It gives me great pleasure to report on a truly remarkable achievement in our sector: 80% of care providers have now adopted digital social care records, marking a transformative milestone for residential and nursing care across the United Kingdom. This digital revolution represents far more than technological adoption—it signals a fundamental shift in how care is delivered, documented and coordinated.
The impact of this transformation cannot be overstated.
The government estimates this digital-first approach will save approximately 30 million administrative hours annually, giving care workers back 20 minutes per shift—precious time that can now be devoted to what matters most: providing quality care to residents.
When you consider the scale of our sector, those minutes multiply into countless hours of meaningful human interaction, enhanced care delivery and improved quality of life for those we serve.
What makes this achievement particularly impressive is the pace of change. The number of providers using digital records has doubled from 40% to 80%, with significant momentum building since July 2024.
This acceleration demonstrates the sector's commitment to embracing innovation despite the considerable challenges many providers face.
The response from industry leaders has been overwhelmingly positive, and rightly so. Digital social care records streamline operations in ways that paper-based systems simply cannot match.
Care plans that once took seven days to complete and sign off can now be done in three days, whilst reviews that
previously consumed four hours can be completed in just 30 minutes.
This efficiency doesn't come at the expense of quality— quite the opposite. With information available at their fingertips, care staff can make better-informed decisions, reduce errors and ensure continuity of care across shifts and settings.
Here at THE CARER, we are particularly proud to have partnered with some of the country's leading digital software providers who can be seen in most of our print and digital issues.
These innovative companies have been at the forefront of this digital revolution, developing solutions that address the real-world challenges care providers face daily. Through automation, artificial intelligence and sophisticated data analytics, these platforms have significantly helped reduce both costs and administrative burdens whilst enabling more proactive, personalised and cost-effective care.
Our role in promoting these technologies and sharing expertise with the sector has been deeply rewarding.
We've witnessed firsthand how the right digital tools can transform operations, empower staff and ultimately enhance the lives of residents.
The innovations we're seeing represent just the beginning—I suspect artificial intelligence in care is still in its infancy, and we can expect to see remarkable developments in the years ahead. Rest assured, we'll continue bringing you the latest innovations, insights and practical guidance as this digital journey unfolds.
I was equally pleased to see the government's announcement of an £820 million support package aimed at helping almost one million young people aged 18-24 into work. This initiative is long overdue and addresses a crisis that has been building for some time.
Having attended numerous seminars over the years, I've heard repeatedly about the recruitment and retention difficulties plaguing our sector.
The funding will create 350,000 new training or workplace opportunities in sectors including construction, health and social care and hospitality—sectors where opportunities for meaningful careers genuinely exist. The care sector, in particular, offers something truly special that often gets overlooked in public discourse: it's one of the most rewarding
The Carer is published by RBC Publishing Ltd, 3 Carlton Mount, 2 Cranborne Road, Bournemouth, Dorset BH2
damage. Views expressed within this publication are not necessarily those of the publisher or the
responsibility for any effects, errors or omissions therefrom. All rights reserved, reproduction is

career paths available, with wonderful opportunities for progression.
But for those who find their calling in care, the rewards are profound. Where else can you make such a tangible difference to people's lives every single day? Where else do you have the opportunity to develop such a diverse skill set, from clinical competencies to leadership abilities? And where else can you progress from entry-level positions to management and beyond, often within just a few years?
However, for this government initiative to truly succeed in our sector, two things are essential. First, the programme must actively highlight the positive aspects of working in care—the job satisfaction, the career prospects, the sense of purpose that comes from making a real difference. Too often, public perception focuses on the challenges whilst overlooking the rewards. This needs to change.
Second, and crucially, comprehensive training must be funded and delivered effectively. The initiative will provide young people on Universal Credit support to develop on-thejob skills, employer networks and CV and interview coaching—all vital components.
But we need to ensure that once young people enter the care sector, they receive the ongoing professional development and support necessary to build sustainable, rewarding careers. Half-measures won't suffice; we need a genuine commitment to nurturing talent and investing in the next generation of care professionals.
The timing of this investment coincides beautifully with our sector's digital transformation. Young people entering the care profession today will be working with modern, efficient systems that their predecessors could only dream of. They'll be part of an industry that's embracing innovation, reducing bureaucracy and focusing increasingly on what matters most: providing excellent care.
This combination of digital innovation and renewed investment in our workforce creates tremendous opportunity. At THE CARER, we'll continue to champion both technological advancement and the people who make our sector what it is. There's much more to come, and we're excited to bring you every development along the way.
I can always be contacted at editor@thecareruk.com

(CONTINUED FROM FRONT COVER)
Earlier this year, NHS England set a target for 80% of care providers to have digital social care record in place by March 2025, following the failure to meet the original March 2024 target.
MEANINGFUL INCREASE
Stephen Kinnock, Minister of State for Care visited Kallar Lodge, a 24/7 residential care home in Dagenham, to see the Digital Social Care Records (DSCRs) in action and speak to staff about the improvements they have brought to their care roles.
Kallar Lodge’s digital care records system is integrated with the London Shared Care Record, which allows care staff to securely access some primary care data to make decisions about a person’s care.
Stephen Kinnock said: “This government is driving digital innovation, and digital care records are making a major difference for people drawing on care and their carers – with the number of care providers using them doubling from 40% to 80%, including a meaningful increase since July 2024.
“A one-stop-shop for a person’s care information – securely available to carers – cuts paperwork, helps reduce errors and gives carers more time to care.
“As we shift more care out of hospital and into the community, digital transformation is critical to ensure we create a coordinated system of social care and primary care.”
The government is shifting more care out of hospitals and into the community by delivering neighbourhood health services nationwide to bring together primary care, community care and social care teams.
Digital social care records the government said, brings key information about people’s care together in one place including:
• personal and demographic information
health conditions, including information on diagnoses, allergies and medical history treatment details including medication type, dosages and administration times care needs, care plans and individuals’ goals risk assessments, for example for falls, pressure sores or safeguarding all the care they have received, including information about meals, hydration, mobility support, interventions and social activities
• communication between their family and the care provider
BUREAUCRACY AND DUPLICATION
Welcoming the announcement The Care Software Providers Association (CASPA) said: “CASPA is proud to have played a vital role in the delivery of DSCR across the sector, working alongside DHSC, care providers and other partners to drive adoption, ensure data standards, and support the shift away from paper-based systems.
“Our work over recent years has helped to tackle one of the greatest practical barriers in social care: bureaucracy and duplication. By helping to implement DSCR broadly, CASPA has contributed to faster, safer care planning and better continuity of care, enabling care professionals to focus on people rather than paperwork.
“We believe this milestone demonstrates what can be achieved when government, industry and the care sector collaborate. But there is more to do: we remain committed to supporting full sector-wide DSCR rollout, as well as wider care technology adoption, ensuring interoperability, data security, and ongoing digital support so all providers can deliver modern, person-centred care.”
Professor Vic Rayner OBE, CEO of National Care Forum said: “The ability to increase the rate of digital adoption across such a broad range of organisations, in such a broad range of settings within such a short time frame is a testament to everyone involved in the delivery of social care.
“This news reflects years of hard work and determination by organisations and people who are committed to ensuring that everyone who receives care and support is not left behind and excluded from the opportunities that digital transformation presents.
“This is just the beginning of the digital potential for social care, and I look forward to the government working in partnership with the sector to build on the digital and data foundations this vital initiative has secured.”
Professor Martin Green OBE, Chief Executive of Care England, said: “Digital records are an important step forward, and many providers are already seeing the benefits in terms of safer, more coordinated and more efficient care. Today’s announcement recognises the dedication of providers and staff who have driven this change, often under very challenging circumstances.
“At the same time, feedback from our members shows that the journey has not been straightforward. Providers have experienced significant variation in local delivery, complex administrative requirements, and uncertainty about the ongoing costs once initial funding ends.
“These practical challenges matter and resolving them will be essential if digital transformation is to be sustained.
“We look forward to continuing to work with the government so that future phases of this programme are shaped by the realities of frontline care and ensure that every provider, regardless of size or location, can participate fully in the digital future of social care.”
Deborah Rozansky, Director of Policy, Research and Information at SCIE, said: “This is a significant achievement for a sector that started from a position where only around 40% of providers were fully digitised, and many were still reliant on paper-based records.
“Reaching the point where 80% of care providers are using digital social care records represents a fundamental shift in how care is planned, delivered and monitored. It also reflects the enormous commitment shown by providers, care staff, people who draw on care and support, local systems and national partners to modernise social care in challenging circumstances.
“The government’s ambition for a left shift and to move from analogue to digital is only possible if strong digital foundations are in place. Greater uptake of digital social care records supports more joined-up assessments, better shared decision-making, and a clearer, more complete picture of a person across health and social care.
“Learning from roundtables on national standards of care indicates that the biggest challenge now is not the availability of technology, but the collective will to redesign systems around people rather than processes. This should be accompanied by investment in relationships and infrastructure, ensuring that the drive to digitise strengthens, rather than diminishes, what matters most to people who draw on care and support. This must go hand in hand with supporting our workforce with the training and skills they need to continue to deliver solutions.
Care staff across shifts and settings can see the same information, supporting continuity of care, preventing errors caused by inaccurate records and crucially improving safety.
The government is also making it easier for care staff and NHS teams to see the same information to support a person’s care.
Through select digital social care records, social care staff in the appropriate roles can view limited information within GP records of those they care for using the NHS IT service GP Connect.
The information that can be securely accessed includes:
Last three encounters of interaction with professionals at the GP.
Details of current and previous medications
Information on allergies and adverse reactions
Active concerns and medical history
Immunisation record
Test results and referrals

The chief executive of
care and
charity, Sue Ryder, looks beyond the headlines of the Budget and sees a chink of light that could mean good things for the availability of palliative care. By James Sanderson (www.sueryder.org/about-us/our-people/our-leadership-team/james-sanderson)

The headlines that dominate the news after a Budget, predictably, talk about taxes, the cost of living and politicking as MPs and reporters pore over the detail. But on Budget day this year, there was an announcement that, while not headlines grabbing, is the source of hope for improvements to palliative and end-of-life care.
The UK Government has been talking about Neighbourhood Health
Centres for some months, and in the Budget they announced that 250 of these would be up-and-running by 2030.
Our hope is that these centres will embed palliative and end-of-life care and put it on an even keel with the other essential NHS services. This would make sure people, many of whom are in care homes, can access the end-of-life care they need.
It is quirk of healthcare-history that hospices sprung up in communities across the country to care for people with terminal cancer. And while palliative care in the UK is regarded as among the best in the world, the unplanned nature of how and where hospices have emerged has created inequity.
While the sector now supports people with any terminal diagnosis, it still tends to see people with cancer over-represented. What researchers call “the oldest of the old”, the over 85s, tend to be underserved, as are people from ethnically diverse communities. And because hospices emerged from charitable activity, what is available to people in one area might not be available to people in the neighbouring town.
There are many changes that need to happen in palliative care to fully address these challenges but the emergence of the Neighbourhood Health Centres offers a chance to significantly improve access to palliative care.
I really welcome the announcement of the new Neighbourhood Health Centres across England. Sue Ryder is calling for the palliative and end-of-life sector to be fully involved from the outset. Around 80% of the care we provide is in the community. By embedding the sector’s expertise as a vital service, we can guarantee high-quality, integrated care for people at the end of their lives.
I know many care homes will have fantastic links into local GPs, district nurses and their local hospice. But others will not necessarily have services on their doorstep that meet the full needs of residents approaching the end-of-life.
If the palliative care sector is involved in the setup, we’re hopeful that the new centres will improve access to palliative care but also improve efficiency for older people who, as we know, are living longer with many comorbidities and may need to see a number of healthcare professionals for different symptoms and conditions.
Care home staff are very much on the frontline of care for people at the end-of-life but not always recognised as such. If done right, these new centres can improve access to palliative care, particularly in areas where service provision is lacking, and could improve in-reach into care homes to better support both staff and residents.
There is great opportunity, and we are ready to work with Government to make sure it fulfils its potential.
Community Integrated Care’s Chief Corporate Services and People Officer, Teresa Exelby, has been named HR Director of the Year at the HR Excellence Awards.
The accolade recognises exceptional leadership in people strategy, culture and workforce transformation.
Teresa received the award in recognition of her significant contribution to strengthening Community Integrated Care’s culture, championing colleague wellbeing and leading sector influencing work that highlights the essential role of social care. Teresa has dedicated the achievement to colleagues across the charity, emphasising that the award reflects the commitment, compassion and teamwork shown every day by people throughout the organisation.

Since joining Community Integrated Care in 2020, Teresa has worked closely with teams at every level to deliver a people centred approach that places colleagues at the heart of the charity’s success. This has included major improvements in engagement, recruitment, development, inclusion and wellbeing, made possible through strong collaboration between the People Team, operational leaders and frontline colleagues.
Under Teresa’s leadership, the charity has continued to build a positive workplace culture with colleagues reporting high levels of pride, connection and motivation. Recruitment and retention have strengthened despite national challenges, and new learning and development programmes have supported hundreds of colleagues to progress in their careers.
The introduction of a pay uplift, the development of innovative wellbeing support and the embedding of
Pet therapy has become a part of the everyday routine in many care homes in the UK. The positive impact animals can have on the well-being of residents is well documented. But bringing animals into a care setting brings its own problems. It can be expensive and disruptive, they can be temperamental, and even the cleanest pets raise hygiene issues.
V-Thera virtual pets allow you to offer all the fun and engagement of a real pet, but in a clean, predictable and flexible way that fits in perfectly with your care home routine.
VIRTUAL PETS, REAL BENEFITS
From the moment the resident first puts the headset on, they are engaged and delighted as the pet sits, lies down, rolls over and feeds on command. They can even throw a ball for the pet to fetch. The experience is involving, relaxing and stimulating, enhancing a positive mood while encouraging movement and communication.
The pets themselves are wonderfully realistic, not just in the way they look, but in how they act. There are four dogs to choose from, and there’s even a moggie for cat lovers. They respond to voice or hand commands, or to big buttons on the screen. It’s ideal for previous pet owners, but also people nervous of animals.
TECHNOLOGY THAT CARES
V-Thera uses the latest Japanese mixed reality technology, meaning the virtual pet appears in the real-world, viewed through the headset. Seeing the
colleague voice have all contributed to making the charity an employer of choice within the social care sector.
Community Integrated Care has also gained national attention for its Unfair To Care campaign, which Teresa has championed on behalf of the charity and the wider workforce. The campaign has played an important role in raising awareness of the urgent need for fair pay and greater recognition in social care.
Reflecting on the award, Teresa said: “I’m incredibly proud, and this is very much a recognition of our entire People Team, our leaders and our colleagues across Community Integrated Care. Everything we achieve happens because of the dedication, compassion and kindness of our teams and the incredible work they do every day, often in challenging circumstances.
She continued: “I feel privileged to work alongside such talented and committed people, and I am proud to be part of such a truly special organisation that puts the people we support at the heart of everything it does.”
Jim Kane, Chief Executive Officer at Community Integrated Care, said: “This award is hugely deserved and reflects the extraordinary impact Teresa has had on our charity over many years. Her leadership has helped us to build a strong, inclusive and values-driven culture that supports colleagues and enhances the lives of the people we support every single day.
Teresa leads with integrity, compassion and purpose, and we are absolutely delighted that her work –and the remarkable work of our teams – has been recognised at a national level.”
familiar surroundings of their care home lounge reduces any sense of anxiety or disorientation for residents. The app can also be used lying down, so it can be used in bedrooms.
The technology itself is completely intuitive, designed for people with no experience of gaming. The headset reads hand movements, so there is no need for hand controls after set-up. Setting the app up is easy and quick for staff, with no training required. It comes preloaded onto the latest Quest 3s headset, so it’s a simple matter of staff switching the headset on, selecting the V-Thera icon, selecting the dog – which you can name – then transferring the headset to the resident. They are immediately immersed in playing with the dog or cat.

The makers recommend sessions of up to ten minutes at a time, it’s very easy to accommodate the technology into the life of the home, and for staff it can create an excellent opportunity to bond with residents. A sharing function even means the sessions can be cast to other screens so all residents can share the experience.
The potential of new technologies like V-Thera for engaging with residents in a positive way points to an exciting future. The combination of advanced Mixed Reality with intuitive and thoughtful design means care homes can adopt the latest technology without disrupting the care routines already in place.
V-Thera was created in Japan by Remedy & Co and is available now in the UK through Care Activity Ltd. Managing Director Alison Lang says, “The minute we saw V-Thera, it was clear to us that this was an exciting innovation, a new way to offer something genuinely engaging to care home residents. The pets are fun, realistic and always ready to play. It is technology that brings care to life.”
Contact alison@careactivityxr.com www.careactivityxr.com
Most over-45s are unaware of the true cost of funding a care home place according to new research that reinforces the need for the government to become more proactive helping people plan for the prospect of needing care in later life.
Research for the Just Group Care Report 2025: Social Care Reform –Stuck in the Waiting Room reveals the massive underestimation of the cost of going into care.
It reveals that 85% of those who had previously helped find care for a loved one were shocked at the cost. The data from the 13th edition of Just Group’s annual research, the UK’s longest running study tracking the knowledge and attitudes of social care among people aged 45+, shows that more than half (60%) think the cost of year’s residential care is less than £60,000, significantly lower than industry estimates for selffunders of £66,456.
How much people aged over 45 estimate a year’s residential care

costs More than three in 10 (31%) expected the cost would be up to £30,000 a year, less than half the true figure. About a third of people (32%) estimated the cost at more than £70,000 a year.
Stephen Lowe, group communications director at Just Group, said: “Year after year, our Care Report
shows people are unprepared for the true cost of care and those who do have experience of the system are left shocked at the level of fees when they come to help loved ones find a residential home.
“With an estimated four in five people aged 65+ likely to require some level of care before they die millions of families are sleepwalking towards a nasty shock.
News release “A combination of the failure of successive governments to grasp the nettle on care funding reforms and a sense that planning for care is too depressing has caused people to tune out of the social care issue. “With the recommendations of the newly established Casey Commission on care funding years away, the Government has a responsibility to make clear what the current rules are and ensure people understand their financial responsibilities for later-life care.
“Too often people are left grappling with unexpected and large financial costs at a time of crisis. Our view is that the Government must support people dealing with the system as it is now, not how it might be in the future, by clarifying its contribution to care costs and creating a ‘Care Wise’ guidance service to encourage people to plan ahead.
Residents at HC-One’s The Oakes Care Home in Huddersfield, West Yorkshire, have enjoyed a series of heart-warming trips to Blackpool over the past few weeks, sparking joyful memories of holidays and seaside adventures from years gone by.
Wrapped up warm against the coastal breeze, residents enjoyed leisurely strolls along the famous promenade, taking in views of the sea, the Blackpool Tower, and the busy beachfront.
The outings brought back fond recollections of childhood trips, weekend getaways, donkey rides, fish and chips on the pier, and the unmistakable scent of fresh sea air.
The visits also provided the chance to create new memories, rein-

forcing The Oakes’ commitment to enriching the lives of those in its care.
Maria King, Regional Admissions Coordinator, said: “Supporting our residents to revisit places that mean something to them is incredibly special. Seeing their faces light up as they remembered past holidays has been truly wonderful.”
Natalie Marshall, Wellbeing Coordinator at The Oakes, added: “Seeing the residents’ faces in Blackpool is heart-warming, we love creating memories for them. It’s moments like these that remind us why wellbeing activities are so important.”


When it comes into law, the Employment Rights Bill will bring sweeping changes to HR practices. Based on the Government’s Plan to Make Work Pay, it will bring into force widereaching reforms that will support employees and businesses across the country, with a view to creating a fair and level playing field and modernising the employment rights framework to suit the economy of today. Below we explore this subject further.
When the Government was formed in July 2024, it had already made numerous commitments to fundamentally change employment law in its pre-election manifesto, the Plan to Make Work Pay. Keeping to its promise of taking action within 100 days of coming into power, the Government released the Employment Rights Bill containing 28 specific reforms in October 2024. Since then, the Bill has undergone significant amendments as it has passed through Parliament, with intense debate happening over its provisions in both Houses of Parliament, and this continues even now, over a year later.
When they do become law, the proposals will change the HR processes for all employers, but some will be of particular interest to those in the care sector.
A new Adult Social Care Negotiating Body will be formed to facilitate the introduction of a fair pay agreement. These are not a common concept in the UK. The objective is to empower workers and the trade unions that represent them to negotiate fair pay and conditions, including staff benefits, terms and training and, in turn, improve domestic recruitment and retention. This will no doubt drive wages up meaning adult social care employers should expect to pay more to their workers. The Government launched a consultation on this on 30 September 2025, open until 16 January 2026, to ensure it hears representations from all areas before confirming plans. It will also monitor implementation of the agreement to make sure it delivers for both workers and employers.
As a separate measure, the Low Pay Commission (the advisory body on national minimum wage increases) has recommended that the issue of pay during a sleep-in shift should be addressed in the fair pay agreement. Currently, workers are not entitled to receive national minimum wage for time spent asleep during a sleep-in shift where suitable sleeping facilities are provided and the worker is expected to sleep for all or most of the shift.
Zero hours workers and low hours workers will, if proposals are confirmed, gain extra rights. They will

activity store
By Ren Spoors, Senior HR & Employment Law Advisor for
have the right to move to a guaranteed hours contract if, in practice, they work regular hours for a defined period.
The Bill also requires employers to provide workers with reasonable notice of shifts and changes to these, to make payments to workers if they change a shift at short notice and to provide written notices to their workers to explain their rights. This will increase the administrative burden on employers and will inevitably remove some flexibility they currently enjoy. On the flip side, some employers may realise that a more stabilised workforce benefits them.
From a wider perspective, there are proposals to change qualifying service for unfair dismissal. Currently, this right is not gained until two years’ service, however the Government wants to remove this entirely, providing the right from the first day of employment alongside a new statutory probation period during which “light touch” dismissals for reasons other than dismissal will be possible. Plans on what exactly this will involve, however, have not yet been released by the Government, although it has indicated that this probation period may be nine months long. This represents a dramatic change to current laws in which employees must wait two years for protection.
Other proposals include:
requiring employers to show that a flexible working refusal was reasonable
• paying statutory sick pay (SSP) from the first day of absence and removing the minimum earnings threshold, giving access to SSP to a much wider group of workers
requiring employers to take all reasonable steps to prevent sexual harassment at work and reinstating liability for third party harassment
requiring employers to inform employees of their right to join a trade union, and allowing trade unions greater access to the workplace to talk to staff
• introducing unpaid statutory bereavement leave, including for pregnancy loss before 24 weeks, and making paternity leave and parental leave a day one right
banning “fire and rehire” dismissals that seek to change employee terms and conditions for certain terms on a “restricted variations” list, including pay, pensions, working hours and shift patterns, except in extremely limited circumstances
implementing trade union reform including simplifying the recognition process.
Outside of the Bill, the Government has plans to gradually remove age bandings from the national minimum wage structure so that every adult worker benefits from a genuine living wage. No further clarification is yet available on what this means for the apprenticeship rate of pay.
Current rules on pay for travel time will be enforced for workers with multiple working sites.
There are still a few final parliamentary stages to go before any of these proposals are confirmed; change is not expected until 2026. Employers should use the lead in time to review current practices and prepare for what is anticipated to be significant change.


