

The mobile edge
Acredia boosts access to information and care
Foxtel’s intuitive Business iQ

Published by:
Positive Impact Media Pty Ltd
ABN 51 063 279 630
41 Bridge Road, Glebe NSW 2037 Australia Ph: 02 9660 2113 Fax: 02 9660 4419 www.intermedia.com.au
Managing Director & Group Publisher: Simon Grover
Editor: Natasha Egan
Journalist: Katarina Lloyd Jones
Freelance Journalist: Jodie Wolf
Advertising & Marketing Manager: Mark Ryu
Graphic Designer: Leanne Hogbin
Production Manager: Jacqui Cooper
Subscriptions: subscriptions@intermedia.com.au ph 1800 651 422
To a successful transition

As the countdown to the new Aged Care Act reaches its final stretch, I welcome you to the Spring 2025 edition of Australian Ageing Agenda
To help with final preparations ahead of the 1 November start date, we have put together a page of transition resources with links (page 36).
This edition also includes details about a new set of quality indicators that support the safer use of medications and compliance with the incoming strengthened quality standards (page 44).
There’s also the latest advice on key sector challenges including worker retention (page 24) and financial performance (page 22).
Elsewhere, we report on a co-designed toolkit that helps providers measure the needs and values of older Aboriginal and Torres Strait Islander people in their care (page 30) and new work underway to help residential aged care providers deliver positive practices for older LGBTIQ+ Australians (page 34).
On one of the newer directions in aged care – a stronger reablement focus – we’re proud to share stories from the successful inaugural Positive Ageing Summit. The May 2025 event drew 250 passionate individuals to Adelaide to explore a holistic approach to better ageing (page 38).
We’re excited to share the conference is returning to the Adelaide Hilton in 2026 and will take place on 20-21 May 2026 for another event showing how allied health can drive better outcomes for older Australians.
In the meantime, we hope you enjoy this edition, and most of all, we wish all aged care providers and professionals success for the transition to the new Act.
permission of the publishers.
Disclaimer: This publication is published by Positive Impact Media Pty Ltd (the “Publisher”). Materials in this publication have been created by a variety of different entities and, to the extent permitted by law, the Publisher accepts no liability for materials created by others. All materials should be considered protected by Australian and international intellectual property laws. Unless you are authorised by law or the copyright owner to do so, you may not copy any of the materials. The mention of a product or service, person or company in this publication does not indicate the Publisher’s endorsement. The views expressed in this publication do not necessarily represent the opinion of the Publisher, its agents, company officers or employees. Any use of the information contained in this publication is at the sole risk of the person using that information. The user should make independent enquiries as to the accuracy of the information before relying on that information. All express or implied terms, conditions, warranties, statements, assurances and representations in relation to the Publisher, its publications and its services are expressly excluded save for those conditions and warranties which must be implied under the laws of any State of Australia or the provisions of Division 2 of Part V of the Trade Practices Act 1974 and any statutory modification or re-enactment thereof. To the extent permitted by law, the Publisher will not be liable for any damages including special, exemplary, punitive or consequential damages (including but not limited to economic loss or loss of profit or revenue or loss of opportunity) or indirect loss or damage of any kind arising in contract, tort or otherwise, even if advised of the possibility of such loss of profits or damages. While we use our best endeavours to ensure accuracy of the materials we create, to the extent permitted by law, the Publisher excludes all liability for loss resulting from any inaccuracies or false or misleading statements that may appear in this publication. Copyright © 2025 – The Intermedia Group Pty Ltd.
Environmental statement: The Intermedia Group takes its Corporate and Social Responsibilities seriously and is committed to reducing its impact on the environment. We continuously strive to improve our environmental performance and to initiate additional CSR based projects and activities. As part of our company policy we ensure that the products and services used in the manufacture of this magazine are sourced from environmentally responsible suppliers. This magazine has been printed on paper produced from sustainably sourced wood and pulp fibre and is accredited under PEFC chain of custody. PEFC certified wood and paper products come from environmentally appropriate, socially beneficial and economically viable management of forests.
Until next time, Natasha Egan
Editor
Tel: 02 8586 6132
Email: negan@intermedia.com.au





Katarina Lloyd Jones Journalist
Jodie Wolf Freelance Journalist
Mark Ryu National Advertising & Marketing Manager









“Fabulous day, discussions, networking and sharing evidence best practices.” Kate Weger comments on LinkedIn on the summary of day 1 of the Positive Ageing Summit
“Sick of the whole focus being on home care packages when there are hundreds of thousands of people under CHSP and hundreds getting assessed every day for the program and there are no services that can be accessed. We’ve got another minimum three years to go of it and probably longer if the start of SaH is any indication. Everyone who has a home support assessment wants lawn mowing and garden care. Completely inequitable that HCP clients get all that done for nothing.”
Margaret Norden comments on AAA on aged care Minister Sam Rae’s assertion of no more Act delays

iStockphoto.com/hxdbzxy and engagement
Australian Ageing Agenda. We know it is a foundational element of safeguarding older people and, by promoting strong and positive cultures, we encourage people into the sector and to remain here doing society’s important work.”
Jenni Hutchins comments on LinkedIn on AAA’s news wrap
“Interesting insights. The gap between retirement living and aged care is getting smaller and it’s good to see allied health getting the attention it deserves. Helping older residents stay well and independent really makes all the difference.”
Anna Bennet comments on LinkedIn on StewartBrown’s first survey of retirement villages


iStockphoto.com/miniseries

incredible passion matched with a depth of sector knowledge.”
Bree-Danielle Wyatt comments on LinkedIn on Shannon Sanderson’s move to Ageing Australia

“Feels a disappointing response from the Prime Minister. He literally has in his hands the ability to change the future path of aged care and our ability to meet the increasing demand that is coming over the next few decades. It is looking like he isn’t taking on board the significance of this time for the aged care industry.” Jeannie-Marie Noyce comments on LinkedIn on news of no more dedicated aged care minister in cabinet

“There have been mixed reactions for sure, with some clients certainly needing aspects of the Act in place for the new Home Care Packages. Others will use the time to embed new processes and get better prepared. As a technology provider, it’s all about readiness and supporting these pivotal changes through change management and training.”
Trevor Carlsson comments on LinkedIn on sector reactions to delays to the new Aged Care Act

Senate inquiry into delayed home care agreed to


Symondson discusses sector’s burning issues
Final draft of rules released
They said it

“People of course want to live within 5 kilometres of where they’ve lived and loved all their lives. So we’re going to see more vertical villages crop up in inner-city locations closer to hospitals and GPs, delivering incredible efficiencies for governments.” Daniel Gannon, Retirement Living Council


“We have to create a climate where existing providers will continue to invest in the sector and new equity will come Grant Corderoy, StewartBrown


“We are not consumers. Hear what I’m saying: do not use the word consumers. Aged care is not a marketplace; we are not pigs going to market… We are participants in our own aged care. We deserve that respect. Please don’t use the word consumers.” Dementia advocate Gwenda Darling
“Leaders surrounded by ethical norms are more inclined to listen to diverse perspectives, call out questionable behaviour, and prioritise people over profit or politics. The result? Better decisions that are not only effective but just.”
Dr Kate Robinson, CommuniKate Consulting
Call for submissions
The next issue of Australian Ageing Agenda (Summer 2025) includes a special focus on operations including workforce and hospitality for residential and home aged care services under the new Aged Care Act. Topics on the agenda include:
• workforce recruitment, retention and management
• staff education and professional development
• food, nutrition and dining
• hygiene, cleaning and laundry
• additional hospitality and hotel services. Get in touch if you have something to share: editorial@australianageingagenda.com.au

iStockphoto.com/Jacob Wackerhausen
DIARY
26 September
Nominations to join the Council of Elders in 2026 close 1 November
The new Aged Care Act comes into effect, including the new Support at Home program and Aged Care Rules
14 providers win grants
BY KATARINA LLOYD JONES
OVER THE next 12 months, 14 residential and home aged care providers are coming together for Aged Care Research & Industry Innovation Australia’s $2 million flagship projects. Participants receive grants up to $120,000 with 1:1 matched co-contributions.
Among them, Lifeview’s aged care home Willow Wood will be a part of Flagship Project 2, which focuses on empowering data literacy and capability to drive quality care. The other seven recipients include:
• Alwyndor Aged Care, SA
• Bolton Clarke Home and Community Support, east Melbourne
• Elderbloom Community Care Centres WA
• Fronditha Care St Albans, Vic
• Glow Health Care Australia, Sydney and regional NSW
• Regents Garden Scarborough, WA
• Warrigal Wollongong.
Flagship Project 1 looks at workforce pressures related to staff burnout, retention and limited career growth. The six recipients include:
• Australian Unity St Patrick’s Green, NSW
• Benetas St Georges, Vic
• integratedliving Australia’s home care services, NSW far north coast
• Beaumont Care Kippa-Ring, Qld
• Feros Care home care, Gold Coast
• Life Without Barriers home care, Darling Downs, Qld.
ARIIA CEO Reuben Jacob tells AAA that grant recipients will participate in a model of “co-ompetition”, where they collaborate and compete to implement innovative, evidence-based solutions that address sector challenges.
Department releases rules
BY KATARINA LLOYD JONES
THE DEPARTMENT
of Health, Disability and Ageing released the Aged Care Rules 2025 on 31 July – the final draft of the supporting legislation for the new Aged Care Act. The release aligned with the three-month lead time peak body Ageing Australia called for.
The 649-page document provides details on how the new Act will work and follows several consultation drafts and over 400 submissions from aged care providers, advocates, workers, carers, healthcare experts and older people.
Some of the updates include allied health professionals now being referred to as practitioners and the removal of hourly caps on house cleaning and gardening services.
It was clarified that the allied health professionals on the aged care service list is not an exhaustive list of Assistive Technology and Home Modifications prescribers.
Upon its release, Minister for Aged
Care and Seniors Sam Rae called it “another meaningful step towards a new rights-based Aged Care Act that delivers the dignified care older Australians deserve.”
Ageing Australia general manager of policy and advocacy Roald Versteeg says they welcome the release of the final draft. But he acknowledged that final requirements are still needed as soon as possible to “support sensible transition.”
“Plenty of work remains upgrading computer systems and training staff ahead of November, but at least the way forward is now clearer,” he adds.
The final rules are subject to passage and Royal Assent of the amending legislation currently before the Australian Parliament. At the time of going to press, the legislation had not yet been passed.
Once passed, the rules will be considered by the Minister for Aged Care and Seniors, and come into effect after he signs the document and it is published on the Federal Register of Legislation.
Acquisition season for sector
BY KATARINA LLOYD JONES
IT HAS BEEN
the sector, with a flurry of mergers and acquisitions taking place, particularly in regional Australia.
August saw BaptistCare acquire Sunrise Supported Living’s Tuncurry retirement village and home care services on the mid-north coast of New South Wales and Whiddon add a second home in Maclean, northern NSW, with the acquisition of Mareeba Aged Care.
Meanwhile, Regis Aged Care purchased four new homes from Rockpool, Quirindi Care Services joined specialist regional aged care provider Apollo Care, mecwacare acquired the Allanvale Private Nursing Home, and Australian Unity acquired national allied health outfit Plena Healthcare.

acquisition of Amana Living’s Kalgoorlie services in March. Combined, Respect has boosted its portfolio by 12 homes in 2025 alone, and now operates a total of 39 aged care homes and over 700 retirement living units.
But Respect has been the busiest, acquiring Chaffey Aged Care in Merbein in rural Victoria alongside three aged care homes and three retirement villages from NVC Group on the mid-north coast of NSW within a week of each other.
This follows Respect’s takeover of seven BlueCare aged care homes in May and the
Respect chief executive officer and managing director Jason Binder tells Australian Ageing Agenda they have the scale to sustainably deliver regional aged care and keep residents at the centre of its vision.
“Our approach is about strengthening what already works and ensuring longterm viability,” says Binder.
Switch for a safer dose
BESTMED medication management integrates with more software partners across home, NDIS and residential aged care, so you spend less time on data stoppages. Whatever your organisations journey, we have the right connections for safer, easier and better care.

Industry movements
De Zilwa retires ahead of Annecto closure
After five years as CEO of not-for-profit aged and disability care Annecto, and 25 years in leadership positions in the sector Cheryl De Zilwa retired in late April. In June, Annecto announced it would cease operations from July 2025, due to financial challenges and shifts in service models.
Sanderson moves to Ageing Australia
Shannon Sanderson has moved from aged care consultancy and data company Mirus Australia to Ageing Australia as the state manager for South Australia. Sanderson tells AAA she is “very excited” to be working with providers in her home state during this time of change.

Thomas appointed interim CEO
Kearns to lead Find a Carer

Brad Kearns, whose experience spans military, police, health and aged care innovation, and workforce transformation, has begun as CEO of care marketplace Find a Carer. He recently held leadership roles at Uniting NSW.ACT, which acquired Find a Carer in 2024. He replaces Zubin Appoo who departed in June.
Laidlaw joins ECH

BlueCare group executive aged care and community services Cathy Thomas has begun as interim CEO of UnitingCare Queensland. She replaces Craig Barke who announced in March he was stepping down. The not-for-profit says Thomas’ history on the executive leadership team since 2016 and leadership roles at BlueCare make her wellpositioned to lead through the transitionary period.
Filsell, McGovern join Bene

Richard Laidlaw has started as head of people and culture at South Australian retirement living and home care provider ECH, where he will drive workforce engagement. A Churchill Fellow and a fellow of the Australian Human Resources Institute, Laidlaw says he is looking forward to applying his passion for technologyenabled innovation.
New roles for Gallagher and Reid


Michael Filsell and Catherine McGovern have joined Bene Aged Care as COO and manager of quality and clinical governance respectively. The pair say they are committed to enhancing operational capability and clinical governance at the South Australian provider.
Finance exec changes at Resthaven

Rob Quinton commenced as chief financial officer at South Australian aged care provider Resthaven Previously, Quinton was the general manager of finance at National Pharmacies. His appointment follows the retirement of executive manager finance and technology

resigned from IRT in May before commencing as COO at Uniting

Lavell named Odyssey CEO
Former director Aaron Lavell has begun as CEO of Odyssey Lifestyle Care Communities. Former CEO Phil Usher will step into an active founder role. Lavell tells AAA he is excited to move to a more hands-on role but does not underestimate the challenges.

Bradley joins ACH Group
Experienced company director has joined the ACH Group board after supporting the South Australian provider as an independent advisor for two years. Bradley says she is looking forward to contributing to ACH Group’s continued commitment to delivering high quality care.

