



at
© The Capsule 2025 All Rights Reserved. No part of this publication may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the publisher by copyright law. For permission requests, contact: thecapsulejournalusf@gmail.com.
Connect with us on Instagram: @thecapsule_usf
Dear Reader,
It is with great excitement and pride that I welcome you to The Capsule—Volume 2!
Two years ago, the idea of this journal was nothing more than a dream. Today, it stands as a vibrant and growing platform for creative expression, run entirely by students of the University of South Florida. What began with a vision to provide authors and artists the opportunity to share their reflections on public health, personal health, and healthcare through prose, poetry, and visual art has evolved into something far beyond what I could have imagined.
This past year has been a whirlwind of growth and recognition for The Capsule. We’ve been featured in multiple USF news articles, including those by the College of Arts and Sciences and USF Honors. Additionally, some members of Volume 1’s editing team and contributors had the privilege of speaking about our journey on the USF Honor Roll Podcast. Even more exciting, several of our executive board members traveled to Philadelphia early April to present at the Annual Health Humanities Consortium, outlining the interdisciplinary collaboration between the arts and sciences through The Capsule and the implications of engaging with the principles of narrative medicine early in one’s education.
These milestones would not have been possible without the unwavering dedication of the executive board and the support of our incredible contributors. The diversity of our submissions—from age, to major, to background—continues to enrich the journal, and I’m constantly in awe of how far we’ve come. This year, The Capsule has surpassed its humble beginnings and continues to thrive in ways I could only dream of.
I want to extend a heartfelt thank you to the executive board for your hard work, passion, and commitment. Your efforts have helped set an extraordinary standard for the future of this journal, and I am deeply grateful for everything you’ve done. As Editor-in-Chief, it’s been an honor to witness The Capsule grow and evolve, and I encourage all our contributors and readers to keep creating, sharing, and advocating for the power of art and community.
I hope you enjoy Volume 2 of The Capsule. May the stories and artworks you encounter inspire, challenge, and connect you, just as they have done for all of us involved.
Sincerely,
Serena Bhaskar Founder and Editor-in-Chief








Special thanks to Dr. Lindy Davidson, Professor Elizabeth Kicak, Dhenu Senthil, and Priya Desai.
USF Sparks Magazine, USF Thread Magazine, USF Creative Writing Club
tic, tic, tic | Savannah Barker | Poetry
Guided by Service, Changed by Experience | Amrita Nayak | Nonfiction
Interlinking Rates of Pregnancy and STIs in Youth with Culture and Education | Sandra Aitcheikh | Article On Malaria & the American Dream | Serena Lozandi | Poetry |
Overlooked | Jemma Parsons | Multimedia |
Diagnosis | Noah Bennett | Nonfiction |
The Enemy Within | Smyrna Davalath | Poetry
Challenges in Costa Rica’s Healthcare System: The Effects of Resource Misallocation on Access and Universal Care | Anthony Valverde | Article
What Remains of You | Olivia Pinilla | Poetry
Prescription Grin | Genevieve Carcano | Poetry
The Female Brain and Alzheimer’s: Exploring the Increased Vulnerability | Gabrielle Luisa Dotti | Article
diag[no]sis | Gabriella Davis | Poetry |
Savannah Barker
Currents charge the follicle passageways. Dead end descends.
Absorbed by the minds of the strange and unkind, mankind notified.
An accidental brush on the left leads to a purposeful thwack on the right, until it feels right. Tame the beast with the curls to keep her silent.
Weapons came from all ways.
But with a swift strike to the side and a strategic method of strangulation, a rubber hair band: victor and ultimate tranquilizer.
Never allow a single strand to fall from its place! For secrets must remain in place.
People often seek wisdom in books or moments of introspection. I, however, sought mine somewhere less conventional–in a tutoring program aimed at supporting Afgan and Ukranian refugees. What began as a high school community service requirement became a journey that would profoundly shape my understanding of narrative health and healing. This experience goes past simply educating, but a story of health and the importance of cultural sensitivity to holistic healing.
After a brief orientation, I was assigned to Gulsoom, an eighth-grade girl from Afghanistan who needed a friend more than immediate progress on the course curriculum. I focused on being a confidant, sharing my own story, initiating conversations, and letting her guide them in the direction she felt comfortable with. I recognized sharing her narrative as an essential aspect of healing and wanted her to see that her story mattered and she was understood. By our third session, Gulsoom voiced her struggles fitting in and forming connections at her new school, issues that had significantly impacted her self-esteem. Having to navigate an unfamiliar culture, language barriers, and differing social norms in order to feel included left her lost and uneasy. Listening to her, I saw how this drastic change and cultural displacement had impacted her mental health, making her feel overwhelmed, anxious, and isolated.
Inspired by a spiritual development class I’d attended, I incorporated activities to boost self-confidence into each tutoring session. Together, we practiced positive affirmations and concentrated on identifying and building on our strengths. Within just a few months, I witnessed a remarkable transformation in Gulsoom. She became more confident at school, made new friends, and her enthusiasm for learning grew steadily. Witnessing Gulsoom’s progress taught me that the need to belong is universal, and it only takes a bit of compassion and active listening to improve emotional well-being. Gulsoom’s willingness to share her story reminded me of how storytelling itself can be healing; the act of listening deeply to personal experiences is as vital as any medical intervention. Creating safe spaces to share experiences reminds individuals that they are not alone in their struggles. Unexpectedly, I found my own confidence levels rising, with the positive affirmations actively reflecting in my own life. As I encouraged and uplifted others, I began to internalize those same messages and realized that I needed to hear these positive affirmations too.
This symbiotic exchange of positivity showed me the power of encouragement and personal development. My next semester in the program introduced me to Neelab. At our first meeting, I asked her to share her hobbies and interests—a question that felt ordinary to me but left her visibly surprised. Coming from a country where gender disparities denied girls like her the opportunity to venture into public spaces, let alone discover themselves, and being the eldest of five siblings, her responsibilities left her with no time to explore a hobby. Understanding her life left me in awe, and I left our conversation with overwhelming gratitude for my own life. The cultural and systemic barriers both Gulsoom and Neelab faced gave me a deeper appreciation for the role of cultural sensitivity in addressing disparities in emotional and mental healthcare, even in non-medical spaces.
Over the subsequent months, Neelab and I grew together. She learned to explore her interests in drawing and writing short stories, while I came to realize that I spent far too much time focusing on what I lacked rather than appreciating what I was blessed with. Discovering her hobbies had a transformative impact on Neelab’s mental health and healing, helping her become more cheerful, confident, and emotionally expressive.
By the end of the year, I had fallen in love with tutoring. Each student I worked with showed me the interconnectedness of the emotional, mental, and social dimensions of health. Grace taught me the power of listening and seeing the strengths in those around me. With her unwavering spirit, Jessica taught me the power of perseverance. Then, there was Max, who modeled empathy and understanding. Each experience with the students reminded me that healing and caring for people isn’t limited to doctors and medicine; it happens in every moment of connection and understanding. Working with a diverse group of individuals from different backgrounds and experiences broadened my perspective on empathy and the many ways people support one another. Sometimes the most significant medical intervention is simply being there for someone when they need it the most.
Sandra Aitcheikh
The sexual revolution contributed to a more open discussion and acceptance of sexuality, while more traditional perspectives, often emphasizing abstinence, have influenced approaches to sexual education and discussions on related topics. These sentiments have gone beyond localized communities and have begun to affect the legislation in these areas. Our legislation dictates the necessary information to teach in schools and can reflect the political climate. The culture behind sexual education and the stigma surrounding it causes a possibility for limitation.
States usually push abstinence-only education and even revoke more holistic sexual education. The more conservative ideology in government does not push for a more comprehensive sexual education. It can increase rates of pregnancy and STIs, which can affect the health of the youth. To understand the extent of the effect of the stigma on the health of populations, it is essential to compare the types of education kids receive to the levels of STIs and pregnancy in people.
A goal is to highlight how the lack of education and misinformation is incredibly dangerous, as people will not make informed decisions, and how this can be caused by a biased health policy. A solution for spreading unbiased information would be to backtrack from mixing political and cultural ideologies into a neutral education system. Misinformation is a pathway for unresearched decisions that can harm population health. Find a better, more objective way to say this. For example, it would be beneficial to compare the rates of STIs and pregnancy in states with a more conservative education to states and countries that employ a more liberal education system to see how policy influences health outcomes.
Public health crises, like the rise of HIV/ AIDS, show how misinformation spreads rapidly. A common misconception is that HIV can be acquired by “...breathing the same air [as other infected people]” (Kaplan, 2022). This shows insufficient education on how infectious diseases spread, making preventative measures challenging to enact. This is why we must take an important look at misinformation and the effects that misinformation has on
the decisions of the youth. Education helps counter false ideas and allows individuals to make safer decisions.
The separation of church and state ensures that legislation is not influenced by religious views. However, to understand the differences that states face in enacting laws, it is important to understand that although the United States claims to have separation of church and state in the legislative process, liberal and conservative ideologies play a decisive role in shaping laws.
A prime example that shows how companies use religion to refuse reproductive rights is the Burwell v. Hobby Lobby case, which refuses to give out contraceptives in their health packages. Birth control, in the view of the company, is called “abortive” (Religion and the Constitution, n.d.) under the Religious Freedom Restoration Act of 1993. The courts granted Hobby Lobby reason under statutory interpretation. This sets a precedent that shows how religion can be an exemption for comprehensive medical coverage. This shows that the court was divided between a faction that wanted laws under a secular influence and one that wanted laws to be influenced by religious culture.
In addition to cultural stigma, Kaplan continues to mention how people can delay their STI treatment and continue transmitting the viruses due to stigma deterrence. Therefore, it is vital to understand the origins of sexual stigma. People reference the role of Christianity, explaining how sex should not be had before marriage (Evans, n.d.). This can be a significant reason for the push for abstinence-only education in schools, primarily since the majority religion advocates for a reduction in education that would encourage premarital sex.
Not separating church and state in health education is counterproductive, as most religious teens do not cite religion for abstinence in adolescence. (Hayward, 2020). The statistics on the sexual health epidemic as teenagers still engage in premarital sex and disregard the information presented (Regnerus, 2007). Education plays a vital role in the safety of adolescents, showing how laws passed influence the level of sexual education received in schools.
Some states have mandates for compre-
hensive sex education, and some states do not have any mandates. Coincidentally, these states that vary in inclusivity and abstinence are correlated to the level of religious worship and political-religious ideology. Comprehensive sexual education includes incorporating the “whole student” without leaving sexual orientation and contraceptives unaddressed (USC College of Nursing 2018).
To understand why comprehensive sexual education is needed in the United States, in 2016, the United States had higher rates of teen pregnancy and sexually transmitted diseases than most other industrialized countries (Sedgh et al., 2015). When compared to other developed countries, American women had lower use of contraceptives and were more likely to have multiple sexual partners. This was correlated to a higher rate of sexually transmitted infections (USC Department of Nursing 2017). Levels of sexual education received and safe sex practices may correlate. To fully show a correlation, external variables in comparison should align. The women studied were of similar socioeconomic backgrounds and became sexually active at the same time (USC Department of Nursing 2017).
Domestically, the state with the highest teen birth rate in 2015 was Arkansas (USC Department of Nursing 2017). The national average of live teen births in the United States is 17 per 1000 females, placing Arkansas at almost double the national average with 30 live births per 1000 females between the ages of 15 and 19 (Arkansas Advocates 2021). It is important to note that “States that have had the most success, and the lowest teen birth rates nationally, do a much better job than Arkansas at educating young people about preventing pregnancy” (Arkansas Advocates 2021). Connecticut and Massachusetts had the lowest levels of teen births in 2016 (USC Department of Nursing 2017). Teen pregnancy rates have been dropping for over a decade - a total of 75% decrease, with an added 13% decrease from 2014 to 2015 (Lefranc, 2018). These numbers show a significant decrease in teen pregnancy rates due to the implementation of comprehensive sexual education programs, showing a possible connection between pregnancy rates and sexual health education. Connecticut has tackled this issue with a progressive tactic - the University of Connecticut has been using a plan called the “Teen Pregnancy Prevention Initiative” to address disparities in the community and target the populations with adoles-
cents who are at a higher risk for early parenthood.
In contrast to the “abstinence-only” policies present in states like Arkansas, Connecticut recognizes that there needs to be adequate access to contraceptives. The state recognizes that contraceptive access is vital and that education is also needed. In fact, in the Youth Risk Behavior Survey (2017), the percentage of teens who engaged in sexual intercourse decreased from 41.8% in 2007 to 32.4% in 2017 (Lefranc, 2018). This shows that teens had an education that would allow them to either safely engage in sexual intercourse or abstain due to the knowledge of STIs and pregnancy.
A common trend between the states with higher levels of teen pregnancy is the prevalence of abstinence-only sexual education. Some states, like Arkansas, do not require sexual education at all (Sex Education n.d.). This may be due to the influence of conservative influence on health policy. The counter to abstinence-only education is comprehensive sex education. In the middle of the two models is a program called “Plus” Education (Abstinence Education Programs: Definition, Funding, and Impact on Teen Sexual Behavior 2018). Abstinence-only education can be called “Sexual Risk Avoidance Education” as pregnancy prevention and STI reduction methods are downplayed. To introduce how the government supports this education (lack of separation of church and state at the origin), the government has been funding states serving this curriculum. The peak of this funding was implemented during the Bush administration to emphasize how this has also been split into party lines. It was reduced by the liberal predecessor, Barack Obama. Showing the different types of sexual education methods is vital for comparing how the education received affected the rate of STIs and pregnancy in the youth.
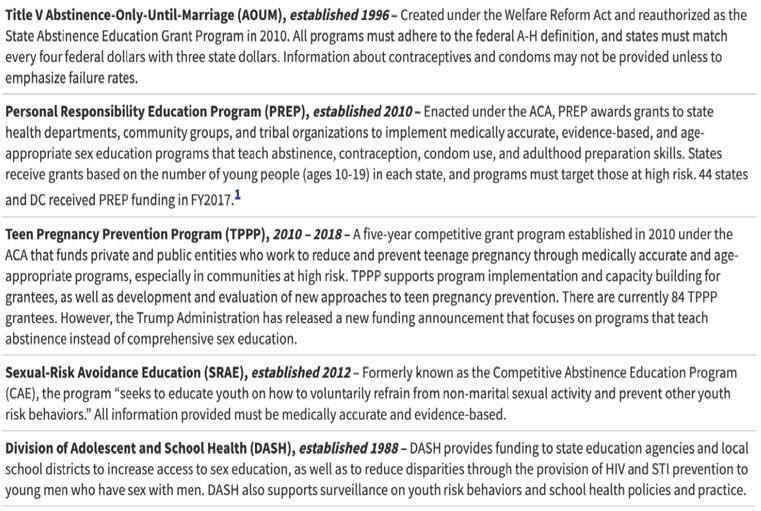
Table 1: Current Federal Funding Streams for Sex Education
Source: Kaiser Family Foundation. “Abstinence Education Programs: Definition, Funding, and Impact on Teen Sexual Behavior.” The Henry J. Kaiser Family Foundation, 1 June 2018, www.kff.org/womens-health-policy/fact-sheet/abstinence-education-programs-definition-funding-and-impact-on-teen-sexual-behavior/.
Table 1 (Women’s Health Policy 2018) proves to be a display of the diverse legislation that is enacted in different areas of our country. Differences in education painted by the political scene display a lack of universal and comprehensive education. Various acts passed, like the Personal Responsibility Education Program (PREP), serve as a proposal for legislation that our government bodies can take to reduce the misinformation currently circulating in schools. It is important to note how the federal government allocates funds for these education systems. Figure 1 will show how the government divides available funds for sexual education.
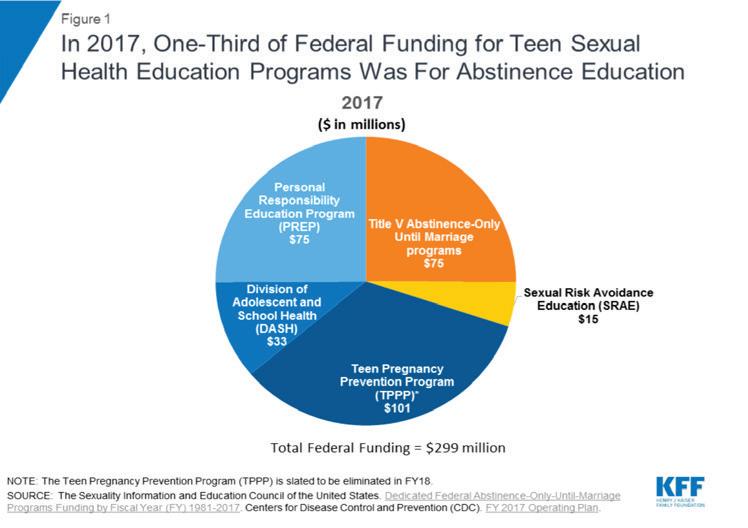
Table 1 explains how much money goes into abstinence-only education compared to more comprehensive and researched education methods. Research shows (Women’s Health Policy 2018) that one-third of federal funding goes to abstinence-only education, leading to the highest rates of pregnancy and STIs in the country. Instead, more funding needs to go to the evidence-backed comprehensive sex education programs. Almost a quarter of funding goes towards education only for abstinence. With an equal amount of federal funding being used for Personal Responsibility Education Programming, or PREP, almost half of the budget can be used for comprehensive education, especially since PREP is medically accurate.
The beginnings of sexual stigmatization in the United States stem from the conservative attitudes towards sex, labeled “taboo,” and leading to misinformation being spread. I propose a resolution for further comparative research on the rates of pregnancy and Sexually Transmitted Infections in states where they have an abstinence-only policy when they transition into a more comprehensive sexual education base, just like the “Teen Pregnancy Prevention Initiative ‘’ in Connecticut. States like Arkansas highlight the sexual stigma that calls for the removal of policies for STI and pregnancy prevention. The United States should prioritize quality and
comprehensive sexual education.
References
“Concealability and Course.” ResearchGate, www.researchgate.net/ profile/David-Evans-48/publication/317721451 The stigma of sexuality concealability and course/ links/594a81570f7e9ba3beaf951a/The-stigma-of-sexuality-concealability-and-course. pdf.
