As our lead story details, recent polling data reveals the complex public mood around immigration.
Half of the British public, according to an IPOS poll see immigration levels as a concern, with three in ten naming it as the single biggest issue facing the country, particularly regarding illegal migration.
Given those numbers, these are legitimate concerns that deserve to be heard.
However, the dramatic decline in overseas care worker applications raises serious questions about whether we are addressing one problem whilst creating another, potentially more damaging crisis in our care sector.
The numbers tell a stark story. Health and care worker visas granted to care workers have plummeted by 81% in the past year, falling from 27,941 to just 5,189. Following the outright ban on recruiting care workers from overseas that came into effect in July 2025, only 303 visas were granted in the July-September quarter.
This sharp restriction comes at precisely the wrong time. Analysis from Age UK a year ago found that 2 million older people in England are now living with some unmet need for social care. These are not abstract statistics but real people struggling with daily tasks such as getting out of bed, washing, and dressing without adequate support.
We cannot, on one hand, express genuine concerns about our ageing population and the care crisis, whilst simultaneously restricting the workers who have been filling critical gaps in our workforce.
International staff have been instrumental in driving down vacancy rates from a high of 10.5% in 2022 to 7% in 2025, and many providers have relied on overseas recruitment as a lifeline in recent years.
It is entirely commendable that the government wishes to train our domestic workforce and encourage British workers into the sector.
Fair pay agreements, better sick pay, and guaranteed hours of work through the Employment Rights Bill are positive steps that should make care work more attractive.
However, these initiatives require time to bear fruit. The transition must be phased in with a more balanced approach that acknowledges the immediate realities facing care providers.
The sudden closure of international recruitment without sufficient domestic capacity
in place risks creating what one analyst described as a "vicious cycle" where older people end up in hospital for avoidable reasons, then remain stuck waiting for care packages whilst their health declines.
The impact of these workforce restrictions is compounded by what former Deputy Prime Minister Damian Green described as the Chancellor's "silence on social care" in the recent Autumn Budget.
Social care's complete omission from Rachel Reeves' Budget, as detailed in our report on the Westminster panel discussion, (see page 5) spoke volumes about the government's priorities. One provider described it simply as a "missed opportunity."
Green noted that if there had been any good news for the sector, the Chancellor would have been "trumpeting it." Instead, the absence underscored social care's status as the UK's "silent public service," whilst providers face rising costs from employer National Insurance increases, National Living Wage rises, and various property and vehicle taxes.
The subsequent fallout regarding the so-called "black hole" in public finances adds another dimension to this frustration. Observers have challenged the narrative around the fiscal gap, with the Office for Budget Responsibility declining to legitimise the £22 billion figure repeatedly cited by ministers.
If, as some observers suggest, the severity of the black hole was overstated, this raises a crucial question: where should that money be redirected? Social care providers and the vulnerable people they serve have a strong claim to those resources.
The sector needs more than warm words about future workforce strategies. It needs immediate, practical support to maintain service provision whilst longer-term reforms take effect.
Without a balanced approach that combines domestic workforce development with continued, carefully managed international recruitment during this transition period, we risk a care crisis that will harm the most vulnerable members of our society.
The government must recognise that immigration policy cannot be developed in isolation from workforce planning. When it comes to social care, these policies have real and immediate consequences for older and disabled people who depend on these services to maintain their dignity and independence.
I would encourage our readers to sign up for our bi-weekly digital newsletter at www.thecareruk.com and follow us on social media for all the latest news.
The Carer is published by RBC Publishing Ltd, 3 Carlton Mount, 2 Cranborne Road, Bournemouth, Dorset BH2 5BR.
I can always be contacted at editor@thecareruk.com
damage. Views expressed within this publication are not necessarily those of the publisher or the editorial team.
responsibility for any effects, errors or omissions therefrom. All rights reserved, reproduction is forbidden unless

(CONTINUED FROM FRONT COVER)
Total work visa grants to main applicants stood at 175,143 for the most recent twelve-month period, representing a 27% decrease compared to the preceding year. This contraction follows enhanced regulatory oversight of sector employers, enforcement measures by the Home Office, and multiple policy adjustments implemented during 2024 and 2025.
SECTOR-SPECIFIC DECLINES
Certain occupational categories experienced particularly pronounced reductions. Caring Personal Service positions saw an 81% fall, with just 5,188 visas granted. Nursing Professionals experienced a 79% decline, with 2,225 visas issued during the period.
The Department of Health and Social Care attributes the nursing visa reduction to the conclusion of the centrally coordinated international recruitment initiative and shifting requirements for internationally qualified personnel.
SKILLED WORKER ROUTE
The broader Skilled Worker visa category also recorded substantial decreases, with grants to principal applicants falling 46% below 2023 levels. Contributing factors include fewer applications being submitted, lower approval rates, and elevated skill requirements that took effect in July 2025, removing more than 100 occupations from the eligible sponsor list.
The initial policy shift occurred in March 2024 under the previous Conservative administration, which prohibited care workers from bringing family dependants and barred organisations not registered with the Care Quality Commission from sponsoring employees.
This change produced immediate effects. Visa grants dropped from 20,439 between October and December 2023 to merely 3,432 in the January to March 2024 quarter, falling further to 1,575 in the April to June 2024 period.
GOVERNMENT MEASURES
Following the general election, the Labour government introduced additional restrictions from April 2025. English care providers must now prioritise recruiting from international workers already residing in the UK who have lost their sponsorship arrangements before seeking staff from overseas.
This requirement produced further declines, with visa grants falling from 1,784 in the first quarter of 2025 to 1,063 in the second quarter.
“HUGE
Nuffield Trust Researcher, Cyril Lobont said: "Social care has been entirely reliant on recruitment of nonUK nationals to meet growing demand, with the number of British nationals working in the sector falling in recent years. The large drop in immigration numbers, especially for work, we see today will likely mean far fewer care workers entering the country, with huge consequences for the fragile care sector.
“Already, the restriction on care workers bringing family members to the UK is having a major impact. Health and Social Care Worker visas were once the main source of overseas social care workers, but the number of visas being granted has now fallen to close to zero.
“The government intends to account for this by attracting more domestic recruits into the sector through its Fair Pay Agreement for adult social care. However, this won't take effect until 2028 and the £500 million
pledged for the first year of implementation is far from what is needed to drive an influx of British nationals into this vital sector.
"When immigration policy is implemented suddenly without proper coordination across government and with little regard for the impact on essential care services, changes can come in at speed, but the problems they create then take years to fix.”
Matthew Taylor, chief executive of the NHS Confederation, said: “Many members of the public are likely to welcome this sharp fall in net migration. Recent IPSOS polling shows that half of the public see immigration levels as a concern, with three in ten naming it as the single biggest issue facing the country, particularly in relation to illegal migration.
“However, this reduction has been driven largely by fewer non-EU nationals arriving for work and study. If this trend continues, it could create serious challenges for how vital public services, including the NHS, are delivered in the future.
“While efforts to boost domestic recruitment are essential, the reality is that the NHS and social care continue to face significant workforce pressures. Migration has historically played a crucial role in meeting these challenges. Today, around one in five NHS workers in England hold a non-British nationality, underlining the international make-up of a workforce we value greatly.
“Given what we know about population trends and the growing health and care needs of our communities, we need a more balanced and informed conversation about the migration our country requires. This should include strengthening the Skilled Worker visa route for health and care professionals so that we can sustain future labour markets and protect the services people rely on.”
While new arrivals have decreased significantly, visa extensions for workers already in the country on work routes have increased. Work-related extensions rose 16% in the year to September 2025, including a 22% increase for Health and Care Workers and a 15% rise for Skilled Workers.
The Home Office indicates these figures reflect substantial numbers of workers who arrived in earlier years now reaching the stage where they must apply to extend their permission to remain in the United Kingdom.
Last month a care provider reversed its own visa policy following a campaign by the GMB Union.
The provider had initially announced plans to sponsor only those staff members deemed 'business critical', placing approximately three thousand care workers at risk of being unable to renew their visas.
However, following widespread concern from staff and union representatives, the organisation has now confirmed it will sponsor any current employee who meets Government immigration criteria.
The GMB union, which organised a petition that attracted more than 700 signatures opposing the original policy, welcomed the reversal.
Will Dalton, GMB National Officer, commented: "The initial visa change would have forced out thousands of loyal, experienced care workers. It would have completely devalued professionals who have shown years of dedication to residents.
"Now, they can sleep easy. We've got to congratulate the company for rethinking; they're going to value quality over quantity and bring confidence to migrant workers dedicated to providing care."

Article by Gill McAteer, director of employment law at Citation (www.citation.co.uk)

In the previous year the total number of vacant posts within the adult social care sector was 111,000. While this figure may show signs of positive growth compared to last year’s figure (which was 12.4% higher), it still indicates a dramatic gap in terms of resource, which indicates a potential issue around employee wellbeing for those active in the sector.
Stress and other ill-health can be major obstacles for care firms in recruiting and retaining employees.
The Chartered Institute of Personnel and Development (CIPD) found that one of the leading causes of long-term absences is mental health issues (29%) with the care sector experiencing some of the highest absence rates generally.
Investing in your approach to people management is a good way to support employee wellbeing, and therefore retention, and it doesn’t need to mean dramatic changes, it can start with easy to implement policies and procedures.
You may already have processes in place to support employee wellbeing, such as line manager meetings and monitoring working patterns to prevent excessive overtime, but it isn’t enough for them to just be in place, managers and leaders within your business need to be proactively signposting to them. Employees often won’t seek out support themselves, especially if they’re overstretched or have been with the businesses for a while and haven’t been reminded of available support.
Consistent reminders of what’s available will help employees feel looked after and encouraging regular
feedback as to whether the support offered is valuable, or if there is anything else that would be useful, ensures employees have a voice.
Staff shortages may put workers off taking leave, so it’s important to keep an eye on this and introduce a system to ensure that employees take regular breaks to avoid burnout. This is particularly important if your business provides rolled up holiday pay for irregular hours and part-year workers, as this could be an incentive for workers to not take as much time off and instead choose to bank the accumulated holiday pay. Wellbeing isn’t just coping with the bad but also celebrating the good. It can be just as damaging for employees who are thriving to feel underappreciated as those who are struggling. So, an increased focus on wellbeing should include celebrating both personal and professional achievements, demonstrating that people can bring their whole selves to work. Sharing positive feedback widely and proudly is a great starting point.
Managers play a key part in supporting wellbeing, but they may not have the training they need to do this effectively and spot the signs that someone on their team is struggling. Managers need training in relation to a variety of topics that they might encounter with employees, this could cover:
• Personal issues outside of work
• Dealing with the loss of service user
• Grievances with colleagues
Employees need a clear and reliable process for escalating any concerns or frustrations they have to prevent them from snowballing. This means managers need guidance on advice they can offer, including up to date information on both internal and external services on offer to help facilitate these delicate conversations or signpost in the right direction. This could be in the form of an Employee Assistance Programme where they may feel more comfortable discussing matters affecting their wellbeing with an independent professional.
It seems that the care sector will continue to face long-term recruitment and retention challenges - it is projected that 470,000 new posts will be needed by 2040 to keep up with population growth and aging. There’s no time like the present to put visible, robust and proactive wellbeing measures in place to support employees who are feeling the pressures the sector is experiencing.
Residents and colleagues at HC-One’s Altham Court Care Home in Lincoln, Lincolnshire welcomed Hamish Falconer, MP for Lincoln and Parliamentary Under-Secretary at the Foreign, Commonwealth and Development Office, for a special visit on Friday 28th November as part of UK Parliament Week.
The visit offered Mr Falconer the opportunity to explore Altham Court’s welcoming and modern facilities, including the hobby room, quiet room, hair salon, café, and beautiful gardens, while meeting residents and learning about daily life at the 46-bed home, which provides both nursing and residential care.
During his time at the home, Mr Falconer enjoyed conversations with residents and colleagues, hearing first-hand about their experiences, community involvement, and the dedicated care provided by the Altham Court team. The visit reinforced the home’s ongoing commitment to creating meaningful community connections and maintaining a warm, inclusive environment for all who live and work there.
UK Parliament Week, celebrated annually, encourages communities

Pet therapy has become a part of the everyday routine in many care homes in the UK. The positive impact animals can have on the well-being of residents is well documented. But bringing animals into a care setting brings its own problems. It can be expensive and disruptive, they can be temperamental, and even the cleanest pets raise hygiene issues.
V-Thera virtual pets allow you to offer all the fun and engagement of a real pet, but in a clean, predictable and flexible way that fits in perfectly with your care home routine.
VIRTUAL PETS, REAL BENEFITS
From the moment the resident first puts the headset on, they are engaged and delighted as the pet sits, lies down, rolls over and feeds on command. They can even throw a ball for the pet to fetch. The experience is involving, relaxing and stimulating, enhancing a positive mood while encouraging movement and communication.
The pets themselves are wonderfully realistic, not just in the way they look, but in how they act. There are four dogs to choose from, and there’s even a moggie for cat lovers. They respond to voice or hand commands, or to big buttons on the screen. It’s ideal for previous pet owners, but also people nervous of animals.
TECHNOLOGY THAT CARES
V-Thera uses the latest Japanese mixed reality technology, meaning the virtual pet appears in the real-world, viewed through the headset. Seeing the
across the UK to engage with the democratic process and learn how Parliament influences everyday life. Altham Court’s participation in the week gave residents a valuable opportunity to connect with their local MP and share their views on local and national issues.
Anna Livsey, Home Manager at Altham Court Care Home, said: “It was a wonderful experience having Hamish Falconer visit Altham Court and see life in our home firsthand.
Our residents really enjoyed the opportunity to share their stories and ask questions about Parliament and local issues. Visits like this mean so much to everyone, they help our residents feel heard and connected to the wider world.”
Hamish Falconer, MP for Lincoln, commented: “Thank you to everyone at Altham Court for such a warm welcome. It’s always a pleasure to return, and I was delighted to see the residents and staff taking part in UK Parliament Week. Their enthusiasm for public life and community engagement is genuinely uplifting, and I’m grateful for the vital work the team does every day.”
familiar surroundings of their care home lounge reduces any sense of anxiety or disorientation for residents. The app can also be used lying down, so it can be used in bedrooms.
The technology itself is completely intuitive, designed for people with no experience of gaming. The headset reads hand movements, so there is no need for hand controls after set-up. Setting the app up is easy and quick for staff, with no training required. It comes preloaded onto the latest Quest 3s headset, so it’s a simple matter of staff switching the headset on, selecting the V-Thera icon, selecting the dog – which you can name – then transferring the headset to the resident. They are immediately immersed in playing with the dog or cat.

The makers recommend sessions of up to ten minutes at a time, it’s very easy to accommodate the technology into the life of the home, and for staff it can create an excellent opportunity to bond with residents. A sharing function even means the sessions can be cast to other screens so all residents can share the experience.
The potential of new technologies like V-Thera for engaging with residents in a positive way points to an exciting future. The combination of advanced Mixed Reality with intuitive and thoughtful design means care homes can adopt the latest technology without disrupting the care routines already in place.
V-Thera was created in Japan by Remedy & Co and is available now in the UK through Care Activity Ltd. Managing Director Alison Lang says, “The minute we saw V-Thera, it was clear to us that this was an exciting innovation, a new way to offer something genuinely engaging to care home residents. The pets are fun, realistic and always ready to play. It is technology that brings care to life.”
Contact alison@careactivityxr.com www.careactivityxr.com
Social care’s total omission from Rachel Reeves’ Autumn Budget “spoke volumes about the Government’s priorities”, former Deputy Prime Minister Damian Green has warned, arguing that the sector has once again been overlooked despite escalating pressures.
Speaking at a Westminster panel discussion the morning after the Budget, Green criticised the Chancellor’s failure to reference social care at all, saying that “if there had been any good news for the sector, the Chancellor would have been trumpeting it”. Instead, he said, the absence underscored social care’s status as the UK’s “silent public service”.
The panel, brought together by Bridgehead Communications to explore the Budget’s implications for the sector, brought together more than 50 care leaders, investors and policymakers, who collectively warned that the Government’s smorgasbord of tax announcements will hit providers and selffunders in an already beleaguered sector landscape.

Panel Chair and Bridgehead Communications Managing Director William Walter set out the fiscal landscape bluntly: “Employer NICs – up. National Living Wage – up. Local authority borrowing – up. Council taxes – up. Property taxes – up. Savings taxes – up. Inheritance taxes – up. Across the board, costs are rising, squeezing care providers and self-funders alike.”
His assessment drew agreement from the rest of the panel, who consistently returned to a recurring theme: the Autumn Budget may not mention social care by name, but its pressures will hit the sector hard.
TAX PRESSURES AND WARNING SIGNS
Speakers warned that rising business costs, driven by tax increases on vehicles that have a considerable effect on rural domiciliary care providers, and on properties over £2 million, the so-called ‘mansion tax’, alongside the latest minimum wage rise, would compound existing instability in the social care sector.
Clare Connell, CEO of Connell Consulting, captured this sentiment in her description of the Labour Government’s recent budget as a repeat of the 1970s: “This Budget reads as though Rachel Reeves and her Treasury mandarins have pulled down a well-thumbed playbook from the 1970s. Dennis Healey showed how tax-and-spend economics ultimately chokes growth and ends in crisis, while Michael Foot proved that artificial job creation without productivity only fuels inflation and instability. Despite all of this, Rachel Reeves, in her infinite wisdom, appears determined to revisit both mistakes at once.”
Offering an alternative to the repeatedly stalled reform agenda, LaingBuisson Founder and Executive Director William Laing outlined a proposal known as the Personal Asset Protection Guarantee, informally described as a “Dilnot Lite” model. Under the system, the state would step in once individuals had spent down a percentage of their assets, protecting households across income brackets while maintaining private care capacity and operating similar to an insurance scheme.
Bringing an international investment lens to this matter, Andrea Auteri, Co-Founder and Managing Director of Elevation Advisors, reminded the room that capital is global and “global capital has a choice”. Investors go where there is “stability and predictability”, conditions that the UK consistently struggles to provide – “the issue with the UK is that it is always thinking six-months ahead”. As a result, sectors such as social care are faced with repeated, ad-hoc tax changes that undermine the confidence required for a long-term pipeline of care investment.
WORKFORCE PRESSURES AND MIGRATION POLICY
The panel’s discussion on the announced minimum wage hike tied in to the Labour Government’s recent overhaul of the legal migration system, presenting further restrictions to an already strained care workforce. One attendee, a small Cornish care provider, reflected on the post-Brexit departure of EU nationals from
the care sector, commenting that the lack of accurate data creates challenges for workforce planning.
Holding a similar sentiment, a representative from Curaa Group, described the Budget as “incredibly depressing”, combined with the government’s migration policy which he viewed as a “knee jerk reaction” to popular political sentiment rather than what was required for policy.
Laing suggested that modest reforms to the benefits system could help maintain support for those who need it while encouraging more people to enter the sector and Andrea Auteri argued that the Government could elevate the profession “to the dignifying level it deserves,” for instance, by lowering tuition costs, similar to the approach taken for nursing education.
Further contributing to this debate, one attendee from The King’s Fund stressed that in the current climate, no political party is likely to prioritise care workforce needs over migration targets. He questioned how the sector can make itself more attractive to potential workers, noting that many make the rational choice to pursue employment in other fields, such as supermarkets, where pay is competitive and working conditions are less physically and emotionally demanding.
Having been absent from the Budget, social care’s future requires cross-departmental coordination. “This was clearly a Budget for the backbenchers,” he said, noting that while markets have remained calm, meaningful reform is unlikely without a catalysing crisis.
Reflecting on local authority funding in this regard, Green stressed that the sector cannot sustainably be financed locally: “In the long run it is impossible to fund adult social care through local authorities … we should abolish the fiction [that social care can be funded locally] and say that this is a national service funded nationally.”
He also highlighted the persistent clash between local authority and NHS budgets, noting that Integrated Care Boards “should have solved” these imbalances, “but it clearly hasn’t worked,” leaving social care underrepresented in planning and resource allocation.
In regard to this, during the Q&A segment of the panel, a provider asked whether taking the funding responsibility away from local authorities would address these imbalances. Green emphasised that the local government sector remains deeply immersed in devolution reform and “extremely patchy across the country,” reinforcing the argument for national funding of adult social care.
Overall, the panel painted a picture of a sector facing rising costs and tightening workforce pressures, all without a clear plan from the Government. With social care absent from the Budget entirely, speakers warned that without national leadership and long-term funding reform, the system risks drifting further into crisis.
Commenting on the event, William Walter, Managing Director of Bridgehead Communications and Chair of the panel discussion, said: “It was refreshing to see such frank discussion across the panel and audience. It is vital that we build a credible vision for care, one that aligns workforce policy with demand and stabilises funding at a national level.
“What came through clearly today is that, for too long, successive governments have prioritised healthcare and the NHS over social care. This Labour Government is no exception, and the continued absence of a viable, long-term funding solution means the silent crisis in social care will only deepen.
“What is needed now is the political drive to change that. We at Bridgehead are proud to continue bringing together policymakers, providers and investors to help shape the long-term reforms the sector so urgently needs.”

The Care Quality Commission (CQC) remains ‘sedentary’ in its approach, despite a new regulatory regime promising a more ‘dynamic’ assessment of its services.
The latest figures show that physical inspections have dropped from a peak of almost 23,000 in 2016, to less than 4,500 inspections conducted so far in 2025. Current figures remain lower than pre-lockdown levels (17,671 in 2019 and 7,711 in 2020), with regulatory action also falling.
According to data obtained by law firm Pannone Corporate under the Freedom of Information Act, the total number of regulatory actions taken by the Commission has decreased year-on-year and recently sat at around half of pre-lockdown levels.
Despite an obvious drop-off in the number of regulatory actions taken in 2020, figures have remained consistently low ever since, between 35,000 per year compared with upwards of 15,000 each year in the period following the CQC’s receipt of enhanced powers in 2015. The use of Warning Notices has also dropped year-on-year since 2022, currently sitting at 98.

