TheVeterinarian



Results of a study published recently in the journal Animal Behaviour, that focused on a group of captive greylag geese, found strong pair bonds between the parent birds produced better breeding results.
Lead author Lauren Common, a Flinders University PhD candidate now based at the University of Vienna’s Konrad Lorenz Research Centre for Behaviour and Cognition, said the personality of both parents, and their similarity in personality traits, can influence their parental success, just as it can in humans.
“Successful pair bonds where partners were similar in their boldness, mainly by responding to risky situations in the same way, can have higher hatching success. Bold parenting style can lead to consistency and responsiveness, which can result in successful reproductive output and the survival of young and fledgeling success,” Common explained.
Greylag geese live in large flocks that include social pairing as well as singles and trios and the birds form long-term monogamous bonds often only broken by the death of one partner.
The study involved 118 geese that were monitored over three breeding seasons where their reproductive and fledgling success was measured.
Co-author Sonia Kleindorfer, a professor and organismal systems biologist at the University of Vienna, and the founder of Flinders University’s BirdLab in the College of Science and Engineering Department, said the coordination of a united
Taronga Western Plains Zoo is celebrating a significant arrival ahead of World Rhino Day with the birth of a southern black rhinoceros calf. Born to first-time mother Mesi on August 24, this healthy male calf brings hope to conservation efforts for this critically endangered species.
The calf’s arrival occurred late at night in the zoo’s black rhinoceros breeding area, where keepers had been closely monitoring Mesi in anticipation of the birth. Despite her initial cautiousness, Mesi quickly adapted to her new role as a mother.
“Mesi gave birth overnight in a behind-the-scenes breeding area within our Black Rhinoceros complex,” black rhino keeper Grace Humphery said. “Being a first-time mum, Mesi took a little bit of time to bond with her calf following his birth. However, within 24 hours she had moved into mum mode, which was great to see.”
Now, Mesi and her newborn calf are inseparable, with the little one meeting all his key developmental milestones.
male and female couple was crucial during incubation when thermal stability and protection from predators was crucial.
“In species with biparental care and monogamy, reproductive output and success may be influenced not only by the personality of each individual but also the behavioural compatibility of the pair. This kind of pairing in greylag geese is linked to their welldeveloped cognitive capacity and social awareness, and individuals consistently differ in personality traits such as boldness, aggressiveness, sociability and other behavioural traits,” Kleindorfer said. To page 30

Mesi’s calf will be an essential part of Taronga Western Plains Zoo's conservation program and serve as an ambassador for his species. The zoo plays a crucial role in the global effort to save Black Rhinos from extinction, as it is the only institution outside of Africa that successfully breeds the southern black rhinoceros.
The calf will stay behindthe-scenes for the next few months, bonding with his mother and familiarizing himself with his keepers --a process crucial for his future health and well-being as he grows into an adult weighing up to 1,300kg.
While celebrating this new life, the zoo also faced a heartbreaking moment with the stillbirth of a calf from another Black Rhino, Bakhita. Bakhita is being closely monitored to ensure her recovery, underscoring the critical need for conservation programs where every birth is a victory for the species.
Taronga Western Plains Zoo is not just a breeding ground for endangered species; it’s also a driving force in To Page 30
Researchers at the University of Adelaide have launched a new tool to help veterinarians and pet owners to manage heartworm infections.
The online dashboard processes near real-time temperature records across Australia, giving access to historical and current weather records, which can assist in determining the suitability for canine heartworm transmission in any Australian postcode.
Canine heartworm disease is caused by infection with a parasite called Dirofilaria immitis. These are nematodal parasites, the larvae of which require approximately six months to mature, during which they migrate from the peripheral bite site to the pulmonary arteries. A feeding mosquito can ingest microfilaria when feeding and transmit them to another dog. Signs of infection include coughing and exercise intolerance, which can progress to right-sided heart failure. To page 30
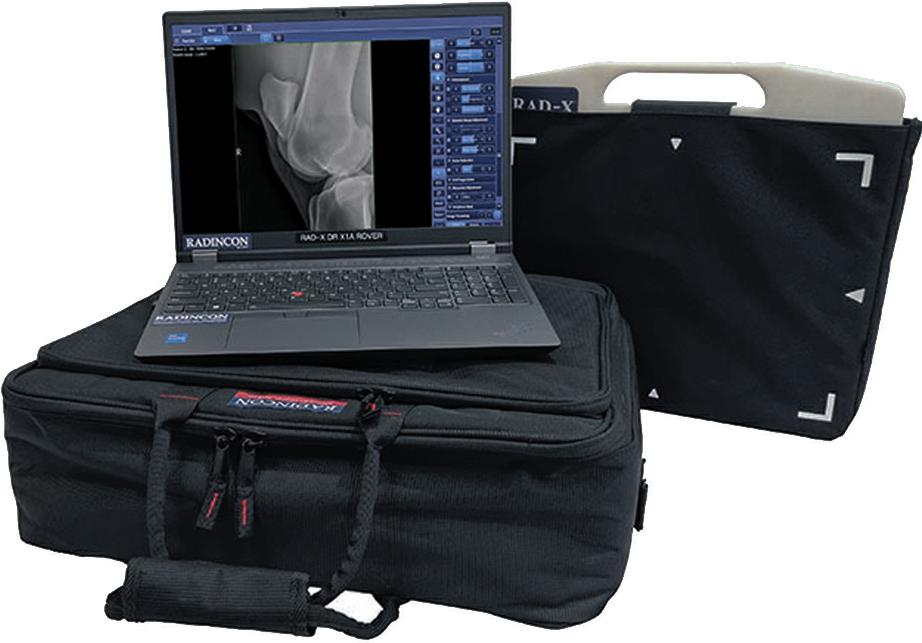
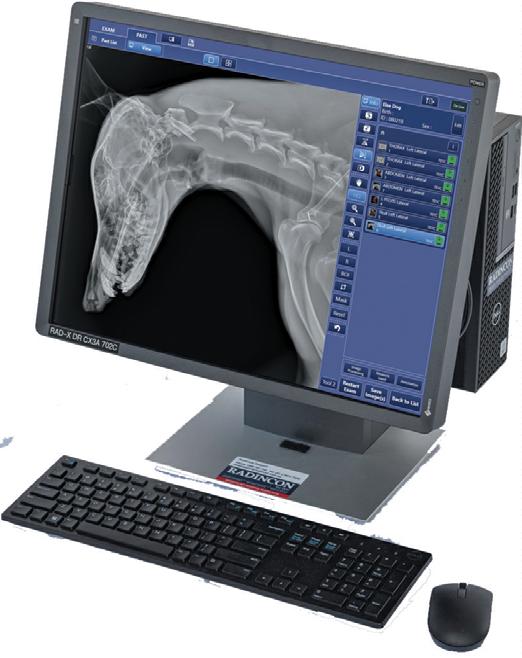
Through innovation, invention, and strategic partnerships with worldwide leaders in diagnostics, Heska provides the benefts of latest generation technologies to veterinary professionals. From our ever-growing and wide range of in-house lab and imaging solutions, to outstanding service and support, discover all the ways Heska helps you provide a voice for your patients.








The Australian Research Council awarded major funding grants recently to the University of Tasmania’s Menzies Institute of Medical Research. The grants will support further research into wildlife disease, the development ofavaccine to protect Tasmanian devils from the fatal facial tumour disease that has ravaged populations of the species in the wild for more than 25 years, and the viability of a control method to help reduce both rabbit and feral cat populations.
Lead researcher Andrew Flies, an Associate Professor at UTAS, and Principal Research Fellow: Immunology at MIMR, received grant funding for two areas of Tasmanian devil research in which he is involved. A $740,000 grant will enable further work on the development of an edible bait to vaccinate wild devils, that can then be used as a model for combatting other wildlife diseases.
Identified as two different transmissible cancers, DFT1 and DFT2 have resulted in the loss of around 68 per cent of populations of devils in the wild.
“The focus is on validating new vaccines specifically designed for marsupials, and this project has assembled a large national and international team of world class researchers and institutions to cover all the expertise and resources we need to determine if we can protect devils from DFT1 and DFT2. They include the Ceva Wildlife Research Fund, Bonorong Wildlife Sanctuary and Animal Control Technologies Australia,” Flies said.
An ARC Future Fellowship grant of $1,065,744 was also awarded to Flies for Be Prepared: Rapid Diagnostics and Field-Ready Vaccines for Wildlife, aproject that addresses wildlife diseases with a focus on developing rapid diagnostic tests and vaccines for the transmissible cancers that are affecting devils. The research also aims to enhance conservation efforts by developing

new tools to understand and prevent disease in other native species.
“Vaccines are among the most effective tools for managing human and domestic animal health, but few vaccines are available for wildlife. This project will translate biomedical technology into applied conservation tools to protect Australia’s iconic marsupials,” Flies said.
This project will also involve close collaboration with Bonorong Wildlife Hospital and Rescue Line to bring solutions to the field to help protect and conserve Tasmania’s wildlife.
ARC funding totalling $580,000 was awarded to Menna Jones, Professor in Biological Sciences
at UTAS School of Natural Sciences, for a project that will investigate the effectiveness of removing rabbit warrens as a method of controlling feral cat populations and restoring vegetation, soil and native animal populations. The research will include the creation of easy-to-follow and use simple and effective methods for the restoration of ecosystems that have experienced widespread environmental damage, as well as a decline in Australia’s native wildlife, caused by large numbers of introduced rabbits, and an increase in feral cat numbers.
■ ANNE LAYTON-BENNETT

On World Animal Day 2024, SPANA (the Society for the Protection of Animals Abroad) issued a call to world leaders to include working animals in the climate crisis discussions at the upcoming COP29 event in November. This year's World Animal Day theme, ‘The world is their home too’ highlights the often-overlooked impact of climate change on the animals that support vulnerable communities worldwide.
Working animals such as donkeys, horses, and camels, play a crucial role in rural communities, where they are used for transporting goods, fetching water,and supporting agricultural activities. However, the increasing frequency of extreme weather events, including heatwaves and floods, is pushing these animals and the communities they serve to their limits.
Linda Edwards, Chief Executive
of SPANA, emphasised the importance of these animals. “For communities like the Maasai, working animals are lifelines. When they’re lost or unable to work, daily life grinds to a halt. These animals are essential for reaching water, transporting goods, and sustaining the heartbeat of local economies,” Edwards said.
The ongoing crisis in Kenya’s Kajiado County,near the border with Tanzania, illustrates the dire situation faced by many working animals. Earlier this year, unprecedented flooding devastated the Maasai communities in Magadi and Shompole, leaving more than 4,400 donkeys without shelter or grazing land. These conditions exposed the animals to extreme weather and deadly diseases, creating a ripple effect that crippled the local economy and threatened the survival of the Maasai people.
With contaminated water sources becoming breeding grounds for parasites and limited access to veterinarycare, the crisis quickly escalated. In response, SPANA partnered with the African Network for Animal Welfare (ANAW) to deliver emergency veterinarycare and vaccinations to the affected animals, helping to stabilize the situation and build resilience against future climate-related disasters.
The plight of working animals in Kenya is not an isolated incident but part of a larger global crisis. The UN's One Health approach highlights the interconnectedness of human, animal, and environmental health, underscoring the need for collaborative solutions to address emerging threats. The health of these animals directly impacts the ecosystems and economies they support.
“With over 200 million working animals worldwide, SPANA’swork is essential in protecting these vital animals – the trucks, tractors, and taxis of rural communities," Edwards said. “Safeguarding and treating these animals isn’t just compassion – it’s essential to avoiding ecological and economic disaster.”
SPANA is urging world leaders to include the welfare of working animals in their discussions at COP29, emphasizing their importance to sustainability and the health of ecosystems. “When animals suffer, ecosystems collapse. That’s why SPANA is calling on world leaders to consider the protection and care of working animals in their COP29 discussions,” Edwards said.
To learn more about SPANA’s initiatives and how they are making a difference for working animals and the communities they support, visitwww.spana.org.




Taronga Western Plains Zoo has announced the birth of two more giraffe calves, adding to the growing 'tower' of giraffes at the zoo. Following the recent arrival of a male calf born to Mvita on August 23, two more calves have joined the herd, bringing the total to three new arrivals this season.
Asmara, another experienced mother at the zoo, gave birth to a healthy female calf on September 14. Just a few days later, on September 20, Zane welcomed a male calf into the herd. All three newborns are thriving, exploring their habitat, and even showing curiosity about their neighbours --the zebras in the adjacent exhibit.
The arrival of these calves marks another success for Taronga Western Plains Zoo’s long-standing giraffe breeding program, which has played a crucial role in regional conservation efforts. Since 1990, the zoo has welcomed 60giraffe calves, contributing to an insurance population for the species. This initiative is critical as giraffe numbers in the wild have
dropped by around 40 percent since the 1980s dueto threats such as poaching, habitat loss, human encroachment, disease, and civil unrest.
In addition to its breeding program, Taronga Western Plains Zoo partners with conservation organizations in Africa to support anti-poaching efforts and wildlife monitoring activities, further underscoring its dedication to protecting giraffes and other vulnerable species.
Taronga Western Plains Zoo’s efforts to safeguard giraffes are directly supported by its visitors. Every admission ticket, overnight stay, and purchase made at the zoo contributes to wildlife conservation, helping to fund essential programs that make a difference for species like giraffes.
With these new arrivals, Taronga Western Plains Zoo is eagerly anticipating the possibility of even more giraffe births as spring continues. The zoo’s breeding bull, Mtoto, has already played a key role in the success of this season's calf births, and the zoo remains hopeful that additional calves will soon join the herd.
On October 14 the Federal Government announced a $95 million package to support high pathogenicity avian influenza (HPAI) preparedness and response.
The rapid global spread of the H5N1 strain of HPAI has led to significant impacts in poultry,wild birds and some mammal species, including respiratory illness, reduction in egg production and sudden death, with Australia the only continent remaining free from free from the strain.
The new funding comes on top of $6.9 m allocation towards HPAI H5N1 preparedness and response announced in July this year, and $1b of biosecurity funding in the 2023 Budget.
The new funding includes $35.9m to support state and territory governments to boost preparedness planning for vulnerable species and places, and key conservation partners to improve protections for captive populations of threatened species.
$22.1m will be used to strengthen public health preparedness by increasing the number ofready-to-use pandemic flu vaccines in the National Medical Stockpile, though human infections with avian influenza viruses are rare.
Wildlife Health Australia will be allocated $7m to improve the early detection and reporting capacity of H5N1 by enhancing WHA’s surveillance activities and supporting global and national One Health outcomes.
WHA administers Australia’s national wildlife health systems and networks, working with partners such as zoos, vets and wildlife rehabilitators around Australia to identify emerging diseases in wildlife and provide data to improve management of disease outbreaks. To page 30

Are you a vet nurse looking to take your career to the next level or explore a new path? We provide an environment where vet nurses can thrive, supported by state-of-the-art facilities, growth opportunities and a collaborative team where everyone is valued equally.
Australia’s Largest Specialty & Emergency Network
Over 1200 dedicated team members and 24 locations nationwide
Australia’s Largest Specialty & Emergency Network
Join our veterinary professionals in felds such as Emergency, Medicine, Oncology, Cardiology, Neurology, Surgery and more. Our centres are equipped with advanced diagnostic tools including MRI, CT and on-site pathology.
Over 1200 dedicated team members and 24 locations nationwide
With locations across NSW, VIC, QLD, SA, WA and the ACT, we partner with local practices to deliver care for specialist cases and emergencies.
As part of our team, you’ll also beneft from the support of our Vet Nurse Advisory Panel—a dynamic group of nurses from both general practice, emergency and specialty areas. This panel drives innovation in pet wellness, market trends, career pathways, sustainability and industry matters.
• Guides education and career development
• Advances pet wellness, nutrition and dentistry
• Provides insights to improve our services
• Elevates your professional profle with marketing exposure
By joining us, you’ll gain access to the broader Animal Referral & Emergency Network, which offers benefts such as paid parental leave, fexible work options, an industry-leading Continuing Education Program and mentorship from some of the most talented professionals in the industry.

