

THE NEW HEALTHCARE REVOLUTION




















































WELCOME TO HEALTHCARE WORLD
Welcome to the latest edition of Healthcare World. We’re looking forward to seeing you all at Abu Dhabi Global Health Week, which brings together some of the most influential experts from across the globe, and we are eager to engage in the many conversations that will shape the future of healthcare. This year, we have curated an exciting and dynamic programme of panels and speakers on the Live Stage in Hall 6. On pages 42-45 you’ll find our full schedule, highlighting the exceptional thought leaders who will be addressing the key topics healthcare.
The focus for Abu Dhabi Global Health Week this year is Wellness and Longevity. As the world population ages and health awareness grows, wellness and longevity have become central to the way healthcare is approached. Experts are increasingly turning their attention to preventative care, lifestyle interventions, and innovative treatments aimed at extending healthy life expectancy.
Vincent Buscemi of Bevan Brittan explores longevity in detail (pgs 30-33), examining how countries are incorporating longevity into their health prevention models. Graham Cookson of the O ice of Health Economics explains how the OHE helps drive smarter healthcare spending. For Hill Dickinson, the aims of longevity science and value-based healthcare align perfectly - longevity science is not only a solution to enhance quality of life but also a way to improve healthcare e iciency. By focusing on maintaining health through innovative science and technology, longevity e orts can ultimately reduce the long-term burden on healthcare systems.
Clinical trials that leverage new research also deliver important results, as Dr Emer MacSweeney reveals as she discusses her work in new treatments for Alzheimer’s disease and dementia on pages 44-46 and also in one of our healthcare panels on stage on 16 April on the Live Stage.
The shi toward value-based healthcare (VBH), which emphasises improving patient outcomes






SARAH CARTLEDGE EDITORIAL DIRECTOR

while controlling costs, is a key area of focus in all this. Methven Forbes, CEO of Fuller and Forbes Healthcare, explains why he feels value may not mean what we think it means on pages 52-55. And don’t miss our expert panel on Personalised Medicine / Population Health and the Preventative Agenda - Who Pays the Bill, where Methven and other experts will be discussing the issues on 16 April.
Digital health and data continue to play a crucial role in all these developments. Browne Jacobson (pgs 6264) draws a parallel with the rise of digital banking apps, highlighting how patient self-management systems could revolutionise the way individuals manage their health. individuals to take control of their well-being in ways that were once unimaginable.
Data experts Burendo (pgs 72-73) reveal how they are using these insights to drive national healthcare projects such as the UK Health Security Agency data dashboard and tracking cancer waiting times. Mohammad AlUbaydli, CEO of Patients Know Best, digital health expert and author of 7 books about the digital health experience, discusses the role of the patient and their involvement in the digital health ecosystem on pages 58-59, and chats to Steve Gardner on the Live Stage in Hall 6.
As we continue to explore the future of healthcare, we remain committed to presenting the latest trends, insights, and solutions that are shaping the sector. In Opinionated, our MD Steve Gardner reveals the new Healthcare World discussion series that will deliver actionable insights to improve patient outcomes on a global scale.
Steve is also hosting HealthBeats, the Abu Dhabi Global Health Week podcast, speaking to global leaders in healthcare. The first of these exclusive interviews with Professor Nicholas Crisp, Deputy Director General National Health Insurance South Africa, is on pages 48-50.
As always, thank you for joining us in these exciting conversations, and we look forward to sharing more insights with you in the coming months.
sarah@healthcareworld.com








The need for a shi from a reactive, sickness-focused healthcare system to one that promotes
The
Guy’s
has never been more urgent, says Vincent Buscemi, Partner and Head of Independent Health and Care at Bevan Brittan

Seating is a critical component of workplace wellness, says Ben Caton, Managing Director at Ergochair
Graham Cookson, CEO, tells Healthcare World how the O ice of Health Economics helps drive smarter healthcare spending 38 VALUE-BASED APPROACHES TO LONGEVITY
The aims of longevity science dovetail neatly with those of value-based healthcare, say Robert McGough, Partner, and Gemma Badger, Senior Associate Hill Dickinson LLP
Meet the experts on the Live Stage in Hall 6 at Abu Dhabi Global Health Week, chaired by Healthcare World’s CEO Emma Sheldon MBE and MD Steve Gardner
CREATING THE BREAKTHROUGH FOR ALZHEIMER’S DISEASE TREATMENTS
Dr Emer MacSweeney, CEO Re:Cognition, tells Healthcare World about the promise of diseasemodifying treatments for neurological conditions
HEALTHBEATS - REFORMING THE SOUTH AFRICA HEALTH SYSTEM
Professor Nicholas Crisp, Deputy Director General, National Health Insurance, discusses the country’s e orts to implement a National Health Insurance (NHI) system with Steve Gardner, Healthcare World Managing Director
TALKING POINT – SARAH CARTLEDGE,
Encouraging men to
Value may not mean what we think, says
Enabling patients to understand their own health information to make informed decisions is paramount, says Mohammad Al-Ubaydli, CEO of Patients Know Best
& AI
58 DEVELOPING RELIABLE HOSPITAL PERFORMANCE BENCHMARKING
Julie Coope, Associate Director BRG, Simon Swi , surgeon and data expert, and Simon Jones PhD, Professor of Population Health at New York University, discuss how to harness data e ective

62 BRIDGING THE DIGITAL DIVIDE: HOW HEALTHCARE CAN LEARN FROM BANKING
Digital banking apps point the way forward for patient self-management to improve healthcare, believe Gerard Hanratty, Head of Health and Life Sciences, and Carly Caton, Partner, at UK and Ireland law firm Browne Jacobson
65 CONVOY OF HOPE
Delivering medical aid, equipment and food to Ukraine
66 LEVERAGING AI FOR HEALTHCARE EDUCATION
AI can help tailor training programmes for the individual to maximise e iciency, says Nick Dobrzelecki, co-founder of The Learnery
70 MEETING THE DEMANDS OF THE HEALTHCARE LANDSCAPE
Upinder Bhat, President and COO DVI Health Solutions Inc, tells Healthcare World about their innovative work in the sector
72 DRIVING TRANSFORMATION IN HEALTHCARE DELIVERY
Burendo is playing a pivotal role in the successful delivery of complex and high-profile national programmes, founder and CEO Glenn Crossley explains to Sarah Cartledge, Healthcare World Editor
76 TAILORED SPACES IMPROVE LIVES
Alastair Demick, Managing Director of Safespaces, tells Healthcare World about the profound impact tailored environments can have on people of determination and their families
78 OPINIONATED – STEVE GARDNER, MD
HEALTHCARE WORLD
Star gazing – Middle East healthcare by 2040
Advancing healthcare globally
At Guy’s and St Thomas’ Consulting, we transform healthcare delivery with clinical expertise from five of London’s world-leading hospitals: Evelina London Children’s, Guy’s, Harefield, Royal Brompton, and St Thomas’.


NEWS
WHO AND AI
The World Health Organization (WHO) has designated the Digital Ethics Centre at Del University of Technology in the Netherlands as a WHO Collaborating Centre on artificial intelligence (AI) for health governance.
The WHO Collaborating Centre designation recognises the Digital Ethics Centre at Del University of Technology’s decadeslong history of cutting-edge research on responsible innovation, and its leadership in incorporating ethical values into design requirements for digital technologies. This inauguration marks the continuation of a strong partnership between the Digital Ethics Centre and WHO with the two entities jointly organising international consultations, workshops, and the development of normative guidance and training in the past.
“WHO is committed to helping Member States plan, govern, and adopt responsible AI technologies,” said Dr Alain Labrique, Director of Digital Health and Innovation at WHO.
The Collaborating Centre on AI for health governance will be instrumental in WHO’s e orts to ensure the ethical and responsible use of AI for health by advancing research on priority topics and providing expert input for WHO’s guidance development and policymaking. The Centre will serve as a hub for

MOLLY CARTLEDGE ANALYSES THE LATEST NEWS ACROSS THE HEALTHCARE SECTOR

education and advocacy for science-driven research and facilitate knowledge-sharing and training through regional and countrylevel workshops.
“The fruit of two decades of research in digital ethics and responsible innovation, the Del Digital Ethics Centre is one of the frontrunners in operationalising ethical values into design requirements for digital technologies such as artificial intelligence,” Professor Jeroen van den Hoven, Scientific Director at Del Digital Ethics Centre noted.
The Responsible and Ethical AI for Healthcare Lab, a collaboration between Del University of Technology and its partners, will provide valuable insight into
MAKING YOUNG MEMORIES
Agroundbreaking study has revealed that babies as young as one year old can store memories in the hippocampus, a key brain region associated with memory formation. This discovery sheds new light on early cognitive development, although it does not yet explain why these early memories are inaccessible to adults, a phenomenon known as “infantile amnesia.”
The study, led by Dr. Nick Turk-Browne, a psychology professor at Yale University, used advanced brain imaging to track the memory processes in infants. The research, published in Science, found that babies can recall and react di erently to images they’ve seen before, suggesting the formation of memory around one year old. “This tells us something about how the brain develops
and what kinds of learning are prioritised in infancy,” said Dr. Turk-Browne.
The mystery of why we forget early childhood memories has long intrigued scientists. “What’s exciting here is that we now have evidence that the hippocampus in human infants is capable of storing memories,” Dr. Turk-Browne explained. The

the challenges involved in the successful implementation of WHO guidance in clinical practice. “The designation of the Digital Ethics Centre at Del University of Technology as a WHO Collaborating Centre strengthens our collective ability to ensure AI serves public health equitably and responsibly. This collaboration will play a critical role in supporting Member States to navigate the opportunities and challenges of AI, fostering trust, transparency, and innovation in digital health,” said Dr David Novillo-Ortiz, Regional Adviser and Unit Head for Data, Evidence and Digital Health at WHO’s Regional O ice for Europe.
study involved 26 infants aged 4 to 25 months, with half being under one year old. The babies were shown faces, objects, and scenes they hadn’t encountered before, while their brain activity was monitored using functional MRI (fMRI), a technology that detects brain activity by measuring blood flow changes.
The key innovation in the study was making it possible for babies to remain awake and engaged during the MRI scans, despite their short attention spans and tendency to move. The babies were comfortably nestled in a special vacuum pillow, with parents nearby to help them stay calm.
As the study progresses, researchers are investigating long-term memory by having parents record weekly videos of their babies and bringing them back for periodic MRI scans. This ongoing research aims to uncover how infants develop memory over time.

COMBINATION OF CHOLESTEROLLOWERING DRUGS COULD SAVE THOUSANDS OF LIVES
Anew study has revealed that a combination of two cholesterollowering drugs could significantly reduce deaths from heart attacks, strokes, and other cardiovascular diseases, potentially saving thousands of lives each year.
Published in the journal Mayo Clinic Proceedings, the research examined data from more than 108,000 patients at high risk of heart attacks or strokes, or those who had already experienced one. The study found that combining a statin with another drug,

AI-POWERED RAPID TEST SET TO REVOLUTIONISE COPD DIAGNOSIS
Agroundbreaking AI-powered test is poised to transform the diagnosis of chronic obstructive pulmonary disease (COPD), a lung condition a ecting 3 million people in the UK. Currently, twothirds of those with COPD are unaware of their condition, despite it being the second most common cause of emergency hospital admissions.
Traditionally, diagnosing COPD requires a spirometry test, which involves forced exhalation and can take over 30 minutes, along with a wait for an appointment. However, Sky News reports that a new rapid test, called N-Tidal Diagnose, promises a much faster and more accessible solution.
ezetimibe, was far more e ective at lowering levels of ‘bad’ cholesterol (LDL-C) than statins alone. This combination not only reduced cholesterol more e ectively but also led to a marked reduction in death rates.
Statins have long been used to prevent heart disease by reducing cholesterol production in the liver. Ezetimibe works by blocking the absorption of cholesterol in the gut, providing a complementary e ect when statins aren’t enough.
The findings showed that patients who were given both drugs from the outset saw a 19% per cent reduction in overall risk of death, a 16 per cent reduction in cardiovascular-related deaths, and nearly 20 per cent fewer major cardiovascular events, including heart attacks and strokes, compared to those on high-dose statins alone.
Globally, cardiovascular diseases claim 18m lives annually, with high LDL-C
Developed by TidalSense, this device allows patients to receive a diagnosis in as little as five minutes.
Dr. Simon Rudland, a GP in Su olk, is enthusiastic about the potential of the N-Tidal Diagnose to improve patient care. “Spirometry is delivered out of a hub, so patients have to travel,” he explained. “With this test, I can instantly begin treatment, avoiding delays and unnecessary medication.”
The AI-powered sensor works by analysing a patient’s breath. Patients breathe normally into a handset, which measures carbon dioxide levels and sends the data to a cloud platform where it is instantly analysed by AI so ware. This innovation helps to distinguish COPD from conditions like asthma, heart failure, and lung cancer.
The device is already approved for use across the EU and is expected to be rolled out in doctors’ surgeries in the coming weeks. Dr. Ameera Patel, CEO of TidalSense, revealed that the company has trained its machine learning model using data from
responsible for 4.5m deaths in 2020, according to the World Health Organization. The study’s lead author, Professor Maciej Banach, estimates that widespread adoption of combination therapy could prevent more than 330,000 deaths each year among patients who have already su ered a heart attack.
The research also found that combination therapy significantly improved patients’ ability to reach the target cholesterol level of under 70 mg/dL, with an 85 per cent increased chance of success.
Historically, doctors have prescribed statins first and added ezetimibe only if needed. However, this new evidence suggests that high-risk patients should begin both treatments immediately. “This study confirms that combined therapy should be the gold standard for very highrisk patients a er an acute cardiovascular event,” says co-author Professor Peter Toth.
The findings could lead to changes in treatment guidelines, o ering both a clinical and economic benefit by preventing the long-term costs of untreated cardiovascular conditions.
more than 2.5m patient breaths, improving its diagnostic accuracy.
For patients like Colin Best, 67, who struggled for years with a delayed diagnosis, this test could provide immediate relief. “It took me a year to convince them there was something seriously wrong,” he said. “With this machine, it’s only five minutes.”
This new technology is expected to alleviate pressure on the NHS by speeding up diagnoses and reducing the need for costly tests.

Fight the forgetting curve
The LearneryTM is a unique microlearning platform that revolutionizes the way health professionals train and upskill. Unlike traditional learning models that deliver large amounts of information all at once, The Learnery breaks content into microlessons and repeats them, so they’re easier to digest and remember.
Up to 70% of what we learn is lost after 24 hours.*
*Ebbinghaus Forgetting Curve
• More effective training & knowledge retention
•Improved compliance
• Enhanced employee confidence & satisfaction
• Reduced employee frustration & turnover




EXPERTS ENTER FOURTH DIMENSION TO CREATE BETTER MEDICAL DEVICES
Experts at the University of Birmingham and Imperial College London have launched a project aimed at revolutionising medical device engineering by incorporating a fourth dimension—time— into design to achieve new functionality.
The 4D Health Tech initiative addresses a critical gap in medical device design: neglect of time-dependent changes in the human body. Traditional medical devices fail to account for growth, movement, and tissue regeneration or degeneration, leading to compromised functionality and shortened lifespan.
For example, paediatric implants do not grow with the child and must be regularly changed. Stoma bags leak because they do not fully conform to skin folds. Bone implants do not predictably degrade as surrounding tissues regenerate.
Backed by £1.2m of UKRI Engineering and Physical Sciences Research Council (EPSRC) funding, the three-year Network Plus aims to position the UK at the forefront of healthcare innovation. Focusing on delivering improved patient outcomes, reducing healthcare costs, and driving more UK innovation in the medical device sector.
Funded as part of a wider £10m investment responding to the national report ‘Tomorrow’s Engineering Research Challenges’, the project will create a network connecting academics, businesses, clinicians, patients and policymakers. This collaboration will serve as a springboard to create bigger, longer-term research projects.
“Our bodies change over time as we grow, move and regenerate, but products designed to replace or repair our bodies typically neglect the dimension of time, compromising their function and lifespan,” says project lead Dr Sophie Cox, from the University of Birmingham, which is ranked amongst the world’s top 100 institutions. Its work brings people from across the world to Birmingham,

including researchers, teachers and more than 8,000 international students from over 150 countries.
.
“We believe that this groundbreaking initiative will position the UK at the forefront of healthcare innovation – as well as helping to improve patient outcomes, reduce healthcare costs, and foster innovation in the medical device sector. Our vision is to transform the way we engineer medical devices. Fostering connections across the supply chain will create a new culture of 4D Health Tech embedding innovative thinking, patient perspective and diversity - ensuring this new age of medical devices o ers improved healthcare outcomes for everyone.”
The project aims to promote the use of innovative materials that degrade predictably and promote faster healing and combine this with expertise in cutting edge automated design, advanced manufacturing processes and patient specific pre-clinical testing to create better medical devices that cater to diverse populations.
The project is led by a team of distinguished researchers from both universities, including Professor Andrew Dove (materials), Dr Sophie Cox (manufacturing), Professor Michael Bryant (testing), Dr Samantha Cruz Rivera and Dr Sarah Hughes (clinical outcomes), and Imperial design experts Professor Robert Hewson and Dr Connor Myant.
“Engineering is the cornerstone to a more sustainable, successful and thriving future for the UK. From developing renewable energy solutions to creating smart cities, engineering innovations are driving progress in every sector,” says Jane Nicholson, Executive Director for Research at EPSRC, the main funding body for engineering and physical sciences research in the UK.
“These new networks will address the strategic challenges outlined by the TERC report. Together, these researchers present a hugely ambitious, thoughtful response to the economic, environmental and social challenges we all face.”







Hill Dickinson’s health and life sciences team provides practical, commercial legal advice to public sector organisations, regulators and businesses at all stages of development, from start-up to established multinational. The firm has a strong international focus and has been supporting healthcare clients looking to work in the Middle East region for many years.
Working with our trusted local partners, BLK Partners, we can support you to exploit opportunities in the region. An understanding of the legal landscape will be essential for you, and we can help make connections and provide access to local expertise on key legal issues including:
For an initial discussion please contact:
Rob McGough Partner
+44 (0)113 487 7972 robert.mcgough@hilldickinson.com


• Regulatory compliance, licensing and permits
• Intellectual property protection and exploitation
• Information governance, data protection and hosting

• Employment rules and residency
• Distribution and reselling agreements
• Public procurement
• Investments and transactions.