Bill Dunkerley, associate partner at Pannone Corporate, commented: “The Care Quality Commission’s new regulatory model has been in place for some time but, despite the fanfare, it could be said to have had something of an inauspicious start.
“How the introduction of a single assessment framework differs, in practice, from the previous assessment models, is questionable. Likewise, whilst in its promotional material the CQC was hopeful that its new approach would enable it to be more dynamic in its assessment of services, and permit more contemporaneous data collection to take place, the extent to which it has achieved these objectives remains to be seen.”
He added: “Far from becoming a more proactive, dynamic and responsive agency, the CQC remains rela-
tively sedentary in its approach. That being said, there are perhaps early indicators that this consolidation of activity is perhaps the forerunner to a renewed and re-focussed CQC, which is not afraid to utilise the full range of statutory powers at its disposal.”
The figures show that the number of times registrations have been cancelled, fixed penalties issued and conditions imposed have remained fairly consistent since the CQC obtained its additional powers in 2015.
The data obtained by Pannone also reveals that there are currently 101 open criminal investigations concerning specific incidents or unregistered providers, and the number of prosecutions brought does appear to be slowly on the increase, with 10 prosecutions being concluded in 2024, and seven so far during 2025. The majority of prosecutions, by far, are brought under Regulation 12 – failure to provide safe care and treatment.
The average fine following prosecution by the CQC is just shy of £102,000, with average prosecution costs being in the region of £12,500. This represents a slight decrease from previous years.
Dunkerley said: “As made clear in the latest State of Care report, the CQC has stated its intention of, “taking action to protect people from poor care”. This mindset is perhaps indicative of a more bullish approach by the Commission, as it becomes accustomed to its new operating model and starts to subject to increasing scrutiny those providers who are not meeting the required standards.
“However, to be an effective regulator going forwards, and one with real teeth, the CQC has to combine its new inspection and assessment framework with meaningful regulatory activity. Whilst the CQC’s recently stated aim is to protect people requiring of care, to be effective it must fully embrace the powers at its disposal. The latest figures are perhaps indicative of that mindset, but only time will tell whether this trend and pattern of behaviour continues.”
Hazel Lodge care home in Battle recently presented local charity Drawing Life with a cheque for £1,000 to help them continue with art sessions in Hastings Contemporary and De La Warr Pavilion.
The sessions which are free to attend give everyone an hour to get lost in a creative activity, the chance to meet others in similar situations and enjoy some clarity and company.
Residents from Hazel Lodge visited one of the art sessions held at Hastings Contemporary Art Gallery and after taking part in the drawing class presented the cheque to Drawing Life founder and artist, Judy Parkinson.


Welcome to Blue Rain - our activity store
on over 14 years
Judy said “On behalf of carers and those they care for we are very grateful for Barchester’s generous donation which will help us continue our work into 2026.
Drawing Life launched a decade ago offering art to people living with dementia, and we soon realised that carers gained as much as the people they cared
“It’s fun,” said Lou, wife and carer for Brian with dementia who attend the monthly sessions together, “A genuine art experience and an hour when the job of caring is lifted.”


•
and
• They can be bought as seen or refurbished and sign-written to your own requirements.
• Fully serviced, new mot & warranty
• Engineers inspection supplied if required.
•


Care home operators across the UK will need to prepare for changes to employment law after the Government announced significant revisions to its Employment Rights Bill this week.
The legislation, which has been progressing through Parliament, will now require employees to complete a six-month probationary period before gaining full protection against unfair dismissal claims. This represents a compromise position between the Government’s original proposal and existing employment law.
Under current regulations, workers must remain with an employer for two years before they can bring unfair dismissal claims to an employment tribunal. The new six-month threshold marks a substantial reduction in this qualifying period, though it falls short of the immediate protection initially envisaged.
The Department for Business and Trade confirmed the policy shift following extensive discussions between trade union representatives and business groups. Officials indicated that the revised framework aims to balance worker protections with operational flexibility for employers.

Employers should, however, note that existing first-day protections against discrimination and automati-
cally unfair dismissal grounds remain unchanged. These safeguards, which cover issues such as pregnancy, whistleblowing, and protected characteristics, will continue from the first day of employment.
The Government has also pledged that any future changes to the six-month qualifying period must be made through primary legislation, providing certainty for employers planning their human resources policies. Additionally, the compensation cap for unfair dismissal claims will be lifted under the new arrangements.
The Bill had encountered resistance in the House of Lords, where peers raised concerns about multiple provisions, including proposals affecting zero-hours contracts. The Government’s decision to modify the unfair dismissal provisions forms part of efforts to ensure the legislation completes its parliamentary journey according to the published timetable.
Business department officials described the six-month qualifying period as “a workable package” that emerged from collaborative discussions between stakeholders. The Government maintains that millions of workers will benefit from enhanced employment rights while employers gain greater clarity about their obligations.
A widely-used diabetes and weight-loss medication has failed to slow cognitive decline in people with early Alzheimer’s disease, pharmaceutical company Novo Nordisk has announced.
The company’s study tested semaglutide – sold under the brand names Ozempic and Wegovy – in people with mild cognitive impairment or mild dementia caused by Alzheimer’s disease. Despite hopes that the drug might protect brain function, trial results showed no significant benefit compared to those who did not receive the medication.
Dr Susan Kohlhaas, Executive Director of Research and Partnerships at Alzheimer’s Research UK, described the news as “disappointing” for those affected by the condition.
“These trial results are another reminder that Alzheimer’s is driven by several different biological processes. No single approach is likely to be enough,” Dr Kohlhaas said. “The field now needs to focus on understanding those processes in much greater detail and developing treatments that can be used together to tackle the disease from multiple angles.”
WHAT THE STUDY INVOLVED
The EVOKE phase 3 trial enrolled participants aged 55 to 85 who showed signs of amyloid protein in their brains – a hallmark of Alzheimer’s disease. A separate group, called EVOKE+, included people whose brain scans also revealed blood vessel damage alongside amyloid buildup. In both groups, semaglutide failed to slow the rate of cognitive decline.
The medication, known as a GLP-1 receptor agonist, is primarily prescribed to manage type 2 diabetes and aid weight loss by reducing appetite, slowing digestion, and improving blood sugar control.
Earlier research had suggested people taking GLP-1 medications for diabetes appeared to have a lower risk of developing dementia, raising hopes the drug might offer protective benefits. However, the EVOKE trial results have not supported this theory.
Full trial findings are expected to be presented at the Clinical Trials in Alzheimer’s Disease conference in December and await publication in a peer-reviewed journal.
LOOKING AHEAD
Despite the setback, experts believe valuable lessons can be learned. Dr Kohlhaas noted that the growing use of GLP-1 medicines through private prescriptions for weight loss presents an opportunity to gather real-world data on their longer-term effects.
“Making full use of that information will help shape future research and strengthen the evidence base the field relies on,” she said.
Alzheimer’s treatment development requires a multi-pronged approach, including therapies that remove harmful brain proteins, protect brain cells from damage, and repair existing harm.
“People with Alzheimer’s urgently need better options, and this setback reinforces the need to invest in the science that can drive real progress towards a cure,” Dr Kohlhaas added.

By Lynne Turnbull, CEO of Disability Positive

The healthcare sector faces an unprecedented challenge: rising levels of ill-health and long term health problems are pushing more people out of work, creating barriers to economic growth, and exacerbating workforce shortages in a sector already under immense pressure. In response, the government is calling on employers to play a more active role in supporting disabled employees and those with long-term health conditions, moving beyond the NHS and creating a partnership between employers, employees, and health services.
Healthcare, as a demanding and often stressful sector, might appear an unlikely leader in this space. Yet it presents a unique opportunity to demonstrate the value of inclusive employment practices. By attracting and retaining talented individuals with lived experience of disability, organisations can not only broaden their talent pool but also build workplaces that are adaptable, resilient, and reflective of the communities they serve.
At Disability Positive, a Disabled People’s Organisation where over 75% of staff and volunteers have lived experience of disability or longterm health conditions, we have seen first-hand the benefits of a supportive, flexible working environment. Our approach prioritises
wellbeing and enables honest conversations, ensuring employees know where to access support and that their needs are understood. This includes embedding wellbeing into HR policies and offering practical measures such as flexible working arrangements, access to specialist advice, and signposting to additional resources.
The results speak for themselves. Disabled employees at Disability Positive do not take more time off sick, nor do medical appointments affect their performance compared to their non-disabled colleagues. When given the right support, disabled employees thrive, underscoring that capability and potential are not defined by disability.
These principles are particularly relevant in healthcare, where the physical and emotional demands of the sector can deter talented candidates with long-term health conditions. Yet by embedding inclusive practices into recruitment and retention strategies, organisations can access a committed workforce while improving morale, loyalty, and organisational performance.
Government initiatives, such as the Disability Confident scheme, offer practical support for employers. The scheme aims to encourage organisations to attract, recruit, and retain disabled employees. Disability Positive holds Disability Confident Leader (Level 3) accreditation and actively supports other organisations on this journey, demonstrating that structured guidance combined with lived experience expertise can create meaningful change.
Beyond recruitment, the government is exploring the collection of workplace health data and retention metrics for disabled employees. This step is crucial. Data allows employers to identify barriers, track progress, and hold themselves accountable for supporting employees with long-term health conditions. It also provides evidence to refine policies and make the business case for investment in workplace wellbeing initiatives.
One innovative approach in development is the ‘Vanguard’ scheme, which invites employers to trial new support models. Disabled People’s Organisations (DPOs) like ours can play a vital role in these trials, offering insight grounded in lived experience and expertise. However, many DPOs operate under stretched budgets and shrinking funding streams, meaning appropriate remuneration for their contribution is essential if they are to participate meaningfully. Without this, the sector risks missing the opportunity to fully leverage the expertise that DPOs bring.
Healthcare employers can take immediate steps to foster an inclusive environment. Start with flexible working policies, ensure line managers are trained in disability awareness, and embed wellbeing support into everyday operations. Importantly, create a culture where employees feel safe to disclose health conditions and seek adjustments without fear of stigma or career penalty. The business case is clear: inclusive employers gain access to a wider talent pool, retain staff longer, and often see higher engagement and performance.
Involvement in government-backed initiatives is also a chance to demonstrate leadership. By contributing to schemes like the Vanguards healthcare organisations can shape policy, refine best practice, and become examples of inclusion. Embedding the social model of disability, recognising that barriers arise from the environment and society, not the individual, is key to ensuring these initiatives are effective and sustainable.
The healthcare sector has an opportunity to lead by example. By embracing disability inclusion, organisations not only meet regulatory and ethical obligations but also improve workforce resilience and patient care. With government support, innovative policy trials, and the expertise of Disabled People’s Organisations, the sector can turn inclusivity into a strategic advantage, proving that when employees are supported to thrive, organisations do too.
The government has confirmed it will increase the thresholds used by the National Institute for Health and Care Excellence (NICE) when evaluating new medicines for NHS use, in a move designed to support the pharmaceutical sector and unlock innovation.
From April 2026, NICE will apply new cost-effectiveness thresholds of £25,000 to £35,000 per qualityadjusted life year (QALY), up from the current range of £20,000 to £30,000. The change follows government commitment to improve the operating environment for life sciences companies in the UK.
Dr Samantha Roberts, NICE chief executive, said: The organisation’s reputation for robust and transparent guidance would remain unchanged as it works with independent committees to apply the new thresholds. She emphasised that in a health service funded by general taxation, it was appropriate for government to decide on health spending levels.
NICE currently recommends approximately 91% of the medicines it evaluates—around 70 per year. Analysis suggests the increased threshold could enable NICE to recommend an additional three to five
new medicines or indications annually.
The assessments use QALYs to estimate health benefits, combining both length of life gained and quality of life improvements compared with existing treatments. For a medicine to be considered costeffective under current thresholds, it should typically generate one additional year of perfect health for no more than £20,000-£30,000 over the cost of current care.
The announcement also includes government support for a new value set for assessing health-related quality of life, based on public judgements of different health states. This will be introduced alongside the EQ-5D-5L measure following peer review and publication.
NICE will apply the threshold changes to new technology appraisals and those currently underway. Evaluations already in progress where treatments are deemed not cost-effective under current thresholds will be paused if the new thresholds could alter the outcome, then reconsidered once NICE has the regulatory power to apply the changes.
Saint Cecilia’s Care Group proudly celebrated the dedication, compassion and exemplary achievements of its care staff at the 3rd annual Saint Cecilia’s Care Awards, held on Friday 28th November. The evening brought together colleagues from across Scarborough, Whitby and Pickering, to honour those who have gone above and beyond in delivering exceptional care over the past year.
Hosted at a packed Scarborough Spa and led by the ever-entertaining ‘Big’ Ian Donaghy (for the 3rd time!), the event was given an extra touch of sparkle with special guest host Amy Garcia from BBC Look North. Amy delivered a warm, professional presentation and made a point of visiting every table to speak personally with staff, finalists and winners - a gesture deeply appreciated by everyone in attendance.
Saint Cecilia’s Care Group was also honoured to welcome distinguished guests, including the Mayor of Scarborough, Thomas Murray, and Scarborough MP, Alison Hume, both of whom took time to meet with staff and hear more about the vital care work carried out across the organisation. Their presence and words of encouragement were warmly received and added an important sense of civic recognition to the evening.

Mike Padgham, Saint Cecilia’s Group Chairman commented: "We were truly honoured to welcome the Mayor of Scarborough, Thomas Murray, and Scarborough MP, Alison Hume. Their presence not only added a special significance to the evening but also highlighted the importance of recognising and celebrating the incredible work of our care staff. We are grateful for their support and for taking the time to meet our teams, finalists, and winners - it made the night even more memorable for everyone involved."
The awards recognised excellence across a wide range of categories, celebrating both emerging talent and long-standing commitment. This year’s winners included:
Emerging Talent – Megan Leybourn
• Values Award – Angus Law
• Unsung Hero – Angie Macdougal
• Leadership Award – Tanya Wormald
• Team Leader Award – Carolyn McLoughlin
• Support Services Award – Sarah Roberts and Dawn Scholefield (Highly Commended: John Loughman)
• Nurse of the Year – Jennifer Mensah
• Inspirational Care Worker – Lucy Royds
• Long Service Awards – Jacie Whittaker (5 years), 'B' Methven, Mike Smith (10 years), Tanya Wormald (10 years), Dani Botelho (10 years), Isabel Santos (10 years), Stacy Cullen (15 years)
Each winner was applauded for their remarkable contributions to the wellbeing of residents and for embodying the values at the heart of Saint Cecilia’s Care Group.
A special thank you was also expressed to the companies who generously sponsored this year’s event, helping ensure the awards remained a meaningful and memorable celebration for all staff involved. Their support played a vital role in recognising the commitment and compassion of care workers across our homes.
In addition to celebrating staff achievements, the evening also raised vital funds for Dementia UK through a Golden Gamble raffle, generating over £1,000 to support the charity’s work. Saint Cecilia’s Care Group extends heartfelt thanks to everyone who contributed to this achievement.
Aaron Padgham, Managing Director of Saint Cecilia’s Care Group, said:
“Every year, we are inspired by the dedication and spirit of our teams, and this event is our opportunity to shine a light on the amazing work they do. Our staff are the heart of everything we do, and we are incredibly proud of each and every one of them.”
Saint Cecilia’s Care Group would also like to looks forward to continuing this growing tradition of recognition and celebration, as the group remains committed to delivering exceptional care to people across Scarborough, Whitby and Pickering.
Directors of adult social services have welcomed the Government’s commitment to neighbourhood health as a cornerstone of the NHS 10-year plan, but stressed that local authorities must be treated as equal partners in its delivery.
The Association of Directors of Adult Social Services (ADASS) has published a comprehensive policy statement emphasising that social care brings decades of experience in delivering person-centred support close to home—principles that lie at the heart of the neighbourhood health model.
The statement, released last month, argues that adult social care’s long-standing commitment to choice, control and community-based support, enshrined in the Care Act, positions local government as a natural leader in shaping these new services.
A FAMILIAR APPROACH FOR SOCIAL CARE
The neighbourhood health model aims to deliver care as close to people as possible, offering individuals choice and control over their support. For social care professionals, this represents familiar territory rather than new ground.

Directors point out that people consistently achieve better outcomes and use resources more efficiently when they direct their own support, rather than relying solely on traditional, professionally-led service models. This principle underpins self-directed support and the use of direct payments—tools that social care has championed for years.
The policy statement emphasises that truly effective neighbourhood health services require more than simply relocating medical services into communities. Success depends on addressing the decline in community assets and infrastructure, and investing in long-term sustainability.
OPPORTUNITIES FOR TRANSFORMATION
ADASS views the neighbourhood health agenda as an opportunity for fundamental change in how health and care services operate. By strengthening connections between statutory services and communities, and tackling social determinants of health such as housing, education and employment, the approach could create a more responsive and equitable system.
The statement highlights several key opportunities, including the potential to advance integrated commissioning, develop neighbourhood teams that bring together health and social care professionals, and empower communities to lead service design based on local insight and strengths.
At its most ambitious, the vision includes delegating budgets to place-based partnerships that bring together community health, mental health, primary care, social care and public health services, with a
renewed focus on personal health budgets as a proven but underused tool.
For neighbourhood health to work effectively, ADASS outlines eight critical design principles. These include ensuring that plans are driven by local needs rather than central diktat, with variations across areas reflecting different community contexts and priorities.
Local authorities must be enabled to take leadership roles, with adequate resourcing and clear accountability across health and care partners. Adult social care’s expertise, knowledge and community connections—built over many years—must be fully recognised and utilised.
The statement calls for a genuinely shared vision across the NHS, adult social care and local government, with partners working towards common outcomes rather than pursuing fragmented initiatives that report separately.
Developing a multidisciplinary workforce represents another crucial element. ADASS argues that equity with NHS staff cannot be achieved unless pay, terms and conditions for social care workers become more closely aligned—a change that must be fully funded.
The statement supports co-locating frontline health and social care teams in the same community premises, with appropriate funding and support for delegated health activities agreed locally with the NHS.
Financial alignment also features prominently in the recommendations. ADASS calls for NHS funding and guidance to shift focus from acute to community care, with budgets realigned to reflect neighbourhood health priorities and clear expectations set for managing system pressures such as hospital discharge.
The policy statement emphasises the importance of embedding lived experience, community voices and unpaid carers into service design and priority-setting. Crucially, it warns that care closer to home must not create unsustainable pressures on family carers, whose voices must be heard and responded to.
Investing in voluntary, community, faith and social enterprise sector initiatives represents an essential element of the preventive approach, ensuring everyone in a neighbourhood has equitable access to services.
ADASS concludes that making neighbourhood health work will depend on the maturity of local relationships, bold leadership, willingness to delegate decision-making, and genuine commitment to working together at an agreed local level—with social care as a full and equal partner every step of the way.

Watch your resident's eyes light up when the beautiful tea trolley arrives! Euroservice
products to residents. How about a delicious snack/pastry trolley or even a drinks trolley for that afternoon tipple?


lovely trolley


Oliver Kent-Braham, Co-Founder and CEO of Marshmallow (www.marshmallow.com) – a car insurance provider for newcomers to the UK – explores what is required to overcome the hidden financial challenges faced by the workforce that keeps the NHS and social care system running
As this audience well knows, the UK’s health and social care system is under immense strain. Chronic staff shortages, rising patient demand and stretched budgets have created a situation where services are under constant pressure.
The health and social services sector is the single largest employer of foreign-born workers in the UK. One in three care workers, and over a quarter of nurses in England, are born outside the UK. We all know that without them, the NHS and our care infrastructure would simply not function.
However, many of these workers still face barriers to financial inclusion that limit both their personal and professional potential. This is more than a workforce issue, it’s an economic one.
The UK is already grappling with over 100,000 vacancies across health and social care. As a result, there are more delayed treatments, a growing patient backlog and an increasing reliance on agency staff, costing the NHS billions of pounds every year. At the same time, our population is ageing rapidly, with demand for carers and nurses only set to increase in the coming decades.
Against this backdrop, migrants are playing a vital role, particularly in this sector. These workers underpin our frontline services. They make sure patients receive care, hospitals can function and care homes can continue to operate.
As newcomers to the UK, migrants make a huge contribution. But while we depend on them, the UK’s financial system largely ignores them. We regularly hear from our customers that they are not given access to essentials like fair insurance, loans, or credit. This blocks them from being able to set up their lives, whether it’s driving to work, buying a car, renting a house, applying for a mortgage, or getting a phone. Time and time again, we hear: “Here, I faced a lot of challenges. It wasn’t that I wasn’t prepared, I was prepared, but the system made it difficult.”
And this isn’t because they are high-risk customers, but because financial providers in the UK do not take into account their credit or employment history from abroad. In practical terms, for example, this means a driver with 10 years’ of experience in their home country is treated as if they are a brand-new driver in the UK.
Supporting a modern day workforce means creating fit-for-purpose solutions that reflect differing circumstances. For example, insurers and lenders could recognise overseas financial histories and employment records, allowing migrant staff to access fair car insurance, home insurance and credit. Care employers could also provide guidance and support to navigate these systems, helping staff secure stability outside of work. Getting this right benefits the UK’s health and social care system as a whole. A more financially secure workforce is less likely to leave, reducing reliance on costly agency staff, cutting recruitment pressures and keeping patients’ care consistent. In turn, this strengthens the NHS and care infrastructure while supporting the wider economy.
However, the challenges in the path are complex and deep-rooted. Outdated financial systems continue to lock people out. If you arrive from overseas, you may have a decades-long financial history, but in the UK, it can often be of little value. This creates a domino effect: without credit, it’s harder to rent or secure housing; without insurance, it’s harder to get a car; without a car, it’s harder to get to work.
Failing to address these barriers comes at a real economic and social cost. NHS staff shortages already run into billions annually, and as care needs grow, barriers faced by migrant workers to access fair financial services make it harder to fill the gap. Without technology and processes that recognise their histories and support their integration to life in the UK, workers struggle to settle, plan ahead and remain in their roles.
The opportunity lies in setting this workforce up for success. That means tackling the hidden barriers to financial inclusion and ensuring migrant carers and nurses are fully integrated into systems that enable stability and growth.
Technology can play a key role in making this possible. Digital tools and data-driven solutions can assess financial risk more fairly. Recognising overseas employment and credit histories can provide accessible products such as car and home insurance, loans and credit-building support. Online platforms can streamline applications and reduce bureaucracy. They can also offer guidance tailored to the unique challenges migrant workers face, making it easier for them to settle, plan ahead and remain in their roles long term.
Giving access to fair financial services strengthens the workforce, reduces reliance on costly agency staff and ensures patients receive consistent, high-quality care. Supporting those who support us isn’t just the right thing to do; it’s the foundation of a sustainable healthcare system and a resilient UK economy. If we want a care and health system fit for the future, we need to start by giving the people at its heart the support they need to build secure lives here in the UK.
For more information or to secure a quote please visit www.marshmallow.com

A lifelong Spurs fan living at a Northwest London home went on a trip down memory lane as he visited the area of his favourite football team.
Michael Alfred (87) lives at MHA Riverview Lodge and is an avid Tottenham Hotspur fan and would regularly attend matches.
Michael, a well-known saxophone player in his younger days, played with Ronnie Scott and Boney M. for seven years.
Michael often speaks about his love for Tottenham Hotspur Football Club, and it was during a 1-to-1 session, with activities coordinator Aly Abdel-Alim, that led to the trip being arranged.
Michael was accompanied by Aly, and the two spent around an hour and a half taking in the sights around the Tottenham Hotspur Stadium and finished off the trip with a bite to eat and a hot drink from the club’s cafe.
The Seize the Day initiative encourages residents to re-experience activities or events from the past or to do something they would like to do for the first time.
Speaking after the visit Aly said: “ Michael really enjoyed going back to the area of where the stadium is and it’s all he has been talking about.
“He was telling me how much the area has changed and telling me what used to be here and picking out stuff he said has recently changed.
“During our 1 to 1 sessions, he would often tell me about his love for Tottenham Hotspur Football Club and how he would visit White Hart Lane.
“When I mentioned the idea of visiting the area he was really keen and would often ask me, when are we going.
“It was a real trip down memory lane for him, and you could see how excited he was, just by his huge smile.
“It was a lovely day out, and one that was finished well with a bite to eat from the club’s cafe.
“I am hoping to arrange another visit, where we can go into the stadium and watch a game, I feel he will really enjoy that.”

