




























August Kingham

My hand is an iron smoothing out creases in examination table paper what passes as linen for a doctor’s bed. I am wishing it would return the favor.
Nailed to the wall across from me is a colorful chart illustrating the levels of pain. Apparently, if I am smiling, it doesn’t hurt.
My pediatrician scratches his head, squints at me, and scribbles a note; I am sent away with the scales fallen from my eyes and strict instructions for my new life; promised they will be my salvation.
Communion looks different now. I have said goodbye to gluten, farewell to fructose. Milk and meat; may we see each other again. My body has become a temple accepting only the purest of offerings while my past burns on the altar.
I am making a pilgrimage to the pharmacy. I part with prescriptions that promise to dull the pain. I am choking on a mouthful of rizatriptan, promethazine, topiramate, and still: my head is splitting apart.
I am sixteen and alone, withering away on the chipped tile of the bathroom floor,
I am forty days without food or water, wandering in the desert of painful solitude but I am not remade; my god has forsaken me. I am so young with so many pills, I have more doctors than friends, I spent prom night in a hospital bed, I have a daily meditation on medication-
So.
I kneel into warrior’s pose every week, feet to the Earth and hands to the heavens, I have a standing appointment for being strategically pierced with tiny needles, Saint Sebastian reinvented,
I journal and track and I pray and I sleep and crucify myself for all these sins but I am still aching.
I want to start over. Take me back.
I want my pediatrician to anoint me with holy oil and ash reach inside my skull and find the original hurt; an apple that rots.
Ask if I am ready to be absolved.
I would have said, “I am.”



Cayley McCloskey
A poem about the birth of a sibling
The warm sunlight rested on your rosy, unblemished cheeks. The noise of the hospital around you silenced at first breath. The family around you awed in wonder, captivated by the beauty of new life.
The moment was infiltrated with love, laughter, tears, astonishment. The mystery of a new life who transformed into my best friend.
A sweet voice cooed and engulfed you in a warm blanket. Your crystal blue eyes fluttered, allowing the new sunlight to pour into your soul.
Friends, family, and providers alike were captivated by your angelic, wispy hair and eyes that twinkled like the sun.
In this moment, the hospital flooded with the love and warmth your new life emitted.

In twilight’s hush, a fading light, There stands a man, a gallant knight. Yet time’s cruel hand, its stealthy creep, Has claimed its toll, in shadows deep.
Oh, my dear grandfather, noble and sage, Your spirit’s fire, a timeless stage. But now, I see, a waning glow, A weakened frame, a steady slow.
Each breath you take, a whispered plea, Echoes of strength, now frailty. Your laughter, once, a vibrant song, Now whispers softly, drawn too long.
The years have etched upon your brow, Tales of triumph, struggles, somehow. Yet, with each passing fleeting hour, I witness life’s diminishing power.
Your eyes, once bright with stories untold, Now mirrored depths, a weariness, a threshold. The vigor that danced in your stride, Fades gently with the ebbing tide.
Oh, how I wish to turn back time, To restore your health, in its prime. To see you rise with youthful grace, And pain and frailty to erase.
But in this moment, I hold your hand, A silent witness to time’s demand. I treasure each tender embrace, In this chapter, a slower pace.
Your wisdom shines, undimmed by age, A beacon, a guide, an eternal stage. Though health may falter,your spirit stands strong, In your legacy, your spirit prolongs.
So here I stand, with love profound, In awe of the strength that still abounds. Your weakening health, a transient phase, Your legacy, a timeless blaze.
Kiara

I am eating again and my Mother is proud of me … she remembers the flood of my emptiness and how many constellations spun in my dizzied belly … the time when I forgot myself human and dreamt myself fever … trying to starve itself into a breath of cool air
I am eating again and my lover has finally met every shadow that I twist to cast … who is a lover if not the one who kisses the places where you split yourself open … who am I if not a constant state of breaking and mending … when the popcorn ceiling is at times all I can swallow … nights spent melting into cold bathroom tiles … is it worth it to love a woman who is sometimes a shell … containing an ocean of echoes … scars lined across the shoreline of skin
I am eating again and how many other ways can I say that I am finally trying to save myself … at least when the sun is out and now it is almost springtime … I finally reset my watch because for the first time I am worried to run out of time … and I guess the music unfolding itself in my head means that I I am healing … I guess that it means there will come a day where I am free
“Sometimes facing the burden together can mend two broken hearts in the end.” The words spoken by Wes Fesler echoed through my mind as my mother and I entered the glass doors to the Intensive Care Unit. I could feel the sweat drip off my mother’s palms and the shadow of fear dissolve across her face as she ruminated on the news that her father had just been airlifted to the West Palm Beach Hospital; bargaining with God for consciousness after a fatal crash. Bobby Williams was not just my 79-year-old grandfather, he was a dedicated teacher, an active member of the church, and a role model for both my mother and I. In addition, my grandfather dedicated the last five years of his life to assisting my grandmother, who had recently been diagnosed with a rare, degenerative neurological condition called Supranuclear Palsy. My grandfather stepped up to become the primary caregiver for my grandmother, who lost her ability to walk, eat, or even form coherent sentences independently. This responsibility impacted my grandfather’s energy and health in various ways, which he often masked underneath the appearance of a jovial, lively man. He had to accept the burden of caring for another life on his own. Sharing his burden did not come until the end of his life where compassion and care came to the rescue. His mind constantly pulled him in various directions, causing him to divert his attention on a busy intersection that became his last commute. Now, my mother and I stand behind the door of a dark, decrepit hospital room, pleading for an opportunity to say goodbye.
The importance of facing the burden together: This sentiment was not only echoed through the way my mother and I depended on each other during these moments but the way the burden was shared amongst the nurses who cared for my grandfather. Empathy can be described as the desire to carry the pain for someone you love. Empathy was continuously shown from my grandfather to my grandmother, and at this moment, the nurses came rushing in like a sea of understanding and support ready to engulf and redistribute our pain. Warm blankets, hot tea, comforting glances. My heart was punctured with the pain of reality, but the nurses bandaged the wound with words
that sounded angelic in the darkness. One nurse pulled me out of my daze, offered consolidation, and revealed another painstaking reality: we were not the only ones experiencing this fight. She lost her mother to cancer only months prior and decided to help others and make her mother proud. A warm smile crept across her face as she uttered the words that continue to echo in my mind: “I know he will be proud of you too.”
2020 was a difficult time for visiting loved ones, as they were essentially prohibited from visiting patients in the hospital for fear of spreading coronavirus to workers and other patients. However, the nurses allowed my mother and I the most precious gift: the opportunity to spend time with our loved one before he passed. Each second spent in his presence felt like the warm embraces he used to engulf me in. Each time I glanced at his face; he still emulated a joyous expression that he carried with him everywhere. Each exhalation he took reminded me of breaths used to explain how to make ginger tea on cold Sunday nights. The genuine smiles, warmth, and space the nurses gifted to my family, and I allowed us all to accept and acknowledge the kiss of grief rather than bearing the heartache alone. With the nurses still present in the room, I kissed my grandfather and whispered “I love you” for a final time. For the first time that day, peace filled my heart and mind. My mother and I solemnly drifted out of the room, but before we made it further, a nurse from my grandfather’s room gently stopped me. “Your grandfather was an excellent patient. We loved him,” she said with a pained smile. I felt my face changing to reflect her expression. The peace I felt after my grandfather passed that night could only be explained by the empathy the nurses and healthcare team displayed to my mother and I during a vulnerable, and dark time. Empathy alleviates the burden and pain that patients and their families experience at times such as these. Facing the burden together mended my heart.




Life is said to be nature’s greatest creation. But what about death? Is it the final chapter, Or the prologue to a new beginning?
People search for immortality, A Fountain of Youth.
But is everlasting pain worth perpetual suffering? Like thorns on a bed of roses, each petal adorned with the price of time.
Why must the end of our journey be veiled in obscurity, wrapped in shadows, or perhaps the light? The light toward peace, A radiant path with golden hues leading to a mystical haven, Where whispers of a gentle breeze cradle our spirits.
Believed to be painful, When it is only relieving, Breaking free from the chains of mortality, Into a place unknown, like a lotus unfolding from the depths of muddy waters.
Death is inevitable, An undeniable destiny to be embraced with reverence. For it is the knot of life and thread of humanity, Each knot a testament to the richness of history, And each thread with lifetimes of experience Woven together to form a borderless tapestry.


the clock ticks on and my mother is awake.
how can she sleep when she still feels it? the blood and the death are leaden as they coat her skin like a vengeful glass of wine. she can’t remember when it spilled, but she knows she’s stained red.
she’s told me that the hangover lingers.
my mother watches as the stars rise and fall. she watches as the sun burns the darkness away, finding solace in the hope that maybe one day the sun will burn the darkness in her too.
a new day begins and she knows she should be looking forward, but
she cannot peel her eyes from the bodies behind her. she could give them all of her, but there would still be suffering— suffering that she cannot carry for them.
her bones are broken, her muscles strained. it is time for breakfast, but she has no appetite. all she tastes is blood. it coats her throat as she stares at the wall.
the clock ticks on and my mother is awake.
i don’t think she’ll ever sleep again.

