GOOD SEX BAD SEX
PEP TALK



You have reached out and picked up a copy of Man2man Summer edition, our first for 2017!
In this edition we introduce two national campaigns being rolled out by our friends at AFAO, the Australian Federation of Aids Organisations. One is a fairly self-explanatory campaign for Young Gay Men to promote the sharing of stories and experience, and the other is the slightly edgier campaign, Grunt, aimed at promoting sexual health awareness amongst trans men. In addition to that, Matteo wrote us an article that explains about being U+something you might have seen on hookup apps. By identifying as U+ it shows that you are HIV + with an undetectable viral load. Read about what that means on pages 14 & 15.

Andrew wrote about the need for respectful language when talking about matters LGBTIQ+. It’s not always so easy to grasp the complexities, so Andy has given us some tips and pointers about where to find some good info, pages 12 &13.
In this edition we have included a submission from one of our readers about his experience using the Post Exposure Prophylaxis (PEP) anti HIV medication. It’s on pages 6 and 7. A big thanks to him for his contribution – the value for me here lies in the lived experience of a peer, who made use of the latest in the prevention of HIV transmission. A heads up for all those of us who enjoy sex in a wide variety of settings.
Finally, Grant wrote us an easy to read description of how to tell if your sex practises are working for your overall mental health. Take a moment to have a look. Even if it doesn’t apply to you directly, you might find some pointers to keep in mind for a mate, pages 4 & 5.
Please take some time to read through our offerings. We encourage you to be in touch with our office: let us know what you think about stuff, tell us what you would like to see more of, and see if you can get us to commit your ideas to print. Want to advertise something? Want to rant about something? Got an idea you want to promote in print? Drop us a line, and let’s have a chat. By the way, keep your eye out for promo of the Rainbow Gala Charity Ball. Tix available soon!


Lube:
One
Four



This publication is an initiative of the Health Promotion Program at the Tasmanian Council on AIDS, Hepatitis and Related Diseases, (TasCAHRD).
Views expressed in Man2Man are those of the authors and do not necessarily reflect the views of TasCAHRD.
Phone: 03 6234 1242
Email: projects@tascahrd.org.au
Post: GPO Box 595 Hobart
Tasmania 7001
Web: tascahrd.org.au
Facebook: Man2ManTas
TasCAHRD receives funding from the Crown, through Department of Health and Human Services, to provide these services.
Editor: Matt Anning
Contributors: Matteo Senesi Andrew Badcock Grant Blake
Our colleagues at TasCAHRD Design & Layout: Ede Magnussen
Printing courtesy of: Xerox Hobart



Sex can play an important role in a person’s sense of wellbeing and identity. It influences how we approach and behave in relationships, and can be a source of excitement that facilitates a meaningful connection between people. At the same time, sex can also produce anxiety, be confusing, and has the potential to be used as an unhealthy coping strategy.
Although sex addiction is not a diagnosable mental illness, it is acknowledged by many mental health professionals as a serious problem. Addiction is often described to involve compulsive behaviours that adversely impact relationships, daily functioning, and can cause significant psychological distress. For example, a person might experience impaired concentration from always have sex on their mind, not complete work tasks due to excessive engagement in sexual activities, place their health at risk, or place the health

of their sexual partners at risk.
Behaviours associated with sex addiction include: spending excessive amounts of time looking for sex (e.g., on hook-up apps), excessive masturbation, excessive pornography use, risking one’s health for sex, and failing to complete or engage with usual activities due to sex.
Psychologists often find that a person with sex addiction typically uses sex to avoid negative feelings (e.g., fear of loneliness, depression, anxiety). When sex is used to escape negative feelings, the effect is typically brief and unsatisfying. This is because the underlying cause of the negative feelings is not addressed. Problematically, the unsatisfied person then finds themselves seeking out more sex to cope with the disappointment of not having their emotional needs met.
Within relationships, using sex to deal with a

