Care Homes in Crisis: Financial Challenges and Future Viability
In the latest episode in a new series of podcasts for the care sector, Howden discuss how the commercial viability of care homes in the UK is becoming a growing concern as the sector continues to face increasing financial and workforce challenges. Listen to the insights of Nadra Ahmed CBE, Executive Co-Chairman of the National Care Association and David Taylor, Executive Director, Howden Health & Care as they discuss the impacts that workforce and funding issues has on care homes being commercially viable and the proactive steps providers can take to ensure they have adequate insurance
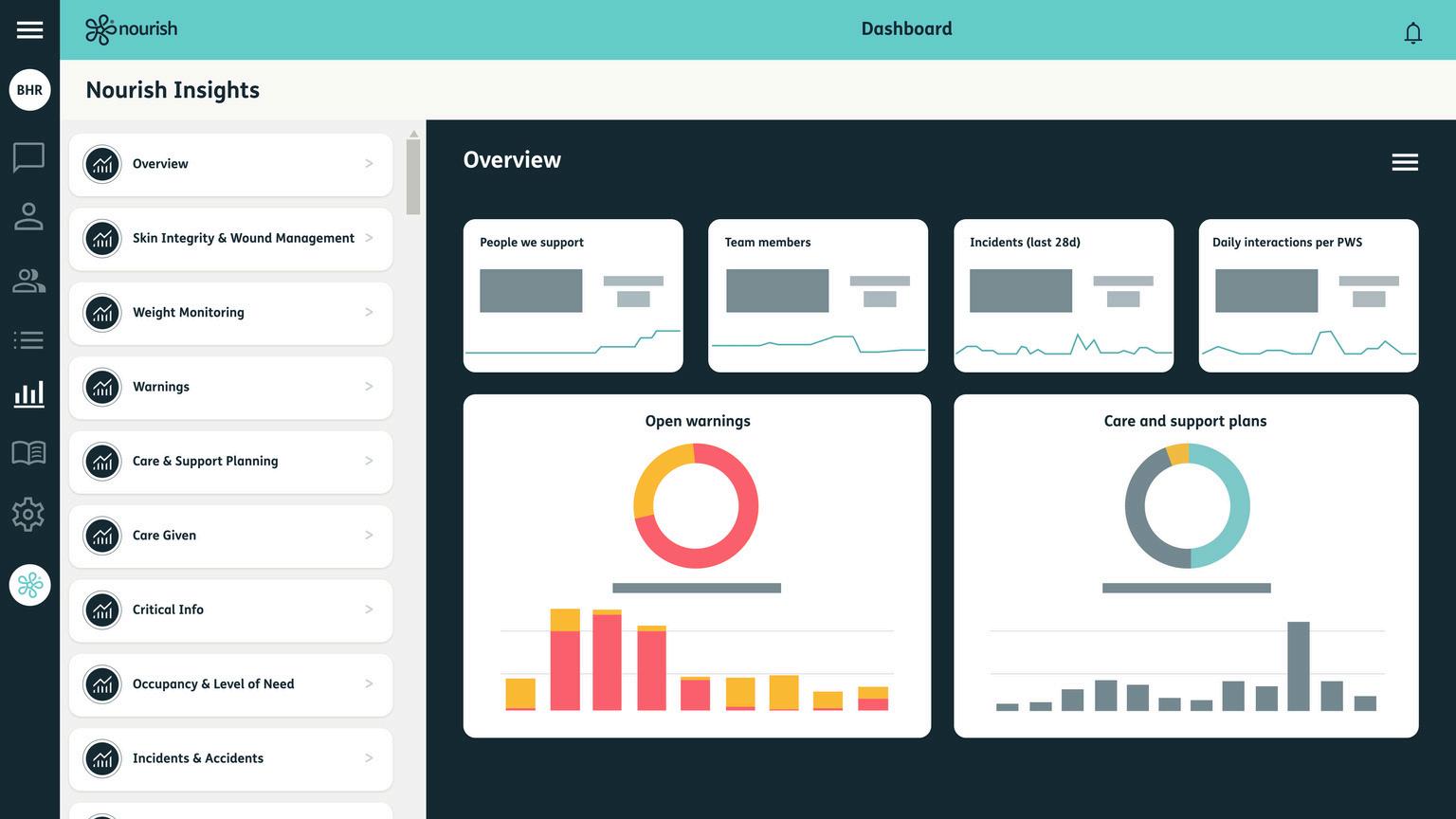
The reveal is in the details:
Using Nourish Insights to understand and act on care data
Care data is two words with three syllables and hundreds of missed opportunities. Over the past five years, the care sector has undergone a significant digital transformation. This shift generated an immense amount of data for care providers, offering unprecedented opportunities to enhance care delivery Every data point gathered in care represents a unique interaction, a personal impact and a human being. Vital threads in the tapestry of our communities. However, as a result, many small and medium-sized providers find themselves with a wealth of data but without the resources to effectively act upon it.