Jamie Foster Partner
+44 (0)20 7280 9196 jamie.foster@hilldickinson.com



UKHSA PATHOGENS THREAT LIST
The UK Health Security Agency (UKHSA) has released an essential new tool aimed at guiding future medical research and development to prepare for the public health threats of tomorrow. This list, featuring 24 pathogen families, highlights the infectious diseases and viruses considered to pose the greatest potential risks to both the UK and global populations.
The comprehensive list is designed to inform strategic investment in diagnostics, vaccines, and therapeutics. By assessing the pandemic and epidemic potential of these pathogens, the UKHSA hopes to accelerate the development of countermeasures and increase preparedness for future health crises.
The list, which includes both well-known and emerging pathogens, provides insights into diseases that could threaten public health in the years ahead. Among the viral families that have been highlighted are the Coronaviridae family (which includes COVID-19), the Paramyxoviridae family (including the highly dangerous Nipah virus), and the Orthomyxoviridae family, which encompasses avian influenza. These pathogens are particularly concerning due to their ability to spread rapidly and cause severe disease, with the potential for significant public health and economic impacts.
The UKHSA’s tool does not rank the pathogens but instead o ers a snapshot of the threat posed by each, with ratings of high, moderate, or low based on pandemic and epidemic potential. These assessments are based on the nature of transmission, disease severity, and the potential impact on public health. The list also includes bacterial pathogens such as Gonorrhoea, which is showing increasing resistance to existing antibiotic treatments.
It will be updated at least once a year, to avoid a repeat of the Covid pandemic, where experts had been planning for an entirely di erent outbreak - influenza. “This guide is vital for both industry and academia, providing a clear focus on where scientific research can be targeted to enhance the UK’s preparedness for health threats. Our hope is that this will speed up the development of vaccines and diagnostics in areas where they are most needed,” says Dr Isabel Oliver, Chief Scientific O icer at the UKHSA.
Pandemic preparedness
The UKHSA’s pathogen prioritisation exercise is part of a global e ort to understand and prepare for diverse pandemic threats. Professor Mark Woolhouse, Director of the Tackling Infections to Benefit Africa programme at the University of Edinburgh, praised the initiative, saying, “Since the COVID-19 pandemic, there have been many e orts to better understand
the variety of pandemic threats that the UK and the world may face. The UKHSA’s pathogen prioritisation work is an important contribution to this ongoing global research.”
The focus on zoonotic diseases—those that can jump from animals to humans— remains a critical component of this research. Dr. Oliver highlighted that the UKHSA will consult with animal health colleagues to keep the list updated, as many emerging infectious diseases have an animal origin.
The tool supports the UK Biological Security Strategy and is one of several measures the UKHSA is using to protect public health. The UKHSA’s Vaccine Development and Evaluation Centre and Diagnostic Accelerator are working with academia and industry to prepare for pathogenic threats.
The List of 24 Pathogens
1. Adenovirus
2. Lassa fever
3. Norovirus
4. MERS (Middle East Respiratory Syndrome)
5. Ebola (and similar viruses, such as Marburg)
6. Flaviviridae (including dengue, Zika, and hepatitis C)
7. Hantavirus
8. Crimean-Congo hemorrhagic fever
9. Influenza (non-seasonal, including avian)
10. Nipah virus
11. Oropouche virus
12. Ri Valley fever
13. Acute flaccid myelitis
14. Human metapneumovirus (HMPV)
15. Mpox
16. Chikungunya
17. Anthrax
18. Q fever
19. Enterobacteriaceae (such as E. coli and Yersinia pestis, which causes plague)
20. Tularaemia
21. Moraxellaceae (which cause lung, urine, and bloodstream infections)
22. Gonorrhoea
23. Staphylococcus
24. Group A and B Streptococcus

MUSHROOMS COULD HELP MANAGE TYPE 2 DIABETES
Anew study suggests that eating mushrooms could help manage Type 2 diabetes by improving insulin sensitivity, a key issue for diabetics. Researchers at Semmelweis University in Budapest found that edible fungi contain compounds that can enhance the body’s response to insulin, potentially o ering a natural alternative for diabetes management.
“Our study reveals the remarkable potential of natural compounds in mushrooms to address key metabolic pathways, “ says Dr. Zsuzsanna Németh, who led the study. The findings could be significant for the global millions living with Type 2 diabetes, a condition o en caused
by being overweight and consuming an unhealthy diet.
Type 2 diabetes occurs when the body’s cells develop resistance to insulin, a hormone produced by the pancreas that helps convert sugars from food into energy. This reaction leads to elevated blood sugar levels, which can increase the risk of heart disease, stroke, kidney disease, vision loss, and amputations.
The research team highlighted the potential of medicinal mushrooms as part of a non-pharmacological approach to disease prevention. Previous studies have shown that fungi contain medically important compounds, such as polysaccharides, terpenoids, phenols, and heterocyclic amines, which have various health benefits, including
anti-inflammatory and anti-diabetic e ects.
Among the most promising findings was the e ect of polysaccharides in white button mushrooms, which have been shown to improve gut bacteria and support healthy glucose metabolism. Lion’s Mane mushrooms also contain antioxidants, while shiitake mushrooms have compounds linked to lowering blood glucose and reducing inflammation.
Dr. Németh and her team concluded that mushrooms, particularly medicinal varieties, could play an important role in complementary therapies for obesity and Type 2 diabetes, helping to manage insulin resistance and improve overall health.
The research was published in the Journal of Molecular Sciences and adds to the growing body of evidence supporting the health benefits of mushrooms in managing chronic conditions.


MEET THE CEO
RECAI SERDAR GEMICI
ALBERT HEALTH
IMPROVING LONG-TERM OUTCOMES FOR PEOPLE LIVING WITH CHRONIC CONDITIONS
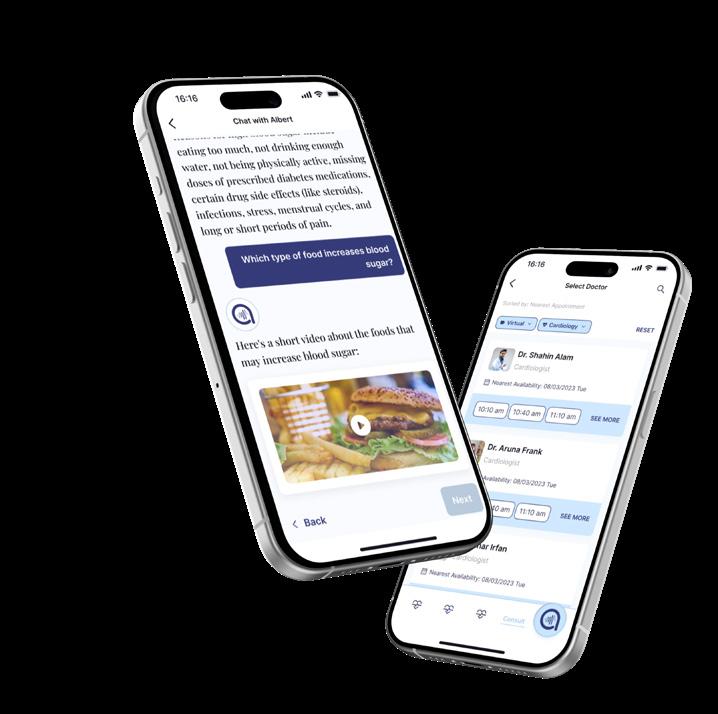
Albert Health is at the forefront of transforming healthcare by shifting the focus from traditional, reactive care to a more proactive, patient-centred model. Founded in 2018 in the UK by Recai Serdar Gemici, Albert Health is dedicated to empowering patients through innovative digital solutions that enable them to take an active role in managing their health. This approach is made possible through cutting-edge technologies such as AI-based health assistants, wearable devices, and mobile applications, which provide patients with real-time access to health data, personalised care recommendations, and continuous support.
With more than 250,000 patients reached so far, Albert Health is reshaping the way individuals engage with their healthcare. The company’s flagship AIpowered assistant, Albert, offers tailored advice, reminders, and real-time guidance, ensuring patients stay on track with their treatment plans. This personalised, 24/7 support enhances patient self-management and improves health outcomes, particularly for those with chronic conditions.
Albert Health is also deeply committed to advancing medical science through rigorous research and clinical trials. The company is currently involved in multiple trials, including one that demonstrates the efficacy of its AI-based coaching in improving HbA1c levels in type 2 diabetes patients. By combining technology, clinical expertise, and evidence-based practices, Albert Health is creating a more inclusive, efficient, and sustainable healthcare system that puts patients at the heart of their care.
What was it that made you want to pursue a career in healthcare?
My journey into healthcare started with a simple observation: people living with chronic conditions face more than just medical challenges—they deal with uncertainty, complexity, and a constant need to stay on top of their treatment.
That became even more real to me through my own family. My mother lives with diabetes and hypertension, and my father has atrial fibrillation. Seeing how much effort it takes to manage these conditions every day made me realise how much support is missing outside of clinical settings.
Earlier in my career, I developed a strong interest in health economics while working in the pharmaceutical industry. Later, during my time in technology and strategy
roles, I began to see the potential of digital tools to fill those everyday gaps in care.
Together with my co-founders, we saw an opportunity to build something more meaningful—something that could offer patients continuous, personalised support and improve how chronic care is experienced.
We believed healthcare needed new thinking—and we were ready to build something that could truly make a difference.
Describe your career journey to date. I studied Industrial Engineering and started my career at Microsoft. Later, I worked in the pharmaceutical industry and then joined Siemens, where I led strategy and business development projects. That’s also where I met my cofounders.
We were part of an innovation group exploring how to drive change inside large organisations. Over time, we found ourselves drawn to healthcare. It was clear that digital solutions could play a much bigger role in supporting patients
and improving care. That shared interest is what led us to create Albert Health.
Since 2018, we’ve been focused on one mission: helping people manage chronic conditions and improve their quality of life—through Albert, our evidence-based, personalised digital health platform that leverages AI.
Why is your offering so important to the healthcare sector?
Chronic diseases are a long-term challenge—both for individuals and for healthcare systems. Managing them well requires more than just prescriptions. It takes consistency, understanding, and support throughout the patient’s daily life.
At Albert Health, we’ve built a digital assistant that helps people stay connected to their treatment in a simple, human way. From tracking medication and symptoms to receiving timely health education, lifestyle guidance, and check-ins, Albert is designed to be with the patient every step of the way—not just during clinical visits.
But the impact goes beyond the individual. By improving adherence, increasing health literacy, and
enabling early intervention, we help reduce complications, give healthcare professionals a clearer picture of their patients’ real needs, and lower costs.
In short, Albert brings continuity, personalisation, and clinical value to the heart of chronic disease care—and that’s exactly what the system needs.

What is your vision and major areas of focus?
We believe healthcare needs a shift—from a system where patients are expected to simply comply, to one where they are active participants in their care. Our vision is to help build that shift.
We focus on improving long-term outcomes for people living with chronic conditions—especially in areas like metabolic health, where the burden is high and support systems are often limited. At the same time, we pay close attention to behavioural factors, because sustainable change in chronic care often depends on small, consistent actions over time. That’s why we design experiences that guide, support, and engage patients in their daily lives—always grounded in clinical evidence.
We work with doctors, medical associations, pharmaceutical companies, hospital groups, and insurers to bring this vision to life—step by step, condition by condition. For us, transformation isn’t just about using new technologies. It’s about rethinking how care is delivered, and making sure patients are no longer on the outside of the system—but at the centre of it.
How important is the Middle East region for your solutions?
The Middle East is one of the regions most heavily impacted by chronic and metabolic diseases. Nearly 70 per cent of deaths in the region are caused by noncommunicable conditions, and $33 billion is spent every year on diabetes alone. These numbers reflect a growing need for long-term, scalable approaches to chronic care.
That’s exactly where we focus as Albert Health. Our multilingual, clinically validated platform is designed to support patients in their daily treatment journeys— while helping health systems improve adherence, reduce complications, and deliver more sustainable outcomes.

As a Turkish team, we also share strong cultural and regional ties that make collaboration more intuitive. It helps us better understand local expectations and co-develop solutions that truly fit the context.
Do you feel it is a good time to invest in Saudi Arabia now?
Absolutely. Saudi Arabia is undergoing a major transformation in healthcare under Vision 2030, with clear priorities around digitalisation, private sector engagement, and better health outcomes. These changes are not just policy-level—they’re creating real momentum across the system.
For Albert Health, this represents a meaningful opportunity. Our focus on chronic disease management, treatment adherence, and patient engagement directly supports the Kingdom’s goals of building a more efficient, technologyenabled care ecosystem.

We’re particularly encouraged by the push for scalable, value-based care models—an area where our digital health platform is already designed to deliver measurable clinical and economic outcomes.
Saudi Arabia is not just investing in technology—it’s rethinking how care is delivered. And that makes it the right time, and the right place, for what Albert Health brings. We’ve already had a very strong start in the country through our collaboration with Tawuniya, the largest insurance company in the Kingdom.
What opportunities do you see in the UAE?
The UAE is making significant strides in building a more connected, patientcentred healthcare system—with speed, ambition, and a clear openness to new models of care. This creates space for digital health solutions that are not only innovative, but also clinically grounded and ready for implementation.
The UAE especially important for us because of the strong alignment between national healthcare goals and what Albert Health delivers: better chronic disease management, improved adherence, and more meaningful patient engagement—all supported by real clinical evidence.
We see an opportunity to move beyond being a vendor. Our aim is to collaborate with healthcare providers, insurers, and public institutions to co-develop long-term, integrated programmes that serve people where they are—at home, in clinics, and across the wider care system.



With its forward-looking approach, the UAE offers a unique environment where digital health can move from promise to practice—and that’s exactly where Albert Health can contribute.


UAE’S LIFE SCIENCES BOOM: DRIVING BIOTECH, PHARMA AND MEDICAL RESEARCH GROWTH IN THE UAE
The UAE is positioning itself as a global life sciences hub, says Dr Gireesh Kumar, Associate Partner, Healthcare Advisory Services, Knight Frank
As part of ‘We the UAE 2031’, the United Arab Emirates is accelerating growth in biotechnology, pharmaceuticals, and medical technology by leveraging its strategic location and investing in innovation, research, and infrastructure.
Key initiatives include:
• Development of life science clusters and specialised vaccine production facilities
• Expansion of biosimilar manufacturing and a stronger focus on chronic disease and rare disease management
• Attracting major pharmaceutical and medical device companies to establish local operations
To support these e orts, the newly formed Emirates Drug Establishment (EDE) will oversee the regulation and management of pharmaceutical products, biologics, medical devices, and food supplements. Additionally, EDE will develop a national framework for pharmaceutical research, clinical studies, and trials, ensuring alignment with global best practices.
These strategic initiatives mark a significant step toward healthcare innovation, enhancing the UAE’s role as a key player in the global life sciences industry.
Key highlights in the sector
• Growing Biotechnology Presence: Abu Dhabi and Dubai are emerging as key biotechnology centres, with dedicated life science clusters and cutting-edge research facilities.
• Operation 300Bn Initiative: The Ministry of Industry and Advanced Technology (MoIAT) has launched the UAE’s largest industrial strategy, allocating AED 300 billion over five years to key sectors, including healthcare. This
funding supports pharmaceuticals, biotechnology, medical devices, and hospital services.
• GCC Biotechnology Market Growth: According to published sources, the GCC biotechnology market is projected to reach $2.6 billion by 2028, with UAE and Saudi Arabia leading the sector.
• Expanding Genomics Industry: The MENA genomics market is expected to grow to $1.2 billion by 2027, with UAE and Saudi Arabia capturing more than 60 per cent of the market.
Developing a world class life science park
To develop a world-class life sciences park comparable to established hubs such as Boston, Basel, San Francisco or Singapore, several critical elements must be in place:
1.Local Human Capital
o A thriving life sciences ecosystem requires a strong talent pipeline of researchers, university students, and technicians, supported by early investments in academic programmes, research partnerships, and collaborations with global institutes.

DR GIREESH KUMAR Associate Partner, Healthcare Advisory Services Knight Frank, MENA Region
“The UAE has made significant strides in developing a world-class life sciences ecosystem, driven by strong government initiatives, investment in R&D, and strategic infrastructure development”

2. Hospital & Clinical Research Infrastructure
o A well-developed hospital network with advanced clinical research capabilities is vital for supporting trials, translational research, and real-world evidence generation.
3. Funding & Investment in Innovation
o Biotechnology and life sciences require long-term capital to fund research, development, and commercialisation, with government funding and private sector participation playing a crucial role in sustaining the ecosystem.

