ALL THINGS VACCINE YOU’LL NEED THIS ONE DAY TAKE IT FROM A LOCAL
Rural Risk Factor

WINTER 2023
FEATURES
18
Rural Risk Factor
One rural community is speaking up on their need for health care as the challenges they face are representative of rural communities across the state. Fighting against the odds of high uninsured rates, local clinic closures and geographic barriers, Marathon, Texas, is saying there are still people out here, and they need health care.
By Alessandra Singh
26
You’ll Need This One Day
There are some lessons in school that might be worth holding onto. At least that was the case for Chris Gallagher, MD, (Medicine ’05) who has built a career upon what he learned in medical school.
By Alessandra Singh
DEPARTMENTS
5 Scope
the access gap to care.

9 Vitals
The telemedicine otoscope gives a HD look into health care.
31 Rounds
This small-town pharmacist offers more of a one-stop shop.
35 Update
Exposure to the struggles of nurses leads Christina Chen, DNP, APRN, in a new direction.
IN EVERY ISSUE
2 Health Matters
3 Feedback
36 Class Notes
Inside
NEAL HINKLE
ISSUE
Winter 2023
VOLUME 33 |
1
THE COVER
18 ON
The Marathon Health Center serves as the beacon of hope for this small community of Marathon, Texas, offering health care via telemedicine.
Photo by Neal Hinkle.
close
Providers get behind the wheel to
PULSE.TTUHSC.EDU | WINTER 2023 1
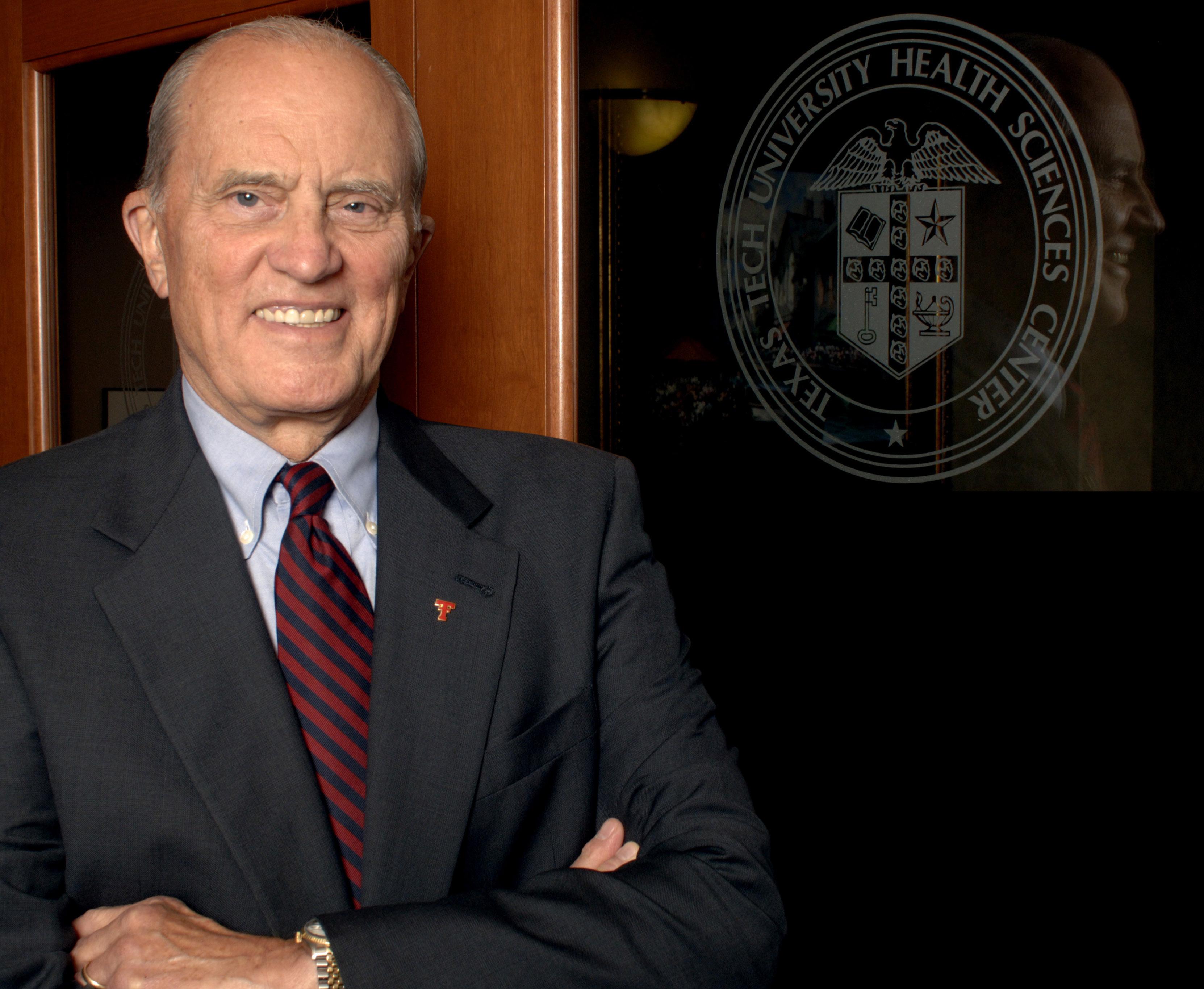
Taking Care of Those Who Take Care of Us
TTUHSC has made significant inroads in reducing the number of West Texas communities with little to no access to primary care, and we continue to seek innovative delivery models to address existing unmet health care needs.
One of the innovative models we have developed is to push health care into communities, as we did recently with Marathon, Texas. Historically, health care pulls services away from a smaller community, requiring residents to seek care in larger metropolitan areas. This type of model provides access to care but at an insurmountable cost regarding navigability by the user.
TTUHSC can push health care into a rural community by working collaboratively with their existing providers and utilizing telemedicine. We pioneered such a model and have used it for many years. Now, with telemedicine surging as a solution to health care shortages in the postpandemic landscape, the legislature is taking notice.
As recently as last month, presenting our legislative appropriations request with the Senate Finance Committee, I had the opportunity on multiple occasions to share with our state legislators and leaders TTUHSC’s efforts to address health care shortages in West Texas. We see the potential to enhance care through telehealth and are working with the Texas Legislature this session to secure $13.5 million over the next two years to establish an Institute for Telehealth Technology and Innovation. With our multiple campus locations, we can establish telemedicine hubs for increased collaboration in West Texas to expand care. In addition, our research experts can strengthen their work in examining the efficacy of health care outcomes, further improving health care via telehealth. Finally, the institute will enhance our academic expertise by preparing health care providers through training to use telemedicine and biomedical technology for care delivery.
TTUHSC is uniquely situated geographically to care for the people in this region, and we will continue to partner with the communities we serve to develop innovative models of delivering health care.
Lori Rice-Spearman, PhD, (Health Professions ’86) PRESIDENT TEXAS TECH UNIVERSITY HEALTH SCIENCES CENTER

Health
A Letter from Our President
Matters
ARTIE LIMMER
2 WINTER 2023 | PULSE.TTUHSC.EDU
We continue to seek innovative health care delivery models to address unmet health care needs.
EDITOR’S NOTE



The opportunity to share in this issue about the health care access challenges faced by those in rural communities took me home again. I grew up in a rural community about 30 miles south of Lubbock, Texas, and I remember hearing conversations between my mother, aunt and grandparents about trips to Lubbock for doctor’s appointments. At the time, I didn’t fully understand the hardships of schedules and transportation costs, etc. Fortunately, there was and remains a hospital and primary care access in my hometown, but that’s not the case for so many others in rural communities across Texas. I’m proud of the community partners TTUHSC has across the region, allowing for access to care closer to home. As Adrian Billings, MD, so poignantly notes in our cover feature, which starts on page 18, “a rural zip code (shouldn’t) be a risk factor,” for health care.