Glover, Candace. “Data: Arkansas Needs a Different Strategy for Preventing Teen Births.” Arkansas Advocates for Children and Families (AACF), 30 June 2021, www. aradvocates.org/data-arkansas-needs-a-different-strategy-for-preventing-teen-births.
Hayward, Geoffrey M. “Religiosity and Premarital Sexual Behaviors Among Adolescents: An Analysis of Functional Form.” Journal for the Scientific Study of Religion, vol. 58, no. 2, 2019, pp. 439–458. https:// doi.org/10.1111/jssr.12588.
Kaplan, Jonathan E. “HIV and AIDS Myths, Misconceptions, Rumors.” WebMD, 12 Dec. 2022, www.webmd.com/hiv-aids/ top-10-myths-misconceptions-about-hivaids.
Lefranc, Mary. “Connecticut Leads the Nation with Lowest Teen Birth Rate.” Connecticut Health Investigative Team, 20 Aug. 2018, c-hit.org/2018/08/20/connecticut-leads-the-nation-with-lowest-teenbirth-rate/.
“42 U.S. Code Chapter 21B - Religious Freedom Restoration.” Legal Information Institute, www.law.cornell.edu/uscode/ text/42/chapter-21B.
“Abstinence Education Programs: Definition, Funding, and Impact on Teen Sexual Behavior.” KFF, 1 June 2018, www. kff.org/womens-health-policy/fact-sheet/ abstinence-education-programs-definition-funding-and-impact-on-teen-sexual-behavior/#:~:text=Abstinence%2DOnly%20Education%20%E2%80%93%20 Also%20called,prevent%20unintended%20 pregnancy%20and%20STIs.
Sedgh, Gilda, et al. “Adolescent Pregnancy, Birth, and Abortion Rates Across Countries: Levels and Recent Trends.” Journal of Adolescent Health, vol. 56, no. 2, 2015, pp. 223–230. https://doi.org/10.1016/j. jadohealth.2014.09.007.
Serena Lozandi
Being illegal means to be forbidden by law.
Forbidden by law to live, Mother hides in the attic during winter, with visions of salted droplets and shivers, rocking back and forth as her body boils over— defending itself against illegal viral parasites and concealing their presence within her fragile body’s blood.
Forbidden by law to live, Mother is a human being in a land in which she is forbidden by law to occupy
The American Dream is a public hospital, a vast waiting room with patients with head wounds, blood dripping down their skulls, drip, drip, dripping onto linoleum floors— blood is wine in fluorescent lighting yet the nurse calls in the patient who has a cough.
Mother is not a patient the American Dream is willing to see. She is forbidden by law, to live and occupy and must hope her shivering body outsmarts the intruders in her blood.
Jemma Parsons

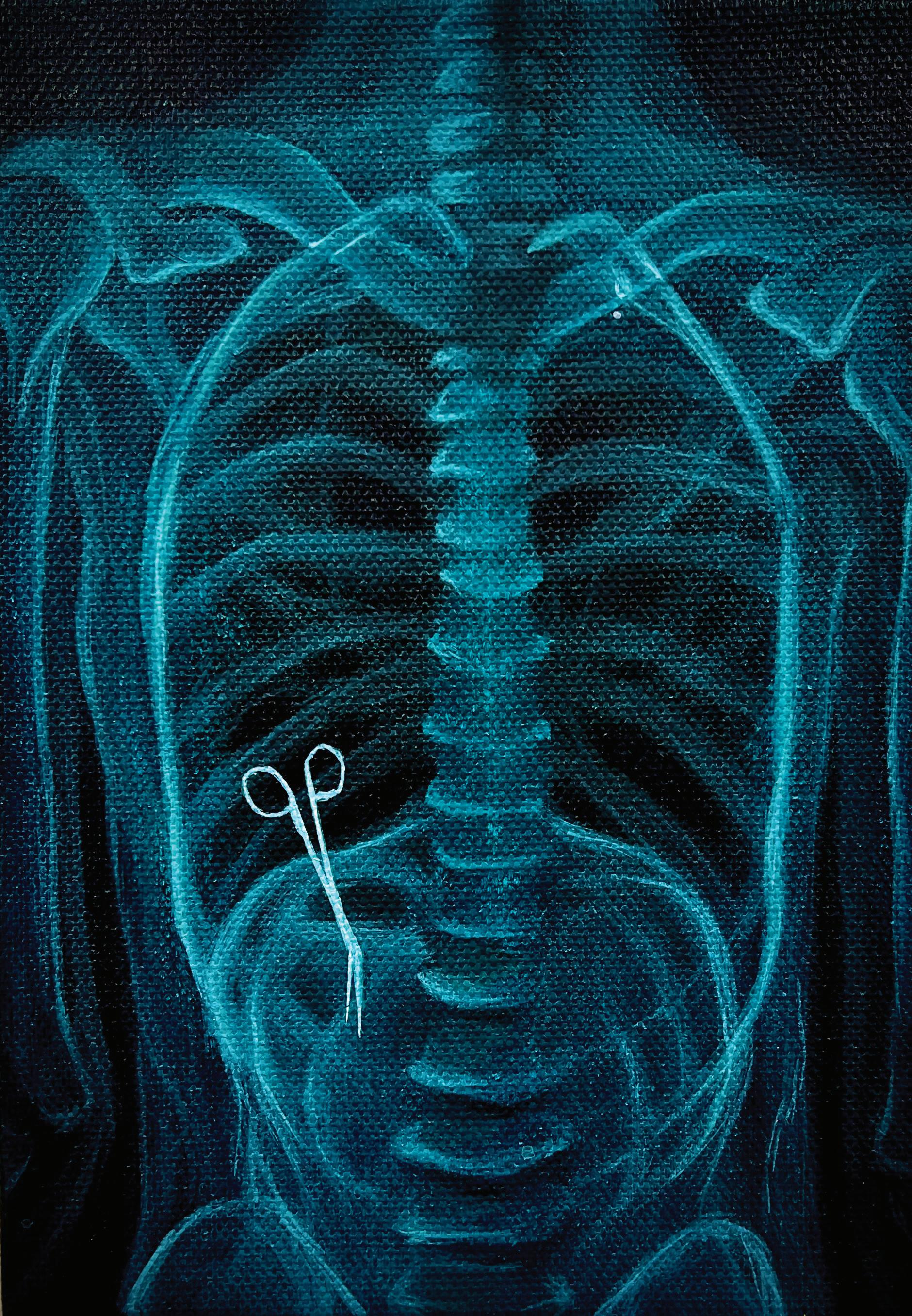
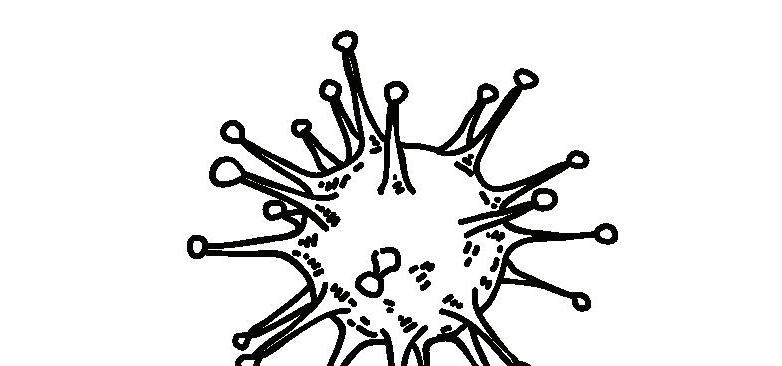
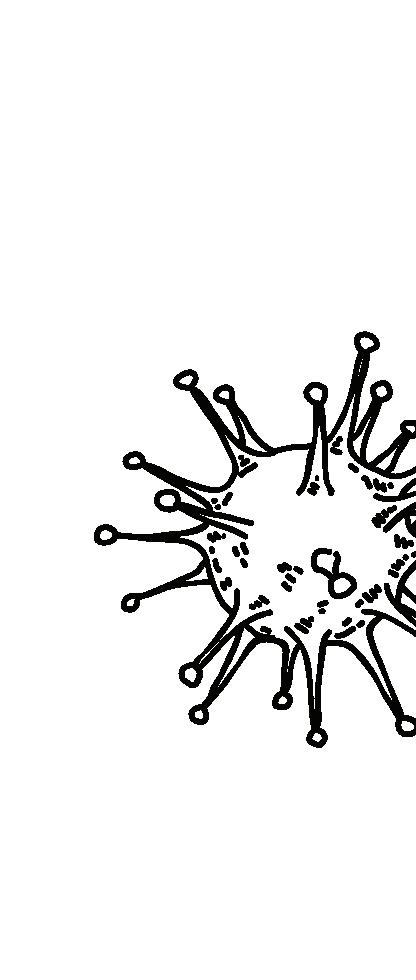
Medical negligence is a leading cause of postoperative death, involving a healthcare provider failing to follow the recognized standard of care during treatment. It may be caused by numerous factors, ranging from high stress conditions to gross incompetence in the healthcare professional. When negligence results in harm to the patient, it is considered to be medical malpractice, which accounts for 5% of personal injury suits.
The understated ubiquity of irreversible damage caused by flawed medical procedures, even those that are extremely routine, is a morbid reality that Americans risk facing every time they visit a hospital, and which they are expected to wave away with legal compensation if victimized. Despite advancements in modern medicine, the consequences of these mistakes are still primitive, grotesque, and deeply dehumanizing.
Acrylic on canvas, 2023
Noah Bennett
Growing up, I had paranoia about the piercing pain in my stomach I would sometimes get from eating. I was told it was just irritable bowel syndrome, and that I would have to ride it out. The pain feels like my guts are on fire. It feels warm and inflamed, yet sharp and dull. It made me feel broken, and the pain was sometimes so intense I could only lie there sweating and gritting my teeth alone. There was no defense, no prevention. I would spend multiple hours in the bathroom per day, until it became worse and worse. I had to seek help. At a doctor’s appointment with my primary care, her assistant suggested that I may have celiac disease, but the doctor ultimately suggested I seek out a specialist. In my head, I thought it was impossible. Celiacs has something to do with eating gluten, right? My stomach hurts no matter what I eat, so it didn’t fit the puzzle to me. I booked an appointment with a gastroenterologist (GI) and my thoughts began to drift. If it can’t be celiacs, what is wrong with me? My fears began to eat me up as I saw no positive outcome.
Upon hearing my symptoms, the GI doctor insisted on a full workup, endoscopy and colonoscopy. Endoscopy shows gastritis in the lower parts of my stomach. Inconclusive, no definite answer is found. I am feeling a little down, but I am both nervous and hopeful for the next procedure to come. The day before the colonoscopy, I went through an entire day of laxatives and stool softeners. The pain within my stomach was immense all day, and I was not allowed to eat any solid food or colored drinks. I grew increasingly tired of chicken broth, being that was all I could eat for the entire day. When the day comes, I arrive at the procedure center and patiently take my seat. The wait feels like hours while I hyperfocus on every name being called back. Eventually, I heard my name. The procedure goes great, and there is no sign of colon cancer. I feel relieved, but a feeling still sinks inside me. I still have no answer, despite this gut-wrenching gauntlet I went through. Negative thoughts began to race through my mind that maybe I was overreacting or faking it this entire time. I desperately needed reassurance that my pain was real. My last hope was the biopsies taken during the procedure. I would lay awake at night, wondering
what I was hoping to get out of this.
After a month’s wait, I arrived for my follow up. I don’t know what answer I was looking for, as none of them sounded great. I knew I wanted an answer, for the fear of the unknown was going to take me down. Upon shaking the GI’s hand, he wasted no time. I was handed a paper with a positive result for… celiacs? This cannot be right. He bluntly tells me that all I need to do is cut out gluten, and I’ll live a long life. The entire visit lasted for what felt like a few seconds. No medication, no surgery that can fix me, I just have to live with it. Is it really going to be as easy as that? It just didn’t make sense to me, it can’t be right. I was sure that gluten had no correlation to my stomach pain, and my family history is almost entirely clear. After sitting in my car for 30 minutes, I decided to text my loved ones and tell them the news. At this point, I was fully breaking down. I stopped to wonder, why am I so upset? It could’ve been way worse, I should be blessed to have an answer. Some may never reach a conclusion, and some may reach a diagnosis far worse than mine. I was devastated, it didn’t matter if it could be worse at the moment. I drove home and went straight to bed. My appetite was gone at the time, but eventually in an attempt to grasp back onto normalcy, I felt the need to get some food. After looking around, a harsh reality crashed into me like a brick wall. Everything in my house had gluten in it. There was not a single piece of food I could eat. What was once my home was now a reminder of what I was trying to forget. I felt my vision go blank as I didn’t want to perceive what I was seeing, but after staring silently at the wall, part of me knew I was going to have to eventually face the fate given to me. At the store, I noticed that true gluten-free options are scarce. Four times the price, just for gluten-free mac and cheese. The noodles didn’t impress me, but I wasn’t going to give up so easily. I ordered a gluten-free pizza from a chain pizza place, learning a hard lesson. Despite the ingredients being gluten-free, my stomach still hurt. The burning feeling in my stomach made my skin crawl at my realization. Cross-contamination. The pizza was cooked in the same oven as the other pizzas. It didn’t matter if the ingredients were gluten-free. It was contaminated.
I decided that maybe it was smarter to cook my own food. I cooked my own lasagna as my family had theirs in the oven at the same time. Contaminated. I cooked soup but had set the spoon down on the countertop for just a second while away. Once again, contaminated. I had no idea it was this serious, no one did. If I continue to eat gluten, I will die. Stomach pain is one of the early symptoms, a warning for what’s to come. The symptoms would eventually slowly kill me. I had to accept that I can no longer eat fast food, restaurant food, or even food at a friend’s house. Slowly, I began to distance myself from friends. I would reject all dinner plans, as I felt like nowhere was safe. I couldn’t even drink beer. Having to explain my condition makes me feel like an outcast, and it reminds me of all the things I will never be able to do again. My own parents don’t even understand. Constantly cooking food that is contaminated. Many times, when I am at an event, I am offered a salad while everyone else gets actual food. The salad became the symbolization of all my negative thoughts. A reminder that no one seemingly knows what it’s like to live like this. A salad made in the same kitchen as everything else is contaminated. The idea of going to birthday parties or dinner plans terrified me. Being offered a measly salad feels dehumanizing while watching others eat actual food.
As I have come to terms with my condition, I’ve adopted a brother outlook. It may have felt like my life was over at first, but I am now more mature. I’ve found multiple restaurants which can accommodate someone like me, and there are brands that make gluten-free alternatives that are almost indistinguishable from “normal” products. Being able to eat out or even just finding a new brand of bread that tastes less terrible is what keeps me going. Things that I took for granted are now something I treasure. Rice was never something I appreciated more than a good meal, but now it feels like the opposite of a salad. Though it is nothing special, it’s always there for me when making dinner plans. Affordable, easy to make, and stores away nicely. The ground will always be beneath my feet, the air will always fill my lungs, and rice will always be gluten free. I always feel blessed to find new foods in stores I can eat, or new places that can cater to my needs. My disease can’t be seen with the naked eye, but it still affects my day-to-day living. It’s almost been a year since my diagnosis, and life has just been trying to regain what I have lost,
and to live a normal life. I now share my story, in the hope that people will begin to understand what it’s like to live with an invisible disease. Through this life-changing diagnosis, I have discovered a love for cooking and medicine, as well as an urge to do well in life despite my limitations. A disease that I thought ruined my life at one point, is now something I refuse to let stop me. I instead weaponize it to keep pushing myself, beyond what I used to believe I was capable of.

Moriah Lee
While working at New York’s Beth Abraham Hospital, neurologist Dr. Oliver Sacks encountered over 80 patients who previously had encephalitis lethargica, a neurological condition which had affected millions in the early 1930s. This had led to a condition called postencephalitic parkinsonism, causing these individuals to be stuck in catatonic states while their minds were fully conscious.
During the summer of 1969, Dr. Sacks realized that the patients were able to respond to certain stimuli, such as saying their name, throwing them a ball, or listening to music (Marshall). This was then followed by the use of a new drug Levodopa, also called L-DOPA, a medication developed for Parkinson’s disease patients. The use of L-DOPA resulted in a massive “awakening” of the catatonic patients, and for a period of time, they were able to walk, talk, and reclaim their lives. Unfortunately, L-DOPA resulted in numerous side effects and rapidly became ineffective, and the vast majority of the patients eventually regressed back to their original states within a year, with many becoming worse than before.
Before the use of L-DOPA, Dr. Sacks experimented with music therapy, which had a measurable impact on many of the patients. Music therapy has been used for a variety of neurological conditions and has many benefits, without the many side effects that often come with pharmaceutical drugs. Understanding the benefits of treatments such as music therapy may help to provide alternatives to the mainstream treatment of medication.
Encephalitis Lethargica
Encephalitis lethargica has two stages:
the acute stage which occurs immediately, and the chronic stage which can occur months to years later. The chronic stage, postencephalitic parkinsonism, results in bradykinesia: slow or delayed movement, or complete inability to move. However, postencephalitic parkinsonism patients can quickly shift from akinetic to perfect mobility rapidly. This can usually be initiated by external stimuli such as tossing them a ball or playing them music. (Hoffman and Vilensky).
Despite years of research, the cause of encephalitis lethargica is still unknown. As encephalitis lethargica has almost completely and mysteriously disappeared, it is difficult to continue researching for a cause, as there are very few cases to glean information from. Identifying a possible treatment is very difficult and as such, no clear and effective treatment has emerged. However, treatments for Parkinson’s disease appear to be fairly effective on some postencephalitic patients, such as the use of music and touch therapy, as well as the drug, levodopa, which is incredibly effective for a short period of time but had a very limited period of benefit.
Dopamine is a brain chemical produced in many regions of the brain, and is linked to many important physical and cognitive functions (Olguín et al). One of these key functions is the motor functions pathway, which can create issues with movement when dopamine levels are abnormal. Medical conditions like Parkinson’s disease and encephalitis lethargica have been linked to insufficient dopamine levels.