Enter 'Nourish Insights', our revelatory data utilisation product that enables carers to effortlessly review and act upon their data Built with a Power BI integration, Insights offers care providers a range of predefined dashboards detailing key areas of their care delivery. Equipping your team with the tools to drill down into specific data for more detailed information on your service. Our dashboards are developed through coproduction with Nourish users, ensuring they focus on the data that unlocks the past, informs the present and shapes the future of your care.
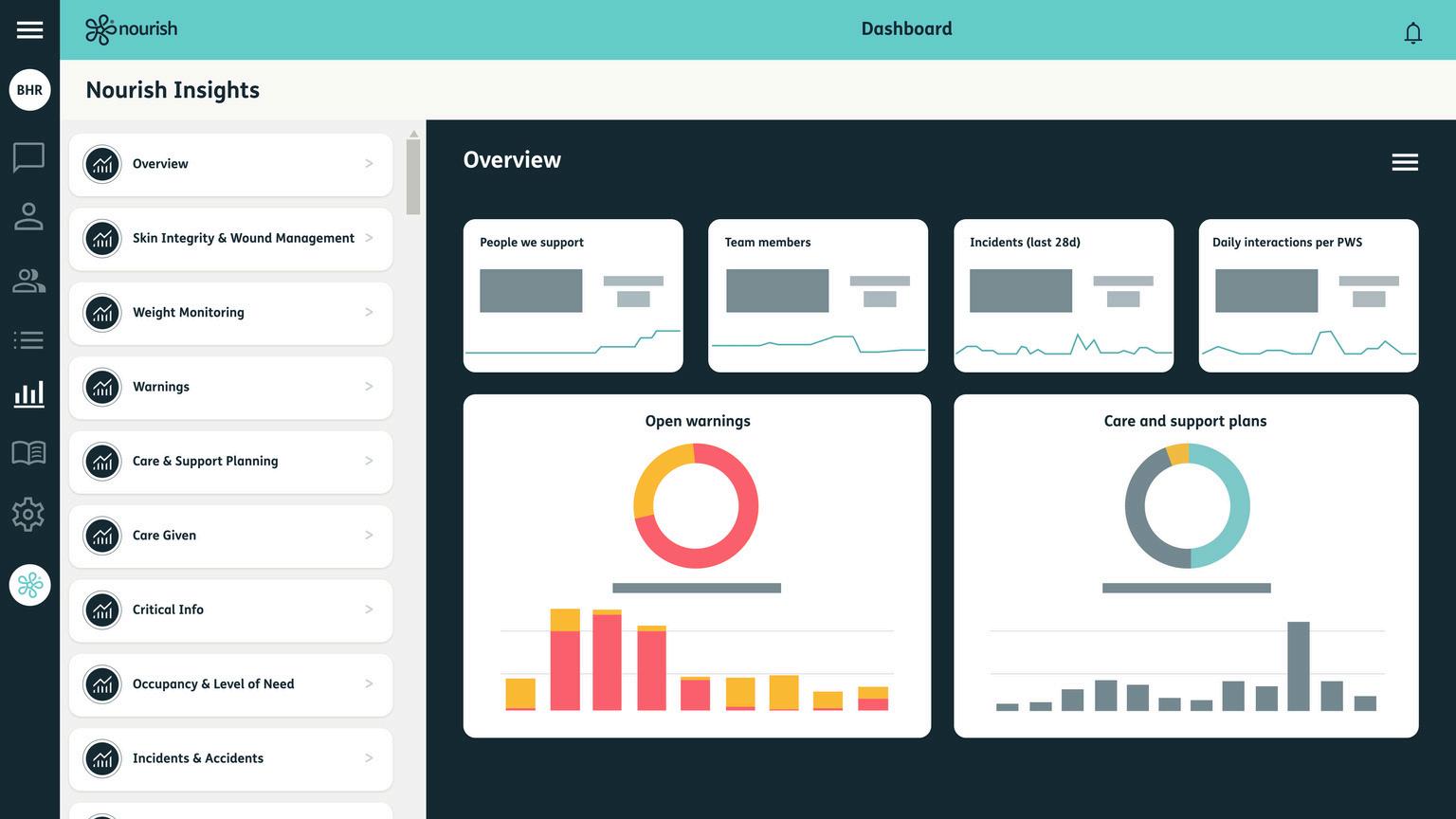
Insights helps care and support providers make sense of their past by presenting all the data gathered by their teams in an easily digestible format. Managers can review data from a top-down perspective with the respective dashboard overview. This comprehensive view details all the relevant, available data you have gathered across your service Which, utilising Power BI, is presented in an easy to understand and exportable format. Additionally, each dashboard offers a selection of more detailed views or ‘pages’ of your data so you can drill down on the points that matter to you A journey that begins on a timeline of your previous month can end as specifically as the word count on a single care plan. Allowing care homes to reflect on their practices and make informed decisions based on historical data.
“The fact our homes can keep an eye on everyone we support at the touch of a button, rather than having to scroll through everyone’s assessments. Compared to the amount of time that manual data collection and analysis takes for the homes. We can do it so much better with the dashboards, it’s game changing.”
Rachel Houghton, Development Manager, Lancashire County Council
Care is all about understanding, a power that comes from knowledge Insights updates regularly, ensuring that providers have all the information they need, accurate and at their fingertips. This enables managers to review data from anywhere. Providing you with the flexibility and context to manage your communities confidently When used in conjunction with Nourish Better Care’s interactions, our powerful data capture functionality, you can rest assured you have everything you need from your digital platform to provide outstanding care and support Because it is all right in front of you when you need it