Meadow View Nursing Home in Chesterfield has found a grand(e) way to support a new resident with scoliosis- an innovative vacuum posture cushion.
The middle-aged client joined the home after a spell in hospital: underweight and fragile, she needed additional skeletal support and 1:1 care. Meadow View- part of Emh Care & Support- could provide the high quality round-the-clock attention she required.
The home’s nurses responsible for the lady were struggling to find a way to keep her comfortable and safe in bed. They raised the issue with the home’s Occupational Therapist, who suggested AAT’s Grande mattress with Treat-Eezi cover.
Using vacuum technology, the mattress-sized beanbag can be

By using the vacuum principle, any air in the cushion is removed, thereby fixing the moulded shape and removing the need for frequent re-positioning. The shape and firmness of the Grande can be adjusted as little or much as needed. The cushion can be precisely moulded to create abduction and adduction wedges, or an asymmetrical body position- all by the care-givers, within minutes(1). The addition of the Teat-Eezi overlay helps maintain blood flow and gives an extra layer of protection against the risk of ulcers.
Meadow View Manager Gillian Kent comments, “The Grande gives support to her overall body structure, yet is soft and comfortable. The team find it’s easy to reform when she is supine, so they can ensure her continued relief and security when she’s lying in her bed. It has really helped her overall daily and nightly relaxation.”
Find out more about AAT’s Grande vacuum posture cushions here: www.aatgb.com/grande
Saint Cecilia’s Care Group Chairman and Honorary President of The Independent Care Group (ICG) Mike Padgham has expressed concern that the Chancellor’s latest Budget fails to deliver the long-term, sustainable support urgently needed within the social care sector.
While the Budget includes significant investment across public services, Mr Padgham says it falls short of addressing the critical pressures facing care providers, warning: “Without targeted support, we will see more care homes and home-care providers closing their doors.”
He acknowledged that an additional grant for social care is welcome, but believes it does not meet the scale of need: “Despite headline increases for the NHS and wider

services, social care once again receives too little to stabilise a system under immense strain.”
Calling for decisive action, Mr Padgham emphasised the essential role of the sector: “We must recognise that social care is not a ‘nice to have’: it underpins the health system, supports our most vulnerable and keeps communities functioning. Now is the time for long-term, sustainable funding – not short-term fixes. If the Chancellor truly wants to build a lasting legacy, social care cannot be the missing piece.”
The ICG has said it will continue to urge the Government to deliver a comprehensive plan that strengthens the workforce, supports providers and ensures older and vulnerable people receive the care they deserve.
New research released today provides data comparing fuel poverty rates among the general population with rates among specific groups of carers.
Around 13% of the UK population lives in fuel poverty. Researchers commissioned by Carers Trust found fuel poverty rates amongst certain groups of carers much higher than the national average. In households with one adult carer, more than a quarter (28%) of unpaid carers live in fuel poverty. This rises to a third (36%) in households where one adult carer is living with children.
RESEARCHERS ALSO FOUND THE AVERAGE RATE OF 13% ACROSS THE UK POPULATION RISES TO A FUEL POVERTY RATE OF:
• 17% for carers on Carer’s Allowance
• 22% for unpaid carers in multi-adult households where the carer is in receipt of Universal Credit
• 49% (a huge jump to almost half) of unpaid carers living in single adult households where the carer is in receipt of Universal Credit.
• 19% (almost one in five) of young adult carers living with other adults.
These stark findings are set out in Running on Empty, a research report commissioned by Carers Trust and carried out by Care Full.
Carers have always found it hard to make ends meet. Many have had to give up paid work altogether, or at least reduce their paid hours significantly, so they can care for a family member or friend. Many rely on benefits like Carer’s Allowance which fall short of what is needed for even a basic standard of living. On top of acute financial pressures, many carers are contending with soaring household energy bills. All too often, reducing energy consumption is not an option. Carers need to keep houses warm and keep equipment running because this is essential for the person they are caring for.
The ‘Running on Empty’ report will be shared with MPs today (Tuesday 2 December) at an event in Parliament. The report includes a series of recommendations for the Government and energy providers to eradicate fuel poverty for unpaid carers, and beyond.
THE REPORT PUTS FORWARD RECOMMENDATIONS INCLUDING:
• Introduce a social tariff to ensure that energy is affordable for those with lower incomes or additional needs, including care and disability.
• Complete and far-reaching reform of social security support for carers, including reform of Carer’s Allowance (and Carer Support Payment in Scotland) to increase eligibility, generosity and support for those with the most intense caring roles.
• Ensure those on Universal Credit can afford essentials.
Reflecting on the findings in the Running on Empty research, Ramzi Suleiman, Policy and Public Affairs Manager at Carers Trust, said: “While the Chancellor’s announcement that energy bills will be reduced by £150 a year from April 2026 will benefit families across the country, we know this won’t even hit the sides in helping pull the most vulnerable groups of carers out of fuel poverty. We heard from carers, some of whom are spending £500 a month on their energy bills.
“Ending carer poverty has to be a priority for this Government. A big part of that will be giving carers access to affordable energy as a right, not a nice-to-have. Carers who rely on social security have intense caring roles – caring for at least 35 hours a week – with many caring for over 50 hours every week. Many cannot balance paid work with their caring responsibilities, so the government must take action to make sure those on Carer’s Allowance or Universal Credit are able to afford life’s basics.”

By Rebecca McGuirk, Head of Employment and Pensions at Trowers

The Employment Rights Bill is a major piece of legislation that will significantly those working and operating in the care sector. It is designed to strengthen workplace protections across a wide range of issues, including dismissal rights, zero-hour contracts, family leave, and trade union reforms.
It was anticipated to receive Royal Assent this Autumn but is currently going through an increasingly lengthy period of Parliamentary ping pong.
The government published an implementation roadmap for the Bill in July. This sets out a timetable for the various measures contained in the Bill, though this may be subject to change.
THE MAIN PROVISIONS OF THE BILL
The Bill covers a lot of ground, so for the purposes of this article we'll just highlight the main provisions.
APRIL 2026
Day one parental rights. The introduction of a day one right to paternity leave and unpaid parental leave is due to come in next April. Paternity leave is currently only available for those employed for 26 weeks or more by the 14th week before the expected week of childbirth, while parental leave is only available to employees with one year's continuous employment. Improved sick pay. There will be an entitlement to statutory sick pay (SSP) from the first day of absence and the removal of the lower earnings limit (lower earners will be entitled to 80% of normal weekly earnings or SSP, whichever is lower).
Stronger redundancy protections. The collective redundancy protective award for a failure to consult will increase from 90 days' full pay for each affected employee to 180 days. Trade union access. There will also be a right for a listed trade union to request access to the workplace to meet, represent, recruit or organise workers and to facilitate collective bargaining, but not to organise industrial action.
OCTOBER 2026
Restrictions on 'fire and rehire'. From October 2026 the practice of fire and rehire, where employers dismiss staff and re-employ them on worse terms, is going to be restricted. A dismissal will be unfair if the reason (or principal reason) was that the employer sought, and the employee refused, a variation to their contract of employment. It will also be unfair if the employer replaces the employee with another person who carried out substantially the same duties, but who is willing to accept the varied terms. The Bill will allow an employer to fire and rehire in limited circumstances such as the need to reduce or mitigate "financial difficulties".
Extended tribunal limits and sexual harassment prevention. Employment tribunal time limits will be extended from three to six months, and there will be a mandatory requirement on employers to take "all reasonable steps" to prevent sexual harassment of their employees. The Bill will also introduce liability on employers for the acts of third parties.
2027
Unfair dismissal protection. Perhaps one of the most significant (and certainly most controversial) measures was the introduction of day one protection from unfair dismissal. While the government has stepped
back from these plans, it said the current two-year qualifying period for unfair dismissal rights will be reduced to six months. This is scheduled to take place sometime in 2027. The Bill allows employers to operate probationary periods during which employees can be dismissed more easily for performance after following a lighter-touch process. The government has committed to consulting on the length of the statutory probation period.
Flexible working and maternity protection. There will also be a day one right to flexible working, but only where this is "practicable". It will be unlawful for an employer to dismiss an employee who is pregnant, on maternity leave or who is returning from maternity leave for six months after their return to work, except in specific circumstances to be determined.
Bereavement leave and employer reporting requirements. 2027 will also see the introduction of a new statutory right to leave for bereavement including pregnancy loss, as well as the mandatory publication of gender pay and menopause action plans for employers with 250 or more employees.
Redundancy consultation. The current collective consultation threshold which kicks in if there are 20 or more redundancies at one establishment will remain, but it will also apply if there is a new threshold number of redundancies proposed at more than one establishment. The details of the new threshold will be set out in further regulations.
Zero-hours contracts. Finally, the Bill provides that workers on zero hours contracts and workers with a "low" number of guaranteed hours, who regularly work more than these hours, will have the ability to move to guaranteed hours contracts which reflect the hours they regularly work over a fixed reference period.
Employers will be required to give employees reasonable notice of shifts which are required or requested to be worked and will also be required to provide reasonable notice of any changed or cancelled shift. The details of these new rights will be the subject of consultation.
This is particularly significant for care workers and represents a major shift in how pay and conditions are determined in the sector.
The Bill provides for the establishment of the Fair Pay Agreement Adult Social Care Negotiating Body (ASCNB). The ASCNB will negotiate changes to pay and terms and conditions for care workers and will include both employers and trade unions. Under the government's implementation roadmap regulations to establish the ASCNB are currently due to come into force next October. The ASCNB will conduct negotiations in 2027 with enough time to prepare the sector for implementation "ahead of 2028-29". The government envisions that the 2028-29 fair pay agreement will be the first of many negotiated in years to come.
The fair pay agreement process is designed to combat the significant challenges faced by the sector which comprises 1.5 million people (equivalent to 5% of all adults in employment). The sector is historically low-paid with most care workers earning at or just above the National Living Wage, around 21% of posts are on zero-hours contracts (compared to 3.5% in the wider economy), and the sector experiences a 25% turnover rate largely due to low pay and poor conditions.
At the end of September, the government issued a consultation, 'Fair pay agreement process in adult social care', to gather views on the design of the Fair Pay Agreement process. This runs for 15 weeks and will close on 16 January 2026.
WHAT NEXT?
Whilst many of these changes will not take effect until 2026 and 2027, employers should begin preparing now by reviewing current policies and practices. The detail of the fair pay agreement process is currently being consulted on but those in the adult care sector will have a much better idea of what this will look like in the months to come.
Hamberley Care Homes honoured its exceptional colleagues at a glittering annual awards ceremony, celebrating dedication, compassion and excellence across its UK services.
Carers, managers and team members from Hamberley homes across the country came together for the prestigious event, held this year at Sopwell House, St Albans.
Hamberley Care Homes CEO Paul Hill, said: “It was a truly special occasion, a night filled with pride, gratitude and admiration for our incredible teams.
“The awards gave us the chance to pause, reflect and celebrate the life-changing work happening every day in our homes.”
Winners on the night included Lara Masucci of Newton House Care Home, who was named Home Manager of the Year, and Emma Burns of Caddington Grove Care Home, who received the

Excellence in Operations Management award.
The Excellence in Marketing Management award went to Kerry Hill of Cofton Park Manor Care Home, while Fiona Smith of Richmond Manor Care Home was recognised for Excellence in People Management.
Two managers received the Outstanding Contribution to Stakeholder Engagement award: Magda Anca of Alston House Care Home and Kay Mitchell of Templeton Place Care Home.
The award for Outstanding Occupancy Performance was presented to Daniela Danciulescu of Brookwater House Care Home, and Outstanding Quality Performance was awarded to Ramona Stanciu of Elstow Manor Care Home.
Simona Varga-Pali of Charrington Manor Care Home received the prestigious Outstanding Commercial Performance award.
Nobi makes lives safer by preventing and detecting falls. Powered by cutting-edge AI technology, this intelligent light monitors the entire room discreetly and accurately — all while blending seamlessly into any interior with its award-winning, homelike design. Nobi supports older adults in living a dignified, carefree and happy life, with complete respect for their privacy.
A fall can dramatically change someone’s life. Rapid assistance after a fall — or, even better, preventing a fall altogether — is invaluable. It is crucial for older adults, but equally vital for caregivers who are committed to ensuring safety, comfort and independence. The moment a fall occurs, Nobi sends an immediate alert to care staff, creating the peace of mind that every incident will be seen and acted upon.
“Long lies” and their harmful consequences belong firmly in the past. With Nobi’s intelligent prevention and detection working in the background, caregivers can focus on warm, meaningful and person-centred care.

From its very beginning, Nobi has carried one clear vision: to make care environments places where safety feels natural, dignity feels effortless, and ageing is embraced rather than feared. The Nobi Light was the first proof of that vision. At first glance, it looks like a simple design light — yet within it, Nobi redefined fall
detection, fall prevention and smarter care. It showed that technology does not need to look technical. It can disappear into everyday life, becoming part of the environment while quietly transforming it.
Today, the Light remains at the heart of everything we do. Around it, Nobi is building the Nobi Care Flow: a connected layer where people, technology and routines work together effortlessly. This care flow gives residents a greater sense of safety, offers caregivers more time and peace of mind, and provides leadership with clarity to run safer, more efficient communities. All intelligence, integrations and software are included, making Nobi one of the most cost-efficient and impactful upgrades in elderly care.
Nobi is more than a smart light.
It is a dignified, intelligent care ecosystem — one that helps care flow again. By bringing safety, clarity and confidence into every room, Nobi supports the people at the heart of care: the residents who deserve to feel safe, and the caregivers who deserve tools that truly help them. info@nobi.life www.nobi.life
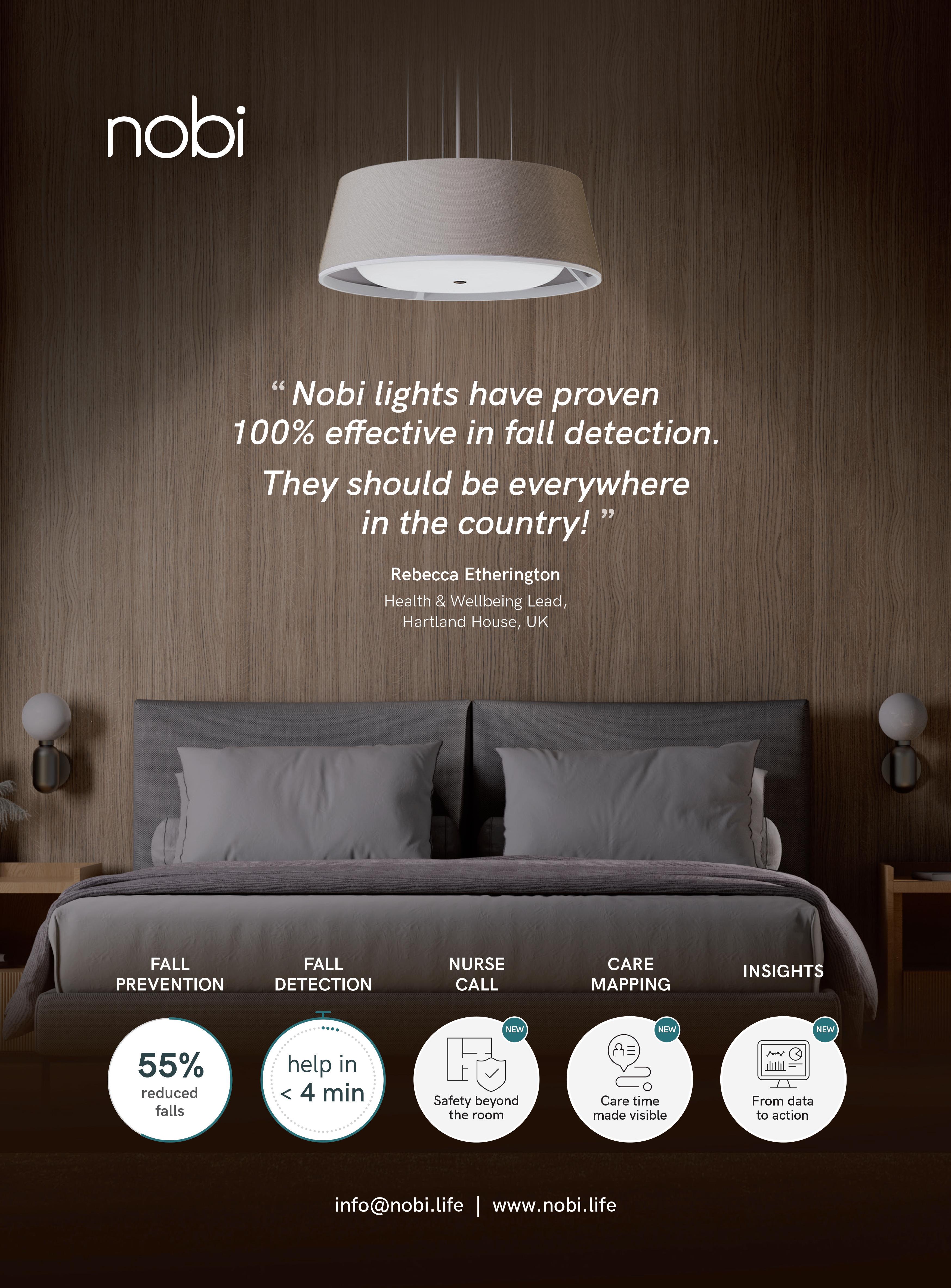


By Chaim Grunfeld, Founder and Director of connectivity specialists, Prime Connect

When the internet falls or the signal is inconsistent, it’s easy to blame Wi-Fi. We’ve all become so used to its ubiquitous presence that it has quickly become a one-size-fits-all descriptor for all kinds of connection problems, whether or not the issue is indeed wireless.
Likewise, when things go wrong, it’s only natural for care home staff to blame IT, demanding they swoop in and fix poor connection with signal boosters and upgraded in-care-home hardware.
The issue is, capricious internet is not always an IT problem.
There are two different kinds of computer networks supporting the internet: WAN (or wide area network) and LAN (local area network). WAN is the pipeline delivering power into your building, whilst LAN makes up your internal system, including all routers, access points, internal wiring, and physical devices like printers.
Whilst poor internet can sometimes be a LAN problem, more often than not, it’s WAN letting the side down.
Think of it a bit like a radio. If the signal emitted by the broadcaster is broken, it doesn’t matter how great your radio is. You could have bought the latest, greatest model on the market, but without the right input, there’ll be nothing but static. Similarly, without the right WAN input into your building, connection will be poor, even if you’ve spent thousands on the best possible internet package.
Fuelling the system
Care homes that invest in great Wi-Fi – and top-notch routers and access points – are essentially sitting on untapped Ferrari potential if they don’t first secure a strong external connection. The car has been left to gather dust in the garage, not because the vehicle itself is faulty, but because the fuel going into the tank isn’t good enough to power it. If the right juice isn’t coming in, it’s unreasonable to expect to get the best results out – no matter how many upgrades you throw at it.
IMPROVING THE PIPELINE
Many care homes still rely on copper broadband or standard BT-style lines, often unaware that leased lines are an available alternative offering more dedicated, reliable connectivity. Shared lines are impacted
by other buildings and users, which slows internet performance, particularly during peak times. A leased line, on the other hand, acts like a private fuel supply, ensuring fast, smooth, uninterrupted connection. Think of the line into your building as a driveway. Shared with others, it can become congested, slowing everyone down. With a leased line, you have your own private way in, with zero obstacles, allowing data to flow freely.
In the UK, Openreach is responsible for providing the physical infrastructure that delivers broadband to properties, regardless of the type of line you select. For care homes, this often involves installing fibre-optic cables directly into the building. Before this can happen, however, a wayleave agreement must also be in place.
Wayleave agreements are essentially legal contracts that grant service providers permission to install and maintain equipment on private property. Without them, installation cannot be carried out, which is why it’s so important to seek informed, prepared providers capable of mitigating potential service disruptions.
Once your external connection has been established, it’s time to look at your LAN. Relying solely on IT teams to solve performance issues can be a mistake, inhibiting both potential and progress. Learning to continually audit and optimise everything from routers and access points to internal wiring is extremely important, as outdated or misconfigured internal infrastructure can easily produce bottlenecks with even the strongest WAN connection, limiting the benefit of upgrades.
Regular assessments and upgrades are therefore vital to ensuring the entire network can handle rising digital demands.
In recent years, the role of the internet in care homes has expanded beyond simple communication. Digital tools are now integral to daily operations, whether it’s carers providing entertainment and opportunities for social engagement to residents, or opting into potentially lifesaving telemedicine services that protect elderly and vulnerable people under their charge.
In other words, reliable internet is no longer all about Netflix or other, luxury whims. It’s about ensuring residents remain safe, healthy, and protected, while also ensuring they are able to maintain contact with loved ones remotely where needed. Homes that fail to invest in both WAN and LAN improvements thus risk falling behind the evolving standard of care, finding it increasingly difficult to fill spaces.
Understanding the difference between WAN and LAN allows care home managers to ensure their facilities are truly equipped to meet rising expectations. In a world where the internet is about so much more than keeping up with TV developments and actually makes a positive impact on care and wellbeing, robust internet infrastructure of every kind is a worthwhile investment.