4. Business Environment & Regulatory Support
o Having an integrated ecosystem that connects business services, research institutions, hospitals, investment firms, and corporates within proximity fosters collaboration and drives innovation.
5. Infrastructure & Cost Considerations
o While existing life sciences clusters provide o ices, labs, and warehouses, the rising cost of living and operations must be factored into future planning.
o Shared lab spaces could be an e ective solution, enabling startups and
researchers to access high-end facilities without bearing the full financial burden.
o Given the climate and cost of living, developing mixed-use communities within these hubs, including residential options, could enhance the attractiveness for global talent.
Assessing the UAE’s life sciences cluster: strengths and challenges
Life Science Cluster
The life sciences sector in the UAE is predominantly centered around Dubai Healthcare City (DHCC), Dubai Science Park (DSP), and Masdar City. While the
sector is witnessing considerable growth, it may take some time before it becomes as established as the mature markets.
1. Talent Pool
Strengths:
• Educational Institutions: The UAE has approximately 15 higher education institutions o ering specialised healthcare and life sciences courses. Masdar City in Abu Dhabi is home to leading institutions such as MBZUAI (Mohamed Bin Zayed University of Artificial Intelligence) and Masdar Institute of Science and Technology,

while DHCC hosts Mohammed Bin Rashid University of Medicine and Health Sciences (MBRU). These institutions have dedicated R&D department focusing on chronic disease management, OMICS, precision medicine, public & mental health and more.
• Strategic Location & Infrastructure: Dubai’s excellent global connectivity and specialised free zones for healthcare and biotechnology attracts skilled professionals.
Challenges:
• Limited Local Research Talent: The UAE has a limited, well-established ecosystem for homegrown specialised workforce such as biotech researchers, pharmaceutical scientists, and biotech entrepreneurs, and the career pathway may not be fully optimised and streamlined as in mature markets.
2. R&D
Strengths:
• Emerging Research Collaborations: Universities and hospitals are increasingly collaborating with multinational corporations for R&D. For example, Burjeel Medical City has partnered with international pharmacologic companies in Denmark and USA for research on rare blood disorders. Beyond these, the UAE is also home to dedicated standalone research facilities, such as Abu Dhabi Stem Cells Center (ADSCC), which specialises in stem cell therapy, regenerative medicine and bone marrow transplants.
• Government Commitment: R&D is a key
priority, with institutions such as M42 in Abu Dhabi enhancing their research capabilities, especially in areas such as multi-omics, precision medicine and therapeutics.
Challenges:
• Limited Clinical Research Facilities: There is a shortage of dedicated facilities for large-scale clinical trials and biotech R&D. Only 8 out of 168 inpatient facilities in the UAE have on-site research centres which include SSMC, Rashid Hospital and King’s College Hospital. Within these 8 facilities, only 3 are private, highlighting the challenges private entities face in securing funding for R&D.
• Regulatory Barriers: The regulatory framework for clinical trials is still evolving, creating challenges for largescale biotech research when compared to countries such as Singapore, which o er fast-track approvals and have a robust regulatory framework.
3. Funding Environment
Strengths:
• Existing Investment Initiatives: Abu Dhabi’s ADQ Life Sciences Fund and government investments in AI-driven health tech and medical tourism are fostering growth.
Challenges:
• Investor Preferences: Investors in the UAE tend to favour sectors with quicker returns, such as real estate, AI, and logistics, over high-risk, long-term biotech investments. Hence, there is limited
dedicated VC focusing on life sciences. Local biotech startups struggle to scale without strong funding incentives and prefer to relocate to a more established ecosystem.
4. Business Environment & Infrastructure Strengths:
• Flexible O ice & Lab Space Options: Companies have access to various space options, including flexi-desks, full o ices, fitted lab facilities, built-to-suit facilities, and warehouses.
• Attractive Regional Headquarters
Location: The UAE’s tax exemption law, 100 per cent foreign ownership, logistics hub and access to regional markets makes it an appealing base for regional sales and distribution operations.
Challenges:
• Limited R&D Presence: Many companies within the life sciences clusters operate as commercial or representative o ices, with fewer entities focused on R&D.
• Lab Space vs. O ice Space Pricing: There is minimal price di erentiation between fitted o ice spaces and lab spaces in the UAE market, whereas international benchmarks indicate a premium of 15–35 per cent for lab spaces. Without su icient incentives, investment demand to develop such facilities is likely to remain limited.
Conclusion
The UAE has made significant strides in developing a world-class life sciences ecosystem, driven by strong government initiatives, investment in R&D, and strategic infrastructure development. However, for the country to achieve global leadership in biotechnology and pharmaceuticals, it must address challenges related to research talent, clinical trial infrastructure, and long-term investment in innovation. By fostering public-private partnerships, strengthening regulatory frameworks, and enhancing research capabilities, the UAE is well-positioned to become a leading hub for life sciences, medical research, and biotechnology in the region and beyond.

The hidden cost of coughs Why investing in prevention pays o

The Challenge
Respiratory infections hit harder than you think:
• Short-term respiratory infections are an underestimated drain on employees, businesses, and the economy.
• Our latest research shows respiratory infections cost UK businesses £44 billion a year.
• Vaccination is a powerful tool to achieve these objectives; adult immunisation programs return 19 times their initial investment.
The Solution
OHE has found that investments in prevention, including vaccines, hygiene, and social distancing, could help boost productivity, reduce costs, and address health inequities.
The Office of Health Economics Turning prevention into prosperity.
Health economics turns data into smarter decisions, enabling healthier lives, stronger economies, and billions saved globally.
At the Office of Health Economics, we provide the evidence to prioritise prevention, guiding policymakers and health systems globally to make smarter, cost-effective decisions. Our research drives impactful policies that improve health, save billions, and secure a healthier, more sustainable future.
LONGEVITY AND PRECISION HEALTH IN ABU DHABI
Andrea Tithecott, Partner, Head of Healthcare & Life Sciences
Al Tamimi & Company, discusses how UAE laws and regulations support longevity and precision health
Abu Dhabi Global Health Week 2025 is a landmark event that showcases the UAE’s vision and achievements in advancing health and wellbeing for its citizens and the world. One of the key strategic themes of the event is longevity and precision health, which aims to personalise the future of medicine by harnessing the power of data, technology, and innovation.
The UAE has been at the forefront of developing and implementing laws and regulations that support this theme, creating a conducive environment for life sciences, pharmaceuticals, clinical research, and data sharing. These laws and regulations reflect the UAE’s commitment to protect human rights and dignity, ensure quality and safety, and foster collaboration and excellence.
The UAE is steadfast in its commitment to becoming a global leader in clinical innovation, aligning with its national policy objectives and vision statements. This dedication is evident in the country’s strategic initiatives aimed at enhancing healthcare quality, fostering longevity, and advancing precision medicine.
The UAE’s healthcare vision is encapsulated in several key strategies and policies, including the Vision 2021 and the National Agenda. These frameworks emphasise the importance of preventive medicine, reducing lifestyle-related diseases, and ensuring a high quality of life for all residents
The UAE aims to be among the best countries globally in terms of healthcare quality, with specific targets such as reducing cancer and cardiovascular disease rates, increasing life expectancy, and improving healthcare infrastructure
The focus on longevity and precision medicine is reflected in its investment in cutting-edge healthcare technologies and research. Precision medicine, which tailors medical treatment to individual characteristics, is a key area of development. The UAE has launched initiatives such as the Emirati Genome
Program, which aims to map the genetic makeup of Emiratis to better understand and treat genetic disorders
The UAE is also making significant strides in drug discovery and development. Institutions including the Gulf Medical University and Al Ain University o er advanced programmes in pharmaceutical sciences, focusing on drug design, medicinal chemistry, and nanotechnology in drug delivery. These programmes are designed to produce skilled researchers who can contribute to the global pharmaceutical industry.
Several factors are critical in influencing better patient outcomes in the UAE:
• Healthcare Infrastructure: The UAE boasts state-of-the-art healthcare facilities, including internationally accredited hospitals and specialised centers like the Cleveland Clinic Abu Dhabi.
• Healthcare Workforce: The country invests heavily in training and retaining skilled healthcare professionals, ensuring high standards of care.
• Regulatory Framework: The UAE has established robust health laws and regulations to protect patient rights and ensure the quality of healthcare services.
• Innovation and Technology: The integration of digital health technologies, telemedicine, and AI-driven healthcare solutions enhances patient care and operational e iciency.

ANDREA TITHECOTT Partner, Head of Healthcare & Life Sciences Al Tamimi & Company
“The focus on longevity and precision medicine is reflected in its investment in cutting-edge healthcare technologies and research”

Legislative support
The UAE has enacted several laws to support its healthcare objectives:
• Federal Law No. 2 of 2019 on ICT in Health: This law regulates the use of information and communication technology (ICT) in health fields within the UAE, ensuring optimal use, compatibility, security, and confidentiality of health data and information. It also establishes a central system to collect, exchange, and

analyse health data and information at the national level, and sets the conditions for storing and transferring health data and information inside and outside the UAE. The law also enables the Ministry of Health and Prevention (MOHAP) to issue licenses for health advertising through the central system, and to ban or block websites that violate the health advertising standards. The law aims to enhance the provision and management of health services,
support public health initiatives and policies, and promote scientific and clinical research using ICT.
• Federal Law No. 49 of 2023 on Human Genome: This law regulates the use of the human genome in the UAE, establishing guidelines for genomic and genetic screening, data confidentiality, and the ethical use of genetic information, while promoting public health and scientific research. It also establishes a national genomic database to store, manage, and use genomic and genetic
data and information, and creates the Emirati Genome Reference, a digital DNA sequence that represents the gene sequence of Emirati individuals. The law aims to ensure the safe and respectful use of the human genome, prevent its use for purposes that violate human rights and dignity, and contribute to the diagnosis, prevention, and treatment of genetic diseases.
• Federal Law No. 38 of 2024 on Medical Products: This law governs medical products, pharmacists, and

pharmaceutical establishments in the UAE, detailing definitions, regulations, and approval processes for medical products and related entities. Building on the issuance of Federal Law 28 of 2023 that establishes the UAE Drug Establishment, a federal institution responsible for creating UAE as a global and regional hub for life sciences and clinical innovation, and also regulating medical products in the UAE, and sets its objectives, powers, and functions. The law aims to ensure the quality, e icacy, safety, and reliability of medical products, as well as their availability and a ordability, and to promote and facilitate scientific research, disease surveillance, and innovation in the medical industries sector.
• Department of Health - Abu Dhabi (DOH) Guidelines for Clinical Trials in Abu Dhabi: These guidelines provide the regulatory and good clinical practice requirements for conducting clinical trials with investigational products and medical devices in Abu Dhabi, outlining the roles and responsibilities of involved parties, ethical considerations, and safety protocols. They also specify the procedures and timelines for obtaining authorisation and approval from the Human Research Ethics Committees (HRECs) for conducting clinical trials, as well as the reporting and notification requirements. The guidelines aim to ensure the protection of subjects, the quality and validity of data, and the
compliance with international standards and best practices.
• Federal Decree-Law No. 4 of 2016 on Medical Liability: This law ensures accountability and high standards in medical practice.
These laws and regulations demonstrate the UAE’s vision and leadership in supporting longevity and precision health, by creating a legal and regulatory framework that enables the use of data, technology, and innovation to personalise the future of medicine and improve health outcomes.
Addressing gaps and meeting vision targets
While the UAE has made remarkable progress, there are areas that require further attention to fully realise its vision:

ANDREA TITHECOTT Partner, Head of Healthcare & Life Sciences Al Tamimi & Company
“The UAE’s commitment to creating a global hub for clinical innovation is evident in its strategic initiatives, robust healthcare infrastructure, and forwardthinking policies”
• Research and Development: Increasing investment in R&D to foster innovation in drug discovery and precision medicine
• Public Health Awareness: Enhancing public health campaigns to address lifestyle-related diseases and promote preventive care
• Healthcare Accessibility: Ensuring equitable access to high-quality healthcare services across all regions of the UAE
• Data Integration: Developing integrated health information systems to improve data sharing and patient care coordination
Conclusion
The UAE’s commitment to creating a global hub for clinical innovation is evident in its strategic initiatives, robust healthcare infrastructure, and forwardthinking policies. By continuing to invest in research, technology, and healthcare workforce development, the UAE is well on its way to achieving its vision of becoming a leader in healthcare excellence and innovation.

a.tithecott@tamimi.com www.tamimi.com
Simplifying healthcare technology and services to improve patient care

Strategy & Design
Transforming ideas into deliverable propositions and insight-driven design.
Operation & Evolution
Future-proofed, adaptable systems that can accelerate with your strategy.
Engineering
Utilising cloud technologies, tech stacks and tools to build durable, scalable systems.
Delivery
Active management and dynamic processes from concept to live deployment.
We work alongside your teams, combining clinical and digital expertise to transform care delivery, optimise operations, and improve patient outcomes.
ADVANCING HEALTHCARE GLOBALLY
Guy’s and St Thomas’ Specialist Care brings together world-leading clinical expertise to transform healthcare delivery, says Vanessa Reeve, Head of Guy’s and St Thomas’ Consulting, Guy’s and St Thomas’ NHS Foundation Trust
Guy’s and St Thomas’ NHS Foundation Trust is one of the largest healthcare providers in the UK. We’re dedicated to creating positive change in the lives of patients and their families in the UK and across the world.
We bring together expertise and excellence from five internationally-renowned hospitals: Evelina London Children’s, Guy’s, Harefield, Royal Brompton and St Thomas’. Collaborating as a service, we lead the way in treating the most complex cases – from before birth to later in life.
Our specialists have expertise in diverse areas including heart and lung care, cancer treatment, surgery, diagnostics, and women’s and children’s health. We’re also committed to education and training, and sharing our knowledge for the benefit of all patients.
Internationally recognised expertise
Across Guy’s and St Thomas’ NHS Foundation Trust, all the hospitals that make up adults and children services are ranked as some of the world’s best for 2024 by US Newsweek, the American weekly news magazine. It includes special recognition for cardiology, cardiac surgery, gastroenterology, obstetrics and gynaecology, respiratory medicine, paediatrics and urology.
We are acknowledged for having some of the ‘World’s Best Smart Hospitals’ for our use of technological innovation in care, including advances in the use of robotics, imaging and artificial intelligence.
We understand what it takes to deliver clinical excellence while balancing high demand for services. Our 25,000 sta manage 1,748 inpatient beds across 4 adult hospitals, treat more than 120,000 children per year at our dedicated children’s hospital, and manage 2.6m patient contacts a year.
Our Trust is also a high-volume centre for robotic surgery. We were the first in the UK to perform 10,000 surgeries with the Da
Vinci surgical system, and we use it across specialty areas including head and neck, gastrointestinal, gynaecology, transplant and urology surgery.
Specialists in research, education, and innovation
We have close academic and research relationships with King’s College London and Imperial College London – many of our consultants also lecture at these universities. This knowledge-sharing gives us access to cutting-edge international research trials, placing us at the forefront of advancing care. We provide education and training to healthcare professionals as part of their continued professional development. In addition to online lectures and courses, we o er clinical fellowships and observerships, as well as visiting doctor programmes.
Based at our Trust, the Centre for Innovation, Transformation and Improvement (CITI) works to develop innovative solutions to the most pressing healthcare problems. It has four areas of focus – artificial intelligence automation, surgical care, remote care, and genomics and precision medicine.
We help advance healthcare practices
We share our knowledge with health systems and providers so they may advance practices, improve processes, and deliver the


best care for their patients. We o er a depth of expertise in innovation, including genetic oncology, remote surgery, international clinical fellowship programmes, and high intensity theatre lists to reduce waiting times for routine procedures.
VANESSA
REEVE
Head
of Guy’s and St Thomas’ Consulting Guy’s and St Thomas’ NHS Foundation Trust
“We understand what it takes to deliver clinical excellence while balancing high demand for services”
We operate at a health system-level to transform care e ectively and e iciently across multiple clinical pathways. In this way we ensure that the right care is provided in the right place at the right time - this could be the introduction of new technologies to monitor the health of patients remotely, or advising on how to develop an integrated care model.
A state-of-the-art healthcare service is built on the dedication and expertise of the people working within it. Ensuring they have the right tools, skills and processes in place is paramount. If we determine that new service innovations and improvements are needed, we will also design, develop,

and implement the training programmes and patient pathways that go with them so that every part of the service works seamlessly together.
Delivering clinically-led solutions
We know what it takes to deliver a gold-standard service in a demanding environment, and what works for one healthcare service may not work for another. That’s why we align closely with health leaders to understand their unique challenges and co-develop solutions that make most sense locally.
We adapt and share knowledge gained from our world-class hospitals to guide improvements in the key areas of healthcare systems, as well as support our clients with their clinical strategies and quality governance structures to drive e iciencies, increase performance, and improve quality of care for better patient outcomes.
Sharing knowledge
A health service is only as good as its people. We are one of the country’s largest postgraduate medical education centres, and part of King’s Health Partners, an academic health science centre which includes globally renowned university King’s College London. Additionally, through the Royal Brompton and Harefield hospitals, we are also part of Imperial College Health Partners Academic Health Science Network. This alliance means we can translate existing best practice into excellent patient care. We design bespoke education and training programmes to help healthcare professionals and the systems they work in to excel. Whether it’s participating in our International Clinical Fellowship Programme, or hands-on support in surgical training for complex cases from our leading consultants, we provide
everything that’s needed. Through our knowledge of clinical service design, we co-develop improvements to existing services, as well as completely new services. We identify the tools, technologies and processes needed to achieve operational excellence.
Through our co-branding partnerships, we enable organisations to benefit from the strength and reputation of our brand, enhancing their market presence while upholding the highest standards of care. By sharing our knowledge, we are committed to advancing healthcare globally.





