

Disclaimer
The opinions expressed in published articles are those of the author(s) and do not necessarily reflect the opinions of the Spinal Research Institute (SRI). The SRI cannot guarantee and assumes no liability or responsibility for the accuracy, currency, completeness or interpretation of the information published.
This publication is not a substitute for independent professional advice. Nothing contained in this publication is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease or condition, nor should it be used as a substitute for your own health professional’s advice. The SRI does not accept any liability for any injury, loss or damage incurred by use of or reliance on the information provided in this publication.
More information about this is available on our website.


Acknowledgement of country
The Spinal Research Institute acknowledges the Traditional Owners of the land on which we work, the Wurundjeri People of the Kulin Nation.
We pay our respects to Elders past, present, and emerging.

Introduction
Disclaimer
Acknowledgement of country
About the Spinal Research Institute
Spinal cord injury facts
A message from our CEO
2024 SCI Research Writing Prize
Judging panel
Winning Entries
Judges’ Choice
Clicking the Home icon anywhere in this document will bring you back to this page.

Integration of technology and specialty nurse counselors to improve urological outcomes in spinal cord injury patients in India
Dr Dinesh Suman, India
Judges’ Choice
The journey of a low-cost open-source manual standing wheelchair
Shovan Parvez, Bangladesh
Redefining motor recovery by exploring non-invasive spinal stimulation
Janie Provencher, Australia
The rhythm of awareness: harnessing heart rate variability to forsee autonomic dysreflexia in spinal cord injury patients
Aarti Belwal, India
Spiritual attitude and involvement in people with spinal cord injury living in the community in Bangladesh
Marjia Rahman Moury, Bangladesh
Is virtual reality the key to better sitting balance?
Garima Wadhwa, India
From shadows to spotlight, humanising the numbers to empower the unseen
Dr Bakhtawar Qureshi, Pakistan
Doctor, will I ever walk again? Navigating the unknown after spinal cord injury
Claudia Schrauwen, Belgium
Occupational time use among people with spinal cord injury living in the community in Bangladesh
Rupam Bosu, Bangladesh
The surprising and increasing choice for colostomy following spinal cord injury
Michelle Boucher, United Kingdom
From instability to independence: sitting balance after spinal cord injury
Nikhil Chowdhary, India
Combining modified exercise and electrical muscle stimulation with bone anabolic treatment may effectively improve bone health in individuals with SCI
Dr Ali Ghasem-Zadeh, Australia
Afterwords
Why Research Matters - Previous Editions
The Spinal Research Institute’s Programs
Author locations
Belgium Claudia Schrauwen
United Kingdom
Michelle Boucher
Pakistan
Bakhtawar Qureshi
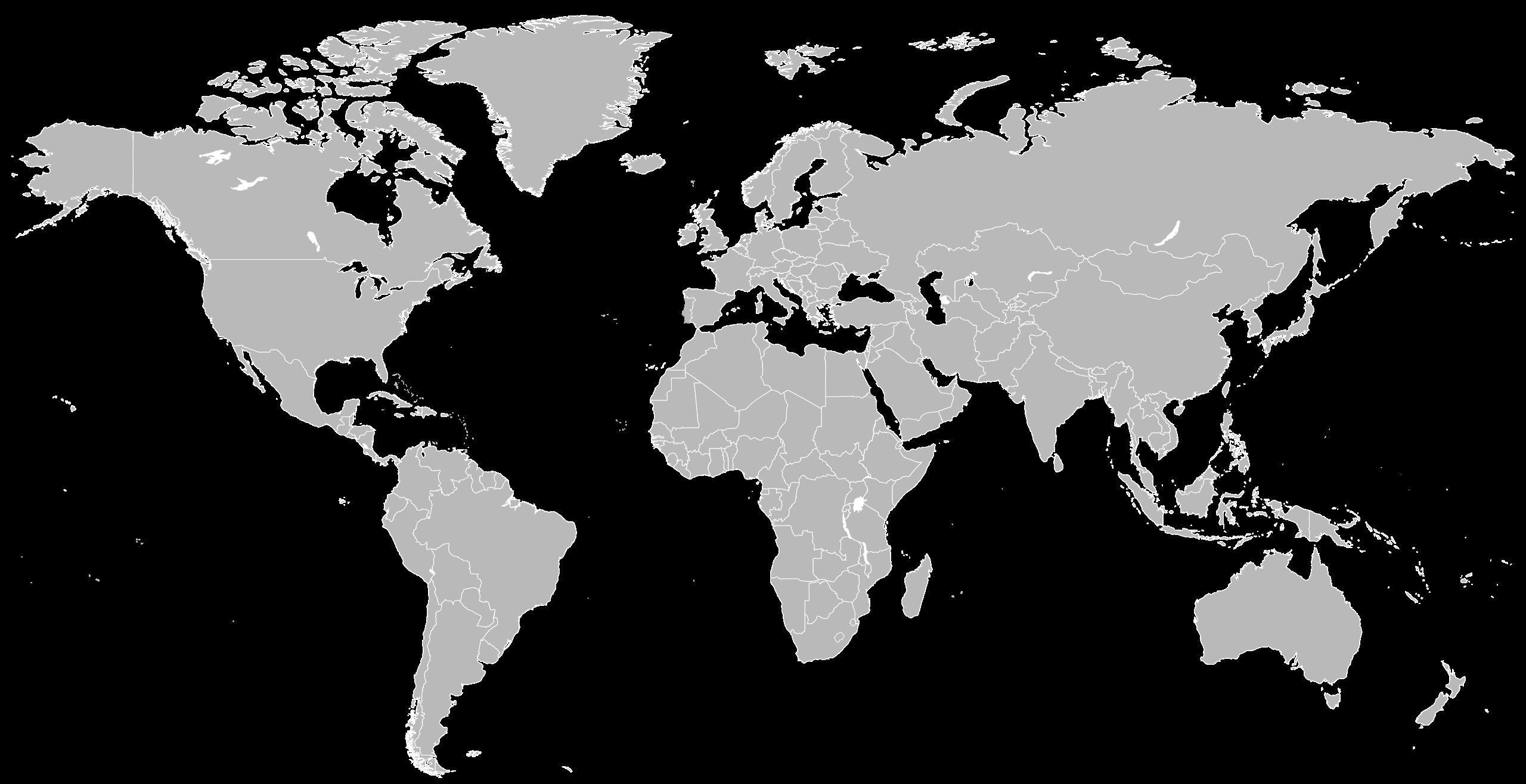
India
Dinesh Suman
Nikhil Chowdhary
Aarti Belwal
Garima Wadhwa
Bangladesh
12 authors
countries
Shovan Parvez
Marjia Rahman Moury
Rupam Bosu
Australia
Janie Provencher
Ali Ghasem-Zadeh
About the Spinal Research Institute
The vision of the Spinal Research Institute is to improve health outcomes and quality of life for people with spinal cord injury.
People with a spinal cord injury face many challenging secondary health complications that diminish their quality of life and capacity for independence. By building global collaboration in spinal cord injury research and clinical trials we aim to reduce the length of time it takes to achieve significant and translatable research outcomes.
Our work supports research collaboration and knowledge sharing, and actively involving people with lived experience of spinal cord injury in the research process to improve research relevance.
Our goal
Spinal cord injury facts
Every year, around the world, 250,000 to 500,000 people experience a spinal cord injury.
People with a spinal cord injury are two to five times more likely to die prematurely than people without a spinal cord injury. Survival rates are lower in low-and-middle-income countries.
Spinal cord injury is associated with lower rates of school enrolment and economic participation, and it carries substantial individual and societal costs.
The majority of spinal cord injuries are due to accidental or preventable causes such as road traffic crashes, falls and violence.
Spinal cord injuries can also occur due to medical reasons such as tumours, bleeding into the spinal canal and infections.
Secondary health conditions
Spinal cord injury affects much more than a person’s ability to walk; there are many secondary health conditions that can impact a person’s life.
This publication illustrates the importance of diverse research in improving quality of life for people with a spinal cord injury.
Mental health issues such as
• depression
• anxiety
Social issues such as
• marginalisation
• pressure on relationships
• barriers to education and employment
Physical conditions such as
• recurrent bronchitis and pneumonia
• sleep apnoea
• blood pressure fluctuation
• recurrent urinary tract infections
• muscle wasting
• osteoporosis
• impotence and infertility
• pressure sores
• bowel dysfunction


A message from our CEO
Welcome to the fifth edition of Why Research Matters, a compilation of the winning entries from the Spinal Research Institute (SRI) Spinal Cord Injury Research Writing Prize 2024.
This year, for the first time, we have two Judges’ Choice winners. One article is on the development of a lowcost open-source manual standing wheelchair, the other on the integration of technology and specialty nurse counsellors to improve urological health. Other pieces feature a wide range of research interest areas including virtual reality-based balance training, analysis of heart rate variability to predict autonomic dysreflexia, and management of bowel function. Thank you to all the researchers who submitted a piece to this year’s Writing Prize and congratulations to the winning entries. I would also like to acknowledge and thank my fellow judges, who volunteered their time and expertise to assess the Writing Prize submissions.