On another note ...
Congratulations! The West Texas Journal of Medicine (westtexasjom.org) published its inaugural issue in December 2022. David Shane Harper, DMSc, PA-C, FCCM, DFAAPA, physician assistant and faculty associate professor for TTUHSC Department of Surgery in Amarillo, began the multidisciplinary online research journal. The publication is independent of TTUHSC; however, many of our faculty experts serve on the advisory board. This is another voice in the conversation about medical and health science to serve critical health care needs of people in this region.
— Danette Baker, MA EDITOR-IN-CHIEF, PULSE OFFICE OF EXTERNAL RELATIONS
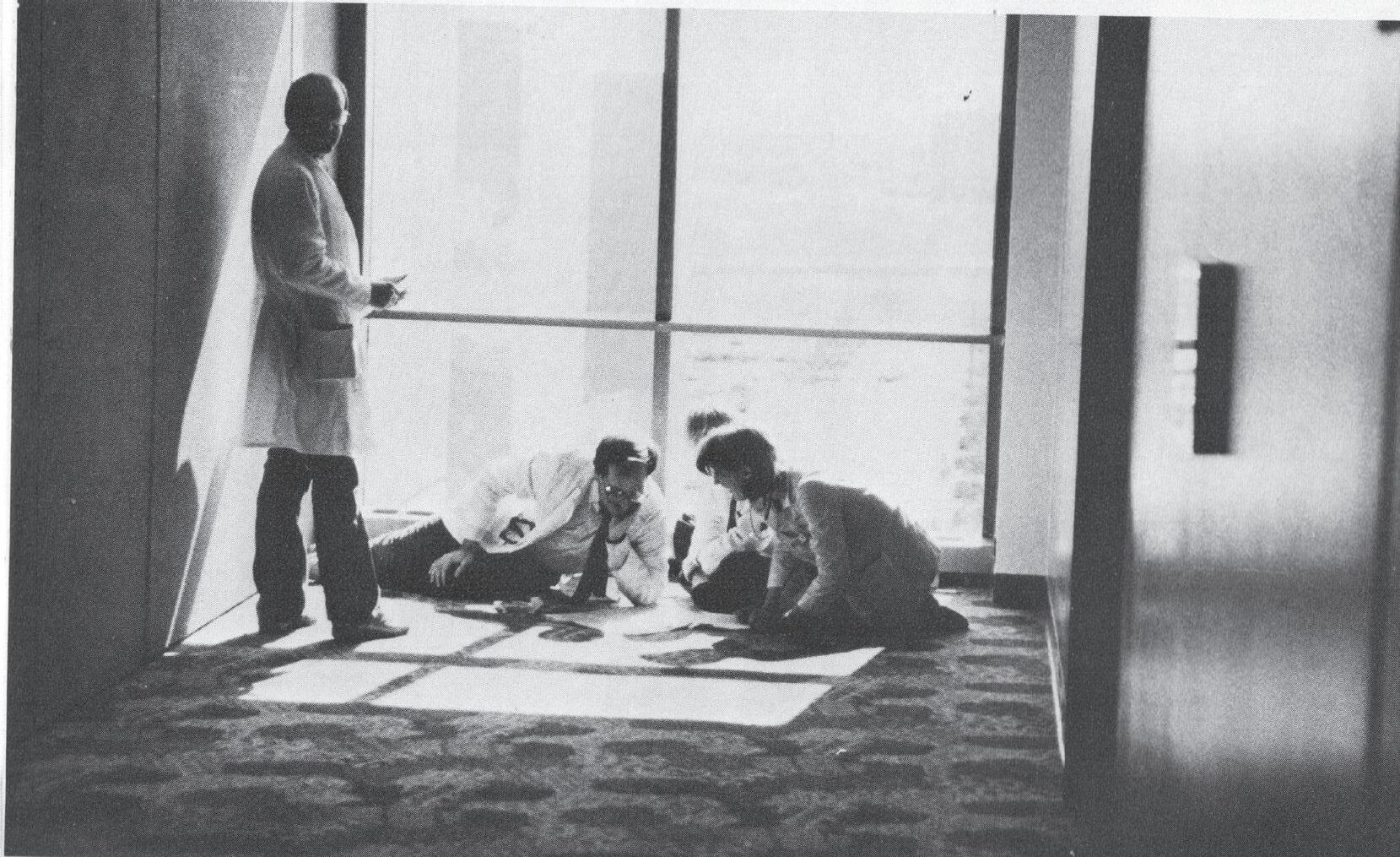
FROM THE PULSE ARCHIVES — SPRING 1989
You’re doing … a unique job in covering West Texas and in bringing medical education and all the good things that go with that into this part of the state.
— Jamie Clements, Chairman
DEAR PULSE, I love this information, and it is really well done! Appreciate what you and your team put together.
— Jean-Michel Brismee, PT, ScD (HEALTH PROFESSIONS ‘03)
DEAR PULSE, Well-done on the organization and execution of the article.
— Bevan Choate, MD (MEDICINE ‘05)
DEAR PULSE,
Did you happen to hear about the three nursing students and four faculty receiving TTUHSC Values Hero Coins? The group cared for a fellow passenger during their flight to the Philippines on a global health trip to care for patients there. They performed CPR for almost an hour on the person while inflight. The students and faculty were given the coins at the (School of Nursing) December graduation. I thought it was such a great story.
— Amy Moore, DNP, APRN, FNP-C PROFESSOR AND ASSISTANT DEAN FOR GLOBAL HEALTH TTUHSC SCHOOL OF NURSING
Volume 33, Issue 1
EDITOR-IN-CHIEF
Danette Baker, MA
MANAGING EDITOR









Alessandra Singh
DESIGN


Jim Nissen
CONTRIBUTORS
Susan Blystone, TR Castillo, Kim Catley, Suzanna Cisneros, Carolyn Cruz, Kate Gollahon, Tina Hay, Mark Hendricks, Neal Hinkle, Kami Hunt, , Artie Limmer
ADMINISTRATION
PRESIDENT
Lori Rice-Spearman, PhD (Health Professions ’86)

VICE PRESIDENT OF EXTERNAL RELATIONS
Ashley Hamm
ASSISTANT VICE PRESIDENT OF EXTERNAL RELATIONS
Mattie Been, Amarillo
Jessica Zuniga, Permian Basin
ASSISTANT VICE PRESIDENT OF COMMUNICATIONS AND MARKETING
Holly Russell
DEVELOPMENT
CHIEF ADVANCEMENT OFFICER
Cyndy Morris
GIFT OFFICERS
Kevin Friemel, Jill Hockenbury, Jordan Nabers, Clarissa Sanchez, Clifford Wilkes
ALUMNI RELATIONS
Peyton Sifrit
CONTACT US pulse@ttuhsc.edu
TTUHSC External Relations
3601 Fourth Street STOP 6242 Lubbock, TX 79430-6242
DENTAL AND ALLIED
SPECIAL COMMITTEE ON POST-SECONDARY MEDICAL,



 HEALTH EDUCATION FALL 1988 SITE VISIT
HEALTH EDUCATION FALL 1988 SITE VISIT
EDITOR’S NOTE: Values Hero Coins recognize TTUHSC students and team members for demonstrating extraordinary actions in showcasing the behaviors of our university’s values. The team’s work in the Philippines is highlighted in our 2022 issue, page 7. Thank you for sharing the rest of the story.
LETTERS TO THE EDITOR
Pulse welcomes thoughts and opinions from our readers via email at pulse@ttuhsc.edu.
Pulse is published twice a year. Content may be reprinted only with the editor’s permission. Discrimination or harassment based on race, color, religion, sex, national origin, age, disability, genetic information, status as a covered veteran or other legally protected categories, class or characteristics is not tolerated. Pulse is distributed in compliance with the State Depository Law and is available for public use through the Texas State Publications Depository Program. In compliance with HB 423. Pulse is also available in a digital format. If you no longer want receive the printed version, please notify the editor in writing.
THE MAGAZINE OF TEXAS TECH UNIVERSITY HEALTH SCIENCES CENTER THE MAGAZINE OF TEXAS TECH UNIVERSITY HEALTH SCIENCES CENTER THE MAGAZINE OF TEXAS TECH UNIVERSITY HEALTH SCIENCES CENTER
2022 ONE FOR THE RECORD BOOKS NEUROLOGICAL RESEARCH THE STROKE ARTIST
Feedback
PULSE.TTUHSC.EDU | WINTER 2023 3
the future belongs to
PROGRAMS OFFERED
Laboratory Sciences & Primary Care
Bachelor of Science in Clinical Laboratory Science
Second Degree Bachelor of Science in Clinical Laboratory Science
Post-Baccalaureate Certificate in Clinical Laboratory Science
Master of Science in Molecular Pathology
Master of Physician Assistant Studies
Rehabilitation Sciences
Master of Athletic Training
Doctor of Occupational Therapy
Post-Professional Doctor of Occupational Therapy
Doctor of Physical Therapy
Doctor of Science in Physical Therapy
Doctor of Science in Rehabilitation Sciences
Doctor of Philosophy in Rehabilitation Science
Concentration in Communication Sciences Disorders
Concentration in Movement Sciences Disorders
Speech, Language & Hearing Sciences
Doctor of Audiology
Bachelor of Science in Speech, Language, and Hearing Sciences
Second Degree Bachelor of Science in Speech, Language, and Hearing Sciences
Master of Science in Speech-Language Pathology

Healthcare Management & Leadership
Bachelor of Science in Healthcare Management
Master of Science in Healthcare Administration
Graduate Certificate in Health Informatics and Data Analysis
Graduate Certificate in Health Systems Policy and Management
Graduate Certificate in Healthcare Finance and Economics
Graduate Certificate in Health Systems Engineering and Management
Graduate Certificate in Long Term Care Administration
Clinical Counseling & Mental Health
Master of Science in Addiction Counseling
Master of Science in Clinical Mental Health Counseling
Master of Science in Clinical Rehabilitation Counseling
Texas Tech University Health Sciences Center School of Health Professions @ttuhsc_shp TTUHSC_SHP www.ttuhsc.edu/health-professions health.professions@ttuhsc.edu 806-743-3220
QUICK DOSE
TTUHSC TOGETHER FACULTY PROFILE FOR THE RECORD
Scope
Driving Access to Care
TTUHSC is using two mobile medical vans to improve access to health care for rural Texans in the Permian Basin. Medicine on the Move, launched in summer 2022, sends medical students, residents and fellows from the Odessa campus to provide blood pressure clinics, back-to-school vaccinations, health education and other services to underserved areas. The vans get the personnel and equipment to the site — the services take place at locations that include schools and churches. Permian Strategic Partnership and the Caring Foundation of Texas are partners in the effort.

PULSE.TTUHSC.EDU | WINTER 2023 5
News Views from TTUHSC
Web + Medicine on the Move initiative. NEAL HINKLE
Mental Health Check
Experts discuss the stigma around mental health and the importance it has in overall health.
DEI Research Grants
 Hollis Franco, PhD, RN, MEDSURG-BC School of Nursing Associate Professor, Assistant Dean of Wellness Lubbock, Texas
Hollis Franco, PhD, RN, MEDSURG-BC School of Nursing Associate Professor, Assistant Dean of Wellness Lubbock, Texas

Why do medical professionals need to be mentally healthy themselves?
FRANCO: “We all need to take care of ourselves and be mentally healthy to care for anyone else. If you don’t take care of yourself, how are you going to take care of others?”
What do you wish people knew about mental health?
FRANCO: “Everyone has mental health just like physical health, and as a society, we are doing better at decreasing the mental health stigma. No matter the circumstance, there is support for you. Please reach out.”
Sarah Wakefield, MD School of Medicine Associate Professor, Chair of Psychiatry Lubbock, Texas

