jacobs School’s culinary medicine interest group. She was a founding board member for the UB Child Care Center and co-chaired UBreathe Free, the committee that made all university campuses smoke free. She was honored as one of 50 of America’s most positive physicians nationally.
A dedicated community volunteer, she is currently on the boards of the Buffalo AKG Art Gallery and the University at Buffalo Foundation and an emeritus member of the boards for the Western New York Women’s Foundation, and Chaîne des Rotisseurs Foundation. She previously served on the boards of Lockport City Ballet and the Kenan Center. She has chaired numerous charity events for schools and cultural organizations, including the Eastern Niagara United Way, the UB Scholarship Galas and Elmwood Franklin School.
She is a features editor and writer for Gastronome and Cuvee, food and wine magazines for the Chaîne des Rotisseurs. She and her husband have also participated in medical missions to Kenya, and they have produced five feature-length films with their son for Vertebra Film Development.

Internationally recognized as a leader in philanthropy, Dedecker retired as president and chief executive officer of the Community Foundation for Greater Buffalo in December 2022.
During her 17-year tenure at the Community Foundation working with individuals, families, foundations and organizations to steward their charitable assets, the Community Foundation grew to more than $870 million.
Dedecker is a member of the Generosity Commission—a blue-ribbon national panel focused on nurturing giving and volunteering. Her recent board service includes FSG and the Global Fund for Community Foundations. She is president emeritus of the Junior League of Buffalo, the Association of Junior Leagues International and the National Women’s Hall of Fame.
In recognition of her civic sector expertise, Dedecker was appointed to the White House Council on Service and Civic Participation and named co-chair of the U.S. Committee of the United Nations International Year of the Volunteer.
For her contributions, she was inducted into the WNY Business Hall of Fame in 2024 and was named the 2018 Buffalo Niagara Executive of the Year by the UB School of Management.

Feldstein leads Retail and Business Banking at M&T Bank, supporting local consumers and business owners across the company’s communities.
In Retail Banking, he oversees a team of more than 7,000 employees across over 900 branches that serve approximately 2 million customers.
In Business Banking, which includes about 800 employees, he collaborates with regional leaders and local business bankers throughout the Northeast U.S. to provide services and financial guidance to more than 330,000 small and mid-sized businesses.
Feldstein has nearly 30 years of experience in the financial and professional services industry. Prior to his current role, he served as M&T’s Western New York regional president.
He is a member of the executive committee for the Buffalo Niagara Partnership and serves on the boards of both the WNY Community Foundation Business Leaders Task Force and the Westminster Foundation. He also serves as the executive sponsor for M&T’s Hispanic/Latinx Employee Group.
Before joining M&T, he held positions at Skadden, Arps, Slate Meagher & Flom LLP in New York and Diamond Management Consulting in Chicago.

Higgins serves as president and CEO of Shea’s Performing Arts Center, where he aims to position the three-theatre campus to sustain and grow its centurylong tradition of delivering exceptional experiences and top performances to theatre goers. His work includes elevating Shea’s Buffalo by upgrading patron amenities and preserving the institution’s historic character, building on the theatre’s foundational standing as a magical place.
For over 19 years Higgins served as a member of Congress, maintaining a focus on targeted initiatives which addressed the needs and leveraged the strengths unique to Western New York. A member of the Congressional Arts Caucus and author of federal Historic Tax Credit legislation, Higgins has long recognized the social and economic value of investments in preservation and culture.
Before serving in Congress, Higgins was elected to the Buffalo Common Council and later the New York State Assembly.

As CEO for Delaware North, a familyowned, global leader in hospitality and entertainment, Jacobs oversees the company and its seven operating subsidiaries, focusing on strategic growth and planning, corporate governance and financial management. Jacobs has served several philanthropic, civic and business organizations, including as board chair for the UB Council, the primary oversight and advisory body to the university’s president and senior officers. He is on the board of The Corps Network, a national organization that engages young people and veterans through service programs, and board chair for biopharmaceutical startup Mimivax. He is a founding board member for the Say Yes Buffalo educational initiative. Jacobs’ service to the United Way of Buffalo and Erie County includes chair of the board of directors and annual fundraising campaign. He is a past member of the board of regents at Georgetown University and served three terms on the board for the UB Foundation. He is past chair of the Nichols School board of trustees, where he founded the Jacobs Scholars program for high-achieving students with financial need.
Jacobs completed a term on the U.S. Department of Commerce’s Travel and Tourism Advisory Board in 2015 and was named to the U.S. Secretary of Interior’s “Made in America” Outdoor Recreation Advisory Committee in 2018.

Letro is a community volunteer and marketing specialist with over 30 years of experience in the broadcast field. She currently serves as the chair of the Western District of New York State Parks, chairs Visit Buffalo Niagara, the region’s convention and tourism bureau, and is past chair of the Buffalo Niagara Film Commission. She currently serves or has served on the St. Bonaventure Board of Trustees, the Community Foundation of Greater Buffalo, the Kleinhans Music Board, and the Theodore Roosevelt Inaugural Site. She is the past chair of the Board of Directors of the Buffalo Philharmonic Orchestra and the Burchfield Penney Art Center.
She is consistently listed in the Business First’s Top 200 Women of Influence and was listed in its Top Ten Women of Influence in 2022.
Letro is business manager of her husband’s law firm, Francis M. Letro Attorneys at Law, and makes her home in the city of Buffalo.

McGlynn is a distinguished leader in the pharmaceutical and biotechnology industries, with a career spanning over four decades dedicated to advancing global health.
McGlynn began her career at Merck, where she held various leadership roles from 1983 to 2009, culminating as president of Merck Vaccines and Infectious Diseases. She later served as CEO of the International AIDS Vaccine Initiative (2011–2015), leading global efforts in HIV vaccine research and advocacy.
Currently, she serves on the boards of Novavax, Inc., Amicus Therapeutics, and the University at Buffalo Foundation, contributing her expertise to organizations focused on innovative vaccines, rare disease treatments, and higher education. She is also president and board chair of the HCU Network America, a nonprofit dedicated to supporting families affected by homocystinuria and advancing research and policy for this rare metabolic disorder.
McGlynn’s contributions have been recognized with numerous honors, including a UB Honorary Doctorate (2017), Distinguished Alumni Award (2010), and the Leadership in Pharmaceutical Award (2003) from UB’s School of Management.

Roth was one of the original founders of Sharp Community Medical Group and has served on the board of directors since its inception in 1989, holding a number of council seats, including the executive committee. He also serves on the Sharp HealthCare Board of Directors. Roth was elected president of Sharp Community in July 2011. In 2008, he was named to the San Diego Magazine’s List of Top Doctors and in 2010, he was the recipient of the Sharp Memorial Hospital/Spirit of Planetree Award.
Roth began his private practice of medicine in 1986 at Sharp Cabrillo Hospital. He went on to found San Diego Internal Medicine Associates in Kearny Mesa, and subsequently San Diego Hospitalist Associates, where he practices internal medicine and leads the Metro Hospitalist team.
He completed his medical education and internship at the University at Buffalo. He completed his residency at UCSD Medical Center. Roth is Board Certified in internal medicine with a specialty in urology.

Walsh is the chairman of Walsh Duffield Companies, Inc., a family-owned insurance agency headquartered in Buffalo. Representing the fifth generation of leadership, he joined the firm in 1973 after gaining experience at Citibank in New York City and Aetna Life and Casualty Company in Hartford. His extensive civic involvement includes leadership and support roles with organizations such as the United Way of Buffalo & Erie County, the Darwin Martin House Restoration Corporation, the Albright-Knox Art Gallery, and the Buffalo Philharmonic Orchestra, among many others.
Walsh is also deeply committed to higher education and athletics. He co-chaired the local organizing committee for the NCAA’s 2003 Frozen Four hockey finals in Buffalo and served as chair of the Yale Alumni Schools Committee of Western New York, interviewing over 900 applicants, and holding various leadership roles with the Association of Yale Alumni, Yale Alumni Fund and its Development Board.
He has received numerous awards for his professional excellence and community service, including the Galanis Award for Excellence in Family Business, the UB President’s Medal, and the NCCJ Citation Award. The United Way recognized him as Philanthropist of the Year.

Wilson currently serves as one of the three Life Trustees appointed to guide the Ralph C. Wilson, Jr. Foundation, a grantmaking organization established by her late husband, Ralph Wilson.
Based in Detroit, the Foundation began with a grantmaking capacity of $1.2 billion over a 20-year period. To date, the Foundation has distributed more than 1,000 grants across its five areas of focus: Active Lifestyles; Preparing for Success; Entrepreneurship and Economic Development; Caregivers; and Nonprofit Support & Innovation.
Mary Wilson has been an outspoken champion for the city of Buffalo and is a supporter of many Buffalo organizations. During Ralph’s ownership of the Buffalo Bills, Mary worked to establish the Western New York Girls in Sports program and continues to bring together more than 200 girls, ages 9-12, to participate in various sports taught by young athletes from local universities and sports clubs. She is a supporter of the Buffalo AKG Art Museum, Burchfield Penny Art Center, Buffalo Philharmonic Orchestra, Hospice of Western New York, First Tee, Oishei Children’s Hospital, SPCA Serving Erie County and FeedMore WNY, among others.
She is a former board member of the USTA Tennis Foundation and played in the Wimbledon Championships in 1976. Wilson was also a past president of the National Senior Women’s Tennis Association.
Steven J. Fliesler, PhD, SUNY Distinguished Professor and Meyer H. Riwchun Endowed Chair Professor of ophthalmology in the Jacobs School, has been honored with the 2025 Schroepfer Medal from the American Oil Chemists’ Society (AOCS).
The medal is typically awarded every other year. This one-of-a-kind prize has been awarded to 12 internationally recognized academic scholars from the United States and Europe since its inception in 2002.
An internationally renowned vision scientist, Fliesler is considered the world’s leading expert on cholesterol metabolism in the retina.
His research was instrumental in describing for the first time the involvement of the lipid intermediate pathway in glycoprotein synthesis in the human retina and the importance of protein glycosylation for normal retinal photoreceptor cell differentiation. The lipid intermediate pathway shares some molecular constituents with the biochemical pathway used for cholesterol synthesis.

“I am extremely honored to have been recognized by the AOCS for my research over the past four decades in the area of cholesterol metabolism in the retina,”
Fliesler says.
“This lifetime achievement award is particularly meaningful to me, because I performed my PhD research under the guidance of Professor George J. Schroepfer, for whom this award is named, at Rice University in Houston, Texas, many years ago.”
“No one is more deserving of this award than Steve Fliesler. Steve has made important contributions to the understanding of Smith-Lemli-Opitz syndrome (SLOS), a devastating disorder caused by mutations in a gene in the cholesterol biosynthesis pathway,” says Ned A. Porter, PhD, professor emeritus of
chemistry at Vanderbilt University School of Medicine.
Indeed, there is now what is known as “the Fliesler model” of the disorder, a pharmaceutically altered rodent that has been important in understanding the consequences of the perturbed cholesterol biosynthesis found in SLOS, Porter notes.

Beth A. Smith, chair of the Department of Psychiatry, was accepted into the prestigious Executive Leadership in Academic Medicine (ELAM) program for 2025-26. The highly competitive fellowship prepares accomplished women professors for senior leadership roles across the health care landscape.
Beth A. Smith, MD ’00, chair of the Department of Psychiatry, has been chosen as a 2025-2026 fellow for the prestigious Hedwig van Ameringen Executive Leadership in Academic Medicine (ELAM) program.
Hosted by Drexel University College of Medicine, this highly competitive, yearlong fellowship builds upon Smith’s outstanding leadership and dedication to advancing psychiatry by her executive leadership skills.
ELAM prepares accomplished women professors at academic health centers for senior roles across the health care landscape, from academic institutions— medicine, dentistry, public health and pharmacy—to hospitals and health care systems, including C-suite positions. During the program, Smith, a clinical professor of psychiatry and pediatrics, will undertake online assignments, engage in community building and lead a collaborative Institutional Action Project focused on an institutional or departmental challenge.
This project will address an institutional
or departmental need or priority, further demonstrating her commitment to impactful leadership.
In a highly competitive selection process, Smith, was one of 100 ELAM fellows accepted into this year’s class. This cohort comprises exceptional leaders who are capable of making critical systemic change.
“I am deeply honored to be selected as an ELAM fellow,” says Smith. “This opportunity marks a personal milestone and a meaningful way to contribute to the future of academic medicine. I look forward to collaborating with leaders across the country, growing through the program’s curriculum, and bringing new perspectives back to Jacobs School to help strengthen our culture of collaboration, excellence and innovation.”
Two Jacobs School faculty members have been named SUNY Distinguished Professors, the highest faculty rank in the SUNY system.
Michael E. Cain, MD, professor of medicine and biomedical engineering; and Jian Feng, PhD, UB Distinguished Professor of physiology and biophysics, were appointed to the distinguished professor ranks by the SUNY Board of Trustees at its meeting on April 29.
The rank of distinguished professor is an order above full professorship and has three co-equal designations: Distinguished Professor, Distinguished Service Professor and Distinguished Teaching Professor.
Cain was named a Distinguished Service Professor in recognition of his “distinguished reputation for service not only to the campus and the University, but also to the community, the State of New York or even the nation, by sustained effort in the application of intellectual skills drawing from the candidate’s scholarly research interests to issues of public concern.”
Feng was named a Distinguished Professor in recognition of his international prominence and distinguished reputation within his chosen field.
Cain, who served as dean of the Jacobs School for 15 years, is an internationally recognized cardiovascular physicianscientist who specializes in the area of abnormal heart rhythms.
He has been recognized for his long-term leadership role in his field with numerous awards, including the Distinguished Service Award from the Heart Rhythm Society, the Stanley J. Sarnoff Spirit Award from the Scientific Board of the Sarnoff Endowment for Cardiovascular Science and the Arthur E. Strauss Award from the American Heart Association.
He is also the recipient of the UB President’s Medal for exemplary leadership, and the Legacy Award from the National Federation for Just Communities of Western New York.
Feng is a world leader in the molecular and cell biology of Parkinson’s disease. His research has centered on proteins and neurotransmitters in the brain that are pathophysiological elements in Parkinson’s.