Levodopa is a medication originally used as a treatment for Parkinson’s disease, due to its ability to treat dopamine deficien-
cy (Gandhi and Saadabadi). However, a study in 2016 found that its use can cause permanent change to an individual’s DNA, causing the medication to become ineffective within a few years, as well as leading to dyskinesia, a condition characterized by involuntary, jerky movements (Figge et al). Levodopa-induced dyskinesia was identified in about 50% of patients within 5 years of beginning treatment.
Listening to music has been found to be highly stimulating for the brain, activating specific regions of the brain which frequently are not activated by other stimuli. Most importantly, music activates key regions of the brain that produce dopamine (Jäncke).
Many studies on music therapy have found that it can facilitate recovery of movement for stroke, Parkinson’s, and traumatic brain injury patients (Trimble and Hesdorffer). A meta-analysis in 2021 found statistical significance that music therapy improved motor function, balance, and freezing of gait (Zhou et al). The study concluded that while pharmacotherapy is symptomatic and loses effectiveness over time, music therapy creates positive emotional response, has effective results, and has no negative side effect, illustrating the benefits of music therapy over pharmaceuticals.
Apart from physical benefits, music therapy can also be extremely beneficial for the emotional wellbeing of patients. Patients with neurological conditions such as encephalitis lethargica and Parkinson’s are often at a higher risk for conditions such as depression (Raglio et al). A review of 25 studies on a variety of neurological conditions found that music therapy decreased rates of depression and anxiety, and improved overall quality of life.
Frances D. developed encephalitis lethargica at 15 years old. This caused her to be frozen in place for over 25 years. In her own words, “[e]ither I am held still, or I am forced to accelerate. I no longer seem to have any in-between states” (Sacks, 1973). She was treated with L-DOPA, which decreased her freezing, but led to many side effects such as tics and respiratory crises. She was forced to discontinue the drug when the side effects became too overwhelming, causing her condition to return even worse than before. Ms. D fell into a deep state of depression after the discontinuation of L-DOPA, as she had briefly felt in control of her life, only to quickly lose her freedom. Prior to the use of L-DOPA, however, Ms. D. exhibited
positive responses to music therapy. Despite only being able to move freely while the music was playing, this was a reliable method that had no negative side effects (Sacks).
Ed M. had a very unique form of encephalitis lethargica, where his body was split in half: one side was very energetic and suffered from jerking and tics, while the other was frozen. His EEG was normally asymmetrical, but when playing the piano or organ, the asymmetry disappeared. Mr. M. was unable to be treated with any medications, as they would help one side of his body, but worsen the symptoms on the other half. Music therapy through playing piano or organ caused the symptoms of both sides to temporarily disappear (Sacks).
Postencephalitic parkinsonism shares many features with Parkinson’s disease, appearing to stem from a dopamine deficiency. As such, studies on Parkinson’s patients can be used as a good model for postencephalitic parkinsonism, which is much rarer. While music therapy tends to have results which are less uniform and systematic, its beneficial effects on Parkinson’s disease, and consequently encephalitis lethargica, are well-supported by research.
As a key factor of postencephalitic parkinsonism is dopamine deficiency, dopamine-producing regions of the brain are an essential area of focus. (Olguín et al). Music therapy helps to stimulate many of these areas, aiding in dopamine production which is crucial for patients with postencephalitic parkinsonism.
While L-DOPA has proven to be highly effective for postencephalitic parkinsonism patients, both case studies and research have found that the effects of L-DOPA are fairly short-term, and frequently cause negative side effects. It functions by becoming a dopamine replacement, an effect which music therapy also achieves. For patients in the chronic stages with postencephalitic parkinsonism, L-DOPA cannot be a truly viable option, due to the many harmful side effects it causes, such as the respiratory crises, and the potential that it could become ineffective before the patient has time to fully recover (Sacks).
As such, music therapy proves to be a much safer and effective treatment option when compared to L-DOPA. The use of medication comes with far more inherent risks compared to non-chemical treatments such as music therapy. Additionally, music therapy is far more enjoyable, cost effective, and does not lose effectiveness. It is also far more versatile compared to med-
ications. Even a medication which is highly effective with generally low side effects can have negative consequences when used in tandem with other medications or on individuals with multiple medical conditions. In contrast, music therapy has essentially no negative side effects and can be adapted to fit the individual patient.
A Culture of Prescribing America is facing a culture of prescribing: the idea that health issues should be solved first and foremost by taking medications. In 2012, nearly 60% of US adults were taking at least one prescription drug. For every additional prescription medication taken, the risk of adverse drug events increases by 7-10% (Brownlee and Garber). Additionally, this culture of prescribing creates financial strain on many individuals, as medications are often incredibly expensive.
The story of the encephalitis lethargica patients of Beth Abraham hospital serves as a reminder of the importance of shifting our society’s focus away from medications. Every day, individuals suffer from negative side effects, financial burdens, and even premature deaths due to unnecessary prescriptions. By exploring alternative treatment options such as music therapy, America can move towards a society in which people can live longer and healthier lives.
References
Brownlee, S., Garber, J. (2019). Medication Overload: America’s Other Drug Problem. The Lown Institute.
Dale, R. C., Church, A. J., Surtees, R. A., Lees, A. J., Adcock, J. E., Harding, B., . . . Giovannoni, G. (2004). Encephalitis lethargica syndrome: 20 new cases and evidence of basal ganglia autoimmunity. Brain, Volume 127, Issue 1, 21-33.
Figge, D. A., Eskow Jaunarajs, K. L., & Standaert, D. G. (2016). Dynamic DNA Methylation Regulates Levodopa-Induced Dyskinesia. JNeurosci, 6514-6524.
Gandhi, K. R., & Saadabadi, A. (2023, April 17). Levodopa (L-Dopa). Retrieved from National Library of Medicine: https://www.ncbi.nlm.nih.gov/books/ NBK482140/#:~:text=Levodopa%20is%20 th e%20precursor%20to,symptoms%20apparent%20in%20Parkinson%20disease
Hoffman, L. A., & Vilensky, J. A. (2017). Encephalitis lethargica: 100 years after the epidemic. Brain, 2246-2251.
Juarez Olguín, H., Calderon Guzman, D.,
Hernandez Garcia, E., & Barragan Mejia, G. (2016). The Role of Dopamine and Its Dysfunction as a Consequence of Oxidative Stress. Oxid Med Cell Longev.
Jancke, L. (2008). Music, memory and emotion. J Biol., 21.
M., K., & MM., E. (2001). A contemporary case of encephalitis lethargica. Clin Neuropathol, 2-7.
Marshall, P. (Director). (1990). Awakenings [Motion Picture].
Raglio, R., Attardo, L., Gontero, Giulia., Rollino, S., Groppo, E., Granieri, E. (2015). Effects of music and music therapy on mood in neurological patients. World J. Psychiatry, 68-78.
Sacks, O. (1973). Awakenings. London: Duckworth & Co.
Sacks, O. (2008). Musicophilia: Tales of Music and the Brain. New York: Alfred A. Knopf.
Trimble, M., & Hesdorffer, M. (2017). Music and the brain: the neuroscience of music and musical appreciation. BJPsych Int., 28-31
Zhou, Z., Zhou, R., Wei, W., Luan, R., & Li, K. (2021). Effects of music-based movement therapy on motor function, balance, gait, mental health, and quality of life for patients with Parkinson’s disease: A systematic review and meta-analysis. Clinical Rehabilitation, Volume 35, Issue 7, 937-951.
Jordan Hamburg
Time is Medicine depicts a standard orange prescription bottle spilling open to reveal pill capsules taking the form of warped clocks. The surreal composition immediately evokes time’s role in physical and psychological healing. The melting clocks, reminiscent of Salvador Dali’s The Persistence of Memory, suggest the fluidity of time and how it stretches and compresses based on perception, especially in the context of illness and healing. Medicine often follows strict temporal frameworks—dosage schedules, treatment timelines, and recovery periods—yet healing itself is not always so clear. Despite similarities in patients’ diagnosis and treatment, their sense of time is not identical, hence the warped clocks. The piece also critiques the healthcare industry’s over-reliance on pharmaceutical drugs, suggesting time as a fundamental healer, sometimes just as powerful as medication.

Liam Mahony
Few areas within the healthcare field are as confounding or nuanced as pain perception. For both medical practitioners and modern philosophers, conceptualizing pain’s effect on the body—and the psyche—is an increasing challenge. In light of these complexities, the account of pain presented by Descartes, often referred to as “the father of modern philosophy,” is worth revisiting. By examining these philosophical ideas and their intersection with new theories in pain, future medical practitioners may better appreciate the gray area within a particularly systematic career field.
At the heart of Descarte’s philosophy is his mind-body dualism. This idea posits that two distinct substances, namely the mechanical matter of the body along with the immaterial substance of the mind, interact with each other. Any dualist like Decsartes has difficulty explaining perception; namely, how do purely biological processes within the body influence an immaterial thinking mind? The Cartesian account for pain, as discussed in the Treatise on Man, is an attempt to mold pain perception into this overarching dualistic philosophy. He claims that “animal spirits” (or fluids within the bloodstream) pass through the initial location of pain and, through the pineal gland, are interpreted in the brain. The soul’s connection through this gland unifies the mind with the mechanical aspects of the body, as Descartes refers to it as “the principle seat of the soul” (Ariew, 443). In a letter to Fromondus, Descartes further develops this position that pain must primarily be a mental phenomenon and interpreted through the rational part of the soul. He mentions that, since individuals still feel sensations in missing or amputated limbs, this sensation “would certainly not have happened if the feelings [or] sensation of pain occurred outside the brain.” (Ariew, 146). Like other perceptions, the rational faculty of the mind and the mechanical aspect of the body work in conjunction with one another to interpret pain. Apart from some of the obvious anatomical errors, Decsartes makes within his theory of pain, a deeper underlying issue still remains. As previously mentioned, Descartes offers a fuzzy connection between the physical and mental realms in processing pain. For instance, if one concedes that pain is primarily a mental sensation, the role the
initial physical stimuli play loses its significance. Although Descartes does believe that some intensely physical pain, like feeling “fire burning in the hand” (Ariew, 453) trumps the mind’s pain-regulating power, what role the mind and body play in perception still appears convoluted. Descartes’ Passions of the Soul tries to respond to this objection, detailing how emotions the mind feels differ from pure bodily perceptions. There are external perceptions worked primarily through the senses, perceptions relating solely to the body (like pain), and perceptions of the soul, which “we do not usually know any proximate cause” for (Ariew, R. 443). Perceptions are interpreted through the soul’s rational interpretations and can excite different behavior than what the body would naturally be inclined to do. Using an analogy of a soldier, Descartes claims that the soul can ignite a feeling of courage even when the body is inclined to flee, since some reasons can: “persuade us that the peril is not great; that there is always more safety in defense than in flight; [and] that we should have the glory and the joy of having vanquished...” (Ariew, 443)
In this natural fight-or-flight situation, Descartes emphasizes that external situations can mitigate the risk-averse inclinations of the body. This, hypothetically, has a neat translation toward pain management. Take running a marathon: although the immediate physical stress is intense, the personal satisfaction one gets after finishing the race makes the pain bearable. Descartes correctly argues that some incredibly painful experiences can be endured through willpower or volition, slightly clarifying this connection between mind and body. Although Descartes does rely on reason in controlling emotions, some physical sensations are simply far more difficult to override.
In part due to the numerous ways Descartes offers in analyzing emotional and rational regulation in pain perception, dualism had a leading influence on medicine and healthcare for hundreds of years after his publications (Gold). Many of his writings focus primarily on how the person themselves manages pain; however, as the research below will suggest, one’s surrounding environment is critical to this understanding as well. Not only is the connection between mind and body unclear, but the connection between the individual and their environment remains similarly ambiguous. This connection is critical to highlight for medical practitioners
today, as the complexities and subjectivity socio-environmental factors have in pain perception add a layer of nuance to a rather pathological-driven field of study.
Biophysical Model and Critiques
Pain is a particularly nuanced and multifaceted topic within healthcare, and increasingly comprehensive theories of pain emerging in the past decades aim to provide fuller pictures of social, pathological, and environmental influences on health. The biopsychosocial model is a recent theoretical approach that emphasizes the role sociocultural factors have in conceptualizing pain (Tracy). Research suggests some genes can only be expressed through the presence of environmental triggers, and these environmentally dependent genes could be modified by social and political factors (Braverman). One example of this theory was done through an experiment conducted by Bath University, in which they revealed participants had a lower pain tolerance (having their hand placed in a cold presser) when measured alone rather than with another friend in the room (Edwards). Non-biological factors, like trust, empathy, and resilience, appear to have a significant effect on how an individual perceives pain (Tracy). As such, US medical school curricula and healthcare training services have been integrating this model into their practices (Roberts). Using biophysical principles has been shown to greatly aid chronically ill and functionally impaired individuals (Kusnanto) as opposed to biomedical models, which have been criticized for their overreliance on using pathology in treatment, particularly for psychological disturbances (Engel). With this evidence at hand, both medical professionals and philosophers alike are distancing themselves from ideas that fail to incorporate environmental influences that affect pain perception. Since George Engel first proposed the biophysical model in the late 1970s, Biomedical theories of pain have borne the brunt of these critiques. The human body is not strictly a mechanical configuration, and pathology itself could never be sufficient to fully comprehend an individual’s perception of pain. Considering the immense influence Descartes had on the scientific revolution in medicine, his ideas have fallen prey to these challenges as well. Practitioners like Jeffery Gold have gone as far as to label Cartesian dualism as “dehumanizing” and reductionist (Gold). Treatment of patients’ bodies as nothing more than a non-emotive mechanism is believed to have substantial roots in Cartesianism. Descartes would, however, challenge the idea that his medical thought is solely
reductionist, as commentators like Gold have targeted him. Differentiating the mind as a unique substance implies that it does not need to process pain mechanically as the body would. In addition, Descartes argues in the Passions how one’s natural environment affects perception. He claims that volition alone is insufficient to cause some bodily movements, such as dilating one’s pupils, since “...nature has joined the movement of the gland that serves to thrust forth the spirits toward the optic nerve in the manner requisite for enlarging or diminishing the pupil...” (Descartes, Ariew, 453).
In response to the challenges above, Descartes mentions how one’s natural environment does play a role in behavior and perception. Whether this short passage provides a strong enough correlation to the larger emphasis environmental factors have in the biophysical model is up for interpretation. Regardless, given the ways the Passions detail how the mind can analyze perception, critiques like Gold’s ultimately fall flat. Even if there is a strong correlation between biomedical models of pain and Cartesianism, it would be an error to conflate dualism with total reductionism. An emphasis on the non-quantifiable factors influencing pain is nonetheless a point of contention in Cartesianism.
Conclusion
The extent to which pain is primarily a pathological phenomenon, nature’s role in pain perception, and the impact pain has to diminish one’s overall well-being make this field of study both a medical and philosophical point of interest. Given its significant biological, social, and normative importance in someone’s life, it is worthwhile to analyze Descartes’ highly influential views in light of modern pain research. Medicine and healthcare, although viewed strictly as a scientific endeavor, carries an immense amount of subjectivity. This case study on pain philosophy serves as a reminder that, given the inescapable nature of nuance within the healthcare field, practitioners should embrace this gray area rather than dismiss it outright.
References
Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014 Jan-Feb;129 Suppl 2(Suppl 2):19-31. doi: 10.1177/00333549141291S206. PMID: 24385661; PMCID: PMC3863696.
Descartes, Treatise on Man. Sélection translated from De l’homme et de la formation du foetus, edited by Claude Clerselier (Paris, 1664). Translated by P. R.
Sloan.
Descartes, R., & Ariew, R. (2000). Philosophical essays and correspondence. Hackett Publishing.
Edwards, Rhiannona,b,*; Eccleston, Christopherb; Keogh, Edmunda,b. Observer influences on pain: an experimental series examining same-sex and opposite-sex friends, strangers, and romantic partners. PAIN 158(5):p 846-855, May 2017. | DOI: 10.1097/j.pain.0000000000000840
Engel, G. (2012). The Need for a New Medical Model: A Challenge for Biomedicine. Psychodynamic Psychiatry, 40(3), 377–396. https://doi.org/10.1521/ pdps.2012.40.3.377
Gold, Jeffrey. “Cartesian Dualism and the Current Crisis in Medicine — A Plea for a Philosophical Approach: Discussion Paper.” Journal of the Royal Society of Medicine 78, no. 8 (1985): 663–66. https:// doi.org/10.1177/014107688507800813.
Kusnanto, H., Agustian, D., & Hilmanto, D. (2018). Biopsychosocial model of illnesses in primary care: A hermeneutic literature review. Journal of family medicine and primary care, 7(3), 497–500. https:// doi.org/10.4103/jfmpc.jfmpc14517
Smith, C. U. M., and others, ‘René Descartes’, The Animal Spirit Doctrine and the Origins of Neurophysiology (2012; online edn, Oxford Academic, 20 Sept. 2012)
Tracy, Lincoln M. “Psychosocial Factors and Their Influence on the Experience of Pain.” Pain Reports 2, no. 4 (2017): e602–e602. https://doi.org/10.1097/ PR9.0000000000000602.
Kavery Kallichanda
The best of my job— Freedom from the monotony of standing an unneeded automation for hours. Fresh air and company, him in his wheelchair and me behind, soaking in the sunshine and human words. Who knew I was his freedom as much as he was mine. Freedom from the monotony of a lonely hospital bed.
Serene Abulhaija
In homes of sand and stone, breath is survival
Burdened by dust that settles like a second skin. The air hums war songs; lullabies fade to echoes. Time is not counted here, only endured.
Mothers knead dough, hands worn and trembling, Their knuckles hardened by hunger and prayer.
Fathers return as shadows, bodies gaunt and hollowed, Bearing the weight of the walls that fell too soon.
In this landscape of constant ache,
Health is a luxury whispered, never promised.
Wounds bloom like open graves beneath fraying gauze, Fevers rage through nights where medicine is a distant wish.
Hospitals collapse before the wounded arrive, And the sick learn that waiting is the closest thing to a cure.
To speak of healing is to dream aloud,
To carve a world no one has seen.
But what is health to the broken-bodied, To the spirit stitched and restitched on scene?
It is the miracle of rising despite it all,
To touch the sun with trembling fingers,
To teach our children to dance in the ruins, Their feet pounding defiance into the earth.
It is knowing that scars are maps, not endings, That even in the hush of grief, we still sing Soft voices threading through shattered streets, Humming lullabies to a land that remembers.
