


















To fellow rheumatologists,
It is with great pleasure to welcome you to the first issue of ‘Voice of APLAR’ Australia. As a sister publication to the regional ‘Voice of APLAR’, this newsletter is focussed on raising awareness of advances in the field of rheumatology through an Australian lens. The publication will celebrate Australian research, local and inspiring rheumatologists, as well as provide a forum for exchanging clinical experience and expertise on managing rheumatic diseases.
It is hard to ignore the current reality of COVID-19 and the challenges it has brought to the delivery of clinical services. However, we have learnt a lot over the course of this pandemic. As Jared Dart discusses in his article, telehealth has been invaluable in providing continuity in care to patients. However, we should ensure we continue to harness the benefits of this platform beyond this period, especially for our patients in rural and regional areas. While it is

likely telehealth has always been in use by some rheumatologists, getting more rheumatologists to embrace this technology will enable greater patient accessibility to specialist care in the future.
Focussing on the needs outside of pharmacotherapy intervention, this edition also explores resources available to patients that may help them manage and take ownership of their condition. Some examples include information resources presented in different languages, which are available on the Australian Rheumatology Association (ARA) website. Education materials that explain common symptoms, such as pain, and a guide on how to selfmanage, are useful. The online patient support program – MyRA –developed through the support of the ARA is an excellent engagement tool for patients with rheumatoid arthritis and has stimulated me to refer my patients to give this a try. Among these discussions, there is an important reminder about the value of simple measures, such




as providing a list of appropriate organisations and mobilising the relevant mental and allied health services, which should be part and parcel of routine patient care.
As my own journey into this speciality has been driven by working with inspirational Australian female rheumatologists, it is wonderful that we can acknowledge and honour the contributions made by such individuals, such as Professor Catherine Hill, the current President of the ARA. I’m sure you’ll enjoy reading her journey as much as I did.
Finally, I would like to thank all the contributors to this first Australian edition of ‘Voice of APLAR’. If you do have suggestions for future editions, the editorial faculty and I would be excited to hear from you. Please send us correspondence outlining your topic of interest and we will respond as soon as possible following a review.
Dr Shikta Dey
Dr Shikta Dey is a rheumatologist driven by a desire to make a difference to the lives of her patients. Inspired by the work of Australian-based rheumatologists Professor Lyn March and Dr Geraldine Hassett, Dr Dey is currently extending her clinical and academic knowledge in the field of obstetric medicine. Training within this area focuses on rheumatic diseases in pregnancy and the post-partum period, with the hope of becoming an expert in managing complex cases during what should typically be a positive and joyous time of life. Combining her knowledge in rheumatology and interest in obstetrics, Dr Dey is currently undertaking a Master of Philosophy degree. Communication is a major and pivotal component in a rheumatologist’s relationships with their patients. Currently based in South-West Sydney and exposed to patients of culturally diverse and linguistic backgrounds, Dr Dey recognises the need to overcome communication barriers toachieve positive outcomes for the patient. As well as being passionate about effective patient communication, she is actively involved in teaching medical students and general physician trainees to help advance their knowledge of rheumatic diseases and in turn to improve her own knowledge and communication skills.
Dr Shikta Dey RHEUMATOLOGIST (EARLY CAREER) AND OBSTETRIC MEDICINE TRAINEE AT CAMPBELLTOWN HOSPITAL, NSW


Of all the conditions that might lend themselves to telehealth, musculoskeletal disorders are obvious candidates. Lockdowns and restrictions on physical movement, in some ways echo the symptoms of rheumatic disease itself, which can significantly impact upon movement and mobility.


So how is telehealth now viewed given current COVID-19 restrictions?
Certainly in the case of inflammatory arthritis, attitudes towards telehealth since the advent of COVID-19 onset have evolved. Positive engagement with telehealth for inflammatory arthritis patients is of particular importance given the increased risk these individuals have for infection, due to the immune modulating disease-specific treatments in use, and the nature of the underlying disease itself.
Published in the Internal Medicine Journal (Vol 51, Issue 5) in May this year was an overview of healthcare access and attitudes towards telehealth during the

early phases of the COVID-19 pandemic. The study was conducted in over 1000 Australians living with inflammatory arthritis as a collaboration between the COVID-19 Global Rheumatology Alliance (GRA), which is an international registry formed in 2020 to collect and interpret the data of rheumatology patients affected by COVID-19, and the Australian Rheumatology Association Database (ARAD), a national database that collects longitudinal outcome data of inflammatory arthritis patients from self-reported surveys at 6–12 month intervals.
So, what did the survey find?
Outside of exploring questions related to access to regular medications, pathology and radiology services, was the question related to general practice and rheumatologist visits. Patients reported higher confidence in telehealth based access to general practitioner and rheumatology services then for those equivalent services in person. Perhaps this is not surprising given the challenges associated with face-to-face care during the varying lockdown periods –what is interesting however is the baseline values associated with telehealth confidence for GP and
rheumatologist access sitting at 86% and 82% respectively, means that the vast majority of patients with inflammatory arthritis are feeling quite confident about their ability to access their clinician. This was largely true regardless of whether the patient was living nearer to, or away, from a major city. So, in essence, the equitable access across the urban vs rural divide, which has always been a challenge with physical bricks and mortar healthcare service delivery, is far less of an issue in telehealth where we have seen (at least on the input from this particular cohort) a much more equitable sense of access.
Not only is the access more equitable across rural and metropolitan communities but it seems that the question of service continuity via telehealth is also not in doubt. During the height of the first wave of lockdowns in 2020 just under 80% of respondents agreed that telehealth and telephonebased consultations during the pandemic were acceptable and over 80% of these felt comfortable continuing with telehealth subsequent to the pandemic.
In this particular study there was an absence of any significant variations in acceptability of
telehealth when accounting for the age of the patient, their location, education level or their current treatment regimen.
The pandemic has fundamentally affected a range of industries and healthcare is certainly no exception. Nonetheless the disruption caused by the COVID-19 pandemic in terms of healthcare professional access has not significantly impacted upon self-reported assessment of inflammatory arthritis at least on the results of this particular study. Respondents for the most part thought that their inflammatory arthritis was only a little or not at all affected (85%).
For his part, though not involved in the study General Practitioner and founder of virtual care platform Welio, A/Prof Jared Dart feels that the results in terms of telehealth patient acceptability are consistent with those that he has seen in his own Brisbane-based clinic. “Patient acceptability, almost irrespective of age, for simple and secure telehealth is very high” says Dart, “what was not so high was the ease of use within which the systems can be deployed in a primary care setting given legacy and interoperability challenges. These are things we have largely
been successful in overcoming with the Welio service, which we have built with GPs nationwide – not only can we have crystal clear video, audio and seamless payment processing for bulk billed or private consultations in a secure environment but we’ve also integrated these with existing patient management systems in the case of best practice.”
Dr Dart refers to existing and emerging evidence towards the acceptability of telehealth, the continuation of rebate items, and the likely presence of intermittent lockdowns as a perfect storm for telehealth uptake nationally, particularly video telehealth.
“Chronic disease follow-up care where the clinician and the patient have an existing and often long-standing rapport, makes a perfect case for telehealth. So the patient demand is there, the clinical context is appropriate, and we’ve now made the systems available to ensure that both patients and practices can make the most of telehealth moving forward”
Patients with inflammatory arthritis find telehealth generally acceptable. A significant increase in experience deploying and using such systems has been fuelled by the COVID-19 pandemic and is set to become a standard feature of practice in the future.
Gout may not be considered the most exciting of conditions to manage given that it’s a common rheumatology complaint and practice is well defined, but increasing reports raise the question as to whether enough is being done to protect and improve outcomes in those afflicted and whether patients are receiving the best advice on how to reduce their risk. In this article, Dr Helen Keen, a leading researcher and consultant rheumatologist based in WA, explores evidence from Australia and the rest of the world that highlight major gaps in the current management strategies for gout and reveals how much still remains unknown.
 Dr Helen Keen CONSULTANT RHEUMATOLOGIST, HEAD OF SERVICE, FIONA STANLEY HOSPITAL, ROYAL PERTH HOSPITAL, WA
Dr Helen Keen CONSULTANT RHEUMATOLOGIST, HEAD OF SERVICE, FIONA STANLEY HOSPITAL, ROYAL PERTH HOSPITAL, WA
Are we there yet?
It appears not. To reduce gout flares and resolve tophi, it is recommended that patients be treated to a target serum urate (SU) level of <0.36 mmol/L. According to data based in the hospital setting, almost 1 in 4 had not had their SU checked; 4 in 5 had not achieved their target SU; just over half received urate lowering therapy (ULT) and had a post-discharge follow up appointment scheduled. Similarly, in a gout specialty clinic setting in QLD, approximately half of patients were not at target SU levels. These observations extended into the community setting where only 1 in 4 Australians treated with ULT were at target, and more than half of patients on ULT continued to experience frequent flares (defined as two or more per year), indicating undertreatment.
Indeed, these gaps are not specific to Australia. A UK survey assessing GP treatment practices of gout found that a fixed dose of ULT is commonly prescribed, SU levels are not routinely measured and that less than a third of patients are at target. It’s likely that these gaps are driven by multiple factors.
While it is acknowledged that not all patients who have ever
had an attack of gout require ULT, treatment is an important consideration for reducing morbidity. Gout is associated with substantial disability similar to rheumatoid arthritis (RA). Based on 30-year data of a WA cohort, patients admitted to hospital with an acute attack of gout had an increased risk of a major adverse cardiovascular event (MACE) in the first 30 days vs. 6 months before and 12 months after admission (risk ratio of 2.49), and an increased risk of death (hazard ratio of 1.25). Regrettably, unlike other forms of arthritis such as RA that has seen a reduction in morbidity and mortality over time, both the disease and economic burden of gout continues.
For instance, looking at the WA cohort from a healthcare expenditure perspective, it is estimated that there will be 58,000 hospital admissions (ED visits and readmissions) for gout in the next 5 years, costing the economy around one billion Australian dollars, of which around 6% is believed to be preventable if SU is at target.
There is emerging evidence that it does. A UK-based study, which wasn’t specifically designed to assess a treat-to-target strategy, revealed how nurses