He has identified the critical roles of the parkin gene in Parkinson’s disease. Feng developed the use of human-induced pluripotent stem cells (iPSC) to generate patientspecific human dopaminergic neurons in vitro to study the role of parkin in the disease.

Among his numerous honors are designation as a UB Distinguished Professor, the Visionary Inventor Award, the Bridge Award for Translational Research, UB Exceptional Scholars: Sustained Achievement Award, the SUNY Chancellor’s Award for Excellence in Scholarship and Creative Activities, and the Stockton Kimball Award.

Teresa L. Danforth, a clinical associate professor of urology, has been named to the American Urological Association 202526 Leadership Class in recognition of her leadership and research achievements.
In recognition of her leadership, research achievements, and educational excellence, Teresa L. Danforth, MD ’07, has been named to the American Urological Association (AUA) 2025-26 Leadership Class.
Danforth is a clinical associate professor and residency program director in the Department of Urology and is also chief of urology at Kaleida Health.
A longtime board member of the AUA’s Northeastern Section, Danforth was elected to the organization’s leadership class this spring, in company with emerging top urologists across the country.
Danforth says that joining the leadership class could lead to making a larger, national impact on the field of urology.
“I think being a part of this leadership course will put me in a position to make more of an impact at that level and will provide me a better skill set and also provide communities and networking opportunities to meet with mentors,” she says.
Involvement has also meant being able to work with and be mentored by renowned urologists and AUA leaders, Danforth says, and collaborating with other inductees on a collaborative research project.
Danforth is co-investigator on two National Institute of Diabetes and Digestive and Kidney Diseases grants: a $3.3 million grant focusing on pelvic pain management and a $1.6 million grant to study catheterassociated urinary tract infection (UTI).

Gary Iacobucci, a general psychiatry resident and research assistant professor in biochemistry at the Jacobs School, was selected as a 2025 Outstanding Resident by the National Institute of Mental Health.
Gary Iacobucci, MD, PhD, wasn’t one of those people who always knew they’d go to medical school. As an undergraduate at the University at Buffalo, his main interest was research. But as he headed into a biochemistry doctoral program at UB, he became more interested in the clinical aspects of what he was studying.
It was clearly the right decision. This summer, Iacobucci was notified by the National Institute of Mental Health that he was selected to receive its prestigious 2025 NIMH Outstanding Resident Award.
A general psychiatry resident and research assistant professor in biochemistry in the Jacobs School, he is one of just 12 residents nationwide chosen for this honor.
Iacobucci’s interest in clinical care began while doing doctoral work in the laboratory of Gabriela K. Popescu, PhD, professor of biochemistry. When he mentioned he was considering medical school, she connected him with a psychiatrist colleague he could shadow.
He began the MD program in the Jacobs School in 2019. And in his fourth year, as all medical students do, he began looking at residency programs.
Iacobucci started looking at the Jacobs School’s psychiatry residency for its strong, high-volume clinical program and emphasis on psychotherapy.
“What I appreciate most is how understanding and flexible the department has been in developing a program that helps me bolster my ability to be a good clinician while allowing me to develop my own unique vision as to what my research program will be,” he says.
David Cazares Dorantes, a secondyear medical student in the Jacobs School, has been selected as one of five recipients of the Association of American Medical Colleges (AAMC) 2025 ACE Award for Advocacy, Collaboration and Education.
The award recognizes academic medicine champions who are honored for leading and collaborating with the nation’s medical schools and academic health systems to improve the health of patients, families and communities nationwide.
The AAMC cited Dorantes’ work at the Good News Clinics in Georgia and as a Spanish medical interpreter, experiences that reflect his commitment to serving vulnerable communities.
He is assistant program manager for UB HEALS, the Jacobs School’s student-run street medicine initiative, and he serves as class representative for Polity, the student
Renée Reynolds, MD, clinical associate professor of neurosurgery in the Jacobs School, has been installed as the inaugural recipient of the Kevin and Janet Gibbons Endowed Chair in Neurological Surgery.
Reynolds officially accepted the role at a ceremony on May 27 to recognize this appointment and to acknowledge the generosity of Kevin J. Gibbons, MD, and Janet Gibbons, who supported the endowed chair, along with UBMD Neurosurgery.
“This endowed chair represents more than just a prestigious title. It is a powerful investment in our future,” said Allison Brashear, MD, MBA, UB’s vice president for health sciences and dean of the Jacobs School. “Her growth will not only advance scientific discovery and advance clinical care and medical education, but her work also directly benefits patients, students and families in Western New York and beyond.”
Elad I. Levy, MD, MBA, the L. Nelson Hopkins III, MD, Professor and chair of neurosurgery, spoke about the Gibbons family’s generosity, dedication, and lasting
government organization. In Buffalo, he works at Jewish Family Services on refugee resettlement. A member of the American Medical Association’s Medical Student Section Committee on Civil Rights, Dorantes is also the UB representative for the Latino Medical Student Association.
“Even so early in his career, David is absolutely committed to putting patients first,” says Allison Brashear, MD, MBA, UB’s vice president for health sciences and dean of the Jacobs School, “whether that means being boots on the ground to help unhoused people get care, translating English to Spanish, or serving in our student-run free clinic. With this award, the AAMC is recognizing the powerful, positive impact his advocacy is having on our community.”
Dorantes takes absolutely nothing for granted. He says there have been multiple times in his life when things looked hopeless, but good people stepped in to help. Those experiences left him with an unwavering sense of responsibility to help improve similar circumstances for others. “When you watch your parents sacrifice
so much, there’s no way I can see those sacrifices and not do everything I can to help my neighbor,” he says.
“UB has a really big presence in the community and that’s huge for me,” says Dorantes. “The Jacobs School has provided me the resources to pursue my advocacy work and my need to serve the community that I live in. I think the school is really good at that, giving us avenues to serve others and not be alienated from the people we care for.”
David Cazares Dorantes is in his second year in the MD program at the Jacobs School. He has been selected as one of five recipients of the Association of American Medical Colleges (AAMC) 2025 ACE Award for Advocacy, Collaboration and Education.
impact.
“It is with humility and gratitude that we acknowledge the support of Kevin, Janet and the Gibbons family, and our UBNS partners,” he said. “You’ve given us the gift of this chair, which will continue to inspire and shape the future of neurosurgery education for generations to come.”
Gibbons served as senior associate dean for clinical affairs and executive director of UBMD Physicians’ Group. He joined the Jacobs School’s neurosurgery faculty after completing his residency at UB in 1993 and would later serve as vice chair and program director.
Levy shared some of Gibbons’ research achievements, including development of the Gibbons classification, used to evaluate motor function in patients with spinal cord injuries. In 2017, Gibbons authored a widely read and cited paper in Neurosurgery assessing surgical headwear and its effects on infection rates.
Reynolds reflected on her journey through medicine and neurosurgery and now as an endowed chair recipient.
“Many of the accolades necessary to be considered for such a recognition can be counted—research papers, grants, selected abstracts, visiting professorships,” she
said, but was reminded of a favorite quote, that “not everything that can be counted counts, and not everything that counts can be counted.”
“There is no greater full-circle moment than watching a resident you have trained move on to independent practice, start to ascend the ranks of our national organizations, become assistant program directors or program directors themselves or, most meaningfully, picking up the phone just to tell you thank you for everything you’ve done to help them get there.”


As they age, some people find it harder to understand speech in noisy environments. Now, UB researchers have identified the area in the brain, called the insula, that shows significant changes in people who struggle with speech in noise.
According to David S. Wack, PhD, first author and associate professor of radiology in the Jacobs School, a study published in the journal Brain and Language found that the left insula shows stronger connectivity with auditory regions in people who struggle with speech in noise, suggesting a permanent rewiring of brain networks that persists even when they’re not actively listening to challenging speech.
“When you have hearing loss, you are recruiting other areas of the brain to do more processing in order to decode what’s going on,” Wack says. “What’s interesting is that we found the insula working harder when the brain was supposedly at rest, when there was no speech in noise.”
The new molecule targets a protein called Magi-1, a scaffolding protein that brings specific proteins together at specific locations within the cell membrane. One of the proteins it interacts with is NaV1.8, an ion channel that plays an important role in transmitting pain.
Prediabetes, when blood sugar is higher than normal but not high enough to be considered diabetes, is more lifethreatening in people aged 20-54 than it is in older populations, according to a paper published in JAMA Network Open.

A vaccine under development at UB has demonstrated complete protection in mice against a deadly variant of the virus that causes bird flu.
The work, detailed in a study published in the journal Cell Biomaterials, focuses on the H5N1 variant known as 2.3.4.4b, which has caused widespread outbreaks in wild birds and poultry, in addition to infecting dairy cattle, domesticated cats, sea lions and other mammals.
In the study, scientists describe a process they’ve developed for creating doses with precise amounts of two key proteins— hemagglutinin and neuraminidase—that prompt the body’s immune system to fight bird flu.
It’s also a potential step toward more potent, versatile and easy-to-produce vaccines that public health officials believe will be needed to counteract evolving bird flu strains that grow resistant to existing vaccines.
“We obviously have a lot more work to do, but the results thus far are extremely encouraging,” says the study’s lead author Jonathan F. Lovell, PhD, SUNY Empire Innovation Professor of biomedical engineering.
That finding, he says, has implications for how dementia may develop, since the insula is also associated with early dementia.
“It’s not that hearing loss causes dementia,” Wack says, “but if we could find a way to preserve the fidelity of the signal coming in, then the brain wouldn’t have to start compensating for that hearing loss.”
A new molecule developed by Jacobs School researchers acts like a local, longlasting anesthetic, providing robust pain relief for up to three weeks, according to the results of preclinical studies reported recently in the journal Pain.
“Local anesthetics dramatically changed health care when first introduced into clinical practice during the turn of the 20th century,” notes Arindam Bhattacharjee, PhD, professor of pharmacology and toxicology and senior author on the paper. “The limitation with local anesthetics is that they aren’t very selective for your pain fibers—they block touch sensation as well— and they don’t last very long. In our new paper we showed that a single injection locally can relieve chronic pain behavior for three weeks.”
“The literature has been inconsistent, particularly when accounting for key modifying factors, such as age, race/ ethnicity and comorbidities,” says first author Obinna Ekwunife, PhD, assistant professor of medicine. “We wanted to explore whether these factors influenced the association between prediabetes and mortality in a nationally representative U.S. adult population.”
The researchers analyzed data from the National Health and Nutrition Examination Survey (NHANES), the ongoing national survey run by the U.S. Centers for Disease Control and Prevention that measures the health and nutrition of children and adults.
The data showed a significant association between prediabetes and mortality before the researchers controlled for variations among demographics, lifestyle factors and comorbidities. But once they controlled for those factors, the association went away.
“However, we found that the significant relationship between prediabetes and mortality was maintained after adjustment when the analysis focused on adults aged 20-54,” says Ekwunife.
John C. Hu, MD, PhD, clinical assistant professor of medicine in the Division of Infectious Diseases, is a co-senior author on a study published in the journal Clinical Infectious Diseases on secondary bacterial pneumonia following viral infections.
The retrospective study design leveraged the VA’s internal Corporate Data Warehouse—a comprehensive national database that includes health records from VA hospitals across the country.
The researchers compared how often people developed bacterial pneumonia after having the flu, RSV, or COVID-19, helping them to see if COVID-19 leads to similar or different risks compared to these other respiratory viruses.
“We found that people who had the flu or RSV were more likely to develop a secondary bacterial infection caused by Streptococcus pneumoniae. However, this was not the case for people who had COVID-19,” Hu says.
“This may suggest that COVID-19 behaves differently from the flu and RSV when it comes to how it interacts with respiratory bacterial pathogens, and perhaps our immune system.”