“You can see what homes are using Nourish and what ones aren’t yet by the quality of the data we have.”
Richard Maddison, Quality Manager, Care Concern Group
Insights not only helps care providers understand their past and present but also prepares them for the future. By revealing trends over time, Insights uncovers details of care that might otherwise be overlooked or forgotten in the bottom of a filing cabinet The functionality unlocks powerful preventative applications of the data you possess. This foresight allows providers to monitor trends and take proactive actions to drive better outcomes and continuously improve your quality of care Moving your care from treatment to prevention, in line with the government’s ambitions for the NHS. The ability to anticipate future needs and challenges is invaluable in promoting independence in your care community. As well as supporting the people utilising your service to achieve their personal aims
“Nourish Insights is brilliant for capitalising on the information our teams collect throughout their day. It gives us the potential to manage our time better, being able to deploy more staff members at appropriate times and being able to get more stuff done in the home. Which means that we can give that time we’ve saved to the residents.”
Ozayr Patel, Intermediate Care, Senior Operations Manager, Lancashire County Council
Crucially, Insights includes the ability to share the information you are reviewing. This makes it an excellent tool for evidencing compliance with regulatory requirements. Care and support providers can export and print the dashboard views they want to share with ease This capability ensures that care homes can confidently showcase their commitment to quality care, and the actions they have taken to provide it.
Nourish Insights harnesses the power of data for care and support providers, presenting it in an easily understandable and actionable format. This empowers you to take control of your time and resources, enabling you to deliver the best care and support possible. By understanding the past, staying aware of the present, and preparing for the future, you can continuously improve your services. Driving improved outcomes for everyone in your community, and ensuring you never miss an insight, or an opportunity, again.