“It’s a constant theme, both in hospitals in the community and around the world, that we’re not measuring serum urate. We’re not using enough urate lowering therapy, and we’re not treating to target, even though we all know how to do it.”

and pharmacists treating gout to a protocol that was targeting SU of 0.36 mmol/L achieved better patient outcomes in terms of lower SU levels, increased adherence to ULT, reduced tophi and fewer flares than doctor-led standard routine care.
Several drugs are available to reduce uric acid levels. Allopurinol, a xanthine oxidase inhibitor, is recommended as first-line. In the context of severe kidney disease, the approach is to ‘start low and go slow’ at 50mg/day. This reduces the risk of allopurinol hypersensitivity syndrome and severe gout flares, which could otherwise lead to patients discontinuing treatment.
Screening for the HLA-B*58:01 allele in those of Asian descent could also be worthwhile before treatment is initiated.
Febuxostat is also a xanthine oxidase inhibitor used more commonly in the second-line setting, although there have been concerns regarding its cardiovascular safety profile. The CARES – Cardiovascular Safety of Febuxostat and Allopurinol in Patients With Gout and Cardiovascular Morbidities study, reported higher all-cause mortality and cardiovascular
mortality with febuxostat than with allopurinol. However, in the European Medicines Agency (EMA)‐requested study - FAST (febuxostat versus allopurinol streamlined trial), no signal of an increased cardiovascular risk with febuxostat was noted, although it should be acknowledged that the study population in FAST was at a lower risk of cardiovascular events than the CARES population. Despite the many options, many questions remain about treatment:
• What are the indications for ULT?
• What is the optimal timing of initiation?
• What is the target level for therapy?
• Should inflammatory prophylaxis be commenced when starting ULT?
Are we giving them the right advice?
A holistic approach to managing gout is advocated by international guidelines. An important component to risk reduction and disease management is educating the patient about the benefits of weight reduction, reducing alcohol intake, and consuming
a healthy diet. However, having conversations about lifestyle behaviours can be a challenge that requires the need to avoid a culture of blame and stigmatisation.
When we reflect on our recommendations on diet for instance, which is to avoid foods that are high in purine, contain fructose or fat, we may be doing a disservice given that so many of these foods are actually healthy for the heart e.g., oily fish, shellfish, lean meats, vegetables, beans and fruits. Recognising that patients with gout are at an increased risk of cardiovascular disease and that this represents a common cause of death in such individuals, a low purine diet appears at odds with promoting a heart healthy diet.
From an evidence point of view, this recommendation on diet has been further cast into doubt by a New Zealand study assessing the effect of different food groups on SU levels.
Overall, very few foods were found to have a significant SU raising effect but rather genetics were thought to be playing a larger role. The lack of robust evidence that diet helps to modify serum levels of uric acid lends support to recommending patients with gout to follow a heart-healthy diet.
Patient
Male, 53 year-old Malaysian, non-smoker, non-alcohol drinker
Presentation
Gout (three attacks in last three months)
Medical history
Hypercholesterolemia
Clinical findings
Blood pressure 123/81; normal renal function; serum urate 0.52
Genetic profile
HLA-B*5801 negative
Treatment
Commenced on allopurinol 100mg plus colchicine (500mcg) prophylaxis daily. Patient informed of the risk of a flare.
Plan
Not to stop the allopurinol unless a rash develops and to manage any potential acute flares.
Review patient in four weeks with a repeat serum urate test. If not at target, to increase dose of allopurinol by 50 to 100mg each month. Review patient again after one month (often takes three or four months to get to target). Once target achieved, to taper the dose of colchicine.
This article is based on the presentation ‘Gout: current management issues’ delivered by Dr Keen during the Australian Rheumatology Association webinar: GP Rheumatology Roundup.
References available on request

I live with multiple chronic health conditions and have good days and bad days but my passion for helping others keeps me going.
Iwas diagnosed with rheumatoid arthritis in 2007 (at 37). I’ve since added fibromyalgia, steroid-induced type 2 diabetes, ankylosing spondylitis and spondylolisthesis. That’s just the main conditions. I can also add in mild depression and anxiety plus a range of related conditions, symptoms and side effects.
I’m not saying any of this to get attention. It’s a simple summary of my medical history. However, I am more than just my conditions. I’m still a person who loves to spend time with family and friends, to get out in nature, to sing in a community choir and to learn new things.
I’d like to give you an insight into how I’ve learned to live with these conditions and how they’ve shaped me. I also ask you to think about how your patients might be coping and what you can do to help them holistically.
My first major diagnosis:
rheumatoid arthritis
My rheumatoid arthritis symptoms developed rapidly over a few months. At first, I thought I might have sprained my thumb. Then the pain switched to my other thumb. Then it moved around various fingers before appearing in the ball of one foot. I remember going to my GP and saying, “My hands hurt but I don’t know why”.
I was lucky that my GP recognised these symptoms as being early signs of RA and a blood test confirmed his diagnosis. He put me straight onto methotrexate, prednisolone and an anti-inflammatory drug. Thanks to his early intervention, my RA did not spread beyond my hands and feet and I have no joint damage there to date.
I wasn’t too shaken by that first diagnosis. Yes, I was concerned but it was caught early and I had a treatment plan. Unfortunately, that treatment wasn’t working well enough and my RA kept

