Tube feeding accessories to support all ages













• Continence • Skin Care
• Wound Care
• Nutrition
• Respiratory
• PPE • Janitorial
• Hospitality

















The Blend Issue Four was created in partnership with...



































• Continence • Skin Care
• Wound Care
• Nutrition
• Respiratory
• PPE • Janitorial
• Hospitality

















The Blend Issue Four was created in partnership with...


















All information, advice and content contained within this publication is provided for general information purposes only, and does not constitute medical, dietitian, psychological or other professional advice. All care is taken in the preparation of the information included in this publication. The publisher does not make any representations or give any warranties about its accuracy, reliability, completeness or suitability for any particular purpose.
To the extent permissible by law, the publisher will not be liable for any expenses, losses, damages (including indirect or consequential damages) or costs that might be incurred as a result of the information being inaccurate or incomplete in any way and for any reason or your reliance on the information, advice or content contained within this publication.
The Blend is curated, written and edited by Melanie Dimmitt and designed by Edith Olsen. The cover photo is by Samantha Allyson Photography.
The Blend creators acknowledge the Aboriginal and Torres Strait Islander peoples of Australia. We acknowledge the Gundungurra, Tharawal and Garigal peoples, the traditional custodians of the lands on which The Blend was made. We pay our respects to ancestors and Elders past, present and emerging.
blend.

68 CURATED CARE
A tale of two self-advocates who won’t settle for stock-standard support.
74
LIMITLESS
Garrett Taira defied all the odds and came back dancing.
80
MAKING CHANGE
Shaping legislation and advising big brands are all in a day’s work for Celia Chartres-Aris.
86 FLYING HIGH
Introducing tube-feeding’s biggest cheerleader, Sutton Short.


94
THE G-WORD
Got a granulation tissue issue? Clinical educator Robyn Wortel has you covered.
96
ARFID EXPLAINER
Dr Tessa Taylor spells out and explores this common condition.
98
DREAM TEAM
We meet a fantasy league of paediatric feeding specialists.
102
LET’S TALK LINGO
A lesson in tube-feeding language with two stomal nurses.

48
It could be blended whole food, a nourishing supplement or a bit of both. 62 PUSH IT
There’s more than one way to wield a syringe.
104 THE BUSINESS OF BLENDS
Behind the scenes of three game-changing startups.
126 TUBIE PICNIC

A deliciously fun affair. Recipes
114 Breakfast smoothie 116 Chicken broth
118 Enchiladas
120 Roast cauliflower and chickpeas
122 Chicken laksa 124 Pork stir fry


A bundle of go-to products.






Aconfession, I wasn’t sure there’d be another issue of The Blend. Not for a lack of love, but because squeezing its production in around day jobs, child-rearing and hand-washing a thousand-odd syringes each day is, in short, a lot. And yet, here we are.
Elizabeth Gilbert, the bestselling author of Eat, Pray, Love, talks about engaging with a creative side-hustle as you would an extramarital affair. No, you don’t have time for it. It’s not convenient and can be an absolute head-f**k to maintain. But you keep that flame alive because, as Elizabeth says, you’re hot for it. You’re obsessed. You can’t get enough.
And this time around, The Blend is especially irresistible.
Issue Four launches in tandem with our new digital destination –theblendmag.com – where you’ll find all of the stories, interviews and recipes from our pages and, I hope, many more. You might also notice that our magazine has had a glowup, with a more editorial feel.
None of this would have been possible were it not for our creative director, Edith Olsen. Ludicrously talented, cool-under-pressure Edie has made The Blend with me from day dot and, once again, has crafted a thing of beauty. Thank you, Edie.
While we’re bringing co-stars centre stage, this issue features a celebration of siblings (pg 38) including teenage sisters, Opal and Iris Shipley. To borrow some words from Iris, who has supported Opal through her tube-feeding journey: “I think a lot of siblings feel like sidekicks sometimes. And I think the truth is that we’re all superheroes.”
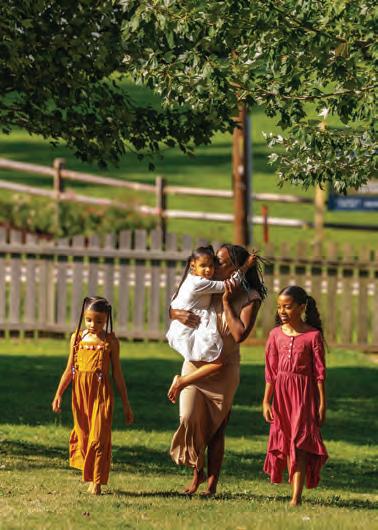
Our cover stars, the social-media darlings that are the Willardson family, generously opened their doors
and hearts for this issue (pg 52). We also spoke with award-winning adviser, lobbyist and policy designer Celia Chartres-Aris, who relies on total parenteral nutrition (pg 80), and a nasogastric-tube-touting youngster changing the face of cheerleading (pg 86).
Our community is a formidable, global force led by innovators like the ones you’ll find on page 104, in our feature on ‘The Business of Blends’. Here, three parents of tubefed kids, all leading blended enteralfood startups, echo a determination to empower tube-feeding people, families and professionals from their widespread corners of the world.
Here’s to another year of sharing our incredible stories. And thank you to our partners, supporters, contributors and you, dear readers, for making it possible to continue this passionate affair.
theblendmag.com
@the_blend_mag


Photographer, ‘Body Talk’, pg 22, ‘The Sibling Bond’, pg 38, ‘Push It’, pg 62, and ‘Curated Care’, pg 66
For those who are tube-fed or have loved ones in the tubie community, it’s a deeply personal journey that benefits from greater awareness and support. I strive to capture the unique resilience of the tube-fed community alongside the joy and fun of everyday life.
Some of the creatives behind The Blend Issue Four share why they love creating content around tube-feeding.

Tameka Simmons
Writer, ‘Soul Sisters’, page 32
Creating and sharing content about tube-feeding is essential to me as a mum and advocate because it sheds light on the realities, challenges and triumphs of this journey. I hope to normalise tube-feeding, break down stigma and empower other families navigating similar paths.

Writer, ‘Body Talk’, page 22
Media representation of tube-fed folk was pretty much non-existent when I got my tube. This is why I am so committed to telling my story whenever I get the chance. I know it is only one of many tubie stories, but if we all raise our unique voices to educate the community about tube feeding – including both the struggles and possibilities of tube-fuelled lives – I am hoping the world will become more inclusive for those of us already living with tubes. It might also take the fear away for those facing the prospect of tube placement in the future.
Our cover stars, the Willardson family, are photographed by Samantha Allyson Photography in their beautiful home in Boise, Idaho.
Tube changes at home
Support to attend school or childcare safely
Regional or remote telehealth support
Assessment and advocacy for funding and consumables
Tube size review for measurements
Support with skin issues
admin@cnqld.com.au
www.cnqld.com.au


In a culture obsessed with appearances, a rising number of us are feeling uncomfortable in our own skin. But what if that skin happens to be flaunting a feeding tube?
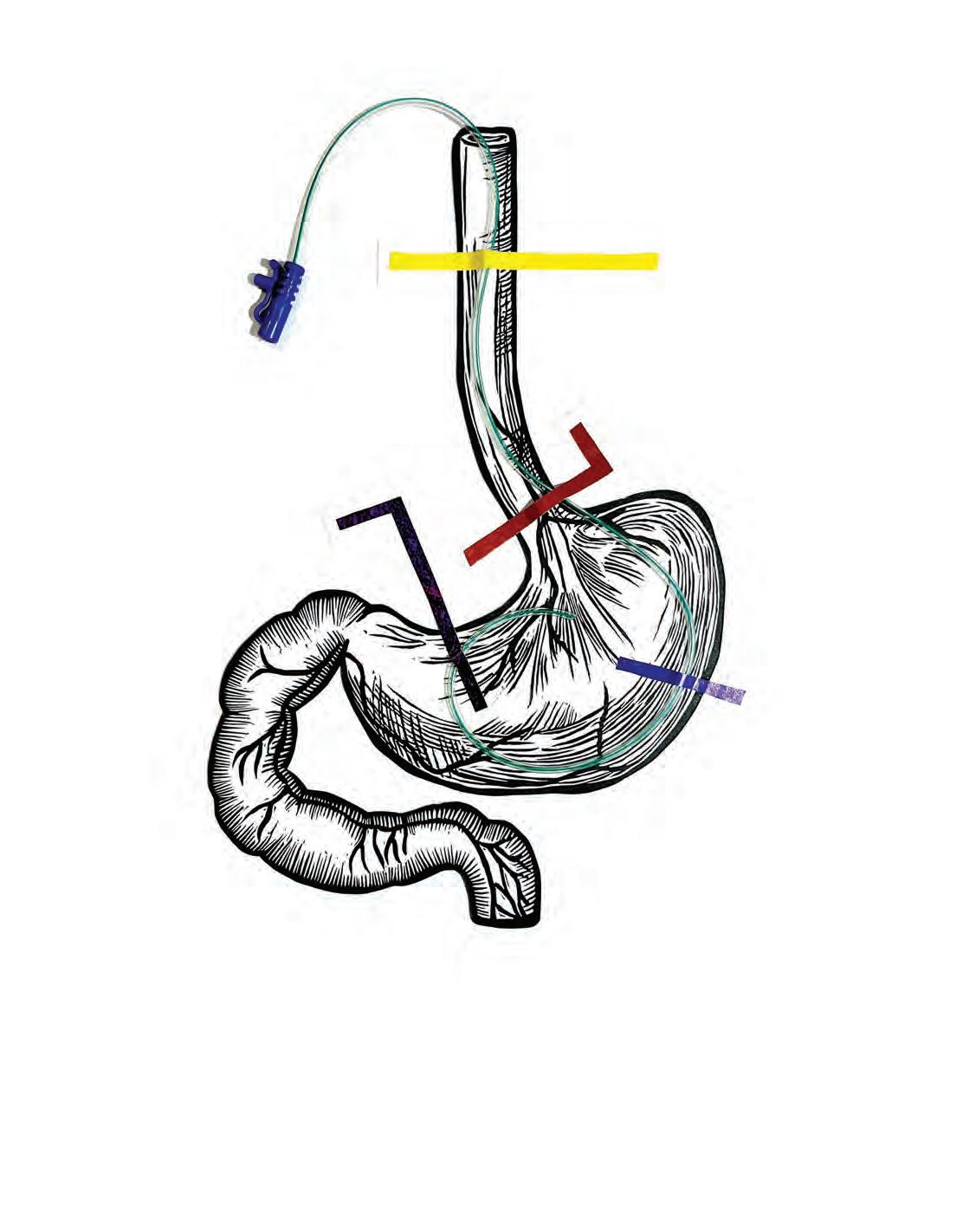
ARTWORK // KATHRYN LEAN
Our more seasoned readers might remember when, in 1989, Andre Agassi immortalised the line “image is everything” in an ad campaign for Canon cameras. He was wearing a lion-manestyle mullet wig at the time but, nevertheless, the then-rising tennis
star uttered a universal truth. Image is powerful. It has an enormous impact on how we perceive and engage with people, brands and, in the context of our own bodies, how we feel about ourselves.
In the decades since Agassi’s line, cameras have made their way into smartphones, social media has run wild and rates of body image dissatisfaction have increased worldwide*.
* Body Image Distress and Its Associations From an International Sample of Men and Women Across the Adult Life Span: Web-Based Survey Study. JMIR Formative Research, November 2021. Accessed via: ncbi.nlm.nih.gov/pmc/articles/PMC8603168
** Nutritional status, perceived body image and eating behaviours in adults with cystic fibrosis. The American Journal of Clinical Nutrition, February 2007. Accessed via: pubmed.ncbi.nlm.nih.gov/17007968
Within this culture, in the enteral feeding community, research** tells us that people with feeding tubes can be “less satisfied with their body image, reported lower self-esteem and poorer quality of life”. But feelings, as we know, are fluid. Here, three people explore some of the thoughts and emotions they’ve experienced around their tubefed bodies – and how these have changed over time. >>

I remember quite distinctly after having my first NG placed, thinking to myself that I would rather die of whatever was wrong with me than have a permanent feeding tube. I must have been about 14 – which I don’t think is the easiest time in life for anyone figuring out identity and body image – and I was already the “sick kid” at school. But I assured myself
that, so long as this tube was only temporary, it was fine.
After that I had a few years without tubes and couldn’t imagine going back there, but then my health took a big dive. I found myself with an NG again, at 20, and remember feeling so lost. Pretty soon after this, I got my PEG-J. A permanent tube made things very real.
While representation for people living with medical devices like feeding tubes has come such a long way, I feel like there’s not enough in the young adult space. I hadn’t seen anyone with a feeding tube and good quality of life. I couldn’t imagine having any kind of life with this piece of plastic, let alone one that was full or worthwhile.
I hated being looked at with pity after trying so hard to put together an outfit I felt good in. I’ve never been too bothered by staring because I kinda get that, but the pity is crushing when you’re just out trying to dance with friends or enjoy the beach.
I’d love to say there was a particular mindset that changed everything overnight but honestly, for me, it was time. I hated my PEG-J and went to great lengths to hide and ignore it as much as I could. I hit a point, though, where I was so completely exhausted and really over hating myself so much. Then one night, in the bathrooms at a gig, my best friend, Angie, said to me: “You’re gonna make feeding tubes look so hot. If anyone can, it’s you.”
That shifted something for me. I’d had plenty of people tell me they
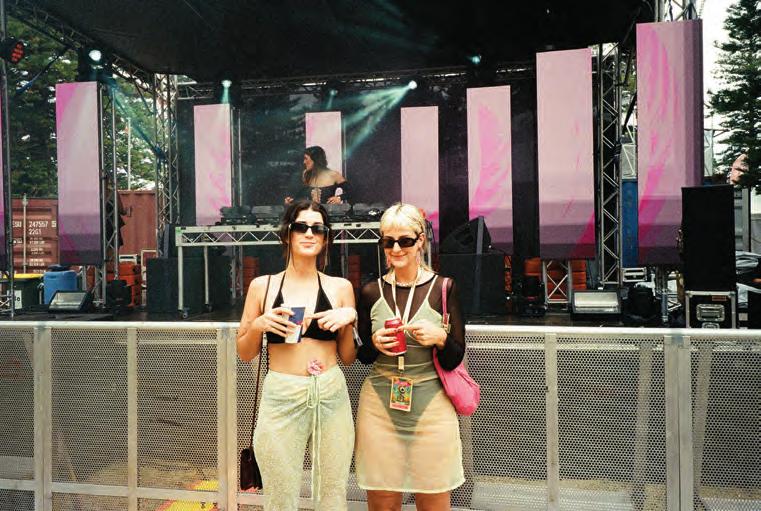
thought I was brave or that I inspired them but that didn’t translate at all to how I felt about myself – or wanted to feel about myself. Not once had I heard anyone talk about tube-feeding as fun, hot, or anything positive at all, so it hadn’t even occurred to me to embrace and own it.
Angie, thanks for the bathroom pep talk. It kinda changed my life. Pilates and running also played a big part in me feeling good, strong and confident in my body again. In hindsight, I don’t think I’d feel nearly as positively about my body, or as confident as I do now, if it weren’t for tube-feeding.
It took years to finally get a diagnosis of gastroparesis, likely resulting from my Ehlers-Danlos syndrome. Jejunal feeds – and total parenteral nutrition (TPN) – absolutely saved my life and I feel immensely grateful for the opportunities I have because of tube feeding.
I was actually fortunate enough to have my PEG-J removed recently,
One night, in the bathrooms at a gig, my best friend, Angie, said to me:
“You’re gonna make feeding tubes look so hot. If anyone can, it’s you.”
That shifted something for me.
after significant improvement from a gastric electrical stimulator, which has been a really interesting adjustment. To my surprise, I miss it a little. It took a long time, but I’d come to be incredibly proud of it and loved the quality of life I had because of it.
If I could give one piece of advice to people who are new to this experience, it would be that, honestly, I wish someone had told me I was allowed to hate it. That I didn’t have to feel inspiring or brave.
It’s okay if, right now, it’s just hard. It will get easier, but you don’t have to be a constant beacon of positivity. I’d also say though that your life can still be exciting and full – not just despite, but likely because of, tube-feeding. >>