The SCI Research Writing Prize aims to engage researchers, foster clear writing skills and champion SCI research to a local and international audience. Writing a clear and concise synopsis of often complex research, is a vital skill for communication with other researchers, clinicians, grant makers, and the spinal cord injury community.
Why Research Matters provides a forum for Australian and international researchers to showcase their work outside of traditional academic publications and enables engagement with the spinal cord injury community through an easy to understand, ‘storytelling’ format. This makes research more accessible and enables all stakeholders to engage in discussion, debate and decision making about the application of research outcomes. Most importantly, it puts research into the hands of the people who will benefit from its impact, in our case, people with spinal cord injury.
Recently, we were thrilled to learn that our SCI Research Writing Prize has inspired a major Australian research institute to launch their own plain language research writing competition. This reinforces to us the importance and impact of research communication and Why Research Matters.
Happy reading!
Kristine Hendry CEO, Spinal Research Institute


2024 SCI Research Writing Prize
We asked spinal cord injury researchers and clinicians to write up to 800 words about their research in a creative way that would appeal to a broad-ranging, non-scientific audience.
The entries had to be easy-to-understand and compelling pieces about published or in-progress spinal cord injury research for a non-scientific readership.
The written pieces had to answer the following questions:
• Why is the research important?
• Why does it interest you (the author)?
• Why should it interest the reader?
The Spinal Research Institute is committed to supporting researchers and clinicians from diverse backgrounds. Since 2022, we have offered special consideration and additional language support to authors from countries with low to very-low English language proficiency based on the EF English Proficiency Index.
We asked the judges to indicate whether they thought these entries would merit publication with additional language support. This publication includes four such entries.
Prize details
All shortlisted entrants receive a place in a workshop that explores research translation and impact, facilitated by Australian course provider Research Impact Academy.
All shortlisted entrants have their writing featured in this publication. Their work will be shared and promoted through the SRI’s networks.
Assessment criteria
Entries were subject to a blind judging, where the writers’ names were not known to the judging panel.
The judging panel considered the following questions.
• Does the written piece convincingly explain why the research matters?
• Is the research explained in a way that is easy to understand?
• Is the piece compelling to read?
Judging panel
Dr Johnny Bourke
Research Fellow Implementation Science, John Walsh Centre for Rehabilitation Research, The University of Sydney, Australia
Dr Johnny Bourke is a Research Fellow at the John Walsh Centre for Rehabilitation Research. His lived experience of high-level spinal cord injury, combined with his academic experience, has allowed him to build a particularly unique understanding of the clinical and theoretical contexts in which rehabilitation and disability services are developed and delivered. Much of his work focuses on using co-design methods to promote the involvement of people with the lived experience of injury and disability in the research process.
Brooke Wadsworth
President, Australian and New Zealand Spinal Cord Society (ANZSCoS) and Allied Health Clinical Lead Inpatients, STARS MNH, Australia
A Physiotherapist for 25 years with a commitment to always putting the patient and their loved ones first, Brooke enjoys splitting her time across clinical, research, leadership and health redesign roles. An interest in assessment and treatment of respiratory dysfunction has supported her contribution to the SCI Physiotherapy Clinical Practice Guidelines and interventions to target successful extubation. She is honoured and enthusiastic about her role as President of the Australia and New Zealand Spinal Cord Society and is an ardent advocate for consumer collaboration and positive team culture.
Kristine Hendry
CEO, Spinal
Research Institute, Australia
Kristine is proud to lead the team at the Spinal Research Institute, pursuing its mission to improve health and quality of life for people with spinal cord injury. Kristine has a background in business management and information technology and worked for Hewlett-Packard, holding leadership positions in account management, program management and business development. Prior to joining the SRI, Kristine worked for MS Research Australia, gaining exposure to health and medical research, and the unique challenges and opportunities of the Australian charity sector.




Integration of technology and specialty nurse counselors to improve urological outcomes in spinal cord injury patients in India
Dr Dinesh Suman, India
Spinal cord injuries (SCI) can dramatically alter lives, creating a cascade of health challenges that extend far beyond the initial trauma. Among the most critical, yet often overlooked, complications is neurogenic lower urinary tract dysfunction (NLUTD). For SCI patients, the inability to properly control bladder function can lead to a host of secondary health problems, including recurrent urinary tract infections (UTIs), kidney damage, and a decreased quality of life. Despite the severity of these issues, post-surgical care for NLUTD is frequently inadequate, leaving many SCI patients with unmet needs and worsening conditions.
This research, carried out over the span of two years, sought to address these gaps by integrating modern technology with the expertise of specialty nurse counselors.
Why This Research Matters
For many, the idea of bladder dysfunction might seem like a minor inconvenience compared to the broader challenges faced by SCI patients. However, this issue is far from trivial. Untreated or poorly managed NLUTD can lead to lifethreatening conditions, including severe kidney damage and sepsis. Moreover, the social and psychological impacts of living with constant bladder issues—such as the need for indwelling catheters, the fear of incontinence, and the stigma that comes with these challenges—can be devastating.
What makes this research particularly compelling is the intersection of healthcare and technology. In a country like India, where medical resources are often stretched thin and access to specialized care is limited,
Judges’ Choice
finding innovative ways to deliver effective care is essential. This study is important not just for the potential health improvements it brings to SCI patients, but also for how it could reshape the delivery of healthcare in resourceconstrained environments.
The Study
During the study, we engaged nearly 8200 SCI patients with neglected NLUTD in a comprehensive intervention program. The program was designed to leverage both technology and human expertise, creating a support network that patients could access from the comfort of their homes.
Key components included:
1. Educational Content Dissemination
We used the SCIBLADDER.COM website and the SCIBladder YouTube channel to distribute educational materials. These resources provided patients and their families with crucial information on managing NLUTD, from understanding the condition to practical tips for maintaining bladder health.
2. Teleconsultations via WhatsApp
Patients were able to participate in regular teleconsultations with healthcare providers through WhatsApp, through audio-video consultations, allowing for continuous monitoring and personalized advice. They were provided scanned copies of medical prescriptions online. This approach ensured that patients could receive timely care, regardless of their geographic location.
3. Support Groups for Peer Interaction
We facilitated online support groups where patients could connect with others facing
similar challenges. These groups provided a space for sharing experiences, offering support, and building a sense of community, which is often missing for those dealing with chronic health issues.
4. Specialty Nurse Counselors
Perhaps the most critical component was the involvement of specialty nurse counselors. These professionals provided one-on-one guidance tailored to each patient’s needs. They offered not only medical advice but also emotional support, rehabilitation assistance, and education for the patients’ families. This holistic approach ensured that care extended beyond the patient to their support system at home.
The Results
The results of this study were striking. Over the two years, we observed significant improvements in urological health among the participants. The incidence of UTIs dropped noticeably, and there was a marked decrease in the reliance on indwelling catheters, which are often a source of infection and discomfort. Additionally, patients reported feeling more confident in managing their condition. This boost in confidence can be directly attributed to the continuous education and support provided through the program.
Another critical outcome was the improvement in patients’ emotional well-being and social engagement. The support from nurse counselors and the connections formed in peer groups helped patients feel less isolated and more empowered. Families, too, became more knowledgeable and involved in care, leading to better home management and an overall increase in quality of life.
Why It Should Interest You
This research is not just about improving urological health; it’s about transforming the way we think about care for SCI patients. It shows that with the right tools and support, even the most neglected aspects of a patient’s health can be addressed effectively. This study has the potential to serve as a model for broader implementation, offering hope and

Dr Dinesh Suman is the Director, NeuroUrology and SCI Andrology at the Indian Spinal Injury Centre, New Delhi. With qualifications including M.Ch. (Urology) and a fellowship in Neurourology from the National Hospital for Neurology and Neurosurgery, London, he has led the department since 1999. He is a founder member of the Spinal Cord Society of India, with over 28 publications and ongoing research in SCI healthcare. He has received multiple awards, including the ET Times Now Award as one of India’s “Promising Urologists.”
improved care to thousands of SCI patients who have been underserved for too long.
The integration of technology and human touch—through education, telemedicine, and specialized nursing care—has opened up new possibilities for healthcare delivery. If you’re interested in the future of healthcare, patient advocacy, or the power of innovation to change lives, this research is a compelling example of what’s possible when we think outside the box.