Kara steps down from CHA
After less than two years as CEO of Catholic Health Australia, Jason Kara has departed the peak body. Leadership and culture Kathy Hilyard is interim CEO and recruitment for Kara’s permanent replacement has begun.
New
CEO for integratedliving



Experienced aged care executive Nick O’Callaghan has started as CEO of integratedliving Australia. O’Callaghan was previously executive general manager of home care at Australian Unity and interim CEO at myHomecare Group. He replaces Catherine Daley who left in July 2024 after 21 years with the home care provider.

Catherine McGovern
Michael Filsell
Cathy Thomas
David Norton
Shannon Sanderson
Cheryl De Zilwa
Robina Bradley
Brad Kearns
Richard Laidlaw
Patrick Reid Ross Gallagher
Aaron Lavell
Jason Kara
Nick O’Callaghan
Release of home care packages must be front-loaded
Do you think the Senate inquiry into home care delays, due to report in midSeptember, can be effective in getting packages released ahead of 1 November?
WE HAVE to continue to try and get packages released regardless of the inquiry. The other challenge we have is making sure that the very significant number of additional packages that the government committed to are released closer to 1 November rather than further from it.
Instead of over 12 months?
They will be released over 12 months, and they’ll have to be because the sector couldn’t just ramp up its capacity in one day. But we would suggest they should be front-loaded.
We would suggest that
because we’re now four months behind – because instead of coming in on 1 July, they’re coming in on 1 November –you should be making up for the fact that we’ve already lost four months by releasing more at the front end than at the back end of the year.
What capacity do providers have to be able to take on more packages?
There are definitely providers that can’t, and there are parts of the country where because of the staffing issues, it would be very hard to ramp up. But we have lots of members telling us, if packages were released, they could deliver them.

Tom Symondson, chief executive officer of Ageing
Is this normally in metropolitan areas? It’s often metro, but also regional. Where it’s more difficult is rural and remote. But in a lot of regional areas, we’ve got incredible shortages of residential beds because it’s so difficult to get them built, but we have flourishing home
If they released 100,000 packages in one day, many of them would not be able to be delivered. It will take time, but you can’t start until you start. We can’t just do it in the hopes that packages
The reason they can’t just switch it on, which is why we need to know how many packages will be released and when even after 1 November, is because you can’t hire the staff your staff so that you’re going to be able to respond to that need. I talk to members all the time who say, I can absolutely increase my ability to deliver home care.
We have to know that they will appear. We have to know when, and we have to know of what value and how many people are likely to be knocking on our doors. ●
As told to Natasha Egan on 6 August
Consumer advisory bodies: love them or hate them?
WE HEAR A range of opinions from older people and providers.
Some older people are thrilled to be involved and feel they help contribute to improved services. Some older people find the meetings pointless, providing feedback that seemingly goes nowhere.
Some providers are running them well and finding enormous value in being better connected and more able to engage with participants, residents and their supporters, resulting in improved services.
Others tell COTA Australia they find the consumer advisory bodies of limited value and not useful – simply a tickthe-box compliance process.

“But it isn’t always easy to do engagement well.”
effective engagement these bodies won’t deliver the voice older people are striving to have heard and providers won’t get the input they need from their participants. COTA Australia wants to work with providers to ensure these bodies are effective for participants and organisations.
the Department of Health, Disability and Ageing, designed to ensure the voices and views of older people on the services they receive are heard and respected.
They were born from the Royal Commission into Aged Care Quality and Safety recommendation to ensure and strengthen positive consumer experiences and to provide valuable feedback to
the governing bodies. In short, consumer advisory bodies aim to give aged care participants and residents a voice and a platform.
That’s why they are critical. But it isn’t always easy to do engagement well. Without
We know that for the consumer advisory bodies to be successful, there needs to be: an effective framework and support for participants skilled and supported staff, so they can empower the participants without inadvertently leading or exerting influence on deliberations
• alignment between individual and organisational aims and outcomes
• clear and direct reporting to the governing body.
We are commencing a project, with support from
To do this, we need to support aged care providers to run effective, engaged and active consumer advisory bodies. We want to build understanding and implementation of positive consumer engagement, and through this, develop resources, tools and support to ensure success.
Hopefully, the next time we talk about advisory bodies all older people and providers involved will be able to say, “we love them” because they are all operating in the way they were intended. As a result, voices are raised, heard and acted upon with improved services, responsive to the needs of those they serve.
Email cota@cota.org.au to find out more about our Consumer Advisory Project. ●
Australia
Patricia Sparrow, chief executive of COTA Australia
Cross-sector collaboration drives better outcomes for community transport
WE UNDERSTAND the value of diversity within organisations – there’s plenty of research that proves this. It brings about enhanced and accelerated change for better outcomes. It delivers far more than a single perspective can.
Recently, during research for the National Community Transport Pricing Model – NCTPM – I witnessed firsthand the benefits of diversity in relation to having all key stakeholders on the one page, working together.
The NCTPM included the Australian Community Transport Association as the peak body working with providers, the Department of Health, Disability and Ageing, and the University of South

Australia, which has overseen the analysis.
The working group involved more than 30 community transport providers, as well as subject matter experts and end-user advocates. All parties worked efficiently, with
everyone engaged, problemsolving and respectful of one another’s position.
Regular updates were received with an openness and a willingness to adapt.
Normally if left to one part of the sector, broad evidence can be missing, and peaks tend to walk the fine line between members and government.
In this case, with a unified approach, the department worked with ACTA to set agendas and talk directly through issues. Insights were gained around ministerial requirements and parameters, and the department learned more about the community transport sector directly from the people on the ground.
The research has resulted in the delivery of the first
Reforms not grounded in evidence will recycle more of the same
THE AUSTRALIAN Association of Gerontology reiterates its call for aged care reforms grounded in evidence, including continuous monitoring and evaluation.
The impact of these reforms should be transparent to all stakeholders to support policy development and ensure public accountability in delivering safe, high-quality funded aged care services to older people. Without this transparency, we risk cycling through repeated reviews, inquiries and policy adjustments.
This is particularly important because the current aged care reforms are not solely based on an evidence-based process. In a royal commission, evidence refers to what is presented to the commissioners, as in a court of law.
However, the commissioners were not required to verify the accuracy of claims made by witnesses, submissions, or
counsel assisting. Consequently, the Royal Commission into Aged Care Quality and Safety’s recommendations were influenced by a mix of opinion, experience, aspiration, and research, resulting in significant differences among commissioners in their final proposals.
Substantial changes have occurred since the royal commission, thanks to government investment aimed at enhancing policy and program evaluation, building capacity, and supporting thorough stakeholder consultations, including with older people and their carers. This progress is most welcome and vital for ensuring evidencebased reform implementation.
evidence-based findings on the actual cost of community transport, Australia-wide, and uncovered policies needed to make it participant-friendly and sustainable.
Of added value, however, not only did the NCTPM collect invaluable data that will direct the future of community transport, the process has become a testbed for how the sector can effectively work hand in hand with the department.
While the NCTPM study reveals a significant funding gap, it highlights a positive path forward. We experienced a powerful collaboration of expertise united by a shared goal, that continuously demonstrated the value of working together.
It’s time to do more of this. ●

However, many reforms originated from government processes and priorities established before the royal commission, leading some to question whether they fully
the clinical capacity of residential care – such as mandatory registered nurse and care staff minutes –are promising, workforce challenges persist across both aged care and health sectors. Given that older people
are the largest users of health services in Australia, shortages will inevitably impact the health and wellbeing of older people, regardless of whether they live in the community or residential care. These workforce shortages are most acutely felt in services that support some of our most vulnerable citizens, including those living in regional and remote communities.
Despite being presented with models showing how a shared health and aged care system could improve outcomes for older adults, communities, and providers, as well as offer systemic efficiencies, the commissioners did not explore these options.
As a sector, we must advocate more actively to ensure these concerns are negotiated in the next National Health Reform Agreement. ●

Anita Westera, president of the AAG
Murray Coates, chief executive officer of Australian Community Transport Association
Are we innovating aged care with intent?
Innovation is positive, but providers, policymakers and innovators must be purposeful with their endeavours, writes LACHIE GREEN.
Innovation in the aged care sector has created numerous positives for the sector, and for the recipients of aged care services. Four years on from the release of the royal commission’s final report, the work of sector stakeholders in identifying gaps and crafting new and exciting solutions should be celebrated.
Novel developments in the sector, particularly those that improve the delivery of personal and clinical care, promise to increase the quality of care and services available to older Australians.
Aged Care Research and Industry Innovation
Australia has reported on numerous successful projects, funded through their grant programs, that are promising to improve sector outcomes. These projects include interventions and strategies to support sleep quality and oral health, improve workforce resilience and retention, boost recognition of delirium, and more.

But personal and clinical care is not the totality of aged care’s function nor purpose, and this is not an uncritical song of praise for innovation. Rather, I’d like to pose a question. We talk of transforming the sector, but what is innovation transforming the sector into? Are we aware of the ideal end state we are working toward in aged care?
The aged care royal commission’s final report describes a “piecemeal approach to reform” that has problematically shaped the sector for decades. Reforms enacted in reaction to individual, discrete problems over many years tended to lack any systemic perspective, contributing to a sector that is, “complex and difficult to navigate.” Commissioners are firm that, “piecemeal adjustments and improvements have not achieved, and will not
sake will not necessarily contribute to a utopian aged care sector but may in fact undermine that goal.”
achieve, the change that is required to ensure high
Without a unifying vision of what aged care should look like, we risk emulating that process through a piecemeal approach to innovation. We risk a sector comprised of numerous shiny, novel developments stitched together to create a total product that we have not anticipated – a Frankenstein’s sector.
Robots in aged care: Robert Sparrow describes one such hypothetical future sector. He visits a hypothetical, high-tech, future aged care home and
Windows in the home are replaced with highresolution digital portals that can display any outlook. There are no people in the care home other than the residents. All care is provided by robots with operational and clinical support from a call centre.
Any visitation from family or friends is done through telepresence devices, allowing people to call directly into the resident’s room. The facility’s operations are effective and efficient. Although no person has visited the home in years, residents converse away with their robotic companions, and they seem happy.
Sparrow is clear in his opinion on such a future from the outset, including in the titular label of dystopia. While the residents of this hypothetical home may be outwardly experiencing some form of enjoyment, it is not uncommon that people adjust their preferences and desires to match a miserable circumstance. Sparrow states: “We need to be extremely careful about concluding that a person’s life is going well just because they are realising their desires.”
Lachie Green
© Lachie Green
Technological advancement may create psychological responses we identify as amusement or happiness, possibly even increase quantitative measures labelled quality of life. But in uncritically pursuing these objectives, we can risk curtailing innately human experiences offered in the delivery of care. Not to mention undercutting the social being of a person.
To Sparrow, the technologically dominated care home does not allow residents to be recognised and respected as human persons; without which, a good human life becomes unattainable.
Sparrow concludes: “While some older persons may well embrace the use of robots in particular roles, overemphasising this possibility risks rendering it a self-fulfilling prophecy, depriving those being cared for of valuable social recognition, and failing to provide respect for older persons by allowing the options available to them to be shaped by the design choices of others.”
So, is Sparrow’s science-fiction reality simply that? No.
The technology, for the most part, exists and is available now.
For example, as highlighted in these media and research articles:
augmented and virtual reality screens are increasingly available to immerse older people in the outside world
care robots are increasing in capacity and capabilities, and we are encouraged to embed them in care and, “not wait while our patients suffer”
mobile telepresence devices are increasingly backed by evidence, describing them as “enjoyable experiences” and promotors of social connectedness
So called social assistance robots are increasing in prevalence and are promoted as a way to address social isolation.
Let me reiterate: innovation is positive, and we should not settle for the status quo in the sector. But I encourage providers, policymakers and innovators to be purposeful with their innovation.
There are countless novel avenues of research and development to explore. Don’t go about that exploration haphazardly. There is no obligation to pursue every angle of innovation that arises, lest we unintentionally create dystopia.
I recommend utilising your organisation’s mission and vision statements as an ethical compass. Sketch your image of the aged care sector that you are seeking to create or contribute to and use that image to be discerning in your pursuit of innovation.
Each time we adopt a new innovative technology, model, practice or intervention, we are making an implicit statement: this is what we want the future to look like.
As we transform the sector, let us do so with intent and purpose. Innovation for innovation’s sake will not necessarily contribute to a utopian aged care sector but may in fact undermine that goal. Be purposeful in your transformation, seek to understand what you are transforming into.
What is the ideal you are aspiring to create or deliver? How does your pursuit of innovation factor into that end? ● Lachie Green is an independent consultant and researcher in aged care ethics and social strategy, who has a background as an aged care professional and is a doctoral candidate at Australian Catholic University