I was initially very apprehensive about the idea of having a feeding tube. I worried about a lot of things. Many of them seem silly or superficial – especially those relating to body image – but I want others to know it is normal and okay to worry about both ‘big’ and ‘little’ things when facing life-altering decisions, even if these worries are not entirely grounded in fact or reality. Which is the nature of worries, right?
I worried about pain and discomfort. I worried about how difficult it might be for me to adjust to the logistics and mechanics and routines of tube feeding. I worried about the social implications and how it might impact upon my children and family, and even my pets. My dog’s enthusiastic greetings would have to be tempered so that she didn’t jump on the tube and my
45, mother and multisport athlete, public speaker and PhD candidate, FRASER
cat was kicked out of my room at night because he could no longer sleep on my tummy.
I worried about going to work with a visible NG across my face, thinking it might impact upon others’ perceptions of my capabilities, functioning or professionalism. I worried that the dysfunctional relationship I already had with food and eating might be amplified once a tube was placed. Spoiler alert: It did!
I was already struggling with incorporating my life-long illness and altered anatomy into my sense of identity and self, and adding a tube on top of this felt overwhelming to me, at the time. This is what I think clinicians and those around us often don’t fully appreciate. By the time we are at a point of acquiring a feeding tube, all of us have been through major health struggles that have led us to this point.
I started on TPN during a six-month hospital stay, after a sudden medical emergency ended in four emergency surgeries, a chopper flight from my regional home town to a larger hospital in the city, and losing most of
my small bowel and stomach. I left hospital tube-free, determined I would not ‘admit defeat’. I tried my best to eat what I could but, without a feeding tube and with a diagnosis of short bowel syndrome – intestinal failure, I would have faced a life of pain and chronic malnutrition. Having an NG placed felt temporary and, even though it was more visible to everyone else, I think I coped better with it from a bodyimage perspective because it could be pulled out without leaving a trace. Once my MIC-KEY button was placed, the reality of a probable lifetime of tube-feeding became more salient for me.
As a triathlete, initially, I would wear my t-shirt down over my tube when running, but I found it was far more comfortable to run with my shirt tucked up under my sports bra or to simply wear a crop top. For a while, I was very self-conscious about the fact that people would see the massive scar up the middle of my tummy, my stolen belly button and the MIC-KEY button sticking out of my guts.
It’s not an objectively pretty sight and I worried about subjecting others to it. But slowly, I have come to realise that most people don’t actually care what you look like. And without my tube, there is no way I could have successfully crossed the finish lines of four half-marathons, Tour de Brisbane, four triathlons and a marathon last year.
When I crossed the finish line of the Gold Coast Marathon, wearing my specially designed tube-feeding running vest with my pump attached to my button, the physicians at the medical tent immediately cannulated me to test my blood for the nutritional and electrolyte abnormalities that
used to land me in hospital regularly. When they ran the tests, my bloods were perfect. I think I was prouder of this result than I was of running a marathon!
My tube has helped me gain an appreciation for what my body is capable of with the right nutrition. As someone who has struggled with an eating disorder post-tube placement, my tube-fuelled athletic achievements have also been integral in helping me to find and embrace strength and health, rather than an obsession with control and becoming the smallest version of myself.
Early on, one of the things that helped me feel more confident in
My tube has helped me gain an appreciation for what my body is capable of with the right nutrition.

myself was to try and personalise the experience of tube-feeding with the help of companies like Tubie Fun and a few Etsy sellers who make cute accessories for tubies. When I first got my tube, one of the things I focused on was choosing a matching tubie pad, clip and port cover set to go with my work outfits each day.
I love long, flowing dresses but, unless they have buttons down the front, they can make it tricky to manage tube-feeding. One of the best things I did for myself was to take my dresses to a clothing

mending service to have large buttonholes sewn into the sides to fit my extension and tubing through, or to unpick parts of the seams to accommodate the tube.
These seemingly small things made such a difference to my mindset. I think it was a way of asserting my own style and personality over what felt like a very clinical and medical thing.
Since getting my tube, I’ve heard stories of tube-fed people out there living awesome lives – as parents, grandparents, artists, bodybuilders, athletes, musicians, academics and so many other things. Every one of these lives helps, by example, to challenge the “tragedy” narrative so often associated with tube-feeding and to highlight what properly nourished bodies can do and achieve, rather than what they look like. >>

I have a feeding tube because I had a stroke, when I was three years old, that severely impacted my eating. I’ve had my permanent low-profile MIC-KEY button since I was nine and while it hasn’t really impacted my confidence or the way I feel about my body, I’m conscious of when I want to show – and not show – my feeding tube to the world.
Recently I’ve decided that if I’m at the beach, I’m going to be wearing a rashie. I don't really want to show my stoma off to everybody. Only my family and friends get the privilege of seeing my naked torso. Because some people haven’t seen a button before it can invite stares and
questions. I just want to hang with my friends.
That said, I’ve been in a photo shoot with my shirt off. It was with other tube-fed kids and adults including Pedro Relvas, who’s a fitness coach and bodybuilder. In the company of other tubies, it felt right to bare all – although I might invest in a spray tan and some tattoos before going shirtless next to Pedro again!
When I first got my G-tube, I was told this would mean being hooked up to a pump 24 hours a day and not eating anything orally, but this hasn’t been the case. Having a feeding tube hasn’t stopped me from doing anything. In fact, it's the opposite.
Your life isn’t over, this button helps you have a life and it gives you some freedom back.
And to those who are new to this experience, I’d say: Your life isn’t over, this button helps you have a life and it gives you some freedom back.
It is scary at first, but then you get over it. And if your friends are anything like mine, they’ll be surprisingly cool about it. To them, I’m just Lewis – and this is the way I eat. And recently, they’ve really had my back.
My mum was asked to sign a form saying I’d be tube-fed with support at school, separately from my peers, but could bring along one friend “for mental moral support”. My mum and I weren’t having a bar of this. Because I only have use of one hand – a side-effect of my stroke – I mastered tube-feeding myself, independently, with my strong hand.
I now feed myself with my friends during breaks at school in the green space, with no PPE and no sterilisation. And you know what? I haven’t died yet!
This article was made in partnership with Avanos. For easily digestible information about tube-feeding at any age and any stage, visit TubeFed by Avanos at tubefed.com.au.


“One thing this journey has taught me is the importance of being adaptable.” Tameka Simmons

Born without eyes and with several other challenges, Evely Diaz was always going to have an extraordinary story. Her mother, South Carolina singer and not-for-profit founder Tameka Simmons – alongside Evely’s sisters, Luna and Skye – shares how tube-feeding plays a supporting role for their family.
WORDS // TAMEKA SIMMONS PHOTOGRAPHY // JASON MCKINNEY

Evely got her feeding tube at three months old. It was during what ended up being a 30-day hospital stay battling heart failure and, initially, the G-tube was recommended to give her an opportunity to rest and heal from multiple life-saving heart procedures.
Her heart wasn’t well at all –and something as natural as breastfeeding was such hard work for her during that time. The tube allowed her to get the necessary nutrition and hydration without exerting herself, which was crucial for her recovery and overall health.
I was just grateful and excited for any intervention that would allow Evely to come home.
At first, I saw the G-tube as a temporary measure to give her heart the opportunity to rest, expecting she would eventually resume nursing and start solid foods months later. Evely progressed well with oral feeding, leading to the removal of her G-tube button. However, shortly afterward, she began experiencing seizures and regressed in her skills.
Evely was diagnosed with a rare form of epilepsy and other conditions that made oral feeding not only challenging, but unsafe.
When the G-tube was placed again, it hit me hard. There was a lot of grief and overwhelming feelings because breastfeeding gave me confidence she was getting what she needed. As she grew, finding the right nutrition for Evely was also incredibly challenging.
The standard commercial formulas recommended by hospitals didn’t align with our family’s lifestyle or values. It felt unsettling to feed her
real ingredients that I felt good about feeding her, knowing it would contribute to her healing and growth.
Tube-feeding was incredibly overwhelming at first. And messy, too! I remember feeling so anxious and sometimes I would even hear phantom beeps from the feeding pump. That feeling still comes back occasionally, but once I found reliable meal options
Sharing meals is an important part of our family life. And we make sure Evely is always a part of it, whether through her specialised feeding routine or by including her in the mealtime atmosphere.
something I wouldn’t choose for my other children. So I started blending meals for her myself, which was both expensive and time-consuming.
Then, during a late-night Google session, I discovered Real Food Blends. This was a game-changer – a whole-food option made with
that I felt good about feeding Evely, things started to get a lot easier. Over time, managing her feeding schedule and ensuring she gets the hydration she needs has become second nature to me. I’ve gotten so used to it that I rarely need alarms to remind me anymore. >>


I’ve connected with a supportive community. Families navigating similar journeys who we’ve met through our family’s not-for-profit, Through Evely’s Eyes, which supports children with rare medical conditions.
The best piece of tube-feeding advice I’ve received from fellow parents is to trust my instincts and advocate fiercely for what works best for Evely. Every child is unique and finding the right nutrition is a journey that requires patience and persistence.
Sharing meals is an important part of our family life. And we make sure Evely is always a part of it, whether through her specialised feeding routine or by including her in the mealtime atmosphere.

Evely’s sisters have been incredibly involved and supportive in her tubefeeding journey. Luna and Skye have grown up knowing this as a normal part of our family’s routine. Luna, being so young when Evely became a G-tube user, doesn’t remember a time before it, while Skye was born into this experience. They both show genuine interest and love helping Evely with her tube feeds. It warms my heart to see their natural empathy and care for their sister.
One thing this journey has taught me is the importance of being adaptable. My primary hope is for Evely to reach her full potential, whatever that may look like. I’m prepared to support her in whatever way she needs, whether that involves continuing with tube-feeding, transitioning to oral feeds if possible, or exploring other options. My goal is to ensure she has the best nutrition and support to thrive in every aspect of her life.
Why does your sister Evely have a feeding tube?
Luna: She has diagnoses that make it hard for her to swallow food and drink like we do. Her feeding tube helps her get what she needs.
What’s your favourite thing about Evely’s feeding tube?
Skye: My favourite thing is helping to prime her food. It’s fun to watch it go through the tube. It looks like the food is on a rollercoaster!
Can you tell us about a time where things got messy with Evely’s tube-feed?
Luna: One time, Evely accidentally pulled her feeding tube out while she was eating, and food went everywhere! It was kind of funny, but also really messy.
What advice do you have for other siblings of someone who tube-feeds?
Luna: I would tell them it’s okay to ask questions if you don’t understand something about the tube. And always be gentle around the tube so it doesn’t get pulled or hurt them.
Skye: I would say it’s nice to help out when you can, like priming the tube, but also to just play and have fun together.

‘Our kids come as they are. Now it’s up to us to get with the program.’
Melanie Dimmitt, Special: Antidotes to the obsessions that come with a child’s disability.
Feeding tubes can make brothers and sisters all the more tight, so we’re told. It’s time these special relationships – in all their rivalry, fun and fierce love – got our full attention.


Iris and Opal Shipley are the finishing-each-other’ssentences kind of sisters. At 18 and 16 years old, respectively, the duo’s banter doesn’t miss a beat – even when speaking from their separate cities in Ohio. Iris lives in Cincinnati, where she’s studying acting, while Opal is in their hometown of Columbus, applying to colleges with her heart set on medical school.
Recent years have inspired Opal’s career aspirations. In early 2020, sudden and serious illness saw her spending months in hospital, requiring years of nasal tubes and, eventually, a surgically placed gastrojejunostomy (GJ) and gastrostomy (G) tube.
The whole Shipley family –including Iris and their younger sister, now-14-year-old June – was shaken by Opal’s rapidly declining health. But even in the darkest of times, they made moments of light. Sometimes, in ways that only a sibling could.
Opal and Iris, while you two were growing up, what did family meals look like?
Opal: Our mum is a huge foodie. She has [inflammatory bowel disease] ulcerative colitis, so she has a lot of gastrointestinal (GI) issues and has always been really aware of what she feeds us. Every meal was like a plethora of nutrition. She loved – and still loves – to cook, so we would have these elaborate dinners. We have a table on both our front porch and on our back deck and we would sit around as a family, eating and talking. It was a huge point of connection.
Iris: Yeah, eating together was definitely the social hour of the day. We all do very different things. Our youngest sister is an athlete. Opal and I were always doing theatre things and our parents both work full-time jobs, so being able to have that moment we all shared was super important. And it got really difficult after everything changed.
When did things start changing?
Opal: My very first issues popped up when Covid started, in March 2020. I have something called rumination syndrome, which is a type of regurgitation that I have no control over. When I eat, my stomach fills up with air and then basically closes itself, and all that air pushes the food out completely undigested. I have other GI issues, but that was the first thing.
Iris: I think one major thing that shifted was, before all of this happened, we would do this thing at dinner called ‘best and worst’. Each of us would say the best part of our day and the worst part of our day. And once Opal became sick, we would all have different bests, but the worsts were always the same. We were worried about Opal.
The continuous theme throughout all of this is that love conquers all.
I remember one day we had just eaten a family meal – it was grilled burgers – and I stood up and threw up into the bushes next to our porch. I knew something was wrong, because I didn’t feel sick. It just kept happening and happening and, by late June, I couldn’t eat anything.
We went to the hospital in early July and the doctors said, “you seem completely fine”. My mum said, “she hasn’t kept food down for about two months”. So they admitted me and, after about a week, ran a test that diagnosed me with rumination syndrome. I then had a nasojejunal (NJ) tube placed, which I had for about 14 months. I despised it. NJs have to be done under fluoroscopy and I had so many of them. It was horrific.
Opal: It was super abrupt when I lost my ability to eat –one day I could eat everything and the next day I could eat nothing – so the biggest struggle for me was genuine grief around not just the food, but the meals. Instead of sitting at the table, I would be laying on the couch, throwing up. And Iris is emetophobic [has a fear of vomit].
Iris: Yeah, I’m not a fan of vomit. So this was a gruelling experience for me. Opal: It was a gruelling experience for both of us.
Iris: But the continuous theme throughout all of this is that love conquers all. Do I hate vomit? Yes, but I love you.
Opal: You’ll hold my hair back now and sit with me.
Iris: Oh my gosh. If you told me a few years ago I’d have cleaned up this much vomit, I would have laughed in your face.
While this was all happening, were you being honest with each other about how you felt?
Opal: Honestly, no. When I first got sick it was peak Covid, so I couldn’t see any of my friends, I was dying and I was a tween. Lots of things were pitted against me.
Iris: It sounds like the beginning of a bad joke.
Opal: Life was a bad joke at that point. I was so angry about my situation that I found it almost impossible to express what I was actually feeling. The only person I would talk to was Iris but even then, I wouldn’t tell her much.
Iris: There was a lot of vulnerability, a lot of tears. I mean, as a young woman in society, I already have preconceived notions about food and body image. And when this became such a significant piece of our life, so quickly, it definitely made an impact on me too. >>

Opal and I spent a lot of time talking about our mental health and what was okay for us to talk about versus not talk about. There were topics of discussion that were sisterly love – I support you and I’m here for you – and then there’d be topics where it was like, I don’t know if it’s safe for us to talk about this, because we’re both really susceptible to this kind of issue.
What topics were off the table?
Opal: Weight was a big one. When I got super sick I lost a ton of weight all at once and I didn’t ever think about it in the right headspace. So talking about the sizes of my clothes or how much weight I had lost wasn’t good for either of us.
Iris: If anything that either of us said could be pulled out of context and used in a comparative sense, we avoided it altogether. Instead, it would be more like, let’s shoot the shit and just connect with each other to forget about all this horrible stuff that’s happening.
Opal: She’s my best friend and, genuinely, there was always support. It was just that there were certain words or details we had to avoid just to try and...
Iris: Protect each other, really. The basis of it all was that we love each other and just needed to protect each other from this evil that is modern societal expectations.