LIVING LONGER, LIVING BETTER: THE HEALTHCARE REVOLUTION DRIVING LONGEVITY
Shi ing from a reactive, sickness-focused healthcare system to one that promotes wellness and longevity has never been more urgent, says Vincent Buscemi, Partner and Head of Independent Health and Care at Bevan Brittan LLP
The traditional healthcare system has long been structured around the model of treating sickness. Valuebased healthcare or VBH models also focus on managing illness and disease a er they have already occurred. Diabetes care, for example, o en centres on minimising the
risk of major complications like amputations rather than addressing the early stages of the disease and preventing its onset. This reactive approach, where intervention comes a er illness, needs a radical transformation if we are to address the complex health challenges of the 21st century.
Prevention is not a new concept and many countries are already beginning to recognise that prioritising prevention over treatment is the key to building a sustainable healthcare future. Integrating health-promoting strategies across various sectors will improve population health, reducing health costs over time and enhancing quality of life. However, reducing the incidence of chronic disease doesn’t have an immediate ROI, so solutions have to be found that can deliver tangible and demonstrable benefits in the short and long terms.
Countries such as Japan and Singapore are leading the charge by integrating prevention into their healthcare models. These nations have acknowledged that waiting until diseases manifest is a losing strategy, both from a financial and health outcomes perspective. Instead of


VINCENT BUSCEMI Partner
Bevan Brittan
“Prevention is not a new concept and many countries are already beginning to recognise that prioritising prevention over treatment is the key to building a sustainable healthcare future”
continuing to treat conditions such as hypertension, obesity, and diabetes reactively, they have begun investing in preventive interventions at policy level. These measures include lifestyle-based, precision interventions designed to prevent the onset of chronic diseases, thus reducing the downstream costs associated with their long-term treatment.
Incorporating prevention-focused health policies requires a systemic shi , and this shi starts with rethinking primary care. In many healthcare systems, hospitals remain the focal point of care, with doctors and specialists providing treatment when people are already ill. This system perpetuates a ‘sick care’ model. However, strengthening primary care and positioning it as a hub for wellness and prevention strategies would help to reframe how we approach healthcare. Primary care could serve as the gateway to holistic health interventions, connecting individuals to resources that support a healthy lifestyle and prevent chronic illness, rather than simply managing it once it occurs.
Emerging technologies and longevity
Advances in genomics and biotechnology are reshaping how we approach both disease prevention and treatment. The cost of sequencing the first human genome in 2003 has drastically decreased – from $3 billion to under $200 today - enabling more widespread access to genomic data that can guide personalised prevention strategies.
Moreover, gene editing technologies like CRISPR open the door for innovative treatments targeting genetic predispositions to chronic diseases. By editing genes or modulating epigenetic factors, we can potentially prevent or
reverse conditions before they manifest. This shi from treating diseases to preventing them at the genetic or molecular level is a powerful example of how medical science is helping healthcare evolve into a preventative and proactive mindset that will redefine inherited and chronic conditions.
However, the promise of personalised medicine goes beyond genetics alone. Wearables and artificial intelligence (AI) are also helping people track their health in real-time, detect early signs of disease, and receive personalised wellness recommendations. Telehealth expansion is another example. It is now common to have GP and other appointments remotely, but why not make preventative and wellness services on telemedicine platforms available, especially in hard to reach areas? These technologies have the potential to revolutionise not just disease treatment, but disease prevention.
Biotech and longevity research is also imperative. Ageing populations come with rising disease level and strain on the system. The WHO predicts that by 2050 the global population over 60 will double and will intensify demand for long term sustainable healthcare models. Investing at policy level into ageing and chronic disease management for healthspan not lifespan must incorporate preventative care models.
Age-related diseases such as dementia and cancer should necessitate prevention measures that improve healthspan, not just lifespan. This refocusing also requires workforce and community engagement - encouraging businesses to implement workplace initiatives or applying interventions that replicate lessons learned from Blue Zone communities can have a significant impact on a local populations; for example, walkable neighbourhoods to improve lifestyle.
The
role of public
health
policy and regulatory frameworks
Health systems can’t and don’t exist in a vacuum - they operate in real time. Not learning those lessons to build the future framework is a potential lost opportunity and a positive prescription for disaster. A truly resilient health system is not just one that is capable of withstanding these shocks when they occur, but is capable of adapting and transforming in the ways that are needed to ensure continued access to quality care.
E ective public health policy is key to supporting these shi s. Global health campaigns and local initiatives focusing
on nutrition, physical activity and mental wellness can help create an environment where healthier lifestyles are the norm, not the exception. In particular, addressing socio-economic inequality is vital in ensuring that everyone has access to the resources necessary to lead a healthy life. Proper housing and education play as much of a part in wellness and health as clinical services.
Governments play a significant role in shaping health behaviours through regulatory measures. Policies such as sugar taxes, restrictions on trans fats, and labelling regulations can encourage people towards healthier choices. The challenge, however, is balancing government intervention with corporate interests. As large corporations have the power to influence public policy, aligning their goals with public health objectives is essential to creating a system where profit incentives and health outcomes are not in conflict. If le solely to the private sector, health solutions may only be accessible to the wealthy, exacerbating global health disparities. This is where government involvement becomes essential to ensure that health promotion strategies benefit all, not just the privileged.
Health systems resilience and global collaboration
The COVID-19 pandemic highlighted the fragility of healthcare systems worldwide, revealing the need for not just more robust systems but systems that can adapt and respond to emerging challenges. To build a resilient health system for the future, global collaboration is essential. In the Pandemic Accord negotiations, the World Health Organization (WHO) has called for international e orts to improve pandemic preparedness, including the development of early warning mechanisms to mitigate future health crises.
A future-ready health system must also align with an evolving regulatory and legal landscape. It falls to government to strike a balance between e iciency and equity to ensure there is a ordability on one level while being able to incentivise innovation on another. As technologies such as AI, genomics, and telehealth become more integrated into healthcare delivery, regulatory frameworks must evolve to ensure patient safety, privacy, and ethical considerations. Harmonising global regulatory standards will be crucial in fostering a cohesive and e ective health system.




The Middle East: A model for future
health systems
The Middle East is uniquely positioned to spearhead the development of new healthcare models. It is becoming a more attractive place to live, work and play. While the Western world struggles with expensive healthcare provision, tight budgets and high taxes, countries like the UAE and Saudi Arabia are free from the constraints of legacy healthcare systems and are actively building innovative approaches to health and wellness.
The Middle East’s access to wealth enables these countries to make long-term investments in wellness infrastructure.

VINCENT BUSCEMI Partner
Bevan Brittan
“By demonstrating better health outcomes at lower costs, the Middle East could provide a model for the rest of the world”
With centralised policy and investment initiatives, they can rapidly incorporate new systems as they are not subject to the bureaucracy and inertia that constrains many western democracies. They are investing heavily in smart cities, such as NEOM, designed with health and wellness at their core. This strategy gives them a unique advantage in embedding wellness and prevention into the foundation of their healthcare models.
Hospitality and community are a huge part of the region’s culture and lifestyle, and align with wellness and longevity. With a growing younger population, there is also an urgent need to address rising rates of chronic diseases and obesity. So there is also a recognition that education plays a role in embedding wellness into people’s mindsets and that without health literacy even the most laudable initiatives will fail. By demonstrating better health outcomes at lower costs, the Middle East could provide a model for the rest of the world. Integrating prevention into every aspect of healthcare—through personalised medicine, technology, public health policies, and global collaboration—will not only improve individual health outcomes but also create more sustainable and resilient healthcare
systems. Furthermore, the Middle East could become a hub for global health innovation, with shared learning across borders and partnerships that transcend traditional geopolitical boundaries.
The healthcare revolution is redefining longevity, driven by emerging technologies, progressive health policies, and global collaboration. Advances in innovation, regulatory frameworks, and cross-border partnerships are essential for delivering high-quality, sustainable care. As organisations expand internationally, navigating complex systems becomes critical. Bevan Brittan’s team of health and care experts provides strategic support to organisations and systems navigating these complexities, ensuring clients capitalise on opportunities in global markets while maintaining compliance and excellence in care delivery, shaping a sustainable, healthier, longer future for all.































































































































































































































SITTING ON A SOLUTION
Ergonomic seating is a critical component of workplace wellness, says Ben Caton, Managing Director at Ergochair
As healthcare continues to embrace cutting-edge technology, one basic yet essential component of employee health and wellness tends to be overlooked: the humble o ice chair. Yet, the reality is stark: 6 out of 10 individuals work from chairs that don’t fit them properly, which can lead to a number of health issues that impact not only personal health, but also workplace productivity and healthcare systems worldwide.
The evidence is clear: ergonomic seating is a critical component of workplace wellness. By prioritising prevention and

back pain, neck sti ness, carpal tunnel syndrome, and other joint-related ailments.
investing in solutions that promote employee health and comfort, organisations can create a healthier, more productive, and sustainable future.
The rising costs
The consequences of overlooking ergonomic considerations in the workplace are far-reaching. Prolonged sitting, particularly in poorly designed chairs, is a major contributor to musculoskeletal disorders (MSDs), a broad category of conditions such as
We o en see individuals who have experienced years of discomfort before seeking an ergonomic solution. By that point, the recovery process can be long and challenging, so a proactive approach is essential.
The statistics paint a concerning picture. In the UK alone, the National Health Service (NHS) spends an estimated £4.76 billion annually on treating MSDs. Globally, the World Health Organization (WHO) reported that over 619 million people su ered from lower back pain in 2020, a number projected to surge to 843 million by 2050. These figures underscore the need for e ective prevention strategies.
















































































Beyond the direct healthcare costs, employers also take a significant hit. Lost productivity due to sick days, presenteeism (working while sick), and decreased employee morale can significantly impact a company’s bottom

line. Research consistently demonstrates a link between ergonomic interventions, improved productivity and reduced absenteeism.
Ergonomics: A proactive investment
The proverb ‘prevention is better than cure’ is particularly relevant in workplace wellness. Addressing ergonomic issues before they escalate into chronic health problems is not merely a matter of employee comfort; it’s a strategic investment in a healthier, more productive workforce.
The key lies in recognising that one-sizefits-all seating solutions fail to address individual needs. People vary significantly in their body types, postural needs, and specific health conditions. A chair that provides optimal support for one person may cause discomfort for another.
Ergochair understands that prevention is paramount. With a commitment to customisation and a track record of helping countless individuals find optimal comfort and support, we are taking the lead in proactive workplace wellness, one chair at a time.
The benefits of ergonomic seating extend far beyond mere comfort. A well-designed chair promotes posture and spinal alignment, reducing muscle strain and pain. It encourages healthy circulation, leading to increased energy levels and improved focus. Ultimately, it contributes to a more comfortable, engaged, and productive workforce.
The future of workplace wellness
As the healthcare industry continues to evolve, the emphasis on workplace wellness is only set to grow. Organisations are increasingly recognising that employee health is not just a cost but a valuable asset. Emerging trends include the integration of ergonomic assessments into wellness programs, the use of wearable technology to monitor employee posture and movement, and the development of AI-powered tools to personalise ergonomic recommendations.
Customer Experiences
The impact of ergonomic seating is best illustrated through the experiences of individuals whose lives have been enhanced by finding the right chair.
• Laura Mathias, “Like many professionals, I’ve faced the daunting task of selecting the perfect home o ice chair. Aesthetics used to take precedence for me over comfort/ ergonomics. However, a proper chair assessment by the Ergochair team made me realise how important it is when I’m sitting at my desk all day, every day. The team opened my eyes to the importance of ergonomics and how it can enhance productivity and general wellness.”
• Caron Cocks, “An o en-overlooked essential piece of o ice equipment… Being a person of petite stature, every care was taken to ensure I received a chair fitted for my frame. As well as the lumbar support, the introduction of the thoracic support was a game changer for me as it supports the correct seated posture and has greatly reduced the tension around my neck and shoulders.”
BEN CATON Managing Director Ergochair
“Research consistently demonstrates a link between ergonomic interventions, improved productivity and reduced absenteeism”
Ergochair is committed to remaining at the forefront of these developments, constantly exploring new ways to enhance the comfort, health, and productivity of workers worldwide. Exporting its researchdriven innovations globally, Ergochair envisions a future where every individual has access to seating solutions that are precisely tailored to their needs, promoting a culture of well-being and maximising employee potential.
• Phillip Cook, “As a business manager, the comfort and wellbeing of sta is paramount. We were guided through two solutions; the first being a set of chairs that were selected in accordance with sta ergonomics. Chairs were then fully customisable. The second solution involved a higher degree of customisation to accommodate specific problems such as back-pain or posture. Ergochair sta spent considerable time understanding each individual’s needs and then o ered a completely bespoke solution. Settings could be further adjusted to refine the set-up. The service was complemented by the quality of the product. It was clear that each chair was well cra ed while being both robust and suited to the o ice environment. Definitely an


DRIVING PROSPERITYTHE SECRET POWER OF HEALTH ECONOMICS
Graham Cookson, CEO, tells Healthcare World how the O ice of Health Economics helps drive smarter healthcare spending
The World Health Organization estimates that the global population aged 60+ will double by 2050, amounting to 2.1 billion people. Unless properly approached, this demographic shi will have seismic negative impacts on already overburdened healthcare systems and national economies.
That’s where health economics comes in: it informs decision-making that unlocks e iciency gains, delivers the most health per dollar, and ultimately leads to healthier, wealthier societies.
Driving better healthcare spending
The O ice of Health Economics (OHE) is a pioneer in the field. As the world’s oldest independent health economics research organisation, we have been at the forefront of the field for more than 60 years. Every day, we work with governments, pharmaceutical companies and patient groups across the world to drive better decision-making and smarter healthcare spending – from addressing global drug shortages to tackling the health impacts of the climate-crisis.
We’re globally renowned for delivering original and independent insights that shape health policy and drive innovation. The route from our research to policy impact is clear. Working with the British Medical Journal (BMJ), OHE has found that 27 per cent of our research is cited in international guidelines, compared to the global average of just 6 per cent.
Addressing global healthcare priorities
The Asian Development Bank estimates that smarter investment into the health of ageing populations can unlock increases of up to 1.5 per cent of national GDP or around the global average economic growth this year.
Conversely, the evidence is clear: poor health equates to poorer societies. Recent OHE research found that UK businesses incur more than £44 billion in productivity losses due to short-term respiratory infections – and that this burden is borne




disproportionately by women. These e ects were made abundantly clear last winter as many UK hospitals were over-capacity due to the large number of people being hospitalised with severe cases of winter flu. The impacts of ill

GRAHAM COOKSON CEO Office of Health Economics
“We have an international reputation for asking the right questions and delivering pioneering, practical solutions that drive innovation in health systems”
health therefore go beyond the individual – it widens inequality, overburdens healthcare systems, and negatively impacts businesses and the national economy at large.
This is why prevention matters – one jab can lead to millions of dollars saved.
Generating evidence that shapes health policy around the world
OHE is a leading voice in the conversation around prevention and adult immunisation.
In 2024, we published a landmark study across ten countries in Asia, Oceania, Europe and the Americas, commissioned by the International Federation of Pharmaceutical Manufacturers (IFPMA). The study showed adult immunisation programmes have a return of up to 19x the initial investment – or up to US $4,637 per individual -- a er monetising the significant health benefits seen outside of the healthcare system.
Our evidence base is trusted by governments and policymakers around the world. OHE’s policy recommendations on adult immunisation have been heard at policy and parliamentary events in New York, Washington, Dublin, London, Berlin, and Seoul.
Unlocking health and e iciency gains for governments and healthcare providers
Our expert economists have backgrounds in government, consultancies, the life sciences industries and academia, with in house knowledge supplemented by a global network of leaders in their fields.
This means we are a well-connected partner with the unique ability to bridge perspectives between the pharmaceutical industry, governments, and healthcare providers to ultimately deliver more equitable health gains. Some of our most recent research on the economic cost of respiratory infections, funded and commissioned by Pfizer, recommended more policy levers to unlock e iciency gains. A key policy recommendation was tax exemptions to encourage employerled vaccination schemes in the UK to lessen the strain on healthcare systems and drive productivity.
Another research project, funded by GSK, found that pharmacy-based vaccination schemes could provide additional revenue streams for pharmacies. They could be at least cost-neutral for the UK, and could free up almost 400,000 GP appointments a year.
Solving problems on a global scale
We have an international reputation for asking the right questions and delivering pioneering, practical solutions that drive innovation in health systems. We have the unique ability to bring together stakeholders from across sectors, across disciplines, and across the world to discuss the biggest questions of today and tomorrow.


VALUE-BASED APPROACHES TO LONGEVITY
The aims of longevity science dovetail neatly with those of valuebased healthcare, say Robert McGough, Partner, and Gemma Badger, Senior Associate Hill Dickinson LLP
Afew years ago, mentions of ‘longevity science’ conjured up images of futuristic science fiction works with cryogenic chambers and impossibly young-looking individuals striving for eternal youth (along with the inevitable societal dystopia that resulted).
With a little more education, it became clear that this was not an entirely accurate view. The less (melo)dramatic reality was of scientists closer to home researching and developing approaches including pharmaceuticals, genomics and other therapies and knowledge.
These ideas aimed to further healthy ageing and extend both lifespan (total duration of life) and healthspan (period of life spent in good health) and, with the help of other burgeoning technologies such as AI, continue to develop in even more exciting ways.
To date the product of longevity work has been targeted primarily at a fee-paying market of high-net worth individuals, given significant development costs and therefore price tags attached. However, more recently broader solutions and applications have emerged.
In Singapore, approaches are being developed for application in a primary care setting. Elsewhere, there are moves to develop urban spaces, and whole ‘longevity




cities’, which apply the findings of longevity research in their design including extensive green space, clean air and clean water. These plans include incentives to engage in physical activity and social engagement with policies to disincentivise unhealthier habits.
Synergies
between longevity science and value-based healthcare approaches
The aims of longevity science dovetail neatly with those of value-based healthcare in a number of ways. Value-based healthcare aims to deliver the outcomes that matter most to patients at the most a ordable cost. However ‘most a ordable’, does not necessarily equate to lowest cost and the value measured is optimally viewed on a longitudinal basis across
a patient journey or pathway analysing from both an individual and wider societal perspective. The most productive valuebased approaches should align the interests of a broad range of healthcare system stakeholders, incentivising them to work together to deliver the best outcomes and giving them each the best opportunity to do so.
This description flags some immediate potential synergies between the two concepts:
• The patient-centric focus on outcomes which really matter to patients chimes clearly with the longevity focus on healthspan and quality of life, rather than extension of life at any cost.

GEMMA BADGER Senior Associate Hill Dickinson
“Challenges include finding ways for healthcare systems to effectively respond to multi-morbidities in an ageing population”
• With value being interpreted more broadly and over a longer period than lowest cost, there is potential for investment in some of the higher priced approaches being developed through longevity research and activity.
• Longevity science recognises the broader societal benefit of achieving healthier ageing throughout the population –linking with the multi-stakeholder approach in value-based healthcare solutions.
• Genomic research also has a key interaction with value-based healthcare approaches, enabling the development of more personalised treatments. By predicting likely disease trajectory earlier, conditions can be tackled more e ectively and healthspan increased as a result.
• A key example of genomics deployment can be seen as part of the NEOM project in the Kingdom of Saudi Arabia – aiming to support individual empowerment and proactive prevention, including the development of a ‘digital twin’ for residents to track their own health. This concept flags a further facet of value-based healthcare which can be enabled through the longevity approach – placing the patient at the centre of their healthcare journey by empowering them with the knowledge and ability to influence it.
• Finally, value-based healthcare aims to eliminate waste. Personalised treatment plans can be deployed to exclude some treatments which may not be e ective. This approach both eliminates physical wastage in healthcare systems, resulting in an overall better experience for patients who are not subjected to treatments or procedures unlikely to benefit them. It can also impact the perennial issue of waiting lists, which reduce when unnecessary planned interventions are removed.



Keeping up the momentum
Challenges include finding ways for healthcare systems to e ectively respond to multi-morbidities in an ageing population. Value-based healthcare approaches look to redesign care pathways centring on patients rather than individual diseases, making the pathways more e icient from both the patient and system perspective. Longevity solutions look to the root cause and predictors of many of those diseases to find ways to influence and treat them earlier. Combining these two responses is powerful.