To dare to imagine that one day, Breath will be more than survival.

Growing up in a Middle Eastern household, Abulhaija experienced love in quiet, unspoken gestures—one of the most tender being the simple act of peeling fruit. Her parents and grandparents instinctively handed her slices of oranges, apples, or pomegranates, never asking if she wanted them but knowing she did. This small yet profound act symbolized care, healing, and connection, reflecting a broader cultural tradition where food serves as both nourishment and remedy. The wisdom of generations before—offering citrus to boost immunity, herbal teas to soothe, and honey as a cure-all—demonstrates how love is carried through everyday rituals.
The Hand That Heals You captures the warmth of these hands—wrinkled, adorned, and marked by time—hands that have carried children, prepared meals, and worked tirelessly yet still take the time to peel fruit. Through this piece, Abulhaija honors her family and the countless others who express love through food, highlighting how the simplest moments often hold the deepest meaning. It is a tribute to cultural heritage, reminding us that devotion is not only found in grand gestures but also in the quiet, ordinary rituals that sustain and heal.
Media: Procreate on iPad Pro
Violet Adams, Madeline Damon, Ciana Raley, and Isabel Reiter
Introduction
Receiving a diagnosis of cognitive impairment (CI) can be life changing, not only for the patient but for their caregivers as well. Disorders such as Alzheimer’s disease present unique challenges in social-emotional wellbeing that can become extremely isolating. Inspired by the Meet Me at MoMA program–the first of its kind designed for adults with dementia–The Art in Mind program at the James Museum of Art (JMA) in downtown St. Petersburg focuses on fostering expression, connection, and a positive experience through the use of interactive art gallery tours. The program offers discussion-based, hour-long tours to adults with Alzheimer’s disease and other forms of CI and aims to enrich the lives of the participants by providing them with intellectual stimulation, social inclusion, and a place to foster emotional connections with their caregivers and each other. Tours are unbiased, non-judgmental, and designed with the participants at the center.
CI presents challenges in data collection, especially when methodology is heavily reliant on self-report data. Researchers in the past have modified their data collection methods by using simplified question formats, observational techniques, and flexible interview strategies (Fisher et al., 2006; Philpin et al., 2005). Additionally, caregivers may also provide valuable insight to the participant’s experience by expanding on responses, validating experiences, and fostering participant engagement. Independent caregiver assessments further improve data accuracy and provide participants with a sense of value in the process (Philpin, et al., 2005; Fry et al., 2021). This study has two goals: (1) to analyze data from previous AIM sessions at the JMA to assess the impact of the tour on individuals with CI and their caregivers, and (2) to create a new caregiver survey to improve measurement of their perspectives on the tours.
Participants
Participants included 32 individuals with memory loss and CI, such as Alzheimer’s disease, along with a subset of their caregivers. Participants had varying levels of memory loss, ranging from mild cognitive impairment (MCI) and dementia to a formal diagnosis of Alzheimer’s disease. No additional demographic information
was collected.
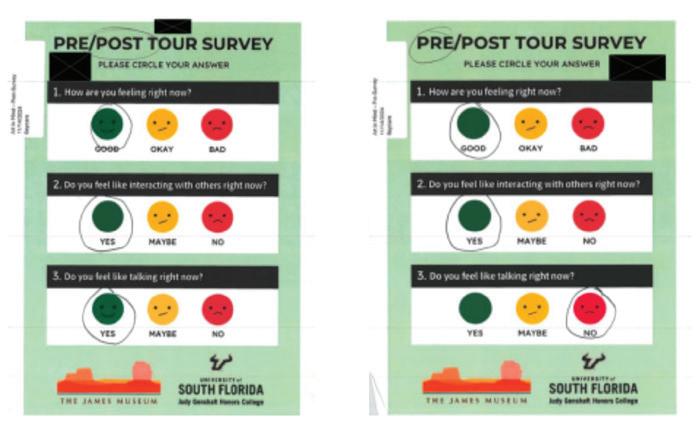
A three-question pictorial self-report Likert scale was developed for the AIM program based on previous research on survey development for those with CI. The survey was originally designed by USFSP Honors students in previous iterations of the Healing Arts course and was first administered in its current form in Spring 2024. This survey is designed for ease of use, even for those with severe impairments. It includes the following questions:
“How are you feeling right now?”
“Do you feel like interacting with others right now?”
“Do you feel like talking right now?”
Response options were either “Good,” “Okay,” or “Bad” for Q1 and Q2 and “Yes,” “Maybe,” or “No” for Q3. Each response option was accompanied by an emotive face (happy, neutral, and sad) to aid comprehension. A sample of this survey can be found in Appendix A, with participant names redacted.
Upon arrival, participants created name tags and completed a pre-tour survey assessing mood, desire to interact with others, and willingness to talk. Each participant was paired with a companion from the Judy Genshaft Honors College, and some were accompanied by caregivers as well. Assistance was provided as needed. The same procedure was repeated for a post-tour survey to evaluate changes in responses. Data was analyzed using the Statistical Package for the Social Sciences (SPSS).
Facilitators were trained to foster a patient, enthusiastic,and relaxing environment, and orient participants to enhance the experience of the memory loss group. Tours incorporated Visual Thinking Strategies (VTS) and Personal Response Strategies (PRS) to encourage discussion, helping participants to explore emotions, memories, and thoughts that might otherwise remain inaccessible.
It was initially hypothesized that the AIM program would increase participant mood, communication, and desire to interact
with others. Given the ordinal nature of the data, a Wilcoxon Signed-Rank Test (non-parametric alternative to paired t-test) was utilized to assess differences in median scores between pre- and post-survey scores.
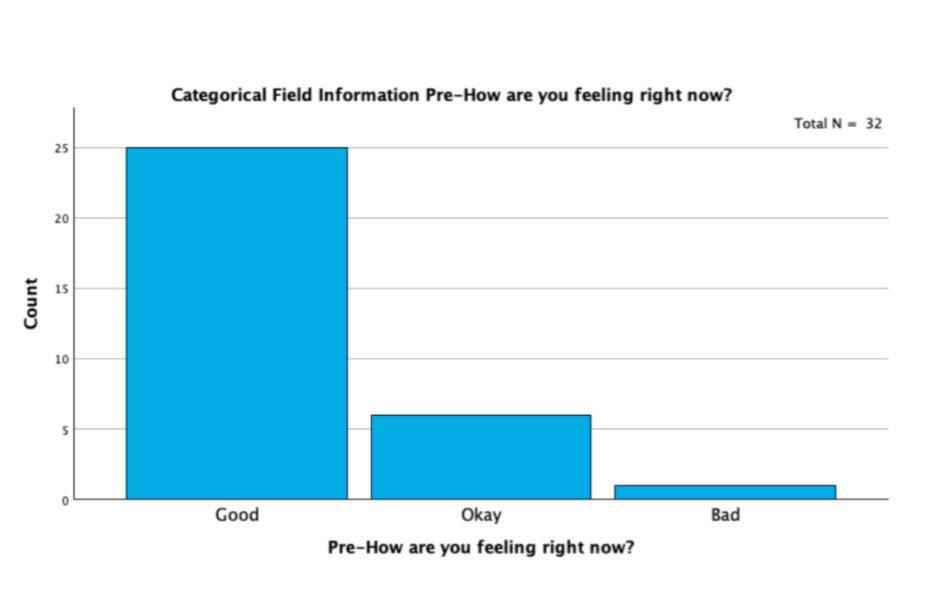
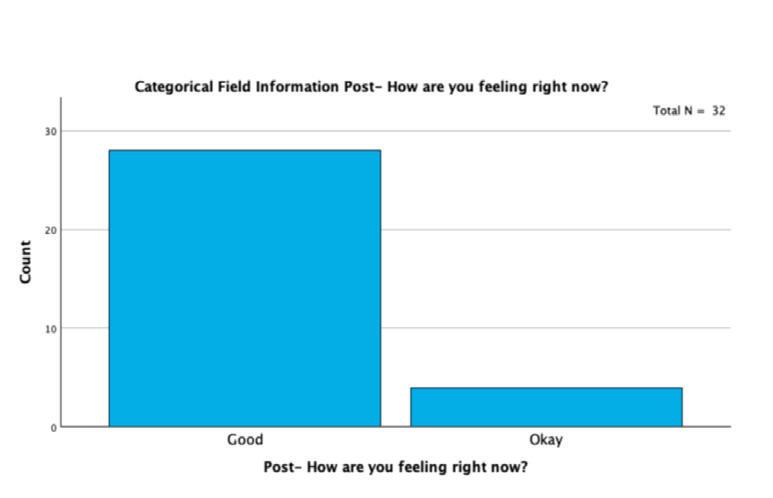
For the first set of variables–“Pre-How are you feeling right now?” and “Post-How are you feeling right now?”–the results were not statistically significant (p= .206), leading to the retention of the null hypothesis. However, an interesting trend emerged: As shown in Figure 1, pre-tour responses ranged from “Good” to “Bad,” whereas the post-tour survey data (Figure 2) indicated that no participants selected “Bad.”
Analysis of Q2, “Do you feel like interacting with others right now?”, also yielded no significant change (p= .915), thus the null hypothesis was retained.
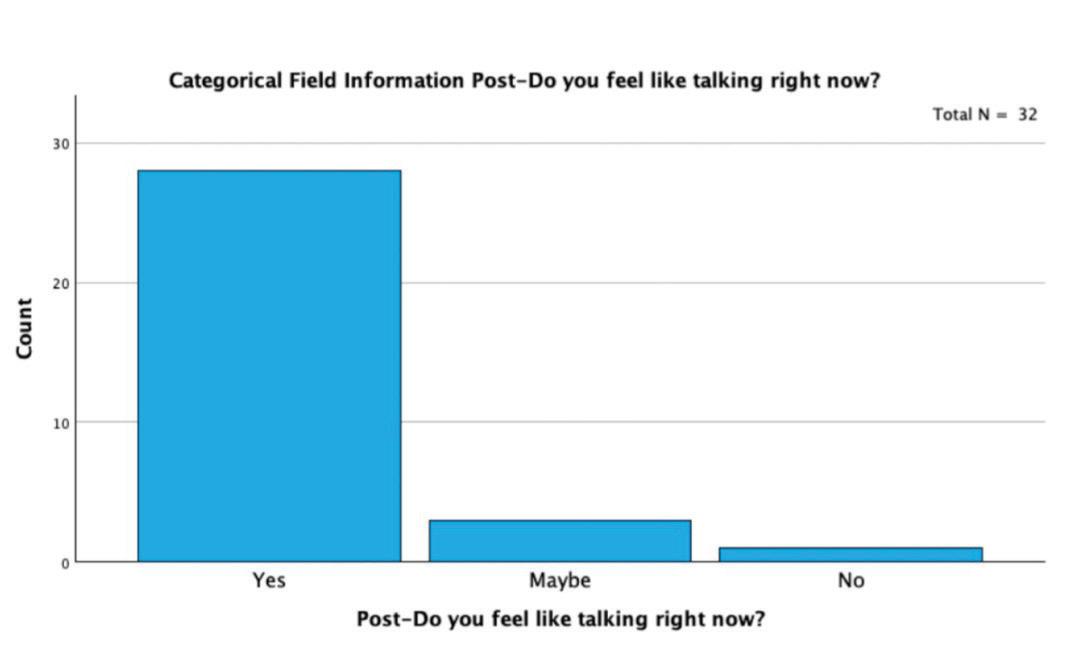
Lastly, analysis of Q3, “Pre-Do you feel like talking right now?” and “Post-Do you feel like talking right now?” showed no statistical significance (p= .885). However, a notable shift in response patterns was observed in Figures 3 and 4: post-tour, fewer participants selected “No,” while responses indicating “Maybe” and “Yes” increased.

Discussion
Although the results did not indicate a statistically significant effect for tour participants, several positive impacts were observed. Notably, several participants who initially responded “No” to Q3 later selected “Yes” in the post-tour survey. Facilitators also reported increased engagement in conversations among both participants and caregivers as the tours progressed.
To more accurately capture the benefits of the AIM program, improvements in data collection are necessary. Given the challenges of surveying individuals with CI, a more detailed questionnaire–despite enhancing reliability and validity and allowing for deeper analysis–may lead to frustration for participants. To address this, the present study proposes the Art in Mind Caregiver Survey (Appendix B) to gain deeper insight into participants’ experiences through caregiver perspectives of the AIM tour’s impact on their companion. The survey includes items assessing participant’s experience including:
- Item 6: “My companion’s mood improved throughout the experience.”
- Item 7: “My companion and I talked about memories during this tour.”
Additionally, items evaluating the caregiver’s own experience include:
- Item 1: “I feel a stronger sense of community after this experience.”
- Item 2 “My mood has improved after this tour.”
- Item 3: “I enjoyed taking part in conversations surrounding the art.”
- Item 5: “I would recommend these activities to other caregivers and groups.”
- Item 8: “I feel closer to my companion after this tour.”
- Item 9: “I would come back to the Art in Mind tour again.”
- Item 10: “I feel personally fulfilled from this experience.”
Through this novel caregiver survey, we aim to provide a more comprehensive evaluation of the Art in Mind program’s impact on both participants and their caregivers.
References
Fisher, Susan E., Burgio, Louis D., Thorn, Beverly E., Hardin, J. Michael. (2006). Obtaining Self-Report Data From Cognitively Impaired Elders: Methodological Issues and Clinical Implications for Nursing Home Pain Assessment. The Gerontologist, 46(1), 81–88. https://doi.org/10.1093/ geront/46.1.81
Fry, M., Elliott, R., Murphy, S., & Curtis, K. (2021). The role and contribution of family carers accompanying community living older people with CI to the Emergency Department: An interview study. Journal of Clinical Nursing, 31(7–8), 975–984. https://doi.org/10.1111/jocn.15954
Hamilton, J. (2024, February 6). The James Museum Launches Art in Mind: An Innovative Initiative for Adults with Dementia. St Pete Catalyst. https://stpetecatalyst. com/w/the james-museum-launchesart-in-mind-an-innovative-initiative-foradults-with-dementia/
Meet me at MoMA. (n.d.). Meet me at MoMA. https://www.moma.org/visit/accessibility/meetme/
Philpin, S. M., Jordan, S. E., & Warring, J. (2005). Giving people a voice: Reflections on conducting interviews with participants experiencing communication impairment. Journal of Advanced Nursing, 50(3), 299–306. https://doi.org/10.1111/j.13652648.2005.03393.
The James Musem. (2024, November 7). Art in mind. The James Museum. https:// thejamesmuseum.org/artinmind/
Williams, R. (2010). Honoring the personal response. Journal of Museum Education, 35(1), 93- 102. https://doi.org/10.1080/105 98650.2010.11510653
Appendix A
Art in Mind Smiley Face Survey
Appendix B
Art in Mind Caregiver Survery
Below are a number of questions regarding your experience today at the James Museum. Please fill in a number indicating how much you either agree or disagree with the given statements.
Rating Scale:
1= Disagree, 2= Neutral/Unsure, 3= Agree
1. I feel a stronger sense of community after this experience.
2. My mood has improved after this tour.
3. I enjoyed taking part in conversations surrounding the art.
4. My companion enjoyed the experience today.
5. I would recommend these activities to other caregivers and groups.
6. My companion’s mood improved throughout the experience.
7. My companion and I talked about memories during this tour.
8. I feel closer to my companion after this tour.
9. I would come back to the Art in Mind tour again.
10. I feel personally fulfilled from this experience.
Scoring Guidelines: Items should be summed. A higher score indicates higher levels of program efficacy.
Ren W.
Three weeks. That’s how long it’s been since my last dose. Not by choice—like hell, I’d put myself through this on purpose. But the hoops I have to jump through just to get a simple refill are ridiculous. It’s like my state wants me to die. I knew quitting cold turkey would be bad, but knowing doesn’t make it easier. The headaches started first, sharp and mean, little knives at my temples. Then the nausea hit with relentless, rolling waves that made food a distant memory. Sleep? Forget it. My body twitches and burns, skin too tight, brain too loud. Everyone warns you about withdrawal, but what do you do when there’s no other option?
Calling the pharmacy is an exercise in futility. I wait on hold, fingers drumming against the counter, only to be met with the same robotic voice: Your prescription has been approved, but processing times may vary. How long? No one can say. A day? A week? A month? Might as well be forever. And yet, I keep calling. Keep trying. Even though the answer never changes. Without my meds, life turns into a stalled out car, sputtering, jerking, going nowhere fast. Maybe I do depend on them. Maybe I need them just to function. But there’s no shame in that. I remember reading something once about how meds are like fuel for brains like mine that keep the engine running. Can’t recall exactly how it was worded, though. Funny how memory slips when your body’s in full-on revolt. The worst part is the exhaustion. Not just tired but a bonedeep, aching fatigue. My hair’s thinning, my stomach’s in knots, and even the simplest tasks feel impossible. Money’s a joke at this point. A cruel one. I blew over a hundred bucks at some rigged fair game, just desperate to win something. Anything. Watched the bills disappear like they meant nothing, like I wasn’t gonna feel that loss clawing at me later. Walked away with empty pockets, forcing a grin like I wasn’t on the verge of losing it in the middle of a crowd.
Oh, right. Meds. That’s what I was talking about. See what happens without them?