The journey of a low-cost opensource manual standing wheelchair
Shovan Parvez, Bangladesh
I have always been deeply fascinated by electronics and gear systems. This passion drove me to venture into the field of electric vehicles, where I began exploring possibilities for innovation. A few years ago, I had the fortunate opportunity to connect with Dr. Monzurul Alam, an academic researcher in the field of spinal cord injury rehabilitation. His dedication to rehabilitation engineering inspired me to focus on developing assistive devices that could significantly improve the quality of life for individuals living with paralysis. Encouraged by his unwavering support and insightful guidance, I decided to embark on a mission to find solutions to overcome the numerous challenges these individuals face.
The Challenge
The World Health Organization (WHO) report on Assistive Technology (2022) highlights a significant disparity in access to assistive technology worldwide. In highincome countries, about 90% of those who need assistive products have access to them. However, in some low-income countries, this access drops to as low as 3%. This stark contrast reveals a critical issue: while assistive technology holds the potential to transform lives, its benefits are not equitably shared across the globe.
For individuals with spinal cord injuries (SCI), this inequality is more than just a challenge—it can be life-threatening. Traditional wheelchairs, although essential, come with serious health risks, particularly in resource-limited settings. In developed countries, persons with SCI live, on average, more than 20 years after the injury. In developing countries, life expectancy varies from 1 to 6 years between the lowest and highest income groups. Many die from preventable secondary health conditions such as pressure ulcers, which could be mitigated
by regular standing. However, standing frames or wheelchairs that allow standing are very expensive, often unaffordable for the majority, especially in developing countries.
The Spark of Innovation
In response to the urgent need for accessible assistive technology, I embarked on a mission to develop a low-cost standing wheelchair. Our goal was to bridge the gap between need and access by creating an affordable solution that could be widely shared and adopted. We made our design open-source so that it could spread globally and allow people everywhere to benefit from this innovation.
The design process began with inspiration from the Centre for the Rehabilitation of the Paralysed (CRP) wheelchair, following WHO guidelines. Using computer-aided design (CAD) and simulations, I developed a prototype that was both functional and cost-effective. The core of the design features a gas spring, a mechanism commonly used in office chairs. We focused on sourcing materials locally to ensure availability in low-resource settings. The result was a prototype costing just AU$244, built with readily available materials from the local market in Dhaka, Bangladesh. This prototype allowed users to transition from sitting to standing, providing not only physical health benefits but also a new level of independence.
The development process didn’t stop there. Continuous improvements were made to enhance functionality and user experience after conducting a user trial approved by the Human Research Ethics Committee of CRP. A significant update introduced a crankshaft mechanism, further simplifying the transition from sitting to standing. This addition demonstrated our team’s ongoing commitment to refining the design and meeting the evolving needs of its users.
The Impact
The low-cost standing wheelchair has already made a significant impact. I am pleased to share that these manual standing wheelchairs are currently being manufactured in CRP’s workshop in Dhaka, Bangladesh, and users have reported notable improvements in their quality of life, including enhanced comfort and increased independence. This project demonstrates that even amidst global disparities, innovative and affordable solutions can emerge from resource-constrained environments.
Crucially, the decision to make the design open-source was key to the project’s impact. By making the design freely available, we aimed to break down barriers to access, encourage global collaboration, and ensure that this innovation could reach communities worldwide.
Future
Although the initial results are promising, our work to close the disparity gap is far from complete. Global collaboration is essential to promote and spread the design, as well as to train and support others in developing their own standing wheelchairs. In this aspect, I request support from the Spinal Research Institute. Continued research is also crucial to evaluate the wheelchair’s effectiveness in various settings and to explore additional cost reductions and accessibility improvements.


Shovan Parvez is a Rehabilitation Engineer at the Centre for the Rehabilitation of the Paralysed (CRP), specialising in assistive technology and robotics. He earned his bachelor’s degree in Electrical and Electronic Engineering from Daffodil International University and has been working with close guidance from Dr. Monzurul Alam on developing numerous opensource assistive devices, including Standing Wheelchair, Standing Frame, and Exoskeleton Walker which aims to increase the accessibility of assistive devices in low economic settings through freely sharing their design (https://openmedtech-lab.github.io).
This ongoing effort is vital to ensure that advancements in assistive technology reach all those in need. I am very honoured and excited to conduct this research and sincerely thank my mentors, family, and friends for inspiring and supporting me on this rewarding journey.


Redefining motor recovery by exploring non-invasive spinal stimulation
Janie Provencher, Australia
Physiotherapists’ Drive
Physiotherapists share a core belief: a deep, intrinsic motivation to support and empower individuals to reach and express their fullest potential. We also have a special relationship with movement, believing it to be a powerful ally in fostering autonomy and self-expression. This intrinsic drive and passion for movement are especially engaged when helping patients regain mobility after a sudden loss of motor function, such as after a spinal cord injury (SCI).
With education and engaged partnership, the right level of challenge, repeated practice, and goal-oriented activities, physiotherapy brings significant improvements in a patient’s life. During the first year of rehabilitation after a SCI, there is often ongoing progress. However, as the SCI transits to the chronic phase, we hit a therapeutic plateau. At this point, interventions no longer seem effective, and both patients and clinicians may feel powerless in the face of persistent disabilities.
Purpose of Research
The transition from initial hope to confronting reality can be challenging. Psychological support, acceptance, and adaptation are crucial for thriving with SCI. At the same time, clinicians’ drive to overcome existing limitations leads to thinking outside the box and seeking innovative solutions. That is the purpose of research.
Research can address this challenge from various angles, including drugs, cell therapy, robotics, surgeries, and neurostimulation.
Harnessing the Potential of Weak Connections
Our team at Spinal Cord Injury Research Centre (SCIRC), Neuroscience Research Australia (NeuRA), is focused on developing a
non-invasive neurostimulation approach. Using electrical stimulation, we explore how to take advantage of the nervous system’s ability to adapt over time - known as neuroplasticity. Transcutaneous Spinal Stimulation (TSS) involves delivering electrical stimulation through electrodes placed on the skin, over the spine. Combined with exercises, TSS aims to boost the excitability of the spinal cord below the level of injury. By increasing excitability, TSS might allow remaining weak connections to function. Repeated use of these newly functional connections could lead to effective changes in the nervous system which may translate into motor recovery. This neurostimulation is low risk and has high accessibility while potentially surpassing the current limitations of SCI rehabilitation.

Key Spinal Stimulation Features
Spinal stimulation involves several critical decisions: At what level of the spine should we place the stimulating electrode? What form of current will best allow TSS to reach the spinal cord? Which stimulation intensity, frequency, and duration will be most effective?
Decades of research on the nerves in the limbs have shown that different stimulation parameters can influence what is being stimulated, and this is also true for nerves in the spinal cord. Selecting TSS parameters wisely, guided by rigorous research on the underlying mechanisms, is crucial for optimizing therapy effectiveness. However, there is a lack of clear justification for the selection of TSS parameters in research studies, and discrepancies exist among different research groups’ conclusions.
“
Repeated use of these newly functional connections could lead to effective changes in the nervous system which may translate into motor recovery.
Another reason to focus on the parameters is that different forms of current require different stimulating devices. TSS can be delivered through either sophisticated devices or simpler clinical devices, such as those used for muscle and nerve stimulation, which impacts the therapy’s accessibility. While recent evidence suggests that TSS suitable for clinical stimulators can be effective, systematic comparisons are limited.
Next Therapy Landscape
Given the importance of stimulation parameters, our team has systematically tested 10 different TSS parameters to establish reliable foundations.

Motivated to support others to reach their potential, Janie trained as a physiotherapist (M.PT, B.PT) at Université Laval, Québec, Canada. To advance neurorehabilitation, she transitioned to clinical research, completing a master’s focused on novel paired electrical and magnetic stimulations for neuroplasticity. She is pursuing a PhD with neurophysiological experts Pr.Simon Gandevia, Pr.Jane Butler, Pr.Janet Taylor, and Dr.Martin Héroux, in collaboration with Advisory Group members David Deitz and Terry Lewis; at Neuroscience Research Australia, affiliated with the University of New South Wales.
Our preliminary findings suggest that TSS parameters compatible with readily approved clinical stimulators effectively trigger muscle responses. Moreover, these parameters require less electrical charge to produce the same response, making the stimulation more efficient.
Identifying the optimal TSS parameters is a crucial step in bringing TSS into clinical practice. Our results will empower researchers and future clinicians to select and justify the optimal TSS parameters. This research project, along with future studies building on its findings, has the potential to transform the landscape of SCI rehabilitation. TSS could easily be integrated into current motor training protocols by physiotherapists and other clinicians already familiar with electrotherapy. It brings us closer to a low-cost, accessible, and promising treatment option for people with SCI.