Rhonda Ponder
AVN, RVN, DipVN(GP), DipVN(Surgery)
National Learning and Development Manager for AREN (Secondment)
Surgical Nurse Team Lead, Adelaide Animal Emergency + Referral Centre (AAERC)
VNCA 2023 Vet Nurse of the Year
“As a Veterinary Nurse of 20 years, I’ve worked in various roles, but always with a passion for Anaesthesia and Critical Care. With the Animal Referral & Emergency Network (AREN), I’ve gained advanced skills, benefted from a network of vets and
specialists and successfully applied for a VTS in Anaesthesia and Analgesia. My dream is to see Australian Veterinary Nurses celebrated as they deserve to be, with AREN practices providing the perfect environment for that recognition.”
No matter where you are on your Specialty and Emergency journey, we can fnd the perfect role for you.
Contact: Alana Hurley 0422
Results of a study published recently inthe journal PLOS ONE suggest orangutans are not the only primate that know which plants are beneficial should they be injured or feel unwe unwell. (The Veterinarian, May 2024). Wild chimpanzees (Pan troglodytes) in Uganda’s Budongo Central Forest Reserve have also demonstrated

their knowledge of ‘therapeutic self-medication using two wellestablished self-medicative behaviours: leaf swallowing and bitter pith-chewing’.
Researchers led by Elodie Freymann, a post-doctoral affiliate from Oxford University’s School of Anthropology and Museum Ethnography in the UK, monitored 51 chimps across at least 16 field sites and then collected plant, tree and herb extracts from 13 species they assumed the animals may have used to self-medicate. When the anti-inflammatory and antibiotic properties of the samples were checked the scientists found 88 per cent of the plant extracts inhibited bacterial growth, while 33 pr cent had anti-inflammatory properties. The scientists also noted these plants were eaten by some injured orsick chimps despite not being part of their normal diet.
Dead wood from a tree in the Dogbane family ( Alstonia boonei )
The recently released 2024 Royal Canin Vet Nurse Survey has highlighted the urgent need for greater recognition of veterinary nurses’ skills by pet owners and expanded opportunities to advance their roles. Conducted in collaboration with the VeterinaryNurses Council of Australia (VNCA) and the New Zealand Veterinary Nursing Association (NZVNA), the survey gathered insights from more than 500 veterinary nurses across Australia and New Zealand.
The survey revealed that 79 per cent of veterinary nurses feel the strain of the clinic environment, citing low remuneration, high pet owner expectations, and staff shortages as significant factors impacting their motivation and passion for the job. Despite these challenges, the drive for professional growth remains strong, with many vet nurses seeking more leadership development opportunities.
Bronwen Slack, Chief Health Officer at Royal Canin ANZ, emphasized the importance of career development in improving workplace culture: “Vet nurses are the backbone of our clinics, and their commitment to professional
growth is evident. The Emerging Leaders Program is pivotal in not only improving job satisfaction, but also fostering leadership within clinics, which leads to better patient outcomes.”
While 93 per cent of vet nurses possess advanced qualifications, more than 75 per cent are calling for mandatory registration to formalize and protect their roles. Only 50 per cent of vet nurses felt their expertise was fully appreciated by pet owners, despite their crucial role in animal care. Furthermore, 64 per cent of respondents are considering leaving the profession within the next five years, raising serious concerns about the sustainability of the industry.
Among their many responsibilities, vet nurses and technologists are involved in monitoring anaesthetics, performing dental cleans, taking x-rays, and providing expert nutritional advice for pets.
“With more than 90 per cent of vet nurses having advanced qualifications, plus invaluable skills from years of experience, they are avaluable, underutilized source of information and expertise for pet owners,” Slack said.

showed the strongest antibacterial activity while it also had anti-inflammatory properties, suggesting it could also be used to treat wounds. Bark and resin from the East African mahogany tree (Khaya anthothecal), and leaves from a fern ( Christella parasitica) exhibited potent anti-inflammatory effects. Amale chimp with an injured hand was observed seeking out and eating leaves of this fern which the scientists suggested may have helped reduce pain and swelling. ToPage 30
The survey also spotlighted the efforts of initiatives like the Emerging Leaders Program, developed by Royal Canin in partnership with the Lincoln Institute of Veterinary Business. This program has supported over 300 vet nurses in developing leadership and non-clinical skills, which has proven to enhance job satisfaction and improve clinic culture.
To further support veterinary professionals, the VNCA and Royal Canin launched the Vet Nurse Mental Health Ambassador Award in 2024. Shannon Molloy from Perth was recognized as this year’s recipient for her outstanding work in promoting mental health within veterinary settings.
Looking to the future, Royal Canin is launching the ROYAL CANIN Academy, a new educational platform designed to provide veterinary nurses and technologists with tailored courses in pet health nutrition education. Set to be available by the end of 2024, this initiative aims to support ongoing professional development and enhance career satisfaction.
Survey Highlights:
■ Demographics: 97 per cent of respondents were female, with 71 per cent under the age of 44.
■ Educational qualifications: 93 per cent of respondents have advanced qualifications or are currently studying.
■ Registration rates: 48 per cent of vet nurses are registered with a registration body, up from 35 per cent in 2023.
■ Top stressors: Low remuneration, staff shortages, and high pet owner expectations.
■ Retention concerns: 64 per cent of respondents are considering leaving the profession within the next five years.
■ Professional recognition: Only 50 per cent of vet nurses felt their expertise was fully appreciated by pet owners.
■ Call for mandatory registration: Over three-quarters of respondents support mandatoryregistration to protect and formalize the profession.
The survey's findings highlight the critical role veterinar y nurses play in animal care and the need for ongoing support, recognition, and professional development to ensure their continued contributions to the field.
For more information about Royal Canin’s initiatives and the ROYAL CANIN Academy, please visitwww.royalcanin.com.





PNEUMONIA/RESPIRATORY DISEASES
– Specific registration for Pneumonia in cattle
– Second follow up injection in severe cases in respiratory infections – approved
– Use with an appropriate antibiotic
MASTITIS
– Double dose in severe infections plus appropriate antibiotic
– Milk Withholdholding Time 12 hours: NO milk withholding time when the period from treatment to the next milking is longer than 12 hours
PAINFUL AND INFLAMMATORY CONDITIONS
– Lameness and foot rot (with an antibiotic)
– Post calving pain management of the cow
– Pain management following de-horning or castration
– Pain related to Pink Eye inflammation
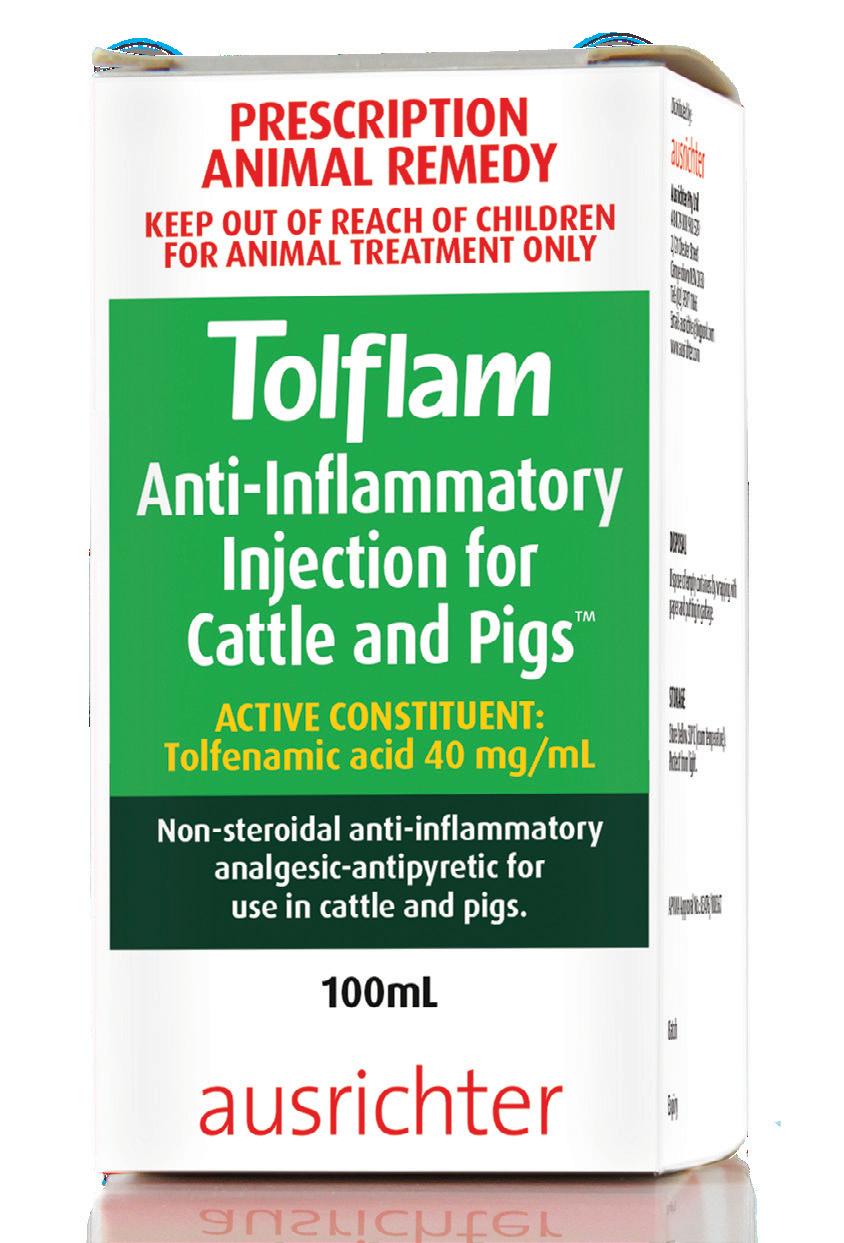
COMPARISON OF TOLFLAM™ & MELOXICAM INJECTIONS FOR CATTLE
conditions – ‘Store below‘
Number of approved doses to be administered 21 Meat WHP days after treatment 10 8 Milk Withholding Time
Time for use after opening6 months28 days
Musician Warren Ellis and conservationist Femke den Haas are the subject of an acclaimed new documentary, Ellis Park.
E llis Park was directed by Justin Kurzel ( Nitram,Snowtown ), and it documents the Sumatran facility of the same name which provides sanctuary for animals sometimes too impaired to be released, often the victims of wildlife traders and illegal private zoos.
Ellis Park’s residents include Rina, a female pig tailed macaque with no arms, Brad, a male crocodile with no teeth, and Oscar, a male slow loris who suffered electrocution burns on apower pole.
Ellis is a member of much-loved bands The Dirty Three and Nick Cave and the Bad Seeds, and den Haas was critical to the establishment of the Jakarta Animal Aid Network.
The film tracks den Haas’ activism, the genesis of the sanctuary and Ellis’ eventual visit to the park. Dutch-born den Haas spoke to The Veterinarian about the film, her work at the park she co-founded with Australians Ellis and Lorinda Jane, and the facilities she and her team have been able to build since its 2021 inception.
How do you feel about Justin Kurzel’s film? Ifeel likeEllis Parkis extraordinary, more than Icould ever expect. The way Justin exposed everything we do here was very real. Often when you have film crews, they romanticise and show a whole different thing from the reality. And that’s what I really loved about Justin; he managed to really show the people behind the scenes and the hard work. I’m still quite emotional about it.
The premiere of the film at this year’s Melbourne International Film Festival looked like a very moving event
Everybody was emotionally touched. I’ve never received so many hugs in my life! They really got it, and were feeling what we’re going through here. I felt a bit like a rock star next to Warren.
How did you deal with having cameras around while you worked?
The film crews were really easy-going and adapted to us. I’ve worked with crews previously who were really demanding that already have the shot in their imagination. It’s difficult to work like that, because that’s not how life goes. Wework with wild animals and we don’tforce the position the animals are in or the way that we rescue them. Wecannot just grab a gibbon without the mask and get bitten because they want (a certain shot). They were never pushy.
What areyou hoping the film accomplishes?
Ihope that through the through the film we can really show the issues that we are still facing through wildlife trade, and the cruelty that is inflicted on animals because of a few greedy people out there. I think anyone who will see (the film will see) how much effort is put in to rehabilitation of animals. If you really see how difficult that process is, and the dedication of the people behind the scenes, hopefully it will make people think otherwise about having an exotic pet or private zoo. I just hope we can move to a world where wild animals can stay wild.
What facilities have you been able to build since Ellis Park began in 2021?
Since that time we’ve managed to safeguard almost three hectares or land, and built a proper veterinaryclinic. We’d love to have a digital x-ray machine, but we still use an oldfashioned one. We have a quarantine, rehabilitation facilities for the gibbons, a socialisation cage for macaques, a bear enclosure for bears that cannot be released, and a verylarge aviary. In April 2022 we had a huge confiscation, 1700 animals in one day, and this included a lot