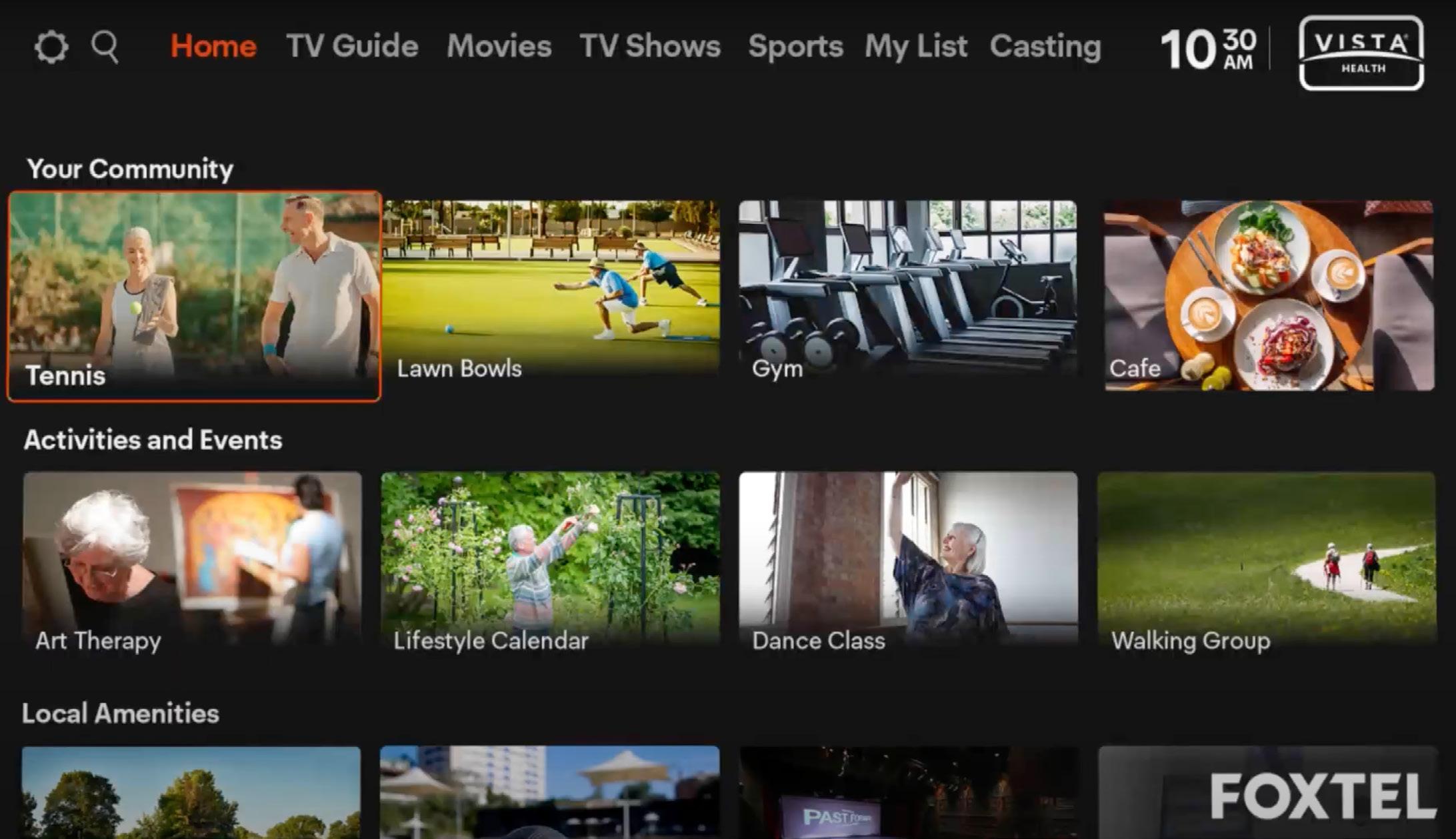
The mobile edge
Acredia’s mobile-first clinical software is transforming aged care delivery for residents and staff through interoperable technology and an openness to meet providers where they are.
The aged care sector in Australia is on the cusp of transformative reform. With the new Aged Care Act due to start on 1 November 2025, providers are reviewing systems to meet new compliance and personcentred care goals. In this evolving landscape, technology is a frontline enabler of better care outcomes.
A key driver of this transformation is mobile-first clinical software that gives frontline workers real-time tools to streamline operations, meet compliance, and spend more time with residents.
Among those doing just this is Acredia, a clinical management platform purpose-built for aged care. Founded in 2019 by health IT innovator Dr Charles Chang, Acredia is cloudbased, interoperable, configurable, and mobile-first.



A vision rooted in innovation Chang is no stranger to pioneering aged care technology. With a doctorate in IT, Chang has delivered innovations from PalmPilot-based care planning to early e-medication systems that made care easier to deliver and safer to document.

“Providers need a software partner that is across regulatory changes and responsive to their requirements,” he says. “No two providers are exactly the same. We don’t force a certain way of doing things upon them. We make our software highly configurable, simple to use, and easy for providers to
Acredia’s clinical management suite includes modules for CRM, HR, clinical care, quality, and maintenance, all integrated to eliminate silos and duplicative data entry. However, the standout feature is Care Direct – a Kate Billing
St Anna’s staff love the “ease of use to get the residents’ information”
(L to R:) Laxmi Ghimire, Jihu Wang, Athin Christou and CM Soithong
mobile app designed specifically for on-the-floor use by nurses and care workers.
Care where it happens
The Acredia Care Direct app turns any compatible smartphone into a point-of-care documentation and decision-making tool. Using NFC tags, QR codes or Bluetooth, staff can access profiles and record notes in real time. This reduces reliance on shared terminals and paper.
“Just because providers operate in a complex environment doesn’t mean their software should be complicated,” says Chang. “If anything, it should be the opposite.”
Care Direct supports AN-ACC reporting and quality tracking. Automation updates notes and follow-up tasks to ensure continuity.
Case
in point: Carinya Lodge
Carinya Lodge in the rural town of Korumburra in Victoria exemplifies the impact of mobile-first software. Carinya Lodge serves South Gippsland’s older adults with 60 aged care beds, 52 independent living units and 135 staff.
For over a decade, Carinya relied on a siloed legacy system. “If a resident had a fall, there were many different categories and buttons that we had to click on to initiate the incident and capture observations,” says Kate Billing, interim Co-CEO Clinical Services.

Attempts to use the mobile version failed due to its unreliability. Billing, who started as a clinical coordinator, knew frontline staff needed a system that worked with them, not against them.
After reviewing five platforms, Carinya selected Acredia. “Acredia stood out because it wasn’t just clinical software – it offered a complete system. We could reduce the number of platforms we were using,” Billing notes.
Implementation and impact
Transitioning to Acredia overhauled nearly all digital workflows. Despite the scale, staff embraced the change.
“They appreciated not having to compete for a computer at the end of their shift just to complete documentation,” says Billing. “Now I walk the floor and see staff talking with residents; not stuck behind a screen. That’s the biggest change – we’ve given time back to care.”
For one personal care assistant, the difference was stark. Previously staying late to finish notes, he now documents on the go and leaves on time without compromising care.
From a management perspective, the transformation has been equally significant. Dashboards show incidents, compliance and care activity as it occurs.
“If something happens on the floor, I see it instantly and can step in if needed,” says Billing. The system has also streamlined preparation of quality indicator reports, collating daily care data automatically.
Smart tags outside residents’ doors and the Acredia Care Direct app allow St Anna’s staff to get up-to-date information discretely
“No two providers are exactly the same.”
In addition to clinical benefits, Acredia’s app for residents and their relatives has enhanced family engagement – a priority for Carinya.
“When Acredia came along and the family app was included, we got very excited,” says Billing. “Families can see what meals residents had or what activity they attended. It makes phone calls and visits more meaningful.”
Living proof: St Anna’s
Another recent convert – St Anna’s Residential and Home Care – has seen these benefits at its 60-bed home in Brompton in Adelaide’s inner north since March.
The “ease of use to get the residents’ information” at the bedside and a system to complement other platforms were among the drawcards of Acredia, says Athin Christou, Manager of Wellness and Technology at St Anna’s.
“We started quite primitive here with our digital maturity and footprint and have quickly expanded and implemented a lot of different technologies,” he says.
The occupational therapist splits his time between managing allied health and technology, meaning he’s involved in both clinical and infrastructure elements of the rollout.
St Anna’s has gone with NFC tags because it is “easier and more cost-effective” for their situation, says Christou. Placed on residents’ doors, staff tap them to see and make notes about care.
“It’s quite impressive,” says St Anna’s Chief Executive Officer Amanda Birkin. “It’s just a tap and there’s the person’s care plan and care requirements.”
Christou echoes Billing’s comments about better documentation due to live information at the point of care and no lineups in nurses’ stations.

providing supervision, oversight, being present and having communication.”
It is also secure and discreet, adds Christou. Each staff member only accesses what they need; others see nothing.
He also highlights the single source of truth among key benefits for residents.
“It’s live, so if I change something on the system, a carer scanning to go into someone’s room is getting up-to-date information,” says Christou. “You’ve got a point of truth at your disposal in your hand.”
Customisation and support
Acredia’s configurability has also been key.
“Every aged care facility is different,” notes Billing. “We learned post-go-live how much we could tailor the system.”
Even during implementation challenges, Acredia’s support team was hands-on and responsive.
“Whenever something came up, I could submit a helpdesk ticket or speak directly with someone. It’s been a big process and continues to be – but absolutely worth it,” Billing says.
Acredia evolves with changing rules, says Birkin. “They will work with us to get it right.”
There’s no one-size-fits-all attitude, says Christou, who has customised forms to suit St Anna’s with Acredia’s support.
“Acredia is a custom fit to your organisation.”
Interoperability and scalability
Acredia is designed with modern integration in mind. Open APIs allow it to work with systems such as PainChek, Xero, and Epicor.
“We aim to be a strategic partner.”
the top attraction for St Anna’s because it addresses one of the provider’s biggest challenges.
“We want to move towards all of our providers working within one ecosystem so that the systems are talking to each other and we’re not having to double information,” says Christou.
By June, St Anna’s had completed one integration, was midway through another, with more to come.
“There’s a bit of work around that because you need to get the software providers chatting, but they’ve been openly working together.”
But the work is worth it, says Christou. He says the value of the already-completed integration involving the hospitality dietary and menu system is “huge,” including for risk mitigation.
“Now you’re not going into two different systems to try to find out a source of truth if they’re interlinked,” he says. “Food, clinical nutrition and hydration are linked so if a speech pathologist does an assessment and changes a directive, the system needs to be able to capture information and pull information so there’s one source of truth, and to mitigate those risks.”
It also supports kitchen operations because staff can know immediately what someone has ordered, for example, adds Birkin.
She says Acredia’s willingness to integrate is appreciated and important for St Anna’s.
“They’re open to allowing that integration so that it works for our business. That’s probably the important part because our business is not about software. Our business is about the care we’re delivering and the kitchen knows who’s in and who’s out for lunch, and how they have to alter the recipe.”
Staff at St Anna’s tap the doorbell tags to see and make notes about care
This culture ties in with Christou’s goals to build an ecosystem of systems that work together at St Anna’s.
“They recognise they’re good at what they do, and other people are good at what they do, and they’re allowing us to be creative and partner with the people that we want,” he says.
Christou points out that aged care is more than clinical and involves supporting residents’ whole life, which includes lifestyle, food and catering.
On how to reduce the risks, he says: “We can bring information to a centralised point.”
For Carinya Lodge, integration has improved data flow and reduced workarounds.
“Our next step is to expand internal communication by upgrading to enterprise mobile devices,” Billing adds, noting the current use of Oppo Android phones has already delivered strong results.
The platform is also scalable. With pricing accessible even to providers with fewer than 40 beds, Acredia is gaining traction across small and medium-sized organisations looking to modernise affordably.
Compliance without the chaos
As providers prepare for the Aged Care Act – with monthly care statements and stronger governance – Acredia positions itself as more than a vendor.
“We aim to be a strategic partner,” says Chang. “The new regulatory environment demands better data, faster insights, and clearer communication. Our job is to make that easier.”
Providers can generate and send statements with one click.
Care statements, email functions and the resident and family app are already in use or nearing rollout at St Anna’s. It is important to involve residents and families in the digital transformation, says Birkin.


“We are bringing our residents along for that technology ride with us,” she says. “The expectations of our residents now, even with the cohort that we have, is that they want access to that information straight away.”
As a result, Birkin says St Anna’s is educating them on smartphone use.
“That’s an important part of what Acredia does; opens it up for them as much as it does for us.”
Integration with My Health Record and streamlined quality reporting reduce spreadsheets and admin burden at St Anna’s, says Birkin.
“It’s not about replacing people,” she says, “it’s about being able to use that time to do other things.”
Looking ahead
With rising cyber risks, tighter reporting windows, and higher expectations, providers need tools that are functional and empowering.
Acredia’s mobile-first approach is proving to be exactly that. For providers like Carinya Lodge, the platform has transformed care delivery, communication, and resident connection.
“We’re very happy with the product. We wouldn’t be telling others to get on board if we weren’t,” says Billing. “Acredia has genuinely improved the quality of care we deliver.”
has also built a Higher Everyday Living Fee tab into Care Direct so staff can view items paid for and mark them as delivered.
This is a “very useful” feature that St Anna’s is looking forward to using in its implementation of HELF, says Birkin. “It gives you the reporting capacity to be able to do that. It’s another point of truth that is documented at the time.”
As the sector braces for its most significant reforms in decades, software like Acredia offers a path forward that is scalable and people centred.
Birkin adds it is nice to have a software vendor that listens to smaller providers.
“We are not a big, multi-site organisation but working with Acredia, we feel that we do have a voice in what we want.” ●
Acredia

StewartBrown senior partner Grant Corderoy told a packed auditorium at Ageing Australia’s state conference in Sydney in June about key numbers influencing the sector’s financial performance.
Among them is that Australians have the world’s fourthhighest life expectancy, making the growing elderly population an important factor in aged care’s sustainability.
“Today, we’ve got just over 200,000 permanent and respite people in residential aged care. In 2030 the demand will be 250,000. In 2040 it’s going to be 370,000 people,” Corderoy says.
Australia also has about 1,185,000 people receiving in-home care.
“That demand is going to go up to 1,275,000 in 2030 and 1.6 million people in 2040,” he says.
The biggest single challenge today for aged care, says Corderoy, is the new cohort entering soon – the baby boomers.
“Many of the baby boomers have wealth… predominantly from the family home.” And they’re tending to use that wealth, says Corderoy, a member of the generation.
Give them the services they need
Baby boomers, leaders and investability are crucial to the sector’s future, says Grant Corderoy. NATASHA EGAN reports.
The sector also must be viable, says Corderoy, but more than that, it needs to be investable.
Investability, he says, is a term stakeholders can expect to hear him use a lot over the coming years, and it is about having a sector that can maintain itself.
“Viability is the ability of an organisation to maintain its operations and generate services over time,” he says, likening it to business as usual.
“Investability is the quality of an organisation or an asset to be financially attractive and continue to be suitable for investment,” says Corderoy. “And not just new investments coming in. We want to attract investment from everyone who is involved with aged care. And therefore, to get an investment, we’ve got to encourage it to be attractive and viable.”
Making the sector investable was a key focus area for the Aged Care Taskforce, says Corderoy, a member of the group.
“We’ve got to be prepared to change our approach.”
“We travel more, we go to restaurants more, we change our vehicles more… But we are also in many ways more demanding,” he says.
“The cohort today are very much grateful for the service that we provide. In the future, the baby boomers are going to say we’re happy to pay for the service, but we want a particular service or style of accommodation that we think is appropriate for what we want to pay.
“Is the sector ready for that? That’s going to be the real challenge.”
Corderoy encourages providers to look to the evolution of other industries such as hotels.
“We’ve got to start to learn from other sectors… we’ve got to be prepared to change our approach, because the demand is coming.”
He also highlighted two key themes influencing future performance: leadership and investability.
Leadership is not just at the board, CEO or executive level, says Corderoy, but rather across all areas of aged care.
“Leadership is a line manager. Leadership is the people on the floor, the people who are face to face with those receiving care.”
It is important to learn how to embrace leadership, because it will improve financial performance and service delivery, he says.
“That’s the challenge that we’ve got to be looking at.”
StewartBrown spelled out the challenge the week after the conference in its Aged Care Financial Performance Survey Analysis Report for the nine months ending March 2025.
It listed the minimum return needed for investability as:
• average earnings before interest, taxes, depreciation and amortisation of $20,000-$22,000 per bed for residential
• 9.5 per cent return on home care revenue.
The March 2025 results show operating EBITDA averaged $8,067 per bed per annum, an improvement on March 2024
($7,222) but well below the target. Home care similarly fell short at 3.8 per cent.
For everyday living “we’re losing $6.60 per bed per day” and “$10.90 per bed per day on accommodation,” Corderoy told Ageing Australia delegates of the latest results.
“This doesn’t sound very investable to me, so this is what we’ve got to change, because at the moment, we’ve made a ‘massive’ return in March of 91 cents per bed per day surplus.”
Part of the solution lies with the incoming demand, he says.
“We’ve got to start to get that thinking around the baby boomers will pay. The challenge is we’ve got to give them the services that they need.” ●
Grant Corderoy addresses Ageing Australia delegates in Sydney
Setting a new standard
In times of uncertainty, people look to leaders for steadiness as well as answers, says DIANA
HORVATOVIC –
chief executive officer
of aged care and independent living provider St Basil’s NSW/ACT.
What are your priorities for the year ahead?
This year, the executive’s focus is on deepening the trust we’ve built with our residents, clients, families, and staff. We’ve worked hard to achieve full compliance across all our services, and now it’s about moving from meeting the standard to truly setting it. That means investing in workforce development, expanding our Euphoria home care program, and ensuring our residential homes continue to feel like vibrant, connected communities. We are also focused on building stronger partnerships across the aged care sector, because tackling the challenges we face requires collaboration and a shared vision for better care.
Where are St Basil’s NSW/ACT’s biggest challenges?
Like most providers, we’re navigating workforce shortages, rising operational costs, and the need to adapt quickly to regulatory change. One of our major challenges is also one of our biggest opportunities: ensuring we meet the needs of a new generation of older Australians who are more informed, have higher expectations, and want greater choice. Balancing personalised, high-quality care with financial sustainability in this environment requires creativity and discipline. We’re working to address these pressures while keeping the wellbeing of our residents and clients at the heart of every decision.

