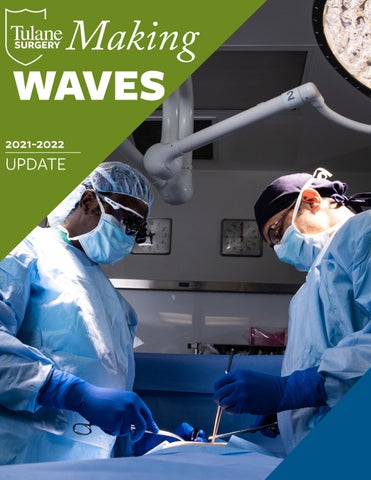
Making WAVES





Each year that I have been the Chair of the Department of Surgery at the Tulane School of Medicine, I am always deeply impressed by the faculty, residents, and staff who continue to uphold our esprit de corps within our department.
We started the 2022 academic year with Hurricane Ida’s landfall as a category 4 Hurricane. This impacted our department in ways we had not seen in a long time. However, even starting the year with the impact of the hurricane, this did not hinder our department’s determination to lead a cascading impact to transform our profession. In the next spread, you will be able to learn more details about how our surgeons and residents overcame the challenges Hurricane Ida presented to them in their personal lives and in our hospitals.
This year our team of surgeons, scientists, residents, and staff exceeded all expectations in the most impactful ways. We now have our first RO1 and R21 in the department in a long time and the grant submissions and clinical trials have exponentially increased. We are fortunate to have a Director of Research who is tracking this success and keeping our processes organized.
We continue to be recognized for excellence in teaching by the students, the department having been nominated for Overall Department each year. Our resident training is high quality and this fall, we celebrated the first full year of Dr. Yu’s tenure as program director. Under his watch, we have solidified our curriculum and have made great strides in a more holistic approach to resident recruitment. We established the inaugural Vice Chair of Surgical Education, filled by Dr. Jacquelyn S. Turner, who in her first 9 months has refined and implemented several pathway initiatives to achieve our goal of diversifying the workforce.
Clinically, the last year and a half have been stressful coming out of COVID, a major Hurricane and the devastating impact of the nursing shortage. It has been hard. FULL STOP. While there is no golden ticket, our future is bright with the announcement of our integration with the LCMC Healthcare system. Our department was ahead of the game in that our residents have long trained at East Jefferson and we have developed the subspecialty expertise that will fill the gaps at that hospital. We have a long road ahead, filled with uncertainty, but I truly believe this is a game-changing opportunity to allow us to continue clinical growth and therefore further support the other missions within the department.
Above all else, we value authenticity, integrity, and an environment of professionalism to shape the future surgeon leaders of tomorrow-we have stayed true to this despite the difficulties of the recent past and the uncertainty of the future. Our faculty, staff and residents are second to none and I am eternally grateful to each for their commitment to our Vision and dedication to the department.
MARY T. KILLACKEY, MD




A professor offering shelter to students. Neighbors coming to the rescue. Co-workers caring for the city’s most vulnerable and bonding in a time of epic need. When wind and rain from Hurricane Ida lashed the Greater New Orleans region on August 29, 2021, the collective response of our community showed — once again — how we are always STRONGER TUGETHER.
“There was so much friendship,” recalled JUAN DUCHESNE, MD, FACS, Chief of Trauma and Acute Care & Critical Care Surgery. “Seeing people come together and just take care of each other, that’s what makes everything easier.”