If you would like to learn more, please contact Nourish directly.
email: hello@nourishcare.com
or click the Nourish logo above to go to their website and find out more.
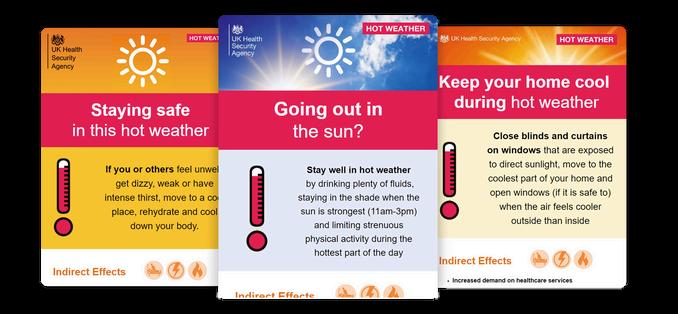
To support stakeholders with their hot weather communications this year, the UK Health Security Agency (UKHSA) has updated their communications toolkit for 2025.
This toolkit communicates health information during hot spells to ensure timely delivery of the right messages to the right people People who are more at risk of becoming unwell in hot weather include:
Older people aged 65 years and over.
People who live alone and may be unable to care for themselves.
People with underlying health conditions particularly heart problems, breathing problems, dementia, diabetes, kidney disease, Parkinson’s disease, or mobility problems.
People on certain medications
People with serious mental health problems.
People who are already ill and dehydrated (for example from diarrhea and vomiting), and more.
Click the image above to find out more on UKHSA’s website
visits
The VIVALDI team recently enjoyed a heartwarming visit to Cavendish Park, a beautiful care home that is part of the Majesticare group. The home spans over three thoughtfully designed levels, each offering a welcoming and homely atmosphere
One of the standout features is the series of stunning terraces on every floor, perfect spots to relax and enjoy the sunset
Mel and her team extended a warm and generous welcome to the VIVALDI team, who were also joined by colleagues:
Kate Meacock (Rights for Residents)
Katie Thorn (Digital Care Hub)
Victoria Hall (UKHSA/UCL)
Ruth Endacott (NIHR).
During the visit, the team had the opportunity to present the VIVALDI project to residents and staff. The presentation was well-received and sparked thoughtful conversations among attendees.
The visit wasn’t just about sharing research, it was also a chance to connect.
Over a delicious buffet, the VIVALDI team chatted with residents and their families, hearing personal stories and reflections that brought valuable insight and warmth to the day.
The team left with full hearts and full bellies, grateful for the hospitality and inspired by the community spirit at Cavendish Park. It was truly a fantastic experience, and the VIVALDI team is already looking forward to returning in the future
“Cavendish Park by Majesticare are proud to be working in partnership with the VIVALDI project. We have keen resident and relative engagement and people are empowered to have a voice on how their information is used. This means that care homes can improve infection control, reduce outbreaks and infections and capture learning, all whilst putting our people at the heart of what we do.”
Mel Hoskins- Registered Manager
Click the Cavendish Park logo to learn more about them.
‘
Sticks and Stones May Break My Bones, but Names Will Never Hurt Me’
Lara Bywater, Director of the OS and LDC Care
This rhyme was repeated almost daily in my childhood, suggesting we should shrug off invisible harm like name-calling, while physical injuries deserved real concern. Yet I still remember the sting of cruel words when I was targeted by the 'tough kids' Words matter language matters
In the care sector, language used to describe individuals holds significant power. Labels like ‘residents’, ‘the disabled’, ‘service users’, or even ‘nonverbal’ maybe convenient shorthand for professionals, but they often dehumanise, reducing people to conditions or needs. People receiving support report these labels as patronising and impersonal.
Why are we afraid to just refer to people as people?
Labels are often used to simplify communication, but over time they shape how professionals see and treat those they support. Calling someone “a schizophrenic” rather than “a person with schizophrenia” reduces them to a diagnosis, ignoring their full identity and story.
Even seemingly neutral terms like “service user”, while designed to be inclusive, can feel cold and institutional, reinforcing a power imbalance that frames the person as a passive recipient rather than an active participant in their own life.