What has helped raise awareness of mental health?
WAKEFIELD: “I think that COVID-19 pushed our society toward a breaking point where mental health became something that we could no longer hide; we had to talk about and then enough people were experiencing mental illness that it actually has reduced some of the stigma associated with it.”
How does a person’s location impact their mental health?
WAKEFIELD: “I think all communities have their strengths and their challenges. … But when you are unhealthy in a rural community, you have less access points to help get you well. You’re more isolated.”
At the intersection of health care and diversity, equity and inclusion, there is vast potential to understand how to continue providing the best care possible to all patients. The key to serving diverse communities is research. Grants totaling $112,000 were the first awards from the Office of Diversity, Equity and Inclusion in partnership with the offices of the Provost and Research. Eight studies are underway focusing on issues related to health disparities and to better serve minoritized individuals at TTUHSC. In September 2023, each project funded will have results presented at the TTUHSC Summit to Transform Healthcare for Everyone.
TOTAL APPLICATIONS FOR DEI GRANTS SUBMITTED
Scope 6 WINTER 2023 | PULSE.TTUHSC.EDU TTUHSC TOGETHER SARAH MAXWELL/FOLIO ART/STOCK IMAGE
22
Molly Minze, PharmD
Associate professor of Pharmacy Practice and associate dean for Student Affairs and Admissions for the Jerry H. Hodge School of Pharmacy

Molly Minze, PharmD, teaches fundamental pharmaceutical tasks with the goal of making students understand challenges that go beyond preparing the correct medication in the right dosage.
An associate professor of pharmacy practice at TTUHSC’s Abilene campus, Minze also emphasizes the need for future pharmacists to grasp how quickly patients can become overwhelmed as they frequently manage multiple prescriptions daily.
Minze is keenly aware of the patient’s perspective. She earned her Doctor of Pharmacy degree from the University of Houston College of Pharmacy and then completed residencies at Veterans Affairs Medical Center in Memphis, Tennessee, and Coastal AHEC and New Hanover Regional Medical Center in Wilmington, North Carolina. She works as an advanced pharmacy practitioner with Hendrick Health in Abilene. Students join her there and at practice sites where they experience the unexpected.
“Every day is different,” Minze said. “That’s why I’m passionate about the patient care aspect and helping students realize opportunities within the profession.”
Minze, who also is associate dean for Student Affairs and Admissions for the Jerry H. Hodge School of Pharmacy, is pleased the school offers eight experiential rotations that are among the most diverse nationwide. Each highlights options beyond the retail sector. “That’s what people know and see,” said Minze, an American College of Clinical Pharmacy Fellow who is raising awareness of opportunities, especially in rural areas.
“We need to help make sure folks are cared for where there is a dearth of health care providers,” she said. Pharmacists are often “the first triage” in such locations as individuals seek advice.
Preparing tomorrow’s pharmacy practitioners is a joy for Minze. “Our students are excellent, and I enjoy seeing the world through their eyes while I share my passion,” she said. “The future is bright.”
Scope PULSE.TTUHSC.EDU | WINTER 2023 7 NEAL HINKLE FACULTY PROFILE
STUDENTS ACROSS FIVE SCHOOLS PARTICIPATED IN A TELEMEDICINE PILOT PROJECT BY INNOVATIVE HEALTHCARE TRANSFORMATIONS (INHT) THAT TAUGHT STUDENTS TELEHEALTH PRACTICES FOR EXPOSURE TO THE CHALLENGES AND


OF IT.

Scope 8 WINTER 2023 | PULSE.TTUHSC.EDU FOR THE RECORD
“I don’t think there’s any cure better than prevention, and that is the main idea (in providing accessible health care to rural communities).”
– KEVIN THOMAS, MD, FAMILY MEDICINE RESIDENT
“The standards you all set for our health care in this community are really high, and I want to personally thank you for that.”
STEPHEN LOWERY, BOARD CHAIRMAN AT MIDLAND DEVELOPMENT CORPORATION
78 KAMI HUNT/STOCK IMAGE/PROVIDED BY WEST TEXAS AHEC
West Texas AHEC seeks to address the health provider shortage by encouraging young students to pursue health careers.
Stat!
ADVANTAGES
SCHOOL OF NURSING SCHOOL OF MEDICINE
JERRY H. HODGE SCHOOL OF PHARMACY
JULIA JONES MATTHEWS SCHOOL OF POPULATION AND PUBLIC HEALTH
GRADUATE SCHOOL OF BIOMEDICAL SCIENCES
SCHOOL OF HEALTH PROFESSIONS
Watch this!
Coming to a doctor’s office near you — your health care in HD. Ariel Santos, MD, MPH, director for the Texas Tech Telemedicine Program, says an exam via telehealth is as effective as the one you would receive in person. That’s because the technology in telehealth tools, such as an otoscope, delivers high-definition video, much like that you see on your television or computer screens. Sit back, relax and see what your physician sees as it’s displayed on the computer screen, but you might want to leave the popcorn at home.
Vitals
Signs from the Schools
4
3
The removable otoscope tip is used to see the respective areas during the exam, such as the inner ear or the throat.
1
Start by clicking the LED button (LED), which turns on a light for the tool.


2
Use the freeze frame button (FF) to create a still image from the live video feed for a particular spot that will allow the telemedicine physician to examine more closely.
With the LED light on, bring the tip of the otoscope, where the camera is located, to a white surface. Click the white balance button (WB), which will enhance the picture quality that appears.
PULSE.TTUHSC.EDU | WINTER 2023 9
NEAL
HINKLE
Virtually Real Health Care
A home health nurse visits an older patient recovering from knee surgery. The patient’s daughter is helping at home — but she might also be siphoning the patient’s painkillers for her own use. The patient has hearing loss and communicates with the daughter via American Sign Language, but the home health nurse suspects that the daughter isn’t translating everything, so she asks for help from a medical interpreter via telehealth.
Students who take the nursing course “Concepts of Community and Public Health” encounter this scenario in a simulation created by Amy Boothe, DNP, RN, CHSE, (Nursing, ’18), associate professor in the School of Nursing.

The goal is to help students understand issues involved in working with vulnerable populations. Boothe developed the telehealth virtual simulation with Brittany Hall, MS, CCC-SLP, (Health Professions ’05, ’03), assistant professor in the School of Health Professions Department of Speech, Language and Hearing Sciences; Emmanuel Sanchez, IT director for the School of Nursing; and Pedro Villa, CHSOS, in the Simulation department.
In the online class, students watch the video clips independently and then respond to on-screen questions about the scenario. The exercise prompts students to think about a range of issues, including how to conduct a health assessment, interact with vulnerable populations, use a medical interpreter, and identify red flags indicating possible opioid abuse.
Boothe has included virtual simulations in her courses for the past three years.

Vitals 10 WINTER 2023 | PULSE.TTUHSC.EDU ADOBE STOCK SCHOOL OF NURSING
The course gives students exposure to a vulnerable population — people who depend on somebody in some way or have some kind of barrier to receiving health care.
— AMY BOOTHE, DNP, RN, CHSE ASSOCIATE PROFESSOR IN THE SCHOOL OF NURSING
Future Physicians
EXPANDING THE SURGICAL TEAM

When Shelton Viney, MD, (Medicine ’77) first opened his practice in Midland, Texas, he saw an immediate influx of patients from Lubbock and the Permian Basin. At times, he said, there were only three surgeons taking on all major surgeries in the area. “I saw a real need for a residency program and expansion.”
After 40 years of private practice in Midland, Texas, Viney, regional chair of the Department of Surgery for the Permian Basin, is seeing the need fulfilled.
A COMMUNITY EFFORT
TTUHSC’s Permian Basin Surgery Residency Program with local surgeons and two hospital leaders created a communitybased consortium where local private practice physicians are
taking the lead to educate residents and train them in the operating room. “They’re doing it to give back,” Viney says, “and they see how the residency will benefit them in the future.”
THE FIRST CLASS
The Accreditation Council for Graduate Medical Education approved the Surgery Residency Program in April — after most physicians had matched for residencies. In July 2022, six residents — two each for the first, second, and third years — joined the program.

CHANGE IS COMING
“Having in-house surgery residents will mean quicker access for patients,” Viney said. “If a patient comes into the emergency room
and the surgeon on call is in a long case, we can send a resident down to evaluate them. It’s already helping a lot.”
Viney said the program also aims to train residents who will stay in the Permian Basin, providing necessary care for the numerous small towns that lack local surgeons.
A LEARNING EXPERIENCE THAT LASTS
After just four months, Tarek Behery, MD, a third-year resident, said they have worked on nearly 200 cases each, giving them an unprecedented level of experience.
“We’re all seeing consults, operating and getting face time with attendings early on,” Behery said. “That hands-on practice will ultimately be beneficial for our full five years.”
Vitals PULSE.TTUHSC.EDU | WINTER 2023 11 KAMI HUNT SCHOOL OF MEDICINE
What do you want to be when you grow up? Fifthgraders in Lubbock, Texas, explored opportunities in medicine at Doc for a Day.
“It helps them see people who look like them and shows them they’re capable of such careers as well,” said Skyler Thipaphay, secondyear medical student and program volunteer.
Medical student teaches fifth-grader through simulation.
All Things Vaccine
Information on whether or not you should receive a vaccine, potential side effects, efficacy data, the number of doses you’ll need, FAQ’s – it’s everything you need to know in one place. Minsu Kim, fourth-year pharmacy student, in conjunction with a pharmacy student from Purdue University created a document that will be implemented next year in all CVS stores called CVS Immunization Stretch Goals.

Vitals 12 WINTER 2023 | PULSE.TTUHSC.EDU JERRY H. HODGE SCHOOL OF PHARMACY
(The document) helps patients who are more curious to know more information about vaccines before they approach or ask the health care team. If they can have the information, like on their way around the store, it might even draw the eyes of people who never really thought about it.
— MINSU KIM FOURTH-YEAR PHARMACY STUDENT
NEAL HINKLE
Meet Pharmacy’s Third Dean
Grace Kuo, PharmD, MPH, PhD, said TTUHSC’s complexity drew her to the university. A passion for caring for underserved populations with a combination of rural and urban settings offers “great educational and service opportunities for our students, faculty and staff.”
Kuo joined TTUHSC on May 16, 2o22, as the third dean of the Jerry H. Hodge School of Pharmacy. Building on the school’s foundation, Kuo hopes to strengthen the pipeline of incoming students and stand out in a crowded field of pharmacy schools. She said academic offerings, such as the PharmD/ MBA, PharmD/MPH dual-degree programs and collaboration with the Texas Tech University School of Veterinary Medicine, will help increase TTUHSC’s visibility.