“Do you love someone one moment and hate them the next?” the cookie-cutter psychiatrist asked.
His buzzing computer filled the emptiness of my silence. In the eternity I required to catch my breath, the robotic man sitting across from me lifted his gaze and we locked eyes. They were beautiful; big and blue, which I had forgotten as he stared at the endless mental illness questionnaire on his laptop. He interrogated me with his questions, trying to puzzle me together as if he could find my defects on his screen. In that brief gaze, we were just two humans at the same clinic, at the same time, in the same office. I snapped back into reality as I pondered on how strange it is to be asked about loving someone one moment and hating them the next.
What does it say about me that my answer is yes?
The first time I was introduced to Bipolar Disorder, I was in high school watching 90210 Beverly Hills. My favorite character, Skylar, had a manic episode that resulted in her running at night searching for her jock boyfriend in hopes of making a sex tape. Her eyeliner smeared into a raccoon resemblance and her actions were obviously irrational.
“She’s so crazy,” my sister said.
I echoed that perception. An echo that, unbestowed to me, entered the cave of my own overlooked cries for help; the layers of my trauma accumulating in my deep black cave. It would soon catch up to me.
The following year, I saw a video of an unstable bipolar woman in my AP Psychology class. She was paranoid that an imaginary person was out to get her, clawing through her blinds eager to spot enemies trespassing her property. There was never anyone there. Like echoes she could feel but could not touch. The imaginary enemy she restlessly searched for was closer than she thought — her own mind. Her own mind, running in a hamster wheel of mania like Skylar. Her own mind, winning a race with no prize.
Her own mind has captured her as a prisoner.
This psychiatrist has caught me. Captured me like a bird in a cage or like Skylar when she was found unconscious on a railroad track.
My psychiatrist’s blue eyes announced he could see right through me and my pretty smile. He saw my golden-brown eyes for what they have become, black caves. He doesn’t even know me, yet he knows my death sentence. He pokes me with his questions as I shrivel up in a gloomy cage.
To some, Bipolar means crazy. I know it did to me. Bipolar meant sex tapes and imaginary enemies. Bipolar meant a cage and a cave or echoes of pain that accumulated to shouts of depression and heartache.
While Bipolar meant many things to me on my journey, the constant truth is that bipolar disorder, a medical diagnosis, is an accumulation of symptoms — it is not a person. Many individuals experience symptoms, and perhaps that leads to irrational behaviors, but that is not who they are. Many individuals experience challenging symptoms and can still maintain fulfilling lives. The most extraordinary people I have ever met overcome their diagnosis every day.
Now, Bipolar means resilience. Now, Bipolar means endurance.
You’re reading my Capsule entry, aren’t you?


Samhita Challa
Summer, St. Pete, Organic Chemistry in 10 weeks. 4th-floor apartment overlooking an empty campus. Sunken red eyes, empty coffee cups.
A call:
“He’s critical, but don’t worry.
We’re going to India; will you be alright?”
“Yes. Will you guys be okay?”
“Yeah, we’ll be back the 19th.”
Their return told me the truth; Gone

“I am fine, sweetheart,” She says, when I am there. “Oh … it hurts!” when I am not.
In my absence, her act crumbles, revealing the depth of her pain. Her words, constructed to shield me from worry, dissolve into her suffering.
“My leg hurts, I cannot do this any longer,” as tears roll down her eyes, her hands acting as napkins to wipe them away.
“But I will continue to work. Cross borders and seas. We need our kids, we need their future, bright as the rising sun.”
Her heart, conquered by determination, she keeps pushing forward, fueled by passion and fire, building us a world where we can thrive, where hope reigns and dreams come alive.
She wears dresses now. The kind that is pink and down to your ankles, her legs are always hidden from my sight. She moves with a grace, that seems to challenge the limits of time and space. Each step of hers, a silent symphony of elegance and pain.
Her dress swayed by the air, dancing in harmony with her spirit. And though her legs remain hidden, the strength and beauty that lies beneath is heard in every footstep.
I can hear her whimper at night, so her cries would not be heard. I tip-toe to my room and stare at the ceiling, wondering what is wrong with her leg.
I climb off the bed and walk to the door. But something makes me immobile. It whispers to lift the blanket off her.
I see her naked leg, with streams of blue rivers. Those varicose veins, all through her legs.
Those veins, they seem to jump out. So does she, by the feeble touch of my hands.
We lock eyes. She realizes, I know it all, and envelopes me in her open arms.
She says, “This pain is worth your happiness.” Do what is best for you,” and smiles with a curve unending.
In these moments, I hold her close, Offering comfort for the burdens she carries silently. Though those varicose veins pull her to the ground, and her agony pierces through the facade, her resilience shines through those slits, reminding me of the unwavering love that binds us together.
Love always, Your child.
A man in his mid 70s sat in his psychiatrist’s office, confessing his inability to focus on tasks particularly when developing speeches for university lectures and events. Oftentimes when attempting to craft a speech, he would take constant breaks, dissociate, and evade the writing process despite his efforts. This lifelong dilemma only intensified with age.
As a shadow in the room, this case immediately captivated my attention, and I eagerly awaited the psychiatrist’s response to the patient’s testimony. The psychiatrist astutely observed that the patient’s absent-mindedness, short attention span, and difficulty focusing indicated towards Attention-Deficit/Hyperactivity Disorder (ADHD). This led to a conclusive diagnosis.
I watched as the patient’s jaw dropped. Unbeknownst to him, ADHD had silently accompanied him throughout his life, while he endured labels of “dumb” and “lazy” (despite his brilliant mind). He revealed that while in grade school, he received below-average grades and faced reprimands such as scolding and even spanking due to his inability to concentrate in class. These labels followed him for decades and even affected his personal relationships. The psychiatrist confirmed that such experiences and labels were common amongst individuals with undiagnosed ADHD.
This patient’s diagnosis is but one example of the countless individuals that navigate their lives with undiagnosed ADHD. This is often accompanied by judgment and diminished self-esteem. The patient’s story, among many others, shed light on the pervasive misconceptions surrounding ADHD. This is an issue that transcends the health care system and dives into the intricacies of societal biases and personal resilience.
This poignant encounter served as a reminder that disabilities and disorders go beyond the surface of individuals and can go unnoticed for years. Society’s tendency to label individuals without truly understanding them aggravate the challenges that such individuals face. If this narrative enlightens even a small community, fostering less judgment and more acceptance, the patient’s legacy will endure, leaving a permanent impact on the perception of ADHD and the individuals who live with it.




Many social, economic, and geographical barriers can prevent patients from getting necessary healthcare resources. Resources are limited, and healthcare professionals face the consequences of unequally distributed resources every day. The issue of resource distribution has disproportionately impacted minority and low socioeconomic status communities because of the lack of health insurance prevalent in these communities and the rising cost of healthcare (Office of Disease Prevention and Health Promotion). Models of resource distribution, such as the first-come-first-serve model, the utility model, and the prioritarianism model, attempt to bridge this divide to ensure that individuals can access necessary healthcare resources regardless of socioeconomic barriers. These models will be analyzed in terms of fundamental ethics such as beneficence, nonmaleficence, and justice. Beneficence is defined as actions that are in the best interest of the patient, nonmaleficence is defined as preventing harm to the patient, and justice is defined as impartial treatment of patients.
The first-come-first-serve model states that the patient who has waited for the longest for a healthcare resource should be the first to receive the resource. The main goal of this approach is to achieve absolute equality by providing care