disagreement means that the reason for the conflict is overlooked and the problem will keep returning. Conflict also arises when a person becomes distressed by their partner’s constant sexual advances, as can be the case with sex addiction or not respecting your partner’s boundaries.
In the digital era, a new variety of problem sexual behaviours have emerged. “Revenge porn,” which is the illegal sharing of private sexualised images or videos of a person, has increasingly become an issue. Similarly, “catfishing,” which is the creation of a false online profile for personal gain, is a fraudulent behaviour that has been associated with criminal prosecutions in Australia.
1. Know the difference between sex for fun versus sex for avoiding negative feelings.
2. Enjoy sex by respecting your
own boundaries and the boundaries of your partner/s.
3. Understand consent: Consent is an agreement about allowable sexual behaviours within a certain sexual experience. Consent can be withdrawn at any time and it must be respected.
4. Speak to your GP, a psychologist or counsellor if you think sex is a problem for you, or has the potential of becoming a problem.
5. Take the stress out of sex – use condoms and find out about PrEP.
6. Be adventurous and have fun!
Grant Blake is a registered psychologist at ForensiClinic Consulting

"He
disclosed to me that he had a recent risky exposure to HIV."
Many of us have had sex that we regret. With any luck, we can write it off as inconsequential, swipe left and move on to the next adventure.
I like sex and I do my best to keep it sensible, if not safe… But a recent hookup with a guy on Scruff left me worried about potential exposure to HIV after a night of alcohol, pot and unprotected sex.
After a little research, and after he disclosed to me that he had a recent risky exposure to HIV, I decided to go on a course of the anti-HIV treatment, PEP.
PEP treatment involves taking a course of antiretroviral medicines after a potential exposure to HIV. It needs to be started within 72 hours of exposure and is taken once or twice daily for 28 days. Initially I was hesitant to go on PEP after reading others’ experiences of the treatment. But in the end, my need for peace of mind outweighed my fears about the treatment. The morning after my possible exposure, I attended my local sexual health clinic, answered a couple of sexual health questions and was prescribed a 28-day course of PEP.
I felt more anxious than usual for the first few days on the medication,
however, this may have been a side effect of googling other people’s experiences on the drugs.
The first noticeable side effects came after three days on the drug. Despite taking the two pills at a regular time with food as directed, I had a little nausea and a rock-hard feeling in my stomach. The brief waves of nausea passed after four or five days and the stomach discomfort came and went throughout the four weeks. Aside from the stomach discomfort, I felt a little more tired than usual and had some difficulty focusing on complex tasks at times. It probably wasn’t as bad as it sounds, especially when you consider the peace of mind I was investing into.
Twenty-eight days later, I am relieved to have finished the treatment and keen to get my follow up HIV tests and look into getting on PrEP as a more longterm protection. While the sex was a little regrettable, getting treatment fast definitely wasn’t.