Researchers have shown for the first time that intermittent fasting increases the efficacy of anti-androgen therapy in prostate cancer, according to a paper reporting preclinical results published in Cancer Research.
Proteins, carbohydrates and fats are necessary for the uncontrolled growth of cancer cells and the typical Western diet in particular, with its heavy animal fat and protein content, has been linked to increased incidence of cancer and poor prognosis.
Consequently, caloric restriction has emerged as a potential strategy for reducing the incidence of cancer and delaying cancer progression. It has been shown in preclinical models to reduce circulating growth factors and hormones that promote cancer.
“Diet can have a significant impact on the biology of prostate cancer and dietary interventions should be seen as an adjuvant tool,” says Roberto Pili, MD, corresponding author and associate dean for cancer research and integrative oncology in the Jacobs School.
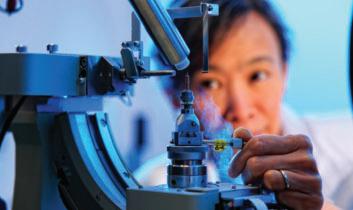
A breast scan for detecting cancer takes less than a minute using an experimental system that combines photoacoustic and ultrasound imaging, according to a study in IEEE Transactions on Medical Imaging.
“Our system, which is called OneTouchPAT, combines advanced imaging, automation and artificial intelligence—all while enhancing patient comfort,” says the study’s corresponding author Jun Xia, PhD, professor in Department of Biomedical Engineering.
Xia and colleagues have been studying photoacoustic imaging, which works by emitting laser pulses that cause lightabsorbing molecules to heat up and expand. This in turn creates ultrasound waves that allow medical professionals to detect blood vessels that often grow more in cancerous tissues.
Typically, these systems require a sonographer to manually scan the breast, or they rely on separate devices for photoacoustic imaging and ultrasound imaging.

OneTouch-PAT combines both scans automatically. The device performs a photoacoustic scan first, followed by an ultrasound scan, then repeats this pattern in an interleaved way until the entire breast is covered. The system then processes the data using a deep learning network to improve image clarity. Ultimately, the research team found that OneTouch-PAT provides a more in-depth and clearer view of breast tumors compared to photoacoustic and ultrasound imaging systems that are operator-dependent.

Monica C. Pillon, assistant professor of structural biology, is senior author on a new study published in Nature Communications that provides a detailed structure of a human enzyme critical for antiviral defense and platelet function.
Monica C. Pillon, PhD, assistant professor of structural biology, is senior author on a new study that provides a detailed structure of a human enzyme critical for antiviral defense and platelet function.
Through biochemistry and advanced imaging, the research, published online in Nature Communications, uncovered the molecular principles underlying SLFN14’s RNA processing activity, Pillon says.
“Gene dysregulation is a hallmark and major culprit of disease. A central determinant of gene expression is RNA abundance, which is fundamentally the balance of RNA synthesis and RNA decay,” she says.
“Ribonucleases are the centerpiece to many RNA processing and decay pathways,” Pillon adds. “For this reason, my research program focuses on understudied ribonucleases, like SLFN14, to understand their vital role in defining eukaryotic gene expression and cell fate.”
During a viral infection, SLFN14 is activated to repress gene expression and limit viral replication. However, exactly how this happens is still an active area of research.
SLFN14 dysregulation is linked to human diseases, including ribosomopathies and inherited thrombocytopenia, a bleeding disorder that is often characteristic of low platelet count and low platelet activation.
By Ellen Goldbaum | Photos by Sandra Kicman
It was about trauma and pain and remembrance. It was about the stories behind the grim statistics. It was about honoring the lives of victims cut tragically short.
Those factors and more made the 2025 Remembrance Conference an equally moving experience whether participants traveled across town or across the country to attend.
The idea for the conference was sparked in 2023 in a conversation between Allison Brashear, MD, MBA, vice president for health sciences and dean of the Jacobs School of Medicine and Biomedical Sciences, and Aron Sousa, MD, dean of the Michigan State University (MSU) College of Human Medicine. Both of their campuses had recently been impacted by gun violence. Soon thereafter, faculty and students from both schools began meeting annually to remember, to heal, to share their experiences and support each other.

in 2024. In June 2025, the Jacobs School hosted a three-day event focusing on the special role medical schools and health care in general can play in working to reduce firearm injuries and deaths through a public health approach.
“The trauma goes beyond the victim,” Brashear noted. “We need to be thinking about what we can do as health care professionals. We want to energize people to go back to their schools and communities and say, ‘What can we do?’”
In his opening remarks, Sousa noted that not all communities are affected by gun violence in the same way. “This is about racism. This is about domestic violence. This is about mental health. That’s why we’re here.”

From Friday afternoon through Sunday morning, 75 participants and speakers gathered at the Jacobs School. They came from UB and MSU, and from local and national universities and organizations including Yale, SUNY Downstate, the University of New Mexico, the Association of American Medical Colleges (AAMC), Western New Yorkers Against Gun Violence, Most Valuable Parents (MVP), St. Joseph University Church, the 5/14 Oral History Project, Erie County Central Police Services, Erie County Medical Center, The Non-Violence Project, BRAVE, SNUG and many others.
They learned that in 2022, more than 48,000 people died from firearms in the U.S.; more than half of those were suicides. In the keynote address that opened the conference, Megan Ranney, MD, MPH, dean of the Yale School of Public Health, explained why public health is the appropriate approach for addressing gun violence.
“We need to be thinking about what we can do as health care professionals. We want to energize people to go back to their schools and communities and say, ‘What can we do?’”
-
Allison Brashear, MD, MBA
It begins with gathering data about the threat, identifying what puts people at higher risk or what protects them, developing and evaluating interventions, and then implementing the most successful interventions.
The Remembrance Conference is the offshoot of a 2023 conversation between medical school deans in the aftermath of deadly shootings at or near their respective schools. Since then, Allison Brashear, dean of the Jacobs School of Medicine and Biomedical Sciences, and Aron Sousa, dean of the Michigan State University College of Human Medicine, have endeavored each year to bring together faculty, staff, students, community groups, elected officials and industry experts to remember, heal, share their experiences and advocate for safer communities.

She said that such a harm reduction approach has been remarkably successful in mitigating the harm caused by car crashes. A combination of drunk driving laws, public education, seat belts, airbags, speed limits and engineering improvements to cars, have all led to reductions in deaths due to vehicle crashes.
Ranney said that such an approach has not been tried, “partly because there was no funding for this type of work and because people like me were told not to work on this.”
She has not been deterred. She cofounded the American Foundation for Firearm Injury Reduction in Medicine (AFFIRM), a nonprofit committed to ending the gun violence epidemic through a nonpartisan, public health approach; it works with a variety of communityfocused organizations, such as 4H Shooting Sports clubs.
Rob Gore, MD ’02, an emergency medicine physician at University Hospital at Downstate in Brooklyn, the author of “Treating Violence: An Emergency Room Doctor Takes on a Deadly American Epidemic,” and a Jacobs School alumnus, is similarly focused on preventing gun violence.

Working as an emergency medicine physician at Brooklyn’s University Hospital at Downstate, he saw how many of his patients were young Black men with life-threatening wounds from gunshots or stabbings. It drove him to start searching for the roots of violence and ways to prevent it. He founded KAVI, Kings Against Violence Initiative, a violence intervention program in Kings County.
KAVI operates programs in schools and hospitals through a network of volunteers who work with patients and their families; they work on multiple levels to prevent acts of retribution, make referrals and ultimately establish support systems. “If your basic needs are not met, you’ll go back out to a volatile situation,” Gore said.
He adds that every health care worker who treats these patients is also affected. “There’s the stressor from trying to keep someone alive,” Gore said. “That’s its own special beast. The idea that ‘Wow, if I just had a little more time and a little more money, I could keep this person alive.’ This is the work. This is the challenge.”
‘Not anti-gun, anti-shooting-people’
Similar conditions working in his state’s only Level 1 trauma center prompted Richard Miskimins, MD, assistant professor of surgery and trauma medical director at the University of New Mexico, to become engaged in this work. New
Mexico, a very rural state, is among those with the highest violent crime levels in the U.S. as well as having one of the highest suicide rates. “It’s a blue state that loves guns,” said Miskimins, who adds, “I am not anti-gun. I am anti-shooting-people.”
His advice for working in this space: “Avoid being an absolutist. Are you unwilling to compromise? Then you’re part of the problem.” He works with organizations that might seem unlikely; he has a strong partnership with a local shooting range, for instance. He and his colleagues do Stop the Bleed events at local high schools, where they also teach conflict resolution and violence interruption.
“Avoid being an absolutist. Are you unwilling to compromise? Then you’re part of the problem.”
- Richard Miskimins, MD
He stressed the need to base firearm injury prevention on solid data and to tailor responses to specific communities. “We track the number of times kids have guns in schools,” he said, “we facilitate coordination between agencies.”
Miskimins has led numerous antiviolence initiatives through social intervention, education, mentorship and legislation. He has worked for the establishment of an Office of Gun Violence Prevention in New Mexico and a safe gun storage law that makes adults criminally liable if their negligence makes a firearm accessible to a minor.
Other legislative initiatives discussed included New York State’s Extreme Risk Protection Order (ERPO), also known as the “Red Flag Law,” which 21 states now have. Gale R. Burstein, MD, commissioner, Erie County Department of Health, and professor of pediatrics, Jacobs School, and

A panel of medical students discussed how relevant discussions about gun safety are to pediatrics, especially since firearm violence is the most likely cause of death for children in the U.S. The students, who established the UB chapter of Scrubs Addressing the Firearm Epidemic (SAFE), noted that so much attention is paid to safety features like bike helmets and seatbelts, it is essential to also include gun safety when talking to patients.
“Normalize the discussion,” said Kerryann Koper, a fourth-year student at

“We want to reach every single medical student,” she said, “and help them incorporate firearm safety into patient care conversations.”
Those conversations often don’t happen because clinicians don’t feel confident about bringing the topic up, a concern echoed later in the conference by keynote speaker Patricia Logan-Greene, PhD, associate professor in the UB School of Social Work and co-leader of the Grand Challenge in Social Work to Prevent Gun Violence. She said that social workers don’t typically bring up the subject because of a

Ryan Belka, JD, assistant attorney general, explained how ERPOs function. If a health care provider has concerns about a patient who has access to weapons, they should report their suspicions to law enforcement who may then choose to file an ERPO.
“We want to reach every single medical student and help them incorporate firearm safety into patient care conversations.”
- Kerryann Koper
the Jacobs School. “Say something like ‘I talk to all my patients about home safety.’”
The students work closely with Buffalo Rising Against Gun Violence (BRAVE) and Should Never Use Guns (SNUG), which also presented at the conference and which Koper said provide critical longitudinal follow-up care after a patient leaves the hospital.
They noted that fewer than 20 percent of medical schools include firearm safety in their curriculum, but Koper said that it’s relevant to every specialty, whether that’s geriatrics and a provider is concerned about a gun owner experiencing cognitive decline, or it’s pediatrics or OB-GYN. “Sixty percent of all homicides involve intimate partner violence,” she said, adding that homicide is the leading cause of death in the U.S. for pregnant women.
lack of training on how to do so.
That’s important, she said, because the majority of school shooters got the guns they used from their home or someone else’s home. She cited a recent study that found that a third of youths questioned said they knew how they could get their hands on a loaded gun in just five minutes.
Social determinants of health are always a factor, she continued. “Good research shows that anti-poverty programs are effective anti-violence programs,” she said, explaining that violence goes down when requirements for programs like the Supplemental Nutrition Assistance Program (SNAP) are loosened.
It was a point also made by HenryLouis Taylor, PhD, professor of urban and regional planning in the School of
Architecture and Planning and associate director of UB’s Community Health Equity Research Institute. He talked about how conditions in underserved communities contribute to gun violence. “We believe there’s an association between these conditions and Black on Black violence,” he said, “the relationship of neighborhood social determinants of health and adverse health outcomes.”
The importance of neighborhoods, especially those that are underserved, is a key factor, agreed Zeneta Everhart, Buffalo Common Council member representing the Masten District, and mother of Zaire Goodman, one of three people who

pervasiveness of violence in general. Participants learned of the physical, social and personal devastation that guns inflict. But by the conclusion of the conference, attendees said they also felt positive and hopeful about continuing to work together to prevent gun violence. They liked that the conference was small enough to be intimate and the fact that attendees came from diverse communities. They said that a remembrance service, led by Pastor Kinzer Pointer and featuring the extraordinary singing of Sasha Joseph, MD, a 2025 Jacobs School graduate, was particularly special. Participants also came away feeling empowered to share what they learned.
“The ripple effects of this disease extend far and wide. It harms our bodies, it harms our psyches, it harms our communities.”
- Megan Ranney, MD, MPH
survived the mass shooting at a Buffalo grocery store on May 14, 2022. “We’ve got to care about the poor people before we solve gun violence,” she said, adding that after a shooting, nobody comes to the neighborhood to help people heal. But that’s precisely when resources and programming are needed most, she said.
Everhart’s observations are borne out by studies showing that after a shooting, kids fare worse in school, even if they didn’t know the person who was shot. “The ripple effects of this disease extend far and wide,” said Ranney. “It harms our bodies, it harms our psyches, it harms our communities.”
The speakers dealt honestly and bluntly with the horror of gun violence and the
“Some people assume, ‘Well, I’m not going into surgery or emergency medicine so why care about this?’” Koper concluded. “But as students, we want to say ‘Open your eyes. It’s everywhere.’”
Sponsors of the 2025 conference included UB’s School of Social Work, Cindy and Francis M. Letro, the AAMC, M&T Bank, Erie County Medical Center, the University of New Mexico School of Medicine, The Ohio State University College of Medicine, Catholic Health, the Community Health Center of Buffalo, Kaleida Health and California Northstate University College of Medicine.

WATCH:
See a video recap of the 2025 Remembrance Conference here.
Mark Your Calendars:
The event will be returning to Buffalo in the fall of 2026.
Visit medicine.buffalo.edu/ remembrance-conference for more details.