The rhythm of awareness: harnessing heart rate variability to forsee autonomic dysreflexia in spinal cord injury patients
Aarti Belwal, India
Spinal cord injury (SCI) is a dangerous condition in which damage to the spinal cord prevents communication between the brain and the rest of the body. Depending on the intensity and location of the injury, this might result in paralysis, loss of sensation, and a variety of other consequences. Autonomic dysreflexia (AD) is one of the most serious consequences for SCI patients. AD is a life-threatening condition caused by the autonomic nervous system overreacting to stimuli below the level of damage, such as a full bladder, tight clothing, or even a wrinkle on bedsheets that causes skin irritation. This response can produce an abrupt increase in blood pressure, resulting in severe headaches, perspiration, and, in extreme circumstances, stroke or death. AD is especially troubling because it can happen without warning, making it crucial for SCI patients and caregivers to be aware of its symptoms and triggers. This impedes independence and hence act as a potential threat to the quality of life of those grappling with SCI.
Early identification of AD is critical to the wellbeing of spinal cord injury patients. Patients and caregivers can take urgent action to prevent the potentially devastating impacts of AD if they detect it early on.
According to research, bladder and bowel problems are frequently the root cause of AD, accounting for more than 85% of cases. Fortunately, advances in treatment have resulted in effective preventive measures and regimens, including antihypertensive drugs, to minimize these potentially deadly increases. Yet, despite these strides, predicting AD before it manifests remains a tough nut to crack.
Recently, Heart rate variability (HRV) has shown to be a valuable tool for predicting AD in individuals with spinal cord injuries. By
analysing HRV, which measures the variation in time between heartbeats, healthcare providers can gain insights into the autonomic regulation of the cardiovascular system. In our work, we are trying to indicate that specific patterns in HRV associated with vesicle pressures can signal the early onset of AD, allowing for real-time monitoring, enabling proactive approach which can dramatically enhance the management and quality of life for individuals at risk of AD.

Individuals with SCI have periodic urodynamics evaluations (UDS) to evaluate Lower Urinary Tract function. During UDS assessments, up to 68% of people with SCI present with AD. In our study, we seek to give a full review of autonomic modulation of the cardio-vascular system during UDS, as well as identify alterations in HRV preceding AD in order to predict episodes across a cohort of SCI patients. A temporary increase in sympathetic activity during the early phase of bladder filling, followed by an increase in parasympathetic outflow to the heart when AD occurs. These findings have substantial therapeutic implications, highlighting the need of detecting early alterations in HRV in order to accurately anticipate AD episodes.
An early warning system for AD onset is provided by HRV. Under constant observation, certain patterns may point to imminent dysregulation. For example, a drop in HRV, especially in the low-frequency component, could indicate elevated sympathetic activity, which is a risk factor for AD. With the ability to get real-time updates on a patient’s autonomic status, this enables medical professionals to intervene before symptoms appear.
Continuous heart rate variability monitoring allows healthcare providers to detect early warning signs and intervene promptly, potentially preventing dangerous blood pressure spikes associated with autonomic dysreflexia. “
Recent research has shown that using the lowest point of statistical variability in heart rate i.e. Standard Deviation of Normal-toNormal Intervals, it is possible to predict AD events within 240 seconds before the first systolic blood pressure peak after AD onset. Continuous HRV monitoring allows healthcare providers to detect early warning signs and intervene promptly, potentially preventing dangerous BP spikes associated with AD.
Imagine a society in which SCI sufferers receive alerts from wearable technology even before symptoms of AD appear. These intelligent gadgets, which can track HRV in real time, serve as the patient’s personal health watchdogs. Through continuous monitoring of minute variations in heart rate, these wearables could identify early indicators of stress that could precede an episode of AD. The device instantly warns patients and caregivers to

Aarti Belwal is a dedicated physiotherapy student specialising in cardio-pulmonary care at the Indian Spinal Injury Center, New Delhi. She is a gold medalist from the Himalayan Institute of Medical Health and Sciences, Dehradun. She is currently focused on her master’s thesis, which explores the early onset prediction of autonomic dysreflexia through heart rate variability in spinal cord injury patients. Aarti is passionate about advancing healthcare solutions that enhance the quality of life for individuals with spinal cord injuries.
potential problems like a full bladder or bowel movements if it detects a reduction in HRV, which is an early warning sign of possible danger. With prompt interventions made possible by this proactive strategy, dangerous BP increases can be avoided, giving SCI patients greater control over their health. Patients with SCIs can stay ahead of AD, transforming a health crisis into manageable and preventable situations.
Therefore, leveraging HRV as a prognostic tool offers a proactive approach to managing AD, enhancing the safety and quality of life for SCI patients.
Acknowledgement: I would like to express my heartfelt gratitude to Dr. Dinesh Suman (Director of Neuro-urology & SCI Andrology) at the Indian Spinal Injury Centre, New Delhi and Ms. Rimsha Siddiqui (MPT-Cardio-Pulmonary, Assistant Professor) at the Indian Spinal Injury Centre, New Delhi for their invaluable guidance in my thesis work.

Spiritual attitude and involvement in people with spinal cord injury living in the community in Bangladesh
Marjia Rahman Moury, Bangladesh
For almost 40 years, the Centre for the Rehabilitation of Paralyzed (CRP) in Bangladesh has been rehabilitating people with spinal cord injury (SCI). During my second-year placement in the SCI unit in CRP, I always wondered how people with SCI would live their lives despite the reality of their disability. I wondered how they would be able to manage their everyday work, be able to smile at little things, be able to find new hope and meaning, and be valuable in others’ lives without feeling lost. All of these aspects made me wonder about their spiritual beliefs and involvement after returning to their community.
An SCI is an event that can completely change a person’s whole life. Imagine someone wellestablished in society, has a wonderful family, has a good career, prays five times a day, and is suddenly disabled by SCI. In some cases, these events cause them to experience psychological issues such as depression. They can also lose their belief in religion and then blame everything on God. In actuality, they can lose their spirituality, however not every person with SCI gives up on their spiritual beliefs. To survive and live, some people search for meaning and purpose and try to adopt new roles in family and society. We occasionally notice individuals with SCI who have started to possess more faith in God or religion after the incident. They believed this was the destiny God had set for them, and they attempted to accept and incorporate it into their lives.
Spirituality refers to how a person seeks meaning, purpose, faith, and connection to life, family, work, nature, or God. We all live with a sense of purpose and hope. Some people want to be recognized in the world for their work, others want to live for their families, and yet others desire to follow the rules and obligations of their religions to be loved by God
and hope for something nice from the Almighty. This is how we move on in our lives using one medium or another. If we see an example, Stephen Hawking, a well-known scientist, suffered from Amyotrophic Lateral Sclerosis (ALS) for 50 years. His disability did not stop him from becoming one of the world’s great scientists and his contributions to physics are immeasurable.
So, how was the spiritual attitude and involvement?
People with SCI who took rehabilitation services from the in-patient unit (SCI unit) of CRP successfully and returned to their community were included as the study population. A total of 101 study participants were recruited. They all lived in the community, and the time since injury ranged from one to thirty years.
The participants were interviewed using the Spiritual Attitude and Involvement List (SAIL) scale. Many spirituality-related scales were found however I chose this scale because it can be applied to both religious and non-religious individuals. Among 101 participants, 2% had a lower level, 37.6 % had a moderate level and 60.4 % had a higher level of spiritual attitude and involvement. In this study, seven aspects of spirituality - meaningfulness, trust, acceptance, caring for others, connectedness with nature, transcending experience, and spiritual activities - were also measured.
Why is this research important?
In this study, health professionals will be able to have a better understanding of the spiritual attitude and involvement of people with SCI living in the community, as well as knowing the dimensions of spirituality. The results indicate
the level of spiritual attitude and involvement of people is quite good. Spirituality helps individuals with SCI by bringing hope, elevating connectedness, improving mental and physical health, and facilitating adjustment; and can help reduce depression, anxiety and self-harm. Like other rehabilitation programs of SCI such as community reintegration and vocational training programs, a spiritual rehabilitation program should be addressed in rehabilitationbased institutions.
Why does this research matter to me?
Occupational therapy is a holistic approach that enables people to become independent in their activities of daily living. Spirituality promotes the motivation to take part in the activities and occupations of patients with chronic illnesses. After SCI, people with SCI become functionally impaired in their community. Encouraging clients to explore their spirituality can enhance their overall well-being and quality of life.

Marjia Rahman Moury is an intern occupational therapist at the Centre for the Rehabilitation of the Paralyzed (CRP). She recently graduated from the Bangladesh Health Professions Institute (BHPI). Her research interest began during her undergraduate studies. She is also interested in conducting research in other areas, such as paediatrics and neurorehabilitation, to make a difference in the field of health sciences.