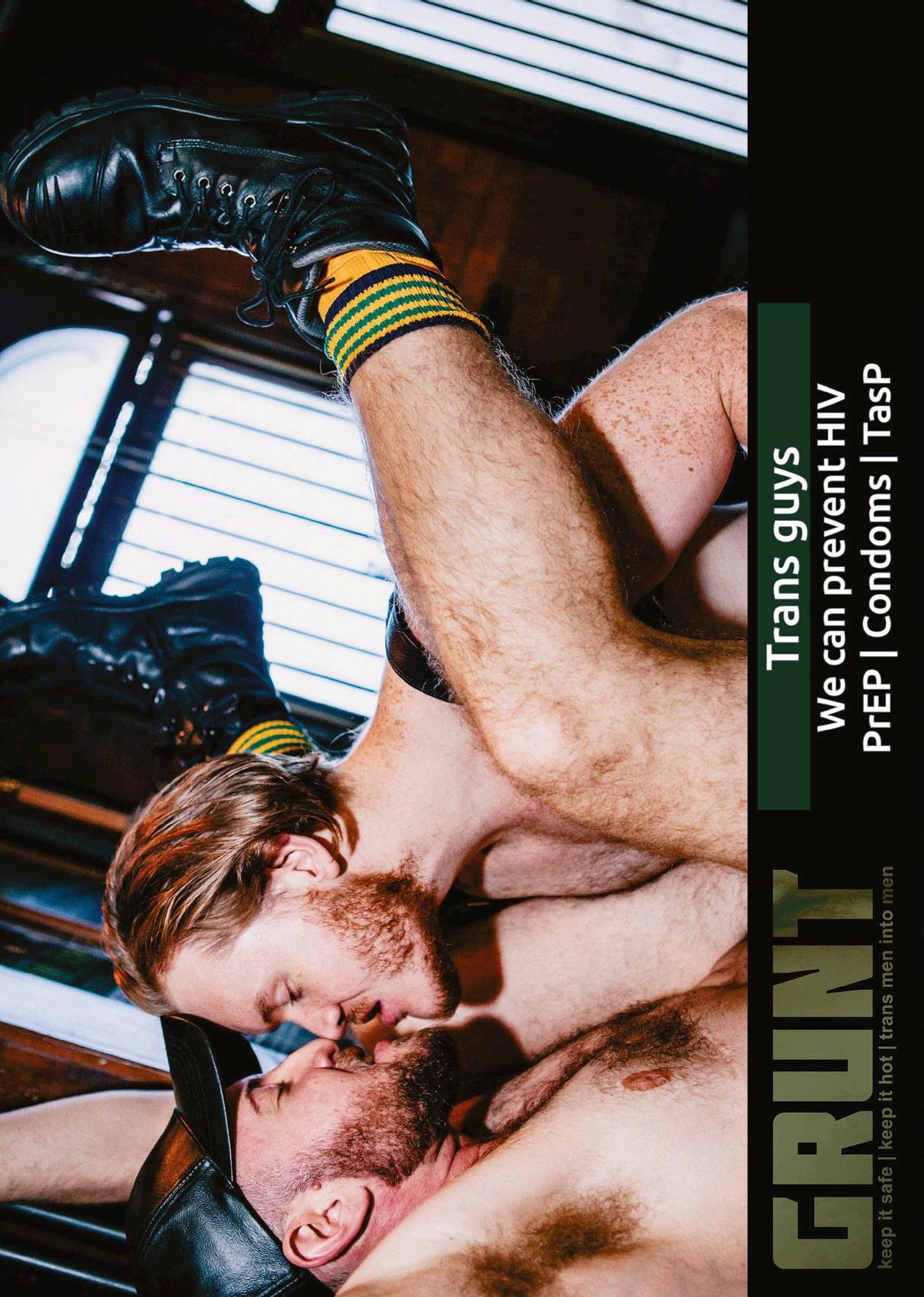
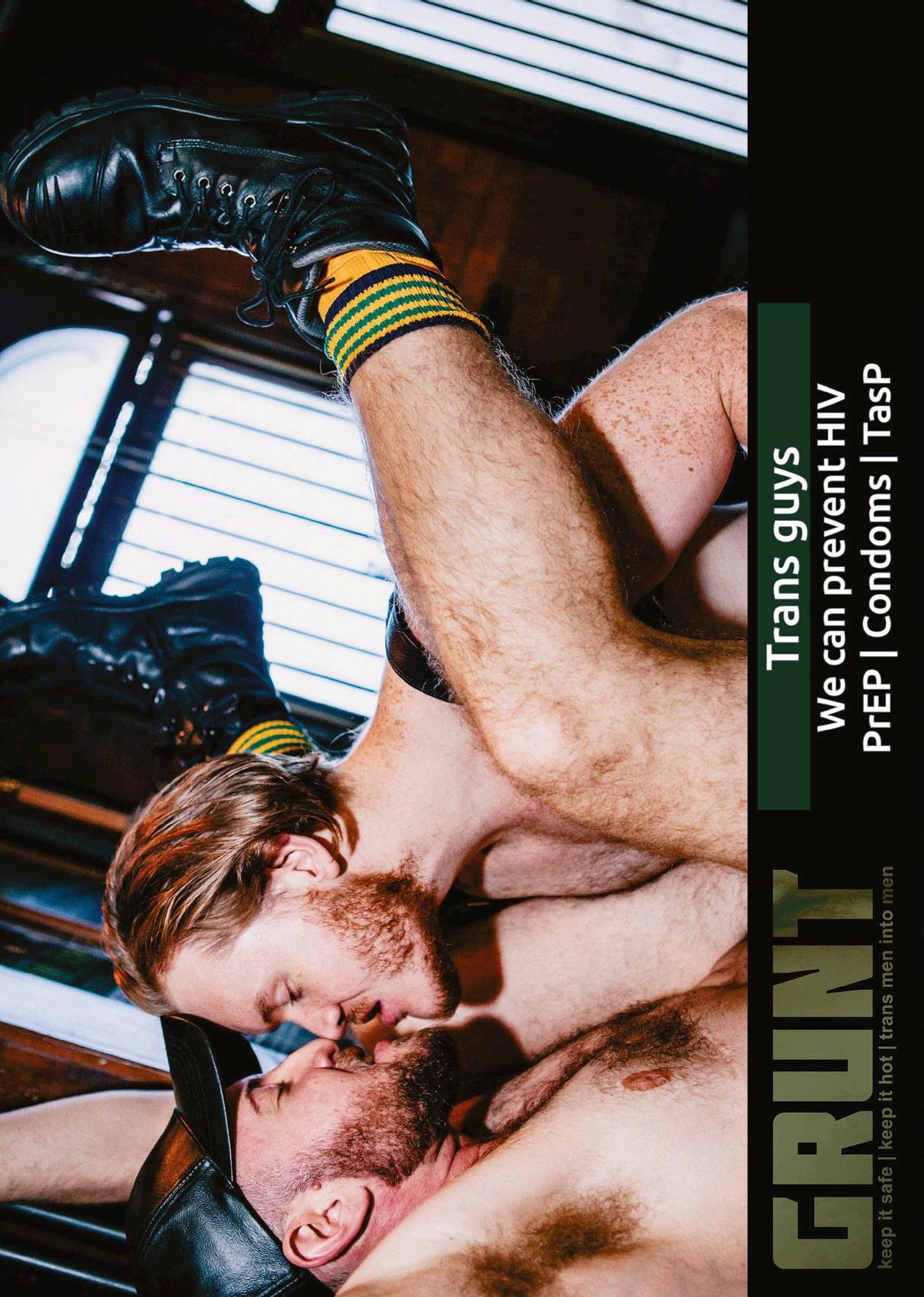
The Peer Advocacy network for the Sexual Health of Trans Masculinities (PASH.tm) and the Australian Federation of AIDS Organisations (AFAO) have launched ‘GRUNT’, a new HIV prevention and sexual health campaign aimed at transgender men who have sex with cisgender men. GRUNT features images of real gay, bi and queer men (both trans and cis) and provides accurate, inclusive and sex positive sexual health information so trans men can keep it safe, keep it hot and have awesome sex. The campaign has grown out of the need to produce accessible and targeted health promotion information for gay, bi and queer trans men who may not have the same level of sexual health knowledge and literacy as their cisgender male counterparts, but are engaging in similar kinds of sex. Ted Cook, campaign lead from PASH.tm explained why the GRUNT campaign is
so urgently needed: “This campaign is so important because trans men into men can’t often see ourselves reflected in sexual health campaigns that target gay men and don't meaningfully and explicitly include trans men, even though we are part of this community.”
GRUNT will consist of a website (www. grunt.org.au), a booklet, a series of posters, a postcard and social media images. The campaign features messages about condoms, PrEP, PEP, risk reduction, resilience and sexual health empowerment.
Ted Cook said “We hope to educate our community while unapologetically celebrating who we are and the guys we hook up with. GRUNT is about positive, accurate and contemporary sexual health information with tools on how to stay safe and have a great time with other guys.”