Advances in patient care. Breakthrough treatments. Training tomorrow’s doctors. America’s teaching hospitals, academic health systems and medical schools form the foundation on which our health care system is built.
Institutions of academic medicine improve the health of our communities and serve as a vital economic engine, generating 7.1 million jobs and adding $798 billion to the nation’s economy.
The Jacobs School is proud to be among America’s academic medicine hubs. Across the nation—with 99,000 students in medical education programs, 162,000 resident physicians, and thousands of other critical health professionals—medical schools, academic health systems, and teaching hospitals are ensuring the health care workforce is prepared to prioritize patientcentered care. Today, and tomorrow.

The practice of modern medicine remains vastly complex.
Yet its fundamental goal hasn’t changed: improving human health.
Achieving that goal means continuously learning more about health, disease and the body’s myriad mysteries. Research is the process that unlocks these mysteries.
As a core component of academic medicine, scientific inquiry touches everything at the Jacobs School of Medicine and Biomedical Sciences. While all research centers strive for excellence, at the Jacobs School, excellence is defined not just by discovery, but by impact.
In Western New York, Jacobs School researchers are already changing lives. Their work and findings today fuel the promises of tomorrow—the discoveries that continue to ripple outward from the lab to the bedside and to communities across Buffalo and beyond.
Deep community engagement, investment in cutting-edge technologies, cultivating the next generation, and collaboration over competition all propel the research enterprise at the Jacobs School. While these efforts have provided great insight, the Jacobs School’s capacity for discovery continues only to grow.
At the Jacobs School, cutting-edge tools and smartly designed spaces provide the means to carry out research processes and transform ideas into discoveries.
Yet the tools and environments that enable scientific inquiry are always changing and evolving. It is through continued investment in this infrastructure that the Jacobs School
Halterman, MD, PhD, senior associate dean and executive director of the Office of Research. “The truest measure of impact is translating discoveries from the bench to the bedside and from the bedside to the community. That’s why we design research spaces with intent, co-locating cores, imaging platforms, biorepositories, and patient exam rooms to bring science and care together.”
Further, research environments themselves must foster collaboration; the Clinical and Translational Research Center (CTRC) is a prime example.
maintains a leading edge and will keep pushing frontiers of knowledge.
Using molecular, cellular, structural and computational biology approaches, scientists at the school are gaining new insights into the body and the function and dysfunction of its systems, cells and molecules every day.
Basic science at the Jacobs School spans genomics and bioinformatics, genome integrity and gene expression, microbial pathogenesis, and the molecular basis of disease, to name but a handful of research areas in focus.
Researchers have access to a full range of state-of-the-art facilities and equipment that power discovery. The university’s core facilities and those at affiliated institutions provide advanced capabilities in imaging, microscopy, tissue preservation, stem cell research and computational analysis.
“From deciphering protein structure and function to developing new drugs to finding the best ways to deliver treatments that improve human health, our research spans the full spectrum,” says Marc
Occupying floors five through eight above the Gates Vascular Institute, just blocks from the Jacobs School’s downtown facility, the CTRC puts clinical and translational researchers in shared space. Patient examination rooms, research labs and animal facilities that include a transgenic mouse facility, are all housed under the same roof.
Floors one through four of the hybrid facility focus on providing comprehensive vascular care while underscoring the synergy between clinical care and discovery.
“The whole point is that form enables function,” Halterman says of the CTRC’s collaborative design. “The CTRC was designed so clinicians and scientists share not just a building, but a workflow. When proximity increases, translation accelerates.”
The CTRC was recently upgraded with a new, powerful Philips magnetic resonance imaging (MRI) scanner used for research. The state-of-the-art tool enables groundbreaking discoveries
for neurological disorders and neurodegenerative diseases, among other translational imaging capabilities.
The center also houses an advanced Bruker MRI system designed for precision imaging and spectroscopy, offering exceptional detail and fine isotropic resolution.
To suit the research needs of advanced biomedical specialties, entire research facilities can require even greater specificity in terms of their purpose and capabilities. One such facility is the University at Buffalo HauptmanWoodward Research Institute (UB-HWI), which officially joined UB in January 2025.
Specializing in structural biology research, the institute had been a staple of the Buffalo Niagara Medical Campus for decades before becoming part of UB. UB-HWI’s federally funded National Crystallization Center gives investigators from across the university—and across the country—direct access to protein crystallization capabilities.
Growing crystals of proteins and other molecules is fundamental to X-ray crystallography, which enables the visualization of molecular 3D structures essential to drug design and development of molecular therapies, such as insulin analogs critical to treating diabetes.
For all the brick-and-mortar spaces propelling research, much of the next frontier will be discovered with the help of digital tools and artificial intelligence (AI).
To that end, Empire AI, a more than $500 million statewide consortium announced last year, is bringing a supercomputing center to UB to catapult AI and data science capabilities across New York State.
“The CTRC was designed so clinicians and scientists share not just a building, but a workflow. When proximity increases, translation accelerates.”
- Marc Halterman, MD, PhD
With the launch of Empire AI’s initial phase already complete, Jacobs School researchers have begun harnessing new AI abilities to better diagnose and monitor disease, predict protein structures and
develop drugs, among other innovations.
Researchers have also developed Semantic Clinical Artificial Intelligence, or SCAI (pronounced “sky”), as a powerful clinical AI tool trained on nearly all available medical literature, existing clinical guidelines, all FDA-approved drug information and toxicogenomic data. With much of its infrastructure and servers housed at UB, SCAI aims to be a key clinical, research and educational partner and consultant, says Peter L. Elkin, MD, professor and chair of biomedical informatics.
“Our paradigm is to ask a consultant when we don’t know,” Elkin says. “And SCAI is a consultant that has the ability to answer health questions on a broad range of topics.”
At the Jacobs School, education emphasizes research at all levels. Students learn not only how to conduct research but why it’s critical to both academic medicine and society at large.
In the process, they gain the perspectives needed to collaborate across disciplines and become researchers—and tomorrow’s scientific leaders—themselves. Undergraduates at the Jacobs School can
choose from a range of scientific majors, like biochemistry and biomedical sciences, that prepare them for further study and research careers. Research faculty teach many undergraduate courses, granting early opportunities for mentorship.
The school’s master’s programs include many research-intensive specialties across biomedical disciplines. New programs are being explored for research administration and health services research degrees suited to health implementation research and managing researchers.
Doctoral students and postdoctoral scholars continue to play an outsized role in the school’s basic research capabilities and breadth. Further, scholars in the MD-PhD program are training to serve as both physicians and scientists, combining clinical care with research acumen to bridge two essential roles.
To support students, trainees and earlycareer researchers, federal funding plays no small role. The Jacobs School continues to obtain T32 and KL2 grants from the NIH, which provide pivotal funds for structured, mentored training programs and key bridge funding to help trainees and junior faculty transition to become independently funded investigators.
In terms of trainee research, the Jacobs School’s proximity to UB-affiliated hospitals and institutions throughout the Buffalo Niagara Medical Campus gives
residents and fellows direct access to patient populations and clinical research facilities and hospitals.
These connections greatly enhance clinical research capabilities and allow trainees to take part in studies addressing some of the most pressing health issues in the region and across the U.S. population— cancer, cardiovascular disease, health care access, pediatric asthma, and neurodegenerative diseases, to name some.
Yet the process of cultivating researchers begins well before residency or postdoctoral training. The Jacobs School is committed to preparing the next
“Exposure to science and medicine early is important because this is when students are exploring what is possible.”
- Jennifer A. Surtees, PhD
generation of scientists, and that means reaching the students and curious minds still years away from entering college.
“Biomedical education is on a continuum,” says John C. Panepinto, PhD, senior associate dean for biomedical education. “So how do we get students thinking about STEM as early as we can?”

As part of its mission to prepare the next generation of scientists and leaders, the Jacobs School regularly welcomes K-12 students from across Western New York to its downtown facility.
The Jacobs School’s diverse research training portfolio cultivates future scientific leaders who connect across disciplines.
A wide array of research opportunities is available to trainees in master’s degree and PhD programs, as well as undergraduate and medical students. Training the next generation of scientists and clinician-scientists lies at the core of a multitude of Jacobs School programs.
Remi M. Adelaiye-Ogala, PhD ’17, assistant professor of medicine in the

Division of Hematology/Oncology, conducts research focused on why some cancers, especially prostate cancers, stop responding to treatment and how to develop better therapies that last longer.
After earning her doctoral degree in cancer pathology from UB/Roswell Park Comprehensive Cancer Center, she spent three years in a postdoctoral fellowship at the National Cancer Institute’s Center for Cancer Research before joining UB as a faculty member.
She says the university’s collaborative research environment, supportive mentoring, and access to cutting-edge research facilities combined to provide a robust foundation for her pursuit of a doctoral degree at UB.
Adelaiye-Ogala says one of the most meaningful parts of her PhD journey was being part of a vibrant culture of interdisciplinary collaboration.
“I loved the opportunity to work across departments and institutions beyond UB,” she says. “This experience truly broadened my horizons and helped me develop a more innovative approach to solving scientific challenges.
“The mentorship I received was incredibly warm and supportive, guiding me through my research and preparing me for academic and professional opportunities,” adds Adelaiye-Ogala, who also has appointments in the departments of Urology, and Pharmacology and Toxicology.
“Being part of such a collaborative and nurturing environment showed me that UB is a place where both scientific achievement and personal growth are valued.”
Adelaiye-Ogala is currently principal investigator on two R01 National Cancer Institute/National Institutes of Health grants, one of which is a MERIT R37 Award, providing her with two years of additional research support because her grant application was ranked so highly.
Her lab utilizes advanced tools to analyze cancer cells in detail, test new drugs in mini tumors (called organoids) generated from patients’ tumors, and in lab mice implanted with human cancer cells.
Introduced as part of the new Well Beyond curriculum for Jacobs School medical students, the Health Sciences Scholarly Project (HSSP) is a comprehensive fouryear capstone program designed to apply scientific literacy and inquiry to practice with the guidance of a research mentor.
The program aims to elevate students’ critical thinking and scientific reasoning to confidently engage with evidence-based medicine, according to program director Kyle Kelleran, PhD, assistant professor of emergency medicine.
“As medicine evolves, so do our future physicians,” he says. “The next generation of physicians are being trained to think beyond the clinic and how to shape the future of medicine.
“The HSSP helps students explore their research and specialty interests but also prepares them to be lifelong learners who strive to improve our health systems, communities and patient care,” Kelleran
adds.
Second-year medical student Lindsey Cunningham says when she began seeking research projects she could engage in, she knew she wanted to contribute to something longitudinal, work that could create tangible, positive change in people’s lives.
“I’ve always been drawn to the intersection of women’s health and public health,” she says.
Under the guidance of her faculty mentor, Amanda M. Ziegler, PhD, research assistant professor of family medicine, Cunningham is evaluating a program for pregnant women affected by substance use disorders in Erie County.
The research is centered on Positive Direction & Associates, Inc., a free community-based resource that uses a patient navigator model to provide substance use counseling, holistic support, education and empowerment to its participants.
The approach to evaluating the program is two-pronged: conducting both a direct evaluation of outcomes of the program and a workforce sector survey to examine the strategies used in Erie County to support pregnant women in accessing substance use disorder treatment.
Once enough responses were received for preliminary data analysis, Ziegler walked Cunningham through the necessary steps.
“This, too, was an amazing opportunity, allowing me to learn how raw survey data can be transformed into meaningful insights that apply to the medical field,” Cunningham says.

Students from K-12 schools throughout Western New York regularly visit the Jacobs School’s flagship downtown building for field trips and inquiry-based workshops aimed at exposing young students to research settings. Many get to visit research labs for a glimpse into the mechanisms behind human health and disease.
Other community outreach highlights have included visiting local schools for microbiome education workshops, hands-on science project demonstrations, and help with running after-school science clubs.
The Jacobs School’s own STEM Outreach trainee ambassador team has carried out much of this work—exposing K-12 students to research, providing mentorship and directly benefitting the community beyond UB.
“Exposure to science and medicine early is important because this is when students are exploring what is possible. And they generally don’t realize the different opportunities and career paths available,” says Jennifer A. Surtees, PhD, chair of the Department of Biochemistry, who has long overseen STEM outreach at the school. “Showing them people who are actually doing this work—and people who look like them—opens their eyes to the possibilities.”

Recently, Surtees and colleagues established a community lab space within the Buffalo Niagara Medical Campus known as CELLS (Community Education Laboratory in Life Sciences) to host authentic research experiences for local high school students and others.
“The more often we give students opportunities to be in the research lab, the more they’re going to be able to decide whether or not it’s the right thing for them,” Panepinto adds. “The ones we want to get are the ones who would love it—if they just had the opportunity.”
It can be difficult to quantify success when so many of the fruits of research, like lives made better by new discoveries, are intangible.
Yet the Jacobs School shines across many of the metrics that indicate research achievement and trajectory.
In 2025, the Jacobs School spent $80.3 million on research expenditures—funds spent to conduct research—the most of any school at UB.
In recent years, some of the faculty-authored papers with the highest impact factor have shed light on cancer-fighting vaccine boosters and improved tumor detection, described more effective malaria vaccines, and reported on AI-powered blood vessel imaging.
While funding and a strong publication record are traditional metrics of research success, it’s the people who are most integral to advancing the school’s research mission. The Jacobs
The first cancer patient Nick Salgia saw while working at an oncology research center had a rare and hyper-aggressive subtype of kidney cancer. Fortunately, a novel immunotherapy had just been approved, and the patient was among the first to get it.