regardless of individual patient characteristics. The first-come-first-serve model is unique because it only considers one factor while resource allocation models often depend on a range of factors that can introduce bias such as treatment history and urgency. One example of these factors impacting patient care can be seen in a case presented by Dr. David Hilfiker, whose patient complained of chest pain. Dr. Hilfiker assumed the pain was due to the patient’s recurring angina and stated that the pain was not an emergency. 20 minutes later, the patient went into cardiac arrest and passed away (Hilfiker). Like many physicians, Dr. Hilfiker used his past experiences with the patient to evaluate the urgency of the problem. Although he did not intend to do so, Dr. Hilfiker caused harm to one of his patients by making a biased, and thus unjust, assumption about the patient’s condition. In contrast, the simplicity of the first-come-firstserve model would have prevented any unjust biases from affecting patient care as it only relies on waiting time.
This model primarily aims to ignore other factors, such as socioeconomic status and race, when allocating resources. However, these factors can impact patients in many ways and cannot be dismissed. An example of this could be seen in patients who do not have healthcare resources such as health insurance. These patients are often diagnosed much later and in a more
severe condition (Garfield et al.) Another example can be seen in patients with end-stage renal disease, ESRD. Studies have found that African Americans are more likely to end up developing ESRD and needing a transplant than their white counterparts (Taber et al.). A late diagnosis, which could be caused by an inability to access healthcare resources or psychosocial factors that cause distrust between the African American population and healthcare professionals, could be the reason African Americans are more likely to need a transplant (Ng et al.). Because African Americans are not diagnosed as quickly, African Americans also are half as likely as their white counterparts to get an organ transplant (Taber et al.). This could be because the organ transplant list uses a first-come-first-serve model, leading later-diagnosed individuals to be closer to the bottom of the list (United Network for Organ Sharing). Thus, ignoring the impact of these factors on the patient’s healthcare access and severity of disease would cause further healthcare disparities in the impacted populations.
The utility model, also known as the maximizing benefit model, states that resources should be allocated to the patients who will benefit from the resources the most. These benefits can be quantified by considering predicted survival rate, years of life gained, and quality of life (Organ Procurement and Transplantation Network). An example is New York’s guidelines surrounding the distribution of ventilators in situations with a shortage. These guidelines state that under circumstances with a limited number of ventilators, the primary goal is to save the most lives possible. Thus, the ventilators should be given to those most likely to survive. (New York State Department of Health).
The utility model upholds the ethical principle of beneficence by emphasizing the efficient use of resources. Patients with better health outcomes will have less need for continuous care and will consume fewer resources. By minimizing the resources used, healthcare professionals can give resources to patients who need treatment. Thus, this model allows for maximum benefit to the most people possible.
However, this model can conflict with principles such as nonmaleficence. Physicians are, first and foremost, advocates for their own patients, not the patient with the best prognosis. The utility model allows physicians to access resources but does not allow them to use the resources to treat their patients unless they have a better prognosis. This would cause harm to the patient who is not receiving the resource, thus violating the ethical principle of nonmaleficence.
This model can also be unjust. As stated, the benefits to a patient post-treatment are quantified through factors such as quality of life (Organ

Procurement and Transplantation Network). Quality-of-life evaluations can often be biased and perpetuate stereotypes against patients with chronic illnesses, congenital disorders, and disabilities. For example, a non-disabled physician might believe that a disabled patient has a lower quality of life, while the patient might have differing beliefs. It would be unjust to say one person should receive a scarce resource because of a better prognosis, which patients have no control over, thus allowing stereotypes to create unequal access to healthcare resources.
The prioritarianism model prioritizes treating patients with the worst prognosis if left untreated. This model is used in the emergency room, where patients with life-threatening issues are always prioritized. The medical community widely accepts this model, as seen through the American Medical Association promoting it in its Code of Medical Ethics (American Medical Association).
This model can uphold justice as it does not consider a patient’s previous health condition as a barrier to receiving treatment. An example is a patient who has refused to comply with physician recommended treatment plans, such as a smoker patient with lung cancer. Some may argue that using resources on the patient will be futile, as the patient will most likely need further treatment if the risk factor is not resolved. However, healthcare providers are morally obligated to do what is best for the patient, regardless of the patient’s lifestyle. Denying treatment based on a patient’s lifestyle choices would be unjust, and by not considering previous health conditions, this model is able to uphold justice.
However, the prioritarianism model can violate the ethical principle of nonmaleficence. Patients who have worse prognoses might require prolonged treatment, which can be problematic in a setting with limited resources. By prioritizing patients who are worse off, patients with better outcomes might become more severely affected while waiting for care, thus further harming the patient.
Resource shortages are frequent in healthcare, and it is vital to consider the ethical dilemmas that can arise when allocating resources. Historically, minority groups and underserved populations have had significant barriers in accessing high quality healthcare to both treat and prevent chronic conditions (Shadmi). There is no ideal model that can eliminate the problem of healthcare disparities and resource distribution. However, by acknowledging the different factors that contribute to this disparity and creating unique models based upon the fundamental ethics of medicine, the healthcare field will be better equipped to handle the varying needs of many
different populations.
American Medical Association. “11.1.3 Allocating Limited Health Care Resources.” ama-assn. org, 2017, policysearch.ama-assn.org/policyfinder/detail/11.1.3%20Allocating%20Limited%20 Health%20Care%20Resources?uri=%2FAMADoc%2FEthics.xml-E-11.1.3.xml. Accessed 22 Apr. 2023.
Garfield, Rachel, et al. “Key Facts About Health Insurance and the Uninsured Amidst Changes to the Affordable Care Act.” kff.org, 25 Jan. 2019, www. kff.org/report-section/the-uninsured-and-the-aca-aprimer-key-facts-about-health-insurance-and-the-uninsured-amidst-changes-to-the-affordable-care-acthow-does-lack-of-insurance-affect-access-to-care/#:~:text=Because%20uninsured%20patients%20are%20 also,rates%20than%20those%20with%20insurance.
Hilfiker, David. “Facing Our Mistakes.” The New England Journal of Medicine, vol. 310, no. 2, Massachusetts Medical Society, Jan. 1984, pp. 118–22. https:// doi.org/10.1056/nejm198401123100211.
New York State Department of Health. “Ventilator Allocation Guidelines.” New York State Department of Health, Nov. 2015, www.health.ny.gov/regulations/task_force/reports_publications/docs/ventilator_guidelines.pdf. Accessed 22 Apr. 2023.
Ng, Yue-Harn, et al. “Does Racial Disparity in Kidney Transplant Waitlisting Persist After Accounting for Social Determinants of Health?” Transplantation, vol. 104, no. 7, Wolters Kluwer, July 2020, pp. 1445–55. https://doi.org/10.1097/tp.0000000000003002.
Office of Disease Prevention and Health Promotion. “Access to Health Services - Healthy People 2030.” health.gov, health.gov/healthypeople/priority-areas/ social-determinants-health/literature-summaries/access-health-services.
Organ Procurement and Transplantation Network. “Ethical Principles in the Allocation of Human Organs.” Organ Procurement and Transplantation Network, optn.transplant.hrsa.gov/professionals/by-topic/ethical-considerations/ethical-principles-in-the-allocation-of-human-organs. Accessed 22 Apr. 2023.
---. Learn How Organ Allocation Works. optn. transplant.hrsa.gov/patients/about-transplantation/ how-organ-allocation-works. Accessed 22 Apr. 2023.
Scheunemann, Leslie P., and Douglas B. White. “The Ethics and Reality of Rationing in Medicine.” Chest, vol. 140, no. 6, Elsevier BV, Dec. 2011, pp. 1625–32. https://doi.org/10.1378/chest.11-0622.
Shadmi, Efrat. “Disparities in multiple chronic conditions within populations.” Journal of comorbidity vol. 3, Spec Issue 45-50. 24 Dec. 2013, doi:10.15256/ joc.2013.3.24
Taber, David J., et al. “Twenty Years of Evolving Trends in Racial Disparities for Adult Kidney Transplant Recipients.” Kidney International, vol. 90, no. 4, Nature Portfolio, Oct. 2016, pp. 878–87. https:// doi.org/10.1016/j.kint.2016.06.029. United Network for Organ Sharing (UNOS). “How We Match Organs.” UNOS, unos.org/transplant/
how-we-match-organs/#:~:text=The%20first%20 step%20Before%20an%20organ%20is%20allocated%2C,order%20that%20the%20other%20candidates%20will%20receive%20offers. Accessed 22 Apr. 2023.
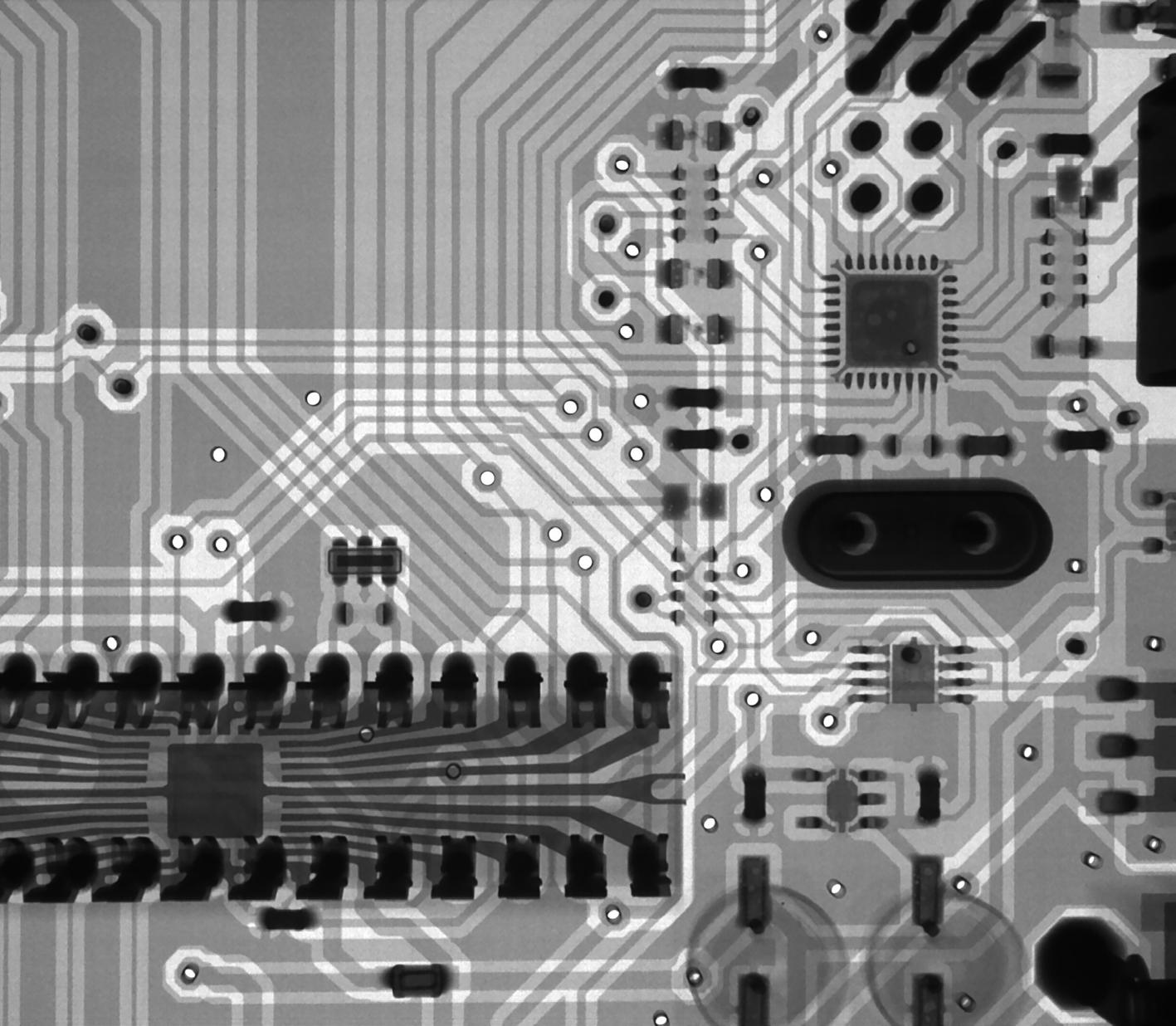
A physician’s capacity to make good decisions is central to trust in the patient-physician relationship. However, there has been a rise in artificial intelligence (AI) and machine learning (ML) systems that can outperform physicians and specialists in certain decision-making tasks. For example, a collaboration between Google Health and physician scientists led to the development of a model that outperformed radiologists in detecting breast cancers from mammograms (Killock, 2020). From the perspective of beneficence to society, AI should be adopted in some way to improve decision making in regards to patient outcomes. This, however, creates some discomfort when the physician and the AI are at odds with each other – especially when the physician is right.
In a world where AI is increasingly responsible for decision making, it becomes ever so more crucial for patients to be able to trust AI. The physician-patient relationship is built on trust and transparency throughout the decision-making process. As the role of decision-making shifts to AI, algorithms need to be transparent to be held accountable (de Laat, 2018). A major issue with certain ML algorithms is that they are designed to be opaque in how decisions are made, termed the “black-box issue” (Reddy et