GEMMA BADGER Senior Associate Hill Dickinson
“Value-based approaches and longevity development benefit from clear thinking about how finances flow between those parties likely to be involved in developing solutions”
Collaboration between healthcare and other organisations involved in influencing the health of individuals and society more broadly is key. The enabler here is movement away from siloed working, finding ways of linking up financial and other incentives between di erent entities to encourage joint working.
Legal tools for future development
So, bearing all of this in mind, what next? Which legal tools and approaches



can be considered to blend and support longevity and value-based approaches most beneficially?
Both approaches depend upon collaboration and joint working over a long period of time, and the sharing of information and data to underpin and iterate the solutions required. Collaboration cannot be enforced through a contract though, rather relationship development is key.
There are approaches to contracting, and the development of a ‘value-based
contract’ which can be used as tools to enable relationships to develop in a collaborative environment. For these to work e ectively, contractual discussions need to be entered into early and avoid putting in place adversarial arrangements. At a broader system level, both value-based approaches and longevity development benefit from clear thinking about how finances flow between those parties likely to be involved in developing solutions. It is possible that a solution being developed in one part of a system
could benefit another part of that system, or another party in the chain. Finances need to be set up to reflect this rather than entrench perverse incentives to engage in non-collaborative practices. CONTACT

gemma.badger@hilldickinson.com
robert.mcgough@hilldickinson.com
www.hilldickinson.com
ABU DHABI GLOBAL













Join Dr Emer MacSweeney from leading mental health practitioners Re:Cognition Health as we discuss her work on clinical trials for the first drugs to treat this debilitating condition, and her plans to roll them out to patients. We will also be joined by Dr Laila Abdel-Wareth, CEO Diagnostics M42, who will discuss the problem and the potential applications of these new treatments in the region.



Data-driven healthcare, personalised population and preventative health have been at the top of the agenda for the discussion in global health systems for several years. But our payor systems are not geared up to fund this activity. This session considers how insurance, outcome-based payment models or government initiatives can be tailored to meet the requirements of the future.







This session will consider how data can be used to drive the highest quality and best outcomes for patients. How can we use data to benchmark quality and measure improvement? How do we find and ensure the quality data to measure our healthcare performance?







In this session we will consider the technologies, data and capabilities required to create the digital health ecosystem of the future. How do the various apps, technologies, so ware systems and the people that operate and use them fit together? Six leading digital technologists consider the answer.







CREATING THE BREAKTHROUGH FOR ALZHEIMER’S DISEASE TREATMENTS
Dr Emer MacSweeney, CEO Re:Cognition, tells Healthcare World about the promise of disease-modifying treatments for neurological conditions
With the ageing global population, Alzheimer’s disease has emerged as one of the most significant challenges facing healthcare systems worldwide. In fact, the World Health Organization (WHO) o icially labelled Alzheimer’s a pandemic in 2018. Alzheimer’s is one of the leading causes of death and disability among older adults, with the condition a ecting millions globally. The increasing prevalence of the disease, combined with the absence of a cure, has placed immense strain on healthcare economies. However, a series of groundbreaking developments in the treatment of Alzheimer’s has the potential to reshape the future of care for those living with the disease.
Dr Emer MacSweeney, a Consultant Interventional Neuro-Radiologist, co-founded Re:Cognition Health in 2011 to provide a specialist service for accurate diagnosis and access to the latest treatments for progressive neurodegenerative and neurodevelopmental conditions and traumatic brain injury. Re:Cognition Health has 10 centres in the UK and the USA, where individuals can enter global clinical trials for new diagnostic biomarkers and emerging brain and mind medications. The inconsistency in diagnosing and treating patients with cognitive impairment in a clear and timely way lay behind the launch. Dr MacSweeney and co-founder Tom Dent believed a multi-disciplinary team providing the right clinical pathway to diagnose cognitive impairment was essential, along with the importance of providing hope, by making available the new and emerging international clinical drug trials in a supportive, compassionate and convenient environment. Last year alone their clinics saw 10,622 patients and now have a sta of 185 in two countries.
The promise of disease-modifying treatments
Alzheimer’s disease has long been regarded as an irreversible and progressive condition that worsens over time, leading to the death of brain cells and a decline in cognitive function. Traditionally, treatments have focused on managing symptoms, rather than halting or reversing the disease’s progression. However, new advancements in research are finally making strides. For the first time, diseasemodifying treatments are emerging - medications designed not just to alleviate symptoms, but to slow down the progression of the disease itself.
Today, Re:Cognition Health is providing treatment with the recently approved monoclonal antibodies against amyloid, leqembi™ and kisunla™ in the UK and the USA. These treatments—Kisunla (denanumab) by Eli Lilly and Lekembi (lecanemab) by Eisai—represent a pivotal shi in the approach to Alzheimer’s disease. The UAE has also recently approved monoclonal antibodies against amyloid. Their approval is a significant milestone, both for the science behind Alzheimer’s treatment and for the millions of individuals who may benefit from them in the near future.
“These drugs have recently been licenced for people with MCI, mild cognitive impairment, which can actually be very mild symptoms of cognition and what’s call mild AD dementia,” says Dr MacSweeney. “But obviously once people have progressed beyond a certain point, then those treatments designed to slow it down are no longer e ective.
Understanding Alzheimer’s disease
The pathology of Alzheimer’s is driven by the accumulation of two key proteins in the brain: amyloid and tau. Amyloid protein clumps together to form plaques, which interfere with communication

between brain cells and lead to cell death. Tau protein forms tangles inside brain cells, further disrupting their function and contributing to cognitive decline. Recent research has revealed that amyloid plaques begin to accumulate in the brain up to 20 years before any symptoms of Alzheimer’s appear. Now, for the first time, biomarkers—biological indicators detectable through specialised tests—can identify the presence of amyloid and tau in the brain long before cognitive decline becomes apparent. This information opens the door to earlier


DR EMER MACSWEENEY CEO Re:Cognition
“The secret is being able to access the medications available now so that you can stay mild in terms of your symptoms. That’s why this is such a pivotal time for this disease”
treatment, potentially slowing or even preventing the onset of symptoms altogether.
Monoclonal antibodies are a class of medication designed to target and remove specific proteins in the body. In the case of Alzheimer’s, monoclonal antibodies like Kisunla and Lekembi are engineered to target and remove toxic amyloid protein from the brain. The results of clinical trials for these drugs have been promising. Not only do they reduce the levels of amyloid in the brain, but they also correlate with a slowing of
disease progression and the preservation of cognitive function.
“The fantastic thing about the large studies that resulted in these two drugs being approved by FDA and MHRA, the drug regulatory authorities, is that not only do they remove the toxic levels of amyloid protein, but their use correlates with slowing a progression of disease and symptoms,” says Dr MacSweeney.
However, it’s important to note that these treatments are not a cure. The damage caused by the accumulation of amyloid and tau proteins over the years cannot

be fully reversed. The goal is to catch the disease early—when biomarkers show signs of abnormal amyloid and tau build up—before irreversible irreparable damage has occurred. “Early action is the most important message because it enables us to make an accurate diagnosis using biomarkers, and then to give people the opportunity to get access to one of these medications designed to slow down further progression,” Dr MacSweeney says.
Preventing Alzheimer’s in the future
In the coming years, Dr MacSweeney believes there will be an increasing number of drugs approved for use, each targeting di erent aspects of the disease and o ering a variety of mechanisms to slow its progression. Looking further ahead, the future of Alzheimer’s care may involve regular testing for biomarkers as part of routine health check ups. “Just as we currently test for conditions like high blood pressure, diabetes, or cholesterol, it’s quite likely that individuals will soon
be tested for amyloid and tau build up around the age of 40 or 50,” she considers. “If these biomarkers are present, individuals could begin preventative treatments to delay or prevent the onset of symptoms, just as we now prevent conditions such as heart disease through lifestyle changes and medication.”
This shi toward preventative care is not as far o as it may seem. In fact, Dr MacSweeney is already undertaking clinical trials involving people who are cognitively normal. “We measure in the clinical trial whether or not they have high biomarkers for amyloid and tau already. If they do, then they can take part in a study, one of which is actually for a vaccine against tau protein. The purpose of these clinical trials today is to create a scenario for the future where su erers can take a drug to prevent them developing symptoms.”
Such treatments could further revolutionise the approach Alzheimer’s disease, enabling intervention before symptoms even begin. “Education is also
key; there are lifestyle changes such as exercise, diet including a low sugar diet, keeping your brain really active, sleep – all these are actually significant and serious, modifiable risk factors, which we should all be doing all the time,” Dr MacSweeney adds.
“The good thing is that either through clinical trials or through the drugs now on the market, if you do have mild cognitive symptoms, there is a chance to access medications that will potentially change your future,” she says. “The secret is being able to access the medications available now so that you can stay mild in terms of your symptoms. That’s why this is such a pivotal time for this disease.”

Award-winning legal and regulatory advice

We are the market-leader in the provision of legal, governance and regulatory advisory services to businesses delivering and providing healthcare services within the UK and internationally.
Our award-winning healthcare teams provide organisations with outstanding corporate, commercial, clinical negligence, litigation, regulatory, property and employment legal advice.
With years of experience and global exposure, our healthcare teams have the expertise to support clients’ endeavours anywhere in the world. Our reputation as a leading healthcare firm has taken us across the globe, working with a wide range of clients (from NHS bodies to independent health and social care providers, operators and developers as well as funders and investors) on a multitude of commercial health projects. Our in-depth practical and commercial knowledge of the challenges and opportunities of expanding overseas are second-to-none and a true benefit to our clients in the increasingly global healthcare market.

Vincent Buscemi Partner and Head of Independent Health & Care vincent.buscemi@bevanbrittan.com


Jodie Sinclair Senior Partner and Head of Employment, Pensions and Immigration jodie.sinclair@bevanbrittan.com

Sarah Skuse Partner and Head of Independent Health & Care Real Estate sarah.skuse@bevanbrittan.com




REFORMING THE SOUTH AFRICA HEALTH SYSTEM
Professor Nicholas Crisp, Deputy Director General, National Health Insurance, discusses the country’s e orts to implement a National Health Insurance (NHI) system
South Africa is a country steeped in a history of complexity, from the harsh realities of apartheid to the present-day struggle for justice and equality. It has been a very unjust society to grow up in and that is reflected in our health system. And while race remains a visible marker of inequality, the real driver today is socio-economic. A tiny fraction of the population enjoys the benefits of
any quality care, while the rest are le with little more than the bare minimum of variable quality.
The current fragmented healthcare system consists of a large private sector catering to a small portion of the population and the public sector struggling to meet the needs of the majority. The NHI aims to establish a single-payer system for more than 62m
people that would provide universal healthcare coverage, funded through taxes. This new system involves long-term, complex reforms including integrating public and private providers, improving digital infrastructure, and addressing medical legal issues.
Addressing the challenges
South Africa’s constitution embraces a concept of consultation and dialogue in policy formulation, ensuring that decisions are made with the input of various stakeholders. This process has o en resulted in delays and ine iciencies, particularly in healthcare. The constitution’s emphasis on rights and consultation, rather than immediate action, has created a situation where

well-meaning policies take years, if not decades, to fully implement.
The health system has become a microcosm of the larger societal issues we face. South Africa’s Gini coe icient, a measure of income inequality, is the highest in the world at around 63-65. Some 40 per cent of the population is unemployed while a small elite controls both wealth and income. Those who can a ord private health insurance enjoy access to any services—doctors, hospitals, diagnostic equipment—while the majority of South Africans are le to rely on a public system that is chronically underfunded and underresourced.
Around 9m people are covered by some form of voluntary health insurance. The private sector largely services this 15
per cent of the population and has the lion’s share of healthcare professionals and resources. More than 90 per cent of dentists, 95 per cent of optometrists and audiologists, and 67 per cent of medical specialists work in this sector. A recent evaluation by the O ice of Health Standards Compliance found that the outcomes and quality of care in the private sector were not markedly better than in the public sector. In many cases, the private sector su ers from the perverse incentives of over-servicing and profit-driven care. While the public sector is constantly under pressure, struggling to provide care to an overwhelming number of patients, it still manages to deliver quality healthcare, o en with fewer resources and under more di icult conditions.
The majority of the population is served by young new graduates and those diehards and academics who have remained faithful to the public service. The number of patients they look a er grows ever greater until they eventually can’t cope anymore and find themselves burning out and either leaving the country or being squeezed out into the private sector.
This stark contrast between the two fragmented and complex systems— the over-resourced private sector and the underfunded public system—has created huge ine iciencies. I believe that simplifying the system will ensure everybody has the right of access to exactly the same quality of healthcare and that we pay for it in a manner that is e icient.
The National Health Insurance (NHI) Act is a piece of legislation that seeks to establish a single-payer healthcare system which has been 20 years in the making, with five years spent in parliament debating its content. But while the NHI Act o ers a hopeful vision for the future, the reality is that achieving true equity will not be an easy or quick process.
Restructuring the funding
South Africa cannot continue to sustain parallel healthcare systems that deliberately allocate health based on the ability to pay. The private sector spends at least five time per capita of what the public sector spends because it is hospi-centric, curative and very heavily specialist. To move towards universal coverage, we must shi the focus of this spending from curative health services to more comprehensive, coordinated care preventive services. Rather than continuing to rely on the more than 80 administrative systems and varying payment mechanisms, we need publicly funded healthcare and to consolidate and streamline the system, ensuring that every citizen has access to the same level of care regardless of their financial status.
But achieving this requires a complete overhaul, starting with better management of the resources that are already in place. The government must focus on using existing funding more e iciently - investing in primary healthcare services, integrating multidisciplinary care, and expanding the use of digital systems to improve patient tracking, reduce duplication of tests, and enhance overall e iciency.
One of the key components of the NHI is the creation of a central fund that

will be responsible for paying healthcare providers. This fund will be financed through taxes, including those already paying for the health system, which will then be used to purchase services from healthcare providers, ensuring that all South Africans have access to the same level of care. This means that funding will no longer be dependent on the ability to pay, and the focus will shi from profitdriven care to patient-centred, equitable service delivery.
To support this transition, we are implementing digital health systems that allow for seamless access to patient records across the entire healthcare system. A single patient identifier will make it easier for healthcare providers to access patient histories, reducing the need for duplicate investigations and ensuring that treatment plans are based on accurate, up-to-date information. Such systems will also allow for more e icient resource allocation, reducing waste and improving care outcomes.
However, these reforms will take time to implement. The first three years of the NHI’s implementation will focus on

PROFESSOR NICHOLAS CRISP Deputy Director General National Health Insurance
“To move towards universal coverage, we must shift the focus of this spending from personal health services to more comprehensive, coordinated care”
strengthening governance structures, developing the necessary policies, and building the digital infrastructure to support the system. While some of these reforms will lead to long-term e iciencies, the immediate reality is that some additional funding will be required to establish this corporate capacity.
The Act provides for several ways to generate revenue for the NHI fund. These avenues include redirecting subsidies currently given to beneficiaries of private healthcare insurers and looking at
alternative revenue models, such as payroll taxes or levies. But these options will require careful consideration and planning, and it is unlikely that they will not provide an immediate solution to the deepening crisis. The immediate need is to simplify the system and use the e iciency gains to fund the gaps.
The NHI o ers a path towards reform, but we must remain realistic about the challenges ahead – it will take time, patience, and a collective commitment. The future of South African healthcare lies in our hands, and if we take the right steps now, we can build a system that is truly reflective of the values of justice, equity, and care for all.
HealthBeats is hosted by Steve Gardner, Healthcare World Managing Director, for Abu Dhabi Global Health Week


CARTLEDGE EDITORIAL DIRECTOR

ENCOURAGING MEN TO TALK ABOUT THEIR HEALTH
Talking about health, especially mental health, has never been easy for men. For many, it’s a conversation they feel they can’t or won’t have. Societal norms, expectations, and the pressure to “man up” o en create barriers to openly discussing health struggles, particularly in the areas of mental health and well-being.
For far too long, men have been conditioned to suppress their emotions and struggles. We see it everywhere: men hug women in times of need, but rarely o er the same gesture to another man. For Nigel Farnfield, proprietor of Surrey pubs The Olive Tree and The Dog and Pheasant, an arm around a friend or a customer’s shoulder, a small act of comfort, can make a world of di erence. “Conversations about mental health are o en brushed aside, with men expected to ‘keep it together’ and handle challenges on their own. This lack of communication can be harmful, especially when it comes to issues like depression, anxiety, and suicide,” he says. In 2023, statistics revealed that 74 per cent of those who took their own lives in England and Wales were men - more than 6,000 lives
lost. Mental health, particularly for men, has become an epidemic—an invisible crisis that too many su er in silence. What’s needed is not just more awareness, but real action to encourage men to speak up and seek help when they need it.
The role of the Distinguished Gentleman’s Ride
This is where the Distinguished Gentleman’s Ride (DGR) comes in. Launched globally, the DGR is more than just a motorcycle event; it’s a celebration of men’s health. By gathering riders together from all walks of life to participate in a shared passion for classic motorcycles, the DGR provides a platform for men to connect, share, and, most importantly, talk. It’s a space where conversations about health can happen organically.
For many men, the DGR represents an opportunity to come together and connect with others who share similar experiences or concerns. It’s a chance to step away from the pressure of day-to-day life and be part of something greater—a cause that transcends personal struggles and encourages solidarity. The event’s relaxed
atmosphere, paired with its charitable focus, makes it the perfect setting for men to start those di icult conversations.
In Guildford, for example, the Surrey Hills Ride has become one of the most successful in the world. Some riders have even reported that the event has led to lifesaving conversations, encouraging them to seek medical advice they otherwise might not have. One of the reasons the DGR is so e ective in encouraging men to talk about their health is because it harnesses the power of peer support. “Many men find it easier to open up when they’re surrounded by others who are willing to listen,” says Nigel, who helps organise the Surrey DGR Ride.
UK television presenter Charley Boorman, who is an Ambassador for DGR and takes part in the ride, famously discovered he had testicular cancer when he took his dog to the vet. The vet encouraged him to look at his dog’s symptoms and Charley realised he had the same condition. Since then, he has used his profile to encourage men to inform themselves about their own health.
In the UK there isn’t a prostate cancer screening programme, unlike the breast, bowel and cervical cancer screening programmes. The current UK advice is that ‘any asymptomatic man, aged 50 and over can make an appointment with their GP to discuss having the PSA (blood) test. GPs should not proactively raise the issue with asymptomatic men.’ However, Charley Boorman had no symptoms and went on to have a testicle removed.
So creating opportunities for men to gather in a non-judgmental, supportive environment is crucial. Whether it’s at a local pub, a football match, or a motorcycle ride, the key is to have a space where men feel comfortable enough to share their struggles without fear of judgment. And it’s not just about starting the conversation. It’s also about being present and engaged in those discussions.
Since its partnership with Movember in 2016, the DGR has contributed more than $50m worldwide toward cutting-edge research in prostate cancer, men’s mental health, and suicide prevention. These e orts are critical in creating tangible, longterm solutions to the problems that a ect so many men worldwide. So if you are free on May 18th, sign up for your local rides - there are 921 across 121 countries to choose from, or even start your own!
www.gentlemansride.com

RETHINKING RESILIENCE IN HEALTHCARE
Value may not mean what we think, says Methven Forbes, CEO, Fuller and Forbes Healthcare Group
For years, Value-Based Healthcare (VBHC) has been championed as a way to make healthcare systems more e icient, accountable, and patientfocused. By linking financial incentives to measurable patient outcomes, VBHC aims to eliminate unnecessary procedures, particularly in fee-for-service systems.
But here’s the problem: if healthcare were a production line, every patient would be the same—but they’re not.
Not all aspects of patient care can be neatly quantified through linear outcome metrics. Treatment successes and failures are influenced by factors beyond a clinician’s control, yet funding hinges on rigid performance targets. The risk? A system where numbers take precedence over people.
In my view, we need a shi —one that acknowledges real-world complexity, values professional judgment, and
promotes resilience rather than financial volatility. Instead of focusing solely on outcomes that can be conveniently measured, we should be asking:
• What is the most cost-e ective yet clinically e ective intervention available?
• Who is the most cost-e ective, appropriate professional to deliver it?
• How do we ensure clinical compliance with the evidence base?
This is where Quality-Based Healthcare (QBHC) o ers a compelling alternative. Unlike VBHC, which can penalise providers for factors beyond their control, QBHC ensures that clinical excellence, professional accountability, and long-term investment in patient well-being drive decision-making.