• We specialise in the sale and purchase of quality used wheelchair accessible vehicles and ambulances.
• They can be bought as seen or refurbished and sign-written to your own requirements.
• Fully serviced, new mot & warranty
• Engineers inspection supplied if required.
• Free delivery service available
• All buses comply with new legislation
•


The Care Quality Commission has announced a comprehensive improvement plan aimed at overhauling its regulatory approach by the end of 2026, with significant implications for care home providers across England.
The health and social care regulator has acknowledged the need to tackle urgent operational issues that have impacted providers in recent months. Registration backlogs and lengthy application processes have been particular pain points for the sector, prompting CQC to trial a simplified registration form and enhanced online guidance.
The watchdog reports progress on these fronts, with increased staffing levels in registration teams leading to a steady rise in completed applications. The organisation has also restructured into four operational inspectorates under dedicated Chief Inspectors, focusing on specific areas of sector expertise.

CQC says it is on track to complete 9,000 assessments by September 2026, representing a significant increase in inspection activity.
Beyond immediate fixes, the regulator is embarking on a more fundamental transformation of its assessment framework and methodology. This work draws on recommendations from several external reviews, including reports by Dr Penny Dash, Professor Sir Mike Richards, and the Care Provider Alliance, as well as an independent IT review.
The planned changes encompass a complete redesign of the regulatory process, new assessment approaches, improvements to the provider portal, and substantial upgrades to digital systems and data management.
Learning from past experiences, CQC says it will implement changes in a phased manner with regular review points to ensure the reforms don’t compromise inspection capacity.
TIMELINE AND NEXT STEPS
The transformation roadmap extends to the end of 2028, with concentrated activity planned for 2026. Key milestones include:
• Spring 2026: Analysis of consultation feedback to develop new assessment frameworks
• Summer 2026: Publication of final assessment framework and supporting guidance for providers
• Late 2026: Implementation of new assessment approach begins
• Ongoing: Continued improvements to registration services and digital infrastructure
CONSULTATION CLOSES SOON
Care home operators have until 11 December to respond to CQC’s ‘Better regulation, better care’ consultation on the proposed assessment framework. The regulator is running targeted engagement sessions for different care sectors, including a dedicated adult social care workshop on 3 December.
An in-person event for adult social care providers will take place in London on 10 December, while service users can participate in online focus groups on 16 December.
CQC has emphasised that provider feedback will be central to shaping the final framework, urging care home managers and owners to participate in the consultation process.
The changes represent the most significant overhaul of CQC’s regulatory approach in years, with the potential to substantially alter how care homes are assessed and rated in England.
A World War Two veteran who played a supporting role in Britain’s wartime intelligence efforts has been honoured as she marked her 102nd birthday.
Doctor Jean Munro, a resident at Lynemore Care Home in Grantown on Spey, was a member of Hut 6 at Bletchley Park, the team responsible for deciphering German Army and Air Force Enigma messages.
Earlier this year, Dr Munro took part in a podcast to mark the 80th anniversary of VE Day. In it, she revealed that she was unable to share details of her top-secret work with family and friends until the 1980s.
Historians believe that breaking the Enigma code may have shortened the war by two to four years, potentially saving hundreds of thousands of lives. “I never thought of it that way, but if I think about it now, I think I’m really glad,”
she says.
In recognition of her service, Dr Munro has been awarded the Freedom of Bletchley Park, a rare honour conferred by the Bletchley Park Trust, and presented with a specially made Veteran’s pin badge.
Pamela Cummings, manager of Lynemore Care Home, said: “We feel deeply honoured to have celebrated not only this milestone birthday, but also the presentation of such an incredible honour in recognition of Jean’s vital work as a codebreaker at Bletchley Park.
It was an emotional occasion to share this double celebration with Jean and her loved ones. She is a remarkable lady and a much-loved part of the Lynemore family.”



When it comes to scaling a care group, the expansion itself is often not the real challenge. The challenge most face is growing without drifting from the values that made the work meaningful in the first place. One significant learning for many of us that have grown a business, is that scale only works when the heart of the organisation grows with it.
The care sector is shaped by regulation, demand and financial pressure - but it’s also personal. Without a clear vision of the experience you want people to have in your homes, growth can quickly become a distraction rather than an achievement. Leaders with clear values that they take with them in everyday life have an anchor that helps guide decisions through periods of change.
The culture within a care home is an essential consideration; it’s easy for this to weaken as numbers increase. To avoid this, leaders need to think carefully about the signals they send to staff and residents.
Something as simple as removing institutional markers, or creating spaces that feel domestic rather than clinical, can help build relationships rooted in humanity rather than hierarchy. Consistency in these choices across new settings is what allows an organisation to grow without becoming faceless.
Staff retention across multiple homes
Recruitment is another area where a shift in thinking can make a profound difference. While practical skills remain important, these are teachable. It’s the emotional intelligence that’s important to look for. You can train someone to use equipment or complete a task, but you cannot train a person to be kind, patient or genuinely curious about others. When you scale, you’ll inevitably bring in people who have not grown up within the culture of the original homes. Recruiting for character gives the organisation a better chance of protecting its identity across multiple sites.
When growing your care group, you need to take your team with you. Internal progression only serves to help strengthen retention - and staff are more likely to remain loyal when they can see themselves in the future of the business. By investing in training, offering qualifications and helping people build confidence and capability over time, you can contribute to a workforce that feels valued. When staff develop from within, the culture gains continuity - which directly improves the quality of care delivered.
FINANCIAL SUPPORT FOR STAFF
Financial wellbeing is also an area that is sometimes overlooked in discussions around scaling. Practical support such as access to meals during shifts or financial wellbeing tools can ease everyday pressures. When a workforce is not carrying constant financial anxiety, relationships within the home tend to be stronger and retention improves. Going above and beyond the government set minimum wage can also
By Lucy Atkinson of Church Farm
make a huge impact on your staff’s day-to-day living; at Church Farm Care, we became a living wage employer to help ease financial stress on our teams. These interventions are more than benefits; they have a strategic purpose because they create a baseline of stability on which quality can be built.
BUILDING A HOME THAT’S FIT FOR PURPOSE
When growing a care group, the physical environment should not be neglected. The environment should not be treated as a backdrop, but a home - and an active contributor to wellbeing. Access to fresh air, sensory gardens, homely lounges, quiet spaces and areas that encourage movement all make a difference to mood and engagement for both residents and staff. As the number of homes increases, it can be tempting to replicate designs for efficiency. Although some consistency is helpful, the key is to maintain a focus on how each space will feel to the people who live and work in it.
UTILISING TECHNOLOGY FOR THE DIGITAL AGE OF CARE
Technology has become a valuable ally in scaling without compromising quality. Digital care planning, acoustic monitoring and movement sensors can improve accuracy and safety while giving staff more time to focus on meaningful interactions with residents. However, it’s important to introduce technology thoughtfully. The aim should be to enhance human connection, never to replace it. When implemented well, technology becomes an invisible support that allows staff to do what they do best.
Owning and running Church Farm Care for twenty years has taught me that business growth only works when values and culture scale at the same pace as buildings and staff. Growth must align with purpose, carried by people who feel valued and supported. For leaders considering expansion, I always return to the same principle: a care group can only grow successfully when the experience of those living and working within it remains at the centre of every decision.
B&M Care have launched three new complex dementia care hubs at Osbourne Court in Baldock, The Radley in Borehamwood and Dalton Lodge in Walthamstow.
The hubs are created for people whose dementia has progressed beyond what traditional residential care homes can safely support, giving families somewhere to turn when options often feel limited or impossible to find, providing highly specialised environments for residents living with advanced or challenging dementia, including people under 65 with young onset dementia who frequently fall through the gaps in existing services.
Currently, it’s estimated there are 982,000 people living with dementia in the UK, and that number is predicted to increase to 1.4 million by 2040. Some people living with dementia experience severe or very advanced symptoms that can lead to intense distress for both the individual and their loved ones. Families often describe this stage as isolating, frightening and difficult to talk about, especially when behaviours such as heightened distress, extreme agitation, aggression, hallucinations and sexualised behaviours begin to emerge.

These symptoms are widely misunderstood and can become overwhelming for relatives as well as care teams who may lack the training, space or resources to offer safe, therapeutic support. With 1 in 6 hospital beds now occupied by someone living with dementia, and forecasts estimating this
is set to increase to 1 in 4 by 2040, people with complex needs are increasingly admitted to hospital simply because there is nowhere else equipped to care for them, B&M Care’s new centres help prevent avoidable hospital admissions and lengthy stays, reducing pressure on NHS bed capacity while giving individuals more dignified, appropriate care.
Caroline Inch, Director of Dementia Care and Operations from B&M Care said, “opening these hubs reflects our commitment to supporting people whose dementia has progressed to a point where families often feel frightened, exhausted and unsure where to turn. People living with complex dementia may have been assessed as unsuitable for other care homes where staff and facilities cannot provide the specialist dementia care their complex needs require.
“Our Complex Dementia hubs provide a compassionate, specialist environment so people who struggled to be supported elsewhere can receive the care they need, moreover this gives reassurance to families in their time of need. By creating these specialist environments, we are also providing the NHS with a trusted partner at a time of significant pressure. Our goal is to give individuals the dignity, safety and personalised care they deserve while helping local services keep people in the right place for their recovery and long-term quality of life”.
The Local Government Association (LGA) and campaigners are calling for urgent action to tackle the exploitation of vulnerable people through ‘patient brokering’in England’s drug and alcohol treatment sector. Patient brokeringinvolves individuals or organisations receiving financial incentives for referring patients to specific private addiction rehabilitation centres, regardless of whether it is in the best interest of the clinical needs of the patient.
Many organisations provide high-quality addiction support but a rise in unregulated private providers has created opportunities for unethical practices to flourish. The practice can lead to inappropriate placements, inflated costs, and compromised care outcomes.
The latest figures published today show that the number of adults in contact with treatment services for drug and alcohol misuse in 2024/25 was up by six per cent on the previous year. This increase sees the highest number of adults in treatment since records began, suggesting there are more vulnerable people at risk of being exploited by unethical patient brokering practices.
The LGA, which represents councils responsible for public health, is warning the practice risks exploiting vulnerable people, risks long-term harm for those seeking recovery, and undermines public confidence in addiction treatment services.
Anyone seeking help for drug or alcohol issues is encouraged to contact their local council, GP, or trusted services such as FRANKor the NHS for free, confidential, and impartial support.
THE LGA IS URGING THE GOVERNMENT TO TAKE DECISIVE ACTION TO:
• Introduce legislationbanning patient brokering and imposing penalties on those who engage in or facilitate it.
• Create a single registered online gateway for the public to access professional addiction help.
• Support and resource local authoritiesto raise awareness and safeguard individuals from exploitation.
• Promote community, NHS and charity-led services, which operate under strict ethical guidelines and offer person-centred care, ensuring efficient use of public funds.
Cllr Dr Wendy Taylor MBE, Chair of the LGA’s Health and Wellbeing Committee, said: “Patient brokering is
a deeply concerning and unethical practice that puts profit before patient wellbeing.
“Vulnerable individuals seeking help for addiction deserve safe, ethical, and clinically appropriate care, and not to be treated as commodities at one of the most vulnerable points in their addiction recovery.
“We must protect the integrity of our addiction treatment system and ensure that adequate safeguards are in place so that every person seeking help is met with dignity, compassion, and respect.”
by
in
year to end June 2025.
The Scottish Government has invested £500,000 to help displaced adult social care workers who are already in the UK, and have found themselves without sponsored employment through no fault of their own.
This fund will help remove barriers faced by these workers when trying to find employment within the Scottish adult social care sector.

Announcing the opening of the fund in the Scottish Parliament today, Social Care Minister Tom Arthur said: “The UK Government’s decision to end the international recruitment of care workers, without sufficient notice or any substantial consultation on the impact, has already been devastating for the care sector in Scotland.
The industry is highly dependent on international workers and we greatly value the contribution made by people who settle and work in our communities.
“The impact of the UK Government’s measures will exacerbate existing workforce shortages across the care sector and directly undermine the ability to provide safe, dignified and consistent care to some of the most vulnerable members of our society.
“Scotland has many talented and compassionate international care workers who call our country home, and through this £500,000 fund I am determined that workers be welcomed here, supporting our communities and making a difference in the lives of our most vulnerable.”
Scottish Care Chief Executive Dr Donald Macaskill said: “Scottish Care welcomes the launch of the Adult Social Care Displaced Worker Scheme and the vital support it offers to international staff who play an essential role in Scotland’s social care sector.
“Recent Home Office policy changes have once again intensified pressures on care providers and staff teams at a time when demand for services is high and organisations continue to face significant challenges in recruiting sufficient numbers of skilled workers.
“Scottish Care will continue to work with the Government and other partners to ensure these valued colleagues remain part of our communities and to advocate for sustainable workforce solutions that safeguard the future of social care in Scotland.”
Staff and Residents at Iris Court Care Home welcomed members of local veterans’ group “ The Muster Point” for a special “Ploughman’s and Patriots “afternoon, which celebrated service, sharing stories and community connection.
Residents and visitors enjoyed a traditional ploughman’s lunch whilst engaging in lively conversation, particularly with the homes residents who had served in the Armed Forces.
The Muster Point attendees expressed their gratitude for the home’s hospitality and meaningful interaction with the residents this afternoon.
The Muster point understand the importance of Veterans supporting Veterans and maintaining strong links In the community.
Following the success of the event, The Muster Point has confirmed it will return to Iris Court with its additional members in 2026, strengthening this growing partnership and ensuring continued support for local veterans.
Tash Begum, General Manager at the home, said: “Iris Court Care Home remains committed to honouring those who have served and look forward to hosting more events that celebrate unity, respect and remembrance.”








Low pay, job insecurity and post-Brexit recruitment challenges are plaguing the adult social care sector in England. With rising demand and chronic underfunding, work conditions are only getting worse. Andreas Georgiadis and Andreas Kornelakis, Associate Professors at Leeds University (www.lse.ac.uk) suggest ways to improve the situation, including better pay and training.
Adult social care suffers from a long-standing “workforce crisis” in England. Recent reports from industry bodies highlight the challenges to the sector’s workers and their ability to offer high quality care. Staff in social and health care are overworked, exhausted and stressed, sometimes to the point of becoming ill, leading to absenteeism or quitting altogether.
Increased workloads and time pressures arise partly due to increased demand for services by a rapidly ageing population. At the same time, over half of adult care providers said they faced challenges recruiting new staff; 31 per cent struggled to retain employees. Difficulties in recruitment and retention intensified after Brexit, as the sector relied heavily on migrant workers.
It is widely known that adult care is one of the lowest paying jobs in the UK. Forty-three per cent of all adult social care workers in England are paid below the real living wage. It will continue to be challenging
for care providers to retain pay differentials between those on the wage floor and those with more experience and qualifications. But pay levels are not the only challenge for care workers, as they also face problems of job insecurity and unpaid overtime.
For example, most of those who do home visits are not compensated for the time they spend travelling to homes, which can make up to a fifth of their working day. The use of contingent contracts in social care may deliver some cost savings for providers, but has the drawbacks of job insecurity for workers, and concerns about service quality.
Funding cuts have also contributed to the workforce crisis. The Health Foundation estimates an additional £8.3 billion will be required by 2033 just for adult social care to keep up with growing demand. In response, the Labour government charged Baroness Louise Casey with preparing a report to recommend ways to address the sector’s funding and workforce crisis. But the independent commission will make its final report by 2028. Until then, problems are expected to pile up.
Nonetheless, the government’s plans on immigration, and especially the axing of care worker visa, will only exacerbate the recruitment and retention problems. Indeed, as Unison’s general secretary, Christina McAnea, stated “…the care sector would have collapsed long ago without the thousands of workers who’ve come to the UK from overseas”. Similarly, Martin Green OBE, chief executive of Care England, characterised the government’s plans as “a crushing blow to an already fragile sector”.
Our recent research offers insights on how to fix the crisis. We propose that “high-road” workforce practices can improve rather than hinder, as it is commonly believed, the operational performance of care providers. We find that relative pay increases and pay progression are strong motivators for employees and this provides support to the longstanding demand by union leaders for a fair-pay agreement in the sector. Investing in skills pays off, especially for those providers who suffer from long-term underinvestment.
The evidence suggests that increased investments in staff training, improved pay, career pathways to promotion and permanent contracts could address the poor performance of care providers. Alternatively, it
also explains why strategies based on cutting costs via the adoption of “low-road” practices, characterised by low-pay growth and lack of investment in skills are likely to be counterproductive.
Evidence also tempers unrealistic expectations that investment in training and rewards practices is a panacea for care providers. They are much more likely to be effective in “low-road” organisations, characterised by persistently poor performance and workforce skill gaps.
We suggest that the effectiveness of “high-road” pay and training practices is expected to reduce after a threshold level of collective staff skills, knowledge and experience is reached. At that point other interventions are needed, for instance, improving efficiency using advanced technologies such as artificial intelligence.
To sum it up, care providers trapped in “low-road” workforce practices can especially benefit from investment in workforce pay and training, which can bring about considerable improvements in their operational performance. Government should therefore move away from visa restrictions. It should also aim to address the adult care crisis by supporting care providers’ investment in their staff and funding comprehensive training and upskilling programmes. It may also enable improved pay and working conditions by supporting sectoral collective bargaining.
High-road practices can help tackle longstanding performance and turnover challenges. These insights are also likely to be relevant to other sectors with similar characteristics. For example, sectors such as childcare, hospitality or retail, which are heavily tilted towards personal services and interactions with users/customers, and at the same time, rely on a workforce that is predominantly less skilled and low paid.
• Andreas Georgiadis is an Associate Professor at the International Business Department of Leeds University Business School and a Fellow of the Global Labor Organization (GLO).
• Andreas Kornelakis is a Reader (Associate Professor) at King’s Business School, King’s College, and a Research Associate at LSE’ Hellenic Observatory.
A care home in Surrey has donated £1,600 to a local charity following a successful ‘night of music’ this summer.
Appleby House, Care UK’s home in Epsom, hosted a magical evening for residents, relatives and the community, by inviting singers to perform at their annual event.
The evening included a raffle, dinner and dancing, and raised £800 for local charity Love Me, Love My Mind. The organisation aims to break down stigma and inspire understanding about mental health. Care UK matched Appleby House’s funding, bringing the total raised to £1,600. The care home’s annual ‘night of music’ started back in 2017 and Home Manager Shona Bradbury believes it is the most anticipated event of the year for residents and the community alike.
Shona said: “When people walk into the marquee, we want them to be blown away. It’s all glittery, and ball gowns and tuxedos. Everyone gets really dressed up!

“It’s an amazing event, and we get to raise money for local charities at the same time. . Looking after your mental health, and raising awareness of support that’s available, is becoming more and more important. It means a lot to us to be able to support Love Me, Love My Mind
“We find that music transcends age and conditions like dementia – colleagues, residents, and the com-
munity just want to get together and listen to amazing singers all night. Appleby House has nurtured a long-standing relationship with Love Me, Love My Mind through their work. This includes weekly collaborations between the charity and the care home throughout the summer in Appleby House’s allotment and garden.
Allen Price, Chief Officer of Love Me, Love My Mind said: “We are delighted to receive a donation of £1,600 from Care UK and Appleby House. For a number of years, Appleby House has donated gifts and presents to our Monday drop-in Christmas dinner, and this generous gift each year makes an enormous difference to our members.
“Two years ago, we started volunteering at Appleby’s forget-me-not allotment. We now have six volunteers from our charity taking part every Wednesday and the allotment looks amazing! It is heartwarming to see residents, families and staff spending time together making memories in the garden.
“Appleby House and Care UK are a very important partners for our grassroots mental health and wellbeing charity, and we are really looking forward to getting out in the garden again next year to grow vegetables, flowers and plants.”
Meadow View Nursing Home in Chesterfield has found a grand(e) way to support a new resident with scoliosis- an innovative vacuum posture cushion.
The middle-aged client joined the home after a spell in hospital: underweight and fragile, she needed additional skeletal support and 1:1 care. Meadow View- part of Emh Care & Support- could provide the high quality round-the-clock attention she required.
The home’s nurses responsible for the lady were struggling to find a way to keep her comfortable and safe in bed. They raised the issue with the home’s Occupational Therapist, who suggested AAT’s Grande mattress with Treat-Eezi cover.
Using vacuum technology, the mattress-sized beanbag can be contoured exactly by the staff exactly as needed, to provide the lady with a secure yet comfortable position without pressure points.