That experience sparked in Salgia a passion to study kidney cancer, an interest that has only strengthened since he entered the MD-PhD program in the Jacobs School of Medicine and Biomedical Sciences in 2020.
Salgia works in the lab of Jason Muhitch, PhD, associate professor and co-chair of the Genitourinary Translational Research Group in the Department of Immunology at Roswell Park Comprehensive Cancer Center, a partner of the Jacobs School.
In August, Cancer Cell, one of the most respected journals in the field, published a study that helps explain why the subtype of kidney cancer that afflicted Salgia’s first patient is so susceptible to immunotherapy. Salgia is first author and Muhitch, Salgia’s faculty adviser, and Eric Kauffman, MD, associate professor of oncology in the departments of Urology and Cancer Genetics & Genomics at Roswell Park, are senior authors.
Thanks to this immunotherapy, the patient Salgia knew is now fully recovered and doing well.
The fact that Salgia was able to not only participate in such impactful research, but also had the opportunity to be first author is noteworthy, says Marc Halterman, MD, PhD, senior associate dean and executive director of the Office of Research in the Jacobs School.
“Nick’s Cancer Cell publication is a remarkable achievement and reflects the caliber of research our students engage in during their PhD training,” he says.
Salgia explains why he was drawn to UB’s MD-PhD program.
“The most important thing about an MD-PhD program is that you really develop expertise on both sides,” he says. “You talk to both basic researchers and clinicians and you feel like you really belong in both conversations. It allows you to be a bridge between the scientist and the patients, between basic discoveries and ways that you can really improve the lives of patients.”
He adds: “One of the strengths of training at UB and at UBaffiliated institutions is the kindness and relatability of mentors here,” Salgia adds. “The mentors put the trainees’ interests first. I think that’s very unique to this institution.”
-Ellen Goldbaum
The Jacobs School’s use of artificial intelligence (AI) is transforming the medical research landscape by accelerating discovery, improving accuracy and enabling personalized medicine.
AI rapidly analyzes massive datasets— such as genomic data, clinical trial results, and electronic health records—to identify patterns and insights. Machine learning algorithms improve diagnostic accuracy in areas such as imaging and pathology.
AI models can also predict how compounds interact with biological targets, significantly speeding up drug discovery and reducing costs.
Ram Samudrala, PhD, professor of biomedical informatics and chief of the Division of Bioinformatics, has created the Computational Analysis of Novel Drug Opportunities (CANDO) platform to make drug discovery faster and less expensive while also being safe and effective.
could easily spot,” Samudrala says.
Thomas D. Grant, PhD ’13, assistant professor of structural biology, is also interested in developing drugs faster, but with a focus on precision medicine to enable the drugs to be designed for individual patients based on their own DNA.

Grant
Grant’s latest National Institutes of Health funding is aimed at revolutionizing the way proteins are studied in their natural environment.
School continues to recruit faculty and investigators with research projects and goals specifically suited to the region’s academic environment and community. By centering recruitment around the school’s research pillars—like humanrelevant models, advanced imaging, and AI—new faculty can plug directly into infrastructure that lets their ideas scale quickly.
Some of the ideas and inventions that flow out of the Jacobs School will even be commercialized. By partnering with industry sponsors aimed at solving problems in the health care space, discoveries can lead to solutions for pressing issues.
Securing intellectual property for any new method, device, process or material starts with disclosing it. The Jacobs School annually accounts for about a quarter of all new technology disclosures made across the university, says Timothy Dee, senior associate director in UB’s Technology Transfer office.
While disclosing new technology is but a first step toward protection, licensing and commercialization, that level of volume speaks to the range of potentially transformative ideas and discoveries originating from the Jacobs School.
CANDO has already led to the creation of innovative biotech startups like AmritX, Meditati and Mansarover Therapeutics, companies that are using the platform to develop treatments for non-small cell lung cancer, opioid use disorder and aging, respectively.
Traditional drug discovery often takes more than a decade to produce results.
Samudrala wanted a smarter and faster way, so he created a platform that looks at how compounds affect the whole body, not just one protein.
“CANDO simulates how thousands of compounds interact with the human body at once—like running millions of experiments in seconds,” Samudrala says.
AI is at the heart of CANDO—using machine learning to analyze huge datasets of drug-protein interactions, predict new uses for existing drugs and design new ones with optimal properties.
“Think of AI in CANDO as the engine that sifts through the noise to find hidden patterns and connections that no human
To accomplish this, Grant is employing a technique called SWAXS (small- and wideangle X-ray scattering) in combination with computational AI tools.
Grant uses SWAXSFold, an AI model he developed using the computing capacity of Empire AI, the $500 million New York State-based research consortium advancing artificial intelligence for the public good.
Empire AI’s computing center, located at the University at Buffalo, is a major resource for the researchers.
“Empire AI is a big part of this, as we wouldn’t be able to do this level of computation without it,” Grant says.
Grant and his colleagues are also developing tools that will help researchers understand how disease-causing mutations change protein structure.
“If we can see exactly how a mutation alters a protein’s shape and function, we can design personalized therapies targeted to that specific change,” he says.
-Dirk Hoffman
Inventions by faculty have led to new imaging tools and medical diagnostics, among many other technologies that are on the path to or have achieved commercialization. “We do have some world-class researchers here. And we have some who are under the radar waiting to break through,” says Michael Fowler,
“We do have some world-
class researchers here.
And we have some who are under the radar waiting to break through.”
- Michael Fowler, PhD
PhD, commercialization manager in the Technology Transfer office.
One research tool developed recently at UB uses a fluorescent molecule to measure cell membrane tension, which can be useful for studying cancers with more fluid membranes. Another technology uses low-voltage electrical treatments to eliminate microbial biofilm development and reduce prosthetic implant infections.
“With each engagement that faculty members have with industry, they get that much better at being able to converse with and understand industry’s needs and being able to better present the value proposition of their work,” says Dee.
While the path from invention to marketplace is rarely linear, Jacobs School researchers have shown that ideas can develop into practical solutions and new products that underscore the linkage between scientific creativity and industry partnership.
through translation, that is, moving research findings out of the lab and transforming them into new treatments and approaches to medicine.

As new knowledge continues to underpin health care technologies, the Jacobs School will remain a driver of medical innovations.
Conducting biomedical research requires immense specificity of knowledge and expertise, so much so that it can be easy to lose sight of its broader intent: improving human health across individuals, communities and populations.
These improvements happen only
At the Jacobs School, translational research is both deliberate and ambitious. Laboratory discoveries are nurtured with the goal of moving them into patient care. Throughout this process, community health remains top of mind.
“We are very cognizant of the fact that discoveries have to move from basic science to the community,” says Teresa Quattrin, MD, associate dean for research integration. “And we are really connecting with the community in better ways. In order to do translational science, you have to listen to what the community needs are.”
Among many prominent examples, Quattrin points to childhood asthma prevalence and a multidisciplinary Jacobs School and UB research team that has worked with Buffalo Public Schools children to enhance comprehensive asthma care.
The commitment to community health on the part of the Jacobs School and university has been recognized repeatedly through federal funding. Earlier this year, the NIH awarded UB’s Clinical and Translational Science Institute (CTSI)

a seven-year, $28.4 million Clinical and Translational Science Award.
This pivotal grant, UB’s third such award, allows the CTSI to continue its mission of improving health for all populations throughout Western New York while speeding the translation of research discoveries into clinical practices.
Additionally, the school’s partnering with so many of the region’s communityfocused organizations and events has enhanced shared missions behind community engagement and well-being. Quattrin notes that this visibility builds trust and keeps researchers attuned to the community while supporting involvement in research and enhancing representation of people too often underrepresented in clinical trials.
Likewise, the Jacobs School has strived to increase both the amount of and access to primary care providers in the region, which will improve community health while boosting research involvement. Last year, UBMD Physicians’ Group, whose doctors are also faculty educators at the Jacobs School, launched UBMD Primary Care as a new clinical practice to expand care for Western New Yorkers across age ranges.
“The delivery of clinical care and clinical research are intimately connected,” Quattrin says.
Like so many areas of medicine, recruitment for clinical trials could be on the cusp of new AI-driven enhancements. New models could help sift through a broad base of patient materials and health records to identify potential trial participants based on a study’s inclusion and exclusion criteria, says biomedical informatics chair Peter L. Elkin, MD.
“For research, we want to speed up the translation of research and set the pipelines up to recruit faster for clinical trials and to do it in a more automated way that would be national in scope using realworld evidence,” Elkin says.
Doing so would fundamentally involve no shortage of patient data. To better harness all of this data and information, shared systems need to speak the same language. Therefore, the Jacobs School, along with UBMD, Kaleida Health, and the Erie County Medical Center, have begun a patient-centered implementation of Epic software to create a unified electronic health record system.
Connecting health records, systems and data will allow for seamless flow of
Clinical trials are considered the cornerstone of health care research because they provide the most reliable and scientifically rigorous method for evaluating new medical interventions— they are the culmination of the discovery pipeline and the bridge between scientific discovery and everyday medical practice.
There are usually about 300 clinical trials at any time that are actively enrolling patients at UB. Of these, more than 90% are in the Jacobs School of Medicine and Biomedical Sciences.
All the work that goes into drug development would amount to nothing in the absence of clinical trials, according to Sanjay Sethi, MD, assistant vice president for health sciences and medical director of UB’s Clinical Research Office.
With rare exceptions, approval of a new medication requires at least two clinical trials where the medication is compared to placebo. These trials must be double blind (neither the participant nor the investigator knows whether the patient is receiving the medication or placebo) and randomized (the allocation to placebo or drug is by chance).
“The new drug has to be better than placebo in both trials to obtain FDA approval—its success has to be reproducible,” says Sethi, professor of medicine and chief of the Division of Pulmonary, Critical Care and Sleep Medicine in the Jacobs School.
Clinical trials are also essential to prove that drugs and treatment protocols are safe. They follow strict ethical and regulatory guidelines, ensuring that new treatments are thoroughly tested for safety and efficacy before they reach the public.
“Though all medications can have adverse effects, the trials help us decide that the benefit of the medications outweighs the risks,” Sethi says.
A recent clinical trial success story at the Jacobs School is the novel approach developed by Andrew H. Talal, MD, MPH, and colleagues to cure hepatitis C virus in people with opioid use disorder using facilitated telemedicine.
The researchers explored the effectiveness of integrating telemedicine into opioid treatment programs (OTP) for hepatitis C management, thereby
removing the need for off-site referrals.
In a five-year study of OTPs in New York State, the researchers enrolled 602 participants and found that 90.3 percent of those in the telemedicine arm at an OTP were cured of HCV infection compared to 39.4 percent of participants referred to an off-site specialist.
The groundbreaking results were published in the Journal of the American Medical Association and Talal was subsequently honored with a 2025 Top Ten Clinical Research Achievement Award from the Clinical Research Forum, a research institute based in Washington, D.C.
“Successful hepatitis C cure is an extremely important milestone in the treatment of opioid use disorder,” says Talal, professor of medicine in the Jacobs School.
The work was supported by an $8.2 million award from the Patient-Centered Outcomes Research Institute and more than $3 million from the Troup Fund of the Kaleida Health Foundation.
Talal and Kenneth V. Snyder, MD ’04, PhD ’02, associate professor of neurosurgery, radiology and neurology, jointly direct Gilead’s “On the Frontlines of Communities in the United States” (FOCUS) program at Kaleida Health.
FOCUS supports screening in the four Kaleida Health emergency departments for HCV and HIV and linkage to care.
The process improvements developed from the FOCUS project have established patient navigation services, community outreach initiatives, and improved collaboration with local health care providers, Talal says.
“We have engaged the entire community in an effort to improve linkage-to-care,” he says. “The results of these endeavors have led to improved rates of HCV eliminations among patients and improved detection within the health system ultimately leading to a healthier community.”
Leonard H. Epstein, PhD, SUNY Distinguished Professor of pediatrics and chief of the Division of Behavioral Medicine, is currently recruiting for a novel clinical trial that aims to overcome the food insecurity-obesity paradox.
Research has shown that women
who cannot regularly access food they need are at a 50 percent greater risk of becoming obese, even though they do not consume more calories.
Epstein’s clinical trial will provide individually personalized meals to participants to improve their health by changing how they metabolize food.
Enrollment remains the biggest challenge in the execution of clinical trials, Sethi says.
“Multiple criteria have to be met to enter a clinical trial, as they are designed with an abundance of caution to minimize risk to participants,” he says.
The UB Participate in Research portal allows interested participants to search for actively enrolling clinical trials at UB.
The Institute for Healthcare Informatics at UB also has the clinical data of all UBMD and Kaleida Health patients, and that can be queried by investigators to find potential participants.
Sethi says the implementation of the Epic electronic health record system will also provide “a tremendous boost to clinical trial enrollment.”
“It has tools that allow matching of clinical trial enrollment criteria with patients’ clinical data, allowing the patients and their providers to be informed of their eligibility to participate in a trial,” he says. “Epic will also provide greater visibility to all active clinical trials to patients and providers, improving access to the trials.”
-Dirk Hoffman