AFAO Chief Executive Officer Darryl O’Donnell welcomed the campaign, saying: “AFAO is proud to be working with PASH.tm to deliver this ground-breaking campaign. Trans men deserve access to quality sexual health information that is developed by them and for them. We’re exceptionally proud that GRUNT delivers that.”
“HIV is real for all of us. We need to do more to ensure trans men are included when we work with gay, bi and queer men so that we’re embracing everyone in our community and reflecting its real diversity,” O’Donnell said.
“I am so thrilled to see Grunt rolling out across the country.” Ted Cook said. “We have worked extremely hard over the last 12 months to develop this Australianfirst sexual health and HIV prevention campaign, developed by and for gay, bi and queer trans men. PASH.tm is run by a small number of volunteers who have poured so much passion, experience and expertise into GRUNT.”
GRUNT was made possible through funding from AFAO. The campaign will be launched across Australia, starting with Sydney on Thursday 25 August cohosted by ACON. The Melbourne launch will be co-hosted by VAC (Victorian AIDS Council) and Equinox Gender Diverse Health Centre on Friday 23 September, and Brisbane will be co-hosted by QuAC in Brisbane on Friday 30 September.
Aram Hosie, PASH.tm Chair said “We are extremely grateful to AFAO for their support in helping us develop this work and to state-based AIDS Councils and LGBTI health organisations around the country for helping us to get it into the hands of those who need it most, trans guys who are having sex with cisgender guys.”
To check out GRUNT, visit www.grunt. org.au or https://www.facebook.com/ pashtm