What was it like – for your whole family – when Opal first came home with a feeding tube?
Opal: It was a major adjustment, I think, for all of us. When I first came home with my nasal tube, the size for my age was a yellow-coloured tube. Our younger sister went and found a yellow piece of yarn, took a piece of my tape, put the yarn in a backpack and taped the end to her nose so we could match.
Iris: I did not do that.
Opal: June was only eight and I was like, this is kind of sweet. Then they both called me “spaghetti nose” for a while.
Iris: Being siblings is maybe one of the more unique relationships in this world. If I saw anyone else with
a nasal tube, I couldn’t call them spaghetti nose. But I knew that it would cheer you up – and it did.
Opal: It really did. With my nasal tube, it was like, haha, this will be gone soon! Then two years went by. Then I got my GJ tube and it was like, this thing isn’t going anywhere.
Iris: Opal and I were in high school for a year together and there was one day, while I was sitting in my classroom taking a test, that I got a call from Opal saying she was downstairs in our theatre room. She said, “Iris, my tube came out. You have to come downstairs right now!” And I was like, what?
I sprinted across this giant high school and she’s there and she’s crying and she’s having a panic
I think a lot of siblings feel like sidekicks sometimes. And I think the truth is that we’re all superheroes.
attack and freaking out. I saw the tube – it had gotten caught on a student’s chair and ripped out of her stomach – and I was just aghast. Number one, it was disgusting. Number two, I was so worried. And number three, Opal, you were just absolutely in a shambles. You couldn’t even make words come out of your mouth.
That was the moment when I was like, wow, this is really serious. But in that moment, all I felt was love for her. There was nothing else on my mind. It was like, okay, let’s call 911. Let’s call Mum and Dad. Let’s get the nurse. Let’s calm Opal down. And we did it –we fixed it. We put that tube back in so the stoma didn’t close up and got her in an ambulance and took her to the hospital. And all was well. Opal: All was well.
For both of you, this has all been happening at a stage of life that’s typically about fun and freedom. How does that work with a feeding tube? Opal: The first thing for me was acceptance. It was realising that this is my life and that’s okay. I might not feel great every day. I might not look my best every day. I might be throwing up for six hours some days. But you only get one life and, feeding tube or not, you can make it awesome.
I’m at the stage where you’re meant to be finding yourself, but I think that was already forced to happen when I was younger. And it’s allowed me to gain confidence, which really is the biggest thing when learning to live your life with a feeding tube and a chronic illness – learning what you need.
I know that if I’m going to go out with friends, I’m going to need to push a bunch of water down my tube. I’m going to need extra electrolytes on board and I’m going to need to bring medication with me in case I start to feel nauseous. I always carry emergency meds and syringes and extensions. Anything can become your new normal, it just takes time. And then you have people in your life like Iris and like my boyfriend, Griffin, who will also start doing these things for you. Griffin carries Zofran [anti-nausea medication] in his wallet at all times.
Iris: For me it was about trust –letting go a little bit. When Opal was younger, it was harder. But she’s reached the age where if she doesn’t want to do something, I can’t make her do it and vice versa. So I could be worrying about, does she have this? What if she does this? What if this happens? But in reality, all I can do is trust that she’s got it.
Opal: As we’ve grown up, I’ve learned to take responsibility and confidence with the decisions that I make about my health. I still rely super-heavily on my family in every single way when it comes to my illness, but it’s gotten to a point where everybody – including me – is able to let go a little bit and take a step back. This is life with illness and not illness with a side of life. We actually get to exist. >>
What do your family meals look like today?
Opal: Now I eat pretty normally, so every night we have dinner together.
Iris: Minus me!
Opal: But Griffin and I went up to visit her a few weeks ago with a friend –and we had a steak.
Iris: We did, we had steak!
Opal: That said, while I have regained the ability to eat, I have not regained the ability of portion control. So I either don’t get enough food or I get a monstrous amount and then it’s on my plate, so I’m like, I have to eat this all – and I make myself sick. It’s still a learning curve. We’re almost a year into this but I am slowly getting better at it.
I think the hardest part about family meals is that it’s still a point of tension and trauma for me, my parents and my sisters. A lot of my GI conditions can be made worse by eating too fast and my parents will see me eating and they’ll be like, “Opal, slow down!” And I’m sitting there like, “I feel fine. Nothing’s wrong!”
Iris: And we’re all sitting there like, “no, you’re not!” – Shipleys are stubborn.
Opal: I lost so many of those family meals and I enjoy them so much now, I wouldn’t give them up for anything. Even if there is an occasional argument.

Looking back, what are the biggest things you’ve learned about tube-feeding?
Opal: It’s difficult, it’s really hard, it’s painful and it’s scary, but it’s magical. It ruined my life for a little bit but, overall, it gave me the chance to have a life again where I can experience the joys of being a teenager – and my sisters – and life can be good.
Iris: I don’t want to speak for anyone, but from my observations, I think a lot of siblings feel like sidekicks sometimes. And I think the truth is that we’re all superheroes. Opal and I are both superheroes. She’s been brave through some crazy stuff, but I’ve also been brave through some crazy stuff for her. The reality of it is that we are both awesome and we love each other. And that’s all that matters.

It ruined my life for a little bit but, overall, it gave me the chance to have a life again where I can experience the joys of being a teenager – and my sisters – and life can be good.

PAIGE (9) AND PORTIA (3)
What does dinner time look like in your family?
Paige: We blend up whatever we are having for Portia. Lasagna, fish, pizza… not quiche. She’s allergic to egg.
What does it look like when you eat together?
Paige: I sit at the bench. Mummy sits on the mat with Portia and tries not to let her food get stolen by the dog.
Why does Portia have a G-tube in her tummy?
Paige: She went to the hospital for surgery because she kept pulling the nose one out.
What would happen when she pulled her nose tube out?
Paige: Sometimes Mum would think I had done it because I was closest to her.
How are things different now that Portia has her G-tube?

Paige: She’s never pulled it out. But Mum has pulled it out by accident.
What’s your advice for other kids who have a brother or sister with a new feeding tube?
Paige: If they have a nose one, watch their hands. Also, make it stand out. Don’t be afraid to show it, cos it’s cool.



Callum, we’ll be chatting with your brothers but feel free to jump in.
Isaac: But not during our responses. That’s just rude.
Why does Callum have a G-tube?
Isaac: Because he can’t swallow water properly. And there are other reasons that I don’t know or remember.
Callum: I don’t even know the answer to this question.
Do you remember when Callum got his G-tube?
Harry: I don’t think I have a single memory where he doesn’t have his tube. In all the photos I’ve seen from Mum and Dad, he has his button.
Isaac: I’m pretty sure it got put in a week or two after his birth, so there wasn’t a lot of time that I would have been able to see him without it. It’s just normal to see him with it.
Callum: Those two were both playing on the playground outside of the hospital.
When you got your tube in? Is that where they were?
Callum: Probably.
Isaac: If anything, we’d remember, Callum.
What is the grossest thing that’s ever happened with Callum’s tube?
Harry: I know what I want to say.
Isaac: So do I, it might be the same thing. Three, two, one…
Isaac + Harry: Changing his tube.
Harry: Also once, when someone forgot to clamp it, stuff just started spilling out of his stomach. That was pretty gross.
Feeding tubes can be gross, but Callum seems pretty cool about his, yeah?
Isaac: Yeah. He might be meeting someone new and then he will just be like, “look what I have!” straight away. It’s something he shows off lots of times.
What’s your advice for other kids who have a brother or sister with a new feeding tube?
Harry: Don’t be afraid of it. Take good care of them. Be nice to them.
Isaac: Be careful around it. And make sure he or she is okay with it and help them if they're worried about it. Help them not think so much about it. Stuff like that.
Also – top thing – don’t get annoyed at them if they’re not eating quick enough or you want to leave the table but you can’t because they’re not done eating. Don’t get annoyed at them if you want them to come back and play with you, but they need to have their meds or something like that. Try to put yourself in their shoes and feel how it would be to be them.
This article was made in partnership with Avanos. For easily digestible information about tubefeeding at any age and any stage, visit TubeFed by Avanos at tubefed.com.au.
LIKE WHAT YOU SEE?
Find original artworks and prints from Kathryn Lean at etsy.com/shop/KathrynLean
@kathryn.lean.artist


Be it blended whole food, a nourishing supplement or a bit of both, fed is always best. Here, three tube-feeding families share why Abbott’s nutrition products work for them.
When Katelyn Armstrong was three months old, she stopped finishing her bottles. At four months old, she had a nasogastric tube placed and, as her mum Chelsea says, things declined from there.
“Her formal diagnosis is ‘failure to thrive’ and she struggles to hold nutrition, gain weight and grow typically for her age. At three years old she had her G-tube put in and it was the best thing that ever happened to her.”
Now five, Katelyn is looking forward to starting school and loves getting outdoors on her bike. A typical day
will see her eating several meals and having PediaSure* Fibre, an Abbott nutrition product, through her tube.
“She generally loves to watch a movie, play on her iPad, play cards or read a story whilst her pump is giving her the extra top-up,” says Chelsea.
“We are so lucky that this supplement can be provided through a nutritional program and covered by the NDIS (National Disability Insurance Scheme). We’ve also found the convenience of the small bottles means we can leave extra supplies at family and friends’ homes, too.”
In giving advice to other families, Chelsea says to always ask questions and take each day as it comes. “And remember, nourishing your child in whatever way it looks is absolutely okay.”
Five-year-old Jon Beit has spinal muscular atrophy, “so his muscles are weak”, says Megan, Jon’s mum. “He’s been tube-fed since he was six months old and it’s been a bit of a journey for us, because I breastfed him until that point.
Then I expressed milk and put it down the tube.
Then I was like, I can’t do this anymore!”


We’re able to add extra calories to his feeds and really play around with the nutrition. Having that little failsafe has been really good.
Jon had his PEG-J (percutaneous endoscopic gastrojejunostomy) tube placed at 18 months and, for a long time, thrived on a blended-food diet and overnight formula feeds.
“He had the best diet of anyone that went to his dietitian because it all went down the tube. Food, medicine, water, no argument,” says Megan. “He’s always just like, ‘eh, whatever!’”
After 18 months of no hospital admissions, in early 2024, Jon became very unwell.
“Whenever Jon gets sick, the first thing that happens is he stops digesting food, so the doctors go straight to continuous feeds through the jejunal part of his PEG-J. We’ve been on PediaSure* since March,” says Megan.
“The good thing about it is, because I get it in the tins of vanillaflavoured powder, we’re able to adjust the calories. Jon’s quite skinny and we have lots of issues with weight, so we’re able to add extra
calories to his feeds and really play around with the nutrition. Having that little failsafe has been really good.”
On the topic of coming to terms with her child needing to tube-feed, Megan says that over time, her perspective has shifted.
“There’s that mental hurdle, as a parent, because tube-feeding is not your expectation of how it should be. But once you realise that it’s your issue – and not the child’s problem – it makes it easier for you to be like, they’re not suffering, I’m suffering, so I can get over it.” >>
Grace O’Flaherty loves her food. While a rare genetic condition, Rett syndrome, impacts this eightyear-old’s physical abilities, she’s developed a healthy appetite.
“She’ll sit down in a therapy session and will not touch a toy. She will not touch a bubble machine, she will barely touch a button – but if you put food in front of her, she will grab it,” says Grace’s mum, Roxanne.
Getting enough food, however, is challenging. Grace experiences involuntary movements and periods of hyperventilation that keep her metabolism firing and make her fatigued. It’s hard for Grace to get enough calories from meals alone, so she has a G-tube.
“We do 500ml bolus feeds of PediaSure* overnight, while she’s snoozing,” says Roxanne.

It’s high in calories and ticks all the boxes for what Grace needs in her day, which is reassuring. It’s also convenient – we just pop it in her school bag like her drink bottle and lunch box.
For breakfast, if she’s up to it, Grace munches on toast, scrambled eggs or cereal. At school she has morning tea and lunch, topped up with 60ml bolus feeds of PediaSure*, before heading home to enjoy afternoon tea and dinner.
“So it’s a big mix,” says Roxanne. “We found our way to PediaSure* because it offers complete, balanced nutrition and ticks all the boxes for what Grace needs in her day, which
is reassuring. It’s also convenient –we just pop it in her school bag like her drink bottle and lunch box.”
Sometimes, Roxanne will also use PediaSure* in her cooking for a boost of calories. “I put it through carbonara and other creamy-based dishes,” she says. “While being fully tube-fed is not a bad thing at all, food is yummy – and I know it’s Grace’s motivator. I hope that she’ll be able to keep enjoying it.”
1. Begin boiling water to cook pasta, following packet instructions.
2. Finely dice the onion and roughly dice the bacon.
3. Slice button mushrooms, adjusting quantity to your preference.
4. In a large saucepan or skillet over medium heat, add butter, olive oil, and garlic; cook for a few minutes until fragrant.
5. Add onion and bacon, stirring until bacon is browned and onions are translucent.
• 3 scoops vanilla-flavoured PediaSure* powder
• 1 small/medium onion, finely diced
• 4 rashers middle bacon, roughly diced
• 6-12 button mushrooms, sliced
• 1 tsp minced garlic
• 1 tbsp butter
• 1 tbsp olive oil
• ½ cup thickened cream
• 1 tbsp Parmesan cheese
• 1 packet of your favourite pasta
* Food for Special Medical Purposes ANZ.2024.55661.PDS.1. Use under medical supervision

6. Add mushrooms, stir, and cover for 3 minutes to allow mushrooms to sweat, enhancing the sauce.
7. In a separate bowl, mix 3 scoops of PediaSure* with ½ cup thickened cream until well combined.
8. Pour the cream mixture into the pan with bacon, onions, garlic, and mushrooms. Sprinkle Parmesan on top and stir.
9. Cook over medium heat until the sauce thickens slightly and turns light brown, about 5 minutes, then reduce to low heat.
10. Drain the pasta and add it directly into the pan. Stir well to coat the pasta in the creamy sauce.
11. Serve with additional cheese on top for extra flavour.

This article was made in partnership with Abbott. To explore their full range of science-based nutrition products for people of all ages, visit abbottnutrition.com.au
How do we teach the world that tube-feeding is normal? By showing the world that tube-feeding is normal. And with two tube-feeding daughters and an online community of more than a million, Shannon Willardson is doing just this.
WORDS // MELANIE DIMMITT PHOTOGRAPHY // SAMANTHA ALLYSON PHOTOGRAPHY


Not long after two-yearold Charlotte Willardson started feeding with a gastrostomy (G) tube, her mother, Shannon, received an SOS text from their babysitter.
“She said that Charlie’s tube had come out. And I’m like, ‘okay, which tube?’ Because if it’s just the extension set, no big deal, right? But she sends me a picture and it’s the entire button.”
Shannon had been touring a local school – one that specialises in supporting children with complex needs. Charlie has a very rare genetic condition which means she needs help to eat and drink, which is why she has a G-tube. A G-tube that, just weeks after being placed, had caught on the side of her crib and popped right out.

“I was like, ‘oh my gosh, okay’,” says Shannon from her family home in Boise, Idaho, recalling the day that saw her rushing Charlie to hospital, having her tube professionally placed for a second time. “I told the lady who was doing the school tour, ‘I’m really sorry. I have an emergency and I have to go!’ It was crazy.”
Nowadays, in far less dramatic fashion, Shannon replaces eight-
year-old Charlie’s G-tube herself. She does the same for her sixyear-old daughter, Ava, who shares Charlie’s genetic condition. A former real estate agent and program manager at LinkedIn, since becoming a mother, Shannon’s skill set has substantially diversified.
“Speaking to my husband, I always threaten that I’m going to go to med school,” laughs Shannon. “Medical parents all deserve honorary nursing degrees and especially since having our girls, I’ve become so fascinated
and interested in all the medical aspects of their care, so I don’t mind changing the girls’ G-tube buttons. In another life, I think I would have pursued something in the medical field. And this way, I’m getting to do it every day.”
Alongside her daughters, husband, Chase, and their 10-year-old son, Jack, Shannon shares moments from her family life across the social media channels she’s been growing since launching her lifestyle blog, For the Love, in 2012.

Today, more than a million followers see what this bunch gets up to – wheelchair wrangling, feeding-pump beeping and syringe washing included.
“Our biggest hope with what we share is, firstly, just to normalise it,” says Shannon. “When people see the whole family doing dinner – and for the girls, that means we’re hooking them up to their feeds – my hope is just to normalise that, yes, they eat dinner a different way. And that’s okay. That’s great.” >>
Medical parents all deserve honorary nursing degrees and especially since having our girls, I’ve become so fascinated and interested in all the medical aspects of their care.


