
Cover Story


Cover Story
A New Haven activist, Yale doctor, and Yale lawyer won Americans the right to oral contraceptives as part of a liberating––and eugenic––movement. Today, patients and doctors still confront the tension between autonomy and coercion.
Dear readers,
Over the past year, The New Journal has been produced in classrooms, coffee shops, and airplane terminals; between phone calls and snack interludes; sometimes standing, often sitting, occasionally lying on the floor. Untethered to one physical place, this magazine has found a home in idiosyncratic corners and ordinary moments. We, too, have found a home in this magazine. During our final production, hugging each other goodbye in the Silliman seminar room, we realized we would carry an indelible piece of TNJ with us.
In Volume 57, Issue IV of The New Journal, writers hunt for truth. In our cover story, Mia Rose Kohn ’27 untangles the contradictory history of the birth control pill. Exploring suspected accounts of drink spiking, Odelya Bergner-Phillips ’28 uncloaks a darker underside of campus party culture.
We wrote our first letter to you last May, amid nationwide campus protests over the war on Gaza. One year later, the Trump administration has revoked the visas of hundreds of international students, some connected to those protests. The targeting of students based on their background, protest activities, or speech, lends unique urgency to our mission as a magazine. At Tufts University on March 25, plain-clothed officers arrested Rümeysa Öztürk, a Turkish PhD student, as she was walking to Iftar dinner to break her Ramadan fast. Öztürk’s legal team argues that she was detained because of an op-ed she co-wrote in The Tufts Daily supporting pro-Palestine protests on campus.
At the end of our term, we write to you from a world very different than that in which we started. Last year, TNJ covered the U.S.’s first state-mandated ethnic studies elective courses, right here in Connecticut. Two months later, the magazine documented the beginnings of a national refugee resettlement program based on New Haven’s Integrated Refugee & Immigration Services (IRIS). But today, the U.S. Department of Education has urged school districts to eliminate any initiatives promoting diversity, equity, and inclusion or risk losing funding. IRIS recently announced that it would be shuttering its doors in New Haven, reeling from the Trump administration’s budget cuts. As the world shifts, it demands more stories.
In our board’s last issue of The New Journal, join us in looking ahead.
Signed,
Outgoing Managing Board
Maggie, Chloe, Aanika, Sam
Thank you to our donors
Mark Badger Kathrin Lassila
Jean-Pierre Jordan
Aliyya Swaby
Laura Heymann
Jeffrey Pollock
Julia Preston
Armand LeGardeur
Katie Hazelwood
Benjamin Lasman
R. Anthony Reese
Andrew Court
Fred Strebeigh
Peter Phleger
Steven Weisman
David Greenberg
Suzanne Wittebort
Romy Drucker
James Carney
Makiko Harunari
Laura Pappano
Marilynn Sager
Blake Wilson
David Gerber
Daniel Yergin
Barak Goodman
Daniel Brook
Eric Boodman
Stuart Rohrer
Sally Sloan
R. A. Reese
Leslie Dach
Editors-in-Chief
Maggie Grether
Chloe Nguyen
Executive Editor Aanika Eragam
Managing Editor Samantha Liu
Creative Director Alicia Gan
Business Manager Alex Moore
Verse Editors
Ingrid Rodríguez Vila Etai Smotrich-Barr
Senior Editors
Jabez Choi Paola Santos
Viola Clune Kylie Volavongsa
Abbey Kim
Associate Editors
Chloe Budakian
Ben Card
Jack Rodriquez-Vars
Tina Li
Sophia Liu
Hannah Mark
Ashley Choi Calista Oetama
Matías Guevara Ruales Josie Reich
Mia Rose Kohn
Copy Editors
Sara Cao
Lilly Chai
Sophie Molden
Sasha Schoettler
Diego del Aguila Vivian Wang
Sophia Groff
Podcast Editors
Suraj Singareddy
Sawan Garde
Design Editors
Ellie Park
Sophie Lamb
Ashley Zheng
Sarah Feng Vivian Wang
Jessica Sánchez
Photography
Lauren Yee
Colin Kim Gavin Guerrette
Ellie Park
Web Design
Aaliyah Short Kris Aziabor
Caleb Nieh
Members & Directors: Haley Cohen Gilliland • Peter Cooper
• Andy Court • Jonathan Dach • Susan Dominus • Kathrin
Lassila • Elizabeth Sledge • Fred Strebeigh • Aliyya Swaby
Advisors: Neela Banerjee • Richard Bradley • Susan Braudy • Lincoln Caplan • Jay Carney • Joshua Civin • Richard Conniff • Ruth Conniff • Elisha Cooper • David Greenberg • Daniel Kurtz-Phelan • Laura Pappano • Jennifer Pitts • Julia Preston • Lauren Rawbin • David Slifka • John Swansburg • Anya Kamenetz • Steven Weisman • Daniel Yergin
Friends: Nicole Allan • Margaret Bauer • Mark Badger and Laura Heymann • Anson M. Beard • Susan Braudy • Julia Calagiovanni • Elisha Cooper • Peter Cooper • Andy Court • The Elizabethan Club • Leslie Dach • David Freeman and Judith Gingold • Paul Haigney and Tracey Roberts • Bob Lamm • James Liberman • Alka Mansukhani • Benjamin Mueller • Sophia Nguyen • Valerie Nierenberg • Morris Panner


The Adrian Van Sinderen Prize has attracted book collecting fanatics, old and new, since 1957.
Adele Haeg
Yale student veterans learn how to bridge the military and the university. By Dani Klein What Flew In
Across Connecticut, researchers, farmers, and environmentalists grapple with the uncertainty of bird flu. By Sarah Cook On Leaving
After a landmark lawsuit, Yale drastically reformed its leave of absence policies for students with mental health crises. Two years out, how far has it come?
By Kelly Kong
Stories of drink tampering haunt the Yale party scene––but barriers to testing and a culture of silence have made the phenomenon largely untraceable.
By Odelya Bergner-Phillips
A New Haven activist, Yale doctor, and Yale lawyer won Americans the right to oral contraceptives as part of a liberating––and eugenic––movement. Today, patients and doctors still confront the tension between autonomy and coercion.
By Mia Rose Kohn
Sussbauer
Ren Topping
Scoot!

Ireally dislike the bookshelves that are color-coded,” says William Bramwell ’27, with a grimace. He thinks it’s tacky.
Bramwell collects books, but he doesn’t consider himself a book collector. “It’s never been conscious, like ‘I’m a collector,’” he explained.
He does, however, have a collection of twenty-six books, which he’s titled “The Wealth of Ideas: The History of Economic Thought.” That title is a play on Adam Smith’s The Wealth of Nations, which he has in hardcover, the 1937 edition.
Some collectors spend vast sums hiring curators to color-code their bookshelves. To them, books are like wallpaper: decorative, and purely material. But not to Bramwell—he’s in it for the “wealth of ideas.”
Bramwell started reading about economic theory during the COVID-19 pandemic. He had never taken an economics class before, but after lockdown orders went into effect and the economy collapsed, he started to pay attention to debates over economic policy that were playing out on the news.
Bramwell, then a high school freshman, first read N. Gregory Mankiw’s Principles of Microeconomics, a standard college economics textbook, cover to cover. Next, Aristotle’s Oeconomica. Then it was Locke, then Hegel, Engels, Marx, and Kahneman. Joseph Schumpeter’s History of Economic Analysis became a “constant bedside companion” of his.
Before Bramwell knew it, he “was tumbling down the rabbit hole of economic thought.”
Now Bramwell is a veritable expert on the history of economic theory, even though his education in the field was “self-directed.” When we met to talk about his collection in the nave of Sterling Library, he gave me a lesson on the theory of marginal utility—very useful, if unprompted.
This spring, Bramwell submitted his collection to be considered for Yale’s prestigious Adrian Van Sinderen Book Collecting Prize. Every year, one senior and one sophomore win the 1000 dollar and 700 dollar prizes, respectively.
Aside from the money, there’s clout associated with the prize in the rather insular world of book collecting, but Bramwell wasn’t collecting books in hopes of winning. He found out about the competition two weeks before submissions were due, years after he had started his collection. The past winners I talked to didn’t curate their collections with the objective of winning the cash either. If money and prestige aren’t driving these collectors, then what is?
The eponymous Adrian Van Sinderen, Class of 1910, endowed the prize in 1957. In his New York Times obituary, Van Sinderen is sketched as a “man of wide interests”: he was a businessman and philanthropist, and an accomplished organist. He won two thousand five hundred horse racing ribbons across the U.S. He wrote over thirty books, twenty-five of them about Christmas. He traveled to every U.S. state and national park, and every continent but Antarctica.
Van Sinderen instructed that his prize be awarded to amateur book collectors “not on the basis of the rarity or monetary value of the books, but rather for the imagination and intelligence used by the student in forming his collection.” Recent winning collections include “Nehru, Nehruvianism, Nehrumania,” and “A Compendium of the Allusions of Lemony Snicket.” Evidently, points for whimsy.
Van Sinderen was in his heyday during the Roaring Twenties. During that period, accumulating stuff was how ordinary Americans signaled their status and education level. Consumerism and materialism were booming. It became stylish to own and display books. You didn’t have to read them—just wear them like shoes or a bag, or match them to the upholstery in your sitting room.
Van Sinderen himself was wealthy, make no mistake. He had the money to romp across six continents in his lifetime, which was not easy to do before the airplane.
Perhaps this curious clause in his endowment of the prize about rewarding “imagination and intelligence” over monetary value is a clue to why he established the prize, and why he wanted it to be his legacy here. He funded this prize, instead of paying for a Van Sinderen Tower or a Van Sinderen Hall.
Van Sinderen may have observed that something was disappearing from how America consumed books—that very “imagination and intelligence,” perhaps. And he must have wanted to preserve it, celebrate it, and teach it.
Book collecting might not seem like a practical pastime for college students, who often lack disposable income and bookshelf real estate. Professional book collectors spend inordinate amounts of time and money competing at auction for first editions and signed copies of texts, after them for their “rarity and monetary value.”
Even so, for almost seventy years, the Van Sinderen Prize has attracted bookish undergraduates interested in collecting. They do it for the sake of the intellectual pursuit and find themselves falling down rabbit holes like Bramwell did. It’s rather curious.
For judge Seth Bellamy ’25, “book collecting is not this seamless act of finding an author and buying all their books.” Enrique Vazquez ’23, who won the prize his senior year, agrees that “part of the fun is the hunt”; he’s found some of his favorite books at sales in church basements or antique stores in rural Minnesota. Professional book collectors have bibliographies, like shopping lists for auctions they attend.
Judges evaluate a collection not on the number of books on the list or their value, but on how cohesive the collec tion is. If the aim of a collection is to answer a question put forth by the col lector, then judges evaluate how well the question is answered. As Bellamy explained, collecting is “cultivat[ing] a way of knowing.”
The question that ties Bramwell’s collection together is: How does our economic system function, and why does it function that way?
Harvard, Princeton, and other uni versities have their own versions of the Van Sinderen Prize, and there’s an


annual national book collecting prize awarded by the Antiquarian Booksellers’ Association of America. Enrique Vazquez ’23 won third place in the national competition in 2023.
The question Vazquez asked in his collection “Tales of the Midwestern Northwoods” was: How do I bring a little bit of home with me to Yale?
After moving to New Haven from Minnesota, Vazquez felt like he was “in two separate worlds.” He started collecting books “out of a desire to stay connected to the Midwest.”
The first book Vazquez bought for his collection was environmentalist Sigurd Olson’s Listening Point, set in what is now known as the Boundary Waters Canoe Area Wilderness in northern Minnesota, where Vazquez also loves to adventure. “It is tradition to sit at Olson’s point and reflect on one’s
Vazquez started to hunt for more books by outdoorsmen, indigenous peoples, trailblazing women, artists, loggers, and families like his who had captured the beauty of that “listening point.” He wanted to be able to transport himself there when he was in New Haven, far from the northwoods and his family.
Van Sinderen, who traveled to six continents, all fifty states, and every national park in the United States, wrote that “the search for books leads one into strange, interesting, and always delightful worlds.” Van Sinderen found those worlds—real and imagined— while searching for books and in his books themselves. For him, it would be ridiculous to evaluate a collection on the material value of the books assembled: the value of books as worlds themselves transcends the paper, ink, and glue they’re made of.
Otherwise he’d borrow.
Graham Arader ’72, who is 72 years old, won the prize twice and is now one of the foremost rare book and map dealers in the United States. He still has every book from the collections he submitted for the prize when he was a student, not to mention thirty thousand other books in his reference library on American history and cartography.
Arader has made a living on books and maps, yet he admits “95 percent of the reason for the existence of libraries was ended twenty years ago by Google.”
For Arader, the aim of the library— and the aim of book collecting—is the preservation of “material culture,” and for the university, “exciting students by showing them the original work of art in the classroom.”