Is virtual reality the key to better sitting balance?
Garima Wadhwa, India
Spinal cord injury (SCI) is a devastating form of disability encountered in today’s healthcare environment. It causes a temporary or permanent loss of motor, sensory, or autonomic systems, leading to long-term impairments in terms of physical and psychological functions.
Most individuals with spinal cord injuries are confined to wheelchairs for mobility and spend most of their time sitting in wheelchairs. Different levels of sitting balance control are required while performing activities of daily living, whether a person is performing a task in quiet sitting, such as having meals or grooming themselves, or if the person is performing a dynamic task, such as propelling a wheelchair. Therefore, limitations in the ability to control postural adjustment in independent sitting can lead to issues such as falls, early fatigue, postural mal-alignment.
There are many training methods that have found significant differences in the sitting balance of individuals with spinal cord injuries. Some examples include task-specific training, conventional balance training, and other methods. However, training in a virtual environment provides engaging and motivating experiences that our traditional therapy lacks.
In order to assess the impact of virtual reality (VR) on the sitting balance of people with spinal cord injuries (SCI), five subjects with neurological levels T4 or lower and a diagnosis of total or partial SCI were included in this study. The age range of participants was 18–35 years, and the length of the injury varied from three to seven months.
The participants were required to play a popular virtual reality-based gaming console called the Nintendo Wii. The participants played bowling, canoeing, tennis, and swordplay games from the Nintendo Wii sports series in an unsupported sitting position, meaning that
they did not have any backrest or other support to help them stay upright. This setup was intentional, as it forced the participants to rely entirely on their own muscles and balance to remain stable while playing the games.
To play the games, the participant needs to hold a Wii motion-sensitive remote in their hands, and they need to mimic the actions displayed on screen by an integrated avatar. For example, in a sword play game, the participants have to imagine their hand holding the Wii remote as a sword, and they have to slice out different objects shown on screen in different directions as marked on the screen. This required them to move their upper body in different directions while maintaining balance, which is particularly challenging for someone with an SCI. Similarly, in the canoeing game, participants needed to paddle by moving their arms in a rowing motion, which also engaged the core muscles necessary for maintaining sitting balance. Each session challenged the participants to engage their trunk muscles actively, helping them to develop better control and stability in a fun and immersive way.
The treatment sessions were held three times a week for four weeks, providing a consistent and focused period for rehabilitation. An improvement was noted on standardized measures of dynamic sitting balance training, i.e., the modified functional reach test and the t-shirt test, after four weeks of intervention training as compared to baseline measurement. The modified functional reach test evaluates dynamic sitting balance by measuring how far an individual can reach forward without losing their balance, while the t-shirt test involves time duration in putting on and taking off a t-shirt, which requires considerable coordination and balance, especially in a sitting position. The improvements in these tests indicate that the participants gained better control over their trunk muscles, which is vital
for performing everyday tasks and improving their overall quality of life.
However, while these findings are encouraging, the study also has some limitations. The most significant shortcoming is the small sample size—only five participants were involved. This makes it difficult to generalize the results to a broader population of individuals with SCI. Additionally, the study was not a randomized controlled trial (RCT), which is considered the gold standard in clinical research. Without a control group, it is challenging to definitively attribute the observed improvements solely to the VR intervention. Given these limitations, the study’s authors recommend further research in the form of a larger RCT.
In summary, this pilot study offers preliminary evidence that virtual reality could be a valuable tool in the rehabilitation of sitting balance for individuals with SCI. By turning rehabilitation into an engaging and interactive experience, VR could help patients improve their physical abilities while also enhancing their motivation and enjoyment of the process. This research opens up exciting possibilities for the future of rehabilitation, suggesting that VR might play a key role in helping individuals with spinal cord injuries regain their independence and improve their quality of life.

For the last five years Garima has worked as assistant professor at ISICIRS, New Delhi. She has completed her post-graduation from ISIC- Institute of Rehabilitation Sciences affiliated to Guru Gobind Singh Indraprastha University (GGSIPU), New Delhi India. She is currently pursuing a PhD from SGT University. She was awarded a gold medal for academic excellence by GGSIPU. Garima has presented scientific papers and posters in various conferences. She has eight years of experience and six publications.


From shadows to spotlight, humanising the numbers to empower the unseen
Dr Bakhtawar Qureshi, Pakistan
All of a sudden those dew drops on green grass become meaningless for feet that can’t feel it. Independence that never felt something other than a usual routine becomes a goal yet to be achieved. Wishes of seeing praise in people’s eyes are replaced with wishes of not experiencing gazes of sympathy. Spinal Cord Injury (SCI) has long been a condition beyond the injury of the spinal cord alone. It has the potential to scar a person’s soul, mind, thoughts, dreams and goals. As evident as the daylight, there is absolutely no doubt about SCI being a clear threat to one’s quality of life.
When it comes to a health concern, we are more focused on numbers and SCI remains a global concern due to its striking statistics. However, regarding SCI survivors, a new challenge arises, steering the focus globally towards gender equity. We need to address the health concerns beyond numbers, beyond neglect. The fact that SCI prevalence has predominantly kept males under the spotlight means that females with SCI and their struggles are, however unintendedly, being overshadowed.
SCI knows no gender and significantly affects the quality of life of every individual that it strikes. Both men and women are prone to the life-altering challenges and the psychological, physical and social toll of SCI, but as expected, it bears down differently on women. Unique challenges pertaining to images of self, menstrual and sexual health, pregnancy, relationship complexities including but not limited to burden of expectations, isolation, separation, divorce, physical and mental abuse are comparatively magnified for women. There is no surprise in expecting that the aftermath of SCI for women belonging to low income and developing countries could additionally bring many difficulties as they are subjected to societal and cultural complexities alongside poor health facilities. Women overall in the
world are seen with spectacles of vulnerability and to cater to this very trait we need to support the hidden and inborn resilience within these powerful humans.
“
SCI prevalence has predominantly kept males under the spotlight. Females with SCI and their struggles, however unintendedly, are being overshadowed.
Being a woman of a developing country working in the field of neurological rehabilitation, SCI has always caught my eye and diving more into it in the context of research has always driven me to unravel the iceberg of concerns of SCI survivors while aiming to bring in an aspect that can spark the light of solutions worth acting upon. I am currently working on a systematic review titled Exploring the Quality of Life of Women with Spinal Cord Injury (SCI); A Systematic Review of Qualitative Research on Physical, Psychological and Social Well-Being. Registered with PROSPERO (CRD42024556802), this review aspires to be one of the most impactful works of its kind by seeking to give voice to the silent struggles of women, one of the most vulnerable yet strongest groups existing in society. An attempt to bridge the gap between acknowledgement and action pertaining to gender equity that we speak much and act less about, this study is aimed at taking into account the lived experiences of women with SCI from around the world by systematically reviewing the qualitative literature post screening and drawing out impactful conclusions.
While literature does exist in form of individual studies highlighting the major physical, psychological and social concerns of SCI women separately, our study is aimed at taking into account the overall picture of all the three major Quality of Life (QOL) domains collectively as we attempt to break down the results for a clear picture of concerns of women post SCI in light of each domain. Behind every statistic is a story, and stories of women with SCI need to be told and heard.
My teammates Dr Naveed Sadiq and Dr Shabbir Ali PT and I are looking forward to narrowing our focus towards the aspects of QOL of women post SCI for a better sight towards each and every significant phase of their lives. Additionally giving an insight of comparison between QOL of women of developing and developed countries to offer proper understanding, a listening ear, and a supporting back so that this research can stand brightly upright for women with SCI when they themselves can’t. No gender should be sidelined in our fight against SCI, because SCI knows no gender.

Being a dedicated neurophysical therapist and passionate researcher, Bakhtawar’s research interest area has long been driven towards spinal cord injury. Hailing from a developing country where the healthcare sector is yet to touch the needed standards, the understanding of unique challenges of SCI survivors has long kept the wheels of her mind in motion. She has been blessed with recognition and awards at both national and international level, leading her to pursue a masters in health research where she is excited to pursue her latest project revolving around the lives of women with SCI.