photo of ftm transmale model viktor belmont, taken by oliver yvng, on may 20th, 2015 in portland, oregon
Andrew Badcock, MindOut Mental Health Project Officer at Working It Out–Tasmania’s gender, sexuality and intersex status support and education service - writes about gathering the tools to promote inclusive language.
Inclusive language begins with understanding the meanings of the words we use or hear, and being confident to ask the person when we don’t know.
As this magazine recognises, not all men who are into men are gay. Some are straight, some are bisexual, and some don’t even see the need for a label at all. So when someone blatantly or ignorantly stamps you or someone else with the wrong label, it has the potential to be hurtful.
This is no different in other population groups of the LGBTI acronym, so while trying to ensure we use language that’s respectful, it sure doesn't mean we won't get it wrong from time to time.

Here's some quick suggestions to add to your toolbox of getting it right, or maybe passing them on to that mate (or mother) who doesn’t quite get it yet.
Firstly, grab the information from those in the know – aka the people who are part of these communities.
The National LGBTI Health Alliance has an inclusive language guide that explores what inclusive language looks like for respecting people of intersex, trans and gender diverse experience. This language is important because it ensures all people are welcome to participate in everyday spaces at work, schools, communities and services. Check it out here - lgbtihealth.org.au/ resources/inclusive-language-guide-
At Working It Out, we share existing content on beingproud.org.au, a website for Information and resources for Tasmanian parents and families of young people who are Lesbian, Gay, Bisexual, Transgender, Intersex, Sexuality Diverse and Gender Diverse. WIO also provides support and cultural awareness training through the development and delivery of programs in schools, aged care and mental health.
The Gender Centre is a NSW service committed to developing and providing services and activities which enhance the ability of people with gender issues to make informed choices. Their website has a great list of resourcesgendercentre.org.au
Then, learn the terms. There's different identities that better define someone's lived experiences than others. For example, some people use bi, heterosexual, straight, queer, gay, lesbian, or pansexual when identifying their sexuality. Someone may describe their gender identity as trans, bi-gender, agender, sistergirl, male, non-binary, cisgender, genderqueer or female. If you don't know what some of these mean, Google is a good place to start for their definition.
Then, stand up for other mates of the LGBTI communities. Often hurtful statements have come from gay men about other men in the GBTIQ communities – for example, if you hear hurtful or unkind statements about a mate who is bi or trans, stand up for them.
Finally, remember that everyone is different, and everyone’s experiences are real. The words someone uses to describe themselves might be considered disrespectful or hurtful for someone else. Listen to how your mate describes themselves, do they use he or she or they as a pronoun? do they describe themselves as a trans-man or just a man? Take their cues, and follow their lead, and you’ll find that using inclusive language is as simple as listening to the words around you.
Andrew Badcock MINDOUT! Mental Health Project Officer