How VBHC works—and why it’s flawed
VBHC was introduced to shi away from fee-for-service models, aiming to align financial incentives with improved patient outcomes and reduced avoidable interventions. VBHC has demonstrated some success in reducing interventions and improving cost e iciency, particularly in elective procedures and standardised treatments, where measurable outcomes align with financial incentives. However, its broader application across healthcare systems has exposed significant flaws such as those relating to complex or high-risk patients. It is easy to see, too, how VBHC can morph primarily into a cost reduction programme, especially in profit-driven models.

METHVEN FORBES CEO Fuller & Forbes Healthcare Group
“QBHC
ensures that clinical excellence, professional accountability, and long-term investment in patient well-being drive decision-making”
VBHC o en creates perverse incentives that undermine patient care and provider stability. It prioritises measurable outcomes, neglecting essential but hard-toquantify aspects like mental health support and chronic disease management. Rigid targets can discourage innovation, and linking clinician income to patient feedback may deter necessary but unpopular medical decisions.
More worryingly, VBHC can incentivise providers to avoid high-risk patients in order to protect performance scores. For example, in the UK, two neighbouring medical centres served vastly di erent populations, with one redirecting complex cases to protect its outcome metrics. While not explicitly promoting “cherry-picking,” VBHC’s financial pressures can lead to such behaviours, ultimately reducing healthcare to a checklist rather than a holistic, patientcentred approach.
Further, under VBHC, funding fluctuates unpredictably, making long-term planning di icult—especially for providers serving economically disadvantaged populations.
For example, in the UK’s NHS Quality and Outcomes Framework (QOF) around 10 per cent of primary care funding depends on hitting performance targets, yet providers in lower-income areas o en struggle to meet targets due to external social factors, reducing their available funding. In a capitated system, where care is free at the point of need, this creates financial disparities among providers—some can a ord better sta ing, while others struggle despite greater patient demand. I see this across our own 18 medical centres in England.
The short-termism of VBHC
While VBHC has successfully reduced unnecessary procedures in elective care, its rigid focus on measurable targets can discourage preventative and holistic care, particularly for complex cases. The financial pressure to meet outcome-based incentives may inadvertently lead to riskaverse practices, undermining long-term patient health.
Healthcare resilience isn’t built through short-term numbers alone. It requires stable funding, professional development, and the freedom for clinicians to address local needs proactively.
The core principles of QBHC
QBHC o ers a flexible, clinically grounded framework that rewards best practices while avoiding penalties for factors beyond a provider’s control.
QBHC does not dismiss e iciency or coste ectiveness but reframes them to ensure clinical excellence remains the priority. It is built on four key principles:

1.Evidence-based medicine as the gold standard: Clinicians follow approved guidelines and best practices to ensure appropriate, high-quality care. Deviations from best practice trigger peer review and additional training, rather than financial penalties. The focus is on learning and improvement, not punishment. Though, if underperformance continues either at a clinical or provider level, then there are regulatory and HR implications to this.
2.Professional accountability over financial penalties: regular case reviews, audits, and mentoring ensure high-quality care, and rather than financial disincentives; underperformance is addressed through professional development.
3.A patient-centred approach that values more than just numbers: Unlike VBHC, which rewards only measurable outcomes, QBHC values comprehensive, integrated care. Factors like mental health, social support, and chronic conditions are recognised as integral to good care, even if they don’t fit into a single performance metric.
4.Stable funding for long-term sustainability: QBHC ensures stable financial models, such as capitated budgets (fixed per-patient payments), block grants (long-term funding) and riskadjusted payments (protecting providers who treat high-risk populations), and removes the financial incentive to exclude complex cases. As always, there are cost implications. However, under this model, quality care costs what it costs, shi ing the focus away from restricting activity for financial reasons towards defining the available funding and the scope of healthcare that can be a orded. I also appreciate that there are di erent permutations of both VBHC and QBHC and the approaches are not entirely opposites.
Why QBHC builds a more resilient health system
Balancing costs without compromising care
One of the biggest misconceptions about QBHC is that it ignores cost-e ectiveness. In reality, QBHC balances financial responsibility with clinical priorities— ensuring that care is high-quality (following evidence-based guidelines), e icient

METHVEN FORBES CEO Fuller & Forbes Healthcare Group
“If
we want a truly resilient healthcare system, we must look beyond financial performance targets and prioritise quality as the foundation of care delivery”
(avoiding unnecessary interventions while ensuring necessary ones), and equitable (ensuring all patients receive appropriate care, regardless of risk level)
Rather than imposing arbitrary financial penalties, QBHC ensures responsible resource use through professional accountability.
Encouraging continuous improvement instead of short-term targets
Rather than restricting providers to short-term performance goals, QBHC fosters a culture of ongoing learning. Mistakes trigger mentorship and systemwide improvements instead of financial penalties, ensuring clinicians remain motivated to refine their practice. By emphasising continuous improvement, QBHC supports long-term patient health and professional growth.
Ensuring equitable access to care
By removing rigid financial targets, QBHC eliminates the incentive to “cherry-pick.” Instead of tying payments directly to narrow patient outcomes, QBHC relies on stable funding and professional peer review. Providers aren’t penalised for treating complex cases; rather, quality is assessed on clinical standards—not just on whether a patient’s metrics meet a specific target. This protects vulnerable patients, ensuring that those with multiple comorbidities or social challenges receive the care they require.
Enabling long-term investment in healthcare systems
Under VBHC, funding fluctuations make it di icult for hospitals and clinics to invest in workforce development, infrastructure improvements, and technology upgrades. QBHC’s stable financial model allows longterm investment, ensuring better chronic disease management, improved preventive care, and more strategic resource allocation.

adopting
funding models, healthcare systems become more adaptable, sustainable, and resilient.
Implementing QBHC: key considerations
Transitioning from VBHC to QBHC requires thoughtful change management. Here’s what it takes to make it work:
Defining “quality” clearly: The evidence base, translated into national and local guidelines must outline what high-quality care looks like, ensuring consistency without unnecessary rigidity.
Establishing strong governance and peer review structures: Clinical audits, peer evaluations, and transparent performance

tracking uphold professional standards without resorting to financial penalties.
Investing in data and technology: Electronic health records, benchmarking tools, and real-time feedback systems support continuous improvement, ensuring data is used for learning rather than merely justifying payments.
Aligning financing with long-term goals: Payment models should support long-term investment, preventative care, and highquality decision-making rather than shortterm cost-cutting.
Engaging clinicians and patients in the process: Frontline healthcare providers must help design QBHC frameworks—
ensuring that metrics and expectations are realistic and clinically meaningful. Patient feedback should drive improvements, capturing qualitative aspects of care that numbers alone cannot measure.
The
way forward: A more resilient, patient-centred future
VBHC began with good intentions, but its rigid focus on short-term metrics has created systemic distortions—penalising clinicians for factors beyond their control and discouraging equitable access.
QBHC provides a more sustainable, evidence-driven alternative. It upholds professional standards without discouraging care for high-risk patients, fostering continuous improvement instead of forcing providers to chase financial targets, and
ensuring financial stability, so healthcare organisations can plan for long-term success.
If we want a truly resilient healthcare system, we must look beyond financial performance targets and prioritise quality as the foundation of care delivery. This may mean assessing the scope of healthcare that can be a orded while ensuring that the quality of care patients receive remains the primary focus. But that is a discussion for a di erent time.


RESHAPING THE CARE MODEL
Enabling patients to understand their own health information to make informed decisions is paramount, says Mohammad AlUbaydli, CEO of Patients Know Best
This month, as the global healthcare community gathers at Abu Dhabi Global Health Week, the transformative potential of digital health and AI takes centre stage again.
At Patients Know Best (PKB), we believe this technological revolution is not just about innovation but about fundamentally reshaping the care model by placing the patient at its core.
Our mission is to empower patients to “know best” by ensuring they can own, understand, and use their health information to make informed decisions with their care team.
This approach benefits patients directly and, when enabled by technology, can revolutionise care delivery, especially in resource-constrained environments. We envision patients as equal partners in their health management, and active providers in its delivery. To achieve this, patients need access to their health records, the ability to understand the information, and the means to act on it.
Data as a cornerstone
PKB has always prioritised securely sharing data with patients, because we recognise data as the foundation for patient engagement and personalised care. Healthcare systems have increasingly embraced automated data sharing, but patient engagement remains inconsistent. While people like Richard Stephen (see case study), who has kidney disease, demonstrate the potential of active patient involvement, they rely on naturally motivated individuals, both clinicians and patients.
We’re now moving beyond this passive engagement digitally - relying on clinicians working to activate patients - to a new era of automated digital activation of patients. By engaging patients with their data and

intelligently explaining what the data means and what the patient must do next, we can automate activation and reduce the burden on the health system.
A new era of activation
A er years of patient registration and data hosting, PKB is poised to deliver meaningful change at scale. We have significantly enhanced our architecture with FHIR, ensuring optimal data handling and we have streamlined interaction for all stakeholders. By integrating an engaged patient user base with their data and the ability to intelligently support their understanding and action, we can now move to automated patient activation, reducing the burden on stretched healthcare providers.
This approach requires collaborative e orts to define actions based on coded data and to align with the preferences of healthcare providers and health economies. Rules generated by third parties, such as healthcare providers, can automatically prompt patients to take action in specific scenarios. This shi removes the burden of initiation from clinicians, empowering patients as proactive partners in their care.
What lies ahead: clinical trials and medication optimisation
Our immediate focus is on clinical trials, helping to bridge the gap between frustrated patients who are not aware of all their options and organisations struggling with recruitment alongside day to day care. We aim to enable organisations to share trial information with eligible patients via

PKB based on structured known criteria, most notably their diagnosis with our patient-consented approach, ensuring the patient’s data is not shared until they decide they would like to.
The second area of expansion is medication optimisation, such as

MOHAMMAD AL-UBAYDLI CEO Patients Know Best
“Patients need access to their health records, the ability to understand the information, and the means to act on it”
prompting patients to contact their organisation for a medication review. Medicines optimisation introduces the capability to use snomed codes in data held in PKB records to apply rules set by clinicians to prompt automated action and early intervention. For example, if you have gout, and are on Allopurinol, have you had your annual check for urate? This process takes the onus away from clinical teams and within PKB we will prompt patients to take action where it may have been missed. The record will then also allow for changes and optimisations to be tracked and quantified as a result of the notifications.
It’s early days, yet the potential is immense. We are witnessing the dawn of a new era in healthcare, one where technology empowers patients to become active participants in their well-being.
The Patient Perspective: What Really Matters in Digital Health
If you’d like to know more, don’t miss this fireside chat on ‘The Patient Perspective: What Really Matters in Digital Health’ 11.25am at Abu Dhabi Global Health Week. Steve Gardner will be sitting down with Dr Mohammad Al-Ubaydli to discuss the role of the patient and their involvement in the digital health ecosystem and to share his insights from his new book Digital Health Records for Governments.
Case study: Kidney patient, Richard Stephen
Diagnosed with Stage 5 Chronic Kidney Disease in 2019, Richard Stephen faced a stark prognosis, but he was determined to maintain his quality of life and avoid dialysis or a transplant.
Access to his health record on Patients Know Best (PKB) became vital. It empowered him to meticulously track his test results and start research on what was needed to improve them.
This information enabled informed discussions with his healthcare providers and further guided his research. PKB led him to actively manage his condition by tracking his blood pressure, documenting exercise and meal plans and maintaining a library of research documents.
Five years later, Richard has defied expectations by avoiding dialysis and a transplant. He attributes this success to the detailed tracking, and the tools and analysis made possible by PKB, demonstrating the power of patient activation in chronic disease management by comprehensive conservative kidney care.

hello@patientsknowbest.com

DATA & AI



DEVELOPING RELIABLE HOSPITAL PERFORMANCE BENCHMARKING
Julie Coope, Associate Director BRG, Simon Swi , surgeon and data expert, and Simon Jones PhD, Professor of Population Health at New York University, discuss how to harness data e ectively
The growing volume of detailed data generated from routine healthcare processes presents not only a significant challenge for healthcare organisations, but also an unprecedented opportunity to improve how care is analysed, administered and tracked. E ectively harnessing this data is a complex task and requires robust and reliable collection processes.
The collection, curation and careful use of accurate data is crucial for tracking patient outcomes and ensuring longterm success. Julie Coope is a Registered
General Nurse (UK) and Registered Nurse (US), as well as an associate director in BRG’s Global Health group addressing data collection and quality for health systems. She was recently joined by two experts: Simon Swi , a doctor, health economist, business leader and external advisor who worked in the National Health Service (NHS) and as an exited founder of a health data services company; and Simon Jones, PhD, a professor of population health in the Department of Population Health at New York University.
JULIE COOPE (JC): Data collection and quality management are foundational elements of the modern healthcare delivery and improvement process. The increasing complexity of health systems, coupled with the growing emphasis on evidence-based practice and value-based care, has made robust data collection and management more critical than ever. While some organisations and regions may do this better than others, nobody has mastered this.
SIMON SWIFT (SS): The desire to collect ‘reliable healthcare quality data’ is more complicated than most hospital executives realise. One challenge that faces healthcare organisations involves the variety of sources of data that exist. Some of this is structured data, but much remains unstructured in the form of text and images. A lot of e ort is required to transform


“It’s
SIMON JONES PHD Professor of Population Health New York City University
essential to make sure everyone is using the same data and definitions. One needs consistency with data and definitions for payment and quality monitoring. It’s a red flag when you see variations in how data is defined”
unstructured data into coded data, and we see increasing investment and support directed to these processes, including to digitise health records and automate processes, but much of this is still done by people, and people are fallible. That means that the data created is not always ‘reliable’.
SIMON JONES (SJ): I agree and would add that we need to ask ourselves two questions when we are interpreting and comparing data. First, what is the motivation of the person recording the data to be accurate? Second, do they use that information for their own purposes? Without ensuring that those collecting health data understand what they are recording, and that it has a use for those teams (as opposed to being fed into some health data collection system), there is a high likelihood that the information will not be as reliable as one might hope or expect.
Understanding data recording can be complicated to collect reliable health quality data; how can we encourage organisations to work towards a single source of truth (SSOT)?
JC: There is a desire for organisations to have one version of the truth, but the motivations and use of that SSOT vary by region and health system. For example, organisations in some regions are heavily incentivised by finance so their documentation focuses more on reimbursement. Other areas may be more heavily incentivised by quality or population health benchmarks. The value placed on enabling reimbursement may be influenced by the unique incentives and priorities in di erent regions or systems.

SS: It comes back to knowing who is recording this data, and why it is being recorded. For example, when a woman gives birth, it is common for there to be a certain amount of blood loss. Sometimes this is recorded in defined measurements, and other times it’s recorded in more general terms like minor, medium or major. This is only one variation, but there are many in medical procedures, and as a result you find variation in the terminology of data that has been recorded. This variation tends to create di erent truths.
SJ: Another challenge involves the need for organisations to simplify clinical coding. This can create variation in coding. If you think about a typical clinical consultation, there are o en a couple of thousand words exchanged, and there can be complex interactions with multiple measurements taken. That entire interaction is then distilled into several codes which remove context and can lead to di erent sources of the truth.
SS: Correct. Another consideration is the impact financial incentives have on how consultations are recorded. For example, changing the complexity of how a clinical course is coded can increase or decrease fees and can lead to apparent variations in care which do not reflect clinical reality all the time.
How can healthcare organisations balance advanced data analysis (such as artificial intelligence and machine learning) with the need for foundational data literacy and standardised documentation for more reliable global comparisons?
SS: Many years ago, when I was running a function for the NHS, we collected a significant amount of data related to quality of care from hospitals in the UK. A er careful analysis, we published the findings on a public-facing NHS website. Several hospitals were outliers, and the


initial reaction by executives from those organisations was anger and frustration because they felt they had been singled out. However, soon a er that initial reaction, board members from those same organisations reached out to learn more about what needed to be done to help address the issues highlighted in the

SIMON
SWIFT
Surgeon & Data Expert
“To improve comparability between organisations you often end up with very focused measures because
the narrower you focus, the more likely you can compare like with
like”
benchmarking report. The lesson I learned was that surfacing information based on lowquality data could be a powerful incentive to get the attention and resources of leaders to improve their data collection e orts.
JC: Organisations can use such findings as an incentive as you mentioned, but there is a data literacy gap as well that makes understanding these global comparisons especially challenging. It requires a significant investment to find people who understand what the data means and to do the necessary inputs, collections and coding correctly. This requires engaging people across an entire organisation at all levels.
Given the disparities in resources and organisational maturity across di erent regions, how can we ensure meaningful comparisons of data or outcomes?
SS: This is a really di icult question to answer. I would start by looking to see if the data standards and classification systems
used are comparable. What incentives or disincentives are there to use specific codes; and, at a fundamental level, what are they recording?
SJ: Another key consideration is understanding the workforce and defining the roles and responsibilities of those clinicians involved in treating and collecting patient data. The way in which these roles are defined and how care teams treat a patient varies widely. This variation inevitably leads to disparities in how organisations are resourced and in patient outcomes. One way to gain more context is to focus on collecting and reviewing qualitative data. What do patient satisfaction surveys tell us, what is being shared in social media, etc.?
JC: I agree that understanding incentives is crucial. For example, if there is an incentive to document a particular diagnosis or procedure in one region versus another will lead to disparities. Also, understanding what patient pathways and organisational structures are used to diagnose and care for a patient is crucial, because di erent regions address this very di erently.
SS: An example of narrowing the focus would be to look at readmission rates. One would need to know many system factors to develop such a comparison, but if, for example, you look at readmission rates following primary coronary artery bypass surgery in women over a certain age, you’re less likely to have system factors to address. In addition, looking at readmission rates will engage the clinicians on the ground whose now ‘metaphorical’ pen is responsible for the data creation.
Summary
Accurate, comprehensive healthcare data can provide organisations with a strategic advantage and better position health systems for future success. By prioritising rigorous data collection and establishing a single source of truth, leaders can make more informed decisions, optimise resource allocation and better forecast future demands. Investing in robust data capabilities will ultimately deliver better patient outcomes and more sustainable services for your organisation.