Is our life different from what we envisioned? Yes, but it’s still full and beautiful and happy and thriving.
Shannon also shares in the spirit of supporting her former self – those parents who are new to a life they never expected.
“I think it can be really empowering and comforting, especially at the beginning, to see other families who are in a similar situation and still living full, happy lives,” she says. “I’m not talking about toxic positivity. It’s not like we’re happy all the time or everything goes smoothly, we’re just normal people. Is our life different from what we envisioned? Yes, but it’s still full and beautiful and happy and thriving.”
Shannon’s feelings around her girls needing to tube-feed have vastly evolved since the notion was first suggested to her for baby Charlie, who seemed to nurse with no issue until she was four months old and started losing weight.
“We thought maybe I had lost some of my milk or there was an allergy situation going on, so we switched to a hypoallergenic formula at that point – and this was still all by mouth,” says Shannon. “But then she started presenting with other complications. She started having infantile spasms at around five months and this is when we realised, okay, something is really wrong.”

working on eating orally, “even just a little bit”, with an occupational therapist and speech and swallow therapist.
appointments we had where they were nudging us in that direction and I was like, ‘no, no, no, let’s keep trying’.”
Around the time Charlie turned one, she was diagnosed with a rare, inherited genetic condition under the umbrella of congenital disorders of glycosylation, called CDG-1p (ALG11-1p). Then came months of
“I was very resistant to the idea of a feeding tube,” says Shannon. “Whether it was conscious or subconscious, it felt like an admission, or submission, to her being really unwell. That’s what it equated to in my mind – she’s not in a good place, she’s really medically complex, she’s not healthy. I don’t know how many gastroenterologist
Things changed when a swallow study revealed that Charlie was silently aspirating and taking food and drink into her lungs.
“We were putting her health in jeopardy by pushing this any further – and once we had her G-tube I was like, oh my gosh, why did we wait so long to do this?” says Shannon. >>

“She was a totally different kid once she was nourished properly. Then with our second daughter, Ava, honestly, I could not wait to get her G-tube placed.”
Ava was, as Shannon puts it, a surprise. After learning of Charlie’s condition, Shannon and Chase decided to grow their family through IVF and had started the process when, despite being on contraceptives, Shannon discovered she was pregnant.
Once she was in my arms, I instantly felt that love you feel for your kids – that crazy love – and I knew everything was going to be fine.
“I called our geneticist even before I called my husband to tell him,” says Shannon. “When we got tested and found out that this baby had the diagnosis – I feel shame in admitting this, in hindsight – I was devastated. I remember thinking and sometimes even saying, ‘can you imagine having two kids with these medical complexities?’ – and there we were. It felt like we were being punked.”
The Willardsons are a family of faith, so Shannon spent her pregnancy with Ava praying for a miracle.
“I know she could have been healed if that was God’s plan for our family, but she wasn’t, which tells me that wasn’t the plan,” says Shannon.
“And I remember so poignantly, when Ava was born, that feeling of being devastated was just gone. Once she was in my arms, I instantly felt that love you feel for your kids – that crazy love – and I knew everything was going to be fine.
“Don’t get me wrong. It’s not like I never have moments, with both of my daughters, where I get those little twinges of sadness about what I thought their life would be. I don’t think you need to feel shame about that as a parent of a medically complex kiddo. But it was such a beautiful thing to experience with Ava, where I was so devastated about her diagnosis during the pregnancy and then, once she was in my arms, that feeling just dissipated and was replaced with overwhelming love.”
Ava, like her sister, now has four bolus feeds of formula each day and doesn’t seem at all bothered by not eating orally.
“Neither of the girls have ever shown interest in food,” says Shannon. “We’ve really tried to get equipment that allows them to come to the table and easily be a part of shared meals. They are extremely social and very aware of people being around them. Charlie, especially, has FOMO [fear of missing out]. If you leave the room and she’s not with you, she’ll start whining like, ‘hello? Bring me with you!’” >>

Charlie and Ava both “light up” when their brother, Jack, is around –and things are about to get a whole lot more socially stimulating in the Willardson household. In recent months, Shannon’s social media feeds have followed her family’s journey with surrogacy and, around the time this magazine is published, they’ll welcome twins.
“I grew up in a big family – with six siblings – and it was total chaos but I loved it,” says Shannon, when asked how she’s feeling about mothering a brood of five. “My dad’s job caused
him to travel a lot and so my mum was doing it solo a lot of the time and she just made it happen. My mum was just a boss, so I’ve probably got a little bit of delusional confidence because of what I was exposed to as a kid.”
She’s also got help. Much like in Shannon’s childhood home, Chase’s work often sees him travelling while she solo-parents – all while creating content and running her own wellness and supplement business, All That Nutrition.
As Shannon shares with her followers, “we would basically be
screwed if it wasn’t for our unicorn nanny and our support system” –which she’ll be expanding once the twins arrive.
“I’m under no illusion that it’s not going to be really hard in a lot of ways, or that we won’t have moments where we’re like, oh my gosh, we really are in over our heads now. I’m anticipating all of that but we’re going to take it as it comes and we’re going to hire more help and figure it out,” says Shannon.
“I think every parent has moments where they feel like they’re drowning and struggling to manage everything going on in their life. And while having more kids will be an adjustment, especially at first, Chase and I know that we’ll figure out how to make it all work and it will be great! I think the part I’m most looking forward to is just more people to love on those girls, you know? There’s just so much that is beautiful and singular about life with them and I feel excited to bring more kiddos into that.”

I think every parent has moments where they feel like they’re drowning and struggling to manage everything going on in their life. And while having more kids will be an adjustment, especially at first, Chase and I know that we’ll figure out how to make it all work and it will be great!

Syringes are a tube-feeder’s best friend –but have you mastered their full potential? It’s time to take the plunge with these tried and tested tips from our community.

Everyone needs to be told about the cut-off extension tube trick. I’m indebted to Sharee Barker for generously sharing this hack – and it truly is a game-changer. When it’s time for a new extension set, because it’s brittle where the clip is, I just cut it at that point and it becomes my ‘straw’. I’m very strategic about where I clip my extension set, so always keep the clip below where the cut mark would be. When I create my blenderised meals, I store them in 500ml jars or plastic containers. Then when it’s time for a feed I just use the modified extension tube to draw the blend into my Medicina ENFit reusable enteral 60ml syringe.
For my coffee consumption I have the perfect Keep Cup for an espresso and once the coffee has cooled – usually with the help of some added cold water – I just pour the coffee into the barrel of my syringe allowing it to gravity-feed into my stomach.
There are three options for wine consumption. Mostly, I just make a blend of wine, cheese, pâté and crackers, then draw it into the syringe like a typical blend. Another option is pouring it straight from the bottle into a syringe barrel and allowing the wine to be gravity fed. The less bogan version would be putting the wine in a jug.
In the photo you can see me finding a solution to only having access to a glass of wine. I drew it into the syringe via the modified extension tube, then I syringed that into the barrel of another syringe and let it gravity-feed into my stomach. >>
Riley does push her own syringes sometimes – we always ask her if she would like to – but the majority of the time she is in the middle of playing or reading so we usually do it. She’s hilarious when she says: “Hurry up, Mum! Let me push it faster!” She just wants to go go go!
I love using my Strucket straining bucket to help drain, dry and store our Medicina ENFit syringes. We also have the Boon Grass drying rack to help dry them after washing. As we travel, we keep a set of clean syringes in a hard pencil case with some spare tubing in there, too.
Riley has three sisters and our youngest, Maisee, has been obsessed with pushing Riley’s medications and flushes since she was a toddler. She’ll run from the other side of the house to help us!

I have always taught my son, Luke, about the purpose of his feeding tube and like to encourage him to be independent with it. Luke doesn’t have the strength to push a blend through a syringe but he definitely gives it a good try, especially when he wants to finish and move on to something else! He prefers to inject water, as it’s easier for him to push.
We like to use the Medicina ENFit 60ml reusable enteral syringes and to help them last longer, I spray the plunger with olive oil spray so they glide easily into the syringe. Once their time has come, we have some fun in the backyard using old syringes as water pistols.

For Luke’s first birthday we created our own version of a ‘cake smash’ photo shoot at home and filled syringes with dyed yoghurt for him to paint a canvas with.

Want to hear more from Kym, Grecian, Eliana and a bunch of other tube-feeding folk? Tune into Tubie Talks, a podcast celebrating the tube-feeding community, on your favourite podcast platform.
This story was created in partnership with InterMed Medical, Australia’s supplier of Medicina syringes.
Shop the full range at shopmedical.intermedmedical.com.au
“I’m a glass half-full person – I’m not going to compromise participation.”
Peter Macaione


Tube-feeding is not a one-size-fits-all thing, so why settle for anything less than a custom-made support team? We hear two stories of self-advocacy, both with a very special nurse in a starring role.


Twenty years ago, Peter Macaione had radiation treatment for head and neck cancer. “In those days it was a terrible, scattergun approach to radiation,” says the 62-year-old musician. “Just target the whole area and hopefully get it, you know?”
Since then, the lead guitarist has struggled to speak and swallow. Having developed a chronic lung condition from food entering his airways, in 2023, Peter went for a speech therapy appointment at The Wesley Hospital in Brisbane – and came home with a gastrostomy (G) tube.
“I wasn’t eating and I was losing weight, big time,” says Peter.
“All of a sudden I was in the emergency department and the gastroenterologist came in and said, ‘Look, we have no choice, we’re going to have to put a feeding tube in’.”
That feeding tube was a percutaneous endoscopic gastrostomy (PEG) with a long tube permanently attached. “And it was kind of getting in my way,” says Peter, who recently made the switch to a low-profile, button-balloon-style G-tube.
“It’s great – a lot more discreet,” he says. “I’ve got a grandchild now, so every time I pick him up he feels for it, saying ‘Poppy belly button! Poppy belly button!’”
While getting the majority of his nutrition through his tube, Peter still carefully swallows water and his daily coffee. “It takes about two hours to
Sarah and the team moved me to the point I felt I had to give something back. It brings me to tears, to be honest.
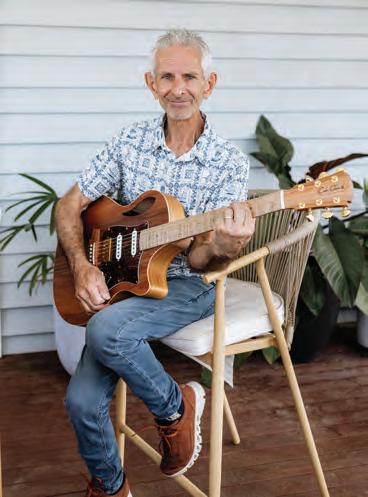
drink it, but it’s worth it,” he says. “I’ll also have a beer. I try to maintain a social presence – I’m not going to shy away from being with mates, so I will sip on a beer or two.”
Soon after completing his cancer treatment, alongside some of those mates, Peter walked the Kokoda Track in Papua New Guinea. Now he and his wife, Jo, are preparing to tackle the Camino in Spain.
“I’m a glass half-full person – I’m not going to compromise participation,” says Peter. And registered nurse, Sarah Jane van Oosterhout, has ensured he hasn’t had to.
Sarah is part of the Abbott Homecare Connect program which, in collaboration with healthcare
providers, sees a team of registered nurses providing nationwide support to people transitioning from hospital to home care.
“She’s just been enormously helpful the whole way along,” says Peter, who was put in touch with Sarah via the rehabilitation team at The Wesley. Soon after he was discharged, Sarah began home visits to help with tube maintenance and, more recently, travel plans.
“She’s arranging for my Ensure* to be sent to our hotel rooms in Spain,” says Peter. “Sarah’s just been fantastic. I cannot praise her enough.”
In a show of his appreciation, last year Peter organised a fundraiser performance with a group of fellow musicians to raise money for new rehabilitation equipment at The Wesley.
“I’m already planning the next one and it’s going to be bigger and better,” says Peter. “Sarah and the team moved me to the point I felt I had to give something back. It brings me to tears, to be honest.” >>



Another 62-year old, Brisbanebased Peter – Peter Russo, who goes by Pete – is also supported by Sarah and Abbott Homecare Connect.
A former military serviceman and air-traffic controller, Pete has motor neurone disease (MND). In 2024, he had a radiologically inserted gastrostomy (RIG) tube placed as a precautionary measure. “We’re geared up and ready to go,” says Pete. “We flush it twice a day and we’ve had some practice feeds, so I know what to expect.”
Pete can still eat safely and, as his partner Tess Nobile points out, amid Pete’s medical appointments and care team coming and going, sharing meals has become all the more important.
“It’s a connection for both of us –and it’s a social thing when we go out,” says Tess. “There’s been a lot of giving up stuff with MND. Pete can’t use his hands or arms and he’s barely walking. So to then concede that he’s got to take his massive enjoyment of food and put it through a tube, that makes us both sad.”

Many people do what the first doctor they see tells them to do, but we’ve learned to ask, what are our real options? Who can service us best?
“But when the time comes when I need to rely on the feeding tube, my attitude might change,” says Pete. “I’m pleased the feeding tube is there because, to say it blatantly,


I won’t starve to death. It’s the most important bit of equipment for me to sustain life.”
Uncertainty comes part and parcel with a neurodegenerative condition – but Pete and Tess can be sure that, throughout their tubefeeding journey, Sarah will be onhand to help.
“She’s very responsive,” says Tess, who will often send Sarah photos of Pete’s tube when seeking guidance. “Sarah’s great at providing that support and reassuring us that we’re not going crazy.”
Pete also receives care at home from community nurses and support workers. “But they didn’t have any RIG experience, so Sarah offered in-home service,” he says. “She also trained our support workers and the community nurses. Nothing was too hard.”
In sharing advice with those who are building a team of specialists and carers, Pete says to be very selective.
“Many people do what the first

doctor they see tells them to do, but we’ve learned to ask, what are our real options? Who can service us best? We’ve got Sarah as a single point of contact – our team are all single points of contact – so we don’t get inconsistent information.”
“It’s personalised support from someone that we’ve formed a relationship and rapport with,” adds Tess. “What I love about Sarah is that she has our whole care team’s details, so we don’t have to repeat ourselves. Everyone’s sharing information, everyone’s updating everyone.”

Tess also urges other caregivers to play “a more vocal role” when supporting their loved ones.
“I know Pete’s living through this, physically, but it’s a ‘we’ journey for us,” she says. “Find your voice and, without any shame, speak up. And don’t be afraid to handpick your team based on what works for you and your family. That’s really important.”
This article was made in partnership with Abbott Homecare Connect. To learn about their nationwide team of registered nurses offering comprehensive home support for patients, caregivers and healthcare professionals, visit abbotthomecareconnect.com.au

From TPN and tube-feeding to a bowel transplant, Garrett Taira has tried it all. We chat with the actor, dancer and chronic-illness advocate about self-esteem, support systems, and the dangers of door knobs.
INTERVIEW // MELANIE DIMMITT WORDS // DANIELLA DOUGHAN
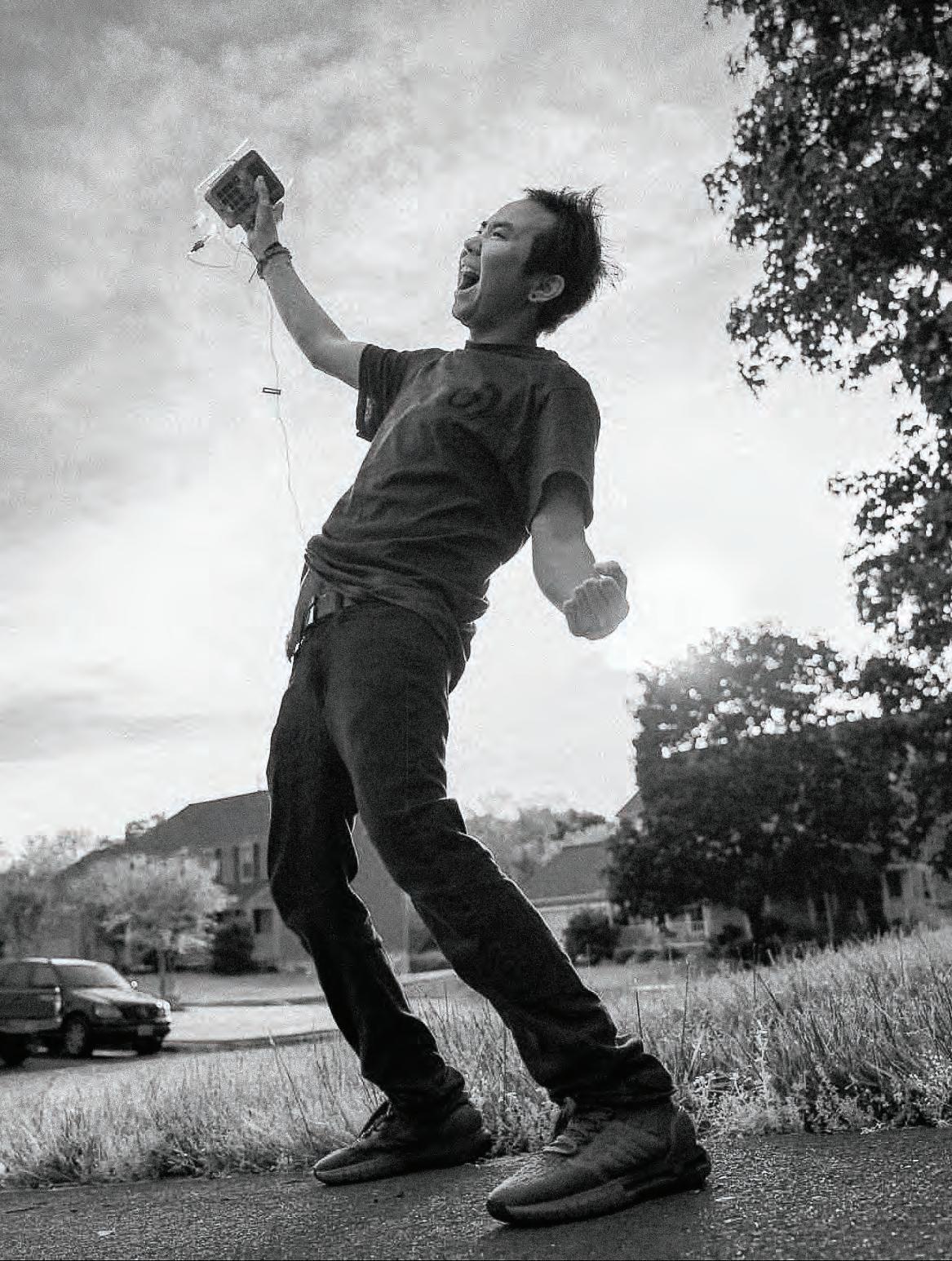
Garrett Taira’s medical history is, in a word, complex. Born in Maryland, USA, with chronic intestinal pseudo obstruction, he’s required daily IV nutrition, multiple hospitalisations and surgeries throughout this life.
On total parenteral nutrition (TPN) from when he was nine months old, Garrett received his first gastrostomy (G) tube at age seven. In 2010, at 18, he suffered agonising pain caused by perforations – holes – in his intestines. After emergency Ileostomy surgery, Garrett woke to find his colon, large intestine and almost 2m of small intestine had been removed. What remained of his small intestine had been brought through his abdominal wall, allowing his body’s waste to travel through a stoma, into an ostomy bag.
In the midst of these extraordinary health challenges, in high school, Garrett found a passion for dance and has gone on to become a professional dancer, actor, comedian and speaker. He’s been featured on The Ellen Degeneres Show, choreographed an award-winning performance at Beyond the Stars Dance Competition and has his own TEDx talk.
In 2022, Garrett went under the knife again – this time for a lifesaving double organ transplant, receiving a new bowel and kidney.