clinical data across research platforms. Researchers can more readily access longitudinal data, from labs to imaging to medications, across broader patient populations as opposed to working with subsets.
In terms of research advancement, the Epic implementation could help clinical observations inform translational and basic research studies. For example, data on patient observations and outcomes could be more readily paired with studies investigating a certain biomarker.
All in all, the move to a smarter, integrated health records system will be a game changer for health care and research in the region, enhancing patient connectivity and care while streamlining the data needed to drive translational research.
“By pairing the unified electronic health record, the biorepository, imaging data, and emerging tools in AI, Western New York becomes a true learning health ecosystem where every clinic visit or hospital stay generates knowledge that drives the next breakthrough,” notes Halterman, of the Office of Research.
Across the country, medical schools seek to conduct leading research. In doing so, they can also tremendously benefit the health of their surrounding communities while fostering collaboration; the Jacobs School and Western New York provide a prime example.
To be most effective, research must engage the community early on and throughout the process, deliver tangible benefits, and be based on community needs rather than researcher presumptions, says Timothy F. Murphy, MD, who was senior associate dean for clinical and translational research before stepping down in October after 44 years of service to the university.
“We have a responsibility as an academic health center and as health care professionals to partner with our community,” says Murphy, who also directed UB’s CTSI since its launch in 2015. “We see our community as an asset. Our community can help us and teach us how to make our research more impactful.”
Research conducted at the Jacobs School has translated into improved survival rates for people with cardiovascular,
neurological and neurovascular conditions, a robust response to the opioid crisis, and bold efforts to confront health disparities and promote health equity across local communities.
Further, the Jacobs School has partnered with community health workers to address hypertension and mental health concerns in pregnant people as part of a more
“We have a responsibility as an academic health center and as health care professionals to partner with our community. We see our community as an asset. Our community can help us and teach us how to make our research more impactful.”
- Timothy F. Murphy, MD
unified effort to reduce maternal deaths.
Jacobs School researchers and faculty have also worked to tailor treatment strategies for HIV and other infectious diseases while continuing to develop and study new treatments and drugs. Their work has benefitted patients infected with HIV variants resistant to traditional treatments and those with co-infections, such as hepatitis C.
For the litany of diseases and conditions that Jacobs School researchers and clinicians study, they also seek to address the underlying conditions affecting individual and community health. In many cases, that means confronting health disparities.
Across disciplines, health disparities remain a persistent challenge within and beyond Western New York communities and affect so many facets of health care and research.
Stroke risk, for example, is disproportionately high among Black and Hispanic Americans. They’re twice as likely to suffer from intracerebral hemorrhage and are affected on average 10 years earlier than other populations.
Researchers at the Jacobs School such as Daniel Woo, MD, professor and Irvin and Rosemary Smith Endowed Chair of neurology, are exploring variations
in stroke risk factors based on race, ethnicity and sex while investigating the genetic epidemiology of stroke. He and his colleagues may have identified a novel risk factor for vascular dementia, the second leading cause of dementia, and are pursuing novel targets for improving outcomes after intracerebral hemorrhage.
Other research studies have led to the creation of smoking cessation programs targeting pregnant people in the community and new ways of increasing local parents’ and children’s interactions with and understanding of clinical research participation.
During the COVID-19 pandemic, Jacobs School research teams leveraged their knowledge of infectious diseases to help keep the Western New York community safe and informed.
By conducting genomic sequencing of COVID-19 samples, researchers tracked the emergence and spread of virus variants within the region, providing essential surveillance while deepening understanding of the virus’ behavior.
Yet for all the developments, new findings and myriad ways that Jacobs School research has enhanced the health of Western New York, there is more to come. As they uncover findings that improve health, researchers remain never satisfied with those results, always curious, and looking to learn more.
One ongoing project follows the success of a substantial undertaking to teach CPR to thousands in the Western New York community. Researchers are now studying how to cultivate youth leadership to promote bystander CPR education in schools and community settings.
Another research team is exploring how embedding community health workers in pediatric clinics could help address root causes of health inequities.
And so much more.
Taken together, these efforts signal that the research enterprise at the Jacobs School isn’t about merely finding answers but creating lasting change. As the school’s research efforts thrive, innovation and community will continue to create a partnership leading to better health and a brighter future for all.
-Keith
Gillogly

Mopioid use disorder (OUD).

Lynch created the MATTERS network to provide medicationassisted treatment to OUD patients in emergency departments and rapidly transition them into long-term treatment at a community clinic. The program provides stigma-free treatment and education.
5,000 referrals and conducted more than 130 community trainings. It partners with over 100 hospitals throughout New York State, and with over 200 treatment organizations.
MATTERS has also installed more than 25 “no stigma” vending machines throughout New York State. They provide free naloxone and free test strips for fentanyl and xylazine.
“People with opioid use disorder can be reluctant to walk into a pharmacy to obtain test strips or naloxone,” Lynch says. “So, we wanted the vending machines to be in different types of places, outside and always accessible.”
CYSTIC FIBROSIS INNOVATIONS CONTRIBUTE TO LONGER LIFESPANS
UB has a rich history in being an innovative leader in cystic fibrosis research.
edical research is ultimately not just about curing disease—it’s about creating a healthier, longer and higher-quality life for everyone.
Since her arrival in 2021 as UB’s vice president for health sciences and dean of the Jacobs School of Medicine and Biomedical Sciences, Allison Brashear, MD, MBA, has repeatedly articulated UB’s goal of “transforming the health of the Western New York community.”
UB research takes on many forms, but the focus always remains on improved disease management, better access to care, community-based research partnerships and equity-driven health initiatives.
Jacobs School investigators are leading advances in many areas including opioid addiction treatment, cystic fibrosis (CF) and multiple sclerosis (MS).
The MATTERS program, a novel statewide electronic referral network, was born out of frustration. It was developed by Joshua J. Lynch, DO, professor of emergency medicine and addiction medicine, because he saw inadequacies in how the health care system treated patients with
The MATTERS network is based on the premise that patients must be linked to treatment promptly, and they must see that they have plenty of choices.
“We know that the window of opportunity when we can intervene with a patient may only be open for a very short time,” Lynch says.
MATTERS is one of a number of multidisciplinary UB initiatives involving faculty from the Clinical and Research Institute on Addictions, who investigate addiction, from exploring its basic scientific mechanisms to developing new approaches to patient care.
Research has shown that quick, barrierfree access to treatment is essential, and MATTERS has grown from a Buffalobased pilot into a national model for tackling the opioid epidemic.
Through its partnership with the New York State Department of Health and other agencies, MATTERS has expanded its network to include inpatient units, medical offices, correctional facilities, first responders and community-based organizations. It has also expanded to offer telemedicine evaluations and harm reduction services.
To date, MATTERS has distributed over 23 million test strips, distributed over 34,000 doses of naloxone (the antidote for an opioid overdose), made more than
Drucy S. Borowitz, MD, clinical professor emeritus of pediatrics, who directed the Cystic Fibrosis Center at the former Women & Children’s Hospital of Buffalo for more than 25 years, was instrumental in helping the development of the breakthrough drug ivacaftor—a CF transmembrane conductance regulator (CFTR) modulator. The first patient in a multisite clinical study was enrolled in Buffalo in 2009.
The research contributed greatly to longer lifespans. For people born with CF since 2020, the Cystic Fibrosis Foundation estimates the median age of survival is 65. The same statistic was 28 years of age in 1990.
Danielle M. Goetz, MD ’03, clinical associate professor of pediatrics, succeeded Borowitz, and is director of the Cystic Fibrosis Center of Western New York at Oishei Children’s Hospital.
Last year, Goetz was asked by the CF Foundation to write a position paper on redefining the CF Care Model that was pioneered in the 1960s and defined by clinical practice guidelines in 1997.
Evolution of the CF Care Model was necessary due to improved survival and outcomes, development of CFTR modulators, and technology advances allowing telemedicine and home monitoring, Goetz says.
“CF care is changing, but it is still important to have an interdisciplinary team and to have patient-centered care,”
Goetz says.
Citing the advent of CFTR modulators, the position paper recommended slightly more flexibility in the timing of clinic visits.
“If a person is stable, they can space out visits to every four to six months instead of every three months,” Goetz says. “Less frequent visits can make their lives a little less hectic.”
Even with a reduction of in-person visits, Goetz says health care providers must still maintain close follow-up and initiate interventions if necessary.
“We need to maintain access to treatments and medications because they have proven to be so beneficial,” she says.
Jack Reeves, a trainee in the MD-PhD Program, has received accolades for his clinical research work with MS patients and his focus on paramagnetic rim lesions (PRLs), chronic active lesions believed to represent smoldering inflammation in MS.
He received the Buffalo Neuroimaging Analysis Center’s highly competitive
“Each patient’s disease is as unique as the person themselves, so it’s important to take the whole person into account when deciding on a medical care plan.”
- Jack Reeves
2025 Marc Stecker Award for Excellence in Multiple Sclerosis Research, which recognizes a student whose research is deeply informed by the lived experiences of people with MS.
One of the award’s criteria is demonstrating a willingness to pursue ideas that are not necessarily part of the mainstream of MS research.
“My main contribution on this front is my work on ‘iron networks.’ Previous research in mice showed that iron is transported between brain areas. My initial results support that a similar phenomenon may be occurring in humans and disrupted
in people with MS,” Reeves says. “This work is novel not just for MS but for neuroscience in general, and I hope that it leads to a deeper understanding of the disease and new treatments for people with MS.”
The bulk of Reeves’ research has looked at the relationship between clinical MS disease progression and PRLs. Specifically, he investigated whether PRLs are related to clinical relapse and clinical disease progression, both of which profoundly impact patients’ quality of life.
He has authored or co-authored seven top-tier peer-reviewed publications on PRLs, contributing significantly to the understanding of chronic inflammation in MS. Reeves was first author on two 2024 papers that represented the first published longitudinal studies of PRLs.
“My research showed that PRLs predict higher rates of clinical relapse and increased clinical disability,” Reeves says. “These findings could help individual patient/clinician teams select appropriate disease-modifying therapies.”
The resolution of existing PRLs may preserve brain tissue (or slow its loss), helping to retain motor and cognitive function longer. And using PRLs as a biomarker to identify people likely to benefit more from certain therapies could allow more personalized treatment, such as starting more aggressive therapy earlier for those with PRLs, thus improving long-term outcomes.
Working with center director Bianca Weinstock-Guttman, MD, in the Jacobs Multiple Sclerosis Center for Treatment and Research at UBMD Neurology, Reeves says he has learned that there’s no onesize-fits-all approach to treating MS.
“Each patient’s disease is as unique as the person themselves, so it’s important to take the whole person into account when deciding on a medical care plan,” he says. By continuing to identify key challenges, exploring innovative solutions and applying new knowledge to real-world problems, UB’s research remains a driving force for positive change in Western New York and beyond.
- Dirk Hoffman