In addition, Kuo wants to prepare students for changes in the field and help them develop a solid professional identity.
“Pharmacists bring a unique set of qualifications and expertise. We are an integral part of the interprofessional team. We are here to help patients achieve optimal medication-related, diseasemanagement outcomes.”
CHEMICAL PROBE PATENT
Nadia German, PhD, director of the Medicinal Chemistry Program in the Jerry H. Hodge School of Pharmacy, and collaborators have received a U.S. patent for a chemical that targets the brain’s dopamine transporter. Modulation of the transporter’s activity results in changes in dopamine levels in the brain and affects one of the telltale signs – neuroinflammation – of Parkinson’s and Alzheimer’s disease.

Vitals PULSE.TTUHSC.EDU | WINTER 2023 13
Web + Learn more about the chemical probe patent.
JERRY H. HODGE SCHOOL OF PHARMACY
PROVIDED BY GRACE KUO/MARK HENDRICKS
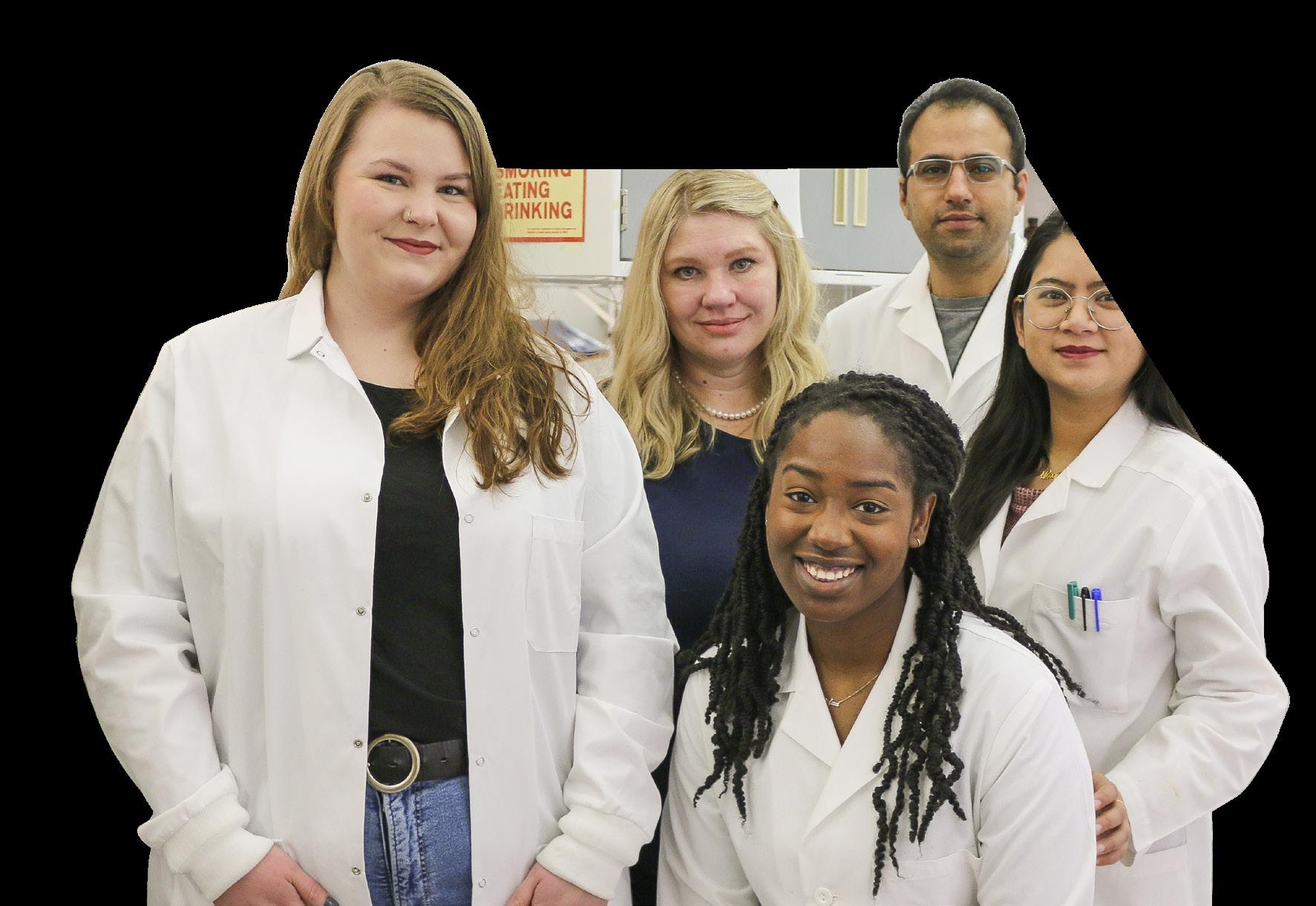
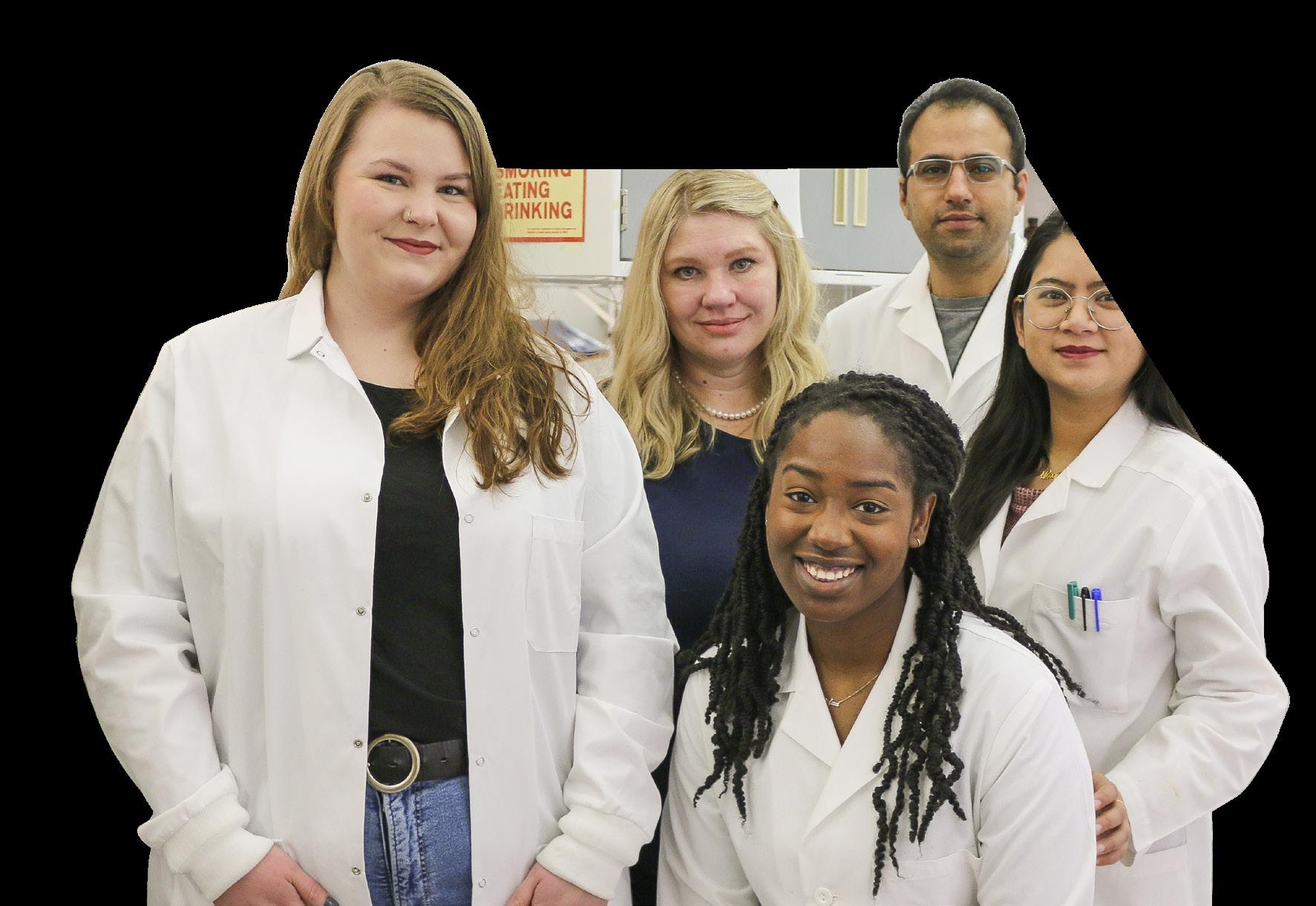
Nadia German, PhD, center, with her lab team.
DEEPER DIVE
Duke Appiah, PhD, MPH, associate professor for the Julia Jones Matthews School of Population and Public Health, is among the recipients of TTUHSC’s new Diversity, Equity and Inclusion grants for his research on health disparities in West Texas. Building on the foundation of his previous research focused on asthma, Appiah aims to explore other health inequities of medically underserved West Texas. He will focus on geographic, racial and ethnic health disparities that will contribute to “information for education (to students and faculty) and intervention (to public health officials).”
CARRINO TO SERVE AS INAUGURAL DEAN



Gerard E. Carrino, PhD, MPH, the inaugural dean for the Julia Jones Matthews School of Population and Public Health began duties Feb. 1, 2023. He previously served at Texas A&M University School of Public Health as head of the Department of Health Policy & Management. There, Carrino led the school’s interprofessional education efforts, oversaw the successful accreditation of its health administration program, and helped to build sustainable degree programs at the university’s McAllen, Texas, site. Carrino also has past senior leadership experience in research, administrative planning, project management and data analysis.
EDUCATION
PhD — Columbia University
Graduate School of Arts and Sciences
MPH — Columbia University
Mailman School of Public Health
BS — University of Akron
RESEARCH
Publications — 6
Presentations — 8
Vitals 14 WINTER 2023 | PULSE.TTUHSC.EDU JULIA JONES MATTHEWS SCHOOL OF POPULATION AND PUBLIC HEALTH
PROVIDED
BY
GERARD
E.
CARRIO, PHD, MPH/TR CASTILLO
Duke Appiah, PhD, MPH
Repurposing Drug to Treat Cancer

For much of the last two decades, Sanjay Srivastava, PhD, associate dean in the Graduate School of Biomedical Sciences, has investigated the use of drugs previously approved by the Federal Drug Administration and used by patients in clinics to treat other diseases such as potential cancer therapies.