By using the vacuum principle, any air in the cushion is removed, thereby fixing the moulded shape and removing the need for frequent re-positioning. The shape and firmness of the Grande can be adjusted as little or much as needed. The cushion can be precisely moulded to create abduction and adduction wedges, or an asymmetrical body position- all by the care-givers, within minutes(1). The addition of the Teat-Eezi overlay helps maintain blood flow and gives an extra layer of protection against the risk of ulcers.
Meadow View Manager Gillian Kent comments, “The Grande gives support to her overall body structure, yet is soft and comfortable. The team find it’s easy to reform when she is supine, so they can ensure her continued relief and security when she’s lying in her bed. It has really helped her overall daily and nightly relaxation.”
Find out more about AAT’s Grande vacuum posture cushions here: www.aatgb.com/grande
A major government funding package worth £820 million is set to create 350,000 new training and workplace opportunities for young jobseekers, with significant implications for the health and social care sector.
Young people claiming Universal Credit will gain access to roles across construction, health and social care, and hospitality, receiving on-the-job skills development, employer networking opportunities, and professional coaching in CV writing and interview techniques. The initiative will support 900,000 young Universal Credit claimants who are actively seeking employment. Following an initial dedicated work support session, participants will receive four weeks of intensive guidance before being referred by their work coach to one of six tailored pathways: direct employment, work experience, apprenticeships, broader training programmes, further learning, or workplace training schemes offering guaranteed interviews developed in partnership with employers.
For the care sector, which continues to face persistent recruitment challenges, this investment represents a vital opportunity to attract young people into rewarding careers in health and social care whilst addressing workforce shortages across residential and nursing home settings.
As part of this training, young people will receive six weeks of training, work experience, and a guaranteed job interview, giving young people their first foot in the door towards meaningful employment, boosting their prospects and supporting a stronger economy as part of our Plan for Change.
55,000 young people also stand to gain from a government-backed

guaranteed job, which will begin roll-out from Spring 2026 in areas with some of the highest need in Great Britain.
THESE REGIONS ARE:
• Birmingham & Solihull
• East Midlands
• Greater Manchester
• Hertfordshire & Essex
• Central & East Scotland
• Southwest & Southeast Wales
More than 1,000 young people are expected to start a job in the first six months alone, with local partners and employers to play a key role in supporting young people as they transition into meaningful employment with fully funded wages and wraparound support for young people.
Alongside this, Youth Hubs – centres where young people can
receive vital help to get them back on track – will be expanded to every local area of Great Britain, bringing the total to over 360. This will ensure young people up and down the country can access the lifechanging support Youth Hubs offer, such as CV advice, skills training, mental health support, housing advice, and careers guidance.
There is an expectation that young people will take up the opportunities they are offered, and sanctions to benefits could be applied for those who don’t engage with the offered support without good reason.
Work and Pensions Secretary Pat McFadden, said: “Every young person deserves a fair chance to succeed. When given the right support and opportunities, they will grasp them.
That’s why we are introducing a range of reforms to help young people take that vital step into the workplace or training and to go on and make something of their lives.
“This funding is a downpayment on young people’s futures and the future of the country, creating real pathways into good jobs and providing work experience, skills training and guaranteed employment.
Richard Rigby, Head of UK Government Affairs at The King’s Trust said: “At The King’s Trust, we know that when you match young people’s potential with opportunity, they can transform their own lives. This Youth Guarantee is a crucial step towards unlocking that potential.
“Increasing training and work experience opportunities, alongside a guaranteed job scheme for the long-term unemployed, will help the young people we support in our centres each day to start overcoming the barriers they face, and take their first steps into work.
If we get this right, we can transform the futures of young people out of work across the UK, and build a healthier, wealthier society.”
Christian Whiteley-Mason, a highly respected Registered Manager, has been honoured with the Recruitment and Retention Award at the inaugural Stars of Social Care LD and Autism Awards.
The awards celebrate outstanding individuals across the learning disability and autism sector, recognising those who make an exceptional difference to the lives of the people they support. Christian’s dedication to building a strong, compassionate, and committed team has set a benchmark for excellence in social care leadership.

Christian said he was incredibly proud to receive the award, reflecting on the evening as “amazing, so Christmassy and fantastic.” He expressed heartfelt gratitude to his team and colleagues, crediting their hard work and unity for the recognition.
This achievement highlights Christian’s ongoing commitment to creating a positive, supportive environment for both staff and the people they care for — ensuring high-quality, person-centred support remains at the heart of his service.

Christmas is a time for fun, festivities and revisiting traditions. Whilst staying healthy may not always be at the forefront of people’s minds during this time, one Christmas activity has several surprising health and wellbeing benefits – carolling.
Joanna Stanford, Lifestyle Manager at The Durhamgate care home (www.adorecarehomes.co.uk/carehomes/the-durhamgate), home to ‘the residents’ choir’, shares how this festive favourite can help support physical and mental wellbeing, whatever your age.
SINGING IMPROVES OXYGEN FLOW
Joanna, from the Durham care home says, “When we sing, we learn to control our breathing to allow us to hold the notes. Whilst this may not seem like an obvious workout, it can help promote steadier, deeper breathing and allow the body to take on oxygen more effectively. If you’re looking for a lower-impact activity that is still beneficial for supporting cardiovascular health, singing is a great way to encourage oxygen saturation levels in the blood, which in turn supports keeping the heart healthy. Some studies suggest that just 5 minutes of singing a day can have these effects – that’s as little as two Christmas carols!”
CAROLS CAN HELP YOUR IMMUNE SYSTEM
One of the most unexpected benefits of singing is that it can help support a healthy immune system.
Joanna explains, “Studies have shown that regularly singing in a group setting can help reduce inflammation in the body, and that singers experience higher levels of antibodies. Both of these are important for the immune system, with antibodies being the first defence against illness, and high inflammation working against the body’s natural ability to fight infection.
With the winter months being peak cold and flu season, it’s important to keep the immune system fighting fit and adding singing into your routine could play a supportive role in helping you feel well. Of

course, on top of this, it is still important to eat well, exercise and reduce the spread of bacteria to give your immune system the best chance of keeping you feeling your best. ”
MENTAL HEALTH CAN BE BOOSTED TOO
Singing doesn’t just bring physical benefits; it can have a positive effect on mental health as well.
Joanna says, “Singing helps to activate the areas in the brain associated with rewards and emotion, releasing endorphins and hormones like dopamine, leaving us feeling happy and with a lifted mood.
Many people find this effect is multiplied when singing in a group –the perfect excuse to get a choir together for some carolling!”
For Mike, one resident at DurhamGate, this is his favourite thing about singing: “I love to be in a group of others, all singing together
with everyone happy. I have fond memories of the time I spent with my family singing my favourite carol, ‘Oh Come All Ye Faithful’, at this time of year.”
MUSIC BENEFITS MEMORY
Another favourite at DurhamGate, which brings back precious memories for many, is ‘Silent Night’. Jean loves this song “as it was my late husband's favourite” and for Eileen, “it really takes me back to being young and being with my family.”
As well as evoking memories, singing can be used to build connections in the brain important for both short and long-term memory recall.
“When singing, we use many areas of the brain at the same time, something that few activities do. This can help strengthen pathways in our brains which support us with memory recall,” says Joanna. One way to enhance these effects is to make singing trickier, to keep the brain engaged with the task. Singing in a different language can be a fantastic way to do this, as more focus is needed on pronunciation.
Christmas carols are great for this, as many were originally written in other languages, but their melodies remain the same in English, providing an element of familiarity when learning the alternative lyrics. ‘Silent Night’, for example, was originally in German and known as ‘Stille Nacht.’”
Janna continues, “The best thing about singing for your health is that it is accessible, free of charge and can be fit into your day with ease –there’s no need to set aside time to work out or the need for any fancy equipment, you don’t even have to have perfect pitch!
The festive season is the perfect chance to give singing a try. Why not learn a few carols and see if it leaves you feeling fitter and happier in the new year?”
Boutique Care Homes has taken a novel approach to launching its newest home, inviting key community partners and stakeholders to spend the night at Keymer Hall before it opens to residents.
The pre-opening sleepover event on 4-5 December brought together the Mayor of Burgess Hill, the CEO of Burgess Hill Town Council, local GPs, social prescribers, and representatives from community organisations including Befriended, giving them an immersive experience of the home’s care environment, facilities and catering.
Martin Murphy, Operations Director of Boutique Care Homes, said the event was designed to build integrated care relationships from day one.
“We wanted the people of Burgess Hill to experience Keymer Hall exactly as our residents will, from the warmth of the welcome to the quality of the food and the comfort of every space,” he said. “The relationships we’re building with local healthcare professionals, community organisations, and the Town Council are fundamental to how we care. This wasn’t about a ribbon-cutting ceremony, it was about demonstrating our commitment to genuine partnership working.”

Attendees included Councillor Stuart Condie, Mayor of Burgess Hill Town Council, Julie Holden, CEO of Burgess Hill Town Council, Jennifer O’Grady, Head of Community Engagement, Dr Mandy Claiden of The Brow Health Centre, members of the local social prescribing team, and Gail Millar, CEO of Befriended.
The evening included tours of the purpose-built home’s residential and dementia care communities, a three-course meal prepared by the in-house chef team, and a quiz night – giving attendees a genuine sense of daily life at the home.
Dr Mandy Claiden of The Brow Health Centre said: “It has been such a pleasure to look around this new home, it’s wonderful, very comfortable. Really a home from home.”
Gail Millar, CEO of Befriended, said the event demonstrated the provider’s commitment to community integration: “You have the most exquisite and beautiful home, it does feel like you’re walking into a five star hotel with a very homely and welcoming feeling. But for me what I love is that as an organisation you have worked so hard to build connections with community. Delighted to be working with you and coming in regularly.”
Mid Sussex Radio presenter Mike Bonsor, who has personal experience of the care sector, said: “I haven’t been in this kind of facility for many years since my mum was going through a care home journey and I only wish this kind of place had been around when she was looking. The standard of the building, accommodation and the attention to detail that has been put into what the team are looking to provide is quite mind-blowing. Putting the needs and wants, the desires of the residents front and centre.”
Christine Bunce, Home Manager at Keymer Hall, said the team is now ready to welcome residents: “Seeing our guests settle in for the evening, enjoying our chef’s incredible food and having such a wonderful time together, that’s exactly what we want life at Keymer Hall to feel like every day. We’ve created something really special here, and watching people experience it for the first time has been genuinely moving. This is what care should be.”
Councillor Stuart Condie, Mayor of Burgess Hill Town Council, said: “I was delighted to attend the launch of the Keymer Hall care home, it is a well planned facility in a beautiful location which is going to be well loved as a home for many of our residents. The staff and the team behind Keymer Hall are not only professional but also caring.”
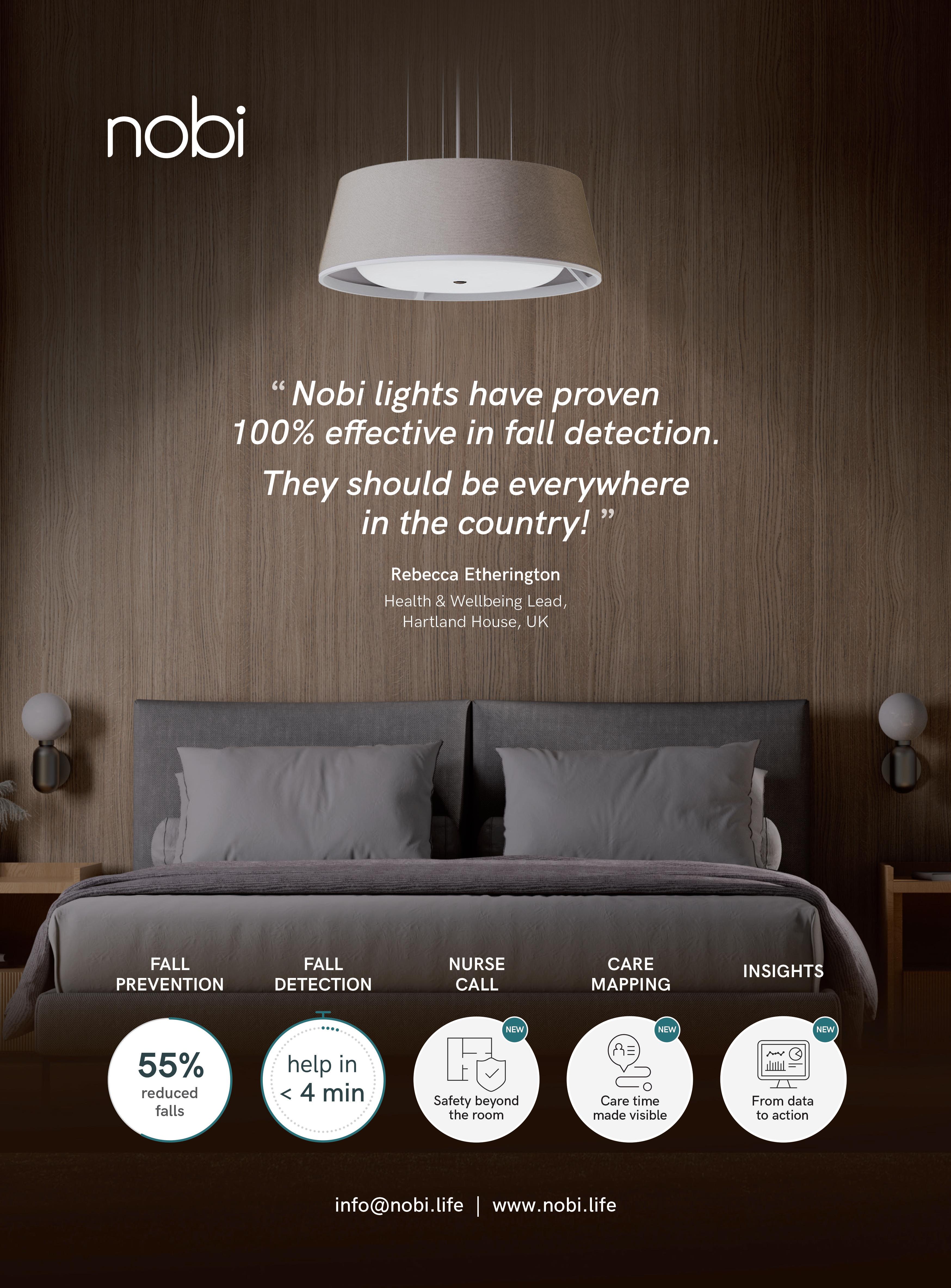
Nobi makes lives safer by preventing and detecting falls. Powered by cutting-edge AI technology, this intelligent light monitors the entire room discreetly and accurately — all while blending seamlessly into any interior with its award-winning, homelike design. Nobi supports older adults in living a dignified, carefree and happy life, with complete respect for their privacy.
A fall can dramatically change someone’s life. Rapid assistance after a fall — or, even better, preventing a fall altogether — is invaluable. It is crucial for older adults, but equally vital for caregivers who are committed to ensuring safety, comfort and independence. The moment a fall occurs, Nobi sends an immediate alert to care staff, creating the peace of mind that every incident will be seen and acted upon.
“Long lies” and their harmful consequences belong firmly in the past. With Nobi’s intelligent prevention and detection working in the background, caregivers can focus on warm, meaningful and person-centred care.

From its very beginning, Nobi has carried one clear vision: to make care environments places where safety feels natural, dignity feels effortless, and ageing is embraced rather than feared. The Nobi Light was the first proof of that vision. At first glance, it looks like a simple design light — yet within it, Nobi redefined fall
detection, fall prevention and smarter care. It showed that technology does not need to look technical. It can disappear into everyday life, becoming part of the environment while quietly transforming it.
Today, the Light remains at the heart of everything we do. Around it, Nobi is building the Nobi Care Flow: a connected layer where people, technology and routines work together effortlessly. This care flow gives residents a greater sense of safety, offers caregivers more time and peace of mind, and provides leadership with clarity to run safer, more efficient communities. All intelligence, integrations and software are included, making Nobi one of the most cost-efficient and impactful upgrades in elderly care.
Nobi is more than a smart light.
It is a dignified, intelligent care ecosystem — one that helps care flow again. By bringing safety, clarity and confidence into every room, Nobi supports the people at the heart of care: the residents who deserve to feel safe, and the caregivers who deserve tools that truly help them. info@nobi.life www.nobi.life



Oliver Kent-Braham, Co-Founder and CEO of Marshmallow (www.marshmallow.com) – a car insurance provider for newcomers to the UK – explores what is required to overcome the hidden financial challenges faced by the workforce that keeps the NHS and social care system running
As this audience well knows, the UK’s health and social care system is under immense strain. Chronic staff shortages, rising patient demand and stretched budgets have created a situation where services are under constant pressure.
The health and social services sector is the single largest employer of foreign-born workers in the UK. One in three care workers, and over a quarter of nurses in England, are born outside the UK. We all know that without them, the NHS and our care infrastructure would simply not function.
However, many of these workers still face barriers to financial inclusion that limit both their personal and professional potential. This is more than a workforce issue, it’s an economic one.
The UK is already grappling with over 100,000 vacancies across health and social care. As a result, there are more delayed treatments, a growing patient backlog and an increasing reliance on agency staff, costing the NHS billions of pounds every year. At the same time, our population is ageing rapidly, with demand for carers and nurses only set to increase in the coming decades.
Against this backdrop, migrants are playing a vital role, particularly in this sector. These workers underpin our frontline services. They make sure patients receive care, hospitals can function and care homes can continue to operate.
As newcomers to the UK, migrants make a huge contribution. But while we depend on them, the UK’s financial system largely ignores them. We regularly hear from our customers that they are not given access to essentials like fair insurance, loans, or credit. This blocks them from being able to set up their lives, whether it’s driving to work, buying a car, renting a house, applying for a mortgage, or getting a phone. Time and time again, we hear: “Here, I faced a lot of challenges. It wasn’t that I wasn’t prepared, I was prepared, but the system made it difficult.”
And this isn’t because they are high-risk customers, but because financial providers in the UK do not take into account their credit or employment history from abroad. In practical terms, for example, this means a driver with 10 years’ of experience in their home country is treated as if they are a brand-new driver in the UK.
UNLOCKING THE WORKFORCE’S FULL POTENTIAL
Supporting a modern day workforce means creating fit-for-purpose solutions that reflect differing circumstances. For example, insurers and lenders could recognise overseas financial histories and employment records, allowing migrant staff to access fair car insurance, home insurance and credit. Care employers could also provide guidance and support to navigate these systems, helping staff secure stability outside of work. Getting this right benefits the UK’s health and social care system as a whole. A more financially secure workforce is less likely to leave, reducing reliance on costly agency staff, cutting recruitment pressures and keeping patients’ care consistent. In turn, this strengthens the NHS and care infrastructure while supporting the wider economy.
However, the challenges in the path are complex and deep-rooted. Outdated financial systems continue to lock people out. If you arrive from overseas, you may have a decades-long financial history, but in the UK, it can often be of little value. This creates a domino effect: without credit, it’s harder to rent or secure housing; without insurance, it’s harder to get a car; without a car, it’s harder to get to work.
Failing to address these barriers comes at a real economic and social cost. NHS staff shortages already run into billions annually, and as care needs grow, barriers faced by migrant workers to access fair financial services make it harder to fill the gap. Without technology and processes that recognise their histories and support their integration to life in the UK, workers struggle to settle, plan ahead and remain in their roles.
The opportunity lies in setting this workforce up for success. That means tackling the hidden barriers to financial inclusion and ensuring migrant carers and nurses are fully integrated into systems that enable stability and growth.
Technology can play a key role in making this possible. Digital tools and data-driven solutions can assess financial risk more fairly. Recognising overseas employment and credit histories can provide accessible products such as car and home insurance, loans and credit-building support. Online platforms can streamline applications and reduce bureaucracy. They can also offer guidance tailored to the unique challenges migrant workers face, making it easier for them to settle, plan ahead and remain in their roles long term.
Giving access to fair financial services strengthens the workforce, reduces reliance on costly agency staff and ensures patients receive consistent, high-quality care. Supporting those who support us isn’t just the right thing to do; it’s the foundation of a sustainable healthcare system and a resilient UK economy. If we want a care and health system fit for the future, we need to start by giving the people at its heart the support they need to build secure lives here in the UK.
For more information or to secure a quote please visit www.marshmallow.com
See the advert on page 11.
Brendoncare has bade a sad farewell to Steph Freeman, who has retired after more than four decades working as a carer at three of its care homes in the Winchester area.
Steph began her career in 1982 at Brendoncare Park Road in Winchester, aged just 16, inspired by her mother, who worked as a cook at the care home. What started as a youthful decision soon became a lifelong vocation. She joined the team there even before The Brendoncare Foundation was established in 1984, meeting one of its founders, Sir Ronald Gibson, on several occasions.
After taking a year away for personal reasons, Steph returned to caring when Brendoncare’s Old Parsonage opened in Otterbourne in 1988. She even visited the residents and her colleagues there in her bridal dress on her wedding day.
Steph spent 30 years there, working both day and night shifts. She proudly recalls being on the very first shift when the home opened and the final shift before it closed in 2018, ahead of the move to Brendoncare Otterbourne Hill where she has worked as a bank night carer.

Steph then helped the residents adjust to the move from a smaller setting to a larger, modern care home. She recalls walking “20 miles on that first night” at Brendoncare Otterbourne Hill as staff famil-
iarised themselves with the new building.
Throughout her career, Steph has cared for residents from all walks of life – including war veterans, survivors of prisoner-of-war and concentration camps, and people with extraordinary life stories.
She has seen care evolve from handwritten notes to modern technology, and from physically lifting residents to safer, more advanced practices. Through it all, she has remained a constant source of comfort and dedication to the residents.
“I’ve loved it. I wouldn’t have stayed if I didn’t enjoy it so much,” Steph reflects. “Brendoncare has always been good to me. I’m proud of what I’ve done – especially supporting people and their families at the end of life.” Brendoncare’s Chief Executive Michael Crutchley presented Steph with an engraved vase, while colleagues at Brendoncare Otterbourne Hill organised a leaving party for her.
Michael Crutchley said of her: “Steph’s story is one of dedication and compassion. She has embodied the values of Brendoncare during her long career with us and we all thank her for her incredible contribution over those four decades.” Steph and husband Colin, who live in Fair Oak, are now embarking on a month-long camper van holiday around New Zealand.
Residents and colleagues at Coppice Court Care Home in Eastbourne, East Sussex, were delighted to welcome a special guest on Friday 28th November, as Josh Babarinde OBE, MP for Eastbourne, visited to meet residents and learn more about life at the home as part of UK Parliament Week.
During his time at the home, he enjoyed conversations with residents and colleagues, hearing about their experiences and learning more about the high-quality care and engaging activities provided at the 52-bed home, which offers both nursing and nursing dementia care. In addition, Mr Babarinde was accompanied by his partner, Connor Cummings on the visit and the home celebrated their recent engagement by surprising them with a congratulations cake.