Vazquez is always thrilled to find marginalia in books he digs up at antique stores. Previous owners of books in Vasquez’s collection left notes in their books about planning future trips, packing lists, or reflections on trails they had trekked. That’s that “material culture.” It
For Vazquez, “books are lived.” Rebecca Romney, a professional book collector who delivered the annual Van Sinderen Prize Lecture this February, said in her presentation: “Book collecting is storytelling, and it’s not just the story of our books but the stories of

Adele Haeg is a first-year in Timothy Dwight College.
By Dani Klein
James, or Jimmy, Hatch ’24 laughed when a Yale professor suggested he apply to Yale as an undergraduate student. Despite his nearly twenty-six years in the U.S. Navy and multiple deployments as a SEAL, he couldn’t believe that Yale would be interested in what he had to say. Hatch had dropped out of high school with a GPA in the “high ones” to join the military. After visiting Yale to give a talk and tour the campus, he wrote and submitted his application, including its two essays, in under an hour. He had low expectations. Yet, in 2019, Hatch matriculated at Yale as a 52-year-old first-year.
Arriving on campus, he was unsure how the community would welcome him.
“I thought I was a monster because I’d been doing what I was doing, I was really good at it, I enjoyed it, and I felt like it was what I should be doing. I was paid to be a criminal,” Hatch said. “I was concerned that people here wouldn’t see the value of that, and in fact, that they would be freaked out by me, but that wasn’t the case.”
Hatch spent four years as a Navy sailor and twenty-two years in the SEAL Teams, during which he served as a parachute instructor and had combat deployments to Bosnia, Afghanistan, and Iraq. He received four Bronze Stars throughout his service, awarded for heroism in combat. In 2009, on a mission to rescue a captured soldier, Hatch was shot in the leg, resulting in injuries that required eighteen surgeries and ended his military career. Hatch was awarded a Purple Heart. Post-traumatic stress disorder,

substance abuse, and a suicide attempt marked his rehabilitation process.
Ten years after his injury, Hatch became the first non-traditional student in Yale’s Directed Studies program for first-years, and he went on to major in humanities. After receiving his bachelor’s degree in 2024, he served as a resource to incoming Directed Studies students, calling himself the “old man with arm tattoos who hands out fliers before the lectures from time to time.” This spring, Hatch became a lecturer for the Jackson School of Global Affairs, teaching a course called “The Impact of War on Its (Willing and Unwilling) Participants.”
To better understand the veteran community at Yale, I talked to fifteen U.S. military service members from five branches of the armed forces—one active duty Marine, a professor who served in the army, and thirteen student veterans in the Eli Whitney Students Program. Founded in 2008, the Eli Whitney program offers adults without bachelor’s degrees who are more than five years out of high school the opportunity to enroll in Yale undergraduate classes full or part-time. The program has doubled in size over the past five years, with twenty-six Eli Whitney students matriculating in 2024, seventeen of them veterans. Yale College is now home to approximately fifty enrolled student veterans. At a moment when elite universities have come under fire from the right for being anti-American, the student veterans who come to Yale grapple with bridging two worlds: the military, and the university.
When veterans enter the higher education market without experience or guidance, they can underestimate their academic potential, which can lead to a phenomenon known as “undermatching.”
Risa Sodi, an Associate Dean of Academic Affairs and Yale’s Director of Advising and Special Programs, said that the admissions office’s greatest challenge with student veterans is urging them to apply to competitive universities. “Sometimes people select themselves out— they just think, ‘I’ll never get into Yale, so I won’t bother applying,’ ” Sodi said.
Yale professor Michael Fotos, who is a founding faculty volunteer with the Warrior-Scholar Project and chairs their Board of Directors, said that veterans’ humility and “gravitas” make them some of the strongest students.
Nearly all of Yale’s Eli Whitney student veterans benefited from specialized programs like Service to School and the Warrior-Scholar Project, which help prepare veterans for college with workshops and counseling. Yale was the first undergraduate college to partner with Service to School.
Brandon Choo ’26, a junior and active duty Marine who most recently served as a scout sniper instructor, enrolled at Yale through the selective Marine Corps Enlisted Commissioning and Education Program. MECEP allows enlisted Marines to become officers while attending a naval ROTC-affiliated college. “I never really thought of an Ivy
League school as a legitimate option for me. It was always kind of like a lofty, faraway place, where the smart people go,” Choo said. “I’m very grateful to all the people who helped me get here.”
Starting in the 2022-2023 academic year, Yale began meeting 100 percent of Eli Whitney students’ demonstrated financial need. Yale also participates in the Yellow Ribbon Program, meaning the university works with the Department of Veterans Affairs to cover some or all college costs not covered by the post-9/11 G.I. Bill, a federal program that subsidizes certain tuition costs for veterans and their families.
Among student veterans, the question of whether they felt prepared for their Yale education is complicated. For some veterans, parts of their military experience mirrored Yale’s academic rigor. A significant portion of Eli Whitney student veterans worked in intelligence, including several students who served as linguists.
According to Robin Dudley ’27, a former Air Force airborne cryptologic language analyst in Mandarin Chinese, her training at the Defense Language Institute was so rigorous that she feels she can now conquer any academic challenge. For Dudley, the Yale undergraduate experience is “a piece of cake in comparison.”
Choo, on the other hand, said that the military and Yale are both demanding but in different ways. “I thought I knew how to manage time very well before I came to Yale, and then I came here, where you have to plan your day down to the nearest thirty minutes every single day for four academic years,” Choo said. “That’s its own type of discipline, but I don’t know if I’d be successful at it had I not had my military experience.”
Niels Newlin ’27 said that Yale’s demands for creative and critical analysis were an adjustment. He served for six years as an Army combat medic, deploying to South Korea during his service, and he grew accustomed to strictly regimented work. In the military, “you’re signing yourself up to not think and just do,” he said.
Patrick McGrath ’26, a Coast Guard veteran, incoming president of the Yale Undergraduate Veterans Society, and current economics major, primarily worked in counter-narcotics operations, participating in high-risk drug busts and seizures in international waters. In high school,
McGrath struggled academically and graduated with few options. He called the academic intensity of Yale far outside his comfort zone and “hands down the hardest thing I’ve ever done in my entire life, by an enormous margin,” but he also enjoys the freedom to budget his own time.
Hatch said he “never got stressed out about exams or grades, or let that control my life. I did study hard, but I didn’t get ridiculous. Nobody was shooting at me, you know what I mean?”
There are similarities between being in a special missions unit and being at Yale, Hatch said: both have rigorous vetting processes and high expectations for their members.
“Yale is in the business of building humans, at least in the undergraduate world. I watched it happen when I was a student: it would take a couple of classes for these kids to understand exactly what the professor needed, and then they’d just start cranking it out,” Hatch said. “Watching that drive, even in a form that seemed decidedly different than the drive I’d needed in my previous life, I could recognize that it was the same drive.”

For Hatch, going from close quarters combat to reading canonical writers like Hobbes, Locke, and Rousseau theorize about the original state of mankind was emotionally jarring. He cried in a professor’s office because of how the reading made him reflect on his military experience.
“I showed up here with some fucking baggage, so to me, I was like, how can any of these people really know what the fuck is going on if they haven’t been in that environment? In war?” Hatch said.
Hatch never wants to embarrass professors because he knows they all genuinely want the best for their students. He has spoken privately with professors after class when they have made incorrect statements about the nature of modern warfare.
“I had a professor say, ‘This kind of combat that happens in The Iliad doesn’t happen anymore—people don’t even see each other, it’s all done by drones.’ And I had to say, ‘That’s not true,’” Hatch said. “The night I got shot, I was ten feet from
the guy who shot me. I looked in his eyes. We see each other all the time, you just don’t hear about it.”
Perhaps the most important thing that service members contribute to campus is their perspective on the enormity of the suffering that occurs as a result of war. John Tesmer ’27, who served as a Russian Linguist in the Air Force, says he has never met a group of people more anti-war than some of the veterans with whom he’s spent time.
“That’s probably the realization of having seen it—you just realize how horrific it is,” Tesmer said. “My personal belief is that war should be avoided at all costs. I don’t think I would have believed that at 18 or 19, before going through experiences that gave me an appreciation for death and destruction at scale.”
Unlike most Eli Whitney students, most Yale undergraduates weren’t even born when the U.S. invaded Iraq in 2003, and most started elementary school nearly a decade after the beginning of the War on Terror.
“I do believe there’s a bubble here, of ‘everything’s gonna be okay,’” Hatch
said. “I also believe that pacifism is great until people want to take your shit and kill your family. I think that’s one of the most difficult things for me to translate here at Yale—it’s hard for me to convey the reality of the threats out there to our country.”
Yale and the military have been closely intertwined for hundreds of years, evidenced by the names etched in the Schwarzman Center Rotunda and the veteran memorial in Hewitt Quadrangle. In past decades, however, Yale’s relationship with the military has been rockier. In the early 1970s, Reserve Officer Training Corps (ROTC) programs withdrew from Yale following failed negotiations to keep the programs on campus in the wake of student protests during the Vietnam War, declining enrollment in ROTC programs, and the University’s decision to stop granting academic credit for ROTCmandated courses.
Yale and peer institutions received backlash to their ban on the ROTC program. Even after the ROTC ban was reversed in 2011, journalist Nathan Harden ’09 criticized Yale for its “steady loss of patriotic ethos over the last forty years,” citing the ROTC ban and the “rabid Vietnam-era anti-military sentiment of the radical Left” as factors that caused Yale’s un-American turn.
In the week after his election to the presidency in 2024, Donald Trump released a video statement in which he vowed to fire “radical Left” accreditors that have allowed colleges to be dominated by “Marxists, maniacs and lunatics,” calling academics at Ivy League schools “obsessed with indoctrinating America’s youth.”
The idea of a student veteran studying at Yale contradicts this image. Associate Director of Yale’s BradyJohnson Program in Grand Strategy Michael Brenes consistently teaches veteran students in the program, which examines large-scale, long-term strategy in issues of political and social change as well as statecraft. Brenes considers the caricature of the Ivy League university as radically anti-America and anti-military reductive.
Coming into Yale after serving for twenty years, former U.S. Army Ranger and Intelligence Analyst Tristan Benz ’27, a Global Affairs major, has encountered

this perceived divide between Yale and the military among his friends. “Some of them look at Yale in a certain political kind of light, and they might assume that I wouldn’t fit in, instead of looking at everything that Yale actually is,” Benz said. “They’re looking at it from a certain perspective that they gather from some media.”
David Allison, an Army veteran, Yale lecturer, and fellow with the Nuclear Security Program, said the people who believe Yale is a bastion of radicalism and criticism of American values have likely never experienced Yale campus life.
“When I think about my soldiers, the soldiers who served under me, I don’t imagine them coming to one of my courses and saying, ‘You’re so different than you were in the military,’” Allison said. “And I’m not getting complaints from undergrads saying, ‘You’re a vicious warmonger.’ There is a lot more overlap than we might anticipate.”
For the vast majority of the 20th century, the U.S. government was almost entirely made up of people who both had military experience and had been through






higher education. According to the Pew Research Center, between 1965 and 1975, at least 70 percent of Congresspeople had experience in the military–largely due to conscription during World War II and the Korean War. Comparatively, that percentage has hovered around 20 percent in the past decade.
“There’s a disconnect between who’s actually fighting the wars and who’s planning the wars,” said Tesmer. “And the people that are planning the wars by and large come from top 25 schools.”
It can be frustrating to observe the separation between the reality of combat zones and the bureaucracy that makes consequential military decisions, especially in the Pentagon, said Paul Lomax ’27, who served in Naval Special Operations and was deployed twice to Afghanistan.
“These are people that aren’t on the front lines, and they’re making the big-time, big-picture decisions in D.C They’re focused on the logistical aspects, and they’re also politicians,” Lomax said. He criticized the U.S.’s withdrawal from Afghanistan as evidence of this disjuncture. “They were just so disconnected
with what was going on on the ground halfway across the world, and a lot of incorrect decisions were made.”
According to Brenes, Yale has a responsibility to give students a human picture of conflict, even if they will never see it up close.
“You will never fully be able to understand what it’s like to be a service member if you’ve never been in that role, but that doesn’t mean that you’re prohibited from studying it or trying to understand it,” Brenes said.
Sometimes that separation is good, Lomax said, and it can allow leaders to make nuanced decisions on consequential issues. However, for other student veterans, it’s essential for traditional students to graduate from Yale with some level of personal connection to the human cost of war.
Thomas Ghio ’26, the outgoing president of the Yale Undergraduate Veterans Society, served in the Air Force as a Tactical Air Control Party, meaning he coordinated airstrikes from the ground.
“A lot of people that come to Yale or schools like Yale become leaders in all kinds of different areas of life, and by having student veterans on campus, it allows them to be exposed to that perspective and and take that with them as they continue their journey and hopefully make a better world for all of us,” Ghio said.
Yale might be the first place that Yalies get to have a real conversation with a veteran, Brenes pointed out.
The landscape of U.S. foreign policy has changed drastically since Hatch first joined the military, to when the U.S. began the War on Terror, to now. Since the end of the Iraq War and the U.S.’s withdrawal from Afghanistan, it’s no longer accurate to assume that any given veteran has deployed overseas or experienced combat. New service members may join the military for education or career opportunities, just as others join due to a sense of duty or patriotism.
Many of the veterans I spoke to mentioned that they had braced themselves for stereotypes about the military at Yale, but they were pleasantly surprised by how students and professors treated them on campus. In fact, multiple students told me their veteran status afforded them higher respect from professors.
Hatch said that the visibility of his military service—in the form of a cane, tattoos covering both arms, and occasionally his service dog—can lend more gravity to his presence on campus.
“There’s a currency to combat and violence,” Hatch said. “If I hadn’t been involved in the special operations world, if I hadn’t served the way that I did, and done the amount of combat deployments that I did, what would make me stand out?”
Hatch’s new class involves reading, discussing, and writing about various literary texts and primary sources that shine light on the experiences of those impacted by war, from civilians to military leaders to soldiers. When the class first began, it struck Hatch that his students
had never met anyone like him—someone who had seen war up close.
The class has hosted several speakers, including a professor from Ukraine and a professor who fled Afghanistan with her child after operating an all-girls school in her neighborhood. Veteran and U.S. Senator Mark Kelly and General Scott Miller are slated to visit the class soon. Facilitating this diversity of perspective is, to Hatch, an act of patriotism.
“If I’m helping you guys, even if you fucking hate the military and disagree with me, if I’m helping you guys, I’m helping our country,” Hatch said. “I truly believe that.”
Hatch has been finding the new class to be a challenging and humbling experience, and the seminar has become
a very tight-knit community. He’s cried reading some of the papers in his class, and he’s been deeply moved by the openness and audacity of some of his students to confront unspoken tensions.
When he looks around at the faces of his students, he worries that they are taking on the weight of the world. While facilitating seminars, he remains vigilant in choosing his words carefully, because, as he said, his job now is “giving these kids ammunition for the fight that they have ahead of them, when they are introduced to this thing called war.” ∎

In the fog before church the cafes are closed, the good grocers also save one in which I know no Spanish and am sorry.
How strange it is to apologize here. Andalusia. Her mute sun is lost on me. Her seasons and signals of seasons have lapsed these six or seven centuries.
I cannot trust Sevilla’s orange trees in their columns on the Feria road. I cannot trust the orange of their oranges.
Lady living here: The locals know they are not to be tasted, or are to be tasted if you fuss to peel and jelly them.
Knowing no better I thank her. I still cannot accept. Not from a jar. I will have the outsides of those oranges bitter as they are. Not the candied rest.
––Netanel Schwartz




Stories of drink tampering haunt the Yale party scene—but barriers to testing and a culture of silence have made the phenomenon largely untraceable.