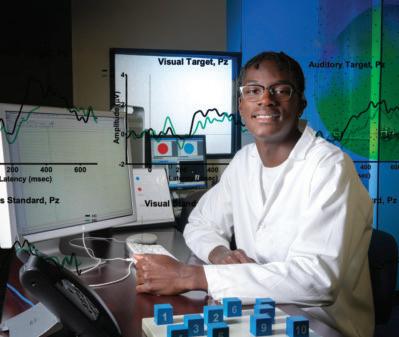
By Keith Gillogly
All the way back in the sixth grade, Trey Lewis participated in a college preparation program that ignited his interest in neuroscience. Always a curious person, Lewis knew he wanted to someday unravel the brain’s mysteries.
Now a junior at the Jacobs School of Medicine and Biomedical Sciences, Lewis is majoring in neuroscience and has tacked on three minors: pharmacology and toxicology, psychology, and biological sciences. Even with all that coursework, Lewis is thriving at the Jacobs School, engaging in research opportunities, and planning to pursue his PhD after undergrad.
“Something I always tell everyone is, I’ll never miss an opportunity,” Lewis says.
The Jacobs School has always prioritized biomedical education that emphasizes student achievement and exceptional education.
With a renewed focus on research experience and experiential learning,
enrollment across undergraduate, master’s and PhD programs has grown to new levels, positioning students for success across disciplines and career paths.
Neuroscience, a growing interdisciplinary program co-managed with UB’s College of Arts and Sciences, is now the secondlargest major at the Jacobs School, says Kelli Hickey, director of strategic undergraduate enrollment and operation.
The school’s largest undergraduate major, biomedical sciences, continues to draw students looking for an expansive and advancement-driven education; many go on to pursue graduate or professional
Trey Lewis, a junior majoring in neuroscience at the Jacobs School, is emblematic of the strong undergraduates who have helped propel the school’s enrollment growth over the past decade. Lewis is minoring in pharmacology and toxicology, psychology, and biological sciences and plans to pursue his PhD.
degrees in medicine or science, and the curriculum is currently being revamped to delve deeper into the basic sciences, Hickey says.
Regardless of program, research opportunities flourish among Jacobs School undergraduates; students are taught by and work with faculty researchers from the start. Providing early exposure to faculty and researchers encourages students to begin exploring labs and seeking mentors.
The Jacobs School’s undergraduate programming also caters to clinical education and experience, preparing students to begin working in clinical spaces following their four-year degrees with majors like medical laboratory science and nuclear medicine technology.
“There are very few medical schools in the nation that have an undergraduate component, so it makes us stand out,” Hickey says. “Students see a connection in these opportunities that maybe they wouldn’t get somewhere else.”
Further, the Jacobs School is intentional about keeping its undergraduates connected, Hickey says. In addition to exclusive events like symposiums and tours for undergraduate students, they are invited to many of the same seminars and presentations as MD and graduate students.
Following his freshman year, Lewis took part in UB’s CLIMB UP (Collaborative Learning and Integrated Mentoring in the Biosciences Undergraduate Program) interdisciplinary summer research program, conducting chemical engineering research.
After his sophomore year, Lewis performed neuroscience research as part of the CSTEP (College Science and Technology Entry Program) Summer Research Program at UB, which offers an intensive STEM research experience. Lewis has worked to identify neuromarkers of cognitive decline associated with multiple sclerosis.
He says he’s most proud of the neuroscience research presentations he’s given recently at UB and CSTEP conferences, holding on to his presenter badges as mementos.
As with undergraduate programs, Jacobs School graduate and doctoral programs have grown. In the past 10 years, enrollment in master’s programs is up by 79 percent, says Beth White, who served as director of graduate enrollment until August 2025. Such growth reflects the robust and diverse program options and speaks to a growing focus on research and workforce skills.
A master’s degree allows for significant research experience and can bolster academic standing before entering a PhD program or medical school. Conversely, some master’s programs, like the biotechnology program, offer internship and practicum opportunities to directly prepare graduates for jobs in clinical lab settings, White says.
She adds that the mentality surrounding master’s degrees has also evolved over time. Now, there’s focus on enriched research opportunities, augmenting credentials and workforce preparation.
“Master’s education used to be, you get a master’s on the way to a PhD. Full stop, that was it,” White says.
White notes that the Jacobs School is exploring obtaining more scholarships for master’s students and looking to grow online course offerings. Internship
opportunities for both master’s and PhD students are also on the rise.
Internships are traditionally less common for doctoral students, but some students have spent summers interning with biotech companies, gaining handson industry experience and, later, job offers, says John C. Panepinto, PhD, senior associate dean for biomedical education.
undergraduate
at the Jacobs School has increased by 39 percent in the past 10 years.
“Our students are hungering for other opportunities,” Panepinto says. “We’ve had students become educators and do research-intensive careers in academia. But we’ve also had students be very successful in the biotech sector, both locally and elsewhere.”
Jacobs School students now have more chances to network with and hear from successful alumni and others in nonacademic roles about various career paths, Panepinto says.
More tailored forms of digital outreach, coupled with new and existing open house and community outreach, have helped
inform potential applicants about the graduate programs’ strengths and options, White says.
In the past 10 years, doctoral student enrollment is up by 40 percent. The growth is a testament to the school’s and faculty’s commitment to biomedical education and research training.
More broadly, UB continues to prioritize doctoral student education, as evidenced by its PhD Excellence Initiative, White says. Beginning in 2019, the initiative has provided critical support to expand Jacobs School doctoral enrollment and enrich programming.
For all students, Panepinto notes that enrollment growth also reflects a renewed focus on the student experience.
Focused career development, building community, and helping students feel included and that they belong are key, he says.
As an undergraduate biomedical sciences major in the Jacobs School, Sofia Alexander was working as a hospital technician and planned to become a physician assistant when COVID hit.
The pandemic thrust her into the demands of health care, leading to burnout—but also clarity: She’d much rather be in the lab than the clinic.
Now in her second year of a Jacobs School microbiology and immunology master’s program, Alexander has realized a new passion for research. “Now that I’m doing my master’s, I know that research is what I want to do,” she says.
Alexander, who’s from Middletown, New York, is studying polymicrobial interactions among bacteria linked to catheter-associated urinary tract infections—a common and potentially deadly condition—in the lab of Chelsie E. Armbruster, PhD, associate professor of microbiology and immunology.
Following her master’s, Alexander plans to pursue a PhD in bacteriology and credits the mentorship and opportunities received during her master’s program with revitalizing her career path.
“Everyone in my lab is very passionate about what they do and very excited,” she says. “Even in such a specific field, every question we ask leads to more questions.”

Highlighting the many facets in which the University at Buffalo is improving the health care of the community was the theme of the 2025 Harrington Lecture as part of UB’s Alumni Weekend celebration this past May.
The two-day event also featured reunion dinners and celebrations and the presentation of the school’s Distinguished Alumni Awards. Awardees included Margaret Paroski, MD ’80, Menghang Xia, PhD ’93, and David Milling, MD ’93.
Allison Brashear, MD, MBA, UB’s vice president for health sciences and dean of the Jacobs School, gave the keynote address titled “Transforming Health Care in Western New York and Beyond.”
Brashear said the goal of UB, and all of its health sciences schools, is to improve and transform the health of Western New York and the rest of the country.
She said UB is going about this by:
• developing medical leaders by prioritizing strategic coordination
• shaping the future with cutting-edge researcher training
• fostering growth by contributing to startups, attracting recruits, and retaining trainees in WNY
“One of the reasons we want Western New York to be healthy is because we want businesses to come to Western New York and thrive,” Brashear said. “We want to create a partnership with them and make sure we have a robust economy for many years to come.”
One of the ways UB is committed to transforming the health of WNY is through all of its schools of health, Brashear said.
“We have 12 decanal units and six of them represent the schools of health,” she said. “Fifty percent of our schools are focused on improving health.”
Beyond the Jacobs School, UB has the School of Nursing, School of Public Health and Health Professions, School of Dental Medicine, School of Pharmacy and Pharmaceutical Sciences, and the School of Social Work.
“All of these professions are really needed in WNY, so we train in the areas, not just of medicine, but in all of the health professions,” Brashear said.
“We also have the fourth largest undergraduate program at UB; we have a robust graduate program, including master’s and doctoral degrees; we have a number of programs in our MD footprint; and then of course we have our residencies and fellowships,” she said.
“The word continuum is one I would like people to remember. UB trains people across the continuum. We start early and we want everyone to practice here and stay in Buffalo.”
Brashear noted the Jacobs School is the “keystone of health sciences downtown,” and said the new Well Beyond medical curriculum launched last July “teaches
medical students to be leaders and lifelong learners. They work with communitybased organizations and are required to complete a research project before graduation.”
Brashear also highlighted the Jacobs School’s “deep partnership” with Kaleida Health, Erie County Medical Center (ECMC), Catholic Health, Roswell Park Comprehensive Cancer Care and the VA Western New York Healthcare System.
“We rely on our hospital partners. We have such a strong physician footprint, that is the secret sauce,” she said. “We could not do anything without our hospital partners.
“The Jacobs School also has a very robust clinical group. UBMD is the clinical arm of our medical school,” Brashear said. “Our chairs are very involved in developing robust clinical programs, both within their departments, and in the ambulatory centers, and in partnership with our hospitals. When you walk into area hospitals or emergency rooms, you are most likely going to see one of our faculty members.”
UB is also partnering with Kaleida Health and ECMC to overhaul the electronic health records system in Western New York.
“Right now, medical records in Buffalo and Western New York are somewhat of a challenge because everyone is on different medical records platforms,” she said. “We are all going to Epic, which is what most academic health systems are on. This will present a robust opportunity to improve access and decrease the cost of care. It will also help to increase clinical trial participation because it interfaces with the clinical trial platform that is already in place.”
“This will be significant for our researchers, our students and for our practice groups when UB goes live in the fall of 2026.”
Brashear noted that research also continues to drive better health outcomes.
“Innovation is at the heart and soul of UB. We are going to drive innovation and fold artificial intelligence into that.”
She noted that drug discovery comes out of National Institutes of Health
(NIH) funding—citing that 30 percent of pharmaceutical drugs are discovered in academic labs. Brashear said funding from NIH has contributed to 99.4 percent of drugs approved from 2010 to 2019, totaling $187 billion.
Brashear said the fact that the Jacobs School had $69 million in research awards in fiscal year 2024 is evidence that it and all of the health science schools are big drivers of research funding at UB.
“And we are not taking our foot off the gas, no matter what is thrown at us,” she said. “We are still going to be submitting grants, we are still going to be nurturing the next generation.”
Following Brashear’s lecture, she joined a panel of academic health leaders moderated by Melissa Rayhill, MD ’10, to speak about ways in which UB is shaping

The Jacobs School Distinguished Alumni Awards were presented to:
• David A. Milling, MD, ’93, who received the MAA’s “Medical Alumnus of the Year” award.
“Dr. Milling has dedicated his career to advancing medical education, mentoring future physicians, and fostering a more diverse health care workforce,” said Rayhill, who counts herself among those whose career has been influenced by Milling. “His leadership has been instrumental in the launch of the Well Beyond curriculum and the integration of innovative, student-centered learning experiences at the Jacobs School.”

the future of health care in Western New York and beyond.
Other panelists were:
• Benny L. Joyner, MD, the A. Conger Goodyear Professor and Chair of pediatrics
• Blackford Middleton, MD ’85, most recently the chief informatics and innovation officer at Apervita, Inc.
• David A. Milling, MD ’93, executive director of the Office of Medical Education and senior associate dean for medical education
• Beth A. Smith, MD, ’00, professor and chair of psychiatry and chief of the Division of Child and Adolescent Psychiatry
• Daniel Woo, MD, professor and Irvin and Rosemary Smith Endowed Chair of neurology
Milling oversees admissions, curriculum, and student and academic affairs as the executive director of the Office of Medical Education and as senior associate dean for medical student education.
• Margaret Paroski, MD ’80, who was honored with the “Distinguished Medical Alumna” award.
Paroski is a distinguished neurologist and a dedicated leader who has profoundly impacted the medical landscape, Brashear said, noting her remarkable career has been characterized by significant contributions to medical education, clinical practice and health care administration.
Paroski currently serves as the chief medical officer of Catholic Medical Partners, a large independent practice association, where she also served as president and CEO from April 2020 until this past March.
Throughout her career, Paroski has
held significant roles, including medical director at Erie County Medical Center, senior associate dean and interim dean at the Jacobs School and executive vice president at Kaleida Health.
Her commitment to the Jacobs School is further exemplified by her more than 40 years as a dedicated faculty member in neurology, during which she received multiple teaching awards and served as the neurology clerkship director for 28 years.
• Menghang Xia, PhD ’93, who received the “Distinguished Biomedical Alumna” award, an honor bestowed upon graduates who have demonstrated exceptional achievement and made significant and lasting contributions to the biomedical field.
Xia’s journey began with her doctoral

degree in pharmacology and toxicology from the Jacobs School , where she was mentored by Suzanne G. Laychock, PhD. It was the foundation upon which she has built an extraordinary scientific career.
Following postdoctoral training at the University of California at San Francisco, Xia has risen to prominence at the National Institutes of Health, currently serving as the Group Leader of Systems Toxicology at NCATS.
Xia’s extensive scholarly contributions, including numerous publications, book editorships, and presentations, have established her as a leading voice in toxicology.
For more coverage of the 2025 Alumni Weekend, including a link to a photo gallery from various events and a recording of the Harrington Lecture, visit medicine.buffalo. edu/harrington
The Jacobs School’s DoctHERS network brought together physicians, clinicians, scientists, health care practitioners, medical students and residents to discuss issues in the medical and scientific field while fostering a community of peers, mentors and opportunities for future generations of women in medicine and science.

Sylvia Sussman, MD, defied convention when, as a mother of three young children, she entered the University at Buffalo School of Medicine in 1956–one of only two women in her class. Graduating in 1960, she built a distinguished career in anesthesiology while inspiring countless others through her courage, compassion and belief that age and gender should never be barriers to achievement. In honor of her groundbreaking path and lifelong mentorship, the Sylvia W. Sussman, MD ’60 Fund was created through her bequest to support UB’s DoctHERS Program. This initiative empowers women in medicine and science–connecting students, faculty, and professionals to foster mentorship, leadership and equity in the field. Dr. Sussman’s legacy ensures that future generations of women can pursue their dreams with confidence and community–just as she once did. Her gift is a testament to the power of perseverance, purpose and giving back.
The Jacobs School’s DoctHERS Symposium celebrated its 10-year anniversary at an event Sept. 27 at The Westin Buffalo. Titled “Leadership Prescription: Vision, Voice, and Vitality for Women in Health Care,” it featured Bonnie Litvack, MD, diagnostic radiologist from Northern Westchester Hospital, as the keynote speaker.
Litvack, past president of the Medical Society of the State of New York, delivered a presentation titled “Empowering Women: The Intersection of Wellness and Leadership.”
Among the Jacobs School alumni and faculty presenters were: Allison Brashear, MD, MBA, vice president for health sciences and dean of the Jacobs School; Benny L. Joyner, MD, chair of the Department of Pediatrics at the Jacobs School; and Surbhi Bansal, MD ’09, associate professor of ophthalmology at Virginia Commonwealth University.
The event was sponsored by the Jacobs School, the Medical Alumni Association, the Loftus Family Fund, and the Susan Sussman, MD, Fund.
The Jacobs School’s DoctHERS Symposium celebrated its 10-year anniversary at an event Sept. 27 at The Westin Buffalo. Pictured from left to right: Surbhi Bansal, Dean Allison Brashear, and Jessica (Aliotto) Donhauser, president of the Medical Alumni Association.

For more information about leaving a legacy, contact Wendy Irving, Esq., dev-pg@buffalo.edu or 877-825-3422.
Honor an individual who has outstanding achievements as a physician or a biomedical scientist, has shown personal leadership and provides exemplary services to their community!
We Want to Hear from You! Have news? Stay connected and share your updates with fellow alumni. Send us your updates in life since graduation: career, family, awards, honors, travel, favorite medical school memory—whatever you wish. And we’ll post it to our online Class Notes section.
We are excited to welcome Jessica (Aliotta) Donhauser, MD ’13, as the new president of the Medical Alumni Association at the Jacobs School of Medicine and Biomedical Sciences for the 2025–2027 term.