of birds from Indonesia and Thailand, and meerkats from Africa, marmosets from Brazil. Suddenly we had all of these animals that don’t belong in Indonesia and I’m so happy we had launched Ellis Park as a sanctuary.Before that we were just a transit rescue centre for Indonesian species, so it was the right moment. We built aviaries and also an enclosure for the meerkats. We managed to pull it off through the support of Warren Ellis and the people who support Ellis Park.
How big is your team?
We have two full time veterinarians here, and 14 caretakers now. We’re also open for veterinarians to come and help, but we’re very selective. We’re afraid that would change the quality of the program if we have too many people, but we’re happy if there are people who have some experience to come and share that.
How did you initially connect with your co-founders, Warren Ellis and Lorinda Jane?
Iknew Lorinda because she did a lot of work
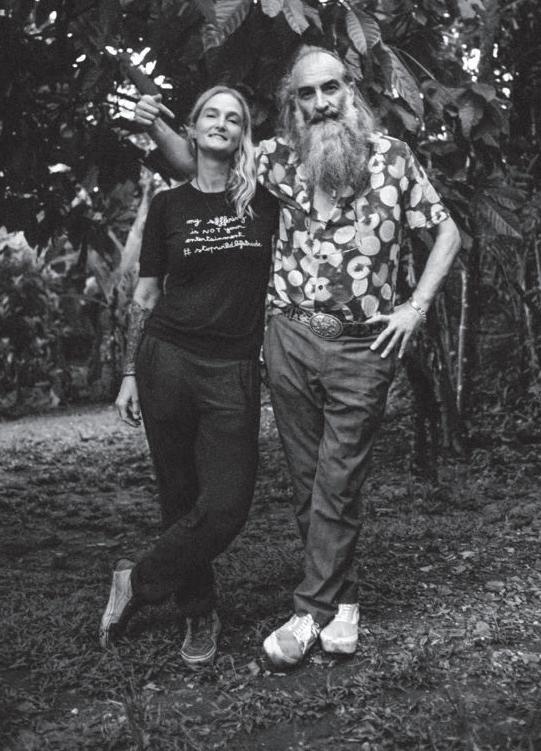
regarding palm oil and orangutan protection. And during COVID Lorinda ran into Warren and they had a talk about wildlife. He was fascinated and wanted to do more. Lorinda said “I know the person to talk to.” Wehad this Zoom meeting and it just clicked, and immediately he was like “this is what I wanna do.” I meet so many people that always say they want to help or applaud the work, but they never help really.
There was a genuine interest
Yes, so many questions and explaining about everything here and I felt immediately he was really real in wanting to help. So we bought a piece of land next to our existing little transit centre that was started here in 2018 as a sanctuary for animals, but we couldn’t release them and we couldn’t give them the space that they needed. Warren was so happy that he could make something happen like that, he could immediately see it. And then I was like “now we have the land, we need to build!” So then we started the Instagram (@ellispark sumatra) to get people involved, and so many people reached out.
When we got the meerkats, time was really limited. They were in really bad condition and needed space with sunlight. Wehad them in the clinic for the first two weeks, getting intensive care, but they needed more space. So we reached out to the public, everyone worked together, and we could build the enclosure for the meerkats. I’d never felt this type of support before.
Before, social media was a place where we share what we do and people go “yay, great”, but never really any support. It’s really hard, because it was the same circle of people involved in animal rescue who all need support. But through Warren we touched this new community of people that had maybe never even heard of a gibbon, and they saw something new and they wanted to help.
Ellis Park premiered in Melbourne in August, and recently screened at the London Film Festival.
Donations can be made to the facility atellispark.org ■ SAM WORRAD
When we think of animals in medieval Europe, the horse immediately springs to mind. Heroic scenes of knights on horseback and the cavalry charging into battle pervade contemporary interpretations of the medieval world. In film and television, the main characters travel on horseback and the clip-clop of hooves serves as a near-constant sonic accompaniment to the action. Indeed, the drawcard of any modern medieval fair is the jousting, with suitably costumed re-enactors hurtling towards each other on their decorated mounts. But were horses as prevalent in medieval Europe as we now seem to think? In short, the answer is a resounding yes.
Horses were an integral part of medieval life, with their multifaceted roles affecting nearly everyaspect ofthe day-to-day.At the most basic level, horses granted movement, as to travel any great, or even short, distance, usually meant taking a horse. If people needed to go to a neighbouring village or into a city, horseback was the quickest way. If they did not (or could not) ride, horses might still pull them in a wagon or carriage, often with goods and luggage onboard. In war, knights depended on horses for mobility and combat. In fact, the use of horses in battle was a defining feature of medieval European warfare, and a knight’s status and effectiveness were often tied to the quality of his horse. For the upper classes, horses were also fundamental to the pursuit of leisure activities, such as tournaments and hunting. While oxen were the primary beast for ploughing, horses could also assist on the farm as, with the right equipment, they could plough a larger amount of land in a shorter amount of time. Moreover, they were essential to carry the harvest into market, where farmers could make their living, and people could stock up on food.
The versatility and importance of horses made them central to the functioning and structure of medieval society. As such, medieval people prioritised horse health and equine medical care – known at the time as marshalcy. This began before a horse was even born. Jordanus Ruffus, a thirteenth-century Italian nobleman working as a farrier at the court of Holy Roman Emperor and King of Sicily Frederick II, recommended that mares and stallions be given proper nutrition as this would result in healthier offspring. Once a foal was born, its mother should receive proper feeding to ensure she could supply her baby with sufficient milk. For the first two years of a foal’slife, it should also be allowed to follow its mother, only separating from her once it reached maturity. The foal itself should be raised in a rocky or stony environment so that its hooves would grow strong, and its legs would become used to walking on harder terrain and traversing up and down hills.
Ahorse might be born and raised inasalubrious environment, but there was always the risk of sickness or injury. One of the most common issues medieval horse owners had todeal with was the spread of the bacterium Bukholderia mallei,which people called farcy when it manifested subcutaneously on a horse’s limbs and body, or glanders when it appeared in the nostrils, submaxillary glands and lungs. There was an awareness that these diseases could pass to a horse through close contact – one late-medieval remedy book notes that farcy could be caught “by smelling a horse nearby that has the malady,” and scientist andphilosopher Albertus Magnus (d. 1280) warned that it might be passed on if an infected horse bit another. At the same time, farcy was thought to arise from excessively moist flesh and overproduction of fluid, which led to swelling and blockages around the glands. Humoral theory, the dominant medical paradigm of the period, reasoned that an unbalanced body, in horses and people, was more susceptible to sickness and less able to fight off disease. It was therefore imperative to keep the humors in check, lest the intemperate human orequine body meet a sickness it could not fight off.
To treat farcy and glanders, medieval horse owners and marshals (those tasked with the medical care of horses and other hoofed animals) had surgical, herbal and religious options, many of which they combined. Albertus Magnus recommended cutting into the skin with a razor to “lay bare all the hidden fleshiness down to the very bottom of the farcy.” Then, the spot must be burned with a hot instrument and covered in a poultice of barley or wheat flour with egg yolks and agrimony or leeks. A mid-fourteenth-centurymedical miscellany from England suggests that glanders could be treated by first giving the horse a draught of groundsel, ale and liquorice, then cleaning out its nostrils.
Aparticular common method of treatment for farcy was charming, that is the use of words for medical purposes. The subcutaneous nodules of farcy were visually similar to human skin degradation from worms. Charms which called upon the Biblical figure of Job, who suffered from worms and skin sores as part of his trials, might then help treat the same in horses. An AngloNorman charm from the latethirteenth century has the healer enumerate Job’s worms from nine to zero, creating a sympathetic link between the sacred past and the present. Just as Job’sworms disappeared, so too might the horses, the power of the spoken words acting as amedicine to apply to the animal.
Another type of condition which people attempted to resolve through religious means was laminitis – known at the time as “founder.” In a remedy for founder from a Middle English medical
miscellany from around 1406, the healer is instructed to:
“Take a handful of oats and bless them and say a Paternoster and an Ave for Saint Hippolytus’ soul and pray to God and to Saint Hippolytus to save your horse and take a holy candle and drop on the oats and sprinkle holy water and afterward, give the oats to the horse to eat and do this three times”.
Once these oats were supercharged with God’s grace, they would be able to heal the horse’s inflamed laminae. Grace was rationalised as a quality which could be infused into other ingredients. Just as something can be made warm once infused with heat or wet once it came into contact with water, so too could ordinary ingredients like oats become grace-infused, thus potent, medical remedies.
There were, of course, mundane forms of treatment for damaged or injured hooves too. One option for horse owners and marshals was to use shoes that did not have calkins.
Leading the horse into water and keeping its legs submerged was also deemed beneficial, the cold helping to ease the swelling. A draught of comfrey could similarly prove therapeutic, the herb believed to have vulnerary properties.
Hoof protection was essential to keep horses in a fit state to travel and work. Iron horseshoes seem to have been used in Europe since around the year 900, though the practice originated much earlier in Central Asia. However, it was imperative that the shoes were the right shape and shape for the individual, and horses needed to be shod properly. Jordanus Ruffus warned against improper shoeing which could cause a horse injury such as rupturing of the coronary band. The unskilled smith might also hammer the nail into the quick of the hoof, resulting in cloying and lameness.
While it might be clear if a misplaced nail was the problem, other types of lameness were not as easy to identify. The Book of Marshalcy, afifteenth-century treatise on horse care, suggested leading the horse around and watching it walk to pinpoint the origin of the lameness. This would then determine the treatment used.If a horse was lame in the shoulder, a therapeutic, curved shoe could help, as this adjusted the horse’s gait. Bleeding near the injurysite might also provide relief. For instance, a horse lame in the knees would benefit from bloodletting on both sides of the pastern.Bloodletting needed to be performed by someone with

adequate skill though. Precise amounts of blood needed to escape and the letting site needed to be cut cleanly, in a way that did not result in more damage. Another treatment which demanded precision was the removal of a hawe (pterygium)in the eye which, if left untreated, could hinder sight. For this surgical procedure, the eyelid was first stitched with a thread and pulled open to expose the fleshy tissue. Then, the marshal must draw the needle and another thread under the growth, raising it enough to slice it out, though careful not to cut too deep into the orbital fat. Likewise, the marshal treating a growth in the mouth next to the jaw teeth needed to pull the tongue to one side to expose the cheek. Then, with a lancet, the marshal had to make a careful incision and cleanly remove the excess tissue, before applying balls of egg yolk and salt into the cheeks. The proliferation of horse health treatises and the frequency with which equine remedies appear in contemporary medical texts indicates that the wellbeing of their beasts was a priority for medieval people.With so many facets of life dependent on horses, owners and marshals went to great lengths to keep them healthy, combining the range of treatments they had at their disposal to engender salubriousness from the moment of the foal’s conception, right across its adult life.
Elizabeth Burrell received her PhD in Historical Studies from Monash University in Melbourne, Australia. She is a Research Officer at the Monash School of Philosophical, Historical and Indigenous Studies and her research focuses on the confluence of medicine, religion and natural science in the ancient, medieval and early modernworld.


PEXION® is the only targeted therapy developed specifically for dogs with idiopathic epilepsy, balancing seizure control whilst preserving quality of life in patients.1,2

Scan to rediscover the role of PEXION in managing canine idiopathic epilepsy*

“PEXION has provided a vital new tool for the treatment of epilepsy in dogs. As a neurologist, I now use it as my frst choice anticonvulsant in drug-naive patients, because of its improved side effect profle over more traditional drugs, its improved hepatic safety, and its short half-life (which means I know whether it’s working fairly quickly). It is also one of the few anticonvulsants that has a sound body of evidence to support its use and it gives us one more option to use in our never-ending quest for that most elusive of things: perfect seizure control.” – Dr Sam Long BVSc PhD DipECVN, Veterinary Referral Hospital.
Interview Questions:
Name: Kim Healy
Qualification: RVN, AVN, FFCP(Veterinary), VTS(Nutrition)
Background: Currently Working in Emergency and Critical Care, Kim has been nursing for 9years, she has worked in a variety on environments including General Practice, Reproduction, Dentistry and Education. Kim is a lecturer for the Bachelor of Veterinary Nursing.
Location: 250 Princes Hwy, Werribee 3030 –Greencross Vet Hospital at the University of Melbourne
Why did you choose the profession What inspired you to become a Veterinary Nurse?
Originally, I wanted to be a vet. I started as a vet nurse then found a passion for what I was doing and decided to continue training and upskilling myself. I wanted to inspire others and encourage veterinary retention and utilisation in practices.
What study and training did you undertake to whereyou are today?
Istarted with the minimum qualification of a Certificate IV and then continued to complete aBachelor of Veterinary Technology. I had always had a passion for nutrition and focused the first 5 years of my career on Nutrition within General Practice and Emergency. Ibecame a board Veterinary Technician Specialist in Nutrition in 2021, at the time, the 2nd in the southern hemisphere.
Ihave a passion for education and started lecturing at conferences and running courses which led me to becoming a higher education lecturer. Now I split myself between education and clinical work. I am currently working towards my 2nd VTS in ECC, with hopes to sit the exam in 2026.
Career Progression and Recognition:
How has your experience as a veterinary nurse been influenced by the level of recognition and acknowledgment you receive from pet owners and colleagues? Could you share an instance where feeling appreciated positively impacted your motivation and passion for the profession?
For Veterinary Nurses, Career progression is not commonly discussed and many of us feel that it is not an option. My motivation to get where I am today was purely self-driven and something that I set out to achieve.
Ihave become more open about discussing my achievements and I have had a positive response from both pet parents and colleagues, being invited to speak at national education events and have other professionals be interested in what I am saying is truly humbling.
Acareer highlight for me is honestly being able to have the trust from veterinarians and am asked to collaborate on patient care, it means they truly value my knowledge and my opinion, they regularly include my recommendations in cases and that makes me feel like an equal. Teaching Vets new techniques that they may not have a lot of experience in such as placing feeding tubes
and then watching them perform that skill on another case does truly motivate me to continue learning and makes me feel like Iam a valuable team member and individual in this profession
Educational and Skill Development:
Royal Canin’s recent survey highlighted that asignificant percentage of veterinary nurses are eager for continued learning. How has advanced qualifications or ongoing education helped you handle complex clinical situations or improve patient care outcomes?
An increase in knowledge and skills becomes increased confidence. Not only in myself but how my colleagues view me. I am given more responsibility in the clinic and can use the skills Ihave learnt. Being able to work at such a high level has increased my day-to-day job satisfaction. It makes me feel like I am truly making a difference in a patient outcome, whether that be in an ECC environment or in a general practice environment. From a general practice perspective being able to perform advanced nutritional consults does truly help the patient, I have excellent adherence to my recommendations, and I feel the owner feels heardwhen we formulate a nutritional plan. Ihave found that many diseases arebetter managed and those patients with co-morbidities who need a nutritional recommendation aregiven a more specific recommendation.
Stressors and Wellbeing:
Stressors like high workloads, demanding clients, and emotional challenges have been proven to impact motivation for many veterinary nurses. Could you provide an example of a particularly stressful situation you've encountered and how you managed to cope, highlighting any strategies that improved your overall wellbeing?
Personally, for me, the most stressful situation is understaffing, the average vet nurse will leave the industry at about 5 years, this means we have a constant influx of less experienced nurses and we lose the experience when that nurse walks away. This puts an increased demand on the experienced nurses in practice and they are often given the task of training new hires. As well as performing their job and managing the expectations of the vets and management. When I am feeling overwhelmed or on the verge of burnout I make sure I speak up to management and take a break, I also try and wind down at the end of a shift with a hobby that I enjoy which is repetitive and low-stress such as painting or craft.
Mandatory Registration and Professional Advocacy:
Royal Canin found that there is support for mandatory registration of veterinary nurses. Can you provide an example that illustrates how mandatory registration could enhance the perception of veterinary nurses as highly skilled professionals and contribute to improved patient careor overall industry standards?
With mandatoryregistration we would become accountable for our actions, currently, we fall under the veterinarian and if make a mistake that falls on our vets, this can be quite stressful for many vets and in some cases that can limit what a vet nurse can do. If we had amandatoryminimum qualification which in

myopinion should be a bachelor’s degree, we would all graduate on the same level and day one competencies would be clearer. Ibelievemandatory registration would also provide us with better recognition from both vets and the general public, aligning us with similar respect to human nurses and veterinary nursing would be seen as a viable career and not just a job.
Advice for pet owners
What would be your one piece of advice for pet owners on preparing for a vet visit?
Can you provide an example of where pet owners can best work with their vet professional team?
The best advice I could give is to call ahead and inform us if your pet needs extra care, perhaps they become stressed so we should put them in a consult room straight away or maybe an anxiety medication should be given prior to the visit. Preparation starts at home and sets us up for a successful vet visit, this makes the visit a morepositive experience for the pet, client and vet team. Clients who have pets that have had a negative experience may be reluctant to seek treatment in the future and this can cause missed health exams and early detection of health conditions.
What’s the one thing you’d like pet owners to know about veterinary professionals caring for their pets?
We do really care about your pet and it hurts when we are told we only care about money. We do a lot of overtime and that is because we stay to help, we stay to see your pet on a Friday night even though the clinic is closing, we miss lunch breaks, we miss family events and are working throughout the night to treat sick pets. We all spend a lot of money on ourselves to attend continuing education events and courses so we can better treat your pet, we don’t get paid to attend these events and sometimes we are doing them remotely at home after a day of work. We collaborate with other vets and seek their opinion if we are unsure what to do, we have group chats and groups where we can ask for help, so there is never only 1 vet looking after your animal, we may be asking a specialist for advice that is no cost to you. We travel to other clinics in our own cars to collect lifesaving medication that our clinic may not have instead of asking you to go to another clinic. Ultimately, it is a thankless job, especially for nurses but we are doing the majority of the patient care, we are there making sure your pet is comfortable, we are advocating for them for additional pain relief, we spend hours every day with them, we do all sorts of things to get them to eat, we talk to them and comfort them like they are own pets. I can honestly say,through all the hardships we are truly here because we love what we do and want to make a difference. A thank you to your vet nurse will change someone’sday.