extraordinary work our people do every day. We celebrate wins, big and small, and we’re honest about challenges so we can solve them together. For our leadership team, it’s about empowering them to make decisions, encouraging collaboration across departments, and making sure they have the resources to lead effectively. Purpose is a powerful motivator. When our people see the difference they make, their commitment naturally follows.
How are preparations for the introduction of new legislation going?
We’re approaching the new legislation proactively, not reactively. Our team has been dissecting the changes for months, mapping them against our current systems, and identifying areas where we can go beyond the minimum requirements. Compliance is nonnegotiable, but our aim is to embed these reforms into the fabric of how we operate, so they enhance, not hinder, the care experience. That means clear communication with staff, training at all levels, and involving our leadership team early so they can support their teams through the transition confidently.
What incoming changes are having the most impact at St Basil’s NSW/ACT?
The introduction of the new Aged Care Act and strengthened quality standards will have the most immediate impact. These changes demand even greater transparency, resident choice, and responsiveness, which align with our values but require operational shifts to deliver consistently. There’s also the ongoing transition to a more sustainable funding model, which impacts how we plan for the future. While these changes bring complexity, they also open the door to service innovation and improved outcomes, something we’re embracing wholeheartedly.
How do you encourage innovation within your organisation?
Innovation isn’t always about big, flashy projects, it’s about creating a culture where people feel safe to suggest new ideas, trial new approaches, and learn from missteps. We encourage our teams to bring forward improvements, whether that’s in care delivery, operational processes, or community engagement. By investing in staff development and giving people ownership over their ideas, we see innovation take root organically. We also look outside our sector for inspiration. There is much to learn from industries that have faced similar challenges in different contexts.
Do you have any words of wisdom on leadership?
Leadership is about clarity, courage, and compassion. Clarity in where you’re going and why. Courage to make decisions that might not be popular but are in the best interest of the people you serve. Show compassion for your team, yourself, and those relying on you. It’s also about surrounding yourself with people who challenge you and bring perspectives you might not have considered. I’ve learned that in times of uncertainty, people look to leaders not just for answers, but for steadiness. Your role is to provide that anchor. ●
Diana Horvatovic

Latest advice on retention strategies
Industry leaders are encouraging aged care providers to look at migrant and internal career pathways to recruit and retain staff, as well as individual workers’ priorities, writes KATARINA LLOYD JONES.
Whigh across the sector, conversations at industry conferences have workshopped how best to respond. Not surprisingly, there is no magic answer to the challenges, but stakeholders agree on the need to act.
by Design panel at Ageing Australia’s Victoria conference in early June, Kellie Nulty, Amanda Tinner and Faye Spiteri have all encouraged providers to look at new ways of attracting and retaining workers.


Nulty – chief executive officer of standalone regional residential aged care provider Red Cliffs & Community Aged Care Services – acknowledges there’s often still a stigma around working in aged care. She says it’s up to providers to make sure they encourage people to come and work in the sector, and to also look at the available migrant pathways.
Tinner – director of Australian migration advisor Visa Executive – similarly encourages providers to look to migrant populations
to build their workforces. people in an environment

“The only way you will cultures is to put them with other people from the same
“And I think working in the immigration space over so many years, we’re all humans and we like to find like-minded people. So, it’s never going to work if you put a square peg in a round hole. Just pick somebody from the same community, especially if you’re from a regional or a rural area.”
Spiteri – chief executive officer of Fronditha Care – says they too have embraced this approach including employing entire families across different sites.
The Strategies for sustainability of the aged care workforce panel moderated by Ageing Australia head of workforce strategy Andrew Hayward (right) with (left to right) Madelyn Dupriez, Kate Hurrell, Alyson Pearce, Sarah Thapa and Mandi Xu
Amanda Tinner

Fronditha Care provides community and residential aged care services that specialise in supporting people from a Greek cultural background.
“Because people want to belong and especially when you’ve got a really culturally diverse workforce, that sense of belonging is what creates that connection to an organisation, which results in retention but also better services to those families as well,” she says.
Panellists on the Strategies for sustainability of the aged care workforce panel at Ageing Australia’s NSW/ACT conference in Sydney in late June similarly encouraged providers to look to migrant pathways.
Madelyn Dupriez – acting human resources manager at Twilight Aged Care – says the residential aged care provider has established a recruitment pathway in Nepal.

Dupriez says 16 staff members have come to Australia and successfully integrated into their workforce.
The Migration Agency has embraced a similar pathway approach, says founder and managing director Sarah Thapa.
The visa consulting service has established a partnership with the government of Kerala in south India to create scalable pathways to bring registered nurses, enrolled nurses and personal care workers to Australia “in line with the demand of industry, not just now to meet the reforms but into the future, so that we have a reliable pipeline,” says Thapa.
This is to shift workforce planning to be predictive rather than reactive, she says.
“I think the reforms have driven a lot of urgency around solving workforce challenges through international recruitment and some of these things,” Thapa adds.
“But I think it’s important to look at not just the stock gaps but considering more long-term talent strategies and having global talent as a component of that. In addition, we’re also investing in global partnerships.”
The provision of internal career progression pathways was also recognised as crucial to retaining workers by both panels, along with Kate Hurrell – CEO of Three Tree Lodge Residential Care Services – who addressed this at the NSW/ACT conference.
“We’ve had to look at how we are using our existing staff. If they gain additional qualifications, how do we create job roles within our organisation to retain them? Because they’re often already in our community, they already have a house, the children are already at school,” says Hurrell.
Spiteri says Fronditha Care supports personal care workers who hold overseas qualifications to get those qualifications recognised in Australia and do further education.
“We have a lot of people throughout our organisation that have been there for more than 15 to 20 years. That encourages other people to stay in the organisation because they can see, for example, our current executive general manager of residential services, has been with the organisation over 30 years, 32 I think. He started as a personal care worker, did nursing, worked his way through the organisation,” she says.
“So he’s a shining example of how the organisation supports its people to progress.”
Consider work-life balance
It is also crucial to understand what workers actually value, says Matt Hodges – national director of education, health and social care at Randstad.
He says research conducted by the recruitment services organisation reveals a disconnect in what employees and employers are prioritising – particularly in the health and care sectors. While employers might traditionally focus on compensation or career progression as the primary motivators of their staff and
believe themselves to be offering a good work-life balance, Hodges says the reality for employees on the ground might be different.
He tells Australian Ageing Agenda the emotionally and physically demanding nature of aged care work means potential workers are prioritising sustainable careers that allow for work-life balance.
“The sheer margin by which ‘Good work-life balance’ (71.33 per cent) outranked other factors for healthcare employees was a significant insight. It underscores that for this sector, it’s not just a nice-to-have, but a fundamental requirement for sustainable employment in highly demanding environments,” he says.
Hodges says Randstad’s research suggests that aged care providers can “significantly enhance their employer attractiveness” by focusing on:
• championing genuine work-life balance by actively promoting flexible rostering, manageable workloads and employee wellbeing programs
• investing in career development and training by offering clear career pathways and opportunities for upskilling or reskilling
• offer a competitive salary and job security
• cultivate a “pleasant work atmosphere” that fosters open communication, respect, diversity and values psychological safety
• generate an authentic message for the organisation that shows genuine support for employee wellbeing.
During the panel discussion in Victoria, Nulty also acknowledged many psychosocial safety hazards in aged care including fatigue and aggression. She says Red Cliffs & Community Aged Care Services is looking at potentially introducing mental health first aid workers to help the workforce connect.
Spiteri adds that reward and recognition are critical, and while from a financial perspective there is a cost to hiring social and mental health workers for staff, the benefit can be seen at the other end.
Speaking on the NSW/ACT conference panel, Russell Kennedy principal Mandi Xu says this is an area the law firm has been working with clients on too.
She says the reforms indicate regulators are looking for employers to be proactive in stamping out psychosocial hazards in the workplace, and inappropriate behaviours like sex-based discrimination and hostile work environments.
If providers see disruptive behaviours during a new staff member’s probationary period Xu encourages them to make the sometimes-difficult decision to let them go, even though the sector is facing workforce shortages.
“I think what we’re seeing is that it’s actually important to keep the right people in as opposed to keeping on people who are actually going to be disruptive,” she says. “And that in itself – by making those tough decisions – you’re creating a good place for people to come to work, and that’s going to assist your retention strategies.” ●
Keeping people, growing talent – a workforce by design panel session moderated by Daniel Parsons (left) featuring (left to right) Kellie Nulty, Faye Spiteri and Amanda Tinner

Working alongside you to turn complexity into clarity and numbers into action

“ As a new Revenue Accountant in Aged Care, the landscape is confusing at first. Provider Assist’s training made everything click, with clear explanations and real-world examples. Their one-on-one support during monthly reconciliations was invaluable, and their responsiveness during critical times like month-end made a huge difference. I’ve really enjoyed working with them—they’re thorough, practical, and genuinely supportive.”
Leonie Koenig - Revenue Management Accountant
“ The surety you have provided has been instrumental in helping us plan and operate with confidence and stability. We are also deeply appreciative too of your guidance in navigating the complexities of the assessments of several of our residents. Your expertise, persistence, and solutions focus approach have been a significant relief for our team here, and for the affected residents and their families.”
Simon Coope - Finance Manager
More than just accountants and analysts, we’re specialist aged care finance & strategy partners. From outsourced finance roles and strategic decision support to budgeting, modelling, pricing, profitability, and education. We’re backed by real-time data, AI innovation, and in-house software from PA Digital plus frontline insights from PA Clinical - connecting care, revenue, and performance like no one else.
Finance Support & Virtual CFO
• Covering sudden finance team gaps (leave, resignations, etc.)
• Ongoing support - Billing, month-end and reporting through to CFO & Board
• Education & Mentoring for finance teams new to the sector
• Reviewing budgets or setting up performance and reporting frameworks
• Payroll Award & EBA compliance
Benchmarking and Competitive Monitoring Reports
• Residential Care RAD and Room Pricing
• Support at Home Service Pricing and Performance KPIs
• AN-ACC, Revenue, Occupancy and Care Minutes
• Quality Indicators
Transition, Change & Project Management
• Industry Change - Pricing Strategy (SAH and Room Pricing), financial modelling and project support for Support at Home and Billing and Funding Transitions
• Digital Transformation: Designing and implementing your Digital Nervous System, Data and System Integration and Implementation, AI and Process Automation
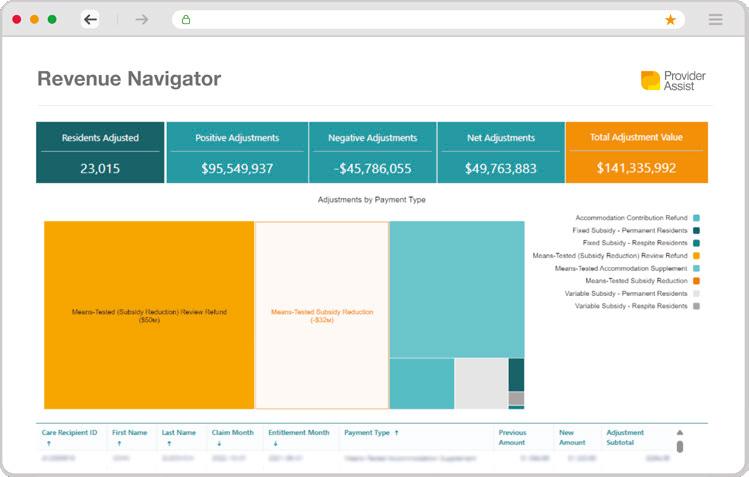
Funding, Fees, Letters, Billing and Reconciliation in a single place AN-ACC Navigator
Manage your entire AN-ACC workflow, no more spreadsheets

MyVitals
Data and insights you need for decision making
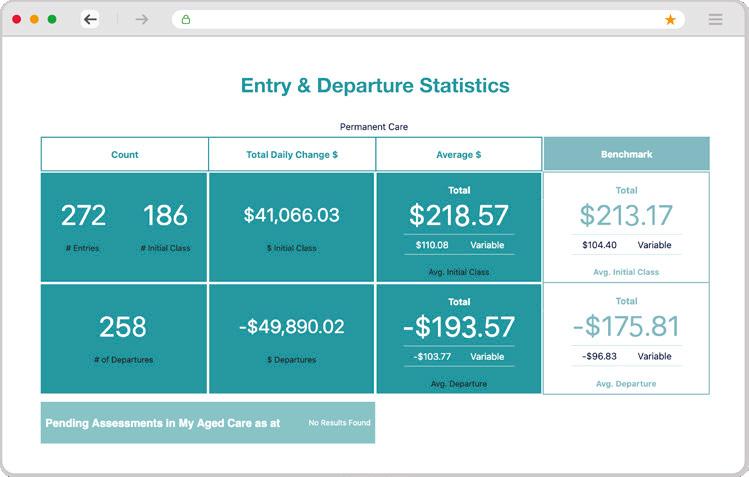
team@providerassist.com.au
Critical missing link
A nurse-practitioner-led model is allowing aged care residents to receive specialised support in their home setting, NICK RYAN tells JODIE WOLF.
Nick Ryan has done a lot during his 30year career in human services, across a variety of roles and sectors, including aged care, government, youth services and education.
“I’ve had a great time,” the chief executive officer of Queensland aged care provider Lutheran Services tells Australian Ageing Agenda of his career to date. “I’ve had a good experience, and I’m still enjoying it.”
The one-time head of the aged care regulator started out as a religious and theological educator, working as a schoolteacher and tertiary lecturer. After that Ryan was a senior public servant in the Queensland Government for 12 years working first in rural and regional policy then in disability, child protection, youth justice, and community services.
He is “proud” to be one of the architects of the Gold Coast schoolies week intervention two decades ago to better support “unaccompanied and often vulnerable” school leavers.
Serving on the boards of the Australian Children’s Education and Care Quality Authority, the Leukaemia Foundation of Queensland and the Archdiocese of Brisbane Catholic Education Council have also been highlights to date.
After an interim CEO role at Southern Cross Care Queensland, Ryan took the helm of Lutheran Services in 2019.

