PROJECT SUMMARIES


Quality Improvement Lead (QIL) Program 2021-2023
© The Australian Council on Healthcare Standards
Apart from any use as permitted under the Copyright ACT 1968, no part may be reproduced by any process without prior written permission from the Australian Council on Healthcare Standards.
Quality Improvement Lead (QIL) Program Project Summaries 2021-2023
ISBN: 978-1-875544-66-0 (E-book)
This booklet is available in PDF format via the ACHS website: www.achs.org.au
For enquiries, please contact us at:
The Australian Council on Healthcare Standards
5 Macarthur Street
Ultimo NSW Australia 2007
T. 61 2 9281 9955
E. achs@achs.org.au

This page has intentionally been left blank.

Project Summaries 2021-2023 | Table of contents | ©ACHS Improvement Academy Contents ACKNOWLEDGEMENT 1 FOREWORD 2 INTRODUCTION: QUALITY IMPROVEMENT LEAD (QIL) TRAINING PROGRAM ······················ 3 GRADUATION CEREMONY PHOTOS 4 PROJECT CATEGORY: ACUTE HEALTH CARE IMPROVING THE EXPERIENCE OF TELERHEUMATOLOGY IN CENTRAL ADELAIDE LOCAL HEALTH NETWORK ································ ································ ································ ························ 5 Ms Leah McWilliams, Dr Oscar Russell and Professor Susanna Proudman INTRODUCING DIABETES FOOT ASSESSMENTS ON COUNTRY ································ ··············· 7 Ms Fiona Miles REDUCING THE TIME TO ANTIBIOTIC ADMINISTRATION IN ADULT PATIENTS WITH SEPSIS IN THE EMERGENCY TELEHEALTH SERVICE 10 Mrs Sallie Walsh, Dr Bradley Wibrow and Dr Justin Yeung SEPSIS RECOGNITION: A PROBLEM WORTH SOLVING 12 Ms Kirsten Thompson STOP THE CLOT: ASSESSING VENOUS THROMBOEMBOLISM RISK FROM THE EMERGENCY DEPARTMENT TO THE FRACTURE CLINIC ································ ································ ·················· 14 Miss Laura Lincoln PROJECT CATEGORY: COMMUNITY REDUCING WORK-RELATED MUSCULOSKELETAL INJURIE S IN THE NT HEALTH ALICE SPRINGS COMMUNITY PRIMARY CARE ADULT NURSING TEAM ································ ············ 17 Ms Anna Huigen PROJECT CATEGORY: DRUG AND ALCOHOL SERVICES TOP END ALCOHOL AND OTHER DRUGS COMMUNITY LINK PROJECT 20 Ms Ingrid Herbert

Project Summaries 2021-2023 | Table of contents | ©ACHS Improvement Academy PROJECT CATEGORY: PARTNERING WITH CONSUMERS CONSUMER FEEDBACK: NOT MEETING THE EXPECTATIONS OF ANYONE 23 Ms Kathy Kinrade JOURNEY MAPPING PATIENT EXPERIENCE: EMERGENCY CAESAREAN SECTIONS 26 Mrs Natalie Benn SAME-DAY REHABILITATION REFORM 29 Mrs Kera Fulurija WORKING WITH INTERPRETERS IN THE HEART OF AUSTRALIA 32 Ms Alison Thorn PROJECT CATEGORY: REHABILITATION HEART YEARNING 2022: IMPROVING THE ACUTE CORONARY SYNDROME PATIENT CARDIAC REHABILITATION JOURNEY ································ ································ ························ 35 Mrs Justine Williams PROJECT CATEGORY: SYSTEMS IMPROVING OPEN DISCLOSURE DOCUMENTATION 38 Ms Jo Muir, Ms Kim Walters and Ms Nicky Cheeseman OUR DATA DRIVES OUR CARE 41 Ms Lucy Lehane REDESIGN OF THE CLINICAL INCIDENT REVIEW PROCESS FOR YORKE AND NORTHERN LOCAL HEALTH NETWORK TO BETTER ALIGN W ITH THE INTENT OF CLINICAL GOVERNANCE STANDARD 1 44 Miss Fiona Murray STANDARDISING THE CLINICAL AUDIT PROCESS IN THE TOP END, BIG RIVERS AND EAST ARNHEM REGIONS ································ ································ ································ ······················· 46 Ms Ali Walker SUCCESSION PLANNING: IMPROVE WORKFORCE CAPABILITY AND FLEXIBILITY ··············· 49 Ms Tina Lloyd and Dr Karen Pedersen
Acknowledgement
The Improvement Academy would like to acknowledge the contribution of the following Faculty members who contributed to the success of these programs and the resulting projects contained in this booklet:
Australian Expert Faculty
Associate Professor Bernie Harrison – Director, ACHS Improvement Academy, NSW
Dr Cathy Balding – Managing Director, Qualityworks PL, VIC
Ms Helen Ganley – Principal, Data Sanity, NSW

Associate Professor Peter Hibbert – Program Manager, Australian Institute of Health Innovation, Faculty of Medicine Macquarie University, NSW
Ms Lucy Lehane
Clinical Educator, ACHS Improvement Academy, NSW
Mr Anothony Lock , DSM - Executive Director, Clinical Performance & Systems – St John (Ambulance) WA
Ms Shelley Thomson - Director, Experience 360, ACT
International Expert via video
Dr Brent James – Clinical Professor (Affiliated), Dept of Medicine, Stanford University School of Medicine, United States
We have all these tools available to us but this course brings together the most relevant ones to use in health and teach you how to use them successfully with confidence. Thank you so very much.
Ali Walker, CNC Monitoring and Compliance QIL Program Participant
Project Summaries 2021-2023 | Page 1 | ©ACHS Improvement Academy
–
Foreword

It gives me great pleasure to introduce the fourth edition of the ACHS Quality Improvement Lead (QIL) Training Program Project Summaries publication. This booklet includes an array of projects from QIL participants, conducted between 2021 and 2023.
These project summaries represent the focus and passion healthcare organisations have on improving their services for clients and patients across Australia. It is wonderful to be part of such important healthcare initiatives and support our QIL participants in their quality improvement journey.
This booklet provides a valuable resource for knowledge sharing amongst our community, providing real-life experiences other healthcare professionals can learn from. Our hope is that inspiration will be formed from these positive projects and empower change across the Australian healthcare system.
Special thanks go to all QIL participants who contributed to this publication and the ACHS Improvement Academy for their dedication to this course and supporting the participants.
We trust that you enjoy reading these Project Summaries and gather insights for ongoing quality improvement.
 Dr Karen Luxford ACHS Chief Executive Officer
Dr Karen Luxford ACHS Chief Executive Officer
Project Summaries 2021-2023 | Page 2 | ©ACHS Improvement Academy
Introduction: Quality Improvement Lead (QIL) Training Program


The ACHS Improvement Academy team believe that championing quality improvement is key to improving healthcare outcomes. Quality Improvement is all about raising the bar in patient care using innovative strategies and patient-centric methodology. Our educational training goes beyond conventional approaches to focus on empowering all clinical and non-clinical executives, managers and staff working in quality improvement.
Our Quality Improvement Lead (QIL) Program is an advanced program for leaders of improvement. This comprehensive, flagship training is a nine-month program, providing a deep immersion in improvement science, reliability science, transformative leadership for improvement and clinical governance for improvement. Led by our expert Faculty, the QIL Program helps participants gain confidence navigating a rapidly changing healthcare landscape.
This Project Summaries booklet contains some remarkable projects undertaken as part of the QIL Program from 2021 to 2023. A great diversity of healthcare settings is represented including remote areas in NT and WA, primary health care, health departments and large teaching hospitals in Australian cities. The projects represented, are at varying stages of completion, but what they have in common is a focus on improving care for health consumers across the system.
Since 2016, more than 602 dedicated participants have completed the QIL Program and have sought to bring a sustainable change to their lead role. Congratulations to all who have participated in the course, we acknowledge your achievements with this publication, and we thank your managers who provided support and sponsorship to join the program.
Thanks, must also go to our predominantly Australian-based Faculty who are recognised internationally as experts in the field of quality and safety, combining both practical experience and publication in academic literature.
We strongly encourage all readers to share the outcomes of these projects with your colleagues.
If you would like more information about any of the Improvement Academy’s programs and events, please visit our website: www.achs.org.au/improvement-academy/
Assoc Professor Bernie Harrison Director, ACHS Improvement Academy
Project Summaries 2021-2023 | Page 3 | ©ACHS Improvement Academy
Graduation Ceremony Photos








Project Summaries 2021-2023 | Page 4 | ©ACHS Improvement Academy
QIL Ceremony 2021
Virtual
Virtual QIL Ceremony 2022 Virtual QIL Ceremony 2023
Improving the experience of telerheumatology in Central Adelaide Local Health Network
Ms Leah McWilliams, Dr Oscar Russell and Professor Susanna Proudman
Problem/Aim s
The rapid uptake of telehealth in rheumatology clinics in response to the SARS-CoV-2 pandemic has highlighted both the benefits as well as the short-comings of this modality, especially by telephone, for patients, clinicians and outpatient administration staff. In our service, video consultation was employed infrequently.
Ms Leah McWilliams Nurse Practitioner Rheumatology Department
The aim of this project was to increase the uptake of video consultation for patients with rheumatoid arthritis, and to improve the experience of telehealth appointments for all stakeholders.
Measurement
Dr Oscar Russell Consultant Rheumatologist Rheumatology Department

