









The latest survey from the Local Government Association makes for sobering reading.
More than a third of councils—and almost half of those responsible for social care—say they will likely need emergency government bailouts to set budgets over the next three years.
This is not a crisis on the horizon; it is a crisis in full view, and one that threatens the very foundation of social care provision across the country.
But one has to admit: there really is no quick fix for this.
Emergency bailouts are, by their very nature, shortterm solutions that paper over the cracks without addressing the underlying structural failures.
They provide temporary relief whilst simultaneously normalising a state of perpetual crisis. As we reported in October 2025, the LGA itself warned that bailouts risked becoming 'normalised'—a prescient observation that has, regrettably, come to pass.
This week alone, we reported that eight in 10 councils warn they will become insolvent over mounting deficits related to the cost of supporting children and young people with special educational needs and disabilities.
The pattern is clear and deeply troubling: councils lurching from one financial crisis to another, held together by emergency measures that do nothing to prevent the next emergency.
I am by no means an economic guru, but we also produce a title for the hospitality and pub sector, and regularly report on the dire state that industry finds itself in. You will have seen it in recent weeks—it has been all over the news.
High taxes, job losses, falling sales. The hospitality sector is struggling, retail is struggling, and the social care sector is struggling.
My point being this: an economy showing little to no growth cannot sustain its commitments. There is a limit to how much can be extracted through taxation before the well runs dry.
The country needs growth—real, sustained economic growth—if we are to ade-
quately fund the public services we all depend upon. Without it, we are simply shuffling the deckchairs on the Titanic, moving money from one struggling sector to prop up another, all whilst the ship continues to sink.
Of course, I accept that whilst increased funding through economic growth is widely seen as necessary to address the chronic underfunding of social care, it is not the only solution.
Sustainable improvement requires a combination of increased investment, structural reform of the system, and workforce development. Throwing money at a broken system will not fix it; we need to rebuild the foundations, as sector leaders repeatedly point out.
The demand for social care services is increasing relentlessly, driven by an ageing population and a growing prevalence of chronic health conditions.
The Office for National Statistics projects that by 2040, the number of people aged 85 and over will have more than doubled, reaching approximately 3.2 million. This demographic shift places immense pressure on the social care system and requires a fundamental re-evaluation of how we allocate resources.
This new challenge will not be met unless we undertake a radical review of how we allocate resources and move as far downstream as possible—shifting from a reactive model to a preventive one.
We need to invest in community-based support, early intervention, and preventive care that keeps people healthy and independent for longer. We need to reform commissioning practices, improve workforce recruitment and retention, and embrace technology and innovation.
Like many, I am fearful of simply handing this enormous bill and problem to the next generation. Our children and grandchildren will inherit not only our ageing population but also the consequences of our failure to plan adequately for it.
If we do not act now—with courage, vision, and a willingness to make difficult decisions—we condemn them to an even more severe crisis than the one we currently face.
Emergency bailouts may buy councils time, but they do not buy solutions. They do not create the economic growth we desperately need.
They do not reform the system. They do not develop the workforce. They do not prepare us for 2040. What they do is kick the can down the road, ensuring that when the next crisis arrives—and it will—it will be even more severe and even more difficult to manage.
I would encourage our readers to sign up for our bi-weekly digital newsletter at www.thecareruk.com and follow us on social media for all the latest news.
I can always be contacted at editor@thecareruk.com
The Carer is published by RBC Publishing Ltd, 3 Carlton Mount, 2 Cranborne Road, Bournemouth, Dorset BH2 5BR. Contributions are welcome for
no
will be
or damage. Views expressed within this publication are not necessarily those of the publisher or the editorial team. Whilst every care is taken when
the
will assume no responsibility for any effects, errors or omissions therefrom. All rights reserved, reproduction is forbidden unless written permission is obtained. All material is assumed copyright

The LGA survey shows budget-setting will be another hugely challenging task for many councils this year and beyond. It found that, of those which responded:
Almost 6 in 10 councils told the LGA it will be fairly or very difficult to set a balanced budget in 2026/27.
While 8 in 10 councils feel they will be able to meet their minimum legal duties in 2026/27, this number halves to 43 per cent by 2028/29.
More than a third (34 per cent) of councils have already applied or are very or fairly likely to apply for Exceptional Financial Support (EFS) in at least one of the financial years between 2026/27 and 2028/29. INCREASE COUNCIL TAX
These EFS arrangements have allowed councils to cover day-to-day revenue costs by borrowing or with capital receipts. In some cases, this has seen councils able to increase council tax above current referendum limits.
Earlier this week seven local authorities responsible for social services have received government approval to increase council tax beyond the typical 5% limit, reflecting the severe financial strain these councils face.
The announcement came as part of England's local government finance settlement, released by the Ministry of Housing, Communities and Local Government (MHCLG). The settlement also revealed increased funding allocations for areas experiencing deprivation and for homelessness support services.
Under the Families First Partnership (FFP) programme aimed at transforming children's social care, councils will receive £2.4 billion over three years. This funding is intended to support the development of family help services, multi-agency child protection teams, and family group decision-making meetings.
According to a parliamentary statement from Alison McGovern, the initiative seeks to transition the system away from costly statutory intervention toward early intervention and preventative measures.
The settlement includes an estimated £4.6 billion in additional adult social care funding for 2028-29 compared with 2025-26 levels, as outlined in earlier announcements. Within this allocation, £500 million has been earmarked specifically for implementing the sector's first fair pay agreement for care workers.
Ms McGovern indicated this funding would result in a larger, better-compensated care workforce with
adequate time to deliver high-quality, compassionate care.
However, the LGA insists these arrangements are not a sustainable way of managing council finances and plugging funding gaps.
The LGA is calling on government to provide a significant increase in resources in the imminent final Local Government Finance Settlement to protect the financial sustainability of councils and our local services and empower councils to unleash growth and service reform at scale.
It said government also needs to commit to deeper, long-term reform of local government finance, including a cross-party review of council tax, business rates retention and other funding sources.
Councils also urgently need clarity on SEND funding and a credible plan to address growing high-needs deficits, which are the result of structural under-funding.
Cllr Louise Gittins, LGA Chair, said: “This research underlines the reality facing councils.
“Councils are doing everything they can to protect the services people rely on but demand and costs continue to rise faster than funding, leaving many with no choice but to consider emergency financial support.
“Short-term fixes will not address these challenges. Councils need sustainable funding and reform so they can focus on prevention, growth and delivering the services communities expect.”
Unite general secretary Sharon Graham said: “This report must act as a wake up call to government. When councils go bust, it is workers and communities that pay the price.
“Time and again we have seen councils reach for the lever to cut jobs and services. This is austerity by any other name.
“We need real investment in our public services and this must be paid for through a wealth tax and local authority debt relief.”
Rachel Harrison, GMB national secretary, said: “Fourteen years of Tory underfunding has had devastating impacts on local government services and workers.
“This year’s pay offer must be fully funded for all councils and schools to ensure no more services are cut and jobs lost to plug the funding gaps.”

By Barry Price, Content Operations and Delivery Manager of QCS,

The Social Care sector remains stuck at a crossroads. Workforce shortages, regulatory uncertainty and rising financial pressures continue to provide unprecedented challenges for providers. According to Skills for Care, around 111,000 posts remain unfilled, representing an 7.0% vacancy rate, these figures are still high compared to other UK sectors. At the same time, providers face constrained fee rates, surging costs: utility bills and water rates have risen by up to 50%, alongside increases in the living wage and National Insurance contributions. Smaller operators are disproportionately affected, accelerating consolidation across the sector.
In this environment, the question is clear: how can providers maintain quality services whilst navigating these pressures? The answer partly lies in connected technology, joined-up data and intelligent systems that support teams to work smarter, not harder.
Recruitment and retention have become critical pain points. With vacancy rates at historic highs, care and support teams are stretched thin, leading to burnout, increased risk and contract hand backs. Traditional approaches, manual processes, fragmented systems, and siloed data only compound the problem. Staff waste valuable time searching for compliance information or duplicating tasks, time that could be spent delivering face to face support.
Connected technology changes this dynamic. By integrating care management, compliance, and learning into one ecosystem, providers can streamline workflows and reduce administrative burden. Intelligent solutions like Lyra, our latest AI innovation, gives teams instant access to the information they need, whether it’s a compliance update, a care and support plan or a learning resource at the point of need.
According to the Department of Health and Social Care an estimated 30 million administrative hours will be saved per year through this digital-first approach so carers can spend more time looking after those with care needs, giving back at least 20 minutes per care worker per shift.
FINANCIAL PRESSURES: DOING MORE WITH LESS
The financial strain on providers is intensifying. Many local authorities are increasing fees paid to providers, but only by modest amounts (typically mid-single digit % increases), Rising utility costs, wage

to Blue Rain - our activity store is built on over
increases and NI contributions are squeezing margins, particularly for smaller operators. Many are forced to consider consolidation or exit the market altogether. In this climate, efficiency isn’t optional, it’s essential.
Connected systems deliver measurable cost savings by reducing duplication, minimising risk and improving resource allocation. For example:
Compliance automation reduces time spent on audits and inspections.
• Integrated learning tools cut training costs while improving staff capability.
Real-time insights help managers make informed decisions, avoiding costly errors.
Minister of State for Care, Stephen Kinnock, has said “A one-stop shop for a person’s care informationsecurely available to carers - cuts paperwork, helps reduce errors and gives carers more time to care”. Our one system approach exemplifies this. By bringing care management, compliance, and learning data together in a single platform, powered by Lyra’s intelligence, providers can unlock efficiencies that directly impact the bottom line. Instead of juggling multiple logins and disconnected tools, teams have one secure login, one source of truth and one partner committed to raising the standard of care everywhere.
The future of health and social care is connected, intelligent and human. Technology isn’t replacing people, it’s empowering them. When data flows seamlessly across systems, providers gain clarity and control. Risks are reduced, compliance is strengthened and staff are freed to focus on delivering compassionate person centred care.
AI technology like our own AI advisor Lyra, transforms how teams engage with content. Instead of searching through policies, they can simply ask questions and receive precise answers instantly. This not only saves time but builds confidence and capability, creating a more knowledgeable and resilient workforce.
As Skills for Care highlights, investment in workforce development and digital tools is key to sustainability. Providers who adopt connected technology today will be better positioned to thrive tomorrow.
The challenges facing the social care sector are real and urgent. Regulatory uncertainty, Workforce shortages and financial pressures won’t disappear overnight. But by embracing connected technology, joined-up data, and intelligent systems, providers can navigate complexity, protect margins and deliver consistently better outcomes for those who use our services.
At QCS, we believe in a better future. One where social care is connected, intelligent and human. With Lyra and our One System approach, we’re helping providers turn data into insights, insights into action and action into better outcomes for every person, every day.
For more information see the advert on page 15.


• We specialise in the sale and purchase of quality used wheelchair accessible vehicles and ambulances.
• They can be bought as seen or refurbished and sign-written to your own requirements.
• Fully serviced, new mot & warranty
• Engineers inspection supplied if required.
• Free delivery service
• All buses comply with new legislation
•


The Competition and Markets Authority (CMA) has opened a formal investigation into major property deals that could reshape the ownership landscape of more than 600 care homes across the country.
The Competition and Markets Authority confirmed it is examining multiple transactions involving Welltower Inc, an American healthcare real estate investment trust, and several prominent UK care providers including Barchester Healthcare and HC-One.
The watchdog has imposed interim measures requiring HC-One and Welltower to maintain separate operations whilst the investigation proceeds. Such enforcement orders are standard practice during merger reviews to prevent premature integration.
According to official documentation, the CMA’s inquiry encompasses 46 separate property transactions spread across arrangements with four operators: Barchester, HC-One, Aria Care and Danforth Care. These deals collectively involve facilities throughout England, including significant numbers in the North East.

HC-One, which maintains its headquarters in Darlington, operates extensively across the region alongside Barchester’s numerous sites.
Welltower describes itself as a real estate investment trust specialising in senior living and healthcare
properties. The company, publicly traded in New York, reports a market value exceeding $135 billion and owns interests in over 2,000 senior housing communities spanning the United Kingdom, United States and Canada.
The CMA initiated its enforcement order on 3 February following a consultation period that began in mid-January. The regulator has not yet published a timetable for completing its assessment.
Corporate filings from October reveal the substantial scale of Welltower’s UK expansion strategy. The company disclosed acquiring Barchester’s property portfolio for approximately £5.2 billion, encompassing 111 operating facilities, 152 sites under long-term lease arrangements, and 21 properties currently under development.
The documentation indicates Welltower has established what it describes as an “exclusive long-term partnership” with Barchester as part of the arrangement.
Regarding HC-One, Welltower reported purchasing complete equity ownership of the operator’s UK portfolio for £1.2 billion in October, whilst simultaneously settling an existing £660 million loan facility.
The CMA’s investigation will examine whether these consolidated ownership arrangements could reduce competition in local care home markets or otherwise harm consumer interests.
Amberley Hall Care Home in King’s Lynn, Norfolk, marked its 20th anniversary on 29 January with a community-wide celebration that blended heartfelt recognition with high-stakes fun.
Dressed in their best for a “Casino Royale” theme, residents, families, and guests gathered in the home’s café, which had been transformed into a stylish casino floor, minus the real gambling. The goal: create a festive atmosphere while honouring the care home’s legacy of support, continuity and community over the past two decades.
Among the guests was Amberley Hall’s longest-serving resident, who has lived at the home since it first opened. Their 20-year stay became a focal point of the afternoon, reflecting the home’s commitment to long-term, personalised care.
The event drew a mix of visitors, some planned, others spontaneous. One guest said she had simply stopped by to visit a friend,

only to find herself swept into a full-blown party. “It was a welcome surprise filled with entertainment and fun,” she said.
Entertainment came courtesy of local singer Emily Blake, who performed live to a warm crowd of residents and staff. Meanwhile, casino-style games like blackjack and roulette offered light-hearted competition. Residents played for mock money, later exchanging winnings for prizes such as bottles of wine and hamper boxes. Even members of the local NHS community got involved. Paramedics and therapists visiting residents were invited to enjoy the buffet, underscoring Amberley Hall’s open-door relationship with the wider healthcare network.
The day closed with a tribute to Amberley Hall staff, many of whom have dedicated years to the care home. Team members were honoured with long-service awards ranging from five to 19 years.

Everyone has different eating habits and food aversions, and this is no different as we progress into later life. In fact, these challenges can escalate as appetite often decreases with age. This is why personalised care plans, including flexibility around food choices, are so important in care homes. The experts at Elmfield Care share how they put this into practice and how other care providers can follow suit.
Esther Cambridge, general manager of Flowers Manor care home, shares: “As we age, our metabolism slows down, and our sense of taste and smell can change. There are specific reasons for this, including medical conditions such as dementia and Parkinson's that can lead to a diminished sense of hunger.


Medication can also have side effects that affect appetite, such as nausea, dry mouth, altered taste perception, or gastrointestinal discomfort. Reduced physical activity can also play a role, as being more sedentary slows down digestion, which can further suppress appetite.”
What are the health risks linked to appetite loss?
Naomie Griffith, general manager of Nodens Manor care home, explains: “There are a number of risks for the ageing population when appetite is diminished. These include malnutrition and unintended weight loss, a weaker immune system that makes it harder to fight off illnesses, as well as muscle weakness, which can increase the risk of falls, fractures and hinder independence.
“A lack of key nutrients that would usually be obtained through a balanced diet, including B vitamins and omega-3s, can contribute to memory problems, confusion and cognitive decline.”
HOW CAN CARE STAFF SPOT APPETITE PROBLEMS IN THEIR RESIDENTS?
Michael Berkley Blezard, general manager of Old Sarum Manor care home, says: “There are many warning signs that residents might display when they are not eating enough. One of the most obvious is sudden, unexplained weight loss. Another key sign is fatigue and weakness, which can make everyday tasks they were previously able to manage more difficult, such as struggling to hold up a newspaper or concentrate on a crossword.
“Other signs include noticeable changes in eating

behaviours, such as skipping meals or no longer enjoying their favourite foods. Care staff might also find food left uneaten after mealtimes or untouched snacks, indicating a growing disinterest in regular eating.
“Some signs can be harder to spot, including increased difficulty with chewing or swallowing. This could be linked to dental issues or dry mouth, but it can easily go unnoticed if not verbally communicated. Additionally, changes in mood can also be associated with a decreased appetite, although this can be harder to directly link to eating habits.”
HOW CAN CARE HOMES ADAPT?
Esther shares how care homes can support those who are struggling: “There are many ways to approach appetite issues, and what works will vary from resident to resident, so it is important to trial different approaches until you find what works best. Being consistent with mealtimes and involving residents in food choices may help. You can also make mealtimes more sociable, if that is something the individual enjoys.
“Another effective approach is offering smaller, nutrient-dense portions more frequently throughout the day, such as every three to four hours. Making meals visually appealing through colourful fruit and vegetables, as well as thoughtful presentation, may also help encourage appetite.
“Supporting good hydration throughout the day is also important, as dehydration can impact how someone feels about eating. Gentle movement, whether it be through light exercise or short walks, can also help stimulate hunger in older people, whilst improving overall wellbeing.”
Why are personalised care plans so important?
Naomi shares why tailoring care for residents is so important: “Every person is different, and this remains true as we age. These individual differences mean that care needs can vary significantly from resident to resident within care homes.
“By personalising care plans around specific food needs, such as dietary requirements or individual preferences, care homes can ensure residents’ needs are fully met. This helps to support healthier and more fulfilling lives.”
In April 2025, the Supporting the Provider Market (STPM) team in County Durham published a new report evaluating the use of pobroll® — a waterproof bed-bathing wrap designed to improve dignity, comfort, and ease during personal care.
Written by Pat O’Brien of pobroll

This evaluation was carried out across 10 care homes with high numbers of residents living with dementia. Each setting was given one or more pobroll® units and invited to share feedback through a structured survey. The findings reveal how even simple tools can make a significant difference in everyday care.
How was pobroll® used?
Most care homes used pobroll® daily or several times per week, showing it quickly became part of regular practice. Staff noted that one of the biggest challenges was not having enough units — all homes requested additional stock after the trial, highlighting a clear appetite for wider adoption.
What did care teams think?
Feedback from the care homes showed strong support for the tool:
Ease of use was rated highly, with an average score of 4.4 out of 5. Staff found pobroll® straightforward to incorporate into care routines.
Training was rated slightly lower, at 3.8 out of 5, suggesting that while the wrap is easy to use, additional training resources could improve onboarding for new users.
Resident response was positive. Three in ten care homes reported improved mood or behaviour dur-
ing bed bathing for dementia patients.
• Key benefits included greater warmth, coverage, and dignity for residents, especially those who might find conventional methods distressing. Some teams also found it particularly useful for end-of-life care Would they recommend pobroll® for bed bathing for dementia patients?
Absolutely. Homes rated their likelihood to recommend pobroll® at 4.3 out of 5, with half of respondents giving it a full 5 out of 5. The overall feedback was clear: this is a valued, meaningful addition to personal care.
Would they recommend pobroll® for bed bathing for dementia patients?
The results of this trial reinforce what many professionals already believe — that small, thoughtful design changes can significantly improve care. For residents who are bedbound or living with dementia, personal care can often be a distressing experience. But with the right tools, it doesn’t have to be.
The pobroll® isn’t a complex device. It’s a simple, dual-layered cotton towelling wrap. But its thoughtful design — offering full coverage, comfort, and support — makes a real difference where it matters most.
If you’re part of a care home, hospice, or hospital and would like to explore how pobroll® could benefit your residents or service users, get in touch. We’re here to support compassionate, dignified care — one small change at a time.
See the advert on the facing page for details, or
The government has initiated consultations on reorganising social care responsibilities across approximately one-sixth of England's council areas, potentially affecting thousands of social care professionals.
The proposals would see 28 of the 153 councils currently responsible for children's and adult social care undergo boundary changes as part of the government's wider initiative to eliminate two-tier local government structures throughout England.
Under existing arrangements in two-tier areas, county councils oversee key services including social care, education and transport, whilst district authorities manage functions such as waste collection, housing and planning applications.
The government's restructuring plans aim to establish unitary local authorities across the country, typically serving populations of at least 500,000 residents. Ministers argue this approach will deliver improved efficiency, effectiveness and faster decision-making processes.