His work recently earned Srivastava a U.S. patent for repurposing the antipsychotic drug pimavanserin, that acts within the brain to prevent hallucinations and delusions, to treat various types of cancer.
Srivastava, a professor in pharmacy, said the patent covers all applications of the drug in the field of cancer and would have to be considered as part of any cancer drug development process. The next step, he notes, is to conduct clinical trials to determine pimavanserin’s active effect against cancer in humans.
It generally takes at least five years before investigators are confident in the drug’s efficacy and safety profile; however, Srivastava believes the timeframe could accelerate with pimavanserin and given its prior FDA approval, “take the drugs to the patient much faster.”
CREATING A SOLUTION
Vitals PULSE.TTUHSC.EDU | WINTER 2023 15 GRADUATE SCHOOL OF BIOMEDICAL SCIENCES KAMI
HUNT/KAISER PERMANENTE WASHINGTON HEALTH RESEARCH INSTITUTE
Web + Learn more about the research of Sanjay Srivastava, PhD.
Schistosomiasis sickens more than 250 million people worldwide. Currently, there is only one treatment, Afzal A. Siddiqui, PhD, has spent 30 years working for a more effective treatment and reached Phase 1 of human trials. The study to evaluate the vaccine’s safety and immunogenicity, is expected to last through April 2024.
A study participant receives the first-ever shot of the SchistoShield investigational vaccine at Kaiser Permanente Washington Health Research Institute on May 23, 2022.
A Place for All
PA’S REACH OUT A HELPING HAND

Access to health care has never been more challenging for more than 3 million Texans who live in a rural area.
Physician assistants can help fill that gap and bring health care to remote, underserved communities. Thanks to a series of grants from the Health Resources and Services Administration (HRSA), an agency of the U.S. Department of Health and Human Services, TTUHSC is developing a Physician Assistant Rural Education and Community Healthcare (PA REACH) program to provide high-quality care in rural areas of West Texas.
ON-THE-GROUND EDUCATION
Site placements will give students the skills and knowledge they need to work in rural areas upon graduation. Typical clinical rotations are six weeks, but PA REACH doubles that time, allowing students several months to be integrated within the community. Students get a feel for common conditions and diseases, referral patterns and how to provide the best care.
“Rural West Texans have higher rates of diabetes, heart disease and hypertension than city populations,” said Christina Robohm-Leavitt, DMSc, PA-C,
Midland regional dean for the School of Health Professions and PA program director. “It’s also harder to get to health care providers, whether it’s primary care or specialists. This program helps provide additional expertise and providers in those areas.”

LOCALIZED CURRICULUM
Students will benefit from a deeper dive into health care disparities and mental health. In addition, a telehealth module will equip them to establish on-screen rapport and evaluate a patient without a physical exam.
Vitals 16 WINTER 2023 | PULSE.TTUHSC.EDU SCHOOL OF HEALTH PROFESSIONS
Inclusive, accessible and barrierbreaking describe the new Your Life Behavioral Health and Wellness Clinic. Barriers of language, distance and even the training of counselors to help with provider shortage are stopped short. The clinic provides behavioral health services for children and adult’s mental health and substance abuse needs in person and through telehealth counseling. Chris Townsend, PhD, LPC, AADC, Your Life Behavioral Health and Wellness Clinic director says, “the clinic is a place of diverse needs and a place of healing, restoration.”
Chris Townsend, PhD, LPC, AADC, in the new clinic.
NEAL HINKLE
Rural Health Care for People with Disabilities
People living in rural areas often have to go the extra mile to receive care — from traveling great distances on narrow country backroads to having limited available resources. And for people with disabilities who live in rural areas, these challenges are greater.
Taryn Richardson, PhD, NCC, CRC, an assistant professor in the Department of Clinical Counseling and Mental Health, said the issues faced by those delivering care in rural areas and persons with disabilities in rural areas can intersect and overlap. With geographic roadblocks, transportation can prove challenging in both cases. For those with disabilities, the challenges don’t end once they reach their destination.
They may face barriers, such as the site not being compliant with the Americans with Disabilities Act Accessibility Standards.
“For example, if they have a visual impairment, are there any resources in braille that they can take home?” Richardson “If they have a hearing disability or are deaf, are there interpreters available for services?”
“They may face instances when accessible resources are not supplied to help them to understand the care they are receiving.”
Persons with disabilities face physical barriers and issues with accessibility. Mentally, there is more. Although subtle, Richardson said they may face anxiety when having to go to a crowded facility.
In Richardson’s area, behavioral health and counseling, there is one goal in mind — “being able to enhance the quality of life for persons with disabilities in their communities.” Her area of expertise can’t do it alone,“We are one piece of a person’s overall well-being.”

Richardson stresses how important collaboration among health care providers and the communities is when it comes to providing quality care.
Assistant Professor Taryn Richardson, PhD, NCC, CRC
That is why it is essential for there to be awareness and advocacy, according to Richardson.
“Engaging with the community, and finding ways to adapt within the legal limits are vital,” she said. “Persons with disabilities want their voices to be heard with new policies and rehabilitation needs.”
“If we have people who feel well, they are more likely to participate in their community. If we support the needs of our clients and patients, it will come back to us (positively) in the long run.”
Vitals PULSE.TTUHSC.EDU | WINTER 2023 17 SCHOOL OF HEALTH PROFESSIONS
KAMI HUNT
Rural Risk Factor
Rural communities are asking for help in a state built on its industrial and agricultural way of life.
By ALESSANDRA SINGH Photographer NEAL HINKLE and KAMI HUNT
18 WINTER 2023 | PULSE.TTUHSC.EDU

PULSE.TTUHSC.EDU | WINTER 2023 19
Eliya and Elias Hernandez - the future of rural communities.

20 WINTER 2023 | PULSE.TTUHSC.EDU
Jody and Bob Freeman experience barriers to care.
risis. A word that has described rural health care since at least the 1980’s.
Defined as a time of intense difficulty, trouble or danger, a crisis in rural health care impacts 3.1 million people in 172 of Texas’ 254 counties.
In the last 40 years, rural Texas hospitals have become crisis casualties. In the 1960s, Texas had 300; today, there are 158. In the last decade, Texas has led the nation in closures — 26 hospitals have closed in 22 communities since 2010.
But “(the crisis) is not going to end when we say it’s going to end; it’s going to end when the rural community says it going to,” Adrian Billings, MD, PhD, chief medical officer of Preventative Care Health Services, a federally qualified health center in Marfa, Presidio and Alpine, Texas, and associate professor for the School of Medicine at the Permian Basin, says.
One community of 365 people – Marathon, Texas, – is not going down without a fight.
“There are still people out here, and we still need good doctors, and we need a system for health (care). A good system,” Ray Santos, a Marathon resident for 24 years, says.
It’s a thought his wife, Hilde Santos, echoes. “I really (worry) about our health care because there is nothing, nothing close, and doctors come and go.”
“They change like I change socks,” Ray Santos says.
“If we want to improve, we have to go through some kind of change,” Ivonne Durant, Ed.D, Marathon ISD superintendent, says.
Their pleads echo across the state. How will we respond?
GET THE FACTS STRAIGHT
Rural Texas has a lot to offer.
Jody and Bob Freeman, long-time Marathon residents, share the story of their grandson who begged them to never sell their house in this small community because he’s never seen stars before like he can see there. His ritual of sitting in the front yard at 2 in the morning, leaves him in awe — out here, the stars have room to shine.
Ray Santos describes this life as “heaven,” followed by a series of questions: “Where else can you sleep with the screen doors open, leave your car unlocked, and get up in the morning and hear nature?”
And there’s more.
“They have a saying here, ‘Big Bend is a great place to retire to and awful to grow old in’ because of health care,” Marci Roberts, director of the Marathon Health Center, says.
It’s a saying that could translate to other rural communities in Texas as the state earned an F for its fifth year in a row on rural access to care, according to the Rural Health Quarterly report card, a publication of TTUHSC’S F. Marie Hall Institute for Rural and Community Health.
The challenges rural Texans face is a 15.8% poverty rate compared to a 13.2% urban poverty rate. A 6% unemployment rate compared to 5.6% in urban areas. As of 2019, 22% of rural Texans have no health insurance, and the state has the highest uninsured rate in the U.S., according to the U.S. Census Bureau. All of which point to social indicators of health.
Also reported is an age-adjusted mortality rate in Texas rural
“Health care in our country, in our state, should be a right and not a privilege, and for rural residents, it truly is a privilege.”
C
ADRIAN BILLINGS, MD, PHD ASSOCIATE PROFESSOR FOR THE SCHOOL OF MEDICINE AT THE PERMIAN BASIN
PULSE.TTUHSC.EDU | WINTER 2023 21
areas that is 18.8% higher than the urban rate. The Texas Almanac notes the population loss increased from 79 to 94 Texas counties in 2010-2018 from the previous decade. Most of these counties are in the Rolling Plains and Panhandle regions, distal from larger urban conglomerations.
Health care is a struggle for most rural Texans; and that’s just not right.
“Health care in our country, in our state, should be a right and not a privilege, and for rural residents, it truly is a privilege,” Billings said.
TIME FOR A DIFFERENT LENS
As Ruben Ortega of Marathon puts it, to make a dent in solving the issues that rural Texans face with health care, “change is inevitable … you have to start somewhere and keep going.”
After multiple failed attempts at a clinic and hospital partnerships, Roberts took a 283-mile round trip to Odessa knocking on hospital doors begging for an out-of-the-box solution to Marathon’s health care needs. She was referred to Tim Benton, MD, regional dean for the School of Medicine at the Permian Basin, and discovered a partner and checked-off her last “to-do” in her community — find a sustainable form of health care through telemedicine.
Marathon residents Steve and Arlene Griffis say, it’s “the future of rural communities.” And now, it’s their reality.
IT’S NOT WHAT YOU THINK
Utilizing telemedicine can appeal to a lot of the challenges that currently face rural Texas communities, Ariel Santos, MD, MPH, director for the Texas Tech Telemedicine Program, said. It erases the issue of transportation and travel times since it can be conducted either in the patient’s home or at their local clinic. After factoring in the expenses saved from missing work, gas money, and possibly child care, telemedicine is cheaper overall, he says.
The misconceptions that surround telemedicine go beyond the myth of it being more expensive, Santos says. There is a lack of trust around conducting your medical business online, which he understands but prompts a question in response. “When was the last time you physically went to the bank?” According to Forbes, 78% of Americans prefer to do their banking digitally via mobile banking or bank website. “So, if you’re confident
enough to handle your money using virtual services, I think it’s kind of equivalent,” Santos says.
Santos also debunks the myth that telemedicine can only be done in certain cases. That’s not completely true. With the technological advancements that can accompany it via specific tools, even a physical exam can be conducted. Almost all specialties can be delivered, if we are creative, Santos says.
Lastly, although different from a traditional clinical exam, telemedicine is not just a Zoom call.
There are a lot of studies that say the quality of care given in the brick-and-mortar of a doctor’s office is equivalent to telemedicine with patient and provider approval rates similar, Santos says.
Telemedicine is also beneficial from a provider’s stand point, he added. With a nurse and physician burnout rate of up to 54%, according to the U.S. Department of Health and Human Services, telemedicine can be a remedy for seeing more patients in less time.
To bring virtual specialties to rural communities efficiently, medical professionals need to be trained in this type of care. Telemedicine needs to be integrated in our academic systems as part of our practice, Santos says. As the world moves forward, so does health care, and telemedicine is where Santos thinks it’s going.
THE IMPORTANCE OF RURAL TRAINING
Being exposed to the challenges rural communities and therefore rural physicians face is important. It helps those who join the medical world in urban areas better assist as they’re needed.
Although, Billings longs for his students to become rural physicians, he recognizes that isn’t everyone’s path. Still, he wants them to be prepared if someone like him calls at 2 in the morning with a critically ill patient. Training in rural areas will give “a much better understanding of the limitations of knowledge (and) the limitations of health care resources to care for that critically ill patient.”
Without this training, a medical professional in an urban area may struggle to put themselves in the shoes of a physician in a rural community with their unique challenges.
Ann Bass, MD, now a Lubbock physician, shares a story of a former patient in Littlefield, Texas, whose daughter had multiple ear infections. Every time the child needed care, the
“They have a saying here, ‘Big Bend is a great place to retire to and awful to grow old in’ because of health care.”
MARCI ROBERTS DIRECTOR OF THE MARATHON HEALTH CENTER
22 WINTER 2023 | PULSE.TTUHSC.EDU