My body has taken me through all my hardships. It’s like when people say, “be proud of your scars”. It’s just like that, but with tubes.
Bowel transplants are very rare, with only 90 or so performed worldwide each year. It’s also a high-risk transplant, with a minimum 12-month recovery period.
Two years on, when we caught up with Garrett he was generous with his time, fast with his laughter and positive with his responses. This is his story.
What was it like growing up on TPN, with an IV line in your chest?
I think the whole reason I did so well was because my parents were so careful. My dad was a dentist and my mum was a speech and language therapist and also trained as a nurse. We were able to be very sterile –although I did get sepsis a lot.
I’d participate in sports and we’d change my TPN tubing after every activity. But sometimes, when you’re in the middle of fifth-grade gym class and your mum’s not there, you don’t know how to change it!
Growing up, the hardest thing to get used to was watching everyone else eat around me. Injecting food is not the same as chewing food!
As the oldest of four siblings, how were you included in family celebrations that centred on food?
Sometimes I would just watch, other times I would eat and then vent my stomach immediately so I could just taste food. But I don’t recommend doing this, you just dehydrate yourself.
You always know – I’m sure a lot of kids can relate – that you’re different and you’re frustrated and you don’t know why it’s you and not the other kids. My parents would always make sure that I stayed grounded and grateful.
You started dancing and acting as a teen. What was it like having tubes while doing these physical things? I was always self-conscious of my body. I had a lot of tubes and I was always wearing a swim shirt at pool parties. I think when I found dance it was really nice because I got a lot of validation from my peers. I had a really good group of friends and classmates who were very supportive. There was a time at the beach when a friend told me I didn’t need to be so self-conscious and I took that on. My body has taken me through all my hardships. It’s like when people say, “be proud of your scars”. It’s just like that, but with tubes. Since then, I’ve stopped wearing a swim shirt. When I danced it was easy for me to focus on the music and let my worries fade away. I felt a lot more present and I think that’s what drove my passion even further. By the time I started acting, my tubes weren’t a big deal for me in front of my peers, or going on dates, because I was very nonchalant about everything.
Sometimes though, my cords would get stuck on door knobs or chairs or something. For tubies, door knobs are our arch nemesis!
For tubies, door knobs are our arch nemesis!
In 2010, you woke up after emergency surgery with an ostomy bag and most of your digestive system removed. How did this shake things up? My intestines never really worked because they were always extended. If I ate a teaspoon of something, I would have a stomachache for weeks. I’d be in so much pain that I would go to school hunched over. I was always so bloated, I looked really distended. My surgery to get the ostomy really changed things. I felt a lot more comfortable when breathing, relaxing and moving. It really improved my quality of life, despite the management of an ostomy on top of TPN.
We tried tube-feeding before surgery with the G-tube and then after surgery with the G-tube, but it just wasn’t working for me. It was a step in the right direction, but we didn’t really get there until more than 10 years later. >>
Is that when you realised you needed a transplant? Yes. TPN taxes the liver, so sepsis had started happening more often. And antibiotics tax the kidneys, so I was getting kidney disease. I was also getting a lot more sad and depressed about where my life was going to go and what was going to happen, because it was all such unknown territory.
In 2022, I went in for a routine check-up and the specialists mentioned I should consider getting a transplant. At the same time, I was really trying to turn my life around. I was taking steps to get out of depression, I was renovating my basement, I was working out, I was trying to get some momentum going to hopefully catch a break.
I think a big reason why I wanted to do the transplant was because I didn’t want my parents taking care of me in their golden years. Without the transplant, in a few more years, I’d have been on dialysis and things would just have plummeted from there. And my parents have sacrificed so much for me already.
Making that decision must have been terrifying. What risks were you made aware of? The doctors said I could still need the ostomy, that there was a chance of rejection, that I’d need a lot of blood transfusions and that the first year would be crazy, because [that’s when] they’re most worried about my body rejecting the new organ and the kidney being able to handle it.
It was my decision to do the surgery. Even when I asked the nurses, “what would you do?” they didn’t say
anything because I’m sure they’ve seen it both ways. But I ended up getting a bowel and a kidney, and dude – when they say intestinal transplants are the hardest to recover from, it’s the truth.
What happened after the transplants? I stopped TPN after about a week and a half. We slowed down and wanted to transfer to tubefeeding. I had a new ostomy with a new intestine. My doctor wanted me to try a little bit of food, so I started with Osmolite through the G-tube, then tried eating things like baby food packets that you squeeze, then more starches like toast, in very small amounts.
Can you eat whatever you want now? I’m eating a very strict diet because I’ve been managing the transplant and getting used to what foods work and what foods don’t. But when I cheat and stray from my diet, it blows my mind. Have you ever seen the movie with Bradley Cooper, Limitless? He takes a pill and can access 100 per cent of his mind. That’s what it feels like.
So you don’t need to be too precious with it? Yeah! You can spin it like a wheel and flick it and stuff, it’s super durable. It’s great. I’d tell anyone who was worried about getting one that you’re going to wish you had gotten it a lot sooner. It’s like you were driving a 1984 Corolla and now you’re in a Tesla!
What are you excited about, career-wise, right now? I think I pursued acting and dancing because I had low self-esteem and was getting external validation from others.
Because I was really self-conscious about how I looked, I always felt like I had to prove something. I have higher self-esteem now so I don’t need the external validation of dancing and filming to make me feel like I’m worthy. What I love about dance and films is storytelling and recently, I’ve been able to do this within our community. I feel like my passion is helping more people who are also struggling while managing chronic illness, or feeding tubes, or just don’t know what the future looks like.
No one ever knows how long a transplant is going to last and since time is so valuable, I want to spend that time doing what I can to help others.
When you got your G-tube out in 2024, you published a beautiful social post – almost like an ode – saying goodbye to it. What was this adjustment like? Oh man, I still feel like I have a G-tube! I still reach for it because I think it’s leaking sometimes. That G-tube was one of the best things that ever happened to me because it brought so much relief to my life – and it was the one thing that was low-maintenance. garretttaira.com
Find more from Garrett – and support his work – on his Patreon platform patreon.com/Garretttaira.
At 22 years old, with multiple organs failing, Celia Chartres-Aris was told she had a less than 10 per cent chance of survival. Today, she’s designing new laws aimed at levelling the playing field for the disability community.
WORDS // KATE THOMAS


Celia Chartres-Aris wants you to know that everything is going to be okay. Those six reassuring words are what Celia longed to hear when she received her first feeding tube.
Celia is a UK-based, multi-award winning adviser, lobbyist, investor and policy designer. Some would say she’s the ultimate advocate. If you’re wanting to design new legislation or improve equity of representation for disabled people, she’s the person you’re likely to turn to.
Apple, LinkedIn and Coca-Cola
have all enlisted her help. So too have the UK Government, the European Union and the United Nations. Her work has been recognised by Forbes, The Financial Times, Metro and the BBC and, in 2024, the Shaw Trust Disability Power 100 named her the UK’s most influential disabled person.
But rewind to 2019 and, as Celia lay in hospital, surrounded by the beeping of monitors and the glare of bright hospital lights, she was about to be met with a smorgasbord of feeding tubes.
“The feeding tubes were coming on and off,” Celia recalls. “I had NGs [nasogastric tubes], which then switched to NJs [nasojejunal tubes].


I left university early but very much had the mentality that I can do anything – and I won’t let my disability stop me.
Then the NJ tubes stopped working and I was completely bed-bound for about a year.”
Growing up in picturesque Hampshire in the UK, Celia was often referred to as “the sick kid”. She was diagnosed with multiple conditions before doctors identified Loeys-Dietz syndrome, a genetic connective tissue disorder that she shares with her father.

Celia began studying law, a passion she had since childhood, with aspirations to pursue a career in politics. “I was mad about it. My family always used to say that I was getting a degree in arguing,” she says with a grin.
During Celia’s second year of university, her health took a dramatic turn from “she’s always ill” to “something really isn’t right”. She began experiencing unexplained stomach issues.
“I was struggling through my degree, just on my final legs trying to pull myself through it,” Celia says. “I left university early but very much had the mentality that I can do anything – and I won’t let my disability stop me.”
After leaving university, Celia met her future husband and began living a more relaxed life, trying to get back on her feet. Then, the pandemic hit and Celia experienced non-Covidrelated multiple organ failure, leading to her being placed on total parenteral nutrition (TPN), where essential nutrients are delivered directly into the bloodstream.
Her doctors gave her a slim chance of going home, just under 10 per cent. In intensive care, she was isolated and too weak to even hold her phone, relying on nurses to relay messages from family and friends. The stakes were especially high but, after months upon months in hospital, she returned home. >>

who are tube-fed can’t have fun. She’s experienced everything from people not making space for her at the dinner table to others pulling on her tube, laughing, or even shouting at her in the street.
In a recent LinkedIn post, Celia shared an encounter where a passerby called her tube “disgusting”. She wrote:
“Do you not think that as a young woman covered in tubes, bags collecting fluids, and goodness knows what, and with a body which doesn’t look like anyone I see in the media, I battle with my appearance and selfconfidence every single damn day.”
This is our lives. This isn’t going anywhere. I’m going to have this for the rest of my life.
“I survived. I did it. I fuelled my organs back up again and we got there,” says Celia. “I was sitting at home, my new life on TPN, not able to eat or drink, trying to rebuild my body back as much as I could, thinking to myself, what am I going to do?”
It didn’t take long before she had an idea. Using her specialist knowledge in human rights law and passion for accessibility, Celia helped birth the world’s first policy think tank focused on disability. From there, her career snowballed to working around the world with governments and policy makers to design new and amend old legislations.
Now 27-years-old, five years after first receiving her TPN, Celia describes her connection with her tube as “a funny relationship”.
“I am never going to sit here and say, ‘I love it. It’s amazing’,” she says.
Celia explains that it’s taken a lot from her, like the experiences of being a 20-year-old out with friends for drinks or dinners. Some of her friendships have faded, because people assumed she couldn’t join in.
“But it’s given me my life – I wouldn’t survive without it,” she says.
Throughout her journey Celia has encountered many misconceptions –one of the biggest being that people
Alongside her post was a photo of Celia, her hair swept to one side and her shirt pulled down to reveal the array of tubes and tape across her chest. She signed off by saying: “This picture is for you. Enjoy my disgustingness. I for one won’t hide, or stop showing what I wish I had seen growing up, to know that all bodies are different, and all bodies deserve to be seen and respected with equity.”
Now would be a good time to mention that, among her other accolades, Celia was the first person to walk London Fashion Week while having a blood transfusion.
She believes that most of the time, when people act with discrimination towards disability and feeding tubes, it’s not out of hatred but, rather, a lack of understanding. She also believes there’s a massive misunderstanding about the purpose of tubes.
“There has been such amazing awareness around feeding tubes and eating disorders,” Celia says. “But there hasn’t been enough conversation around people that live with these forever. This is our lives. This isn’t going anywhere. I’m going to have this for the rest of my life.”
It can feel taboo and unsexy to talk about things like food digestion and bathroom habits. But Celia implores us to shake off our discomfort and try, especially for those who are new to tube-life.
“I wish people would be able to see [tubes] as these incredible life-giving things, not something disgusting that we don’t want to talk about or see. The ultimate goal would be – and I hate the word normal but I’m going to use it – to normalise tube-feeding
as part of everyday life. It’s just your body.”
Celia’s daily routine is centred around her food pump schedule. She starts her day by unplugging at 7am and reconnects at 4pm. Everything she does revolves around these times.
You don’t need to do things the way everybody else does. Being different is the one thing that we all have in common. Everything is going to be okay.
Following such a strict schedule can feel limiting – and Celia emphasises that there simply isn’t enough psychological support for people transitioning to life with a tube. “What’s not covered are the mental health implications of adjusting your lifestyle and learning to socialise and participate again,” she says. And she’s petitioned her own hospital about this on numerous occasions.

“As soon as somebody is given a tube, there should be an automatic referral to a mental health support team. It’s vital.”
Drawing from her own experiences, Celia highlights the need to find coping mechanisms that work for you.
“I always focus on the purpose behind it and think about where I’d be without it. When I didn’t have my TPN, I dreaded food. Everything I ate made me sick and I often had blisters and burns all over my mouth from vomiting.”
Celia stresses that it’s okay to feel sad that life didn’t turn out how you’d
planned or hoped. You don’t have to feel positive all the time, but it’s important to “remember that your tube has given you your life back”. All the happy moments – playing with your dog or going on vacation – are possible because of it and fuelled by it.
“I wouldn’t be able to do any of the things I’m doing now if I didn’t have my tube,” she says. “The alternative would not make me happier. It wouldn’t make my life better.”
Celia often feels nervous about sharing her personal experiences. However, that anxiety is outweighed by her desire to shed light on the realistic side of disability. She believes that every story she shares helps someone out there feel less alone.
“Trust me, everything you’re thinking, I get it,” she says. “The biggest thing I’ve always wanted to be told is that you don’t need to do things the way everybody else does. Being different is the one thing that we all have in common. Everything is going to be okay.”
celia.chartresaris
Not long after her feeding tube was placed, this cheerleader was back in the air, chasing her dreams, bringing thousands of supporters along for the ride.
INTERVIEW // MELANIE DIMMITT WORDS // DANIELLA DOUGHAN

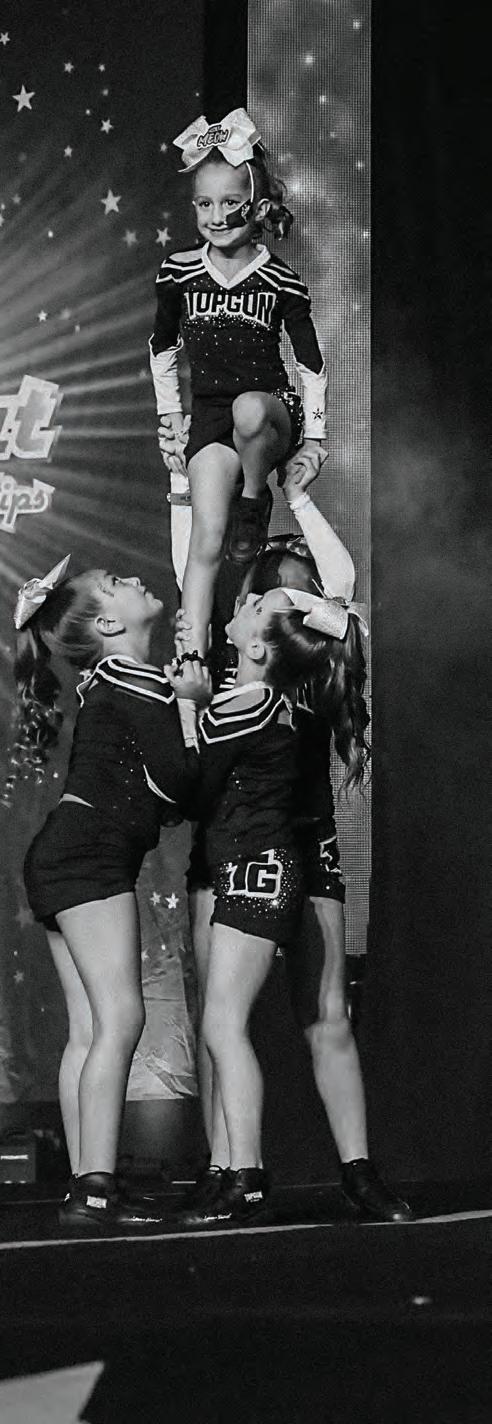
Eight-year-old Sutton Short had never seen anyone with a feeding tube before she had her nasogastric (NG) tube placed in December 2023. The Florida-based youngster was more concerned about making it on to her dream elite cheerleading team, the Biker Babes, as a “flyer” – the athlete lifted into the air during a pyramid or stunt.
Sutton made the team, feeding tube in place, and now has the goal of competing in state and then world championships.
“It feels like a dream and it feels amazing,” says Sutton when we speak to her and her mum, Kali.
Before having her NG tube placed, Sutton was worried about how it would feel and whether she could continue doing what she loved.