Presently, 132 of the 153 social services authorities operate as unitary bodies, with 21 county councils managing children's and adults' services in the remaining areas. The reorganisation will also impact 20 smaller unitary authorities neighbouring the affected counties.
The restructuring process requires affected councils to submit reorganisation proposals to ministers. The government will then consult on these submissions, either as presented or in amended form, before making final decisions on which proposals to approve.
Following ministerial approval, legislation will be introduced to establish new council structures, with timetables set for elections and the commencement of operations for the new authorities.
Social workers and other social care staff employed by affected councils will transfer to the newly established bodies under the Transfer of Undertakings (Protection of Employment) Regulations 2006 (TUPE). This legislation safeguards employees' existing terms and conditions of employment and ensures continuity of

service is maintained throughout the transition.
Cllr Matthew Hicks, Chair of the County Councils Network, said: “The launch of the consultation period for the remaining 14 areas invited to submit reorganisation proposals is an important milestone. These reforms represent the largest and most complex changes to local government in generation, so we urge all stakeholders and local residents in each area to engage with the consultation.
“County councils have worked hard to put forward ambitious, evidencebased proposals that will improve services and deliver fewer, leaner councils: fully in line with the government’s stated criteria. Conversely, some of the competing proposals put out to consultation risk splitting high performing care services into smaller councils – well below the stated criteria. At the same time, they promise hundreds of millions of in savings to adult and children’s services with little supporting evidence.
“It is vital that the government uses this consultation period to closely scrutinise and rigorously evaluate all proposals against their own statutory criteria. Crucially, all final decisions by ministers on which proposals to implement, starting with those in Devolution Priority Programme areas due next month, must be evidence-based and not politically driven. The decisions will shape local areas for years to come, so it is vital they ensure any new councils are able deliver savings to reinvest in frontline services, safeguard care to the most vulnerable and foster the economic growth this country desperately needs.
“Building on our experience of working through dozens of reorganisation programmes over the last two decades, the County Councils Network will continue to support its member councils’. This will include engaging the government over their timescales for implementation this parliament, recognising the views of all our member councils.
The team at Sanctuary Care’s Breme Residential Care Home in Bromsgrove transported residents to tropical shores with a brilliant Barbados-themed day, an enriching experience designed to bring warmth, fun and connection during the winter months.
From the moment residents’ families and friends stepped into the not-for-profit home, they were greeted with an
immersive Caribbean atmosphere. The reception shimmered with an under-the-sea mermaid theme, while the beachthemed décor and colourful balloon arches created a tropical feeling throughout the building. Resident Carol Bridgewater said: “We danced, laughed and got to experience a bit of sunshine in the winter months. I had the best day – we all did!”



The government has outlined how it intends to manage councils’ accumulated special educational needs and disabilities (SEND) deficits and has announced it will pay 90% of these deficits.
This a direct recognition of County Councils Network (CCN) advocacy over the past few years the network said.
The network has published agenda-setting research on the impact of growing SEND deficits on local authorities and what the future looked like without government action.
The CCN’s research, published last Autumn, projects that these deficits are set to reach £6.6bn next month.
The government has said that it will provide a grant for councils to pay off their deficits in Autumn 2026, subject to each local authority submitting and securing the Department for Education’s approval of a local SEND reform plan.
Cllr Bill Revans, SEND spokesperson for the County Councils Network, said:

“The County Councils Network (CCN) has long called for government to address the worsening special educational needs and disabilities (SEND) deficits crisis, and today’s commitment is a very welcome and crucial step in solving the issue. A pledge that the government will eliminate 90% of councils’ historic deficits
will be a significant relief to our member councils with the deficit set to reach £6.6bn nationally by the end of next month and direct recognition of the CCN’s advocacy.
“The CCN will now engage with its member councils on the impact of these proposals and it is crucial that any long-term solution is also fair to all councils. Alongside this, the government should reform the outdated dedicated schools grant formula to recognise the disproportionate SEND pressures faced by county and rural unitary councils.
“Looking ahead, it is vital that the Schools White Paper sets out comprehensive reform to the SEND system. Councils will do all they can to improve local services and control future expenditure through local SEND reform plans, but previous initiatives such as Delivering Better Value have shown in the absence of comprehensive changes to the system at a national level, councils will be doing so with one arm tied behind their backs.”
For deficits that arise in 2026–27 and 2027–28, the government has said it will ‘take an appropriate and proportionate approach, though it will not be unlimited.’ From 2028–29, SEND spending will be covered within the government’s DEL budget so local authorities will not be expected to fund future SEND costs from general funds.
Dela
Jan, a Registered Nurse at Hilton Park, was praised for her exceptional commitment to residents and their families, as well as the warmth, passion, and enthusiasm she brings to her role every day.
Geanina Tinca, General Manager at Hilton Park Care Home, said: “I’m delighted to have such a caring and talented individual as part of our team. This award is a small way of showing how much Jan’s dedication and hard work are valued.
As a nurse, Jan brings genuine passion and commitment to enhancing the lives of our residents and supporting their families. Known for her warm smile and approach-
able nature, she creates an engaging and comforting environment for everyone in our care.”
Jan was presented with a certificate and award in recognition of her dedication. Reflecting on the honour, she said: “This came as a big surprise to me I wasn’t expect this.. I absolutely love my job, so to receive this recognition for doing something that means so much to me is incredibly rewarding.”
Jan’s compassion, professionalism, and dedication make her an outstanding member of the Hilton Park team, embodying the core values of care, kindness, and commitment that define the home.


your resident's eyes light up when the
products to residents. How about a delicious


lovely trolley


By Chris Hornung, Managing Director, Public Sector, Totalmobile

The year ahead will bring no surprises for the public sector. Budgetary pressure will remain the dominant theme. The next Budget will show how far the government is prepared to go to balance the books, but even with new measures, local authorities and public bodies are unlikely to see much relief.
The squeeze is here to stay for a while more, and that reality will shape every part of the sector in 2026.
The budget will set the tone. If funding continues to tighten, the shift toward preventive community-based care becomes even more urgent – because without it, the system will keep absorbing costs rather than reducing them, forcing further cuts.
Across all services – healthcare, social care, emergency services, infrastructure - the challenge is no longer about doing more with less- it’s about doing things differently. Incremental savings have already been made. What’s left now is real transformation.
HEALTH AND CARE: JOINED-UP BUDGETS, JOINED-UP THINKING
In 2026, we’ll start to see the first moves toward shared budgets between NHS community services and local authority care. At present, those two funding streams often pull against each other. Local authorities focus on prevention but lack the resources to fund it properly. The NHS, meanwhile, is paid to treat people once they are already unwell.
Bringing those budgets together allows for a more joined-up approach, one that supports people earlier and reduces costly, lengthy hospital admissions. Technology will be a key enabler of that change, providing the solutions to monitor and support people safely in their own homes.
POLICING: TRANSPARENCY UNDER PRESSURE
Public confidence in policing has been shaken by recent investigations, including the BBC Panorama investigation into misconduct at Charing Cross Police Station. That kind of exposure will only increase the pressure for transparency.
Forces can no longer operate as closed systems. They will need reliable data to demonstrate account-
ability, who was on duty, where they were, and what actions were taken. This isn’t just about compliance; it’s about trust. Without it, confidence in policing will continue to erode.
LOCAL GOVERNMENT: FROM SURVIVAL TO STRATEGY
From April 2026, councils will return to multi-year financial settlements. Having visibility of budgets beyond a single year allows councils to plan strategically, to invest in transformation in year one and see benefits in years two and three. The current one-year cycle has made that almost impossible.
Councils that use this opportunity to take a more innovative approach - embracing digital solutions, automation, and new delivery models - will be the ones that thrive. Those who remain risk-averse will struggle to keep pace.
Artificial intelligence will start to feature more prominently across public services next year, though adoption will be slower than in the private sector. Caution around data security and public perception will continue to hold some organisations back.
The key will be to use AI safely within existing, secure platforms rather than through open, public systems. When the technology operates inside trusted environments, using data that already sits within the organisation, risk remains low and benefits can be realised faster.
The real risk lies in inaction. The longer the public sector hesitates, the further it falls behind.
Across every part of the public sector, one theme runs through everything: a loss of public confidence. People no longer assume that the services they rely on will deliver effectively. That perception of inefficiency and bureaucracy is difficult to shift, but it won’t change through caution.
Restoring trust requires openness, transparency, and innovation. The public doesn’t expect perfection. They expect progress and they want to see public sector bodies take measured risks, try new things, and deliver services that feel modern, responsive and deliver meaningful change.
The coming year will be another difficult one, but it may also mark the start of quiet transformation. Shared budgets, transparent policing, longer-term financial planning, and practical use of AI all point towards a more connected, forward-looking public sector.
The challenge now is to turn those opportunities into action. The levers are there. It just takes the courage to pull them.
An experienced care professional with more than 25 years in health and social care has been appointed as manager at Cedar Lodge in Brimington, Chesterfield.
Sharon Ricci has taken on the role at the Milewood supported service following a lengthy and varied career across nursing, residential and specialist care settings. She joined Cedar Lodge in September 2024 as deputy manager and has now progressed into the management position.
She began her career as a care assistant in a nursing home before moving into support work across a wide range of services, including learning disabilities and young adults with mental health needs. Sharon later spent time working at Rampton Hospital on the personality disorder wards, before going on to hold home manager roles at several services across Yorkshire and Derbyshire. She has also previously been a registered manager of an elderly residential care home.

Currently completing her Level 5 qualification in Leadership and Management, Sharon brings a strong person-centred ethos to her role at Cedar Lodge, working alongside an established staff team supporting nine individuals.
Sharon Ricci said: “Since starting at Cedar Lodge, I have been privileged to work with an excellent staff
team and to support the individuals in a genuinely homely environment. Every day is different, which is what makes the role so rewarding. Being able to have a positive impact on people’s lives and support them to achieve their goals and aspirations is incredibly important to me.
“I strongly believe that good care and support must be person-centred and built around privacy, dignity and respect, while empowering people to make their own decisions and have control over how they want to live their lives. We achieve this in very practical ways, such as ensuring people’s bedrooms are decorated how they choose, with personalised door signs, colours and furniture that reflect who they are.
“I’m really looking forward to continuing my work at Cedar Lodge, listening to feedback, completing audits and working closely with other managers so that, together, we can continue to thrive.”
Martyn Heginbotham, chief executive of Milewood, added: “Sharon brings a wealth of experience, compassion and leadership to Cedar Lodge. Her commitment to person-centred care, combined with her hands-on understanding of a wide range of care settings, makes her an excellent fit for the service. We are delighted to see her step into the manager role and are confident she will continue to build on the strong foundations already in place.”
The cleaning and facilities management landscape is shifting faster than ever. As we move into 2026, the industry is no longer just about "maintenance"—it’s about technology, sustainability, and the well-being of the people who keep our buildings running. For professionals across the North and beyond, there is one date that needs to be circled in the calendar: 18-19 February.
The Cleaning Show returns to Manchester Central, transforming the heart of the city into a hub of innovation. Whether you are managing a healthcare estate, a retail portfolio, or a growing cleaning enterprise, the challenges remain the same: how do we drive efficiency while managing rising costs and labour shortages?

This year’s event is designed to answer those questions. Moving away from the buzzwords of the past, the show floor is a practical, "boots-on-the-ground" environment where the latest tech—from autonomous robotics to smart building sensors—is available for live demonstration. It’s one thing to see a machine in a brochure; it’s quite another to see it navigating a busy floor in person.
But the show is more than just a showroom. It is a vital meeting point for the industry. The seminar programme features some of the sector’s brightest minds, tackling the issues that matter right now: the impact
of new sustainability legislation, the roadmap to Net Zero, and strategies for better staff retention. In an era of remote meetings, the value of face-to-face networking at Manchester Central cannot be overstated. It’s where deals are struck, partnerships are formed, and the "unfiltered" advice of your peers is shared over a coffee.
For those in the healthcare and social care sectors, the stakes are even higher. The show offers a unique opportunity to source non-disruptive, highperformance solutions that meet stringent hygiene standards without compromising on resident or patient comfort.
Why pre-register? Time is the most valuable asset in facilities management. By pre-registering now, you ensure a seamless entry to the event, bypassing the queues and gaining early access to the exhibitor list and seminar schedule. Most importantly, trade registration is completely free for those who sign up in advance.
Don’t miss the chance to see where the industry is heading. Join us in Manchester this February to find the tools, the tech, and the people that will help you future-proof your business.
Secure your free pass today at www.thecleaningshow.co.uk
Three quarters of hospices in England are already running a deficit this year, new figures reveal, as the sector warns it is heading towards a financial “cliff edge”.
75% of hospices report they are in deficit at this point in the financial year, up from 70% at the same time last year, which was already the worst year on record for the hospice sector.
New data from Hospice UK shows the situation is continuing to deteriorate, with 83% of hospices expecting their financial position to be worse than last year. At least 25 hospices have made cuts to services since April last year, while two in five are planning further cuts in the year ahead.
As a result of the funding crisis, 380 hospice beds are currently out of use across England, despite rising demand for end of life care.
Hospices provide vital care for people at the end of their lives, but the majority of that care is funded through charitable income such as marathon runs, gifts in wills and charity shops. Government funding covers only around 40% of the care that hospices provide.

Toby Porter, CEO, Hospice UK said: “Hospices are stuck in a doom loop. Last year was the worst financial year on record, and this year is looking even worse.
“We can’t fundraise our way out of this crisis, skydiving won’t save hospices. We urgently need fair and
long-term NHS funding to avoid a financial cliff edge.
“With assisted dying potentially on the horizon, we must make sure hospice care is available for everyone who needs it.
“Right now, with many hospices cutting services, it’s a real worry that people might choose assisted dying because they can’t get the care they need.”
Barbara-Anne Walker, Chief Executive of Ashgate Hospice said:
“Outstanding and well-loved and supported hospices like Ashgate are having to close beds and cut jobs and services not because they are not needed but because we can’t afford to keep them open.
“At the same time, we see people dying in hospital corridors and this disconnect in our health system is heart-breaking. We aren’t saying the NHS needs to pay for everything, but there needs to be a much fairer contribution and an end to the postcode lottery which means your likelihood of accessing high quality end of life care depends on where you live.
“We wouldn’t fund maternity care this way – there would be a national outcry and rightly so. We only get one chance to get end of life care right which is why the government needs to step in – we are hopeful that at long last things are going to change.”
Residents at a Lowestoft care home marked a joyous occasion celebrating 90 years of Sir Billy Butlin’s holidays with a very special visitor – ex-Red Coat and 1960s entertainer Steve Hall.
Steve, a regular favourite at The Dell – part of the Wellbeing Care group –brought his signature charm and energy to the care home, performing a selection of beloved songs such as ‘Delilah’ by Tom Jones and ‘She Loves You’ by The Beatles.
Residents and their families joined in with singing, clapping, foot-tapping, and even dancing, creating an inclusive, uplifting atmosphere. Steve’s talent for “working the room” ensured that every resident was involved, bringing smiles and laughter to all corners of the home.
Butlin’s, a popular UK holiday destination with resorts across Minehead, Skegness and Bognor Regis, employs ‘Red Coats’ who perform for and interact with guests to make their stays magical and memorable.
Winnie Percy, aged 95, shared her excitement: “I love his voice and to hear him sing brings me great happiness and enjoyment. I can’t wait for him to return on February 14th for our Valentine’s Day party!”
Joy Henshaw, Regional Director at Wellbeing Care, said: “Steve’s visits are always a highlight. Music has such a powerful way of connecting people and bringing joy, and seeing our residents so engaged and happy is wonderful. Butlin’s is celebrating its 90th anniversary this year, and to share that milestone with Steve really brought the history to life and created magical memories for everyone here.”