PULSE.TTUHSC.EDU | WINTER 2023 23
Rural residents like Michael Stangl value quality local care.
mother and daughter would walk to the clinic because they didn’t have transportation. When Bass referred the child to a specialist, the clinic staff had to arrange a ride. The specialist used this first visit as a new patient consult and sent them home with a scheduled appointment to return for treatment. This was a common occurrence that frustrated Bass with her urban colleagues because they didn’t understand the plight faced by many in rural areas. “They are living near the poverty level,” Bass says. “And so, you’re asking them to take an entire day off of work or to drive an hour or more for care.”
Instances like this are why Billings believes all medical students should have rural health training, whether they’re planning to provide care in an urban or rural area.
THE BENEFITS TO WORKING IN RURAL HEALTH CARE
Rural health care is an area of the medical field that takes an independent person, Bass says.
Medical professionals are hard workers. It’s an attribute Bass recognizes as the foundation needed for those who want to
serve rural communities because of the health care shortage that leaves you on call 24/7.
There’s something that rural health care can offer that a lot of organized systems in urban areas can’t – freedom, Bass says. Without the overhead of a large hospital system, a medical professional in a rural area has the freedom to decide how to run the practice. Leaving room for a type of care that Bass defines as the most rewarding, and one in which she thrived – delivering what she calls some of her best care.
Billings says rural health care provides an amazing opportunity to have a more robust relationship and not be anonymous, going beyond the exam room, describing it as being “somewhere between a patient and a family member.”

When Bass worked as a rural physician in Littlefield, Texas, she reiterates Billings’ thoughts stating “There’s a sense of pride to belonging in the community with them.”
It’s the reason why Billings, Texas Academy of Family Physicians’ Family Physician of the Year, calls himself a “community physician” although his specialty is family
24 WINTER 2023 | PULSE.TTUHSC.EDU
Residents in Marathon, Texas, now have access to health care via telemedicine, connecting them with TTUHSC experts.
medicine. The residents whom Billings trains have been shocked by this feeling. Sharing a common answer in exit interviews when asked the best thing about their training are the relationships they were able to build with their patients.
HOW WE CAN HELP
In addition to the training of urban and rural health care professionals, communities can support health care pipelines beginning with local students.
Most of these rural students are diverse, often involved in multiple activities at once such as UIL, playing sports and playing in the band. So, we need to not only look at these students by their SAT and MCAT scores but also at how well-rounded they are, Billings says.
“That is what we want in health care. That is what we want in a civic leader,” he says. “These are the ones who have roots in rural communities and are most likely to return to either their own communities or similar rural communities in Texas.”
There’s a term that Billings coins from Paul Farmer, MD, PhD, a medical anthropologist and physician that Billings never met but calls his mentor from afar – accompaniment. Don’t come in the community as an expert trying to tell these rural communities what they must do.
TTUHSC’S LEGISLATIVE INITIATIVE
Since 1987, TTUHSC has been providing telehealth to people living in the predominantly rural West Texas area. With 35 years of service in this region, the university is proposing to the 88th Texas Legislature an opportunity to build on their experience and existing telehealth platforms through the creation of an Institute for Telehealth Technology and Innovation.
Focusing on three existing pillars, the institute will further TTUHSC’s initiatives in health care delivery, with a focus on rural communities: 1) increase access to care by collaborating with hospital partners in
“You really have to show up and accompany these rural communities and say, ‘This is who we are.’ Create trust, friendships,” Billings says.
Start with a question by asking them what they need as individuals and communities. It’s important to immerse yourself in the communities, “look them in the eyes and shake their hands,” Billings says.
For long-time Marathon residents Jody and Bob Freeman, they’re “excited to have (a telemedicine) facility (locally) because it’s 30 miles to the closest doctor just for a routine check-up.” A check-up that they almost can’t get unless they’re willing to wait, sometimes 30 days or more.
As a society, we have to agree on a basic foundation of care that will be available to all, and “if it cannot be in person, we (should) enable a telemedicine presence in these rural communities,” Billings says.
It can be an all-around good alternative to what we’ve called a crisis for too long – rural health care. “We have to embrace telemedicine and give it a chance,” Santos says. There’s no harm in trying when the system is already challenged.
Because “a rural zip code (shouldn’t be) a risk factor for a patient’s health,” Billings says
TTUHSC’s service area to expand specialty care and chronic disease management; 2) strengthen research and establish a way to analyze, examine clinical efficacy and health care outcomes; and 3) train future health care workers on telehealth best-practices using biotechnology in the delivery of care.
TTUHSC is moving toward establishing the institute with a recent one-time federal award of $2.6 million in the FY 23 Omnibus Appropriations Bill – led by efforts from U.S. Rep. August Pfluger – to purchase equipment for TTUHSC’s telehealth hub at
the Permian Basin campus. Equipment includes electronic health monitoring modules and computer hardware for a school-based module to utilize telehealth with TTUHSC’s partnerships of Ector County Independent School District and Medical Center Hospital while also providing health care access to 19 rural-based school districts in the Midland and Odessa area.
The university’s state request of $6.75 million per year, if approved by the Legislature, is part of TTUHSC’s non-formula base funding in the state budget.
“We have to embrace telemedicine and give it a chance.”
PULSE.TTUHSC.EDU | WINTER 2023 25
ARIEL SANTOS, MD, MPH DIRECTOR FOR THE TEXAS TECH TELEMEDICINE PROGRAM