The Category 4 storm caused more than $75 billion in damage, was responsible for 55 deaths, and left more than one million households without power at a time when temperatures in the area hit 100 degrees.
In the aftermath, Tulane students who had sheltered in place during the storm were evacuated to Houston, where the university arranged for temporary housing until students could travel home. Tulane clinics shuttered during the storm reopened within days. And Tulane surgeons got back to work even as they wrestled with ensuring the safety of their own families amid power outages and damage at their homes.
MICHAEL GHIO, MD, a general surgery resident, was at the hospital when the storm hit. He said an undercurrent of fear and confusion was palpable among his fellow residents, who had never weathered a serious storm in New Orleans. But as the power flickered, they made the best of a tough situation, Dr. Ghio said. A combination of teamwork and friendly competition helped the residents manage patients with limited resources. They kept morale up by playing board games during the quiet times.
“We functioned as a beautiful team, dividing up responsibilities and teams amongst us and working shifts,” said Dr. Ghio who worked alongside fellow surgical residents
ALEXANDRA ONYIEGO, MD, KAREN IRIZARRY, MD, KEVIN SLAUGHTER, MD and HECTOR MEJIA-MORALES, MD.
Although most of his neighbors evacuated before the storm, ANIL PARAMESH, MD, FACS, Professor of Surgery, Urology, and Pediatrics at the School of Medicine, felt safe sheltering at home with his family based on the storm’s projected path. He also opened his home to two Tulane undergrads to ride out the storm.
 Chrissy Guidry, DO, Director of Well-being, Graduate Medical Education, joined residents in a game of “Organ Attack!”
Chrissy Guidry, DO, Director of Well-being, Graduate Medical Education, joined residents in a game of “Organ Attack!”
When the trajectory of the storm shifted closer to home, Dr. Paramesh started to doubt his decision to stay.
“We realized a little too late that it’s too late to leave,” said Dr. Paramesh, describing the chaotic scene as Ida blew through. “We saw lots of debris flying all over the neighborhood. My chimney broke, and I had bricks flying around my yard and water leaking.”
After the storm, Dr. Paramesh, surveyed the neighborhood’s extensive damage and sent neighbors photos and regular updates. The storm had knocked out major transmission lines, severing the city’s connection to the outside power grid. Officials were predicting it would take weeks — if not months — to restore power. Dr. Paramesh returned the students to campus, to be evacuated to Houston, and found a place for his family and their dogs a few hours away in Fairhope, Alabama.
While in Alabama with his family, Dr. Paramesh continued working remotely, taking daily calls about patient management with Tulane Medical Center. While the transplant program was put on temporary hold in the storm’s aftermath, the team was busy taking care of patients who had been transplanted at other facilities where there now had no electricity.
Dr. Paramesh and his family returned to New Orleans three days later, when the hospital began housing staff and physicians in local hotels. The hospital also provided food, cleaning supplies and gas, which was a
scarce resource as people scrambled to keep generators running. “I’m so thankful for the hospital. They really took care of their staff and faculty, and it made it easier to come back to work,” he said.
MARY T. KILLACKEY, MD, FACS was fotunate enough to have running water which allowed her to stay in New Orleans to cover transplant services while other faculty sorted plans. Dr. Killackey got to the hospital roughly 24 after the storm. and in the subsequent 72 hours, I was blown away and yet, not surprised.
Chief Resident, Kevin Slaughter, who had essentially been awake for 48 hours straight, was focused. He had a handle of all the surgical inpatients and led his junior residence with confidence and grace. They were all singularly focused on providing the same level of care to all of the patients. “It reinforced everything I knew about these residents and validated my knowledge that I would allow any Tulane trained surgeon to operate on me or my own family— you don’t get any better than these surgeons.” said Dr. Killackey.
Dr. Duchesne recalled having a bad feeling as he looked at the storm’s projected path. He grew up in Puerto Rico and had seen his share of hurricanes, but his experience with Hurricane Katrina made him wary of Ida’s arrival, he said. As the hurricane closed in, Duchesne packed up his family and headed to Houston in an RV they had purchased previously for family trips.
They spent three days in Texas before returning home to assess the damage. Driving Highway 90 to his home in Luling, the storm’s impact was a shocking sight despite knowing the devastating potential of a Category 4 storm, he said. Wide swaths of downed trees and debris from obliterated homes littered the road. Streets had turned into rivers.
The real shock came as Dr. Duchesne and his family approached their own home. Large oak trees had been flattened. A fence had been ripped out and blown away. Every shingle on the roof, gone, and a gaping hole caused by what they later learned was a lightning strike. It was also clear that a tornado had torn through the property. “I was in total disbelief, a state of shock,” he said.
What followed is still a bit of a blur, Dr. Duchesne said. Weeks of cleanup and rebuilding — of his own home, as well as pitching in to help neighbors get their homes back in order. Friends and neighbors all showed up with equipment to help clear debris from his property. They took in friends who needed a place to stay or something to eat.
They worked from sunrise to sunset for weeks, in a hurry not only to restore a sense of normalcy in their lives but also because Dr. Duchesne was preparing for his daughter’s wedding. The event was scheduled to take place on their property in October, less than two months after the storm. “[My daughter] trusted us and it really gave me the motivation to make our place amazing,” he said. “It was a bad situation, but it’s all about resilience.”
On the big day, the weather cooperated, and their guests were gifted with a beautiful sunset over the water.
“That was a great moment of satisfaction and of resilience,” Dr. Duchesne said. “We had close to 200 people at our home for the wedding and there seemed to be a sense of relief among everyone there. It’s a small community, and after everything we went through together, people were ready to have a good time.”
THE DEPARTMENT OF SURGERY has collaboratively defined who we are and the vision of our future based on six strategic pillars:
Our rich history has created the foundation for our latest innovations and forward-thinking strategies to cultivate education research and patient care. We expect each member of our team to make a celebrated contribution to this well-known reputation.
We are the clinical powerhouse of the Gulf South. Our surgeons are the first choice among patients and providers. We focus on organizing care for complex patients and meeting the health needs of underserved populations.
We develop the modern surgeon through a curriculum that drives excellence in surgical skill and these four areas: effective teaming, learning systems, wellness, and leadership development.
Our research is meaningful and unique and translates to clinical practice. Moreover, our academic surgeons lead the way in shaping the guidelines that improve the quality and efficiency of surgical practice.
We successfully recruit diverse faculty and trainees from all populations and geographic regions, so our the impact reaches into every community.
We intentionally create an esprit de corps where the whole person thrives. Our alumni seek and hold leadership roles in our societies and in other centers, allowing us to spread our cultural principles throughout the surgical profession. We will achieve the successful transformation of our profession by each student, resident, and faculty sharing these core experiences from their time at Tulane.
This year, the division performed the highest total number of solid organ transplants in the past decade and an all-time high number of living donor kidney transplants, despite operations at Tulane Medical Center shutting down for several weeks after Hurricane Ida. Our surgeons also performed 17 kidney transplants (an all-time high) at Children’s Hospital New Orleans, with 14 deceased donor and 3 living donor kidneys.
Our faculty continued to excel at research with a collaborative team of students, residents and fellows, successfully publishing 90 articles in impacted journals, including Annals of Surgery, Annals of Oncology, and Journal of the American College of Surgeons. Our team has successfully established Tulane as the institution with the most comprehensive experience with radiofrequency ablation of thyroid nodules in North America. Nearly 50 percent of our practice is related to referrals from out of state. We performed more than 500 surgeries and, for the second year, we were honored to be the sole endocrine oral paper at The American Surgical Association, the most renowned national surgical organization in the U.S.
The past year has been both engaging and industrious for our division with the openings of the Weight Loss Clinic and Reflux Center of Excellence at Tulane Lakeside Surgical Center in Metairie, LA. Moreover, the Tulane Bariatric Center has been recognized nationally as the Comprehensive Center under the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program. In addition to first-class fellowship training, and exemplary patient care, our division’s research efforts have proven to be advantageous - having published an article in the Journal of Surgical Endoscopy.
Our division has consistanly been recognized internationally for academics, exemplary patient care and research. Upholding a long tradition of excellence, Tulane’s trauma surgery division continues to forge new heights in the field of trauma surgery research by leading national multi-center studies as well as significantly contributing to practice management guidelines for pre-hospital procedures in urban areas.