By Odelya Bergner-Phillips
John ’27 was at a fraternity formal at Noa, a Thai restaurant on Crown Street, in spring 2024.
John is “not the type to get blasted,” he told me, especially when he is out with a date, as he was that night. “I wouldn’t have embarrassed myself like that.”
But he hardly remembers anything from the event.
In fact, by his recollection, the night was a short one. He remembers sharing a drink with one of his friends. He remembers being at the formal for just a few minutes. John was shocked to hear, afterwards, from his friends that he had stayed for the entire event––roughly an hour and a half of his memory gone. He remembers telling his date he had to throw up. He remembers getting into an Uber and making it back to his residential college. “It was there that my body gave out. I couldn’t really move,” John said. His friends had to physically drag him inside until a First-Year Counselor (FroCo) spotted them. Concerned, the Froco called the ambulance. John and the friend with whom he shared the drink ended the night at the Yale New Haven Hospital.
He is not sure what time he checked into the hospital, but believes he left at around 4 a.m., after waking up with a pounding headache on a stretcher in the hospital hallway. “I guess hospitals are pretty busy, and if you have a drunk, you are not going to waste an entire room on them,” he recalled. He wasn’t tested—he doesn’t know exactly why—but his friend was. His friend tested positive for Rohypnol.
Rohypnol, colloquially known as “roofies,” can be odorless and tasteless, and is one of the most commonly used drugs in drink spiking and date rapes, as it can slip undetected into a drink. Like John experienced, Rohypnol, a central nervous system depressant, causes memory loss, vomiting, headaches, and loss of mobility.
To this day, though he did not test himself, John feels certain that the fateful drink he and his friend shared was spiked.
John’s friends told him that for most of the night, before he lost his ability to speak, walk, or even stand, he seemed fine—just drunk—to those around him. Despite his seemingly normal presentation, he believes he was feeling the effects of having been drugged. “There’s a period of time when you seem fine, but you are actually already roofied, and you can’t remember anything before you collapse.”
The next day, after returning home from the hospital, John felt fine, aside from a lingering headache. But this episode had unfolded during finals
period, and he quickly had to regroup and attempt to focus on his studies. As John tried to prepare for his exams, he found himself returning to the confusion that night––a suspected drink spiking with no clear culprit or motive. Categorized as a “date-rape drug,” Rohypnol is commonly used to drug people to facilitate sexual assault. But John was not assaulted, adding to the disturbingly random and senseless feeling—what exactly had happened to him, and why?
I sought to understand the prevalence of experiences like John’s on Yale’s campus: nights out that seemed normal but ended with a blackout, sickness, and memory loss. Dozens of people I spoke to, either in interviews or informally, had a story, believing that they, a friend of theirs, or a friend of a friend had experienced drink spiking. I realized, however, that assessing the prevalence of drink spiking at Yale was not possible and, at this time, largely indeterminable. There is no data available on the number of Yale students roofied, let alone on the number of drink spikings happening in the City of New Haven. At every stage of the phenomenon, physically, medically, and legally, drink spiking enacts a disappearing act—it often goes unknown, undetected, random, and untraceable.
These barriers make drink spiking so difficult to measure and protect against. The tracking procedures that do exist are underutilized, as victims are clouded by either the drugs themselves, which often cause memory loss and impair victims’ ability to advocate for themselves, or by shame and fear that they might be penalized for drinking underage.
Few people wanted to speak publicly about their experience with suspected roofieing. Some felt ashamed about being a victim, and others worried about damage to their professional future should they be named in this piece, particularly in connection with underage drinking. Those who did speak did so only under the condition of anonymity, and are identified as John, Jane, and Jessica.
The last time the Yale Daily News reported about instances of drink spiking on Yale’s campus was in the 2018-2019 academic year. That October, the Yale Daily News covered a drink tampering incident at a suite party in Durfee Hall on Old Campus, after which two female students were hospitalized and one tested positive for Rohypnol. The incident was investigated by the Yale Police Department, but in an article months later, the Yale Daily News reported that no suspect had been identified.
College students are a higher risk group for drink-spiking, a 2017 study found. This past November at Cornell University, the Cornell Police received a report about a female student being coerced by several male students into taking ketamine and possibly other drugs before being sexually assaulted at a fraternity, leading to the fraternity’s temporarily suspension, and the Cornell
Interfraternity Council’s decision to suspended all social activities the following weekend. According to The Guardian, the incident is under investigation, but no further reporting has emerged. Given the public nature of the incident, its communal response and reactions were similarly public, including in an editorial published by The Cornell Daily Sun, spurring dialogue in the Cornell community. At the start of this academic year, the Boston Police Department issued a community alerts warning for college students in the region against the dangers of “scentless, colorless, and tasteless drugs” such as Rohypnol. In California, the state assembly recently passed a law requiring state universities and community colleges to have free and accessible drug testing devices in health centers.
In New Haven, the number of publicly reported cases is sparse––so is the public conversation around drink spiking. The New Haven Police Department hasn’t issued warnings and the state of Connecticut hasn’t passed bills. Yet the lack of news coverage does not align with the magnitude of the topic in casual, campus conversation. Roofieing, particularly in the context of fraternity parties, is normalized in postings on Fizz, an anonymous social app. In December 2024, three posts by Yale students referenced a fraternity’s reputation for roofieing each garnered over two thousand upvotes. One post, from early March, asked: “does anyone know if i can get tested for roofie drugs in my system?”
The five students I interviewed could all name at least one person who thinks they have been roofied. Ava Boston ‘26, Chief of Service of Yale Emergency Medical Services, an undergraduate organization that provides standby coverage to Yale’s campus, noted, “I’ve had friends that this has happened to at Yale, or at least they believe it happened to them… It does happen here, and it’s extremely sad.”
Without large-scale institutional data, students have come up with their own precautions and conceptions of the issue. Recent graduate Amanda Ivatorov ’24 spent her senior year studying drink spiking in the Yale community. She wrote to me that in her freshman year, multiple of her peers were roofied at a fraternity-sponsored, off-campus event. With guidance from two doctors at the Yale School of Medicine, Ivatorov designed a study of the student response to NightCaps, a commercially sold product placed on top of cups to protect against spiking.
Yale students in Ivatrov’s study completed a brief survey before they received a NightCap in February 2023, and were surveyed again in April and May 2023. The majority of respondents expressed worry about roofieing—of the 171 respondents, 60 percent agreed that “At social events on and near Yale’s campus, I am worried about drink spiking.” These results suggest a fear among many students, amplified by the perception that everyone around them has some connection to the issue.
But a true assessment of the prevalence is nearly impossible, as most cases of suspected drink spiking remain unconfirmed and are often either not investigated or unsolved.
“Perhaps Jane’s experience would have been different if someone had recognized her abnormal behavior that night. But drink spiking is essentially impossible to distinguish from normal intoxication, even with common sense and extensive training.”

In Yale’s 2024 Title IX Report on the Higher Education Sexual Misconduct and Awareness, Yale women who experienced sexual assault with penetration involving physical force or inability to consent were asked whether they had been given drugs or alcohol without their knowledge or consent. Some— 8.5 percent—said they suspected it, and another 10.3 percent said they did not know. None of the participants said they were certain.
Why do so many students, who suspect their drinks have been spiked, not get tested?
Some never make it to the hospital or receive medical care at all.
Jane ’28 believes her drink was spiked during a night out at a Yale fraternity earlier this semester. She was out with a group of friends and remembers receiving her last drink of the night—a vodka Sprite. She does not remember what happened next. “You could tell me I cartwheeled out of there and I’d believe you because I just have no clue.”
Like John, much of her knowledge of that night is pieced together from small moments she remembers and what her friends reported to her in the following days. She told me that her friends took her back to her suite, but Jane remembers little from the night. “Apparently the whole way home I couldn’t walk on my own,” she said. “I had to be handed off to someone because I was so unstable with my walking, I was zig-zagging and pulling in different directions.” While she doesn’t remember this walk back to her dorm, she remembers lying on her friend’s floor asking, “Is this real?”
Then, she became “horribly violently ill.” She told me she was throwing up until the late afternoon the next day, and still shaking two mornings later. “I couldn’t eat, I couldn’t drink, I just kept throwing up everything,” she said. “I thought I was dying.”
Jane told me she did not seek medical services or get tested because she felt too sick to get herself to the Yale Health Center. “I didn’t want to have to put on clothes and leave my suite because I was so ill.” After vomiting for hours, throughout the night, and the following day, she still did not understand the extent of her memory loss and strange behavior from the night before—she did not yet suspect that she had been roofied.
Only after talking with friends and doing online research, hours after her incessant illness finally receded, did she begin to suspect she had been roofied. Her reaction to the drink that night had been abnormal. “I know my limits and this was within my limit,” she told me. She had never once been sick or thrown up after a night out. Jane spoke to a friend who also suspected she had been roofied on a different night but—like Jane—had not been tested. Both had had the same symptoms, and both came to assume that their drinks had been spiked. After online research, over a day later, Jane concluded it would have been “too late” or too expensive to get tested, especially after looking into hair follicle testing. Such testing can pick up drugs in the system
longer than a blood or urine sample might, but costs upwards of 150 dollars. According to U.S. Drug Test Centers, one of the largest drug testing facilities in the country, Rohypnol typically passes through the system and is no longer detectable within twenty-four hours. Days later, Jane learned of another friend who had the same reaction after drinking at the same fraternity that same night out.
Perhaps Jane’s experience would have been different if someone had recognized her abnormal behavior that night. But drink spiking is essentially impossible to distinguish from normal intoxication, even with common sense and extensive training. During their training, FroCos are given scenarios about alcohol and drug-related situations. While FroCos are not trained to provide medical care, FroCo Trinity Lee ’25 explained that their training emphasizes looking out for students who seem to be “acting a bit off” or “out of character.”
An Associate Dean of Student Affairs, Tom Adams is Director of Yale’s Alcohol and Other Drugs Harm Reduction Initiative (AODHRI), which is focused on addressing alcohol and drug use on campus through education and programming. Adams wrote that AODHRI primarily works “through educational programming, including the Work Hard, Play Smart course for incoming first-years, the ‘Talking About Alcohol’ guide for Yale College families, and trainings for student leaders including FroCos, CCEs, and Camp Yale Program Leaders.”
Symptoms of a drink spiking may not always manifest in obvious ways. Yale Emergency Medical Services acts as a standby service at Yale events, including First-Year Formal and Senior Masquerade, during which students may be drinking or show up intoxicated. Boston shared that “a misconception about drink spiking is that sometimes people think it tends to be this big, dramatic thing,” whereas “sometimes it just looks like someone has drunk a lot more than they actually have.”
Adams wrote that “in any case where a person has an unexpected reaction to drinking, they should seek medical attention. If they suspect that their drink was spiked, testing is available from a medical professional.”
But testing is often not easily accessible. Hospitals have no standardized way to discern if a drunk patient has also been drugged, nor a protocol to drug-test intoxicated patients. The symptoms for alcohol intoxication and date-rape sedative drugs are the same, according to Dr. Jessica Stetz, an emergency medicine physician at Downstate Health Sciences University Hospital in Brooklyn, New York. “Honestly, you can’t tell the difference,” she said.
Stetz explained that “clinically, it doesn’t really change anything” to know whether a patient has been drugged or is simply intoxicated. There are no reversal agents, she explained, and no particular treatment. “If somebody has normal vital signs, no signs of trauma, and is comfortable, sometimes we just let them sleep it off.” She added that doctors do not test for roofieing since it does not change
their medical management, unless a patient has requested a test and is hoping to collect evidence for a legal case or has told a story that raises particular concern.
Dr. Matthew Griswold, an emergency medicine physician and toxicologist at Hartford Hospital in Connecticut, also said that it can be difficult to distinguish between an intoxicated or drugged patient. Griswold emphasized that without a specific request or a suspicious story reported by the patient or those accompanying them to the hospital, doctors are unlikely to test for roofie drugs. In confusing, late nights out, students arriving at a hospital extremely inebriated, or under the influence of drugs, may not know to request a test, or be lucid enough to do so.
There are tests, Griswold said, that are administered in some cases. A urinalysis conducted in the hospital can indicate “broad classes of drugs,” he explained, but such testing is “very broad strokes,” frequently showing false negatives. If someone is on anti-anxiety medication, for example, that may show up as a positive and not indicate to the physician what specifically the patient has consumed. More specific drug testing is not a part of standard protocol to test intoxicated patients because such tests have to be sent to a large national drug laboratory, and, according to Griswold, could cost several thousand dollars.
Stetz also mentioned a specific test kit used with victims of drug-facilitated sexual assault. The kit requires urine as early as possible from the time of suspected drug ingestion to maximize the amount of drugs detectable in one’s system and thus the test’s effectiveness. It is rarely deemed necessary or used. In the past twenty-five years, Stetz believes she has probably only done one such test.
John ’27 is not sure why he was not tested when he ended up at Yale -New Haven Hospital. While he did not explicitly request testing, he recalled being told that the hospital didn’t have any more tests. He wonders if telling doctors he had taken an edible that night might have influenced their decision not to test. “Maybe they had my best interests in mind and it would have shown up, or maybe they didn’t believe me, or something like that,” he said.
“She did not feel anything at first. ‘And then very soon, I think within like ten to fifteen minutes, both of us completely blacked out.’ ”

Another suspected victim of drink spiking, Jessica ’28, was not tested at Yale-New Haven Hospital, despite her friends’ request on her behalf.
She and her friends had attended a party at a Yale sports house in December 2024. She and a male friend shared a drink, which they got from the student bartender at the party. She did not feel anything at first. “And then very soon, I think within like ten to fifteen minutes, both of us completely blacked out.” The next thing she remembers was waking up early in the morning in a hospital bed.