BRIDGING THE DIGITAL DIVIDE: HOW HEALTHCARE CAN LEARN FROM BANKING
Digital banking apps point the way forward for patient selfmanagement to improve healthcare, believe Gerard Hanratty, Head of Health and Life Sciences, and Carly Caton, Partner, at UK and Ireland law firm Browne Jacobson
Making payments, collecting savings and budgeting plans can all be completed with the touch of a few buttons on smartphone apps. For many people, such apps have replaced the need to visit physical banks or use telephone services for managing day-today finances.
Yet in healthcare – particularly in statebased systems such as Britain’s NHS – it’s o en the case that patients must call their GP or even queue outside their practice between 8am and 8.05am to have a chance of a same-day appointment, required for follow-on treatment or a prescription.
In an era where technology seamlessly integrates into our daily lives, the healthcare sector remains an outlier.
An outdated regulatory system prevents patients from taking the same control over their health data as they can with financial data, not to mention personal information, in many other parts of our lives.
The ability to share such data with healthcare providers and other relevant bodies could hold the key to the macro shi from a predominantly curative healthcare system that prioritises treatments of diseases to a preventative model, characterised by
early interventions, to address numerous challenges faced by state-based healthcare systems.
It could drive operational e iciencies to free up clinician and sta time, improve care by giving providers a more holistic picture of a patient’s health and support population-wide initiatives such as incentivisation for leading a healthier lifestyle. Cross-border data sharing could also enable collaborative research projects on diseases such as cancer.
The best part is this isn’t a future technology to plan for but one we have access to right now. Yet we aren’t taking advantage of existing healthcare apps or wearables and reaping the benefits such action could drive.
Learning from the digital banking revolution
Banking has long embraced digital technology, o ering customers smartphone apps and real-time metrics to manage finances e ortlessly.
UK Finance reported that 87 per cent of adults used a form of online or remote


banking in 2023 – up from 54 per cent a decade earlier and amounting to about 47m people. Three in five (60 per cent) people were using mobile banking, about 32m people.
Challenger banks such as Monzo, Revolut and Starling have innovated user interfaces to enable customers to pay bills, send payments to friends, monitor spending, create savings pots and manage mortgages on a single app.

GERARD HANRATTY Head of Health and Life Sciences Browne Jacobson
“Countries like Estonia and Denmark are pioneers in this field, having integrated digital health solutions that allow citizens to access and manage their medical data online securely”
Healthcare can replicate this model to empower patients. Apps that track health metrics such as blood pressure, glucose levels and medication adherence could revolutionise patient self-management and preventive care.
Countries like Estonia and Denmark are pioneers in this field, having integrated digital health solutions that allow citizens to access and manage their medical data online securely.
Incentivisation for good health
Last year, a study led by health experts at the University of Stirling found that o ering financial incentives is e ective in helping men to lose weight.
The research split 585 men living with obesity across England, Scotland and Northern Ireland into three groups. They were each given short, medium and long-term weight loss targets but with varying levels of support and incentives. The group that received supportive text messages plus the opportunity to earn £400 for hitting targets lost the most weight.
Incentivisation is an under-explored mechanism for achieving objectives in healthcare, but could be a crucial driver in encouraging people from inactivity to activity.
The NHS Couch to 5K programme is a great example of how this could work, while in private healthcare we’ve seen companies like Vitality o er Apple Watches as part of private health or life insurance plans, with customers able to reduce payments by undertaking physical activity.
Engaging, user-friendly and supportive environments are key to successful health self-management, and we are already seeing some great examples of how technology and education is being combined to encourage people to take active roles in managing their own health. These include:
• Health-tracking apps and wearables: Providing real-time data on measurements such as physical activity, sleep and diet be supported by features including goal setting, reminders and rewards to enhance engagement.
• Gamification: Incorporating game-like elements into health management tools, such as earning points, badges or completing challenges.
• Personalised health plans: Tailoring AIdriven plans based on a person’s health data, preferences and goals, making them more relevant and e ective.
• Educational resources: Providing accessible, clear and engaging educational materials about health, wellness and disease prevention.
• Financial incentives: Insurance premium discounts, vouchers or direct rewards can be a powerful motivator for many people.
• Social support networks: Community platforms where individuals can share their experiences, challenges and successes to boost motivation and accountability.
Many people are already signed up to a large number of these applications and taking key measurements of their health every day to determine how many calories they’ve burned or if their heart rate is a cause for concern.
This data has powerful potential, if plugged into the right platforms and organisations, to drive better health outcomes and reduce healthcare costs – yet this is only happening in certain parts of the world or in limited circumstances.

CARLY CATON
Partner Browne Jacobson
“Creating digital health wallets can be a costeffective and relatively easy solution to active health management”
Active health management is a key pillar of creating a preventative healthcare system. By identifying issues before they arise, lifestyle changes can be made to avert the need for treatment and clinical resource.
Digital health wallets could pave the way forward
Creating digital health wallets can be a cost-e ective and relatively easy solution to active health management. These are secure, centralised platforms that store, manage and share personal health information.
O en accessed through a mobile app, digital health wallets empower individuals to control their own health data, and facilitate access and management by trusted healthcare providers and as permitted by the individual.
Independent providers in the UK are creating these wallets, but the UK’s NHS app is arguably the most powerful of them all should it be given the right environment to flourish. At present, it is very underutilised, as are so many potential sources.
A digital wallet provides secure access to view and manage information from a user’s GP and other healthcare records, including appointments, test results and medications. The Covid-19 pandemic accelerated its rollout, but further progress has been limited since the end of lockdown.
There’s huge potential to enhance the NHS app so that users can book appointments at any GP, attend virtual appointments where appropriate, and access follow-up treatment, services and prescriptions. At a time in which the government wants to reform the NHS into a more streamlined organisation, this upgrade could generate huge cost and resource savings.
Taken even further, integrating this app with other digital tools already being used

to collect and monitor an individual’s health and lifestyle, it’s clear to see the enormous potential technology has to spearhead a truly preventative healthcare system.
Challenges and potential solutions in bridging digital divide
While the integration of digital tools presents a promising outlook, state-based healthcare systems face unique challenges.
The primary concerns revolve around data security, patient privacy and the digital divide that could marginalise those without access to technology.
Addressing these issues requires robust cyber security measures, widespread digital literacy campaigns and policies ensuring equitable access to digital health tools.
More broadly, regulatory frameworks must evolve for digital technology to reach its full potential in healthcare.
Facilitating the sharing of personal health data and anonymised data across borders can accelerate research and development, leading to breakthroughs in treatment and disease management.
Last year, Browne Jacobson contributed to a report entitled Opportunities for collaboration between the UK and UAE in cancer care by the UAE-UK Business Council in a section on barriers and opportunities regarding data sharing and privacy.
We called for governments to co-operate in aligning their respective regulatory regimes to achieve data adequacy. This agreement would enable them to
collaborate more e ectively in a global health data exchange that powers new research and development into diseases that don’t have international borders, such as cancer.
Developing joint health data hubs, harmonising ethical and technical guidelines for AI and genomics, and facilitating cross-border clinical trials and research partnerships, could also go a long way to making significant progress in discovering cures to diseases.
Governments can take cues from the European Union’s GDPR approach to data protection and privacy, ensuring that data sharing is secure and transparent. Additionally, international co-operation, such as in the EU’s health data sharing projects, can set a precedent for global health data exchange.
A call for global collaboration
As we continue to navigate the complexities of digital integration in healthcare, the lessons from banking provide a beacon of innovation and e iciency. It is imperative that we seize this opportunity to transform healthcare, making it more accessible, secure, and patient-centric through digital technology.

CONVOY OF HOPE
Delivering medical aid, equipment and food to Ukraine
In May 2022, Simon Brake and three friends came together with a vision to provide vital medical aid to Ukraine during the ongoing conflict. Mighty Convoy has now evolved into a significant humanitarian mission, run entirely by volunteers. Joining forces with International Christian Medical and Dental Association (ICMDA), and Christian Medical Association of Ukraine (CMAU), this new charity partnership is now known as the Convoy of Hope and was o icially launched at The Palace of Westminster.
The reception was hosted by Daisy Cooper MP, who reminded supporters that three years has passed since the Russian invasion of Ukraine, and the need for humanitarian aid is still ongoing. A significant proportion of humanitarian aid arriving in Ukraine is donated, funded and/or transported by small organisations and charities. Mykhaylo Korchynskyy, a lawyer and lieutenant in the Armed Forces of Ukraine, travelled from Ukraine along with Uliana Kovalyshyn of CMAU to express their thanks on behalf of the people of Ukraine for the vital help they are receiving.
To date, Mighty Convoy (mightyconvoy. org) has organised an impressive 12 convoys
delivering 49 vehicles to Ukraine, including 38 ambulances and 9 pick-up trucks, and 2 refrigerated vans donated by Iceland and Sainsburys supermarkets, filled with 35 tonnes of medical aid, and 30,000 meal pouches donated by the Country Food Trust. It has raised more than £330,000 from generous donors and the convoys benefit from the support of organisations such as Specialist Vehicles Solutions, which provide the ambulances that are essential to the operation, many of which are still in service in Ukraine.
The new charity pools fundraising, medical, logistical and freight expertise. ICMDA provides the bulk of the medical aid transported by the convoys, ensuring that the vehicles are stocked with lifesaving supplies, ranging from oxygen concentration units to field dressings, anaesthetic machines, and baby incubators recently donated by the Royal London Hospital. CMAU plays a pivotal role in distributing the supplies once they arrive in Ukraine, enabling the medical aid to reach more than 300 hospitals, clinics, and frontline units across the country.
Mighty Convoy operates a “pay-to-drive” funding model. Volunteers raise £7,000 per vehicle, which goes toward the procurement of vehicles, collection of medical aid, and the organisation of the convoys. These volunteers drive the vehicles to Ukraine and witness first-hand the profound impact their e orts have on those in need.
List of ambulance requirements
Defibrillator
Oxygen cylinder (full set with humidifier)
Laryngeal mask
Blood pressure monitor
Subclavian catheters
Portable ECG monitor
Hard plastic stretcher with patient fixation
Electronic and mercury thermometers
“There are some people who have driven down to southern Europe, so they are used to long distance driving. It’s tiring but we stop regularly to make sure the drivers swap over,” says Simon who had visited Ukraine before the war. “There’s a frisson of excitement when we arrive at the border and arrive finally in Ukraine. I’m pretty used to it now, but for everyone else they are faced with the reality of everything they have only ever seen on the news.”
At the event Uliana Kovalyshyn of CMAU revealed that so far 173 medical facilities have been destroyed completely and more than 1200 damaged. “There are 50,000 Ukrainians now who have lost limbs. The ambulances are an essential link with the patient and hospitals, as the ability to quickly evacuate wounded soldiers or patients in critical moments can mean di erence between life and death,” she said.
Several UK NHS trusts supply the Convoy of Hope with equipment from ventilators to incubators to anaesthetic machines to dressings. “But we could do with much more,” says Simon Brake. “We need NHS trusts, private hospitals and medical suppliers to open their doors and send us what they don’t need any longer, rather than sending it to incinerators or landfill. That will make a phenomenal di erence.”
Tourniquets www.mightyconvoy.org


LEVERAGING AI FOR HEALTHCARE EDUCATION
AI can help tailor training programmes for the individual to maximise e iciency, says Nick Dobrzelecki, co-founder of The Learnery
Iremember the first time I heard someone mention AI in healthcare education. It was a couple of years ago, and at the time, the focus was on AI’s potential to create content. But for me, the conversation that was missing—the one I felt we needed to have—was about the
ethical and moral implications of AI in our field. We have a responsibility to ensure that the databases we use are accurate and that the data we rely on is protected. This is not just a technological concern; it’s a fundamental issue of trust and responsibility.
One of my biggest concerns with AI in education is the reliance on the internet as a source of truth. Many companies are using AI to generate content, pulling information from the web without rigorous validation. That approach is not just flawed; it’s dangerous. In our work, we have made a deliberate decision not to use AI for content creation until we have a structured database of verified educational material. For us, that source of truth must be something as reliable as NHS content. Without a vetted, standardised foundation, AI-generated content risks being riddled


with inaccuracies, ultimately harming the very people it aims to educate.
While AI-driven content creation is o en touted as the future, I believe that’s the easy part. Developing algorithms to generate content is relatively straightforward. What is far more complex—and far more valuable—is using AI to enhance productivity in ways that actually support learners. This is where AI’s potential excites me: not in writing textbooks, but in tailoring education to individuals in a way that maximises e iciency and e ectiveness.
Creating individualised learning paths
Right now, we train all learners the same way. Regardless of prior experience or education level, everyone starts at the same baseline. That’s an outdated and ine icient model. AI gives us the opportunity to change that. Imagine a system that assesses a learner’s background, education, and experience before they even begin training. Instead of a one-size-fits-all approach, we could create individualised learning paths—shorter, more focused orientations for experienced professionals, and longer, more supportive training for those just starting out.
This shi would have significant benefits, not just for learners but for healthcare organizations as well. If we can fasttrack experienced professionals through their training while providing additional support to those who need it, we reduce frustration, increase engagement, and, most importantly, get sta into patient care roles more quickly and e ectively.
Take nursing, for example. We know that burnout is a major issue, particularly in the first three to four years of a nurse’s career. A significant part of that burnout comes from feeling overwhelmed and underprepared. If AI could help tailor training to individual needs—o ering more guidance where necessary and removing unnecessary bureaucracy for experienced nurses—we could ease that transition and improve retention rates.
Likewise, senior sta o en feel frustrated by redundant training. They are required to check o the same boxes year a er year, even when they’ve mastered the material. If AI could assess their competencies and verify their knowledge in real time, we could eliminate unnecessary steps and allow them to focus on what truly matters: providing excellent patient care.
Integrating healthcare systems to support clinicians
But AI’s potential in healthcare education goes beyond training. Integration is the next frontier. Right now, our systems— electronic medical records (EMRs), learning platforms, diagnostic tools—exist in silos. This lack of integration creates ine iciencies and gaps in education and patient care. At an upcoming conference in Abu Dhabi, I’ll be speaking about how we can bridge these gaps. How do we integrate EMRs with learning management systems? How do we connect radiology and diagnostic data with training modules? The ultimate goal
is to create a seamless, intelligent system that not only educates but also supports clinicians in real time.
Imagine an ecosystem where AI continuously learns from a clinician’s experiences, updating training programmes dynamically based on real-world performance. Instead of rigid, scheduled training modules, education would become fluid and adaptive. AI could analyse data to determine which competencies need reinforcement, tailoring training to individual and organisational needs. This kind of personalised, just-in-time education would revolutionise how we think about professional development in healthcare.

NICK DOBRZELECKI Co-Founder The Learnery
“AI can help deliver targeted education, ensuring that both new and experienced clinicians receive the training they need without unnecessary redundancy”
This level of sophistication requires us to build ethical AI models from the ground up. Instead of retrofitting AI onto existing data, we are taking a structured approach—creating standardised databases first and then layering AI on top. By learning from past mistakes, we can build a system that is not only e ective but also ethical and transparent.
For clinicians at the top of their field— surgeons, cardiologists, specialists—AI could play an even more nuanced role. These professionals already engage in continuous learning through research, teaching, and professional development. But AI could help ensure that their knowledge remains cuttingedge. Instead of testing them on the basics, AI could assess their familiarity with the latest guidelines and best practices, ensuring they are always operating with the most current knowledge.
Take the example of an ICU nurse. A new graduate may have learned the latest evidence-based practices in school but lacks hands-on experience. Their training should focus on reinforcing knowledge and building confidence. In contrast, a seasoned


nurse may have decades of experience but could benefit from refreshers on high-risk, low-utilisation scenarios—those rare but critical situations where up-todate knowledge can mean the di erence between life and death. AI can help deliver targeted education, ensuring that both new and experienced clinicians receive the training they need without unnecessary redundancy.
Globalising
healthcare education
This approach also has global implications. Healthcare is increasingly international, with clinicians moving across borders to fill workforce gaps. Yet, standards of care vary from country to country. AI-driven education could help standardise training worldwide, ensuring that a doctor trained in the UK could seamlessly transition to a role in Riyadh or New York. By integrating AI into healthcare education on a global scale, we could improve consistency and quality of care across borders.
Of course, change is never easy. One of the biggest challenges we will face is shi ing mindsets. Healthcare professionals

NICK DOBRZELECKI Co-Founder The Learnery
“AI-driven education could help standardise training worldwide, ensuring that a doctor trained in the UK could seamlessly transition to a role in Riyadh or New York”
are accustomed to traditional training models and adapting to an AI-driven system will require a cultural shi . There will be questions: Why is my training di erent from my colleague’s? Why do I have to complete six weeks of training while someone else only does two? We will need to educate not just our learners but also our organisations, demonstrating that this approach is about fairness, e iciency, and, ultimately, better patient care.
We are at the doorstep of the future. The technology is here. The data is being structured. The opportunities are endless. Now, the challenge is not just implementing AI, but rethinking how we approach education, training, and professional development in healthcare. The question is not if AI will transform healthcare education—it’s when, and more importantly, how we ensure it is done ethically, e ectively, and equitably. This is not a distant vision for 2050. This is happening now. In the next few years, we will see AI-driven education platforms revolutionise how we train healthcare professionals, making learning more personalised, e icient, and impactful. We are not just preparing for the future—we are building it.