raging so my GP referred me to a rheumatologist. Little did I know that I had another health issue developing at the same time.
My surprise second diagnosis
At some point in my life, I had inhaled tiny particles of a fungus known as Cryptococcosis neoformans. This can be found in things like bird droppings and garden mulch. I don’t know when I came into contact with it and the fungus can remain dormant in the body indefinitely. However, in the months after I developed RA, my immune system was severely compromised and the fungus took the opportunity to grow into a nodule in my lung.
The growing nodule did not cause me any symptoms and it wasn’t until I had a chest x-ray when applying for a clinical trial for an RA biologic medication in 2008 that a lump in my lung was picked up. That was a scary time for me. My RA was out of control and I was also undergoing a series of tests to try and work out what the lump was. The obvious candidate was cancer but the test and biopsy results were mixed.
It wasn’t until I had surgery to remove the lump that they ruled out cancer but it still took a few days for the pathology team to work out what it was. I ended up needing a daily antifungal tablet for several years but the nodule was removed cleanly and the fungus has not returned.
Seeking support from others
After I recovered from the surgery, I was getting great medical support but I was struggling to deal with the stress of it all. I came across an article about Naomi Creek from the Young Women’s Arthritis Support Group (YWASG) and decided to reach out to her.
Until I joined YWASG, I hadn’t met anyone else with RA. My family and friends didn’t understand how it affected me.
What I really wanted was to hear from others with similar conditions and to ask them lots of questions like:
• Were my RA symptoms normal?
• How did others manage things like working, socialising or relationships?
• What non-medicinal things did others do to help manage their inflammation, pain and fatigue?
• What other resources were out there to help people like us?
The tips and emotional support I’ve received from other YWASG members over the years has been priceless. They helped me discover how to live with RA as opposed to treating it.
This group has been so important to me that I’m now one of the co-leaders. I still remember what it felt like to be newly diagnosed and the relief of finding people who understood me and could help me. Now, I pay it forward and use my experience and knowledge to help others. They still help me as well.
From 2013 to 2015, I developed one condition after another. I’d experienced excess fluid in my ankles (peripheral oedema) for several years, but it was hard to work out which of my medications was the main cause. I’d also felt more intense joint and muscle pain than what my rheumatologist felt was consistent with my inflammatory markers. We eventually worked out that I had fibromyalgia.
Six months later, I was diagnosed with steroid-induced type 2 diabetes and shingles on the same day. I’d also experienced rapid vision loss over several months and was diagnosed with steroidinduced cataracts in both eyes next. I’d lost 50 per cent of vision in one eye and 20 per cent in the
Although this is my story, I’m sure you’ve seen similarities to the stories of some of your patients. Here are my suggestions for things you can do to help them live better with their conditions.
• Give your patients a list of links or phone numbers for the major patient organisations and peak bodies for their condition.
• Ask your patients if their conditions prevent them from doing things they enjoy and suggest ways they can get help with this, such as mental and allied health support. Treat the whole person, not just the condition.
• Tell them about relevant government supports and benefits they might be eligible for, such as the NDIS, the Mobility Allowance and the Chronic Disease Management Plan. There is a comprehensive list of these supports on the CreakyJoints Australia website.
other eye. Thanks to cataract surgery, I can see well again now.
After each diagnosis, I felt like a fence post being hammered further and further into the ground. I’m fairly resilient but it became harder and harder to pick myself up again each time.
After trying different medication combinations over the next few years, my conditions were relatively stable, so it was disheartening to be diagnosed with ankylosing spondylitis in 2017 and spondylolisthesis in 2019. I can still walk and stand for short periods but I am currently on a waiting list for a spinal fusion for the spondylolisthesis.
Changing my lifestyle
I’d been through several job changes to try and accommodate my pain and fatigue levels, but, when I finished a contract job in 2014, it was obvious that enough was enough and I needed to stop work. Thankfully, I was approved for a partial Disability Support Pension.
I also sought support through the GP Mental Health Treatment Plan as I was struggling to cope with so many different issues. The clinical psychologist I saw helped me work through things like learning to accept where I was at, pacing myself, managing my sleep patterns and calming my stress and pain levels through meditation. This did not replace my need for medications, but it certainly complemented them.
I still have trouble trusting my body at times or working out which symptoms belong to which condition or even if the symptoms are worth mentioning to my doctors. However, I’ve become an expert in taking control of my health management. I keep a diary of my symptoms and medication changes so I can see patterns more easily. I also write my own medication lists and medical history summary so I just hand that over to
OTHER HELPFUL RESOURCES INCLUDE CREAKYJOINTS AUSTRALIA’S
Patient PrepRheum podcast series creakyjoints.org.au/patientpreprheum
A Patient’s Guide to Living with Rheumatoid Arthritis in Australia creakyjoints.org.au/pg-ra
A Patient’s Guide to Living with Axial Spondyloarthritis in Australia creakyjoints.org.au/pg-axspa
Medicinal and Non-Medicinal Arthritis Treatments creakyjoints.org.au/education/arthritis_treatment_ options
Above all, listen to your patient’s concerns, even the small ones. Treat them with respect and show interest in their personal lives. Remember, we are people first and being a patient is just one aspect of our lives.
any new member of my healthcare team. That way, I know they have the most up-to-date information.
These days, my social life is much quieter than it used to be. I don’t go for long bushwalks or camping trips anymore, but I have found a whole new network of friends through the chronic illness community.
During my health freefall years of 2014 and 2015, I still needed to do some paid work to supplement our household income (this is allowable under the DSP). I also wanted to do something productive and satisfying so I started working parttime as a freelance website content writer from home and gradually built up some regular clients.
When Naomi from YWASG was approached by Seth Ginsberg, the co-founder of the Global Healthy Living Foundation (GHLF) and CreakyJoints in the US, to start CreakyJoints Australia, Naomi invited me to join her and become the CreakyJoints Australia editor — an opportunity I jumped at.
CreakyJoints Australia is run by patients for Australian arthritis patients and their families. We share information about treatments, government supports, patient stories and tips for living well with arthritis, especially during the COVID-19 pandemic. Alongside CreakyJoints Australia, we are currently working on developing the GHLF Australia branch of our organisation, which will focus on vaccine education and patient support, education and advocacy across a range of chronic health conditions.
I feel lucky to be doing such exciting work while choosing my hours to fit around my good and bad days and my health appointments. I’ve also volunteered in several health consumer representative roles and helped to make things better for others with health issues. I’m driven by my own health experiences and they now empower me.
Arthritis, pregnancy and the path to parenthood by Suzie May suzieedwardmay.com
Chronically Fully Sick podcast and multiple social media platforms facebook.com/chronicallyfullysick
Arthritic Chick website and multiple social media platforms arthriticchick.com
The Rheuma Mill website and multiple social media platforms therheumamill.com
CONNECT WITH ROSEMARY