There are just 40 days to go until the announcement of the Longitude Prize on Dementia’s £1 million grand prize winner on 18 March 2026 at 1930 GMT.
Since 2022, the £4.4 million global prize has funded and supported the development of 24 different assistive technologies that use AI and machine learning to help people living with dementia remain independent for as long as possible.
Five finalists were announced in 2024, each receiving £300,000 to develop their ideas into real-world products. Each has been codesigned with people living with dementia to ensure each solution meets the needs of its intended end-user. The overall winner will receive £1 million in March to help bring their product to market, making it available to buy soon.
In the running to win the Longitude Prize on Dementia are:
• AUTONOMOUS by Associação Fraunhofer Portugal Research (Portugal), Carnegie Mellon University and LUCA School of Arts: A smart watch companion that helps maintain routine
• CrossSense (UK): AI smart glasses that support with daily activities
• MemoryAid by Western Sydney University and Deakin (Australia): A video phone designed to help stay connected with loved ones
• SenS2 by Supersense Technologies (UK): A household assistant that uses radar technology to map disruptions to routines
• Theora 360™ by Clairvoyant Networks, Inc. (USA): Situational awareness technology designed to help detect and predict falls
While all finalists have developed different solutions, they share the common goals of helping people living with dementia to stay in their homes for longer, continue doing fulfilling daily activities and maintain social interactions. The Longitude Prize on Dementia is funded by Alzheimer’s Society and Innovate UK and delivered by Challenge Works (part of Nesta).

Recent findings from Alzheimer’s Society reveal the critical need for products and services that enable independence and maximise quality of life.
Its Lived Experience Survey 2025 of over 3,000 people affected by dementia[1], found that three-quarters (76%) of respondents – comprising those living with the condition, unpaid carers, and loved ones – say dementia negatively impacts their ability to carry out daily tasks independently, their hobbies (67%) and their self-confidence (64%). People also reported a negative impact on their physical health and their mental health (both 69%).
Around one million people in the UK are living with a form of dementia today and this number is projected to rise to 1.4 million by 2040 [2]. As a progressive condition, individual care needs and the level of support or treatment a person receives will increase over time as their symptoms worsen.
AI-driven technology has the potential to alleviate the emotional and economic demands of care; the cost of dementia in the UK is estimated at £42 billion per year (as of 2024), with people living with the condition and their families shouldering the bulk of the costs.
Dr Jennifer Bute was diagnosed with young-onset Alzheimer’s disease in 2009 at the age of 63, leading to her retiring early from her career as a GP. As a member of the Longitude Prize on Dementia’s advisory panel of people with lived experience of dementia, she said:
“Dementia affects memory and independence. While we wait for more treatments, artificial intelligence is already helping people in the
earlier stages of dementia to live more independently. Everyday technology can remind me about meetings and medication or to read books aloud for me.
“If technologies are built only for carers it can unintentionally reduce independence. To truly protect and prolong independence, technology must always be co-designed with people living with dementia. The five finalists have done exactly that, creating diverse and inspiring technologies that have real potential to improve life after diagnosis and I’m excited about what is now coming.”
Professor Fiona Carragher, Chief Policy and Research Officer at Alzheimer’s Society, commented:
“One in three people born in the UK today will develop dementia in their lifetime and sadly, as symptoms worsen, individuals progressively lose their independence, and with that their sense of self. It'll take a society to beat dementia. Alongside supporting the science that's on the cusp of finding more effective treatments for the future, we're harnessing the huge progress and momentum of tech and AI to help people affected by dementia here and now.”
Caroline Purslow, Head of Global Health, at Challenge Works said:
“Four years ago, we launched the Longitude Prize on Dementia to help meet the urgent need for intuitive technologies that are purpose built for and with people living with dementia – empowering people to lead fulfilling lives, as independently as possible. Fast forward to today, we’re seeing inspiring technologies come to fruition, all of which have the potential to be life changing. Announcing the winner in March will be further evidence of the critical role innovation and challenge prizes have to play in helping to solve some of the biggest challenges of our time.”
Find out more about the five finalists in the running for the Longitude Prize on Dementia at dementia.longitudeprize.org
Care UK’s matched funding scheme has restarted for the new year, and Ridley Manor in High Wycombe was one of the first homes to donate to charity. The care home hosted a festive fair with local stalls and a raffle to raise money for Lane End Village Hall. Residents, relatives and members of the community were immersed in the day, enjoying a buffet, mulled wine, and other treats.
Having raised £400 for Lane End Village Hall, Customer Relations Manager Hayley Devereaux said: “We hold a Christmas fair every year, but each year we choose a different local charity. I'd seen a Facebook post about Lane End Village Hall’s restoration project, and it made perfect sense to get involved. “It is a significant change for the village hall, but we need to make sure we celebrate it as a pillar for the whole community. The majority of Ridley Manor’s

residents have lived in Lane End at some point or they grew up in the village. It’s really important that we keep this community space going.”
As part of Care UK’s matched funding scheme, the home’s original donation was matched, so a total of £800 has now been donated to Lane End Village Hall.
Hayley said: “It's fantastic to be in the position to give back to your local community. Obviously we can't always raise a massive amount, but for Care UK to match it, it makes a real difference for local charities and their causes.” Throughout January, Care UK matched over £4,000 in colleagues’ donations, with causes ranging from Alzheimer’s charities to bowel and prostate cancer charities, alongside many, many more. In 2025, more than £34,000 was gifted to local and national charities.
The law is changing for care homes, but understanding your obligations has never been easier
Providing both comfort and dignity to those in your care is at the core of the Care homes profession, but when it comes to both residents and their families, one of the most important things you can offer is trust.
Moving to a care home can be an emotional time for some and transparency and fairness are key in reassuring prospective residents and their families that they will be cared for with compassion and respect - This, and compliance with the law.
Earlier this year we saw the introduction of the Digital Markets, Competition and Consumers Act 2024 (DMCCA) - a landmark piece of legislation that affects business and how they are required by law to safeguard their customer with fair trading practices. These changes may sound like legal jargon, but they directly impact how care homes operate, communicate, and contract with residents.
Compliance can be complex and that’s why the Business Companion Care Homes Guidance is essential reading for anyone working in the Care Homes sector. Written by legal experts this free and easy-to-read guide will walk you through all the steps to ensure you are safeguarding your customers and operating within the law.
WHAT’S CHANGED UNDER THE DMCCA?
The introduction of the DMCCA represents one of the biggest shifts in consumer law in over a decade. It replaces the old Consumer Protection from Unfair Trading Regulations and introduces stricter rules to protect consumers from misleading or unfair practices across

almost all sectors. For care homes, this means:
• Clearer Pricing and Transparency: The Act bans “drip pricing” which is when unavoidable fees are hidden until late in the process. Care homes must now present the full cost of services upfront, including any mandatory charges.
Fake Reviews and Misleading Endorsements: The DMCCA prohibits the use of fabricated or manipulated reviews. With care homes increasingly relying on their online reputation, ensuring authenticity is now a legal obligation.
Stronger Enforcement Powers: The Competition and Markets Authority (CMA) can now impose fines of up to £300,000 - or 10% of global turnover - for breaches. Compliance isn’t optional; it’s critical.
• and much more!
These changes underline the importance of reviewing your policies, contracts, and marketing materials. The Care Homes Guidance on Business Companion provides practical steps to help you stay compliant and avoid costly mistakes.
KEEPING CONSUMER VULNERABILITY IN MIND
Vulnerability can arise from a number of different situations and factors throughout a person’s life, such as age, health, bereavement, or financial stress. As someone working in the Care homes sector, you’re
dealing with vulnerable individuals on a daily basis and recognising these factors isn’t just good practice; it’s a legal and ethical responsibility.
The Business Companion Consumer Vulnerability Guide offers checklists and practical advice to help you identify and support your residents who may be vulnerable when it comes to things like decision making and communication, ensuring your care home delivers not only compliance but compassion.
Your Go-To Resource for Compliance
Business Companion is more than just a care home resource - it’s a comprehensive hub for businesses across a broad range of sectors. From selling online to handling complaints, delivery charges, and even net zero strategies, the platform covers hundreds of topics delivered to you through clear, easy-to-read guidance. Backed by the Chartered Trading Standards Institute and the Department for Business & Trade, Business Companion is free, authoritative, and regularly updated by legal experts.
Act Now
The DMCCA is already in force, and enforcement powers are live. Don’t wait for a compliance issue to arise - visit Business Companion’s Care Homes Guidance today. Review your contracts, pricing structures, and communication strategies and explore the wider resources available to future-proof your business against legal pitfalls.
In a sector built on trust, staying informed isn’t just smart - it’s essential.
To find out more, visit: www.businesscompanion.info

A staff member at a Harwich home marked 20 years of service with the home and says she has no plans to go elsewhere.
Amanda Gouldstone started working at MHA Alexandra House in 2006 after she was made redundant in her role as a hairdresser.
Amanda joined the home as a care assistant and has had various roles in her time including being a senior care assistant, reflexologist, and administrative support assistant.
Currently Amanda splits her time between two roles, an activity coordinator and care assistant.
MHA Alexandra House provides residential or dementia care for 47 residents.
To mark her time with the home, Amanda was presented with her long service certificate and a voucher from home manager, Kerry Graves.
Speaking after the celebrations Amanda said: “I feel as if the last 20 years have gone in the blink of an eye.
“Initially when I joined I did find the transition from being a hairdresser to working in care tough.
“I gave myself a month and told myself if I didn't find my feet, I would leave and try

something else, but here I am 20 years later.
“I am so happy I decided to continue and I genuinely love working at MHA Alexandra House.
“I love working with our residents, promoting their independence is something I really enjoy, and I have learned so much from them over the years
“The home is great, we are blessed to be so close to the seafront, which is great for residents especially when it comes to planning activities.
“The presentation from Kerry and the rest of the staff was a surprise, I didn't expect it all, but it was very nice.
“I don't have any plans on moving elsewhere or changing careers, I may decide to go back to the role of a senior care assistant, but that's something I need to think about.
“I am very happy at MHA Alexandra House and will stay as long as I am needed.
“Working in care is very rewarding, my advice to anyone considering a change of career or about to start a career in care would be to give it a go.
“You won't know if it's for you or not until you decide to give it a go, but one thing is for sure, you will really enjoy it, and it does become more than just a job.”
To mark this year’s International Day of Education, Sheila Clitheroe, a resident at award-winning Little Bramingham Farm, the Luton-based residential care home run by charity, Friends of the Elderly, has been reminiscing about her career as a Music Teacher and Choir Mistress.
Sheila has been a resident at Little Bramingham Farm since May 2022, “I love living here, there’s always so much going on. Nearly three and a half years later, I still enjoy every day and can’t believe how quickly the time has flown,” said Sheila.
Sheila spent over 22 years working as a Music and Infant School Teacher - and even after she had to retire early due to a very bad back, still returned to the Education Sector as a Supply Teacher delivering lesson plans, managing classrooms, and ensuring the pupils continued to enjoy their classes and meet their learning objectives.
“I taught at Ramridge Infants School in Luton where I held the School’s Music post as well as being one of the Infant School Teachers for years one and two, so Reception children in today’s schooling,” continued Sheila. “When I started teaching, things were very different to how they are today. For example, the classes were organised in family groupings, so my class of 40 children, consisted of all ages.
“In my role as Music Teacher, I delivered music education to pupils across the entire school. I greatly enjoyed the concerts, rehearsals and lessons, but the most fulfilling aspect was supporting shy children as they found their voice and became confident participants within the group.

“The children were such characters and sometimes a bit cheeky but, on the whole, well-behaved. Once I had to reprimand a pupil for calling someone a ‘Daft Ada’ only to find out that he was chatting about Darth Vader in the Star Wars film. Thinking back to that still makes me laugh.”
Shelia has always loved music, organising the school concerts, musicals and Nativities and she had a special trick for keeping her pupils interested and engaged in her classes and at rehearsals. “I used to sing instructions,” continued Sheila. However, Sheila’s singing didn’t stop there. “At the end of each day the chairs would go up and if I saw anything out of place or laying on the floor I’d sing ‘I see pencil’, which used to get all the children looking around to find the pencil and tidy everything away. It was much better
than shouting at them.”
Sheila’s pupils never played pranks on her; “They wouldn’t dare!” said Sheila. “The pupils were extremely helpful and didn’t play around. When the school got us our first computers back in the early 1980s, they were the Acorn BBC Micros, which where were part of the BBC's Computer Literacy Project. Quite often the pupils could get it working, where I couldn’t,” continued a smiling Sheila. “I had always used a blackboard and chalk, so computers were a totally new thing for me.”
Sheila has many fond, heartwarming - and some moving - memories of her teaching years and pupils. “When I was teaching, there was a different attitude towards safeguarding,” continued Sheila. “It was there and present, but so was trust. I had one pupil who turned up regularly at school, dirty, quite smelly and hungry. I would raid the lost property box for clean clothes, get him to shower to wash and dress and then make sure he had something to eat like toast as there were no Breakfast Clubs in those days.”
After Sheila retired, she took on the role of Supply Teacher at schools in the Stopsley area of Luton and also became a Choir Mistress at her local church. “Perhaps I was looking for a ‘Choir Purpose’,” chuckled Sheila.
“When I first started as the church’s Choir Mistress, I had three eight-year-old Choristers, but I built the Choir up to nearly 35 members which included all vocal ranges – Trebles, Sopranos, Altos, Tenors and Bass voices. My passion has always been encouraging everyone to enjoy music, and I have always been very happy with my choice of career roles,” added Sheila.
“Sheila is a wonderful lady and often talks passionately about her music teaching years,” said Emma Lawrance, the Registered Manager at Little Bramingham Farm. “Shelia takes part in our wide variety of meaningful activities, but without a doubt, she’ll always be at our music-orientated events or sessions, albeit one of our regular singers giving a performance or sharing musical time with our visiting intergenerational group, Musical Bumps; Sheila will definitely be there, singing and joining in.”
“I really wanted to make sure that the pupils’ early years at school were fun, enjoyable and happy. Looking back, I hope that all my pupils – over all the years – thought and felt that I was a caring Teacher who encouraged them to just do their best and never stop trying,” concluded Sheila.
Care & Dementia is the UK’s leading event for transforming social care and improving the lives of people living with dementia. Building on the successful foundation of The Alzheimer’s & Dementia Show and UK Care Week, it creates an essential, dedicated platform for both care professionals and the public.
Taking place on 25-26 March at the NEC in Birmingham, this event represents a powerful evolution in the sector. Combined with the incredible momentum of Naidex, it creates a vibrant environment where vital communities meet to explore best practices, support services, and innovative products.
A WORLD-CLASS SPEAKER PROGRAMME
Carefully curated CPD sessions bridge the gap between industry innovation and personal care. The full programme is now live, featuring expert voices designed to provide actionable insights for every attendee.
CARE KEYNOTE THEATRE

A must-attend for those looking to stay ahead of industry trends. Featuring leading voices from the CQC, Alzheimer's Society, Dementia UK, National Care Forum, and Care England, these sessions explore policy changes, funding models, and the future of the care sector. Sessions include Where is Social Care on the Political Agenda? with Damien Green from the Social Care Foundation. This is followed by a collaborative discussion titled Building Knowledge of the Sector - One Mind at a Time, featuring Amrit Dhaliwal (Walfinch), Samantha Crawley (EQ Care Group), and Sam Monaghan (Chief Executive at Methodist Homes MHA).
DEMENTIA MATTERS THEATRE
This theatre provides practical support for both professionals and family carers. The programme features Dementia devastates lives, innovation transforms them: Alzheimer’s Society Innovation Team (Alzheimer’s Society) and Dementia and Safeguarding - Protecting Rights, Reducing Risks: Kirsty Dallison-Perry (Dementia UK). These are complemented by In Conversation: A Carer’s Perspective: Frances Lawrence (Dementia Carers Count) & Rosie Brooks (Dementia Carers Count) and a highly informative Learn about dementia from people living with dementia Q&A: Ronnie Dean, Beth Britton MBE & George Rook (Dementia campaigner).
INTERACTIVE FEATURES & PRACTICAL SUPPORT
Alongside the conference sessions, the event features a range of interactive experiences designed to provide practical support. Professionals can earn up to 12 CPD points through the accredited programme while accessing tailored advice at the CQC Inspector Hub. New for 2026, visitors can access a complimentary, confidential consultation to explore available options for early dementia or mild cognitive impairment at the Re:Cognition Health Assessment Clinic. For families and caregivers, the event offers 1-to-1 Advice Clinics with Admiral Nurses from Dementia UK, the Dementia Interpreters Workshop, and immersive training experiences like the Virtual Dementia Tour and the Autism Reality Experience. Visitors can also explore the Innovation Hub to discover the latest technologies and solutions for social care and rehabilitation.
Attendance is free. Ensure you are part of the UK’s most significant gathering for the care community. For more information and tickets visit www.naidex.co.uk/careanddementia
A new study of baby name trends spanning the last 100 years has revealed that several nostalgic baby names are back in fashion. The research conducted by Crystal Care Collection, as part of its wider focus on family connection, highlights the intergenerational link between modern families and those living in care homes today. Whilst these names fell out of fashion in the mid to late 20th century, they are now being widely chosen once again, as parents look for classic names that stand the test of time.
The study analysed Office for National Statistics data, comparing the top 100 baby names from 1924 with the most recent figures from 2024, with the top five revived baby names for both boys and girls including:
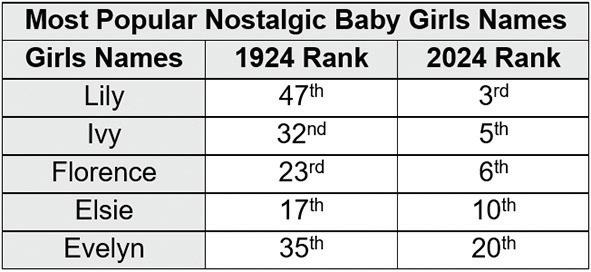
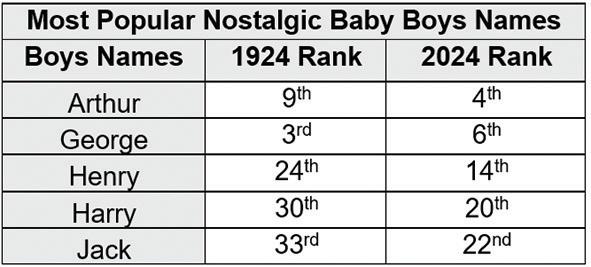
In 1924, these ten names ranked comfortably inside the top 50, reflecting the familiar, heritage-led naming styles common at the time. However, between 1954 and 1984, almost all the names disappeared from the top 100 altogether. Only one (George) stayed in the top 100 list, while the others fell in popularity in the mid-century as modern baby names surged. These drops weren’t short-lived, as some names dipped out of the charts for just two decades, while others fell out of favour for as long as 70 years. By 2024, all ten names not only re-entered the top 100 but soared into the top 25, showing a trend towards classic names as modern parents begin to look back to family-linked, sentimental names.
Residents of Crystal Care Collection have responded warmly to the idea that their names are now some of the most common in nurseries across the country today.
Evelyn, 91, a resident at Furze Field Manor in West Sussex, shares her reaction, “Being called Evelyn always felt quite special because being born in Switzerland in 1934, it was an unusual choice at the time. My mother named me after one of her favourite authors, Evelyn Goodman, who was the writer behind the classic illustration books that she would read to me as a young girl. I’m happy to hear that parents are choosing it again, because they see it as a name with a legacy and a sense of connection to the past.”