A team comprising a consultant, advanced trainee and nurse practitioner from Central Adelaide Local Health Network (CALHN) rheumatology units, with support from CALHN outpatient staff, process-mapped all the stages of telehealth consultations. We surveyed clinicians and patients with contact with the Royal Adelaide Hospital and Queen Elizabeth Hospital CALHN rheumatology outpatient clinics from the beginning of 2020 to gain insight to their experience of barriers and enablers of telehealth. Suggestions for improvement, including indications for use of telehealth, were sought from patients, clinicians and outpatient staff.
Design
Ideas that have been included in a new model for telehealth for rheumatoid arthritis include:
Professor Susanna Proudman Director Rheumatology Department


1. criteria for the use of telehealth (stable disease, poor mobility, rural and remote location, provision of prescriptions);
2. modifying the use of the video software with greater input from administrative staff; and

Project Summaries 2021-2023 | Page 5 | ©ACHS Improvement Academy Projectcategory:AcuteHealthCare
The Royal Adelaide Hospital, South Australia
The Queen Elizabeth Hospital, South Australia
The Royal Adelaide Hospital, South Australia
3. a new platform for communicating with patients about their appointment and providing resources for troubleshooting and for managing rheumatoid arthritis
Strategy
After testing the new model with patient focus groups, the next stage will be to implement the model in CALHN rheumatology clinics. The proportion of consultations delivered by video will be measured and patients and clinicians

surveyed about their experiences of video consultation. Further ‘Plan, Do, Study, Act’ cycles will be employed to modify the model to ensure improvement in the number and experience of video consultations for rheumatoid arthritis

Conclusion
The model could then be modified for other rheumatic diseases and rolled out more widely across CALHN rheumatology.
At the time of publishing this booklet, the project was ongoing.
Project Summaries 2021-2023 | Page 6 | ©ACHS Improvement Academy
Figure 1. Driver Diagram
No pt prep. for appt.
Introducing diabetes foot assessments on Country
Ms Fiona Miles
Problem/Aims
The Gove District Hospital (GDH) services over 14,000 people1 and has no visiting podiatry or foot assessments on campus, often resulting in poor outcomes for clients with diabetes in this remote community.
 Ms Fiona Miles
A/Safety and Quality NMC Nursing Department Gove District Hospital Northern Territory Health
Ms Fiona Miles
A/Safety and Quality NMC Nursing Department Gove District Hospital Northern Territory Health
This project aimed to introduce a foot assessment to all patients admitted with diabetes complications or those with diabetes and a lower limb wound within 48 hours of admission.
Background
A Darwin study found a 25% mortality rate at five years for diabetic foot ulcers2, and in Central Australia, 60% of Indigenous participants reported foot pain, of which 70% were untreated3. In East Arnhem, diabetes complications are listed as the fourth most preventable reason for hospital admissions1. Another study found that 84% of lower limb amputation patients identified as Aboriginal Australians4

Measurement
Interviews with patients revealed dissatisfaction with a service at GDH not being available, and patients revealed being advised to see a podiatrist while on holidays. Sessions with clinicians revealed that none were performing basic foot checks. GDH did not have equipment for this task
Project Summaries 2021-2023 | Page 7 | ©ACHS Improvement Academy Projectcategory:AcuteHealthCare
Design
A large part of this project was to design a userfriendly assessment form. Three forms were distributed to clinicians for feedback. Input was sought from senior podiatrists. Physical and visual assessments alone needed to provide enough information for risk rating to allow for times when an interpreter was unavailable. Keeping the form to one page was also vital to improve acceptability


Strategy
The form was trialled on four occasions and minor changes were made each time. One of these was making all the ‘yes’ answers red flags so that a glance down the line would elicit this information.

Results
Initially, data collection relied on manual entry; however, the recently introduced electronic clinical information management system will capture this data when assessments move from paper to electronic. After full implementation, the numbers of patients with diabetes admitted will be compared to the number of diabetic foot assessments performed. Regular in-service training is now in place for all clinical staff to improve uptake. Checking admissions and assisting with foot assessments is occurring, and doctors are now asking for their patients to be assessed.

Project Summaries 2021-2023 | Page 8 | ©ACHS Improvement Academy
Figure 1. Diagnostics, Cause and Effect Diagram
Figure 2: Intervention
Conclusion
Diabetic foot checks are now available at GDH, however not every patient who meets the criteria is receiving one yet. The high turnover of clinicians has affected the uptake of this service, and other competing projects have severely reduced education opportunities.

Plans for next steps
Referrals created under this program will now form part of the business case to obtain a visiting podiatry service for GDH
References
1. NT Primary Health Network, Rural Workforce Agency NT. East Arnhem Region data report: Overview of selected demographic and health data for the East Arnhem region of the Northern Territory. 2020. https://www.ntphn.org.au/wpcontent/uploads/2021/06/East-ArnhemRegional-Data-Profile_FINAL.pdf
2. Jeyaraman K, Berhane T, et al. Mortality in patients with diabetic foot ulcer: A retrospective study of 513 cases from a single centre in the Northern Territory of Australia. BMC Endocr Disord 2019;19(1): https://doi.org/10.1186/s12902-018-03272
3. Sadler S, Gerrard J, et al. Aboriginal and Torres Strait Islander peoples’ perceptions of foot and lower limb health: A systematic review. J Foot Ankle Res. 2022;15(1): https://doi.org/10.1186/s13047-02200557-0
4. Stuart L, Kimmel L, et al. Incidence of lower limb amputation in Central Australia. Aust Health Rev 2021;45(3). https://doi.org/10.1071/ah20182
Project Team
Mary-Clare Arkcoll, Cara McLoughlin, Olivia Kehoe, Genevieve Stawarz, Tania Whight, Sally Lamond, Simone Tribe, Tamara Jubb, Eliza Graham, Ryan Bonnefin, Hillary Bloomfield.
Project Summaries 2021-2023 | Page 9 | ©ACHS Improvement Academy
Reducing the time to antibiotic administration in adult patients with sepsis in the Emergency Telehealth Service
Problem/Aims
Sallie Walsh Quality and Performance Coordinator Command Centre WA Country Health Service

In 2019/2020, Western Australia Country Health Service (WACHS) had six Severity Assessment Code 1 (SAC 1) cases related to delayed recognition of sepsis, including two deaths. This year, a death of a child in Perth from sepsis prompted a system-wide review of sepsis management.
The aim of this quality improvement project is to have 100% of adult patients referred to the Emergency Telehealth Service (ETS) after being diagnosed with sepsis to receive antibiotics within 60 minutes of presentation. The ETS is a specialist-led 24/7 virtual emergency medicine service which covers 86 rural hospitals, mostly without medical practitioners onsite, in Western Australia.
Background
Bradley Wibrow ICU Lead WA Country Health Service


Delays in recognition and administration of antibiotics are associated with increased mortality, whereas sepsis bundles, particularly where time to antibiotics being given is improved, are associated with improved mortality. WACHS introduced an adult sepsis pathway including the quick Sepsis Related Organ Failure Assessment (qSOFA) screening tool (pulse rate, respiratory rate and conscious state) in 2018, and uptake has been variable.
 Justin Yeung Medical Director Command Centre WA Country Health Service
Justin Yeung Medical Director Command Centre WA Country Health Service
Measurement
We audited charts from 74 patients referred to the ETS from April 2020 to May 2021 who had diagnoses of sepsis, septicaemia, or septic shock. Despite qSOFA being positive in 49% of patients, there was no evidence of this being documented by the site nurses or ETS clinicians.
Project Summaries 2021-2023 | Page 10 | ©ACHS Improvement Academy
Projectcategory:AcuteHealthCare
Mrs Sallie Walsh, Dr Bradley Wibrow and Dr Justin Yeung
Mrs
Dr
Dr
There was no documented evidence of the sepsis pathway being used. The average time to antibiotics after emergency presentation was 92 minutes (62 minutes post-referral to ETS).
Design
A survey sent to all WACHS staff identified confusion around who starts the sepsis pathway, lack of knowledge of the pathway and requests for more education. We processmapped all stages from the patient presenting, referral to ETS, to administration of antibiotics. We then facilitated virtual workshops to determine the primary drivers and brainstorm potential solutions.

Strategy
Strategies have been stratified into high priority, including mandating calculation of qSOFA at triage points; a sepsis stamp on triage documents and a poster to highlight sepsis; education (recording tutorials); and ensuring all referral sites have iSTAT point of care blood machines for lactate measurement and training. Medium priority changes include amended triage documentation; a qSOFA policy document; creating a new streamlined adult and paediatric pathway; and provision of case example newsletters. Lower priority changes including a mandatory annual sepsis module and computer program prompts.
Conclusion
A thorough diagnostic phase has enabled the team to identify strategies which target the key drivers for delayed recognition and treatment of sepsis among adult patients referred to the ETS after being diagnosed with sepsis.
Plans for next steps
We seek to implement these changes, starting with those identified as high priority. Audits will then be repeated, and staff engagement sought to evaluate the utilisation of the pathway and qSOFA measurements
At the time of publishing this booklet, the project was ongoing.

Project Summaries 2021-2023 | Page 11 | ©ACHS Improvement Academy
Figure 1. Pareto Chart
Projectcategory:AcuteHealthCare
Sepsis recognition: A problem worth solving
Ms Kirsten Thompson
Problem/Aims
Despite the implementation of NT-wide sepsis pathways, our health services continue to have gaps in the sepsis knowledge and skills required to detect sepsis on presentation to their emergency departments (EDs).
Ms Kirsten Thompson Sepsis Nurse Management Consultant Clinical Excellence and Patient Safety Northern Territory (NT) Health

This project aims to improve the recognition of sepsis at triage, and subsequent appropriate allocation of Australasian Triage Scale (ATS) 2, to a minimum of 85% of the time for all patients with sepsis presenting to Hospital X ED triage by December 2022.