LinkedIn: Rosemary Ainley linkedin.com/in/rosemaryainley

Twitter: @rosieainley twitter.com/rosieainley
EULAR 2019: IL-17A inhibitors (TALTZ®) now recommended as a first-line treatment option for patients with PsA who are cDMARD-IR.1
IN BIOLOGIC-NAÏVE PATIENTS WITH PsA WHO ARE cDMARD-IR, TALTZ® DEMONSTRATED
†SIMULTANEOUS IMPROVEMENT IN JOINTS (ACR 50) AND SKIN (PASI 100)a SUPERIOR TO ADALIMUMAB at Week 24 (p=0.036; SPIRIT H2H primary endpoint), which was sustained across 1 year (p<0.001).2,3
†PROVEN EFFICACY ACROSS PsA DOMAINS including resolution of enthesitis, dactylitis and fingernail psoriasis at Week 24 (SPIRIT H2H).2
aAll patients in the SPIRIT H2H trial had coexistent psoriasis with BSA ≥3%.2
†LONG-TERM EFFICACY IN JOINTS with 52% maintaining or achieving ACR 50 at 3 years (SPIRIT-P1).4
WELL-DEFINED SAFETY PROFILE5
TALTZ® was extensively studied in 11 clinical trials in PsO, four in PsA, and two in r-axSpA.5
Study details: SPIRIT H2H (N=566): Multicentre, randomised, open-label, parallel-group phase IIIb/IV trial. Biologic-naïve patients with active PsA and coexistent psoriasis (BSA ≥3%), and inadequate response to cDMARDs were randomised to receive TALTZ® 160 mg starting dose, then 80 mg every 4 weeks or adalimumab 40 mg every 2 weeks. Primary endpoint was the proportion of patients simultaneously achieving ACR 50 and PASI 100 at Week 24 (superiority test for TALTZ® vs adalimumab), which was met.2
SPIRIT-P1 (N=417): Multicentre, randomised, double-blind, placebo-controlled phase III trial. Biologic-naïve patients with active PsA were randomised (1:1:1:1) to placebo, TALTZ® 80 mg Q4W, TALTZ® 80 mg Q2W or adalimumab 40 mg Q2W (active reference; study not powered to compare TALTZ® and adalimumab). Primary endpoint was the proportion of patients achieving ACR 20 at Week 24, which was met.6
PBS INFORMATION: Authority required. For the treatment
TALTZ® Minimum Product Information. INDICATIONS – TALTZ is indicated for the treatment of adult patients with moderate-to-severe plaque psoriasis who are candidates for systemic therapy or phototherapy; treatment of active psoriatic arthritis in adult patients who have responded inadequately, or who are intolerant, to previous DMARD therapy. May be used as monotherapy or in combination with a conventional DMARD (eg methotrexate); treatment of active ankylosing spondylitis in adult patients; treatment of adult patients with active non-radiographic axial spondyloarthritis with objective signs of inflammation as indicated by elevated C-reactive protein (CRP) and/or MRI evidence, who have responded inadequately to, or are intolerant to, nonsteroidal anti-inflammatory drugs (NSAIDs). CONTRAINDICATIONS – Serious hypersensitivity to ixekizumab or any of the excipients. PRECAUTIONS – Chronic or active infections, do not administer in patients with active tuberculosis; hypersensitivity – discontinue treatment immediately if a serious hypersensitivity reaction occurs; inflammatory bowel disease – exercise caution; immunisations – do not use with live vaccines; Use in Pregnancy Category C. ADVERSE EFFECTS Clinical Trials Experience – Very Common (≥10%) injection site reactions (including erythema and pain), infection (including nasopharyngitis, upper respiratory tract infection and viral upper respiratory tract), Common (≥1 and <10%) nausea, oropharyngeal pain, tinea infections, grade 1 or 2 neutropenia, rhinitis, conjunctivitis, influenza, oral candidiasis and inflammatory bowel disease. DOSAGE AND ADMINISTRATION – Dosage: Plaque Psoriasis: two 80 mg by subcutaneous injection at Week 0, followed by one 80 mg injection every 2 weeks at Weeks 2, 4, 6, 8, 10 and 12, then one 80 mg injection every 4 weeks. Psoriatic Arthritis: two 80 mg by subcutaneous injection at Week 0, followed by one 80 mg injection every 4 weeks. Axial spondyloarthritis (radiographic and non-radiographic): 80 mg by subcutaneous injection every 4 weeks. Elderly Patients (≥65 years): dose adjustment not required. Renal Impairment or Hepatic Impairment: no dosage recommendations. Administration: subcutaneous injection, avoid area showing psoriasis if possible. Single-use in one patient only. TALTZ contains no antimicrobial preservative, discard any residue product. Based on PI last amended 06 July 2021
References: 1. Gossec L et al. Ann Rheum Dis 2020;79:700–12. 2. Mease PJ et al. Ann Rheum Dis 2020;79:123–31. 3. Smolen J et al. Ann Rheum Dis 2020;79:1310–9. 4. Chandran V et al. Rheumatology (Oxford) 2020;59:2774–84. 5. TALTZ® (ixekizumab) Approved Product Information, 06 July 2021. 6. Mease PJ et al. Ann Rheum Dis 2017;76:79–87.
ACR: American College of Rheumatology Response Criteria; BSA: Body Surface Area; cDMARD: Conventional Disease-modifying Antirheumatic Drug; IL-17A: Interleukin-17A; IR: Inadequate Responders; NRI: Non-responder Imputation; PASI: Psoriasis Area and Severity Index; PsA: Psoriatic Arthritis; PsO: Psoriasis; Q2W: every 2 weeks; Q4W: every 4 weeks; r-axSpA: Radiographic Ankylosing Spondyloarthritis. TALTZ® is a registered trademark of Eli Lilly and Company. Eli Lilly Australia Pty Ltd. 112 Wharf Road, West Ryde NSW 2114, Australia. ABN 39 000 233 992.



Outcomes in systemic lupus erythematosus (SLE, or ‘lupus’) are “unacceptable”, said Professor Eric Morand, speaking during an Eli Lilly-sponsored symposium on janus kinase (JAK) inhibitors at the 2021 APLAR conference. In addition, Prof. Moran noted that “there have been some hurdles” in terms of treatment advances for lupus, and getting treatments for this disease to the same level as those in other rheumatology indications.
 Professor Eric Morand
Professor Eric Morand
There are several reasons why effective and safe treatments for SLE are important. One is the substantial negative impact that the disease has on patient quality of life. The second is organ damage, which is both “inexorable” and clinically meaningful, and is associated with increased mortality.
Speaking of mortality, there has been no improvements in mortality rates for patients with SLE over recent decades. This contrasts with the progressive
reductions in mortality seen in patients with rheumatoid arthritis as advances in therapy have been implemented in clinical practice.
Prof. Morand described the lack of new breakthrough therapies for lupus as “a drought”. In fact, the majority of the most common therapies (such as corticosteroids and immunosuppressants) have been used for up to 70 years.
Referring to the lack of new therapies, Prof. Moran highlighted two main problems. The first relates to the choice of endpoints in clinical trials of SLE treatments, which has been termed a “crisis” in the field. The second is that SLE biology is both complicated and heterogeneous. The disease also shows a lot of heterogeneity in clinical presentation.
Prof. Morand noted that it is difficult to understand the pathology of lupus. “It’s complicated, but I think it’s solvable”, he said. The wide variety of presentations seen among patients with SLE suggests that individual targets might differ between patients. Therefore, a multi-targeted approach might be better.
JAK inhibitors have effects on multiple cytokines. “There is a lot of evidence” for involvement of the JAK-STAT pathway in the pathogenesis of SLE, Prof. Morand told delegates.
Therefore, perhaps JAK inhibitors can provide a multidirectional approach to the treatment of lupus and potentially circumvent the problem of biological heterogeneity between subgroups of patients with SLE. Targets of JAK inhibitors include type 1 interferon but also things like interleukin-6 and interleukin-21.
Biomarker data from phase 2 trials showed that the JAK inhibitor baricitinib decreased the expression of a number of genes that are increased in patients with SLE, mostly those induced by interferon. There was also a significant reduction in antidouble strand DNA with baricitinib, perhaps due to the multi-targeting action of JAK inhibitors. This may be an advantage compared to an agent that targets only, for example, interferon pathways.
From a clinical perspective, a phase 2 study of baricitinib in patients with active SLE using a novel endpoint (resolution of arthritis or rash) was positive, and a phase 3 trial is underway.
Safety is also very important for new treatments. Although there were higher rates of serious infections with higher baricitinib doses in the phase 2 study, the safety findings were described by Prof. Morand as “relatively encouraging”.
A phase I trial of tofacitinib has also been completed and published. “We are excited to see the further development of JAK inhibitors in this space”, said Prof. Morand.
He noted that “the word is out” about JAK inhibitors in lupus, and early clinical trial data with JAK inhibitors are supported by a number of case reports of SLE patients treated off-label with these agents.
In conclusion, Prof. Morand stressed the need to develop and approve better therapies for SLE. “We have to do better”, he said.
*55% of TREMFYA patients with ACR50 at Week 100†1,2
*90% of TREMFYA patients remained on TREMFYA at Week 100†1,2