Dilated
(DCM) is the second most common form of acquired heart disease in dogs1
Treating early with VETMEDIN® is proven to delay the onset of clinical signs by 63% and extend life in preclinical DCM.1

To learn more about identifying preclinical DCM in dogs, scan the QR code to visit Boehringer Ingelheim Cardiology Hub. If you do not have an Animal Health Academy account, please register using the access code “myAcademy”.
For more information talk to your Boehringer Ingelheim Territory Manager today or call our Customer Care Team on 1800 808 691.

risk of poor welfare outcomes?
If livestock at risk of poor welfare could be identified using a risk assessment tool, more targeted response strategies could be developed by enforcement agencies to facilitate early intervention, prompt welfare improvement and a decrease in reoffending. This study aimed to test the ability of an Animal Welfare Risk Assessment Tool (AWRAT) to identify livestock at risk of poor welfare in extensive farming systems in Australia. Following farm visits for welfare- and non-welfare-related reasons, participants completed a single welfare rating (WR) and an assessment using the AWRAT for the farm just visited. A novel algorithm was developed to generate an AWRAT-Risk Rating (AWRAT-RR) based on the AWRAT assessment. Using linear regression, the relationship between the AWRAT-RR and the WR was tested. The AWRAT was good at identifying farms with poor livestock welfare based on this preliminary testing. As the AWRAT relies upon observation, the intra- and inter-observer agreement were compared in an observation study. This included rating a set of photographs of farm features, on two occasions. Intra-observer reliability was good, with 83 per cent of Intra-class Correlation Coefficients (ICCs) for observers > 0.8. Inter-observer reliability was moderate with an ICC of 0.67. The AWRAT provides a structured framework to improve consistency in livestock welfare assessments. Further research is necessary to determine the AWRAT's ability to identify livestock at risk of poor welfare by studying animal welfare incidents and reoffending over time.
Natarsha Williams1,Sarah Chaplin2,Lauren Hemsworth1, Richard Shephard3,Andrew Fisher1
Anim Welf. 2024 Sep 16:33: e32.doi: 10.1017/awf.2024.28.
1Animal Welfare Science Centre, Faculty of Science, University of Melbourne, Parkville, VIC 3010, Australia.
2Agriculture Victoria, Department of Energy, Environment and Climate Action, Tatura, VIC 3616, Australia.
3School of Electrical and Data Engineering, Faculty of Engineering &IT, University of Technology Sydney, Sydney, NSW, Australia.
Amulticomponent microneedle patch for the delivery of meloxicam for veterinary applications
This study evaluates the use of poly (vinyl alcohol), collagen, and chitosan blends for developing a microneedle patch for the delivery of meloxicam (MEL). Results confirm successful MEL encapsulation, structural integrity,and chemical stability even after ethylene oxide sterilization. Mechanical testing indicates the patch has the required properties for effective skin penetration and drug delivery, as demonstrated by load-displacement curves showing successful penetration of pig ear surfaces at 3N of normal load. In vitro imaging confirms the microneedle patch penetrates the pig's ear cadaver skin effectively and uniformly,with histological evaluation revealing the sustained presence and gradual degradation of microneedles within the skin. Additionally, in vitro drug diffusion experiments utilizing ballistic gel suggest that microneedles commence dissolution almost immediately upon insertion into the gel, steadily releasing the drug over 24 h. Furthermore, the microneedle patch demonstrates ideal drug release capabilities, achieving nearly 100 per cent release of meloxicam content from a single patch within 18 h. Finally, in vivo studies using pigs demonstrate the successful dissolution and transdermal drug deliveryefficacy of biodegradable microneedle patches delivering meloxicam in a porcine model, with over 70 per cent of microneedles undergoing dissolution after 3days. While low detectable meloxicam concentrations were observed in the bloodstream, high levels were detected in the ear tissue, confirming the release and diffusion of the drug from microneedles. This work highlights the potential of microneedle patches for controlled drug release in veterinary applications. Katherine Miranda-Muñoz1,Kirsten Midkiff2,Alan Woessner13, Mahyar Afshar-Mohajer4,Min Zou4,Erik Pollock5,David GonzalezNino6,GaryPrinz6,Lillian Hutchinson7,Ruohan Li7, Topage 30
It is important to understand the reasons for companion animal relinquishment to help reduce the financial and ethical problems arising from too many dogs and cats in shelters. This study investigates the socioeconomic factors and reasons behind companion animal relinquishment in Australia, utilizing data from five animal shelters, over a five-year period (Financial Year 2018/19 to 2022/23). Descriptive statistics reveal that the median Index of Relative Socio-Economic Advantage and Disadvantage (IRSAD) decile of companion animal guardians who relinquished their companion animal was decile 4 out of 10, indicating that they live in areas of lower-than-average socioeconomic status. Cats accounted for 59.4 per cent and dogs for 40.6 per cent of all relinquishments, with more relinquishments from lower socioeconomic deciles (1-5) (cats: 62.6 per cent, dogs: 65.8 per cent). The median age of relinquished cats was 5 months and dogs 16 months, with human factor-related issues (e.g., Housing, Financial Constraints, Human Healthcare) cited in 86 per cent of cases. Descriptive analysis for the five financial years shows a declining trend in numbers of relinquishments, with housing issues (31.2 per cent) identified as the primary reason, followed by ownership decisions (16.2 per cent), financial constraints (11.2 per cent), and human health issues (10.4 per cent). Comparing the reasons for relinquishment between lower (decile 1-5) and higher (decile 6-10) socioeconomic status demonstrated that financial difficulties were a more common reason in lower vs. higher socioeconomic groups, while human health and familyrelated issues are more common in higher vs. lower socioeconomic groups. These findings highlight the critical role of socioeconomic factors in understanding why people relinquish their companion animals, which can inform targeted interventions to support companion animal welfare across different socioeconomic backgrounds.
Sonya McDowall1,Susan J Hazel2,M Anne Hamilton-Bruce3, Rwth Stuckey1,Tiffani J Howell1
Animals (Basel). 2024 Sep 2;14(17): 2549.doi: 10.3390/ani14172549.
1School of Psychology and Public Health, La Trobe University, Bundoora, VIC 3082, Australia.
2School of Animal and Veterinary Science, Roseworthy Campus, The University of Adelaide, Adelaide, SA 5005, Australia. 3Adelaide Medical School, The University of Adelaide, Adelaide, SA 5055, Australia.
Free article
Proteus mirabilis, a microorganism distributed in soil, water, and animals, is clinically known for causing urinary tract infections in humans. However,recent studies have linked it to skin infections in broiler chickens, termed avian cellulitis, which poses a threat to animal welfare. While Avian Pathogenic Escherichia coli (APEC) is the primarycause of avian cellulitis, few cases of P.mirabilis involvement are reported, raising questions about the factors facilitating such occurrences. This study employed a pan-genomic approach to investigate whether unique genes exist in P. mirabilis strains causing avian cellulitis. The genome of LBUEL-A33, a P. mirabilis strain known to cause this infection, was assembled, and compared with other P. mirabilis strains isolated from poultry and other sources. Additionally, in silico serogroup analysis was conducted. Results revealed numerous genes unique to the LBUEL-A33 strain. No function in cellulitis was identified for these genes, and in silico investigation of the virulence potential of LBUEL-A33's exclusive proteins proved inconclusive. These findings support that multiple factors are necessary for P. mirabilis to cause avian cellulitis. Furthermore, this species likely employs its own unique arsenal of virulence factors, as many identified mechanisms are analogous to those of E. coli. To Page 30



































- Dr Phil Tucak Veterinarian and AVA Veterinary Business Professional of the Year 2020





... automating routine tasks to spend more quality time with clients is fundamental for veterinary business’ ‘












The Vetplus business efficiency program offers a number of time-saving opportunities for your staff, using automation to handle routine bookings and reminders, digital solutions like the new Pet Health Passport app, plus a suite of ready-to-go marketing campaigns where all the hard work has already been done. Do more with less! To discover what Vetplus can offer your practice, scan the QR code or talk to your Boehringer Ingelheim Territory Manager for details.






Lisa Singh is a practice broker with Practice Sale Search and is the foremost expert in corporate practice sales working in practice brokerage today. To speak with Lisa or someone from Practice Sale Search, please email info@ practicesalesearch.com.au orcall 1300 282 042.
InMay 2000, a relatively unknown chef called Anthony Bourdain decided that he was going to change careers and not run kitchens in New York City anymore. Asafinal goodbye to his previous career, he wrote a book revealing some things that he felt restaurant patrons should know. The book was called “Kitchen Confidential”; it would become a worldwide best seller and launch his second career as a famous food and travel journalist.
Having recently said goodbye to almost a decade working in Acquisitions for one of the larger dental corporates in Australia, I am at a similar juncture in my career, and there are some things that I think practice vendors should know about corporate acquisition.
Over my eight years, I would have spoken to and visited close to a thousand practices wanting to sell and had my hand in the actual purchase of close to a hundred. Being involved with that many practices and transactions, I saw many put their best foot forward in terms of presentation and negotiation, and get the best possible offer that we could have given them… Unfortunately, I also saw many practices that could have done better for themselves, if only they had known what to look for and how best to deal with us.
Now that I have left the world of corporate acquisitions and jumped over to selling practices, I can share with you my top 5 secrets about how corporate acquisition works and how vendors can get a better result for themselves.
Part 1 of this article was in the previous issue and covered secrets 1–3.
4. It is not as hard as you think for an owner-operator buyer to compete with a corporate Many Vendors think that it’s impossible for an owner-operator to compete with a corporate for good practices, because the corporates have deeper pockets and can afford to pay more. Often, vendors don’t seek out owner-operator buyers and just stick to seeking interest from corporates, which is how the corporates like it. In reality, owner operator-buyers can absolutely compete with corporates for some practices:
a. They can compete on terms Corporates generally don’t buy practices that allow vendors to exit inside a 2-year time frame or pay 100 per cent upfront or without future targets. What is the opportunity cost to the vendors of the time and stress that come along with these terms? Some vendors will accept less money to get fewer post-sale terms.
b. You can compete on compatibility
Many vendors prefer the idea of selling to a person, rather than a company. They prefer knowing the ethics and clinical ability of the clinician who will take over from them when they leave. If they are going to stay in the practice, they like the idea of having an owner onsite who they can talk to about clients, staff and problems, rather than needing to call a “head office” in another state.
5. Understand your targets
If you are thinking about selling to acorporate, like the price they are giving you, but don’t COMPLETELY understand how they calculated your post-sale profit target, STOP! Make sure you get clarity before proceeding.
Don’t let a big, shiny headline purchase price woo you into signing on to an offer that has a postsale target calculated in a way that you don’t understand.
You will need to be able to reach this target to get the full sale price that they are offering. You need to understand not just how they calculated it, but also, as importantly, feel confident that you will be able to replicate it!
In my experience, missing targets due to a vendor’s poor understanding of them is way too common, and the #1 reason for disharmony in practices that have been sold to corporates.
Conclusion
It is not uncommon for a practice owner to feel overwhelmed or unprepared when negotiating the sale of their practice with a corporate.After all, it isn’t a level playing field with you on one side (often selling a business for the first time) negotiating against someone who has done this a hundred times before. How do you ensure that you don’tshortchange yourself in the biggest deal of your life? If only you had someone on your side who had also done the transaction a hundred times before and knew the moving parts as well as the corporates did.




P. J. Guzmán Ramos LV, MSc, DVMS, PhD, Dip. ECVIM-CA A/Prof in Small Animal Medicine School of Veterinary Medicine Murdoch University
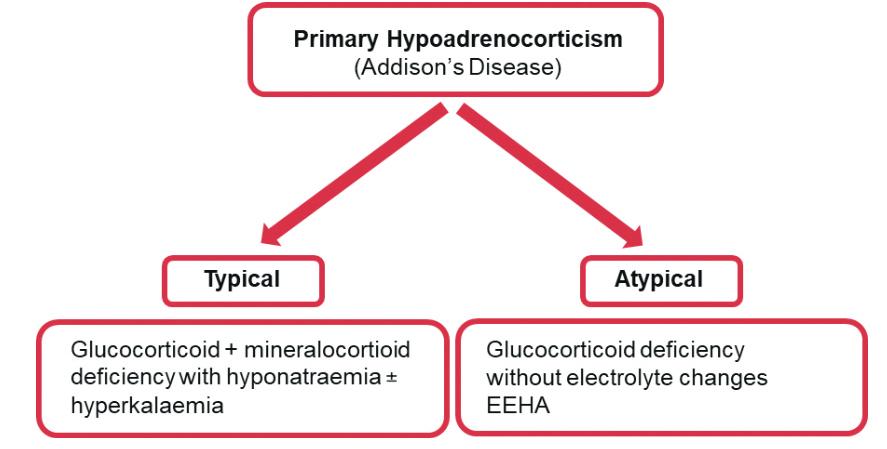
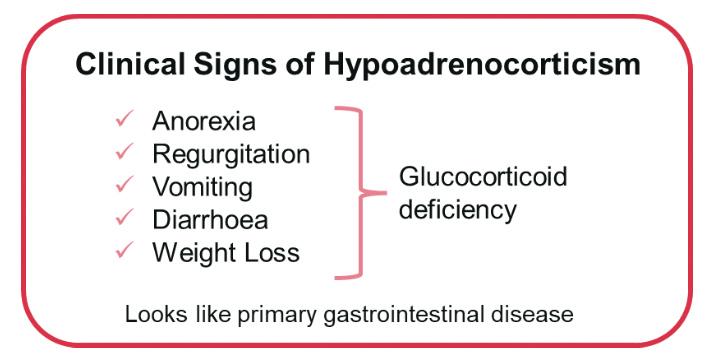
Canine hypoadrenocorticism is an uncommon endocrinopathy with reported prevalence that ranges from 0.06 per cent to 0.08 per cent1 Primary hypoadrenocorticism (Addison’s disease) is referred to as ‘typical’ when describing glucocorticoid and mineralocorticoid deficiency with hyponatraemia and/or hyperkalaemia. ‘Atypical’ hypoadrenocorticism loosely describes the presence of glucocorticoid deficiency in the absence of the electrolyte changes expected with hypoaldosteronism and can be primary (affecting cortisol production by the adrenal glands) or secondary (affecting ACTH production by the pituitarygland).2 The European Society ofVeterinary Endocrinology (ESVE) established project (Agreeing Language In Veterinary Endocrinology (ALIVE)) has suggested that ‘atypical’disease is better referred to as eunatraemic, eukalaemic hypoadrenocorticism (EEHA; Figure 1). Historical, clinical and clinicopathological features may immediately raise suspicion for the presence of typical primary hypoadrenocorticism (e.g. hypovolaemic shock in a young, previously well, purebred dog with characteristic electrolyte changes). However, in dogs with less severe illness, including most with EEHA, these features are often non-specific and characterized by a waxing and waning presentation. Dogs with EEHA are often older, and the disease may occur in any breed. Most commonly reported clinical signs are gastrointestinal, including anorexia, regurgitation, vomiting, diarrhoea and weight loss (Figure 2).2 The prominence of gastrointestinal signs is not unexpected because of the physiological role of glucocorticoids in maintenance of gastrointestinal integrity. Dogs with glucocorticoid deficiency alone often remain undiagnosed for longer periods because signs are indistinguishable from primarygastrointestinal disease, and more specific clinical and clinicopathological consequences of mineralocorticoid deficiency are absent.2 In view of this, hypoadrenocorticism should be considered a differential in dogs with chronic intermittent gastrointestinal signs. The prevalence of EEHA in dogs with chronic gastrointestinal signs was originally described to be 4 per cent (6/151), greater than the prevalence in the general population.3 However, more recent studies have identified lower prevalences of 0.3 per cent (1/282)4 and 0.9 per cent (1/112)5.The lower suggested prevalence opens discussion about the need for testing for hypoadrenocorticism in all dogs with chronic gastrointestinal signs; although hypoadrenocorticism is unlikely to be present in these dogs, identification of the disease can prevent further unnecessarytesting and identify adisease that is readily treatable.