Constantly using labels can cause people to internalise them, damaging self-esteem, autonomy, and identity For instance, someone called “non-verbal” may start to see themselves only through that lens, rather than as a whole person.
Labels also fuel bias amongst teams. A support worker who hears someone described as “difficult” may unconsciously lower expectations or show less empathy, leading to poorer care, even abuse, fewer meaningful interactions, a diminished quality of life for the person receiving support and a culture where such attitudes are normalised.
To counteract the dehumanising effects of labels, at LDC we embrace a person-centred approach to language. This means using terminology that recognises individuals first and foremost as people not as conditions or problems to be managed. Instead of “challenging behaviour”, we say “a person experiencing distress” or “having a bad day”. These subtle shifts help reaffirm dignity, reinforce humanity, and promote empathy in relationships.
Addressing the use of dehumanising labels requires more than a simple change in vocabulary. It demands a cultural shift one that is rooted in awareness, education, and reflection LDC ensures that language is a core part of all training and meetings We encourage anyone in the organisation to challenge use of stigmatising language, irrespective of their position.
Care should never be a process that objectifies or diminishes people At its core, caregiving is a deeply human act—one that should honour the totality of those receiving support.
By shunning harmful labels and embracing more respectful, empathetic language, the care sector can move closer to truly personcentred care
So far this year, there has been a notable shift in in the issuance of Prevention of Future deaths reports (PFDs), particularly in relation to care homes and community. When compared to the same period in 2024, there is a discernible increase in both the number and scope of these reports – highlighting the systemic pressures and the desperate need for reform in adult social care services.
Role of PFD reports
PFD reports are issued by coroners in situations where the coroner feels that action could and should be taken to prevent future deaths. The reports are intended to highlight circumstances to relevant organisations and urge them to take corrective actions. The reports are published online and are available for anyone to read. Statistical Overview: A Year-on-Year Comparison
Recent figures confirm that the number of deaths reported to the Coroner in 2024 were the lowest since 1995 – and down 10% as compared to 2023. Despite this reduction in deaths reported to the coroner and a drop in the number of inquests opened by 1%, the number of PFD’s issued surged by 25%, with 713 being issued in 2024.
Of those 713 reports, 34 were linked to care homes and 20 to community health care and emergency services, highlighting persistent vulnerabilities in these settings. So far in 2025 (up to 12 May 2025), 210 PFDs have been issued – down from 242 in the same period in 2024. However, those related to care homes and community care have doubled – from 11 this time last year to 22 in 2025, suggesting a heightened scrutiny of adult social care.
Key Themes Emerging from PFD Reports
An analysis of recent PFD reports reveals recurring themes that warrant attention:
1. Inadequate investigation – a number of PFD reports have identified that internal investigations in many cases were inadequate and were carried out by people who had not received sufficient training to carry out such functions.
2. Policy failure and poor governance – outdated or unclear policies were noted in a number of cases with lack of effective pre admission assessments or care plans being specifically mentioned. A number of reports identified that serious incidents did not trigger a policy based review and that in some cases falls were not adequately monitored or reported.
3 Inadequate training – specifically in emergency response and life training proceedings, as well as in carrying out investigations. One case highlighted the lack of awareness of anti-choking devices.
4. Poor communication and record keeping – a number of cases raised concerns with poor continuity of medical information (leading to medication errors), lack of records and lost or inconsistent records
Implications for Adult Social Care Providers
The rising number of Prevention of Future Death (PFD) reports highlights the need for adult social care providers to take proactive steps in addressing systemic failings. These reports not only underscore areas requiring urgent improvement but also reflect the broader pressures facing the sector, including workforce shortages, funding constraints, and increasing care complexity. In response, providers should consider the following key measures:
· Improving Communication Protocols: Establishing clear, consistent communication pathways between care staff, families, and healthcare professionals to ensure coordinated and person-centred care.
· Prioritising Workforce Development and Retention: Investing in ongoing training, career development, and fostering supportive working conditions to attract and retain skilled staff—an increasingly difficult task amid high vacancy rates and burnout.