†Bionaïve 8-weekly dose PsA patients (N=248)1,2
PBS Information: Authority Required. Refer to PBS Schedule for full details. Product Information is available from www.janssen.com.au/TREMFYA_PI
ACR50, American College of Rheumatology 50% improvement; PsA, psoriatic arthritis.
References: 1. McInnes IB, et al. Arthritis Rheumatol. 2021; 73(4): 604 -616. 2. McInnes IB, et al. Efficacy and safety of guselkumab, a monoclonal antibody specific to the p19-subunit of interleukin-23, through 2 years: Results from a phase 3, randomized, double blind, placebo-controlled study conducted in biologic-naïve patients with active psoriatic arthritis. Poster presented at Innovations in Dermatology 2021; Virtual; March 16 -20, 2021 3. Pharmaceutical Benefits Scheme www.pbs.gov.au (accessed August 2021) ©Janssen 2021. ®Registered trademark of Janssen-Cilag Pty Ltd. ABN 47 000 129 975. 1–5 Khartoum Road, Macquarie Park NSW 2113. Telephone 1800 226 334. CP-254190. McCann Health. JATR22807Mc. August 2021.



According to Professor Kevin Winthrop, “we worry about JAK inhibition in viral infections”. Speaking at a symposium on janus kinase (JAK) inhibitors at the 2021 APLAR conference sponsored by Eli Lilly, Prof. Winthrop noted that there is a clear signal for reactivation of latent viral infections in patients being treated with janus kinase (JAK) inhibitors, but less is known about the risk of new infection with other viruses such as SARS-CoV-2.

Based on the mechanisms of action of JAK inhibitors, these agents could theoretically increase the risk of new viral infection because they interfere with signalling of both type 1 interferons and interferon-gamma, which are known to be very important in antiviral host responses.
Research conducted since the start of the pandemic indicates that some medicines used by rheumatology patients might pose a risk but that some may protect against severe COVID-19 disease. Therefore, it has been an open question for some time whether JAK inhibitors increase the risk of severe COVID-19.
The latest data showed a statistically significant doubling of the risk of mechanical ventilation requirement or death in COVID-19 patients whose rheumatoid arthritis was treated with JAK inhibitors versus tumour necrosis factor blockers. However, Prof. Winthrop noted that TNF blockers may protect against severe COVID19, meaning that using this group of agents as the reference might make other treatments look more harmful than they really are.
Of currently available JAK inhibitors, there is some evidence that baricitinib might be unique due to its ability to both reduce inflammation (similar to all other JAK inhibitors) and to diminish AP2-associated protein kinase (AAK1). The latter would diminish binding of the SARS-CoV-2 virus to the ACE2 receptor, which is

“Clearly baricitinib has a role in the management of these individuals”
how it gains entry into cells. Prof. Winthrop suggested that baricitinib might therefore have antiviral as well as anti-inflammatory effects.
This raises the question of how to manage patients hospitalised with COVID-19. Prof. Winthrop noted that an anti-inflammatory approach (especially using dexamethasone, and, more recently, interleukin-6 inhibition) has certainly been shown to protect against poor outcomes in patients with very severe COVID-19.
Some of the best data available actually came from studies of baricitinib. “Clearly baricitinib has a role in the management of these
individuals”, said Prof. Winthrop.
The addition of baricitinib or placebo to remdesivir shortened time to clinical recovery and there was “a hint of a mortality benefit” in patients treated with baricitinib versus placebo in a NIH trial.
More recently, a study showed that adding baricitinib versus placebo dexamethasone not only significantly reduced mortality but was also safe, with similar rates of serious infection and venous thromboembolism in patients treated with baricitinib versus placebo.
Prof. Winthrop said that this data “really put baricitinib on the map as standard of care for certain individuals in the hospital with COVID”.
To finish his presentation, Prof. Winthrop touched on the use of COVID-19 vaccines in patients being treated with JAK inhibitors. This group do
appear to have slightly lower immune response to COVID-19 vaccines compared with control patients. However, this needs to be studied further. Furthermore, the clinical consequences of this smaller quantitative response to COVID-19 vaccination are not yet known – it’s possible that a slightly diminished antibody titre after vaccination in patients treated with JAK inhibitors might not make any difference clinically, but this needs to be studied further.
“We have a lot of work to do” concluded Prof. Winthrop. “The pandemic has been a whirlwind. The role and risk of JAK inhibitors is still being elucidated, but I am very excited about their therapeutic potential against COVID-19”.