A topic Ryan is clearly passionate about is the organisation’s nurse practitioner model, which was introduced in May 2021 to address care gaps for residents with complex health needs, particularly in rural and remote areas.
“Typically, the needs of a resident get to a point where a regular registered nurse with the existing prescriptions and medical treatment requires more intensive support that would normally require a general practitioner coming out, or as is often the case, transportation to hospital,” Ryan explains.
He provides the example of a wound that can no longer be effectively managed under the normal treatment plan prescribed by a GP.
“A nurse practitioner is this critical missing link that enables a strong network between local hospitals and residents. They’re able to provide a higher level of medical care.”
If a resident is transported to hospital, the nurse practitioner is well placed to be an “articulate advocate” for them, Ryan adds.
As a specialist in residential aged care, with a
“The needs of the resident are already understood, reported and referred.”
master’s degree and specific registration, nurse practitioners work collaboratively in a healthcare team that includes GPs. They provide higher levels of nursing and medical care, including the ability to order diagnostic tests and prescribe specific medications. This enables Lutheran Services to give residents a much better and less disruptive care experience, says Ryan.
This nurse practitioner model aims to reduce ambulance transfers and hospitalisations and improve the quality of life of residents. It also saves costs for the healthcare system as a result.
“We’re still in the process of looking at the social impact assessment; we’re still gathering data on the rate of reduction of avoidable hospitalisations,” Ryan explains.
“That means the saving of an ambulance service that would normally be called to transport or transfer a resident. It’s the cost of having a resident in accident and emergency,” he says.
“It ensures that when a general practitioner comes on site, they have a lot of the preparatory diagnosis and analysis. The needs of the resident are already understood, reported and referred so the doctor then makes the best use of his or her skills and time.”
At the time of speaking, Lutheran Services has five nurse practitioners with plans to recruit a sixth before the end of 2025. The first, Mel Wagner, commenced in 2021 and is now a chief clinician.
“Mel Wagner is exceedingly good at what she does, and all of our registered nurses look to her as a leader and a guide for how they undertake their clinical practice,” says Ryan.
“I’ve also met the GPs she works with [who] sing her praises about what a real difference this model makes. This means the best possible quality of life.”
Ryan tells AAA that so far the model is going “very, very well” but he stresses it is still “preliminary days” and the “real work” now is to show its impact.
“It’s very easy to talk about a service in terms of what it costs,” he says. “We know that this particular approach would save hospitals in Queensland, tens, if not hundreds of thousands of dollars in avoidable hospitalisations.”
However, Ryan stresses it’s about far more than money.
“This investment saves the system a lot of money, but way more important than that, it means that a resident receives a high level of a more specialised level of support, clinical care assessment and a referral whilst
Nick Ryan




The conversation moves onto the evolution of aged care standards post-royal commission, with Ryan emphasising the key changes in resident experience, corporate governance, and quality of care.
Previously CEO of the Australian Aged Care Quality Agency from 2014 to 2018, Ryan notes the Aged Care Quality Standards –which were implemented in 2019 and will be updated in November – focus more on resident outcomes and experiences, as well as stronger corporate governance, than previous standards.


“In the time since I’ve left the role, the major change has been the 146 recommendations that emerged from the royal commission and how they’ve been implemented. However, certain things remain the same, and that is the responsibility of aged care providers, especially at a governance level,” says Ryan.
“One of the best things about the new Act is that the strengthened standards, whilst they’re new, continue the work that’s been going on for the last eight years to be clearer about what the experience of care would look like from a resident’s point of view, and not just what a provider might do.”
Ryan notes the new Act and standards respond to findings and recommendations of the royal commission, which was called towards the end of his time with the quality agency.

“Whilst change is difficult, change is important because it was important to hear of areas where aged care can improve, and it took time to work out how that could be supported, regulated and, most crucially, properly funded,” he says.



When he isn’t being a busy CEO, Ryan tells AAA he spends his free time walking his dogs beside the Gold Coast Broadwater and dining with family, including his 21-year-old son and 18-year-old daughter.
“I love living on the Gold Coast and working in Brisbane.”
Ryan struggles to think of something he dislikes about his role aside from wishing for “change to happen more quickly”. But he’s “old enough now” to understand there are “certain steps” before change can occur.


Lutheran Services, one of state’s oldest not-for-profit aged care and community service providers, is celebrating 90 years in 2025.

With over 6,000 people supported every year and more than 2,200 staff across 25 sites, Ryan says the key to loving his work as much as he does is simple and ultimately lies with those he works with.

“I work with a great team of people whose professionalism I admire and respect and whose company I thoroughly enjoy.” ●
Nick Ryan is a:
• former under-14 ACT orienteering champion
• graduate of the University of Divinity and University of Canberra
• fellow of the Australia and New Zealand School of Government and Australian Institute of Company Directors
• grandparent of two dogs and two cats.






Tool tackles culture gaps
A co-designed evolving toolkit helps providers measure the needs and values of the older Aboriginal and Torres Strait Islander people in their care. JODIE WOLF reports.
When staff understand the values of older Aboriginal and Torres Strait Islander people, care services can improve quality of life.
So says Associate Professor Kate Smith, a researcher dedicated to improving the experience of ageing for Aboriginal peoples. Smith is the research lead at the Centre for Aboriginal Medical and Dental Health at the University of Western Australia and the co-director of the UWA National Good Spirit Good Life Centre for Research Excellence in Indigenous Ageing Well.
Over the last 22 years, she has led over 15 projects on the topic of Indigenous ageing well. More recently she has co-developed a quality-of-life assessment framework for older Aboriginal Australians called Good Spirit, Good Life.
“The GSGL package, which took three-and-a-half years to develop including validation, was launched in July 2020 at a community stakeholder event in WA, which was open while other states were in lockdown,” Smith tells Australian Ageing Agenda “National partners and policy officials joined online.”
Work on complementary resources, education and promoting the toolkit is ongoing.
Good Spirit Good Life is a culturally informed, validated, strengths-based assessment package that helps aged care providers identify how to best support an older Aboriginal and Torres Strait Islander person to have a good spirit and life – or quality of life – in older age.
The tool evaluates wellbeing using 12 linked factors that Aboriginal people believe to be important (see box opposite). Maintaining these factors will keep an older Aboriginal person’s inner spirit strong.
The tool has also been recently reviewed and validated with minor revisions for Torres Strait Islander people and Aboriginal people living in remote regions, Smith tells AAA
A valued member of the GSGL team is Lianne Gilchrist, a postgraduate student at the University of Western Australia who worked closely with Smith as a research officer during the development, validation and translation stages of the project.


Madelyne Glover
assessment tool evaluates wellbeing using 12 linked factors that Aboriginal people believe to be important.”


Gilchrist’s master’s research focuses extensively
“The GSGL tool is crucial as it’s the first validated older Aboriginal and Torres Strait Islander people, developed and informed by Aboriginal and Torres Strait Islander Elders’ ways of knowing, being and doing,” says Gilchrist.
“It addresses a critical gap where conventional assessment tools failed to accurately capture the culturally specific wellbeing priorities of older Aboriginal and Torres Strait Islander peoples.”
It has led to the more recent development of valuable educational resources, says Gilchrist, including two videos available online (iawr.com.au/gsgl).
Dr Kate Smith Lianne Gilchrist
Hall and Prior Aboriginal health officer Carl Garlett

It is also the only quality of life tool, care framework and care planning package for older Aboriginal and Torres Strait Islander peoples, a population who face many barriers to living a good life and accessing culturally safe, trauma-informed care, she says.
The research project was overseen by an Elders governance group and service partners, which Smith says was vital to the successful outcome of the co-design and validation process in multiple regions around Australia.
This includes Perth, Kimberley, Melbourne, Shepparton, Torres Strait Islands and the North Peninsula Area of Far North Queensland, and national translation.
“It was also launched and strongly supported by the then Minister for Indigenous Australians and Aged Care Ken Wyatt, and WA’s then Minister for Aboriginal Affairs and our treasurer Ben Wyatt,” Smith tells AAA
“I am proud of the continued strong and vocal support of our GSGL Elders Governance Group for the GSGL, ensuring that the health and aged care services [and other services such as mental health] across the region know about GSGL, saying ‘this is everything that is important to us’.”

A key health and aged care service in the state, Moorditj Koort Aboriginal Corporation, uses the GSGL connection framework to inform all of their “wonderful programs” for older people, she adds.
At the national level, Smith says they are happy the translation of GSGL into the new Single Assessment System for aged care – and the Aged Care Quality and Safety Commission using it as evidence in quality of life and cultural safety standards – will also help inform the provision of holistic, culturally responsive care for older Aboriginal and Torres Strait Islander peoples.
Gilchrist adds there were no major development challenges but during translation, some clinicians needed support to confidently deliver an Indigenous-informed tool, highlighting the need for sufficient educational resources and training to support effective implementation.
She expresses her pride in the outcome, most notably the ownership the Elders have of it. “The trust they placed in us from the very beginning, and their continued support, has been instrumental in promoting the tool and its adoption.”
Feedback from providers has been “overwhelmingly positive” according to Gilchrist, who says that one provider has fully incorporated the GSGL tool into their new admission process, making staff training in its use mandatory.
“This demonstrates the tool’s practical value and seamless integration into existing care frameworks,” she says.
Smith is also pleased with positive reports from providers that the toolkit is helping inform holistic, more culturally responsive care that is important to their older clients’ wellbeing.
“There has been a request for more training specific to the aged care workforce,” she says.
“We have a Yamatji master’s student, Kevin Taylor, who is completing his research co-designing an education package with project partners Moorditj Koort Aboriginal Corporation and residential and home aged care provider Hall and Prior.
“Health providers are also applying the framework successfully with its 12 interconnected factors to shape programs, such as healthy lifestyle programs to enhance connections to spirit and the wellbeing of older Aboriginal and Torres Strait Islander community members.”
Hall & Prior became aware of the tool and the potential benefits it could offer to their residents and staff when chief executive officer Graeme Prior was asked to join the Good Spirit Good Life working group in 2016.
Madelyne Glover, allied health manager at Hall and Prior, says the organisation chose to implement the GSGL framework five
Good Spirit Good Life factors
• Family and friends
• Connection to Country
• Community
• Culture
• Health
• Respect
• Elder role
• Support services
• Safety and security
• Spirituality
• Future wishes
• Basic needs
years ago as it was an evidence-based quality-of-life tool co-created with Aboriginal people encouraging culturally safe engagement informed by authentic insight from Aboriginal end users.
“Hall and Prior cares for many Aboriginal consumers who access our services, across both residential and home care. We had used a variety of quality-of-life tools in the past, however, none that were accurately culturally specific,” Glover tells AAA
“We identified this as a gap that needed to be filled and started implementing the GSGL tool across our sites as soon as possible.”
Hall & Prior has developed a close relationship with the GSGL team at UWA, which has assisted education and training for staff and enabled full use of the tool, she adds.
The tool is available to use where appropriate for all 2,500 consumers in Hall & Prior’s care, says Glover, providing valuable insights into the specific needs for consumers who identify as Aboriginal or Torres Strait Islander.
In Smith’s opinion, the education package by Kevin Taylor is necessary for the aged care space, and she says the team has further GSGL education development occurring in the healthcare space.
“The work Caleb Rivers is doing with Elders on Spirit and models of care is also necessary for broader health education and implementation,” she says.
Smith commends the GSGL work from “fantastic” Aboriginal postgraduate students in her team and Gilchrist’s successful work on validating the tool in remote regions with local researchers and interpreters, supporting national translation.
“Her finding on changing the wording to ‘Connection to Island Home’ rather than ‘Country’ for older Torres Strait Islander peoples also informed other policy documents with support from National Aboriginal and Torres Strait Islander and Aged Care Council, such
Continued page 35 >
Hall and Prior resident Rocco Sirolli (left) with his son-in-law Les
Image credit: Ryan Ammon from Ammon Creative


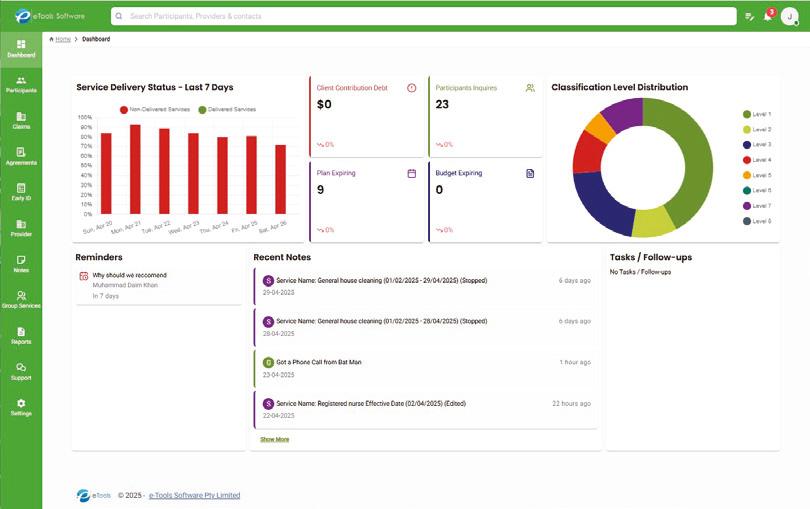

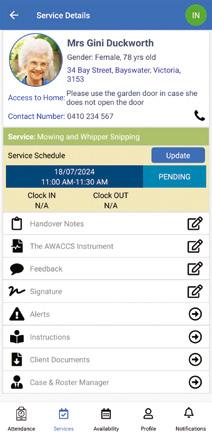






Removing the fear
A project underway aims to help all aged care homes deliver positive practices for older LGBTIQ+ Australians.
JODIE WOLF reports.
Discrimination and unsafe care practices can mean members of the LGBTIQ+ community are reluctant to be their true selves when receiving care.