Arthur, a resident at Rownhams Manor in Southampton, says, “I was named after my uncle Arthur, but my parents were also inspired by the mythical King Arthur, so it has always felt like a strong name. Although it was quite a common name at the time, I haven’t met many Arthurs born after me, so it is a surprise to see it come back into fashion. But it’s lovely to think that younger generations are choosing names that connect them to their family and the past.”
Jack, a resident at Somer Valley House in Midsomer Norton, added, “My given name is Henry, but instead everyone called me Jack because it was much more popular at the time. It is great to see both of these names are popular again and I think television and films play a big part in nostalgic names coming back.”
Music, memories and a lifelong passion were celebrated at Spynie Care Home recently, as residents were treated to a special visit from the Elgin City Band.
The visit was particularly meaningful for resident John Marshall, who is approaching his 86th birthday and has been part of Elgin City Band for more than 70 years.
Born in 1940, John joined the band in the early 1950s and has remained involved ever since, making him one of its longestserving members. Over the decades, he has played almost every instrument in the band, stepping in wherever needed. His favourite, however, has always been the bass trombone.
John’s musical journey has included many memorable moments, including his first official engagement in February 1952, when the band played at the proclamation of Her Majesty Queen Elizabeth II. He later went on to meet the Queen in per-

son, an experience he still counts among his most treasured memories.
During the visit to Spynie Care Home, John was able to reunite with his fellow musicians and joined in on his trumpet, delighting residents, staff and band members alike. The performance filled the home with music, nostalgia and a strong sense of community, sparking conversations and smiles throughout the afternoon.
Jamie Taylor, home manager at Spynie Care Home, said: “This was a truly special day for everyone, but especially for John. Seeing him reconnect with the band that has been such a huge part of his life, and still being able to play alongside them, was incredibly moving. Music has a powerful way of unlocking memories and emotions, and this visit brought so much joy to our residents.”

In today’s highly regulated health and social care environment, providers face the dual challenge of ensuring compliance while striving to deliver safe, high-quality, and commercially sustainable services. Care Inspections UK Limited (CiUK) has emerged as a trusted partner in this landscape, providing a professional and independent inspection service that goes beyond the standard requirements of the Care Quality Commission (CQC), The Care Inspectorate Wales (CIW) and the Care Inspectorate (Scotland), collectively “The Inspectorates”
What sets CiUK apart is its status as a registered inspection body, operating with the highest levels of professionalism and governance. This official recognition imbues care providers with confidence that inspections are carried out with rigour, objectivity, and an unwavering focus on evidence. Every report is underpinned by validated, research-based methodology, ensuring the outcomes are credible, balanced, and practical.
BEYOND CQC/ CIW/ CI STANDARDS
While CQC/ CIW/ CI inspections focus on fundamental areas such as safety, effectiveness, responsiveness, and leadership, CiUK’s approach extends further. Each CiUK inspection covers all the domains CQC/ CIW/ CI would expect, but also incorporates additional layers of analysis essential for continuous improvement. This Includes:
• Operational risk management involves identifying risks before they become incidents, reducing exposure for service users and providers.
• Quality enhancement: Assessing opportunities to raise standards in care delivery, staff engagement, and governance.
• Commercial sustainability: Offering insight into how operational practices influence financial performance, helping providers balance compliance with business viability. The result is an inspection report that is not only regulatory-ready but also a strategic tool for improvement.
By Kevin Groombridge
Professionalism is at the heart of CiUK’s ethos. Inspections are conducted by highly experienced professionals who bring frontline expertise from clinical, managerial, and governance roles in the care sector. This depth of knowledge allows CiUK to deliver meaningful feedback that resonates with staff at every level, from frontline carers to boardroom directors.
Independence is equally vital. As an external registered inspection body, CiUK reassures providers that its findings are unbiased and transparent. In a sector where credibility matters, this impartiality is invaluable in preparing for CQC inspections and demonstrating accountability to commissioners, investors, and the wider community.
Care providers today operate in an environment of heightened scrutiny and rising expectations. CIUK’s inspections do more than highlight compliance gaps; they provide a clear roadmap for reducing risk, enhancing quality, and driving organisational improvement.
By identifying weaknesses early, providers can take corrective action before issues escalate. At the same time, CiUK’s focus on strengths and opportunities supports a culture of positive development. This balanced approach ensures that inspection outcomes are constructive, not punitive, fostering continuous organisational improvement.
One of the most overlooked aspects of care provision is its commercial dimension. Poor compliance and weak governance inevitably carry financial consequences, from reputational damage to contract loss. CiUK recognises this and integrates commercial insight into every inspection. CiUK helps providers achieve operational excellence and commercial resilience by aligning care quality with business performance.
THE CIUK DIFFERENCE
Choosing Care Inspections UK Limited means selecting a partner committed to professionalism, independence, and comprehensive excellence. CiUK inspections do more than prepare organisations for regulatory visits—they empower providers to deliver safer, higher-quality care while protecting their reputation and commercial future.
CiUK delivers evidence-based assurance and
for providers who want more than compliance.

THE WEIGHT CARE TEAMS CARRY, OFTEN SILENTLY
There is a moment in every care professional’s life that stays with them. For me, it was a late evening on the unit, years ago, when a nurse quietly said, “I hope everything was done right today. Sometimes I fear what I do not see.” Her words were simple, but they held the unspoken truth of our sector. Care is built on love, but it stands on safety. And safety, in the real world, is fragile. It lives in the seconds we do not have, the pressures we do not voice, the documentation that steals time from the people we came to serve.
Medication rounds, audits, handovers, stock checks, and incident reviews are essential but relentless. Behind every one of them is a carer trying to do the right thing, a senior hoping they have not missed a detail, and a manager carrying the weight of an entire home on their shoulders. For years, I watched this tension unfold. The intention was always pure, but the systems were not always kind. And that is where Empathika began.
It was never just a technological project. It was a response to the tired eyes of the night nurse, the rushed signatures at the end of a shift, the quiet fear of missing a dose, and the pressure to be perfect in a world that gives little room for human error. As a pharmacist, my world has always been accuracy, governance, and risk. But as a human being raised in a family dedicated to care, my world has also been empathy, dignity, and service. Empathika is where those two worlds meet.
TURNING PRESSURE INTO CLARITY, AND FEAR INTO CONFIDENCE
By Sibtain Nandjy, Chief Medical Officer, Empathika
Medication is one of the most sacred responsibilities in care. It is where mistakes can cause harm, where delays can cause distress, and where oversight can save lives. Yet traditional approaches relied on memory, paper trails, and hope. Empathika was created to take the weight off people’s shoulders, not add to it. She records every dose in real time. She alerts before errors happen. She tracks stock, expiry dates, and changes in treatment. She protects controlled drug processes with dual witnessing and biometric verification. She gives managers visibility before problems even surface. Above all, she protects carers from carrying fear into their work. She holds the details so they can hold the residents.
One of the greatest challenges in care is not the work itself, but the constant interruption of it. A senior searching for stock. A carer chasing signatures. A manager preparing for an unannounced inspection. Empathika brings calm into the noise. Live dashboards show managers exactly where the home stands. Incidents, handovers, and reviews are captured without confusion. Compliance becomes a natural outcome of daily practice, not a monthly marathon. Families feel the difference because they see teams who are present, not pressured.
People often ask what makes Empathika different from other systems. The answer is simple. She was not built from a boardroom. She was built from lived experience. Every feature has a why. Every process has a story. Every safeguard has a person behind it. And that is why she feels different. She listens. She steadies. She gives time back to the floor.
The future of care will not depend on technology alone. It will depend on how well technology honours the people who use it. Empathika exists for that purpose. To make safety feel gentle. To make compliance feel natural. To make care feel like care again. Because at its core, Empathika is not equipment. She is a commitment. A promise that no carer will stand alone under the weight of responsibility, and no resident will be cared for in fear or uncertainty.
Dudley Council is investing £300,000 in a project to improve the way people are supported when leaving hospital.
The authority has commissioned Dudley Council for Voluntary Service (Dudley CVS) in collaboration with NHS partners to deliver a new social prescribing two-year pilot that will enable a range of voluntary sector organisations to deliver support in the community to help people live independently following a stay in hospital. Volunteers, social prescribers and voluntary organisations will work together to help bridge the gap between hospital and home, addressing the non-clinical factors which can delay discharge or contribute to avoidable readmission. Social prescribing connects people to practical, social and emotional support that tackles the root causes of poor health such as loneliness, debt, housing issues or lack of confidence.
Simple steps such as linking isolated residents to befriending groups, encouraging those with physical health conditions to take up accessible exercise, helping people to make new friendships and take part in social activities, supporting people in financial difficulty to access organisations such as Citizens Advice means that people feel supported beyond the hospital environment and empowered to live independent lives.

While the service supports safe and timely discharge from hospital, it is deliberately designed to extend well beyond the hospital setting. Volunteers and staff from a range of voluntary sector organisa-
tions will provide up to 12 weeks of intensive, community-based support after a resident returns home — a period when people are most at risk of deterioration, loss of independence or readmission. This approach helps reduce avoidable readmissions and ensures support continues beyond clinical care and into everyday life.
This new pilot will enable an expansion of social prescribing into a hospital discharge setting using a voluntary sector collaborative investment model.
Councillor Andrea Goddard, cabinet member for health and adult social care, said:“As part of the remodelling of our Adult Social Care provisions, we are progressively shifting towards a prevention first, place based model that strengthens community resilience, reduces avoidable hospital admissions, supports timely discharge, and enables residents to remain independent in their own homes.
“The hospital discharge social prescribing pilot – Community Bridge Project is a perfect example of how we can work smarter and allow more people to stay in their own homes for longer. Dudley CVS have proven that this model works, and I’m really pleased that we’ve been able to invest in the voluntary sector to deliver this service.”
Kate Green, Deputy Chief Officer Dudley CVS, said: “Leaving hospital is a critical moment in someone’s recovery. Enabling and supporting voluntary sector involvement through a bespoke funding programme will mean that the sector can play an integral part in helping people live healthily and independently.”
A fall- the F word- is massively on the increase: among older people, up 57% last year!(1) More than 40,000 people are hospitalised each year because of a fall on stairs(2) Falls cost on many levels: ambulance call-outs, stays in hospital, admission into care, provision of home care. There is the psychological cost too: people become wary doing everyday activities.
Yet, with prescription of appropriate equipment, many of those could be avoided. AAT’s S-Max Sella stairclimbing wheelchair is proven over 20 years to make traversing stairs safe for people with mobility issues/ a disability(3) Battery powered, Sella not only travels up and down stairs, but outside steps too. It removes the barrier(s) that prevents someone- young or old- being able to fully access their home environment.
Unlike alternative solutions, it is completely mobile/portable. The Sella stairclimber requires no installation nor electric supply to function. It is not limited to the staircase, meaning it can be used to move its passenger anywhere in the property and beyond without them needing to transfer off it.
Sella has an impeccable safety record and is the stairclimbing choice for virtually every local authority in the UK. As a result, it has the unique capability to be re-prescribed (re-issued) multiple times, giving the council best value and use of equipment resources.
The Nelson family demonstrates Sella’s value. They were prescribed one by their OT Fran Richardson after numerous “near misses” carrying their disabled son on the stairs. Fran commented,” “The stairclimber eliminates the risks associated with using the stairs for the family. Its versatility ensures it effectively addresses their current challenges and supports their long-term needs. The Sella cost less than half of the alternative options.”
Full details of the Sella stairclimber, including video of it in action, and how to book a free no obligation assessment, can be found @ www.aatgb.com/s-maxsella/ (1) https://operabeds.com/blogs/knowledge-hub/falls-in-the-elderly-uk-65-injury-and-accident-statistics