al., 2019). If AI is utilized too much and lacks transparency, it may undermine the relationship between physicians and their patients, leading to reduced trust and decreased patient autonomy. This decreased autonomy comes from the lack of informed consent that “black-box” technologies necessitate. As such, it is important to prioritize the explainability of AI (Amann et al., 2020).
The incorporation of AI into healthcare adds stakeholders to the ethical challenges regarding responsibility and liability for decision making. When AI is used in the decision-making process, it is important to reevaluate who the stakeholders are in ethical dilemmas. Situations arise where physicians may be at odds with what an algorithm may recommend for diagnosis or treatment. In these scenarios, liability may fall upon the AI model and its developers if proven inaccurate, or it may fall upon the physician if they are proven wrong in their decision and the AI was ultimately right (Grote & Berens, 2020). To clarify the physician-AI relationship from a liability standpoint, regulatory entities may need to make new protocols to assess the liability in certain scenarios on the part of the physician and the AI.
The status quo sees decision making authority shift from physicians to algorithms. It is import-
ant in this new world to make sure that we are balancing the authority of decisions between the physician and the AI, while also making sure to acknowledge the limitations of both stakeholders. As we emerge to a society that is based more on relying on AIs for decision making, it is important to hold these algorithms accountable through increased transparency methods and proper liability delegation.
It is important to remember that technological innovation is good if ethical principles are held up. Technology must attempt to be a force for beneficence in society as long as it doesn’t compromise the other virtues. This calls for innovation in the realm of ML models, but also for disclosure about the limitations of models. The use of algorithms is very good in medicine, but it must be ensured that algorithms are balanced with good ethics.
Amann, J., Blasimme, A., Vayena, E., Frey, D., Madai, V. I., & the Precise4Q consortium. (2020). Explainability for artificial intelligence in healthcare: A multidisciplinary perspective. BMC Medical Informatics and Decision Making, 20(1), 310. https://doi. org/10.1186/s12911-020-01332-6
de Laat, P. B. (2018). Algorithmic decision-making based on machine learning from big data: Can transparency restore accountability? Philosophy & Technology, 31(4), 525–541. https://doi.org/10.1007/ s13347-017-0293-z
Grote, T., & Berens, P. (2020). On the ethics of algorithmic decision-making in healthcare. Journal of Medical Ethics, 46(3), 205–211. https://doi. org/10.1136/medethics-2019-105586
Killock, D. (2020). AI outperforms radiologists in mammographic screening. Nature Reviews Clinical Oncology, 17(3), 134–134. https://doi.org/10.1038/ s41571-020-0329-7
Reddy, S., Allan, S., Coghlan, S., & Cooper, P. (2020). A governance model for the application of AI in health care. Journal of the American Medical Informatics Association, 27(3), 491–497. https://doi.org/10.1093/ jamia/ocz192
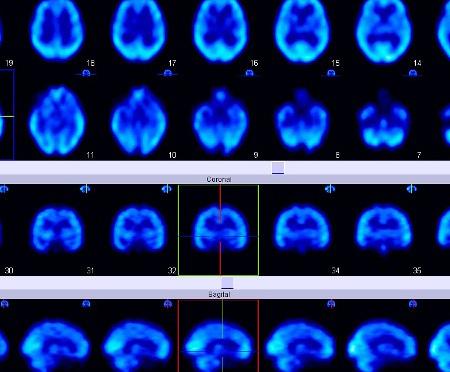
Parkinson’s disease (PD) is a neurological disorder that affects the motor functions of the brain and the production of dopamine needed to control body movements. It is a degenerative disease that causes movement problems, usually identified with the presence of tremors in the hands, slowness in pace, or rigidity in one’s posture. The impact of the disease differs from person to person, depending on how early the diagnosis was made, the patient’s symptoms, and response to medication. PD has been studied immensely and researchers have been able to conduct research in a multitude of fields pertaining to the subject, yet the exact cause of PD is still being studied. There are currently multiple advanced treatments for PD, but there is still no cure. Additionally, there are still no diagnostic tests that can directly identify PD, and diagnoses are instead being made based on patient medical history and physical exams (Armstrong & Okun, 2020).
Although the cause and cure of Parkinson’s disease are being researched immensely, there is a lack of focus on developing advanced support systems for PD patients. All around the world, patients don’t have experienced caretakers and proper accessibility services to help them support their quality of life due to financial challenges and the severity of their disease. For