As part of the day’s activities, the wellbeing coordinators, Gabby Kent and Tia Downer, hosted a warm and friendly coffee morning for residents. The gathering offered a lovely opportunity for chats about the hobbies
residents enjoy most and what they love about living in Eastbourne, creating a relaxed space for everyone to connect and share their stories. UK Parliament Week, which runs each year to engage people from across the UK with the work of Parliament, encourages communities to learn about how democracy works and how they can get involved in shaping the future. Coppice Court’s celebration of the week provided residents with a unique opportunity to connect with their local MP and discuss topics that matter to them.
Elga Ekonomi, Home Manager at Coppice Court Care Home, commented: “Having Josh visit us as part of UK Parliament Week was a real highlight for our residents and team. They thoroughly enjoyed welcoming him into our home and sharing their stories. It’s so important for older people to feel connected to their community and to national events like this, which remind us that every voice matters.”
Dementia has retained its position as the UK’s biggest killer for another year, claiming 76,894 lives in 2024 according to new analysis from Alzheimer’s Research UK. The figure represents more than one in ten (11.8%) of all deaths across the country, surpassing fatalities from heart disease and stroke.
The findings, compiled using the latest data from the Office for National Statistics, the National Records of Scotland and the Northern Ireland Statistics and Research Agency, reveal a continuing upward trend. Deaths from dementia have risen from 74,261 in 2022 and 75,393 in 2023, even as mortality rates from other major conditions have declined.

• Pneumonia develops when swallowing difficulties allow food or drink to enter the windpipe, irritating the lungs and triggering infections.
• Starvation and dehydration occur as residents lose their appetite, forget to eat, or lose the ability to swallow, increasing vulnerability to infections through poor nutrition.
• Severe urinary tract infections can escalate to sepsis when incontinence and hygiene challenges go unmanaged.
• Untreated underlying conditions such as diabetes or hypertension may worsen when residents forget check-ups and medication.
• Weakened immune systems become less effective with age, with dementia-causing diseases exacerbating this decline.

The increasing dementia death toll is partly attributed to the UK’s ageing population, with age remaining the single biggest risk factor for the condition. However, a critical factor distinguishes dementia from other major health challenges: unlike heart disease or stroke, no treatments are currently available on the NHS that can slow, stop or prevent dementia’s progression.
Two new treatments for early Alzheimer’s disease received UK licensing last year but were not approved for NHS use, leaving a significant gap in the therapeutic landscape for care providers and families managing the condition.
The analysis highlights stark gender differences in dementia mortality. Women continue to be disproportionately affected, with 48,915 female deaths compared to 27,979 male deaths in 2024. Dementia has been the leading cause of death for UK women since 2011, whilst heart disease remains the primary killer for men, claiming over 41,000 male lives last year.
Regional variations also emerged in the data. England recorded the highest dementia death rate at 12%, followed by Northern Ireland (11.1%), Wales (11%) and Scotland (10.6%). These figures represent a shift from 2023’s pattern, though experts emphasise that consistent nationwide action remains essential regardless of regional rankings.
Research from Alzheimer’s Research UK’s Dementia Attitudes Monitor reveals a concerning knowledge gap: whilst dementia is the most feared health condition among the public, only six in ten people understand that it is fatal.
Dementia is not an inevitable consequence of ageing but rather results from diseases affecting brain areas that control vital bodily functions. As the condition progresses, it causes the body’s systems to fail, ultimately leading to death through various mechanisms.
CARE PROFESSIONALS SHOULD BE AWARE OF THE PRIMARY CAUSES OF DEATH IN PEOPLE WITH DEMENTIA:
• Falls and injuries pose heightened risks, with advanced age slowing recovery and increasing mortality following necessary surgical interventions.
Dementia is estimated to cost the UK economy £42 billion annually through its impact on the NHS, social care services and unpaid care provision. Families bear the heaviest burden, covering 63% of total costs.
With the UK population continuing to age, the number of people living with dementia is projected to exceed 1.4 million by 2040. Without improvements in prevention, diagnosis and treatment, the death toll is expected to climb steadily.
Alzheimer’s Research UK is urging the Government to take immediate action on multiple fronts. The organisation emphasises the need for increased investment in scientific research into new treatments, improved diagnostic pathways and broader prevention measures.
Hilary Evans-Newton, Chief Executive of Alzheimer’s Research UK, stated that whilst more potential treatments and simpler early diagnostic tests now exist than ever before, these breakthroughs require government support to reach patients. She called for proper backing of research and clinical trials, alongside a comprehensive plan to prepare the NHS for delivering new tests and treatments.
Early and accurate diagnosis remains crucial for connecting people with appropriate support and will be essential for accessing emerging treatments. However, Alzheimer’s Research UK’s recent Dementia Unseen campaign revealed that one in three people with dementia currently miss out on a diagnosis.
The organisation is calling for clear national diagnostic standards and sustained investment in NHS dementia services to address this gap—a development that would have significant implications for care homes in planning resident support and accessing future therapeutic interventions.

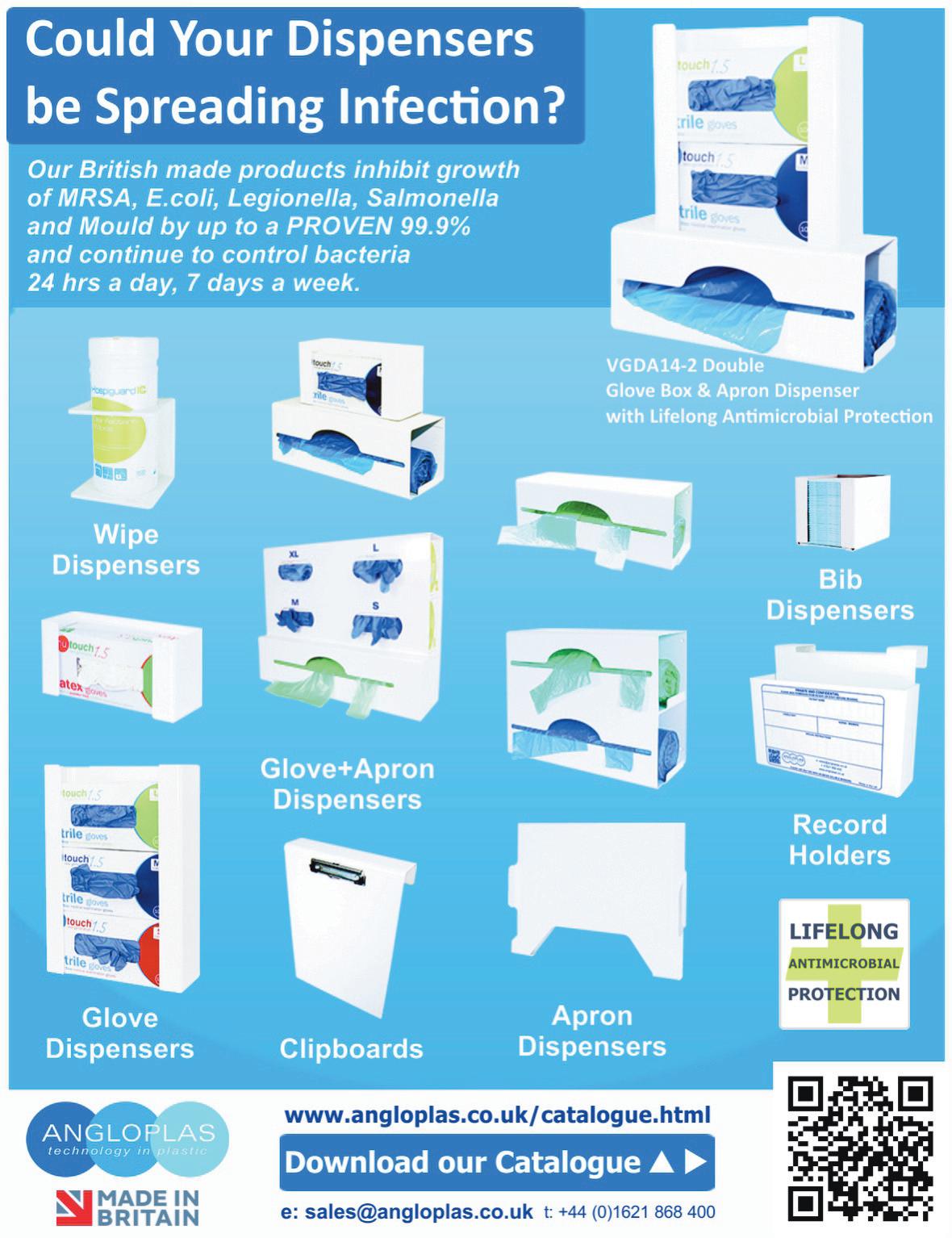

At Heanton Nursing Home in Braunton, music isn’t just background noise, it’s a source of comfort and connection.
For people living with a Dementia, the right song can create a sense of calm, familiarity and belonging, moments that lift the atmosphere and bring people together. Robin Mitchell, who leads regular singalongs at Heanton, has seen first-hand how powerful music can be, and how important it is to get it right.
The music filling the lounge might surprise people. Rather than relying on traditional wartime tunes, the playlists are shaped around the eras that today’s older adults grew up with - the 1960s and 70s. Research into dementia and the brain has shown that the music people listen to in their teens and twenties tends to stay with them throughout life. According to Dementia UK, those years form strong emotional connections in the brain, meaning familiar songs from that period can create a sense of comfort and recognition, even decades later.
By Abigail Denford, home manager of Heanton Nursing Home

For Heanton’s residents (who the home fondly refers to as family members), that means the sound of Sweet Caroline (released in 1969), ABBA, or Tom Jones is often what gets toes tapping and faces lighting up. Music from that era isn’t just nostalgic, it’s part of peoples lived experience, connected to the times they
were working, raising families or even dancing at the weekend.
“When the right song comes on, you can see the change,” says Robin. “Someone who’s quiet might start tapping their feet, moving with the rhythm or joining in with a few words. It’s like the music gives everyone a lift.”
Studies by the NHS, Dementia UK and Alzheimer’s Society have long supported this approach, showing that familiar, preferred music can help reduce anxiety, encourage communication and social interaction, and promote a sense of wellbeing. It can also offer peace and comfort at more reflective moments.
Robin adds, “Even a song that brings a tear can be a positive thing, it helps people express how they feel. Everyone connects to music in their own way, and that’s what makes it special.”
Music plays an important role at Heanton. As a complex care home, someone’s feelings is an important part of truly understanding each person they support. Noticing the small things, tuning into emotions, and anticipating needs long before they’re expressed. Robin’s singalongs are a perfect example of this approach, using music to reach family members on an emotional level, helping them create moments of connection and enjoyment that feel familiar, personal and real.
the
on as part
the
project she is undertaking to explore the impact of volunteering on communities during her year in office.
She joined Pets as Therapy volunteer Jenny Welham and Ruby, her eight-year-old Cairn Terrier–Toy Poodle cross, on their regular round of the home. Together, they visited more than 30 people living at Lace Hill Manor, including several who are currently bed bound, providing comfort, companionship and plenty of smiles along the way.
Jenny and Ruby have been volunteering for years and have been visiting Lace Hill Manor since it opened two and a half years ago.
Jenny said: “Ruby would work all day if she could. She absolutely loves it. She always seems to find the people who need her most.”

Before becoming a volunteer, Jenny served as a police officer for 20 years and later worked as a teacher before mental ill health meant leaving the career she loved. Volunteering, she says, has been transfor-
mative.
“Pets as Therapy has had such a positive impact on my life after losing the career that meant so much. For 45 years, I have lived and worked in the same town so I know many of the residents and their families. It’s nice to have that connection and, although I can’t do paid employment anymore, to still use my skills. It’s given me purpose and focus.”
Pippa thanked all the staff at Lace Hill Manor Care Home for “making me so welcome and for giving me such a special time.”
She added: “Pets as Therapy are a community of pet owners and amazing pets, brightening days and bringing joy to people in care homes, schools and more. The pictures of Ruby with several of the residents illustrate the comfort and smiles that she and Jenny bring on their fortnightly visits.”
Shilpa Nair, manager at Lace Hill Manor, which provides residential and dementia care, said: “Jenny and Ruby’s visits are always a highlight here at Lace Hill Manor. From the moment Ruby bounds into the room she brings a smile, and connects with people in such a special way.
“We are incredibly grateful to Jenny for her dedication and to the High Sheriff for taking such a genuine interest in the power of volunteering. Her visit meant a great deal to everyone here.”
A new academic report from the University of Oradea has placed a spotlight on the urgent need for the adoption of better prevention, training, and safer treatment technologies to reduce harm from the growing volume of healthcare waste produced worldwide, says leading independent healthcare waste management company, Anenta. Shedding light on hazardous medical waste and its rising risks to clinical staff, healthcare workers, and those who handle medical waste, Anenta believes that the ‘Healthcare Waste Toxicity: From Human Exposure to Toxic Mechanisms and Management Strategies’ report is a sharp reminder that producers of healthcare waste need to be vigilant and diligent.
In Anenta’s view, this is particularly important in relation to the disposal of sharps, infectious, pharmaceutical, pathological, cytotoxic, and chemical waste, and applies to GPs, hospitals, laboratories, pharmacies, research centres, dental clinics, care and nursing homes.
“The findings of this study reiterate just how important segregation, governance, and training are in preventing harm to staff and the wider community,” said Kim Ormsby, Assistant Director at Anenta, adding: “It’s vital that every measure, including handling, transportation, treatment, storage, and disposal is properly understood, implemented, and audited, which is exactly why we’ve created a free e-learning module on healthcare waste to help businesses in the primary care sector.”
Covering a number of topics such as waste segregation, simplification of waste processes, waste reduction, and colour-coded containment, the 45-minute training module is accessible free of charge to care homes, and healthcare professional via the Health Education England online portal. These courses help those in the primary care sector meet duty of care obligations and ensure consistent adherence to environmental and CQC standards.

This, in turn, helps smooth the pre-acceptance and duty of care audit process, which is essential for compliance under the Environmental Protection Act 1990, and helps avoid the risk of waste contractors refusing to make collections due to instances of ‘non-compliance.’
Aided further by Anenta’s remote hazardous waste audits, which give care homes, nursing homes and producers of healthcare waste the ability to conduct compulsory duty of care and pre-acceptance audits in as little as 40 minutes, Anenta has removed the need for tedious third-party on-site audits, which can take up to 6 days. In addition to saving time, Anenta’s online solution also reduces costs by up to £800. Combined, this process helps to ensure compliance for care homes whose staff are exposed to a range of different types of waste, includ-
ing sharps, clinical, infectious, and offensive waste.
“Protecting workers and the wider community from the dangers of medical waste is critically important,” says Ormsby. “Without consistent training and clear policies, staff can all too easily be put at unnecessary risk, which is why we work closely with care and nursing homes to ensure that their waste management processes are streamlined and effective, ensuring a safer healthcare environment for all.”
Anenta, which was awarded the Healthcare Waste Management Company of the Year title at the prestigious Healthcare Business Review Europe Awards 2025, acts as an external contract manager delivering bespoke, affordable, and professional services across recycling, general waste, saniwaste, confidential, and clinical waste streams. Managing over 450,000 collections annually from more than 20,000 locations, Anenta has saved its clients over £13 million directly, while introducing workplace efficiencies that have generated a further £35 million in savings.
Much of these savings are possible thanks to Vector, Anenta’s proprietary, multi-stakeholder system, which equips all parties in the healthcare waste supply chain with real-time updates on documentation, billing, compliance and outcomes. Highlighting inefficiencies and providing data-driven insights to improve service, delivery and operational performance, Vector ensures the delivery of fair billing practices through the analysis of thousands of invoices to identify and address any instances of overcharging.
Free training module:
https://portal.e-lfh.org.uk/Component/Details/763177
Website www.anentawaste.com
Contact page https://www.anentawaste.com/contact-us/ Call 03301222143


As sustainability rises up the agenda for care organisations, heat is a natural target for efficiency improvement. Andy Green, Head of Technical Solutions at Baxi, discusses the importance of planning a net zero pathway and some of the achievable options for care home operators
The UK’s circa 17,000 care homes may vary in size and age, but reliable heating and hot water is essential in each to prioritise the wellbeing and comfort of their residents. As this service is typically the largest user of energy in care home facilities, it’s also a good starting point for reducing operating costs and associated carbon emissions.
Let’s consider some of the achievable measures to improve the efficiency of the heating system and reduce its carbon impact
In our recent survey of over 400 care homes managers, budget pressures, eligibility for funding and technical understanding of achievable options were the top challenges listed when considering decarbonising heat in their buildings. Subsequent focus group sessions also revealed that unplanned replacements are common, frequently resulting in a like-for-like distress purchase rather than enabling the care home operator to plan and implement a phased approach to net zero. But with care homes coming under increased pressure to adopt sustainable practices in line with the nation’s wider 2050 net zero target, putting a roadmap in place is absolutely key. Fortunately, care home managers have access to heat experts like Baxi for support. We work closely with care homes first to understand the viable options for improved system efficiency and then to help them plot their unique net zero pathway.
The first step should always be to understand how and where energy is being used in the building. Identifying and limiting any heat loss to the environment will not only immediately improve operating costs but can significantly reduce the size or capacity of plant required when refurbishing the system – which in turn will lower the required capital expenditure.
Practical examples might include building fabric upgrades such as roof and wall insulation, draught proofing and/or improving the thermal performance of windows and doors. Adding lagging to poorly insulated pipework will also prevent heat losses within the system for improved performance. Where necessary, adjust the heating controls and thermostat settings to optimise the temperature regimes and balance energy efficiency with thermal comfort.
‘HEAT
Light refurbishment still accounts for much of the work in the care home sectors according to our focus group research, despite the willingness shown for embarking on heat decarbonisation projects.

If upgrading to more efficient gas condensing boilers or direct-fired water heaters, use this opportunity to prepare the heating system for the integration of low temperature heat pumps at a future stage. Addressing the system’s distribution pipework and heat emitters will allow the system to operate more efficiently at a maximum flow temperature of 55°C (or lower), in line with Building Regulations. This will also allow the condensing boilers and water heaters to operate in condensing mode, where they achieve their maximum efficiencies.
Replacing existing gas boilers or water heaters with heat pumps is the ultimate goal. New build care homes will be designed to require less heat for operational use and optimised for a decarbonised electricity grid. In buildings like these, a fully electric approach to heating and domestic hot water (DHW) based around renewable solutions such as our Auriga mid temperature and Auriga HP + high temperature heat pumps will be the favoured approach, particularly when combined with solar thermal and/or solar PV solutions. In care homes with complex refurbishment challenges, a phased pathway may be necessary. In such buildings, a hybrid heat pump system combining heat pumps with existing boilers and/or water heaters is often a fast, affordable solution to partial decarbonisation. This will enable a large portion of the heat in the building to be decarbonised while meeting safe operation requirements.
Each care home project and building will have its own requirements, so it is advisable to consult with the experts. Experienced heating and hot water solutions providers like Baxi can help break down the complexities for care homes by clearly explaining the options and outlining the associated carbon, energy and cost impacts of each. Working together, we can help ensure that the right decision is made to meet the specific needs of your building to set it on its path to net zero.
For more information, visit: Baxi Commercial Heating and Hot Water Solutionswww.baxi.co.uk/commercial
PROUD memories of national service and wartime efforts were shared when a Rotherham care home held a party to celebrate achieving “Veteran Friendly” status.
Whiston Hall Care Home, on The Manorial Barn Chaff Close, marked the occasion with a gathering of residents, staff, family members, and friends of the home – alongside local dignitaries.
The care home’s veterans were also in attendance, including Alan Taylor, 88, who served in the British Army’s Royal Signals Corps during his national service from 1956 to 1958, posted to Germany, Egypt, and then York.
Fellow resident James Broughton, 92, joined the Royal Engineers Corps when he was 18 and served two years in Hong Kong. Henry Graham, 94, served in the Army Medical Corps from 1951-53, training to the level of nurse.

Mary Barton, 85, served two years in the Auxiliary Corps at the Catterick Garrison, in North Yorkshire, where many of the residents completed their training. She was charged with driving officers around the base, during which time she met her husband, and the couple were stationed in Germany for 10 years. Effie Copley, 99, worked in the Sheffield steelworks for two years during the Second World War, for which she was honoured as one of the “Women of Steel” with a monument in Sheffield city centre in 2016.
The spouses of veterans also shared their stories, including Lorna Gibbs, 86, whose husband served as a trainer of new recruits in the Grenadier Guards. And Janet Pearn, 79, who was a sergeant in the Army for eight years.
The party to honour the veterans and celebrate Whiston Hall’s Veteran Friendly Framework (VFF) sta-
tus included live music from Keeley May Vocals, dancing, prosecco and bucks fizz, and a cake made by the care home’s chef, Deepak Pattar.
The Lord Mayor of Rotherham, Cllr Rukhsana Ismail, was among the dignitaries at the event – taking to the dance floor with fellow partygoers.
She said: “Whiston Hall’s accreditation for being Veteran Friendly is obviously something they take very seriously and are proud of. They are committed to understanding the veterans’ needs, providing tailored support and promoting respect and recognition for all their residents.
“Thank you to the incredible staff and management at Whiston Hall for creating such a joyous atmosphere – I just wish I’d worn my dancing shoes as I took a turn on the dance floor.”
Jake Richards, MP for Rother Valley, and Paul Thorp, Cllr for Sitwell Ward, also celebrated with residents and staff at the event.
Mr Richards said: “It was lovely to join the staff and residents at Whiston Hall Care Home as they celebrated becoming a veteran friendly location. The wonderful entertainment team put on a real show for the residents to celebrate this achievement.”
Marie Keaveney, activities coordinator at Whiston Hall Care Home, said: “It was an honour for us to be able to throw this party and pay our respects to our veterans. We have so many residents who themselves served or had spouses that did.
“It was a massive part of there lives and we are privileged to be able to know all of these fantastic people. The staff team has always got involved and it like one big family here at Whiston Hall.”
Residents, staff, friends, and family at Wisden Court, part of the Runwood Homes group, came together on the 12th of November to celebrate a special milestone, Lillian’s 103rd birthday. The day was filled with joy, music, and heartwarming moments as everyone gathered to honour Lillian’s remarkable life and spirit.
The celebrations included a lively party with entertainment from vocalist Becky, who delighted the crowd with her performance. The event brought together residents, staff, and Lillian’s family and friends for a memorable afternoon of singing, laughter, and shared memories.
The Wisden Court team loved to see everyone come together to celebrate an incredible occasion. Lillian was smiling throughout the day, surrounded by love and happiness.
Lillian herself shared that she had a fabulous birthday with friends and family, expressing her gratitude for all the thoughtful gestures and the wonderful atmosphere created in her honour.
This celebration not only marked Lillian’s 103 years but also highlighted the sense of community and togetherness that makes life at Wisden Court so special.