Background
Sepsis is a medical emergency, and if not recognised early, leads to delayed management and increased risk of patient morbidity and mortality.
Measurement
Utilising quality improvement methods, including brainstorming, the project team identified several barriers to early sepsis recognition specific to the hospital ED. Analysis with cause-and-effect and Pareto charts enabled the team to identify contributing factors and common themes, and then prioritise what processes needed improvement.
Design
Process mapping and a driver diagram were useful for specifying the important drivers and concepts for change and how these would be implemented. This included ongoing focused clinical education for triage nurses and ED clinicians using various modalities; improvements to the triage process by taking a full set of vital signs as part of the triage assessment and commencing the sepsis pathway as indicated; and utilising ongoing evaluation to monitor compliance with the new triage process.
Project Summaries 2021-2023 | Page 12 | ©ACHS Improvement Academy
Results
Pre-intervention auditing of patients presenting with sepsis to the hospital ED in October 2021 revealed 57% of patients were allocated an appropriate ATS at triage. The ATS 2 allocation average was 54% at the start of 2022 (February to June) and increased to 82% in the second half of the year (July to November). Updated data to the end of January 2023 shows ATS 2 allocation is consistently on target between 85% to 100%, with an average now of 88% (July 2022 to January 2023).
Conclusion
Focused education, including simulation training for triage nurses and ED clinicians, has shown a positive impact. To sustain improvements from this project, the hospital ED will need to embed ongoing education and compliance monitoring into practice.

Plans for next steps

This evidence of successful improvements in sepsis recognition will help support its application in other EDs across the Northern Territory.
Project Team
Shannon Corbishley, CNE (KH)
Kayla Pontifex, CNE (sepsis portfolio)
Dylan Bradbury, CNM ED
Aruna Shivam, FACEM
Victoria Owen, ED RN
Executive sponsor, Mish Hill, CNMO, NT Health.
Project Summaries 2021-2023 | Page 13 | ©ACHS Improvement Academy
Figure 1. Diagnostics, Cause and Effect Diagram – Sepsis Recognition
Stop the clot: Assessing venous thromboembolism risk from the Emergency Department to the Fracture Clinic
Miss Laura Lincoln
Problem/Aims
Miss Laura Lincoln
Patient Reported Measures Manager
Patient Safety Quality and Excellence
St Vincent’s Health Network, Sydney
The identified problem was the significant variation and lack of standardisation in the documentation of venous thromboembolism risk assessments in the emergency department (ED). Practice did not meet Ministry of Health policy requirements or align with the Framework for Venous Thromboembolism Prevention and/or the Venous Thromboembolism Clinical Care Standard.
The aim of this project was for 100% of patients who presented to the ED with a lower limb injury and were unable to fully weight-bear to have a documented venous thromboembolism risk assessment in their medical record on admission within 12 months.

Background
In March 2021 following a serious adverse event review, a recommendation was given for a multidisciplinary team to review and map out the outpatient’s fracture journey from the ED to the fracture clinic. Combining this with our Ministry of Health requirements and the general desire from staff to have standardised practice in venous thromboembolism risk screening and management, a multidisciplinary group was formed to review the process and implement a change to improve patient safety.
Measurement
Data was collected on risk assessment completion weekly and fed back to clinical teams monthly to understand challenges and successes. The team then progressed through

Project Summaries 2021-2023 | Page 14 | ©ACHS Improvement Academy
Projectcategory:AcuteHealthCare
the cycle depending on what the initial data showed and gave directions on where the team should focus
Design
A series of diagnostics were completed to understand the problems, issues, challenges and barriers to documenting a venous thromboembolism risk assessment in the ED. This was complimented by patient feedback in understanding the ED to fracture clinic journey. A Modified Venous Thromboembolism Risk Assessment Tool was developed.
Strategy
The Tool was augmented with a venous thromboembolism education campaign for
staff, a one page information sheet for patients and amendment of local policy to define roles and responsibilities for venous thromboembolism risk assessment.

Results
The modified simple paper-based venous thromboembolism risk assessment has been adopted for use in the ED. It is currently used as part of standard practice within ED.
At the time of writing this report, audit results of documentation of venous thromboembolism risk assessment were not available.

Project Summaries 2021-2023 | Page 15 | ©ACHS Improvement Academy
Figure 1: Process Map
Conclusion
The development of a simple paper-based venous thromboembolism risk assessment combined with an education campaign for staff, information for patients and more clearly defined roles and responsibilities for venous thromboembolism risk assessment have standardised practice in venous thromboembolism risk screening and management within ED.
Plans for next steps
Documentation of venous thromboembolism risk assessment for patients who present to the ED with a lower limb injury and are unable to fully weight-bear will be monitored as part of the regular audit program.

Project Summaries 2021-2023 | Page 16 | ©ACHS Improvement Academy
Projectcategory:Community
Reducing work-related musculoskeletal injuries in the NT Health Alice Springs Community

Primary Care Adult Nursing Team
Ms Anna Huigen
Problem/Aims
The aim of this project was to reduce musculoskeletal injuries in the NT Health Alice Springs Community Primary Care Adult Nursing team staff during home visits and clinic appointments to zero by the end of November 2022.
Ms Anna Huigen RN
Nurse Management Coordinator
Urban Primary and Public Health Care
Northern Territory Health Central Australia and Barkly
The team comprises four permanent nurses and 2–3 casual nurses and provides wound care to clients in the clinic and home settings in Alice Springs. Both settings pose risk for musculoskeletal injury to nursing staff through twisting, lifting, bending, kneeling, pulling, pushing and carrying movements, particularly when attending to wound care in clients’ homes.
Background
NT WorkSafe1 reported that by health sector occupation, registered nurses accounted for 19.4% of serious injuries, with body stresses accounting for 21.8% of the main mechanism of serious injury. Lower back and shoulder injuries were the main body parts affected. Apart from high compensation costs and loss of client servicing due to lost workdays, Richardson et al.2 found that musculoskeletal injuries sustained by nurses in the workplace cause negative effects on ‘nurse wellbeing, quality of life, and job satisfaction’ and contributed ‘to difficulties with the retention of nurses in the workforce’.
Measurement
Riskman is the NT Health tool used to record, address, and evaluate quality and safety breaches. The number of Riskman nursing staff

Project Summaries 2021-2023 | Page 17 | ©ACHS Improvement Academy
incidents of musculoskeletal injuries for the past year was tallied (n=1). Staff absenteeism due to musculoskeletal injury was also recorded in days (n=5). However, a staff survey highlighted that all nursing staff in the team (n=5) had sustained a work-related musculoskeletal injury in recent years but had not formally lodged a Riskman incident or necessarily taken leave to recover but still had suffered pain and inconvenience as a result. Anecdotally, this had led to some staff considering other employment options.
Design
Beginning in April 2022, the project team used quality tools including brainstorming, affinity diagrams using Mentimeter, and sticky notes
and a staff survey that resulted in a cause-andeffect diagram and Pareto chart. Four interventions were identified, and a driver diagram (Figure 1) was created to assist with stating the changes likely to produce the desired effects. Coincidentally, the proposed interventions correlated strongly with themes identified by Rogers et al.3, who addressed musculoskeletal injury in the hospital setting.

1. implement regular morning stretching sessions for nursing staff
2. educate staff on correct work health and safety processes specific to the workplace
3. purchase of fully electric beds and home visit ergonomic aids
4. ensure adequate staffing to complete tasks without undue pressure.

Strategy
The interventions were tested in multiple Plan, Do, Study, Act (PDSA) cycles starting in April 2022 and entered into Riskman to ensure continuity and accountability. Two PDSA cycles (1 & 4) have been completed and two cycles (2 & 3) are still in process.
Results
Since commencing the project, the aim of reducing work-related musculoskeletal injuries to zero has been achieved. The number of days since the last workplace-related musculoskeletal injury (occurred 25/03/2022) is 497 (as of 20/07/2023).
Project Summaries 2021-2023 | Page 18 | ©ACHS Improvement Academy
Figure 1. Driver Diagram
Conclusion
Given the small data set and multiple interventions, it is difficult to conclude if one intervention was more effective than another, if multiple interventions worked in combination, or if it was the fact that the project caused nursing staff to place their safety ‘front of mind’ and increase their mental and physical considerations when engaged with direct client wound care.
Plans for next steps
Given the successful outcome to date, the interventions will be embedded into normal daily nursing practice wherever possible, and we plan to complete the remaining PDSA cycles over 2023.