A resident at RMBI Care Co. Home Zetland Court, in Bournemouth, has been overwhelmed with kindness after receiving more than 550 birthday cards from people across the country to mark her 102nd birthday.
Joan Rollason, who lives at the Home’s dementia house, celebrated her milestone birthday on Sunday 30 November.
When staff asked Joan what she would like to mark the occasion, she simply replied: “Everyone.”
Unsure how to fulfil such a special request, the team decided to reach out to the local community to see if they could help Joan feel surrounded by “everyone” on her big day. They invited people to send her birthday cards, hoping to reach at least 102 to match her age.
What followed far exceeded their expectations. The appeal quickly spread throughout Bournemouth and beyond, reaching playgroups, children’s clubs, community organisations, social care groups, BCP Council, various Masonic lodges, workplaces and households up and down the country.
Birthday cards began arriving in their hundreds, along with flowers, teddy bears and plenty of chocolates. Staff at Zetland Court say they are still receiving cards for her. Once the celebrations are over, residents plan to give the cards a second life, transforming them into new crafts and decorations as part of an upcoming creative activity.
To mark the occasion, Joan has enjoyed two birthday celebrations. On Thursday, she attended Zetland Court’s dementiafriendly café, where she was surprised by Bournemouth’s town crier, who proudly announced her 102nd birthday. On her birthday itself, she enjoyed a second party at the Home with her family, friends and a special visit from the Mayor.
Sue Wiffen, Zetland Court’s Deputy Home Manager for Dementia, says: “We simply wanted to make Joan’s wish come true, and the response has been extraordinary! Joan was delighted and deeply touched by the kindness shown by so many people. It has made her 102nd birthday truly unforgettable.”
Grove House, a 47-bed residential facility located in Adlington, Chorley, has become the focal point of local opposition after Lancashire County Council included it amongst ten elderly care facilities currently under formal review as part of cost-saving measures.
The Speaker has publicly declared his determination to campaign against the potential closure, describing any decision to shut the facility as completely unacceptable. He has called upon council officials to prioritise investment in the home rather than pursue closure plans that would displace vulnerable residents from what he described as their final place of residence. Sir Lindsay

emphasised the home’s significance to the local area and questioned whether forcing elderly residents to relocate aligned with community values.
The county council’s review encompasses four additional residential care homes across Lancashire: Favordale home situated on Byron Road in Colne, Milbanke Care Home in Kirkham, Thornton House in Thornton Cleveleys, and Woodlands in Clayton-le-Moors.
Five day centres are also included in the consultation: Byron View (Colne), Derby Centre (Ormskirk), Teal Close (Thornton Cleveleys), Milbanke Day Centre (Kirkham), and Vale View (Lancaster).
A spokesperson for Lancashire County Council stated that the authority remains focused on achieving improved outcomes for service users whilst maintaining fiscal responsibility. The council has encouraged members of the public to participate in the ongoing consultation process before any final determinations are made. A definitive decision regarding the future of all ten facilities is scheduled for February 2026.
Nursing staff across the UK feel more undervalued than at any point in the past decade, according to the latest Royal College of Nursing employment survey, with the organisation now calling for urgent action to “make the next 10 years better than the last”.
More than 21,000 RCN members from across all health and care settings participated in the biennial survey, which paints a concerning picture of a workforce under significant strain. While there are small signs of progress, the findings reveal that nursing staff believe their skills and expertise remain unrecognised, with workload pressures preventing them from delivering the standard of care they aspire to provide.
Pay fairness emerged as the single biggest concern among respondents. Two-thirds believe their salary does not reflect the responsibilities, skills and risks they face daily. The survey shows record numbers of members dissatisfied with their pay band, reflecting widespread frustration with the current framework, which the RCN says is “not fit for purpose” and requires fundamental reform beyond annual cost-of-living increases.
Retention continues to pose a significant challenge for the workforce. Four in 10 nursing staff are considering or actively planning to leave their roles, citing feeling undervalued, low pay, excessive pressure and emotional exhaustion as the primary drivers. The RCN has warned this represents a serious threat to both workforce stability and patient care.
Workload pressures remain acute, with many nursing staff regularly working beyond contracted hours—often unpaid—and more than eight in 10 reporting working whilst unwell. These pressures are taking a toll on morale, health and the ability to provide quality care.
Perhaps most concerning is a dramatic decline in advocacy for nursing as a career. While most respondents still describe nursing as rewarding, only a third would now recommend it as a profession—the lowest figure since the survey began 10 years ago.
The survey also highlights the impact of rising living costs, with some nursing staff reconsidering pension contributions and struggling to meet basic expenses.
When asked what would make the biggest difference, nursing staff overwhelmingly prioritised a pay rise, followed by more annual leave and greater flexibility in working arrangements.
Professor Nicola Ranger, RCN General Secretary and Chief Executive, said: “Ten years on from our first employment survey and the results continue to paint a worrying picture—many nursing staff are considering or actively planning to leave their roles.
“The current pay framework is broken and long overdue reform to the pay structure is needed. No annual cost of living pay increase is ever going to be enough to deliver the fundamental change we need.
“Despite these challenges, nursing is an amazing profession. Our challenge now is to make the next 10 years better than the last, for nursing as a profession but crucially for patients too.”
Professor Ranger outlined the key priorities: securing fair pay and recognition for all nursing staff; investment in safe staffing, including mandated minimum nurse-to-patient ratios across all settings; and employer action to create safer workplaces where every member of the nursing workforce is supported, valued and protected.
“These ambitions are not new—but they need to be realised now more than ever,” she concluded.
Local charity St Peter’s Hospice is celebrating a double award win with accolades for its collaborative clinical work and its outstanding garden.
Teams at Bristol’s only adult hospice are delighted with the recognition for their respective areas, which they say has given a boost to hard-working staff and volunteers.
The first win was the Outstanding Collaboration Award at the annual North Bristol NHS Trust Staff Awards, which was presented to the team at St Peter’s Hospice alongside Southmead Hospital’s Psychology ILD (interstitial lung disease) multidisciplinary team.
The award recognised the Hospice team’s compassionate care for patients living with life-limiting respiratory conditions and their seamless collaboration with staff at Southmead Hospital.

Caroline Mundy, Head of Clinical Engagement at St Peter’s Hospice, said: “We are delighted to win this important award, which reflects the dedication, teamwork and compassion that drive our service.
“Our partnership work has been ongoing over the past six years and we’ve built a service that ensures patients living with life-limiting respiratory illness can access compassionate hospice care when they need it most.
Working together means we can offer patients the best possible care and support.”

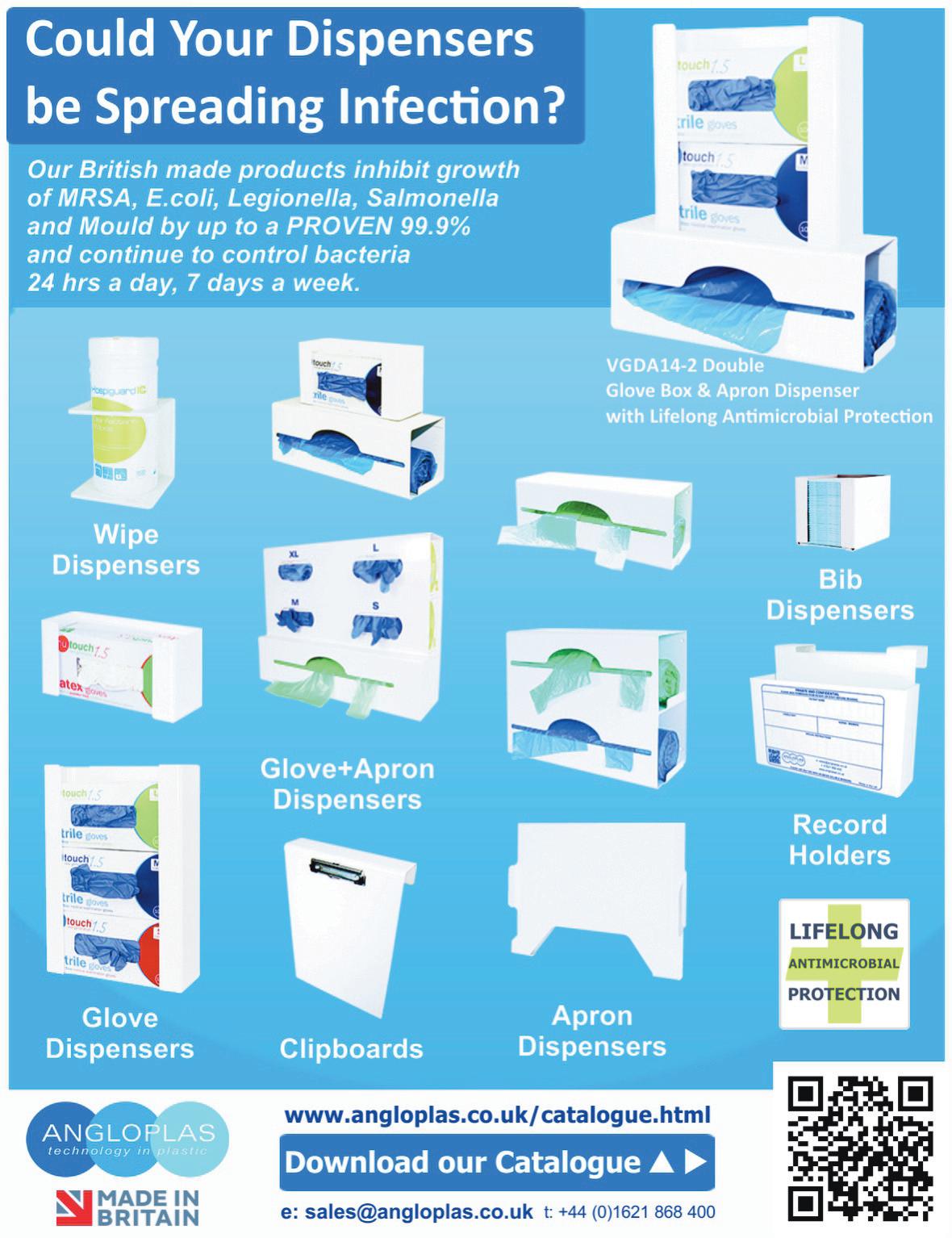
Elsewhere in the organisation, the Hospice’s Head Gardener and team of dedicated volunteers were awarded a ‘Level 5 – Outstanding’ award at the 2025 It’s your Neighbourhood Awards, organised by the RHS.
This award celebrates the contribution of volunteers looking after a garden or community space. Head Gardener Anneke van Eijkern attended the awards ceremony with six volunteers who were presented with the award by the Lord Mayor.
Anneke said: “We are delighted with this award which recognises the vital contribution made by volunteers to maintaining community gardens.
Our community here is obviously a special one for patients, their families and visitors and our staff, but increasingly members of the public who use our café and visit us for our annual Open Gardens event.
“All community gardens that entered were recognised with an award at different levels according to how much progress they are making against specific criteria set by the RHS. This was the first year we’ve entered so we were very pleased to be awarded level 5 – Outstanding!”
St Peter’s Hospice is Bristol’s only adult hospice. All care at St Peter’s Hospice is provided free of charge but the charity relies on gifts in wills, donations, fundraising and money raised through its retail shops to deliver its services.

Choosing a new care home for a loved one is such an important decision, especially when that involves moving a considerable distance. We spoke to Gill Lancaster whose father recently moved from Leicester to Danforth Care Home’s Primrose House in Brough, East Yorkshire about how she made the decision and how well it turned out. WHAT PROMPTED THE MOVE?
Over the year preceding the move my dad gradually became more physically frail and at the same time early signs of dementia became evident. I’m an only daughter and because of his condition I became increasingly concerned about the distance between us, a 2 hour drive. It was getting harder to speak to him on the phone and trickier to keep up with what was going on with him medically. So, I began to talk to him about moving to be closer to me, but he wasn’t keen. He was settled and tired, a move was very unappealing, but I was concerned about what might be ahead.
HOW DID YOU FIND PRIMROSE HOUSE?
In the first instance, simply by looking on the map for care homes close by, reading reviews and asking about. From this research, Primrose House topped the list, so I arranged to go and have a look. First impressions were great; it’s modern, bright, immaculately clean and the bedrooms wouldn’t be out of place in a hotel. It’s great to see ¾ beds rather than the singles that so many care homes have. What was also quickly evident was the attitude of the staff. The dining room/sitting room were lively with plenty of chat and the odd resident being helped to eat, where needed. It felt warm and welcoming, plenty of smiles.
WHAT CONVINCED YOU AND YOUR DAD TO MAKE THE MOVE?
A couple of things but the most significant was the impression that Braiden, the Manager at Primrose House made on me and my father. The next step after my favourable first visit was for my dad to be assessed to confirm that Primrose House could meet his needs and Braiden travelled down to Leicester to do that. He was a great mix of warmth and professionalism and clearly knew his stuff. I was amazed how well my dad took to him and the discussions we had convinced both of us that Primrose House might be a great place for him to live. After a week or so of thought and prompted by further health concerns I convinced my dad to make the move.
HOW WAS THE MOVE?
Well, it was complicated by my father being admitted to hospital for a kidney problem. He went into A&E at Leicester Royal Infirmary and then moved to Leicester General Hospital after initial treatment. This is standard practice in the city which has medical facilities on different sites, but dad became very confused. I’d already given notice at his Leicester care home but once I’d visited a couple of times it became clear that the best course of action would be to bring him straight from hospital up to Brough, to reduce the number of moves involved. I spoke to Primrose House and they speedily got everything in place –

far faster than we’d originally agreed - so that I could do just that. He left Leicester General in a private ambulance and 2 hours later the paramedics and carers
HOW WERE THE FIRST FEW DAYS FOR YOUR DAD?
Within hours of arrival, we had a pair of lovely laundry assistants labelling clothes, and carers popping in to meet my dad and ensure we had drinks and anything else we needed. With a view out to the garden my dad was interested to look out and the trains passing were a bonus - he was soon asking questions about their destination. There was plenty of warm and welcoming attention as we unpacked.
Over the next few days my dad quickly settled into life at Primrose House. One of the early positives was that I started to find him out of his room, eating in the dining room. My dad’s tendency was to be quite reclusive, but the carers gently but persistently encouraged him out to benefit from a change of scene and atmosphere. His feedback was soon positive especially with respect to the quality and character of the carers, the heat of the food and the taste of the orange juice! It was great to see him begin to light up and joke with them when they came to speak to him. They admired his Lego house and quickly learned what made him tick, adjusting their approach accordingly.
HOW WAS PRIMROSE HOUSE FROM YOUR PERSPECTIVE?
Really impressive. There are practical things like admin/paperwork which they are very efficient at, but it was the quality of the care that I became increasingly aware and appreciative of.
For example, it sounds trivial, but you hear a lot of ‘please’ and ‘thank you’ between the staff at Primrose House. They seem kind and supportive to one another and that makes for a special atmosphere that extends beyond the care they give to residents. On that front, the approach is uniformly brilliant. Down at eye level, even for patients in bed, they hold hands for reassurance, always explaining clearly what’s
going on and any choices to be made; they are calm, kind and patient, but also fun.
I also really appreciated their approach to my dad’s mobility. On arrival he was being moved by hoist but through a quick assessment of muscle strength they raised the question of whether my dad would like to work towards better mobility. He decided this would be a good project for him, I engaged a recommended physio, and we were soon in business. I was delighted to see that as soon as the plan was established an assessment was carried out to switch my dad away from using the hoist to a transport system that meant a little more use of his muscles. In this way they began to support his efforts right from the get go as much as they were able. Unfortunately, my father fell ill, soon after this promising start so it was not to be, but if only they’d had longer I’m convinced he’d have got back on his feet.
Following a few weeks of illness, Gill’s father sadly passed away at the care home. In this last couple of questions, she discusses those final weeks and her concluding thoughts about Primrose House.
Dad and I had had several discussions about his death over the course of many years. He wasn’t frightened about being dead, he was frightened about the process of dying so it was important that I managed that, for him, as best as I could. He said he didn’t want to go into hospital anymore, so my hope was for him to stay in his bed at Primrose House, in comfort as far as possible, right to the end. And that is exactly what happened, completely due to the combined efforts of the GP and her team, and Braiden and his whole team. I cannot imagine that my dad could have had better care anywhere.
My dad was prescribed palliative drugs for pain and anxiety and the carers made sure that he got these whenever it looked like he needed them, transferring him seamlessly from injection to syringe pump for symptom management. All the emphasis in those final few days was on keeping him as comfortable as they could. They checked in very regularly, stopping to speak to him and be present alongside caring for any physical needs. They were sensitive to visitors too and I was often asked if I was OK or needed a drink. Despite the awfulness of the situation, I felt so glad he was there.
ANY LAST THOUGHTS?
My abiding memories of my father’s short time at Primrose House are of a truly excellent team working seamlessly together to deliver something that is crucial – elderly care up to the end of life. I feel like I did my best by my dad and I believe the care he received was exceptional. Both things feel important at a difficult time. I can so clearly picture two different carers popping in during his last day, sitting on his bed, holding his hand and talking so compassionately to him. They are special people, and they do an amazing job.
Primrose House is still a fairly new home but I’m confident it will go from strength to strength; it certainly deserves to.
A new academic report from the University of Oradea has placed a spotlight on the urgent need for the adoption of better prevention, training, and safer treatment technologies to reduce harm from the growing volume of healthcare waste produced worldwide, says leading independent healthcare waste management company, Anenta.
Shedding light on hazardous medical waste and its rising risks to clinical staff, healthcare workers, and those who handle medical waste, Anenta believes that the ‘Healthcare Waste Toxicity: From Human Exposure to Toxic Mechanisms and Management Strategies’ report is a sharp reminder that producers of healthcare waste need to be vigilant and diligent.
In Anenta’s view, this is particularly important in relation to the disposal of sharps, infectious, pharmaceutical, pathological, cytotoxic, and chemical waste, and applies to GPs, hospitals, laboratories, pharmacies, research centres, dental clinics, care and nursing homes.
“The findings of this study reiterate just how important segregation, governance, and training are in preventing harm to staff and the wider community,” said Kim Ormsby, Assistant Director at Anenta, adding: “It’s vital that every measure, including handling, transportation, treatment, storage, and disposal is properly understood, implemented, and audited, which is exactly why we’ve created a free e-learning module on healthcare waste to help businesses in the primary care sector.”
Covering a number of topics such as waste segregation, simplification of waste processes, waste reduction, and colour-coded containment, the 45-minute training module is accessible free of charge to care homes, and healthcare professional via the Health Education England online portal. These courses help those in the primary care sector meet duty of care obligations and ensure consistent adherence to environmental and CQC standards.
This, in turn, helps smooth the pre-acceptance and duty of care

audit process, which is essential for compliance under the Environmental Protection Act 1990, and helps avoid the risk of waste contractors refusing to make collections due to instances of ‘noncompliance.’
Aided further by Anenta’s remote hazardous waste audits, which give care homes, nursing homes and producers of healthcare waste the ability to conduct compulsory duty of care and pre-acceptance audits in as little as 40 minutes, Anenta has removed the need for tedious third-party on-site audits, which can take up to 6 days. In addition to saving time, Anenta’s online solution also reduces costs by up to £800.
Combined, this process helps to ensure compliance for care homes
whose staff are exposed to a range of different types of waste, including sharps, clinical, infectious, and offensive waste.
“Protecting workers and the wider community from the dangers of medical waste is critically important,” says Ormsby. “Without consistent training and clear policies, staff can all too easily be put at unnecessary risk, which is why we work closely with care and nursing homes to ensure that their waste management processes are streamlined and effective, ensuring a safer healthcare environment for all.”
Anenta, which was awarded the Healthcare Waste Management Company of the Year title at the prestigious Healthcare Business Review Europe Awards 2025, acts as an external contract manager delivering bespoke, affordable, and professional services across recycling, general waste, saniwaste, confidential, and clinical waste streams. Managing over 450,000 collections annually from more than 20,000 locations, Anenta has saved its clients over £13 million directly, while introducing workplace efficiencies that have generated a further £35 million in savings.
Much of these savings are possible thanks to Vector, Anenta’s proprietary, multi-stakeholder system, which equips all parties in the healthcare waste supply chain with real-time updates on documentation, billing, compliance and outcomes. Highlighting inefficiencies and providing data-driven insights to improve service, delivery and operational performance, Vector ensures the delivery of fair billing practices through the analysis of thousands of invoices to identify and address any instances of overcharging. Free training module:
https://portal.e-lfh.org.uk/Component/Details/763177 Website www.anentawaste.com
Contact page https://www.anentawaste.com/contact-us/ Call 03301222143


As sustainability rises up the agenda for care organisations, heat is a natural target for efficiency improvement. Andy Green, Head of Technical Solutions at Baxi, discusses the importance of planning a net zero pathway and some of the achievable options for care home operators
The UK’s circa 17,000 care homes may vary in size and age, but reliable heating and hot water is essential in each to prioritise the wellbeing and comfort of their residents. As this service is typically the largest user of energy in care home facilities, it’s also a good starting point for reducing operating costs and associated carbon emissions.
Let’s consider some of the achievable measures to improve the efficiency of the heating system and reduce its carbon impact
In our recent survey of over 400 care homes managers, budget pressures, eligibility for funding and technical understanding of achievable options were the top challenges listed when considering decarbonising heat in their buildings. Subsequent focus group sessions also revealed that unplanned replacements are common, frequently resulting in a like-for-like distress purchase rather than enabling the care home operator to plan and implement a phased approach to net zero. But with care homes coming under increased pressure to adopt sustainable practices in line with the nation’s wider 2050 net zero target, putting a roadmap in place is absolutely key. Fortunately, care home managers have access to heat experts like Baxi for support. We work closely with care homes first to understand the viable options for improved system efficiency and then to help them plot their unique net zero pathway.
The first step should always be to understand how and where energy is being used in the building. Identifying and limiting any heat loss to the environment will not only immediately improve operating costs but can significantly reduce the size or capacity of plant required when refurbishing the system – which in turn will lower the required capital expenditure.
Practical examples might include building fabric upgrades such as roof and wall insulation, draught proofing and/or improving the thermal performance of windows and doors. Adding lagging to poorly insulated pipework will also prevent heat losses within the system for improved performance. Where necessary, adjust the heating controls and thermostat settings to optimise the temperature regimes and balance energy efficiency with thermal comfort.
‘HEAT
Light refurbishment still accounts for much of the work in the care home sectors according to our focus group research, despite the willingness shown for embarking on heat decarbonisation projects.