“I was like, ‘What is it going to look like?’ ‘Am I going to feel it when it’s in?’ I thought I couldn’t cheer, because I thought there was no way I could tie it up like I do, so I thought it could get pulled out.”
Sutton’s trick? Tying her NG tube up in her ponytail, thanks to a handy video from one of her Instagram followers, a gymnast who also has an NG tube. Sutton’s Instagram account @thelittlestflyer has quickly fostered an online community of tube-fed kids and their parents, searching for and sharing advice.
“When I first got my tube, a couple of minutes afterwards, I kind of felt it in my throat, and it was uncomfortable to sleep because it was in my throat all night,” says Sutton. “But then by the
You should try and do your activities. I was a bit cautious at first, but now I’m my normal self!
second day I had it, I didn’t feel it. A couple of weeks later I kept waking up in the morning and I’d think I didn’t have anything on me, but then I saw my tube and realised ‘oh I do have something on me!’”
Sutton’s sisters, six-year-old twins Sawyer and Merritt, also needed to get familiar with her NG tube. “My sisters were just worried, they thought it could come out very easily,”

says Sutton. “Actually, in the pool once I was swimming and my sister Sawyer came swimming towards me and she kinda pulled my tube out a little and she panicked. She was so scared. My grandma helped me put it back in and it didn’t hurt because she’s a nurse.”
Now that everyone has adjusted, Sutton says she hasn’t fundamentally changed since getting her tube put in, but there have been some unexpected benefits.
“I’m the same person, but I went from 28 to 38 pounds and I definitely have more energy. We were at this festival and it had this tall climbing tower and if you make it to the top you press a blue button. I couldn’t do that before – I didn’t have enough strength in my arms and my legs when I tried – but I did it with my tube. It felt amazing!”
When it comes to feeding, Sutton does a 10-hour feed at night and has recently adjusted to a one-hour feed during the day, after two daytime feeds caused stomach aches from the volume.
“Then for lunch I have something out of my lunchbox like half a bagel and some snacks while I’m on camp.”
Summer camp, Sutton says, is a daytime camp full of activities including acting, where she simply adjusts her tube to the task at hand. “We have a bunch of activities, so I’ll tie my tube up and then just put it down for my feeds.”
As for Sutton’s advice for anyone new to the tube-feeding world, it’s all about continuing to do what you love.
“I’d say, just tie it up in your hair with bobby pins or just put it through your shirt. You should try and do your activities. I was a bit cautious at first, but now I’m my normal self!” >>


When did you realise that Sutton might need a feeding tube?
We’d been on this journey since she was a baby and never gained weight. It was seven years of feeding therapy and trying a high-protein, then a high-fat diet and pushing Sutton to eat and her fighting back and me feeling like I’m force-feeding my child. At the end of last year we were told Sutton’s weight was too low and that she needed to be tube-fed. It was overwhelming, stressful and nervewracking but I turned a corner in my brain and thought, maybe this will be a good thing. It was a real process of absorbing it.
How did you find the right balance of what goes in Sutton’s tube? We were in the hospital for a week, so we did a lot of experimenting there. We use the PediaSure Peptide 1.0 Cal formula and that has worked for a really long time.
Her night-time feed is pretty easy when she’s sleeping and it doesn’t bother her. It’s pretty flexible and we’ll start anytime between 8pm and 10pm – some nights she doesn’t get home from cheer until 9.30pm!
Sutton does eat regular food, too, so I don’t feel as stressed about it if she misses something.
How did you help prepare Sutton for having her feeding tube placed?
She’s very smart and really likes medical things so it was just about being completely honest. We searched for videos of tubes being placed and it was really hard to find them. That’s why Sutton wanted her tube being placed shown on her Instagram – because nothing existed, especially for kids.
Sutton asked if she could still cheer with a tube, and I was like, “I don’t know, let’s Google it”. We couldn’t find anyone else who did it, so once we found out from our doctor she could still cheer, Sutton said, “I want to be that person that people can find, and show everyone you can still do it”. That’s how we started her Instagram and that’s why she asks for everything to be put on there.
We started it in December 2023 and now Sutton has over 21,000 followers. It’s been amazing to hear stories from other tube-feeders all over the world. We get a lot of DMs
Sutton said, “I want to be that person that people can find, and show everyone you can still do it”. That’s how we started her Instagram and that’s why she asks for everything to be put on there.
from parents who find our account and their kids are just super grateful to see another kid happy with a tube. We get messages from parents whose kids are about to get tubes and Sutton will send them private DMs saying “good luck, you’re going to do great”.
How do you deal with unwelcome advice or comments? The good far outweighs the bad and when we’re helping families, we know we’re doing the right thing. We’ll get a few Munchausen syndrome [a psychological condition where someone pretends to be ill] comments or people saying that we’re exploiting our child, but Sutton wants to do this. In the beginning I blocked a few people, but now her followers will clap back at people for us so I don’t have to.
Sometimes at cheer competitions, Sutton gets stopped and asked for photos which is really cool!
What are your hopes for how Sutton will eat in the future? Our doctor is really progressive with the NG tube and feels as long as Sutton doesn’t
mind it being on her face, there’s no problem continuing. She even has patients who put it in at night and take it out during the day by themselves. So if Sutton did need it longer-term, that could be an option. Right now, Sutton changes her tape every week and her friends get excited. She designs her tapes herself and to her, it’s like an accessory. We are hoping to wean her off but she needs to get her weight to a stable level and then needs to eat enough to sustain her weight. It’s just one day at a time, one appointment at a time.
How often does Sutton need her tube replaced? About every six months as long as we keep it clean. We’re very particular and we never give her anything without flushing it afterwards with seltzer water to make sure there are no clogs. We’ve only had to change it once, after about six months. Changing it is a whole process and we have to go to hospital because it has a stylet [a thin wire that helps during placement] in it, so she needs an x-ray to make sure it’s in the right place.
What advice do you have for parents who are new to the experience of tube-feeding their child? Just know that it’s amazing. It really does help them so much – and it’s not as scary or complicated as it seems. You get used to it and when you see your kids doing so well from it, you realise it’s the right decision.
Have faith that the doctors know what they’re doing and that kids can adjust to way more than you think they can.
How do you feel when you see Sutton cheering and hear her speak so confidently about her experience? I’m so unbelievably proud. I never thought she’d be changing people’s lives but she does and it’s incredible. It brings a lot of awareness to not only the tube-feeding community, but people who would never have an association with tube-feeding.
I think the cheer community is known for everybody looking a certain way. It’s not very common to have a disability in the cheer community – aside from disability teams – and Sutton is bringing a lot of awareness that you can have differences and still do what you want to do.
@thelittlestflyer
“We want tube-feeding families and people to be fully informed.”
Sarah Thomas

Avanos clinical education specialist Robyn Wortel gives us the low-down on a very common stoma issue –granulation tissue – and how to wave it goodbye.
WORDS // ROBYN WORTEL ARTWORK // KATHRYN LEAN

Granulation tissue has a few names. It could be called granulation. It could be called hyper-granulation. It could be called proud flesh – which always makes me think of it standing up there proudly, like Captain America.
It all means the same thing, which is a proliferation of cell growth coming from within the stoma tract itself.
That proliferation is the body’s way of trying to heal itself, because the stoma is not a natural body opening –it’s a created opening – and the body is clever in trying to heal things that it thinks shouldn’t be there.
While the jury is out on the precise cause of this phenomenon – and it doesn’t happen in every person, or in any one person all the time –generally, clinicians agree that it seems to be caused by irritation. If a feeding tube doesn’t fit well, chances are it’s irritating the stoma and the stoma is probably going to react and try to protect itself.
The problem with the granulation tissue is that it’s moist, tender and, usually, painful. It will leak, it will stain clothes and it might have a bit of an odour. All of these irritations are really unpleasant and uncomfortable.
So, how do we treat granulation tissue? The answer will come from your healthcare professional, who’ll have their own tips and tricks they like to use.
Here are some of the common approaches that will be in their toolkit:
First of all, you’ve got to make sure that your tube fits well. If you’ve got a low-profile tube, the stoma needs to be measured for length. If you’ve got a long tube that has a moveable skin disc, you need to make sure that skin disc is sitting approximately 2-4mm above skin level.
If you’ve got a well-fitted feeding tube, chances are you won’t see a lot of granulation tissue. But if you do happen to have some, you need to treat it. And there are a couple of things that can be done at the discretion of the healthcare professional who’s looking after you.
One option for treating granulation tissue is a hydrocolloid dressing applied underneath the skin disc of the tube to apply skin-touch pressure, which helps to flatten granulation tissue. This needs to be applied to that flesh until the red, elevated, excessive tissue has flattened and no longer appears at the mouth of the stoma.
This article was made in partnership with Avanos. For easily digestible information about tube-feeding at any age and any stage, visit TubeFed by Avanos at tubefed.com.au.
Certain topical creams can work, like a hydrocortisone cream, which can be prescribed by the healthcare professional looking after you.
A clinician might also choose to do a hypotonic saline solution – we’re talking about 18 per cent saline, so it’s really, really salty – and that salt helps to draw the moisture out of the tissue.
Silver nitrate sticks are another option – although they can sting. These burn the granulation tissue away, but you also need to make sure that the good skin around the stoma is protected so that you don’t end up with burnt skin, extending the issue further.
The incidence of granulation tissue is fairly high. Florida-based paediatrician Astrid Leon reported on hypergranulation in children*, suggesting it’s the most common complication in paediatric patients.
Meanwhile, alongside her team at Melbourne’s Northern Health, dietitian and nutritionist Emily Farrugia did a systematic review and analysis around hypergranulation, infection and misplacement**, finding that one in 10 adults with a gastrostomy will experience a complication related to one of these issues.
In my own experience, more often than not, granulation tissue will arise when a tube isn’t a good fit. So like I said, it’s best to get this right at the start.
* ‘Prevention of hypergranulation tissue after gastrostomy tube placement: A randomised controlled trial of hydrocolloid dressings’, International Wound Journal, 30 August 2018, accessed via: doi.org/10.1111/iwj.12978
** ‘Proportion of unplanned tube replacements and complications following gastrostomy: A systematic review and meta-analysis’. Nutrition & Dietetics, 23 August 2023, accessed via: doi.org/10.1111/1747-0080.12839

Disorder – and it’s getting around. Dr Tessa Taylor, founder of Paediatric Feeding International, gives us the downlow on this feeding difficulty.
Why is ARFID having a moment?
There’s lots of buzz around ARFID, with claims that it’s “new”, “rare” or “doesn’t have a treatment yet”. However, it’s more of a name change than a new condition. Paediatric feeding disorders (PFD) already have a well-established, empirically-supported treatment dating back 50 years.
The PFD diagnosis is also more comprehensive than ARFID. That said, if you have concerns about your or your child’s eating, you
don’t need to decide whether it’s a disorder or which disorder it is, what to label it, or if it is severe enough to seek help.
How does ARFID tend to show up in the children you support?
Feeding difficulties come in many different forms. A person might only eat a narrow range of foods or limited variety – no vegetables or fruits, for example – graze on snacks, or consume very specific textures or brands.
In children, mealtimes may feel drawn out and involve them leaving the table, pushing plates away, or crying. You might notice difficulty chewing or swallowing, and foods might be spat out or held in the mouth for long periods. Children might not drink water from a cup, use utensils, or take their medication.
Caregivers may have to shop all over and bulk-buy very specific cups or foods, contact companies if they run out of alphabet-shape potatoes or change the yoghurt pouch label or cap colour, deliver fast-food fresh to school, go to midnight bowling so their child will eat, or pack camping cooking gear in their car so the temperature will be just right.
How is ARFID treated? This approach is individualised and focuses on each person’s current specific feeding needs.
Because feeding difficulties can have multiple causes, evaluations

by multiple professionals – such as a gastroenterologist, allergist, speech pathologist for swallow safety, dietitian – are needed to ensure that medical and physical issues are addressed first.
Approaches involve changing aspects of the mealtime environment or foods and drinks, such as providing incentives and positive interactions for swallowing – and setting small, achievable mealtime requirements and gradually increasing them. Services may need to be intensive but can work quickly, within days and weeks, with big achievements.
Family involvement is also critical to success, considering unique family dynamics and culture – and caregivers need lots of support to learn how to keep up the gains by themselves.
Tubes can be necessary and beneficial – literally life-saving – in the short-term while a person secures help, to get them healthy enough to participate in therapy and address nutritional deficiencies and hydration. People may also have a combination of both ARFID and PFD and need tubes longer while working on increasing oral intake and learning skills.

How has this kind of intervention helped your clients? One of my clients – a nine-year-old, healthy boy – suddenly stopped swallowing even his own saliva, which caused a huge regression in his life. His mouth was constantly full of saliva so he was no longer speaking or using his hands, which were busy holding a napkin in one hand and his lips together with the other. This boy had also stopped participating in activities, was back in nappies, out of school and not sleeping properly.
He had two hospitalisations and the full gamut of medical work-ups. For 10 days he did not respond to treatment – which is highly unusual. We ended up having to also work with him outside of meals, across his whole day.
The moment when he finally swallowed some saliva, we were all crying and couldn’t believe it. His mum was jumping up and down, hugging him and celebrating. The process took seven weeks but he finally got off his nasogastric tube, gained weight, and reached a variety of 94 foods across food groups.
Another more typical example was an extreme premmie with a G-tube who had to learn his mealtime skills
later in life. He had already been through an unsuccessful hospital admission that stopped the tube feedings to promote hunger. This child had two intensive admissions with us, the second focusing on chewing and increasing food texture. He was such a trooper and learned it all! We’ll always remember his “graduation meal” where he was able to order off the menu at a cafe and drink from a cup instead of his mum having to pack formula and purées.
What advice do you have for families currently facing feeding challenges? You’re not alone. You may hear that children will grow out of it, eat if hungry, are fine if they’re not underweight, or are not ready for feeding intervention. But research suggests this is not the case and, in fact, the problems can worsen over time.
Feeding difficulties are complex and people need the right help – and this support is available. It can work quickly and have rippling positive effects into other areas for the person and their loved ones.
This story was made in partnership with Paediatric Feeding International, a feeding therapy clinic and program providing international consultancy and home services for paediatric feeding difficulties including tube weaning and ARFID. Connect with Dr Tessa Taylor and her team at paediatricfeedingintl.com where you’ll find resources including her ARFID Eating Brief and Checklist.
With collaborative care crowned the best approach for paediatric feeding issues, you’ll want to surround your kid with a fantasy league of specialists. Here’s one we prepared earlier.