Doctor, will I ever walk again? Navigating the unknown after spinal cord injury
Claudia Schrauwen, Belgium
Imagine that one day you’re living your life as usual, you are walking, eating, and doing daily tasks without a second thought. Then, in an instant, it all changes and you are not able to move anymore. This is the reality for approximately 250,000 to 500,000 people worldwide each year, according to the World Health Organization, after experiencing a traumatic spinal cord injury (SCI).
When the spinal cord is injured, signals will no longer get through properly to the brain, leading to partial or complete paralysis. For example, some people might lose the ability to walk, while others might also struggle to use their hands. This all depends on the injury’s severity and location. Losing the ability to move parts of your body can turn your world upside down. Everyday tasks like getting dressed, brushing your teeth, even typing on a phone, can become major challenges. For many, it means relying on a wheelchair to get around and needing assistance with daily activities.
After suffering a spinal cord injury, one of the first questions that comes to mind is, “Will I ever walk again?” Unfortunately, predicting the outcome of such an injury is incredibly difficult and often uncertain. The spinal cord is a complex and delicate part of the body. The way it heals, or doesn’t heal, can vary greatly from person to person. In some cases, a person who seems to have a better chance of recovery might not regain as much function as expected. On the other hand, someone who is told they might never walk again could end up proving the doctors wrong.
This unpredictability makes the road to recovery a rollercoaster of emotions and can take a heavy toll on mental health. The constant “what ifs” can lead to feelings of helplessness and despair. Some people struggle with depression, while others may experience anxiety about their future. The pressure to
stay positive and hopeful can be exhausting, especially when progress is slow or uncertain.
Understanding this profound mental and emotional impact is one of the drivers of my research as I want to alleviate both the physical and mental suffering associated with spinal cord injuries by enhancing our ability to predict outcomes from the onset and throughout the progression of the injury. By combining different medical imaging techniques, such as Magnetic Resonance Imaging (MRI) and Positron Emission Tomography (PET), with (fine) movement tests in an animal model of traumatic SCI, I aim to better predict how well someone will recover their ability to move after an injury. This approach can help us make more accurate predictions and a more personalized recovery plan. Right now, SCI is often measured with standard imaging methods (anatomical MRI and CT scans), but these can sometimes overlook early changes and provide less detailed information about the recovery that will unfold.
The pressure to stay positive and hopeful can be exhausting, especially when progress is slow or uncertain. “
Our imaging data have demonstrated the spontaneous partial recovery after an incomplete cervical lesion over time during both the acute and chronic phases following an injury. Various factors, such as the formation of abnormal tissue and inflammation visible on specific MRI scans, as well as the loss of synapses (the tiny gaps between nerve cells where chemical signals are exchanged) seen
on PET scans, have already provided greater insight into the natural recovery process after an injury. Combined with the follow-up of blood biomarkers and the measurable recovery of muscular ability, this will create a strong paradigm for predicting injury outcomes.
Restoring ability to grasp a cup, write with a pen, or use a smartphone can make a world of difference.
By improving our ability to predict the outcomes of spinal cord injuries, we can help ease the uncertainty that so often accompanies these life-altering events. For patients, this means not only a clearer understanding of what to expect but also a sense of empowerment in their recovery journey. With more accurate predictions, targeted treatments can be developed, and care can be personalized to meet everyone’s unique needs. I believe research in this area is crucial, as even small improvements can significantly enhance quality of life. Restoring the ability to grasp a cup, write with a pen, or use a smartphone can make a world of difference.

Claudia is a PhD researcher at both the University of Antwerp and the University of Namur, Belgium. She is supported by a prestigious FWO fellowship and her research by a grant from the Wings for Life Foundation, whose funding has been instrumental in advancing her work. Claudia’s research focuses on biomedical imaging, biomarkers, and therapeutic interventions following spinal cord injury (SCI). Her passion is to help the millions affected by SCI, transforming lives, and pushing the boundaries of medical science.
The road ahead presents opportunities for growth and I believe that this research offers hope, a way to navigate the unknown with greater confidence and support.

Created with Biorender

Occupational time use among people with spinal cord injury living in the community in Bangladesh
Rupam Bosu, Bangladesh
As a child, I came across a quote that really stuck with me: “Time is what we want most, but what we use worst.” Time is incredibly valuable, and that sentiment has stayed with me into adulthood. When it came time to choose a topic for my undergraduate research, I became intrigued by the idea of understanding how people with spinal cord injuries (SCI) manage their daily lives in Bangladesh.
SCI can drastically change a person’s daily routine, making everyday tasks like activities of daily living (ADLs), instrumental activities of daily living (IADLs), health management, rest and sleep, education, work, play, leisure, and social participation more challenging and timeconsuming. Despite the frustrations that can come with these changes, individuals with SCI often demonstrate remarkable resilience and adaptability. I was particularly curious about how they redefine their use of time in the face of such life-altering circumstances.
I interviewed 116 Bangladeshi SCI patients to understand their daily lives, personal values, and societal values. I discovered that people are driven to do meaningful, purposeful things that define them. All of my study participants completed rehabilitation at the Centre for the Rehabilitation of the Paralysed (CRP). CRP is the only and largest rehabilitation center in Bangladesh and South Asia. I collected participants’ socio-demographic status, causes of injury, type of paralysis, duration since rehabilitation, current employment, income source, monthly income, and assistive device. When I collected this information, I realised that there is a significant difference in daily time usage between the tetraplegic and paraplegic groups of SCI. My study’s limitation is that it cannot distinguish between the two groups. I only calculated the amount of time individuals with SCI spent in each occupational
area. I found individuals with SCI spent 9.0 hours resting, 7.5 hours working, 5.0 hours taking care of themselves, 3.0 hours on unpaid work, 3.0 hours on housework, 3.0 hours chilling, and 2.0 hours on leisure activities. Additionally, they spent 1.5 hours on studying, 1.5 hours on travelling, 1.0 hour on caring for others, 1.0 hour on playing with children, 1.0 hour on sports, and 1.0 hour on socialising. The study also delved into the reasons behind their engagement in these activities, as well as their personal and their societal values toward these activities. People with SCI spent the least time caring for others, playing with children, playing sports, and socializing because they wanted to keep themselves behind the screen.

While Bangladesh is classified as a developing country, its rural areas lack the same level of development and accessibility as their urban areas. Majority of individuals with SCI come from rural areas. Consequently, upon reintegrating into their own surroundings, they encounter many challenges encompassing physical, emotional, social, psychological, and
economic dimensions. Individuals with SCI will be able to overcome these challenges by receiving comprehensive rehabilitation services, a supportive environment, supportive family and community relationships, an inclusive society, employment opportunities, self-assurance, and effective time management.
“
I interviewed 116 Bangladeshi SCI patients to understand their daily lives, and personal and societal values. I discovered that people are driven to do meaningful, purposeful things that define them.
The role of occupational therapy is crucial in addressing these issues and facilitating meaningful participation in activities that improve independence, productivity, and overall well-being. Occupational therapy practitioners assess the client’s capacity to participate in occupational performance, which refers to the optimal performance of a chosen occupation through the interaction between the client, their environment, and the occupation. Engaging in meaningful activities designed to provide a sense of accomplishment and enjoyment may significantly enhance one’s state of psychological well-being. The presence of time management issues can profoundly disturb an individual’s daily schedule and impact their temporal activity patterns.
Temporal activity patterns refer to the time aspect of activity performance and examine the personal nature of the activity in terms of frequency, duration, and organisation, which can have practical implications for improving self-perception, personal values, and interests.
Besides this, it was inspiring to see how individuals with SCI found creative solutions to daily challenges, using assistive devices and

Rupam Bosu has a B.Sc. in occupational therapy, at Dhaka University. He is working as an Intern Occupational Therapist at the Centre for the Rehabilitation of the Paralysed (CRP). He recently graduated from the Bangladesh Health Professions Institute (BHPI). His research interest was sparked by clinical placement during his undergraduate studies. He would like to continue undertaking SCI research to make a difference in the lives of people with SCI. He is particularly interested in men, women, and older people with SCI.
modifying their environments to suit their needs. However, some faced barriers to being productive, such as the lack of accessible work environments, ignorance, and lack of motivation. This lack of productivity could lead to increased stress, depression, and low selfesteem among those affected.
My research highlighted the incredible resilience of individuals with SCI while also underscoring the need for better support, motivation, and accessible work environments to ensure they can lead fulfilling, independent lives. This work is essential in creating more inclusive communities that cater to the needs of all individuals, including those with disabilities. This research was personally meaningful to me, as it shed light on how people adapt to life with SCI and how they redefine independence and participation in their communities. It speaks to broader issues of time, independence, and inclusivity within society, prompting us to consider how truly inclusive our societies are for everyone.