Professor
A five-year study launched in March 2024 with almost $1 million from the Medical Research Future Fund is working on tools to support providers to address this. The Rainbow Inclusive Aged Care Project aims to create a transferable model of inclusive care for the LGBTIQ+ ageing community and identify inclusive practices in residential care.
Mark Hughes, a professor of social work at Southern Cross University and one of the project’s chief investigators, has been researching this area for 25 years. As a gay person specialising in gerontology, he says researching LGBTIQ+ older people is a “natural fit”.
“In our communities people are afraid of residential aged care. They’re afraid of having to go back into the closet later in life and about the quality of care that’s going to be provided to them. From previous research that I’ve been involved in, people have said they’ll do extraordinary things to try to avoid going into residential care,” Hughes tells Australian Ageing Agenda
“We’re trying to understand what works in residential care, what things are going on there that are inclusive for our communities, and how we can learn from those things and replicate them.”
The study involves five universities and several industry partners including Wesley Mission Queensland, Amana Living in Western Australia, Older Persons Advocacy Network, Australian Association of Gerontology, Ageing Australia, LGBTIQ+ Health Australia and GLBTI Rights in Ageing.
Meaghan Vosz, a SCU research fellow also on the project, explains that because gender and sexually diverse older people have experienced much discrimination in their lives, the “fear of mistreatment” in aged care is real.
“As a queer researcher living in regional New South Wales, I am deeply committed to working alongside GSD older people and service providers to uncover the ways that residential aged care can be safe and centred around kindness for everyone working, living and visiting aged care communities,” says Vosz – who shortens gender and sexually diverse to GSD.
Data collection has commenced, and observations in 12 aged care homes are planned for June and July, Hughes tells AAA. The first stage involved setting the collaborative research conditions.

“With a project like this, it’s important to draw upon lived experience expertise, to bring in a wide range of stakeholders and set up good participatory research processes, which we’ve been doing over the last year,” he says.
“It’s exciting. Later in the year we’ll be doing interviews with family members, residents, friends, workers, visitors and we’ll be launching a national survey of residential aged care staff, workers and volunteers.”
Vosz shares that six LGBTIQ+ older people have been recruited as co-researchers, and fieldwork is underway at aged care partner sites.
“Each of the communities we are visiting is welcoming and each is different,” she says. “The model we develop over the next few years will need to adapt to different settings and cultures within each community.”
Hughes highlights the importance of participatory research and involving diverse groups, including transgender people. They have set up a lived experience advisory group, communities of practice, and a national reference group to ensure inclusive research.
“They’ve been heavily consulted in the development of the survey and the other research tools,” he says.
When considering a provider’s role, Vosz points out that not everyone feels safe to be open about their gender and sexual diversity and building relationships and a sense of acceptance can take time.
“There are ways to signal to GSD visitors, staff and residents that a space is safe and inclusive – such as undertaking training, including GSD-affirming activities, and collaborating with LGBTIQ+ community organisations to recognise important community events like IDAHOBIT [International Day Against Homophobia, Biphobia, Interphobia and Transphobia] and Pride,” she says.
“I’m learning that at the heart of including gender and sexual diversity is kindness, being curious, gentle, warm and accepting of what’s important to each person. Rainbows are a great symbol for inclusion of GSD older people. They can reflect myriad possibilities of diversity: cultural, ethnicity, gender, sexuality and history.”
Our conversation turns to the new Aged Care Act and Hughes emphasises the need for better recognition of the diversity of older people. He stresses the need for naming and addressing specific challenges like homophobia and transphobia and supporting a rights-based aged care system with obligations for inclusive services.
Mark Hughes
Meaghan Vosz
“Legislation policy talks very broadly about diversity but doesn’t name the groups and the ways in which they’re impacted,” says Hughes.
He adds the Act should provide “enshrined obligations” on aged care providers to provide inclusive services for a wide range of communities.
The project is oriented in a positive direction, says Hughes, to learn what’s working and how to scale that up.
A survey now open for staff, volunteers, and students on placement in residential aged care has been designed to unpack and understand workers’ perspectives of enabling and constraining factors for inclusive care.
The team plans to recruit 2,500 participants across all states and types of providers with a broad representation of different roles in those organisations.
Hughes tells AAA the goal is to produce a model of inclusive residential aged care that is transferable sector-wide.
“We don’t want to produce something that can only be delivered in central Melbourne or central Sydney. Most people are going to need to access services from mainstream providers [so our model must] be transferable and useful for them.”
Vosz adds: “At the end of the study I’d love to see our model and the resources we create being used in every aged care home in Australia. I’d like for residential aged care to be a place where GSD people feel safe, accepted, welcomed and honoured.”
Contact the project team at rainbow.aged.care@scu.edu.au Scan QR code to access the survey ●
Continued from page 31
as the new aged care framework for Aboriginal and Torres Strait Islander peoples,” Smith tells AAA.
“We will be launching some of the student GSGL outcomes at the Australian Association of Gerontology conference in November.”
Gilchrist shares that the team is currently planning to integrate the GSGL framework into the health sector across diverse settings, similar to how it has been incorporated into aged care policy and practice.
“This expansion aims to broaden its impact and ensure culturally safe care in all health sectors,” she explains.
Glover has high hopes for the GSGL tool’s future.
“It would be great to see this evidence-based tool used by providers nationally across both residential and home care to continue to improve the quality of life of Aboriginal people in Australia.”
Smith’s hope for the remainder of this year is that the new Aged Care Act supports the rights of older Aboriginal and Torres Strait Islander peoples to receive “culturally safer assessment and care” from a “culturally responsive and respectful” workforce.
“Enabling older people and their families to have strong connections for a good spirit and life in older age,” she says.
Gilchrist agrees, noting that the Act aims for fair, culturally safe assessment and service delivery.
“We believe that the GSGL assessment package will empower providers to deliver truly culturally safe care, ensuring the Act’s promise is fully realised for older Aboriginal and Torres Strait Islander peoples,” she says.
“With the new rights-based Aged Care Act, we envision older Aboriginal and Torres Strait Islander peoples at the heart of aged care.” ●

Transition tools
The AAA team has put together a list of free resources created by the Department of Health, Disability and Ageing and other stakeholders to support providers to transition to the new Aged Care Act on 1 November. Scan the QR codes to access them.
Department’s one-stop hub
The department has created a dedicated page with all the relevant links to documents, eLearning modules, toolkits, checklists and summaries related to the Statement of Rights, the Financial and Prudential Standards, the regulatory model, quality indicators, the Strengthened Aged Care Quality Standards, the new Support at Home model, worker screening changes, fees and means testing, compliance and enforcement, care minutes and more.

7 key areas of change
Peak body Older Persons Advocacy Network has identified the seven key areas of change for older people with the new Act and has created summaries for each. It has also provided the links to relevant webinars and information posters where available.

Care minutes statement requirements
Help for communication practitioners
A new animation developed by the department aims to help providers communicate to clients about how parts of the new Act fit together and put older people’s rights at the centre of care. In addition to English, the video is available in several languages including Arabic, Chinese, Greek, Italian, and Vietnamese. It is also available in Auslan.

Provider communication toolkit
If providers need help to communicate the changes to the families of older people or to their employees, the department has published a communication toolkit, which includes an infographic and animation, a discussion guide and suggestions for social media posts on the topic.

Peak’s Act resource round-up

To help providers prepare to submit their first Care Minutes Performance Statement for the 2025-26 Aged Care Financial Report, the department has published a breakdown of the new Care Minutes Performance Statement and audit requirements, with links to relevant documents and an introductory video.
Training support for facilitators
Ageing Australia has also collated a list of freely accessible resources for providers, including the dates of publication for each resource. There are also links to Ageing Australia member resources, including readiness action plans for residential care, Support at Home and the new Act more broadly.

iStockphoto.com/watchara songprasert
Support at Home training

The department has published a face-to-face training package to help facilitators deliver engaging and empowering conversations with older people, their families and carers on the changes accompanying the new Act. The package includes a ready-to-use presentation and detailed facilitator guide covering the rights of the individual, supporting the needs of older people, decision-making, changes to service delivery, accessing government funded services, key changes to residential aged care and specialist programs, safety and empowerment, and how to navigate raising concerns.
The department has made a twopart learning package for Home Care Package and Short-Term Restorative Care providers to learn about the changes and responsibilities under the Support at Home program. The department recommends all providers complete at least Learning Package 1 – Program Overview. Learning Package 2 –Delivering Service Modules includes six modules that offer more detailed guidance.

iStockphoto.com/ipuwadol


Finding their tribe
Following an immensely successful first year, the Positive Ageing Summit will return to Adelaide in May 2026 to further explore a holistic approach to better ageing. NATASHA EGAN reports.

On 28-29 May 2025, 250 passionate individuals assembled at the Adelaide Hilton for the inaugural Positive Ageing Summit where they engaged in countless allied health-driven conversations on improving outcomes for older Australians.
The overarching sentiment was summed up by the inaugural Paul Johnson Positive Ageing Award winner Bernard Morrison in his acceptance speech.
“Positive Ageing Summit 2025 was such an inspiring few days.”
“I feel like I’m in my tribe here. We’re all here for a common purpose. And I genuinely hope that this is the first of many Positive Ageing Summits,” Morrison, an occupational therapist and general manager of wellbeing and allied health programs at Eldercare, told his peers.
The award is sponsored by BallyCara, where the late Paul Johnson, a tireless positive ageing advocate, worked for over a decade. BallyCara executive chairman Marcus Riley presented the award to Morrison during the final session of the conference Riley also delivered the closing keynote on how wellness-driven services can reshape aged care and moderated a panel focused on retirement living. He was among more than 30 industry leaders who took to the stage over the two days.
The summit featured 20 keynote, panel and masterclass sessions sharing and discussing the latest evidence, practice and strategies, with journalist and presenter Jess Adamson as emcee. The event was supported by 20 partners and exhibitors led by platinum sponsor Bolton Clarke. Networking included a welcome cocktail reception at the Hilton’s Collins Bar after day one.
“It was an amazing success,” says Dr Tim Henwood, who acknowledges his bias given his role as conference advisor. But he adds the event was like no other he has been to.
“We had a whole lot of delegates attend who sat, transfixed with the stage – whoever was on stage and whatever the topic at hand – throughout the whole event. People didn’t drift away. They
weren’t on their phones or computers, which shows me there is a community out there that believes in reablement, wellness and allied health as a health pathway for older Australians,” Henwood tells Australian Ageing Agenda
Henwood, principal consultant at AgeFIT Solutions, specialises in targeted exercise programs for seniors in community and residential aged care. He says there were ample learnings for attendees to improve the services they deliver to residents and clients, regardless of what they already knew about allied health,
“Positive Ageing Summit gave everybody a takeaway of something they can transition into their organisation or into their practice. It also linked like-minded people together in the form of camaraderie –a shift that I’ve never seen at a conference before,” he says.
Attendee Dr Natasha Reid – a senior research fellow and behavioural scientist at University of Queensland’s Centre for Health Services Research – agrees.
“The best thing about it was having 250 people in the room all interested and passionate about increasing health and wellbeing for others, particularly through holistic and integrated care,” Reid tells AAA
Likewise for Vanessa Jones, director of marketing and engagement at McLean Care.
“This was complimented by some fantastic speakers,” Jones tells AAA Vanessa Harrison, deputy state operations manager Queensland at Arcare, also rated the content highly.
“Positive Ageing Summit 2025 was such an inspiring few days filled with insightful, knowledgeable presentations, engaging panels, and meaningful conversations around all the many facets of ageing,” Harrison tells AAA.
The speaking program – curated by Henwood – delivered evidence, policy and practice from national and international speakers with academic, professional or lived experience. He notes the presentation of Australia’s chief allied health officer Anita


Hobson-Powell, who shared the government’s new attention on allied health.
“The government is trying to establish a structure around allied health across all sectors, which is incredible to see, having been on this soapbox for 25 years,” says Henwood.
Of other sessions, He says: “We approached allied health from the dietetics, podiatry and exercise physiology directions, and then we also approached allied health from the multidisciplinary direction presented by Christina Wyatt.”


“I found the inaugural event both informative and highly relevant to my role.”
Wyatt – the professional practice advisor at Occupational Therapy Australia – delivered a keynote on how multidisciplinary teams boost aged care outcomes, and joined a panel on real-world barriers to allied health in aged care and how to overcome them.
“The summit also heard about the value for carers and consumers,” says Henwood, including from Council of Elders chair Anne Burgess and Vector Consultants director Judith Leeson who formed a panel sharing the consumer perspective.
“We also saw some incredible speakers like Kate Weger, who brought so much passion to the value of reablement until death. Jo Boylan brought so much passion to the value of pushing your residential aged care space to embed reablement so people can mobilise and enjoy the dining experience.
“And people like Bill Yeates, who did the incredible morning breakfast masterclass, and talked about his lived experience with dementia and how reablement has played a key role in his ongoing wellness and capacity to still function and live independently.”
For the breakfast session, HammondCare executive Marie Alford moderated a 40-minute compassion, rights and reablementthemed discussion with Yeates, HammondCare GM Dr Duncan McKellar and Dementia Doulas International CEO Wendy Hall.
Eliza Peka, general manager of community clinical services at Feros Care, says she found the event well suited to her job.
“It was encouraging to hear several presenters acknowledge they were preaching to the converted when advocating for greater investment in allied health and contemporary approaches to ageing and wellbeing,” Peka tells AAA
“As someone working in community home care, I found the inaugural event both informative and highly relevant to my role. I particularly appreciated Dr Chris Bollen’s presentation and his strong advocacy for a better understanding of frailty and healthy ageing – this resonated deeply with me as a provider actively implementing the Restorative Care Pathway.
“The content struck a thoughtful balance between community and residential aged care, which is why I’ll be encouraging my colleagues from our residential aged care team to attend next time.
The exhibitors were also directly aligned with our work, offering valuable opportunities for connection and collaboration.”
Podcaster and Positive Ageing Summit ambassador Anthony Nguyen was among those in the exhibitor hall, where delegates could watch him record interviews for his Pioneers in Aged Care podcast.
“The Positive Ageing Summit was the most enjoyable industry event I’ve ever been to,” Nguyen tells AAA. “Everyone was there to genuinely connect and collaborate.”
In August, Nguyen released five interviews recorded at the event with aged care leaders, including summit speakers:
• OneCare CEO Peter Williams, who linked a health-literate workforce with wellbeing and allied health engagement
• Dr Jennie Hewitt, general manager of reablement at Whiddon, who discussed the latest evidence on falls prevention
• Dr Tim Henwood, who joined a panel discussing reablement and restorative care across the sector.
The other interviews released during the podcast’s Positive Ageing Summit Throwback Week were with Belinda Sutherland, general
Credit:
Photographics
Credit: Oneill Photographics
Credit: Oneill Photographics
Anita Hobson-Powell shares national plans for allied health
Bill Yeates speaking during the breakfast masterclass


manager of health and wellbeing at Wesley Mission Queensland, and Dr Rebecca Bilton, program and research director at Aged Care Research and Industry Innovation Australia.
“If there was one overarching message from the Positive Ageing Summit, it was the importance of reablement and a person-centred approach to aged care. Many speakers emphasised a shift from ‘doing for’ to ‘doing with’ to empower older individuals to maintain their independence and achieve their personal goals.”
Nguyen also notes the practical nature of the program. “Sometimes these big events can be all theory and no action, but at PAS there were so many real-world examples and people genuinely sharing what’s working on the ground.”