Together we have treated >362,000 * patients in 90 countries with XELJANZ4
* Real-world experience as of October 2020 in patients with RA, PsA and UC.
With a continuous safety profile to:
• 9.5 years in RA1
• 4 years in PsA5
• 4.4 years in UC6
PBS Information: Authority required for the treatment of adults with severe active rheumatoid arthritis and for adults with severe active psoriatic arthritis. Refer to the PBS Schedule for full authority information. This product is not listed on the PBS for ulcerative colitis.
Before prescribing, please review full Product Information available from https://www.pfizer.com.au/products
This medicinal product is subject to additional monitoring in Australia. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse events at www.tga.gov.au/reporting-problems.
XELJANZ® (tofacitinib (as citrate), 5 mg and 10 mg) Film-coated tablets. Therapeutic Indications: Adults – moderate to severe active rheumatoid arthritis (RA) (use alone or in combination with conventional synthetic DMARDs [csDMARDs]); active psoriatic arthritis (PsA) (use in combination with csDMARDs); moderate to severe active ulcerative colitis (UC). Contraindications: Hypersensitivity to tofacitinib citrate or to any of the excipients; concomitant biological agents or other potent immunosuppressive agents; severe hepatic impairment. Special Warnings and Precautions For Use: Mortality; thrombosis; specialist physicians with expertise in management of conditions for which XELJANZ is indicated should intitate and monitor therapy (e.g. rheumatologist or gastroenterologist); monotherapy not studied in PsA patients; serious infections including pneumonia, cellulitis, herpes zoster, urinary tract infection, diverticulitis and appendicitis; other bacterial, mycobacterial, invasive fungal and opportunistic infections, including tuberculosis, cryptococcus, oesophageal candidiasis, pneumocystosis, multidermatomal herpes zoster, cytomegalovirus and BK virus infections (see PI for others); viral reactivation; malignancy and lymphoproliferative disorder; non-melanoma and melanoma skin cancer (dose-dependent adverse reactions seen in patients treated with XELJANZ 10 mg twice daily compared to 5 mg twice daily include herpes zoster infections, serious infections, non-melanoma skin cancer, higher rate of all-cause mortality and thrombosis; in UC long-term extension study, malignancies were observed more often in patients treated with XELJANZ 10 mg twice daily compared with 5 mg); cardiovascular; gastrointestinal perforations; hypersensitivity; live vaccinations; chronic and interstitial lung disease; renal transplant patients; Asian patients; pregnancy (Category D), contraception; lactation; elderly; diabetic patients; renal or hepatic impairment; lymphopenia; neutropenia; low haemoglobin; dose-dependent hyperlipidaemia; liver enzyme elevations. See PI for details. Interactions With Other Medicines and Other Forms of Interactions: Increased exposure with CYP3A4 inhibitors (e.g., ketoconazole) and potent CYP2C19 inhibitors (e.g., fluconazole). Decreased exposure with CYP3A4 inducers (e.g. rifampicin). Use caution with medicines that lower heart rate and/ or prolong the PR interval. Higher incidence of adverse events in combination with methotrexate versus XELJANZ alone. Use in combination with phosphodiesterase 4 inhibitors not studied. See PI for details. Adverse Effects (Undesirable Effects): Common: upper respiratory tract infections, nasopharyngitis, pneumonia, influenza, herpes zoster, sinusitis, pharyngitis, urinary tract infections, bronchitis, anaemia, headache, dizziness, hypertension, diarrhoea, nausea, dyspepsia, abdominal pain, vomiting, constipation, gastritis, gastroenteritis, rash, rheumatoid arthritis, arthralgia, fatigue, peripheral oedema, pyrexia, Gamma glutamyltransferase increased, blood cholesterol increased, weight increased, blood creatine phosphokinase increased, hyperlipidaemia, cough. See PI for details. Dose and Method of Administration: RA – 5 mg twice daily as monotherapy or in combination with methotrexate or other csDMARDs; PsA – 5 mg twice daily in combination with csDMARDs; UC – 10 mg twice daily for induction for 8 weeks and 5 mg twice daily for maintenance. Dose modifications. XELJANZ 10 mg twice daily not recommended for treatment of RA or PsA. See PI for details. Before prescribing, please review Product Information available from Pfizer Australia Pty Ltd. ®Registered trademark. V10919.
Abbreviations: JAK, Janus kinase; PsA, psoriatic arthritis; RA, rheumatoid arthritis; UC, ulcerative colitis.
References: 1. Wollenhaupt J, et al. Arthritis Res Ther 2019; 21: 89. 2. Bird P, et al. Clin Rheumatol 2020; 39: 2545–51. 3. XELJANZ® Approved Product Information. 4. Pfizer Inc. Data on file: Internal calculations by Pfizer based on IQVIA Database. 5. Nash P, et al. Rheumatol Ther 2020; 7: 553–580. 6. Sandborn WJ, et al. Clin Gastroenterol Hepatol 2019; 17: 1541–50.
Pfizer Australia Pty Ltd, Sydney, Australia. Medical Information: 1800 675 229. PP-XEL-AUS-0698. PFI4577. 05/21.


Over the period from 1980 to 2015, patients from Western Australia (WA) who had rheumatoid arthritis (RA) were 2.5 times more likely to die than individuals from the general population. Interestingly, if the analysis was restricted to the last 5 years of data (2011–2015), the magnitude of elevated age-adjusted mortality risk in patients with RA was reduced, at only 1.5 times higher than that in the general population.
These findings were presented by PhD student Khalid Almutairi during an oral abstract session of the APLAR 2021 meeting. The research, funded by the Arthritis Foundation of WA as part of the Western Australian Rheumatic Disease Epidemiological Registry, included more than 17,000 patients with a confirmed diagnosis of RA.
The study linked populationlevel statistics from a variety of WA health administration dataset sources, including hospital morbidity figures, emergency department data, and death registry information. Mortality rate ratios were
calculated using a direct age standardisation method.
Throughout the study, the leading cause of death in patients with RA was cardiovascular disease, which was responsible for more than a quarter of all deaths in these patients. This was followed by cancer (which was the cause of death in 17% of patients), while <6% of RA patients each died from rheumatic diseases, chronic obstructive pulmonary disease, dementia and diabetes.
Another focus of the study was on the presence of comorbidities in patients with RA, and how these might relate to inhospital mortality. The prevalence of
comorbidity (based on the Charlson Comorbidity Index) decreased over time from 2001 onwards, and especially between 2011 and 2015. Over the same period there was a corresponding reduction in mortality in patients with RA.
The decline in mortality seen after 2001 coincides with the introduction of biologic therapies for RA, and therefore is likely to reflect improvements in the management of RA. In addition, better management of comorbidities in more recent time periods probably contributed to the reduction in comorbidity burden in patients with RA that was seen from the start of the new millennium.
While it is encouraging to see these improvements in excess mortality for patients with RA, this group remain 1.5 times more likely to die than their counterparts in the community. Therefore, as stated by Khalid Almutair, “there is room to achieve further improvements”.
This study reminds us as clinicians that there is room for us to optimise “(CVD)” risk factors in our patients with rheumatoid arthritis, with assistance from our primary health colleagues CVD risk factors should be emphasised in routine care.


Inspiring a generation of young women to take up the challenge in science, technology, engineering and math (stem education)
From US President to classroom chatter it seems like everyone is talking about the opportunities that STEM programmes offer young women today and how vital they are to the future empowerment of women but also to the future of Australia.
The Australian Government’s strategy for women in science, technology, engineering and mathematics (STEM) aims to increase gender equity in STEM education and careers.
Professor Catherine Hill, President of the Australian Rheumatology Association (ARA), is pioneering how the speciality of rheumatology is improving clinical practice and research, contributing to decision-making in drug regulation, and providing mentorship, serving as a role model for young women.
As the President of ARA, Professor Hill aims to lead the small but mighty association to improve access to high quality rheumatology care for all Australians — including those in rural areas and paediatric populations, increase training opportunities for rheumatology trainees, and enhance research opportunities for ARA members. Let’s see what makes her tick!
Professor Hill discovered her
passion for rheumatology when she worked as a Resident Medical Officer at the Repatriation General Hospital with Professor Michael Ahern and Professor Malcolm Smith. Like many physicians at the start of their careers Catherine found support and mentorship from her colleagues — Dr David Henderson, Dr Kevin Pile, and Professor Les Cleland. Although she was exposed to a broad range of complex diseases, it was musculoskeletal diseases that caught her imagination attention.
Being drawn to the discipline of epidemiology, Professor Hill won the AFA-Heald scholarship in 1998, which gave her the opportunity to study and undertake research at Boston University with Professor David Felson. This represented one of her greatest career highlights. The skills developed after obtaining a Master of Science in epidemiology and biostatistics, lead to her subsequent research career in rheumatologic diseases, including vasculitis, gout, and osteoarthritis.
It was the result of having many supportive mentors along her journey that helped shape Professor Hill and her career. Recognising the importance of mentorship, she is passionate about providing supervision and training for rheumatology trainees and PhD students so that they too can grow just as she did.
A little known yet common vasculitis condition affecting Caucasian women, most commonly between the ages of 70 and 80 years, giant cell arteritis (also known as temporal arteritis), received little attention until relatively recently. Under Professor Hill’s leadership she established the South Australian Giant Cell Arteritis Registry in 2009. The registry collected the data necessary to advance the knowledge about giant cell arteritis for the very first time in Australia.
Extending her experience in rheumatology and epidemiology, Professor Hill took on the role of Chief Investigator of the North West Adelaide Health Study (NWAHS). This study aimed to gather data to assist in optimising strategies for the prevention, early detection, and management of a broad range of chronic conditions. As the Chief Investigator, Professor Hill played a critical role in the collection of data on musculoskeletal disorders. Work from the NWAHS was published as part of the Global Burden of Disease 2012 study, which recognised musculoskeletal diseases as one of the three most important diseases in terms of global disease burden.
Locally and internationally, Professor Hill has played a pivotal role in creating awareness for musculoskeletal diseases through the combination of her rheumatological and epidemiological expertise
Locally and internationally, Professor Hill has played a pivotal role in creating awareness for musculoskeletal diseases through the combination of her rheumatological and epidemiological expertise.
Improving patient accessibility to medications
In addition to rheumatology and epidemiology, one of Professor Hill’s professional interests is drug regulation. She has been involved in numerous associations including the Australian Committee for Prescription Medicine of TGA and the Drug Utilisation Sub Committee. Currently, she is a member of the Pharmaceutical Benefits Advisory Committee involved in the decision-making for listing medications on the PBS. Additionally, she is the Chair of the South Australian Medicines Evaluation Panel, which reviews the use of high-cost medicines and monitors compliance of their use in all public hospitals.
Overall, Professor Hill carries a phenomenal amount of experience in rheumatology, epidemiology, and drug regulation. With several leadership roles, she is an inspirational figure empowering the next generation of women, bringing us closer to bridging the gender gap in science, technology, engineering and mathematics.