School without meds is wading through wet cement. And money’s always gnawing at the back of my mind. Groceries cost a fortune, so I just...don’t eat sometimes. It’s not the best plan when I’m already running on fumes, head bobbing in class, and words blurring together on the page. But hey, money’s just a revolving door anyway, right? Sleep’s a gamble, too. Six hours if I’m lucky. Mornings come too fast, and with no ride home till late afternoon, the day stretches on forever. Between trying to keep up with school, grabbing vending machine snacks
without breaking the bank, and squeezing in time for friends, it’s a miracle I haven’t just shut down completely. They say therapy’s supposed to help, but when I sit there, staring back at my therapist, the words just…stop. They pile up in my throat, stuck behind a wall I can’t seem to break through. So I nod, smile, talk about the good stuff, curating a highlight reel instead of telling the truth. I brought that up once, admitted how I hold back. My therapist just shrugged, said it’s normal. But it doesn’t feel normal. It gnaws at me. I want to open up, I really do, but it’s like I’m wired to hesitate. Even with people who are supposed to feel safe, it takes forever to let them in. And when I finally try, my thoughts scatter. Stringing them together feels impossible. You’ve probably noticed by now. Half the time, I can’t even tell a proper story. If you ever find yourself where I am—stuck without medication—it’s a deeply isolating experience. For me, it felt like everything was slipping through my fingers. I cherished the days when I had them, when things felt steady, manageable. Without them, I was scared, desperate. I lashed out at people who didn’t deserve it, turned that frustration inward when there was nowhere else for it to go. Time lost meaning; days blurred into exhaustion, sickness, and loneliness. It’s hard when no one really understands—maybe one person will, if you’re lucky. Medication has been life changing for me. It’s given me a stability, a sense of self I couldn’t hold onto before. If you rely on them too, I hope you never have to go without. But if you do, please know that you’re not alone. The worst part is people telling you you’re incoherent. I spill my guts, lay everything out raw, and they act like it’s fiction, like I’m just being dramatic. They’ll say they don’t understand, like that’s my fault, like putting this into words isn’t already the hardest thing in the world. But that’s why I’m writing this. I need you to listen. Not correct me. Not tell me what I’m doing wrong. Just listen. Because I might never change, and I might never get this all out the right way, but I’ll always be trying. Even if it takes me a lifetime to figure out how to say it right.
Matthew Lim
Currently the number of people diagnosed with Parkinson’s Disease is 8.5 million, but this number is expected to increase to 12 million people in 2050 (Soilemezi 2023). Not only do individuals experience non-motor symptoms, but there is a huge social need which makes up a burden for the patient and families. There have been studies showing the economic burden of neurological diseases such as personal, intangible, psychosocial, and indirect costs due to these diseases (Navarta-Sánchez 2023). However, a big concern for individuals and caretakers is the social burden of taking care of people with neurological disorders due to the extreme stress and social effects it can have. Communities and individuals must adjust their everyday lives to accommodate for this change of daily routine and life. People must learn to cope and adjust with the negative aspects regarding the healthcare system like difficulty with getting treatment or limited access to specialists. Many different communities have systems in place to help individuals with these conditions, but it can be limited in many ways. Differing societal perceptions due to cultural frameworks influence the ethical decision-making approach to care for individuals with neurodegenerative disorders (e.g. Alzheimer’s and Parkinsons) in residential homes and community settings. Culturally different communities deal with neurodegenerative disorders through the process of Advance Care Planning, and this system has been under development in western nations over recent years.
SECTION ONE: Communities Dealing with Neurodegenerative Disorders and Addressing the Problem
Community Support of People with Parkinson’s Through Caregivers
Neurodegenerative disorders involve not only the person inflicted but the caregivers or family members. This situation cannot be handled alone and requires a support system in the community to achieve successful results like sustainable long term care and a better quality of life. One study examined individuals with Parkinsons and family caregivers from Denmark, Norway, and the United Kingdom. This study
provided important information about the support or lack thereof from health services in their respective countries. The participants of the study explained healthcare professionals who specialize in Parkinson’s disease were able to provide beneficial support as they didn’t have a complete understanding of what each family needed (Navarta-Sánchez 2023). This point was reaffirmed in each family, showing how influential professional help was and how reliant these families were on this aid for themselves and the person with Parkinson’s Disease. It illustrates how general healthcare services and other external social services were limited in how helpful it could be for the families. Many of the people with Parkinson’s disease (PD) themselves outlined how the clinical expertise and the support they received from health care specialists like neurologists, physiotherapists, and PD nurses were helpful sources of support. People with Parkinson’s Disease (PwPD) believed these specialists were helpful for “managing their individual symptoms, treatments and addressing their concerns. [A]ccording to many [PwPD] and [Family caregivers], more flexible access to PD specialists was necessary to respond to symptoms that arose unexpectedly” (Navarta-Sánchez 2023). Family caregivers are reliant on the professional advice of health specialists, and the inaccessibility of these services inhibits the much needed guidance for assisting PwPD.
Caretaker’s Responsibility when assisting People with Parkinson’s
Another main concern for communities with people with Parkinson’s disease is who the responsibility is to take care of the person. “Many people with Parkinson’s Disease in the United Kingdom, Denmark, Norway and Spain considered themselves to be jointly responsible in the management of their condition and making decisions to adapt their everyday activities” (Navarta-Sánchez 2023). The family caregiver shoulders a huge responsibility as they spend the most time managing the PwPD’s everyday life. Especially because most family caregivers are emotionally connected to the person with Parkinson’s disease, it is difficult to not be concerned with any physical or emotional changes the person may undergo during the process. Many family caregivers “in all four countries indicated that cognitive changes in PwPD gave them much greater cause for
concern... cognitive changes were reported to be the most difficult aspect to live with” (Navarta-Sánchez 2023). As the person with Parkinson’s health deteriorates, many of the caretakers undergo emotional tribulation as they slowly lose someone they love. The slow degradation is the cause for much of the turmoil on caregivers as it is a gradual process, and extremely heartbreaking to witness firsthand. In addition, these concerns were also illustrated in a study in which the family caregivers felt much concern and uncertainty about the future of their person with Parkinson’s. The study showed they felt it was essential for family caregivers “to receive support to maintain their health and emotional well-being, and their ability to help” (Navarta-Sánchez 2023). Therefore, it is shown in western nations of Norway, Spain, Denmark, and the United Kingdom to put an emphasis on establishing systems in which the caregivers can receive the help they need in order to maintain their current condition and well-being.
Defining Advanced Care Planning
Neurodegenerative disorders like Parkinsons are incurable at later stages and detrimental to a person’s wellbeing if medical attention is not sought out on the early onsets of the disease as it decreases optimization of medical intervention. Western nations have started to adapt Advance Care Planning into their healthcare systems to plan ahead for the onset of symptoms. The goal of Advance Care Planning is to help the person inflicted make treatment decisions in advance. Advanced Care Planning is something that enables individuals who have the cognitive function, to make decisions upon the consequences of serious illness scenarios, to define goals and preferences for future medical treatment, and to discuss these plans with family and health care providers (Giordano 2022). Advanced Care Planning is a planning system which allows individuals to define their medical goals for the future in the present while they are still able to make conscious decisions. The planning system is beneficial for neurodegenerative disorders like Parkinson’s as it allows for the PwPD to make their own decision in the medical future and plan what they want to do medically or even
physically. This allows for some of the ethical implications of making decisions for the PwPD to be bypassed as they are making decisions for themselves and can make these decisions.
Advance Care Planning involves future medical decisions and routine medical care, but specifically for Parkinsons there is an emphasis on quality-of-life plans, meaning a better living situation (Lum 2019). The discussion for Advance Care Planning for patients with Parkinsons include advanced decision, living wills to communicate decisions if they are no longer able to, and medical orders for stuff like resuscitation, intensive care units, artificial feeding, and preferred place of death (Nimmons 2020). There have been some studies to integrate Advanced Care Planning into clinical care through key factors that influence how patients and care partners plan future medical discussions. One study by Dr. Lum, PhD researcher interested in palliative care, indicates positive examples of patients who did Advanced Care Planning as part of their routine care. The patients agreed that the routine assessment of Advance Care Planning offered the opportunity to have ongoing conversations about medical care preferences and allow for an important systematic approach to continual engagement with patients (Lum 2019). One can see how Advanced Care Planning can be beneficial for patients and caretakers due to the continuity of Advanced Care Planning and its effectiveness to help plan the future of the patient and their environment. Different societal perceptions due to continuously fluctuating cultural frameworks emphasizes how different the ethical decision-making approach for care of individuals with neurodegenerative disorders and the process. Literature has found in the United States people with Parkinson disease significantly increased the chance of utilizing advanced planning. In South Africa a different study found that 95% of respondents had completed a living will in the form of an ACP (Churm 2022). In a different study analyzing the implementation of Advanced Care Planning for Parkinsons, three US studies had people utilizing documentation from Advanced Care Planning at rates between 15% and 53% (Nimmons 2020). These statistics suggest that even within the same country, population differences (e.g. ethnicity or societal/cultural norms) can influence the effect decision making and ACP has on PwPD. Advanced Care Planning is only effective if the individual values the assistance the process can provide, and
genuinely dedicates the effort to utilize the system to enhance their end-of-life plans.
Differing societal perceptions due to cultural frameworks influence the ethical decision-making approach to care for individuals with neurodegenerative disorders (e.g. Parkinsons) in residential homes and community settings. Different communities have differing decision making processes for those with the neurodegenerative disorders as shown by the development of Advance Care Planning over the recent years in western nations. This is targeted at an audience of people also going through the struggles of having a family member who has any sort of neurodegenerative disorder. This review provides insight to the intended audience on how their experience is similar to many other people’s experiences and they are not alone. This topic further discusses insight on the study behind bioethics of caring for people with neurodegenerative disorders and showcases how many different people and cultures deal with a growing modern day medical problem. Systematic development in healthcare planning for people with neurodegenerative disorders is essential for early treatment of patients with symptoms. Analyzing how differing perspectives influence the way these individuals are handled will provide further insight on whether communities are equipped with infrastructure to deal with difficult to handle medical situations.
References
Sokol, Leonard L et al. “Advance care planning in Parkinson’s disease: ethical challenges and future directions.” NPJ Parkinson’s disease vol. 5 24. 22 Nov. 2019, doi:10.1038/s41531-019-0098-0
Nimmons, D et al. “Experiences of advance care planning in Parkinson’s disease and atypical parkinsonian disorders: a mixed methods systematic review.” European journal of neurology vol. 27,10 (2020): 1971-1987. doi:10.1111/ene.14424
Lum, Hillary D et al. “Framing advance care planning in Parkinson disease: Patient and care partner perspectives.” Neurology vol. 92,22 (2019): e2571-e2579. doi:10.1212/WNL.0000000000007552
Churm, Deepta et al. “How Do Patients With Parkinson’s Disease Approach Advance Care Planning? A UK-Based Mixed Methods Study.” Journal of geriatric psychiatry and neurology vol. 35,1 (2022): 168-175. doi:10.1177/0891988720988917
Wendrich-van Dael, A., Bunn, F., Lynch, J., Pivodic, L., Van den Block, L., & Goodman, C. (2020). Advance care planning for people
living with dementia: An umbrella review of effectiveness and experiences. International journal of nursing studies, 107, 103576. https:// doi.org/10.1016/j.ijnurstu.2020.103576
Kelly, A. J., Luckett, T., Clayton, J. M., Gabb, L., Kochovska, S., & Agar, M. (2019). Advance care planning in different settings for people with dementia: A systematic review and narrative synthesis. Palliative & supportive care, 17(6), 707–719. https://doi.org/10.1017/S1478951519000257
Giordano, A., De Panfilis, L., Perin, M., Servidio, L., Cascioli, M., Grasso, M. G., Lugaresi, A., Pucci, E., Veronese, S., & Solari, A. (2022). Advance Care Planning in Neurodegenerative Disorders: A Scoping Review. International journal of environmental research and public health, 19(2), 803. https:// doi.org/10.3390/ijerph19020803
Geshell L, Kwak J, Radhakrishnan K. Perspectives and Experiences of Persons With Dementia With Advance Care Planning: An Integrative Literature Review. Journal of Geriatric Psychiatry and Neurology. 2019;32(5):231-245. https://doi.org/10.1177/0891988719853040
Navarta-Sánchez, M. V., Palmar-Santos, A., Pedraz-Marcos, A., Reidy, C., Soilemezi, D., Haahr, A., Sørensen, D., Smidt, H. R., Bragstad, L. K., Hjelle, E. G., Haavaag, S. B., & Portillo, M. C. (2023). Perspectives of people with Parkinson’s disease and family carers about disease management in community settings: A cross-country qualitative study. Journal of clinical nursing, 32(15-16), 5201–5218. https:// doi.org/10.1111/jocn.16636
Soilemezi, D., Palmar-Santos, A., Navarta-Sánchez, M. V., Roberts, H. C., Pedraz-Marcos, A., Haahr, A., Sørensen, D., Bragstad, L. K., Hjelle, E. G., Haavaag, S. B., & Portillo, M. C. (2023). Understanding support systems for Parkinson’s disease management in community settings: A cross-national qualitative study. Health expectations : an international journal of public participation in health care and health policy, 26(2), 670–682. https://doi.org/10.1111/ hex.13691
Tan, S. B., Williams, A. F., & Morris, M. E. (2012). Experiences of caregivers of people with Parkinson’s disease in Singapore: a qualitative analysis. Journal of clinical nursing, 21(15-16), 2235–2246. https://doi.org/10.1111/ j.1365-2702.2012.04146.x
Schulmann, K., Ilinca, S. & Leichsenring, K. (2017). Community care for people with dementia: A handbook for policymakers, EURO. CENTRE.REPORT 10. Vienna: European Centre.
https://www.researchgate.net/profile/Katharine-Schulmann-2/publication/317579245Co mmunitycareforpeoplewithdementiaAhandbookforpolicymakers/links/5940ea 8945851554614adae3/Community-care-forpeople-with-dementia-A-handbook-for-polic ymakers.pdf
Efficiency was king. I watched as Dr. A moved from one patient’s room to the next with speed. Every interaction was fast, clinical. Dr. A’s stoic look, the monotonous beeping of the machines, the click-clack of his keyboard while putting in orders for medications. It was about the metrics–checking off symptoms, ordering labs, staying on schedule. I understood the pressure was what fused the unit together, pushing against inevitable mortality. The medical-surgical floor was busy and full of patients, and time of the essence, but for some, brevity wasn’t something they could afford.
Then there was Ms. Andrews, a younger woman recovering from a salpingectomy as a result of an ectopic pregnancy. She had complaints of severe shoulder pain and was noticeably distressed, grasping her shoulder while Dr. A performed a physical examination. He simply couldn’t brush this off as a normal side effect of surgery. His expression changed swiftly as he took a deep breath in, as though putting a mental halt to the background noise and grounding himself in the present moment. Dr. A took the time to truly listen to Ms. Andrews and ordered a CAT scan to assess the cause of her pain. While her physical pain remained, the burden of the unknown vanished with her results: residual carbon dioxide gas that was trapped in her abdomen had irritated the phrenic nerve. Had Dr. A not taken a few extra minutes to assess her pain levels and understand the cause of her pain and distress, Ms. Andrews would not have recovered as quickly as she did.
What does quality patient care look like in a system that too often prioritizes efficiency and cost-cutting over compassion and individualized treatment? At what point will we transition from seeing patients as case numbers and statistics to human beings in need of listening ears? Quality care in such a world would strive to balance the demands of both time and resources with a deeper need for understanding, dignity, and respect. Patient-centered care encourages healthcare providers taking the time to truly listen, despite the pressures of a system that encourages haste. The provider-patient relationship should be one that is built on trust and consistency, wherein there is no doubt or hesitancy. The difference that just a few more minutes of provider-patient interaction can make is potentially the difference between life and death. We, as the future of healthcare, must strive to make healthcare more humanized, and wholeheartedly and humbly listen to the needs of those in our care.
Smyrna Davalath
The yarn unravels endlessly, Tangled in the looms of my thoughts
With no plans of straightening out.
How the thoughts spread
Through hollow chambers,
Spreading like wildfire
Burning down trees of fragile sanity.
Thump. Thump. Thump.
Footsteps of a giant Bounding on my trampoline heart
Unrelentlessly.
The urge to stand
Thrusting deeper into the wave of thoughts, Drowning.
Eyes red, swollen
Painted with energy.
Staring at the popcorn ceiling
Lost in apprehension.
They say get over it!
As if it is as simple as covering up a rogue speckle of paint, Eliminating a burdening spot.
Little do they know
It is the wrong shade of paint.
Air lingering with fresh peony, Masking my problems
Rather than facing the enemy from within
I come to realize
The enemy is not underneath my bed, Or lurking in the shadowed corners. It exists simply in my mind
In the disguise of a faceless angel, Yet having arms that extend to grasp me tightly
With the force of one ton of rocks.
The enemy is from within
Deceiving me with the mask of sanity
Anthony Valverde
Introduction
The improper distribution of biomedical engineers, specialized physicians, and equipment by the Costa Rican Ministry of Health has left Costa Rican universal healthcare stagnant and questioned by its citizens. Despite its successful implementation of Equipos Basicos de Atencion Integral de Salud (EBAIS) for first response medical attention throughout Costa Rica, these medical centers only hold primary healthcare teams that include a physician, a nurse, and a trained community health worker (Gawande, 2021). If a patient requires anything beyond these services, the EBAIS must send them to a hospital, where hospitals in rural areas are still scarce and lack specialists and equipment. The only hospitals available to provide complete medical treatment are located in the capital of San Jose, forcing patients to travel to the capital while creating a bottleneck in Costa Rica’s three main public hospitals.
In 2016, the Ministry of Health acknowledged the shortage of biomedical engineers and specialized physicians in specific zones but argued that sufficient doctors were certified by El Colegio de Medicos y Cirujanos en Costa Rica (CMCCR). Biomedical engineers specialize in developing and maintaining medical equipment and technologies, while specialized physicians are highly trained physicians in specific fields like cardiology or neurology, offering advanced patient care. However, waiting lists contradicted this claim, as most certified doctors were general practitioners and specialist training is limited to the Universidad de Costa Rica in conjunction with the Caja Costarricense de Seguro Social (CCSS) – Costa Rica’s social security (Avalos, 2016a). Moreover, 91% of specialists work in San Jose, leaving rural areas severely underserved. Even in San Jose, there is insufficient equipment and staff to meet demand, with government-owned biomedical workshops unable to produce adequate devices to treat its demand. As of February 2016, more than 153,000 patients were awaiting surgery with an additional 140,000 amputees needing prosthetics (Avalos, 2016b). The shortage of specialists and equipment prevents adequate care, leaving minor conditions untreated and increasing reliance on private services. This raises healthcare costs and forces patients to self-manage their conditions, highlighting significant ethical
concerns in Costa Rica’s healthcare system.
The CMCCR integrates approximately 700 general practitioners into the workforce annually from eight universities (Avalos, 2016b). However, transitioning from a general practitioner to a specialized physician is highly restricted, requiring a convention between the Universidad de Costa Rica and the CCSS (Avalos, 2016b). The concentration of medical specialization programs in the Central Valley further limits access for aspiring physicians from rural areas.