A major study led by the University of Hertfordshire has shown how linking care home data with NHS and social care records can improve residents’ lives, strengthen policy decision-making and ensure critical health needs are not being missed.
The DACHA study, a £2.4 million research project funded by the National Institute for Health and Care Research (NIHR) and supported by NIHR ARC East of England, has shown that a minimum dataset (MDS) –which brings together essential information already recorded about care home residents but currently stored in separate systems – can be distilled to provide information useful to plan, deliver and evaluate care.
The project was led by Claire Goodman, MBE, Professor of Health Care Research at the University of Hertfordshire and carried out in collaboration with 10 universities and senior partners including the National Care Forum, The Health Foundation and four NIHR Applied Research Collaborations.
In England, there are more than 1.5 million people aged over 85 and around 370,000 care home residents – and nearly three-quarters of care home residents are over 801.
Yet despite the digitalisation of patient and social care records, there is no standardised approach to recording or linking data between care homes, the NHS, and social care services.
Prof Goodman said: “Most people living in care homes have multiple long-term conditions, such as dementia, diabetes, or heart failure this affects them in different ways. Shared data can enable health and care professionals discuss their care and to review the events leading up to crises or hospital admissions and the factors that may have contributed to it.
“Without information on a person’s baseline mobility, how their dementia affects them, recent weight loss, or their individual priorities, clinicians only get a partial picture of what is happening which in turn can affect clinical decision-making.”
The MDS addresses these obstacles by creating a vital bridge that connects information about residents’ health and care needs with their NHS and social care records, providing a standardised dataset that can be understood by all service providers.
It also helps avoid duplication of data collection, reducing burden on care home staff, and enables services to better understand not just medical conditions, but also what helps with residents’ quality of life, preferences and social care needs – making care more person centred.
Prof Goodman added: “The UK holds a wealth of routine health and social care data, but having data is not enough.
“When structured and shared, this everyday data can be a powerful tool that can ensure targeted NHS support to help reduce unplanned hospital admissions, enable personalised care planning, and improve resident wellbeing and safety.
“When professionals are working from the same information from linked datasets, it builds trust between services and a shared understanding that supports collaborative problem-solving rather than attributing blame.
“The MDS is about creating a foundation for meaningful, joined-up care that does not require extra form filling for an already stretched workforce.
“Better data, designed around people’s lives, leads to better care and better use of the NHS and social care resources.”
The content of the MDS prototype – a first in the UK using routine data from both health and social care –was developed through evidence reviews, national surveys, and consultations, linking data from residents’ digital care records with information held about them in NHS and social care databases.
The team tested the prototype in 45 care homes across England, which demonstrated linking data is feasible and valuable. The DACHA study has also developed resources to support large-scale research to continue in care homes, including the creation of the UK’s first care home trials archive to enable use of high-quality data for secondary research.
KEY ACHIEVEMENTS
• Consensus on core measures of an MDS that are valuable for care at every level – individual, service, and
organisational: drawing on routine information already held by care homes, hospitals, GPs, and regulators, alongside new measures of cognition, delirium, and care related quality of life
• A pilot MDS was successfully implemented in 45 care homes proving that accessing and linking routine data in this way is both feasible, and can provide resources for others looking to link these data
• First UK care home trials archive: The team created a live resource of anonymised trial data from more than 6,000 residents across more than 300 care homes in England, Scotland, and Northern Ireland. This archive reduces research waste and supports robust, large-scale studies without burdening care home staff
• Supporting policy implementation that is digitising adult social care by working with care home staff and software providers to understand what is needed to implement digital care records that inform care. The finalised MDS and the data directory were shared with the Department of Health and Social Care (DHSC) and NHS England
• Quality-of-life outcome measures were tested as part of the MDS, helping fill a gap in the evidence that everyone recognises is central to the experience of living in a care home. They are being considered for inclusion in NHS Digital’s social care data directory and discussed with the UK Health Security Agency
The researchers said the next steps should focus on expanding the MDS as a key resource for policy makers, care homes and health systems, embedding it in supporting ICSs (Integrated Care Systems) planning and ongoing evaluation, while supporting staff to use the data to plan, deliver and review care.
Rachel Squire, Care Home Manager at Milford Care, said: “Unlike the NHS which has one big system that holds information about all patients, care homes exist in small and disconnected pockets, which too often leaves us isolated and competing, rather than learning from one another.
“The DACHA study showed us that using the data we already collect every day – without extra forms or added burden – we can finally share what works, learn from each other, and deliver a personalised care experience for the people we look after.
“By removing the constant pressure to repackage the same information for GPs, local authorities, or the Care Quality Commission, the data is simply taken from the systems we already use. This has given us back time to focus on what truly matters: our residents’ wellbeing, their goals, and their quality of life.
“Moving into a care home is not the end of life – it’s a different chapter. People still deserve purpose, achievement, and joy.
“Being able to share data also gives care homes reassurance that they are on the right track rather than waiting years for an inspection to tell us how we are doing.
“The DACHA study has fundamentally changed the way we connect with and support our residents.”
Liz Jones, Deputy CEO and Policy Director at the National Care Forum (NCF) said: “Historically there has been a lack of consistency in the collection of people’s medical histories, needs and preferences, creating inaccuracies and duplications that have made it difficult for care homes to truly understand the needs of a person coming into their care.
“The DACHA study has demonstrated the possibility of being able to link data across different systems as well as being able to include key quality of life measures, such as physical health, emotional wellbeing and social life, to support discussion with residents about better care and a better day-to-day experience.
“NCF are proud to have played a part in such an essential programme of research which will, we hope, create better outcomes for people drawing on care, their families and those who deliver care.”
Professor Ann-Marie Towers, Deputy Director, Health and Social Care Workforce Research Unit at Kings College London, and project co-investigator, said: “As part of the social care system, care homes strive to provide 24-hour care in non-clinical, homely environments, respecting people’s choices, supporting their independence and maintaining their quality of life.
“However, until the DACHA study, most care homes did not systematically collect information about residents’ quality of life or have the tools and language needed to demonstrate their impact on residents’ outcomes.
“By novel linking of care home data with data held about residents by the NHS, the DACHA study has showcased how joined up health and social care data can help commissioners and decision makers better understand the needs of their local populations.”
Technology decisions in adult social care are no longer confined to IT teams or procurement processes. They shape everyday experiences. They influence how people are supported, how staff work, and how services demonstrate that they are safe, effective and accountable. At the same time, the sector is under immense strain. Demand is rising. Workforces are stretched. Regulation is intensifying. Digital tools are increasingly positioned as part of the solution, expected to stabilise systems that are already under pressure.
It is no surprise, then, that social care has leaned heavily on frameworks, standards and guidance to help make sense of risk, data and technology. These are important. But they are not enough on their own. When you step away from policy documents and listen to lived experience, a more complicated picture emerges.
Families may experience monitoring tools as reassuring. People drawing on care can experience those same tools as intrusive, empowering, or something in between. Care leaders are often focused on accountability, liability and safety. All of these perspectives are valid, yet they rarely point in the same direction.
The danger is not disagreement. It is pretending these tensions do not exist.
SAFETY,
Safety often becomes the organising principle for digital decisions. Sensors, alerts and data sharing systems are introduced to reduce risk and provide reassurance in a system where staffing is limited and time is scarce.
For some people, this technology creates freedom and confidence. For others, it feels like constant visibility. Even where consent is given, the emotional experience of being monitored is not always fully
explored.
These decisions may be made in assessments and meetings, but their impact is felt in bedrooms and living rooms. Dignity and privacy are not technical concepts. They are personal, value-based, and deeply contextual.
How often do we revisit these choices?
How clear are we about what data is collected and why? What happens when one person’s sense of safety conflicts with another’s sense of dignity?
Consent in digital care is often treated as a single action. A form signed. A box ticked. A decision made.
In reality, consent is fragile and changeable. Technologies are frequently introduced during moments of transition, or gradually become part of daily routines before anyone has time to reflect. What starts as a choice can quietly become the default.
As systems grow more complex, understanding becomes harder too. Many people, including professionals, are still learning how data is stored, shared and analysed. That makes meaningful consent difficult to sustain over time.
True consent requires revisiting, re-explaining and re-negotiating. It also requires making refusal possible, even when doing so feels uncomfortable or increases perceived risk.
WHO BENEFITS, AND WHO CARRIES THE COST?
Technology is often discussed in terms of efficiency and innovation. For care workers, the experience can be mixed. New systems promise time savings, but sometimes introduce extra steps, new pressures and new forms of oversight.
At the same time, when tools are designed and introduced well, they can reduce duplication, improve coordination and support better care. The difference is rarely the technology itself. It is whether people were involved in shaping it, and whether their expertise was respected. When systems fail, it is frontline staff who absorb the impact. They manage workarounds, late alerts and broken workflows. How organisations acknowledge that reality shapes trust far more than any digital strategy document.
Having honest conversations about technology in care is uncomfortable. It forces us to confront trade-offs rather than hiding behind process or policy. But discomfort is not failure. It is a signal that something important is being examined.
Throughout March, Digital Care Hub is creating space for these difficult conversations, from privacy and consent to robotics and the future of care work. Because comfort is easy. But courage is what leads to better decisions.
Technology is the topic, but dignity, safety and relationships are what’s truly at stake.
Join the conversation at www.digitalcarehub.co.uk/digital-care-in-focus #DigitalCareInFocus #DifficultConversations
Professor Sir Mike Richards has resigned as Chair of the Care Quality Commission (CQC). He has agreed to continue until another Chair can be appointed.
Prof Sir Mike said: "It has been a privilege to serve as Chair of the Care Quality Commission, following my independent review of the Assessment Framework. I am extremely grateful for the trust placed in me. We have made progress on several critical improvements. I am particularly pleased that we now have specialist sector teams in place and will shortly be communicating the consultation response on the new Assessment Approach. "However, it has become increasingly clear that the turnaround of the CQC—alongside the work required to establish it as the world’s leading health and care regulator—will demand a longer-term commitment as Chair than I am able to make.

"Finally, with Sir Julian Hartley’s departure, there is an urgent need to appoint a permanent CEO. After careful consideration, I believe it would be best for this appointment to be led by a new Chair who can commit to providing long term continuity. "I remain fully committed to the CQC’s future success and to supporting any incoming Chair during the transition."
Dr Arun Chopra, Interim Chief Executive Officer of the CQC said: "On behalf of the leadership team and the wider organisation, I would like to thank Sir Mike for his contribution to rebuilding the CQC- from his
Independent Review and in his role as our Chair over the last year. We are committed to delivering on the recommendations that he made and to rebuilding our organisation so that we deliver for patients and people who use services."
Professor Martin Green OBE, Chief Executive of Care England, said: “Sir Mike took on this role at a very difficult time for the CQC. Confidence in the regulator, especially from adult social care providers, was already fragile, and the system was clearly not working as it should.
What mattered about his independent review of the Single Assessment Framework was that it reflected what providers had been experiencing on the ground for some time; delays that made no sense, a loss of sector expertise, and a framework that felt disconnected from the reality of delivering care. He was prepared to say that out loud, and that was important. Many of the problems facing the CQC have not gone away, and there is still a long way to go. But his work helped to open the door to a more honest conversation about what regulation needs to look like if it is to support good care rather than get in the way of it.
As the CQC moves into its next phase, the priority must be stability and follow-through. Providers need clarity, consistency and a regulator that understands the pressures they are under. We are ready to work with the new leadership to make sure the lessons of past years are not lost, and that regulation starts to work properly for the people who rely on and deliver care every day.”
Parley Place care home in West Parley received an amazing afternoon of entertainment courtesy of a newly formed group of musicians, called “Swing Squad”.
Swing Squad is made up of 5 teenagers ranging from 13-17 years old and playing predominantly Swing and Jazz music. The teenagers, Sam, Eli, Arthur, Reuben and Jack arranged the set list for the whole performance and delivered this to the residents in a professional yet fun way. They were joined by two very special guests - Prisha, an outstanding vocalist, and Eliana, who accompanied her beautifully on piano. The residents thoroughly enjoyed the performance and chatting with the band members afterwards. It’s clear that this group have the skills and passion to entertain crowds and will go far.
Gina Smith, General Manager at Parley Place, said: “We love to support our community and when we saw an advert for Swing Squad wanting to play locally, we jumped at the chance. For our resident’s music is so important and these teenagers gave an exceptional performance” Jan, resident at Parley Place said “It’s heart-warming to see such passion for music from a group of teenagers who brought a wave of positive energy with them to the home this afternoon. They all spoke so clearly, introducing the songs and playing them so wonderfully, we thoroughly enjoyed it, thank you Swing Squad”
The Swing Squad came together at the end of December 2025 as a dynamic group made up of three brothers and two close friends. Working entirely independently, they chose their own repertoire, sourced and arranged the music themselves, and organised their own rehearsal schedule, an impressive achievement for such young musicians.

Four of the five band members are part of the Poole Society for Young Musicians, whose encouragement and support have been invaluable. The group recently took part in a performance class run by the Society, where they received exceptionally positive and constructive feedback that gave their confidence a huge boost.
Alison Kay of the Poole Society for Young Musicians said, “We are thrilled to see such a highly energised group of young musicians inspired through the Poole Society for Young Musicians to come together as Swing Squad and to share their music with our community. Inspiring the next generation to love music and to strive for excellence is at the heart of everything we do!”



Four years after its emergency launch during the darkest days of the pandemic, the Vivaldi Social Care research programme has established itself as a vital tool in protecting care home residents from infection. Unveiled at a wellattended Parliamentary Reception, the programme's groundbreaking approach to data collection is delivering the robust evidence base that care homes need to combat outbreaks and safeguard vulnerable residents.
Vivaldi has established the first large-scale, safe and efficient data pipeline for care home research. This is done by linking routinely collected digital care records with health data.

Nearly 700 care homes are signed up, representing around 28,000 residents, creating a growing evidence base that is transforming how infections are understood, prevented and managed in social care. This work has significant implications for adult social care delivery, outcomes and evidence-led national policy making, aligning effectively with the Government’s 10-Year Health Plan.
The Parliamentary Reception brought together care sector leaders, parliamentarians, regulators, policy makers and those with lived experience of care to hear about Vivaldi’s progress, impact and future ambitions. Guest speaker Neil O’Connor, Deputy Director of Baroness Casey’s Independent Commission on Adult Social Care, shared insights into the potential direction of social care policy. By engaging directly with Parliamentarians, the event aimed to inform debate and shape future policy discussions to further the health of care home residents through applying a health and social care approach.
Professor Laura Shallcross MBE commented: “Vivaldi Social Care demonstrates how linked, high-quality
social care data can be used to make real world impacts for those living and working in care settings. This is the beginning of a structural change in social care where data is shared and analysed on a large scale to improve outcomes. With the NHS 10 Year Plan having been launched, Vivaldi offers to tick all three boxes regarding prevention, community and digitalisation, a matter close to our hearts and the government’s.”
Professor Martin Green OBE commented: "Vivaldi’s data pipeline is critical step forward for the sector. I encourage care providers to sign up and start contributing to the data that will improve outcomes for residents, families and staff across the sector, while informing policy decisions at regional and national levels."
Zoë Fry OBE, Director of Nursing, The Outstanding Society, commented: “Vivaldi’s Social Care is unique – it really is research led by social care, for social care. By strengthening the role of data and evidence, it helps place social care on a more equal footing with the NHS, which is exciting and important for the whole health and social care system.”
Chris Day, Director of Engagement, CQC commented: “The Vivaldi project is a groundbreaking study to help better track and understand how and why people move through the health and care system. As the regulator of health and care services CQC sees first-hand the importance of joining up how people access health and care services. We believe by better understanding how and why people move between services we can drive change that improves the care people receive.
Yorkshire-based care operator Park Lane Healthcare has announced the addition of Astrum House to its portfolio, further expanding the range of care services it provides across the sector.
Formerly known as the STAR Foundation, Astrum House is located on Nightingale Close and will form part of the Moorgate Care Village in Rotherham, alongside The Croft, The Lodge, and The Hollow, which are also part of Park Lane Healthcare. The 60-bed care home provides specialist support for individuals with physical disabilities and mental health needs.
The deal was funded through a partnership with US-based Omega Healthcare Investors Inc. Omega is a significant healthcare real estate investment trust, specialising in the long-term ownership and financing of nursing and senior care facilities across the US and UK.

Chris Lane, chairman at Park Lane Healthcare, said: “We are delighted to welcome the residents and staff of Astrum House into the Park Lane Healthcare family.
“The addition of Astrum House broadens the care we provide at Park Lane Healthcare and reflects our commitment to offering services tailored to each individual’s needs. It also strengthens our culture of continuous learning, enabling our teams to share knowledge and expertise across our homes.”
Emma Wooton, registered manager of Astrum House, said: “Joining the Park Lane Healthcare family is a really positive step for Astrum House. There is a strong shared commitment to person-centred care, dignity and independence, and it is reassuring for both residents and staff to be part of a wider organisation that genuinely values its people.”
Ashmead Care Centre in Putney celebrated the completion of their £1.2m wellbeing-focussed refurbishment with an open day attended by the community, including local MP, Fleur Anderson.
On the afternoon of Friday 24 January, the Care Centre, which is part of the Maria Mallaband Care Group, brought together the wider community and special guests to celebrate the end of a five-month refurbishment, showcasing upgraded living spaces and facilities.
The day included live music from a harpist and singer, dancing, catering, and free treatments in the home’s new wellbeing suite, which has a hair and nail salon and a wellness room offering classes and treatments such as massages and yoga.
With works completed in December, guests explored the bespoke reception with new café and seating area, nursing unit and a luxury private dementia unit, alongside renovations to hallways, dining rooms, lounges, and the terrace and outdoor spaces.

Luminita Cupsa, Home Manager at Ashmead Care Centre, said: “It was wonderful to welcome so many
members of the local community into Ashmead and to see the new spaces being enjoyed exactly as we’d hoped. The open day really brought our vision for a warm, welcoming environment to life, and the feedback from those living with us, families, and visitors has been overwhelmingly positive. People were up and dancing, it was fantastic!”
The day was also the official launch of the home’s partnership with Hair Angels, a specialist dementia-friendly hairdressing service that will visit Ashmead’s salon twice a week. With friendly dementiatrained staff, this service is particularly beneficial for those living at the home, but it’s extended to the wider community too.
Luminita Cupsa, said: “Every decision we’ve made has been with one goal in mind… to enhance the quality of life for the people living here. From the calm, self-care spaces we’ve created, to the encouragement of movement and social connection, this refurbishment has been all about making people feel happier, healthier, and more at home.”
Residents at a Wiltshire care home teamed up with local schoolchildren to celebrate one of Britain’s most iconic bears.
It was a truly ‘bear-illiant’ morning at Care UK’s Salisbury Manor on Shapland Close, as residents welcomed children from Chafyn Grove Independent School to mark Winnie the Pooh Day for a special storytelling session.
The residents, who had been practising their best character voices, sat alongside the children to read Winnie the Pooh tales, supported by storyteller, Frances Owen. The morning also featured Pooh-themed colouring activities to encourage conversation and creativity, while the children delighted residents with a performance of Bees and Honey. Venetia Coupe, daughter of a resident and beekeeper, also led a honeytasting session featuring honey sandwich, as a nod to Winnie the Pooh’s

favourite treat.
Tracey Pearce, Home Manager at Salisbury Manor, said: “We’ve had a wonderful time sharing stories and poems from Winnie the Pooh here at Salisbury Manor. Seeing the children enjoy performing and the residents sharing their favourite Pooh stories was truly heart-warming.
“Intergenerational activities are a big part of life at the home. They can be incredibly beneficial to both younger and older people alike and can help provide residents with a stronger sense of wellbeing and purpose. A lot of residents also have fond memories of reading Winnie the Pooh stories growing up, and sharing them with their own children, so the activity was a great opportunity for them to reminisce.
“We’d like to thank Chafyn Grove Independent School for visiting us to celebrate Winnie the Pooh Day."

As awards season gets underway with Oscars, BAFTAs, and Grammys making for many a headline, social care’s top talent has joined the party with its own glittering celebration – the annual Champion Awards hosted by leading dementia specialist, Belong, has celebrated the best amongst its villages and community care teams.
Twelve accolades were handed out at the sparkling ceremony to its colleagues and volunteers from across the North West and West Midlands for exceptional performances supporting older people to live active and fulfilling lives.
What’s more, once again, its customers were front and centre of the initiative with their nominations determining the finalist shortlists, before a panel of independent judges determined winners with the results revealed at Manchester Hall.
The Belong Champion Awards 2025 winners are:
• Newcomer Award: Alicia Nield-Spurrier, Belong Crewe
• Be Your Best Mentor of the Year: Elaine Cooke, Belong Wigan
• Leader Award: Emma Spurrier, Belong Crewe
• Team of the Year: Tetley Household, Belong Warrington

• Belinda Jones Dementia Champion of the Year: Jessica Murphy, Belong Crewe
• End-of-Life Care Award: Nicola Davies, Belong Wigan
• Care From the Heart Compassion Award: Laura Picton, Belong at Home Wigan
• Volunteer Award: Eileen Allman, Belong Newcastle-under-Lyme
• Respect for All Inclusion Award: Greenall Household, Belong Warrington
• Community Engagement Award: Experience Team, Belong Wigan
• Better Tomorrow Innovation Award: Emma Palin, Belong Newcastleunder-Lyme
• Central Services Contribution Award: Suzanne Roberts, Central Services
Judges’ feedback lauded finalists, praising their dedication, passion and commitment, going ‘above and beyond’ for residents, as well as a person-centred approach to care, team spirit, and making ‘real difference’ in older people’s lives.
Speaking of the event, Belong’s chief executive, Martin Rix, said: “Once again, our Belong Champion Awards have shone a spotlight on the incredible work happening day in, day out, across our villages and home care teams. It’s especially important to us to have our customers at the heart of everything we do, and they’ve embraced the opportunity to thank our dedicated colleagues.
“It really is people who ultimately create culture and make our organisation such a great place to live and work. Congratulations to all our finalists and winners.”

They may not have made it to snowy Italy in person but sports fans at care homes in the south have enjoyed putting their own take on Winter Olympics-themed fun.
Colten Care residents have participated in gentle, good natured rivalry in activities such as broomstick curling, noodle hockey, snowball throws and chair skiing.
At Woodpeckers in Brockenhurst in the New Forest, first-time broom curler Elsebeth Hacking surprised everyone by becoming champion, while fellow residents laughed, clapped and cheered each other on.
Pat Spring Smyth said: “I had a great time laughing at my attempts. It might have been better if I’d skied!”
There was a similar chair-based curling contest held over eight rounds at Abbotts Barton in Winchester, after which residents donned snow goggles and bobble hats for a bobsleigh and toboggan game and headed for après-ski hot chocolate.
At Canford Chase in Poole, a snowball relay game was led by Companion and keen snowboarder Justin Corder who kitted himself out in full outdoor gear including helmet, goggles and boots.