Jonathan Smithers, newly appointed CEO of Arthritis Australia, is leading the way when it comes to operating and implementing disease awareness and consumer education strategies in peak medical bodies. In this exclusive interview, we gain insight into how Arthritis Australia is breaking down unnecessary barriers and overcoming challenges in the arthritis sphere.
An estimated 1 in 7 Australians have arthritis, this proportion of 3.6 million is projected to rise to 5.4 million by 2030.1,2 With “over 100 different types of lived experience of arthritis” affecting people of all ages, it is the leading cause of chronic pain and second leading cause of overall disease burden, further leading to early retirement and economic strains on those affected.1-3
The most common form of arthritis in Australia is osteoarthritis followed by rheumatoid arthritis,1 for which treatment approaches and access to support services can depend on location. ‘’Geography is important here. Significant parts of the population live in rural and remote areas, so not everybody has equal access to the health services they need,” comments Mr Smithers. ‘’Arthritis Australia
consistently makes the case for greater provision of services across the whole country.”
Arthritis Australia advocates for, receives and distributes federal grants to its affiliated state and territory organisations (e.g., Arthritis ACT/NSW/NT/QLD/ SA/TAS/WA) which deliver direct programs to consumers. An example of this action can be seen through the $1 million ‘Better Ageing’ grant, which facilitated the provision of group exercise classes to senior Australians and the $4 million National Strategic Action plan funding towards arthritis awareness, prevention, education, and patient-centred care and support, including to indigenous communities.4
“The consumer perspective drives our strategy”, says Mr Smithers. This is backed by their Consumer Advisory Panel comprised of consumers with a diverse range of arthritis-related conditions from each state and territory. Sitting alongside is the Scientific Advisory Panel, with representation from a wide range of senior clinicians and allied health professionals. These panels are designed to give the best range of advice to the Board to ensure resources are spent wisely. ‘’We also have close ties with external medical bodies, particularly the Australian Rheumatology Association, collaborating to improve consumer health outcomes.”
“The more knowledge consumers have about their conditions, the better able they are to manage them. This should lead to greater confidence and will also assist their doctors as in diagnosis and management of their conditions.”
How is Arthritis Australia engaging with consumers?
Aiming to be “the pathway for best information”, Arthritis Australia provides a wide range of consumer resources from online information sheets to hardcopy booklets catered towards a variety of arthritis types (Box 1). With COVID-19 leading to potential shortages in biologic pharmaceuticals, a current focus has been to ease concern amongst patients with rheumatoid arthritis by reiterating advice for patients to consult their doctors as soon as possible to discuss medication options (Box 1).
Staying on the forefront of technology, Arthritis Australia has been pivoting towards digitalbased resources to increase its reach and engagement with consumers. To this point, there are currently 5 active websites with a sixth in development (Box 1). Each one has been designed specifically to a different
arthritis type. The websites allow consumers to record and rate their symptoms and track their disease progression (see 16-17 in this issue for more information on MyRA). 5
The user-friendly dashboard allows patients to learn more about their condition, make adjustments to their lifestyle to help alleviate symptoms, as well as better communicate their experience with their rheumatologists.
Further implementations of a consumer-focused strategy – How is Arthritis Australia looking beyond supplying educational resources?
When people think of arthritis, they will often conjure an image of an elderly person. This simply isn’t the case as Mr Smithers puts, “it could be anybody, at any age – arthritis does not discriminate. There are more than 100 different arthritis conditions with differing levels of discomfort and disability, and many Australians are living with multiple types at the same time.”
Australia has a limited cohort of paediatric rheumatologists, despite the high demand from the >6,000 children with juvenile idiopathic arthritis.6,7 The impact of living with the condition can be quite profound for both the child and their family, leading to withdrawal from social circles.8,9 Arthritis Australia is combatting this key issue, working with the Australian Paediatric Rheumatology Group, with a paediatric rheumatology scholarship and although the process is “frustratingly slow when there is a current pressing need,” says Mr Smithers. “On the positive side however, it is a practical way to help paediatricians upskill to have a health system that meets medical demand in the future.”
Arthritis Australia continues to put in the hard yards with their Accessible Design Division, which Mr Smithers describes as “a very interesting part of our work is it facilitates meaningful solutions to common accessibility problems”.
The Division is headed by Senior Technical & Design Lead Alexandra Brayshaw, with scientific guidance from Dr Brad Fain (Principal Research Scientist at the Georgia Tech Research Institute), and is focused on improving the design of general goods and pharmaceutical products to be more accessible, along with educating and gaining procurement amongst industries and government.
This year, ‘Voltaren Osteo Gel 12 Hourly’, launched with a new ‘easy to open’ butterfly cap, which was the first therapeutic product to receive an accessibility certification from the Division. This has driven a collaborative effort through the formation of the Accessible Product Design Alliance, joining together the