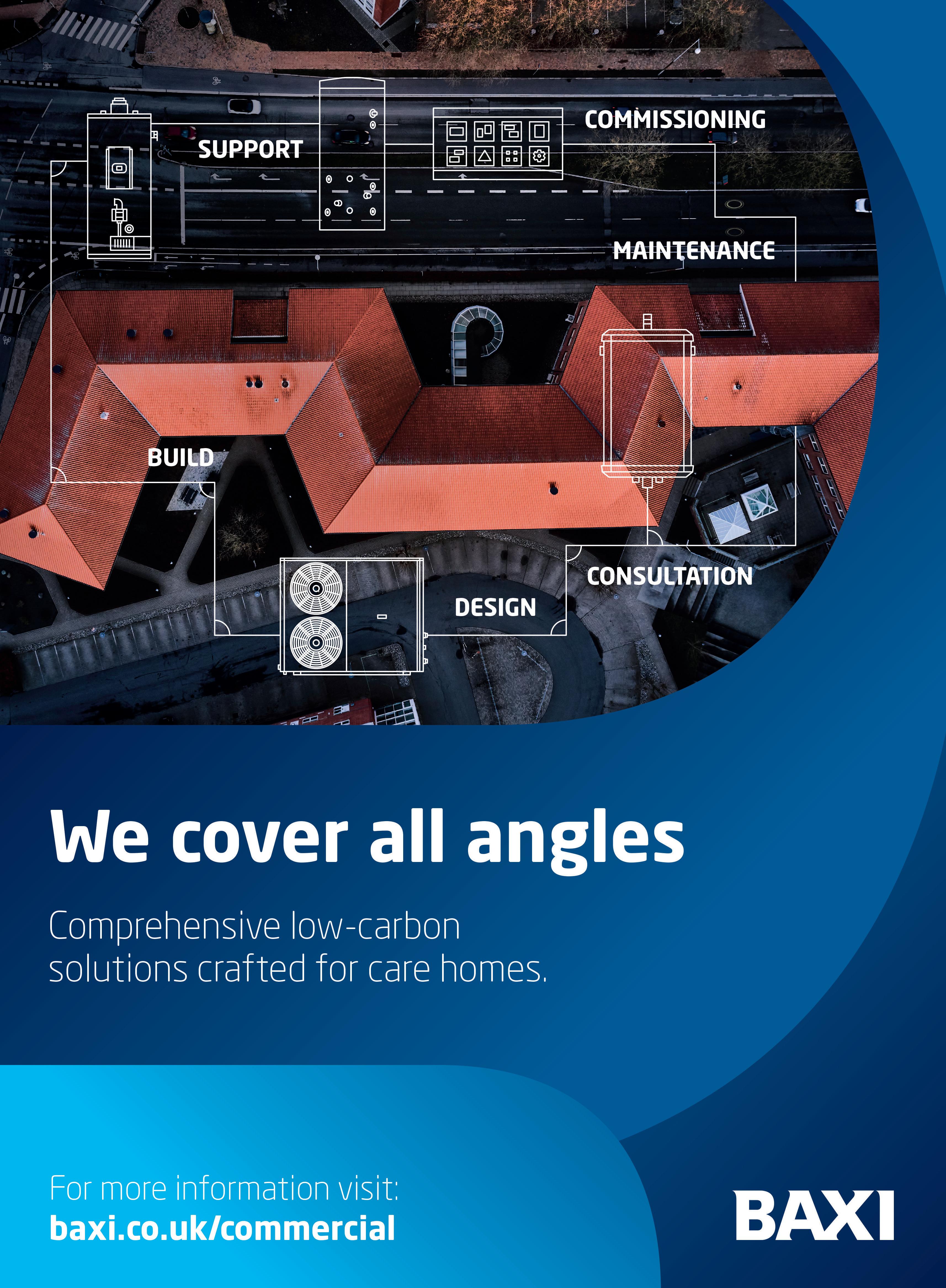
The UK healthcare sector seems to have entered a period of active growth following a multi-year post-pandemic recovery, according to leading global property adviser Knight Frank, with a record year for healthcare property transactions in 2025 reflecting investors’ confidence in the outlook for the market. Knight Frank’s 14th annual Healthcare Trading Performance Survey, whose respondents account for over 100,000 care beds across 781 UK towns and cities, reveals that UK healthcare operators have delivered growth in EBITDARM margins to an average 30.1% in 2025, up 4 percentage points from the prior year. 18% of care homes achieved EBITDARM margins in excess of 40%, up from 13% in 2024, and the proportion of homes categorised as loss-making fell year-on-year from 5% to 3%.
This robust improvement in profitability was driven in large part by a sector-wide uptick in weekly fee income. Average fees across UK care homes grew by 9.8% to £1,298 per week in the past year, with weekly fees for personal care experiencing the most profound growth at 12%. Occupancy, too, has experienced a notably bounceback from the pandemic period, with nationwide care home occupancy reaching 88.7% in 2025 versus 88.3% in 2024.
INVESTORS CAPITALISING ON GROWTH:

healthcare property deals had transacted this year, £6 billion of which were completed by Knight Frank, with Primary Health Properties’ £1.8 billion bid for Assura PLC marking the standout deal due to close in the final quarter of the year.
HEADWINDS REMAIN:
While profitability gains have been noted across the UK healthcare sector in 2025, the prospects for future growth remain challenged by rising cost pressures, exacerbated by the latest Budget announcement. Staffing costs per resident have increased 7% year-on-year to £37,877 as wages rise faster than RPI inflation, while property costs per bed have increased to an average of £4,427, up 18% on 2024.
The year-on-year improvement in key UK care home performance metrics reflects the sector’s entry into a stage of active growth, following a multi-year period of recovery from the impacts of the pandemic. This has been reflected in record transactional activity in the UK healthcare property market this year, with global investors increasing their exposure to UK care homes to capitalise on the sector’s strong performance, as well as the defensive characteristics it demonstrated throughout recent years.
Knight Frank recently forecast that c. £12 billion of UK healthcare property transactions are forecast to complete in 2025, more than treble the long-term yearly average. As at the end of Q3, £8.6 billion of UK
Ryan Richards, Associate at Knight Frank, commented: “Having remained resilient to macroeconomic turbulence in the period immediately following the pandemic, key performance metrics for the UK healthcare sector indicate that the market is now transitioning into a period of growth. As well as validating the conviction shown by investors who backed the sector during less certain market conditions, this is likely to prompt further global capital to funnel into the market. While the outlook across UK real estate is not universally positive, we have noted increased interest in historically ‘alternative’ sectors including healthcare from an ever-wider pool of investors. Beyond specialist capital sources, overseas institutional investors and family offices, for instance, are also seeking to increase their exposure.
“Stock selection will be critical moving forward. As macroeconomic and regulatory uncertainty persist into 2026, cost pressures will continue to be front-of-mind for operators and investors. While fee increases have enabled operators to absorb a proportion of recent cost rises, questions remain over the sector’s capacity to further increase fees at a rate which offsets the impact of cost inflation on balance sheets. Established operators with modern, high-quality stock will be best positioned to outperform in the years ahead, and will likely be a key target for investors seeking to increase their allocations to the asset class in 2026 and beyond.”
When care home resident Brenda, 93, was invited to her granddaughter Pippa's wedding, Gurprit Gill, owner of Walfinch home care in Sutton Coldfield, was determined to help.
Gurprit says: “We provided home care for Brenda before she went into a care home, and when the wedding came round, her family asked us to take her. I did the preparations and asked our carer Favour to take Brenda along.”
Favour, who dressed for the wedding, says: “I helped Brenda into her wedding outfit and took her to the ceremony, at All Saints Church, Four Oaks, and then on to the reception in the church hall afterwards. We even had a little dance together!
“She loved it, and although she has quite severe dementia, she recognised lots of family members, particularly Pippa, and knew it was her wedding day. It was a delight to see, because Brenda had not always recognised family in the recent past.”
Helping families celebrate together

The wedding also fulfilled a personal ambition for Gurprit. “This was one of the reasons I started my Walfinch home care business. I have always wanted to help grandparents get to family events, as sometimes my own grandma could not attend our family celebrations because she received care. She remained at home, and my uncle stayed to care for her.
“It was heartbreaking that they could not be there, so now I want to make it possible for people to
enjoy their lives, including family events.”
Community commitment
Gurprit and her team's caring attitude extends into their local community. “We run four Walfinch Thrive Club sessions a month in co-operation with St James' Church, Mere Green, which are free to everyone. One is called Sip and Paint, where people can paint pottery while enjoying refreshments, and another offers art and crafts, where people can learn oil and watercolour painting. We also have two dementia-friendly art and crafts sessions monthly.
“The art and craft sessions are all led by artist Cathy Cocks, and as well as painting, include making paper roses, drawing fireworks, and colouring – things which stimulate the brain. The sessions also combat loneliness and isolation. We provide transport, because many elderly people cannot afford to get to them,” says Gurprit.
The sessions also enable local people to find out more about care services, from Walfinch team members. “We have gained new care clients, and helped people understand what care services we provide, including helping people get to family events,” says Gurprit.
Gurprit's team are also organising a forthcoming care and wellness day at St James' Centre, to include a breathwork class, arts and crafts and pampering sessions.


Nursing staff are warning that patients face a “devastating” winter as new analysis reveals a rise in 12-hour waits for hospital admission – a 90-fold increase in just six years. We believe ministers have acted with “insufficient urgency” since last winter, failing to invest in hospital and community capacity or boost staffing levels.
Between July and September this year, 116,141 patients waited more than 12 hours in A&E after a decision to admit, compared to just 1,281 in 2019 – an increase of almost 9,000%. Over the same period, overnight bed capacity has grown by only 2%, adding just 2,192 beds. That means 52 patients who are sick enough to be admitted competing for each additional bed.
The situation is compounded by limited capacity in community and social care, leaving thousands stuck in hospital despite being ready for discharge. NHS discharge data from October 2025 showed an average of 13,117 patients stayed in hospital each day despite being ready for discharge – up 6% on last year.
This analysis is included in a briefing paper titled Bracing for winter: a close look at NHS emergency and elective care in England and its implications for corridor care.

In the Westminster government’s Urgent and Emergency Care Plan For 2025/26, NHS leaders and the government committed to publishing data on incidences of corridor care, however almost six months later this has failed to materialise.
Ministers must deliver on this commitment and fund more beds, improve nurse staffing levels, and accelerate investment in community services.
Pressures on services mean more patients are also leaving A&E without treatment, jumping from 100,000 in 2019 to more than 320,000 in 2025. This reflects growing frustration with under-staffed, under-resourced services struggling to meet demand.
“Nursing staff and patients alike endured a horrendous winter last year, with corridor care rife across
every service. Worryingly, after no respite in the summer, the signs point to the coming colder months being devastating and more dangerous for patients,” said Professor Nicola Ranger, RCN General Secretary and Chief Executive. She added: “Nursing staff have repeatedly warned about a corridor care national emergency, but the lack of urgency in tackling the crisis is unacceptable. Bed capacity has remained static, nurse numbers in hospitals haven’t increased to the level required and community services are not being invested in anywhere near fast enough. Yet again this winter, nursing staff have been set up to fail and patients set up to suffer.”
In the absence of published data on corridor care, waits of 12 hours or more are the clearest indicator of corridor care taking place in hospitals, with staff unable to move people to a ward despite them being unwell enough to be admitted. Corridor care means patients are treated on trolleys, chairs, and even in cupboards or offices, often without access to lifesaving equipment like oxygen and suction. Nursing staff report patients enduring intimate examinations in public areas, while temporary escalation spaces are counted as safe, clinical “beds” in official figures – masking the true scale of the crisis.
In January this year, thousands of nursing staff shared devastating testimony of patients enduring corridor care, with some dying and being undiscovered for hours. In May 2024, we declared a “national emergency” over the issue of corridor care.
“To consign corridor care to history where it belongs, we need ministers to boost capacity at the front door, delivering new funding to improve staffing levels and the number of beds in hospitals. At the back door, we need to see a much more rapid timeline of investment to grow staff and provision in primary, community care and social care. Ministers must also stop delaying publishing the data on just how widespread corridor care is. Patients deserve transparency over care standards,” Nicola said.
The team and residents of Sanctuary Care’s home in Chesterton are beaming with pride after achieving Veteran Friendly Framework (VFF) status!
Broadmeadow Court Residential Care Home has been awarded prestigious VFF status, in recognition of the team’s dedication to supporting the practical, emotional and social needs of the armed forces community.
As part of their commitment, the dedicated staff, who currently care for two veterans, established close links with local armed forces community groups, creating important bonds and connections.
One of their residents for whom this means so much is 88-year-old Jim Holding, who served with the Royal Horse Guard with the Household Cavalry at Knightsbridge Barracks in London. Jim said: “One of my proudest photographs is of me as standing with my horse and The Queen on parade.
“We went through months of training for these parades, mainly in the dark so people could not see. The training was tough, but they soon whipped us boys into shape – it taught you such discipline and the regiment is your family for life.”

Speaking about the home’s VFF status, Jim, who moved into the not-for-profit Sanctuary Care home in Broadmeadow Court two years ago, said: “I’m glad we’ve got this, as it may bring other veterans into the home.”
As part of their dedication to providing truly person-centred support to all of their veterans, the team ensures that any external healthcare professionals are fully aware of their service status, discreetly placing poppies outside their bedroom doors to remind visitors.
The home also has dedicated champions, who have undertaken specialist training, which they then use to train their colleagues on how to provide the very best support to their veterans and their loved ones.
Christine Singer, manager of the Sanctuary Care home and proudly part of a military family, herself shared: “Achieving Veteran Friendly Framework accreditation is a milestone we hold with immense pride.
“This recognition reflects our unwavering commitment to honouring and supporting those who have served. It strengthens our ability to enrich the lives of our residents and ensures that the veterans in our care receive the personalised support and understanding they truly deserve.”
The VFF is a collaboration between Armed Forces charities Royal Star & Garter, Royal British Legion and NHS Veterans’ Covenant Healthcare Alliance (VCHA).
Kathryn Glass is the VFF Project Lead at Royal Star & Garter and responsible for supporting and assessing care homes going through the scheme. She said: “We’re delighted that Sanctuary Care’s Broadmeadow Court Residential Care Home has achieved VFF status. This is a great commitment to their continuous improvement in the delivery of person-centred care for veteran residents and their partners.”

In today’s highly regulated health and social care environment, providers face the dual challenge of ensuring compliance while striving to deliver safe, high-quality, and commercially sustainable services. Care Inspections UK Limited (CiUK) has emerged as a trusted partner in this landscape, providing a professional and independent inspection service that goes beyond the standard requirements of the Care Quality Commission (CQC), The Care Inspectorate Wales (CIW) and the Care Inspectorate (Scotland), collectively “The Inspectorates” What sets CiUK apart is its status as a registered inspection body, operating with the highest levels of professionalism and governance. This official recognition imbues care providers with confidence that inspections are carried out with rigour, objectivity, and an unwavering focus on evidence. Every report is underpinned by validated, research-based methodology, ensuring the outcomes are credible, balanced, and practical.
BEYOND CQC/ CIW/ CI
While CQC/ CIW/ CI inspections focus on fundamental areas such as safety, effectiveness, responsiveness, and leadership, CiUK’s approach extends further. Each CiUK inspection covers all the domains CQC/ CIW/ CI would expect, but also incorporates additional layers of analysis essential for continuous improvement. This Includes:
• Operational risk management involves identifying risks before they become incidents, reducing exposure for service users and providers.
• Quality enhancement: Assessing opportunities to raise standards in care delivery, staff engagement, and governance.
• Commercial sustainability: Offering insight into how operational practices influence financial performance, helping providers balance compliance with business viability.
The result is an inspection report that is not only regulatory-ready but also a strategic tool for improvement.
Professionalism is at the heart of CiUK’s ethos. Inspections are conducted by highly experienced professionals who bring frontline expertise from clinical, managerial, and governance roles in the care sector. This depth of knowledge allows CiUK to deliver meaningful feedback that resonates with staff at every level, from frontline carers to boardroom directors.
Independence is equally vital. As an external registered inspection body, CiUK reassures providers that its findings are unbiased and transparent. In a sector where credibility matters, this impartiality is invaluable in preparing for CQC inspections and demonstrating accountability to commissioners, investors, and the wider community.
Care providers today operate in an environment of heightened scrutiny and rising expectations. CIUK’s inspections do more than highlight compliance gaps; they provide a clear roadmap for reducing risk, enhancing quality, and driving organisational improvement.
By identifying weaknesses early, providers can take corrective action before issues escalate. At the same time, CiUK’s focus on strengths and opportunities supports a culture of positive development. This balanced approach ensures that inspection outcomes are constructive, not punitive, fostering continuous organisational improvement.
One of the most overlooked aspects of care provision is its commercial dimension. Poor compliance and weak governance inevitably carry financial consequences, from reputational damage to contract loss. CiUK recognises this and integrates commercial insight into every inspection. CiUK helps providers achieve operational excellence and commercial resilience by aligning care quality with business performance.
THE CIUK DIFFERENCE
Choosing Care Inspections UK Limited means selecting a partner committed to professionalism, independence, and comprehensive excellence. CiUK inspections do more than prepare organisations for regulatory visits—they empower providers to deliver safer, higher-quality care while protecting their reputation and commercial future.
CiUK delivers evidence-based assurance and actionable insight for providers who want more than compliance.
Artificial intelligence is becoming part of everyday life and many residential care services are beginning to explore how it could support better care. When used responsibly, AI has the potential to reduce administrative pressure, give teams faster access to information and help staff make more informed decisions. But like any new technology, it requires careful planning, clear safeguards and open conversations with residents, families and colleagues.
At a recent roundtable hosted by Casson Consulting and the Access Group, care providers and digital specialists reflected on some of the opportunities and challenges facing the sector. The discussion echoed what we at Digital Care Hub hear from providers across the country. There is enthusiasm about using AI to free up staff time, improve consistency and spot risks earlier. Practical examples include tools that help identify trends in care records, digital assistants that help staff find policies quickly and early exploration of companion technology that could complement activity programmes. As Hallmark Luxury Care Homes noted, the aim is not to replace staff but to support them with the right information at the right time . Any use of AI in care relies on trust. Residential care is built on strong relationships, so residents, families

and staff must feel confident about why AI is being used and how their information is being protected. Katie Thorn, from Digital Care Hub and the Oxford Project: The Responsible Use of Generative AI in Care, highlights the importance of involving people at every stage. This includes explaining what a tool does, how decisions are made and how staff will continue to use their professional judgement.
A key theme from the roundtable, and from our wider work, is the need to recognise the limitations of AI. These systems can reflect the biases in the data they are trained on, so staff should be supported to question outputs rather than assume they are always correct. Good training, clear policies and safe channels for raising concerns are essential. Sharing examples where AI has not worked well is just as important as sharing successes. This helps the whole sector build confidence and avoid repeating mistakes.
Introducing AI into a residential care setting is not about rushing. It is about moving safely and purposefully. With the right digital foundations, strong governance and meaningful involvement of residents and colleagues, AI can become a valuable support for thoughtful, person-centred care.
For further information on Digital Care Hub and how they can help you, see the advert on page 37.
Nursing leaders are warning of a “devastating” winter ahead as new figures reveal a staggering 90-fold increase in 12-hour hospital admission waits over the past six years.
Analysis shows that between July and September this year, 116,141 patients waited more than 12 hours in A&E departments after a decision to admit them – compared to just 1,281 in 2019. This represents an increase of almost 9,000%.
The situation is placing unprecedented pressure on emergency and elective care services across England, with implications for patient flow throughout the entire health and care system. CAPACITY CRISIS
Despite the dramatic rise in demand, overnight bed capacity has grown by only 2% since 2019, adding just 2,192 beds. This means 52 patients who are sick enough to be admitted are now competing for each additional bed.
The pressures are being further compounded by limited capacity in community and social care services, which is preventing timely hospital discharge. NHS data from October 2024 revealed an average of 13,117 patients remained in hospital each day despite being medically fit for discharge – a 6% increase on the previous year.
These findings are detailed in a new briefing paper titled Bracing for winter: a close look at NHS emergency and elective care in England and its implications for corridor care, published by the Royal College of Nursing.
GROWING FRUSTRATIONS
The crisis is also reflected in patient behaviour, with more people leaving A&E without receiving treatment. This figure has jumped from 100,000 in 2019 to more than 320,000 in 2024, reflecting growing frustration with under-staffed and under-resourced services.
Professor Nicola Ranger, RCN General Secretary and Chief Executive, said: “Nursing staff and patients alike endured a horrendous winter last year, with corridor care rife across every service. Worryingly, after no respite in the summer, the signs point to the coming colder months being devastating and more dan-
gerous for patients.”
In the absence of published data on corridor care – which the government committed to releasing almost six months ago – waits of 12 hours or more are considered the clearest indicator of the practice taking place in hospitals.
Corridor care sees patients treated on trolleys, chairs, and even in cupboards or offices, often without access to essential equipment like oxygen and suction. Nursing staff have reported patients enduring intimate examinations in public areas, whilst temporary escalation spaces are being counted as safe, clinical “beds” in official figures.
In January, thousands of nursing staff shared testimony of patients enduring corridor care, with some dying and remaining undiscovered for hours. The RCN declared a “national emergency” over the issue in May 2024.
Professor Ranger emphasised the need for urgent government intervention: “Nursing staff have repeatedly warned about a corridor care national emergency, but the lack of urgency in tackling the crisis is unacceptable. Bed capacity has remained static, nurse numbers in hospitals haven’t increased to the level required and community services are not being invested in anywhere near fast enough.”
The RCN is calling on ministers to boost capacity through new funding to improve staffing levels and increase hospital bed numbers. The organisation is also urging a more rapid timeline of investment to grow staff and provision in primary, community and social care services.
“Ministers must also stop delaying publishing the data on just how widespread corridor care is,” Professor Ranger added. “Patients deserve transparency over care standards.”
The capacity constraints in community and social care remain a critical bottleneck, with care home sector leaders emphasising that investment in these services is essential to ease hospital pressures and ensure safe, timely discharge for elderly and vulnerable patients.