26 WINTER 2023 | PULSE.TTUHSC.EDU
Chris Gallagher, MD, (Medicine ‘05) at Access TeleCare headquarters located in Dallas, Texas.
You’ll Need This One Day
Chris Gallagher, MD, (Medicine ’05) draws
from his experiences during medical school for
real-world application.
By ALESSANDRA SINGH Photographers CAROLYN CRUZ and ACCESS TELECARE
In a time with no streaming services, a flip phone in his back pocket and just happy to have DSL in his home, Chris Gallagher, MD, (Medicine ’05) experienced telemedicine for the first time and never forgot its impact.
Making rounds with Christopher Blewett, MD, in fall 2003, Gallagher witnessed the immediate relief he provided to an Alpine, Texas, family whose newborn had an abdominal wall defect. The uncommon condition stumped the local practitioner, who reached out to Blewett, a pediatric surgeon at TTUHSC. The family’s fear of the unknown was quickly put at ease by the telemedicine visit with Blewett that addressed the diagnosis, level of urgency and the infant’s prognosis.
Gallagher calls this the power of telemedicine – access. Watching the calm wash over this family through the ability to talk to a specialist, that they
otherwise wouldn’t have been able to do, is something he never forgot. “You have these moments in training where they just stick with you,” he said.
Fast forward 10 years, Monday to Friday, Gallagher is an academic cardiac electrophysiology fellow at UT Southwestern in Dallas, Texas. On the weekends, he is a moonlighting hospitalist in the rural East Texas 96-bed facility of Hopkins County Memorial Hospital in Sulphur Springs, Texas (now known as CHRISTUS Mother Frances Hospital – Sulphur Springs). For an entire year, every weekend Gallagher lived in a hospital room and ate cafeteria food — and looked forward to being there. Although doing cardiology and electrophysiology care didn’t quite make sense at the time in a rural setting, he couldn’t deny the passion he felt for his weekend practice. Gallagher left UT
Southwestern for a full-time position at the hospital and shortly thereafter became the chief medical officer.
Within a few months, the hospital’s challenge of not being able to keep and treat their critical patients locally became evident. They needed to build an ICU program that would alleviate this issue. After a long year of trying to recruit one pulmonary critical care physician — with no luck — Gallagher realized the approach needed to change.
Recalling the telemedicine visit with Blewett 10 years prior, Gallagher asked the hospital board to let him take a risk.
The hospital was transferring out 20-plus patients a month they could manage locally with access to specialists via telemedicine. With a forward-thinking mindset, Gallagher created Access Physicians in the fall of 2013, and a rural hospital serving a population more than
PULSE.TTUHSC.EDU | WINTER 2023 27
15,000 unknowingly established Texas’ first 100% virtual ICU.
On the third night of implementation, the medical team saved a patient’s life who months before would have been at another hospital. By 2015, the difference between nocturnal in-person care and telemedicine was nonexistent so the hospital transitioned to solely nocturnal telemedicine for ICU and hospitalist services. Patient care is still traditional with a physician doing daily rounds but now they visit via a TV monitor on a cart that pans, tilts, zooms and uses complementary examination tools.
It’s a form of medicine that Gallagher calls a team sport. Access Physicians
had a mission to fill the gaps in health care to the communities who would otherwise not receive it. It’s a model he continued to build on after stepping away from the hospital where he originally started it.
The tides began to turn for Access Physicians when the pandemic hit, and before the end of 2020, the company received multiple inquiries about an acquisition but one in particular stood out – SOC Telemed. In an article with D Magazine, Gallagher calls them an inspiration and the one they’ve been chasing.
SOC Telemed acquired Access Physicians for $194 million and after five
ABOUT ACCESS TELECARE
Providing quality health care while ensuring equitable access to specialists across the country. That is why a group of physicians established Access TeleCare, formerly SOC Telemed founded in 2004. Their vision: deliver high-quality specialty care via telemedicine for both in-patient and out-patient services.
HOW IT IS DONE
For in-patient care, a nurse rolls the telemedicine equipped cart into the patient’s hospital room. On that cart is a screen, comparable to a high-definition computer display monitor, in which you can see the telemedicine physician live


in their office, and a HD webcam remotely controlled by this physician.
The cart is equipped with diagnostic tools, much like those your physician would use in-person, such as a stethoscope. The images and live monitoring conducted in-person by a health care provider via these tools are visible to the telemedicine physician treating the patient. Chris Gallagher, MD, (Medicine ‘05) CEO of Access TeleCare, says the company makes the process uncomplicated with training.
On-site nurses facilitate the process and remain with the patient throughout the physician encounter. The remote physician has complete control over the cart’s functions and manages the exam.
months, Gallagher assumed the CEO role for the nation’s largest provider of acute care telemedicine. They’ve since rebranded as Access TeleCare, truly embodying Gallagher’s philosophy of the power of telemedicine– access.
“That access is for patients to have access to the providers they need when they need it. And that access is timely. Patients need urgent care when their condition demands it, not when it’s available,” he said.
“It’s access for hospitals. To really work at their fullest capabilities, they need to have a diversity of specialists on their medical staff to handle whatever comes through the door.”
Gallagher says, “For telemedicine to work, it has to be intuitive,” and that is why providers at each partner facility are trained on the proper use of the cart in a six-week orientation.
ACCESS TELECARE’S CORE SERVICE LINES
Cardiology
Hospitalists
Infectious disease
Neurology
Psychiatry
Pulmonary and critical care
Maternal-fetal medicine
Cardiac arrest (code blue)
28 WINTER 2023 | PULSE.TTUHSC.EDU
Now, serving and filling the gaps for 1,400 facilities in 50 states, Access TeleCare has an almost equal distribution at helping 52% rural facilities and 48% urban. Gallagher fostered a love for caring for those underserved in rural communities and continues to follow through on the promise to provide them with the quality health care they deserve.
Hendrick Medical Center in Abilene, Texas, an Access TeleCare partner, has struggled to recruit specialists in maternal-fetal medicine, Jacqueline Zimmerman, DO, an obstetrician at
Hendrick Medical Center said. Their out-patient support was good but in-patient was lacking services needed for their high-risk patients.
Through Access TeleCare, the patients and physicians now have 24-hour access to maternal-fetal specialists that are only a quick phone call away. As a physician herself, Zimmerman feels supported in the care she can provide with help from the Access TeleCare program, which she calls an asset and is thankful for.
“We really didn’t feel like we had any good alternatives until they came along.
So, it’s improved our quality of care, and we’re really happy with it,” she said.
For Gallagher, it’s rewarding to serve the rural communities and “really see the good and the help you can bring to the patients.” Knowing he has done this to an even further extent develops a degree of pride, but he’s also thankful for the cooperation and collaboration that made it happen with the “orchestra of health care professionals” behind it.
The book on telemedicine is still being written, he says, every day they look for new ways to be more efficient and “push what is possible.”

PULSE.TTUHSC.EDU | WINTER 2023 29
“Patients need urgent care when their condition demands it, not when it’s available.”
CHRIS GALLAGHER, MD, (MEDICINE ’05) CEO, ACCESS TELECARE
A remote physician in his office meets a patient with the help of in-person staff at a partnered facility.
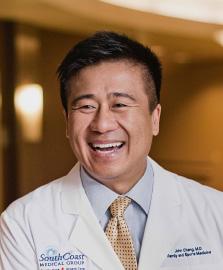
presidential distinguished alumni AWARD for HEROISM
john cheng, M.D.
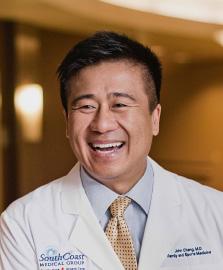


SCHOOL OF MEDICINE, 1995
The Presidential Distinguished Alumni Award for Heroism was presented for the first time posthumously to John Cheng, M.D., recognizing his heroism and celebrating his unwavering dedication to the service of others. On May 15, 2022, he saved dozens of lives when he tackled the gunman during a mass shooting in California. He was a 1995 TTUHSC medicine graduate and completed residencies at UCLA David Geffen School of Medicine and the Kaiser Permanente Southern California in Los Angeles. Cheng also completed a fellowship at the Kaiser Permanente Southern California in Fontana. He earned a reputation as an energetic student and resident who was deeply devoted to patient care and carried that same ethic to his practice at South Coast Medical Group in southern California.
presidential distinguished alumni award
Valerie E. Kiper,
DNP, MSN, RN, NEA-BC
SCHOOL OF NURSING, 2013
Valerie E. Kiper, DNP, MSN, RN, NEA-BC, received her Doctor of Nursing Practice in Executive Leadership from TTUHSC in 2013. She is an associate professor for the RN-BSN program at TTUHSC School of Nursing, and in 2021 became the first regional dean for the TTUHSC School of Nursing in Amarillo. Kiper has 43 years of nursing experience and 37 years of health care management experience in acute care settings, holding various executive and nursing leadership roles. Her past leadership experiences include roles as president and secretary of the Texas Organization of Nurse Leaders, representing the organization on various committees and serving on multiple local community boards. Kiper also formed a local nurse leadership group, which provides nursing scholarships and recognition for outstanding nurses in the Texas Panhandle and has become a model for communities across Texas.
Scan the code with your phone’s camera to see the 2021-20222 Distinguished Alumni Awardees and nominate candidates for 2023.

ROTATIONS COMMENTARY HEALTH SCENE
A Slice of Small-Town Life
Connecting with TTUHSC Alumni


NEAL HINKLE
Rounds
In 2019, Nathan Buerkle, PharmD, (Pharmacy ’09) bought Haskell Drug Store, fulfilling his dream of owning a pharmacy. But being in a small town means Buerkle does much more than fill prescriptions. Haskell Drug Store also houses a gift shop for bridal registries and a baby boutique.
“There are fewer options for certain products and services,” he said. “We want to meet the needs of the community.”
PULSE.TTUHSC.EDU | WINTER 2023 31
Scan with your phone camera to come along for a day in the life of a small-town pharmacist.
Take it From a Local
KAYTLIN KRUTSCH, PHARMD, MBA, (PHARMACY ’14) SHARES ON BRIDGING COMMUNICATION GAPS IN HEALTH EDUCATION.

Knowledge isn’t enough.
I’ve sat in meetings with pharmaceutical company representatives, researchers and health care professionals as they discuss how they’ve read, attended training, or conducted research and know what is best for their patients. Yet they struggle to get patients to trust their judgement and follow their advice.
As a pharmacist, I know how they feel. I was trained to specialize in medication knowledge, but I don’t prescribe — I advise. To effect change, I must convince someone else to make the decision. But how? As a health care professionals’ colleague, I hear the frustrations being unable to help those they’ve sworn to serve.
On the other hand, those they serve are my family and my community, whom I listen to express their distrust for decisions made for them by health care professionals. I’m a first-generation college student from the Texas Panhandle working on my second doctorate –this one in translational science. I left the region for part of my education and then returned to start a family and serve the community I grew up in.
I am the bridge between two worlds. I’ve listened to each group, laypeople and health care professionals, confidentially discuss their fears and frustrations without the filters they use when talking to one another. And, belonging to both groups, I can empathize with them both.
The best way forward is through understanding each other. Be a part of the community you serve. Take the time to listen to opinions different from your own and be curious and respectful about the differences. The future of health care is together.
Rounds COMMENTARY
NEAL HINKLE
Kaytlin Krutsch, PharmD, MBA, (Pharmacy ’14), is an assistant professor and researcher in the School of Medicine’s InfantRisk Center at Amarillo. She received the 2022 Jerry H. Hodge School of Pharmacy Distinguished Alumni Award.
32 WINTER 2023 | PULSE.TTUHSC.EDU
Scan with your phone camera to hear about TTUHSC’s grassroots presence.
Signs of the Times
CLEAR
WAY OUT
SIGNED WITH LOVE
3