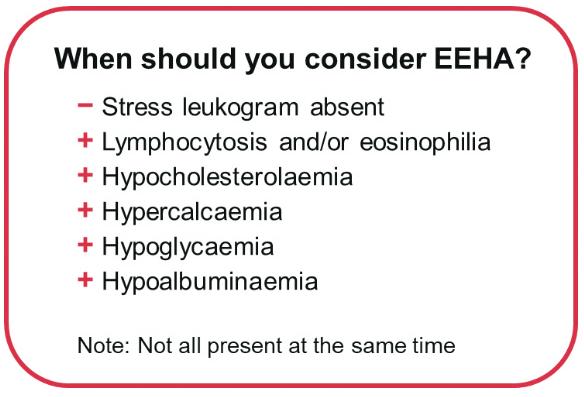
Given the intermittent and poorly specific nature of the clinical signs an index of suspicion is required from veterinarians to test and diagnose EEHA. Main clinicopathological abnormalities that can raise the suspicion for EEHA include the lack of stress leukogram in a dog that is systemically unwell; however, many dogs with primary gastrointestinal disease are not severely ill, and the absence of a stress leukogram is not particularly notable. Lymphocytosis or eosinophilia is reported in only 10 to 20 per cent of cases of hypoadrenocorticism; therefore, most cases would be missed if relying on the presence of these widely recognised albeit uncommon features. Furthermore, eosinophilia is common in dogs with primary gastrointestinal diseases including parasitism and eosinophilic chronic enteropathies. On serum biochemistry, the presence of hypocholesterolaemia (75 per cent in EEHA cases), hypercalcaemia (up to 30 per cent of cases), hypoglycaemia (up to 30 per cent of cases) and/or hypoalbuminaemia (up to 75 per cent in EEHA cases) should also raise the suspicion for EEHA and prompt further testing (Figure 3).2 In particular,hypoadrenocorticism is a major differential for severe hypocholesterolaemia, along with chronic gastrointestinal disease, liver failure and lymphoproliferative disease.
Abdominal imaging via ultrasound is usually part of the investigation of dogs with chronic/intermittent gastrointestinal signs and can provide further insight as to whether adrenocortical
function testing is required. One study evaluated the adrenal gland size of 30 dogs with hypoadrenocorticism, 14 healthy dogs and 10 dogs with diseases mimicking hypoadrenocorticism. The study suggested that identifying a left adrenal gland thickness less than 3.2 mm was highly suggestive of hypoadrenocorticism.6 However, caution must be taken due to the small size of this study and the lack of consideration of effects of body size.6-8 Furthermore, a more recent study suggested that higher adrenal gland cut-off values of 3.9 and 4.2 mm be used for the left and right adrenal glands, respectively,in dogs with EEHA.9 However, adrenal glands of greater thickness can be seen in 10-20 per cent of dogs with EEHA.
The gold standard diagnostic test to confirm or exclude hypoadrenocorticism is the ACTH stimulation test. In the absence of recent corticosteroid administration, this test has near perfect sensitivity and specificity. This test has some limitations such as the high cost and intermittent unavailability of synthetic ACTH (Figure 4).
Resting cortisol concentrations <55nmol/L have been described to have a sensitivity of 99.4-100 per cent but regrettably its poor specificity (63.3-78.2 per cent) prevents its use to confirm the diagnosis.10-12 Given its high sensitivity,it can be used as a screening test to rule out hypoadrenocorticism. If EEHA is confirmed, measurement of aldosterone concentrations pre- and post-ACTH could be considered. Aldosterone secretion is reduced or absent in
some dogs with reference interval electrolyte concentrations, and presumably these dogs are at higher risk of developing an Addisonian crisis unless appropriately treated. In addition, endogenous ACTH concentrations should be assessed to differentiate between primary and secondary disease. If the latter is confirmed, advanced imaging could be considered to determine the underlying causes., and other pituitary deficiencies could be considered, such as central hypothyroidism.
Upon confirmation of the diagnosis and in the absence of mineralocorticoid deficiency, treatment with physiological dose of corticosteroids should be implemented lifelong.
Summary
Ideally, and if possible, adrenocortical function testing should be recommended in all dogs with chronic intermittent gastrointestinal signs, but even more if the above clinicopathological and/or abdominal imaging features are identified such as the lack of stress leukogram in a very ill dog, lymphocytosis, eosinophilia, hypercalcaemia, hypocholesterolaemia, hypoglycaemia or hypoalbuminaemia or small adrenal gland size. The test is unlikely to be positive in many cases, especially in the absence of these features, but identifying hypoadrenocorticism would dramatically alter the course of diagnosis and treatment. Failure to exclude EEHA could lead to more invasive diagnostic tests such as endoscopy and intestinal biopsies that could precipitate deterioration and also have a high economic cost. In addition, misdiagnosing EEHA as a chronic enteropathy could lead to inappropriate therapeutic interventions such as the unnecessary use of antimicrobials, excessive dosages of corticosteroids, or administration of other immunosuppressive drugs that can be potentially associated with adverse effects.
References
1.Hanson, J.M., Tengvall, K., Bonnett, B.N. and Hedhammar, A. (2016), “Naturally Occurring Adrenocortical Insufficiency – An Epidemiological Study Based on a SwedishInsured Dog Population of 525,028 Dogs”, Journal of Veterinary Internal Medicine, John Wiley & Sons, Ltd, Vol. 30 No. 1, pp. 76 – 84, doi: 10.1111/JVIM.13815.
2. Guzmán Ramos, P.J., Bennaim, M., Shiel, R.E. and Mooney, C.T. (2022), “Diagnosis of canine spontaneous hypoadrenocorticism”, Canine Medicine and Genetics, Springer Science and Business Media LLC, Vol. 9 No. 1, pp. 1 – 13, doi: 10.1186/S40575-022-00119-4/TABLES/3.
3. Hauck, C., Schmitz, S.S., Burgener, I.A., Wehner,A., Neiger,R., Kohn, B., Rieker,T., et al. (2020), “Prevalence and characterization of hypoadrenocorticism in dogs with signs of chronic gastrointestinal disease: A multicenter study”, Journal of VeterinaryInternal Medicine, John Wiley & Sons, Ltd, Vol. 34 No. 4, pp. 1399 –1405, doi: 10.1111/JVIM.15752.
4. Gallego, A.F., Gow, A.G. and Boag, A.M. (2022), “Evaluation of resting cortisol concentration testing in dogs with chronic gastrointestinal signs”, Journal of Veterinary Internal Medicine, John Wiley & Sons, Ltd, Vol. 36 No. 2, pp. 525 –531, doi: 10.1111/JVIM.16365.

5. Tardo, A.M., Del Baldo, F., Leal, R.O., Galiazzo, G., Pietra, M., Gaspardo, A. and Fracassi, F. (2024), “Prevalence of eunatremic, eukalemic hypoadrenocorticism in dogs with signs of chronic gastrointestinal disease and risk of misdiagnosis after previous glucocorticoid administration”, Journal of Veterinary Internal Medicine, John Wiley & Sons, Ltd, Vol. 38 No. 1, pp. 93 – 101, doi: 10.1111/JVIM.16921.
6. Wenger, M., Mueller, C., Kook, P.H. and Reusch, C.E. (2010), “Ultrasonographic evaluation of adrenal glands in dogs with primary hypoadrenocorticism or mimicking diseases”, The VeterinaryRecord, Vet Rec, Vol. 167 No. 6, pp. 207 – 210, doi: 10.1136/VR.C4235.
7. Büttelmann, G., Harder,L.K., Nolte, I. and Wefstaedt, P. (2023), “Impact of body weight and sex in selected dog breeds on the canine adrenal gland dimensions measured by computed tomographic imaging”, BMC Veterinary Research, BioMed Central Ltd, Vol. 19 No. 1, pp. 1 – 11, doi: 10.1186/S12917-023-03641-0/TABLES/5.
8. Soulsby,S.N., Holland, M., Hudson, J.A. and Behrend, E.N. (2015), “ULTRASONOGRAPHIC EVALUATION OF ADRENAL GLAND SIZE COMPARED TO BODY WEIGHT IN NORMAL DOGS”, Veterinary Radiology & Ultrasound, John Wiley & Sons, Ltd, Vol. 56 No. 3, pp. 317 –326, doi: 10.1111/VRU.12236.
9. Reagan, K.L., McLarty, E., Marks, S.L., Sebastian, J., McGill, J. and Gilor, C., 2022. Characterization of clinicopathologic and abdominal ultrasound findings in dogs with glucocorticoid deficient hypoadrenocorticism. Journal of veterinaryinternal medicine, 36(6), pp.1947 – 1957.
10. Bovens, C., Tennant, K., Reeve, J. and Murphy, K.F. (2014), “Basal Serum Cortisol Concentration as a Screening Test for Hypoadrenocorticism in Dogs”, Journal of Veterinary Internal Medicine, John Wiley & Sons, Ltd, Vol. 28 No. 5, pp. 1541 – 1545, doi: 10.1111/JVIM.12415.
11. Gold, A.J., Langlois, D.K. and Refsal, K.R. (2016), “Evaluation of Basal Serum or Plasma Cortisol Concentrations for the Diagnosis of Hypoadrenocorticism in Dogs”, Journal of Veterinar y Internal Medicine, John Wiley & Sons, Ltd, Vol. 30 No. 6, pp. 1798 – 1805, doi: 10.1111/JVIM.14589.
12. Lennon, E.M., Boyle, T.E., Hutchins, R.G., Friedenthal, A., Correa, M.T., Bissett, S.A., Moses, L.S., et al. (2007), “Use of basal serum or plasma cortisol concentrations to rule out a diagnosis of hypoadrenocorticism in dogs: 123 cases (2000 – 2005)”, Journal of the American Veterinary Medical Association, American VeterinaryMedical Association, Vol. 231 No. 3, pp. 413 – 416, doi: 10.2460/JAVMA.231.3.413.





















In the beginning…
The story of the domestic cat, scientifically known as Felis catus,begins long before these graceful creatures curled up on our couches or snuggled into our beds. Their tale begins with the African wildcat, Felis silvestris lybica,solitary hunters adept at surviving in diverse environments across Africa, Europe and Asia.
Around 10,000 years ago, in the fertile lands of Mesopotamia - modern-day Iraq, Iran, and Turkey - wildcats began a unique relationship with humans who were transitioning from nomadic to settled agricultural lifestyles. That a very close relationship developed is evident from archaeological findings in Cyprus dating to 7500 BC of a cat buried alongside a human.
We know little about the wildcat before this time except as one branch of the Felidae family. Although their pre-human history remains unknown and shrouded in mystery, we know their past shaped them into the elusive, independent, and formidable hunters our ancestors first encountered.
So it was that the dawn of agriculture, when Neolithic humans began building permanent dwellings and cultivating crops, marked a profound turning point in evolutionary history. Not just in our journey but in feline history as well. Many historians mark this moment as the beginning of the domestication process and the origin of the domestic cat.
As we delve into the burgeoning alliance between humans and cats, an intriguing question will emerge: who truly domesticated whom? Contraryto the popular belief that humans initiated the domestication process, evidence suggests a more nuanced narrative.
Cats are naturally curious and observant. As wildcats patrolled their lands hunting for food or protecting their territory they would have observed the unusual activity of these bipedal creatures. Naturally cautious as well, perhaps these wildcats kept their distance from human settlements. But, as time passed, one or two adventurous felines couldn’t resist a stealthy visit. We’ll never know for certain what transpired but perhaps it went something like this…
The cave-age farmers were delighted with their harvest and eagerly stored the surplus grain from their crops. But they hadn’t reckoned with the little creatures that also delighted in the easy food supply. Very soon, the sheer volume of rats and mice devouring and spoiling the grain was threatening to undermine the burgeoning agricultural era. Enter Felis silvestris lybica.To these wildcats, finding a dense and thriving population of rodents in one location must have been a boon - an unexpected and sumptuous feast.
The early farmers at first tolerated the presence of these feline hunters but quickly recognized their value and became more and more reliant on feline visits for rodent control. As human survival depended on the safety of the grain stores, perhaps a farmer decided to leave a little bit of food – maybe a sliver of meat or a clay dish of warm cow’smilk near his dwelling – to entice the wildcat to stay around. Perhaps, over a few days of venturing close then running back into the night shadows, our adventurous wildcat ate the food. Imagine this pattern repeating many times over the following weeks and months and years. How must the wildcat have felt to have a steady supply of copious food to hunt and eat?
Would he view these strange bipedal creatures as an amazing and never-ending source of cat food? Eventually, a hesitant outstretched hand made contact with a nervous, brave Felis. How much time passed before the wildcat was invited indoors? No longer cowering beneath a bush in the rain or suffering outdoors through a cold winter, safe from predators and inclement weather. Food and shelter. Perhaps our wily Felis recognized a good deal when they saw one. Full board in exchange for a few rats.
Over generations, natural selection favoured cats with traits that made them better suited for cohabitation with people. These traits included amore docile temperament and an increased tolerance for human presence.
As for our ancestors, they believed the domestication process was in full swing – but, really, who had domesticated whom?
The cult of the cat
It may have been in Mesopotamia that cats first assumed a practical role as guardians of granaries and storehouses but it was in ancient Egypt that their skills and prowess were so revered as to give them god-like status.
Around 4000 years BC, settlements and crops sprang up along the Nile River in North Africa. As had happened in Mesopotamia, rats plagued the grain stores of these early farmers. And again, a similar story of wildcat turned rat-catcher re-enacted itself along the banks of the Nile. Before too long Felis silvestris lybica was controlling more than just rodents. Scorpions and snakes, including the deadly Cobra, were fair hunting game as well.
The ancient Egyptians gratitude towards these amazingly efficient vermin hunters gradually morphed into fascination. The wildcats turned house cats were beautiful creatures. In fact, African wildcats of today (those who chose not to cross the Egyptian threshold) look the same as they have for thousands of years. They are slightly larger than domestic cats, with long slender legs and a pointed face. Their coat is soft and sleek, sandy brown with faint tabby stripes. The back of the ears is russet coloured and the end of their tail is ringed with black. Their similarity to the domestic cat is more than skin deep. Felis catus and Felis silvestris lybica are genetically indistinguishable and can interbreed.
Beauty was highly prized in Egyptian culture. Appreciating the grace and poise of these regal creatures was one thing but the Egyptians also paid close attention to the unique behaviours and mannerisms of their feline companions. They not only respected the wildcat’s hunting skills but also their intelligence, courage and dash of kittenish playfulness. Over time, the Egyptian’sastute observations led to an astounding revelation. They found cats seemed to detect changes in the weather, could predict earthquakes and possessed other inexplicable, uncanny – and seemingly mystical - abilities. In an age where magic was an accepted fact, these small furry creatures with their extraordinaryphysical and supernatural abilities were considered magical.
So began a golden age for the once wild cat. Devoted Egyptians regarded cats as sacred companions and spiritual guardians, able to ward off evil spirits and bring good fortune to their households.
The goddess Bastet
For thousands of years, the cult of the cat presided over the land. The ancient Egyptian goddess, Bastet, with the body of a beautiful woman and the head of a cat, was the deity honouring the connection between the feline and the divine. There were temples to Bastet throughout the land but the most lavish and grand of these temples presided over the city of Bubastis. Sacred temple cats lived here, with maidens and priests to honour and serve them. Each year, hundreds of thousands of pilgrims travelled to Bubastis to worship Bastet in a frenzy of all things feline.
Cats were revered for their beauty, dressed in jewels and fed delicacies. They were adored for their grace and elegance and immortalized in sculptures, paintings, ornaments and jewellery. Even Queen Cleopatra’s exotic eye make-up was said to be inspired by feline facial markings.
Their status was such that it was forbidden to mock or laugh at a cat or risk a fine or a flogging. Killing a cat, even accidentally, was considered agrave offense punishable by death. The Greek historian, Diodorus, reported of an incident where a Roman soldier inadvertently ran over and killed a cat in his chariot. Despite royal entreaties for mercy, the populace was so incensed they lynched and killed the soldier for his crime.
Perhaps the greatest example of Egyptian devotion to the cat can be found in the Battle of Pelusium in 525BC. Exploiting the Egyptian’s love for cats, the Persians drove animals, mainly cats, before their invading forces as they descended on the city of Pelusium on the Nile. The soldiers painted cats on their shields and many held cats in their arms. Fearing to harm even a single cat hair if they retaliated, the Egyptians lay down their arms and surrendered the city.
So beloved were cats to the Egyptians that, when a cat died, distraught owners would shave off their eyebrows as a sign of mourning and would continue to mourn until their eyebrows grew back.
Toensure their eternal happiness, cats were afforded the same mummification and burial as that given to a family member. A wealthy family might afford a lavish tomb with gold and gifts to help the soul’s passage in the afterlife but mass burials were also common. In Bubastis alone, over 300,000 mummified cats were found in one cat cemetery.
The ancients believed the soul would eventually return to the cosmos and reside in the starry heavens above. Imagine for a moment, the sorrowful yet hopeful (eyebrow-less) gaze of the recently bereaved searching the night sky, wondering if that twinkling star was a familiar, adored feline companion forever shining bright. What comfort to know a spiritual connection remained with the revered furry little god in the afterlife.
Next time you find your cat snoozing comfortably on your bed, spare a thought for that day long ago when a wildcat ancestor first chose to cross the threshold. That choice forever altered the lives of two worlds. And, certainly,in the chronicles of feline history, there was no doubt as to which species had truly been domesticated.
■ OLIVIA POZZAN





Single-dose, in-clinic treatment: ensures built-in compliance from day 1. Unique combination of 3 proven and trusted active ingredients: gentamicin, posaconazole and mometasone furoate. Provides at least 4 weeks efcacy.1,2 Safe, efective, convenient.1,2
Talk to your MSD Animal Health Territory Sales Manager about how MOMETAMAX ULTRA can beneft your patients, your clients and your practice. For technical queries please phone 1800 033 461 to speak to an MSD Animal Health Technical Services Veterinarian.