If upgrading to more efficient gas condensing boilers or direct-fired water heaters, use this opportunity to prepare the heating system for the integration of low temperature heat pumps at a future stage. Addressing the system’s distribution pipework and heat emitters will allow the system to operate more efficiently at a maximum flow temperature of 55°C (or lower), in line with Building Regulations. This will also allow the condensing boilers and water heaters to operate in condensing mode, where they achieve their maximum efficiencies.
Replacing existing gas boilers or water heaters with heat pumps is the ultimate goal. New build care homes will be designed to require less heat for operational use and optimised for a decarbonised electricity grid. In buildings like these, a fully electric approach to heating and domestic hot water (DHW) based around renewable solutions such as our Auriga mid temperature and Auriga HP + high temperature heat pumps will be the favoured approach, particularly when combined with solar thermal and/or solar PV solutions. In care homes with complex refurbishment challenges, a phased pathway may be necessary. In such buildings, a hybrid heat pump system combining heat pumps with existing boilers and/or water heaters is often a fast, affordable solution to partial decarbonisation. This will enable a large portion of the heat in the building to be decarbonised while meeting safe operation requirements.
Each care home project and building will have its own requirements, so it is advisable to consult with the experts. Experienced heating and hot water solutions providers like Baxi can help break down the complexities for care homes by clearly explaining the options and outlining the associated carbon, energy and cost impacts of each. Working together, we can help ensure that the right decision is made to meet the specific needs of your building to set it on its path to net zero.
For more information, visit: Baxi Commercial Heating and Hot Water Solutionswww.baxi.co.uk/commercial
PROUD memories of national service and wartime efforts were shared when a Rotherham care home held a party to celebrate achieving “Veteran Friendly” status.
Whiston Hall Care Home, on The Manorial Barn Chaff Close, marked the occasion with a gathering of residents, staff, family members, and friends of the home – alongside local dignitaries.
The care home’s veterans were also in attendance, including Alan Taylor, 88, who served in the British Army’s Royal Signals Corps during his national service from 1956 to 1958, posted to Germany, Egypt, and then York.
Fellow resident James Broughton, 92, joined the Royal Engineers Corps when he was 18 and served two years in Hong Kong. Henry Graham, 94, served in the Army Medical Corps from 1951-53, training to the level of nurse.

Mary Barton, 85, served two years in the Auxiliary Corps at the Catterick Garrison, in North Yorkshire, where many of the residents completed their training. She was charged with driving officers around the base, during which time she met her husband, and the couple were stationed in Germany for 10 years. Effie Copley, 99, worked in the Sheffield steelworks for two years during the Second World War, for which she was honoured as one of the “Women of Steel” with a monument in Sheffield city centre in 2016.
The spouses of veterans also shared their stories, including Lorna Gibbs, 86, whose husband served as a trainer of new recruits in the Grenadier Guards. And Janet Pearn, 79, who was a sergeant in the Army for eight years.
The party to honour the veterans and celebrate Whiston Hall’s Veteran Friendly Framework (VFF) sta-
tus included live music from Keeley May Vocals, dancing, prosecco and bucks fizz, and a cake made by the care home’s chef, Deepak Pattar.
The Lord Mayor of Rotherham, Cllr Rukhsana Ismail, was among the dignitaries at the event – taking to the dance floor with fellow partygoers.
She said: “Whiston Hall’s accreditation for being Veteran Friendly is obviously something they take very seriously and are proud of. They are committed to understanding the veterans’ needs, providing tailored support and promoting respect and recognition for all their residents.
“Thank you to the incredible staff and management at Whiston Hall for creating such a joyous atmosphere – I just wish I’d worn my dancing shoes as I took a turn on the dance floor.”
Jake Richards, MP for Rother Valley, and Paul Thorp, Cllr for Sitwell Ward, also celebrated with residents and staff at the event.
Mr Richards said: “It was lovely to join the staff and residents at Whiston Hall Care Home as they celebrated becoming a veteran friendly location. The wonderful entertainment team put on a real show for the residents to celebrate this achievement.”
Marie Keaveney, activities coordinator at Whiston Hall Care Home, said: “It was an honour for us to be able to throw this party and pay our respects to our veterans. We have so many residents who themselves served or had spouses that did.
“It was a massive part of there lives and we are privileged to be able to know all of these fantastic people. The staff team has always got involved and it like one big family here at Whiston Hall.”
Residents, staff, friends, and family at Wisden Court, part of the Runwood Homes group, came together on the 12th of November to celebrate a special milestone, Lillian’s 103rd birthday. The day was filled with joy, music, and heartwarming moments as everyone gathered to honour Lillian’s remarkable life and spirit.
The celebrations included a lively party with entertainment from vocalist Becky, who delighted the crowd with her performance. The event brought together residents, staff, and Lillian’s family and friends for a memorable afternoon of singing, laughter, and shared memories.
The Wisden Court team loved to see everyone come together to celebrate an incredible occasion. Lillian was smiling throughout the day, surrounded by love and happiness.
Lillian herself shared that she had a fabulous birthday with friends and family, expressing her gratitude for all the thoughtful gestures and the wonderful atmosphere created in her honour.
This celebration not only marked Lillian’s 103 years but also highlighted the sense of community and togetherness that makes life at Wisden Court so special.

When great-grandmother Dorothy “Dot” Gaskell picks up her needles each morning, her hands move with the easy rhythm of more than nine decades of practice.
At 101, the great-grandmother from the Wirral, still knits every day, and now she has a new apprentice sitting beside her: 24-year-old live-in care worker, Saima Salamat.
When Saima took on her live-in care placement with Agincare, an independent national care provider, she didn’t expect to become a knitting addict. But then she met Dot.
“I’d never picked up a pair of needles in my life,” Saima laughs. “Now I can’t stop. I’m on my third scarf. Dot has turned me into a knitting addict, she even holds my hand in the shops, so I don’t spend all my money on wool!”
“She saw me knitting one evening and wanted to try,” Dot smiles. “I showed her how to cast on, and she was off! She’s a quick learner.” Dot, who was born in 1924 and has lived in the same house for most of her life, worked as a seamstress in her younger years and has been part of the local knitting club for decades. Every Monday, she and Saima make their way to the nearby community centre for tea, cake and conversation with fellow knitters. “Mainly ladies,” Saima smiles, “but we’ve two brave gentlemen as well.”

The club’s creations go to good causes, including hats and mittens for premature babies and shoeboxcharity collections.
“They can’t believe how neat my stitches are,” Saima adds. “Dot’s a brilliant teacher, but also very strict!” Saima, from Bradford, joined Agincare three years ago and has been supporting Dot for the past six months. Dot has three golden rules for knitting and life: don’t knit when you’re tired, don’t buy more wool than you need, and always finish what you start.
Their friendship has blossomed beyond care routines with coffee trips, shopping outings and a shared
sense of humour.
“It doesn’t feel like a job,” says Saima. “I’m learning from Dot every day about patience, positivity and making the most of life.”
“I’ve worked in betting shops, cafés, shoe stores… nothing stuck,” she adds. “But care is different. I’m growing every day.”
Latest research shows that interest in traditional hobbies and pastimes has rocketed with online searches up by over 80% for terms like ‘crochet’ and ‘pottery’ over the past ten years.
The trend is reflected on TikTok where #Crochet views grew by 145%, #Knitting views grew by 176% and #BakingTok views surged by 130% between 2023-2025.
The growing interest in crafts reflects a wider shift as people slow down, take a break from screens, and find meaning in small, mindful activities.
“Stories like Dot and Saima’s show what person-centred care is really about,” says Agincare Live-in Care Managing Director Sam Mayes.
“It’s not just about supporting daily routines. It’s about shared experiences, laughter, and learning from each other. Creativity brings people together, and that connection can be life changing.
At Agincare, we see how creative hobbies help people stay connected, boost wellbeing, and bring joy to everyday life, whether that’s in one of our care homes, through live-in care, or in supported living.
“Creative activities are so important as we age,” added Sam.
“They keep the mind active, support fine motor skills, and give people a sense of purpose. But perhaps most importantly, they bring joy, whether that’s through creating something new or teaching someone else how to do it.
“When older people share their skills, it’s empowering. They see their experience valued, and younger generations gain something real and lasting in return.”
Tech teams and entrepreneurs from around the world are being called to the Isle of Man to design new products and services to transform solutions in health and social care innovation.
The government is inviting entrants to this year’s Innovation Challenge to find cutting-edge solutions that address real system needs and support the Island’s ambition for technology-driven healthcare progress.
After three years of championing FinTech, Cleantech, and Data & AI, the Isle of Man is now focussing on healthcare, attempting to solve pressing issues around rising demand, workforce shortages, and the need for more integrated, patient-centred care.
Organised by the Department for Enterprise’s Executive Agencies –this year’s Challenge is delivered in partnership with the Department of Health and Social Care, Manx Care, and Public Health Isle of Man.

The 2026 Innovation Challenge will bring together public sector expertise, clinical leadership, and the Isle of Man’s unique testbed environment to pilot, scale, and showcase innovations that deliver real-world impact.
THE CHALLENGE WILL FOCUS ON THREE CORE THEMES:
• Working Smarter: Transforming how healthcare systems operate, connect, and communicate – freeing up capacity, improving experiences and delivering better outcomes.
• Wellness: Transitioning from reactive treatment to proactive prevention, supporting self-care, early intervention and community-based support.
• Home First: Delivering high-quality care beyond hospitals and clinics, making healthcare more accessible, personalised, and integrated into daily life.
A special Biosphere Award will honour the finalist who demonstrates the greatest commitment to positively contributing to the Biosphere.
Tim Johnston MHK, Minister for Enterprise, said: “Refocusing this year’s Innovation Challenge on health and social care enables us to tackle some of the most urgent issues facing society today.
“The Isle of Man offers a uniquely collaborative environment where innovative companies can test, refine, and prove solutions with direct access to government, healthcare partners, and a fast-moving digital ecosystem.”
Claire Christian MHK, Minister for Health and Social Care, said: “This Challenge is about transforming lives by piloting solutions that put people first and bring care closer to home. By harnessing emerging technologies, we aim to set a new benchmark for what’s possible in healthcare – delivering better outcomes, greater wellbeing, and a health system ready for the future.”
Lyle Wraxall, Chief Executive, Digital Isle of Man, said: “The Innovation Challenge has always been about solving real-world problems through collaboration. Expanding into Health and Social Care is a natural evolution, reflecting our commitment to focus innovation where it matters most, improving lives and strengthening essential services. This is an opportunity for innovators to make a lasting impact on one of society’s most critical public services.”
“If you are a tech business, whether already working in digital health or simply looking for a real-world opportunity to apply your technology in new ways, we want to hear from you. The Isle of Man offers a uniquely collaborative environment where innovative companies can test, refine, and prove solutions with direct access to government, healthcare partners, and a fast-moving digital ecosystem. This is the moment for ambitious innovators to get involved and help shape the future of Health and Social Care.” Applications opened 27th November, with registration available until 27th February 2026.
Finalists, to be announced on 3rd April, will benefit from mentorship, networking, and international exposure. The Challenge will then culminate in a finale showcase event in June 2026 where the winners will be chosen.


A recent report from Terrence Higgins Trust and KPMG UK suggests that the UK care system may need to adapt to meet the requirements of a growing number of people ageing with HIV.
The findings indicate areas where improvements could be made in training, consistency of care, and in reducing the widespread stigma that continues to influence access to health and social care services.
The report, based on a roundtable of clinical, policy and community experts, shows that more than half of people accessing specialist HIV care in England are now over 50. Many live with complex long-term conditions linked to both ageing, years of untreated HIV and early HIV treatment. Yet care homes, primary care and community services often lack the knowledge needed to meet their needs.
Care home staff often receive little or no HIV training, which can lead to stigma, unnecessary “infectioncontrol” measures, and reluctance among residents to disclose their status or having their status revealed without their consent. The report highlighted that older women living with HIV face particular challenges, such as poor access to menopause support, incorrectly adjusted medication and heightened stigma.
The report calls for mandatory HIV training across health and social care, improved multidisciplinary working, and age-inclusive standards in both clinical and care home settings. It also recommends routine opt-out HIV testing as part of NHS Health Checks for over-40s to improve diagnosis and engagement in care.
The recommendations arrive at a key moment, as HIV commissioning has recently shifted to Integrated Care Systems (ICSs) and the Government prepares a new national HIV Action Plan. The report urges ICSs, care providers and local authorities to work together to make sure older people living with HIV can access joined-up, respectful and informed care.
Richard Angell OBE, Chief Executive of Terrence Higgins Trust, said: “For many people living with HIV, the stigma is more harmful than the virus. As this report makes clear, we need action to ensure that everyone ageing with HIV can rely on a care system that understands their needs and treats them with dignity. Too many older people are facing unnecessary barriers because staff aren’t trained, services aren’t joined up, and outdated attitudes persist.”
Guillaume Favier, Partner, Healthcare and Life Science Strategy at KPMG UK, said: “Remarkable advances in HIV treatment now mean that people living with HIV can enjoy the same life expectancy as those without, and there’s an inspiring shift towards effective prevention. Yet, as this community ages, it’s vital that our health and social care systems adapt in tandem to meet their evolving needs.”
The full report, Towards an inclusive and integrated approach to care delivery for people growing older with HIV, is available on KPMG UK’s website.
Excelcare recently hosted a very special celebration in honour of Julia Tant, a lifelong artist who lives at Westport Care Home.
Julia has dedicated her life to art, and had her extraordinary work displayed in several galleries. Her passion for creating continues to shine, and when her artwork was recently featured in a companywide email, it caught the attention of Chief Operating Officer, Sam Manning. So inspired by her talent, Sam purchased four of Julia’s pieces to be displayed proudly in the wellbeing room at Excelcare’s Support Office, which were unveiled by Excelcare’s CEO, Ozzie Ertosun:
“Julia is incredibly artistic. Many years ago, Sam and I were doing an audit at Westport when we noticed someone had been drawing on all the walls — and it turned out to be Julia! We thought we might be looking at the future Banksy. Julia has been drawing for most of her life, and her passion for art shines through in everything she does. She’s had her work displayed in galleries and even written to Buckingham Palace! We’re so privileged to have her as part of our community, and we’d like to thank her for sharing her incredible talent with us all.”

Julia’s work has left an indelible mark on the London art scene. Known for her compelling portrayals of women, LGBTQ+ identities, class, and childhood, her art challenges societal norms and invites viewers to engage in meaningful dialogue.
Her artistic journey began later in life; she did not attend art school until the age of 45 and completed
her degree in Fine Art and Critical Studies from Central Saint Martins at 50. Despite starting her formal education later than most, Julia’s commitment to her craft is evident in her extensive exhibition history. Her work has been displayed in various venues, including galleries, restaurants, and shops, embodying her belief that art should be accessible to all. This philosophy is encapsulated in her mantra: “Put the art where the people are, as well as get the people to go where the art is” (loughboroughjunction.org).
Beyond her artistic endeavours, Julia Tant has been a fervent advocate for social change. She played a pivotal role in organizing the first Women’s Liberation Conference in the UK and was instrumental in saving the Carnegie Library from closure in 1999. Her activism reflects a deep commitment to community and cultural preservation.
This recent celebration was a joyful gathering of team members and friends, filled with creative activities, delicious snacks, and artistic inspiration. The highlight of the day was the unveiling of Julia’s artwork, a touching moment that reflected the gallery experiences she has cherished throughout her life.
It was a truly memorable day, celebrating not only Julia’s incredible talent but also her lifelong love of art. Her work will now continue to inspire all who visit the Support Office, immortalising her artistic legacy for years to come.

In today’s highly regulated health and social care environment, providers face the dual challenge of ensuring compliance while striving to deliver safe, high-quality, and commercially sustainable services. Care Inspections UK Limited (CiUK) has emerged as a trusted partner in this landscape, providing a professional and independent inspection service that goes beyond the standard requirements of the Care Quality Commission (CQC), The Care Inspectorate Wales (CIW) and the Care Inspectorate (Scotland), collectively “The Inspectorates” What sets CiUK apart is its status as a registered inspection body, operating with the highest levels of professionalism and governance. This official recognition imbues care providers with confidence that inspections are carried out with rigour, objectivity, and an unwavering focus on evidence. Every report is underpinned by validated, research-based methodology, ensuring the outcomes are credible, balanced, and practical.
BEYOND CQC/ CIW/ CI STANDARDS
While CQC/ CIW/ CI inspections focus on fundamental areas such as safety, effectiveness, responsiveness, and leadership, CiUK’s approach extends further. Each CiUK inspection covers all the domains CQC/ CIW/ CI would expect, but also incorporates additional layers of analysis essential for continuous improvement. This Includes:
• Operational risk management involves identifying risks before they become incidents, reducing exposure for service users and providers.
• Quality enhancement: Assessing opportunities to raise standards in care delivery, staff engagement, and governance.
• Commercial sustainability: Offering insight into how operational practices influence financial performance, helping providers balance compliance with business viability.
The result is an inspection report that is not only regulatory-ready but also a strategic tool for improvement.
Professionalism is at the heart of CiUK’s ethos. Inspections are conducted by highly experienced professionals who bring frontline expertise from clinical, managerial, and governance roles in the care sector. This depth of knowledge allows CiUK to deliver meaningful feedback that resonates with staff at every level, from frontline carers to boardroom directors.
Independence is equally vital. As an external registered inspection body, CiUK reassures providers that its findings are unbiased and transparent. In a sector where credibility matters, this impartiality is invaluable in preparing for CQC inspections and demonstrating accountability to commissioners, investors, and the wider community.
Care providers today operate in an environment of heightened scrutiny and rising expectations. CIUK’s inspections do more than highlight compliance gaps; they provide a clear roadmap for reducing risk, enhancing quality, and driving organisational improvement.
By identifying weaknesses early, providers can take corrective action before issues escalate. At the same time, CiUK’s focus on strengths and opportunities supports a culture of positive development. This balanced approach ensures that inspection outcomes are constructive, not punitive, fostering continuous organisational improvement.
One of the most overlooked aspects of care provision is its commercial dimension. Poor compliance and weak governance inevitably carry financial consequences, from reputational damage to contract loss. CiUK recognises this and integrates commercial insight into every inspection. CiUK helps providers achieve operational excellence and commercial resilience by aligning care quality with business performance.
THE CIUK DIFFERENCE
Choosing Care Inspections UK Limited means selecting a partner committed to professionalism, independence, and comprehensive excellence. CiUK inspections do more than prepare organisations for regulatory visits—they empower providers to deliver safer, higher-quality care while protecting their reputation and commercial future.
CiUK delivers evidence-based assurance and actionable insight for providers who want more than compliance.
The number of care home patients aged 65 and over in England receiving NHS prescriptions has increased, according to new 2024/25 estimates published by the NHS Business Services Authority (NHSBSA).
The NHSBSA’s primary care prescribing patterns report for patients aged 65 and over shows that an estimated monthly average of 331,000 care home patients received NHS prescriptions, up from 323,000 in 2023/24.
These patients received an estimated 42 million prescription items at a drug cost of £410 million in 2024/25, compared to 40 million items costing £396 million the previous year.
The report reveals that care home patients aged 65 and over received a higher rate of prescribing than non-care home patients. This includes medicines associated with a risk of falling and anti-cholinergic burden –the combined side effect risk from drugs that interfere with memory, alertness, and movement.

However, they received less prescribing of medicines associated with kidney injury. OTHER KEY FINDINGS INCLUDE:
• Care home patients aged 65 and over were more likely to receive vitamin D and pain relief medications, whilst non-care home patients were more likely to receive Atorvastatin – a medicine that lowers cholesterol in your blood to help prevent heart problems like heart attacks and strokes.
• The total drug cost for paracetamol has doubled over the last five years to an estimated £22.4 million for care home patients aged 65 and over.
• Almost two-thirds of care home patients aged 65 and over who received prescriptions were female, with just over four in 10 of all care home patients being females aged 85 and over.
THIS YEAR’S REPORT INCLUDES NEW FEATURES SUCH AS:
• geographical breakdown of overall prescribing
• new anticoagulant prescribing metric
• comparison of prescribing metrics by estimated care home length of stay
The NHSBSA estimates provide insights at both national and local level, showing trends over time and variation for key prescribing metrics.
The full report is available at: https://nhsbsa-data-analytics.shinyapps.io/estimated-prescribing-patterns-for-care-home-patients/
A spritely great grandmother from Basingstoke celebrated her milestone 107th birthday with family, friends and the team at her Sanctuary Care home.
Born at University College Hospital in London, Doris grew up in Wood Green and spent her early years in the capital. Her first job was as a typist for a film company in Soho, but her favourite role was working in administration for the NHS.
In 1941, Doris married her first husband, Sidney, whom she met at his father’s tea shop. Sidney served in Africa with the Grenadier Guards, and the couple endured four years apart during the war. Doris vividly recalls a doodlebug landing on her kitchen roof and fondly giggles when speaking of “handsome men in uniforms” and the days when men dressed smartly in hats.
Later in life, Doris travelled extensively with her second husband, Ron, visiting destinations such as New Zealand, Singapore, San Francisco, and the Bahamas. She eventually retired to Lowestoft, Suffolk, where her passion for gardening even earned her a feature in a gardening magazine. Doris moved to Alton, where she lived for 20 years before moving to Basingfield Court last year.
Despite her many adventures, Doris still has one daring ambition: skydiving.