“The act of drink spiking itself functions as an erasure—erasing John’s, Jane’s, and Jessica’s memories of their experience and stripping them of autonomy.”
Neither she nor her friend remembered the rest of their night, after they got that drink. The rest of the night was recounted to them by their friends. Their friends told Jessica that she seemed “very immobile,” “groggy,” and “not able to move.” She and her male friend, with whom she’d shared the drink, were both told by their friends that they had been throwing up. One of her friends called a FroCo, who subsequently called an ambulance. At the hospital, Jessica’s friend “repeatedly kept trying to tell [the doctors] that they think I had been drugged and they were really not caring about that.” Jessica told me that in the morning, the doctors told her she was “over-intoxicated,” attributing her physical symptoms to her alcohol consumption that night. She was shown the results of a blood test—the only test done—that indicated she had alcohol in her system. A blood test would show the presence of particular drugs if such a specific panel had been requested—as far as Jessica is aware, such panels were not requested, although she is not sure.
After being discharged from Yale New Haven Hospital, Jessica and her male friend returned later that day to request drug testing: “We weren’t going to do much with the information. We were just curious because it was a very weird experience and we wanted to know for our own sake.” She said that hospital staff told them that they didn’t provide such testing. The two of them went to CVS and purchased a home drug test kit for 37.99 dollars, a urine test that purports to identify fourteen drugs, including amphetamines, cocaine, ecstacy, and benzodiazepines.
Both her and her friend’s at-home tests showed a positive for buprenorphine, an opioid. According to American Addiction Centers, mixing such a drug with alcohol is extremely dangerous, causing vomiting and impaired thinking, among other symptoms.
At-home drug tests available for purchase frequently have false negatives, Griswsold explained,
and can also show misleading positives, including as a result of prescribed medications that an individual may already be taking. He also highlighted the high cost of detailed drug testing sent to laboratories, a cost that Jane mentioned being wary of when researching the possibility of getting tested a few days after her suspected drugging. “We’re trying to be really mindful about not spending our patients’ money when unnecessary,” Griswold said, adding that doctors “are not always sure when we send that testing to somebody’s insurance that they will pick it up, in which case [the patients] are on the hook for a huge amount of money.”
Both Stetz and Griswold explained that testing that might pick up Rohypnol, for example, would only be useful for the court of law, detectives, or forensic work, and not for the physicians. Stetz said that if doctors utilize the test kit for drug-facilitated sexual assault, results are not even sent to doctors. They are, instead, stored by law enforcement, according to the state’s rules of evidence.
In a statement, Tim Brown, Director of Communications for Yale Health, wrote that evaluations of intoxicated students at the Acute Care Department at Yale Health include a protocol for alcohol breathalyzer testing to assess the level of intoxication, with further evaluation based on the clinical team’s assessment. Like in the hospital, drug testing is not a part of the standard protocol. Acute Care closes at 10 p.m., meaning late-night emergencies often end up at the hospital, rather than Yale Student Health Services.
Urine drug testing, including testing for Rohypnol, is available, if a student requests it, through Quest labs within Yale Health during regular operating hours. “The half-life of these drugs means they clear the system quickly, making timely testing necessary,” Brown wrote, which means students suspecting they may have been drugged should seek testing as soon as possible. Testing provided in the Student Health or Acute Care at Yale Health, including a standard drug screen and a specific test for Rohypnol, is included in Yale Health’s Basic Student Health Services, and is free for students.
For Jane, however, by the time she was well enough to leave her dorm several days later and had suspected something would be wrong, it would have been too late for a urine test at Yale Health.
More complex forensic drug screenings are not performed at Yale Health, but instead at Yale New Haven Hospital. Brown wrote that they are performed “only in cases where an assault has occurred or is suspected/possible (i.e., the person has no memory of what happened and/or does not have anyone to account for their whereabouts).” In such cases, tests are free of charge. If a patient is not a possible victim of assault, they cannot request extensive forensic drug testing panels. If someone, like John, Jane, or Jessica, wanted to know if they had been drugged, the emergency room would only provide testing for a limited panel of substances. In such cases, patients would be charged for their tests.
For the few victims of roofieing who could confirm they were drugged and might go to the police, crimes often remain unsolved. Rohypnol, along with many other drugs used to facilitate drink spiking, are illegal in the United States under the Controlled Substances Act. Drink spiking is a felony.
But at a party, identifying a drink spiker is nearly impossible. John, who is himself a fraternity member, described the safety mechanisms in place at fraternity parties. Many frats have a member who stays sober the whole time to monitor the party. When working at the bar, John was trained to identify who was drinking shots if one person requested multiple, but he said, “There are so many people that I can’t possibly always make sure that everyone’s okay.” Presidents from four Yale fraternities did not respond to email requests for further comment on safety measures in place.
After a party, identifying a culprit may be just as hard. John was contacted by a detective from the New Haven Police Department––he is not quite sure how they got his name, but knows other students who suspected they had recently been roofied at the same restaurant, Noa, and wondered if they might have come forward to the police. Police records indicate that the detective received the complaint three days after the formal, and began speaking to students within a week. Beyond a conversation with a detective, John never heard any updates on the case: “I don’t think they did anything, to be honest.”
John’s suspicions were essentially correct: police records from the investigation indicated that the investigator “did not develop any suspicion to believe the Noa staff had tampered with the complainant’s drinks or that they had knowingly provided alcohol to the minor complainants.”
Jessica did not consider reporting her suspected drink spiking after receiving positive results on the at-home drug test, because she didn’t think the incident could be feasibly traced back to any one person. “I feel like it would be a lot more mess and drama than we needed,” she said.
In an email, the New Haven Police Department wrote to me that they do “not have any statistical/ data reports available regarding incidents of drink spiking, drink tampering, or date-rape drugs.”
Police records from the investigation into Noa cited individuals declining to speak with investigating police officers out of concern “about being identified and charged for consuming drugs/alcohol as a minor,” or possessing or using a fake ID, a criminal offense in itself. Yale has a medical emergency policy, in which if students request help for themselves or fellow students in medical need, they will not face discipline from the Yale College Executive Committee. Nonetheless, the policy states that this amnesty does not “protect [students] from criminal or civil liability or prevent investigation or other action by federal, state, or local authorities, including Yale Police.” John, Jessica, and Jane were all drinking underage.
The act of drink spiking itself functions as an erasure—erasing John’s, Jane’s, and Jessica’s memories of their experience and stripping them of autonomy. Rohypnol and other drugs used in drink spiking make victims lose awareness, the capacity to make choices in the moment, and to remember what has happened to them. Jessica described the experience as “out of body, because you had no control.”
Without memory or clarity of what actually happened on a night out gone wrong, it’s difficult to tell one’s own story or understand who might be accountable. “I think it’s just hard not to blame yourself when it happens,” Jessica said. “It’s hard not to be like, oh, I should have been more careful about who I took a drink from, or I should have not done this or that.”
Ultimately, there are few protective measures in place. Ivatorov, who surveyed the student body, wrote to me that “It’s alarming that no harm-reduction measures have been standardized or broadly implemented that directly help students protect themselves,” including the NightCaps drink cover that she studied, or other drink testing mechanisms, like tester sticks, which are now required at California State University and California community colleges.
Police records from the investigation into Noa emphasized the importance of testing to substantiate the “belief” that a drink had been drugged. Without proof, the detective ultimately wrote that they had not developed any reasonable suspicion that the “experiences of altered mental status were caused by the malicious actions of another person/s.
In talking to John, Jane, and Jessica, it’s clear that the path to accessing tests is opaque and their availability is unpublicized. Not one of these three students knew that tests were available through Yale—for free. Without more testing and subsequent tracking of cases, it is impossible for students to know for certain what happened to them in frightening nights ending in memory loss and extreme sickness. Testing is also necessary for the Yale community to understand how prevalent this issue––which is certainly present in casual discourse––is in reality.
“Before I was roofied, I didn’t think that what happened to me would happen,” John reflected. Now, he’s more cautious when he drinks. But he’ll never really know what happened to him that night, or why.∎
Odelya Bergner-Phillips is a first-year in Timothy Dwight College.
The men in my ears clacked about The Iliad as I walked. I used to pause my podcasts and take out my earbuds when I went walking down Main Street, in case I saw someone. But today it snowed hard so I could not expect that, so I let them clack on about Greece, and the Greeks, and I laughed silently inside puffed cheeks numbed to the cold.
I turned the corner and began up the hill. Around a slight bend a woman was also walking, coming down. She was far; we walked, both knowing we would pass the other, and uncertain what to do in the interim. This knowledge crushed me like a tight squeeze of the calves, like the muscles in my thighs and in my calves were clamped and all the juices were drying up. My muscles became raisins; the men kept clacking, but I took one earbud out, for politeness; I kept my eyes down and pretended like my mind did not race. What if she spoke a cursory, pithy remark about the weather, about the snow and its falling like little powdered sugars from a donut God breathed on, about the funny little happenstance that two people might walk in such conditions? I needed pith in response. I have often lamented my failures in pith. The men clacked; the raisins dried themselves; I stared down and considered the footprints I knew I was leaving but never turned to see.
We passed each other. She smiled, and I laughed as if she said something pithy, and I stuffed the men back into my right ear and let them clack until I died.
Up the hill the road turns blind for a leftbound walker, so I crossed the street, like always: when coming up from town, you round the bend and cross at the treelog mailbox. And I crossed and began walking on her footprints. I knew they were hers; they were fresh, and it was snowing. They were small,
too, certainly smaller than my too-big expensive winter boots. I stepped in her footprints, stomped over them, clomped on half of one and none of the next. My boots were larger; my strides were longer; I felt a sense of conquest. A terrible, stupid sense of conquest knocked me on the head like an unwinking brick, and I picked it up and stared at it, waiting for it to realize itself.




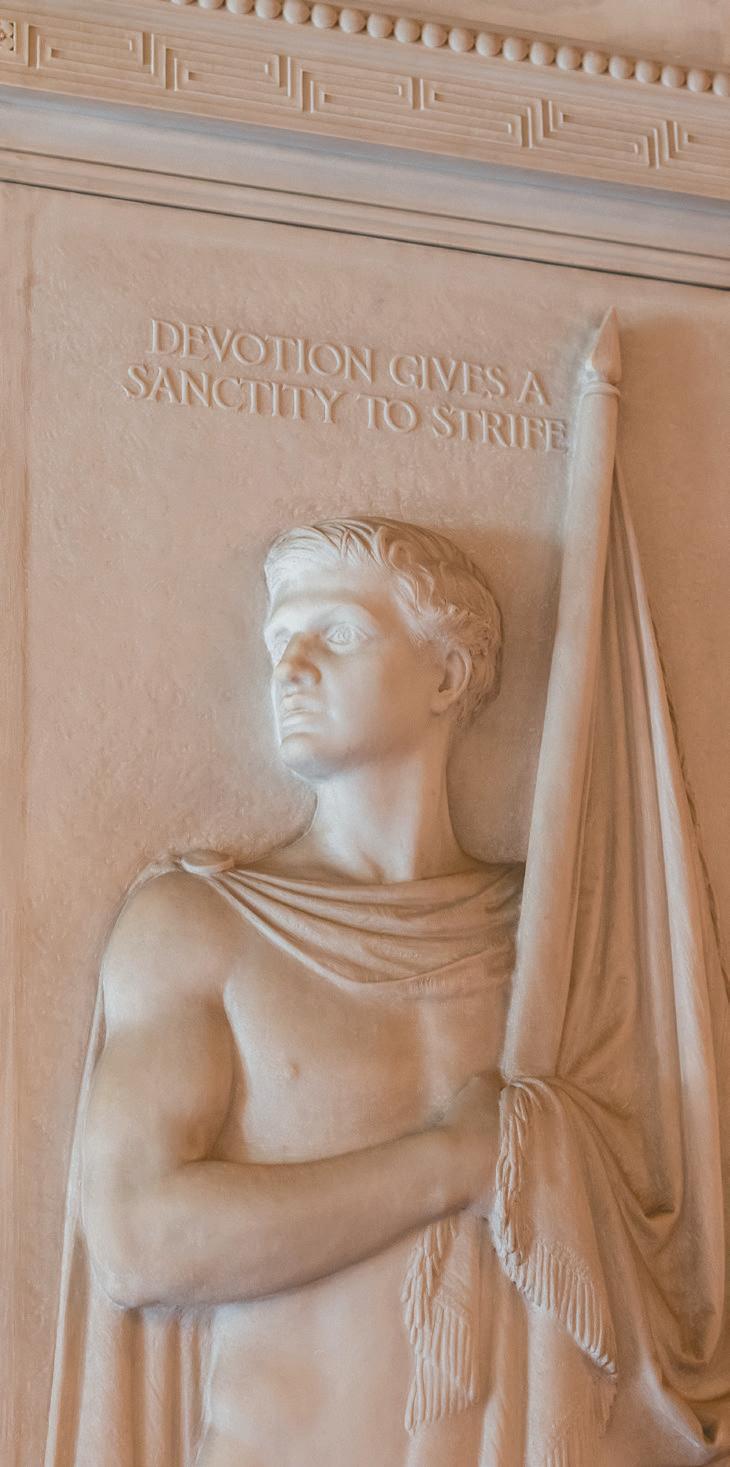
Across Connecticut, researchers, farmers, and environmentalists grapple with the uncertainty of bird flu.
By Sarah Cook

On a chilly day in January, Jay Joseph stepped outside his backyard in Stonington, CT, to check on his four peacocks. At his feet, he found one of them dead with no sign of injury. He was mystified. Naturally, he turned to the internet. Someone suggested a duck could have broken the peacock’s neck, an explanation that seemed unlikely but plausible to Joseph.
The next day, he found three of his chickens dead. He sent his dead birds to a testing center at the University of Connecticut. The samples came back positive for bird flu.
Within forty-eight hours of the test result, Connecticut’s state veterinarian, Thamus Morgan, arrived at Joseph’s house with two Connecticut Department of Agriculture officials wearing hazmat suits. Within minutes, Joseph’s ducks, chickens, peahens, and peacocks, twenty-three birds in total, were put in gas chambers. “The ball just came down on us,” Joseph said.
He remained puzzled. Did they all need to die? Joseph, a hobby farmer who runs a contractor business, first brought home two peacocks six years ago after seeing the birds during a vacation in Puerto Rico. He grew fascinated by their

through contact with an infected animal. The virus spreads through saliva, nasal secretions, or feces of infected birds, and the symptoms in birds can include fever, coughing, nausea, muscle aches, and pink eye. Among poultry, fatal and highly pathogenic, spreading bird-to-bird, or through contaminated surfaces. According to Rebecca Eddy, Director of Communications for the Department of Agriculture, the mortality rate among domestic poultry is nearly 100 percent.
Given the high pathogenicity of the virus, the current response to a positive bird flu case in the United States and most countries, per standards from the World Organisation for Animal Health, is to kill the entire flock. Although bird flu is most prevalent among wild birds in Connecticut, the birds that are euthanized to stop the spread of bird flu are usually domesticated, like Joseph’s.
“There are a handful of exceptions, but with regard to public health, de-populating free-ranging wild birds is ineffective in addressing most public health issues and can have negative impacts on rare species,” Will Healey, communications director of the Connecticut Department of Energy and Environmental Protection, said. “Surveillance and biosecurity measures relative to domestic animals are the best ways to prevent the spread of the virus.”
While H5N1 was first identified in birds in China in 1996, an especially virulent subtype of highly pathogenic avian influenza called clade 2.3.4.4b emerged in North America in 2022 and began spreading rapidly. Since 2022, there have been seventy cases in humans. The risk of spreading between humans remains low. Yet as the virus spreads, it can mutate into more contagious variants, infecting humans at higher rates. Such a mutation

Joe’s and other grocery stores recently placed limits on egg purchases). On the national level, in late February 2025, the Secretary of Agriculture, Brooke Rollins, announced a one billion dollar strategy to take on HPAI, including economic relief for farmers, investments in biosecurity, vaccine import, and support for temporary import of eggs to lower prices. A single bird flu case could wipe out an entire flock––an event which would be particularly detrimental on large poultry farms, like Hillandale Farms in Connecticut, which produces eggs for Eggland’s Best. Large farms disproportionately control egg production (in the U.S., the top five egg companies, which include Hillandale Farms, own about 46 percent of laying hens).
In Connecticut, there have been four confirmed cases of bird flu in backyard flocks: two in 2022 and two in 2025, as well as about eighty-two cases in wild birds since 2022, though none in livestock so far. In the U.S., since 2022, there have been 12,706 wild birds that have tested positive for bird flu, and one hundred sixty-eight million poultry affected. By population, the density of wild bird flu cases is roughly 75 percent greater across the country than in the state of Connecticut.
One case, though, can wipe out an entire farm. Bird flu is not preventable, and there is no current cure. While cases in Connecticut are still low, if the virus spreads, more farms run the risk of seeing what happened to Joseph’s birds: mass selective slaughter.