Care Show London 2026 running on 29-30 April at Excel London, will be opening its doors for the third consecutive year to the whole care community. Matthew Moore, Show Manager highlights what is on offer at Care Show London as well as key speakers and sessions to look out for.
KEY THEMES AND GOALS FOR CARE SHOW LONDON THIS YEAR
Care Show London is the meeting place for the social care community, united by a shared commitment to delivering the highest standards of care. The show provides a platform to learn best practice, explore innovative products and services, and develop practical skills to support day-to-day work.
The focus this year is on helping you confidently navigate the future of care. Through expert-led sessions and sector insight, you’ll gain the clarity, support, and direction needed to prepare for what’s next, with key themes including workforce, regulation, policy, AI and technology, business sustainability, palliative care, and more.
CONFERENCE PROGRAMME
Care Show London conference programme covers key challenges within the sector, matching these with established care professionals who are able to provide solutions to these. With over 180 experts in the sector speaking at the show, we'll cover everything from strategic business support to specialised dementia care, to sustainability wins and so much more!
With seven dedicated theatres hosting sessions across the two days and over 60 hours of world-class education, attending this event will provide you with the tools and solutions to improve the quality of care you provide.
Must see sessions:
• Keynote Theatre – CQC update: our journey, priorities, and what’s next for adult social care
People & Business Theatre - Winning self-funded clients through strategic marketing and sales
Technology Theatre - What's happening internationally? How social

care across the globe is using technology to improve outcomes
Catering, Hydration and Nutrition Theatre - Cognition-supporting Vitamin B12 needs our attention: how to incorporate more into meals with ease
IHSCM Leadership in Tough Times Theatre - How to build an effective team
Care Providers’ Voice Masterclasses - What will the care workforce look like in 2030?
The Outstanding Society Learning Lounge - Safe medicines management: complex medication and reporting
Key speakers: Chris Badger, Chief Inspector of Adult Social Care & Integrated Care, CQC
Isaac Samuels OBE, Co-Chair, NCAG & TLAP
Fran Vandelli, Dementia Lead, Bupa Care UK
Aneurin Brown, CEO, Hallmark Luxury Care Homes
Emma Jane Tinkler, Programme Manager, HC-One
Kevin Humphrys, CEO, Oakland Care Group
• Michelle Corrigan, Programme Director, Digital Care Hub
Clare Jefferies, Business Director, Home Instead Wimbledon & Kingston
Giuseppe Di Martino, Learning Disability and Autism Commissioner, Slough Borough Council
Katy Hague, Chief of Staff, Crystal Care Homes
Lucy Campbell, CEO, Right at Home UK
Sarah Sabater, CEO, CareYourWay
Charles Taylor, Owner, Taylor & Taylor Care Group
Alyson Vale, Business & Operations Director, Abbotsford Care Ltd TOP SUPPLIERS
Alongside the dedicated conference programme, Care Show London hosts over 200 top suppliers from the sector, offering a wide range of products and solutions to help improve your business. From catering suppliers to software providers, you’re sure to find an exhibitor with what you’re looking for.
NETWORKING
With so much happening at the show, don’t forget to make time to connect with sector peers. With over 3,750 care professionals expected at Care Show London, it’s a great opportunity to meet like-minded professionals who understand your challenges and desire to build strong relationships.
Care Show London 2026 is your opportunity to confidently navigate the future of social care. With expert-led sessions, innovative suppliers, and thousands of professionals under one roof, the show provides the knowledge, connections, and tools you need to stay ahead and succeed in a changing landscape.
Register now to join your community for two days of learning, networking and inspiration. Visit the Care Show London website or click visit https://forms.reg.buzz/care-show-london-2026/carer
To view the conference programme, visit: https://www.careshowlondon.co.uk/thecarer26

Ready-to-use activity products designed to support meaningful engagement in everyday life.
Everything you need to inspire connection, stimulation and wellbeing CREATIVE & SENSORY ACTIVITIES
Art, craft and sensory products designed to engage, calm and inspire. COGNITIVE & REMINISCENCE
Memory-based activities and conversation starters that encourage connection. GAMES & GROUP ACTIVITIES
Inclusive games and group activities suitable for a wide range of abilities. ONE-TO-ONE & MEANINGFUL ENGAGEMENT
Personalised activity products that support wellbeing and individual needs. Thoughtfully selected to be accessible, inclusive and easy to use in busy care environments.
Explore our full activity range - www.bluerain.store where you will also find our informative blogs and contact form as friendly advice is always on hand.
See thee advert on page 4.
HipSaver Soft Hip Protectors protect the elderly and disabled people from fallrelated hip fractures.
Designed to protect elderly people from fall related hip fractures, HipSavers are a leading brand of soft hip protectors. Used in the NHS since 2002, HipSaver Soft Hip Protectors are user friendly, affordable and cost-effective personal protective garments. Soft, comfortable, effective and compatible with incontinence protection, HipSaver Soft Hip Protectors are perfect for use in care homes and by elderly people living independently.

HipSavers should be worn day and night for 24 hour protection and especially during physical and recreational activities, when accidental falls, slips and trips can lead to hip fractures.
Available as comfortable underwear or long casual pants in several sizes for men and women, HipSavers feature soft protective airPads permanently sewn into the garments over the hip areas prone to injuries and fractures. HipSaver TailBone models have an
additional protective airPad over the coccyx on lower back for protection during swaying, accidental knocks, bumps and backward falling.
Machine washable at high temperature and tumble drier friendly, HipSavers are practical, hygienic and durable.
HipSaver Soft Hip Protectors - affordable protective garments for the elderly and disabled people! For more information, contact Win Health Medical Ltd - 01835 864866 - www.win-health.com
See the advert on page 3 for further products.
MAG Laundry Equipment is a multiaward-winning supplier of commercial washing machines & tumble dryers that supports over 10,000 care homes across the UK.
Clean laundry and bedding is critical for care homes, hospices, nursing homes, hospitals and other healthcare organisations. With a nationwide fleet of accredited engineers MAG Laundry Equipment has successfully assisted over ten thousand care homes with their products, services, information and support.

affordable machines on the market. Care homes have peace-of-mind that their laundry machines can quickly be maintained and repaired as MAG Laundry Equipment supply, install and service equipment across England, Scotland and Wales.
If you are looking for high quality wash results that remove stubborn stains then speak with MAG for their recommendations. Complete thermal disinfection is a standard feature on their washing machines for nursing homes.
MAG’s product range includes commercial washing machines, tumble dryers, ironers, presses and detergents. For 100 years, since 1922, MAG’s products have been developed and improved to become some of the most reliable, energy-efficient and
To find out more about how MAG can support your care home telephone 01353 883025 or visit www.maglaundryequipment.co.uk. See the advert onthe back cover of this issue.

Repose Furniture is one of the UK’s leading manufacturers of bespoke seating solutions, with a reputation built on craftsmanship, innovation, and a strong commitment to improving the quality of life for its customers. Established in 1999 and based in the West Midlands, the company has grown from a small family business into a trusted supplier to both the domestic and healthcare markets. Every chair produced by Repose is handmade in the UK, with an emphasis on quality, durability, and comfort, ensuring that each product meets the specific needs of its user. Whether for home use or demanding healthcare environments, Repose combines skilled upholstery techniques with modern engineering to create chairs that provide postural support, pressure management, and ease of use. Their wide product portfolio includes rise and recline chairs, hospital and care home seating, bariatric solutions, and specialist products designed to address particular medical and lifestyle needs. An essential element of their offering is flexibility: customers can choose from a range of back styles, seat cushions, mechanisms, and fabrics, allowing each chair to be tailored to the individual. Interchangeable parts mean that a chair can adapt as a user’s requirements change, extending the product’s longevity and ensuring value for money. The healthcare sector is a particular area of expertise for Repose. They strive to design chairs that balance comfort with clinical functionality. Features such as tilt-in-space mechanisms, adjustable cushioning, and pressure relief options make their healthcare seating particularly suited to long-term use in hospitals, hospices, and


Meadow View Nursing Home in Chesterfield has found a grand(e) way to support a new resident with scoliosis- an innovative vacuum posture cushion.
The middle-aged client joined the home after a spell in hospital: underweight and fragile, she needed additional skeletal support and 1:1 care. Meadow View- part of Emh Care & Support- could provide the high quality round-the-clock attention she required.
The home’s nurses responsible for the lady were struggling to find a way to keep her comfortable and safe in bed. They raised the issue with the home’s Occupational Therapist, who suggested AAT’s Grande mattress with Treat-Eezi cover.
Using vacuum technology, the mattress-sized beanbag can be contoured exactly by the staff exactly as needed, to provide the lady with a secure yet comfortable position without pressure points.
By using the vacuum principle, any air in the cushion is removed, thereby fixing the moulded shape and removing the need for frequent re-positioning. The shape and firmness of the Grande can be adjusted as little or much as needed. The cushion can be precisely moulded to create abduction and adduction wedges, or an asymmetrical body position- all by the care-givers, within minutes(1). The addition of the Teat-Eezi overlay helps maintain blood flow and

gives an extra layer of protection against the risk of ulcers.
Meadow View Manager Gillian Kent comments, “The Grande gives support to her overall body structure, yet is soft and comfortable. The team find it’s easy to reform when she is supine, so they can ensure her continued relief and security when she’s lying in her bed. It has really helped her overall daily and nightly relaxation.”
Find out more about AAT’s Grande vacuum posture cushions here: www.aatgb.com/grande

care homes. The company’s bariatric range demonstrates the same careful attention to detail, offering robust yet comfortable solutions for larger users.
While customisation is the centre of the Repose offering, they also recognise the urgency often faced in healthcare settings. To address this, Repose have developed their Healthcare Express Chairs, designed to deliver high-quality healthcare seating at speed. The models in this range can be despatched within just five
continues to be a trusted partner in multiple sectors throughout the country and beyond.
In combining bespoke design with reliable express options, Repose Furniture stands out as a manufacturer that truly understands the diverse needs of its customers. For over 25 years, it has delivered not just chairs, but comfort, dignity and independence
Adults aged 80 and over, as well as all residents in care homes for older adults, will become eligible for the NHS respiratory syncytial virus (RSV) vaccine from 1 April 2026, NHS England (NHSE) and the UK Health Security Agency (UKHSA) have announced.
The government has decided, in line withJCVIadvice, that the RSV vaccine should be offered to additional groups in the population most vulnerable to serious outcomes from RSV infection and who are therefore most likely to benefit from vaccination.
VACCINATION WILL THEREFORE BE OFFERED IN ENGLAND FROM 1 APRIL 2026 TO:
• adults aged 80 years and over
• all residents in care homes for older adults
THIS IS IN ADDITION TO THE EXISTING PROGRAMME, WHICH OFFERS RSV VACCINATION TO:
• adults turning 75 years
• adults aged 75 to 79 years when the programme began
• pregnant women (to protect their newborn babies)

Those who are eligible for both RSV and COVID-19 vaccinations will be able to get both vaccines at the same appointment once the spring 2026 COVID-19 campaign begins on 13 April 2026, in line with JCVI guidance. Individuals eligible for both programmes include people who have not already had an RSV vaccine and are either:
• aged 75 or over
• a resident in a care home for older adults
Stephen Kinnock, Health Minister, said: “RSV can cause serious illness in older people, which is why this government introduced new year-round vaccination programmes in September 2024. By expanding this life-saving vaccination programme to also include adults aged 80 and over, and residents in care homes for older adults, we are taking another important step to protect those most at risk.
“I am pleased to accept the advice from the JCVI, which has carefully reviewed the evidence showing the clear benefits of extending this programme.
“I would encourage everyone who becomes eligible for the RSV vaccine from April to come forward and get vaccinated as soon as they have been invited to do so by their GP. Getting vaccinated is the best way to protect yourself and reduce pressure on the NHS during winter months.”
Dr Conall Watson, Consultant Epidemiologist at the UK Health Security Agency, said: “RSV lung infection is less well known than COVID or flu but for older adults it puts thousands in hospital each year with a risk to life.
“This extension of the RSV vaccination programme to everyone over 80 or living in a care home for older adults means many more will soon be able to get protected. This follows advice from JCVI based on new evidence showing the clear benefit of vaccination for these groups.”
Analysis has shown those aged 75 to 79 already getting the vaccine are much less likely to be hospitalised. And the evidence is clear that the RSV vaccine offered to pregnant women is providing excellent protection to babies. When you are offered the vaccine, don’t hesitate.
Rownhams Manor care home recently celebrated the 101st birthday of resident Brendon Cooke and his extraordinary life, defined by adventure, dedication, and family.
Brendon, a lifelong sailor, began his distinguished maritime career at just 17 years old as a cadet. Over the course of more than 40 years at sea, he built an impressive legacy in the shipping industry, including 20 years serving as a captain with the P&O Steamship Company.
His career took him across the globe, with voyages to destinations including Japan, India, and Australia, where Brendon and his wife married.
Brendon is the proud father of three daughters, and despite his many professional accomplishments and worldwide travels, he considers his family to be his greatest achievement.
Reflecting on his long and fulfilling life, Brendon offers simple but powerful advice: “If you want something, don’t stop until you have it.”
Brendon’s family and friends, and the team at Rownhams Manor, gathered to celebrate his birthday in the home, where the kitchen team bakes him a surprise nautical inspired cake.
Samantha Squibb, the General Manager at Rownhams Manor, said, “Celebrating Brendon’s 101st birthday has been a privilege for everyone at Rownhams Manor.
His remarkable life, from decades at sea to the family he is so proud of, is truly inspiring. Supporting residents like Brendon to celebrate milestones such as this is central to what we do, as it allows us to honour their stories they continue to share with us.”

Leading independent healthcare waste management specialist Anenta, which acts on behalf care homes and nursing homes throughout England, has been named UK Healthcare Waste Management Services Company of the Year for the second year running at the international Healthcare Business Review Europe Awards 2026.
The back-to-back win reinforces Anenta’s position as the UK’s leading independent healthcare waste management company, recognising the continued impact of its technology-led approach, sector expertise and commitment to driving efficiency, compliance and cost control across healthcare estates.
Anenta was selected following a rigorous evaluation by a panel of C-suite executives, industry experts, and the editorial board of Healthcare Business Review. Judges highlighted the continued evolution of Anenta’s proprietary Vector platform, alongside the company’s proven ability to deliver measurable financial and operational benefits for healthcare organisations.
Saving clients millions
Highlights identified by the judges include Anenta’s work to save primary care clients over £13m in charges and the equivalent of £35m in efficiencies by cutting the amount of client staff time spent handling waste administration, auditing and dispute resolution.