forces of not-for-profit consumer health organisations: MS Australia, MND Australia and Cerebal Palsy Alliance, just to name a few. Read more about the Division here: arthritisaustralia.com.au/
The backbone of Arthritis Australia and its founding reason supported by their mission statement “freedom from arthritis”, is their research program. A significant proportion of their funds is dedicated for grants and scholarships as a way towards curing disease including translational research to alleviate difficulties which consumers have now. However, in a crowded and fragmented space where there is never enough money to go around, obtaining funding from governments and benevolent institutions is a common challenge. By teaming up on a new project with Research Australia to create a National Strategy for Research, Arthritis Australia is looking forward to coordinate strategic objectives with a strong consumer perspective to improve outcomes.
In summing up, Mr Smithers remarked, “to deliver great outcomes for consumers it is vital to have a fully functional professional and disciplined organisation“. For itself and with other organisations, Arthritis Australia is helping to relieve the impact of arthritis. Mr Smithers is executing the organisational strategy to help consumers with arthritis in Australia and is showing impressive strides with great future prospective. Arthritis Australia is an organisation truly about “empowering people with knowledge. The more knowledge consumers have about their conditions, the better able they are to manage them. This should lead to greater confidence and will also assist their doctors as in diagnosis and management of their conditions.”
BOX 1: RESOURCES FOR PATIENTS AND DOCTORS FROM ARTHRITIS AUSTRALIA
ARTHRITIS AUSTRALIA ONLINE RESOURCES
Information sheets (available in 15 languages) arthritisaustralia. com.au/get-support/resources/information-sheets
Booklets arthritisaustralia.com.au/get-support/resources/ booklets
Videos arthritisaustralia.com.au/get-support/resources/videos
Exercise videos arthritisaustralia.com.au/get-support/resources/ working-out-with-michael-slater COVID-19 arthritisaustralia.com.au/managing-arthritis/covid19
INTERACTIVE WEBSITES
MyJointPain myjointpain.org.au
MyBackPain mybackpain.org.au
MyRA (rheumatoid arthritis) myra.org.au
Empowered (hear stories and expert opinions on rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and nonradiographic axial spondylarthritis) empowered.org.au
MyPsA (psoriatic arthritis, launched August 2021) mypsoriaticarthritis.org.au
MyAS (ankylosing spondylitis) under development
The value of these websites has been made particularly clear in the remote communities of Australia where access to face-to-face programs led by state and territory-based organisations are often limited
References 1.
2. Ackerman IN, Bohensky MA, Pratt C, et al. 2016. Counting the Cost: the current and future burden of arthritis. Arthritis Australia.
3. Arthritis Australia. Fast Facts. arthritisaustralia.com.au/what-is-arthritis/fastfacts
4. Arthritis Australia. $5 million in government funding committed for arthritis initiatives, inc Action Plan and Better ageing grant. arthritisaustralia.com.au/5-million-in-government-funding-committed-forarthritis-initiatives-inc-action-plan-and-better-ageing-grant
5. Arthritis Australia. Our Websites. arthritisaustralia.com.au/get-support/our-websites
6. Australian Rheumatology Association. Paediatric Rheumatology. rheumatology.org.au/patients/search-results-area-of-interest. asp?AoI=Paediatric+Rheumatology&RoC=A&submit2=Find+A+Rheumatologist
7. Arthritis Australia. Children and Arthritis. arthritisaustralia.com.au/managing-arthritis/arthritis-andchildren
8. Lundberg V, Lindh V, Eriksson C et al. 2012. Health-related quality of life in girls and boys with juvenile idiopathic arthritis: self and parent reports in cross-sectional study. Pediatric Rheumatology 10:33–40.
9. Bouaddi I, Rostom S, Badri DE et al. 2013. Impact of juvenile idiopathic arthritis on schooling. BMC Pediatrics 13: doi:10.1186/1471-2431-13-2.
7. Arthritis Australia. Children and Arthritis. arthritisaustralia.com.au/managing-arthritis/arthritis-andchildren
8. Lundberg V, Lindh V, Eriksson C et al. 2012. Health-related quality of life in girls and boys with juvenile idiopathic arthritis: self and parent reports in cross-sectional study. Pediatric Rheumatology 10:33–40.
9. Bouaddi I, Rostom S, Badri DE et al. 2013. Impact of juvenile idiopathic arthritis on schooling. BMC Pediatrics 13: doi:10.1186/1471-2431-13-2.
“Given the importance of supporting mental health and wellbeing in RA, the program also provides a touchpoint to assess emotions and feelings of stress, fatigue, anxiety, and depression”


Introducing MyRA, an online rheumatoid arthritis (RA) support program for patients, delivered by Arthritis Australia, to allow people to selfmanage and take ownership of their disease journey. Recognising that everyone’s RA is different, and patients’ information needs vary over time based on fluctuating disease status, the idea of developing an evidence-based resource that better aligns with this reality of living with RA, was born. Staying true to the patient experience, MyRA (myra.org.au) was launched last year with more than 1600 patients currently registered. Built with support from the Australian Rheumatology Association and industry partners – MyRA is designed to be an accessible, interactive, and an informative resource for those referred into the program. Read on to find out more about this program, how your patients can access it and what we have learnt about RA patients during the process of developing this support resource.

an understanding of the different healthcare professionals that they may encounter along the way. There is plenty of practical advice on how to live with arthritis: from tips on healthy eating, exercise, rest and sleep to how to care for joints and manage pain, as well as simple measures to adapt the home environment to be more comfortable.
What can patients expect from the program?
Comprehensive information on RA including causes and diagnosis as well as exploring its impact on the patient, their family, carers and friends. Patients may also want to know what their future looks like living with a chronic condition and may want to seek reassurance. Given that much of Australia is currently grappling with COVID-19 and navigating stay-at-home orders, social restrictions and lockdowns, access to clinical and support services may be a challenge. The website includes a COVID-19 FAQ section that helps to address the many common concerns likely related to treatment at this time.
Registered patients can also access information related to tests, treatment options, and gain
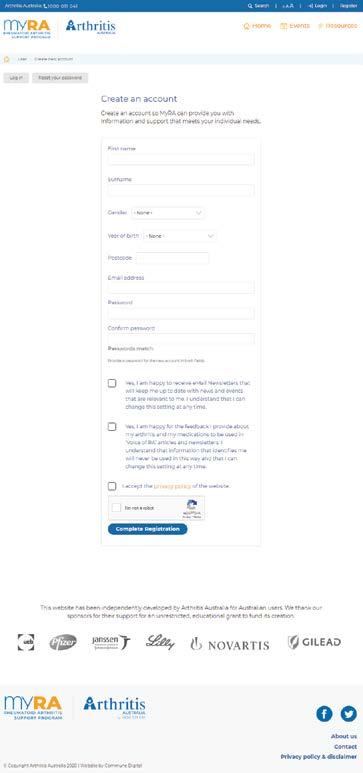
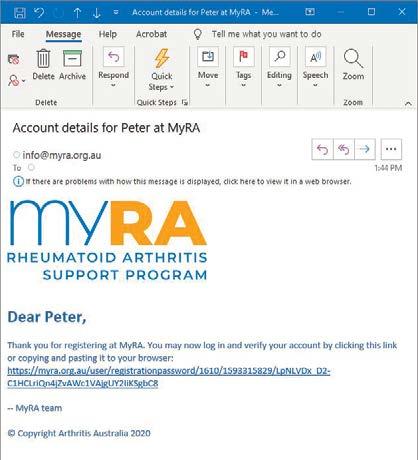
How can patients register?
There are two ways to sign up to the program. The patient can go via the ‘Register’ prompt or through the self-assessment activity on the homepage. Both navigate to the ‘Create an account’ page. Once the form is completed, an email will be sent to confirm their registration.
Given the importance of supporting mental health and wellbeing in RA, the program also provides a touchpoint to assess emotions and feelings of stress, fatigue, anxiety, and depression and allows the patient to understand when they should see a doctor. Details of support networks and services are also provided.
What evidence helped shape this program?
In order to identify the most appropriate information sources to include in this program, the established Education Needs Assessment Tool (ENAT) was used to inform the ENAT survey, a patient-based online survey that was completed by people diagnosed with arthritis (n=852).
Using a Likert scale of 1 to 5 (1 was considered not at all important and 5 was considered extremely important), survey participants were asked to rate the importance of seven key

themes that included disease understanding, treatments (prescribed and self-selected), pain management, movement, feelings and support. The survey also revealed that information needs vary over time based on disease/symptom severity. This exercise also explored the role of health literacy, empowerment and relationships with healthcare professionals and their impact on behaviour and outcomes. Three survey questions were developed to provide insights into these patients. ‘Confidence with forms’, represented a measure of health literacy, ‘Confidence in ability,’ provided an indication of empowerment and ‘Confidence in doctor’, reflected the relationship with the doctor. Figure 1 shows a significant gap in confidence in managing arthritis with only half of respondents feeling ‘extremely’ or ‘quite a bit’ confident. Similarly, approximately half of the respondents felt confident that they were receiving the best advice from their doctor. Most felt confident in completing medical forms.
To explore the program and see how it could help support your patients with rheumatoid arthritis, visit: myra.org.au
Extremely
Quite a bit
Somewhat
A little bit
Not at all
0
Extremely
Quite a bit
Somewhat
A little bit
Not at all
Extremely
Quite a bit
Somewhat
A little bit
Not at all