One Dose. Healthy Ears. Happy Dog.
Tendon and ligament injuries significantly impact the equine community, affecting companion to top-level performance horses. These injuries contribute significantly to lost performance time, financial losses, recurrence risks, and reduced athletic potential. These delicate structures are crucial for movement and stability, but when injured, they can result in lameness, reduced athletic ability, and in severe cases may have career or life-ending consequences.
Horses with tendon or ligament injuries require rest and rehabilitation, leading to lost training days and missed competition opportunities. This downtime affects performance schedules and can be financially costly for owners and trainers. The expenses associated with diagnosing, treating, and managing these injuries escalate quickly. Even after recovery, there’s a high risk of recurrence. This cycle of injury, treatment, and rehabilitation can be frustrating for horse owners and trainers, impacting their confidence in the horse’s long-term prospects. While some horses can return to riding and competition after appropriate treatment, their athletic abilities may potentially be compromised.
Mature adult tendons, unlike other tissues such as bone or muscle, seem to lack the natural capacity to restore their structure to the preinjury state. Instead, tendon healing involves the formation of fibrotic scars, which compromises the mechanical strength of the tissue (Tang et al, 2014). Consequently, tendon injuries can lead to significant dysfunction and disability. This may partially explain why up to 67 per cent of horses treated using conservative methods experience re-injury within two years of the initial injury (Dyson 2004).
Tendon healing is a complex process, and understanding the limitations of this healing response is crucial for effective management and prevention of re-injuryin horses. The superficial digital flexor tendon (SDFT) in horses, which plays a vital role in locomotion and energy storage, is particularly susceptible to these challenges. The primary energy-storing tendons in horses are the SDFT; these tendons are prone to overload-induced injuries due to the extreme loading conditions experienced during ridden work and competition. In fact, between 75 and 95 per cent of all tendon injuries in horses occur in the forelimb SDFT (Thorpe et al 2010). Tendon and ligament injuries pose significant challenges for the equine industry, affecting performance, finances, and the well-being of these magnificent animals (Shojaee 2014). Preventing such injuries in horses involves a combination of management practices and care.
The ArcEquine utilises microcurrent therapy –atype of electrotherapy – that introduces very low-level electrical currents into the body to support and aid the body’s own natural healing process. Microcurrents are found naturally in the body and bioelectrical impulses are fundamental to all communications between cells, organs, and tissues. The electrical currents are
vital to good health – not only in horses, but in all animals. Microcurrent therapy is drug-free, non-invasive, and well-evidenced. It has two predominant effects on the body; to reduce pain, swelling and inflammation, and to facilitate tissue repair. Many equestrians have used the ArcEquine to manage conditions including laminitis, navicular, and arthritic changes, in addition to increasing the recovery of soft tissue injuries such as tendon and ligament injuries.
Hannah Bailey purchased an ArcEquine device when her horse, Rosewater Danny Boy, sustained aSDFT injury while contesting the Badminton Grassroots Championships in 2022. “There was no hole, just damaged fibres, so Danny had a week of shockwave therapy followed by ArcEquine use,” Bailey said. “I was recommended the ArcEquine by my vet’s receptionist following her positive experience.
no extra treatment during this time. The repair between the six-week scans was solely from the ArcEquine.
“To say that we were all shocked is an understatement. My vets shared the scans with each other and couldn’t believe the repair! However, you can’t argue with what’s in a black and white scan image. Iwas given the go ahead to start walking and Danny is about to go and do his first intermediate I, which is mad considering he should just be coming back into full work now and was so close to completely ending his entire career if the tendon had blown.
“I have since sent the images to two friends who have both subsequently purchased an ArcEquine for their horses,” Bailey said.
ArcEquine has become the UK’s most popular equine microcurrent device with elite equestrians (including multinational Olympic Team members)
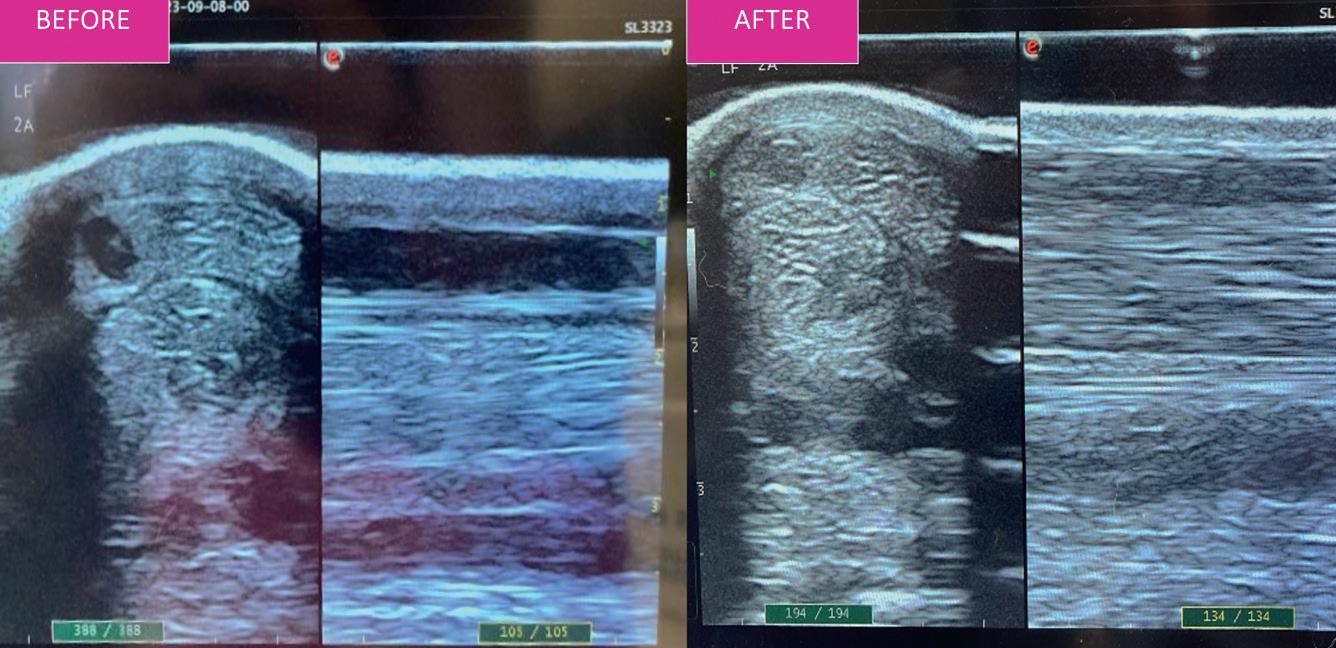
Beforeimage (left) taken on September 8 2023, and after image (right) on October 21 2023 –six weeks and one day apart.
“My vet was pleasantly surprised by the improvement on the second scan six weeks later and so Danny was able to return to work. Now, while this was amazing, the ArcEquine had its true value come into play last year when Danny sustained another SDFT injury.The scans showed a decent sized hole with just a few millimetres top and bottom before it fully ruptured, making it an incredibly worrying time.”
“Danny, meanwhile, isn’t a horse who will tolerate box rest, and he was eventing fit and suddenly out of work.
“He created his own entertainment in the field –much to my vet’s horror when she drove in one day to visit another horse,” Bailey said. “Danny had been written off for at least six months with a guarded prognosis about returning to work, to the point that we did discuss putting him to sleep if any further damage occurred as he isn’tahorse who will retire to a field. As Ididn’t have insurance cover I had to keep to ashoestring budget and therefore Danny had

and thousands of other equine enthusiasts worldwide now relying on ArcEquine to help with the wellbeing of their horses. The ArcEquine has helped customers to more effectively manage equine pain-related conditions and promote enhanced recoveryfollowing tissue damage, while also offers a maintenance programme to support ongoing health and fitness. The ArcEquine has numerous advantages over other devices on the market, relating to its ease of use, robustness, and wearability. Not only are the devices rechargeable and so fully reusable, multiple iterations and refinements of the products over the last 15 years have helped it evolve into a product that is compact and easy to use at the yard, without the need for clinical expertise. ARC Microtech has been built on family values and prides itself on its ethical, customer centric ethos. The Team is passionate, all of whom have seen first-hand the many benefits gained from using microcurrent therapy.Dedicated customer service is always available to provide ongoing support and advice.
References
1. Dyson SJ.Medical management of superficial digital flexor tendonitis: a comparative study in 219 horses (1992–2000). Equine Vet J.2004;36: 415-419.
2. Shojaee, A., 2023. Equine tendon mechanical behaviour: Prospects for repair and regeneration applications. Veterinary Medicine and Science, 9(5), pp.2053-2069.
3. Tang QM,Chen JL,Shen WL, et al.Fetal and adult fibroblasts display intrinsic differences in tendon tissue engineering and regeneration. Sci Rep. 2014;4:1-12.
4. Thorpe CT,Clegg PD,Birch HL.A review of tendon injury: why is the equine superficial digital flexor tendon most at risk? Equine Vet J. 2010;42:174-180.