“What is there to tell? I’ve always wanted to jump out of an aeroplane; in fact I’ve always wanted to do a lot of silly things,” she laughs.
Doris has always been active – from playing hockey as a girl to cycling throughout her life. She proudly notes that she has never smoked, saying, “It simply wasn’t one of my vices – in fact I’ve never really had any vices!”
Today, she remains very active, joining in with exercise sessions at the care home, choir practice, animal visits, bingo, and socialising with her fellow residents. Family has always been central to Doris’ life. She is the proud mother of two children, with five grandchildren and nine great-grandchildren.
When asked about her outlook on life, Doris reflects: “Well life has all sorts of highs and lows, but I take them all as they come.” She adds, “You just need to mind your own business, keep yourself to yourself, and take each day as it comes.” And with a smile, she quotes another famous Doris: “Que sera sera.”
Doris celebrated her special day with a tea party at the home, with a special visit from the Mayor of Basingstoke and Deane, Councillor Colin Phillimore.

How technology-driven engagement is boosting morale, staff retention, and wellbeing in UK care homes.
In today’s social care environment, the pressures on providers have never been greater. Rising costs, recruitment uncertainty, and increasing expectations from families and the CQC are leaving many care homes stretched thin. Yet, amid these challenges, one innovation is quietly reshaping daily life for both staff and residents - the Mobii Interactive Projection System from OM Interactive.
Drawing on OM Interactive’s 2025 Nationwide Survey of care professionals, The Mobii in Care: Executive Insights 2025 reveals powerful evidence that interactive technology can do more than engage - it can rebuild morale, reduce workload, and help care teams deliver the quality of care they aspire to.
Care work is among the most rewarding professions, but it is also one of the most emotionally demanding. Many care teams report that introducing the Mobii has brought back a sense of joy, pride, and connection to their daily work.
“Staff feel able to offer a more meaningful experience for service users,” says Marion Hunt, Advanced OT/Sensory Lead at The Hatherton Centre, MPFT.
That feeling matters - because it directly supports staff retention and resilience. When staff see residents light up with engagement, they’re reminded why they chose care in the first place.
Most managers surveyed said the Mobii has made a positive difference to staff workload, reducing stress and freeing up time to focus on genuine interaction. “It’s very easy to set up and use, which frees up the team’s time to spend more time engaging in a group activity,” shares Celia Milton, Activity Champion at Anchor’s Limegrove Care Home.
For carers, it’s not just about having a new tool - it’s about having something that makes their day feel easier, more purposeful, and more connected.
ENHANCING WELLBEING FOR RESIDENTS AND STAFF
The impact on residents is equally remarkable. An overwhelming 90% of care homes said the Mobii has enhanced wellbeing and engagement for both residents and staff. Through light, sound, and movement, it brings interactive experiences directly onto any surface - sparking laughter, movement, and conversation.
“The residents who would seem lethargic and unalert would be revived when the therapeutic games are played,” explains Carolyn Weisey, Activities Coordinator at St Annes Care Home.
Even residents living with advanced dementia have shown renewed participation. “Increased participation, especially from our residents living with more advanced dementia,” adds Celia Milton.
For many homes, this shared experience creates a calmer, happier environment - one where relationships thrive, and residents and carers alike feel more connected. SUPPORTING CQC EXCELLENCE
In a sector where inspections and accountability are central, the Mobii also provides measurable support for achieving CQC excellence. Homes using the Mobii report improved outcomes within the “Caring” and “Responsive” categories - both areas where person-centred engagement is critical.
“It can be used for person-centred activities as there is something to suit all needs - and CQC love that,” says Colette Yuksel, Activities Coordinator at Stocks Hall Nursing Home Burscough.
This ability to provide inclusive, evidence-based engagement demonstrates a home’s commitment to meaningful care - something inspectors, families, and staff all value highly.
With the upcoming Immigration Bill expected to limit access to overseas care workers, providers across the UK face mounting pressure to retain and support their teams. Recruitment challenges, rising agency costs, and burnout are creating a perfect storm - one that demands creative, proactive solutions.

The Mobii offers exactly that. It simplifies activity planning, empowers staff to deliver more meaningful sessions, and helps build a workplace culture centred on pride, teamwork, and connection.
As Katherine Huntley, Activities Lead at Dewdown House, puts it:
“Staff love playing with this alongside the residents - it really helps with bonding.”
Real-World Results from UK Care Providers
The survey findings speak for themselves:
• 94% said the Mobii enables more quality time with residents.
89% saw improved mood and interaction.
81% reported enhanced wellbeing and engagement.
90% saw improved memory recall.
93% would recommend the Mobii to other care providers.
These numbers reflect what many care professionals already see every day - a calmer, happier, more connected environment where both residents and carers can thrive.
TECHNOLOGY WITH HEART
As social care continues to evolve, the most successful innovations will be those that combine practicality with compassion. The Mobii proves that technology doesn’t have to replace the human touch - it can enhance it, helping carers do what they do best: connect, comfort, and care.
For care providers looking to strengthen staff wellbeing, enrich residents’ lives, and demonstrate excellence to the CQC, the question isn’t whether they can afford to invest in engagement technology.
It’s whether they can afford not to. For
or

Artificial intelligence is becoming part of everyday life and many residential care services are beginning to explore how it could support better care. When used responsibly, AI has the potential to reduce administrative pressure, give teams faster access to information and help staff make more informed decisions. But like any new technology, it requires careful planning, clear safeguards and open conversations with residents, families and colleagues.
At a recent roundtable hosted by Casson Consulting and the Access Group, care providers and digital specialists reflected on some of the opportunities and challenges facing the sector. The discussion echoed what we at Digital Care Hub hear from providers across the country. There is enthusiasm about using AI to free up staff time, improve consistency and spot risks earlier. Practical examples include tools that help identify trends in care records, digital assistants that help staff find policies quickly and early exploration of companion technology that could complement activity programmes. As Hallmark Luxury Care Homes noted, the aim is not to replace staff but to support them with the right information at the right time

Any use of AI in care relies on trust. Residential care is built on strong relationships, so residents, families
and staff must feel confident about why AI is being used and how their information is being protected. Katie Thorn, from Digital Care Hub and the Oxford Project: The Responsible Use of Generative AI in Care, highlights the importance of involving people at every stage. This includes explaining what a tool does, how decisions are made and how staff will continue to use their professional judgement.
A key theme from the roundtable, and from our wider work, is the need to recognise the limitations of AI. These systems can reflect the biases in the data they are trained on, so staff should be supported to question outputs rather than assume they are always correct. Good training, clear policies and safe channels for raising concerns are essential. Sharing examples where AI has not worked well is just as important as sharing successes. This helps the whole sector build confidence and avoid repeating mistakes.
Introducing AI into a residential care setting is not about rushing. It is about moving safely and purposefully. With the right digital foundations, strong governance and meaningful involvement of residents and colleagues, AI can become a valuable support for thoughtful, person-centred care.
For further information on Digital Care Hub and how they can help you, see the advert on page 37.
HC-One’s Sedgley Court Care Home in Dudley, West Midlands marked the official opening of The Sedgley Arms, unveiling its warm and welcoming new bar space designed to bring residents, families and the wider community together.
The launch event embodied everything the bar promises to be, “a hub of laughter”, filled with joy, connection and cherished memories. Residents were treated to a live performance from a crooner singer, capturing the smooth vocals and timeless charm of 1920s to 1950s classics from icons such as Sinatra and Crosby. The nostalgic theme continued with a drinks menu inspired by residents’ favourite beverages from years gone by, including Cherry B, Snowballs, glass-bottled Coca-Cola and a variety of alcohol-free options.
Guests also enjoyed a wide selection of treats, soft and hot drinks, as well as traditional pub games including darts, cards and dominoes,

which further brought the lively pub atmosphere to life.
Designed with resident wellbeing at its heart, The Sedgley Arms offers social, emotional and mental health benefits by providing a space for meaningful interactions, friendship building and inclusive activities.
Already, the space has sparked heartwarming moments where residents can “come alive” in the pub setting, reconnecting with a part of themselves they cherish. Residents joy captured the spirit of what the bar aims to achieve: belonging, confidence and connection.
Home Manager Emma Chaffe said: “We are thrilled to open The Sedgley Arms. It’s more than just a bar, it’s a space where residents can enjoy companionship, engage in stimulating activities, and create joyful memories with friends and family in a warm and inviting atmosphere.”
When Spring Grove Care Home in Hampstead undertook a major wet room refurbishment programme, the challenge wasn’t just to modernise. It was to do so without disrupting the daily lives of residents. With 46 en-suite bathrooms to upgrade, traditional tile-based installation methods posed clear limitations: long downtime, specialist trades, and significant disruption.
Springdene Group, which operates the care home, turned to Multipanel, the UK’s leading bathroom wall panel brand. Its rapid-installation system enabled each bathroom to be completed in just 1.5 days. For care home operators and specifiers working in live environments, that turnaround is more than a number. It is a strategic advantage.
THE INSTALLATION CHALLENGE IN LIVE CARE SETTINGS
Spring Grove is home to residents living with Alzheimer’s and other forms of dementia. Routine and consistency are essential in this setting. In any live-in care environment, prolonged bathroom refurbishments can be distressing for residents and difficult to manage operationally.
The key to Springdene’s approach was finding a wall surface solution that delivered on performance, appearance and speed. Tiling was ruled out early in the process due to the disruption it causes. Long curing times, noisy wet trades and ongoing grout maintenance were all barriers to efficiency. In contrast, Multipanel’s wall panel system provided a fully waterproof, grout-free alternative that could be installed quickly by a team of multi-skilled tradespeople.

Each bathroom was completed in just 1.5 days from start to finish, allowing entire floors to be refurbished in a matter of weeks rather than months. This helped keep disruption to a minimum, allowing residents to stay in their rooms or return swiftly.
COMBINING
For Springdene, speed was only one part of the equation. The visual appearance of the finished bathrooms also played a crucial role. The team was keen to avoid the clinical or institutional look often associated with healthcare environments. Instead, they wanted a modern, hotel-style aesthetic that felt calm, comfortable and familiar.
Multipanel’s tile-effect panels provided the perfect solution. With clean lines and smooth, gloss surfaces, the panels helped create stylish bathrooms that felt bright and contemporary. The result was a space that improved the daily experience of residents and supported a high standard of living.
“Mutipanel allows the care home to move away from an institutional aesthetic without compromising on hygiene or durability,” said Jamie Sandilands, Specification Sales Director at Grant Westfield, manufacturer of Multipanel. “The installation speed surprised even experienced contractors on-site.
Being able to complete each bathroom in just 1.5 days is a game-changer for care home refurbishment projects.”
Beyond speed and style, the refurbishment also had to meet the requirements of inclusive design. Each bathroom needed to be safe and accessible for users with a range of mobility and cognitive needs.
Slip-resistant vinyl wet room flooring was combined with Multipanel’s waterproof wall panels to create level-access, easy-to-navigate spaces. The design meets both Lifetime Homes and accessibility standards, ensuring long-term safety and usability.
Multipanel panels also reduce long-term maintenance. With no grout and a smooth surface, they are simple to clean and resistant to mould or moisture ingress. This minimises the time staff spend on repairs or deep cleaning, allowing them to focus on care delivery.
The project began with a free trial bathroom installation, provided as part of Multipanel’s specification support. This included complimentary product supply, installation and onsite training led by a trained installer.

The trial gave Springdene the chance to evaluate the product in real conditions and train their trades team at the same time. Following its success, 12 rooms were refurbished, with a further 12 scheduled. The group is now planning similar upgrades across its other care homes, Springview in Enfield and Spring Lane in Haringey, covering nearly 120 rooms.
For architects, developers and specifiers working in healthcare, retirement living and supported housing, Spring Grove’s approach offers a proven model for fast, specification-led refurbishment.
Multipanel panels are five times quicker to install than traditional tiles. Their 30-year warranty, FSC certification and EPD credentials make them suitable for projects with performance, compliance and sustainability targets.
As the care sector continues to face rising demand and operational pressure, solutions that combine design, efficiency and compliance are increasingly important.
“The Spring Grove project is proof that you don’t have to compromise on aesthetics or performance to gain speed,” said Jamie Sandilands. “Our approach allows specifiers to deliver contemporary, durable bathrooms that work for everyone - residents, staff and operators alike.”
EXPERIENCE IT FOR YOURSELF
Multipanel’s Free Trial Scheme allows care providers and specifiers to experience the installation, performance and support service first-hand before committing to a full rollout.
For more information, visit www.multipanel.co.uk or contact the specification team to discuss upcoming projects. 0131 290 286.
The National Care Forum (NCF) has announced the appointment of two new board members at its AGM today.
Professor Vic Rayner OBE, Chief Executive Officer, said: “Many congratulations and a big welcome to Alison Beachim, CEO of New Outlook Housing Association & Vision Homes Association and Jonathan Palmer, CEO of Somerset Care as they join the NCF board. The expertise and breadth of knowledge of these new board members, combined with the continued commitment and support provided by the existing board will further equip NCF to represent not-for-profit care provision at a time when our members, and the wider adult social care sector, continues to operate under considerable strain.
“We extend our sincere thanks to Rob Martin, who served as a board member in his former role as Managing Director Care Services at Anchor, and Maxine Espley, Chief Executive at Hightown Housing for their many years of support as they step down from the board.” she concluded.

The new board members join the existing board which comprises Andy Cole of Royal Star & Garter (Chair), Sarah Clarke-Kuehn from Sanctuary, Rachael Dodgson of Dimensions, Jim Kane from Community Integrated Care, Oona Goldsworthy of Brunelcare, Dan Hayes of The Orders of St John Care Trust, Brian James from Cedarmore Housing Association, Maria Mills of Active Prospects, Martin Rix from Belong and Alison Waller of Corserv Care.
NCF members heard from Chris Badger, new Chief Inspector for Adult Social Care at the Care Quality Commission who provided an update on the progress that CQC are making on its improvement journey. He shared the CQC’s latest position on strategic development, with a focus on the adult social care sector, progress on the work to scale the volume of inspections and resolve registration delays, the plans to refine the assessment approach and how CQC plans to make assessment judgements and determine ratings.
Nine caregivers from across the UK have formed the Home Care’s Got Talent Choir to create a new version of Robbie Williams’ ‘Angels’ in a bid to take the charts by storm and become this year’s Christmas No.1.
The caregivers recorded their rendition of the 90s classic at the legendary Abbey Road Studios, joining the long line of music legends who have performed there over the years. The iconic location also serves as the backdrop for the single’s music video which offers a behind-the-scenes look at the recording as well as videos of the caregivers with their clients.
Several famous faces have also shared their talents for the project having joined the Home Care’s Got Talent judging panel earlier this year. Musician Kuill from The Voice, Married at First Sight’s Matt Jameson as well as Bucks Fizz star Jay Aston have contributed to the single.
The caregivers travelled from as far away as Scotland and North Wales to take part, representing home care providers Caremark, Home Instead, Voyage Care, Visiting Angels, Mochridhe, Vitality Care and Calon Lan Community Care. With the support of the public, they believe they can surpass the original version’s chart success from 1997 and go all the way to No.1.

Alongside raising awareness of the incredible work caregivers do to support clients in the comfort of their own homes, the single has another positive purpose at its core. All profits raised by the single’s downloads will be donated to the Care Workers’ Charity. The charity is dedicated to supporting the social care workforce, those providing care and support to the million+ people drawing on social care. In particular, they provide crisis support, mental health initiatives and advocacy for fair treatment, pay and recognition.
Dan Archer, UK CEO of in-home care company Visiting Angels and founder of Home Care’s Got Talent said: “This wild idea came about following this year’s Home Care’s Got Talent final. I was challenged to create a Christmas No.1 using the brilliant singers that we’d found over the last two years from the competition. Robbie’s ‘Angels’ seemed like the perfect fit. When you listen to the lyrics, they speak to what carers do ‘and through it all, she offers me protection’!
“The journey to get here has been brilliant. Not only do we have nine brilliant care workers in the choir, but we’ve also had the support of industry heavyweights to bring this together.”

Relatives of residents who have died in Royal Star & Garter Homes have praised the love and support they have received from the charity through its new bereavement project.
Royal Star & Garter has been working with family members to shape the support it offers when they are bereaved. As a result, the charity has introduced new initiatives within its Homes to help those affected by loss, including creating a bereavement booklet, which offers practical help and emotional support to grieving relatives.
The impact it is having is being shared as part of National Grief Awareness Week, which is running from 28 December.
Royal Star & Garter provides loving, compassionate care and support to veterans and their families, living with disability or dementia, through its Homes in Solihull, Surbiton, High Wycombe and Worthing. It also has other services reaching out into the community.
The charity is helping support grieving relatives through its newly developed bereavement programme, which was developed with the support of a significant grant from the Armed Forces Covenant Fund Trust. Each Home now has a Heavenly Postbox, where grieving relatives can write letters to their loved ones on seed-embedded note paper, which are later planted in the Homes’ gardens.
Some of their Homes are now also hosting in-person groups and gatherings for bereaved relatives. They also provide books to support those affected by loss, and work with healthcare professionals and external organisations to signpost and ensure the effective delivery of support. Each Home also has an ‘In Memory’ book for residents, relatives and staff to leave messages about those who have died.
In High Wycombe, Remembrance butterflies, inscribed with a resident’s name, can also be placed in a specially created Reflective Garden.
Michaela’s father Peter was a resident at the High Wycombe Home. She was pleased to be invited to a relative group gathering but felt some trepidation before attending. However, Michaela said: “From the moment I walked in I was made to feel very welcome. I was asked to place Dad’s remembrance butterfly in
the Reflective Garden, which felt wonderful.” Her sister has also attended subsequent gatherings, and Michaela added: “It is wonderful to hear other families showing the love that I also have for the charity. We feel very honoured to be part of the Royal Star & Garter family.”
For Liz, whose mother Kitty lived at High Wycombe, seeing tributes written in the ‘In Memory’ book brought solace. She said: “Reading all the lovely messages gave me great comfort. I know Mum has not been forgotten and she was loved.” She continued: “I now find it easier to look beyond what happened. I am not so upset, I have a feeling of happiness, and the sadness has been lifted from me.”
John died at the Solihull Home in 2024, where he had lived with his wife Margaret. She has written letters on seeded paper which were planted in May, and she looks forward to watching the flowers bloom from her words of love and remembrance. Margaret goes to the garden for “peace and reflection” and said: “It’s somewhere I can just sit and think of my John. I close my eyes, and I remember him and the good times dancing and laughing.”
Chrissie Morris, who has been leading the work said: “We hope that by providing bereavement support it will help families navigate their grief and encourage them to access valuable bereavement support if needed. Relatives are part of the Royal Star & Garter family. Some come to regard the Homes as an extension of their own home, and the staff and other residents as an extension of their own family. Our bereavement support helps maintain this relationship. I’m delighted we are now able to provide this vital support to those who need it.”

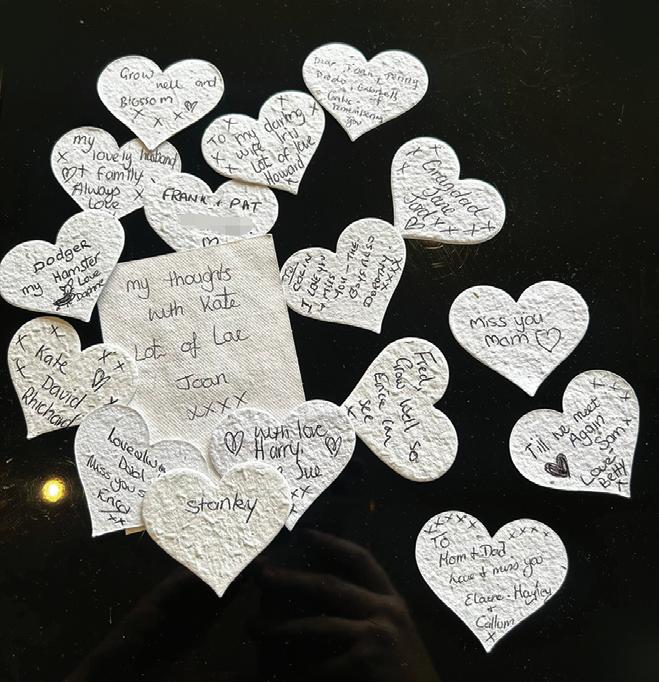
Family, friends and community well-wishers sent more than 100 birthday cards to help a Winchester dementia care home resident celebrate her centenary.
Olwen Davies was the delighted centre of attention as she enjoyed a 100th birthday tea party at Colten Care’s St Catherines View.
She welcomed a host of guests including daughter Jennifer, a son who travelled from France and civic visitors the Mayor of Winchester, Sudhakar Achwal, and his wife, fellow councillor and former Mayor, Vivian Achwal.
The deluge of cards was boosted by a community Facebook appeal issued by St Catherines View Companionship Team Leader Laura Sheldrake.
It resulted in Olwen receiving 116 cards from well-wishers across England and Wales.
Laura said: “Olwen had one wish for her milestone birthday: to celebrate it

with her family and friends. We were pleased and privileged to help stage a tea party in her honour.
“As well as her nearest and dearest, she loved chatting with the Mayor and seeing his Mayoral chain which at one point he took off for her to have a closer look at.”
Asked about her secret for a long and happy life, Olwen replied: “A loving family!”
On the birthday celebration itself, Olwen said: “I can’t believe the Mayor came. He was lovely and wished me a happy birthday.”
Daughter Jennifer, a regular visitor at St Catherines View, described her mum’s 100th birthday as ‘such an achievement’, adding: “She is a remarkable lady who is loved by all who meet her. We thank the staff at St Catherines View for giving her such a wonderful day.”
A care home in Godalming held a right royal knees up to mark a special anniversary.
Care UK’s Jubilee House, on Pound Lane, welcomed the guest of honour, the Mayor of Godalming, Councillor Bob Crooks, along with members of the community, to celebrate the home’s 25th birthday with a Royal-themed tea party.
On the day, team members and residents dressed to impress, and the home was decorated with regal bunting, balloons and decorations.
Guests enjoyed tea, scones and a delicious buffet, crafted by Head Chef, Rodrigo Cid – making everyone feel as if they had stepped into Buckingham Palace on a Sunday afternoon.
Resident Penny Hill said: “I enjoyed every moment of the 25th birthday of our home, I have loved living here over the past few years!”