This has been made possible through Anenta’s use of its proprietary Vector technology, which analyses hundreds of thousands of data points each month to identify any instances of waste collection or disposal partner billing inaccuracies so that these can be addressed before payment.
This rigorous yet collaborative approach, which identifies and addresses cases of overbilling, contract non-compliance or inefficiencies, was described by the judges as ‘setting a benchmark for best practice, valued by both healthcare providers and waste contractors for its focus on transparency, accuracy and continuous improvement.’
Alex D’Souza, Managing Editor of Healthcare Business Review Europe, commented on the award, saying: “Anenta continues to stand head and shoulders above other healthcare waste management service providers. Retaining this award reflects both Anenta’s consistency and outstanding leadership, as it continues to set itself apart through innovation, depth of sector knowledge and a clear focus on delivering tangi-
ble outcomes for healthcare organisations.”
D’Souza added: “The 2026 award recognises Anenta’s continued leadership in supporting NHS Integrated Care Boards (ICBs), helping unify complex waste arrangements under a single service specification, with consistent contract terms and a common environmental model. This scalable approach is raising standards across the healthcare waste management landscape, setting the bar for efficiency and collaboration.”
Graham Flynn, Managing Director of Anenta, commented: “This is a tremendous endorsement of our team, our technology and our approach. It is particularly meaningful because recognition comes from senior decision-makers who understand the operational and compliance pressures facing healthcare providers.”
Graham added: “As we move through 2026, we look forward to making a significant difference to an increasing number of businesses in the healthcare sector, enhancing levels of efficiency, compliance and cost control for healthcare estates, private healthcare businesses, dentists and care homes. Our focus remains on being a trusted partner — helping organisations operate with confidence, while continuously raising standards of healthcare waste management across the sector.”
Looking ahead, Anenta aims to build strong growth across its client base, with care homes and dental practices identified as key expansion areas. This reflects increasing regulatory scrutiny and risk in these environments, where correct segregation and management of clinical and healthcare waste is critical and time-consuming.
Anenta currently acts on behalf of more than 9,000 GP practices and 9,000 pharmacies across England, handling in excess of 39,000 healthcare waste management queries each year. It supports NHS organisations, GP practices, pharmacies, laboratories, dental practices and care homes. Its services include the provision of remote duty of care, and pre-acceptance audits, supported by free, standardised e-learning programmes. This approach helps clients meet their compliance obligations while reducing risk, enabling healthcare organisations to focus frontline teams on patient and resident care rather than administrative burdens associated with waste management. For more
Effective hygiene and odour management forms the cornerstone of quality care in residential and nursing home settings. Beyond mere cleanliness, these practices directly impact resident dignity, health outcomes, and the overall therapeutic environment that supports recovery and wellbeing.
THE FOUNDATION OF DIGNIFIED CARE
Personal hygiene represents far more than basic cleanliness—it embodies respect for the individual and recognition of their inherent worth. When residents feel clean and comfortable, their self-esteem improves, social interactions flourish, and psychological wellbeing strengthens. Conversely, poor hygiene practices can lead to social isolation, depression, and a profound loss of personal dignity.
HEALTH AND SAFETY IMPERATIVES
Proper hygiene protocols serve as the first line of defence against healthcare-associated infections. In residential settings where vulnerable populations live in close proximity, maintaining rigorous standards becomes critical for preventing cross-contamination and protecting community health.
Poor odour control often signals underlying health issues requiring immediate attention. Persistent odours may indicate skin breakdown, urinary tract infections, or inadequate wound care management. Staff trained to recognise these warning signs can intervene early, preventing minor concerns from escalating into serious medical complications.
Regular hygiene assessments should form part of comprehensive care planning, with individualised approaches reflecting each resident's preferences, cultural background, and physical capabilities.
BEST PRACTICE FRAMEWORK
Person-Centred Approach: Every hygiene intervention should begin with respectful communication. Explain procedures clearly, seek consent where possible, and honour personal preferences regarding timing, prod-
ucts, and assistance levels. This collaborative approach maintains autonomy whilst ensuring necessary care delivery.
Environmental Management: Maintain optimal room ventilation, use appropriate air fresheners sparingly, and address sources of odour promptly rather than masking them. Regular deep cleaning schedules, combined with immediate response to accidents, create pleasant living environments for all residents.
Product Selection: Choose gentle, pH-balanced cleansing products suitable for sensitive or compromised skin. Avoid harsh chemicals that may cause irritation or allergic reactions. Consider fragrance-free options for residents with respiratory sensitivities or cognitive conditions that may cause distress with strong scents.
Staff Training and Support: Comprehensive training programmes should cover infection control principles, dignity preservation techniques, and proper use of personal protective equipment. Regular refresher sessions ensure consistent standards across all care teams.
DIGNITY-PRESERVING
Maintaining privacy during personal care represents a fundamental aspect of dignified treatment. Use privacy screens, ensure doors remain closed, and limit the number of staff present to those directly involved in care delivery. Explain each step of the process and pause if residents express discomfort or distress.
Timing considerations prove equally important. Schedule hygiene activities around residents' natural rhythms and preferences where possible. Some individuals prefer morning care, whilst others feel more comfortable with evening routines. Flexibility demonstrates respect for individual choices and promotes cooperation.
Cultural sensitivity requires ongoing attention. Some residents may have specific religious or cultural requirements regarding personal care practices. Understanding and accommodating these needs shows respect
for diversity and supports emotional wellbeing.
When residents resist hygiene care, often due to cognitive impairment or past traumatic experiences, staff require specialised approaches. Gentle persistence, distraction techniques, and breaking tasks into smaller steps can reduce anxiety and promote acceptance.
For residents with dementia, maintaining familiar routines and using consistent caregivers helps reduce confusion and resistance. Simple, clear instructions and positive reinforcement encourage participation and preserve remaining independence.
BUILDING SUSTAINABLE SYSTEMS
Effective hygiene programmes require robust documentation, regular auditing, and continuous quality improvement processes. Track infection rates, resident satisfaction scores, and family feedback to identify areas for enhancement.
Invest in appropriate equipment and supplies to support best practice implementation. This includes adequate changing facilities, proper lifting equipment, and sufficient staffing levels to avoid rushing through personal care tasks.
CONCLUSION
Excellence in hygiene and odour control represents a fundamental expression of caring that extends far beyond basic cleanliness. When implemented thoughtfully, these practices preserve dignity, protect health, and create environments where residents can thrive with confidence and comfort.
The investment in comprehensive hygiene programmes yields dividends in improved health outcomes, enhanced resident satisfaction, and strengthened family relationships. Most importantly, it affirms the value and worth of every individual in our care, supporting their right to live with dignity and respect throughout their residential care journey.
Chiltern Water & Environment was established in 1991 by Robert Hunt after gaining 25 years' experience as an operational
We

professional but personable manner. Our steady growth has reflected our clients' trust in our services. Our current clients include large housing associations, pharmaceutical companies and facilities management companies, as well as individual landlords and small busi-
nesses. We ensure all our customers receive the same level of care and attention to detail.
Duty Holders of all commercial and public building premises are legally required to assess the risk from legionella to anyone using the water systems and put in place legionella control measures if required. The HSE has produced ACoP L8 and HSG274 as guidance for Duty Holders obligations.
We have clients throughout the South East, London and the Midlands, and carry out water tests nationally and internationally. We currently provide regular water sampling and testing for over 500 sites.
Tel: 01844 347678
Email: info@chilternwater.co.uk. Web: www.chilternwater.co.uk

Remedial works • Swimming and spa pool testing
Tel: 01844 347678
Email: info@chilternwater.co.uk www.chilternwater.co.uk
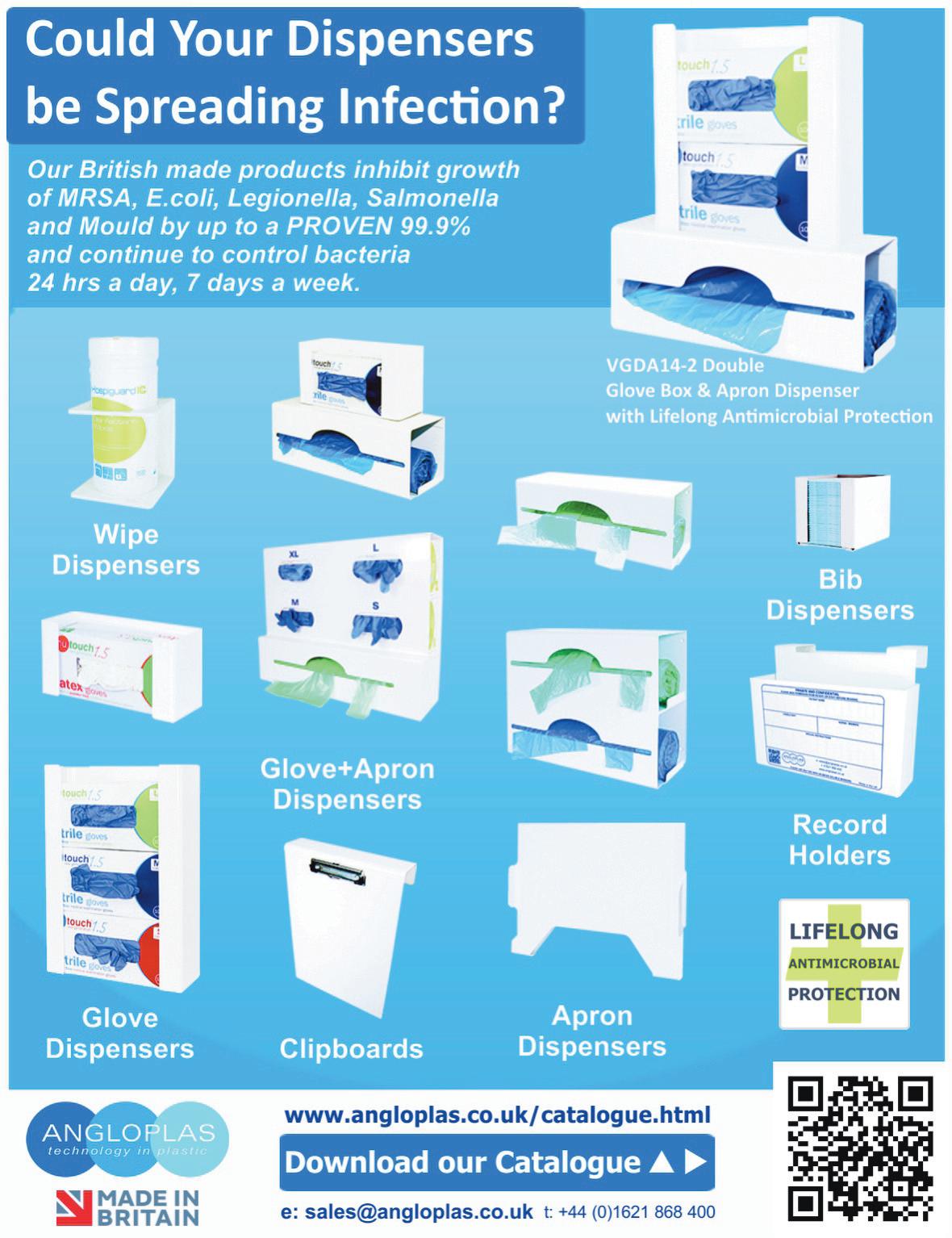
Angloplas are a UK manufacturer who specialise in producing dispensers for the health and hygiene industry. Although these are designed to keep the workplace tidy and uncluttered they are, more importantly, built knowing the control of healthcare-associated infections (HCAIs) are a priority for healthcare providers, and who are employing a combination of infection prevention and control strategies, including hand hygiene, cleaning, training and the adoption of new technologies, to tackle the problem.

As a result, a wide range of infection control products and technologies are emerging on the market, including antimicrobial technology. Angloplas’ range of dispensers are produced in the world’s first proven Antimicrobial PVC with silver ion technology and which is exclusive to Angloplas. This helps reduce the risk of cross infection by stopping the growth of bacteria and mould and works continuously for the lifetime of the product, reducing levels of bacteria such as MRSA, E Coli, Legionella, Salmonella and mould by up to 99.99%. For non-clinical environments Angloplas has recently launched its new Budget Range of products which are made to the same exacting standards as the antimicrobial protected ones but with lower price tags.
You can order Angloplas products directly from its website at www.angloplas.co.uk
by Lorcan Meikitarian, Chair of the CHSA

The world is changing, becoming more complex and challenging. It’s easy for business ethics to be a casualty but at the CHSA, we argue they have never been more important.
Ethical businesses operate with integrity, fairness and respect for people, communities and the environment. Rooted in the oganisation’s publicly stated core values, an ethical approach provides a framework for decision-making that brings with it reliability and accountability. These businesses are transparent in their dealings. They do not mislead, and they provide evidence that justifies the claims they make. This approach also fosters integrity and fairness, which inspires confidence and loyalty. It can also be a powerful motivator, attracting new talent and fostering commitment amongst the existing workforce. Ultimately, it underpins long term relationships, which in turn generate a better financial performance.
The words are meaningless if not backed up with the right action. For us at the CHSA, putting the talk about ethics into practice means five things:
1. adhering to national and international laws;
2. respecting human rights;
3. treading lightly environmentally;
4. cutting no corners when it comes to giving the customer what they believe they are paying for; and
5. and finally, being truthful, meaningful and transparent in all sales and marketing claims.
Adhering to the law is a given. Respect for human rights may be more complex. UK businesses in our

sector are likely to have it baked into their day-to-day operations. The challenge may come when examining their supply chains. In response we introduced a preference for an ethical audit for all CHSA manufacturing members. For CHSA Accredited Product, the manufacturer, whether based in the UK or overseas, must provide a copy of their most recent official ethical audit report. The report must meet the CHSA’s minimum requirement, and encompass labour standards, and health and safety. Compliance will be compulsory by the end of 2027. It will be a requirement of membership for those who fall within the Scope.
We all need to tread lightly environmentally. In 2022 we developed our Roadmap to Sustainability. It provides members with a framework for moving to sustainable solutions. Key to making a substantive, long term change is a thorough assessment of the corporate environmental impact. This requires a detailed understanding of carbon emissions at the product and corporate level. Calculating these emissions is complex. To support members, we delivered a webinar with a panel of experts able to provide guidance on overall approaches and the pros and cons of the different methodologies.
An ethical business supplies what it sells, without cutting corners. Setting and maintaining standards is in our DNA. We set up our Accreditation Schemes to tackle the problem of businesses selling product short or not fit for purpose. The Schemes have been incredibly successful. The logo for each Accreditation Scheme is a formally registered Trademark. It means every company displaying one must comply with the relevant standard and technical regulations. We audit accordingly and act wherever we find an infringement.
The fifth and final strand of our approach to ethics in business is honesty in sales and marketing. Our members do not play fast and loose with their sales and marketing messages and product claims, and they want their suppliers and the wider industry to know and understand this. This is why they introduced


a commitment to ethical marketing. It has four ethical principles:
1. All statements and claims are truthful.
2. Supporting evidence, such as data sheets, reports and certificates is available on request to substantiate all product and service claims.
3. All statements and claims are transparent. For example, it is clearly indicated if the claim applies to the product, the packaging or both.
4. All statements and claims are meaningful. For example, the term eco-friendly must be defined in relation to all aspects of the product and substantiated across the full lifecycle.
We are in the process of getting every member to sign this commitment.
Our Code of Practice underpins our entire ethical approach at the CHSA. Every member joining the CHSA makes a commitment to live by the Code; signing it is a requirement of membership. At its heart is a commitment made by every member to “maintain a high standard in the conduct of its business”.
In more detail it requires every member to conduct business dealings ‘in an open honest, fair and proper manner’, to ‘ensure all public statements made by and on behalf of the member are decent, honest and truthful’, to ‘hold and provide evidence on request for product and service claims’, and to ‘refrain from making inaccurate, misleading or malicious statements’. In essence it demands members trade ethically.
Our goal at the CHSA is always to advocate an ethical approach. Over recent years we have introduced many initiatives designed to bring this approach to life in very practical ways. This means our members’ customers and suppliers can trust them to trade honestly and fairly.


Sustainability and efficiency are top priorities for UK healthcare providers. With the government’s Net Zero 2050 target and NHS contracts requiring Carbon Reduction Plans that include Scope 3 emissions, kitchens must reduce food and plastic waste while controlling costs and protecting service users. It’s a challenging balancing act made much easier with the right tools. The Speedwrap Pro is the perfect example of a tool that delivers small, practical improvements that add up to major gains in productivity, safety, and sustainability.
It uses a patented safety blade that only unsheathes once the lid is pressed, reducing accidental cuts and lost time injuries. BioCote® antimicrobial protection inhibits harmful microbes, simplifying hygiene routines. And its intuitive design enables staff of all abilities to work efficiently, reducing food waste and ensuring proper storage and wrapping practices.
Hospitals like Stepping Hill in Stockport have already enjoyed all of these benefits, as well as the benefits of Ecocling - a PVC-free, recyclable film

exclusively compatible with Speedwrap Pro. It allows food waste and cling film to be separated for recycling; with food helping to power the national grid, and film being converted to refuse-derived fuel.
Erica Bell from Stepping Hill says: “As a trust, we love that Ecocling is recycle-ready and works with our food waste recycling process. The dispensers and refill rolls are modern, easy to clean, and safer to use. They make a real difference to our day-to-day operations."
Speedwrap Pro’s new refill rolls for cling film, foil, and parchment are plastic-free, replacing old adapters with cardboard cores. One catering service saved over 27,000 plastic adapters annually, cutting 178kg of plastic and enough CO2 to charge 1.2 million smartphones.
For healthcare kitchens, Speedwrap Pro is more than a dispenser – it’s a vital tool that cuts waste, improves staff safety, and reduces costs, all while maintaining the quality and hygiene standards critical to patient care.
Learn more at www.prowrap.co.uk or email sales@wrapex.co.uk
Mobile Kitchens Ltd specialises in the hire or sale of temporary catering facilities and foodservice equipment.
Ideal for events or to provide temporary catering facilities during your kitchen refurbishment, our versatile units and equipment offer an efficient and economic solution to the caterers’ needs.
Production Kitchens, Preparation Kitchens, Ware-washing Units, Dry Store Units, Cold Rooms and Restaurant Units are available as individual units in their own right or they can be linked together on site to form a complete complex. Alternatively, we can offer modular, open-plan facilities, usually for larger, longer-term hires.
We offer a free design service, and project management from concept through to delivery and installation on site, plus full technical support throughout the hire period.

We have many tried and tested design layouts and would be pleased to put forward our recommendations for your project.
So if you’re planning a refurbishment or need to cater for an event then why not give us a call and we’ll be happy to provide advice and put forward a competitive proposal.
For further information or to arrange a site visit, email: sales@mk-hire.co.uk or call us on 0345 812 0800, or visit our website: www.mk-hire.co.uk
Disease-related malnutrition remains one of the most persistent challenges in UK residential and nursing care. It affects millions, increases vulnerability to illness, slows recovery, drives hospital admissions, and places strain on already stretched care teams. Yet despite the scale of the problem, the tools available to homes have not kept pace with the needs of increasingly complex residents.
Hiquid Food, a Norwegian medical nutrition company, is entering the UK market with a clear mission: to make effective nutritional support simpler, more acceptable for residents, and easier for staff to deliver.
Simple, seamless meal enrichment
Many residents struggle to consume enough calories and protein, even with carefully prepared meals.
Hiquid Food’s freeze-dried powders, made from organic whole foods, allow caregivers to enrich everyday dishes like porridge, soups, puddings, purees, and drinks. This discreet approach reduces refusals and preserves dignity, helping residents receive the nutrition they need through meals they already enjoy.
ORAL NUTRITIONAL SUPPLEMENTS WITH HIGH ACCEPTANCE
For individuals at greater nutritional risk, Hiquid Food offers compact, nutrient-dense oral nutritional supplements designed for those with low appetite or increased medical demands. They are easy to consume, well tolerated, and provide balanced support in small volumes.
WHOLE FOOD GASTROSTOMY NUTRITION
For residents requiring enteral feeding, Hiquid Food’s whole-food gastrostomy products offer a

gentle, reliable option created with a focus on tolerance, safety, and long-term stability.
Better outcomes and operational efficiency
Care providers face rising acuity and workforce pressure. Hiquid Food products reduce complexity through easy mixing, no additives, and no large volumes while supporting improved resident strength, immunity, and recovery. Better nutritional status means improved wellbeing and lower overall care costs. With long shelf-life, low weight, and high versatility, the products are also environmentally responsible and easily integrated into a wide variety of meals.
As Hiquid Food launches in the UK through Food Untethered, they look forward to working closely with care homes, clinicians, and NHS commissioners to strengthen nutritional care in a practical, residentcentred way.
For more
information: contact@fooduntethered.com
See the advert below for further information.