How technology-driven engagement is boosting morale, staff retention, and wellbeing in UK care homes.
In today’s social care environment, the pressures on providers have never been greater. Rising costs, recruitment uncertainty, and increasing expectations from families and the CQC are leaving many care homes stretched thin. Yet, amid these challenges, one innovation is quietly reshaping daily life for both staff and residents - the Mobii Interactive Projection System from OM Interactive.
Drawing on OM Interactive’s 2025 Nationwide Survey of care professionals, The Mobii in Care: Executive Insights 2025 reveals powerful evidence that interactive technology can do more than engage - it can rebuild morale, reduce workload, and help care teams deliver the quality of care they aspire to.
Care work is among the most rewarding professions, but it is also one of the most emotionally demanding. Many care teams report that introducing the Mobii has brought back a sense of joy, pride, and connection to their daily work.
“Staff feel able to offer a more meaningful experience for service users,” says Marion Hunt, Advanced OT/Sensory Lead at The Hatherton Centre, MPFT.
That feeling matters - because it directly supports staff retention and resilience. When staff see residents light up with engagement, they’re reminded why they chose care in the first place.
Most managers surveyed said the Mobii has made a positive difference to staff workload, reducing stress and freeing up time to focus on genuine interaction. “It’s very easy to set up and use, which frees up the team’s time to spend more time engaging in a group activity,” shares Celia Milton, Activity Champion at Anchor’s Limegrove Care Home.
For carers, it’s not just about having a new tool - it’s about having something that makes their day feel easier, more purposeful, and more connected.
ENHANCING WELLBEING FOR RESIDENTS AND STAFF
The impact on residents is equally remarkable. An overwhelming 90% of care homes said the Mobii has enhanced wellbeing and engagement for both residents and staff. Through light, sound, and movement, it brings interactive experiences directly onto any surface - sparking laughter, movement, and conversation.
“The residents who would seem lethargic and unalert would be revived when the therapeutic games are played,” explains Carolyn Weisey, Activities Coordinator at St Annes Care Home.
Even residents living with advanced dementia have shown renewed participation. “Increased participation, especially from our residents living with more advanced dementia,” adds Celia Milton.
For many homes, this shared experience creates a calmer, happier environment - one where relationships thrive, and residents and carers alike feel more connected. SUPPORTING CQC EXCELLENCE
In a sector where inspections and accountability are central, the Mobii also provides measurable support for achieving CQC excellence. Homes using the Mobii report improved outcomes within the “Caring” and “Responsive” categories - both areas where person-centred engagement is critical.
“It can be used for person-centred activities as there is something to suit all needs - and CQC love that,” says Colette Yuksel, Activities Coordinator at Stocks Hall Nursing Home Burscough.
This ability to provide inclusive, evidence-based engagement demonstrates a home’s commitment to meaningful care - something inspectors, families, and staff all value highly.
With the upcoming Immigration Bill expected to limit access to overseas care workers, providers across the UK face mounting pressure to retain and support their teams. Recruitment challenges, rising agency costs, and burnout are creating a perfect storm - one that demands creative, proactive solutions.

The Mobii offers exactly that. It simplifies activity planning, empowers staff to deliver more meaningful sessions, and helps build a workplace culture centred on pride, teamwork, and connection.
As Katherine Huntley, Activities Lead at Dewdown House, puts it:
“Staff love playing with this alongside the residents - it really helps with bonding.”
Real-World Results from UK Care Providers
The survey findings speak for themselves:
• 94% said the Mobii enables more quality time with residents.
89% saw improved mood and interaction.
81% reported enhanced wellbeing and engagement.
90% saw improved memory recall.
93% would recommend the Mobii to other care providers.
These numbers reflect what many care professionals already see every day - a calmer, happier, more connected environment where both residents and carers can thrive.
TECHNOLOGY WITH HEART
As social care continues to evolve, the most successful innovations will be those that combine practicality with compassion. The Mobii proves that technology doesn’t have to replace the human touch - it can enhance it, helping carers do what they do best: connect, comfort, and care.
For care providers looking to strengthen staff wellbeing, enrich residents’ lives, and demonstrate excellence to the CQC, the question isn’t whether they can afford to invest in engagement technology.
It’s whether they can afford not to. For

A National Audit Office report has revealed that GPs are failing to provide adequate support and follow-up care for England’s 1.5 million frail older people, leaving vulnerable patients at heightened risk of medical crisis and avoidable hospital admissions.
The report examines how the NHS identifies and manages frailty—a medically recognised syndrome affecting multiple body systems that leaves people exhausted and often housebound—and concludes that early intervention is falling short despite the growing demands of an ageing population.
The GP contract requires GPs to identify any registered patient aged 65 years or over who is living with moderate to severe frailty. However, in 2024-25 GPs only assessed one in six patients aged 65 or over for frailty (1.9 million people). This is well below the one in four assessed when the requirement was introduced in 2017-18.

Once they have assessed patients GPs are not providing the required support and follow-up for people diagnosed as living with severe frailty.
OF THE 226,000 PATIENTS DIAGNOSED WITH SEVERE FRAILTY IN 2024-25, ONLY:
• 16% (37,000) had a medication review;
• 18% (41,000) had a falls risk assessment; and
• 29% (66,000) had given consent for an enriched summary care record.
There is significant variation in the proportion of patients who were assessed for frailty across the country. The report finds a worrying inconsistency in delivery of the required support and follow-up for those diagnosed as living with severe frailty.
Support that GPs provide under the Enhanced Health in Care Homes programme is deteriorating in some
important aspects of care. For example, the percentage of residents who had a personalised care and support plan agreed or reviewed has fallen sharply, from 76% in 2022-23 to 44% in 2024-25.
Urgent community response services are meeting targets. The aim of urgent community response teams is to provide urgent care to people in their homes which helps to avoid hospital admissions and enables people to live independently for longer.
The 2025 10 Year Health Plan did not explicitly introduce any further developments on frailty although it set out the intention to develop several new service frameworks, with early priority given to frailty. The more recent planning guidance mentions frailty as a priority for the new neighbourhood health service and asks for growth in community health services.
THE NAO REPORT MAKES A NUMBER OF RECOMMENDATIONS, INCLUDING:
• NHSE should set clear and consistent requirements for GPs to assess and support people living with frailty
• NHSE should set out a timetable for its work to standardise community health services and details on how community health services will align with and support the move to neighbourhood health services
• DHSC should commission a systematic evaluation to demonstrate whether its patchwork of frailty initiatives is working together to provide an effective and holistic approach
Gareth Davies, head of the NAO said: “With the need for health and social care services set to increase in our aging population, it is crucial that people with frailty are supported effectively and consistently across the country. Our report shows that many older people are not getting the support they need.
“The NHS needs to seize the opportunity of the 10-year health plan to build the more effective and sustainable service that it recognises older people need.”
When Spring Grove Care Home in Hampstead undertook a major wet room refurbishment programme, the challenge wasn’t just to modernise. It was to do so without disrupting the daily lives of residents. With 46 en-suite bathrooms to upgrade, traditional tile-based installation methods posed clear limitations: long downtime, specialist trades, and significant disruption.
Springdene Group, which operates the care home, turned to Multipanel, the UK’s leading bathroom wall panel brand. Its rapid-installation system enabled each bathroom to be completed in just 1.5 days. For care home operators and specifiers working in live environments, that turnaround is more than a number. It is a strategic advantage.
THE INSTALLATION CHALLENGE IN LIVE CARE SETTINGS
Spring Grove is home to residents living with Alzheimer’s and other forms of dementia. Routine and consistency are essential in this setting. In any live-in care environment, prolonged bathroom refurbishments can be distressing for residents and difficult to manage operationally.
The key to Springdene’s approach was finding a wall surface solution that delivered on performance, appearance and speed. Tiling was ruled out early in the process due to the disruption it causes. Long curing times, noisy wet trades and ongoing grout maintenance were all barriers to efficiency. In contrast, Multipanel’s wall panel system provided a fully waterproof, grout-free alternative that could be installed quickly by a team of multi-skilled tradespeople.

Each bathroom was completed in just 1.5 days from start to finish, allowing entire floors to be refurbished in a matter of weeks rather than months. This helped keep disruption to a minimum, allowing residents to stay in their rooms or return swiftly.
COMBINING SPEED WITH
For Springdene, speed was only one part of the equation. The visual appearance of the finished bathrooms also played a crucial role. The team was keen to avoid the clinical or institutional look often associated with healthcare environments. Instead, they wanted a modern, hotel-style aesthetic that felt calm, comfortable and familiar.
Multipanel’s tile-effect panels provided the perfect solution. With clean lines and smooth, gloss surfaces, the panels helped create stylish bathrooms that felt bright and contemporary. The result was a space that improved the daily experience of residents and supported a high standard of living.
“Mutipanel allows the care home to move away from an institutional aesthetic without compromising on hygiene or durability,” said Jamie Sandilands, Specification Sales Director at Grant Westfield, manufacturer of Multipanel. “The installation speed surprised even experienced contractors on-site.
Being able to complete each bathroom in just 1.5 days is a game-changer for care home refurbishment projects.”
Beyond speed and style, the refurbishment also had to meet the requirements of inclusive design. Each bathroom needed to be safe and accessible for users with a range of mobility and cognitive needs.
Slip-resistant vinyl wet room flooring was combined with Multipanel’s waterproof wall panels to create level-access, easy-to-navigate spaces. The design meets both Lifetime Homes and accessibility standards, ensuring long-term safety and usability.
Multipanel panels also reduce long-term maintenance. With no grout and a smooth surface, they are simple to clean and resistant to mould or moisture ingress. This minimises the time staff spend on repairs or deep cleaning, allowing them to focus on care delivery.
The project began with a free trial bathroom installation, provided as part of Multipanel’s specification support. This included complimentary product supply, installation and onsite training led by a trained installer.

The trial gave Springdene the chance to evaluate the product in real conditions and train their trades team at the same time. Following its success, 12 rooms were refurbished, with a further 12 scheduled. The group is now planning similar upgrades across its other care homes, Springview in Enfield and Spring Lane in Haringey, covering nearly 120 rooms.
For architects, developers and specifiers working in healthcare, retirement living and supported housing, Spring Grove’s approach offers a proven model for fast, specification-led refurbishment.
Multipanel panels are five times quicker to install than traditional tiles. Their 30-year warranty, FSC certification and EPD credentials make them suitable for projects with performance, compliance and sustainability targets.
As the care sector continues to face rising demand and operational pressure, solutions that combine design, efficiency and compliance are increasingly important.
“The Spring Grove project is proof that you don’t have to compromise on aesthetics or performance to gain speed,” said Jamie Sandilands. “Our approach allows specifiers to deliver contemporary, durable bathrooms that work for everyone - residents, staff and operators alike.”
EXPERIENCE IT FOR YOURSELF
Multipanel’s Free Trial Scheme allows care providers and specifiers to experience the installation, performance and support service first-hand before committing to a full rollout.
For more information, visit www.multipanel.co.uk or contact the specification team to discuss upcoming projects. 0131 290 286.
Alzheimer’s Society teams up with British Deaf Association to support Deaf people affected by dementia
People in the Deaf community will now be able to access dementia support more easily, thanks to a partnership between Alzheimer’s Society and the British Deaf Association.
The charities have worked together to make Alzheimer’s Society’s support services, such as its Dementia Support Line, more accessible. A SignVideo option on Alzheimer’s Society’s website links the user up with a British Sign Language interpreter who can then live translate information from the Dementia Support Line team.
Each week, around 1,500 people reach out to Alzheimer’s Society’s Dementia Support Line for help. Expert Dementia Advisers provide personalised support to people facing the daily challenges of life with dementia, signposting callers to a network of emotional support, practical advice and a community that understands their situation.

Paul Reynolds, Associate Director of Commercial and Partnerships, at Alzheimer’s Society, said: “Receiving a dementia diagnosis can be a worrying time but Alzheimer’s Society is here to help guide people from every community to the care, support and treatment that is so vital.
“We know that people in the Deaf community are often overlooked when organisations are designing their services, leaving them to depend on family or friends to help them access support.
“That’s why we’re committed to making our resources more inclusive and accessible – ensuring no one faces dementia alone, regardless of how they communicate.”
Rebecca Mansell, Chief Executive Officer of the British Deaf Association (BDA), said: “We are proud to partner with Alzheimer’s Society to raise awareness of dementia within the Deaf community and ensure vital information is accessible in British Sign Language (BSL). This initiative was originally led and developed by BDA Scotland, whose outstanding work on dementia laid the foundation for this collaboration.
“This important partnership aims to build a strong bridge between Alzheimer’s Society and the Deaf community – improving access to information, support, and understanding of dementia. It comes at a crucial time, as we work together across the UK to make a meaningful difference.”
As part of their partnership with British Deaf Association, Alzheimer’s Society will also run Deaf awareness sessions for their Dementia Advisers and will continue to create advice videos using British Sign Language. It will take a society to defeat dementia. With your help we can continue to provide advice and support through our support services. To donate or find out more, visit alzheimers.org.uk/Christmas or call Alzheimer’s Society’s Dementia Support Line on 0333 150 3456.
Hundreds of residents from Bupa care homes have knitted almost 54,000 premature baby bonding squares as part of a nationwide donation drive for neonatal units.
The 10cm x 10cm squares are widely used by hospitals to help mothers and premature babies bond while the babies are in hospital. The squares are kept with mother and baby and then swapped, allowing the baby to be comforted by their mother’s scent, while helping the mother maintain her milk supply and emotional bond.
The donations are part of celebrations for Bupa Care Services’ 40th anniversary, with residents wanting to give back to their community in a special and unique way.
Neonatal units rely heavily on donations of the bonding squares, which are small but vital items that can be costly to source from independent sellers.

The initial goal was to collect 25,000 handmade squares, but thanks to the efforts of residents, that milestone was reached by August this year, with the target then raised to 40,000 to mark 40 years of Bupa Care Services. By November, the total had surpassed all expectations at an incredible 53,884 squares.
Bupa colleagues, local communities and families also helped boost the total, with every square individually hand-counted.
Believed to be the largest organisation-wide collection of its kind, Bupa has now approached the
Guinness World Records team to verify whether the achievement could set a new record.
Betty, 85, resident at Sunnyview House Bupa Care Home, West Yorkshire, said: “After losing my husband earlier this year, helping the premature babies gave me something to focus on. I love knitting and knitting the squares gave me a purpose.”
Harriet, resident at Elm View Bupa Care Home, Somerset, said: “When I worked I was in nursing, and my daughter went into nursing looking after premature babies. So I know how much these bonding squares would have been appreciated by mum and baby. It brings me joy to know I can still help those in need.”
Tom Hoosen-Webber, General Manager for Bupa Care Services, said: “I’m incredibly proud but not surprised by the amazing generosity of our Bupa care home residents. Their time, skill and kindness have created thousands of invaluable gifts for new mothers and their babies.
“This project has been a powerful reminder of the compassion, creativity, and community spirit that define our Bupa care homes and Richmond Villages. It’s been a joy to see everyone come together to make a difference – one square at a time.”
Residents will continue their knitting next year, under a new initiative ‘Need for Knitting’. Bupa homes and Richmond villages will choose their own charities to knit for, with residents continuing to hand-knit donations for the likes of homeless shelters, animal rescue centres, children’s hospital charities and more.

The award-winning TLC Group is proud to announce that its only residential home of nine homes, Cuffley Manor Care Home in Potters Bar, Hertfordshire, has been awarded the Gold Standard for Dementia Care by the National Dementia Care Accreditation Scheme (NADCAS), recognising the home as a leading provider of high-quality, specialist dementia support in the region.
The Gold Rating is the second-highest level of accreditation offered by NADCAS and is awarded only to care homes that demonstrate exceptional standards in personalised care, staff training, resident engagement, safety, wellbeing, and environmental design.
Over recent years, Cuffley Manor has invested heavily in enhancing its dementia care offering — from adopting evidencebased care approaches to delivering regular specialist training and creating calming, thoughtfully designed spaces tailored to the needs of residents living with dementia.
Millie Solley, Practice Development Lead for Cuffley Manor said: “This accreditation is a testament to the compassion, exper-
tise, and dedication of our entire team. We are proud to offer families complete peace of mind, knowing their loved ones are supported in a luxury environment with consistently outstanding dementia care.”
The Gold Standard marks a significant milestone for Cuffley Manor’s commitment to delivering high-quality, luxury care for older adults in Potters Bar and the surrounding area. It reinforces the home’s reputation as a trusted destination for families seeking specialised dementia support with a homely, person-centred focus.
This recognition from NADCAS highlights the progress made by Cuffley Manor in strengthening its dementia care practices. It also serves as an encouragement for the team to continue learning, adapting, and refining the support they provide. As the needs of residents evolve, the home remains focused on sustaining an environment where people living with dementia can experience comfort, dignity, and a sense of belonging.

The NHS is grappling with an unusually severe and early flu season, with latest data revealing hospital admissions for influenza at unprecedented levels for this time of year. The surge comes as delayed discharges continue to rise, presenting significant challenges for care home providers and community health services.
According to NHS England’s urgent and emergency care daily situation reports, an average of 1,717 patients occupied hospital beds due to flu every day last week—the highest figure ever recorded for early December. This represents a more than sevenfold increase compared to the same week in 2023/24, when just 243 patients were hospitalised with influenza, and a 56% rise from last year’s figure of 1,098. Despite the dramatic spike in flu cases, overall virus-related hospital pressures have actually decreased compared to last year. Last week saw 2,943 adult and paediatric beds either closed or occupied due to Covid-19, flu, norovirus and paediatric RSV combined, down from 3,546 during the same period in 2024. This improvement is primarily attributed to lower levels of norovirus and Covid-19 infections.

However, delayed discharges remain a persistent concern with direct implications for the care sector. The data shows 13,232 hospital beds were occupied daily by patients who no longer met the criteria to remain in hospital—an increase from 11,969 the previous year. These delays are frequently caused by insufficient availability of follow-up social or community care, highlighting the critical role care homes and community
services play in maintaining hospital flow.
There was more positive news regarding ambulance handover times, with 29.7% of delays exceeding 30 minutes last week, compared to 36.1% in 2024. Similarly, the proportion of handovers taking longer than an hour dropped from 16.4% to 10.0%—a significant improvement despite increased overall demand.
Rory Deighton, acute and community care director at the NHS Confederation, warned that the early and intense flu season is compounding pressures on services that have already experienced one of their busiest summers on record.
“NHS service leaders are doing all they can to ensure all patients are kept safe and receive the care they need,” Mr Deighton said. He noted that whilst improved ambulance handover times were welcome, the combination of higher delayed discharges and rising demand creates bottlenecks that can lead to longer A&E waits.
Mr Deighton emphasised that discharge delays, often stemming from gaps in social or community care provision, coupled with surging demand, place enormous strain on the entire healthcare system. He added that health service leaders are working to provide patients with better access to GPs, urgent treatment centres, and community support for falls and frailty.
Residents from Exemplar Health Care made history at this year’s Nursing Live conference, becoming the first people with lived experience to host a full panel session.
Their session, Lived Experience, Lasting Impact: Residents Leading the Way, captivated a packed audience of more than 120 delegates in the Learning Lab theatre. Demand for the session was so high that seating had to be closed off, with attendees gathering wherever they could to listen in.
The talk was led by three of Exemplar Health Care’s Regional Service User Ambassadors. Dave from Willowbeck and Alex from Maypole Grove both took to the stage, while Adam from Greenside Court participated via video to help further bring the group’s message to life.

Together, they shared their deeply personal stories, exploring the importance of co-production in social care and why people’s voices must be heard, valued, and acted upon. Their presentation built on Exemplar Health Care’s Service User Engagement Strategy – an approach that empowers people living in its homes to lead the way in shaping care delivery, training, and organisational policy.
Dave shared his moving story of recovery following a brain stem stroke sustained in a skiing accident. He reflected on his journey from the early days of communicating through eye blinks to becoming a public speaker (helped by eye gaze technology) and advocate for others.
“It’s important to remember there will be some of us who need you to speak up for us. In my experience, there seems to be a bit of a myth that you shouldn’t speak on behalf of someone. In my book, your knowledge of an individual is just as important as anyone else’s, and your knowledge of them should include when they will appreciate you sharing it.”
His talk explored what true person-centred care looks like in practice, emphasising that small, human acts of inclusion and understanding can profoundly change how someone feels about their care.
“I remember being asked for some suggestions for a nice walk in the hills or being asked for help with
another service user’s computer because someone thought to ask if I might be able to help. It added to the sense that I could participate in the world, like I can make a contribution.”
Adam’s story, shown on screen, told of his remarkable recovery and personal growth after his life was changed by a brain injury caused when his drink was spiked at a party. He described his journey from losing all mobility and speech to rebuilding his confidence and finding purpose through the Ambassador programme.
“Becoming an ambassador made me feel important again. I’ve gone from needing help with everything to helping others. I never thought I’d have a voice again, but now, I use it to make a difference.”
For Alex, the event marked a personal milestone. Once nervous about public speaking, she delivered her part of the presentation with warmth and confidence, sharing how the ambassador role has helped her rebuild her independence and self-belief.
“My family didn’t think I’d get any better, but when I came to Exemplar Health Care everything changed. The team take me to Download Festival every year and help me keep doing the thing I love. It’s a full-on week but I get to see my friends and have fun. The Ambassador role has also changed my life. I’d never had the confidence to speak in front of anyone really, and now look at me, in front of all of you!”
Following the session, audience members described the talk as “moving”, “inspiring” and “a highlight of the conference”, with many approaching the speakers afterwards to thank them personally for their honesty and insight.
Sophia Feurtado, Service User Engagement Manager at Exemplar Health Care, said: “This was a truly landmark moment – not just for Exemplar Health Care, but for the social care sector as a whole. Our ambassadors spoke with courage and authenticity, and the response in the room was incredible. Their stories remind us that the people we support are experts by experience, and that listening to them can change how we provide care for the better.”
Warwick House is a residential home in Paignton supporting up to six adults with autism, learning disabilities and mental health needs.
Ross, 39, brings a wealth of experience to the role, having worked in social care since January 2018. He began his career as a support worker for adults with learning disabilities and behaviours that may challenge, before spending time supporting young people in their transition from care to independent living.
He went on to serve as deputy manager in supported living services for adults with learning disabilities, later progressing to service manager where he successfully combined and led two operations. Ross then returned to supporting young adults as a multi-site home manager, before realising that his true passion lay in working with adults with learning disabilities.
In early 2023, Ross became registered manager of a 10-bed residential home for deafblind adults with complex health needs. He oversaw a significant service

turnaround, transforming a setting that had been at risk of closure into a stable and highquality home.
Following this achievement, Ross sought what he describes as his “forever home” in social care, joining Salutem as Warwick House’s new registered manager.
Ross said: “After researching Salutem, I felt the company’s values aligned with my own, and the location was perfect for me. When I met senior managers and the CEO, I immediately recognised how supportive and encouraging the organisation is. I couldn’t wait to join. My key responsibility now is not only to ensure the service runs smoothly and compliantly, but to continue the fantastic work of the previous manager. It’s a true privilege to be here and to be part of Salutem as the organisation continues to grow and excel.”
John Godden MBE, chief executive of Salutem Care and Education, said: “Ross brings excellent experience, strong values and a clear passion for delivering high-quality, personcentred support. His track record in service improvement and leadership is outstanding, and we are delighted to have him join the Salutem family. Warwick House is a very special service, and I am confident Ross will help it continue to flourish.”
Home adaptations teams have a unique tool to help expediate fast, efficient aids to help people be safe at home.
The number of, and wait time for, adaptations continues to grow, with stairs being the second most common hazard in the home. In conjunction with Occupational Therapists, AAT has developed its Universal Seat System for its brand-leading S-Max Sella stairclimber.
The combination amplifies adaptations teams’ ability to optimise use of budgets- usually without even requiring DFG funding- to deliver a safe stairway transfer solution within days, by recycling (re-issuing) the equipment.
The S-Max Sella provides a safe stair transfer solution in 99+% of cases which AAT assesses. The portable Class 1 Medical device certified kit requires no installation nor structural alteration to the home. The addition of the Universal Seat System means the Sella can be easily set up to ensure almost every potential user is safe and supported when using the Sella, irrespective of their physical and/or mental impairment. It is achieved without the need to purchase extra accessories. No other stairway transfer system offers such flexibility.