· Enhancing Discharge Planning Processes: Strengthening partnerships with hospitals and community services to ensure patient discharges are safe, well-timed, and supported especially crucial given the challenges in managing complex needs post-discharge.
· Embedding Quality Assurance and Monitoring: Introducing or reinforcing internal audit systems to regularly evaluate care quality, identify risks, and ensure compliance with established standards.
While these actions are critical, they must be supported by broader policy and funding reforms to address the systemic challenges that continue to strain adult social care services across the UK.
RWK Goodman’s expert Health and Social Care Team provides support to health and social care provides including care homes, supported accommodation providers, domestic care agencies and children’s services Click here or or the image above to visit their website and find out more
Webinar recording available now
Last month, Skills for Care curated a webinar with the Department of Health and Social Care (DHSC) to provide an overview and insight into this year’s recently renewed LDSS funding.
First launch in September 2024, the LDSS is enabling adult social care providers to claim funding to develop managers and staff using many popular vocational qualifications and learning programmes. This webinar explores how the funding works in practice and the benefits this brings to services wishing to deliver high-quality care.
Featuring the experiences from providers who have successfully claimed and demonstrations on the claims process, the webinar introduces this year’s funding opportunity and covers some Frequently Asked Questions from users.
Click here to view the webinar and read more about the funding or click the button below.
Dementia Action Week 2025: PainChek backs national campaign to prioritise dementia care
During Dementia Action Week (19-25 May 2025), the team behind PainChek, the digital pain assessment tool, is joining national calls to prioritise dementia diagnosis and personalised care.
One in three people living with dementia in the UK remain undiagnosed, meaning thousands are being left without the specialist support they need. PainChek has long supported the care sector and its advocacy for increased government investment in dementia care and greater access to technology to support people living with dementia and their carers.
Drew Hunt of PainChek says: “We fully support the Alzheimer’s Society’s focus on dementia diagnosis this year. Getting a diagnosis is the crucial first step to accessing personalised and appropriate care, support and treatment.”
However, stigma remains a barrier to timely diagnosis, appropriate treatment, and quality care for dementia, significantly impacting individuals and their families. Dementia campaigner, writer, and trainer, Beth Britton explains:
“There has always been a stigma around dementia, with people often receiving a delayed diagnosis and there being a misconception that it only affects older people. After diagnosis, people aren’t given the tools and support they need. Not only this, but a person’s life with dementia starts before diagnosis, especially during the wait for a memory clinic appointment. People need support and hope at all these stages.”
Chris Norris, who was diagnosed with frontotemporal dementia 12 years ago, echoes the need for more holistic approach: “Dementia doesn’t just apply to the person with the diagnosis, it applies to their family too. That’s why we need to look after everyone caring for and supporting the individual. If my carers aren’t well and well-supported, I’m not well or well-supported.”
Professor Martin Green, Chief Executive of Care England and Independent Sector
Dementia Champion for the Department of Health and Social Care, says: “There is not currently an understanding that dementia care needs to be a priority – if dementia was something that affected children, society’s approach would be much different. We need to address the disparity in resources and the lack of ambition to give people living with dementia the choices to do the things they enjoy.”
Dementia care specialist Hannah Miller adds: “It is true that education around dementia is desperately needed – society is decades behind where it should be. Goal setting is a key part of learning disability care, but this seems to disappear when talking about care for dementia A mindset shift is needed to reinforce the fact it is possible for people living with dementia to have a positive experience at some points, of some days.”
Drew says: "With global cases of people living with dementia expected to triple to 153 million by 2050, now is the time to act - to break down barriers to diagnosis, equip the care sector with the tools and resources it deserves, and end the stigma associated with the condition.”
CRED Talk: Empowering better end of life dementia care in care homes: developing and implementing the EMBED-Care Framework
Thursday 12th June 2025 15:00 – 16:00 via Microsoft Teams Webinar
Please click here to register for the event.