Naomi Hansen BVSc MACVSc graduated from Queensland University in 1997. She worked in mixed animal practice in Queensland after graduation, before moving to Canberra to work for John Aspley Davis at Kippax Veterinary Hospital. She has completed aresidency in emergency and critical care at Melbourne University and was a resident in the same field at the Pennsylvania University Veterinary Hospital in the US. She is Veterinary Emergency & Critical Carein Sippy Downs, Qld. Hansen is a member of the Emergency and Critical Care Chapter of the ACVS.
Australia is home to some of the most venomous snakes in the world with the snakes known to be more active in the summer months (October to May). Retrospective human data suggests that 54% snake bites occurred around the victims’ home which makes their pets very susceptible.
In Australia approximately 550 people per year are admitted to a public hospital following a snake bite, of these people, an average of two will die from the bite or associated
complications. The brown snake has been implicated in the majority of these deaths (23/35 deaths from snake envenomation between 2000 and 2016 were attributed to brown snake envenomation).
The species more commonly associated with severe snake envenomation in domestic animals across Australia are the brown snake (Pseudonaja sp.), tiger snake (Notechis scutatus) and red-bellied black snake (Pseudechis porphyricus). This list is not exclusive and there are other snakes that
have been associated with morbidity and mortality in domestic animal species but they are less commonly reported. These ‘other’ snakes include the death adder (Acanthophis sp. ), copperhead (Austrelap sp .), eastern small eyed sake (Cryptophis nigrescens ), white lipped snake ( Drysdalia coronoides), black whip snake ( Demansia sp .), king brown snake (Pseudechis australis: note this is a member of the black snake family), spotted black snake ( Pseudechis guttatus), Taipan (Oxyuranus scutellatus).
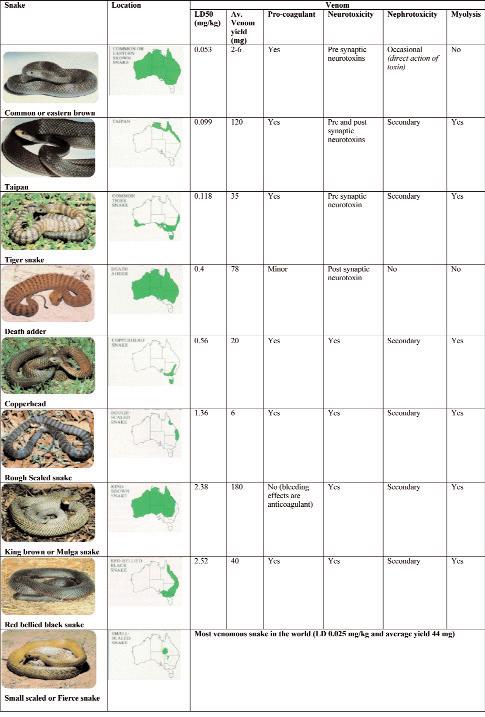
These ‘other’ snake species are less documented and for some (death adder and taipan) a specific antivenom is required. Tiger-brown antivenom is recommended for copperhead, eastern small eyed snake, white lipped snake and spotted black snake. Tiger-brown or CSL black snake antivenom is recommended for king brown envenomation.
Snake identification
Correct snake identification is essential to the correct management of snake envenomation
In veterinary practice, we often assume the species of the offending snake on the basis of geographical location and results of preliminary testing (i.e. PCV/TP, coagulation times, CK and AST).
This preliminary assumption is justified for two reasons:
■ Most snake envenomation patients are started with a vial of polyvalent (tiger-brown) antivenom.
■ The SVDK can take 30 minutes to return a result, this is a long time in an unstable patient.
BUT veterinarians should be more diligent in the use of snake venom detection kits (SVDKs), especially if there is clinical support for systemic envenomation and antivenom administration is required. Correct identification of the snake involved allows us to target our therapy with a monovalent antivenom.
SVDKs are considered 100% specific (i.e. a positive result is positive) but the sample timing and test technique may result in a false negative.
The reliability of the SVDK depends on the sample source and time lapse since the bite:
Venom (bite site or fang): The most reliable sample source
Urine: The protein binding of venom varies with the snake species so false negatives can occur if the urine concentration of venom is low (more likely to provide a positive response within 12h of envenomation)
oCats: may record a false negative result in the initial 5 hour period following envenomation
Blood: Read the directions carefully when testing blood (more likely to provide a positive response within 4 hours of envenomation
Knowledge of the offending snake species allows for better case management through:
■ Administration of the appropriate antivenom
■ Prediction of the clinical progression
■ Prediction of potential complications
SVDKs (Elisa test) can accurately identify the type of snake in 30 minutes of a bite
Clinical progression
The differential diagnosis for snake envenomation includes all forms of lower motor neurone paralysis/paresis (i.e. Tetrotoxins, tick intoxication, polyradiculoneuritis, organophosphate or carbonate intoxication, thromboembolic disease and meningitis/myelitis).
To differentiate these potential diagnoses from snake enveomation: the clinical onset of snake envenomation is generally acute, the progression rapid and is commonly accompanied by a coagulopathy.
Many of the clinical signs observed in human snake envenomation patients can be applied to domestic animals and will assist in the early detection of systemic envenomation:
<1 hr Headache, irritability, photophobia, nausea, vomiting, diarrhoea, confusion, coagulation abnormalities +/- hypotension and loss of consciousness (collapse). Collapse and vomiting may occur within minutes of a bite followed by an apparent ‘recovery’.
Aperiod of apparent recovery may be observed within 30 minutes of the bite, preceding the progression of clinical signs
1-3 hr Cranial nerve paralysis (dilatedpupils, salivation and respiratory distress), abdominal pain, haemoglobinuria, hypertension, tachycardia, haemorrhage
>3 hr Flaccid limb and respiratory muscle paralysis leading to respiratory failure, peripheralcirculatory failure (pallor and cyanosis), myoglobinuria and death.
Muscle destruction (myolysis) is associated with muscle tenderness and predisposes kidney failure.
The rate of progression is variable and depends on the patient body size, physiological status, snake venom potency and the dose of venom delivered.
Brown snake envenomation has been associated with an acute deterioration and death from severe cardiac depression (within 5 minutes of the onset of clinical signs)
Toxic components of snake venom
1. Neurotoxin
Neurotoxins act at the neuromuscular junction (NMJ) causing a progressive paralysis.
The initial effects of a neurotoxin appear 2-4 hours post envenomation (time taken for the venom to travel to the NMJ and attach)
Post-synaptic neurotoxins (tiger, brown, taipan and death adder) block neuromuscular transmissionby occupying the acetylcholine receptors at the motor endplate (this is reversible with antivenom)
Pre-synaptic neurotoxins (tiger, brown, taipan and rough scaled snake)block acetylcholine release and their onset is delayed 30-60 minutes (this is reversible with antivenom)
Mydriasis and slow pupillary light responses
Complete paralysis may take from 3-18 hours.
Upper respiratory dyspnea may occur before respiratory paralysis from paralysis of the tongue and pharynx. These patients often require intubation +/- temporary tracheostomy and may require a period of ventilatory support.
Antivenom: Severe pre-synaptic paralysis (tiger snake, taipan and rough scaled snake) will not be reversed by antivenom BUT post-synaptic paralysis (death adder) may be reversed by antivenom
2. Pro-coagulant
Pro-coagulants act as prothrombin activators (fibrinogen consumption).
The clotting mechanism is activated by the conversion of prothrombin is converted to thrombin and fibrinogen converted to fibrin
Rapid defibrination or fibrinogen depletion (< 30 minutes) results in a clinical coagulopathy in the presence of normal platelet numbers and function (prolongation of both PT and aPTT) Fortunately, fibrinogen levels are rapidly restored (within 3-4 hours), this means that an improvement (they do not need to be ‘normal’ merely improving)in fibrinogen or PT when tested 4-6 hours after administration of anti-venom supports neutralisation of the pro-coagulant effect and resolution of the coagulopathy.
Restoration of the consumed coagulation factors may take upto 24 hours sequential in clinc coagulation tests maybe prolonged for this period and there is no benefit from additional antivenom provided fibrinogen and PT levels are showing improvement at 4-6h.
IF the fibrinogen is persistently low when tested 4-6 hours after anti-venom administration thereis indication for administration of more anti-venom.
Coagulopathies associated with tiger snake envenomation may resolve spontaneously (12-18 hours)
Fibrinogen, FDP and D-dimer levels will facilitate identification of fibrinogen consumption and differentiate a defibrination coagulopathy from an anticoagulant coagulopathy (unfortunately these tests are not always available)
Antivenom: Antivenom is the only effective treatment for this coagulopathy (several vials may be required).
Allow at least three (4-6) hours to lapse before deciding if more antivenom is required (a drop in fibrinogen
after this period or progressive prolongation of PT suggests the need for further antivenom treatment)
3.Anticoagulant
Rapid reversible coagulopathy without defibrination. FDP and D-dimer negative.
Antivenom: is the only effective treatment and the response is rapid.
4. Nephrotoxin
There are NO isolated nephrotoxins in Australian snake venom BUT secondary kidney damage from Australian snake envenomation does occur.
Kidney damage is believed secondary tothe following mechanisms:
■ hypotension
■ myolysis
■ coagulopathy
5. Myotoxin
Myotoxins bind to the muscle fibres causing progressive destruction of the muscle cells.
The myolysis may take several hours tobecome clinically evident (creatinine kinase (CK) elevation and myoglobinuria)
The muscle damage cannot be reversed but the progression can be attenuated by antivenom administration
Patients show signs of progressive muscle weakness and pain
Muscle weakness must be differentiated from a flaccid neuropathy on neurological examination.
Clinical complications: Secondary renal failure, hyperkalaemia and hypocalcaemia.
Antivenom: Rapid resolution of clinical signs (weakness and pain) and a fall in CK (the halflife CK is 3-6h and AST 12 hours)
Medical management of snake bite
Critically ill patients
The initial approach to all critically ill patients is as easy as ABC … snake envenomation patients are no exception:
THERAPEUTIC AIM: Maximise oxygendelivery to the tissues (maximise oxygen uptake, oxygen carrying and oxygen delivery).
1. Airway and Breathing:
Neurotoxins may cause upper airway paralysis before respiratory paralysis, these patients will improve with intubation and may require a temporarytracheostomy.
Chronic dyspnea from a functional upper airway obstruction predisposes laryngeal oedema and pulmonaryoedema,complicating recovery
Airway support
Aim for a sPO2 >92-93% (FiO22 21%)and pCO2 35-40 mmHg
The ‘cut off’ values for ventilatory support are sPO2<60 mmHg (FiO2 21%)and/or pCO2 >60 mmHg
Serial sampling will allow early identification of ventilatory and/or respiratory failure (sPO2 trending down and/or the pCO2 trending up)
Early identification and management of respiratory and/or ventilatory complications will minimise future complications.
Intubate and ventilate with 100% oxygen if ventilator y or airway failureis evident on presentation.
2. Circulation:
Patients may present in shock (poor pulses, tachyarrhythmia, pale mucous membranes and hypotension)and require intravenous fluid resuscitation. Hypotension and renal hypoperfusion will contribute to renal failure post treatment. Rapid volume resuscitation from shock is essential.
Systemic envenomation patients should be connected to an ECG and monitored continuously until they are stable. ECG monitoring will assist in the early detection of arrhythmias associated with envenomation, electrolyte disturbances and/or antivenom reactions.
Brown snake envenomation is reported to cause cardiac arrest in humans.
Prior to initiating an intravenous fluid resuscitation regimen collect 2-3 mL whole blood and record the following baseline blood values (blood, except coagulation study sample, can be collected from the peripheral catheter):
1. Packed cell volume (%) and total protein (g/dL)
2. FRESH blood smear (platelet evaluation)
3. Serum colour
4. Serum glucose (mMol/L)
5.ACT (seconds) or PT/aPTT (seconds)
6. Lactate (mMol/L)
7.Electrolytes (Na+, K+, Cl-)
8. +/- CPK, BUN, Creatinine, blood gas and acid/base values
Collect another 2-3 mL of ‘pre treatment’ blood and store it appropriately for the following tests: CBC (EDTA tube), serum biochemistry (Lithium Heparin or Clot tube), FDP/D-dimer and/or fibrinogen levels.
● Blood may be collected via the peripheral catheter or saphenous vein (avoid using the jugular or cephalic veins for sampling in coagulopathic patients). If possible collect a ‘pre treatment’ urine sample (SVDK, USG, urine colour,dipstick and microscopic evaluation for casts).
● Voided or catheterised samples are preferred (avoid cystocentesis in coagulopathic patients)
● Repeat urine sampling may be required to monitor renal function. In paretic patients it may be beneficial to place a sterile indwelling urinary catheter at this time.
● In acute envenomations a repeat urine sample may be required to positively identify the snake species via a SVDK, iffa false negative is recordedinitially.
The frequency of subsequent testing (blood and urine) is determined by the results of the initial testing and the patient’s progress.
The snake venom detection kit (SVDK)
■ Sampling: The best sample for testing is a swab from the bite site
● Urine is a useful alternative but false negatives can occur (especially within the first 5 hours in cats
● Blood may be used (read directions carefully)
● If a dead snake is available a swab from the fangs may yield an accurate result
The SVKD is 100% specific (a positive result is a positive result) but false negative results can occur as a result of sample timing and testing technique.
Rules of intravenous catheter placement
Placement of an intravenous catheter is essential in the management of systemic snake envenomation
■ The following rules apply when placing an intravenous catheter:
1. ‘Threestrikes and you areout’ let another staff member have a go!
2. The vein order for peripheral catheter placement:
■ cephalic veins ➸ lateral/medial saphenous veins ➸ jugular veins
3. On all veins, start distally and work proximally along the vein
4. A peripheral cut down should only be attempted by an experienced staff member and only if necessary(remember to maintain sterility and bandage appropriately to avoid phlebosis)
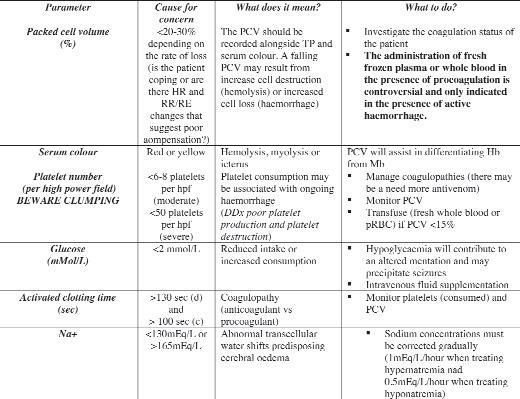
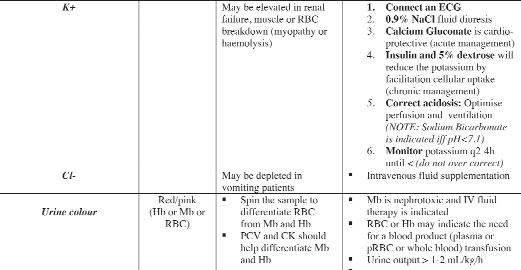
3. Fluid resuscitation or rescue phase:
Snake bite patients with acute systemic envenomation may present in circulatory ‘shock’,these patients require volume resuscitation as soon as possible.
Recently, fluid resuscitation techniques have been reviewed as the health of the endothelial glycocalyx can be affected by the rate at which fluid resuscitation is undertaken (i.e. the volume of fluid infused and time over which that infusion is actioned).
The type of crystalloid utilised for fluid resuscitation has also been under review with a trend away from 0.9%NaCl toward Hartmanns.
Fluid resuscitation or rescue:
● Hartmanns: Bolus therapy 10-20ml/kg (dogs) upto 90ml/kg/h and 5-7ml/kg (Cats) upto 60ml/kg/h
Monitor these patient’s q 10-15 minutes and reduce their fluid rate as they start to respond (HR, RR, thoracic auscultation, pulse quality and mentation)
Be careful not to overload them with fluids Patients that present in circulatory shock have a reduced capacity to perfuse their gastrointestinal tract, lungs, kidneys and brain. Rapid correction of their perfusion status is essential to minimise post treatment complications like renal failure, gastrointestinal ulceration and ARDs
Snake envenomation patients arein the ‘high risk’ categoryfor DIC
Monitoring intravenous fluid resuscitation is similar for all critical patients:
Blood Pressure: Record a baseline blood pressure (mmHg) and resuscitate to a MAP of 80-100 mmHg (do not over resuscitate)
Heart rate/Respiratory rate: Thoracic auscultation q 10-15 minutes during fluid resuscitation will assist in the early detection of a patient’s response and prevent over resuscitation. Resuscitate to a physiologically appropriate heart rate and cease resuscitation if pulmonary‘crackles’ areaudible
Oxygenation: Oxygen supplementation is indicated during resuscitation to maximise delivery to the tissues. Hyper or hypoventilation post envenomation will contribute to tissue hypoxia and acidemia. Supplement to a sPO2 of >95% , in severe cases this may require intubation and ventilation on 100% oxygen.
Pulse rate and character: Pulse character provides a crude evaluation of blood pressure. Areduction in pulse rate accompanied by an improvement in pulse character supports a favourable response to fluid resuscitation.
Packed cell volume/Total protein: Record a baseline PCV and TP, if either or both
ofthese are low monitor them q30-60 minutes as they will DROP during fluid resuscitation.
ECG: Continuous ECG monitoring will assist in the early detection of atrial or ventricular arrhythmias.
Lactate (if available): The serum lactate value is valuable indicator of perfusion. Adjunct or alternate to serial BP monitoring may be the implementation of a resuscitation regimen that ceases when the patients serum lactate is < 2.0 mMol/L
Donot over resuscitate snake envenomation patients as they may be renally compromised and may not be able to ‘deal’ with high volumes of intravenous fluids
4. Antivenom: The appropriate antivenom should be administered as soon as signs of enveno-mation are observed. Identification is often unreliable and snake venom detection kits (SVDK) should be used but if unavailable use Tiger snake antivenom in Tasmania, tiger and brown snake antivenom in Victoria and poly-valent antivenom in other states.
The amount of antivenom required depends on the amount of venom injected (the size of the snake, the number of strikes, the effectiveness of the strike and the fullness of the venom glands)
Antivenoms are prepared from horse serum (containing no more than 170 mg/mL equine plasma protein)
The risk of anaphylaxis is low (<1% in human literature but increases with prior exposure to horses, equine tetanus vaccines and a general allergic history)
Recent studies suggest more than one ampoule is required to neutralize the procoagulant effects of brown and tiger snakes and we routinely start with two vials in severe envenomations.
Antivenoms should be administered slowly (over 30-60 minutes) diluted in an isotonic intravenous fluid
Premedication: Not routinely used in veterinary patients
Serum sickness: Fever, rash, aching joints, renal impairment and a generalised lymphadenopathy that occurs in 10% people treated with polyvalent antivenoms (up to 14 days post treatment)
Medical management of human envenomations advocates intravenous adrenaline only for life threatening hypotension or anaphylaxis (its use has been associated with cerebral haemorrhage). Human literature suggests adrenaline, antihistamines and corticosteroids be administered only in the event of a clinical reaction
5. Analgesia and sedation
Opioid analgesia is advised
● Buprenorphine 0.01-0.02mg/kg q8h (SC/IV/IM)
● Methadone 0.2-0.3mg/kg q4-6h (SC/IV/IM)
● Fentanyl as a CRI
Snake envenomation can be very painful and we have been using combination CRI therapy to manage pain (i.e. Fentanyl/Lignocaine/ Ketamine) in patients that are clinically uncomfortable
Monitoring the snake envenomation patient post treatment
1. Blood tests: Monitor PCV/TS, Platelets, Serum colour,ACT,Glucose, Electrolytes, CPK, BUN, Creatinine, Acid/base and blood gas status q6-12h
2. ECG: Continuous monitoring is indicated until the patient is stable
3. sPO2: Monitor q2-4 until the patient is weaned off oxygen supplementation
4.BP: Monitor for hypotension q2-4 until the patient is stable
Management of hypotension: Volume expansion (HTS and/or colloids)
Vasopressors (iff the patient is normovolemic and ECG and BP monitoring is available)
5. Urine output: Monitor q4 until CPK stars to decline (the half life of CPK is 3.5 hours)
6. Urine composition: Dipstick and microscopic evaluation
Anti-venom
The number of units of neutralising capacity and ampoule volume varies between snake species
Administration:
1. Dilute antivenom up to 1 in 10 in an isotonic crystalloid (Saline, Hartmans or Dextrose)
2. Rate: 1vial over 15-30 minutes
3.Have adrenaline on standby in case of areaction
Brown snake venom: Defibrination coagulopathy (pro coagulant effects)
■ Indicators for antivenom treatment: coagulopathy and/or nephrotoxicty
■ There is a risk of cardiotoxicity (collapse, arrhythmias and cardiac arrest)
■ Avoid hypertension (risk of haemorrhage)
■ Platelets are not affected but platelet consumption and thrombocytopaenia have been observed following brown snake envenomation
■ FFP is contraindicated until all circulating venom is neutralised
■ Large amounts of antivenom (Humans: 2-6 vials) may be required to reverse the defibrination coagulopathy (allow 4hours before deciding to administer more antivenom and do not be guided by the PT/aPTT as these parameters may take 12 hours or longer to resolve)
Aretrospective survey published in March 1998 (Australian Veterinary Journal) raises a few issues pertaining to the veterinarymanagement of domestic animal snake envenomation: Few venom detection kits were used prior to the administration of antivenom
Many domestic animals are treated with antivenom on the basis of geographical location and snake distribution
Dogs are more sensitive to venom than cats (lethal dose tiger snake venom 0.1 mg/kg cats and 0.03 mg/kg dogs)✛
The severity of a patients presentation has an impact on the decision to treat
There are a variety of ancillary therapeutics instigated in the management of both cat and dog envenomations
✛ Barr SC. Clinical features therapy and epidemiology of tiger snake bite in dogs and cats. Aust Vet J 1984; 61:208-212
i MA Johnston et al. Successful recuscitation after cardiac arrest following massive brown snake envenomation. MJA Dec 2002; 17:646-649
* Tiger snake antivenom is a cheaper option for these species of black snake
Death adder venom:
Paralysis (post synaptic neurotoxin)
■ Indications for treatment: Paralysis
■ Paralysis starts with ptosis, spreads to the cranial nerves to peripheral muscles and may cause respiratory paralysis within 6hours if untreated
■ The use of anticholinesterases (eg. Neostigmine) may assist in management of post synaptic paralysis (more Ach available at NMJ may overcome blockade)
Taipan venom:
Paralysis (pre and post synaptic neurotoxin) Myolysis
Defibrination coagulopathy (pro coagulant)
■ Systemic envenomation is common post bite so antivenom is indicated in all Taipan bite patients
■ The paralysis and coagulopathy may be profound
■ Large amounts of antivenom (Humans: 3-8 vials)may be required to reverse the defibrination coagulopathy
Respiratory paralysis may occur within 2-4 hours of bite and complete defibrination within 1 hour of bite
Black snake venom: Myolysis
Coagulopathy (anticoagulant)
■ Indicators for antivenom treatment: Myolysis
■ Myolysis predisposes secondary renal failure and hyperkalaemia
■ Anticoagulant coagulopathy (prolonged bleeding time with a normal fibrinogen and no FDPs)
■ Paralysis is of little clinical significance
■ One vial of antivenom is usually sufficient
Tiger snake venom:
Paralysis (presynaptic paralysis)
Myolysis
Defibrination coagulopathy (pro coagulant effects)
■ Most tiger snake bites result in systemic envenomation
■ The paralysis appears to affect the head (ocular, facial and glossopharyngeal muscles) beforethe respiratory muscles
■ Presynaptic paralysis is NOT reversed by antivenom so early treatment (before onset of major paralysis) is indicated
■ Myolysis predisposes secondaryrenal failure and hyperkalaemia
■ Defibrination coagulopathy may spontaneously resolve (15-18 hours after envenomation)
All species from the Pseudonaja genus: Western brown snake, common brown snake, peninsula brown snake, Ingram’s brown snake, speckled brown snake, dugite.
All species from the Pseudechis genus: Mulga snake, spotted black snake, Collett’ssnake, Butler’ssnake, red-bellied black snake, Papuan black snake.
All species of the Notechis genus: common tiger snake, western tiger snake, peninsula tiger snake, Krefft’s tiger snake, Tasmanian and King Island tiger snake, Chapel Island tiger snake
Some species of black snakes*:Red-bellied black snake, Collett’ssnake, spotted black snake
Some copperheads (Austrelaps species): Lowland copperhead, highland copperhead, pygmy copperhead
Some broad headed snakes (Hoplocephalus species): Stephen’sbanded snake, broad-headed snake, pale-headed snake)
Rough-scaled snake
Maybe of some value in treating sea snake envenomation
All species from the Acanthophis genus: Common death adder, northern death adder, desert death adder
All species from the Oxyuranus genus: Irian Jaya taipan, coastal taipan, inland taipan, Papuan taipan