Indu upadhyaya, a food safety expert at the University of Connecticut, works to educate local residents on biosecurity recommendations for bird flu. As backyard flocks have shot up in popularity since COVID-19, perhaps in response to the ongoing egg shortage, Upadhyaya’s current recommendation to residents is to avoid contact with waterfowl, which can be breeding grounds for HPAI infection.
HPAI in birds can present with sudden death, like Joseph observed, as well as symptoms like swelling, respiratory problems, or uncontrollable diarrhea. If any of these symptoms are present, Upadhyaya recommends sending samples off to Connecticut Veterinary Medical Diagnostic Laboratory. But currently there is no cure or vaccine. According to Upadhyaya, if a positive result comes back, the only option is killing the entire flock, a practice known as culling.
At the federal level, Robert F. Kennedy Jr., Secretary of Health and Human Services, has emphasized biosecurity over culling, arguing birds should not be killed but rather given time to build up immunity. Immunity to bird flu, however, would require prior exposure to a mild strain or vaccination, Upadhaya said. In the U.S., vaccination is not commonly used in backyard or commercial flocks, and birds, regardless of their lifespan, remain susceptible to new infections without controlled exposure or vaccination.
Even with testing centers, Upadhyaya worries that “viruses and bacteria are extremely smart.” There may be even more cases than reported, in animals or in humans. The virus can mutate and reorganize itself in many ways, and it may become more pathogenic in the future.
This uncertainty is making poultry farming, already a difficult profession, even more challenging. Extreme weather caused by climate change has made the job unpredictable. And while chickens are typically thought to be more controllable than crops, with bird flu, farmers could lose their flock any day. “It’s piling on,” Ella Kennen, coordinator at the New Connecticut Farmers Alliance, said.

to raise for eggs, but said that due to the increasing risk of bird flu, the price was 50 percent more than it would have been last year.
Bird flu, to Kennen, remains a looming fear— “the pendulum swinging over your head and you’re just waiting for it to drop that balance.”
At the New Connecticut Farmers Alliance, Kennen works primarily with new farmers in the first ten years of their careers. Though no case of bird flu has been reported in Connecticut livestock, the threat of H5N1 still hangs over farmers. One bird flu case could jeopardize an entire flock, and chickens take time to raise.
If an entire flock of chickens is killed, it could take weeks or months to recover a flock. “Birds get the short shift,” Kennen said. Chickens on farms are labeled as “broilers”—chickens raised for meat—and “layers” raised for eggs. Broilers take about six to ten weeks to mature, but layers need up to six months to reach reproductive maturity. Since the current outbreak began in 2022, 148 million birds in the United States have been ordered to be euthanized, collapsing farmers’ years of work.
It is more costly to buy flocks now, too. Farmers usually purchase pullets, birds almost at reproductive maturity, or day-old birds, and the prices of both are on the rise. Murray Gates, from Artza Mendi Farm in Baltic, Connecticut, recently bought five hundred chickens
For diverse and smaller farms, the economic risk of losing a flock is lower than for industrial poultry farms. For diverse and smaller farms, like most Connecticut farms, Gates explained, risk is spread out among revenue sources. “If you’re a large farm, all of your eggs are in a single basket.” Small farms, though, have less profit and less of a cushion for large losses if a single flock gets wiped out. Most farmers, including Gate, already work multiple jobs on top of farming.
Steadfast Farms in Bethlehem has Connecticut’s only USDA-approved poultry slaughter and processing facility, where they expect to slaughter fifteen thousand to thirty thousand chickens this year for other farmers in the greater New England area. Despite national concerns about bird flu, starting this year, the farm is adding three thousand chickens and 350 turkeys. Aaron McCool, the farm’s director of operations and sales, said the farm has always practiced biosecurity. “Anyone who raises poultry commercially thinks about avian influenza in

the same way that every human thinks about a cold sometime in their life,” McCool said.
Steadfast Farms is also a member of the National Poultry Improvement Plan, or NPIP, which is a program that regularly tests for illnesses such as bird flu and pullorum, diseases which could lead to the farm depopulating its birds. NPIP would provide economic support in case of depopulation.
In recent months, McCool told me that Steadfast Farms has increased their spending on biosecurity necessities by 15 percent. When they suspect a bird is sick, they isolate it from the others and change their boots and outfits between visiting different species.
Still, McCool explained that no matter how much Steadfast Farms spends on biosecurity, they cannot control bird flu outbreaks. “No matter what you do, avian flu is not a preventable disease. All it takes is one duck flying over with a dropping.”

THe connecticut audubon society has twenty-two sanctuaries stretching over three thousand four hundred acres.

Tom Anderson, the director of communications for the Connecticut Audubon Society, told me that H5N1 is not their biggest concern. In the last fifty years, the number of birds in North America has dropped by three billion, or 30 percent, due to construction and domestic cats, along with pesticide use and building collapses. “Avian flu is not even on the radar compared to those others,” Tom assured me. I wondered how he felt about the media attention bird flu gets over these other concerns. Tom defined it as an issue of attention. “Four billion birds dying every year because cats kill them is a big problem. But it’s hard to write or broadcast a news story about that,” he said.
Similarly, at Steadfast Farms, McCool says he is less concerned about bird flu than with feeding people. “Avian influenza is not new, but this national story is new. We always ask why the negative stories about what could happen become so popular, instead of the stories about what these local farms do for their communities, how they give back, and how they serve the people that they feed.”

While bird flu might not be the primary worry for Anderson and McCool, for Joseph, he cannot forget.
After news coverage of his bird flu case, Joseph receives messages from across the country from people asking if he wants them to send him new birds. He appreciates the outreach, but is reminded of the loss of his birds whenever he looks out on his backyard. He took the pump out of the pond where his ducks used to swim and let the pond freeze over. “The backyard is dead now,” he said.∎
Sarah Cook is a senior in Grace Hopper College.

A New Haven activist, Yale doctor, and Yale lawyer won Americans the right to oral contraceptives as part of a liberating—and eugenic movement. Today, patients and doctors still confront the tension between autonomy and coercion.


In the spring of her senior year of high school, Asha Goyal ’27 made an appointment with her doctor at home in Los Angeles, CA Each month of that year, she had spent five days out of commission. She was nauseated. Her temperature fluctuated. She had joint pain, and back pain, and stomach pain. Her period could not be subdued by any amount of Advil or number of hours spent clutching a heating pad to her abdomen. She told her doctor. He told her to tolerate the pain––to wait until she was 25, when her body would “mellow out.” Asha, 18 at the time, did the math: she would spend eighty-four weeks of the next seven years in pain. “That’s nearly two full years of my life that I’m going to be miserable,” she said on the patient table. “And I’m supposed to wait it out?” Her doctor was silent.
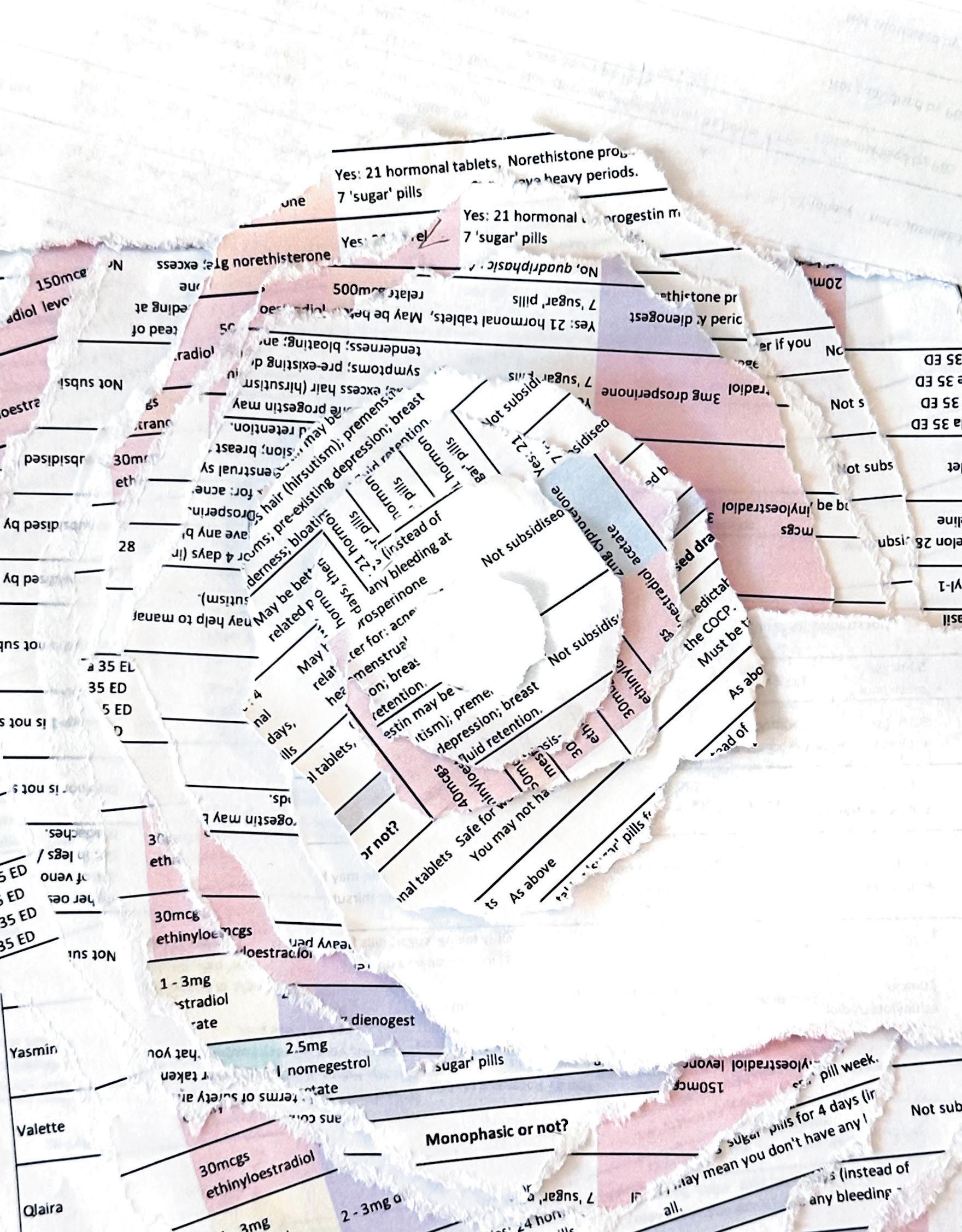
In the absence of satisfying medical advice, Asha’s mother made a common suggestion: might she try a birth control pill to regulate her cycle? Asha figured it was worth a shot. She knew friends who were taking oral contraceptives. Some took pills with both estrogen and progestin—hormones that suppress ovulation and regulate menstrual bleeding––and some took pills with only one of the two hormones. In February 2023, during Asha’s freshman year as a mechanical engineering major at Yale, her new doctor at the Yale Health Center prescribed an estrogen pill.
Then Asha got her period. It lasted fourteen days. Her doctor said to give her body three months to adjust to the pill, and suggested skipping the five placebo pills at the end of her pack, which typically induce a period. But Asha got her period again in April. It lasted thirty-five days, until the end of May. She had worse mood swings, pain, and acne than ever. When Asha went back to her doctor before leaving for her summer study abroad program, her doctor said to give it six months. A week after the appointment, she had another painful, fourteen-day period. “I think I spent like 40 percent of last year bleeding,” Asha says.
She spent about the same proportion of her time crying. Three weeks in, as Asha packed for spring break, she was overcome by a foreign, persistent sadness. She cried through her study abroad
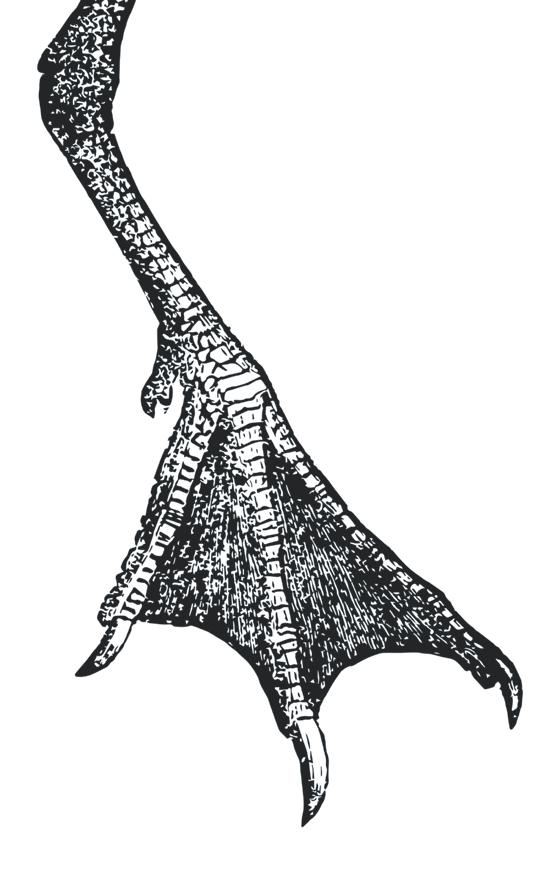
Illustrations by Mia Rose Kohn.