“The Positive Ageing Summit was the most enjoyable industry event I’ve ever been to.”
On top of new friendships forged, a lot of respect was shared on the excellent jobs people are doing in this space, adds Henwood.
“I’m incredibly connected, but I’ve never been to an event where all those people were in the one space, and they were just generating this incredible reablement and wellness energy. I think Bernard Morrison put it nicely. It was a tribe of people coming together who are all like-minded about an evidence-based outcome that can have great impacts for the health of older Australians.”
Luke Mapunda, health service team leader of residential at ACH Group, also delights in gathering with passionate professionals.
“I was reassured by listening to the presenters, that at my workplace, we are already implementing a lot of the recommendations,” Mapunda tells AAA
The value – and indeed necessity – of progressive strength-based exercise to age well was a strong theme throughout the two days and among Mapunda’s takeaways. Delegates heard from experts including Associate Professor Justin Keogh from Bond University about how such measures can improve health outcomes and reduce strain on the health system.
“I left the event with even more conviction on the importance of correctly prescribed exercise in older adults, and that we need to ensure we continue to work collaboratively to have the most meaningful impact on people. To me, exercising the right way should be something all older adults strive to do,” says Mapunda.
“The evidence on the benefits for exercise is undeniable, but still only a small percentage of people exercise in the correct way. We need to get to the bottom of why this is and address these reasons.”
The importance of working together was a conference theme that Laura Beres, president of ANFE Community Care, connected with.
“My main takeaway from the summit the last couple of days has been around not only the necessity of collaboration and working together as a sector, but the ultimate outcomes that will achieve for the people in our communities,” she tells AAA
After the event, Henwood published a series of posts on LinkedIn related to Positive Ageing Summit 2025 presentations that challenge people delivering aged care services to do better.
“They are there to be thought provoking,” Henwood tells AAA “Unless your classes are 100 per cent full, unless you’ve got clients who are stronger, fitter, faster, pushing back on disability and have an extension of their independence, and unless heavily engaged allied health teams do multidisciplinary engagement that manage a client’s pathway, I challenge you that you could do better,” he says.
“And if you could do better, the platform that you could learn how to do better is definitely the Positive Ageing Summit.”
Following the two-day conference, nine delegates joined the Positive Ageing Summit Site Tour, which included two aged care homes in Adelaide, wine tasting in the Adelaide Hills and lunch in the Piccadilly Valley.
Anthony Nguyen (right) interviews Lorraine Poulos Bolton Clarke’s Deidre McGill and Dr Tim Henwood
Dr Tuire Karaharju-Huisman speaking on the retirement living panel
Marcus Riley (left) and Bernard Morrison Credit:


Among those who took part in all aspects of the summit is Dr Tuire Karaharju-Huisman, research lead at Hur Australia, a sponsor and exhibitor at the event.


“I can’t wait to attend again next year.”
Karaharju-Huisman – a physiotherapist and exercise physiologist – also joined Southern Cross Care SA, NT & Vic CEO David Moran and Retirement Living Council executive director Danial Gannon in the panel discussion moderated by Marcus Riley on how the retirement living sector can drive healthier, more independent ageing.
“The inaugural Positive Ageing Summit truly delivered what it set out to do – inspire collaboration, share evidence-based strategies, and empower everyone to look for better services in aged care,” Karaharju-Huisman tells AAA
“With holistic health at the centre, all aspects of care were discussed, from retirement living to end-of-life care, emphasising the role of allied health services, carrying the theme that restorative care must be the default approach in aged care.”
Karaharju-Huisman also attended the tour to “aged care sites that have truly put positive ageing in practice”. This included Clayton Church Homes’ Summerhill Residential Care Home, and Carmelite by Southern Cross Care SA, NT, Vic, which offers residential care, retirement living, community health and wellness, and day therapy.
“At both sites we met residents and staff with smiles on their
faces, welcoming us all to their home. Whilst the architecture at the sites was just stunning, it was the details in the care that truly reflected holistic care, and excellence in care services,” KaraharjuHuisman tells AAA
“It is not too often that you walk away from an event with a smile on your face, feeling confident that there are many people with a great passion for positive ageing. After the many challenges for the industry in recent years, it is great to hear about the positive experiences and models that can be replicated throughout the sector. I can’t wait to visit the symposium again next year.”
Natasha Reid, Vanessa Jones, and Luke Mapunda also say they are looking forward to the next Positive Ageing Summit – which returns to the Adelaide Hilton on 20-21 May 2026.
Henwood, who is staying on as conference advisor, says programming is already underway and delegates can expect it to be even better than this year. He is most looking forward to continuing to build the positive ageing community.
“If we build that community, we can build the opportunities. And if we can build the opportunities, we’re going to be ready for this incredible groundswell of older adults who are going to both need and want allied health and exercise as a pathway to their better health in their later life,” he tells AAA
Scan the QR code to view AAA’s extensive online coverage of the inaugural event
Site tour delegates tasting wine in the Adelaide Hills
Delegates converse at the welcome reception
L to R: Michael Cheng, Dr Tim Henwood and Christina Wyatt
Credit: Dr Tuire
Karaharju-Huisman
Credit: Oneill
Support healthy ageing, dismantle ageism

It is a human right to have access to good quality care, says Jo Boylan, who calls on all aged care homes to embed health-promoting models of care. KATARINA LLOYD JONES reports.
Advancing healthy ageing is a significant and achievable paradigm shift for aged care and Australia can be a global leader if providers set up restorative care and rehabilitation as the initial default response to older people declining in residential facilities, says Clayton Church Homes’ chief executive officer Jo Boylan.
She admits this is a big ask, as it requires providers “racing in” to introduce resources and interventions to prevent further decline as soon as they see signs of frailty or sarcopenia.
Speaking at the Positive Ageing Summit in May, Boylan reminds delegates it is a human right that all residents “have equal access to good quality care and services” and that the sector must prepare for an ageing population.
Pointing to the World Health Organisation’s United Nations Decade of Healthy Ageing (2021–2030) plan – which flags physical activity, social engagement and the environment as key to wellbeing – Boylan says executives need to look at their homes and ask if they are doing enough to promote wellbeing.
Clayton Church Homes, says Boylan, has a goal of keeping older people walking “right up until they die.”
This requires the not-for-profit to put interventions in place to “push back on disability every day” and to focus on early intervention.
But aged care providers should be funded for these rehabilitation and health-promoting models designed to avoid extensive decline, says Boylan, as without the funding, providers become resigned to it and start to “normalise decline”.
“We need to be funded in a way that will make healthy normal,” she says. “What you fund is what you get,” adds Boylan. “The alternative is a lingering life with advanced frailty and the body breaks down.”
Too often, however, older people are arriving at aged care homes on a declining trajectory and providers simply provide comfort care, when they should instead be working to push them back above the disability line.
“Only then will they have a quality of life,” she says.
Clayton Church Homes has three stages they work from to embed a recovery pathway for residents. Boylan says this is made up of:
• the repair stage: focused on movement, for example, walking
on the parallel bars and having care workers do six walks a day with residents
• the strength stage: introducing progressive strength-based workouts with weights and machines, plus six walks a day – with the walks getting progressively longer
• the functional stage: restoring function, coordination, change of direction, balance and strategies to prevent falls – moving the individual towards a “maintaining phase” where they can start going to the gym and back to normal activities.
She says this health-promoting pathway takes five to 10 weeks for full recovery but is dependent on multidisciplinary teams of care workers and allied health professionals.
But these multidisciplinary teams must be led by registered nurses, who “hold the keys to recovery,” Boylan emphasises, as every day it is the RNs who are reading progress notes and scanning for signs of decline.
“Moving a person from illbeing to wellbeing is everyone’s business,” says Boylan. “The RN coordinates this process in partnership with the exercise physiologist; the care workers can be directed to provide the six walks per day to start the first phase toward recovery and the exercise physiologist will provide up to three intensive sessions per week to build that endurance.
“And you only have to do that for a short while; this all happens quickly. But if you don’t do it, it won’t happen.”
Another key part of making healthy normal is tackling ageism, which Boylan describes as “rife in the health system.”
Conversely, when you have a recovery culture, it encourages staff to put in more effort, as they know the benefits the resident will achieve, she says.
“They will put in more effort, knowing the benefits the resident will achieve. Their effort equals rapid recovery. And believe it or not, we’ve got amazing muscle memory, and we recover quickly.”
The Clayton Church Homes model is easy to implement but can be hard to sustain, Boylan says, and providers must keep trying every day to introduce health-promoting models to their homes.
“Anything short of this borders on ageism. So, we need your grit and your unbelievable Australian spirit to help our Australians live well,” she reminds delegates. ●
Jo Boylan speaking at the Positive Ageing Summit










Supporting safer use of medications
New quality indicators can support clinical governance and medication management in residential care and compliance with the strengthened standards, share the team behind their development.
Ensuring safe and appropriate use of medicines is fundamental to delivering high-quality residential aged care.
In 2022, the Department of Health, Disability and Ageing published the updated Guiding Principles for Medication Management in Residential Aged Care Facilities, which adopts a systems-based approach and outlines best-practice recommendations to improve medication safety.
Many elements of the guiding principles align with the strengthened Aged Care Quality Standards, which come into play on 1 November with the new Aged Care Act.
Monash University and the New South Wales Therapeutic Advisory Group have developed a series of quality indicators known as the MEGA-MAC indicators that support aged care homes to measure concordance with the guiding principles.
The 28 indicators across four domains were developed in partnership with residential care organisations as part of the Maximising Embedded Pharmacists in aGed cAre Medication Advisory Committees, or MEGA-MAC, project funded by the Medical Research Future Fund.
Providers and clinical staff can use the MEGA-MAC indicators to demonstrate activities that meet the new standards.
MEGA-MAC indicator 1: the MAC meeting
The MEGA-MAC domain 1 indicator can provide evidence of clinical governance processes to improve the safety and quality of clinical care services.
This domain focuses on assessing the structure and function of an aged care home’s medication advisory committee. These multidisciplinary committees, usually referred to as a MAC, provide overarching governance of medication management to ensure safe and appropriate use of medications.
The MEGA-MAC indicators can be used to demonstrate the MAC meets quarterly, is multidisciplinary, uses trends in data to drive quality improvement, and focuses on individuals’ experiences around medication management to ensure clinical care services promote person-centred care. Standard 5, outcome 5.1: clinical governance
MEGA-MAC indicator 2: policies, procedures and guidelines
The MEGA-MAC domain 2 indicator can provide evidence the residential care provider maintains current policies, procedures and guidelines that guide staff on how to undertake medicationrelated processes.
For example, MEGA-MAC indicator 2.1, “The collection and review of feedback from the resident, carers, family and/or substitute decision-makers regarding medicine use” may support the provider to demonstrate how they partner with individuals

when designing, delivering and evaluating quality improvement activities. Standard 2, outcome 2.1: partnering with individuals
MEGA-MAC indicator 3: the admission process
The MEGA-MAC domain 3 indicator can provide evidence of systems in place to support the quality use of medicines during the admission process.
Indicator 3 focuses on ensuring medication-related information is communicated and documented in a timely manner to avoid potential medication-related harm. The domain 3 indicator can be used to support documenting key medicationrelated information – such as allergy or vaccination status – and to support the timely assessment of an individual’s swallowing ability at admission. Standard 5, Outcome 5.3: safe and quality use of medicines
MEGA-MAC indicator 4: the medication review process
The MEGA-MAC domain 4 indicator can provide evidence of systems in place to support regular medication reviews, particularly at the commencement of care and for those with potential high-risk medication regimens.
Timely medication reviews, either by a residential medication management review pharmacist or aged care onsite pharmacist, are a key strategy in supporting appropriate medication use. Standard 5, outcome 5.3: safe and quality use of medicines
Where can I find the MEGA-MAC indicators?
The MEGA-MAC indicators can be found on the NSW TAG website (nswtag.org.au). The NSW TAG also has additional resources for quality use of medicines in older adults, including polypharmacy indicators and deprescribing tools for clinicians and consumers.
The MEGA-MAC indicators are designed to be used as part of quality improvement initiatives, and support audit and feedback to monitor progress over time.
Individual MEGA-MAC indicators can also be used to demonstrate activities that meet the strengthened aged care standards beyond what is discussed in this article. Each of the four indicator domains offer a suite of resources to support their use, including indicator specification documents and data collection tools that collate and present results. Scan the QR code to find out more ●
The MEGA-MAC indicators were developed by the Centre for Medicine Use and Safety at Monash University (Professor Simon Bell, Dr Amanda Cross and Ms Brooke Blakeley) and New South Wales Therapeutic Advisory Group (Professor Sarah Hilmer and Dr Alexandra Bennett)



When they put their trust in you, it’s vital to have information you can trust.
AMH Aged Care Companion

PRACTICAL REFERENCE FOR AGED CARE
Covers over 70 conditions to assist healthcare professionals in delivering effective care.

DESIGNED FOR OLDER PEOPLE’S UNIQUE NEEDS
Provides information on treatment options to minimise harm caused by inappropriate use of medications.

SUPPORTIVE TOOL FOR MEDICATION REVIEW
Features evidence-based insights to optimise disease management, including deprescribing and frailty.