AIDS is the long-term consequence of HIV (Human Immunodeficiency Virus) infection – it is what HIV turns into if it is not adequately treated. Australia has recently declared that AIDS (Acquired Immune Deficiency Syndrome) is no longer a public health issue thanks to the discovery of antiretroviral therapy (ART), and the successful disease prevention and health policies adopted since 1982, when the first case of AIDS was diagnosed in Australia. The peak of HIV epidemic was reached in the 1990’s when around 1000 Australians died from HIV each year. Professor Andrew Grulich from the Kirby Institute (UNSW) says that “nowadays AIDS it’s only a transitory thing for most people and once they go on treatment, they don’t have AIDS anymore”.
Despite AIDS being not a threat anymore in Australia, new HIV infections have been on the rise for 3 decades. Recently, however, PrEP (Pre-Exposure Prophylaxis) has been adopted as an HIV prevention
mechanism, resulting in the first decrease of new HIV infections in more than 30 years.
PrEP is a preventive treatment containing the anti-retroviral drug Truvada, the same drug commonly prescribed to HIV+ people to suppress the virus in the system. PrEP is currently the subject of intensive studies as it could provide an easy and accessible prevention to HIV pandemic, an alternative to condoms and significantly reduce new HIV infections, all aiming to meet the goals established by UNAIDS (www.unaids.org) for 2020.
A recent study investigated how efficiently PrEP therapy protects us from HIV with a trial where 557 HIV- participants voluntarily took Truvada for 48 weeks. The patients represented a heterogeneous sample of men who have sex with men (MSM) adopting unsafe and safe sex practices (with and without condoms). Two individuals became infected with HIV, and both took PrEP fewer than two doses per week (Liu
et al., JAMA 2016) showing that PrEP is effective when Truvada levels in the blood are high, but it might not be effective at lower levels. This reinforces the idea that PrEP cannot be used as an ad hoc strategy, compared with condoms, rather that it requires a adherence to dosage indicated by the physician in order to provide protection.
To add complexity to the puzzle, two separate cases presented in February and in October last year reported HIV infection of PrEP users despite showing good adherence to Truvada. Upon further examination, the HIV virus contracted was a rare mutated form resistant to Truvada, bypassing the defences offered although the drug level in the blood was ideal.
When replicating, HIV virus is extremely prone to copy itself in wrong ways, inserting random mutations in its genetic material. In humans, inserting mutations in our DNA could have very adverse effects, as is the case with cancer, even though in biology random mutations are the bases of evolution, where mutation upon mutation can eventually lead to a beneficial mutation. Similarly, HIV can evolve and overcome obstacles in the environment such as the drug in the blood stream. HIV drug resistance has been documented in the past in HIV+ patients with low adherence to treatment, and this leads eventually to HIV mutating and becoming resistant. In these cases, a different drug has to be prescribed to act in a different way to suppress the virus. For this reason, it is important that HIV+ people go on treatment and adhere to the dosage prescribed and test regularly. Correct treatment suppresses the HIV virus in the bloodstream making it “undetectable [u]”. Reaching an undetectable HIV status
(and maintain it) nowadays not only guarantees avoiding AIDS later in life but it is also a stepping stone to celebrate because HIV does not represent a burden anymore, and HIV+ people can regain a freedom often lost in a sense of shame and social judgement.
Having an undetectable viral load does not mean someone is cured from HIV, rather that the viral level in the blood is so low that there is virtually no chance of passing the virus onto another person. Also, Undetectable has been recently described by the media as the new “safe” sex due to the absence of the virus in the blood stream. Supporting this idea, the observational PARTNER study (Rodger et al., JAMA 2016) investigated the outcome of around 1200 sero-discordant partnerships (one partner HIV+ and one HIV-, homo- and heterosexual couples) practicing condom-less sex. The aim of this study was to investigate the rate of HIV transmission to the HIVpartner while the HIV+ partner was on ART with an undetectable viral load. After more than 55,000 condom-less sex acts, 11 HIVpeople became positive (although eight of them reported condom-less sex with other partners). None of the transmissions were phylogenetically linked with the actual HIV+ partner, which indicates that no transmission occurred within the couple, giving solid credit that ART is an efficient method to prevent HIV infections amongst sero-discordant couples.