Nealsen Veerasawmy, Home Manager at Jubilee House, said: “It’s been fantastic to celebrate our 25th birthday in style – with a party fit for a king – from the music to the decorations, and of course the wonderful food.
“It certainly has been a busy 25 years! We’ve welcomed some real characters to the home, built relationships with brilliant local organisations, and worked hard to create a homely environment for everyone who spends time with us here at Jubilee House.
“I’d like to extend a huge thank you to our dedicated team for making Jubilee House a wonderful place to call home.
Hosting community events is our favourite way to connect with the local people, and the guests made it such a memorable birthday!”
Merceode Lodge, a new, purpose-built residential and dementia care home set to open in Marchwood in the new year, has announced the appointment of Helen Chapman as its General Manager.
Helen is an accomplished professional with extensive experience as a Regional Manager, Operations Manager, and CQC Registered Manager within the Adult Social Care and Healthcare sectors.
Helen’s commitment to excellence has consistently resulted in “Gold Standard” service and improvements in quality outcomes across the care homes she has supported. Helen is particularly passionate about wellbeing for both residents and colleagues and has introduced a range of initiatives within previous roles to promote holistic support. Her vision for Merceode Lodge is to build a nurturing environment where residents can

empowered to deliver the very best care. Helen said, “I’m thrilled to be leading Merceode Lodge as we prepare to open our doors. My passion has always been creating environments where residents, families, and team members can thrive. I believe wellbeing and community should be at the heart of everything we do, and I’m excited to build a home that reflects that.”
With an all-inclusive approach, Merceode Lodge will ensure peace of mind for residents and their families, with no hidden bills or unexpected costs.
Merceode Lodge will provide high-quality residential and dementia care for up to 66 residents. Every bedroom will be ensuite, and residents will be able to enjoy a wide range of facilities including a cinema room and an on-site hair salon.

Residents at Bullsmoor Lodge Care Home in Waltham Cross are discovering the benefits of mindfulness through new monthly “Namaste Sessions” – gentle, therapy-inspired gatherings designed to promote relaxation, emotional connection and wellbeing, particularly supporting residents living with late-stage dementia.
Under the supervision of Care Home Manager Lisa Coombs, the programme takes a sensory-first approach to enhance residents’ quality of life. By combining soothing music, mindful breathing, gentle movement and sensory therapy, the sessions aim to create a calm and restorative environment that supports a person-centred approach to wellbeing.
The Namaste sessions are designed for older adults, to help them to slow down, reconnect, and experience moments of peace and comfort. The sessions are also tailored ensuring that all residents – regardless
of mobility or cognitive ability – can take part and benefit.
Lisa said: “Our Namaste sessions have quickly become a highlight of the month. They offer residents time to pause, reflect and feel grounded. We see smiles, calmness, and even improved social connection afterwards – it’s a simple yet powerful practice that truly supports wellbeing.”
The monthly mindfulness and therapy sessions are part of Bullsmoor Lodge’s ongoing commitment to providing holistic care –addressing not only physical health but also emotional and mental wellbeing.
As more care homes embrace the benefits of mindfulness and sensory therapy, initiatives like this reflect a growing movement towards compassionate, person-centred care that honours the whole individual.

Home adaptations teams have a unique tool to help expediate fast, efficient aids to help people be safe at home.
The number of, and wait time for, adaptations continues to grow, with stairs being the second most common hazard in the home. In conjunction with Occupational Therapists, AAT has developed its Universal Seat System for its brand-leading S-Max Sella stairclimber.
The combination amplifies adaptations teams’ ability to optimise use of budgets- usually without even requiring DFG funding- to deliver a safe stairway transfer solution within days, by recycling (re-issuing) the equipment.
The S-Max Sella provides a safe stair transfer solution in 99+% of cases which AAT assesses. The portable Class 1 Medical device certified kit requires no installation nor structural alteration to the home. The addition of the Universal Seat System means the Sella can be easily set up to ensure almost every potential user is safe and supported when using the Sella, irrespective of their physical and/or mental impairment. It is achieved without the need to purchase extra accessories. No other stairway transfer system offers such flexibility.

HipSaver Soft Hip Protectors protect the elderly and disabled people from fall-related hip fractures. Designed to protect elderly people from fall related hip fractures, HipSavers are a leading brand of soft hip protectors. Used in the NHS since 2002, HipSaver Soft Hip Protectors are user friendly, affordable and costeffective personal protective garments. Soft, comfortable, effective and compatible with incontinence protection, HipSaver Soft Hip Protectors are perfect for use in care homes and by elderly people living independently.

Available as comfortable underwear or long casual pants in several sizes for men and women,
HipSavers feature soft protective airPads permanently sewn into the garments over the hip areas prone to injuries and fractures.
HipSaver TailBone models have an additional protective airPad over the coccyx on lower back for protection during swaying, accidental knocks, bumps and backward falling. Machine washable at high temperature and tumble drier friendly, HipSavers are practical, hygienic and durable.
HipSavers should be worn day and night for 24 hour protection and especially during physical and recreational activities, when accidental falls, slips and trips can lead to hip fractures.
HipSaver Soft Hip Protectors - affordable protective garments for the elderly and disabled people! For more information, contact Win Health Medical Ltd - 01835 864866 - www.win-health.com See the advert on page 3 for further products.
At Blue Rain, our mission is simple: to provide everyday activity products that spark joy and enrich lives — whether for those who need a little extra support, a burst of motivation, or simply a reason to have fun.
We take pride in listening to our customers, understanding what truly matters to them, and sourcing or creating products that meet those needs perfectly. Many of our items are available as ready-to-go activity kits and bundles — complete with everything you need — so

you can skip the preparation and focus on the joy of the moment.
As Blue Rain Activity Store continues to grow, our heart remains the same: creating meaningful moments of happiness, connection, and creativity for people of all ages and abilities.
From rainy-day craft sessions to sunny outdoor adventures — or simply time spent together — we’re here to make every experience easy, special, and unforgettable.
See the advert on page 6 for further information.

Repose Furniture is one of the UK’s leading manufacturers of bespoke seating solutions, with a reputation built on craftsmanship, innovation, and a strong commitment to improving the quality of life for its customers. Established in 1999 and based in the West Midlands, the company has grown from a small family business into a trusted supplier to both the domestic and healthcare markets. Every chair produced by Repose is handmade in the UK, with an emphasis on quality, durability, and comfort, ensuring that each product meets the specific needs of its user.
Whether for home use or demanding healthcare environments, Repose combines skilled upholstery techniques with modern engineering to create chairs that provide postural support, pressure management, and ease of use. Their wide product portfolio includes rise and recline chairs, hospital and care home seating, bariatric solutions, and specialist products designed to address particular medical and lifestyle needs. An essential element of their offering is flexibility: customers can choose from a range of back styles, seat cushions, mechanisms, and fabrics, allowing each chair to be tailored to the individual. Interchangeable parts mean that a chair can adapt as a user’s requirements change, extending the product’s longevity and ensuring value for money. The healthcare sector is a particular area of expertise for Repose. They strive to design chairs that balance comfort with clinical functionality. Features such as tilt-in-space mechanisms, adjustable cushioning, and pressure relief options make their healthcare seating particularly suited to long-term use in hospitals, hospices, and
As part of the offering, AAT will also support the adaptation team in the assessment process, to ensure the relevance of the solution for the person, the occupation and the environment, and personally train the carer in the Sella’s safe operation.
“We have numerous examples of community equipment services (eg Nottinghamshire & Nottingham City) now buying not just additional Sella stairclimbers, but Universal Seat Systems, to have in equipment stores ready to go, so they can quickly deliver a solution for a client,” says Peter Wingrave, AAT Director.
“Even if it is a short-term solution whilst a larger and/or more permanent adaptation is undertaken, our Sella/Universal Seat System and re-issue capability gives a highly costeffective and fast way to manage the potential risk of someone falling on the stairs: a genuine adaptation without delay.”
Full details of the Sella and Universal Seat System can be found on AAT’s website @ https://www.aatgb.com/s-max-sella/ where adaptations teams can also book a free, no obligation client assessment or team demonstration session.
Consort’s PLSTiE range of Low Surface Temperature (LST) fan heaters offers a safe, efficient, and modern heating solution. They are designed for environments where safety and comfort are paramount. With a maximum surface temperature of 43°C, these heaters adhere to the NHS Estates Health Guidance Notes standards, making them suitable for use in hospitals, care homes, schools, and nurseries.

The PLSTiE heaters are equipped with features such as intelligent fan control, open-window detection, and quiet operation, all of which contribute to
|
energy efficiency and comfort. Slim and splash-proof (IP24), they combine safety, performance, and flexible installation for various interiors. The PLSTiE WiFi models connect directly to the Consort Connect app, allowing remote control, scheduling, and energy monitoring. BIM downloads for the PLSTiE
Angloplas are a UK manufacturer who specialise in producing dispensers for the health and hygiene industry. Although these are designed to keep the workplace tidy and uncluttered they are, more importantly, built knowing the control of healthcare-associated infections (HCAIs) are a priority for healthcare providers, and who are employing a combination of infection prevention and control strategies, including hand hygiene, cleaning, training and the adoption of new technologies, to tackle the problem. As a result, a wide range of infection control products and technologies are emerging on the market, including antimicrobial technology. Angloplas’ range of dispensers are produced in the world’s first proven

Antimicrobial PVC with silver ion technology and which is exclusive to Angloplas. This helps reduce the risk of cross infection by stopping the growth of bacteria and mould and works continuously for the lifetime of the product, reducing levels of bacteria such as MRSA, E Coli, Legionella, Salmonella and mould by up to 99.99%.
For non-clinical environments Angloplas has recently launched its new Budget Range of products which are made to the same exacting standards as the antimicrobial protected ones but with lower price tags.
You can order Angloplas products directly from its website at www.angloplas.co.uk See page 4.

care homes. The company’s bariatric range demonstrates the same careful attention to detail, offering robust yet comfortable solutions for larger users.
While customisation is the centre of the Repose offering, they also recognise the urgency often faced in healthcare settings. To address this, Repose have developed their Healthcare Express Chairs, designed to deliver high-quality healthcare seating at speed. The models in this range can be despatched within just five working days. The Multi Bari Express and bestselling Boston Express, for example, are available on this five-day lead time, offering care providers a rapid solution without sacrificing quality or functionality. For less specialist needs, some homecare models are even available on faster turnaround times, demonstrating Repose’s ability to balance responsiveness with craftsmanship.
Repose’s reputation is further reinforced by its after-sales support, 5-year manufacturing warranty, and commitment to ethical and sustainable practices. With a UK-based factory, a dedicated distribution network, and close relationships with healthcare professionals, the company continues to be a trusted partner in multiple sectors throughout the country and beyond.
In combining bespoke design with reliable express options, Repose Furniture stands out as a manufacturer that truly understands the diverse needs of its customers. For over 25 years, it has delivered not just chairs, but comfort, dignity and independence — values that remain at the core of everything it does. For further information, see the advert on page 25 or visit www.reposefurniture.co.uk
By Zoe Cottrell, registered dietitian, member of
the British Dietetic Association and registered with the Health and Care Professions Council

Malnutrition remains a significant issue in care homes, where the elderly are particularly vulnerable. As a registered dietitian working in the community and in hospital wards, often with elderly people who have experienced fall, I wish more people knew about the prevalence of malnutrition and how to combat it before they ended up in hospital.
Recent statistics paint a stark picture: Around one in 10 people over the age of 65 are malnourished or at risk of malnutrition , and this figure rises alarmingly to 45% among those in their 90s. According to the British Association for Parenteral and Enteral Nutrition (BAPEN) , malnutrition costs the UK approximately £23.5 billion annually, with older adults being disproportionately affected.
As the population ages, addressing malnutrition and its associated complications, such as frailty and sarcopenia, becomes ever more critical. By focusing on early detection and strategic nutritional interventions, including the use of protein, care homes can play a vital role in safeguarding the health of their residents.

In the world of care catering, gravy is often an after though – adding some flavour and moisture to food but it can be nutritionally empty. At ProSauce, gravy is the starting point for a quiet revolution.
ProSauce Gravy is more than a condiment. It’s a nutrient-rich, flavourforward solution designed to meet the complex needs of care homes and hospitals. Developed by Stella West-Harling MBE, in conjunction with dietitians from the NHS and top UK universities, the gravy reflects lived experience and professional insight: meals should provide good nutrition and flavour, whilst being cost-effective.
Crafted for operational ease, ProSauce Gravy is shelf-stable, easy to portion, and compatible with diverse dietary needs. It delivers 12g of plant-based protein per serving, whilst being gluten-free and nutrient dense. Whether served in or over meat, or plant-based dishes, it
The first step in combating malnutrition is recognizing its early signs. The Malnutrition Universal Screening Tool (MUST) is a valuable resource for this purpose, enabling caregivers to systematically assess the risk of malnutrition in residents by considering factors such as Body Mass Index (BMI), unintentional weight loss, and the impact of acute illness on nutritional intake.
KEY EARLY SIGNS TO MONITOR:
1. Unintentional Weight Loss: A significant early indicator of malnutrition is unintentional weight loss. Regularly monitoring residents' weight and comparing it to previous measurements is essential. A loss of even 5% of body weight over a few months can signal malnutrition and warrants immediate attention.
2. Decreased Appetite: A reduced appetite is often a precursor to malnutrition. Residents may skip meals, eat smaller portions, or show a lack of interest in food. It's important to understand the reasons behind these changes, which could be linked to dental issues, depression, or medication side effects.
3. Physical Changes: Signs such as muscle wasting, thinning hair, dry skin, or dental problems may indicate nutritional deficiencies. These physical symptoms are often subtle but crucial indicators of potential malnutrition.
4. Fatigue and Weakness: Increased tiredness or difficulty performing daily activities can be related to inadequate nutrition. This could also signal the onset of sarcopenia, where the loss of muscle mass and strength makes everyday tasks increasingly challenging.
(CONTINUED ON THE FOLLOWING PAGE...)
makes supporting nutritional goals easy in a way that is familiar to the diners.
Early adopters are using ProSauce in care homes and hospices with feedback highlighting ease of use for kitchen staff and it’s cost effectiveness. With the additional protein in the gravy, chefs can use less meat in meals to reach the same nutritional standards, which in turn saves costs and improves the stainability credentials of the kitchen.
In a sector defined by improving health and care, whilst managing increasing costs, ProSauce Gravy offers possibility. It’s a small change with big impact: maintaining flavour, supporting health, and reminding us that every meal is an opportunity to care.
Visit the ProSauce website to order your free 20 portion sample box and experience how ProSauce Gravy can help transform mealtimes in care settings.
www.prosauce.co.uk


(CONTINUED FROM PREVIOUS PAGE)
THE ROLE OF NUTRITION IN PREVENTING AND MANAGING FRAILTY
Frailty, a condition characterized by decreased strength, endurance, and physiological function, is closely linked to malnutrition and is a major concern in care homes. Proper nutrition is key to preventing and managing frailty, particularly through the adequate intake of protein, which is essential for maintaining muscle mass and function.
STRATEGIES FOR NUTRITIONAL INTERVENTIONS:
1. Prioritize Whole Foods: Ensuring a diet rich in whole foods is foundational. Protein-rich foods like eggs, lean meats, fish, dairy products, and legumes should be emphasized, as they not only support muscle health but also provide essential vitamins and minerals that contribute to overall well-being.
2. Incorporate Protein Supplements When Necessary: In cases where residents struggle to meet their protein needs through diet alone—perhaps due to a lack of appetite or difficulty chewing—protein powders or fortified drinks can be effective. These supplements can be easily added to meals, snacks, or beverages, ensuring that residents receive the protein they need without overwhelming them with large portions of food.
3. Distribute Protein Throughout the Day: Research shows that distributing protein intake evenly across all meals is more effective for muscle protein synthesis than consuming large amounts at a single meal.
Caregivers should ensure that residents receive adequate protein at breakfast, lunch, and dinner to maximize the benefits for muscle maintenance and frailty prevention.
ADDRESSING BARRIERS TO ADEQUATE NUTRITION
While boosting protein intake is essential, we should also address the barriers that may prevent residents from consuming enough nutrients. Factors such as taste preferences, difficulties with swallowing, or digestive issues can all impact nutritional intake. Caregivers should work closely with dietitians to develop personalized nutrition plans that accommodate these challenges, potentially incorporating protein powders and other supplements in palatable and easy-to-digest forms.
NUTRITION IS KEY TO INCREASING HEALTHSPAN
Malnutrition in care homes is a pressing issue that requires vigilant monitoring and proactive management. While the numbers alone tell us the stakes are high, intervention is more than about reducing costs. The ability to stand up from a chair unaided allows our elderly residents independence. By spotting the early signs of malnutrition and implementing strategic nutritional interventions, caregivers can help prevent and manage frailty, significantly improving the quality of life for residents. By addressing malnutrition and frailty head-on, care homes can help residents not only avoid the adverse effects of these conditions but also thrive in their later years.
Disease-related malnutrition remains one of the most persistent challenges in UK residential and nursing care. It affects millions, increases vulnerability to illness, slows recovery, drives hospital admissions, and places strain on already stretched care teams. Yet despite the scale of the problem, the tools available to homes have not kept pace with the needs of increasingly complex residents.
Hiquid Food, a Norwegian medical nutrition company, is entering the UK market with a clear mission: to make effective nutritional support simpler, more acceptable for residents, and easier for staff to deliver.
Simple, seamless meal enrichment
Many residents struggle to consume enough calories and protein, even with carefully prepared meals. Hiquid Food’s freeze-dried powders, made from organic whole foods, allow caregivers to enrich everyday dishes like porridge, soups, puddings, purees, and drinks. This discreet approach reduces refusals and preserves dignity, helping residents receive the nutrition they need through meals they already enjoy.
ORAL NUTRITIONAL SUPPLEMENTS WITH HIGH ACCEPTANCE

For individuals at greater nutritional risk, Hiquid Food offers compact, nutrient-dense oral nutritional supplements designed for those with low appetite or increased medical demands. They are easy to con-
sume, well tolerated, and provide balanced support in small volumes.
WHOLE FOOD GASTROSTOMY NUTRITION
For residents requiring enteral feeding, Hiquid Food’s whole-food gastrostomy products offer a gentle, reliable option created with a focus on tolerance, safety, and long-term stability.
Better outcomes and operational efficiency
Care providers face rising acuity and workforce pressure. Hiquid Food products reduce complexity through easy mixing, no additives, and no large volumes while supporting improved resident strength, immunity, and recovery. Better nutritional status means improved wellbeing and lower overall care costs. With long shelf-life, low weight, and high versatility, the products are also environmentally responsible and easily integrated into a wide variety of meals.
As Hiquid Food launches in the UK through Food Untethered, they look forward to working closely with care homes, clinicians, and NHS commissioners to strengthen nutritional care in a practical, resident-centred way.
For more information: contact@fooduntethered.com
See the advert below for further information.

Care homes across the UK are transforming how they deliver care thanks to SyndoraAlto, the newly rebranded name behind CHARIS, the UK’s most advanced digital nurse call system.
Fully supplied, installed, and maintained from just £6.40 per bed, per month, CHARIS delivers smarter, safer, and more connected care through real-time alerts, mobile integration, and intuitive smart displays that help staff respond faster when residents need them most.
Every CHARIS system comes fully inclusive with 15” smart displays, help buttons, pull cords, guaranteed radio coverage, and 24/7 UK technical support, all backed by SyndoraAlto’s trusted installation and maintenance team.

For care providers not yet ready to replace their existing nurse call system, AltoEnhance offers the perfect first step into digital care.
Available from just £129.00 per month, AltoEnhance seamlessly connects to your current nurse call system, bringing digital reporting, mobile alerts, and actionable insights without the need for a full system upgrade.
“Technology should make care easier, not harder,” says Louis Johnson, Managing Director. “CHARIS and AltoEnhance connect people, information, and action empowering care teams to deliver truly person-centred care.” Meet the team & learn more at www.syndoraalto.com See the advert on the front cover for more information.
Alarm Radio Monitoring is the market leader in the design, manufacture and installation of bespoke, end-to-end, wireless alarm systems and solutions for the healthcare, leisure, custodial and education industries.
We have been providing wireless alarm and nurse call systems for over 30 years. Supplying care homes and hospitals with an essential lifeline that supports the delivery of outstanding care.
We believe in excellence which translates into: Advanced Technology Industry-leading wireless alarm technologies and software
Bespoke Solutions
We design systems to your needs rather than your team having to work around the system Innovative Design

Pushing boundaries with the reliability that comes from decades in the industry
Flexible Finance Options
Ensuring organisations of any size can provide safety for their staff and clients 24 Hours a Day, 365 Days a Year Service
Your ARM service team
Falls are a significant concern for vulnerable individuals, especially seniors and patients at risk. Medpage, a leader in assistive technology, offers a range of cuttingedge products designed to enhance safety and provide peace of mind for caregivers and families. Here’s an in-depth look at some of their standout solutions:
MPRCG1 (2023) BED LEAVING DETECTION ALARM WITH CAREGIVER RADIO PAGER
The MPRCG1 is a comprehensive system tailored for fall prevention in domestic, commercial, and NHS care settings. This all-inclusive kit includes a bed pressure mat sensor, a BTX21-MP alarm sensor transmitter, and an MP-PAG31 radio pager. The system is designed to alert caregivers when a patient leaves their bed, reducing the risk of falls. Key features include:
Wireless Alerts: Notifications are sent to the caregiver’s pager via tone or vibration.
Customizable Alarm Delays: Options for instant, 15-minute, or 30-minute delays.
Durable Design: Antimicrobial and disinfectant-resistant materials ensure longevity.
Ease of Use: Minimal installation required, making it user-friendly and portable.
HDKMB2 HOSPITAL DISCHARGE KIT FOR FALLS RISK PATIENTS

The HDKMB2 is a thoughtfully curated kit aimed at supporting patients transitioning from hospital to
home care. It includes essential tools to mitigate fall risks and promote recovery. This kit is ideal for caregivers seeking a comprehensive solution to enhance patient safety during the critical post-discharge period.
CMEX-21 MULTI-PORT WIRELESS SENSOR INPUT EXPANDER FOR NURSE CALL CONNECTION
The CMEX-21 is Medpage’s latest innovation, designed to integrate seamlessly with existing nurse call systems. This multi-port expander allows for the connection of multiple wireless sensors, enhancing the monitoring capabilities of healthcare facilities. Its versatility makes it a valuable addition to any care environment, ensuring timely responses to patient needs.
RON-WC2 WATERPROOF DISABLED PULL CORD ALARM TRANSMITTER WITH WIRELESS ALARM RECEIVER
The RON-WC2 is a robust solution for disabled individuals requiring immediate assistance. This waterproof pull cord alarm is ideal for use in bathrooms and other high-risk areas. Paired with a wireless alarm receiver, it ensures that help is just a pull away.
(CONTINUED ON FOLLOWING PAGE...)