program in July, through time with family in August, and through the first two months of her sophomore year. “I physically could not cope with life. I just couldn’t move.” She loved her classes, her friends, her comedy group, yet the tears came every night. Asha could never predict when her body would start bleeding, or crying. “I just did not feel like myself,” she says. Her body and her mind felt like those of a stranger.
According to a 2023 study published by the National Library of Medicine, 83 percent of participants said their doctor had not mentioned the possibility of psychological side effects when prescribing a birth control pill. Of those who experienced such changes, over one-fifth felt that their provider did not address their concerns. Asha’s doctor had said that mood swings and bleeding between periods could be a side effect of the pill. But was her depression a “mood swing”? The term felt inadequate, and she felt unprepared for her debilitating symptoms.
Every day she asked herself, “What if tomorrow I take the pill and it’s all better? What if I stop today, and then six months of depression have all been for nothing?” Was three months long enough? Six months? Six months and one day? “I really just should have stopped,” Asha says in retrospect, pausing. “I hoped that they would be able to fix me.”
Anabel Moore ’25, a pre-med student at Yale, had hoped the same. When she was 17, her period cramps were so painful, she fainted in the bathroom of her Woodinville, WA, high school, smacking her head on the white tile floor. Plus, she had a boyfriend. Birth control seemed like the obvious course of action.
Her doctor prescribed a birth control pill with only progestin. This pill would have fewer side effects than estrogen pills, he said, and would not increase Anabel’s risk of blood clots, which ran in her family. Anabel also couldn’t risk the weight gain, fatigue, or depression that her friends warned her about. She was playing elite club soccer.
The side effects came anyway. Almost immediately, she had panic attacks and bouts of despair so severe she visited a psychologist, who prescribed antidepressants. Two months after beginning her oral contraceptive, she had brain fog and memory problems. Her hair—usually unmanageably thick––fell out in clumps. As an aspiring doctor, Anabel had pored over medical journals before going on her pill. She still felt unprepared by her doctor and shocked by her side effects.
“Autonomy and health had always gone hand in hand,” she says. “But I felt like I was sacrificing my physical and mental health for my sexual health, as in, those three couldn’t all coexist at the same time.” Her contraceptive pill accomplished what it was supposed to for sexual health. But at what cost?
“It is designed to give women agency, but it feels as though, in order for us to be agents, we have to forego our own basic needs,” she says with matterof-fact acceptance.
The decision to take any medication is a cost-benefit analysis. For Anabel and Asha, the costs seem high in hindsight. The costs also seem hard to calculate. Should they have considered the
weight gain they both experienced and that is the most commonly reported reason American women discontinue the pill? Or, that not a single medical study has found a correlation between oral contraceptive use and weight gain? Should Asha, who was taking an estrogen pill, skim the World Health Organization’s list of Group One carcinogens, where she would see that estrogen-containing birth control pills increase current users’ risk of breast cancer by 24 percent, and, if taken for more than five years, increase risk of cervical cancer by 60 percent? Or should she have prioritized the 30 to 50 percent decreased risk of ovarian and endometrial cancer that the pill can offer? Anabel and Asha might be alarmed by the articles in The New York Times, Washington Post, New York Post, and more that reported on a trend of women quitting the pill “en masse,” as The New York Times wrote in 2024. Anabel might read the increasing number of negative posts about birth control on X, especially about oral contraceptives. Asha might search “birth control” on YouTube, where 74 percent of the videos feature a woman quitting her pill because of side effects, according to a decade-long study published in 2019 by Harvard Medical School researchers. Anabel and Asha could also be reassured by reading that doctors are prescribing the pill at all-time highs in 2023, according to health analytics firm Trilliant Health.
The decision to take the pill turns into a paradox, one that feels impossible to solve even for two women churning out mechanical engineering problem sets and MCAT practice tests. Anyone who wishes to solve the pill paradox must navigate several tensions: between social and medical trends, between reported symptoms and studied outcomes, between the promise of autonomy and the costs of control.
Anabel and Asha are not the first generation to perform this cognitive dance. Sixty years ago, a New Haven activist and a Yale doctor won Americans the right to oral contraceptives, in a movement for progress that also inflicted pain. For the promises of science and the experiences of individuals have seldom aligned in the history of the birth control pill.
Police to decide the fate of birth control clinic,” reported the Yale Daily News on November 7, 1961. The Planned Parenthood clinic on Trumbull Street had been open for three days, headed by Yale School of Medicine’s C. Lee Buxton, chairman of obstetrics and gynecology, and Estelle Griswold, a 61-year-old gray-haired, firecracker feminist from Hartford. The clinic operated in direct violation of an 1879 Connecticut law, introduced by a New Haven senator, that effectively criminalized contraception. It was a more restrictive version of the federal Comstock Act, nicknamed the “chastity laws,” which, by the beginning of the 1960s, many states treated as “mere dead words,” as a Supreme
Court justice wrote in June 1961. Forty-three states had no legislation on birth control or varying restrictions on advertising the pill. Not Connecticut. The sale and advertisement of contraceptives was strictly prohibited, although affluent, married women could typically obtain medication illegally.
Griswold and Buxton were arrested in their clinic. In the four years following, their case was argued appeal after appeal, all the way to the Supreme Court––first by Yale Law School graduate Catherine Roraback LAW ’48, then Yale Law professor Fowler V. Harper, and finally Yale Law professor Thomas L. Emerson LAW ’31. In 1965, the Yale-led team won. Griswold v. Connecticut was one of the most influential cases in modern constitutional history and set a precedent of citizens’ right to privacy, later leveraged in Roe v. Wade. The pill got a new nickname: “Freedom in a tablet.”
The tablet which Griswold freed from back-door clinics and underhand prescriptions does not have a simple relationship with liberty. Estelle Griswold’s inspiration and national counterpart Margaret Sanger, the founder of the Planned Parenthood World Population Organization, built the American contraceptive movement on a foundation of eugenics.
Three decades before Griswold’s Supreme Court battle, the Yale Daily News interviewed Sanger. The “proletariat,” she said in 1934, willfully refused to employ contraceptive knowledge she claimed they did, in fact, possess.
“Did you ever realize that the lower classes are in that position on the ladder of society just because of their deplorable lack of control and ignorance in vital matters of how to cut down the birth-rate?” Sanger asked. “This condition of over-production could be done away with in one generation by proper birth control going hand in hand with sterilization of mental defectives.” She continued, expressing her admiration for the courage of the Nazi regime to sterilize their mentally and physically “unfit” population.
Like Margaret Sanger, Estelle Griswold was a champion of science and women’s rights. Also like Sanger, she aligned herself with the American

eugenics movement. Behind eugenicists’ mathematical illustrations and methodical texts, racism became a kind of science too. It was this science––of population control––by which doctors and activists promoted the pill as the drug of the future.
Between the 1930s and 1960s, Yale welcomed this movement to its campus. Among other speakers, they hosted Guy Irving Birch, director of the American Eugenics Society and founder of the Population Reference Bureau (still active today) to discuss sterilization and his self-coined term “population explosion.” Dr. John Rock, co-developer of the oral contraceptive pill, also lectured at Yale. To an audience of three hundred male students in Harkness Hall, Rock, the Yale Daily News reported, spoke about the “male coital urge” and impending population crisis and food shortages. He did not speak about women’s health.
Nine years before his lecture at Yale––and five years before the Food and Drug Administration approved his pill––Rock and his research partner performed the first large-scale clinical trials on Puerto Rican women in April 1956. The U.S. territory was one of the most densely populated areas in the world, and, luckily for Rock, had no laws against contraceptives. Sign-ups filled quickly. The women, eager to try this alternative to sterilization, did not know that they were participants in a trial.
After one year of the experiment, doctors running the operation reported back to Rock: the pill was found to be 100 percent effective, but side effects were too debilitating for the pill to be considered “generally acceptable.” Women were overcome by nausea, migraines, blood clots, pain, symptoms Rock waved away as psychosomatic. Three young women died. Their deaths were never investigated. In 1960, the pill was approved by the FDA, which continued its support of the pill even after a 1961 report raised concerns over deadly clotting in pill-users. They reasoned that the frequency of such clotting was lower than deaths from pregnancy.
The pill was the future. The pill was control––but of whom and by whom was less clear.
Dr. Megann Licskai GRD ’22, Lecturer of History of Science, Health and Medicine at Yale, teaches about contraceptives as two-headed technologies: tools of the feminist fight and tools for manipulating women. Margaret Sanger embodies this contradiction. She responded with compassion to countless letters of women begging for contraception care. She also lectured to the Ku Klux Klan. She opened health centers on the El Paso border. She funded them by stirring concern among wealthy families about the economic and racial threats of migrant reproduction.
“I think the most generous reading of Margaret Sanger is that she was a one-issue woman,” Licskai says, sighing. “She was an extreme opportunist, and she was going to get her message out whatever way she could.”
Perhaps Rock made a similar calculation: women might suffer on his pill, but their circumstances would improve. The pill was a means to this end.

“The problem,” says Licskai of this thinking, “is when we use the pill as answers to social or systemic problems, when the answer is just, ‘don’t have the family that you want,’ because we lack these broader social structures to support that family.”
A small pill in a plastic sleeve that promised to solve poverty was a miracle to a generation of progressive scientists. Sanger and Griswold’s names are uttered upon the lips of constitutional scholars and reverent feminists. Far less remembered are the women sterilized on the El Paso border and killed in the Puerto Rico trials of that small pill.
Contraception is never ideal for the patient.
It will always change something about your body,” says Dr. Meredithe McNamara, adolescent gynecologist and Assistant Professor of Pediatrics at the Yale School of Medicine. This is a fact doctors do not routinely acknowledge, she says after a long exhale. “Overwhelmingly, I find that it is not an easy or joyful decision for a young person to opt for any method of menstrual control.”
The changes that occur to women’s bodies when using a birth control pill can be divided into two categories: preventing pregnancy and everything else. The pill’s contraceptive function is highly reliable, at 99 percent when the pill is taken as directed. Other changes vary widely in frequency, and range from regulated menstrual cycles to sleep disturbances, libido loss, and migraines. The side effect sheet enclosed in each pill package unfolds to several feet long. In one popular TikTok trend, women wear the sheet as a shirt or blanket. Some women also experience few side effects or even mood improvement.
The pill’s history, says McNamara, can explain the discrepancy between its reliable ability to prevent pregnancy and unpredictable effects on other aspects of health. “Medicine has not existed historically to serve the needs of the patient only,” she says. Doctors, researchers and political actors have historically taken interest in the first change the pill produces: preventing pregnancy. The other effects––like those Dr. John
Rock deemed psychosomatic––impact only the person consuming the pill, and those close to them.
“I think there is a quickness to prescribe the birth control pill that goes back to its history,” says McNamara. “The field of contraception came about in part to accomplish eugenics, to prevent people from procreating who some people deemed should not procreate.” Oral contraceptives, specifically, were thought of as a miracle solution, a fix for “all of society’s ills,” she explained. The same miracle is sometimes promised to patients.
“It is really uncomfortable to address the fact that this amazing, liberating option might have big consequences for our health.”
Even though the pill was not created to relieve period pain or regulate bleeding, doctors frequently prescribe it to do so. Like Asha, 82 percent of women aged 15 to 19 who take a birth control pill employ it for non-contraceptive reasons, according to a 2011 study conducted by sexual health NGO Guttmacher Institute. Like Anabel, 58 percent of adult women take the pill for both contraceptive and non-contraceptive reasons. Dermatologists prescribe the pill to treat hormonal acne, with more than an eighth of oral contraceptive users relying on the medication for this function. Intrauterine devices (IUDs), patches, and implants are rarely prescribed to regulate heavy periods and certainly not prescribed or inserted by dermatologists.
Patient satisfaction may also be suffering because contraceptive care is a political––as well as medical––issue.
“There are lots of competing political interests that guide whether or not people get good information about contraception,” says McNamara. “There are people who think that contraception is immoral, and so they’re trying to take research down. There are people who over emphasize the benefits and effects of it, so that certain groups of people do not have children. None of that has to do with the individual.”
In February, the Trump administration removed CDC- and FDA-produced research about contraception, along with information about adolescent and LGBTQ health. The administration republished the information after a lawsuit.
McNamara cannot control politics or social media tides, but she can provide her patients with thorough contraceptive counseling––something many patients do not receive. According to a survey conducted by leading health policy organization Kaiser Family Fund, only 30 percent of women felt that they received all the information they needed from their doctors before choosing a birth control method. That number dropped to 12 percent among Asian and Pacific Islander women and 28 percent among Black women. 80 percent of women like Asha and Anabel experienced multiple side effects that were worse than they expected.
Before McNamara practiced autonomously, she completed a fellowship in adolescent medicine, a pediatric residency, and an additional fellowship in adolescent gynecology––disciplines which center counseling as part of medical care, she says. The vast majority of doctors prescribing birth control, like primary care providers, adult gynecologists, and dermatologists did not receive this counseling-centric training. “Most people in medicine are not taught how to offer neutral, thorough, and open contraceptive counseling,” she says. “I think it’s at the root of a lot of dissatisfaction with contraception.”
Several days before we spoke, one of McNamara’s residents had treated a teenage girl with menstrual cramps so severe she was vomiting and missing school. The resident prescribed a birth control pill. Why not a patch, ring, or well-timed Naproxen, a pain killer effective in treating menstrual cramps? McNamara asked her resident. Had the patient expressed interest in a birth control pill? She had not.
“The way that we’re taught to care for patients is very much, ‘I’m the expert. You do what I tell you to do,’” McNamara says. Days before the incident, McNamara had even taught a lecture on shared decision-making in contraceptive counseling. The resident was not a bad doctor, McNamara insists. She was simply following her prior medical training that ingrains, according to McNamara, a paternalistic directive to offer medications.
Dr. Sangini Sheth ’03, another gynecologist at Yale Health and professor at Yale School of Medicine, also pointed to the “paternalistic” mode of counselling most doctors provide as a source of patient dissatisfaction.
Dr. Aaron Lazorwitz, Assistant Professor of Obstetrics, Gynecology and Reproductive Sciences at Yale School of Medicine researches contraceptive side effects. During his years as a medical student and resident, Lazorwitz was shocked by his patients’ dramatically variable responses to oral contraceptives and his superiors’ lack of knowledge or interest as to why. “I would ask attendings and experts in the field,” he says. “There was no explanation for it.” We can do better, he thought.
“Acceptance,” he says, has been the status quo of women’s health. Funding hasn’t been plentiful either. Although most oral contraceptive pills have far less estrogen than their predecessors and more advanced formulations of the progestin hormone, the pill and its many side effects have remained quite similar since the 1950s, says Lazorwitz. He performs the surly voice of one of his colleagues. “We don’t need to make things better. Women can take these pills, and they can deal with the side effects. They’re fine.” In other words, if the pill was stopping pregnancy, the pill was working.
In November 2024, Lazorwitz began a study on birth control and genetics, which seeks to discern why the same medication causes such a variety in type and intensity of side effects. In a previous study, Lazorwitz identified a gene in contraceptive implant users that affected their metabolism of hormones. The same gene might predict how patients react to
oral contraceptives. Future pill formulations, prescription practices, and more personalized care would benefit from this understanding.
“The pill has a very troubled past,” he says. “There are lots of drugs we’ve tested in populations we shouldn’t have.” His goal is to provide the very best options to his patients so that they can choose––not be coerced by lacking information, care, or good options.
“The pill is not not the bad guy. It’s more that we can’t rely on only the pill.” Lazorwitz hates when he hears physicians boast that everyone should be on this pill or that IUD. He believes there are as many right answers to contraception as there are individuals.
political interests. “I’m interested in the place where the far left meets the far right on subjects like vaccination and birth control, this idea of naturalness, where ‘natural’ becomes a stand-in for ‘good,’” Licskai says. Are some of the rampant negative social media posts about birth control pills selling this moralizing concept? Could they be selling products, like natural family planning apps, she wonders?
Sheth is wary of contraceptive misinformation on social media. “But,” she says, “I can’t shut down the conversation just because a patient says, ‘I saw this on social media,’ because that’s a part of their world.”
Isit with Wilhelmina McQuarrie ’27, a Yale sophomore studying political science, in the nave of Sterling Library on a beige leather chair. Her story is much like those of Asha, Anabel, and the ten other women with whom I spoke. She suffered difficult side effects, and received conflicting advice from doctors she saw at home, at school, and while traveling. Yet, when she opens her mouth to speak about her experience, she pauses. “Thank God for birth control,” she says. She needs to say this, she feels. Women’s autonomy is endangered by abortion bans and threats from President Trump to enforce the Comstock Act, which was never fully repealed. On April 1, the President’s administration terminated U.S. funding for contraceptive care in developing nations, leaving fifty million women without access to birth control.
Wilhelmina feels caught. How can women hoping to defend their autonomy raise concerns about their health––concerns that might erode support for contraceptives? “It is really uncomfortable to address the fact that this amazing, liberating option might have big consequences for our health,” she says.
Wilhelmina’s ability to engage in this discomfort is a feature of the political climate of the last six decades, according to Licskai. The 1970s initiated a loss of trust in medical authority––and more generally in all forms of institutional authority, as one scholar notes in an article published in the National Library of Medicine. This loss of trust may have also empowered patients. “On the one hand, it’s fantastic that patients are able to say, ‘I’m not going to accept medical authority without question,’” which was not the case for much of the 20th century, she says. “It also means that it’s really hard to know what to trust, whom to trust.”
Social media has exacerbated this fraying of unilateral scientific authority into the pluralistic, experience-driven authority of social media. The discomfort is a trade of one sometimes-corrupt truth, in exchange for many sometimes-false truths––between a doctor saying, the unfit must be sterilized, and a woman posting, the birth control pill must have caused my infertility.
Doubt is also easy for opportunists to commandeer, and patients may fall prey to a new set of
After seven months of being on the pill, Asha told her doctor that the medication was not working for her. She switched to a different estrogen pill in late September, which restored her upbeat spirit and gracious sense of humor. But, a year after beginning birth control, her periods are similar and sometimes longer than they were before. “Looking back, I wish I had just powered through those five days a month,” she says.
When Anabel left her soccer team before college––and was more comfortable with an invasive procedure and conversations about her body––she opted for an IUD at Yale Health, which was itself a harrowing process, causing the worst pain of her life and persistent issues with placement and bleeding. Increasingly, Anabel has been considering giving up hormonal contraceptives altogether, but for now, she’s decided to keep the IUD. “It’s just this perfect catch-22. There’s no good option.” she says, arms crossed with the resolute composure of a future doctor. “I have so many fish to fry in the world, and it’s like, I gotta pick my battles.”
McNamara never discusses her own contraceptive care with her patients, but she shares in Anabel’s frustration. She is keenly aware that science has yet to explain everything about her body. “I know that I cannot take a birth control pill,” she admits. “I get horrible brain fog. I feel very weird. It’s a totally bizarre reaction, and I have never found anything in the medical literature that describes it.”
Even as a trained physician, McNamara struggles to resolve the conflict between her own experience and medical information, between her values and those of some other doctors, between her commitment to contraceptive care and the injustice from which her field was born. How could her patients solve the paradox, she wonders?∎
Mia Rose Kohn is a sophomore in Grace Hopper College and an Associate Editor of The New Journal.
ZACK BEAUCHAMP
DAVID
SEYLA
FRANKLIN
MICHELLE GOLDBERG
RONNIE GRINBERG
REBECCA KOBRIN
JOSHUA LEIFER
ANTOINE LILTI
SUSIE LINFIELD
JAMES LOEFFLER
HELENA
STEVEN
ELISABETH ZEROFSKY