In 2016, former CMCCR president Alexis Castillo Gutiérrez projected that Costa Rica would need 600 specialized physicians in public hospitals by 2025 (Avalos, 2016b). However, this projection failed to account for the ongoing construction of medical centers in rural areas, further increasing the demand for specialists (Caja Costarricense de Seguro Social, 2021). Even if these physicians were available, the lack of incentives discourages them from working outside urban centers.
Rural healthcare facilities face additional recruitment challenges despite offering higher wages. Specialized physicians gravitate toward urban areas where they have access to better resources and career advancement opportunities. This imbalance exacerbates healthcare disparities, leaving many rural communities underserved.
Costa Rica’s biomedical engineering field faces similar challenges due to limited educational opportunities. The Universidad Latinoamericana de Ciencia y Tecnología is the only institution in the country offering an undergraduate program in Biomedical Engineering (Barquero, 2020). As a result, many aspiring biomedical engineers seek education abroad, leading to a workforce deficit.
An audiologist from Hospital Max Peralta highlighted two major obstacles in the development of biomedical solutions: the shortage of engineers capable of designing new medical devices and the CCSS’s lack of an in-house laboratory for equipment (Valverde and Quesada, personal communication, May 13, 2022). Due to these limitations, Costa Rica relies heavily on foreign designs for medical devices, limiting innovation and production.
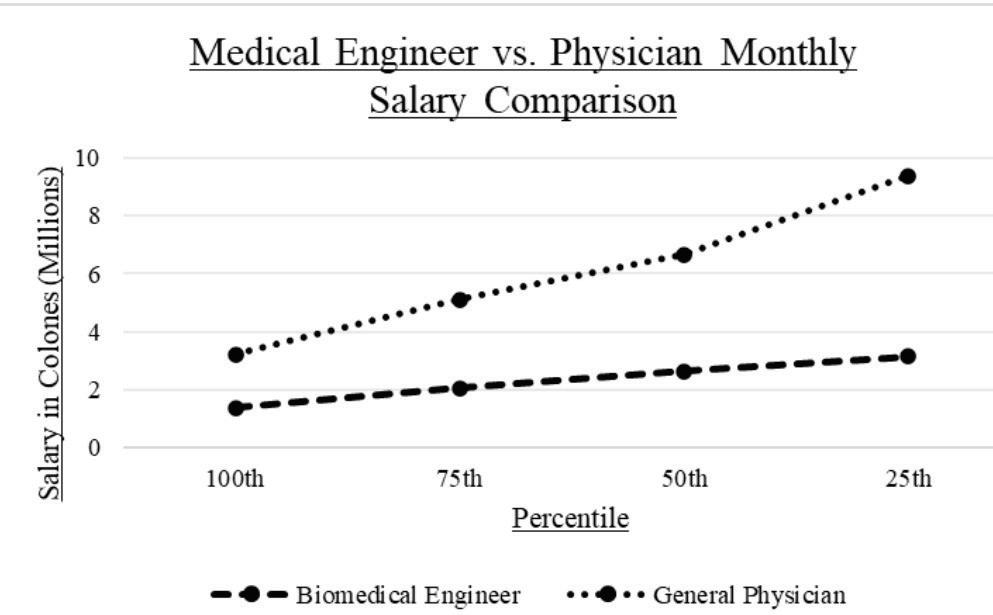
Salary disparities further discourage professionals from entering the field. As Figure 1 illustrates, salary disparities exacerbate the issue— while physicians experience a 13% salary increase every 16 months, only the top 25% of biomedical engineers earn above ₡2,650,000 after 15 years (Salary Explorer, 2021a; 2021b). This financial gap makes biomedical engineering a less attractive career choice, compounding the shortage of professionals. Without stronger incentives and investment in biomedical education, Costa Rica will continue to depend on imported medical technology, limiting its ability to develop tailored healthcare solutions.
Supply and Demand of Biomedical Services and Technology
Data retrieved by ErgoTec – a Costa Rican ergonomic research laboratory – and the Universidad Tecnologica de Costa Rica in 2016, displayed that more than 140,00 Costa Ricans had physical impairments that prevented them from walking or going upstairs. The main bottleneck in the production of biomedical solutions from the CCSS does not exclusively belong to its material and client finances, but also to its dependence on one biomedical workshop.
The Taller Nacional de Ortesis y Prótesis (TNOP), the only solution offered by the CCSS, has experienced an increase in demand of 71%, mainly for prosthetics below the knee, with an increase in patients of 187% (Solis, 2015). It is important to note however, the TNOP is not being accessed by a large portion of the population with physical impairments. Despite 140,000 struggling with mobility challenges, the TNOP has been treating 473 to 2,117 patients a year until 2018 (Barquero, 2020). Many of these amputees have sought the TNOP for biomedical support and have been waiting more than two years (Solis, 2015). Additionally, unlike Don Manuel’s hip prosthetic which was fully funded with
his surgery by the CCSS, only a portion of the limb prosthetic’ cost is funded by the CCSS.
Additionally, the TNOP faces another obstacle when fulfilling its demand; it only produces prosthetics with basic functionalities. If a personalized prosthetic with more complex usage is required, one would have to resort to the Centro de Protesis Avanzadas (CPA), a private Biomedical Engineering company whose clients are primarily medical tourists. Both the lack of biomedical engineers and workshops available are heavily decreasing the TNOP’s capability of fulfilling its demand.
Patient Perspectives on Healthcare Inequities: Don Manuel’s Journey
According to a survey conducted by la Contraloria General de la Republica in regard to the perception of public services in 2018, 76.5% of interviewees reported additional expenses in private medical centers (Fernandez, 2018). As patients evade waiting lists, public employees are pulled to the private sector and the CCSS loses capacitated medics and specialists. However, these patients are still forced to rely on the CCSS biomedical services due to economic barriers when requiring major medical procedures, often facing systemic failures in care. The story of Don Manuel Gimenez, a lifelong coffee grower from Manzano, exemplifies these challenges (Valverde and Gimenez, personal communication, 2022). In 2010, Don Manuel began experiencing severe groin pain that disrupted his daily life (1:20). Seeking care, he followed the required process–first visiting the EBAIS, then being referred to the San Juan de Dios hospital for radiographs to then return to the EBAIS, and then sent back to the San Juan de Dios for treatment. This bureaucratic cycle is meant to regulate patient loads in hospitals and ensure proper treatment allocation, but in Don Manuel’s case, it led to prolonged suffering and instability.
After two years of being incapacitated, he was informed that he would not receive surgery (3:07). At 53, he was deemed “too young” for a hip replacement, as the hospital restricted the procedure to patients over 65 (4:02). This policy aimed at conserving limited medical resources, directly violated nonmaleficence by prolonging his pain and disability. Nine years later, a neighbor eventually recommended the Centro Nacional de Rehabilitacion (CENARE), another CCSS-funded institution, where he received a prosthetic hip within a month (5:22). The delay, however, had already caused unnecessary suffering– an outcome that disregarded beneficence by prioritizing resource allocation over
patient well-being, leaving Don Manuel to suffer unnecessarily for almost a decade. Don Manuel’s experience highlights the ethical failures within the CCSS system, where grid policies, personnel shortages, and bureaucratic obstacles prevent timely medical interventions. His case, however, underscores how these limitations force patients into prolonged hardship, challenging the system’s commitment to patient care.
The shortage of specialists in Costa Rica is not unique, and other countries have implemented strategies to address this issue. Germany, for example, successfully addressed specialist shortages through structured incentives, including financial bonuses, loan forgiveness, career advancement opportunities, and mandatory rural service for new professionals (Busse et al., 2017). These measures encourage healthcare workers to practice in underserved areas, ensuring a more even distribution of specialists. Costa Rica could adapt similar strategies to attract and retain specialists in rural regions, helping alleviate the current shortage and improve healthcare access. Once a structure for rural medical outreach has been established, it must be maintained as the volume of aspiring medical professionals will continue to seek these opportunities. Once we have more incentives than deters. Collaboration between public and private sectors could allow for resource pooling, providing specialists with better facilities and equipment while ensuring broader and more equitable access to care.
Conclusion
Don Manuel’s case highlights both the strengths and shortcomings of Costa Rica’s health care system. While his surgery and rehabilitation at CENARE were successful and free of cost, his treatment journey was marked by frustration, long delays, and significant personal sacrifice. The burden of traveling for care and losing more than a decade of productivity as an agriculturist underscores the need for systemic improvements. No prosthetic or treatment can restore the years he lost. Despite the CCSS’s extensive network of 30 hospitals and 250 clinics (Harrah, 2018), long waiting lists persist due to the ongoing shortage of biomedical engineers and specialized physicians. Without enough biomedical engineers and specialized physicians, rural healthcare facilities remain underutilized, and patients are forced to endure excessive delays or travel long distances for specialized care. Costa Rica’s medical system is essential
for ensuring healthcare access, yet its personnel shortage continues to disrupt its stability. If this trend persists, the strain on public healthcare will worsen, and the growing reliance on private services – available only in the Central Valley to a limited economic group – will deepen inequalities in medical access.
References
Ávalos, Á. (2016, Septiembre 21). Médicos generales abundan mientras faltan especialistas. La Nación. https://www. nacion.com/el-pais/salud/medicos-generales-abundan-mientras-faltan-especialistas/ ELX3CUL7EVCCZFUANWJUKRSPHU/ story/#: :text=Actualmente%2C%20 hay%20835%20m%C3%A9dicos%20 en,El%20otro%2039%25%20son%20especialistas
Ávalos, Á. (2016, August 20). Salud declara escasez de médicos en 7 especialidades. La Nación. https://www.nacion.com/el-pais/ salud/salud-declara-escasez-de-medicos-en-7-especialidades/VCSQAFFUGJGIDON7XZB4VBEZZY/story/
Barquero, K. (2020, August 10). Ulacit pionera en abrir ingeniería biomédica, carrera con alta demanda laboral en el mundo. Periódico La República. https:// www.larepublica.net/noticia/ulacit-pionera-en-abrir-ingenieria-biomedica-carrera-con-alta-demanda-laboral-en-el-mundo
Busse, R., Blümel, M., & Köhler, M. (2017). Health systems in transition: Germany. European Observatory on Health Systems and Policies.
Caja Costarricense de Seguro Social. (2021). Portafolio proyectos de inversión en infraestructura y tecnologías 2021-2030. https://www.ccss.sa.cr/img/proyectos/ portafolio.pdf
Duran, F., & Herrero, F. (2001). Financiamiento del desarrollo: El sector privado en el sistema de salud de Costa Rica. Comisión Económica para América Latina y el Caribe. https://repositorio.cepal.org/bitstream/handle/11362/5086/1/S0104341 es.pdf
Fernández, A. (2018, November 8). El crecimiento de servicios privados de salud y su posible impacto en el sistema de salud costarricense. Semanario Universidad. https://semanariouniversidad.com/ suplementos/crecimiento-de-la-oferta-deservicios-privados-de-salud-y-su-posibleimpacto-en-el-sistema-universal-de-saludcostarricense/
Gawande, A. (2021, August 20). Costa Ricans live longer than we do. What’s the secret? The New Yorker. https://www. newyorker.com/magazine/2021/08/30/costa-ricans-live-longer-than-we-do-whatsthe-secret
Harrah, S. (2014, August 8). Health care around the world: Costa Rica. UMHS. https://www.umhs-sk.org/blog/healthcare-around-world-costa-rica
Instituto Nacional de Estadística y Censos. (n.d.). Anuario estadístico - población. https://www.inec.cr/anuario-estadistico/ anuario-estadistico-poblacion
Quesada, J. (2019, March 14). Solo hay 53 médicos especialistas por cada 10 mil habitantes. CRHoy. https://www.crhoy.com/ nacionales/solo-hay-53-medicos-especialistas-por-cada-10-mil-habitantes/
Medical Technology Schools. (2022, May 11). Biomedical technician schoolsprograms & certifications. https://www. medicaltechnologyschools.com/biomedical-technician
Michigan Technological University. (2021, October 4). What is biomedical engineering? Michigan Technological University. https://www.mtu.edu/biomedical/department/what-is/
Ministerio de Salud, Costa Rica. (2016, August 19). Salud declara escasez de médicos especialistas en zonas y cantidades determinadas. https://www. ministeriodesalud.go.cr/index.php/noticias/noticias-2016/991-salud-declara-escasez-de-medicos-especialistas-en-zonas-y-cantidades-determinadas
Ministerio de Salud, Costa Rica. (2021, March 10). Alcance n° 50 a la gaceta n° 48 de la fecha 10 03 2021. https://www.ministeriodesalud.go.cr/gestores en salud/ conis/regla invest biomedica.pdf
Rupp, S. (2018, January 3). Dearth of biobiomedical engineers delaying medical advancement. Electronic Health Reporter. https://electronichealthreporter. com/dearth-biomedical-engineers-delaying-medical-advancement/
Salary Explorer. (2022). Doctor/physician average salaries in Costa Rica 2022. The Complete Guide. http://www.salaryexplorer.com/salary-survey.php?loc=52&loctype=1&job=13&jobtype=2
Salary Explorer. (2022). Biomedical engineer average salary in Costa Rica
2022. https://www.salaryexplorer.com/ salary-survey.php?loc=52&loctype=1&job=582&jobtype=3#disabled
Segura, H. A. (2015, December 10). Cenare reabrió las puertas a la hospitalización de pacientes para ofrecerles rehabilitación. https://www.ccss.sa.cr/noticias/servicios noticia?cenare-reabrio-las-puertas-a-la-hospitalizacion-de-pacientes-para-ofrecerles-rehabilitacion
Solis, M. (2015, December 10). Tres prótesis al día confecciona la CCSS. https:// www.ccss.sa.cr/noticias/servicios noticia?tres-protesis-al-dia-confecciona-la-ccss
Universidad de Costa Rica, Oficina de Registro e Información. (2021). Cortes por carrera y recinto. Admisión ordinaria. https://ori.ucr.ac.cr/sites/default/files/archivos/2021/Cortes Primer Ingreso-2021. pdf
Umaña, J. (2018, April 10). Ergotec USA impresión 3D y novedosos métodos para hacer prótesis mejores y más baratas. Hoy en el TEC, Tecnológico de Costa Rica. https://www.tec.ac.cr/hoyeneltec/2016/11/30/ergotec-usa-impresion-3d-novedosos-metodos-hacer-protesis-mejores-mas-baratas
Valverde, A., & Quesada, L. (2022, May 10). Estatus biomédico de Costa Rica. https://docs.google.com/document/d/1nsIMTf6wY 5xMOM4rO7O49Tv65WkcogcazRL2hegow/edit?usp=sharing
Valverde, A., & Gimenez, M. (2022, May 11). El caso de Don Manuel GiménezEstatus biomédico de Costa Rica.
Olivia Pinilla
I yearned to hear your voice, that passed like calm waves to my grueling doubts.
I passed by your room adorned with your priceless possessions, yet it lacked your gleaming presence, void of all signs of your memories and marks. We were frightened by endless what-ifs and the unrelenting unknown. How will it end? Would you come back?
You didn’t. You couldn’t.
Your bouts of surviving, outlawed by the infection and its grasp on you. What do we do without you?
No one shares how betrayed you feel, being robbed of closure, selfishly clinging onto moments you didn’t think would last.
How do we continue with our lives, when we couldn’t see you in your last moments. Your body remained in its fragile state, yet your spirit had risen, unbound, unseen.
There are days where I still feel you close, with the wind carrying your songs of laughter and love, But I wish you were still here.
as it happens I have become all bark
Genevieve Carcano
and no bite. there is only so much the mouth is good for.
many strange and spirited betrayals of the body and this one comes on unrecognized, as if I am welcoming an old friend– a vector in disguise–(yet I refuse lovers. cavities are contagious, you wouldn’t want to catch one there, at the vulnerable edge.)
“mountain dew mouth” I never drank soda.
sure, I have a (sweet tooth) I try to hide that one under the tongue.
I didn’t grow up with much. nothing I was born with was mine and I shouldn’t have expected my teeth to be.
they are but the public instrument playing the poor man’s song, the saxophone begging on the side of the street. but it is all off key
and its song is telling me soon I won’t be able to even bark.