OPTIMISE HEALTH OUTCOMES
Maximise the benefits of medication to improve and assist overall quality of life.





























































My fifteen steps to change
Advocate WILLIAM YEATES shares
what he learned from his Walking the
Talk for Dementia experience.
When I was diagnosed with younger onset dementia in 2019, I chose not to quietly fade into the background. Instead, I made a commitment to be visible, to advocate, and to help shift the way people understand and respond to dementia.
That decision has taken me places I never expected including last year when I was invited to join something extraordinary: Walking the Talk for Dementia. This was no ordinary event.
Over four days from late August, a group of around 70 people from across the globe, including 12 of us with lived experience of dementia, walked together through the final stages of the historic Camino de Santiago pilgrimage in Spain. We walked to connect. We walked to learn. And we walked to imagine a different future for people living with dementia.

route took us toward Santiago de Compostela, where all Camino routes converge.
What made this journey remarkable wasn’t just the landscape, or even the destination. It was the people. We were a mix of advocates, clinicians, researchers, policymakers and carers. There was so much respect, the sense that every person had something important to say.
On the final day, our small group had grown to hundreds. Locals joined the walk. Passers-by clapped and cheered. As the 12 of us with dementia carried the purple banner into the city square, I was overwhelmed by emotion. It was, without question, one of the most powerful moments of my life.
Writing my learnings
An invitation I couldn’t ignore
The walk is by invitation only. Fernando Aguzzoli Peres, the founder of Walking the Talk for Dementia, reached out after hearing my keynote at the Alzheimer’s Disease International Conference in Krakow, Poland in April 2024. He told me he was inviting people with lived experience from around the world to be part of something unique, a gathering where all voices mattered equally. There would be no name tags, no hierarchies, just people walking and talking side by side as one community.
With support from HammondCare, I was able to make the trip. Without them, I wouldn’t have been able to go. And I’m so grateful I did, because what I experienced over those four days has stayed with me ever since.
A walk with purpose
Each day we walked about 10 kilometres through the Spanish countryside. For many of us, that was enough – not just physically, but emotionally. The Camino is a deeply symbolic path, and our
After the walk, many participants shared their reflections through videos or blog posts. I wanted to do something different. I wanted to capture what the experience had taught me.
So I wrote My Learnings from the 2024 Walk the Talk for Dementia (see box opposite). They are my reflections from conversations, moments of connection, and the thinking that happens when you walk side by side with people who truly listen and want to change the world’s attitude to people living with dementia.
What I want for myself
The first five learnings are deeply personal. They reflect what I need not just to survive with dementia, but to live with purpose and dignity.
I want to be accepted as I am. To stay connected and involved. To live in a community that respects my rights – these are the same fundamental rights as everyone else. To have access to appropriate care and support services when I need it, not just at the end, but throughout my journey.
William ‘Bill’ Yeates
William ‘Bill’ Yeates (far right behind banner) among lived-experience representatives on the final day of the walk
These aren’t extraordinary requests. They’re things all of us want, regardless of a diagnosis.
And yet, for many people living with dementia, they remain out of reach.
What I hope others will do
The next group of learnings emerged from the time I spent listening to others on the walk.
People living with dementia are often seen as incapable of learning, contributing to society or making decisions. But this simply isn’t true. We may need more time. We may need your patience. But we still have something to say.
One of the most powerful things an ex-student named Alison ever said to me was: “Just keep swimming.” It means never give up. This sums up how I manage my diagnosis on a daily basis.
What I wish for the world
The final group of learnings looks outward, at how society views dementia as a whole.
We need to stop thinking of dementia as just cognitive decline. It’s more than that. It touches your identity, ability to connect and find meaning.
We also need to shift from awareness to action. A “dementia-friendly” community isn’t just a slogan, it’s one where I’m treated as an equal. Where people don’t walk away when I struggle to find a word.
And finally, we need to reimagine how we invest in dementia. Research is vital, but not just in new drug treatments, in better support for people living with dementia.
One unforgettable moment
There were so many moments I could write about, the late-night pizzas, walking along the cobblestones, the people I now consider lifelong friends. But the one that stays with me is the moment we arrived in Santiago de Compostela.
Hundreds of people clapping. A shared sense of achievement and being part of the world around me. And Ron, in his wheelchair being carried by fellow walkers up the final stairs, simply because he wanted and deserved to be there.
That was memorable. That’s the kind of world I want to live in.
What now?
I’ve shared these learnings widely: on LinkedIn, with dementia organisations, and at conferences around the world. I still get people contacting me to ask if they can use these learnings.
Ultimately, Walk the Talk for Dementia wasn’t just about me.
My hope is simple: that these learnings help shape a world where people living with dementia are seen, heard, and supported to live a more enjoyable and meaningful life. ●
William “Bill” Yeates is a living experience associate consultant for The Dementia Centre; in July 2025, he accepted a position on the board of Alzheimer’s Disease International as the representative with lived experience of dementia

My learnings from Walking the Talk for Dementia
1. I want to experience, feel and uphold my connection and involvement in the world around me.
2. I want to live in an inclusive, dementia-friendly community that respects my rights as a human being.
3. I want to retain my independence and dignity and for as long as possible.
4. I want to show the world that with the right help, care and support, we can learn how to live well with dementia.
5. I want to talk about the importance of adopting a holistic, person-centred approach in managing my diagnosis.
6. I want you to accept that where I may struggle to learn new things, it doesn’t prevent me from growing as a person.
7. I want you to know that by adopting the motto “Just keep swimming”, I haven’t and will never give up on life.
8. I want you to look beyond my diagnosis and see the person I am and have always been.
9. I want you to walk alongside me, and be my companion, as I travel through my journey with dementia.
10. I want you to work with me and help me as I make decisions on how I want to lead my life.
11. I want the world to recognise that despite our diagnosis, we retain many strengths and there is still so much that we can do.
12. I want the world to accept that dementia not only impacts on the person living with dementia but also our loved ones.
13. I want the world to appreciate that dementia is more than just cognitive decline.
14. I want the world to understand that without research there is no ray of hope.
15. I want the world leaders to understand that there is an urgency to prioritise the development and implementation of their dementia action plans and frameworks if we are going to move forward in our fight against this condition.
Copyright © William Yeates 2025
Australian Ageing Agenda’s regular dementia section is guest edited by The Dementia Centre, HammondCare. For further information contact hello@dementiacentre.com
L to R: Bill Yeates and other walk participants John Crowley, Allan Young, Natalie Ive, Trish Springfield, Br John-Richard Pagan, Jay Reinstein, and Laurie Waters (front row)
UV tech reduces respiratory infections
Germicidal ultraviolet light devices are a promising innovation for aged care homes and their residents, write PROFESSOR GERAINT ROGERS
and DR ANDREW SHOUBRIDGE.
Each winter, common respiratory viruses spread quickly through the Australian population. For most people, these infections cause only a few days of discomfort. However, for our aged care residents who may be experiencing significant age-related frailty and existing health conditions, the consequences can be far more serious.
During the Covid pandemic, people aged 65 and over accounted for 95 per cent of deaths related to the virus, and outbreaks in our aged care facilities often resulted in death rates above 50 per cent. The speed at which infections moved through our shared living environments was deeply concerning, with outbreaks often affecting most residents despite the best efforts of care staff.

The impact of the pandemic made it clear to us that we need better strategies to control how respiratory viruses spread in aged care settings, especially through the air. At the time, the tools we had – such as physical distancing, wearing masks, hand washing, and cleaning surfaces – were focused mainly on transmission through cough droplets or direct contact. We had very few practical ways to deal with airborne transmission, which involves much smaller particles that can stay in the air for much longer and travel farther.
In response, our research team in South Australia explored whether germicidal ultraviolet light devices could help prevent the spread of respiratory viruses in our aged care facilities. These devices use UV light to make viruses in the air non-infectious. They offer protection not just against Covid, but also against common seasonal viruses and future outbreaks.

While the effectiveness of this technology had already been shown in laboratory settings, we did not know how well it would work in actual aged care environments. Our findings, which we recently published in JAMA Internal Medicine, aimed to close that gap. Led by Professor Geraint Rogers, we designed a clinical trial to study the effect of UV devices in communal areas across facilities operated by Helping Hand, Eldercare, and the Riverland
Mallee Coorong Local Health Network. We placed the UV devices in shared spaces such as dining rooms, hallways, indoor courtyards, and lounges. To keep the project affordable and avoid disrupting residents, we did not install any devices in private rooms. We then randomly assigned these spaces to begin the trial in either an active phase, with the devices turned on, or a control phase, with the devices turned off. Every six weeks, the spaces would switch between the two phases, and we continued this pattern for two years. We measured the impact of the intervention by tracking how many cases of acute respiratory infections occurred during each phase.
The results were encouraging. During the active phases, the number of respiratory infections dropped by more than 12 per cent. That translates to about 92 fewer infections for every 1,000 residents each year.
Since these infections can make aged care residents three to nine times more likely to be hospitalised and nine to 11 times more likely to die, this reduction could significantly improve health outcomes. It could also ease pressure on hospitals and healthcare services. Our results suggest that using UV technology more widely could be a strong way to protect residents.
As new respiratory viruses continue to emerge more frequently, we believe that UV light can play a key role in helping our sector be better prepared for future pandemics. More importantly, this technology allows us to rethink seasonal viruses like influenza and RSV. These illnesses
should no longer be seen as an unavoidable part of ageing, but as a disease burden we can actively prevent.
Scan the QR code to access the paper ●
Professor Geraint Rogers leads Microbiome and Host Health research at the South Australian Health and Medical Research Institute and a research team at Flinders University
Dr Andrew Shoubridge is a post-doctoral research scientist whose work focuses on improving health outcomes in later life
Dr Andrew Shoubridge (left) and Professor Geraint Rogers
An illustration of germicidal UV light in aged care
Credit: Flinders



Human-centred innovations
Executives tour a Melbourne home to see technology that is revolutionising the aged care experience. NATASHA EGAN reports.
For Medical and Aged Care Group, innovations such as robots and virtual reality both modernise care and enrich residents’ lives in joyful, meaningful and dignified ways.
When implemented thoughtfully, they can truly revolutionise the aged care experience, says the family-owned provider, which has nine aged care homes in Melbourne. To share their experiences and insights, MACG welcomed 10 aged care executives to Casey Aged Care in Narre Warren in May 2025 as part of a SAGE Study Tour.
The Melbourne SAGE program included a small group tour designed for executives of small to medium providers over three days. MACG was among eight host organisations.
At Casey Aged Care, the tour showcased MACG’s use of companion robot Abi, SilVR Adventures’ immersive VR experience, and Sensory Wizard, the interactive projection technology for occupational therapy and engagement.
“Innovation for us is deeply human-centred,” says Cameron McPherson, chief executive officer of MACG.
“Whether it’s through robotics, VR, specialised care environments, every step we take is guided by the belief that technology should really empower, enhance and deepen our human connection, never to replace them,” McPherson tells Australian Ageing Agenda
“These innovations are most impactful when they are thoughtfully integrated into the care ecosystem and supported by the warmth, empathy, and intuition of our care staff. Embracing that personal connection is essential to unlock the full benefits of what technology can offer.”
The tour aimed to share both the experience and impact of these digital tools on the lives of residents. It was led by Judy Martin, executive lead of SAGE International at Anchor Excellence, and attended by aged care leaders from Shepparton Retirement Villages, Helping Hand Aged Care, OneCare, TULICH, Optimum and Cykel Architecture.
Tech snapshot
MACG evaluates tools on how they help residents feel connected, cared for, and engaged. Abi, the AI-powered robot from Australian company Andromeda, for example, has become a valuable part of the resident engagement strategy.
Abi can converse with residents in their native language, respond to song requests, initiate games and group conversations, and engage in topics aligned with residents’ interests.
She stimulates cognition, encourages interaction, and helps break down barriers between isolated residents. Her visits to MACG homes generate excitement and spark ongoing conversations.
MACG has also observed that Abi-led group sessions yield higher participation rates and more sustained interest than traditional group activities. And residents continue discussing her activities well after the sessions, boosting social engagement and wellbeing.
The rollout of SilVR Adventures’ immersive and multi-sensory VR experiences, for example, is allowing residents to virtually revisit meaningful places, explore new environments, and engage in group travel experiences.
VR stimulates memory and fosters reminiscence, which can provide emotional and psychological benefits. In one example, MACG residents reliving travels from decades ago led to storytelling and bonding among peers, carers, and family members.
McPherson wants his peers to know the outcomes of using these technologies have been “overwhelmingly positive”.
“For other aged care organisations considering the introduction of technology and innovation in their care environments – we couldn’t recommend it more.”
He shares the following tips for success:
Start with the why: Clearly define the outcomes you’re hoping to achieve – be it reducing social isolation, stimulating cognitive activity, or enhancing multicultural engagement.
Pilot in small groups: Trial new tech with a small group of residents to identify what resonates and use those insights to refine broader rollouts.
Train and empower staff: The enthusiasm and confidence of a care team is essential. Provide hands-on training and help them see the technology as an ally, not a replacement.
Keep it personalised: Choose technologies that can adapt to each resident’s needs, history, and preferences. Whether it’s Abi speaking to someone in their native language or SilVR Adventures transporting a resident to their hometown –personalisation is the magic.
Involve families: Sharing these innovations with residents’ families creates excitement and strengthens trust. It’s also a wonderful way to co-create meaningful content, like personalised VR experiences.
“The transformation we’ve seen in resident engagement, emotional wellbeing, and interpersonal connection has been nothing short of profound,” McPherson tells AAA. ●
Abi the robot, SilVR Adventures’ immersive VR experience and Sensory Wizard are among innovations at Medical and Aged Care Group homes.






Australia’s newest event dedicated to improving aged care, Positive Ageing Summit returns in 2026 for its second year. The summit will bring together experts, healthcare professionals, providers, and policymakers to explore the importance of transforming care for older Australians. Whether you’re on the board or the frontline, this two-day event is your opportunity to gain actionable insights and connect with industry peers.
Healthy reasons to get some pork on your fork
• Pork is an excellent source of protein for everyone, for healthy bones, muscle recovery and growth*.
• Pork is packed with thiamin for energy production and niacin to support mental health and mood and reduce fatigue in the grown-ups*.
• Pork is a source of phosphorus, magnesium and Vitamin B12 for children aged 1-3 years, which supports kids' growth and development*.
• Pork fillet, leg steak, and pork strips are even low in fat and low in saturated fat.
• Pork fillet, leg steak and shoulder roast contain folate, which is important for healthy pregnancy*.