This session is presented by Catherine Evans (King’s College London) and Nathan Davies (Queen Mary’s University London) They are researchers in dementia and end of life care They will present the programme EMBED-Care – Empowering Better End of Life Dementia Care, focusing on the EMBED-Care framework to integrate palliative care for people with dementia in care homes. The framework uses the Integrated Palliative care Outcome Scale-Dementia (IPOS-Dem) to support holistic assessment linked with decision support tools to manage symptoms and concerns identified, and review and evaluate outcomes of care. The framework is delivered on a digital app.
This is a great opportunity to discuss palliative and end of life care for adults with dementia – what are the priorities, how can we implement them, and how do we know if making a difference?
Chaired by: Zena Aldridge, Social Care Nurse Fellow, NIHR We will be hearing from:
Catherine Evans is a clinical academic nurse in palliative care and ageing She is a Professor of Palliative Care at the Cicely Saunders Institute King’s College London, and honorary Nurse Consultant, Sussex Community NHS Foundation Trust. Catherine leads a research programme on integration of palliative care in community settings for adults with multiple conditions, including dementia and frailty. Her interventions incorporate new models of integrated community palliative care, use of person-centred outcome measures for holistic assessment linked with clinical decision aids, and digital healthcare for remote assessment and management of care She leads the EMPOWER Dementia Network+empowering a meaningful life for all, and co-leads the programme EMBED-Care Empowering Better End of Life Dementia Care. She is passionate about building research capacity in nursing, social care and professions allied to healthcare, pursuing this in her roles as a deputy-director of the King’s Clinical Academic Training Office and lead for the NIHR INSIGHT South London Programme inspiring health and care practitioners to pursue research
Nathan Davies is Professor of Ageing and Applied Health and Care Research, at Queen Mary University of London, where he also co-leads and the Centre for Psychiatry and Mental Health (CPMH). He is an internationally renowned expert in dementia care, with interests in ageing, dementia, clinical decision making, unmet complex needs and eHealth. He leads and is Co-Director of the Alzheimer’s Society Doctoral Training Centre for Integrated Care (ICare-DTC), hosting 29 PhD students over the next eight years Nathan has an extensive record of high impact research in dementia care, developing interventions on decision making and inclusion which have been implemented internationally in health and care services. His work has included a decision aid for family carers supporting people with dementia, and a novel toolkit of rules-of-thumb for practitioners making end of life care decisions.
Please join us in creating a credible platform for social care research education and debate #CREDTALKS
“Nurses have the chance to engage directly with service users, staff, and relatives to conduct meaningful research that can drive real change in the sector. ”
Nuno Santos Lopes, Director of Research and Innovation/Social Care Nurse
There are 2 new and exciting opportunities for nurses who work in social care to improve their research skills and help create a research-friendly culture at work. You can apply for funding to work on research for 1 day a week for a year for:
Social Care Nurse Research Internships - 12 places available
Social Care Nurse Research Champions - 24 places available
Who can apply?
Registered nurses who work in social care settings.
Social care nurses practice in environments outside of the NHS, more often for independent sector organisations. Whilst the majority work in residential care settings, others may practice within settings such as charities, local authorities, faith groups and education.
Eligibility criteria
To be eligible for these programmes, you need to: be a registered nurse in England be employed by a non NHS organisation delivering social care services have approval from your employer to participate 1 day per week for 1 year (0.2 FTE)
If you are not sure whether you are eligible, please email nursingandmidwifery@nihr.ac.uk
Click to view Dementia Community events on
Join Dementia Community for their regular, free, 1-hour webinars. Topics for June 2025 are ‘Changing the conversation about hearing and dementia’ & ‘Introducing Take Note: 100 musical ideas’.
Topics for July 2025 are ‘Alleviating social isolation through intergenerational connections’ & ‘Designing inclusive environments for people living with dementia’.
Find out more & book here:
Thank you to our partners who we work closely with in developing our strategy
Thank you for reading. See you for our next issue in July where we will be sharing more info about what we are working on for Care Show Birmingham and more from our partners on topics that matter to you.
Be sure to sign up to ensure you don’t miss a publication. Click the button below to register for FREE membership, receive event notifications and best practices updates
Please feel free to share with your team to spread the opportunities.