References
1. NT WorkSafe. 2020-21 Work health and safety statistics: Health and community services. 2022. Available from: https://worksafe.nt.gov.au/forms-andresources/statistics/2020-21-work-healthand-safety-statistics-health-andcommunity-services
2. Richardson A, McNoe B, et al. Interventions to prevent and reduce the impact of musculoskeletal injuries among nurses: A systematic review. Int J Nurs Stud. 2018;82:58–67.
3. Rogers B, Buckheit K, et al. Ergonomics and nursing in hospital environments. Workplace Health Saf. 2013;61: 429–439.
Project Team
Janet Coyne, RN (team leader); Renee Staszczak, RN; Sarah Nungirayi, RN; Katie Harder, RN; Meng-Po Tsai, RN

Guidance Team
Kevin Orrell, UPPHC District Manager; Emma Corcoran, Clinical Nurse Consultant, Quality Improvement.
Project Summaries 2021-2023 | Page 19 | ©ACHS Improvement Academy
Top End alcohol and other drugs Community Link Project
Ms Ingrid Herbert
Problem/Aims
Ms Ingrid Herbert Clinical Nurse Manager Alcohol and Other Drugs (AOD) Withdrawal and Inpatients Services Top End Mental Health and AOD Services

Nearly 20% of the annual admissions to Royal Darwin, Palmerston Hospitals (RDPH) emergency departments (Eds) reported recent alcohol use, intoxication, and alcohol-related harms. Between 2020 and 2021, the top 10 frequent attenders presented with severe alcohol dependence and complex psychosocial needs1. This cohort often have high rates of nonadherence with discharge planning, high rates of ‘take own leave’ or ‘discharge against medical advice’, resulting in suboptimal care and worsening of pre-existing medical conditions.
The aim of this project is to reduce crisis presentations to healthcare facilities by 10% within 12 months for clients admitted under the Community Link Project, and to create an alternate model of care through the provision of integrated case management between AOD services, Mission Australia, Larrakia Nation and Primary Health Services.
Background
Since the 1980s the Northern Territory has had the highest levels of alcohol consumption per capita and the highest rates of hospitalisation and deaths due to alcohol misuse in Australia2
Approximately 48% of adults in the Northern Territory exceed the National Health Medical Research Council guidelines related to alcohol consumption, with consumption rates 173% greater than the national average3.
Measurement
During the evaluation phase, participants will be asked to complete an interview at the end of their stay, or earlier if they leave the program. Other data to be collected include:
• total number of participants
• duration of stay
• progression to ongoing treatment

Project Summaries 2021-2023 | Page 20 | ©ACHS Improvement Academy
Projectcategory:DrugandAlcoholServices
• impact of the project on the consumer’s substance use

• number of ED presentations in the 12 months before accessing the project and 12 months post-project.
Design
The project team identified staffing, the physical environment, assessment tools, risk assessment and interventions and systematic processes as important considerations for the success of the project (Figure 1). Some of the main issues identified were:

• The usual three-month rehabilitation program was felt to be too long by patients, so a shortened length of stay of one month was set.
• A more rapid admission process was identified as important by clients, and the decision to utilise a local non-government organisation admission paperwork was made.
• Lack of clinical staff in residential rehabilitation made managing clients with complex medical and psychosocial needs more difficult.
• Full attendance to rehabilitation programs is usually mandatory; however, flexibility was needed for this cohort to fit with their other frequent medical appointments.
Organisational Expectations
Strategy
Inclusion criteria for the project include those who:
• present frequently to RDPH with AODrelated issues
• request an initial one-month stay in a residential rehabilitation facility
• have complex psychiatric needs and substance use disorders
• have complex medical needs impairing their ability to complete residential rehabilitation programs
• with cognitive issues affecting participation in rehabilitation programs.
During August 2022 and February 2023, 13
clients were assessed as meeting the inclusion criteria; all identified as Aboriginal or Torres Strait Islanders. Among these, 92.3% (12) identified as homeless and 84.6% (11) were diagnosed with chronic medical conditions requiring ongoing treatment; 15.3% (2) took own leave or were discharged against medical advice without medical follow-up. 61.5% (8) clients declined the community liaison bed and 15.3% (2) progressed to admission.
Clients will transition from either the hospital or the AOD detox unit into a medium-term rehabilitation bed for up to one month, and during this time they will be supported by AOD services through regular medical reviews and integrated case management.
Project Summaries 2021-2023 | Page 21 | ©ACHS Improvement Academy
Figure 1. Cause and Effect Diagram
Results
This project is ongoing and evaluation results are unavailable.

Conclusion
Plans involve continuing to pilot the project. This project will not be without its challenges, given the complexity and extensive physical, mental, and psychosocial needs of this cohort.
References
1. Clifford S, Smith JA, et al. A historical overview of legislated alcohol policy in the Northern Territory of Australia: 1979–2021. BMC Public Health. 2021 Oct 23;21(1)
2. Stephens D, Clifford S, et al. Demand Study for Alcohol Treatment Services in the Northern Territory [Internet]. Darwin: Menzies School of Health Research; 2019. Available from: https://www.menzies.edu.au/icms_docs/30451
5_Demand_Study_for_Alcohol_Treatment_Servi ces_in_the_Northern_Territory
3. Northern Territory Primary Health Network; [cited 2023 Aug 9]. Available from: https://www.ntphn.org.au/programs/alcoholand-other-drugs/
Acknowledgements
AOD Community Link
Project Team
Jeffery Lyons, Aboriginal liaison officer; Zoe Fisher, nurse practitioner candidate; Dr Christine Watson, addiction specialist.
L-R: Jeffery Lyons, Aboriginal Liaison Officer; Zoe Fisher, AOD Nurse Practitioner candidate; Ingrid Herbert, Clinical Nurse Manager; Dr Chris Watson, Addiction Specialist

Project Summaries 2021-2023 | Page 22 | ©ACHS Improvement Academy
Projectcategory:PartneringwithConsumers
Consumer feedback: Not meeting the expectations of anyone
Ms Kathy Kinrade
Problem/Aims
Ms Kathy Kinrade Director Quality and Education Bairnsdale Regional Health Service (BRHS)

Bairnsdale Regional Health Service (BRHS) is a subregional service across acute, subacute, community and aged care servicing the people of East Gippsland, Victoria. The BRHS Board of Directors and Chief Executive Officer (CEO) had concerns around feedback not being acknowledged or responded to in a timely manner by the Quality and Safety Unit, and this led to a structural review and appointment of a Director of Quality and Education in January 2021.
Complaints and compliments were received from a number of avenues. Initial review of the documentation available for consumer feedback identified three phone numbers, three email addresses and two patient brochures/postcards, along with a website. These were all active and were managed across the Clinical Operations, CEO and Quality and Education directorates.
Although feedback was entered into the Riskman module, this was not used in a timely manner or seen as the source of truth. The existing feedback policy was difficult to understand and was onerous for the Quality Team staff who managed the system. This team had developed its own reporting data sheets and paper-based files, with working files stored on desktop computers. One team member entered minimal data into Riskman in order to be able to generate the monthly reports and labelled these as ‘pending’, which led to the loss of data and inability to identify complainants.
The aim of this project was to ensure all feedback is captured in one data system, allowing oversight of the key performance indicators: that all feedback is acknowledged within three business days; and all complaints, excluding complex issues, are closed within 30 working days.

Project Summaries 2021-2023 | Page 23 | ©ACHS Improvement Academy
Background
It is the right of healthcare consumers to have concerns addressed in a transparent and timely way1. Furthermore, the Clinical Governance Standard2 requires that processes are in place to ensure that complaints are received, reviewed and resolved in a timely manner.
Measurement
Measurement included monitoring of rates of feedback acknowledged within three business days and closure of complaints, excluding complex issues, within 30 days. Qualitative feedback was sought from staff and consumers.
Design
Process mapping was undertaken to understand the following:
• the varied number of entry points available for consumers to give feedback
• the points of contact within the organisation where feedback was received
• the databases and tools utilised
• the gap in key performance indicators related to meeting the requirements for feedback acknowledgement and closure
• ways to improve the content of feedback provided to consumers.
The initial assessment revealed that 16 feedback items had not been answered or entered into the Riskman system over a threemonth period from January to March 2021. With an average of 20 feedback items received per month, this represented approximately 10% of the total. Three complainants escalated their concern to the Health Complaints Commissioner due to the lack of a response, and another two escalated their concern to the local Member of Parliament and the Board Chair.
Strategy
Plan, Do, Study, Act (PDSA) Cycle 1 involved removing the extra reporting databases and using Riskman as the source of truth for all feedback, which was to be entered by the Quality Team on the day of receipt. Education on Riskman was provided for all executive assistants, with excellent uptake by this group.
PDSA Cycle 2 involved a review of the entry
points for feedback. The primary feedback brochure was rewritten to ensure it was consumer-focused and that the health literacy level was appropriate. A new single email address was created. All email to this address was received by the administration and the Consumer Experience Quality Coordinator. Education was provided to ensure staff who receive feedback were informed of the changes.
PDSA Cycle 3: Improvement systems were introduced in the Quality Unit to ensure the quality of the feedback process and that performance indicators were met. A template response was implemented for acknowledgement and as a base for feedback letters, and an investigation template was introduced to assist managers. A visibility board and daily staff meetings were initiated to monitor feedback progress. A review of the reporting template for the Executive and Board meetings was undertaken to ensure the correct information was provided to meet their needs.
PDSA Cycle 4 will involve a survey of consumers to ensure it is user-friendly and meets their expectations.
Results
To date, both quantitative and qualitative data and feedback have been positive regarding the improvements implemented. Figure 1 shows that the performance indicator of acknowledgement has been met every month since July.

The rate of closing feedback within the 30-day timeframe has improved, with a high level of work completed to close outstanding complaints in July (Figure 2)
Conclusion
Although BRHS is a relatively small hospital, the process around feedback management had become complex and unwieldy. As a result, the system, processes and policy had failed to support the Quality Team to achieve the performance expected of them. The PDSA cycles allowed the system shortfalls to be addressed and improvements made to enable staff to reach the desired goals, and this is reflected in team morale.
Project Summaries 2021-2023 | Page 24 | ©ACHS Improvement Academy
Plans for next steps
To continue to explore options to implement a real time feedback product at BRHS. This will give opportunity for consumers to provide feedback at time of attendance, whether a
compliment, complaint or suggestion. The benefit of a system which does that is a decreased response time to the consumer, decreased chance of reputational risk in a rural setting and improvement actions being implemented in a timely manner.