Inrecognition of World Menopause Day on October 18, WellVet, a not-for-profit initiative, run by Vetsnet CIC, has announced completion of its comprehensive suite of free menopause resources for veterinary team members. The 23 bitesize videos and audio include information and practical advice based on the pillars of lifestyle medicine and the neuropsychology of hormones and areaimedat both individuals impacted directly by symptoms of perimenopause and those wanting to support them.
Resources can be accessed at www.wellvet.co.uk/resources/me nopause-resources-for-veterinaryteams.
The site also includes links to additional resources, including ashort animation produced in collaboration with the University of Edinburgh raising awareness about the importance of this topic. As part of the project, WellVet Director, Liz Barton also
founded the peer-support group Veterinary Menopause Chats on Facebook, as a space for veterinary team members to share their experiences, knowledge, and ideas for help.
“We now know that for more than half of veterinary team members, perimenopause symptoms impact their mental health,” Barton said. “A third report a significant impact on their working life and career. Symptoms typically occur between the ages of 40–60 years, and can last for adecade or more with significant health impacts including cardiovascular, neurological and orthopaedic disease. We also know that misdiagnosis is common and women often wait until symptoms are severe and debilitating before seeking help. These videos will empower individuals to take control of their symptom monitoring, have meaningful conversations with medical professionals, and make adjustments to improve their
health and wellbeing. The content also provides guidance to help all of us support friends, family, colleagues and clients who may be impacted.
Barton believes perimenopause is the most significant health challenge the profession needs to focus on.
“We saw a significant positive shift in the way we think and talk about mental health and wellbeing through the 2010s,” she said. “Now we need the same to happen with menopause. In a predominantly female profession facing aworkforce crisis, it’s vital we support team members in the workplace. Perimenopause also coincides with the peak ages for women to die by suicide. We must do more to provide meaningful support.”
“I have to extend a huge thanks to the sponsors without whose support and encouragement these resources could not have been created. We would welcome additional support to continue
After 35 years of dedicated service to the pet-owning community, the Adelaide Animal Emergency and Referral Centre (AAERC) is embarking on an exciting new chapter. The centre will soon relocate to a new facility, adopting a new name as it continues its mission of providing exceptional care to the animals of Adelaide.
On October 28 AAERC will close its doors at the current location due to the construction of a new highway. It will reopen on November 1 as the Greencross Vet Centre in Norwood, co-located
with the Adelaide Veterinary Services & Referral Centre (AVSARC) at 102 Magill Road. This new location will be one of the only sites in South Australia offering a combined general practice, emergency, and referral veterinary service.
“We’re thrilled to be entering thisnew chapter with the opening of the Greencross Vet Centre in Norwood,” Di Whatling, Business Manager of Greencross Vet Centre said. “By co-locating our general practice, emergency, and referral services at the same location, we're making it easier
for pet owners to get comprehensive veterinary care without the need to travel between clinics.”
The new Norwood site has been expanded to accommodate both the team members and equipment from the Kurralta Park location. This expansion ensures a more integrated model of care, providing pet owners with easy access to routine checkups, emergency treatment, and specialist dermatology services — all under one roof. The upgraded facility is designed to meet the growing needs of the veterinary community in Adelaide,

developing and hosting these resources, and most importantly to encourage team members to access the content so they can give and receive support at this challenging life stage.”
WellVet is also exploring research collaborations to better understand the impact on veterinary team members. Anyone interested in getting involved or sponsoring the next phases of this vital work is warmly invited to contact liz@wellvet.co.uk.
offering a comprehensive, roundthe-clock solution for local pets.
Greencross Vet Centre will continue to provide its exceptional level of care in this state-of-the-art facility, with plans to serve the community for many years to come. The addition of GP services alongside the existing emergency care will ensure clients receive the highest-quality veterinary support in a seamless and convenient manner.
Greencross Vet Centre is part of the Animal Referral & Emergency Network (AREN), Australia's largest network of specialist and emergency veterinary sites, with 23 locations nationwide.

Businesses Club IT and Colourworks recently hosted the inaugural ‘Putt for the Playground; Charity Golf Day at Ocean Shores CountryClub, raising an impressive $2,000 to support the construction of a new playground at the Byron Bay Wildlife Sanctuary. The event attracted more than 50 enthusiastic golfers, all united by a shared commitment to giving back to the community.
The day kicked off with a bit of rain, but once the skies cleared, the participants
were treated to perfect golfing conditions. The event showcased the community's spirit and dedication, with golfers from various backgrounds coming together to support the Sanctuary’smission of providing a safe and engaging space for children.
“A huge thank you to everyone on the Club IT and Colourworks team for pulling together what sounds like a fantastic afternoon,”
Amanda Gorvin, General Manager of Byron Bay Wildlife Sanctuarysaid. “The Sanctuary is extremely grateful for your support and for choosing us to be your charity partner for the inaugural Golf Day.The new playground will be a wonderful addition to our facilities, providing a fun and engaging space for our young visitors.”
“Everyone seemed to have a really great day out golfing. Spirits were high, and the team’s passion and support were not unnoticed,” Cat Gerke, Marketing Manager of Byron Bay Wildlife Sanctuarysaid. “It means a lot to us, and the funds raised will really make a difference for the playground project. We are excited to see the positive impact this new playground will have on the families who visit us.”
The Charity Golf Day featured a range of activities, including longest-drive and closestto-the-pin contests, which added to the fun
and excitement of the event. Participants also had the chance to win raffle prizes generously donated by local sponsors, including items like a Dometic Esky, a Srixon Golf Bag, Callaway Ball Packs, and gift packs from East Ballina Amcal Pharmacy, Seven Mile Brewing, and Active Life Physio.
“This is our first time collaborating with another like-minded local business to give back to the community. We hope this golf day becomes an annual event, bringing even more support and joy to our local area,” Ben Smith, Manager of Club IT said.
The success of the event was made possible through the hard work and dedication of the Club IT and Colourworks teams, as well as the support of the local community and sponsors. The funds raised will contribute significantly to creating a wonderful new playground that will enhance the experience of visiting Byron Bay Wildlife Sanctuary for children and their families.
Club IT and Colourworks extend their heartfelt thanks to all participants, sponsors, and volunteers who contributed to making the day a resounding success. The collaboration and generosity displayed at the event are a true reflection of the community’s commitment to supporting local initiatives and making a positive impact.
Abstracts - microneedle patch
From page 14
Kushan Kompalage8, Christopher T Culbertson9,Ryan Jared Tucker8, Hans Coetzee8,Tsung Tsai2, Jeremy Powell2,Jorge Almodovar17 ACS Nano. 2024 Sep 17;18(37): 25716 -25739.doi: 10.1021/acsnano. 4c08072.
1Department of Biomedical Engineering, College of Engineering, University of Arkansas, Fayetteville, Arkansas 72701, United States.
2Department of Animal Sciences, University of Arkansas, B110 Agriculture, Food and Life Sciences Building, Fayetteville, Arkansas 72701, United States.
3Arkansas Integrative Metabolic Research Center, University of Arkansas, Fayetteville, Arkansas 72701, United States.
4Department of Mechanical Engineering, University of Arkansas, 204 Mechanical Engineering
From page 5
Data collation is coordinated by WHA from wild birds sampled from around Australia by program partners including biosecurity agencies, universities and DAFF’s Northern Australia Quarantine Strategy. Confirmatory testing occurs at CSIRO’s Australian Centre for Disease Preparedness (ACDP).
“We are pleased the response to the current H5N1 avian influenza threat has been a true ‘One Health’
Self-medicating chimps
From page 7
Another chimp with a parasitic infection was recorded consuming bark of the cat-thorn tree (Scutia myrtina).
Earlier studies demonstrated the ‘careful selection and ingestion of whole hispid leaves’ helped to expel internal parasites, while the bitterpith chewing was considered ‘phytochemical’ self-medication. Previous research also suggested dead wood may be a source of sodium where
From page 1
The study adds to a growing body of work that shows animals such as greylag geese can have consistent
Building, Fayetteville, Arkansas 72701, United States.
5Department of Biological Sciences, University of Arkansas, Fayetteville, Science Engineering Building, Fayetteville, Arkansas 72701, United States.
6Department of Civil Engineering, University of Arkansas, 4190 Bell Engineering Center, Fayetteville, Arkansas 72701, United States.
7Ralph E. Martin Department of Chemical Engineering, University of Arkansas, 3202 Bell Engineering Center, Fayetteville, Arkansas 72701, United States.
8Department of Anatomy and Physiology, College of Veterinary Medicine, Kansas State University, 213 CBC Building, 1212 MidCampus Dr North, Manhattan, Kansas 66506, United States.
9Department of Chemistry, Kansas State University, 228 Coles Hall, 1710 Denison Ave, Manhattan, Kansas 66506, United States.
approach from the Federal Government, with the $95m package allocated across environment, health and agriculture,” said Rupert Woods from Wildlife Health Australia.
“Wewelcome the $7m earmarked for WHA to support the H5N1 preparedness and response activities for wildlife, including surveillance. Surveillance will be paramount in the identification of H5N1, if and when it arrives on Australian shores.”
this mineral was otherwise scarce, but this latest study evaluated the pharmacology of two species of dead wood to determine if multiple functions or health benefits could be identified or confirmed.
The researchers said the study was one of the first to provide both behavioural and pharmacological evidence of the medicinal benefits to wild chimpanzees of feeding on bark and dead wood.
“As we learn more about the pharmacological properties of
individual differences in behaviour.
What is now also called personality was once considered a figment of human imagination – or anthropomorphism.
“But more than that, personality
From page 1
Dirofilaria immitis requires specific temperature conditions to mature within its mosquito vector and reinfect its host. The research found that suitable temperature conditions are not continuously met for locations where most Australians and their pet dogs live. The length of the disruption in the transmissibility of D. immitis varies greatly across Australia, and to some degree, between years.
The dashboard provides an indication of when the temperature conditions are most likely disabling the transmissibility of D. immitis for the 83 per cent of the Australian territory where transmission is not possible year-round. Veterinarians will be able to access when, and
Abstracts - genomic insights
From page 14
While antigenic gene clusters responsible for serogroups were identified, no clear trend was observed, and the gene cluster of LBUEL-A33 did not show homology with any sequenced Proteus serogroups. These results reinforce the understanding that this disease ismultifactorial, necessitating further research to unravel the mechanisms and underpin the development of control and prevention strategies.
Bruno Henrique Dias de Oliva1, Arthur Bossi do Nascimento1, João Paulo de Oliveira2,Gustavo Henrique Migliorini Guidone1, Beatriz Lernic Schoeps1,Luana Carvalho Silva1,Mario Gabriel Lopes Barbosa1, Victor Hugo Montini1,Admilton Gonçalves de Oliveira Junior2,Sérgio Paulo Dejato Rocha3
Braz J Microbiol. 2024 Sep 5.doi: 10.1007/s42770-024-01508-6.
1Laboratory of Bacteriology, Department of Microbiology, Center of Biological Sciences, State University ofLondrina, Rodovia Celso Garcia Cid, PO-BOX 6001, Londrina, 86051-980, Paraná, Brazil.
2Laboratory of Microbial Biotechnology, Department of Microbiology, Center of Biological Sciences, State University of Londrina, Londrina, Brazil.
3Laboratory of Bacteriology, Department of Microbiology,
plants ingested by chimpanzees in the wild, we can expand our understanding of their health maintenance strategies. This paper demonstrates how watching and learning from our primate cousins may fast-track the discovery of novel medicines, while also emphasising the importance of protecting our forest pharmacies,” Freymann said. Further information can be found at www.doi.org/10.1371/journal.pone.03 05219.
■ ANNE LAYTON-BENNETT
traits in animals can be linked to successful love matches and reproductive success. Therefore, these traits may be targets of natural and sexual selection,” Kleindorfer said.
■ ANNE LAYTON-BENNETT
dirofilariosis prevention plan for their canine patients and guardians.
Sydney Magazine Publishers Pty Ltd
ACN 102752787 ISSN 1447-9768
PO Box 6130 West Gosford NSW 2250 Tel: 0432 575 877
Publisher - James Martin
Email: james.martin@vetmag.com.au
Editorial Advisory Board
Thomas Donnelly BVSc DipVP DipACLAM
Nicholas Kannegieter BVSc
DipVetClinStud PhD FACVSc
David Lidbetter BVSc MVS FACVSc DipECVS Dip ACVS
Angus Martin BVSc
Mary Porter BVSc (Hons) MACVSc
Jeffrey Smith BVSc FACVSc Dip ACVO
David Vella BSc BVSc (Hons) DABVP
Designer - Anne Norrell Email: annenorrelldesign@gmail.com
To have your say, email editor@vetmag.com.au
Printed by Newstyle Printing 41 Manchester St, Mile End SA 5031 Post Print Approved PP255003/06488
All material in The Veterinarian is subject to copyright and must not be reproduced wholly or in part without the written permission of the Editor.
Views expressed in The Veterinarian are not necessarily those of The Veterinarian or Sydney Magazine Publishers Pty Ltd.
Subscriptions - Clem Martin Tel: 02 9487 6627 Email: clem.martin@vetmag.com.au
Mail POBox 6130 West GosfordNSW 2250
Phone (02) 9487 6627 www.theveterinarian.com.au
for how long, heartworm may be transmitted at a specific location, assess the associated risk of infection and advise on a patient-dependent
The dashboard can be found at heart worm-mapping.adelaide.edu.au/shiny.
■ JULIAGARDINER
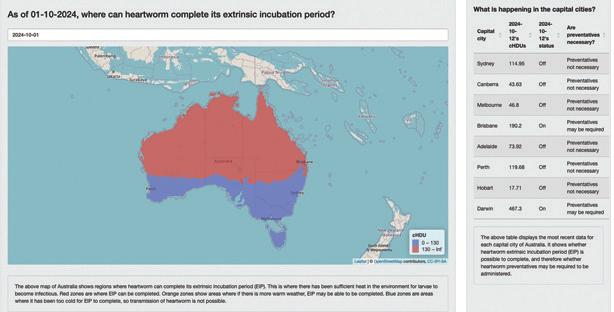
From page 1 international conservation. As a founding member of the International Rhino Foundation (IRF), Taronga actively supports efforts to save rhinos in Africa, Indonesia, and India through anti-poaching units, habitat protection, and veterinary expertise.
“Taronga Western Plains Zoo is the only institution outside of the African continent that is successfully breeding the critically endangered southern black rhinoceros, so ever y birth is critical,” Taronga Chief Executive Cameron Kerr AO said.
CREATURE Feature

Greatwhiteshark( Charcharodoncarcharia s)
FamedbadguyintheJawsseriesofblockbusters,thegreatwhiteistheonlysurvivingspecies ofitsgenusandcanbefoundincoastalsurfacewatersofallmajoroceans.Greatwhitesare oneofthelongest-livedcartilaginousfishesknown,withlifespansestimatedatupto70years.
Theonlypredatorthegreatwhitehasistheorca.