this reason, providing patients better care and support should be a top priority. By uplifting the PD community that consists of healthcare providers, researchers, patients, and their loved ones, Parkinson’s disease can remain a topic of high importance for the healthcare sector to focus on.
Advancements have been made in terms of finding the cause of Parkinson’s disease, yet there seems to be a lack of research analyzing how genetic differences across ethnicities impact the severity or likelihood of getting the disease. With theories around what factors affect one’s susceptibility to PD, genetic analyses that span across various ethnicities can provide data that is more conclusive. Focusing more on genetic research and support programs for PD patients would promote community awareness of the disease and allow patients across multiple populations to have a bigger representation within the PD research sector (Armstrong & Okun, 2022).
As the global presence of Parkinson’s disease continues to increase, there should be a greater emphasis on how PD impacts communities which genetic research can achieve by analyzing differences on a genomic scale. It is shown that while environmental factors contribute to risk of developing PD, genetic differences account for varying levels of cognitive decline amongst Black and Hispanic patients in comparison to White patients (Ben-Joseph et al., 2020). Many studies
show that in selected ethnic populations, there are differences in susceptibility to certain diseases compared to White populations (Ben-Joseph et al, 2020). Additionally, the prevalence of PD across the world was the highest in areas with larger geriatric populations due to age being a risk factor (Ben-Joseph et al., 2020). However, it is evident that genetic variation amongst populations has a significant impact on how PD affects individuals (Ben-Joseph et al., 2020). In terms of future research, there should be a better focus on populations that contain more ethnic variation to garner a larger gene pool and document more accurate findings.
Lack of healthcare resources in third-world countries can prevent PD patients in those locations from receiving proper care and diagnosis of the disease. There is an increased need for accessible care, PD treatments, and neurospecialists for the consistently rising level of PD cases in those areas. Although these countries receive assistance from PD foundations and global health organizations, there is still a disparity in levels of care minorities receive compared to majority populations. Even in countries that have structured healthcare systems to support PD patients, like the United Kingdom, there was an imbalance in the number of Black patients that were seen by neurologists in comparison to White patients (Ben-Joseph et. al, 2020). There should be an increased effort to provide better care to these underserved communities and also gain a better insight on how PD impacts these underrepresented populations (Ben-Joseph et. al, 2020).
Parkinson’s disease disengages motor functions and can progress greatly in a short period of time, leading to the inability to speak coherent sentences or to stand up and walk for even a short period of time. When an individual is diagnosed with PD, they are often seen as a perfect soul in a broken body, with their quality of life slowly declining. This illusion of being ‘broken’ or incapable of living a fulfilling life is harmful to the patient’s mental and physical wellbeing, which is why developing support programs for the PD community should be a priority especially due to the growing population of PD patients that is expected to double in the next decade. Programs, such as community-based participatory research (CBPR), have been found to increase awareness of PD within communities and increase health literacy with PD patients by establishing relationships within these new populations (Kipnis et al., 2024). By implementing more support programs that are community-based, PD patients will have better life outlooks after their diagnosis (Kipnis et al., 2024).

Technology has made support systems more accessible and assists greatly for its use in telehealth, yet many PD patients still struggle to stay connected to their healthcare providers and attend scheduled appointments for their treatments (Riggare et al., 2022). Following the COVID-19 pandemic, great advancements have been made in accessibility to healthcare through the use of Telehealth. Because the PD population tends to be of older age, the majority of people may not be as comfortable using technology in comparison to the younger populations. However, multiple health organizations have simplified technology to make it easier for use by PD patients. (World Health Organization, 2022).
Although there have been efforts to create better treatment options for PD patients, it is important to acknowledge the current advancements that have already been made to reflect and find the best methods of suppressing the symptoms and progression of PD. Currently, carbidopa and levodopa are the leading medications for PD. Since PD leads to the loss of neurons and therefore decreases the amount of dopamine in the brain, levodopa acts as a building block for dopamine to offset these decreased levels, and carbidopa acts as extension of levodopa, allowing it to last longer on smaller dosage periods (Css-Admin, 2022). The carbidopa/levodopa combination subsides tremors and lack of coordination and balance, and dosage is adjusted according to the patient’s symptoms. Although carbidopa/levodopa is able to treat the leading symptoms, it doesn’t help with the overall progression of the disease, and also has side effects such as dizziness and nausea (Css-Admin, 2022). A major side effect of using levodopa includes dyskinesia, which includes rapid involuntary movements throughout the body such as swaying and fidgeting (Css-Admin, 2022). With the creation of new medications that target more symptoms caused by PD, there has been a rise in efforts to provide treatments that cater to every patient’s needs (Css-Admin, 2022).
Research advancements have generated important information on the cause and progression of PD, but in the future, resources should be allocated towards conducting genetic research and improving support programs that assist PD patients and their loved ones. Effective collaboration is key to learning more about the disease and the patients. This can lead to a better understanding of what their needs are and encourage the creation of better support systems and programs (Riggare et. al, 2021). Numerous foundations, such as the Michael J. Fox Foun-
dation for Parkinson’s Research and the Parkinson’s Foundation, are dedicated to finding a cure and uplifting the PD community to promote their mission of ending PD for good. The PD community has the capabilities to improve our efforts exceptionally, by providing a supportive and comforting environment for PD patients and by expanding on our research efforts for a cure.
Armstrong, Melissa J., Okun, Michael S. “Diagnosis and Treatment of Parkinson Disease: A Review.”
JAMA : the Journal of the American Medical Association, vol. 323, no. 6, 2020, pp. 548–60, https://doi. org/10.1001/jama.2019.22360.
Ben-Joseph, Aaron et al. “Ethnic Variation in the Manifestation of Parkinson’s Disease: A Narrative Review.” Journal of Parkinson’s disease vol. 10,1 (2020): 31-45. doi:10.3233/JPD-191763
Riggare, Sara et al. “A Long Way to Go: Patient Perspectives on Digital Health for Parkinson’s Disease.” Journal of Parkinson’s disease vol. 11,s1 (2021): S5S10. doi:10.3233/JPD-202408
Css-Admin. “Carbidopa/Levodopa: Side Effects, Dosages & More Faqs: APDA.” American Parkinson Disease Association, 16 Mar. 2022, https://www.apdaparkinson.org/article/carbidopa-levodopa-answers-to-frequently-asked-question s-2/.
Gilbert, Dr. Rebecca. “New Treatments for Parkinson’s Disease: APDA.” American Parkinson Disease Association, 19 Oct. 2021, https://www.apdaparkinson.org/article/new-treatments-for-parkinsons-disease/.
Kipnis, Danielle, et al. “Community-Based Participatory Research Approach to Address Health Care Disparities Confronting Members of the Black Diaspora with Parkinson’s Disease.” Parkinsonism & Related Disorders, vol. 119, 1 Feb. 2024, pp. 105936–105936, https://doi.org/10.1016/j.parkreldis.2023.105936.
World Health Organization. “Parkinson’s Disease.” World Health Organization, World Health Organization, 2022. https://www.who.int/news-room/factsheets/detail/parkinson-disease.

The
Noise Pollution on Global Citizens Living in Urban and Rural Environments: A ReviewKavita Parbhoo
Noise pollution and its impact on health are being increasingly recognized by researchers. Noise not only affects the auditory system but also causes annoyance and increased disturbances to sleep (Munzel). As noise levels continue to rise in several locations around the globe, increasing numbers of individuals are faced with problems including but not limited to hearing loss, increased physical and mental health risks, and decreased success in their daily lives. Despite the known effects of increased noise exposure on the auditory system, noise is proven to disturb sleep as well as increase annoyance and risk of contracting several non-auditory diseases (Munzel). The prevalence of noise is increasing in magnitude and severity because of growing populations and urbanization (Thattai et al). The World Health Organization (WHO) claims that noise pollution is second only to air pollution in terms of the environmental health threat in Europe (Bonn and Copenhagen). However, this problem is not limited to Europe. City traffic is one of, if not the most, common sources of noise in large urban areas. Countries around the world are filled with dense urban populations that contain background noises severe enough to cause hearing loss and several other health risks like cardiovascular disease (CVD) and declines in mental health. Noise-induced hearing loss (NIHL) is commonly referred to as the “silent epidemic,” and it goes unrecognized in