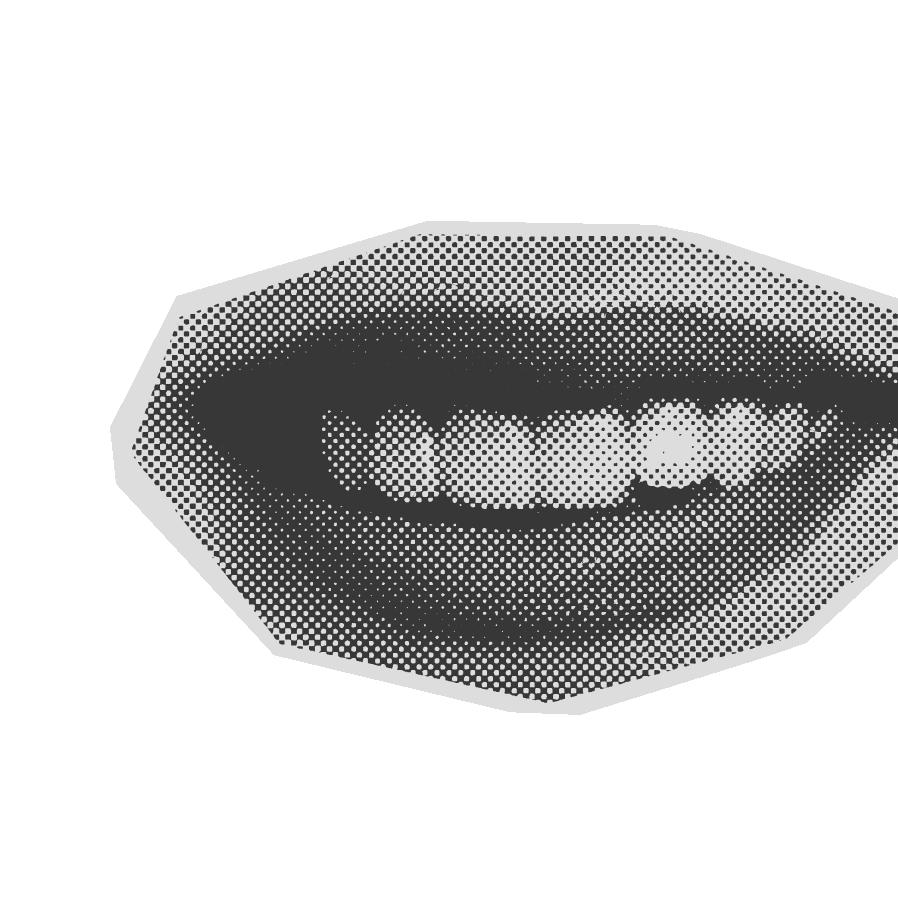
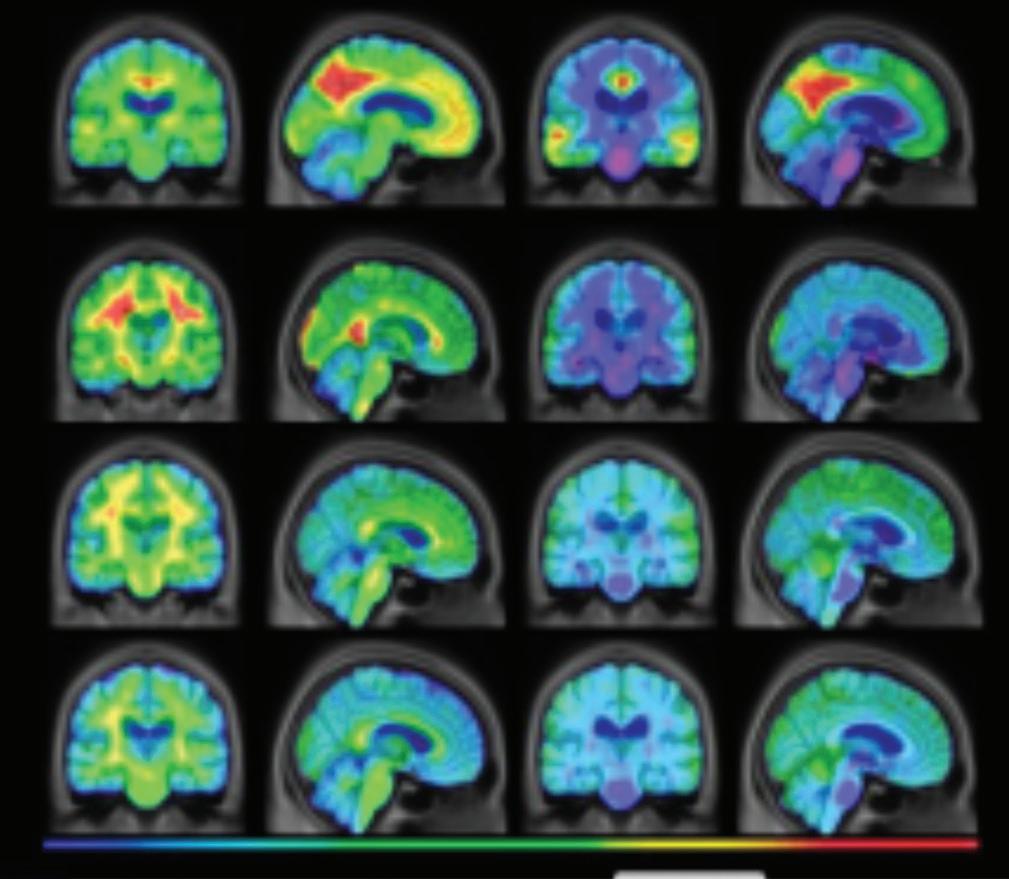
Gabrielle Luisa Dotti
An Insight in Alzheimer’s Disease Alzheimer’s disease (AD) is a brain dis order characterized by the slow decay of brain cells, leading to memory loss, impaired thinking skills, and changes in behavior. As Alzheimer’s Disease is the most common form of dementia worldwide, AD accounts for 60-80% of all dementia cases (Alzheimer’s Association). Symptoms typically begin after the age of 65, with early signs including memory failure and confusion. Over time, the disease progresses to more severe symptoms, such as significant memory loss, mood swings, and difficulty performing tasks. AD disproportionately affects women, with over 6.2 million Americans diagnosed, 4.1 million of whom are women (Budson). Understanding the gender differences in Alzheimer’s is crucial not only for biology but also for the development of a better healthcare policy. A broader perspective, including the humanities, helps frame this issue as not just a medical challenge but also a societal one. Literature, philosophy, and ethics also provide valuable insights into the way Alzheimer’s reshapes identity and interpersonal relationships, reinforcing the urgency of addressing this disparity. Biological, genetic, hormonal, and social factors all contribute to women’s increased vulnerability to AD, offering insights for better detection, treatment, and prevention.
In the early stages of AD, symptoms such
as memory loss, mood changes, language difficulties, and trouble completing daily tasks appear similarly for men and women (Touroutoglou). However, as the disease advances, notable differences emerge in symptom progression and brain changes between genders. Research shows that women’s symptoms tend to progress more quickly than men’s (Reed-Geaghan). Women also have a longer life expectancy by about five years, which increases their likelihood of developing AD in old age due to the gradual death of brain nerve cells over time (Budson). Neuroimaging studies using MRI technology, a non-invasive medical imaging technique that creates detailed images of the body’s internal structures (Mayo Clinic), reveal gender-specific differences in how AD affects the brain. Women’s MRIs frequently show greater atrophy, the gradual wasting away or shrinking of tissue or organs, in the hippocampus and overall brain matter compared to men’s, as well as higher levels of neuroinflammation and other pathological changes (Klingenberg et al.). These findings emphasize the unique biological and clinical pathways through which AD impacts women, underscoring the necessity of gender-specific medical interventions.
A combination of biological, genetic, and hormonal factors increases women’s vulnerability to Alzheimer’s Disease. One key biological difference is the higher levels of amyloid proteins in women’s brains, in which these proteins contribute to its development by forming plaques—masses
of beta-amyloid proteins. These plaques disrupt nerve cell communication and lead to cell death (Reed-Geaghan). Studies suggest that genes associated with beta-amyloid, a protein that is commonly found in small amounts in the brain, are more actively expressed in women, raising their risk for AD (Reed Geaghan). Genetic factors, such as the presence of the APOE-ε4 allele, a genetic variant linked to fat metabolism, have been linked to an increased risk of AD in both men and women, in which research indicates that women with this allele may be at an even higher risk than men (Riedel et al.). Additionally, women’s immune systems tend to display stronger responses compared to men’s, which paradoxically may contribute to neuroinflammation, a chronic inflammatory process that happens in patients with Alzheimer’s Disease (Cleveland Clinic). Microglia, the brain’s immune cells, become activated in response to harmful substances like beta-amyloid plaques. While this activation helps protect the brain initially, excessive inflammation can damage healthy brain tissue and worsen AD progression (Cleveland Clinic). Hormonal changes, particularly related to menopause, also play a critical role. A woman’s risk for AD increases as her estrogen levels decline. Estrogen has neuroprotective properties, including the ability to shield the brain from harmful processes that contribute to AD (Brann et al.). Early menopause or hormonal variations can therefore leave women more vulnerable to developing the disease. The loss of estrogen also ties into broader discussions in humanities disciplines about the ways in which aging disproportionately affects women, shaping their roles in society and healthcare systems.
Biological changes associated with aging, such as the decline in estrogen, are not just medical or physiological events—they also have deep social, cultural, and political implications. From a societal and cultural perspective, aging impacts individuals differently based on gender, and women will often deal with unique challenges as they age. These challenges may include how society views aging, the expectations that are placed on women in various stages of life, and even the resources available to support them in their health and well-being. The decline in estrogen is not just a medical event but is also part of a larger conversation about how healthcare systems deal with the needs of aging populations, particularly for women who are at higher risk for conditions like Alz-
heimer’s disease. As estrogen levels drop during menopause, women face increased risks for conditions like osteoporosis, heart disease, and Alzheimer’s (Valencia-Olvera et al.). This highlights gaps in healthcare, especially in terms of gender-specific care and support for aging women. Beyond physical health, the decline in estrogen impacts emotional well-being and cognitive function, emphasizing the need for healthcare systems and policies to evolve and provide comprehensive care for aging women (Russell et al.).
Two significant studies conducted in Sweden provide really important evidence of women’s increased risk for Alzheimer’s disease (AD), emphasizing the importance of considering gender-specific factors in dementia research. The first study, which analyzed a group of 16,926 individuals, investigated the rates of both Alzheimer’s and non-Alzheimer’s dementia across different age groups (Beam et al.). The results revealed that, while dementia rates were comparable between men and women up until the age of 80, women experienced a significant increase in AD diagnoses after the age of 85, with rates significantly higher than those analyzed in men (Beam et al.). These findings suggest that women’s longer life expectancy do play an important role in their increased vulnerability to Alzheimer’s, as the aging process itself shows to increase the risk for this neurodegenerative disease. The second study, which focused on individuals aged 75 to 79, also revealed a gender disparity in Alzheimer’s diagnosis, with women being diagnosed at a higher rate than men (Fratiglioni et al.). Specifically, the study reported that for every 1,000 individuals, 19.6 women and 12.4 men were diagnosed with Alzheimer’s disease, which emphasizes the gender differences in the beginning of the disease (Fratiglioni et al.). Together, both of these studies strengthen the idea that age is a significant risk factor for Alzheimer’s disease, while also highlighting the importance of more gender-specific research. Such research is crucial to developing specific strategies for prevention, diagnosis, and treatment in the context of women’s unique health risks as they age.
Alzheimer’s disease disproportionately affects women due to a combination of biological, genetic, hormonal, and social factors. Gender-specific differences in brain structure, immune response, and life
expectancy contribute to women’s heightened vulnerability to AD. Recognizing these differences is essential for healthcare providers and policymakers to develop personalized treatment plans, preventative strategies, and support systems tailored to women’s needs. Expanding research into these gender disparities not only advances scientific understanding but also paves the way for improved healthcare practices and policies. The humanities provide a crucial perspective for considering the broader implications of these differences, highlighting the emotional, ethical, and philosophical dimensions of AD. Addressing the implications of these findings for healthcare, caregiving, and future research can lead to better outcomes for the millions of women at risk or living with Alzheimer’s Disease. By incorporating and understanding how Alzheimer’s Disease can be developed both biologically and socially, society can build a more compassionate and effective response to AD that recognizes the deeply human cost of this devastating disease.
References
“Alzheimer’s Disease: Causes, Symptoms, Treatment & Stages.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/9164-alzheimers-disease.
Alzheimer’s Disease International, Mana Communications. Over 41 Million Cases of Dementia Go Undiagnosed across the Globe - World Alzheimer Report Reveals, 21 Sept. 2021, www.alzint.org/newsevents/news/over-41-million-cases-of-dementia-go-undiagnosed-across the-globeworld-alzheimer-report-reveals/
Brann, Darrell W, et al. “Neurotrophic and Neuroprotective Actions of Estrogen: Basic Mechanisms and Clinical Implications.” Steroids, U.S. National Library of Medicine, May 2007, pmc.ncbi.nlm.nih.gov/ articles/PMC2048656/.
Beam, Christopher R et al. “Differences Between Women and Men in Incidence Rates of Dementia and Alzheimer’s Disease.” Journal of Alzheimer’s disease: JAD vol. 64,4 (2018): 1077-1083. doi:10.3233/ JAD-180141
Budson, Andrew E. “Why Are Women More Likely to Develop Alzheimer’s Disease?” Harvard Health Publishing, 20 Jan. 2022, www.health.harvard.edu/blog/whyare-women-more-likely-to-develop alzheimers-disease-202201202672.
Fratiglioni, L et al. “Very old women at highest risk of dementia and Alzheimer’s
disease: incidence data from the Kungsholmen Project, Stockholm.” Neurology vol. 48,1 (1997): 132-8. doi:10.1212/ wnl.48.1.132
Klingenberg, Malte, et al. “Higher Performance for Women than Men in MRI-Based Alzheimer’s Disease Detection.” Alzheimer’s Research & Therapy, U.S. National Library of Medicine, 20 Apr. 2023, www.ncbi.nlm.nih.gov/pmc/articles/ PMC10116672/.
“MRI” Mayo Clinic, 9 Sep. 2023, https://www.mayoclinic.org/tests-procedures/mri/about/pac-20384768
Reed-Geaghan, Erin. “Why Does Alzheimer’s Affect More Women than Men?” BrightFocusFoundation, 1 Sept. 2022, www.brightfocus.org/alzheimers/article/ why-does-alzheimers-disease-affect-more women-men.
Riedel, Brandalyn C, et al. “Age, APOE and Sex: Triad of Risk of Alzheimer’s Disease.” The Journal of Steroid Biochemistry and Molecular Biology, U.S. National Library of Medicine, June 2016, pmc.ncbi.nlm.nih.gov/articles/ PMC4905558/#:~:text=The%20sex%2Dbased%20prevalence%20of,risk%20factors%20for%20Alzheimer’s%20disease.
Russell, Jason K, et al. “The Role of Estrogen in Brain and Cognitive Aging.” Neurotherapeutics : The Journal of the American Society for Experimental NeuroTherapeutics, U.S. National Library of Medicine, July 2019, https://pmc.ncbi. nlm.nih.gov/articles/PMC6694379/
Touroutoglou, Alexandra. “Early Signs of Dementia in Women.” Mass General Brigham, 3 Apr. 2023, www.massgeneralbrigham.org/en/about/newsroom/articles/ early-signs-of-dementia-in-wo men.
Valencia-Olvera, Ana C, et al. “Role of Estrogen in Women’s Alzheimer’s Disease Risk as Modified by Apoe.” Journal of Neuroendocrinology, U.S. National Library of Medicine, Feb. 2023, pmc.ncbi.nlm.nih. gov/articles/PMC10049970/.
“What Is Alzheimer’s Disease?” Alzheimer’ s Association, www.alz.org/alzheimers-dementia/what-is alzheimers.
“Why Is Dementia Different for Women?” Alzheimer’s Society, 8 Mar. 2024,
Gabriella Davis
it seems that your [insert body part here] is too big/too small/too abnormal/too wrong
test (noun): a critical examination, observation, or evaluation. a means of testing. a procedure performed to detect, diagnose, or monitor disease.
draw blood, dissect its structure and soul, measure antigens and antibodies and antinomy check & recheck & recheck & recheck &
Attention: If you or a loved one has been diagnosed , you may be entitled to care and treatment .
can you define your pain, rank it on a scale, and soliloquize your hurt so that they may believe you? doctor, doctor, give me the news is it in my body or my mind? physical or just psychosomatic?
Hi, this is [Insert Name Here] from Dr. [Insert Name Here]'s office.
We just wanted to let you know that all your labs came back normal!
Have a great day!
Adam Mansoor
Dengue fever, caused by the dengue virus (DENV), is a vector-borne disease (VBD) primarily transmitted by Aedes aegypti mosquitoes. Vector-borne diseases are infections spread through the bites of infected arthropods, such as mosquitoes, ticks, and sandflies (Fournet et al., 2024). Dengue transmission occurs when an infected mosquito bites a human, introducing the virus into the bloodstream and allowing it to replicate within the host.
Although dengue is commonly found in tropical and subtropical regions such as Southeast Asia, Central and South America, and the Caribbean, it has not historically been endemic to Florida (Yang et al., 2021). However, recent cases of locally acquired dengue in the state have raised concerns about the virus’s potential for sustained transmission within the United States.
In July 2024, a case report highlighted the emergence of locally transmitted dengue in South Florida, raising concerns about the potential for wider spread (Rodriguez et al., 2024). This concern was realized when, on December 18, 2024, the Florida Department of Health in Hillsborough County reported six new cases of locally acquired dengue fever and issued a mosquito-borne illness alert (Florida Department of Health, 2024). The sustained transmission of dengue fever in Florida is a growing concern, warranting closer examination of the factors that could have contributed to the recent outbreak.
Florida’s warm, humid climate and abundant wetlands create ideal breeding conditions for mosquitoes, significantly increasing the risk of mosquito-borne disease transmission. Since the state experiences high temperatures and frequent rainfall nearly year-round, mosquito populations thrive in stagnant water sources found in marshes, lakes, and even urban environments. These conditions prolong mosquito lifespans, accelerate reproduction, and expand their geographical range, making Florida particularly vulnerable to the threat of vector-borne disease (Filho et al., 2019). Despite the well-documented impact of urbanization on pollinators such as bees and butterflies, less research has been done on how urban environments influence mosquito populations (Fournet
et al., 2024). This research gap raises concerns regarding whether human-modified landscapes may be inadvertently expanding mosquito habitats, creating new risk factors for disease transmission. In addition to environmental factors, human behavior may also play a significant role in the recent rise of dengue cases in Florida. Florida is a major travel destination, attracting millions of visitors each year to its theme parks, beaches, and nature reserves, many of which are outdoor attractions that put both residents and visitors at risk of mosquito bites. Furthermore, a growing number of Floridians have been engaging in outdoor recreational activities, such as hiking, camping, and water sports (Florida Department of Environmental Protection, 2024). Because mosquitoes are most active in warm, humid environments with standing water, prolonged time spent outdoors significantly increases the chance of being bitten (Filho et al., 2019).
Careful assessment and management of urban green spaces are essential to mitigating VBD risks. The built environment contributes to mosquito breeding in multiple ways, such as stagnant water accumulation due to inefficient plumbing, poor drainage systems, and inadequate ventilation in buildings. These factors increase human exposure to mosquitoes and elevate the risk of disease transmission (Abdulwahab et al., 2024; Caminade et al., 2019).
The burden of mosquito-borne illnesses is not evenly distributed across populations. A 2023 study found that lower-income neighborhoods in the U.S. experience 63% greater mosquito densities and higher rates of mosquito-borne illnesses compared to wealthier communities, illustrating a significant public health disparity (Yitbarek et al., 2023).
Globally, dengue fever also exhibits a pronounced disparity in its impact, disproportionately affecting low- and middle-income countries (LMICs). More than 70% of countries and territories affected by dengue and other tropical diseases fall into this category, where urbanization, climate variability, and limited public health resources create ideal conditions for transmission (Manderson et al., 2023). While the scale of poverty and its impact vary worldwide, it is essential to recognize that the burden of dengue is not confined to LMICs. In Florida, economically disadvantaged communities—often characterized by lower income levels—also face heightened vulnerability to VBD out
breaks due to limited healthcare access and aging infrastructure (Melix et al., 2020). Addressing these disparities is crucial to mitigating the impact of dengue in an equitable manner.