Dr. Matteo Senesi Menzies Institute for Medical Research University of Tasmania
A
new campaign for young gay and same-sex attracted men

"OUTspoken" is a new nation-wide initiative, produced by the Australian Federation of AIDS Organisations (AFAO), for young gay and other same-sex attracted men.
OUTspoken is based around the website www.outspoken.org.au. The key resources for this campaign are a series of engaging and entertaining videos of young gay men sharing their stories. These young men share their stories on a range of topics such as coming out, meeting people and relationships, sexual health, HIV prevention, stigma, testing and sexually transmissible infections (STIs).
President of AFAO, Bridget Haire, points out the importance of specifically engaging with and providing information to young gay and other same-sex attracted men. "Young gay and same-sex attracted men are diverse, experiencing different degrees of awareness, ease, maturity and well-being related to sexuality. Targeting information to these men is vital because of the immediate impact it can have on young men who may have very limited knowledge and understanding about gay sex, risk and relationships. Attitudes and behaviours developed at this age are also strong predictors of behaviours in later life, informing long term health and wellbeing."
The OUTspoken campaign and the videos can also be seen in the community on social media and other website, and a series of posters. For more information, go to the website: www.outspoken.org.au

Q-Life, National
LGBTIQ web based and phone counselling and support service, everyday, 3.00 pm until midnight. P: 1800 184 527 www.qlife.org.au
Antidiscrimination Commission
Assists in pursuing claims of discrimination on grounds of sexuality, gender identity etc. www.antidiscrimination.tas.gov.au
Gay & Lesbian Switchboard
Confidential peer-based telephone counselling, information & referral service specifically for the GLBTI communities of Victoria & Tasmania. P: 1800 184 527 www.switchboard.org.au
Scarlet Alliance
Sex Worker Outreach Project. www.scarletalliance.org au
Sexual Health Service
Counselling, support, referrals & STI & HIV testing. P: 1800 675 859 (Free call) E:sexual.health@dhhs.tas.gov.au
TasCAHRD
Tasmanian Council on AIDS, Hepatitis & Related Diseases. P: 1800 005 900 (FreecallInformation,9am - 5pm) www.tascahrd.org.au
Tasmanian Gay & Lesbian Rights Group (TGLRG)
A community-based organisation campaigning for LGBTI human rights in Tasmania. Stall at the Salamanca Market every Saturday. www.tglrg.org
Tas Police LGBTI Liaison Officers P: (03) 6230 2111(Hobart)
P: (03) 6336 7000 (Launceston)
P: (03) 6434 5211(North West) www.police.tas.gov.au
TasPride
Dedicated to celebrating & uniting the Tasmanian GLBTI community as well as bringing you the annual TasPride Festival. www.taspride.com
Working It Out
Tasmania's sexuality & gender support & education service which also provides counselling & support for LGBTI Tasmanians, their friends & family. www.workingitout.org.au
SOUTHERN
Family Planning Tasmania
421Main Road, Glenorchy P: 03 6273 9117
Mon-Tue & Fri9:00am-5pm;Thur 9:00am-6:30pm http://www.fpt.asn.au
Provides free and confidential sexual health care to people of all ages. Services include: contraception, pregnancy counselling, sexual health checks, pap smears, information and referral.
Sexual Health Service
60 Collins St, Hobart P: 6166 0990 or Toll Free: 1800 675 859
Mon-Fri 8:30am-5:00pm. Clinic times may vary. http://www.dhhs.tas.gov.au/ sexual health/sexuaI_health_ service_ tasmania
Free and confidential counselling and medical appointments for any issues concerning sexual health.
Anglicare NSP Hobart
18 Watchorn St, Hobart P: 1800 243 232
Mon – Fri 12.30 am – 4.30 pm