MEETING THE DEMANDS OF THE HEALTHCARE LANDSCAPE
Upinder Bhat, President and COO DVI Health Solutions Inc, tells Healthcare World about their innovative work in the sector
As the healthcare sector moves toward advanced so ware to improve operations and patient care, legacy systems struggle to keep up. They o en lack the flexibility and interoperability needed to thrive in today’s complex ecosystem, making it di icult for hospitals and clinics to share patient data e ectively. This fragmentation can lead to delays in treatment or errors in patient care, so organisations are increasingly turning to advanced so ware solutions to make operations safer and more e icient.
Outdated systems can result in serious backlogs: during the COVID-19 pandemic, many healthcare providers struggled to e iciently manage vaccine appointments due to inflexible legacy systems. While another global pandemic may or may not be hovering on the horizon, it is paramount that healthcare systems have the latest so ware as part of their push for preventative care.
At the same time, it’s o en true with healthcare innovation that bitter experience leads to productive solutions. Upinder Bhat, President and COO of DVI, discovered this to be true when he spent time taking his great friend to regular hospital and pharmacy appointments for diabetes treatment. “I realised there was no communication between the hospital

UPINDER BHAT President/COO DVI Health Solutions Inc
“DVI believes in evolving alongside the healthcare industry and equipping our customers with the most advanced solutions to meet the demands of a rapidly changing landscape”
and the pharmacy and this led to a lot of wasted time and e ort on everyone’s part,” he recalls. “It was clearly the result of legacy systems which are not equipped to handle the growing demands of today’s world.”
As DVI specialises in modernising outdated platforms and o ers cloud-based solutions that improve performance, security, and scalability, it was obvious to the tech entrepreneur that the solution to pharmacy compatibility issues actually lay within his grasp. Upinder realised he could blend his vast experience in technology with DVI capabilities to establish a new system specific to pharmacies.
Revolutionising healthcare
By o ering customised solutions for the healthcare industry, DVI focuses on improving patient care, streamlining workflows, and boosting e iciency. Through advanced data tools and predictive analytics, the company enables its clients to make better, data-driven decisions via a simplified cloud-based, end-to-end so ware option. “Cloud technology o ers unparalleled advantages in terms of cost savings, scalability, and accessibility. DVI assists in migrating client applications and infrastructure to the cloud,” says Upinder. “Our team ensures that cloud environments are optimised for peak performance, providing realtime access to data and facilitating better collaboration across teams.”
Their platform reduces the need for multiple systems by automating tasks, enhancing patient care, and providing configurable workflows. Using advanced analytics, DVI supports healthcare professionals with real-time insights into patient data, prescriptions, and treatment specifics. “Our analytics solutions help organisations make sense of large volumes of data to enable more informed decisions,” explains Upinder. These decisions can be made faster, ultimately improving the quality of care, such as more

rapid treatment with faster prescriptions. Their technology creates coherent systems where tasks that once took days can now be completed in minutes. For example, a shi to microservices has revolutionised processes such as verifying patient eligibility, cutting delays and improving service delivery.
“We’re now at the stage with AI and RPA (robotic process automation) where it seems hard to believe that systems don’t and can’t talk to each other,” says Upinder. “On the one hand we can communicate across the world, but on the other hand we struggle to send a simple update from one provider to another.” Solving such global issues may well be the work of governments, but it’s companies such as DVI that identify where small fixes can make

huge improvements. “Data is at the core of modern operations. Our analytics solutions help organisations make sense of large volumes of data to make more informed decisions.”
Speciality pharmacies
Specialty pharmacies manage complex therapies for chronic and rare conditions, necessitating meticulous coordination among healthcare providers, insurers, and patients. This complexity demands advanced technological solutions to ensure e iciency and optimal patient care. By partnering with healthcare customers to build custom solutions, Upinder and his design team are enabling such specialised pharmacies to serve their clients better and faster.
By working hand in hand with healthcare partners to co-create solutions that are e ective, DVI enables their customers by building a comprehensive suite of solutions designed to address their specific needs and pain points. They o er a seamless end-to-end experience, enabling pharmacies to automate manual tasks, integrate customisable workflows, and access real-time patient data. By consolidating disparate systems into a single, secure, and scalable platform, their solutions empower specialty pharmacies to operate more e iciently, reduce costs, and improve patient outcomes.
Expanding horizons
Looking ahead, DVI is investing in artificial intelligence to revolutionise healthcare.
“With an AI based product that DVI currently o ers, we are poised to introduce transformative tools that enhance predictive care, improve clinical workflows, and drive databased decision-making,” says Upinder.
“DVI believes in evolving alongside the healthcare industry and equipping our clients with the most advanced tools to meet the demands of a rapidly changing landscape.”

DRIVING TRANSFORMATION IN HEALTHCARE DELIVERY
Burendo is playing a pivotal role in the successful delivery of complex and high-profile national programmes, founder and CEO Glenn Crossley tells Sarah Cartledge, Healthcare World Editor
The British healthcare sector faces many challenges including tightening budgets, outdated digital infrastructure, increased accessibility requirements and higher cyber security risks. All these issues are putting already resource-stretched teams under additional pressure.
As an organisation, Burendo has extensive experience of working with healthcare organisations to simplify solutions, optimise services, streamline data, improve patient care and get products and services delivered, all within highly regulated, dynamic environments in both the public and private sectors. The company has been involved in several recent programmes contributing to national healthcare initiatives that are fundamental to improving service delivery, patient care, and operational e iciency.
Founder Glenn Crossley is unusual in that he doesn’t come from a traditional tech background. He began in the Royal Marines, where he honed discipline, leadership, and a tactical mindset which served him well when he moved into the public sector at the Department of Health where he played a pivotal role in creating the Shipman Witness Database.
As a result, he found himself in team management roles just a month a er starting his first job. Over the years, Glenn’s career evolved across multiple sectors, including financial services, healthcare, and tech delivery, building a diverse and robust portfolio of expertise in so ware delivery, data integration, and public sector digital transformation. In 2018, Glenn earned significant recognition as a top influencer in the tech world through his work with Gartner. He went on to found Burendo out of his desire to create something impactful within the tech and healthcare sectors.
Growing Burendo
The Blended Agile Delivery (BAD) toolkit served as the foundation for Burendo’s growth. The open-source toolkit was developed to compile the best practices in agile so ware delivery, and Glenn’s vision was clear—to provide organisations with the tools they needed to accelerate their digital transformation e orts. As a result, Burendo quickly grew from a small consulting firm into a tech powerhouse, expanding to 150 employees and becoming the UK’s fastest-growing tech company, building strong relationships with major organisations such as ASDA, Equifax, NHS, and William Hill as Burendo solidified its reputation as a leader in delivering highperformance technology solutions for the public and private sectors.
Transforming government programmes
• COVID-19 Response: Burendo played a crucial role in the rapid deployment of the NHS COVID-19 vaccination booking system, enabling millions of people to access vital vaccinations e iciently. In addition to the vaccination booking system, Burendo helped develop and implement the COVID Pass, which allowed citizens to safely and securely prove their vaccination status, facilitating the safe reopening of society. These


solutions contributed significantly to the government’s e orts to manage the public health crisis.
GLENN CROSSLEY CEO Burendo
“Together with UKHSA, we’ve developed a public health data dashboard that’s simple to use, easy to update, and designed to grow with increasing health data”
• NHS DigiTrials: Recognising the importance of accelerating clinical research, Burendo partnered with NHS DigiTrials to enhance the platform’s capabilities. An agile strategy and outcome-based delivery approach streamlined the clinical trials process, improving e iciency and accessibility for researchers and patients alike. Burendo’s ability to integrate innovative solutions with real-world healthcare needs has created faster access to clinical trials for patients. “Utilising data and automation, we’re proud to have provided assistance in this national clinical-trials government project e ectively saving lives and tackling some of the biggest healthcare challenges,” says Glenn.
• Cancer Waiting Times: Burendo has contributed to the improvement of cancer waiting times by providing

data analytics and programme management expertise. By optimising processes and streamline workflows, Burendo has contributed to the NHS’s e orts to reduce delays and improve patient outcomes, using data to understand bottlenecks and then implement solutions to reduce them.
• Vaccine Booking System: Burendo’s team, within the Vaccination Data Service (VDS), is assisting the UK’s Respiratory Syncytial Virus (RSV) vaccination programme. The programme has already achieved a significant 62 per cent reduction in RSV-related hospitalisations among individuals aged 75-79. Their support involves identifying approximately 800,000 people with email addresses in the Personal Demographic Service (PDS), and a total of 1.2m individuals who are eligible for the vaccine.
• UKHSA Data Dashboard: As a strategic partner of the UK Health Security Agency (UKHSA), Burendo played a critical role in the delivery of
the data dashboard. This comprehensive tool provides real-time insights into public health threats, enabling timely and informed decision-making.
https://ukhsa-dashboard.data.gov.uk/
Burendo, within Genomics England’s high-performance computing teams, has been at the forefront of creating integrated data solutions that empower healthcare organisations to make better, faster decisions. This has been achieved by leveraging his expertise in designing and managing largescale high-performance and high-throughput computing (HPC/HTC) clusters across hybrid multi-cloud distributed systems, directly contributing to groundbreaking advances in genomics and precision medicine through the continuous improvement of these critical computing infrastructures.
One of the core elements of its approach is a commitment to agile methodologies, prioritising flexibility, rapid iteration, and continuous improvement. Burendo places a strong emphasis on designing solutions that are intuitive and accessible. This
user-centric approach is particularly critical in healthcare, where patient engagement and adherence are key to successful outcomes. Whether designing a vaccination booking system or a clinical trials platform, Burendo ensures that all solutions are easy for patients to navigate, leading to improved engagement and a more seamless experience.
By harnessing the power of data analytics, Burendo provides actionable insights that help healthcare organisations make informed decisions. From identifying operational bottlenecks to predicting patient outcomes, these data-driven solutions optimise healthcare delivery, improve e iciency, and support better decision-making at all levels of the healthcare system.





Prioritize clinical benefit and safety for patients with our dedicated medical team



Create your own health management program in under one month

Generate real-world evidence through patient-reported outcome and clinical data
We have touched the lives of more than 250,000+ patients through our collaborations









TAILORED SPACES IMPROVE LIVES
Alastair Demick, Managing Director of Safespaces, tells Healthcare World about the profound impact tailored environments can have on people of determination and their families
In the healthcare sector, there is a growing recognition of the impact of the environment on health and wellbeing. This understanding is particularly crucial in the provision of care for people of determination.
For individuals with conditions such as autism, epilepsy, sensory processing disorders, or learning disabilities, the environment can be a significant source of stress and anxiety. Overstimulation, unpredictability, and potential hazards can trigger behaviours of concern, delay development, and compromise overall well-being. Recognising these challenges, Safespaces, a company with more than 24 years’ experience, champions the creation of tailored, safe environments designed to promote independence, dignity, and an enhanced quality of life.
The Safespaces philosophy
The Safespaces philosophy is rooted in a deep understanding of the connection between environment and behaviour. By carefully considering an individual’s sensory, physical, and cognitive needs, we create spaces that provide a sense of security, encourage relaxation, and promote engagement.
We don’t o er a one-size-fits-all solution. Every individual is unique, and their environment should reflect that. We work closely with families, caregivers, and healthcare professionals to gain a comprehensive understanding of each person’s specific needs and preferences. This collaborative approach allows us to design and create spaces that are truly tailored to the individual.
This bespoke approach involves a comprehensive assessment process, taking into account factors such mobility, sensory sensitivities, cognitive abilities and behaviours.
As a proudly British company, Safespaces designs and manufactures all its products in the UK, ensuring the highest standards of quality and cra smanship. Our tailor-made safe rooms and high-sided beds are used in various settings, including family homes, schools, hospitals, and healthcare settings.
Benefits of tailored safe environments
The benefits of providing tailored, safe environments for people of determination are far-reaching. These spaces can:
• Improve sleep quality: A calming and comfortable sleep environment promotes better sleep patterns, leading to improved mood, concentration, and overall health.
• Promote relaxation and calmness: Features such as calming colours, so lighting, and comfortable materials help create a soothing atmosphere.
• Reduce anxiety and stress: By minimising sensory overload and creating a sense of predictability, safe environments can significantly lower stress levels.
Real-World Impact
• “The Safespace has helped George’s bedtime routine. Before, settling George took anywhere from one to three hours, and sometimes failed altogether! While I was with George upstairs, my older daughter Lucy (13) was le alone for long periods. However, bedtime is now a completely di erent experience. With the Safespace, we can put on the sensory equipment, sit quietly next to George, hold his hand, and he generally falls asleep within 30–45 minutes in a relaxing, calm, and safe environment. In just three months, we’ve seen huge improvements in George and our whole family. He settles much better and is gaining independence at bedtime.”
• “When Thomas spends time in his Safespace, he is less anxious, calmer, and more able to focus on his tasks. The Safespace allows him to access the sensory support he needs to stay calm and engaged in his learning. As a result, he can remain in the classroom for longer.”
• “Our Safespaces bed has had a huge positive impact on our whole family. Our son is safer, less stressed, and able to calm down more quickly. Our daughter isn’t being woken up by her brother’s constant running around. Bedtime has become a much less stressful experience for all of us.”
• “The Safespace has transformed my son’s life—and ours. I don’t think we would have survived these di icult years without it. He never slept a single hour of a single night in seven years until we got the Safespace. Within four days, he slept through the night—and he has done so every night since. It truly saved us all. My son was very destructive and dangerous at night; he was also a bolter and su ered from anxiety, autism, and ADHD. The Safespace made him feel secure, and we finally knew he was safe, allowing us all to sleep again. He loves it—it’s his own little haven. I have been recommending it to anyone in the same predicament we were in. He is almost 13 now, and it has helped with his concentration, focus, and anxieties. Having it in our home is a dream come true.”

ALASTAIR DEMICK Managing Director Safespaces
“We envision a future where every person of determination has access to a safe, supportive, and empowering environment”
• Enhance safety: By eliminating potential hazards and incorporating safety features, these environments help minimise the risk of injuries.
• Improve family well-being: By reducing stress and enhancing the individual’s quality of life, safe environments positively impact the entire family.
• Facilitate learning and development: A supportive environment enables individuals to engage in learning activities and develop new skills more e ectively.
Creating a safer world for all
As awareness of the environment’s impact on well-being continues to grow, the demand for tailored Safespaces is increasing worldwide. Safespaces remains committed to leading this field, continually innovating and developing new solutions to meet the evolving needs of its clients.
We envision a future where every person of determination has access to a safe, supportive, and empowering environment. By working collaboratively with families, caregivers, and healthcare professionals, we can make this vision a reality.
By prioritising individual needs and embracing a holistic approach to environmental design, Safespaces is creating spaces that truly enhance the lives of people of determination—promoting independence, dignity, and a brighter future.



STEVE
OPINIONATED
BY 2040
I’ve spent a lot of time on interviews in the last couple of weeks. We’ve had a really successful Healthcare World Series previewing the ‘Live’ Stage for Abu Dhabi Global Health Week (we’ll see you there!) and I’ve recorded a number of my podcasts for ‘HealthBeats’ (available on Apple Podcasts, Spotify and all reputable podcast providers – if you haven’t subscribed yet, why not? I’m o ended!)
Over the course of these various discussions, I’ve speculated with a number of di erent healthcare leaders questioning how healthcare might change over the next 10-15 years. The answers were startling.
We’ve covered everything from the rise of value-based care and outcome-based payment models (they’re coming) to true equality in the funding and delivery of healthcare for men and women (it’s not).
We discussed the far-reaching e ects of global political situations, the consumerisation of healthcare and the demands we expect to see from a data and tech literate and health conscious Gen Z. We have also examined whether we will solve the issues of interoperability and cross border data
GARDNER Managing Director

sharing, and we asked the question of whether we can use that data to its fullest potential.
We’ve wondered where the workforce of the future is coming from and how we can ensure it is socialised around the use of data and technology. We’ve considered what new diseases and treatments are around the corner and whether we’re ready for the next pandemic.
We’ve even considered what the best health system might look like for the future and how primary care will evolve once we have real access to remote systems and technology.
The point of all of this is that it got us thinking here at Healthcare World Towers.
We are at a crucial point in global healthcare and the levels of ambition, innovation and enthusiasm in the Middle East region seem to be stronger than anywhere else in the world.
There is political turmoil in the US and there are far-reaching e ects on global public health a er their decision to defund the World Health Organization. With the sudden implosion of the NHS a er the abolition of NHS England, it seems that now, more than ever, there is an opportunity for
the Middle East region to take a leading role in the development of global healthcare.
In Saudi Arabia, Healthcare World is working with the Saudi Commission for Health Specialities to help fuel their desire to be global leaders in the workforce agenda. We’re in discussions with the Health Holding Company about inward investment ideas and bringing global providers, suppliers and investors to the Kingdom. We’ve also been working with NEOM over the last couple of years helping to shape their thinking on healthcare innovation which is second to none globally.
In the UAE we’ve worked with the Dubai Health Authority over a number of years. Throughout Abu Dhabi Global Health Week we’ve worked extensively with Department of Health as well as both M42 and Pure Health who regularly speak on our stands and at our forums.
With this in mind, we would like to think we’re well placed to help curate the debate and ask the questions that have been coming up repeatedly on my interviews in recent weeks. To bring together providers, providers, payors, governments and regulators with international healthcare leaders and those from around the world keen to participate and understand the hotbeds of healthcare this region o ers.
We want the major providers right through to the individual clinics, the governments through to the small independent suppliers, the clinicians through to the patients to get around the table with us to discuss the future of healthcare across the region.
In the next twelve months we are going to be putting together our series of Healthcare World, Middle East Healthcare Forums. We’ll be hosting round table events in Dubai, in Abu Dhabi and in Riyadh.
We’ll be running in person events as well as hosting podcasts and running online discussions on the Healthcare World Series. The result of these discussions will be a series of intelligence reports, investment guides, market overviews and white papers. And we would like the whole global healthcare community to take part.
At Healthcare World we believe the Middle East represents a golden opportunity to get health care right - to deliver data driven, digitally enabled care that centres on patient and prevention. Drop us an email if you’d like to participate. I’ll see you there!
steve@healthcareworld.com

Ergochair has your back.
Ergochair’s software helps healthcare professionals prescribe chairs customed to your unique needs in seconds. Using powerful diagnostics, support for pre-existing conditions, and thousands of components for ultimate personalisation.
ergochair.co.uk






