The wireless ARM Nurse Call system has been developed over 30 years with both the client and user in mind.
It enables staff to efficiently answer calls, making the management of resources more flexible and provides the functionality you would expect of any nurse call system.
The system is quick and easy to install and works wirelessly, using radio communication between both the call points and the system infrastructure.
Data Analysis software provides a full audit trail of events
The all-new call logging software from ARM enhances the functionality of your care call system dramatically.
• It can help you track the quality of your service to your residents.
• It can help you demonstrate compliance with your aims and best practices, both to relatives and to authorities.
• It can help you find bottlenecks in service provision, track staffing requirements, and allow you to ensure staff are meeting expectations.
• Most importantly, it provides assurance that you know and can demonstrate what is happening in your care home.
Call messages can be sent direct to staff to speed up response times and can also be integrated to work with smart phones & messaging.
Courtney Thorne, a long-standing innovator in healthcare communication systems, is setting new standards in the care home sector with its advanced wireless nurse call technology—designed to improve resident safety, enhance staff efficiency, and support a more responsive care environment.
With over 30 years of experience serving the UK healthcare market, Courtney Thorne’s systems are now trusted by thousands of care homes nationwide. Unlike traditional hardwired solutions, their wireless nurse call systems offer non-invasive installation, scalability, and smart analytics—making them ideal for both new builds and retrofit projects.
“At the heart of our technology is the belief that better communication leads to better care,” says Graham Vickrage, Managing Director at Courtney Thorne. “Our wireless systems not only reduce response times but also empower staff with the tools they need to deliver safe, person-centred care.”
Care providers are increasingly choosing wireless systems for their flexibility, reliability, and cost-effectiveness. With a full suite of accessories—including neck pendants, door monitors, fall detection, and
bed sensors—Courtney Thorne systems can be tailored to meet the specific needs of each home and resident.
In an industry where compliance, safety, and staff pressures are always front of mind, Courtney Thorne provides more than just products—they offer ongoing support, training, and a commitment to innovation that helps care homes future-proof their operations.
For more information or to book a free demo, visit www.c-t.co.uk or contact info@c-t.co.uk.

(CONTINUED FROM PREVIOUS PAGE)
Features include:
Waterproof Design: Suitable for wet environments.
Wireless Connectivity: Reliable transmission to the alarm receiver.
Ease of Installation: Simple setup for quick deployment.
WHY CHOOSE MEDPAGE?
Medpage’s commitment to innovation and quality is evident in their product range. Each solution is designed with the user’s safety and convenience in
mind, making them a trusted choice for caregivers and healthcare providers alike.
By investing in these advanced fall prevention tools, families and facilities can create safer environments for those at risk. Medpage continues to lead the way in providing practical, reliable solutions that make a real difference.
For more information, visit Medpage’s official website or contact their team to explore these products further. Safety starts with the right tools, and Medpage delivers just that. www.easylinkuk.co.uk
T: 01536 264 869


Young people only make up 11% of care workers. When they’re the ones to pick up the mantles left by 25% of the workforce likely retiring within the next 10 years… it isn’t the most comforting news, especially when the care sector is already stretched so thinly.
We’ve previously discussed how you can attract the under-25s. But it isn’t just about recruiting young care workers. It’s about keeping them, too.
Care can already be an overwhelming career. So, imagine what it’s like when you’re first experiencing it. A lot of young care workers are dropped into the deep end, especially if it’s their first job in the industry.
Combine this with irregular, unsociable hours, and you have a recipe for burnout.
So, what can you do to keep Gen Z in the care sector?
First: training.
Despite qualifications, jumping into the real thing is something new entirely. Plus, since the typical care worker in the UK is aged 45, many vacancies are likely to be filled by those with extensive backgrounds in care. It’s possible, then, that more in-depth training could slip through the cracks for new carers.
It’s easy to get swept up in the waves of care’s responsibilities, whether you’re used to it or not. Offering new hires more in-depth training, ongoing support, and perhaps even a mentor can help them stay afloat amongst the workload.
Next: regular shifts and flexibility.
You may think routine and flexibility contradict each other, but they actually go hand-in-hand.
Burnout in shift work largely stems from poor work-life balance, resulting from staff having little to no control over when they work. Short notice of shifts, combined with irregular and unpredictable ones, leaves workers with a life revolving around work. Even for the biggest workaholics, having no time for a personal life doesn’t make for a healthy one.
Providing enough notice for shifts allows your team to plan around them. Offering rotating schedules and shift patterns also makes hours more predictable, meaning staff can plan even further in advance. (It’s easier for you, too!)
Things come up. Life happens. Ruling your rota with an iron fist gets you nowhere – apart from having unhappy staff.
Flexibility is often misconstrued as spontaneity, but it instead gives staff a voice. Allowing staff to set availability and arrange shift swaps immediately gives them that control they were missing.
You’ll agree that when you aren’t burned out or struggling with poor mental health, you’re better at, well, everything. You’re more productive, more motivated, and you care a lot more about what you’re doing.
This is what Gen Z prioritises. For that, they’re given a bad reputation – just like care gets a bad reputation for a poor work-life balance. But that doesn’t mean the two can’t work together.
By embracing what Gen Z prioritises, you’re not only attracting young care workers, but you keep them.
Decades down the line, who knows, maybe they’ll be the ones retiring and passing the mantle down to their younger counterparts.
www.rotacloud.com

Savers®. The NEW Fall Savers® Wireless eliminates the cord between the monitor and sensor pad. This results in less work for nursing staff, improved safety for patients and reduced wear and tear on sensor pads. Wireless advantages include the ability to use one monitor with two sensor pads simultaneously and support for many new wireless devices.
BENEFITS INCLUDE: Safer for patients; less work for staff
Bed and chair pads available
One monitor works with two sensor pads
Integrates with most nurse call systems
A variety of options, including: Call button Pager
The TreadNought® Floor Sensor Pad is built to last with a durable construction that far out lasts the competition. Our anti-bacterial floor sensor pad is compatible with most nurse call systems or can be used with a portable pager to sound an alert when a person steps on to the sensor pad. Caregivers typically place the sensor pad at the bedside, in a doorway or other locations to monitor persons at risk for falls or wandering. An optional anti-slip mesh reduces the potential for slippage on hard surface floors.
FEATURES INCLUDE:
Connects directly to most nurse call systems
High Quality anti-bacterial Floor Sensor Pad
Large Size Pad: Measures (L) 91cm x (H) 61cm
Options (sold separately):
Anti-slip mesh for hard surface floors
See the advert on this page for further details or visit www.fallsavers.co.uk.

Every day, care organisations are working tirelessly to deliver essential support in the face of growing needs and rising costs. However, too many providers are stuck balancing tight budgets, having ‘just enough’ to stay afloat. The hard truth is, just enough isn’t enough—not for the providers, not for the employees, and certainly not for the clients who depend on them.
Rising operational costs—from wages and the Fair Pay Agreement to energy bills—compound historic underfunding and financial pressures. And demand for care continues to increase, creating a widening gap that organisations are often forced to fill with limited resources.
Providers then end up in survival mode, unable to invest in improving their services for today and the future.
THE NEED TO RETHINK FINANCIAL STABILITY
Care providers need to have healthy finances in social care, and that doesn’t come at odds with delivering compassionate care.
A financially strong organisation has the breathing room to improve services, retain employees, and innovate to make a meaningful difference to the lives of people they support. And having this financial security means providers can actually plan for the future rather than constantly reacting to the present.
BENEATH THE SURFACE
Social care organisations face a web of financial intricacies. Local authori-

how financial pressures continue to challenge social care providers.
ty support often comes with layers of red tape. Managing aged debt and resolving invoicing errors take a significant amount of time that few organisations can spare. Regulation and compliance require meticulous reporting, and the sheer volume of admin work to manage all these leaves teams stretched thin.
At the same time, there’s an expectation for providers to keep doing more. But without the right tools and systems in place, these compounded financial struggles threaten to overwhelm this indispensable sector.
Social care providers aren’t just keeping their organisations alive; they’re safeguarding the wellbeing of countless individuals and families.
Providers need to be able to prioritise long-term financial resilience. And part of this means having the tools—including robust financial management softwaresimplify manual processes, optimise resources, and reduce inefficiencies.
By championing financial sustainability, we’re creating conditions where employees can thrive, where clients receive the quality of care they deserve, and where the sector can confidently meet future challenges.
Find out more at: www.oneadvanced.com/ai
See the advert on the back cover of this issue.
For many care managers, a normal day looks like organised chaos.
You start with care planning, then switch into scheduling. Finance needs attention. A medication update comes through. Audits are approaching. Each task lives in a different place. Another login. Another spreadsheet. Another hour lost.
It is no surprise that so many feel stretched too thin.
The challenge is not the work itself. Care managers are experts at ensuring people receive safe, person centred care. The problem is that many tools in use today simply have not kept up with the demands of modern care.

Too often, care teams are asked to work across platforms that don’t speak to each other. Notes get duplicated. Information gets missed. Important changes take too long to reach the right person. This creates stress for managers and their teams. It also creates risk.
But it doesn’t have to be this way.
When information flows through one connected system, everything becomes clearer. There is one place to update, one record for the whole team to rely on, one view of the care being delivered across every visit or shift. Tasks that once took hours can be completed in minutes. Insights that once required detective work become visible instantly.
This is why more providers are turning to all-in-one care management platforms like PASS.
With care planning, rostering, eMAR and finance in the same system, teams stay aligned and up to date. Real time records help reduce errors and support smoother inspections. Smart automation removes manual admin and frees up more time for face-to-face care.
AI also plays a role. Not by replacing clinical judgement, but by helping care teams stay ahead of change. If something looks different in a note, or if patterns in data suggest a growing risk, the system can highlight it quickly for a manager to review.
Technology becomes a helpful assistant, while care professionals remain firmly in control. Over 1,200 services across the UK are already benefiting from this clearer, more connected way of working. Many report stronger communication, improved compliance, and calmer days as a result.
Care will always be complex. People have unique needs. Things change. But systems that support care don’t need to add to the chaos. When everything comes together in one place, focus can return to what matters most. Delivering outstanding care, every day.
Learn more at www.everylifetechnologies.com


As cyber threats continue to rise across the UK, adult social care finds itself increasingly targeted. Phishing, credential theft, ransomware and supply-chain attacks now routinely affect small and medium providers, many of whom lack the internal infrastructure to respond. What was once an “IT issue” has become a board-level risk, capable of disrupting care delivery, compromising sensitive data, and jeopardising business continuity.
Against this backdrop, the sector has made remarkable progress. Five years ago, only 13 percent of social care providers had completed the Data Security and Protection Toolkit (DSPT). Today, that figure has risen to more than 75 percent. This shift shows a growing recognition that cyber security isn’t optional – it is foundational to safe, high-quality care.
At Digital Care Hub, we’ve learned that providers don’t struggle with willingness; they struggle with capacity. Many care organisations simply don’t have the time or expertise to produce robust cyber and data protection policies from scratch. That’s why one of the most transformative tools we’ve developed has been our Data Policy Builder. It allows providers to create clear, compliant, tailored policies, giving them a practical starting point for good governance and DSPT completion. For many services, it’s the difference between feeling overwhelmed and feeling in control.

But compliance is only the beginning. The next challenge for the sector is building true cyber resilience – moving from “ticking the box” to embedding safe digital practice into everyday operations. That means regular staff training, clear incident response plans, secure access controls, and awareness of evolving scams and threats. It also means understanding your digital supply chain and ensuring partners meet appropriate standards.
The renewed government funding for Better Security, Better Care through to 2029 signals a long-term commitment to these priorities. It will support new voluntary cyber and data health checks, help providers navigate upcoming DSPT enhancements, and strengthen local support networks that have been vital in driving progress so far.
But ultimately, resilience will be built provider by provider, through small, consistent improvements: policies that are actually used, staff who know what to do when something looks suspicious, and leaders who recognise that cyber security is now as essential to safe care as medication management or safeguarding.
Social care has already proven how quickly it can rise to a digital challenge. The next four years offer an opportunity to turn that momentum into lasting, sector-wide confidence.
For further information please visit https://digitalcarehub.co.uk/cyber-security
Restrictive practices such as physical restraint, bed rails, or lap belts remain one of the most challenging aspects of health and social care. Intended to keep patients safe, they can also cause harm, distress, and loss of dignity when used unnecessarily. Across the UK, the principle is clear: care must always use the least restrictive option.
Legislation provides the framework, but culture and staff behaviour shape daily practice. Nurses, carers, and clinicians often make quick decisions balancing safety with autonomy. Without training, restrictive practices risk becoming routine. To change this, staff need better understanding of the human impact and confidence to use alternatives.

That’s where Restrictive Practice makes a difference. Developed through codesign workshops with patients and carers, this gamified e-resource gives a voice to those most affected by restraint. Their lived experiences shaped the learning, helping staff see restraint
not as a neutral safety tool, but often as something frightening or disempowering. The results are powerful. Staff trained with the resource led Quality Improvement projects, achieving measurable reductions:
- Bed rails dropped from 360 to 277 incidents
- Bed bumpers from 303 to 227
- Lap belt use halved, from 46 to 22
These improvements represent safer, more compassionate care and reassurance for families.
Restrictive practices may never disappear entirely, but they should be the exception, not the rule. With the right knowledge and tools, staff can choose safer alternatives and build a culture of dignity, compassion, and respect across UK care services. See our advert on the front cover or visit www. RestrictivePractice.com


A recent Home Office action against Burlington Court Care Home highlights how easily care providers can fall foul of sponsor licence rules. Even small administrative oversights, such as failing to report a change in ownership, can have serious consequences for both employers and their overseas staff.
2025 IMMIGRATION CHANGES AND THE CARE SECTOR
While changes to the Immigration Rules are frequent (albeit not always groundbreaking), 2025 has shaped up to be a significant year for immigration changes, especially those aimed at the sponsored work sector. The need to reduce net migration continues to remain at the forefront of government policy making.
The Immigration White Paper, published in April, signalled the end was coming for those looking to make applications as care workers outside the NHS, along with several other jobs deemed to be of lower skill level (most roles below RQF level 6 - graduate level). The White Paper also introduced other suggestions to further tighten up the rules including increasing the required English levels and even the qualifying
period needed to reach settlement. Those in certain care worker roles had already been barred from being able to sponsor dependants and care worker sponsors faced extra scrutiny when applying for and assigning certificates of sponsorship.
In July 2025, some of the suggested amendments were implemented so that now only those who were already being sponsored in certain care roles or have lawfully been working with their employer for at least three months can apply for further permission as Skilled Workers. There is now a complete ban on recruiting new care workers from abroad. With many care worker sponsors having had their licences revoked in the last few years, there is already a large pool of workers who are at risk of having their leave curtailed. It is clear from changes made in 2024 that the government has been keen for existing sponsors to focus their recruitment efforts on these affected workers.
SPONSOR LICENCE COMPLIANCE: CHANGE OF OWNERSHIP RISKS
Change of ownership has long been one of the biggest pitfalls for those holding a sponsor licence. It catches out both large corporations and small businesses alike. A sponsor may have all the necessary dayto-day policies in place for monitoring workers yet still fail to recognise the need for a new licence or transfer when there is a majority change in ownership. Often there is no change to the operational activities of the company nor the workers’ terms of employment, so sponsors blindly carry on without even considering the need for this to be reported to the Home Office.
It was this exact scenario that Glasgow’s Burlington Court Care Home found itself in. There had been a change in majority ownership of
By Natasha Willett, Partner, Latitude Law (https://latitudelaw.com)
the company, and the workers had been transferred to the new employer under UK TUPE rules. Such action would prompt a new sponsor licence application, or transfer to the purchasing company’s sponsor licence, to be made within 20 working days of the transfer. Requesting that the existing sponsored workers have their sponsorship transferred is part of this process. It is understood that 15 sponsored workers have been affected by this change and face having their current permission curtailed for what, on the face of it, appears to be an administrative oversight. The Home Office has always taken the view that sponsorship is a privilege not a right and tends not to offer much flexibility or discretion when compliance duties are not adhered to.
COMMON REPORTING PITFALLS
Even in cases where there is a change in minority ownership, it is still something which must be reported to the Home Office. Failure to report changes in company name and address are also routine acts which could result in compliance action being taken against a licence holder if not reported. Reporting failures have seemingly become so frequent that is has recently prompted the Home Office to issue a notice on its SMS message board to remind licence holders to regularly review and update details, including those for Key Personnel. Failing to change or deactivate Key Personnel when they leave a business is another common issue we see at Latitude Law.
KEY TAKEAWAY FOR CARE PROVIDERS
The action taken against Burlington Court Care Home serves as a reminder to sponsors that if any changes occur – whether it be to the business or to a worker’s personal circumstances – this will probably require a report to the Home Office to stay compliant.
Competency assessment might not be anyone’s favourite phrase, but in domiciliary, residential, and specialist care, it is the backbone of safe, high-quality support. The challenge is making it genuinely useful, not just another hoop to jump through.
Care staff need more than theory. They need time to learn, practise, and make mistakes in a safe environment before they are expected to apply new skills with real people. That is where a blended learning approach truly shines. High quality eLearning builds consistent knowledge. Virtual sessions keep teams connected and engaged. Face to face training gives carers the chance to try techniques, ask questions, and build confidence before working directly with residents
and service users in their homes or care settings.
But learning does not stop in the classroom. Competency assessments in real care environments provide the feedback carers need to know they are using best practice techniques, communicating well, and delivering safe, person-centred care. It is the bridge between “I know it” and “I can do it.”
This balance of learning plus real world assessment creates confident, capable staff who trust their own skills and feel supported rather than judged. Managers also get clear, reliable evidence for CQC and Skills for Care requirements without drowning in admin.
At myAko, we have developed tools with our long term partners,
that make this process simple and sustainable. Better learning, better practice, better competency. It is a straightforward formula that leads to stronger teams and better outcomes for residents and service users.
Because when staff feel skilled, supported, and confident, the quality of care speaks for itself.

Kevin Ashley Founder I CEO myAko https://www.myako.online/




"23 years, operating 4 Devon Nursing homes, has been pretty tough, as anyone in social care, knows, only too well. And if it was hard already, after 2024 budget, it's just got harder.
Anyway, at heart, I am just customer of Eden Alternative, and it was a stroke of luck to come across this whilst on holiday in New Zealand in 2009. It started in USA in 1994 and now runs in 22 countries.
The fact that I am now involved with this not-for-profit organisation (in the UK area) came about when one of the 2 main UK directors died suddenly just before Covid. But it's something I have run with for 11 years to help make 'vision' a reality, not a struggle. So, being both a customer and helping the admin seems quite natural.
It is a modern philosophy of care, but moreover, it's a programme that is straight forward, tried and tested for 30 years and really works.

Its member care organisations generally become trainers for their own teams, and run it themselves.
The programme is run in person over 2-3 days or online 1 hr a wk for 7 weeks. You choose.
It addresses loneliness, helplessness and boredom and operates through 10 principles to underpin 7 critical domains of wellbeing.
Moreover, it's effective, transformational and really works. As residents, and team members wellbeing, matter so much , it's a must, in my opinion.
Geoffrey Cox
Southernhealthcare.co.uk
eden-alternative.co.uk"
In today’s regulated care environment, having clear, current, and wellcommunicated health and social care policies is essential for delivering safe, compliant services. The Care Quality Commission (CQC) now places increasing emphasis on how policies are implemented and understood—especially during registration and inspections.
Outdated or poorly communicated policies can significantly impact your CQC rating. Even if documentation is comprehensive, failure to ensure staff understand and follow procedures may lead to a “Requires Improvement” or even “Inadequate” rating under the ‘Effective’ domain.
Well-maintained policies promote consistent standards across care teams and help safeguard services when incidents arise. In regulatory investigations, the first request is often to review relevant policies—making accuracy and accessibility key to reducing legal and compliance risks.

However, keeping policies up to date is challenging. Constant changes in legislation, best practice guid-
ance, and case law mean that policies can quickly become obsolete.
W&P has been a trusted provider of CQC-ready care policies and procedures for over 20 years. Our expert team monitors industry developments to ensure your policies remain fully compliant.
Our Online Policy Portal simplifies policy management. With just a few clicks, providers can update content, distribute documents to staff, track confirmations, and monitor compliance via a real-time dashboard. You can even provide temporary read-only access to inspectors—demonstrating transparency and accountability instantly.
Ensure your care service meets CQC expectations with fully up-to-date, easily accessible, and well-communicated policies.
Email: info@wandptraining.co.uk
Call: 01305 767104
See the advert on page 2 for details.
Global assists clients throughout the U.K. who specialise in the healthcare sector to achieve their objectives of purchase, development and refinance.
We have organised over £1.8bn for clients in the past 30 years, providing clients with competitively priced funding to refinance existing debt, ease cashflow and develop businesses further.

From helping clients make their first purchase through to allowing groups to grow significantly in size we assist at every stage of your business expansion. Every proposal is individual and deserves to be treated that way, so we hope you will allow us to be of assistance to you and call us to chat through your plans and requirements, I am sure we will be able to tailor a facility to your requirements.