The NSP provides free clean, sterile equipment, information, education, support and referrals to people who access the service. A 24 hr vending machine is located at the lower section of the building. There is a $2 fee for this service.
Nufit (Anglicare NSP) Glenorchy
436 Main Rd Glenorchy P: 1800 243 232
Mon – Fri 10:00 am – 4:30 pm
Nufit is an NSP which provides clean, sterile equipment, information, education, support and referrals.
The Link Youth Health Service and Head Space
57 Liverpool St, Hobart P: 03 6231 2927
Mon – Fri 9.:00 am - 5:00 pm
www.thelink.org.au
The Link offers free counselling. case management, support, information and referrals for young people aged 12-24 in regards to mental health, alcohol and drugs, sexual health and family planning. Outreach is also available. Free condoms and an NSP is also available for people aged 12-24.
Hobart Community Legal Service
Provides advice and representation to clients in areas such as: discrimination law, employment law, consumer credit, Centrelink disputes, and child support. They offer free evening information sessions at the Hobart office on Monday and Wednesday evenings from 6:00pm, where volunteer solicitors give information on all legal areas. Mon-Thur 9am-5pm; Fri 9am-lpm www.hobartlegal.org.au
Appointments are required for some services, ring ahead to find out.
166 Macquarie Street, Hobart P: 03 6223 2500
7 Station Lane, Sorell P: 03 6265 1911 Shop 3, Covehill Fair, Bridgewater P: 03 6263 4755
Flamingos Dance Bar
Tasmania's weekly dub committed to providing a tolerant, safe, informative and fun environment for people of alternative sexualities and their friends to be able to enjoy themselves and socialize in a non threatening environment. www.flamingosbar.com
NORTHERN
Shield
Uniting & Supporting Northern Tasmanian LGBTI youth www.shieldtasmania.org
Launceston - Family Planning Tasmania
269 Wellington St, Launceston P: 03 6343 4566
Mon-Fri 9:00 am – 5:00 pm http://www.fpt.asn.au
Provides free and confidential sexual health care to people of all ages. Services include: contraception, pregnancy counselling, sexual health checks, pap smears, information and referral.
Launceston - Sexual Health Service
34 Howick Street, Launceston 7250
P: 03 6777 1371 or Toll Free: 1800 675 859
Mon-Fri 8:30 am-5:00 pm. Clinic times may vary.
www.dhhs.tas.gov.au
Free and confidential counselling and medical appointments for any issues concerning sexual health.
Burnie - Family Planning Tasmania
1 Pine Ave, Upper Burnie P: 03 6431 7692
Mon, Wed & Thur 9:00 am-4:30 pm
www.fpt.asn au
Provides free and confidential sexual health care to people of all ages. Services include: contraception, pregnancy counselling, sexual health checks, pap smears, information and referral.
Devonport - Sexual Health Service P: 03 6777 1371 or Toll Free: 1800 675 859
Clinic times may vary.
Free and confidential counselling and medical appointments for any issues concerning sexual health.
Salvation Army Building
111 Elizabeth St, Launceston P: 03 63316760
Mon-Fri 8:30am-3:00pm
This is the only primary NSP in Northern Tasmania. The service provides non judgemental clean, ster access the service.
East Coast Queer life Support
(ECQLS) North East support association coordinating & providing services & social activities for GLBTI people.
Call Peter on 0467 000 748, or email ecqls.tas@gmail.com.
DS Coffee House, Red Velvet Lounge, Fleurty's Cafe, Restaurant Waterloo, Lebrina, Kusinat, Republic Bar, Criterion cafe, Lansdowne cafe, Retro cafe, Machine Laundry Cafe, Jackman and McCross, Basket and Green, Deloraine Deli, O'Keefe's Hotel, Stonies Fifties cafe, Fitzpatrick's Inn, The King of Burnie Hotel, Hotel SOHO, Restaurant Red, Pickled Evenings Indian Restaurant, Cafe Bozzey.
If you notice any details that are out of date in these listings or if you would like to add your details here, please call us on 03 6234 1242