PROGRAM
WEDNESDAY, APRIL 30, 2025 | 4:00–6:30
THURSDAY, MAY 1, 2025 | 9:00–5:30

After a landmark lawsuit, Yale drastically reformed its leave of absence policies for students with mental health crises. Two years out, how far has it come?
By Kelly Kong

Isaac monks videocalls me from his dorm room. Behind him, Yale merchandise—a blue-and-white hockey jersey, a striped scarf, a “Y” pillow—lines the walls.
A member of the Class of 2027, Monks is looking to graduate in two years. However, Monks’ journey here started in 2021. This is both his fourth year, and sophomore year, at Yale.
“And that is my lore,” he laughs.
Monks, 22, is among the last students who took a medical withdrawal for mental health reasons before Yale implemented monumental reforms to absence policies between April 2022 and January 2023. These changes came about after first-year student Rachael ShawRosenbaum’s campus suicide in March 2021 precipitated a class-action lawsuit against the university.
Monks’ mental health struggles in high school escalated to severe depression after arriving at college. Just a month into his first year, his then-residential college dean told Monks that if he couldn’t keep up with his classes, he was not going to “make it” at Yale.
“That, like, broke my spirit entirely. I barely left my room. I never ate,” said Monks. “I had been, you know, basically just starving myself for days and days and days.” Weighed down by the depression, Monks missed more of his classes and deadlines.
Just a few days later, Monks was called into his dean’s office again to discuss his academic difficulties. This time, his dean recommended a “medical
withdrawal” to him. “They kind of presented it as the only option,” Monks explained. “They were like: you don’t want to fail this semester. You don’t want to do this.” His dean then told Monks he had one day to make this decision.
Monks withdrew in fall 2021, in the pre-reform era. At the time, students who withdrew lost all campus access, Yale healthcare, and student jobs. They were also asked to move out within seventy-two hours of processing their withdrawal. During their time away, they were required to complete two credits—classes either at Yale Summer Session Online, or other colleges—and remain “constructively occupied” or else forfeit their right to return as a student. The reinstatement application required transcripts from their outside courses, two letters of recommendation, a statement about the circumstances of their leave and readiness to return, as well as an interview with the Chair of the Committee on Reinstatement and a clinician of Mental Health and Counseling.
Monks applied for reinstatement to return in fall 2022 to be in the Class of 2026, but was rejected for not completing the two credit requirements because he failed his “Intro to Programming” class.
In January 2023, three semesters into Monks’ leave, Yale announced landmark mental health reforms.
Just a few months prior, in April 2022, Yale had removed the requirements to complete coursework and to interview with the committee chair, requirements which had originally prevented
Monks’ return. By 2023, the need for letters of recommendation and the “constructively occupied” requirement were also eliminated.
After the reform, Monks set his eye on returning to Yale in the fall of 2023. This time, his reinstatement application was accepted. But it had already been two years since he first enrolled at Yale, and he struggled to relate to other firstyears who were not his age. “I was also at a point in my first semester coming back where I was like, I’m not in any clubs. I don’t have any friends.”
His relationship to school had shifted. “It literally does not matter what I do at Yale, as long as I finish.”
In Yale’s current Medical Leave of Absence policy, students are no longer burdened with a checklist of reinstatement requirements to return.
Rates of depression, anxiety, and suicidal behaviours have increased steadily among young adults in recent decades. The American Psychiatric Association reports that 75 percent of mental health illnesses show up by age 24, meaning that the years students spend in college are hotbeds for mental health crises.
For the past four years, mental health advocacy group Elis for Rachael has called for policy change, and Yale’s decision to comply was monumental. More than two years into the reforms, students continue to see the updates as a significant step in the right direction. Nevertheless, student advocates argue that ongoing policy flaws in housing, deans’ support, and student privacy still
reveal a lack of consideration for its most vulnerable individuals.
Lucy kim ’24 was among the last group of students who took leave pre-reform, doing so after struggling with a rare sleep disorder. After Kim’s withdrawal was processed in Fall 2021, she immediately lost the top three things she would have needed for recovery—a place to live, a social support network, and healthcare.
She was eventually able to acquire insurance through a working parent in California. However, Kim was unable to return home for multiple reasons, including lack of space. To this day, she still remembers the frantic seventy-two-hour countdown to find temporary housing in New Haven through Facebook groups after her withdrawal was processed. Soon enough, she had spent most of her savings on the apartment, working part-time as a private tutor, essay reviewer, and at a test-prep academy to make ends meet.
Kim points out that the old policies placed significant burdens on students dealing with medical crises. For one, the regulations often left low-income students in a health crisis, working side-jobs to pay for living expenses. The same student was also required to complete coursework and seek recommendation letters, all while trying to focus on their recovery.
Even before Elis for Rachael formed, there were long-standing frustrations with Yale’s inaction. “At least half a dozen different student groups over the past decade had written very well researched reports to the Yale Administration, saying: Here are the problems with your mental health services. Here is what you should do about it,” said Paul Johanson ’88, an advocate from Elis for Rachael.
In 2013, the Yale College Council (YCC) released a report based on interviews and survey responses of one thousand undergrads, detailing problems in delays of mental health and counseling treatments, insufficient leave policy, and more. In early 2015, a wave of student advocacy for withdrawal policy reform came after the death of Luchang Wang ’17, who, in her suicide note, discussed her fears about withdrawing from Yale and not being able to return. In April
2015, Yale College responded with a change of terminology: post-medical withdrawal “readmission” into Yale was renamed to “reinstatement.” They also eliminated the application fee of 50 dollars for reinstatement. YCC conducted a similar survey on mental health feedback again in 2018.
Johanson cites bureaucratic lethargy as one main reason for Yale’s lack of response. “It’s very easy for inertia to set in and for nothing to happen.”
But in March 2021, the suicide of Rachael Shaw-Rosenbaum ’24 reignited

the ongoing debate of mental health policies at Yale. Johanson and other alumni founded the nonprofit group Elis for Rachael, demanding the university change its approach to students in mental health crises.
Then, in November 2022, the Washington Post published the article, “What if Yale finds out?”, following the university’s withdrawal policies. Yale’s attitude toward Elis for Rachael changed “literally overnight,” Johanson said. “Within twenty-four hours of his article coming out, the people we had been negotiating with for a year and a half wanted to talk to us in earnest.”
Two weeks after the article, Elis for Rachael filed the lawsuit. Two months
later, Pericles Lewis, Dean of Yale College announced the policy change. The lawsuit, as a result, was settled. Under the new policies, “medical withdrawal” was renamed to “medical leave of absence.” The “leave” status conferred benefits not available to “withdrawn” students, including campus access and Yale Health Center coverage. Financial support for the continuing insurance premiums for students receiving the highest levels of financial aid may also be granted. Furthermore, students can continue campus jobs, meet with advisers at the Office of Career Strategy, and use library resources.
As Lewis wrote, the goal of these changes was to make it easier for students to take time off should they ever need to and easier to return. And it has, for the most part, achieved its purpose.
Kim recalls feeling immense relief after hearing the news, especially realizing other students wouldn’t have to go through the same isolating experience. “I had kept thinking to myself, ‘If only I had gotten sick a semester later or a year later,’” she said.
Still, some regulations have not changed since the reform. Students who take any form of leave of absence today are still expected to “move out within a few days, usually within 72 hours.”
At Columbia University, student residents who take a leave of absence have thirty days to move out of their housing, from the day of their student eligibility status change. Students with “exceptional health care needs resulting from critical, acute conditions,” may also request to remain in housing beyond the thirty-day period.
But Yale’s move-on policy appears to solely take “enrollment regulation” into consideration, not acknowledging the fact that many low-income students in health crises may need more time to secure stable housing before departure.
After his seventy-two-hour moveout, Monks returned home to Oklahoma. But his family was upset with him over his decision to take a medical leave of absence. Monks was eventually left without stable housing. A first-generation, low-income student, he moved to Providence, RI, and worked over forty hours a week as a casino dealer to pay for rent and living expenses. “My family
is not necessarily in the position to just give me everything that I need so I can go to therapy and just live a chill life,” said Monks.
Chloe Hong ’25, who has also taken leave both before and after reform, believes that Yale does not want to change its move-in policy because it wants to avoid liability for student incidents.
“[The policy] makes it very obvious that their intention is: We don’t want you to die on this campus—we want you to die somewhere else,” said Hong.
The move-out policy pertains to students on mental health leaves, but the Mental Health and Counseling Office (MHC) does not have any involvement with the housing regulations, according to Paul Hoffman, Chief of MHC When asked about the move-out policy, the Yale College Dean’s Office wrote in an email that only students who are enrolled are eligible to live on campus. “Almost always, students have already made their transition plans before they take leave. The college can provide assistance, when necessary, in packing and shipping belongings and in making travel plans, and usually can be flexible in the exact departure schedule.”
Hubert Tran ’27, co-president of the Yale Student Mental Health Association, points out that students in mental health crises do not always have open volition or clarity on whether they take leave or not. In many cases, college administration or medical providers recommend leave of absence to students, and leave them alone to apply for leave by themselves without guidance or knowledge on the outcome.
“[Taking a leave] is not out of the fact that they just want to take a vacation,” said Tran.
In Monks’ case, he felt that the leave was, in some way, “pressured” onto him.
Neither Kim nor Monks knew whether their leave request was going to be accepted or rejected. With the seventy-two-hour deadline ticking away, they were not sure if it would be cost-effective to make plans before leaving, nor where exactly to go after the leave gets processed.
“If [Yale] had an ability to offer, like, maybe some sort of temporary housing, at least, like, a week, right? Give me a week to calm down and figure out how I’m going to get home. That would be good,” said Monks.
Another point of contention in Yale’s mental health support is students’ inconsistent experiences with residential college deans.
Deans often serve as the first point of contact both for students exploring mental health support, as well as those considering time off. Paul McKinley, Senior Associate Dean of Strategic Initiatives and Communications, wrote that while deans provide no clinical care themselves, they are trained to “become well acquainted with clinical resources” to guide students seeking professional help. Deans also participate in mental health first aid.
Several students, however, express a wide range of experience in discussing mental health with their respective deans.
Jaimee Nguyen ’26.5, who also took leave post-reform, has had two different deans during her time at Yale. When she went to her first dean in her freshman year for support in her declining mental health, the dean offered one option: to take a leave of absence. “She didn’t really offer me other options or other support,” said Nguyen.
Her second dean responded differently: “He gave me a lot of reassurance that, like, everything would be fine if I needed to take a leave,” said Nguyen. “And he’s very pro-mental health, which is definitely helpful.”
Beyond serving as holistic academic advisors, deans often introduce mental health support networks and experience at Yale. Yet, just as residential college assignments are randomized, each dean’s perception and leniency towards mental health issues seem like a matter of luck. Hong notes that students’ inconsistent experiences may be caused by inadequate understanding of mental health struggles.
James, who asked to only be referred to by his first name for privacy reasons, made an appointment with his dean to get an extension for mental health struggles. In that meeting, his dean asked him to use Google Calendar to schedule out his life. “I was like it’s a little hard because I can’t really plan out say an anxiety attack or a panic attack,” said James.
His dean’s response, however, shocked him. “‘You just kind of block out some time on your GCal. You can kind of work around the attacks,’” James recalled her saying. “I was like:

this is the most unhelpful conversation I’ve had.”
Monks comments that non-medical professionals may also have an outdated understanding of mental health struggles as polarizing, life-or-death situations, which ignores a students’ nuanced needs for recovery.
“I was being treated as if it was going to be the end of my life. Like it’s either you leave Yale to save your life, or you’re going to stay here and end your life,” said Monks.
He suggests that beyond training deans to properly deal with mental health crises, Yale should consider implementing “leave advisors” who professionally make recommendations to students on whether or not to take leave, and guide them through their term of absence.
Johanson, an Elis For Rachael advocate who has interacted with several students who were treated at Yale for mental health reasons, says that he has heard of several cases in which students believe deans have acquired information not at their discretion: “Medical information often filters into places where [students] felt it shouldn’t have been filtered,” he said.
C., who has requested to be identified by a pseudonym to protect her privacy