Their multidisciplinary approach – a combination of dietetics, speech and occupational therapy, and psychology – draws a complex crowd to Kids Feeding Specialists in Sydney. Poised to tackle a vast spectrum of feeding challenges, once a family is in their care, this team pays as much attention to their emotional state as their nutrition, feeding skills and development.
“I just felt there wasn’t a safe space in the private health sector for children with complex feeding difficulties – and families weren’t getting the specialist multidisciplinary support they required at such a stressful time in their lives,” says founder Simone Wright.
“That’s the gold-standard, best model of care,” says Simone, while literature* examining treatment for PFDs very much has her back.
The Kids Feeding Specialists team are regularly involved in training medical students and also offer clinical supervision, both in the clinic environment and online.
“Our space arose from my passion to put together an experienced
elsewhere, so we hear about their experiences. You don’t want a sterilefeeling, clinical environment – and we definitely don’t provide that.”
Claire Davidson, another senior paediatric dietitian on the team, loves not having to rush from one family to another. “There’s so much pressure and stress on parents and when their kids have eating difficulties, those parents are looking around comparing,” says Claire.
I love having the time to say,
‘Every child is different. We don’t have to aim for a so-called normal diet. Let’s work with what your child can do and look at their nutrition within what they can do’.
Feeding difficulties are common in children – all the more so for children with disability and infants born prematurely.
A senior paediatric dietitian with more than two decades of clinical experience, Simone points out that when it comes to paediatric feeding disorders (PFDs), a collaborative approach is essential.
multidisciplinary team to support children – and we now have an amazing team of clinicians with similar passions and interests,” says Simone.
That team works together in a space that is very intentionally not situated in a hospital.
“We break that standard, ‘clinical’ barrier,” says Dr Amanda Khamis, a senior speech pathologist at Kids Feeding Specialists. “A lot of the families that we see have been
* Pediatric Feeding Disorder: Consensus Definition and Conceptual Framework. Journal of Pediatric Gastroenterology and Nutrition, Volume 68, Number 1, January 2019. Accessed via: pubmed.ncbi.nlm.nih.gov/30358739/
“So I love having the time to say, ‘Every child is different. We don’t have to aim for a so-called normal diet. Let’s work with what your child can do and look at their nutrition within what they can do’.”
Senior occupational therapist Mearelle Kachwalla says that families are relieved to have found the team’s support.
“A mother we’re working with broke down in tears and I thought, ‘oh no’, I thought I was being really gentle! But she said, ‘these are tears of relief because for 10 years I thought I was doing something wrong’,” says Mearelle. “Families carry so much guilt. We’re here with empathy and really allow families to feel heard, understood and supported, which means we get the whole picture.”

A really important part of this whole feeding journey is getting the right diagnosis. It’s not enough to make the observation that “this child is really anxious about choking and its getting in the way of their eating” when the anxiety is so extreme it impacts their functioning, and prevents them from doing the work they need to do with their feeding therapist.
If we’re seeing an anxiety-based mental health condition, we need to diagnose it so a child can receive the correct treatment. And so people can understand that this is not just “picky eating”, this rigidity is real and it’s very hard to shift.
One thing I really like to do is see the parent or parents in isolation, for their own sessions, so I can help them manage whatever is going on for them –whether it be grief, anxiety or stress. Just upskilling on how to manage those big emotions so they don’t show up as much in the feeding situation.
All the research we have tells us that negative emotions around food and eating is one of the biggest contributors to food refusal. So we need to manage anxiety – both in parents and in children –to create good outcomes.
We’re able to sit with a family’s really heavy emotions, rather than trying to push them away and fix them. It’s really important that a family feels heard, listened to and validated before they can move forward and do the really hard stuff they need to do. And this is really hard, anxiety-provoking stuff.

Belle was born at 27 weeks and was on oxygen for six months – and with all of the tubes, suction and general care in hospital, an oral aversion was created. She would not take to breastfeeding or bottle feeding and had not eaten anything solid until we met with Kids Feeding Specialists. We see the whole team once a month, with ongoing weekly support from Amanda and Simone as needed.
During our first meeting, Simone said “we want to support the parents as much as we support the child”. That meant so much to me because, for months, I felt like no one was listening to me in the hospital setting. Simone suggested changes to Belle’s enteral feeding regime and immediately, her frequent daily vomiting ceased. Belle has now been weaned from her tube feeding and her love for eating is growing every day.

You don’t want to feel like your child is just another patient, just another number. My goal as a parent is to surround Charlotte with a team of superstars who are genuinely invested in making her life better. And as soon as we met Simone, she was clearly one of those people. Her team is actually interested in and genuinely cares about complex children.

Alysia has Rett syndrome and has been PEG-fed since she was three years old. She was also eating orally up to the age of 13, when she had her spinal fusion. Since then she’s been fully tube-fed and was having problems tolerating her formula. Alysia started to vomit after each feed and was crying and very unsettled both day and night, so I contacted the Kids Feeding Specialists team and Simone advised us to start blended foods. We tried breakfast first and within two days, the vomiting stopped. We then started on blends for dinner and it’s been fantastic. Alysia has been so happy. She loves the Greek food I cook!
Charlotte was born with a rare genetic condition called Cockayne syndrome and requires blended tube feeds to optimise her growth. It would be easy to go into Charlotte’s sessions and focus entirely on her tubefeeding and growth, but Kids Feeding Specialists is more holistic than that. They make the space and time to say, “hey, how are you going? How are you dealing with this at the moment?” It’s about the family as a whole as opposed to just the professional piece around Charlotte’s diet.
To families who are new to this experience, I’d say take the time to find those superstars. Be ruthless. Move on, if you need to, from therapists that aren’t there to support you in the way that you need. And once you find that A-team, hold on to them for dear life!


This story was made in partnership with Kids Feeding Specialists. For more information about their multidisciplinary offering and to connect with the team, head to kidsfeeding.com.au
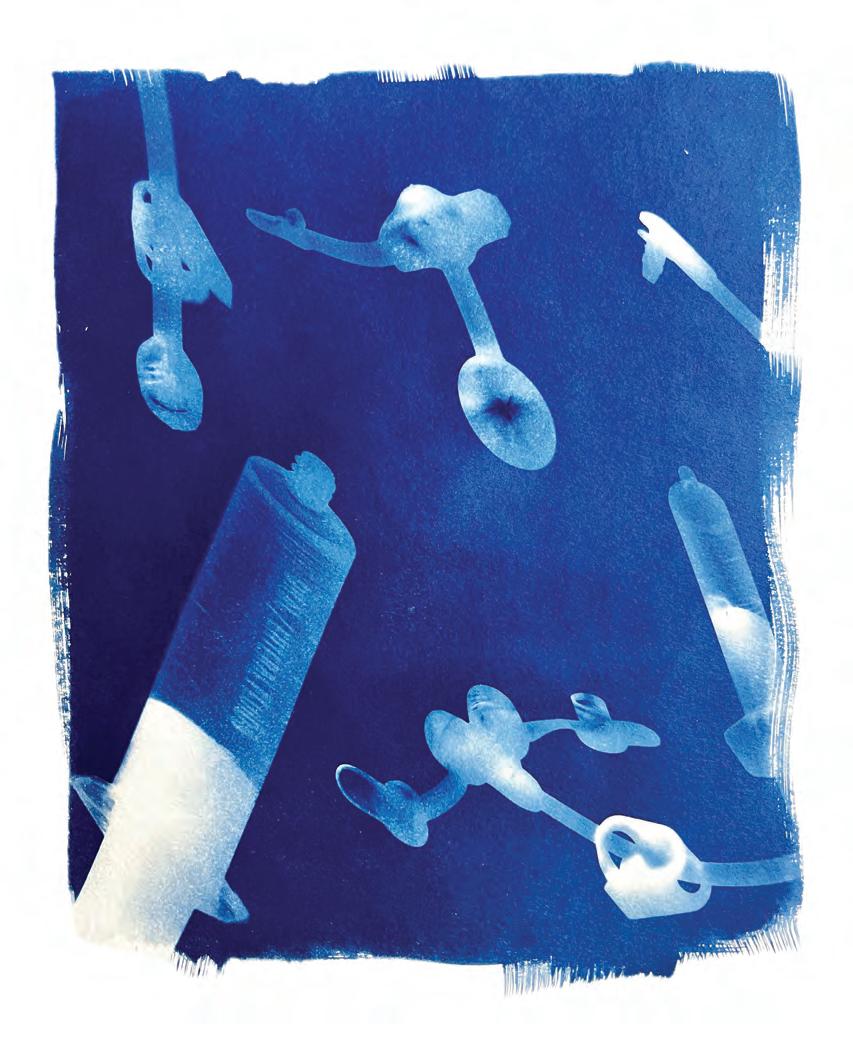
Psst… is that really a PEG? Children’s Nursing
Queensland founders Natalie Gentile and Lisa Gyselman help us get tube-feeding fluent.
ARTWORK // KATHRYN LEAN
As stomal therapists and paediatric nurses, we have lots of success managing leaking devices, healing broken skin, recommending products and ensuring correct sizing of tube-feeding devices. However, we regularly have issues knowing if our clients really have a PEG, or not!
“PEG” is a term often used to describe all feeding buttons when in reality, it describes only one way of inserting a feeding tube.
We’ve put together a short, nonexhaustive list of tube-feeding terms which may help with a more accurate description of what you or your child has. Here goes:
Percutaneous endoscopic gastrostomy (PEG)
A method of insertion for a gastric feeding tube into the stomach. It’s often performed by a gastroenterologist in a two-step procedure and involves inserting a feeding tube endoscopically (through the mouth). The tube is then pulled out of a hole (stoma) that is made in the stomach.
A laparoscopic surgical approach (often keyhole surgery) to insert a gastric feeding tube into the stomach. The stomach is brought up to the abdominal wall and sutured in place to create a stoma.
A low-profile device is placed in the stoma for feeding.
Nasogastric tube (NG or NGT)
A thin tube is placed through the nose, down the oesophagus and into the stomach for feeding. The tube is taped in place on the face.
A laparoscopic surgical approach (often keyhole surgery) to insert a gastric feeding tube into the jejunum (part of the bowel). The jejunum is brought up to the abdominal wall and sutured in place to create a stoma. A low-profile device or longer tube is placed in the stoma for feeding.
An endoscopic procedure to insert a feeding tube into the stomach that also has a longer ‘tail’ that passes into the jejunum (part of the bowel). The double access points allow for a combination of stomach and jejunal feeding or medication administration. The device often requires a general anaesthetic for placement or changing.
So, why does it matter what we call them? They do the same thing… right? Well, they are all designed to deliver nutrition to the body, but their use and care can be very different.
Providing incorrect care of the device, due to misunderstanding the procedure used to insert the tube, can cause big issues. This is particularly true for the postoperative period and through the first six months after the initial procedure.
Someone describing a jejunostomy as a “PEG” increases the risk of feeding issues – and the stoma itself is likely to be prone to different complications.
A PEG is more likely to experience things like buried bumper syndrome or hypergranulation, while laparoscopic gastrostomies generally have a higher risk of mucosal prolapse.
It can be hard to get the terminology right – especially when clinicians get it wrong, too. But in the spirit of promoting safe care, we’d strongly suggest getting familiar with – and fluent in – your or your loved one’s feeding tube.
cnqld.com.au
@childrens_nursing_queensland
Children’s Nursing Queensland


Meet three entrepreneurs charting new territory in the commercial blended whole-foods space, each from their own corner of the globe, all inspired by their tube-feeding child.
INTERVIEWS // MELANIE
DIMMITT
When did tube-feeding first become a part of your son Otto’s life? Otto was 13 months old when he got his feeding tube. This time of his life was, without doubt, the most sorrow-filled period in my life. Otto had several diagnoses and more kept coming. When he got his feeding tube, I remember thinking: “My kid is now so sick that he cannot even eat.” That said, the feeding tube was necessary and, after a while, we were happy that we didn’t have to spend hours struggling and forcing him to eat by mouth.
How did you discover the option of blending real food for Otto?
Otto was not thriving on the synthetic commercial formulas. When asking our healthcare professionals for help, the only advice we got was to give the formula over a longer period of time or give less of it with more calories. None of that advice helped and in the end my husband and I did our own research. We got inspired by the community in international groups and, when Otto started having blended real food, his vomiting stopped almost immediately.

Why was Bellyfood a business you needed to create? In our network we had quite a few parents that wanted to do blended food for tube-feeding but none of them had the knowledge or the energy to develop recipes and prepare the food. At that time I decided that everyone with a tube – no matter what background – should have access to healthy, organic, realfood blended meals.
How has Bellyfood developed since you got started? I founded Bellyfood in 2019 and so much has happened since then. Our first meals were frozen, today
they are shelf-stable. In the beginning, our main focus was to develop ready-to-eat meals for tube-feeding but over the years we’ve written articles and developed our Bellyfood platform that contains tips and tricks, information on equipment, stories from people who have a tube, recipes and much more. I’m proud that we chose to develop this database of knowledge and today it means almost as much as our products.
What challenges have you come up against as a maker of realfood blends in the enteral feeding market? First of all the regulation, which has been written for products consisting only of food isolates/ powders. Secondly, not a lot of healthcare professionals have been taught about real-food tubefeeding. In our experience, those who are aware of it had heard that it is unhygienic and not safe.
It’s one thing to develop a product in a niche category with limited knowledge – and quite another to re-educate an entire industry. Relatives, communities and tube-fed people have raised their voices and we are seeing a positive change in what is recommended in Denmark.
Today, communities for blending food for tube-feeding are growing rapidly and recently, the largest hospital in the country published a book on how to make blended tube-feeds. This is a huge acknowledgment.

What are your hopes for the future of Bellyfood? I hope we can provide even more diversity in the food that we offer people with a feeding tube. They should have the opportunity to choose between different meals – as all other people do.
Also, I hope that real-food tubefeeding in general will be recognised as an equal – and even better –opportunity for people with a feeding tube. Real food is for real people and should be a first choice.

It’s one thing to develop a product in a niche category with limited knowledge – and quite another to re-educate an entire industry.
bellyfood.dk @bellyfood.dk Bellyfood.dk

Why was blended real food the right option for your son, William?
William had very complex needs from birth but feeding was perhaps one of the most stressful. He failed to gain weight and was given an NG tube due to failure to thrive. His diagnosis was unclear and we were just trying to get through each day and meeting multiple specialists as his condition changed. For feeding, commercial formula through a pump was presented as the only option and, at the time, we did not think about questioning the medical team. When William was a baby,
formula felt quite natural – and we then moved on to a Ketogenic diet to try and manage his seizures.
As William reached an age where most children would be eating real food orally, I was unpacking boxes of formula and had a moment of realisation that I wouldn’t consider this okay for myself or anybody else as the only ‘food’ I had for every meal.
I then started researching alternatives, discovered the real-food blended diet and very soon after this, we started introducing real food as part of William’s diet.
At what point did you start to build your business, Wilbo’s Blends?
William really began to thrive when he started with real food and as a result, I became incredibly passionate about the blended diet and was meeting more people in similar situations. I also started to experience and understand the many barriers that existed to using a blended diet.
I started Wilbo’s Blends to increase the awareness, access and knowledge around the blended diet –although I was probably a little naive,
at the beginning. I didn’t realise just what a big undertaking it was to get Wilbo’s Blends from a concept to something that delivered material change to the people that mattered to me.
Launching our meals was a great moment, but there were plenty of times I didn’t think it would happen along the way. We are now involved in a number of projects working with clinicians, researchers and other medical industry professionals to continue to make real food a real alternative for enteral nutrition.
What are the biggest challenges you’ve come up against since launching into the enteral feeding market? The biggest challenge is change. While enteral feeding has not changed for 40 years, healthcare has changed dramatically. More patients are using enteral nutrition and for longer. Change in healthcare is slow and people are rightly cautious, but anecdotal evidence for the benefits of blended diets now has a lot of clinical research to support it.
We have seen professional bodies and healthcare institutions starting
William really began to thrive when he started with real food and as a result, I became incredibly passionate about the blended diet and was meeting more people in similar situations. I also started to experience and understand the many barriers that existed to using a blended diet.
to change their attitudes and policy toward a blended diet. This has removed much of the professional resistance as many myths have been dispelled.
We’re having more conversations on ‘how’, rather than ‘if’, blended diets should be used. There’s still a huge amount more to do – especially in adult services – but I’m optimistic for the future.
On that topic, what are your hopes for Wilbo's Blends? Our main priority right now is improving equity of access. We have been working for a long time on getting Wilbo’s Blends prescribed on the NHS [National Health Service] in the same way commercial formula is today, which would be a huge step forward, but we still have a long way to go here.
We have recently launched our dietetics services and I want to grow this and continue the work we do in training other dietitians and medical professionals. I would also love to do more research into the use of real food and how it can improve a wider group of people’s health and wellbeing in the future.
We have two new meals coming out very soon and I want to continue to expand the variety and create more options. We certainly have plenty to do!
wilbosblends.co.uk
@wilbosblends
Wilbo’s Blends

Sarah Thomas Founder of Wholesome Blends, AUSTRALIA
When did your son, Lewis, start a real-food blended diet? By the time Lewis got a permanent feeding tube at age nine – after having multiple NG tubes across six years and being told he would “grow out of his eating issues” – I had that lived experience. I was more empowered, as a medical mother and Lewis’s advocate, to push for what he needed.
I think if Lewis had had a permanent tube put in at three years old, when he had a stroke that impacted his eating, I would have done what I was told. But after all of those years, I couldn’t comprehend why Lewis and his identical twin brother, Cohan, needed a different diet.
Why did you go that next step – or giant leap – to creating a real-food blend product? When you have a child who is medically complex, you do whatever we can to improve things for them. I often say that I don't have a medical background, but I have a PhD in Lewis. And for me, that passion to create a natural product started selfishly – for my son – because he needed it.
I also knew that if Lewis needed this product, somebody else might too. And I really wanted the community to come along on this journey with us.
In the very early days of Wholesome Blends, I had a booth at a kid’s disability expo to see whether or not parents wanted a real-food blend in a pouch. I discovered that they very much did – but what I didn’t
expect was the flood of allied health professionals who kept contacting me after that expo saying, “when is it going to be ready?”
The big driver for me was – and will continue to be – that I don’t ever want anybody else to feel shamed, scared and threatened for putting real food through their child’s tube, like I was.
What are the biggest business challenges you’ve faced since launching Wholesome Blends?
The first major challenge was getting someone to make my products. When I would tell manufacturers that I wanted them to create a product that had never been made before –a food for special medical purposes with no need to focus on taste or smell – they couldn’t understand why someone would want to do that.
Because of the “medical” element, manufacturers felt the risks were too high and put it straight in the too-hard basket. I got 19 no’s and on the 19th one, I put my foot down and challenged it. When I was able to get face-to-face with that manufacturer and explained what I was trying to do, they understood and got on board. But it was trial and error for a long time.
Then came the challenges from the medical sector that, at the time, wanted to stop this kind of product being available in Australia. But I knew, as the end user myself, that the families had the power to make
that decision. My focus was on showing the community that I wasn’t a big pharmaceutical company just trying to make money – I was one of them and I was trying to help.