several nonoccupational settings as well (Balanay and Kearney). With an increasing number of individuals moving into larger cities, the threat that noise pollution poses to global populations needs to be addressed. These effects will continue to worsen over time, especially with the introduction and development of newer technologies and machinery.
The Centers for Disease Control and Prevention (CDC) states that noise levels above 70 decibels (dB) over a prolonged period of time will begin to damage one’s hearing (CDC). Safe sounds and noises include breathing, normal conversation, and machinery hums. On the other hand, noises such as city traffic (as heard while inside a vehicle) and louder machinery such as a washing machine or dishwasher are at the 70 dB mark. At this level, an individual may feel some slight annoyance. Many sounds and noises that are heard daily, such as lawnmowers, motorcycles, subway trains, radios and stereos, shouting, and sirens, have a noise level of 90 dB and higher. These sounds can result in damage to hearing and possible hearing loss after just 1 to 2 hours of exposure. Exposure to loud events, such as sporting events, loud entertainment, and even car horns, can lead to potential hearing loss after 5 to 15 minutes (CDC). Many of these sounds are extremely common in larger city environments, and some sounds are louder than one
may think. The U.S. Environmental Protection Agency, as well as the World Health Organization, recommend maintaining environmental noise levels below 70 dB over 24 hours to prevent noise-induced hearing loss (CDC). However, these levels of sound exposure are often never maintained due to noise established by headphones, construction sites, traffic in large cities, and other common factors that increase environmental noise levels.
Noise pollution presents a serious problem for those living in all kinds of environments around the globe. From dense, urban cities to rural environments, noise plays a significant role in the negative physical and psychological effects experienced by citizens. Noise has been found to cause several health disparities with cardiovascular or neurological origins. Additionally, psychological impacts include the development of several mental disorders including but not limited to depression, anxiety, and cognitive decline. Further research must be conducted regarding the impacts of noise pollution in rural areas, as there is not sufficient evidence to firmly establish which types of noises are causing which outcomes. Furthermore, noise reduction strategies should be implemented in all areas, along with general education on the impact of noise pollution and its sources. With traffic and vehicular noise having one of the most emphasized impacts on human health and well-being, solutions are suggested to be implemented for more positive outcomes. Noise pollution poses a serious threat to human health and will continue to worsen if not addressed in an appropriate manner.
Balanay, Jo Anneg, and Gregoryd Kearney. “Attitudes toward Noise, Perceived Hearing Symptoms, and Reported Use of Hearing Protection among College Students: Influence of Youth Culture.” Noise & Health, vol. 17, no. 79, 2015, p. 394, doi:10.4103/14631741.169701.
“What Noises Cause Hearing Loss?” Cdc.gov, 8 Nov. 2022, https://www.cdc.gov/nceh/hearing_loss/what_ noises_cause_hearing_loss.html.
Munzel, T., et al. “Cardiovascular Effects of Environmental Noise Exposure.” European Heart Journal, vol. 35, no. 13, 2014, pp. 829–836, doi:10.1093/ eurheartj/ehu030.
Bonn & Copenhagen. “New Evidence from WHO on Health Effects of Traffic-Related Noise in Europe.” Who.int, https://www.who.int/europe/news/item/3003-2011-new-evidence-from-who-on-health-effectsof-traffic-related-noise-in-europe. Accessed 1 Feb. 2024.
Thattai, D., et al. “Analysis of Noise Pollution Level in a University Campus in South India.” IOP Conference Series. Earth and Environmental Science, vol. 80, 2017, p. 012053, doi:10.1088/17551315/80/1/012053.

Alcohol consumption among college students is a significant public health concern due to its potential consequences, which may include academic issues, increased engagement in risky behavior, and traffic fatalities. The academic issues associated with alcohol consumption can include missed classes, poor academic performance, and even dropping out of school. Students who drink are more likely to participate in risky actions such as driving intoxicated, engaging in unprotected sex, and abusing drug substances. Therefore, it is crucial for college students to be aware of the potential consequences of drinking and make responsible choices when it comes to alcohol consumption. This includes setting drink limits, avoiding binge drinking, and never drinking and driving. Additionally, seeking support from on campus resources such as counseling services and peer support groups can help address underlying issues that may contribute to excessive drinking. By raising awareness and promoting responsible alcohol consumption, the negative impact of alcohol on college students’ lives can be reduced and increase the quality of their health (National Institute on Alcohol Abuse and Alcoholism, 2020) .
Alcohol is a commonly used and frequently misused legal substance, and there is a well-established link between driver alcohol consumption

and traffic accidents. As any prosecutor is aware, excessive use of alcohol is at the heart of many criminal cases, contributing to the well-established link between driver BAC (Blood Alcohol Concentration) and traffic accidents. The increased release of dopamine associated with alcohol consumption can also contribute to the positive reinforcing effects of alcohol, leading to addiction (Rubenzer, 2008). Alcohol can also cause blood vessels to dilate, resulting in flushing, warmth, and a decrease in blood pressure (Rubenzer, 2008). While moderate drinking may not pose significant risks, excessive and prolonged alcohol use can have detrimental effects on the body.
The higher the BAC level, the more pronounced the effects of alcohol on an individual’s cognitive and physical abilities, making it more dangerous for the individual to engage in certain activities such as driving. Thus, it is recommended that individuals do not drive with a BAC level of 0.08 or higher, or 0.04 for those operating commercial vehicles such as trucks (Davies & Bowen, 2000). The BAC in the entire body is proportionate to the total body water content since alcohol is completely soluble in water (Brick, 2006). Due to physiological variations, water content may vary depending on the individual. As a result of the low water content of fat cells, obese individuals have 5 pounds less water per pound of body weight than those of typical
build (Martin et al., 2013). Compared to men, women often have a larger percentage of body fat. Body water makes up around 68% of the weight of an average male, compared to 55% of the weight of an average female (Martin et al., 2013). It’s important to understand that BAC can also vary significantly from person to person based on other factors such as metabolism, alcohol tolerance, and food intake. Therefore, it’s difficult to predict an individual’s exact BAC without a blood test. Failing to consider individual differences can result in inaccurate BAC levels (Bloomberg et al., 2005).
Alcohol consumption poses numerous public health risks, including increased chances of accidents and injuries. One of the most significant risks associated with alcohol consumption is driving under the influence (DUI). Many states have implemented strict penalties for DUI, including the use of ignition interlock devices (breathalyzer devices installed in vehicles) for convicted offenders (Brick, 2006). Since alcohol impairs cognitive and physical abilities, consuming it poses a danger to those operating motor vehicles (Martin et al., 2013). The National Highway Traffic Safety Administration (NHTSA) in the United States has established guidelines and regulations related to BAC limits to promote safe driving and reduce alcohol-related accidents. BAC calculations are commonly used in forensic investigations, clinical settings, and public health research. The NHTSA has published guidelines for calculating an individual’s BAC and computing the correlation between alcohol intake and intoxication (NHTSA, 1994).
In the Bloomberg relative risk study, it was found that among drivers who survived fatal crashes, the risk of crash involvement across all ages and genders increased with a statistical S-shaped curve as the driver’s BAC level increased (Bloomberg et al., 2005). To parallel the correlation between BAC and the risk of being involved in a fatal car accident, the relative risk of crashing is higher at all BACs, specifically with BACs of 0.08 and higher (Bloomberg et al., 2005). The results of this study highlight how the probability of being involved in a traffic accident is significant, regardless of how low an individual’s BAC is, but increases at 0.08 and higher.
According to the NHTSA, almost 31% of all traffic crashes that occurred in the United States involved drunk drivers (NHTSA, 2022). In 2021, there were 13,384 people killed in these preventable crashes. (NHTSA, 2022). Despite various efforts to improve road safety, alcohol-impaired driving remains a pressing issue in the United States. The statistics provided are a sobering reminder of the substantial number of lives lost and the significant proportion of traffic fatalities attributed to this dangerous behavior.