around her medical history—told me that after telling a MHC clinician about occasional thoughts of self-harm, she started getting calls from various staff at Yale Health asking for her location. They also asked whether she is safe or “has a safety plan.” Soon after, her residential college dean also started scheduling unprompted meetings with her to discuss her mental health.
Three days after that counseling session, C. says she returned to her dorm to find metal bars installed over windows on her floor (she lived on the fourth). She says no one offered an explanation to her for why the bars were installed. As of early April, only one bar appears to remain, in the hallway.
These meetings, calls, and protective bars, reportedly installed at other universities for suicide prevention purposes, made C. suspect that her medical information had not only traveled throughout clinicians at Yale Health, but also to her residential college administration without her permission.
“I find it very hard to trust [people here] now,” she said. “I don’t feel comfortable telling anyone anything.”
McKinley, however, writes that students need to “give consent”—likely by signing an Authorization for Release of
Mental Health Record—for their health care providers to communicate with residential college deans.
Yale Health similarly states that medical records are “strictly confidential, stored in a restricted area and available only to individuals involved in your care and authorized administrative personnel on a need-to-know basis.” C., however, expresses that Yale Health does not make clear to students what reportable, “need-to-know” mental health crises are, leaving her at a loss to what she can comfortably share with her providers without worrying about external involvement, or being asked to take a leave.
Kim recalls that when she mentioned to her Yale provider about taking a medical leave, her provider, unprompted, offered to email her dean. It was unclear to Kim whether her provider was only communicating her medical leave considerations, or sharing her health information as well.
“As students, we are consumers of Yale Health. Our clinicians are connected to the Yale Health system,” said Kim. “The system is not transparent. It’s unclear to us as students what communication goes on between our medical providers and our academic faculty and deans.”
This uncertainty, coupled with fears of being “recommended” or forced to leave campus, has deterred C. from seeking further mental health treatment at Yale. She still feels the paranoia of “being watched” by Yale Health and her residential college administration—the anxiety of everyone knowing her private medical information, though she only disclosed it to one provider.
The lack of transparency has not prevented her from communicating to her dean and providers when she experienced much more severe crises, but made her lose trust in all mental health services’ ability to protect her information.
Kim and C. demand more transparency to who is currently able to access medical information at Yale Health. Beyond that, however, they ultimately hope for more privacy enforcements on medical data.
Johanson recognizes the precedent Elis for Rachael set for effective student activism. He continues to believe that beyond its bureaucratic inaction, Yale
cares. The Dean’s Office and MHC, for one, cared enough to not let the lawsuit drag on and continue to delay changes.
“Are they only [making changes] because they know somebody is paying attention? I don’t think so. They do seem genuine and sincere, and, as I said, it certainly wouldn’t have happened in under a year,” said Johanson. “Yale finally decided: they wanted to do something.”
He cautions that the campus must continue to pay attention to current issues for student voices to be heard. Otherwise, Yale’s opaque decision-making processes will retreat into dormancy again.
Monks highlights that student perspectives may be the most valuable resource for administrative change.
Kim, now pursuing a joint master’s in public policy at Yale, remains optimistic that the university will listen, as long as students raise their voices.
“My hope is that Yale is prepared to educate and nurture a population of students that face these mental health issues without being discriminatory and without placing stigma,” said Kim, “Ultimately, I want to believe that Yale would like to change in the direction that its student body wants it too.” ∎
Kelly Kong is a first-year in Morse College.
We rode bikes up to the reservoir in the afternoon. Dad crouched at the water molding pink clumps of PowerBait onto his hook while I foraged for Indian paintbrush up the wooded hill. I must have suckled on forty of those sweet stems by the time his line caught and he called to me from the end of the old pier. Still halfsick from the nectar, I tucked a final morsel behind my ear and rushed down the slope
It’s not pulling so hard yet, he said. You hold it.
I clutched it low, by my waist with my knees bent, like he’d taught me. The pressure of the taut line rippled up the rod and across my fingers.
The jolt came violently. He cast his arm across my chest and tore the rod from my hands. Leaning, straining, grunting—he fought with his entire face furrowed toward a point on the bridge of his nose. He shouted to grab the net, but not at me, for in the same moment he snatched it and dove to the deck.
The silver and lenticular fish that he pulled from the water seemed impossibly large as it flailed in the net. It kicked into the air and fell to his feet, flapping across
the dock. I remember the sound most— scale on skin on damp wood. Slap of flesh and squelch of fat. Every squeaking slip followed by some mumbled curse. His panting flooded my ears.
There was a final burst of percussion before the combined energy of the wres tlers drained through the slat gaps. Four limbs and a tail descended gratefully to the pier to rest. There he lay, his beerbloat heaving, his neck soaked in sweat and water both.
I peeled the green-white stem from its sticking place behind my ear and considered who needed it most: Dad or the fish.∎
––Ren Topping





By Michelle So
As I sat performing my lab titration, I enviously eyed the other students around me. They appeared calm. They had not run up three flights of stairs. They had not panted tardy apologies to the teaching fellow. When class ended, they’d search the hallways for gleaming metallic bodies—skateboards, bikes, scooters. In a flash, they mounted. Outside, while I lingered at the crosswalk, my classmates zipped past me. By the time the light turned green, they were long gone. I began to consider an alternate universe in which I owned a scooter. The more I thought about it, the more I revelled in it.

leaving its rider “totally cut up” on asphalt. Annie’s roommate (with whom she shares the scooter) once tumbled forward over the handlebars, subsequently “making out with the pavement.”
Warned by Annie’s tales but undeterred, I was determined to get to the bottom of this scooter phenomenon at Yale the only way I could—by getting a scooter myself.
In the foreword of the 1961 children’s handbook Scooters! by Michael and Eric Dregni, Robert Ammon explains that documenting the history of the motorscooter was “a difficult and often thankless task. Difficult not so much because the threads in the web of history are lost in the mists of golden time, but more often because no one gives a hoot.”
disparity between the “three thousand-pound metal cages” and pedestrians has become an abhorrent inequality.
To Kyle, scooters have the potential to “fill this weird third gap.” “Well, I don’t want to run to class, but I don’t feel safe riding my bike on the street,” he explained. “I can’t ride my bike on the sidewalk because it’s impractical and also illegal.”
Yet Kyle still expressed strong reservations about scooters. “There is no way to look dignified on a scooter. Like, you see people on a bike, they just got class, right? There’s just no way to, like, just scoot along and look cool on a scooter.”
Sheepishly, I thanked him for his time and made my way back to my dorm. III.
TScooters are everywhere at Yale. I have seen six-foot-plus basketball players and chemistry students alike coasting along on them. In 2023, Yale Facilities banned electric scooters, among other electronic micro-mobility devices, citing risk of lithium-ion battery fires. But with e-scooters formally banned, kick scooters still remain our college’s guilt-free, childish pleasure. Popular among athletes, these vehicles allow hurried Yale students to race down the sloping New Haven streets.
Jackson St. Aubyn ’27, an offensive lineman on Yale’s football team, explained that wheeled vehicles are enticing to him and his teammates after a long practice. “My legs were just always so tired. I just didn’t want to walk up Science Hill or all my classes, I was just always sore,” he said.
“Obviously, scooters are for athletes,” kick scooter-owner Annie Chian ’28 insisted. Annie is not a college athlete, but touted the Yale stereotype: “I only take my scooter to [rock] climbing practice…because it’s the one commitment I have in my life that makes me feel like an athlete.” She recalled scooting to climbing practice once with a friend, who happened to have the same make and model. A pas de deux of scooters, she called it.
Still, scootering is a fraught sport: Annie had cautionary tales of a friend’s scooter breaking into pieces mid-street,
Eighty years later, in search of a human-powered vehicle expert to field my questions, I visited the Benjamin Franklin College Justa Sanchez Bike Shop, run by both paid college aides and student volunteers (bikes and scooters are, after all, anatomically and practically second cousins).
That day, the shop was manned by Benjamin Franklin College Fellow Kyle Sirianno, who previously worked as a refrigerant specialist for the Yale Health and Safety Department. He wore a mechanic’s apron and ambled around in clip-on cycling shoes, throwing out words like “axel,” “thread body,” and “dropouts.” Kyle spoke nostalgically of the cyclist-friendly 50s and 60s (an era he was, unfortunately, unable to witness himself on account of not being alive) and the injustices of our car-centric society.
“There is one feud, and it’s between people moving themselves through shared spaces … and cars,” says Kyle. According to him, the David-and-Goliath-esque
here was another hurdle I needed to surpass before getting on the scooter: breaking the news to my parents.
At 8 years old, I was a devoted backyard scooterist. I rode my red-rimmed Razor in my tiny Los Angeles backyard. It wasn’t much fun, going in circles and feeling my spine rattle over uneven tiles. I tried skating down the slanted driveway for a smoother ride, but I would end up speeding by too fast for my parents to feel secure.
Eventually, I outgrew the red Razor scooter and retired it to the unofficial “junk” corner of the yard. Color fading, wheels rusting, and the foam handles hardening and cracking, it disappeared from my memory.
When I called up my father one Sunday morning to ask what he thought about scooters, his grimace was unmistakable. “Well…” I said slowly, “I’m thinking of getting one. It’s purely for research. For an article I’m writing. About scooters.”
“What’s wrong with walking?” My mother poked her head into the frame.



They grilled me for the next half hour: What about momentum? Energy conservation? How much faster is it, really?
My parents, in agreement, are an unarguable, unbreakable force. There was no use pleading for parental permission. I have to run, I told them. Before I hung up, my mom warned me to watch out for the road—it’s always lup lup dup dup, Cantonese for lumpy-bumpy.
I mulled over it some more. My mom’s concerns were not unfounded. In New Haven, there have been a handful of fatal accidents involving scooters, including a 2023 incident involving a University of New Haven graduate student and another two-scooter collision in 2024, resulting in the death of one rider.
The next day, I received a WhatsApp message from my mom. The article link: “Cal Student still critical after crash, GoFundMe underway.” Her caption: “Wear a helmet!”
In january, i discovered that an acquaintance was offering her scooter for forty-five dollars—a steal!
We met up for lunch. Emily Chang ’28 held the folded scooter as we sat at the end of a long table. It had red wheels the diameter of large cookies and was emblazoned with the Razor logo. She explained that her first semester schedule had only a fifteen-minute slot for a twenty-minute walk. Determined to arrive at class on time, she invested in a Walmart scooter. The scooter cost roughly eighty dollars. However, between Emily and her roommate, the scooter was brought out a mere total of five times that semester.
“I’m having second thoughts about buying it,” I confessed, stirring my soup. I decided on an arrangement: I would pay her fifteen dollars upfront to use
the vehicle for one week. If I changed my mind, I would return it; if I fell in love with life on two wheels, I would pay the remaining thirty. We shook on our deal, and I walked out holding the brand new scooter.
That day, under a winter sun, I took note of my first ride across Yale’s stonetiled paths.
The rocky floor jolted me about. Passersby blurred. My bangs floated like a mane around my cold-rouged cheeks. Icy gales forced my fingers into a raptorial grasp around the handlebars.
I’ve joined the club, I whispered into the wind.
A woman immersed in her phone suddenly swerved into my trajectory.
“On your left!” I screamed.
In the days following, I felt brazenly aware of my surroundings. My senses were heightened and my perceptions piqued. Minor inclines elicited sweat, while fractionally downward tilts made rides feel joyously carefree.
Yet, there were drawbacks. Maneuvering through doorways and tight corners was a debacle. The act of scooting itself was, to my chagrin, less effortless than certain athletes made it seem. I’m rather short, and kicking off the ground required substantial effort. Rather than the serendipitous gliding I envisioned myself undertaking, scooting more resembles a constant one-legged pistol squat.
I eventually met my tipping point when I fell off my ride in the middle of College Street. The front wheel got stuck in a rut, and the rest of me, carried by forward momentum, continued forward onto the asphalt. A single passerby stopped and asked if I needed help. Slightly embarrassed and still in shock, I exhaled, “Fine!” and carried my scooter away.
The incident barely drew blood, but I decided one instance of public humiliation

was more than enough. I messaged Emily that I was ready to return the scooter. That evening, I parked the salt-studded, slightly scratched-up scooter into the Timothy Dwight bike rack.
But, as Greek tragedies go, fate was determined to drag me through further trials. The scooter disappeared. Stolen, more precisely. My initial shock gave way to anger, then a hopeless irony. I had heard of the notorious Yale bike thieves; never would I have imagined a person so petty as to steal a used scooter.
I explained the situation and paid Emily back thirty dollars.
If anything, I’ve learned that being on two wheels is an exercise in humility. I’m short forty-five dollars and limping with a bull’s-eye-shaped bruise on each knee. I hope whoever is now in possession of the scooter will feel as keenly aware of their surroundings as I did. To some bitter end, I hope they, too, encounter a rut in the road. While my days of scootering have ceased, I still treasure the fractional joys afforded by minutes saved: finding myself higher in the coffee shop queue, texting a lunch date “I’ll wait for you in the common room,” or matching the speed of a low-flying bird. My world grew larger as the time spent commuting grew shorter.
Oh wheels… I miss them. Perhaps I’ll pay Kyle another visit. This time, for a bike.
Michelle So is a first-year in Timothy Dwight College.


48 Idyllic garden 51 Anti-burglary device
53 Actress Lucy of “Kill Bill”
55 Like some home projects
TEDx event
Common default font 17 Very, very
White House figure 20 “Hasta la vista!”
23 Exhibit bias
24 Slip up
25 Barrier in badminton
26 Small recess
28 Athletics broadcast network
30 Japanese truck manufacturer
32 In need of turning in
35 Event where many clowns work
37 Offer one’s two cents
39 Wilson Contreras or Brendan Donovan
43 Goes wild
44 Befuddle
45 Date night purchase
46 Troubles
57 Source of hydroelectric power
59 Premium subscription with streaming access
62 Love, in the Louvre
64 Small gears
65 Wanes
66 “On the contrary!”
67 Dramatic serial, for short
68 Fashion magazine with a palindromic name
69 Extremely pale
70 –Cat 71 Small payments
British fellow 2 “Present.” 3 Glowing beams 4 Start over at the end 5 Chihuahua, e.g. 6 They hold ponytails


7 Ye Shoppe 8 Subway guide 9 Like Prime Minister Leo Varadkar 10 Networking site 11 Arriving after the bell
12 None too speedy
15 “Sad” figure in a meme
21 Southwest burger chain
22 Gecko or anole
from Flaticon.com. ANSWER TO PREVIOUS (FEBRUARY) PUZZLE
27 Get cozy, maybe
29 Push forward
31 Location of neighborhoods like WeHo and Boyle Heights
40 Prefix with -ceratops
41 Lime-green lepidopteran with vestigial mouthparts
42 “Redbull gives you wings”, for one 47 Some Apple computers 49 Dispensary purchase 50 Graceful and flexible
52 Hank of baseball fame
54 It may be sought on Pinterest
56 Affirmatives
33 Country with the largest exclave in the world 34 It’s called unagi in sushi restaurants 36 Win over with charm 38 Contended (with) 39 Do some needlework
57 SNL alum Carvey
58 “Famous” figure in cookies
60 Chaotic situations
61 Some Apple computers
63 Take advantage of

The New Journal was founded in 1967, under the following mission statement: “This university has once again reached that stage in history when people are talking about the New Yale, presumably to be distinguished from the Old Yale, which in its own day was presumably considered new. Wishing to share in this modernity, we have chosen The New Journal as the name for our publication. Besides, things seemed slow around here.”
Today, The New Journal is published five times during the academic year by The New Journal at Yale, Inc. One thousand copies of each issue are distributed free to members of the Yale and New Haven community. The New Journal is printed by TCI Press, Seekonk, Massachusetts; bookkeeping and billing services are provided by Colman Bookkeeping of New Haven. Office Address: P.O. Box 3311, New Haven, CT 06515.
While this magazine is published by Yale College students, Yale University is not responsible for its contents. All contents Copyright ©2024 by The New Journal at Yale, Inc. All rights reserved. Reproduction either in whole or in part without written permission of the editors in chief is
Recycle