Care homes across the UK are transforming how they deliver care thanks to SyndoraAlto, the newly rebranded name behind CHARIS, the UK’s most advanced digital nurse call system.
Fully supplied, installed, and maintained from just £6.40 per bed, per month, CHARIS delivers smarter, safer, and more connected care through real-time alerts, mobile integration, and intuitive smart displays that help staff respond faster when residents need them most.
Every CHARIS system comes fully inclusive with 15” smart displays, help buttons, pull cords, guaranteed radio coverage, and 24/7 UK technical support, all backed by SyndoraAlto’s trusted installation and maintenance team.
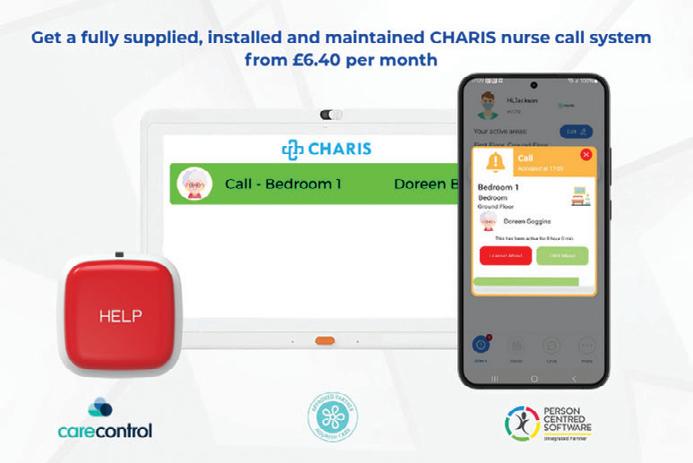
For care providers not yet ready to replace their existing nurse call system, AltoEnhance offers the perfect first step into digital care.
Available from just £129.00 per month, AltoEnhance seamlessly connects to your current nurse call system, bringing digital reporting, mobile alerts, and actionable insights without the need for a full system upgrade.
“Technology should make care easier, not harder,” says Louis Johnson, Managing Director. “CHARIS and AltoEnhance connect people, information, and action empowering care teams to deliver truly person-centred care.”
Meet the team & learn more at www.syndoraalto.com
See the advert on the front cover for more information.
Alarm Radio Monitoring is the market leader in the design, manufacture and installation of bespoke, end-to-end, wireless alarm systems and solutions for the healthcare, leisure, custodial and education industries.
We have been providing wireless alarm and nurse call systems for over 30 years. Supplying care homes and hospitals with an essential lifeline that supports the delivery of outstanding care. We believe in excellence which translates into: Advanced Technology Industry-leading wireless alarm technologies and software
Bespoke Solutions
We design systems to your needs rather than your team having to work around

Falls are a significant concern for vulnerable individuals, especially seniors and patients at risk. Medpage, a leader in assistive technology, offers a range of cuttingedge products designed to enhance safety and provide peace of mind for caregivers and families. Here’s an in-depth look at some of their standout solutions:
MPRCG1 (2023) BED LEAVING DETECTION ALARM WITH CAREGIVER RADIO PAGER
The MPRCG1 is a comprehensive system tailored for fall prevention in domestic, commercial, and NHS care settings. This all-inclusive kit includes a bed pressure mat sensor, a BTX21-MP alarm sensor transmitter, and an MP-PAG31 radio pager. The system is designed to alert caregivers when a patient leaves their bed, reducing the risk of falls.
HDKMB2 HOSPITAL DISCHARGE KIT FOR FALLS RISK PATIENTS
The HDKMB2 is a thoughtfully curated kit aimed at supporting patients transitioning from hospital to home care. It includes essential tools to mitigate fall risks and promote recovery. This kit is ideal for caregivers seeking a comprehensive solution to enhance patient safety during the critical post-discharge period.
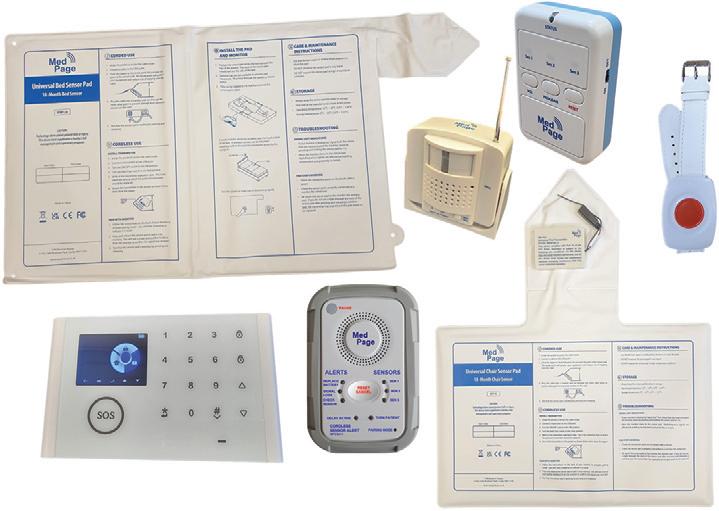
CMEX-21 MULTI-PORT WIRELESS SENSOR INPUT EXPANDER FOR NURSE CALL CONNECTION
The CMEX-21 is Medpage’s latest innovation, designed to integrate seamlessly with existing nurse call systems. This multi-port expander allows for the connection of multiple wireless sensors, enhancing the monitoring capabilities of healthcare facilities. Its versatility makes it a valuable addition to any care environment, ensuring timely responses to patient needs. RON-WC2 WATERPROOF DISABLED PULL CORD ALARM TRANSMITTER WITH WIRELESS ALARM RECEIVER
The RON-WC2 is a robust solution for disabled individuals requiring immediate assistance. This waterproof pull cord alarm is ideal for use in bathrooms and other high-risk areas. Paired with a wireless alarm receiver, it ensures that help is just a pull away.
For more information, visit Medpage’s official website or contact their team to explore these products further. Safety starts with the right tools, and Medpage delivers just that. www.easylinkuk.co.uk
T: 01536 264 869

The wireless ARM Nurse Call system has been developed over 30 years with both the client and user in mind.
It enables staff to efficiently answer calls, making the management of resources more flexible and provides the functionality you would expect of any nurse call system.
The system is quick and easy to install and works wirelessly, using radio communication between both the call points and the system infrastructure. Call messages can be sent direct to staff to speed up response times and can also be integrated to work with smart phones & messaging. Data Analysis software provides a full audit trail of events
The all-new call logging software from ARM enhances the functionality of your care call system dramatically.
• It can help you track the quality of your service to your residents.
• It can help you demonstrate compliance with your aims and best practices, both to relatives and to authorities.
• It can help you find bottlenecks in service provision, track staffing requirements, and allow you to ensure staff are meeting expectations.
• Most importantly, it provides assurance that you know and can demonstrate what is happening in your care home.
Courtney Thorne, a long-standing innovator in healthcare communication systems, is setting new standards in the care home sector with its advanced wireless nurse call technology—designed to improve resident safety, enhance staff efficiency, and support a more responsive care environment.
With over 30 years of experience serving the UK healthcare market, Courtney Thorne’s systems are now trusted by thousands of care homes nationwide. Unlike traditional hardwired solutions, their wireless nurse call systems offer non-invasive installation, scalability, and smart analytics—making them ideal for both new builds and retrofit projects.
“At the heart of our technology is the belief that better communication leads to better care,” says Graham Vickrage, Managing Director at Courtney Thorne. “Our wireless systems not only reduce response times but also empower staff with the tools they need to deliver safe, person-centred care.”
Care providers are increasingly choosing wireless systems for their flexibility, reliability, and cost-effectiveness. With a full suite of accessories—including neck pendants, door monitors, fall detection, and
bed sensors—Courtney Thorne systems can be tailored to meet the specific needs of each home and resident.
In an industry where compliance, safety, and staff pressures are always front of mind, Courtney Thorne provides more than just products—they offer ongoing support, training, and a commitment to innovation that helps care homes future-proof their operations.
For more information or to book a free demo, visit www.c-t.co.uk or contact info@c-t.co.uk.

We here at Edison Telecom Ltd have been providing specialist solutions to your call system requirements tailor-made to each customers needs for over 25 years, says director Bob Johnson. Is your current Nurse Call “legacy”, obsolete, so full of software bugs or commercially not viable for your current supplier/maintainer to maintain?

We may have just the part and expertise that you are looking for to give your nurse call a further extension to life, adds Bob, “Edison will treat your nurse call with the same compassion that you give to those in your care. There will come a time when your equipment is beyond repair but Edison are experts in extending the life of obsolete systems.” www.edisontelecom.co.uk



Every day, care organisations are working tirelessly to deliver essential support in the face of growing needs and rising costs. However, too many providers are stuck balancing tight budgets, having ‘just enough’ to stay afloat. The hard truth is, just enough isn’t enough—not for the providers, not for the employees, and certainly not for the clients who depend on them.
Rising operational costs—from wages and the Fair Pay Agreement to energy bills—compound historic underfunding and financial pressures. And demand for care continues to increase, creating a widening gap that organisations are often forced to fill with limited resources.
Providers then end up in survival mode, unable to invest in improving their services for today and the future.
THE NEED TO RETHINK FINANCIAL STABILITY
Care providers need to have healthy finances in social care, and that doesn’t come at odds with delivering compassionate care.
A financially strong organisation has the breathing room to improve services, retain employees, and innovate to make a meaningful difference to the lives of people they support. And having this financial security means providers can actually plan for the future rather than constantly reacting to the present.
BENEATH THE SURFACE
Social care organisations face a web of financial intricacies. Local authori-
ty support often comes with layers of red tape. Managing aged debt and resolving invoicing errors take a significant amount of time that few organisations can spare. Regulation and compliance require meticulous reporting, and the sheer volume of admin work to manage all these leaves teams stretched thin.
At the same time, there’s an expectation for providers to keep doing more. But without the right tools and systems in place, these compounded financial struggles threaten to overwhelm this indispensable sector.
PAVING A SUSTAINABLE WAY FORWARD
Social care providers aren’t just keeping their organisations alive; they’re safeguarding the wellbeing of countless individuals and families.
Providers need to be able to prioritise long-term financial resilience. And part of this means having the tools—including robust financial management softwaresimplify manual processes, optimise resources, and reduce inefficiencies.
By championing financial sustainability, we’re creating conditions where employees can thrive, where clients receive the quality of care they deserve, and where the sector can confidently meet future challenges.
Find out more at: www.oneadvanced.com/ai
See the advert on the back cover of this issue.
FALL SAVERS ® WIRELESS MONITOR
Eliminate all cables with our new generation falls management solutions!
Upgrade your falls programme with the latest technology from Fall Savers®. The NEW Fall Savers® Wireless eliminates the cord between the monitor and sensor pad. This results in less work for nursing staff, improved safety for patients and reduced wear and tear on sensor pads. Wireless advantages include the ability to use one monitor with two sensor pads simultaneously and support for many new wireless devices.

BENEFITS INCLUDE:
Safer for patients; less work for staff
Bed and chair pads available
One monitor works with two sensor pads
Integrates with most nurse call systems
A variety of options, including: Call button Pager
The TreadNought® Floor Sensor Pad is built to last with a durable construction that far out lasts the competition. Our anti-bacterial floor sensor pad is compatible with most nurse call systems or can be used with a portable pager to sound an alert when a person steps on to the sensor pad. Caregivers typically place the sensor pad at the bedside, in a doorway or other locations to monitor persons at risk for falls or wandering. An optional anti-slip mesh reduces the potential for slippage on hard surface floors.
FEATURES INCLUDE:
Connects directly to most nurse call systems
High Quality anti-bacterial Floor Sensor Pad
Large Size Pad: Measures (L) 91cm x (H) 61cm
Options (sold separately):
Anti-slip mesh for hard surface floors
See the advert on this page for further details or visit www.fallsavers.co.uk.
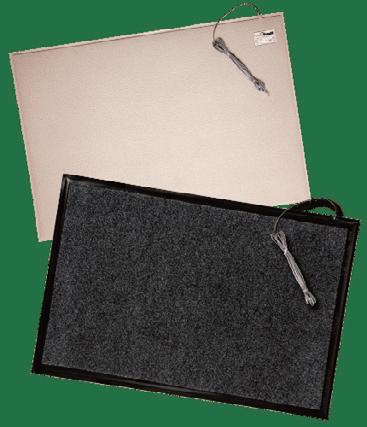

Working in social care is demanding. It is one of the most heavily regulated yet underfunded sectors, with providers expected to comply with regulations, meet Quality Statements, follow good practice guidance, respond to local authority monitoring, and operate under constant scrutiny.
Regulation itself isn’t the problem — it protects people and improves standards. The challenge is capacity. Larger organisations may have in-house quality assurance teams, but smaller providers rarely have the time or budget to review compliance in depth. Many owners and managers tell us they feel overwhelmed and unsure how well their service is really performing, especially since the introduction of the Single Assessment Framework.
For many, confidence in compliance is the number one concern — not because standards are poor, but because there simply isn’t time to step back and take a full, objective view.
CAN AN EXTERNAL AUDIT HELP?
In short, yes — when it’s done properly. A high-quality external audit provides:
• A clear snapshot of current performance
• Identification of good practice and priority risks

• Practical advice on how to improve
• Evidence to support action plans and improvement journeys
• Demonstration of good governance and continuous improvement — a key CQC focus
• Reassurance for owners, directors, and managers
HOW W&P CAN HELP
W&P have supported health and social care providers for nearly 25 years, completing hundreds of audits across a wide range of services. This experience gives us deep insight into what regulators look for — and what genuinely improves outcomes.
Our audits are supportive, non-judgmental, and practical. They typically include around six hours on-site, followed by a detailed report that links evidence to regulations and Quality Statements. Reports also include clear guidance, tips, and sources to help you respond confidently.
Every audit is tailored to your needs — whether that’s safeguarding, medication management, or overall governance — ensuring it is truly fit for purpose.
If you would like to know more, then please contact us on audits@wandptrainng.co.uk or call 01305
767104 for a no-obligation chat on how our audits can help you. See the advert on page 2 for details.
Competency assessment might not be anyone’s favourite phrase, but in domiciliary, residential, and specialist care, it is the backbone of safe, highquality support. The challenge is making it genuinely useful, not just another hoop to jump through.
Care staff need more than theory. They need time to learn, practise, and make mistakes in a safe environment before they are expected to apply new skills with real people. That is where a blended learning approach truly shines. High quality eLearning builds consistent knowledge. Virtual sessions keep teams connected and engaged. Face to face training gives carers the chance to try techniques, ask questions, and build confidence before working directly with residents and service users in their homes or care settings.
But learning does not stop in the classroom. Competency assessments in real care environments provide the feedback carers need to know they are using best practice techniques, communicating well, and delivering safe, person-centred care. It is the


bridge between “I know it” and “I can do it.”
This balance of learning plus real world assessment creates confident, capable staff who trust their own skills and feel supported rather than judged. Managers also get clear, reliable evidence for CQC and Skills for Care requirements without drowning in admin.
At myAko, we have developed tools with our long term partners, that make this process simple and sustainable. Better learning, better practice, better competency. It is a straightforward formula that leads to stronger teams and better outcomes for residents and service users.
Because when staff feel skilled, supported, and confident, the quality of care speaks for itself.
Kevin Ashley
Founder I CEO, myAko
myako.online/care
"23 years, operating 4 Devon Nursing homes, has been pretty tough, as anyone in social care, knows, only too well. And if it was hard already, after 2024 budget, it's just got harder.
Anyway, at heart, I am just customer of Eden Alternative, and it was a stroke of luck to come across this whilst on holiday in New Zealand in 2009. It started in USA in 1994 and now runs in 22 countries.
The fact that I am now involved with this not-for-profit organisation (in the UK area) came about when one of the 2 main UK directors died suddenly just before Covid. But it's something I have run with for 11 years to help make 'vision' a reality, not a struggle. So, being both a customer and helping the admin seems quite natural.
It is a modern philosophy of care, but moreover, it's a programme that is straight forward, tried and tested for 30 years and really works.

Its member care organisations generally become trainers for their own teams, and run it themselves.
The programme is run in person over 2-3 days or online 1 hr a wk for 7 weeks. You choose.
It addresses loneliness, helplessness and boredom and operates through 10 principles to underpin 7 critical domains of wellbeing.
Moreover, it's effective, transformational and really works. As residents, and team members wellbeing, matter so much , it's a must, in my opinion.
Geoffrey Cox
Southernhealthcare.co.uk
eden-alternative.co.uk"
Restrictive practices such as physical restraint, bed rails, or lap belts remain one of the most challenging aspects of health and social care. Intended to keep patients safe, they can also cause harm, distress, and loss of dignity when used unnecessarily. Across the UK, the principle is clear: care must always use the least restrictive option.
Legislation provides the framework, but culture and staff behaviour shape daily practice. Nurses, carers, and clinicians often make quick decisions balancing safety with autonomy. Without training, restrictive practices risk becoming routine. To change this, staff need better understanding of the human impact and confidence to use alternatives.
That’s where Restrictive Practice makes a difference. Developed through codesign workshops with patients and carers, this gamified e-resource gives a voice to those most affected by restraint. Their lived experiences shaped the learning, helping staff see restraint
not as a neutral safety tool, but often as something frightening or disempowering.
The results are powerful. Staff trained with the resource led Quality Improvement projects, achieving measurable reductions:
- Bed rails dropped from 360 to 277 incidents
- Bed bumpers from 303 to 227
- Lap belt use halved, from 46 to 22
These improvements represent safer, more compassionate care and reassurance for families.
Restrictive practices may never disappear entirely, but they should be the exception, not the rule. With the right knowledge and tools, staff can choose safer alternatives and build a culture of dignity, compassion, and respect across UK care services.
See our advert on the front cover or visit
Global assists clients throughout the U.K. who specialise in the healthcare sector to achieve their objectives of purchase, development and refinance.
We have organised over £1.8bn for clients in the past 30 years, providing clients with competitively priced funding to refinance existing debt, ease cashflow and develop businesses further.

From helping clients make their first purchase through to allowing groups to grow significantly in size we