I am incredibly lucky, now, to have more support from tubefeeding families and people than I ever thought I would have in this business. Our community gives me the confidence to not doubt myself –and push for them.
What are your hopes for the future of Wholesome Blends? We’re very lucky to have the support of the NSW state health system. Wholesome Blends is a registered product on their enteral-feeding contract and we’re trying to secure more tenders across the country, within hospital settings and in the community with Home Enteral Nutrition (HEN) programs. We were also thrilled to win the 2024 Telstra Best of Business Awards for Accelerating Women in Queensland. We’re going to continue to advocate for the community and educate clinicians and, since launching our blended-feeds cookbook, Blended: Sharing Recipes for Love & Stories for Life, we’re working on more recipes. It’s all about sharing information and knowledge. We want tube-feeding families and people to be fully informed so they can have a choice about what they put in their bodies, with the full support of their medical teams.
My focus was on showing the community that I wasn’t a big pharmaceutical company just trying to make money –I was one of them and I was trying to help.
wholesomeblends.com.au
@wholesomeblendsau
wholesomeblend

This collection of recipes is brought to you by Blended: Sharing recipes for love & stories for life.

• 200g Greek yoghurt
• 50g Rolled oats, uncooked – ground
• 20g Medjool dates (pitted)
• 50g Avocado
• 50g Frozen mixed berries
• 170g Banana (frozen is fine)
• 50g Flaxseeds, ground
• 400ml Full cream milk
1. Add all ingredients in order to a blender
2. Blend on high until smooth and creamy
3. Adjust the milk if you’d like a thinner consistency and consume immediately
Total 1002g

• 700g Left-over food scraps, frozen
• 4-6 Chicken frames, organic, cooked
• 1/3 cup Olive oil
• 2 large Brown onions, with skins
• 4 medium Carrots
• 4 stalks Celery
• 700g Broccoli, heads and stalks
• 400g Pre-washed spinach
• Handful Sweet potato skins, cooked or uncooked
• 5 stalks Rosemary
• 1 bunch Thyme
• 1 bunch Parsley
• 2 tsp Salt
• 4 litres Water
• ½ cup Apple cider vinegar
1. Collect leftover greens and veggie scraps and put in freezer until needed for broth
2. Preheat oven to 220°C
3. Coat chicken frames in olive oil and roast in oven until golden
4. Add all veggies, herbs and salt to a large slow cooker
5. Add up to 4 litres of water to veggies and herbs
6. Add cooked chicken frames, including juices from the pan
7. Add apple cider vinegar
8. Replace lid and allow to cook on low for 12 to 24 hours (the longer, the better)
9. Once cooked, allow to cool
10. Strain cooled broth into a large bowl or jug
11. Portion into sealable plastic bags or freezerproof containers
12. Thaw and use as desired
Makes 3-4 litres, depending on cooking duration.

CURATED BY //
Beef mixture
• 15ml Olive oil
• 40g Red onion sliced
• ½ clove Garlic
• 350g Beef mince lean
• 1 tsp Taco seasoning
Sauce
• 180ml Passata
• ½ tsp Cumin, ground
• ½ tsp Coriander, ground
• ½ tsp Smoked paprika
• 80g Tortillas (approx. 4 small)
• 50g Cheese tasty, grated
• 5g Spring onion, raw, chopped
• 250ml Sarah’s Chicken Broth (for blending)
Beef Mixture
1. Preheat the oven to 180°C
2. Add half the olive oil to a large non-stick frying pan over low heat. Add the sliced red onions and stir for 1 minute. Then add the minced garlic and stir for another minute until combined
3. Increase the heat to high and add the beef mince, stirring regularly to break it up. Cook for 5–7 minutes or until the mince is cooked through
4. Sprinkle in the taco seasoning and cook for an additional 2 minutes, stirring to combine Remove the beef mixture from the pan, but leave any remaining oil in the pan.
Nutrition Information Average quantity per 100g
Sauce Mixture
1. In the same pan, add the rest of the olive oil and gently heat
2. Add the sliced red onions and garlic, cooking for about 2 minutes or until softened
3. Stir in the passata, cumin, coriander, and paprika. Let the sauce simmer for 4–5 minutes
Assembling the Enchiladas
1. Lightly spray an oven dish with olive oil
2. Take a tortilla and spoon a quarter of the beef mixture down the centre. Roll to enclose the filling, placing the seam side down in the dish
3. Repeat with the remaining tortillas and beef mixture
4. Pour the sauce mixture over the top of the tortillas and sprinkle with cheddar cheese
5. Bake in the oven for 15 minutes or until the cheese has melted and the enchiladas are heated through 6. Once cooked, remove from the oven and sprinkle with fresh coriander and spring onions
To Blend
For a blended consistency, add all ingredients to a blender but remove half of the tortilla shells. This will help maintain a consistent texture. Add more tortillas if you prefer a thicker blend.
Total 1005g or 4 single Enchiladas.

Ingredients
• 350g Cauliflower
• 180g Chickpeas
• 70ml Extra virgin olive oil
• 1 Clove garlic (crushed)
• 5g Smoked paprika
• 3g Cumin ground
• ½ tsp Chili powder
• 20 ml Lemon juice
• 20g Fresh coriander
• 100g Avocado
• 250 ml Sarah’s Chicken Broth
1. In an oven preheated to 220°C, toss cauliflower and chickpeas with olive oil, garlic, smoked paprika, cumin, chili powder and lemon juice. Roast for 20 minutes or until tender and lightly golden. Allow to cool
2. In a high-powered blender, add roasted ingredients including juices from pan, coriander, avocado, chicken broth. Blend until smooth and creamy
Makes 3-4 litres, depending on cooking duration.
Total 1000g
Nutrition Information Average quantity per 100g

• 15ml Peanut oil
• ½ Clove garlic, minced
• ½ tsp Turmeric powder
• 2 tbsp Laksa paste, store bought
• 300ml Sarah’s Chicken Broth
• 120ml Coconut cream
• 10ml Soy sauce
• 20g Bok choy, chopped
• 200g Udon noodles
• 250g Chicken breast, raw
• 1 large Boiled egg
• 5g Bean sprouts
• 5g Spring onion, chopped
• 10g Fresh coriander leaves, chopped
• 5ml Fresh lime juice
1. Prepare the Laksa base: Heat the peanut oil in a large pan over medium heat. Add the garlic, turmeric, and laksa paste. Sauté for about 1 minute until aromatic
2. Simmer the soup: Pour in the chicken broth, coconut cream and soy sauce. Bring the mixture to a boil, then reduce heat to low and simmer for 5 minutes
3. Prepare noodles: While the soup is simmering, cook the Udon noodles as per package instructions. Be careful not to overcook them, especially if using fresh noodles
4. Add vegetables: Add the bok choy to the soup, cooking for another 2 minutes
5. Gently add in pre-cooked Udon noodles, cooking for another 2 minutes. Stir in the lime juice just before removing from heat
6. Serve: Ladle the laksa into bowls and top with boiled egg, bean sprouts, spring onions and fresh coriander. Serve with a lime wedge on the side
Add required portion to blender and high powered blender and blend until desired viscosity is reached.
Remember, the longer the noodles are left in the laksa broth, they will absorb the liquid, so add more chicken broth if needed.
Serves 3, Total 1000g

• 20ml Olive oil
• 300g Pork loin, thinly sliced
• 30g Red onion
• 100g Cooked brown rice
• 30g Baby corn
• 50g Broccoli florets
• 30g Carrot, thinly sliced
• 40g Capsicum, thinly sliced
• 30g Snow peas, thinly sliced
• 1 tbsp Soy sauce
• 3 tbsp Hoisin sauce
• 15 ml Sesame oil (optional)
• 300 ml Sarah’s Chicken Broth to blend
1. Heat olive oil in a large pan over medium-high heat. Add the sliced pork and red onion and cook until browned, about 5–7 minutes
2. Remove the pork and set aside. In the same pan, add the brown rice, baby corn, broccoli, carrot, capsicum, snow peas, and until tender-crisp, about 3–4 minutes.
3. Add the pork back to the pan along with the soy sauce, hoisin sauce and sesame oil. Stir for another 2–3 minutes
4. Allow the mixture to cool slightly, then transfer to a blender with the coconut milk
Add required portion to high powered blender and blend until desired viscosity is reached.
Total 1004g or 3 serves
If you go down to the park today, you’re sure of a big surprise
If you go down to the park today, bring your tube-feeding supplies
For every kid with tubes and cheer, Will gather ’round to eat right here, Today’s the day the tubie gang has their picnic.
PHOTOGRAPHY // DEBI BRETT FOR TUBIE FUN AND AVANOS
blend.










We are an Australian owned and operated, award-winning family business celebrating a different way of feeding. Through walking the same journey with our tube-feeding child, we know first-hand the highs, lows and everything in between that this lifestyle brings. It’s our mission to provide the tube-feeding community with a wide range of high-quality products that are both fun and functional. We want to help children and adults who tube-feed feel confident and express their personalities –all while normalising this wonderful way of feeding.
tubiefun.com.au @tubiefunau Tubie Fun

Misti and Will Staley created a ‘helping hand’ for tube-feeding their son, Freeman. The FreeArm holds gravity syringe meals and pump meals to make eating at home, hospital or on-thego a breeze. The FreeArm bends up easily for travel, frees your hands, takes the place of an IV pole and is NDIS purchasable through Tubie Fun, Surgical House, InterMed Medical and more!
amslmedical.com.au/pages/freearm-muscle @freearm.tube.feeding.assistant FreeArm
Wonsie specialises in larger-sized cotton bodysuits for kids and adults. We are committed to providing quality, practical clothing solutions for people with a variety of needs and have a bodysuit range which is designed specifically to assist easy tube-feeding access. Our range also includes adaptive swimwear, incontinence aids and bedding protection. Our goal is to provide products which give peace of mind and help make daily life a little easier for all families. We offer worldwide shipping and are a registered NDIS provider.
wonsie.com.au @wonsie @WonsieKids



Wholesome Blends is Australia’s leading provider of blended whole-food options for tube-fed children and adults. Our nutritious, all-natural and high-calorie meals are shelfstable, meaning they don’t require refrigeration for storage. They’re free from dairy, soy, nuts, eggs, GMOs, added sugars, preservatives and additives. Made with love by a tubefeeding family for other tube-feeding families, Wholesome Blends offers four convenient varieties, making it easier for families to access a healthy, blended whole-food diet.
As the business grows, we’re thrilled to announce that Wholesome Blends will be evolving into Blended by Sarah, bringing even more passion and care to our products.
wholesomeblends.com.au @wholesomeblendsau Wholesome
Kate Farms believes that nutrition is the foundation of health
That’s why they created Pediatric Blended Meals: wellbalanced, nutrient-dense meals made with whole foods, pea protein, and vitamins and minerals. Pediatric Blended Meals provide you with less mess and no fuss compared to making blended meals at home and delivers plant-based nutrition. The resealable meals are made with similar care, love and attention that parents put into the meals they make at home. Pediatric Blended Meals are compatible with certain tube feeding adapters, allowing high-quality nutrition to flow smoothly through feeding tubes with little to no manipulation. Kate Farms products are only available in the United States. katefarms.com @katefarms @kate_farms

Abbott is a leading provider of home enteral nutrition. The Abbott Homecare Connect service is dedicated to ensuring a seamless transition from hospital to home for patients nationwide. Their highly skilled team of Clinical Nurse Educators delivers unparalleled care, prioritising safety, quality, reliability and connection. With a focus on patient wellbeing and dignity, Abbott Homecare Connect provides individuals with exceptional nursing support which empowers them to maintain their independence and confidence.
abbotthomecareconnect.com.au
Real Food Blends is a ready-to-feed, 100 percent real-food option for people with feeding tubes. Enjoy nutritional variety with eight different meals and one snack made with real protein sources, fruits, vegetables, whole grains and fat sources. Each pouch is made of five to eight ingredients, that’s it! Available in the US only.
realfoodblends.com
ENRICH is a nutritionally formulated meal replacement and the debut product of WHOLE Enteral, the business baby of tubie Mum, Ali Howell, and speech pathologist Dr Emily Lively. Plant-based, free from nuts, soy, dairy, eggs and gluten, ENRICH can be enjoyed by adults and children with a range of digestive challenges. Being ready-made, shelfstable and nutritionally balanced, ENRICH is perfect for home, holiday, school or hospital use.
whole.net.au @whole_en @whole.en
Functional Formularies offers organic, plant-based, whole food nutrition to those who need it most. Our adult and paediatric blenderised formulas are designed for tube feeding but can also be used as oral meal replacements. Each pouch is made with a variety of whole-food ingredients chosen for their unique ability to form a well-balanced, nutritionally optimised tube-feeding formula. Explore our range of formulas and experience the difference that high-quality, whole-food nutrition can make!


This widely used and loved bottle drying rack just happens to work a treat for syringes and other bits of tube-feeding kit. You can buy the Boon Grass Drying Rack from several retailers. Helpful hack: Dry your syringes tip-down on this one.

Created by Sarah Thomas, the founder of Australia’s beloved Wholesome Blends products, Blended is a celebration of family, flavour and health. As Wholesome Blends evolves into Blended by Sarah, this cookbook reflects Sarah’s continued passion for nourishing meals that bring people together. Inside, you’ll find Sarah’s personal favourites, expert contributions from dietitians and chefs and treasured family recipes. With tips, tricks and heartwarming stories, Blended makes it easy to enjoy the joy of home blending while celebrating the love and connection that food brings to our lives.
wholesomeblends.com.au @wholesomeblendsau @wholesomeblend
If you’re new to blenderised tube-feeding and aren’t sure where to start, this ebook is for you! Inside this offering from Hilarie Geurink you’ll find 18 dietitian-created, high-calorie recipes with directions for how to easily swap out your formula for these nutritious, blended meals. You’ll also find lots of helpful advice on how to prepare, store and consume the blended meals.
blendedtubefeeding.com

This comprehensive book from dietitian Lina Breik adopts a reader-friendly approach by demystifying nutrition jargon and presenting tube-feeding in an accessible manner. Its goal is to bridge the gap between you and your feeding tube, empowering you to understand and discuss your nutritional needs effectively with your care team. tubedietitian.com
TubeDietitian
Dietitian Claire Kariya shares 20 tried-and-tested blended meal recipes, each with their own nutritional information, in this photo-filled, downloadable ebook.
naturaltubefeeding.com @naturaltubefeeding @naturaltubefeeding
Easy
Swallow: Transitioning off a PEG tube back to oral
This recipe book is the work of trained chef and head and neck cancer survivor Yvonne McClaren, who you can meet in Issue One of The Blend.
yvonnemcclaren.com
@yvonnegracemcclaren
@nofeedingtubes
Written by medical mama Gemma Keir, this kids’ picture book follows the story of a young girl, inspired by the UK’s Chanel Murrish, who’s had an NG, PEG and MIC-KEY button.
theabilitiesinme.com
@theabilitiesinmebookseries
@theabilitiesinmebookseries


The Blend magazine is an independent publication
Founder and editor Melanie Dimmitt melaniedimmitt.com.au
Creative director Edith Olsen
Published by Printcraft Pty Ltd Legal stuff
No part of this publication may be reproduced by any means without prior written permission of the editor. Views expressed within The Blend magazine are not necessarily those of the editor.
theblendmag.com