HipSaver Soft Hip Protectors protect the elderly and disabled people from fall-related hip fractures. Designed to protect elderly people from fall related hip fractures, HipSavers are a leading brand of soft hip protectors. Used in the NHS since 2002, HipSaver Soft Hip Protectors are user friendly, affordable and costeffective personal protective garments. Soft, comfortable, effective and compatible with incontinence protection, HipSaver Soft Hip Protectors are perfect for use in care homes and by elderly people living independently.

Available as comfortable underwear or long casual pants in several sizes for men and women,
HipSavers feature soft protective airPads permanently sewn into the garments over the hip areas prone to injuries and fractures.
HipSaver TailBone models have an additional protective airPad over the coccyx on lower back for protection during swaying, accidental knocks, bumps and backward falling. Machine washable at high temperature and tumble drier friendly, HipSavers are practical, hygienic and durable.
HipSavers should be worn day and night for 24 hour protection and especially during physical and recreational activities, when accidental falls, slips and trips can lead to hip fractures.
HipSaver Soft Hip Protectors - affordable protective garments for the elderly and disabled people! For more information, contact Win Health Medical Ltd - 01835 864866 - www.win-health.com See the advert on page 3 for further products.
At Blue Rain, our mission is simple: to provide everyday activity products that spark joy and enrich lives — whether for those who need a little extra support, a burst of motivation, or simply a reason to have fun.
We take pride in listening to our customers, understanding what truly matters to them, and sourcing or creating products that meet those needs perfectly. Many of our items are available as ready-to-go activity kits and bundles — complete with everything you need — so

you can skip the preparation and focus on the joy of the moment.
As Blue Rain Activity Store continues to grow, our heart remains the same: creating meaningful moments of happiness, connection, and creativity for people of all ages and abilities.
From rainy-day craft sessions to sunny outdoor adventures — or simply time spent together — we’re here to make every experience easy, special, and unforgettable.
See the advert on page 6 for further information.

Repose Furniture is one of the UK’s leading manufacturers of bespoke seating solutions, with a reputation built on craftsmanship, innovation, and a strong commitment to improving the quality of life for its customers. Established in 1999 and based in the West Midlands, the company has grown from a small family business into a trusted supplier to both the domestic and healthcare markets. Every chair produced by Repose is handmade in the UK, with an emphasis on quality, durability, and comfort, ensuring that each product meets the specific needs of its user.
Whether for home use or demanding healthcare environments, Repose combines skilled upholstery techniques with modern engineering to create chairs that provide postural support, pressure management, and ease of use. Their wide product portfolio includes rise and recline chairs, hospital and care home seating, bariatric solutions, and specialist products designed to address particular medical and lifestyle needs. An essential element of their offering is flexibility: customers can choose from a range of back styles, seat cushions, mechanisms, and fabrics, allowing each chair to be tailored to the individual. Interchangeable parts mean that a chair can adapt as a user’s requirements change, extending the product’s longevity and ensuring value for money. The healthcare sector is a particular area of expertise for Repose. They strive to design chairs that balance comfort with clinical functionality. Features such as tilt-in-space mechanisms, adjustable cushioning, and pressure relief options make their healthcare seating particularly suited to long-term use in hospitals, hospices, and
As part of the offering, AAT will also support the adaptation team in the assessment process, to ensure the relevance of the solution for the person, the occupation and the environment, and personally train the carer in the Sella’s safe operation.
“We have numerous examples of community equipment services (eg Nottinghamshire & Nottingham City) now buying not just additional Sella stairclimbers, but Universal Seat Systems, to have in equipment stores ready to go, so they can quickly deliver a solution for a client,” says Peter Wingrave, AAT Director.
“Even if it is a short-term solution whilst a larger and/or more permanent adaptation is undertaken, our Sella/Universal Seat System and re-issue capability gives a highly costeffective and fast way to manage the potential risk of someone falling on the stairs: a genuine adaptation without delay.”
Full details of the Sella and Universal Seat System can be found on AAT’s website @ https://www.aatgb.com/s-max-sella/ where adaptations teams can also book a free, no obligation client assessment or team demonstration session.
Consort’s PLSTiE range of Low Surface Temperature (LST) fan heaters offers a safe, efficient, and modern heating solution. They are designed for environments where safety and comfort are paramount. With a maximum surface temperature of 43°C, these heaters adhere to the NHS Estates Health Guidance Notes standards, making them suitable for use in hospitals, care homes, schools, and nurseries.

The PLSTiE heaters are equipped with features such as intelligent fan control, open-window detection, and quiet operation, all of which contribute to
|
energy efficiency and comfort. Slim and splash-proof (IP24), they combine safety, performance, and flexible installation for various interiors. The PLSTiE WiFi models connect directly to the Consort Connect app, allowing remote control, scheduling, and energy monitoring. BIM downloads for the PLSTiE
Angloplas are a UK manufacturer who specialise in producing dispensers for the health and hygiene industry. Although these are designed to keep the workplace tidy and uncluttered they are, more importantly, built knowing the control of healthcare-associated infections (HCAIs) are a priority for healthcare providers, and who are employing a combination of infection prevention and control strategies, including hand hygiene, cleaning, training and the adoption of new technologies, to tackle the problem. As a result, a wide range of infection control products and technologies are emerging on the market, including antimicrobial technology. Angloplas’ range of dispensers are produced in the world’s first proven

Antimicrobial PVC with silver ion technology and which is exclusive to Angloplas. This helps reduce the risk of cross infection by stopping the growth of bacteria and mould and works continuously for the lifetime of the product, reducing levels of bacteria such as MRSA, E Coli, Legionella, Salmonella and mould by up to 99.99%.
For non-clinical environments Angloplas has recently launched its new Budget Range of products which are made to the same exacting standards as the antimicrobial protected ones but with lower price tags.
You can order Angloplas products directly from its website at www.angloplas.co.uk See page 4.

care homes. The company’s bariatric range demonstrates the same careful attention to detail, offering robust yet comfortable solutions for larger users.
While customisation is the centre of the Repose offering, they also recognise the urgency often faced in healthcare settings. To address this, Repose have developed their Healthcare Express Chairs, designed to deliver high-quality healthcare seating at speed. The models in this range can be despatched within just five working days. The Multi Bari Express and bestselling Boston Express, for example, are available on this five-day lead time, offering care providers a rapid solution without sacrificing quality or functionality. For less specialist needs, some homecare models are even available on faster turnaround times, demonstrating Repose’s ability to balance responsiveness with craftsmanship.
Repose’s reputation is further reinforced by its after-sales support, 5-year manufacturing warranty, and commitment to ethical and sustainable practices. With a UK-based factory, a dedicated distribution network, and close relationships with healthcare professionals, the company continues to be a trusted partner in multiple sectors throughout the country and beyond.
In combining bespoke design with reliable express options, Repose Furniture stands out as a manufacturer that truly understands the diverse needs of its customers. For over 25 years, it has delivered not just chairs, but comfort, dignity and independence — values that remain at the core of everything it does. For further information, see the advert on page 25 or visit www.reposefurniture.co.uk
By Zoe Cottrell, registered dietitian, member of
the British Dietetic Association and registered with the Health and Care Professions Council

Malnutrition remains a significant issue in care homes, where the elderly are particularly vulnerable. As a registered dietitian working in the community and in hospital wards, often with elderly people who have experienced fall, I wish more people knew about the prevalence of malnutrition and how to combat it before they ended up in hospital.
Recent statistics paint a stark picture: Around one in 10 people over the age of 65 are malnourished or at risk of malnutrition , and this figure rises alarmingly to 45% among those in their 90s. According to the British Association for Parenteral and Enteral Nutrition (BAPEN) , malnutrition costs the UK approximately £23.5 billion annually, with older adults being disproportionately affected.
As the population ages, addressing malnutrition and its associated complications, such as frailty and sarcopenia, becomes ever more critical. By focusing on early detection and strategic nutritional interventions, including the use of protein, care homes can play a vital role in safeguarding the health of their residents.

In the world of care catering, gravy is often an after though – adding some flavour and moisture to food but it can be nutritionally empty. At ProSauce, gravy is the starting point for a quiet revolution.
ProSauce Gravy is more than a condiment. It’s a nutrient-rich, flavourforward solution designed to meet the complex needs of care homes and hospitals. Developed by Stella West-Harling MBE, in conjunction with dietitians from the NHS and top UK universities, the gravy reflects lived experience and professional insight: meals should provide good nutrition and flavour, whilst being cost-effective.
Crafted for operational ease, ProSauce Gravy is shelf-stable, easy to portion, and compatible with diverse dietary needs. It delivers 12g of plant-based protein per serving, whilst being gluten-free and nutrient dense. Whether served in or over meat, or plant-based dishes, it
The first step in combating malnutrition is recognizing its early signs. The Malnutrition Universal Screening Tool (MUST) is a valuable resource for this purpose, enabling caregivers to systematically assess the risk of malnutrition in residents by considering factors such as Body Mass Index (BMI), unintentional weight loss, and the impact of acute illness on nutritional intake.
KEY EARLY SIGNS TO MONITOR:
1. Unintentional Weight Loss: A significant early indicator of malnutrition is unintentional weight loss. Regularly monitoring residents' weight and comparing it to previous measurements is essential. A loss of even 5% of body weight over a few months can signal malnutrition and warrants immediate attention.
2. Decreased Appetite: A reduced appetite is often a precursor to malnutrition. Residents may skip meals, eat smaller portions, or show a lack of interest in food. It's important to understand the reasons behind these changes, which could be linked to dental issues, depression, or medication side effects.
3. Physical Changes: Signs such as muscle wasting, thinning hair, dry skin, or dental problems may indicate nutritional deficiencies. These physical symptoms are often subtle but crucial indicators of potential malnutrition.
4. Fatigue and Weakness: Increased tiredness or difficulty performing daily activities can be related to inadequate nutrition. This could also signal the onset of sarcopenia, where the loss of muscle mass and strength makes everyday tasks increasingly challenging.
(CONTINUED ON THE FOLLOWING PAGE...)
makes supporting nutritional goals easy in a way that is familiar to the diners.
Early adopters are using ProSauce in care homes and hospices with feedback highlighting ease of use for kitchen staff and it’s cost effectiveness. With the additional protein in the gravy, chefs can use less meat in meals to reach the same nutritional standards, which in turn saves costs and improves the stainability credentials of the kitchen.
In a sector defined by improving health and care, whilst managing increasing costs, ProSauce Gravy offers possibility. It’s a small change with big impact: maintaining flavour, supporting health, and reminding us that every meal is an opportunity to care.
Visit the ProSauce website to order your free 20 portion sample box and experience how ProSauce Gravy can help transform mealtimes in care settings.
www.prosauce.co.uk


(CONTINUED FROM PREVIOUS PAGE)
THE ROLE OF NUTRITION IN PREVENTING AND MANAGING FRAILTY
Frailty, a condition characterized by decreased strength, endurance, and physiological function, is closely linked to malnutrition and is a major concern in care homes. Proper nutrition is key to preventing and managing frailty, particularly through the adequate intake of protein, which is essential for maintaining muscle mass and function.
STRATEGIES FOR NUTRITIONAL INTERVENTIONS:
1. Prioritize Whole Foods: Ensuring a diet rich in whole foods is foundational. Protein-rich foods like eggs, lean meats, fish, dairy products, and legumes should be emphasized, as they not only support muscle health but also provide essential vitamins and minerals that contribute to overall well-being.
2. Incorporate Protein Supplements When Necessary: In cases where residents struggle to meet their protein needs through diet alone—perhaps due to a lack of appetite or difficulty chewing—protein powders or fortified drinks can be effective. These supplements can be easily added to meals, snacks, or beverages, ensuring that residents receive the protein they need without overwhelming them with large portions of food.
3. Distribute Protein Throughout the Day: Research shows that distributing protein intake evenly across all meals is more effective for muscle protein synthesis than consuming large amounts at a single meal.
Caregivers should ensure that residents receive adequate protein at breakfast, lunch, and dinner to maximize the benefits for muscle maintenance and frailty prevention.
ADDRESSING BARRIERS TO ADEQUATE NUTRITION
While boosting protein intake is essential, we should also address the barriers that may prevent residents from consuming enough nutrients. Factors such as taste preferences, difficulties with swallowing, or digestive issues can all impact nutritional intake. Caregivers should work closely with dietitians to develop personalized nutrition plans that accommodate these challenges, potentially incorporating protein powders and other supplements in palatable and easy-to-digest forms.
NUTRITION IS KEY TO INCREASING HEALTHSPAN
Malnutrition in care homes is a pressing issue that requires vigilant monitoring and proactive management. While the numbers alone tell us the stakes are high, intervention is more than about reducing costs. The ability to stand up from a chair unaided allows our elderly residents independence. By spotting the early signs of malnutrition and implementing strategic nutritional interventions, caregivers can help prevent and manage frailty, significantly improving the quality of life for residents. By addressing malnutrition and frailty head-on, care homes can help residents not only avoid the adverse effects of these conditions but also thrive in their later years.
Disease-related malnutrition remains one of the most persistent challenges in UK residential and nursing care. It affects millions, increases vulnerability to illness, slows recovery, drives hospital admissions, and places strain on already stretched care teams. Yet despite the scale of the problem, the tools available to homes have not kept pace with the needs of increasingly complex residents.
Hiquid Food, a Norwegian medical nutrition company, is entering the UK market with a clear mission: to make effective nutritional support simpler, more acceptable for residents, and easier for staff to deliver.
Simple, seamless meal enrichment
Many residents struggle to consume enough calories and protein, even with carefully prepared meals. Hiquid Food’s freeze-dried powders, made from organic whole foods, allow caregivers to enrich everyday dishes like porridge, soups, puddings, purees, and drinks. This discreet approach reduces refusals and preserves dignity, helping residents receive the nutrition they need through meals they already enjoy.
ORAL NUTRITIONAL SUPPLEMENTS WITH HIGH ACCEPTANCE

For individuals at greater nutritional risk, Hiquid Food offers compact, nutrient-dense oral nutritional supplements designed for those with low appetite or increased medical demands. They are easy to con-
sume, well tolerated, and provide balanced support in small volumes.
WHOLE FOOD GASTROSTOMY NUTRITION
For residents requiring enteral feeding, Hiquid Food’s whole-food gastrostomy products offer a gentle, reliable option created with a focus on tolerance, safety, and long-term stability.
Better outcomes and operational efficiency
Care providers face rising acuity and workforce pressure. Hiquid Food products reduce complexity through easy mixing, no additives, and no large volumes while supporting improved resident strength, immunity, and recovery. Better nutritional status means improved wellbeing and lower overall care costs. With long shelf-life, low weight, and high versatility, the products are also environmentally responsible and easily integrated into a wide variety of meals.
As Hiquid Food launches in the UK through Food Untethered, they look forward to working closely with care homes, clinicians, and NHS commissioners to strengthen nutritional care in a practical, resident-centred way.
For more information: contact@fooduntethered.com
See the advert below for further information.

Care homes across the UK are transforming how they deliver care thanks to SyndoraAlto, the newly rebranded name behind CHARIS, the UK’s most advanced digital nurse call system.
Fully supplied, installed, and maintained from just £6.40 per bed, per month, CHARIS delivers smarter, safer, and more connected care through real-time alerts, mobile integration, and intuitive smart displays that help staff respond faster when residents need them most.
Every CHARIS system comes fully inclusive with 15” smart displays, help buttons, pull cords, guaranteed radio coverage, and 24/7 UK technical support, all backed by SyndoraAlto’s trusted installation and maintenance team.

For care providers not yet ready to replace their existing nurse call system, AltoEnhance offers the perfect first step into digital care.
Available from just £129.00 per month, AltoEnhance seamlessly connects to your current nurse call system, bringing digital reporting, mobile alerts, and actionable insights without the need for a full system upgrade.
“Technology should make care easier, not harder,” says Louis Johnson, Managing Director. “CHARIS and AltoEnhance connect people, information, and action empowering care teams to deliver truly person-centred care.” Meet the team & learn more at www.syndoraalto.com See the advert on the front cover for more information.
Alarm Radio Monitoring is the market leader in the design, manufacture and installation of bespoke, end-to-end, wireless alarm systems and solutions for the healthcare, leisure, custodial and education industries.
We have been providing wireless alarm and nurse call systems for over 30 years. Supplying care homes and hospitals with an essential lifeline that supports the delivery of outstanding care.
We believe in excellence which translates into: Advanced Technology Industry-leading wireless alarm technologies and software
Bespoke Solutions
We design systems to your needs rather than your team having to work around the system Innovative Design

Pushing boundaries with the reliability that comes from decades in the industry
Flexible Finance Options
Ensuring organisations of any size can provide safety for their staff and clients 24 Hours a Day, 365 Days a Year Service
Your ARM service team
Falls are a significant concern for vulnerable individuals, especially seniors and patients at risk. Medpage, a leader in assistive technology, offers a range of cuttingedge products designed to enhance safety and provide peace of mind for caregivers and families. Here’s an in-depth look at some of their standout solutions:
MPRCG1 (2023) BED LEAVING DETECTION ALARM WITH CAREGIVER RADIO PAGER
The MPRCG1 is a comprehensive system tailored for fall prevention in domestic, commercial, and NHS care settings. This all-inclusive kit includes a bed pressure mat sensor, a BTX21-MP alarm sensor transmitter, and an MP-PAG31 radio pager. The system is designed to alert caregivers when a patient leaves their bed, reducing the risk of falls. Key features include:
Wireless Alerts: Notifications are sent to the caregiver’s pager via tone or vibration.
Customizable Alarm Delays: Options for instant, 15-minute, or 30-minute delays.
Durable Design: Antimicrobial and disinfectant-resistant materials ensure longevity.
Ease of Use: Minimal installation required, making it user-friendly and portable.
HDKMB2 HOSPITAL DISCHARGE KIT FOR FALLS RISK PATIENTS

The HDKMB2 is a thoughtfully curated kit aimed at supporting patients transitioning from hospital to
home care. It includes essential tools to mitigate fall risks and promote recovery. This kit is ideal for caregivers seeking a comprehensive solution to enhance patient safety during the critical post-discharge period.
CMEX-21 MULTI-PORT WIRELESS SENSOR INPUT EXPANDER FOR NURSE CALL CONNECTION
The CMEX-21 is Medpage’s latest innovation, designed to integrate seamlessly with existing nurse call systems. This multi-port expander allows for the connection of multiple wireless sensors, enhancing the monitoring capabilities of healthcare facilities. Its versatility makes it a valuable addition to any care environment, ensuring timely responses to patient needs.
RON-WC2 WATERPROOF DISABLED PULL CORD ALARM TRANSMITTER WITH WIRELESS ALARM RECEIVER
The RON-WC2 is a robust solution for disabled individuals requiring immediate assistance. This waterproof pull cord alarm is ideal for use in bathrooms and other high-risk areas. Paired with a wireless alarm receiver, it ensures that help is just a pull away.
(CONTINUED ON FOLLOWING PAGE...)

The wireless ARM Nurse Call system has been developed over 30 years with both the client and user in mind.
It enables staff to efficiently answer calls, making the management of resources more flexible and provides the functionality you would expect of any nurse call system.
The system is quick and easy to install and works wirelessly, using radio communication between both the call points and the system infrastructure.
Data Analysis software provides a full audit trail of events
The all-new call logging software from ARM enhances the functionality of your care call system dramatically.
• It can help you track the quality of your service to your residents.
• It can help you demonstrate compliance with your aims and best practices, both to relatives and to authorities.
• It can help you find bottlenecks in service provision, track staffing requirements, and allow you to ensure staff are meeting expectations.
• Most importantly, it provides assurance that you know and can demonstrate what is happening in your care home.
Call messages can be sent direct to staff to speed up response times and can also be integrated to work with smart phones & messaging.
Courtney Thorne, a long-standing innovator in healthcare communication systems, is setting new standards in the care home sector with its advanced wireless nurse call technology—designed to improve resident safety, enhance staff efficiency, and support a more responsive care environment.
With over 30 years of experience serving the UK healthcare market, Courtney Thorne’s systems are now trusted by thousands of care homes nationwide. Unlike traditional hardwired solutions, their wireless nurse call systems offer non-invasive installation, scalability, and smart analytics—making them ideal for both new builds and retrofit projects.
“At the heart of our technology is the belief that better communication leads to better care,” says Graham Vickrage, Managing Director at Courtney Thorne. “Our wireless systems not only reduce response times but also empower staff with the tools they need to deliver safe, person-centred care.”
Care providers are increasingly choosing wireless systems for their flexibility, reliability, and cost-effectiveness. With a full suite of accessories—including neck pendants, door monitors, fall detection, and
bed sensors—Courtney Thorne systems can be tailored to meet the specific needs of each home and resident.
In an industry where compliance, safety, and staff pressures are always front of mind, Courtney Thorne provides more than just products—they offer ongoing support, training, and a commitment to innovation that helps care homes future-proof their operations.
For more information or to book a free demo, visit www.c-t.co.uk or contact info@c-t.co.uk.