The surprising and increasing choice for colostomy following spinal cord injury
Michelle Boucher, United Kingdom
Why are increasing numbers of people with Spinal Cord Injury (SCI) choosing to have a colostomy to manage their bowel function, and why are they choosing it much sooner? A colostomy is where the bowel is diverted out through a small opening in the tummy, so that stool is collected in a disposable bag stuck onto the tummy. Why would someone learning to live with and adapt to a body which has already undergone the significant change of SCI choose to further change the appearance and function of their body by choosing a colostomy?
The observation in my clinical practice that more people were choosing to have a colostomy and choosing it in the early months following their injury led to curiosity about why they were making this choice. This curiosity has drawn me to follow in the wake of those living with SCI who are leading change in how bowel function is perceived and managed, it has altered the direction of my career pathway from clinician to aspiring researcher, and it has grown in me the desire to translate their experiences and perspectives into research which informs and facilitates their choices in how their bodies are managed.
We know that SCI can have a devastating effect on bowel function, and that managing this and preventing incontinence are top areas of concern to those living with SCI. As knowledgeable professionals we have created guidelines and practices which seek to maintain the ‘normalcy’ of bowel function. Manual evacuation and digital stimulation are the mainstay of how many with SCI daily manage their bowels and are considered ‘non-invasive’ methods. The intervention of an operation to create a colostomy is in contrast considered ‘invasive’, stigmatising, with most guidelines agreeing it should only be considered as a last resort if all else fails to maintain satisfactory bowel function.
But what if patients see bowel management differently to how professionals see it? What if they would like an option which fits in with their desired lifestyle, rather than one which makes their lifestyle revolve around managing their bowel function? What if they would like choice? Robust information? What if professionals have got it wrong about what feels ‘invasive’ and what doesn’t? What if they have unwittingly been enforcing regimes on their patients which restrict their lives and limit their ability to enjoy and participate in work, leisure, travel and social activities?
These are some of the discoveries I made in doctoral research which focused on listening to and developing understanding about patient perspectives. The research explored the experiences of those living with SCI who had

chosen to have a colostomy either as a last resort years after their injury as has been traditional, and of those who are challenging accepted practice and guidelines by choosing to have a colostomy in the early months following injury. Interviews and documentary analysis were the main methods used.
“
What if patients see bowel management differently to how professionals see it? What if they would like an option which fits in with their desired lifestyle, rather than one which makes their lifestyle revolve around managing their bowel function? What if they would like choice?
Findings have demonstrated that colostomy is an option which restores dignity, is a means of regaining control over their bodies, it increases independence, and it facilitates the return to work and other desired lifestyle choices. The research has been pivotal in challenging the way professionals think about bowel management, and opening the way for those living with SCI to have more control and choice about how their bodies are managed. It was revelatory to discover differences between how professionals and those living with SCI perceive bowel function, which in turn explains why colostomy is becoming more popular.
The research has followed where those with SCI are leading and has been instrumental in translating their choices into meaningful changes in professional practice. Inpatients in this spinal treatment centre are now given high quality regularly scheduled information about bowel management choices open to them.

Michelle has worked as a Stoma Care Clinical Nurse Specialist at Salisbury District Hospital for 11 years. Her research into colostomy following spinal injury was sparked by seeing the transformational difference it can make to people’s lives, and the observation that patients are challenging the way we perceive bowel management.
Pathways have been developed to facilitate their choices and professional education has been extended. Inpatients are free to choose colostomy as an early option not only to resolve bowel management difficulties, but also if they consider it will improve their quality of life and enable them greater choice, independence and flexibility in their onward living, working and social situations.
The research into ‘spinal colostomy’ has only just begun. To provide the high-quality robust information which those living with SCI need to make informed choices about the management of their bowel function there is more to discover. Complications from colostomy need to be more fully explored and quantified, so that meaningful comparison can be made with those of more traditional manual methods of bowel management. Those living with SCI have indicated that they want to know more about how having a colostomy affects their social and sexual lives, and participation in activities such as sport. These are some of the areas in which more research is planned, with research designed and led in partnership with those affected by SCI.

From instability to independence: sitting balance after spinal cord injury
Nikhil Chowdhary, India
Globally, spinal cord injury (SCI) is one of the most debilitating nervous system injuries, leading to severe irreversible neurological deficits and functional impairments that drastically reduce quality of life. Individuals with SCI are susceptible to numerous secondary complications, including increased risk of falls during stationary sitting which can further result in serious injuries such as fractures. The challenge of maintaining sitting balance is particularly of importance as it is crucial for independence in performing activities of daily living and overall well being. Impaired sitting balance increases the risk of pressure sores, postural deformities and has profound physical, psychological implications often leading to lack of employment and vocational opportunities in individuals with SCI even after community reintegration, social isolation and decrease in overall quality of life.
Sitting balance is essential for various simple daily tasks such as feeding and grooming to complex tasks such as navigation using a wheelchair. The ability to maintain sitting balance is directly linked to trunk stability and mobility, which are often compromised in individuals with SCI. Limitations in achieving proper postural corrections in an unsupported sitting position significantly impact the degree of independence in daily life. Hence effective sitting balance control is crucial for maintaining independence and is a primary rehabilitation goal in individuals with incomplete SCI.
Research on effective sitting balance training protocols for those with incomplete SCI is limited with no general consensus on the most optimal method of training sitting balance. Recent advancements in rehabilitation have introduced virtual reality (VR) as a promising tool for retraining sitting balance offering enhanced engagement, motivation, and repeatability of virtual tasks through an enriched environment which acts like real life
simulation. In my postgraduate thesis work I have tried to investigate the effect of VR-based sitting balance training on balance and quality of life in individuals with incomplete SCI, as quality of life is directly tied to dynamic sitting balance and ability to sit unsupported.
Our four-week VR-based sitting balance training program, utilizing Nintendo Wii Sports Resort programme, yielded significant improvements in sitting balance and quality of life. The high intensity, repetitive, and task-oriented approach likely leveraged neuroplasticity to drive these gains. Notably, these findings align with previous research

demonstrating similar improvements in sitting balance among individuals with other neurological disabilities, such as stroke and cerebral palsy. The consistency of these results across populations suggests that VR-based sitting balance training may be a valuable therapeutic tool for enhancing functional abilities in individuals with various neurological conditions.
We discovered that a fourweek virtual reality-based sitting balance training program significantly improved sitting balance and quality of life. “
Virtual reality-based balance training offers a promising solution by enhancing body awareness and spatial orientation, which can provide individuals with greater awareness of their body’s displacements. This can help recalibrate proprioceptive information and compensate for sensorimotor deficits. The VR games encourage exploration, challenging individuals’ limits of stability. Participants who engaged in VR games demonstrated significant improvements in forward reach (assessed by the Modified Functional Reach Test) and multidirectional reach (assessed by the Prokin 252 Trunk sensor). These gains were accompanied by enhancements in Quality of Life (QoL) scores across all domains of the ISCoS QoL Basic Data Set version 1.0. These findings suggest that VRbased interventions can substantially improve QoL for individuals with SCI. Each VR-based intervention session lasted 30 minutes, with a frequency of five days a week. Hence we discovered that a four-week virtual reality (VR)-based sitting balance training program significantly improved sitting balance and quality of life.

Nikhil Chowdhary is a physiotherapy student pursuing his Masters of physiotherapy at the Institute of Rehabilitation Sciences, an Indian Spinal Injury Center in New Delhi. He holds a Bachelor’s degree from Centre for Physiotherapy and Rehabilitation Sciences, Jamia Millia Islamia, New Delhi. Nikhil’s current research focuses on virtual reality and its effect on sitting balance in incomplete spinal cord injury, demonstrating his dedication to innovation and patient care.
It’s a challenge for healthcare professionals to help individuals with incomplete SCI regain their sitting balance. However, integration of virtual reality (VR) technology into rehabilitation represents a transformative approach offering a promising and affordable solution. VR technology provides instant feedback in a safe space, boosting focus and motivation. By using this study’s findings, physical therapists can make significant strides in improving sitting balance in people with incomplete SCI. This innovative approach could transform the rehabilitation process, making it more engaging and effective for those with SCI.
Acknowledgement
I would like to express my sincere gratitude to my esteemed guides, Mrs. Stuti Khanna and Ms. Garima Wadhwa from the Institute of Rehabilitation Sciences at the Indian Spinal Injuries Centre, and Dr. Shefali Walia from Gurugram University, for their invaluable guidance and mentorship.