References
1. Australian Commission on Safety and Quality in Health Care. Australian Charter of Healthcare Rights | Australian Commission on Safety and Quality in Health Care [Internet]. Safetyandquality.gov.au. 2023. Available from: https://www.safetyandquality.gov.au/ourwork/partnering-consumers/australian-charter-healthcare-rights
2. Australian Commission on Safety and Quality In Health Care. Clinical Governance Standard | Australian Commission on Safety and Quality in Health Care [Internet]. www.safetyandquality.gov.au. 2017. Available from: https://www.safetyandquality.gov.au/standards/nsqhs-standards/clinical-governance/clinicalgovernance-standard
Project Summaries 2021-2023 | Page 25 | ©ACHS Improvement Academy
Figure 1
Figure 2
9 7 11 11 4 4 10 26 22 44 51 45 36 0 0 0 0 0 0 0 1 6 2 0 0 0 0 10 20 30 40 50 60 Sep-20 Oct-20 Nov-20 Dec-20 Jan-21 Feb-21 Mar-21 Apr-21 May-21 Jun-21 Jul-21 Aug-21 Sep-21 # Business Days Feedback Acknowledged
Days September 2020 to September 2021 < 3 days > 3 days 1 12 9 15 3 2 11 12 8 2 47 45 34 5 9 2 0 0 0 5 1 0 0 68 6 13 0 10 20 30 40 50 60 70 Sep-20 Oct-20 Nov-20 Dec-20 Jan-21 Feb-21 Mar-21 Apr-21 May-21 Jun-21 Jul-21 Aug-21 Sep-21 # Business Days Feedback Closed Within KPI of 30 Business Days September 2020 to September 2021 Closed within KPI Closed outside KPI Started new process
Within 3 Business
Projectcategory:PartneringwithConsumers

Journey mapping patient experience: Emergency caesarean sections
Mrs Natalie Benn

Problem/Aims
Mrs Natalie Benn Clinical Risk Coordinator Quality and Safety Department St John of God Health Care
An emergency caesarean section is the correct course of action in any emergency or complex situation to protect the safety of mothers and babies. In Australia, one in three women describe their birth (including emergency caesarean section) as traumatic1 and often the impact of their trauma and experience is suffered in silence. Understanding the lived experience of those undergoing an emergency caesarean section is important in gaining a deeper insight and perception, ultimately leading to quality improvement and better patient satisfaction.
This project aims to understand and improve the consumer experience when involved in an emergency caesarean section by comprehensively partnering with consumers. The application of quality improvement methodology/actions to areas identified for improvement from journey mapping will measure success.
Background
A high-level flow diagram was undertaken to define the baseline number of opportunities that patients and consumers involved in an emergency caesarean section had to discuss their birth experiences. The flow diagram identified that patients and consumers were not given the opportunity to discuss their experience in order to gain a deeper insight into patient needs, behaviour, experience, motivation and desired outcomes. This project aims to give a voice to the patient so we can identify areas for improvement and partner better with our consumers in leading patient driven quality improvements.
Measurement
Qualitative data were collected through workshops with consumers and informed the
Project Summaries 2021-2023 | Page 26 | ©ACHS Improvement Academy
development of the journey mapping tool.


Design
An affinity diagram with multi-voting determined key reasons and causes that limit the opportunity in capturing patient information. A Pareto diagram was used to prioritise the top reasons that have greatest impact in relation to the identified problem. This supported the notion of having an embedded process to capture patient and consumer experiences. It recognised the need for governance changes, template development and process design. The project design has been titled JEM (Journey Emotional Map), allowing consumers to drive change and identify quality improvement initiatives supporting the shift to value-based outcomes.
Strategy
A journey mapping tool has been developed collaboratively with consumers. The participants included patients who are primigravida, multigravida, midwifery-led and private obstetric-led care staff. The journey mapping groups and sessions were clearly outlined in the framework. Ten patients were offered the opportunity to participate and six agreed to engage. To date, two 60-minute interactive online sessions have been completed and another two have been scheduled a week apart. The findings are being collated onto the journey map.
Results
Since the implementation of the journey mapping process, patients who have experienced an emergency caesarean section have had the opportunity to give a deeper insight of their experience, needs, behaviour, emotion, desired outcomes, and outcomes not met. So far, some of the learnings have included collaborating with the mental health nurse to support the multidisciplinary team on the antenatal and postnatal department; consumer awareness around birth and trauma, including symptoms and what to expect emotionally and physically when involved in an emergency caesarean section for both the patient and their support person. These learnings are leading to
Project Summaries 2021-2023 | Page 27 | ©ACHS Improvement Academy
Figure 1. Driver Diagram
the improvement of the JOY antenatal program, the development of a referral and role description of a perinatal mental health nurse and have opened midwifery discussions around the patient’s physical and emotional expectations and changes to the hospital’s partnering with consumers framework.
Conclusion
It is expected that more learnings and areas of improvement will be identified. The outcome is leading to quality improvement initiatives that meet the needs of consumers.

Plans for Next Steps
After the trial of this project, the journey mapping framework and template design method will be available to all St John of God hospitals and across all departments. The journey mapping process recognises that patients are an integral part and resource in our work to improve outcomes. It is imperative we meet the needs of the consumers of today and in the future.
References
1. Managing Birth Trauma [Internet]. www.gidgetfoundation.org.au. [cited 2023 Aug 8]. Available from: https://www.gidgetfoundation.org.au/adj usting-to-parenthood/managing-birthtrauma
Project Summaries 2021-2023 | Page 28 | ©ACHS Improvement Academy
Projectcategory:PartneringwithConsumers
Same-day rehabilitation reform
Mrs Kera Fulurija
Problem/Aims
By August 2023, our goal is to send out patient reported experience measures (PREMS) to 100% of patients who complete outpatient rehabilitation programs and to provide these hospitals with a live dashboard displaying meaningful data to support them to provide a fit for purpose health service.
 Mrs Kera Fulurija
Mrs Kera Fulurija
 Project Manager – Rehabilitation Strategy Group Services St John of God Healthcare
Project Manager – Rehabilitation Strategy Group Services St John of God Healthcare
Background
St John of God Health Care (SJGHC) is a not-forprofit organisation that operates 19 hospitals across Australia. Six SJGHC hospitals in Victoria provide outpatient rehabilitation services; all six hospitals were in scope for this project.
Our hospitals have limited optics on their outpatient rehabilitation service patient experience, activity, workforce and financial performance. Therefore, they are unable to make evidence-based decisions about quality improvement, service development, workforce requirements and service offering to remain fit for purpose for the communities they serve.
Measurement
We investigated the drivers for poor optics through workshops with end-users and documented their response in affinity diagrams We observed and mapped each hospital’s administration processes and held interviews with senior leadership to understand how the lack of data affected decision-making. These findings were documented using a fishbone diagram.
We found 100% of hospitals used arduous paper-based activities. No hospital collected PREMS and 100% of the hospitals cited inaccurate data in the patient administration system (WebPAS) was the driver of poor optics.
Project Summaries 2021-2023 | Page 29 | ©ACHS Improvement Academy
Design
We brainstormed solutions with end-users and focused on three solutions:
1. A gold standard administration process that supported operational requirements.
2. Standard configuration of webPAS to collect the data required for business optics and PREMS.

3. An online education and training program for caregivers.
Strategy
The above three solutions took over 12 months to iteratively develop with Plan, Do, Study, Act (PDSA) cycles (Figure 2). There was significant engagement with multiple key stakeholders to ensure the solutions met our caregiver expectations.

In March 2023, we rolled out these products iteratively across each hospital and used the PDSA system between each implementation. We found caregiver anxiety and lack of team communication was the biggest risk for ‘go-live’
success. To combat this, we built a checklist that outlined everyone and everything that they needed to do; we held regular sessions to reduce anxiety; and the change manager flew to Victoria to support the go-live. We found this support improved the caregiver’s confidence and limited issues with the go-live. Now all sites are live, we have monthly meetings between all sites to provide ongoing support.
Results
In June 2023, we reached our stretch goal of 100% PREMS surveys being sent to patients who completed their rehabilitation programs.
Project Summaries 2021-2023 | Page 30 | ©ACHS Improvement Academy
Figure 1. Driver Diagram
Conclusion
By August 2023, we intend to have a live interactive data dashboard to provide optics around workforce, finance and patient activity. This result will support sites to review their health service and plan their future service provision, engage in continuous quality improvement and optimise patient experience.


Plans for next steps
Our SJGHC mental health hospitals are interested in adopting these solutions and we are supporting them with this.

Project Summaries 2021-2023 | Page 31 | ©ACHS Improvement Academy
Figure 2. PDSA Cycles by Site
Projectcategory:PartneringwithConsumers
Working with interpreters in the heart of Australia
Ms Alison Thorn
Problem/Aims
The aim of the project was to increase interpreter use in Mental Health Services Central Australia Region. The goal was to offer 100% of Aboriginal clients at the subacute facility whose first language is not English an Aboriginal interpreter by November 2022.
Ms Alison Thorn Nurse Education Coordinator Mental Health, Safety and Quality Team Mental Health Services Central Australia Region Northern Territory Health

Background
The Northern Territory (NT) is culturally and linguistically diverse. Aboriginal people account for approximately 30% of the NT population1 and experience a higher burden of disease. They account for 70% of hospital admissions and 72% of service occasions at health centres in the NT2
More than 100 Aboriginal languages and dialects are spoken. Although NT Health staff are culturally and linguistically diverse, previous research has identified low uptake of Aboriginal interpreters in health care in the NT. Subacute is an eight-bed step-up, step-down mental health residential facility in Alice Springs. There have been extensive mental health quality improvement and Aboriginal cultural safety projects undertaken in previous years. However, the use of Aboriginal interpreters remains low. This project is inspired by cultural safety and working with interpreters being identified as a mental health strategic priority area.
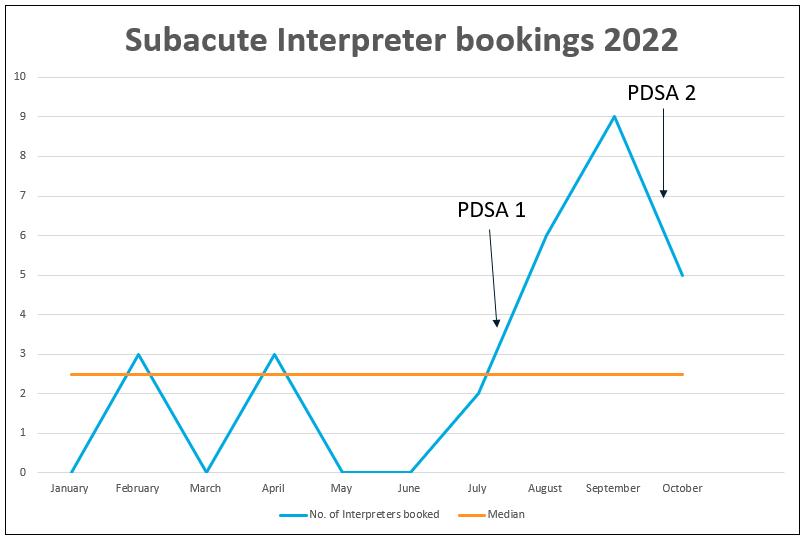
Measurement
Data from mental health interpreter booking logs was collected from January 2022 at baseline and monthly until October 2022 after interventions. The data log included the number of Aboriginal interpreters booked per month. Qualitative data of staff feedback from training sessions was also collected.