(CONTINUED FROM PREVIOUS PAGE)
Features include:
Waterproof Design: Suitable for wet environments.
Wireless Connectivity: Reliable transmission to the alarm receiver.
Ease of Installation: Simple setup for quick deployment.
WHY CHOOSE MEDPAGE?
Medpage’s commitment to innovation and quality is evident in their product range. Each solution is designed with the user’s safety and convenience in
mind, making them a trusted choice for caregivers and healthcare providers alike.
By investing in these advanced fall prevention tools, families and facilities can create safer environments for those at risk. Medpage continues to lead the way in providing practical, reliable solutions that make a real difference.
For more information, visit Medpage’s official website or contact their team to explore these products further. Safety starts with the right tools, and Medpage delivers just that. www.easylinkuk.co.uk
T: 01536 264 869


Young people only make up 11% of care workers. When they’re the ones to pick up the mantles left by 25% of the workforce likely retiring within the next 10 years… it isn’t the most comforting news, especially when the care sector is already stretched so thinly.
We’ve previously discussed how you can attract the under-25s. But it isn’t just about recruiting young care workers. It’s about keeping them, too.
Care can already be an overwhelming career. So, imagine what it’s like when you’re first experiencing it. A lot of young care workers are dropped into the deep end, especially if it’s their first job in the industry.
Combine this with irregular, unsociable hours, and you have a recipe for burnout.
So, what can you do to keep Gen Z in the care sector?
First: training.

Despite qualifications, jumping into the real thing is something new entirely. Plus, since the typical care worker in the UK is aged 45, many vacancies are likely to be filled by those with extensive backgrounds in care. It’s possible, then, that more in-depth training could slip through the cracks for new carers.
It’s easy to get swept up in the waves of care’s responsibilities, whether you’re used to it or not. Offering new hires more in-depth training, ongoing support, and perhaps even a mentor can help them stay afloat amongst the workload.
Next: regular shifts and flexibility.
You may think routine and flexibility contradict each other, but they actually go hand-in-hand.
Burnout in shift work largely stems from poor work-life balance, resulting from staff having little to no control over when they work. Short notice of shifts, combined with irregular and unpredictable ones, leaves workers with a life revolving around work. Even for the biggest workaholics, having no time for a personal life doesn’t make for a healthy one.
Providing enough notice for shifts allows your team to plan around them. Offering rotating schedules and shift patterns also makes hours more predictable, meaning staff can plan even further in advance. (It’s easier for you, too!)
Things come up. Life happens. Ruling your rota with an iron fist gets you nowhere – apart from having unhappy staff.
Flexibility is often misconstrued as spontaneity, but it instead gives staff a voice. Allowing staff to set availability and arrange shift swaps immediately gives them that control they were missing.
You’ll agree that when you aren’t burned out or struggling with poor mental health, you’re better at, well, everything. You’re more productive, more motivated, and you care a lot more about what you’re doing.
This is what Gen Z prioritises. For that, they’re given a bad reputation – just like care gets a bad reputation for a poor work-life balance. But that doesn’t mean the two can’t work together.
By embracing what Gen Z prioritises, you’re not only attracting young care workers, but you keep them.
Decades down the line, who knows, maybe they’ll be the ones retiring and passing the mantle down to their younger counterparts.
www.rotacloud.com

Savers®. The NEW Fall Savers® Wireless eliminates the cord between the monitor and sensor pad. This results in less work for nursing staff, improved safety for patients and reduced wear and tear on sensor pads. Wireless advantages include the ability to use one monitor with two sensor pads simultaneously and support for many new wireless devices.
BENEFITS INCLUDE: Safer for patients; less work for staff
Bed and chair pads available
One monitor works with two sensor pads
Integrates with most nurse call systems
A variety of options, including: Call button Pager
The TreadNought® Floor Sensor Pad is built to last with a durable construction that far out lasts the competition. Our anti-bacterial floor sensor pad is compatible with most nurse call systems or can be used with a portable pager to sound an alert when a person steps on to the sensor pad. Caregivers typically place the sensor pad at the bedside, in a doorway or other locations to monitor persons at risk for falls or wandering. An optional anti-slip mesh reduces the potential for slippage on hard surface floors.
FEATURES INCLUDE:
Connects directly to most nurse call systems
High Quality anti-bacterial Floor Sensor Pad
Large Size Pad: Measures (L) 91cm x (H) 61cm
Options (sold separately):
Anti-slip mesh for hard surface floors
See the advert on this page for further details or visit www.fallsavers.co.uk.


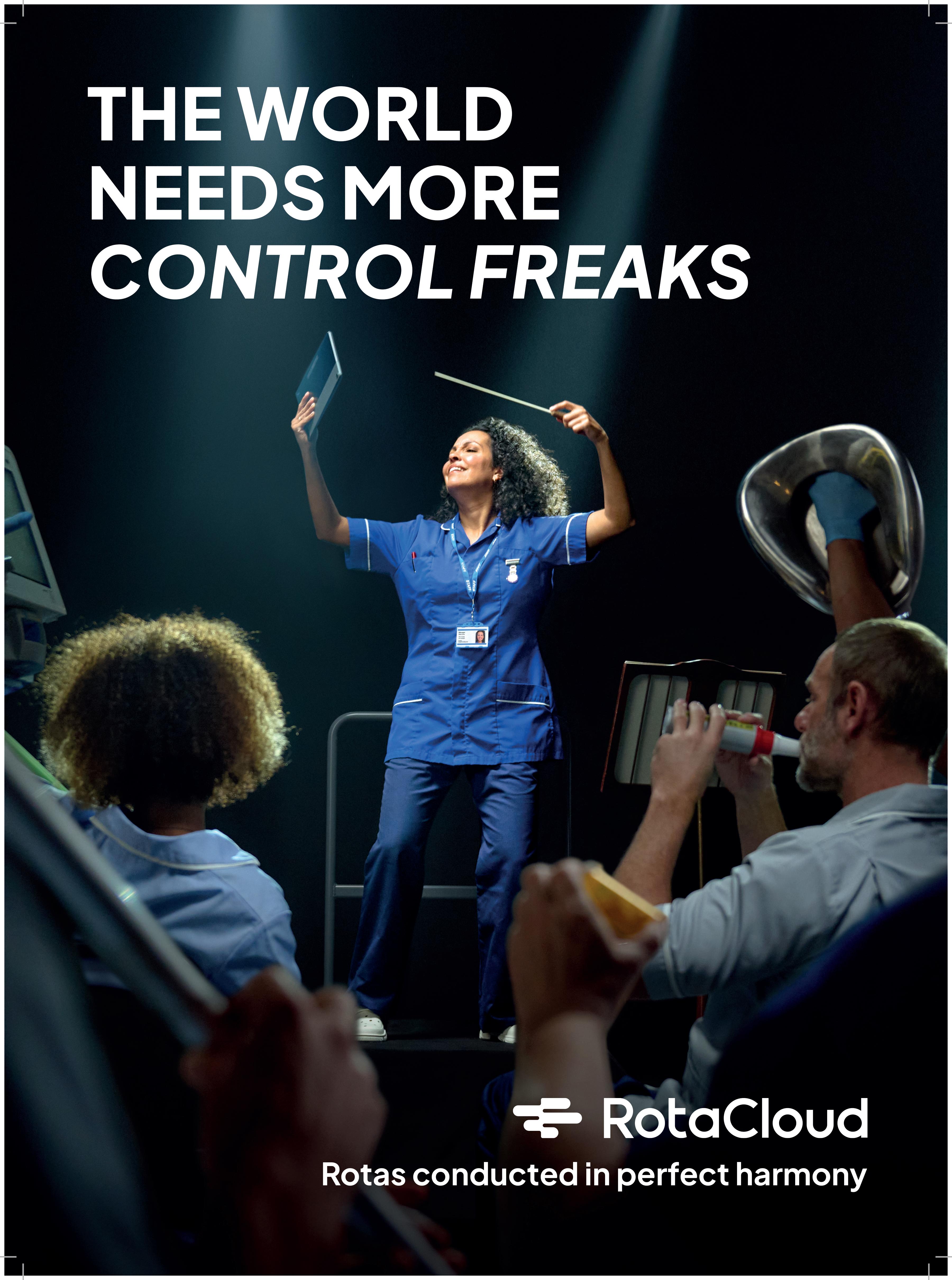
Every day, care organisations are working tirelessly to deliver essential support in the face of growing needs and rising costs. However, too many providers are stuck balancing tight budgets, having ‘just enough’ to stay afloat. The hard truth is, just enough isn’t enough—not for the providers, not for the employees, and certainly not for the clients who depend on them.
Rising operational costs—from wages and the Fair Pay Agreement to energy bills—compound historic underfunding and financial pressures. And demand for care continues to increase, creating a widening gap that organisations are often forced to fill with limited resources.
Providers then end up in survival mode, unable to invest in improving their services for today and the future.
THE NEED TO RETHINK FINANCIAL STABILITY
Care providers need to have healthy finances in social care, and that doesn’t come at odds with delivering compassionate care.
A financially strong organisation has the breathing room to improve services, retain employees, and innovate to make a meaningful difference to the lives of people they support. And having this financial security means providers can actually plan for the future rather than constantly reacting to the present.
BENEATH THE SURFACE
Social care organisations face a web of financial intricacies. Local authori-

how financial pressures continue to challenge social care providers.
ty support often comes with layers of red tape. Managing aged debt and resolving invoicing errors take a significant amount of time that few organisations can spare. Regulation and compliance require meticulous reporting, and the sheer volume of admin work to manage all these leaves teams stretched thin.
At the same time, there’s an expectation for providers to keep doing more. But without the right tools and systems in place, these compounded financial struggles threaten to overwhelm this indispensable sector.
Social care providers aren’t just keeping their organisations alive; they’re safeguarding the wellbeing of countless individuals and families.
Providers need to be able to prioritise long-term financial resilience. And part of this means having the tools—including robust financial management softwaresimplify manual processes, optimise resources, and reduce inefficiencies.
By championing financial sustainability, we’re creating conditions where employees can thrive, where clients receive the quality of care they deserve, and where the sector can confidently meet future challenges.
Find out more at: www.oneadvanced.com/ai
See the advert on the back cover of this issue.
For many care managers, a normal day looks like organised chaos.
You start with care planning, then switch into scheduling. Finance needs attention. A medication update comes through. Audits are approaching. Each task lives in a different place. Another login. Another spreadsheet. Another hour lost.
It is no surprise that so many feel stretched too thin.
The challenge is not the work itself. Care managers are experts at ensuring people receive safe, person centred care. The problem is that many tools in use today simply have not kept up with the demands of modern care.

Too often, care teams are asked to work across platforms that don’t speak to each other. Notes get duplicated. Information gets missed. Important changes take too long to reach the right person. This creates stress for managers and their teams. It also creates risk.
But it doesn’t have to be this way.
When information flows through one connected system, everything becomes clearer. There is one place to update, one record for the whole team to rely on, one view of the care being delivered across every visit or shift. Tasks that once took hours can be completed in minutes. Insights that once required detective work become visible instantly.
This is why more providers are turning to all-in-one care management platforms like PASS.
With care planning, rostering, eMAR and finance in the same system, teams stay aligned and up to date. Real time records help reduce errors and support smoother inspections. Smart automation removes manual admin and frees up more time for face-to-face care.
AI also plays a role. Not by replacing clinical judgement, but by helping care teams stay ahead of change. If something looks different in a note, or if patterns in data suggest a growing risk, the system can highlight it quickly for a manager to review.
Technology becomes a helpful assistant, while care professionals remain firmly in control. Over 1,200 services across the UK are already benefiting from this clearer, more connected way of working. Many report stronger communication, improved compliance, and calmer days as a result.
Care will always be complex. People have unique needs. Things change. But systems that support care don’t need to add to the chaos. When everything comes together in one place, focus can return to what matters most. Delivering outstanding care, every day.
Learn more at www.everylifetechnologies.com


As cyber threats continue to rise across the UK, adult social care finds itself increasingly targeted. Phishing, credential theft, ransomware and supply-chain attacks now routinely affect small and medium providers, many of whom lack the internal infrastructure to respond. What was once an “IT issue” has become a board-level risk, capable of disrupting care delivery, compromising sensitive data, and jeopardising business continuity.
Against this backdrop, the sector has made remarkable progress. Five years ago, only 13 percent of social care providers had completed the Data Security and Protection Toolkit (DSPT). Today, that figure has risen to more than 75 percent. This shift shows a growing recognition that cyber security isn’t optional – it is foundational to safe, high-quality care.
At Digital Care Hub, we’ve learned that providers don’t struggle with willingness; they struggle with capacity. Many care organisations simply don’t have the time or expertise to produce robust cyber and data protection policies from scratch. That’s why one of the most transformative tools we’ve developed has been our Data Policy Builder. It allows providers to create clear, compliant, tailored policies, giving them a practical starting point for good governance and DSPT completion. For many services, it’s the difference between feeling overwhelmed and feeling in control.

But compliance is only the beginning. The next challenge for the sector is building true cyber resilience – moving from “ticking the box” to embedding safe digital practice into everyday operations. That means regular staff training, clear incident response plans, secure access controls, and awareness of evolving scams and threats. It also means understanding your digital supply chain and ensuring partners meet appropriate standards.
The renewed government funding for Better Security, Better Care through to 2029 signals a long-term commitment to these priorities. It will support new voluntary cyber and data health checks, help providers navigate upcoming DSPT enhancements, and strengthen local support networks that have been vital in driving progress so far.
But ultimately, resilience will be built provider by provider, through small, consistent improvements: policies that are actually used, staff who know what to do when something looks suspicious, and leaders who recognise that cyber security is now as essential to safe care as medication management or safeguarding.
Social care has already proven how quickly it can rise to a digital challenge. The next four years offer an opportunity to turn that momentum into lasting, sector-wide confidence.
For further information please visit https://digitalcarehub.co.uk/cyber-security
Restrictive practices such as physical restraint, bed rails, or lap belts remain one of the most challenging aspects of health and social care. Intended to keep patients safe, they can also cause harm, distress, and loss of dignity when used unnecessarily. Across the UK, the principle is clear: care must always use the least restrictive option.
Legislation provides the framework, but culture and staff behaviour shape daily practice. Nurses, carers, and clinicians often make quick decisions balancing safety with autonomy. Without training, restrictive practices risk becoming routine. To change this, staff need better understanding of the human impact and confidence to use alternatives.

That’s where Restrictive Practice makes a difference. Developed through codesign workshops with patients and carers, this gamified e-resource gives a voice to those most affected by restraint. Their lived experiences shaped the learning, helping staff see restraint
not as a neutral safety tool, but often as something frightening or disempowering. The results are powerful. Staff trained with the resource led Quality Improvement projects, achieving measurable reductions:
- Bed rails dropped from 360 to 277 incidents
- Bed bumpers from 303 to 227
- Lap belt use halved, from 46 to 22
These improvements represent safer, more compassionate care and reassurance for families.
Restrictive practices may never disappear entirely, but they should be the exception, not the rule. With the right knowledge and tools, staff can choose safer alternatives and build a culture of dignity, compassion, and respect across UK care services. See our advert on the front cover or visit www. RestrictivePractice.com


A recent Home Office action against Burlington Court Care Home highlights how easily care providers can fall foul of sponsor licence rules. Even small administrative oversights, such as failing to report a change in ownership, can have serious consequences for both employers and their overseas staff.
2025 IMMIGRATION CHANGES AND THE CARE SECTOR
While changes to the Immigration Rules are frequent (albeit not always groundbreaking), 2025 has shaped up to be a significant year for immigration changes, especially those aimed at the sponsored work sector. The need to reduce net migration continues to remain at the forefront of government policy making.
The Immigration White Paper, published in April, signalled the end was coming for those looking to make applications as care workers outside the NHS, along with several other jobs deemed to be of lower skill level (most roles below RQF level 6 - graduate level). The White Paper also introduced other suggestions to further tighten up the rules including increasing the required English levels and even the qualifying
period needed to reach settlement. Those in certain care worker roles had already been barred from being able to sponsor dependants and care worker sponsors faced extra scrutiny when applying for and assigning certificates of sponsorship.
In July 2025, some of the suggested amendments were implemented so that now only those who were already being sponsored in certain care roles or have lawfully been working with their employer for at least three months can apply for further permission as Skilled Workers. There is now a complete ban on recruiting new care workers from abroad. With many care worker sponsors having had their licences revoked in the last few years, there is already a large pool of workers who are at risk of having their leave curtailed. It is clear from changes made in 2024 that the government has been keen for existing sponsors to focus their recruitment efforts on these affected workers.
SPONSOR LICENCE COMPLIANCE: CHANGE OF OWNERSHIP RISKS
Change of ownership has long been one of the biggest pitfalls for those holding a sponsor licence. It catches out both large corporations and small businesses alike. A sponsor may have all the necessary dayto-day policies in place for monitoring workers yet still fail to recognise the need for a new licence or transfer when there is a majority change in ownership. Often there is no change to the operational activities of the company nor the workers’ terms of employment, so sponsors blindly carry on without even considering the need for this to be reported to the Home Office.
It was this exact scenario that Glasgow’s Burlington Court Care Home found itself in. There had been a change in majority ownership of
By Natasha Willett, Partner, Latitude Law (https://latitudelaw.com)
the company, and the workers had been transferred to the new employer under UK TUPE rules. Such action would prompt a new sponsor licence application, or transfer to the purchasing company’s sponsor licence, to be made within 20 working days of the transfer. Requesting that the existing sponsored workers have their sponsorship transferred is part of this process. It is understood that 15 sponsored workers have been affected by this change and face having their current permission curtailed for what, on the face of it, appears to be an administrative oversight. The Home Office has always taken the view that sponsorship is a privilege not a right and tends not to offer much flexibility or discretion when compliance duties are not adhered to.
COMMON REPORTING PITFALLS
Even in cases where there is a change in minority ownership, it is still something which must be reported to the Home Office. Failure to report changes in company name and address are also routine acts which could result in compliance action being taken against a licence holder if not reported. Reporting failures have seemingly become so frequent that is has recently prompted the Home Office to issue a notice on its SMS message board to remind licence holders to regularly review and update details, including those for Key Personnel. Failing to change or deactivate Key Personnel when they leave a business is another common issue we see at Latitude Law.
KEY TAKEAWAY FOR CARE PROVIDERS
The action taken against Burlington Court Care Home serves as a reminder to sponsors that if any changes occur – whether it be to the business or to a worker’s personal circumstances – this will probably require a report to the Home Office to stay compliant.
Competency assessment might not be anyone’s favourite phrase, but in domiciliary, residential, and specialist care, it is the backbone of safe, high-quality support. The challenge is making it genuinely useful, not just another hoop to jump through.
Care staff need more than theory. They need time to learn, practise, and make mistakes in a safe environment before they are expected to apply new skills with real people. That is where a blended learning approach truly shines. High quality eLearning builds consistent knowledge. Virtual sessions keep teams connected and engaged. Face to face training gives carers the chance to try techniques, ask questions, and build confidence before working directly with residents
and service users in their homes or care settings.
But learning does not stop in the classroom. Competency assessments in real care environments provide the feedback carers need to know they are using best practice techniques, communicating well, and delivering safe, person-centred care. It is the bridge between “I know it” and “I can do it.”
This balance of learning plus real world assessment creates confident, capable staff who trust their own skills and feel supported rather than judged. Managers also get clear, reliable evidence for CQC and Skills for Care requirements without drowning in admin.
At myAko, we have developed tools with our long term partners,
that make this process simple and sustainable. Better learning, better practice, better competency. It is a straightforward formula that leads to stronger teams and better outcomes for residents and service users.
Because when staff feel skilled, supported, and confident, the quality of care speaks for itself.

Kevin Ashley Founder I CEO myAko https://www.myako.online/




"23 years, operating 4 Devon Nursing homes, has been pretty tough, as anyone in social care, knows, only too well. And if it was hard already, after 2024 budget, it's just got harder.
Anyway, at heart, I am just customer of Eden Alternative, and it was a stroke of luck to come across this whilst on holiday in New Zealand in 2009. It started in USA in 1994 and now runs in 22 countries.
The fact that I am now involved with this not-for-profit organisation (in the UK area) came about when one of the 2 main UK directors died suddenly just before Covid. But it's something I have run with for 11 years to help make 'vision' a reality, not a struggle. So, being both a customer and helping the admin seems quite natural.
It is a modern philosophy of care, but moreover, it's a programme that is straight forward, tried and tested for 30 years and really works.

Its member care organisations generally become trainers for their own teams, and run it themselves.
The programme is run in person over 2-3 days or online 1 hr a wk for 7 weeks. You choose.
It addresses loneliness, helplessness and boredom and operates through 10 principles to underpin 7 critical domains of wellbeing.
Moreover, it's effective, transformational and really works. As residents, and team members wellbeing, matter so much , it's a must, in my opinion.
Geoffrey Cox
Southernhealthcare.co.uk
eden-alternative.co.uk"
In today’s regulated care environment, having clear, current, and wellcommunicated health and social care policies is essential for delivering safe, compliant services. The Care Quality Commission (CQC) now places increasing emphasis on how policies are implemented and understood—especially during registration and inspections.
Outdated or poorly communicated policies can significantly impact your CQC rating. Even if documentation is comprehensive, failure to ensure staff understand and follow procedures may lead to a “Requires Improvement” or even “Inadequate” rating under the ‘Effective’ domain.
Well-maintained policies promote consistent standards across care teams and help safeguard services when incidents arise. In regulatory investigations, the first request is often to review relevant policies—making accuracy and accessibility key to reducing legal and compliance risks.

However, keeping policies up to date is challenging. Constant changes in legislation, best practice guid-
ance, and case law mean that policies can quickly become obsolete.
W&P has been a trusted provider of CQC-ready care policies and procedures for over 20 years. Our expert team monitors industry developments to ensure your policies remain fully compliant.
Our Online Policy Portal simplifies policy management. With just a few clicks, providers can update content, distribute documents to staff, track confirmations, and monitor compliance via a real-time dashboard. You can even provide temporary read-only access to inspectors—demonstrating transparency and accountability instantly.
Ensure your care service meets CQC expectations with fully up-to-date, easily accessible, and well-communicated policies.
Email: info@wandptraining.co.uk
Call: 01305 767104
See the advert on page 2 for details.
Global assists clients throughout the U.K. who specialise in the healthcare sector to achieve their objectives of purchase, development and refinance.
We have organised over £1.8bn for clients in the past 30 years, providing clients with competitively priced funding to refinance existing debt, ease cashflow and develop businesses further.

From helping clients make their first purchase through to allowing groups to grow significantly in size we assist at every stage of your business expansion. Every proposal is individual and deserves to be treated that way, so we hope you will allow us to be of assistance to you and call us to chat through your plans and requirements, I am sure we will be able to tailor a facility to your requirements.