Combining modified exercise and electrical muscle stimulation with bone anabolic treatment may effectively improve bone health in individuals with SCI
Dr Ali Ghasem-Zadeh, Australia
Individuals with spinal cord injury (SCI) face numerous health challenges, including a significant risk of bone loss due to the lack of regular mechanical loading on their bones.
Bone; alive and smart tissue
Bone undergoes continuous remodelling throughout life, removing old bone or small cracks and replacing them with new bone to maintain its integrity and strength. Alongside hormones, such as sex hormones, continuous loading plays a crucial role in this process. However, in individuals with SCI, the absence of loading on the bones of the lower extremities causes the thigh and leg bones to lose bone mass, leading to the deterioration of bone microstructure, and an increased susceptibility to low-trauma fractures.
Bone loss following SCI occurs below the level of the injury, but the severity of bone loss and the cellular activity adapting bone to its loading are region specific. Weight bearing regions like the tibia are subjected to higher loads and strain—amount of deformation or changes— rates than less weight bearing regions, like the fibula, or non-weight bearing regions like the radius.
It has been reported that, contrary to expectations, individuals with tetraplegia do not experience bone loss in the upper extremities, such as the wrist. This finding underscores the complexity of bone biology and the site-specific nature of bone formation and resorption. For example, differences in loading-induced microstrain (microscopic stress) within the range typically encountered by a bone do not significantly alter modelling or remodelling. However, when loading
exceeds a strain threshold that threatens fracture, modelling increases bone formation and bone volume, thereby restoring normal strains. Conversely, when loading is reduced, as occurs in SCI, strains fall below a critical threshold, inhibiting remodelling and initiating unbalanced remodelling, which leads to bone loss and a decrease in bone volume, ultimately restoring the strains.
This raises the question: what type of exercise (or stress to the bone), at what intensity, and with what frequency is most effective for maintaining bone health across different groups, such as males versus females, acute versus chronic conditions, and young versus older individuals?
The Role of Modified Exercise in Bone Health
For many years, the interaction between muscle and bone was thought to be solely mechanical: muscles acted like pulleys, and bones functioned as levers to enable movement. However, recent research has recognised that muscles, particularly when contracted, also act as secretory organs that release substances regulating metabolism. Additionally, new findings have revealed that, osteocytes—the most prevalent cells in bone tissue—function as endocrine cells, sending signals to various organs, including the kidneys and muscles.
These discoveries underscore the critical role of exercise in promoting bone health, revealing that the relationship between muscle and bone is more complex and interconnected than previously understood. For individuals with SCI, modified exercises tailored to their specific capabilities and limitations provide a
foundation for maintaining and improving bone health.
Enhancing Bone Health with Electrical Muscle Stimulation
Simple exercise or even modified exercise alone may not be sufficient to counteract the severe bone loss often seen in individuals with SCI. This is where other interventions, such as electrical muscle stimulation (EMS), can complement exercise to maximize bone health outcomes. EMS uses electrical impulses to induce muscle contractions in paralysed or weakened muscles, mimicking the effects of voluntary physical activity. EMS has been shown to promote muscle hypertrophy, increase blood flow, and provide mechanical loading to bones. By inducing muscle contractions, EMS exerts forces on bones that help stimulate bone remodelling. When used alongside modified exercise, EMS can enhance the overall mechanical stimulation of bones, creating a synergistic effect that promotes bone density and strength, and prevents bone loss and fractures in individuals with SCI.
Bone Anabolic Treatments
Anabolic treatments, such as parathyroid hormone and sclerostin inhibitors, have been shown to promote bone formation and increase bone mass by stimulating osteoblast activity (the cells responsible for new bone formation) and reducing osteoclast activity (the cells responsible for bone resorption). These treatments can be particularly beneficial for individuals with SCI, who often experience rapid bone loss and an increased risk of fractures. By enhancing bone formation at the cellular level, anabolic treatments help counterbalance bone resorption.
Synergistic Effects of Combining Exercise, EMS, and Anabolic Treatments
The combination of modified exercise, EMS, and bone anabolic treatments represents a comprehensive strategy to improve bone health in individuals with SCI. Modified exercise and EMS provide mechanical stimuli that promote bone remodelling and maintain bone density, while bone anabolic treatments target the

Dr Ali Ghasem-Zadeh is a Senior Research Fellow in the Departments of Endocrinology and Medicine at the University of Melbourne’s Austin Health and collaborates with the Department of SCI. He has published a paper on the bone microstructure of patients with spinal cord injury using High-Resolution Quantitative Computed Tomography, in the journal Bone. He is the author or coauthor of 66 published papers, with over 4,480 citations (h-index 34), including publications in The Lancet and Nature review.
biological pathways involved in bone formation, enhancing the body’s ability to build new bone tissue. This combined and personalised strategy can help reduce the risk of fractures, improve quality of life, and promote greater independence for individuals with SCI.

Above
High resolution images of distal tibia of:
Top: Young male with spinal cord injury
Bottom: Age-sex matched control

Why Research Matters - Previous Editions
The Spinal Research Institute has published the work of 54 authors from 19 countries in five editions of Why Research Matters!

The 2020 edition of Why Research Matters contains 12 written pieces.
Contributing researchers are from 8 countries.

The 2021 edition of Why Research Matters contains 8 written pieces.
Contributing researchers are from 5 countries.
View Edition 1, 2020
View Edition 2, 2021
The 54 authors are from Australia, Norway, Ireland, USA, The Netherlands, China, UK, South Africa, New Zealand, Canada, Denmark, Pakistan, Sweden, India, Malaysia, Germany, Belgium, Bangladesh, and Chile.

The 2022 edition of Why Research Matters contains 13 written pieces.
Contributing researchers are from 11 countries.

The 2023 edition of Why Research Matters contains 11 written pieces.
Contributing researchers are from 6 countries.
View Edition 3, 2022
View Edition 4, 2023

The Spinal Research Institute’s Programs
Spinal Cord Research Hub (SCoRH)
The Spinal Cord Research Hub (SCoRH) is the world’s first online platform for spinal cord injury research collaboration. This Australian innovation was developed by the Spinal Research Institute, with support from leading local and international experts in spinal cord injury research, and launched in 2018. SCoRH enables researchers and clinicians to connect, share and collaborate in one easy-to-use online space, and to work across health disciplines and geographic boundaries to impact greater numbers of health outcomes for spinal cord injury. SCoRH members have access to two free services (outlined below) developed to remove barriers to collaboration and consumer engagement in the research process.
Research Group Facilitation
This service supports established groups to overcome obstacles that prevent or hinder their progress. Researchers globally are time-poor, and administrative tasks such as organising meetings with group members in a range of international locations can be prohibitively timeconsuming. Additionally, as group members are concurrently working on other projects and managing conflicting priorities, it can be difficult to maintain momentum, leading to a lack of clarity about group actions and goals. Research Group Facilitation provides structure and focus that can assist with these issues.
Consumer Engagement Consultation Service
This service supports researchers who would like to know more about how to include consumers in the design and implementation of their research. Including the perspectives of consumers is best practice in SCI research and is increasingly required in order to secure funding through grants. However, it is not always clear how researchers might approach this in their own projects. The Consumer Engagement Consultation service provides guidance about the ways in which consumers might be involved in different stages of the research process.
Mentor Program
The Spinal Research Institute’s Mentor Program was established in 2021 after being successfully piloted in 2019. The program has four aims:
• Progress the research careers of talented emerging researchers.
• Provide guidance and support to strengthen their specific research projects.
• Produce the next generation of leaders to advance spinal cord injury research more broadly.
• Enhance international collaborations in spinal cord injury research.
Mentoring in research equips individuals with skills that might not be available within their own organisation or institution. The mentor/mentee relationship is not bound by geographical limits, and supports growth beyond the mentee’s physical location to help develop their networks .
SCI Research Collaboration Grants
In 2016, the SRI commenced offering SCI Research Collaboration Grants to facilitate early to mid-career researcher attendance at the International Spinal Cord Society Annual Scientific Meeting, with a particular focus on researchers from middle and low income countries. The objective of this grant is to support researchers to build their collaboration networks and develop future leaders for the next generation of researchers. Over the past seven years, the Spinal Research Institute has offered 106 grants to researchers from 26 countries including 13
low and middle income countries. Five grantees had lived experience of SCI, and nearly 60% have been awarded to female researchers.
The grant enables recipients to exchange knowledge, and to build relationships with other researchers, institutions and countries involved in spinal cord research. Recipients of the grants represent diverse areas of research such as Psychology, Physiotherapy, Occupational Therapy, Nursing, Medical and Science backgrounds. Research focus areas have included health integration, electrical stimulation, trunk control, food nutrition and epidemiology.
Consumer Engagement Program
In Australia, 20,800 people live with a spinal cord injury. They are key stakeholders in the research process and it is vital that their voice is heard to ensure that research meets their needs and priorities.
For the past four years the Spinal Research Institute has been actively progressing our innovative Consumer Engagement Program. This flagship program is working to transform the spinal cord injury research field by, for the first time in Australia, supporting people with lived experience of spinal cord injury (‘consumers’) to become involved in co-design and co-delivery of research projects. It does this by improving knowledge and understanding of the research process and upskilling members of the spinal cord injury community so that they can participate as partners in research.
The program also engages researchers, championing the inclusion of lived experience in research, and we aim to create a set of world first protocols to formalise and guide the consumer engagement process.
Increased collaboration between researchers and consumers will result in more relevant research, to improve outcomes for people with spinal cord injury in areas such as: respiratory and cardiovascular health, bladder and bowel function, sexual function, pain management, upper limb function (for people with quadriplegia), treatment of pressure sores, and management of sleep apnea - all secondary health complications of spinal cord injury that can impact on quality of life.