Project Summaries 2021-2023 | Page 32 | ©ACHS Improvement Academy
Design
Brainstorming workshops were held with the subacute nursing and medical teams to identify barriers for clients accessing interpreters. The steps involved in booking interpreters was process mapped to identify any gaps that could be addressed.


Strategy
Suggestions that arose from brainstorming sessions were tested in two Plan, Do, Study, Act (PDSA) cycles. The initial cycle included

reviewing the process for booking interpreters in addition to developing and refining the process map. The second cycle was reimplementation of the Working With Interpreter Training (WWIT) for the mental health service.
Results
Run charts demonstrate that as a result of these interventions the number of Aboriginal interpreter bookings per month doubled over all PDSA cycles. Qualitative data indicated that overall staff felt positive about the WWIT, as it was helpful and informative.
Project Summaries 2021-2023 | Page 33 | ©ACHS Improvement Academy
Figure 1. Diagnostics
Figure 2. Annotated Run Chart
Conclusion
As these improvements become more established it is hoped Aboriginal interpreters will continue to be booked for clients at the subacute facility to improve mental health outcomes. The Aboriginal Interpreter Service was not included as a key stakeholder; however, their engagement in future would enhance the impact of the project.
Plans for next steps
If improvement is sustained through ongoing PDSA cycles, the project could augment existing mental health quality improvement projects, inform local guidelines, and support the development of an orientation package for staff. If successful, the project could be expanded to other areas within Mental Health Services in Central Australia and the Barkly regions.
References
1. Australian Bureau of Statistics. Aboriginal and Torres Strait Islander people: Census [Internet]. Canberra: ABS; 2021 [cited 2023 August 9]. Available from: https://www.abs.gov.au/statistics/people/ab original-and-torres-strait-islanderpeoples/aboriginal-and-torres-strait-islanderpeople-census/2021.
2. NT Health Annual Report 2021 - 2022. Available from: https://health.nt.gov.au/__data/assets/pdf_fil e/0003/1179111/nt-health-annual-report-202122.pdf. Darwin: Northern Territory Government; 2022.

Acknowledgements
Louise Dennis, Aboriginal Cultural Advisor, Mental Health Services Central Australia and Barkly Regions, NT Health
Project Team
Louise Dennis, Aboriginal cultural advisor; Taiwo Abraham, subacute facility team manager; Julieth Chisvuure, subacute team leader; Jose Hamindun De Las Alas, subacute nurse; Eleazar Sy, subacute nurse; Fatima Sheriff, subacute nurse; Janet Ndiweni, subacute nurse; Mary Angeline Tan, subacute administration officer.
Project Sponsor
Sherrilee Portlock, Quality and Safety Manager.
Project Summaries 2021-2023 | Page 34 | ©ACHS Improvement Academy
Projectcategory: Rehabilitation
Heart Yearning 2022: Improving the Acute Coronary Syndrome patient cardiac rehabilitation journey
Mrs Justine Williams
Problem/Aims
The Northern Territory Top End Coronary Database (NTTCD) data captures Phase 1 inpatient cardiac rehabilitation (CR) and Phase 2 CR referral rates. Data shows that 20% of acute coronary syndrome admissions had the current Phase 1 CR education form completed and that 54% of these patients had a referral to Phase 2 CR. The project target is to improve both Phase 1 CR education and Phase 2 CR referrals for patients to 70%.
Mrs Justine Williams
Cardiac Research Coordinator and Quality Nurse, Division of Medicine – Cardiology Royal Darwin Hospital Northern Territory Health
Background
Despite the documentation of substantial morbidity and mortality benefits, CR services are vastly underutilised, and many patients do not receive the benefits of CR due to low referral rates. Of those patients referred, commencement rates vary from 28.4% to 60%1 Research has shown that heart attack survivors who complete CR are 40% less likely to experience another attack2

Measurement
At six and 12 months post-implementation of interventions, the NTTCD quantitative data for Phase 1 CR education and Phase 2 CR referrals for acute coronary syndrome patients will be reviewed. For consumer-related interventions, qualitative interviews on how the interventions have improved communication and health literacy levels will occur.

Design
A TEAMs survey and face-to-face interaction with cardiology nursing, medical staff, and the external CR provider was used for the data collection regarding the barriers and enablers for both Phase 1 and Phase 2 CR. Post-review, the themes that emerged were charted using
Project Summaries 2021-2023 | Page 35 | ©ACHS Improvement Academy
Pareto and driver charts, identifying areas of Phase 1 and Phase 2 CR that required intervention and change ideas proposed. PDSA cycles were used for the implementation of interventions.

The project also included six consumer interviews, where patients were asked how they knew what questions they should ask about their heart story and care once they left hospital. Two themes were identified: health literacy and communication.
Strategy
PDSA Cycle 1: A Phase 1 CR education form was developed and approved via stakeholder consultation and the Royal Darwin and Palmerston Regional Hospital (RDPH) Forms Committee, aiming to reduce variability in education content delivery and standardise documentation.
PDSA Cycle 2: Phase 2 CR improvement involved discussion and co-design of the referral form with the Phase 2 CR stakeholders.
PDSA Cycle 3: This cycle will trial the use of visual cues to alert the patient to questions they may want to ask when participating in conversations about their journey to wellness. The evaluation of the visual cues will be through survey/discussion with patients.






Results




The CR form is now a hospital record and becomes part of all cardiology admissions. Implementation occurred in September 2022. New Phase 2 referral form implementation took place in October 2022. Visual cue implementation was in November 2022. First evaluations will occur in March 2023 by the cardiology research coordinator.






Conclusion
There was no simple solution to improving the CR process. The interventions implemented were a result of the engagement with both internal and external clinical stakeholders as well as the consumers.
Project Summaries 2021-2023 | Page 36 | ©ACHS Improvement Academy
To improve the Phase 2 Cardiac Rehabilitation referrals for Acute Coronary Syndrome (ACS) patients Patient and family care Staff education and awareness of ACS Reliable Phase 2 referral Education and awareness Have the patient actively involved about CR Set discharge processes to ensure the patient/family have had education Education program specific to ACS and CR Old CR referral form needs reviewing Standardising the process for referring ACS patients to CR Allow the patient to have access to their Phase 1 CR education record so that they know the education process Visual Cue: Design a poster making patients aware that CR is a treatment for ACS – ask the Nurse or Doctor Develop a ACS checklist for the patient to make them part of the discharge process To provide the CCU Staff with specific education about ACS and CR, Phase 1 and Phase 2 Redesign the old referral form to make it easy to complete. Develop a guideline for CR referral to reduce variation in the process Aim Primary Driver Secondary Driver Change Idea Driver
Figure 1. Driver Diagram
Diagram - Improving the Acute Coronary Syndrome Patient Cardiac Rehabilitation Journey
Plans for next steps

The outcomes of this project will be shared with internal and external partners in the healthcare sector, including NT Phase 2 CR provider Healthy Living NT and the SA/NT Australian Cardiac Rehabilitation Association.
References
1. Driscoll A, Hinde S, et al. Estimating the health loss to poor engagement with cardiac rehabilitation in Australia. Int J Cardiol. 2020; 317:7–12.
2. CSIRO. A mobile platform for cardiac rehabilitation.
https://www.csiro.au/en/research/healthmedical/diseases/Cardiac-rehab-app
Project Team
Liz Hitchcock, Aboriginal Health Practitioner; Cardiac Care Unit nursing team; Healthy Living NT.
Project Summaries 2021-2023 | Page 37 | ©ACHS Improvement Academy
Improving open disclosure documentation
Ms Jo Muir, Ms Kim Walters and Ms Nicky Cheeseman
Problem/Aims
The aim of this quality improvement project is to ensure open, honest, empathetic and timely communication with patients and families is routinely undertaken and documented when care does not go to plan.