Dr. Chaffin, who was elected as a member of the American Association of Plastic Surgeons, presented her work on complex wound reconstruction at the Symposium for Advanced Wound Care and the Boswick Wound and Burn Care Symposium.

It has been a year of continued growth for pediatric surgery, including the completion of the new 57,000 square foot surgery center at Children’s Hospital of New Orleans and a focus on development of clinical programs in pediatric trauma, burn and wound care. In October 2021, David Yu, MD, FACS, FAAP, joined the Division of Pediatric Surgery.

The TULANE SURGICAL SOCIETY celebrated thier annual gala on March 26, 2022, after a two-year hiatus. The gala was held at the Higgins Hotel and honored Tulane Surgety alumna MARLETA REYNOLDS, MD (R ,76). Dr. Reynolds is currently a Professor of Surgery at Northwestern and a pediatric surgeon at Ann & Robert H. Lurie Children’s Hospital of Chicago.
TULANE SURGICAL SOCIETY 2021 - 2022

President: David Yu, MD, GS ,11

President-Elect: Marie Unruh, MD, GS ,13
Vice-President: Matt Zelhart, MD, GS ,16
Secretary: Catherine Baucom, MD, PhD, GS ,11
Treasurer: Sandy Florman, MD, GS ,00 (2021)
MEMBERS-AT-LARGE: (TERM ENDING)
Ralph Corsetti, MD, GS ,96 (2022)
John Lindsey, MD, GS ,91 (2023)
Jyoti Arya, MD, M ,94, GS ,99, F ,07 (2024)
Anne Rizzo, MD, GS ,94 (2025)
Kira Long, MD, GS ,16 (2026)
RESIDENT MEMBER: Erik Green, MD, GS ,22
FOR MORE INFORMATION, VISIT:
We cannot achieve our vision without your support. Your gifts in support of resident research and extraordinary faculty will help continue the DEPARTMENT OF SURGERY’S nearly 200-year-old mission of education, research and clinical work.
Your generosity would help guarantee that the Department of Surgery recruits and retains renowned faculty to endowed chairs and professorships.

ENDOWED ACADEMIC EXCELLENCE FUND | $50,000+
Your gift establishing an Academic Excellence Fund will provide flexible funding that allows Dr. Killackey to respond to the department’s most critical needs and exciting opportunities.
ENDOWED EARLY CAREER PROFESSORSHIP FUND | $300,000+
Your gift will recognize the promise and potential of a junior faculty member to help ensure students receive the highest quality medical education.
ENDOWED CHAIR | $1,500,000+
Faculty at Tulane are uncovering discoveries that work to eradicate disease and improve health worldwide.
Your gifts would allow us to elevate research by supporting residents in their research years, ensuring the department will remain a beacon of innovation for aspiring surgeons.
CURRENT-USE RESIDENT SUPPORT ANY AMOUNT
Provide immediate support to the residency program.
ENDOWED RESIDENT SUPPORT FUND | $100,000+
Establish an endowed fund to provide ongoing research support of the residency program.