It underscores the ongoing need for initiatives and measures to combat this problem and make the roads safer for everyone.
Conclusion
Alcohol consumption among college students presents an array of public health concerns ranging from academic issues to possible traffic fatalities. The ramifications associated with excessive drinking extend beyond individual health, and can have adverse effects on society. Understanding the physiological and behavioral factors that influence BAC is essential for an accurate assessment and effective intervention. Although progress has been made, the persistence of alcohol related accidents underscores the need for a comprehensive approach.
To prevent occurrences of impaired driving, educational campaigns can be conducted to create awareness, while stricter DUI laws and enforcement can be implemented to discourage driving under the influence. In addition, promoting alternative modes of transportation, such as ride-sharing services or public transportation, can provide a safe and reliable means of transportation for those who consume alcohol. As a result, encouraging responsible drinking can promote overall public health and safety. The best way to prevent DUI-related accidents and legal issues is not to drink and drive. Designating a sober driver, using rideshare services, or relying on public transportation are responsible alternatives. It’s crucial to prioritize responsible drinking and never drink and drive, as alcohol impairs judgment and reaction times, significantly increasing the risk of accidents and injuries on the road.
References
Blomberg, Richard D., et al. “The Long Beach/ fort lauderdale relative risk study.” Journal of Safety Research, vol. 40, no. 4, Aug. 2005, pp. 285–292, https://doi.org/10.1016/j.jsr.2009.07.002.
Brick, John. “Standardization of alcohol calculations in Research.” Alcoholism: Clinical and Experimental Research, vol. 30, no. 8, 25 July 2006, pp. 1276–1287, https://doi.org/10.1111/j.1530-0277.2006.00155.x.
Davies, B T, and C K Bowen. “Peak blood alcohol prediction: An empirical test of two computer models.” Journal of Studies on Alcohol, vol. 61, no. 1, Jan. 2000, pp. 187–191, https://doi.org/10.15288/ jsa.2000.61.187.
“Drunk Driving.” NHTSA, National Highway Traffic Safety Administration, 2022, www.nhtsa.gov/ risky-driving/drunk-driving.
Martin, Teri L., et al. “A review of alcohol‐impaired driving: The role of blood alcohol concentration and complexity of the driving task.” Journal of Forensic Sciences, vol. 58, no. 5, 23 July 2013, pp. 1238–1250, https://doi.org/10.1111/1556-4029.12227.
National Highway Traffic Safety Administration. “National Highway Traffic Safety Administration.”
Encyclopedia of Law Enforcement, 2004, https://doi. org/10.4135/9781412952415.n323.
National Institute on Alcohol Abuse and Alcoholism. (2020). College drinking. Retrieved from https:// www.niaaa.nih.gov/publications/brochures-and-factsheets/college-drinking
Rubenzer, Steven J. “The standardized field sobriety tests: A review of scientific and legal issues.” Law and Human Behavior, vol. 32, no. 4, 2008, pp. 293–313, https://doi.org/10.1007/s10979-007-9111-y.

The integration of humanities in public health and medicine has the immense potential to advance advocacy, foster empathy, and increase health outcomes. As a health humanities journal, The Capsule’s aims include raising discussion and awareness of existing health disparities and inequalities in our communities and globally. Several student organizations here at USF are active in fighting health disparities and inequalities globally or in the Tampa Bay community. This section is dedicated to celebrating these organizations’ missions and accomplishments as well as providing opportunities for readers to directly combat health inequalities head-on.
We are Thirst Project at USF.
Thirst Project at USF is a nonprofit organization aimed at ending the global water crisis by building freshwater wells in developing communities that are in need of safe, clean drinking water. Water plays an incredibly critical role in effectively treating or managing AIDS. Our current mission is focused on providing 100% coverage of safe, clean drinking water to the entire Kingdom of Eswatini- a small country in southern Africa that has the single highest–density HIV/AIDS population in the world. As an organization, we spend most of our efforts fundraising to build wells, volunteering, and raising awareness on the lasting epidemiological, economic, and social effects of unsafe drinking water.


We are Hearts for the Homeless.
Hearts for the Homeless is an organization dedicated to bridging the health equity gap through our volunteering services. Our mission here at H4H Tampa is to contribute to the health of people experiencing homelessness through blood pressure and mental health screenings that are sensitive to their life experiences. Our foundation is built on eliminating disparities, especially in the underserved populations. In the past year, we have consistently visited local shelters and churches to take blood pressure for undeserving folks to decrease the risk of cardiovascular disease. We additionally host GBMS for members to connect, donation drives and training sessions for students to get cleared in taking blood pressure and mental health screenings.

MSCD is an undergraduate club focused on uplifting and creating a safe space for underrepresented groups in the field of Communication Sciences and Disorders (CSD), which includes Speech-Language Pathology and Audiology. As of 2021, only 8.7% of CSD professionals identify as a minority. Our club’s mission is to represent the minority population in the CSD field and promote the field to more diverse populations. We are the only student organization of this kind in the state of Florida. Club activities involve hosting guest speakers to discuss their experiences as minorities and provide advice to undergraduate students looking to go into the CSD field. The club additionally hosts de-stress events, community outreach, and sharing opportunities around the community.


Project Downtown Tampa is USF’s premier homeless support organization dedicated to the physical, intellectual, and emotional empowerment of Hillsborough County’s homeless population. Our mission is to “feed only for the sake of God alone. Neither reward nor thanks do we wish” (The Qu’ran 76:8-9). Our organization visits the Tampa Bay Community every Friday, making sandwiches and passing out water without a falter for the past 15+ years. Our volunteers serve hot food made fresh from Jannah Market, hand-made hygiene kits, relief blankets and anydonations we receive from the community.

UAMWA at USF provides a support network for women and other gender minority students during their pre-health journeys at USF. We welcome all students who identify as women to our club on pre-health tracks such as premed, pre-PA, and pre-nursing students. We offer service opportunities at places like the American Cancer Center Hope Lodge, mentorship from USF Morsani medical students, and provide MCAT, application prep materials, and shadowing resources. We additionally host events every semester such as suture clinics and women in medicine events for networking and exposure to the medical field. Our club’s mission is to create a welcoming community for pre-health women to gain the support they need on their journeys into the healthcare field.


DM at USF is an inclusive and diverse student organization dedicated to fundraising and bringing awareness to Johns Hopkins All Children’s Hospital, St. Petersburg through Children’s Miracle Network through year-long events and activities. Many of these events include dodgeball tournaments, Fall Fests, and Bloom events where individuals could connect. Dance Marathon takes place each year and this year we raised around $43,0000! Don’t be fooled by the name, Dance Marathon is so much more than just dancing! This year it was circus-themed with activities such as escape rooms, lip sync battles, live performances, raffle items, free food, giveaways, henna, and more. Most importantly, the children and families affected most directly by the donation were there to tell their stories, play games with the dancers, and celebrate the yearlong effort of raising funds and awareness for John Hopkin All Children’s Hospital. Join and get involved with this incredible organization today!
GenConnect is an undergraduate club combining healthcare and technology via community outreach. Our club’s mission is to educate senior citizens about the importance of technology and its benefits. Our curriculum includes teaching seniors how to communicate with loved ones on social media, find entertainment and learn about basic cybersecurity. The club organizes volunteer opportunities for members to teach senior citizens at nursing homes either in-person or virtually. This is alongside club general body meetings where members can learn more about volunteering, the curriculum and gift-making for senior citizens. We believe this club is a great initiative to bridge the gap between generations.



Sarah Ahmad (she/her) is a current sophomore at USF studying Biomedical Sciences in the 7 year BS/MD program. She is passionate about public health research, specifically understanding the way diseases disproportionately impact minority communities. Outside of academics, Sarah enjoys spending time volunteering at local nonprofit clinics and participating in community outreach!
Alphy Maria Antony (she/her) is a senior graduating in Health Science at University of South Florida, Tampa. She enjoys writing poems and reading all genres of books in her leisure time. She has been writing since 7th grade, with topics always revolving around mental health and the different perspectives of it. She believes her poems are open for personal interpretations, such that the readers can pick the pieces they relate to and take it in, as they understand it. Her piece“To: mom”, brings light on a medical condition named ‘varicose veins’ that several adults suffer from prolonged standing during their work or personal life.
Amira Elfeel (she/her) is a 4th year Public Health student who is also pursuing a minor in Chemistry on the pre-health track. Since Amira is interested in health professions, she aspires to work with underserved populations through volunteering and service activities to alleviate and understand disparities that these communities may face. She plans to use her progression within the public health field to combat social inequities in healthcare.
Cali Camp (she/her) is a sophomore at USF, pursuing a degree in English, with a Creative Writing concentration and a minor in Linguistics. She is the blueprint of the angsty bisexual poet stereotype. Cali enjoys coffee, concerts, and writing about the ones she loves/hates. When she isn’t partaking in literary activities, you can find her in her bed, likely sleeping.
Samhita Challa (she/her) is a sophomore majoring in Biomedical Sciences at USF, planning to become a physician. She’s passionate about bioethics and understanding how medicine can be practiced with a greater emphasis on patient centered care.
Riya Choksi (she/they) is a fourth-year student double majoring in Biomedical Sciences and Psychology at the University of South Florida. Through her research, she hopes to gain a better understanding of the effects of music on coordination and cognition in preschoolers. Riya has been serving on the USF HOSA executive board since 2022, where they guide students through various healthcare professions and assists in conducting all organization events. Beyond these career-related activities, they enjoy graphic design and writing poetry for Sparks magazine.
Ryan Chowdhury (he/him) is a sophomore studying Biomedical Sciences with a minor in Psychology. He is interested in exploring the connections between art, music, and health. Ryan’s academic pursuits include investigating the intersection of scientific advancements and human experiences, particularly within the field of health humanities. Outside of his studies, he enjoys engaging with various forms of artistic expression and believes in the importance of interdisciplinary approaches to promoting holistic wellness.
Cobi Gardner (he/him) is a graduating senior at the University of South Florida. He is a studio art major focusing on ceramics and photography.
Sofia Girgenti (she/her) is a first-year student at USF, studying behavioral healthcare. She is from Tampa and has enjoyed writing her whole life. She also is passionate about music and the outdoors. She he hopes to continue writing for many years to come and appreciates the opportunity to share and better her work.