Effective dengue fever management requires an integrated approach combining research, community involvement, and equitable solutions. Key strategies include enhanced surveillance, community education, waste management, and vector control (Bardosh et al., 2017). Each of these components plays a crucial role in minimizing disease transmission and protecting vulnerable communities.
Surveillance systems are essential for tracking dengue outbreaks and identifying high-risk areas before they escalate into widespread public health crises. Geospatial mapping and real-time data collection enable public health officials to pinpoint mosquito breeding sites and detect infection trends in specific regions (Bardosh et al., 2017). Strengthening these surveillance systems ensures proactive intervention rather than reactive crisis management, reducing the likelihood of bigger outbreaks.
Community education is one of the simplest yet most effective strategies for dengue prevention. Examples of this approach could include broadcasting public service announcements (PSAs) reminding homeowners to eliminate sources of stagnant water, such as pet bowls or uncovered rain barrels, to mitigate VBD risk. SMS messages regarding personal preventive measures like wearing protective clothing and ensuring window screens are not damaged could also be simple methods of primary prevention.
Poor waste management contributes significantly to dengue outbreaks by creating ideal mosquito breeding grounds. Discarded tires, plastic containers, and clogged gutters can all collect rainwater, allowing mosquito larvae to grow in stagnant water sources (Filho et al.). An effective waste disposal program that focuses on eliminating standing water and reducing litter could decrease mosquito populations in urban areas and minimize VBD risk.
Vector Control Measures
Direct mosquito control remains one of the most effective ways to combat dengue transmission. Traditional strategies that use chemical pesticides may harm the environment. However, biological measures, such as introducing Wolbachia bacteria to reduce Aedes aegypti susceptibility to the dengue virus, have shown success in reducing dengue incidence. A study found that in areas with Wolbachia-infected A. aegypti mosquitoes, there was a 77.1% reduction in symptomatic dengue cases and an 86.2% reduction in dengue-related hospitalizations in Indonesia (Utarini et al., 2021).
Conclusion
The dengue outbreak in Hillsborough County can serve as a catalyst for systemic change in Florida’s approach to vector-borne diseases. Florida could lead in addressing these public health challenges effectively and equitably. As climate change continues to reshape vector-borne disease patterns, comprehensive, equity-driven approaches are more critical than ever in protecting the health of all Florida residents. The fight against dengue fever and other vector borne diseases requires concerted effort from public health officials, researchers, community leaders, and policymakers to implement evidence-based strategies that address the social and environmental factors that contribute to disease transmission.
References
Abdulwahab, A. A., et al. (2024). Climate change, vector-borne diseases, and conflict: Intersecting challenges in vulnerable states. Journal of Infectious Diseases and Epidemiology, 10, 326. https://doi. org/10.23937/2474-3658/1510326
Bardosh, K. L., et al. (2017). Addressing vulnerability, building resilience: Community-based adaptation to vector-borne diseases in the context of global change. Infectious Diseases of Poverty, 6(1), 166. https://doi.org/10.1186/s40249-017-0375-2
Caminade, C., et al. (2019). Impact of recent and future climate change on vector-borne diseases. Annals of the New York Academy of Sciences, 1436(1), 157–173.
https://doi.org/10.1111/nyas.13950
Florida Department of Health. (2024, December 18). DOH-Hillsborough County issues mosquito-borne illness alert update. Florida Department of Health. https://hillsborough.floridahealth.gov/ newsroom/2024/12/MosquitoBorneIllnes-
sAlertDecember1 82024.html
Filho, W. L., et al. (2019). Climate change, health and mosquito-borne diseases: Trends and implications to the Pacific region. International Journal of Environmental Research and Public Health, 16(24), 5114. https://doi.org/10.3390/ ijerph16245114
Fournet, F., et al. (2024). Green cities and vector-borne diseases: Emerging concerns and opportunities. Euro Surveillance, 29(10), 2300548. https://doi.org/10.2807/1560- 7917. ES.2024.29.10.2300548
Manderson, L., et al. (2023). Global dengue fever burden and socioeconomic factors influencing disease spread. International Journal of Public Health Science, 12(3), 87–102. https://doi.org/10.xxxxxx/ xxxx
Melix, B. L., et al. (2020). Florida neighborhood analysis of social determinants and their relationship to life expectancy. BMC Public Health, 20(1), 632. https:// doi.org/10.1186/s12889- 020-08754-x
Rahastri, A., & Sulistyawati, S. (2024). The impact of COVID-19 on dengue cases in low- and middle-income countries: A systematic review. International Journal of Public Health Science, 12(3), 45–62.
Rodriguez, L. O., et al. (2024). Local transmission of dengue in South Florida: A case report. Cureus, 16(7), e65375. https://doi. org/10.7759/cureus.65375
Utarini, A., et al. (2021). Efficacy of Wolbachia-infected mosquito deployments for the control of dengue. The New England Journal of Medicine, 384(23), 2177–2186. https://doi.org/10.1056/NEJMoa2030243
Yang, X., et al. (2021). Global burden for dengue and the evolving pattern in the past 30 years. Journal of Travel Medicine, 28(8), taab146. https://doi.org/10.1093/ jtm/taab146
Yitbarek, S., et al. (2023). Urban mosquito distributions are modulated by socioeconomic status and environmental traits in the USA. Ecological Applications, 33(5), e2869. https://doi.org/10.1002/eap.2869
HEALTH HUMANITIES
ORGANIZATIONS SPOTLIGHT & CONTRIBUTOR BIOGRAPHIES
The intersection of humanities with public health and medicine holds remarkable potential to drive advocacy, nurture empathy, and improve health outcomes. As a health humanities journal, The Capsule strives to spark conversations and raise awareness about the health disparities and inequalities that persist both locally and around the world. At USF, many student organizations are actively working to address these disparities, whether globally or within the Tampa Bay community. This section is dedicated to honoring the missions and achievements of these organizations, while also providing readers with opportunities to take meaningful action in the fight against health inequalities.
The Scribe is a USF-based literary journal started by the Tampa chapter of Sigma Tau Delta. The Scribe accepts a variety of literary-related work written by undergraduate students from all of USF’s campuses. Our team’s goal is to provide students with the opportunity to publish literary analyses and have their work edited by a team of experienced editors. Our journal draws from the diverse and incredible voices on campus and then shares them for students to read and connect with. The Scribe was created to amplify work that unveils the truth and meaning behind literary expression and strengthen the bonds between the community of literature lovers at USF. We are proud to share that this semester, Spring 2025, we will be releasing the first volume of The Scribe!

Project Period (PP) is dedicated to ending period poverty and raising awareness about menstrual health. We organize donation drives, menstrual hygiene kit distributions, educational events, and community collaborations to support those in need. We collect monetary donations and unopened menstrual products during on-campus tabling events. At monthly packing parties in the Marshall Student Center, volunteers assemble kits that are distributed to shelters, low-income schools, and community pantries across Tampa Bay. Our outreach extends beyond campus, ensuring access to menstrual products both locally and internationally. In addition to providing supplies, we fundraise for menstrual health organizations such as Days for Girls, Anera, and Period. org. We also host educational events, stigma-reducing initiatives, and stress-relief activities like arts and crafts to engage students in the conversation about menstrual health. Our mission is to promote menstrual equity by ensuring access to essential products, educating communities, and creating a supportive environment where menstruation is understood and destigmatized.
The Creative Writers Club fosters a diverse community of writers both within and outside of the Creative Writing major/minor. We believe that the art of writing provides insight into our psyche, and that through understanding the stories we create we can begin to understand ourselves.


Women of Color in Medicine was founded in March 2024 to create a supportive community for women of color pursuing careers in the medical field. The club is dedicated to mentorship, professional development, and volunteer work that uplifts both its members and the broader community. Since its inception, the club has hosted impactful events, including an MCAT and DAT workshop to support aspiring medical and dental professionals, a Naga Tea fundraiser, and a "Cards for Hospitalized Kids" initiative where members earned volunteer hours by creating uplifting messages for patients. The club has also welcomed two inspiring women of color doctors as guest speakers, organized a women's hygiene kit sorting event, and volunteered at a local preschool to promote early education and wellness. Through hands-on service, networking opportunities, and skill-building workshops, Women of Color in Medicine empowers its members while fostering meaningful connections. As the club continues to grow, it remains committed to providing resources, advocacy, and a space where women of color in medicine can thrive.
The HPV Awareness Association (HAA) at USF is an undergraduate organization which serves to promote and destigmatize HPV awareness to contribute to global cancer prevention. Human papillomavirus (HPV) is estimated to cause 36,500 new cancer cases each year in the United States, and despite this fact, the topic remains stigmatized and many people are unaware of the information and prevention strategies concerning the virus. For this reason, the HAA strives to address this public health concern through awareness in the form of conferences, seminars, and the dissemination of informational material; advocacy through engagement with policymakers regarding HPV education and vaccination; and fundraising to raise funds for HPV research and accessible HPV vaccinations. Recently, the HAA had a conference- the conference was designed to serve as a pivotal space for the dissemination and driving action of HPV prevention and education in our communities, where two guest speakers (Dr. Daley and Dr. Avila) presented about HPV and its cancer-causing properties. Additionally, students put together 210 safe-sex kits which are being donated to the New Life Church of Tampa. The HAA’s goal is to reach both the youth and underserved communities and equip them with knowledge on and resources for preventing HPV.

Serene Abulhaija (she/her) is a second-year Arab American student majoring in both Biomedical Sciences and Psychology at the University of South Florida. As an Arab American, she is passionate about integrating diverse perspectives into health and the humanities. Serene aspires to attend medical school to become a psychiatrist, combining her love for science and art to explore the human mind. She enjoys using her scientific knowledge as inspiration for meaningful, thought-provoking creations that bridge medicine, mental health, and human experience. She is excited to contribute to The Capsule’s mission of uniting science and the humanities.
Violet Adams (she/her) is a third-year honors student studying Psychology and Environmental Science and Policy. Beyond her studies she is involved in various organizations on the St. Pete campus including the Student Success Center, the USF Family Study Center, and the Student Green Energy Fund. Her hobbies include running, painting, and yoga.
Sandra Aitcheikh (she/her) is a sophomore at USF passionate about how our public health can be improved, especially by pushing education.
Savannah Barker (she/her) is a junior pursuing a degree in English with a concentration in Creative Writing. She is passionate about the literary arts and has always felt called to spread awareness about health and mental health through art.
Noah Bennett (he/him) is a junior at the University of South Florida currently in Biomedical Science. He works as a Registered Pharmacy Technician, and is an avid musician. His first semester was as a double music performance major, but later decided to switch towards a degree in the medical field. He also has interests in marine biology, the ocean, and loves theme parks. After graduation, he hopes to move on to either Medical School or Pharmacy School at USF. Being on both sides of the coin, The Capsule aligns with his mission to share the human experience behind healthcare workers and patients alike.
Genevieve Carcano (she/they) is a senior at the University of South Florida studying both Humanities & Cultural Studies and English. She finds health to be an overlooked area in the Humanities field and hopes to help raise awareness with this poem. Some of her hobbies are reading, shopping, baking, and trying out new coffee shops.
Madeline Damon (she/her) is a senior honors student at the University of South Florida, majoring in Criminal Justice with a pre-law concentration. Post graduation, she has been accepted at Stetson University of Law as a student in the Social Justice Advocacy program. Outside of her academics, she stays busy by engaging with the community through a variety of activities and volunteer efforts, running a small business, traveling for hiking opportunities, and spending time with her animals.
Smyrna Davalath (she/her) is a third-year student at USF majoring in Psychology with a minor in Public Health. Her involvement with the Capsule stems from her desire to share her personal experiences in a creative form and tie mental health experiences with the humanities.
Gabrielle Luisa Dotti (she/her) is a freshman at the University of South Florida, where she is pursuing a degree in Biomedical Sciences. She volunteers and is part of an Alzheimer’s research at Byrd Alzheimer’s Center and Research Institute at USF where she has the goal to help and improve Alzherimer’s patients’ health. In her free time she loves to hang out with her friends on the beach and read books. She also loves to explore the city of Tampa and go to new places. She found writing as a way to express her interest in medicine and helping people and hopes to be a part of The Capsule and share her passion for helping in neuro diseases and writing articles.
Gabriella “Gigi” Davis (they/them) is a fourth-year Honors student majoring in environmental science and English. They’re an award-winning poet and author, with two published personal anthologies. Their interest in health humanities has been fostered by their parents, an obstetrician-gynecologist and a retired paramedic. They believe that exploring the overlap between health and the humanities is essential in creating an environment that prioritizes both the scientific and the sociocultural.
Jordan Hamburg (she/her) is a student at the University of South Florida, where she is pursuing a degree in Biomedical Sciences. She thoroughly enjoys learning about health and medicine as she plans to become a certified anesthesiologist assistant. She also enjoys exploring creative outlets such as art.
Kavery Kallichanda (she/her) is a third-year honors student at the University of South Florida. She is double majoring in Biomedical Science and Biomedical Anthropology with minors in Spanish and Biomedical Physics. She is passionate about exploring the medical humanities and more holistic approaches to medicine as she prepares to apply to medical school. In her free time, she enjoys reading, singing, crocheting, and walking.
Moriah Lee (she/her) is a first-year honors student at the University of South Florida, studying biomedical sciences on the 7-Year BS/MD Program. After graduating, she plans to go to medical school, and become a surgeon. When not studying, she pursues her love for music through piano, guitar, and song writing, and is very interested in exploring connections between the arts and medicine.
Matthew Lim (he/him) is a freshman majoring in BMS at USF Tampa campus. He absolutely loves how The Capsule’s guiding principle is focused on promoting the interdisciplinary study of medicine in humanities as he believes it’s a growing field that needs more attention. He is thrilled The Capsule can promote the voices of each student’s personal passion and extremely thankful for this wonderful opportunity.
Serena Lozandi (she/her) is a Senior at the University of South Florida, majoring in Biology with a concentration in Medical Biology and minoring in Creative Writing. With a strong passion for health equity, she is particularly interested in addressing disparities in healthcare access and outcomes for underrepresented communities. Her academic background bridges the sciences and the humanities, allowing her to explore the intersection of medicine, storytelling, and patient advocacy. She uses her experiences to promote positive health practices among her community as a Health Education Action Team leader and certified peer educator.
Liam Mahony (he/him) is a senior studying philosophy who hopes to connect research in theories on health with philosophical and literary discourse.
Adam Mansoor (he/him) is a second-year honors student at USF who is interested in exploring the intersection of environmental health and public health as it relates to living a healthy life.
Amrita Nayak (she/her) is an honors freshman at USF majoring in Public Health on the pre-med track. Passionate about prioritizing prevention over treatment, she aspires to become a pediatrician. Amrita is an active leader, serving as an officer on the USF PAMSA Community Outreach Committee. Beyond academics, she enjoys performing Indian classical dance and dedicating her time to volunteering with various non-profit organizations.
Jemma Parsons (she/her) is a sophomore majoring in Biomedical Sciences in the 7-Year BS/MD track at USF. Her passion for art has always remained an outlet and beloved hobby that she hopes to pursue in tandem with a medical education, ideally incorporating more anatomical and biological themes as time progresses. She is originally from NYC but is a diehard USF fan and will never skip a home game at Yuengling or RayJay.
Olivia Pinilla (she/her) is a Junior majoring in Biology with a double minor in Public Health and Entrepreneurship & Innovation at the University of South Florida. Olivia has previously been involved with the Capsule, submitting a scholarly article about Parkinson’s Disease for Volume 1. Olivia has actively engaged in public health and the humanities at USF through her involvement in various organizations including Bulls for Moffitt, Dean’s Student Leadership Society, Global Health Catalysts, and the Judy Genshaft Honors College Student Council. She is interested in pursuing concurrent degrees in public health and medicine after college.
Ciana Raley (she/her) is a second-year honors student majoring in Health Sciences and minoring in Psychology. Beyond her schooling, she works at Publix and Great Explorations Preschool, serves as the Public Relations Chair in Planned Parenthood Generation Action, and volunteers at Johns Hopkins All Children’s Hospital. Reading, trying new foods, and traveling are her favorite things to do.
Isabel Reiter (she/her) is a third-year honors student studying Psychology at the University of South Florida St. Petersburg. She serves as the Data and Systems Manager in the PEDS Lab at Johns Hopkins All Children’s Hospital and hopes to become a clinical psychologist concentrating on childhood development. Outside of her academic pursuits, she is also in several leadership roles on her campus as a Tour Guide Captain and a Head Orientation Leader. She enjoys crocheting and reading in her free time.
Hannah Thomas (she/her) is a senior, graduating in the Summer of 2025 majoring in Biomedical Sciences. Her involvement with the Capsule stems from her desire for a creative outlet that intersects both medical science and the arts. She aspires to become a physician and focus her care on patients in underserved or rural areas. On a casual Saturday, you might find her at a bookstore, perusing the classical literature and philosophy sections. When she’s not stressing over exams, she’s trying new recipes and cultivating her passion for photography.
Anthony Valverde-Kong (he/him), is an international student from Costa Rica studying Mechanical Engineering at the University of South Florida. Anthony comes from a Costa Rican-Chinese descent, allowing him a diverse experience and perspective within health and medicine. Currently, Anthony is the founder and president of Bulls Integrative Health Society and is a member of the USF Olympic Weightlifting Club. Anthony also oversees the Marshall Student Center as a building manager and serves as the treasurer for Synergy Central American Alliance, a nonprofit organization focused on allocating funds for conservation within national parks. Anthony’s interests involve olympic weightlifting and environment conservation, which highlight his interdisciplinary passions. His goals include pursuing a PhD in Biomedical Engineering and creating a biomedical consulting company to provide more accessible and equitable product solutions for the people of Costa Rica.
Ren W. (he/him) is a junior at the University of South Florida, where he is majoring in English with a concentration in Creative Writing and minoring in Art Studio. He also serves as the Vice President of the Creative Writing Club. Through his writing and art, Ren seeks to explore and depict the complexities of mental illness, focusing on the struggles that are often overlooked or misrepresented.