Background
Jo Muir Manager Safety Improvement Safety Quality and Consumer Engagement South Metropolitan Health Service


Initiation of open disclosure for Severity Assessment Code (SAC) 1 and 2 clinical incidents is monitored via a dashboard using clinical incident management system data. The rate of open disclosure initiation for these serious incidents was not as high as expected. This project aims to improve documentation of open disclosure to demonstrate that the organisation meets the requirements of the Australian Open Disclosure Framework1
In discussion at clinical governance meetings, the reason given for poor results was that the data was inaccurate because the field in the clinical incident management system was not updated and there were inconsistencies in data capture.
 Health Service
Health Service
Measurement
Safety Improvement Officer Safety Quality and Consumer Engagement South Metropolitan Health Service
Open disclosure policy at South Metropolitan Health Service requires open disclosure for SAC 1 and 2 events to be recorded on a specific medical record form. A retrospective audit was undertaken, which demonstrated that open disclosure was marked as ‘initiated’ in the clinical incident system in 58% of incidents, but evidence of disclosure was only found for 21% of cases. There were no cases where open disclosure was ‘unknown’ or ‘no value’ where evidence of open disclosure was found on medical record review.
Project Summaries 2021-2023 | Page 38 | ©ACHS Improvement Academy
Projectcategory:Systems
Ms
Ms Kim Walters Safety Improvement Lead Safety Quality and Consumer Engagement South Metropolitan
Ms Nicky Cheeseman
Design
A senior staff survey was conducted to better understand the barriers to documentation of open disclosure. Information from the audit and survey was used to populate a driver diagram (Figure 1) and generate ideas for improvement. Change ideas were assessed using an impact effort matrix to determine where to focus the change efforts.

Strategy
Quick wins and some weaker actions have been implemented and the existing open disclosure dashboard, which updates daily, has been used to measure improvement. A GANTT chart was developed to manage the project, including high-impact, high-effort actions that will take time to implement and measure outcomes.

Results
Improvement in documentation will be measured by follow-up medical record audits.
Conclusion
Limitations and challenges encountered during the project included resistance to implementing mandatory education in the Open Disclosure documentation process, clinical staff
availability for education, and establishing a reliable data source to develop a tracking process for ongoing disclosure conversations. Stakeholder engagement, scheduling protected time with clinical staff away from wards for training and working closely with data analysts are strategies added to the project plan to address these challenges.
Project Summaries 2021-2023 | Page 39 | ©ACHS Improvement Academy
Figure 1. Driver Diagram
Plans for Next Steps

Staff surveys adapted from the pilot survey will be undertaken and results used to modify actions using Plan, Do, Study, Act cycles. Regular follow-up audits are scheduled, commencing April 2023. Oversight and governance will ensure the changes are sustained until they are fully embedded in the organisation’s safety culture.
References
1. Australian Commission on Safety and Quality in Health Care. Australian Open Disclosure Framework [Internet]. 2014. Available from: https://www.safetyandquality.gov.au/sites/de fault/files/migrated/Australian-OpenDisclosure-Framework-Feb-2014.pdf
Acknowledgements
Maxine Wardrop, Executive Director of Safety, Quality and Consumer Engagement, South Metropolitan Health Service; Andrea Hickert, Co-Director Service 4, Fiona Stanley Fremantle Hospital Group; Alison Stewart, Clinical Risk and Consumer Feedback Officer, Western Australia Country Health Service; John Anderson/Gillian Scott, Area Director Clinical Services, Director Clinical Services, Fiona Stanley Fremantle Hospitals Group; Suki Loe, Nurse Director, Informatics, South Metropolitan Health Service.
Project Summaries 2021-2023 | Page 40 | ©ACHS Improvement Academy
Our data drives our care

 Ms Lucy Lehane
Ms Lucy Lehane
Problem/Aims
Ms Lucy Lehane Quality and Safety Nurse Specialist Chris O’Brien Lifehouse
Robust systems for the collection of quality and safety data are well established at our hospital. However, frontline staff do not have regular, easy access to unit specific data, which impedes their ability to engage in data-driven continuous quality improvement. The project aim is for 100% of staff on a surgical unit to access quality data and be empowered to engage in quality improvement by November 2021.
Background
Transparency about performance and engagement of clinicians in the monitoring of safety and quality systems are essential to the delivery of safe and high-quality healthcare1 Highly reliable organisations routinely display key quality measures2 and clinician-driven quality improvement is more effective than manager-driven quality improvement systems3 The Box Score developed by the Scottish National Health Service brings together quality performance measures which are displayed on unit level boards. Providing the tools to identify trends and improve efficiency resulted in reduction in falls, improved staff satisfaction and a 15% decline in cost per patient in a hospital where the Box Score was implemented4
Measurement
A survey of the 20 staff in the unit was undertaken to define the baseline level of access to quality data (15% were informed of monthly unit-specific quality data), quality improvement capability (30% understood the quality improvement process) and awareness of improvement activities (25% were aware of quality improvement activities in progress). The Quality Activity Register was analysed to determine the number of quality activities by unit in the preceding two years. Whilst the number of activities initiated in the unit was in the 60th percentile, only three staff had been
Project Summaries 2021-2023 | Page 41 | ©ACHS Improvement Academy
Projectcategory:Systems
involved in the projects. These measures will be repeated at six and 12 months from project commencement. Incident data including falls, pressure injuries, medication incidents and infection rates will be compared to baseline data at 12 months.
Design
The project team included members of the quality team and ward staff with executive sponsorship from the Director of Operations. The team mapped the current process for
disseminating quality data. Results from a group brainstorming exercise were collated into a cause-and-effect diagram and ranked. As a result, a report containing meaningful and useful unit-specific quality data was developed for presentation at the monthly unit meeting.
Our initial plan was to develop an electronic summary dashboard for quality indicators. This was hampered by limitations of the existing incident reporting platform. Transition to an updated incident and patient feedback platform is in progress.

Strategy
A quality report using the existing platform was developed and refined in response to feedback from the unit team. Early reports contained too much data. A pared-back report with monthly numbers of pressure injuries, falls, infections and medication incidents is provided for presentation at monthly unit meetings.
Results
The quality report has been presented at three meetings. ‘Quality champions’ for each clinical risk have been nominated on the unit. It is anticipated that when the survey of staff is repeated at six and 12 months, there will be a significant increase in quality improvement confidence and capability and in improvement projects entered into the Quality Activity Register. Clinical incidents are expected to decline.
Conclusion
The project has confirmed that clinicians want to access quality data specific to their unit to drive improvements to patient care. The process of building a fit for purpose report sharpened our understanding of the limitations of existing incident and feedback platforms.
Plans for next steps
As a result the organisation is transitioning to systems that will be used across the hospital to present quality data and empower clinicians to drive QI.

References
1. Australian Commission on Safety and Quality in Health Care. National Model Clinical Governance Framework; 2019. https://www.safetyandquality.gov.au/topi c/national-model-clinical-governanceframework
Project Summaries 2021-2023 | Page 42 | ©ACHS Improvement Academy
Figure 1. Driver Diagram
2. Chassin M, Loeb J. High-reliability healthcare: Getting there from here. Milbank Q. 2013;91:459–490.
3. Scott I. What are the most effective strategies for improving quality and safety of health care? Intern Med J. 2009;39:389–400.
4. Mate K, Rakover J, et al. A simple way to involve frontline clinicians in managing costs. Harvard Business Review. 2017. https://hbr.org/2017/10/a-simple-way-toinvolve-frontline-clinicians-in-managingcosts

Project Summaries 2021-2023 | Page 43 | ©ACHS Improvement Academy
Projectcategory:Systems
Redesign of the clinical incident review process for Yorke and Northern Local Health Network to better a lign with the intent of Clinical Governance Standard 1
Miss Fiona Murray
Problem/Aims
Miss Fiona Murray Director of Safety and Quality Safety and Quality Directorate Yorke and Northern Local Health Network

In 2021 the Yorke and Northern Local Health Network underwent an external review of its safety and quality systems, and accreditation against the National Safety and Quality Health Service Standards. These both identified that the clinical incident review process did not meet Standard 1 Clinical Governance Standard (Action 1.11). In response to this, a Clinical Incident Review Committee was established.
A subsequent review in 2022 concluded that despite the creation of the Clinical Incident Review Committee, the clinical incident review process was still not effective. A subjective uniprofessional perspective dominated, focusing on ‘mistakes made’ with a person-centric focus. Participation was limited, thus risking missing important views, with a risk that the wrong conclusions were drawn, leading to flawed recommendations and limited system improvements.
A new improvement project commenced in August 2022 with the purpose of understanding why the previous intervention had failed and to provide recommendations for a new approach.

Measurement
Semi-structured interviews were conducted with existing committee members, a review of performance metrics was undertaken, including the Committee’s key performance indicators: number of meetings cancelled or not quorate; incident data, including length of time to complete; and number of times the same incident was reviewed.
Project Summaries 2021-2023 | Page 44 | ©ACHS Improvement Academy
Design
A rapid review of the literature was conducted, and examples of best practice sought from other jurisdictions. An evaluation of tools such as the London Protocol and root cause analysis was undertaken. Following this, a suite of tools was chosen to support a consistent process.
Strategy
The Safety and Quality team undertook training in root cause analysis and other identified tools. Restorative justice culture training was provided to all members of the Safety and Quality team and members of the Clinical Incident Review Committee. Membership of the committee was broadened and a process whereby sites were invited to participate in their incident reviews was established.
A new clinical incident review process was designed and tested and changes made based on feedback received after each Clinical Incident Review Committee meeting.