August Kingham (he/they) is a student at University of South Florida, where he is pursuing a degree in Creative Writing. He is physically disabled, queer, and a Florida native. He also works part time as an Editor for Creation Literary Magazine. August writes about religion in the mundane, the strange within the ordinary, and growing up different. You can find him on Instagram @_augustblues.
Arelis Rodriguez Martinez (she/her) is a current junior studying English at the University of South Florida. Rodriguez Martinez is a Puerto Rican author that prides herself on her holistic approach to creating both music and literature. Her focus, and hope, is to offer a loving, healing, and captivating perspective to the reader - no matter the genre, to inspire readers like the authors that have personally impacted her. Bipolar, based on true experiences, has been written in hopes to provide a different perspective to mental illness and contrast lingering stigmas in our society.
Andrea Marcano-Rodriquez (she/her) is a second-year majoring in Biology and minoring in Political Science. She plans on pursuing a career in Forensic Psychiatry.
Cayley McCloskey (she/her) is a second-year honors student studying Health Science with the aspirations to become a Nurse Practitioner. She works at Moffitt Cancer Center and interns at Tampa General Hospital to further her understanding of how to improve patient care. In her free time, she loves to explore her passion for music by teaching violin, and involving herself in USF Symphony Orchestra, USF Honors Orchestra and Honors Choir. She also enjoys writing and speaking and engages these hobbies as the host of The Honors LLC Podcast and an editor for the Tampa Chapter of the Citizens Climate Lobby.
Kavita Parbhoo (she/her) is a senior at the University of South Florida, graduating in Spring of 2024. She is majoring in Cell and Molecular Biology and minoring in Psychology. After she graduates, she plans on attending medical school to pursue a career as a cardiothoracic surgeon one day. Some of her hobbies include baking, reading, weightlifting, and spending time with her family.
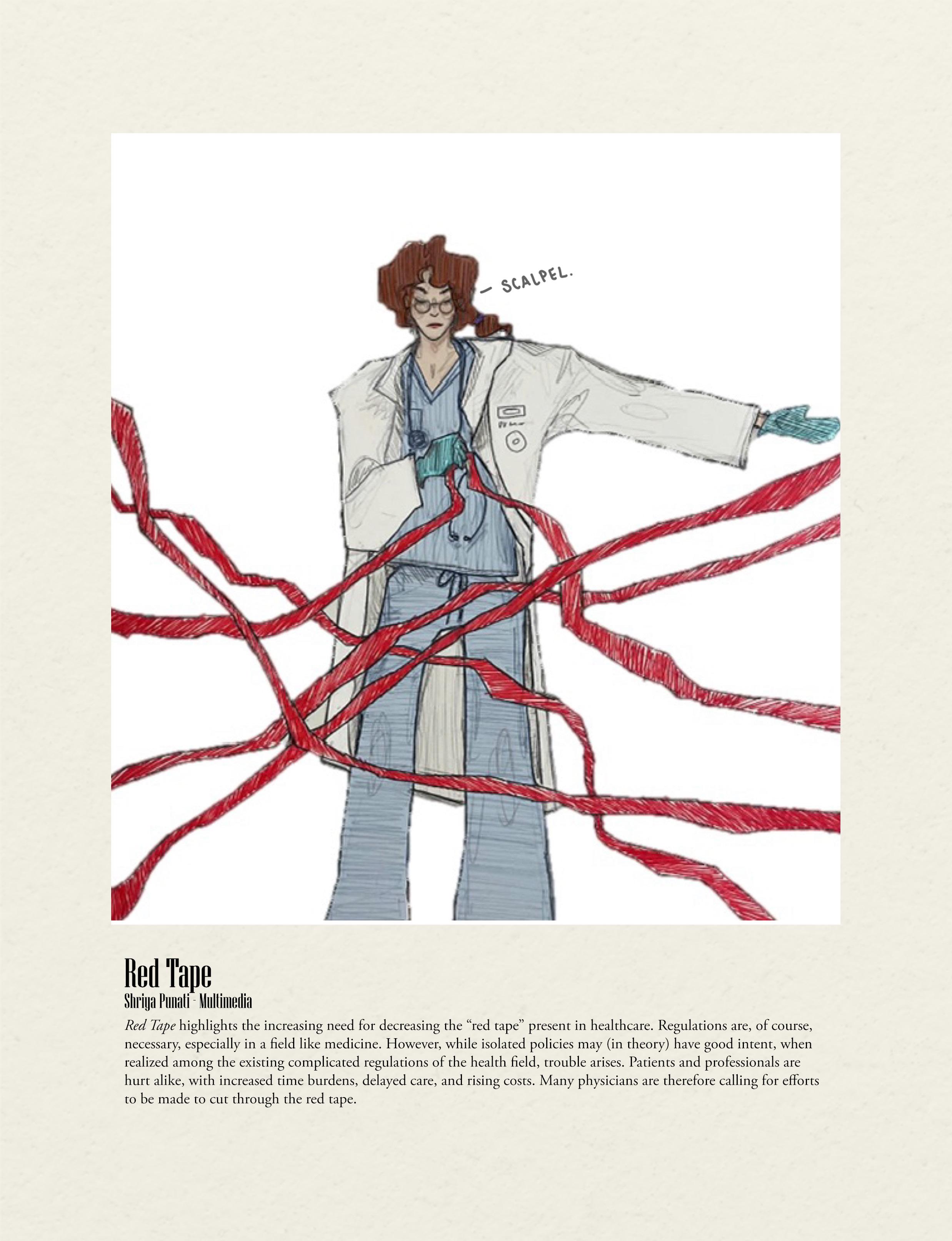
Shriya Punati (she/her) is a second-year biomedical sciences major, on a pre-medical track. She enjoys art and drawing in her free time. Through her medical journey, one of her goals is to work towards raising awareness about the disparities and inequities present in the current healthcare system.
Olivia Pinilla (she/her) is a second-year student majoring in Biology with a minor in Public Health and Entrepreneurship. Her interests encompass biological sciences, medicine, leadership training, and public health with a focus on health disparities in the Hispanic population. Olivia is a National Hispanic Scholar and is the Secretary of Bulls for Moffitt and Volunteer Co-Chair of the Judy Genshaft Honors College Student Council. Olivia plans to attend medical school and continue her studies in the public health sector.
Jasmin Pruthi (she/her) is a second year majoring in Biomedical Sciences and Psychology with a minor in Aging Sciences. Due to her aspirations to become a physician, she has been exposed to various aspects of healthcare and intends to make the field more compassionate, culturally sensitive, and patient-centered. She has developed an interest in gerontology and aims to foster a deeper understanding of human experience in later stages of life. In this poem, she hopes to provide a platform of the multifaceted dimensions of aging, including the emotional and existential aspects.

Gabriela Wachi SharpFish (she/her) is a sophomore at USF studying dance with a concentration in modern. An artist as well as an indigenous individual, she finds dance both as a healing modality and a universal language. This personal belief and experience have allowed her to pursue dance through a social justice lens. As a choreographer, she never realized how empowering and emotional this process would be for herself and others who do not identify as indigenous. She wishes her dance pieces inspire readers to make a change and support the survivors in their communities.
Rohit Veligeti (he/him) is a sophomore at the University of South Florida majoring in biomedical sciences with the eventual goal of going to medical school. One of his biggest interests is exploring the intersection between the world of tech and medicine. Rohit believes that critical on the frontier between emerging technologies and medicine is the field of bioinformatics which aims to improve patient outcomes through creating more informed diagnostics and therapeutic interventions.
Kiara (she/her) is a junior, pursuing a major in econometrics and quantitative economics. She is a third-culture kid born in India and raised in Dubai. Her passions include reading, writing, and painting, which serve as her outlets and anchor in this slightly crazy world.
Sun (she/her) is a sophomore majoring in Biomedical Sciences with aspirations of pursuing a career in the medical field. Her academic journey reflects a profound passion for understanding the intricacies of the human body and exploring avenues for improving healthcare outcomes.