Aproud Buffalo native, Donhauser completed both her medical degree and pediatric residency at the Jacobs School. Her deep ties to the community and passion for academic medicine continue to shape her work today.
In addition to serving as a dedicated pediatric hospitalist at Oishei Children’s Hospital and clinical assistant professor of pediatrics at the Jacobs School, she also works closely with students in her new leadership role as assistant dean of student and academic affairs.
Renowned for her teaching ability, Donhauser has been awarded the Jacobs School’s Faculty Teaching Award three times (2017, 2022, 2023) and was honored with the Outstanding Resident Teaching Award in 2014.
A member of the Gold Humanism Honor Society, she earned the Daigler Chief Resident’s Award in 2016 and received the Leonard Tow Humanism in Medicine Award from the Jacobs School in 2019.
Thanks to the generosity of alumni, faculty, staff, students, friends, corporations, foundations and more, the Jacobs School of Medicine and Biomedical Sciences achieved a fundraising record in fiscal year 2024-25.
The Jacobs School received gifts totaling $35.87 million for the year, surpassing its annual goal by 18.1% and marking a 39.7% increase over the previous year.
Support from individuals, corporations and foundations exceeded $19 million, double the amount of giving from these groups since fiscal year 2023.
Friday, May 1 and Saturday, May 2, 2026
Celebrating our 180-Year Legacy of Education, Innovation, and Healing
Join your classmates and fellow alumni for reunion events, including a special 50th anniversary celebration for the Class of 1976, the Harrington Lecture, Distinguished Alumni Awards, an event highlighting the school’s 180th anniversary, our annual medical school Commencement, and more!
As president of the Medical Alumni Association, Donhauser will build upon recent momentum by strengthening connections with regional alumni and expanding local engagement efforts. She is eager to connect with alumni near and far to help cultivate a stronger, more vibrant Jacobs School of Medicine and Biomedical Sciences alumni network.
Whether you’re in Buffalo or beyond, now is a great time to get involved. Have ideas for alumni activities in your area? Want to reconnect with classmates or support current students? We want to hear from you! Please send your welcome messages for Jessica Donhauser or any suggestions and opportunities for alumni engagement to ubmed@buffalo.edu.
Notable gifts included: a $1.5 million endowed chair in the Department of Psychiatry, a $1 million endowed professorship in nutrition, and two fully funded endowed scholarships for medical students.
In addition, alumni of the school confirmed planned gifts to the Jacobs School of $7.36 million to support student scholarships, research and other school priorities, ensuring a lasting legacy of impact for future generations.
Thank you for your continued support of the Jacobs School and its mission!
An endowed chair in the Department of Psychiatry at the Jacobs School of Medicine and Biomedical Sciences will honor Emeritus Professor Barry S. Willer, PhD.
This position is being funded by a $1.5 million gift from UBMD Psychiatry, the department’s clinical practice plan. Comprised of over 50 faculty members, the group used several years of significant clinical revenue to fund this investment.
Beth A. Smith, MD, ’00, chair of the Department of Psychiatry and president of UBMD Psychiatry, said that gains from clinical operations are often invested back into the clinical practice. This year, the group felt it was imperative to invest longitudinally to aid in the expansion of the department’s commitment to academic research.
“We looked at our strategic plan and considered our strengths and areas for growth,” Smith said. “We have a substantial clinical footprint, robust community engagement, and an excellent teaching component with some of the highest rates of medical students entering the field of psychiatry nationwide. Through this investment, we saw an opportunity to strengthen our research mission and invest in recruiting and retaining toptier researchers. This fundraising effort speaks to our faculty’s commitment to cutting-edge research, to the culture of the department and how highly we value mentorship and collaboration.”
Allison Brashear, MD, MBA, UB’s vice president for health sciences and dean of the Jacobs School, said, “Barry Willer’s collaborative and innovative approach to research has redefined how we understand and treat traumatic brain injury, leading to global policy changes and improved outcomes for countless individuals.
This endowed chair position honors his extraordinary legacy while advancing UB’s commitment to transformative research that changes lives. It also strengthens our ability to recruit world-class faculty, secures competitive funding, and provides our students and trainees with the tools they need to solve the most pressing health challenges. With this appointment, UB Psychiatry affirms its role as a national and international leader in mental health research and care.”
Willer, a trailblazing brain injury expert and longtime member of the psychiatry department, is internationally recognized for making significant contributions to treating sports-related concussions and traumatic brain injuries. His prolific 40-year career has led to the development of tools that remain gold standards in the field, including the community integration questionnaire and the “whatever it takes” model. Through a longtime collaboration with UBMD Orthopedics and Sports Medicine members John J. Leddy, MD, and M. Nadir Haider, MD, PhD, Willer is also credited with developing the current recommended treatment model for sportsrelated concussions.

“Our research moved the field from a very passive wait and see, ‘rest is best’ approach, which had no scientific support and did not facilitate recovery, to an early, individualized, active controlled aerobic exercise therapeutic approach,” said Leddy, clinical professor in the Department of Orthopaedics and medical director of the Concussion Management Clinic. “It’s used all over the world to help athletes and nonathletes recover from concussion.”
The group’s development of the Buffalo Protocol has improved recovery outcomes for thousands of patients, influenced the return-to-play guidelines for the National Football League, National Hockey Leage and the International Consensus Conference on Concussion in Sport, and provided instrumental guidance on return-to-duty protocols adopted by the U.S. military. “Dr. Willer brought a brilliant research mind to bear upon, and systematically investigate, a vexing clinical problem, and this approach literally changed the field forever,” Leddy said.
Willer served as the director of research for UB’s Concussion Management Clinic, where he led studies that shaped the future of brain injury care. His seminal work with a team of researchers and students explored how exercise accelerates recovery from concussion by improving brain efficiency, as demonstrated through fMRI studies. He has also led investigations into emotion regulation in individuals with moderate to severe traumatic brain injury, developing a computer-based treatment protocol now being tested in a multi-site, multi-national randomized controlled trial.
“Without Dr. Willer, Buffalo would not have a world renown concussion clinical and research program,” Leddy said, noting that his career also would have taken a very different arc without Willer’s mentorship. “Buffalo and I are forever indebted to Dr. Willer for his decision to investigate ways to help patients recover from a common and potentially devastating brain injury.”
Barry S. Willer, left, and John J. Leddy pioneered a treadmill test to assess the degree of exercise tolerance in patients with concussion that is still considered best practice in the field.
The Barry S. Willer, PhD, Endowed Chair for Psychiatric Research will build on Willer’s extraordinary legacy of research, teaching and service. The search for the inaugural chair is underway, with appointment anticipated by July 2026. Interested donors can support the endowed chair by contacting the Jacobs School Office of Advancement at 716-823-2403 or jeffryco@buffalo.edu.
GERALD “JEFF” FRIEDMAN, MD ’57
Former gastroenterologist and professor emeritus at Icahn School of Medicine
Gerald “Jeff” Friedman of Scarsdale, New York, passed away on June 9, 2025. He was 98 years old.
Born in 1927, Friedman was an Army veteran who served in Japan during World War II. He graduated from Rutgers College of Pharmacy in 1951 and earned a PhD in pharmacology from Syracuse University. He earned his medical degree from the University at Buffalo and later a master’s degree from the Institute of Clinical Nutrition at Columbia University.
An award-winning, preeminent gastroenterologist and professor emeritus at Icahn School of Medicine at Mount Sinai in New York City, Friedman taught
A cherished alumnus, donor, emeritus faculty member, volunteer and lifelong friend of the Jacobs School.
Howard Wilinsky, MD ’61, a psychiatrist and longtime faculty member at the Jacobs School, died on Sept. 9, 2025. Wilinsky’s connection to UB spanned generations. A legacy alumnus, he was the first in his undergraduate class to be accepted into medical school, granted early admission at the end of his junior year. He completed his internship and psychiatric residency at Edward J. Meyer Memorial Hospital, served in the U.S. Public Health Service Commissioned Corps, and returned to UB in 1967 to begin a distinguished career in academic medicine and private practice.
A member of the American Board of Psychiatry and Neurology, his professional career spanned more than 60 years. He led the Forensic Psychiatric Service and held a voluntary faculty appointment as assistant clinical professor in the Department of Psychiatry. Even after retiring in 2014, Wilinsky remained strongly committed to the Jacobs School, contributing to the admissions committee, the Gold Humanism Honor Society and the Medical Emeritus Faculty Society. He
physiology and pharmacology and remained in private practice for more than 50 years. He was a lead editor and a contributor to many professional texts. He lectured nationally and internationally, and he served as a consultant to several pharmaceutical companies. After leaving private practice, Friedman taught nutrition to medical students at the Icahn School of Medicine at Mount Sinai. He became an advocate and spoke nationwide and in Washington, D.C., in support of a mandatory nutrition curriculum for medical students. Most recently, he authored “The You Factor” (2025) with his daughter Wendi Friedman Tush. The book offers a pragmatic, drug-free approach to weight loss and improved health to mimic the mechanism of GLP-1 drugs.
In 2024, Friedman and his daughter agreed to establish an endowed professorship in nutrition at the Jacobs School.
For many years, Friedman and his wife, the late Roberta Doris Friedman, served on the Board of Directors at Shakespeare and Co. in Lenox, Massachusetts. Friedman was learning to play the guitar during his last two years.
He is survived by his daughter, Wendi, and granddaughter Gabrielle Friedman of New York City, his son Gary D. Friedman and wife Elaine R. Friedman, grandson Grant Friedman, and granddaughter Halle Friedman of New York City. He is also survived by nieces, nephews, extended family, friends and many others who loved him.
Memorial gifts directed to the Gerald Friedman ’57 and Wendi Friedman Tush Professorship in Nutrition and Health can be made by contacting the Jacobs School Office of Advancement at 716-823-2403 or jeffryco@buffalo.edu.
was also a valued member of the Emeritus Center board.
A committed humanitarian, he volunteered with the Human Rights Initiative, assisting in the screening of refugees seeking asylum, an extension of his belief in medicine’s role in advocating for justice and human dignity. He also started a successful eating disorder unit at BryLin Hospital. He was inducted into UB’s chapter of the Gold Humanism Honor Society in 2016.
A Rochester native, he attended Williams College and followed in the footsteps of his father, Isadore Wilinsky, MD ’28, to UB for medical school.
A savorer of books and classical music, he viewed the arts as gifts to be shared, facilitating discussion groups, and taking courses in music, theater, and literature, well into his final years. He was an accomplished piano player and longtime philharmonic supporter. He was an outdoorsman and adventurer, too. He never missed an opportunity to be active or outside, and his zeal for travel took him and his beloved wife, Shirley, to over 25 countries across six continents.
Survivors include his wife, Shirley; four daughters; eight grandchildren; and two great-grandchildren.

Jacobs School graduates urged to make the most of their unique training as they head out to change the world for the better
More than 170 medical students were celebrated at the medical school event on May 2.

If a single theme resonated across dual Jacobs School commencement ceremonies this spring, it was that graduates not only have the skills and training to make an impact on the world around them, but that their expertise and intellectual vigor are needed now more than ever. Amid so much uncertainty and upheaval surrounding the fields of science and medicine at the national level, more than 480 Jacobs School students were honored at the school’s medical and biomedical sciences commencement ceremonies in May.
“Your beginner’s mind is invaluable in medicine, especially as the pace of medical advancements accelerates. And I hope you maintain that mindset, even when you’re no longer a beginner.”
– David J. Skorton, president and CEO of the
AAMC

Nine members of the Class of 2025 earned dual MD/PhD degrees, one earned an MD/ MBA degree, and another earned an MD/ oral and maxillofacial surgery degree.
During a special ceremony, Jeremy M. Jacobs Sr., chairman of Delaware North and chair emeritus of the UB Council, was awarded the Chancellor Charles P. Norton Medal, UB’s highest honor, presented annually to publicly recognize major achievements that dignify Buffalo. Jacobs began serving on the UB Council in 1997 and was chair from 1998 to 2025. This year, he was named chair emeritus in recognition of his leadership and significant contributions to the university.
“Those of us gathered today greatly look forward to seeing you take what you have learned at the University at Buffalo and apply it to the greater good.”
– UB President Satish K. Tripathi




“You have the power to inspire, to innovate, to lead, and, most importantly, to comfort and heal.”
– Allison Brashear, dean of the Jacobs School
“We
who are educated in biomedical science must do a better job in contributing to the public understanding of science. You are the science superpower, and we need you to continue to use that power for the public good.”
– Mark O’Brian, professor of biochemistry


A total of 31 doctoral, 73 master’s and 201 baccalaureate degrees in biomedical science fields were awarded during the biomedical sciences commencement ceremony on May 18.
Six graduate students and 13 senior undergraduates were singled out for special honors, including five graduates who received a SUNY Chancellor’s Award for Student Excellence, the highest State University of New York undergraduate honor.
Eleven of the doctoral degrees and six of the master’s degrees were awarded in the Roswell Park Comprehensive Cancer Center Graduate Division.
For more coverage of the Jacobs School commencement ceremonies, visit medicine. buffalo.edu.



University at Buffalo 916 Kimball Tower Buffalo, NY 14214-8028