The role of the Committee was clearly articulated as a resource that works collaboratively with Yorke and Northern Local Health Network services to determine the intrinsic aspects of system failures; and to identify and advise on opportunities for improvement. The following principles now underpin all incident review activities:
• a just culture
• focus on systems and not people
• a human factors approach
• emphasis on learning.
Results
Following these changes there has been a noticeable improvement in Committee performance, with 100% attendance and no meetings cancelled or non-quorate. Average time to closure of an incident has gone from 101 workdays to 65 workdays. There has been an increase in the number of ISR1 or 2 incidents being reported from 19 to 33, which we interpret as people feeling more confident to report them.
Conclusion
Providing an explicit focus in the CIRC on systems, not people, reinforcing the restorative
just culture approach at every meeting and establishing best practice methodologies for conducting incident reviews have achieved profound culture change and increased the effectiveness of the incident review process across YNLHN.
Plans for Next Steps
The next steps include a review process to revisit the recommendations to ensure that they have become embedded as a system change. We will also redesign the way in which learnings are disseminated and instigate a parallel process to provide professional debriefs and psychological support to those involved.
Project Summaries 2021-2023 | Page 45 | ©ACHS Improvement Academy
Standardising the clinical audit process in the Top End, Big Rivers and East Arnhem regions
 Ms Ali Walker
Ms Ali Walker
Problem/Aims
Ms Ali Walker
Clinical Nurse Consultant Monitoring and Compliance
Clinical Excellence and Patient Safety Division Northern Territory Health
The project aim was to develop a process tool for audit tool compliance against relevant standards, legislation, and organisational requirements that was designed to ensure all audit tools meet compliance and are comparable across different organisational sectors. This project informs a much larger body of work around audit program governance for the organisation.

Background
The Top End, Big Rivers and East Arnhem regions Standards and Safety and Quality committees receive audit reports regularly and have noted the need for progress from the audit results multiple times. A review of the existing audit tools found numerous tools with the same name but different criteria. Indications are that audit tools are changed to suit other areas; the organisation is unable to measure consistently across all sectors; and audit program governance needs to be stronger. The flow-on effect is potential consumer harm and missed opportunities for improvement.
Measurement
We used the Plan-Do-Study-Act (PDSA) cycle to develop the process tool with the help of fishbone and driver diagrams to differentiate issues needing corrective action and actions to drive those changes. The fishbone diagram helped work out requirements in the process tool in combination with the background issues. The driver diagram (Figure 1) assisted in the development of actions and information development for the process tool. Testing the process tool by reviewing existing audit tools through the process tool helped design further requirements, e.g., an ethics questionnaire. The
Project Summaries 2021-2023 | Page 46 | ©ACHS Improvement Academy Projectcategory:Systems
creation of a flowchart of the process assisted staff in following the process from start to completion
Design
Developing a process tool as an intervention to address non-standardised audit tools across
the region’s health services that is easy for staff to use and meets legislation, standards, and organisational requirements was challenging. An online review of other audit programs was conducted to ascertain suitable process tools. Few online process tools for online clinical audits met the project criteria.
Strategy
Feedback from project team members was invaluable in addressing the tool’s usability and trialling the process tool showed where it lacked information and understandability. The PDSA cycle assisted in collecting this information and finding potential solutions.
Results
Two PDSA cycles were completed to assist with the development of the process tool and review it, and feedback from project team members enabled improvement in the template. An action list, an accountable person, and timeframes stemmed from the PDSA cycle and closed the loop in the process tool development.

Conclusion
The audit development/review tool has now been distributed across the Northern Territory to assist staff in updating their audit tools. The
clinical audit program is undergoing a transition from regional to Territory-wide currently and audit tools will undergo the same process using the tool to ensure compliance.
Plans for Next Steps
The next steps include reviewing all existing audit tools and determining the criteria required for each so that the organisation has comparability across all regions for any particular audit and sharing our learning from this process with other organisations yet to develop a robust, compliant audit program.

Project Team
Kirsten Thompson, NMC Sepsis; Mary-Rose Godsell, SNA Infection Prevention and Management; Marguerita Brown, Clinical Information System Audit Officer; Amy Drahm, Clinical Incident Management System Coordinator
Project Summaries 2021-2023 | Page 47 | ©ACHS Improvement Academy
Figure 1. Driver Diagram
Guidance Team
Mish Hill, Chief Nurse and Midwifery Officer and EDoNM Top End, Big Rivers and East Arnhem Regions; Cheryl MacDonald, Deputy Chief Nursing and Midwifery Officer; Linda Reid, CNC TEHS Safety and Quality

Project Summaries 2021-2023 | Page 48 | ©ACHS Improvement Academy
Projectcategory:Systems
Succession planning: Improve workforce capability and flexibility
 Ms Tina Lloyd and Dr Karen Pedersen
Ms Tina Lloyd Senior Quality Improvement Coordinator Patient Safety and Clinical Quality Western Australian Department of Health
Dr Karen Pedersen Senior Policy Officer Patient Safety and Clinical Quality Western Australian Department of Health
Ms Tina Lloyd and Dr Karen Pedersen
Ms Tina Lloyd Senior Quality Improvement Coordinator Patient Safety and Clinical Quality Western Australian Department of Health
Dr Karen Pedersen Senior Policy Officer Patient Safety and Clinical Quality Western Australian Department of Health
Problem/Aims
This project aims to improve the West Australia Department of Health Patient Safety and Clinical Quality (PSCQ) Directorate workforce capability and flexibility in relation to succession planning for new managers and emerging leaders. The project addresses orientation for new managers, the helpfulness of manager handovers and the confidence to perform managerial processes.
Background
The PSCQ management team highlighted an inability to take leave, retire or cover their role appropriately in the event of unplanned absences. The emerging leadership group within the Directorate had also previously communicated their dissatisfaction with lack of opportunities to take on management roles or tasks.
Measurement
To understand barriers and perceptions to succession planning, we undertook workshops and interviews with managers and team members, and the results were displayed in a cause-and-effect diagram highlighting the key themes.
Stakeholders then participated in an ‘idea storm’ to generate improvement ideas based on the barriers identified, which were fed into a driver diagram (Figure 1). The diagram listed 17 change ideas, though three factors emerged that contributed to management capability at the point of succession: manager induction, management processes, and manager handover.
Aligning with the three change ideas, a questionnaire was designed to establish baseline data. The emerging leaders were asked about their recent experience in acting managerial roles for induction, handover,
Project Summaries 2021-2023 | Page 49 | ©ACHS Improvement Academy
knowledge gaps and professional development as well as opportunities for improvement. Three measures were established to increase the orientation rates, increase process confidence

and increase helpfulness of handovers. The questionnaire will be used through each Plan, Do, Study, Act (PDSA) cycle to measure progress and inform next steps.
Design
Several resources were developed to support manager induction, management processes, and manager handover. These are hosted on the redesigned PSCQ intranet hub and include:
• A new page for PSCQ onboarding that includes a ‘Managers Welcome’ to orient new managers. This was designed to complement existing Departmental employee resources and included information and relevant links for key processes identified as knowledge gaps via the survey.
• A ‘Managers Resources’ page providing a standardised template for unit and role handover and additional information on managerial processes.
Strategy
Two change initiatives are running in tandem, with concurrent PDSA cycles: 1 PSCQ manager
induction and processes; and 2 resources for improving handovers. Both initiatives have been launched with a series of communications and are currently in the study phase of Cycle 1.

Results
So far, we have achieved the launch of a new and improved hub, with resources for manager induction and handover. This project has resulted in greater awareness of the gaps to succession planning, and how managers can directly influence and control these areas.
Anecdotal feedback confirms that the new hub has been well received and the induction is being used as an information source. A number of PSCQ team members are also opting to use the handover template. Future survey results will provide further evaluation of these strategies and activities. A key learning is that the culture of teams or organisations can result in greater project complexity and longer cycle
Project Summaries 2021-2023 | Page 50 | ©ACHS Improvement Academy
Figure 1. Driver Diagram
time than envisioned at the outset.
Conclusion
Early indications are that the new resources are effective, though significant work needs to be undertaken to champion and embed. Continuing communication and open feedback channels will be ongoing throughout the project delivery.
Plans for Next Steps
More PDSA cycles are planned, and steps include:
• another round of communications; including standing item for leadership team meetings
• continued greater executive support with increased influence

• repeating the questionnaire for each cycle
• formalising the orientation process
• feedback to unit and Directorate team members on project findings and outcomes.
Project Summaries 2021-2023 | Page 51 | ©ACHS Improvement Academy



















 Ms Fiona Miles
A/Safety and Quality NMC Nursing Department Gove District Hospital Northern Territory Health
Ms Fiona Miles
A/Safety and Quality NMC Nursing Department Gove District Hospital Northern Territory Health




















 Project Manager – Rehabilitation Strategy Group Services St John of God Healthcare
Project Manager – Rehabilitation Strategy Group Services St John of God Healthcare






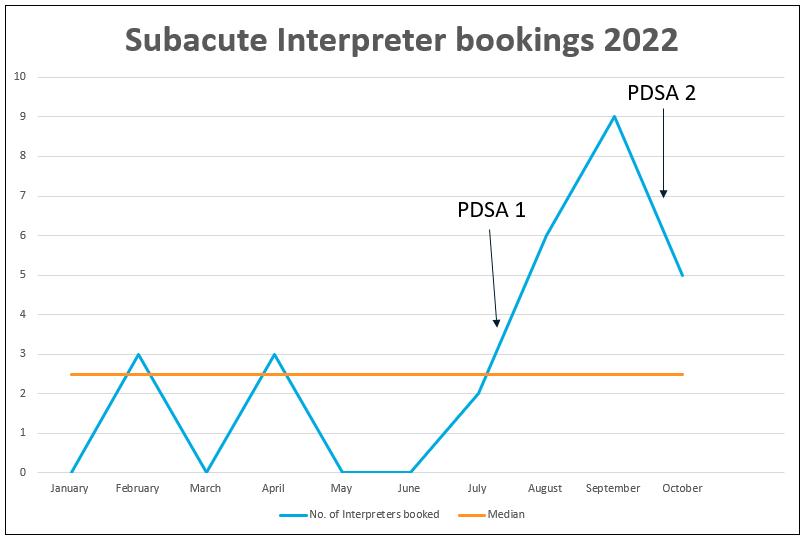






















 Ms Ali Walker
Ms Ali Walker