CATCHING UP
4 |
MULTI-TASKING TEAMWORK
5 |

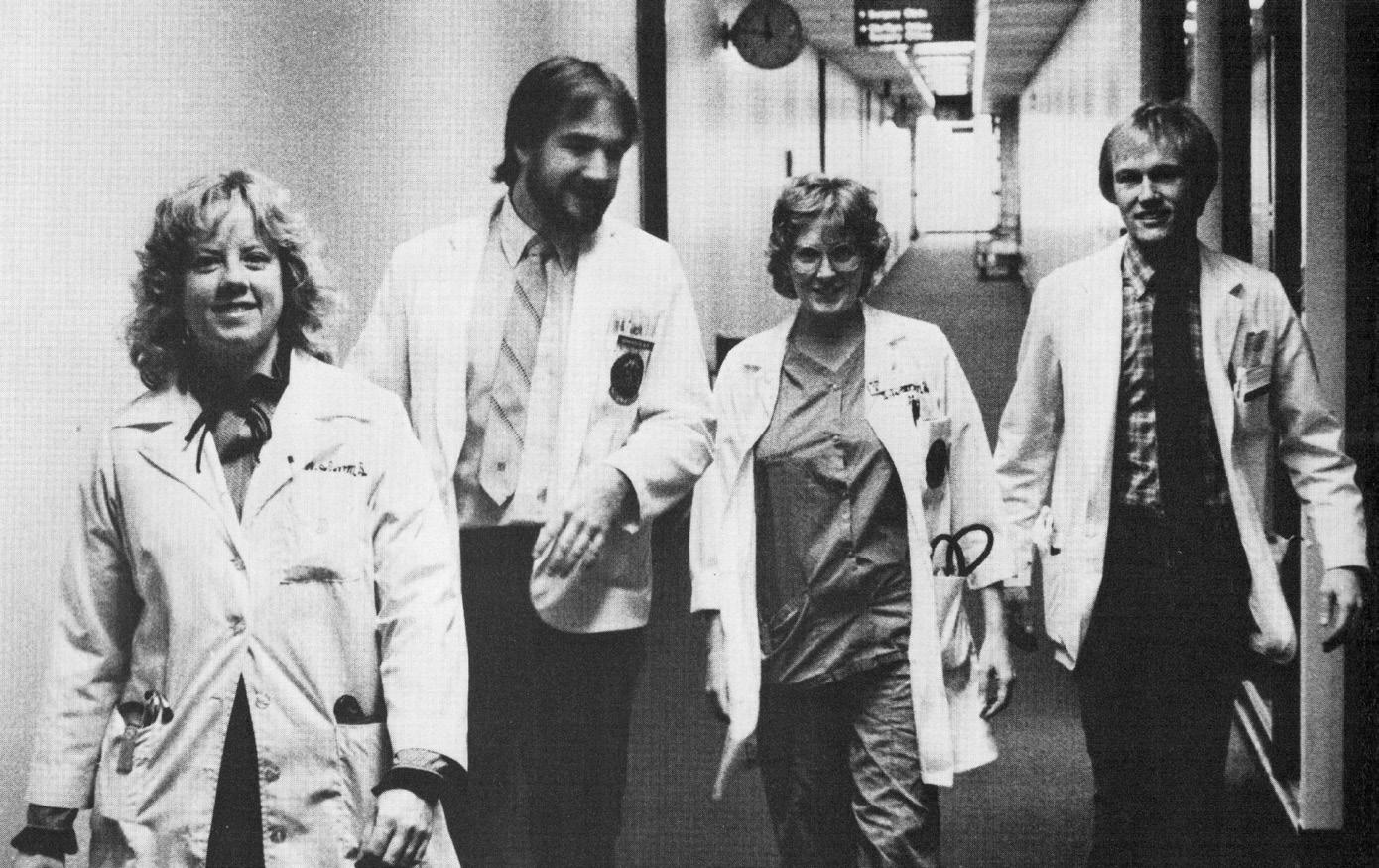
Rounds 5 4 3 2 1 HEALTH SCENE
PLEXUS, UNIVERSITY YEARBOOK
THE HALLS
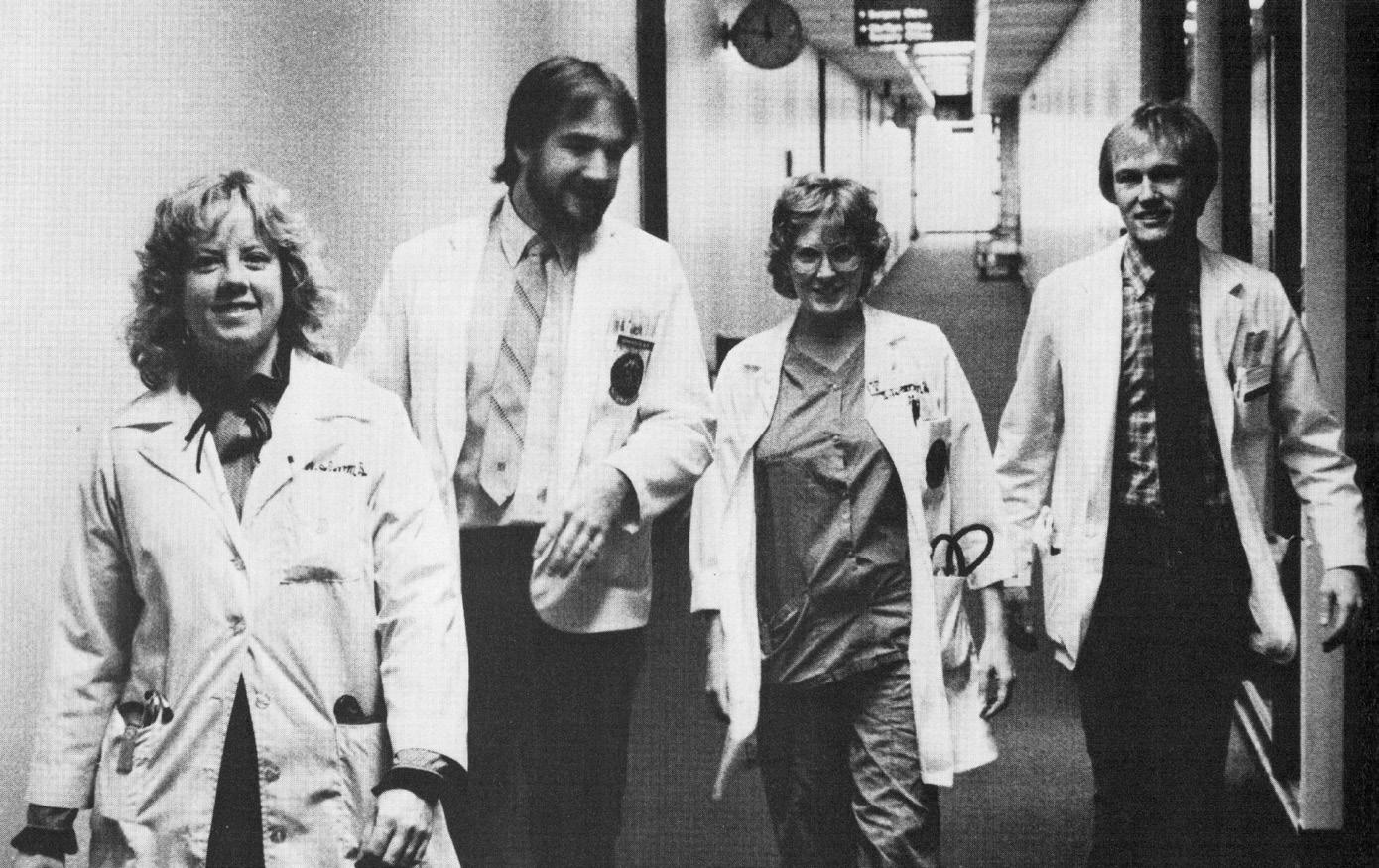
1 | Students in 1983 own the hall with their white coat strut.
YONDER
2 | The 1992 Lubbock campus connects to its agricultural roots as horses graze the field outside the building.
| It’s all about the hand signs as these 1990 students of occupational therapy show their love for TTUHSC.
In 1985, the Texas Tech University Daily (now the Daily Toreador) was the go-to for campus news.
This is multitasking in 1983 — catching some rays during group study session.
PULSE.TTUHSC.EDU | WINTER 2023 33
Gifts of Impact
From his first drawings as an intern — a hospital project in Amarillo, Texas — to his founding of Medica Development, LLC, Bill Persefield has forged a 45-year career as a renowned health care architect. Persefield’s goal is to work with only the best on his hospital ventures, and he asked TTUHSC to partner in helping deliver quality, innovative health care. He and his wife, Ellen, (TTU ’81) have included TTUHSC and the Texas Tech University College of Architecture in their estate planning and will establish a scholarship endowment to help ensure TTUHSC continues to recruit and train the caliber of health care providers for which it has gained statewide reputation.
To make your GIFT OF IMPACT, contact Nathan Rice, CFRE, at giftplanning@ttu.edu or 806.742.1781.
Learn more about smarter ways to give: www.ttusystem.myplannedgift.org

“Because of my deep love for the university and what it did for us, I wanted to continue that for others through our gifts, service and commitment.”
— WILLIAM “BILL” PERSEFIELD, AIA, ACHA, NCARB, (TTU ’77) CHIEF EXECUTIVE, MEDICA DEVELOPMENT, LLC
ALUMNI PROFILES NEWS & NOTES FRIENDS WE’LL MISS
Update
Catching Up With TTUHSC Alumni & Friends
Christina Chen, DNP, APRN, PMHNP-BC
CLINICAL ASSISTANT PROFESSOR OF PRACTICE
The Ohio State University, Columbus, Ohio Nursing Graduate: 2022, 2018
HEALING THE HEALERS
Upon application to TTUHSC’s Psychiatric Mental Health DNP program, Christina Chen, DNP, RN, PMHNP-BC, originally hoped to help veterans like herself.

Amid the program’s experiences, including a global pandemic, Chen saw other vulnerable groups in need. One specifically — the health care professionals themselves.
While a full-time graduate student, Chen worked in Lubbock, Texas, during the peak of COVID-19 as a night shift charge nurse for University Medical Center’s intensive care unit. Working exhausting hours, Chen recognized other nurses’ struggles.
“Everyone talked about ‘superheroes on the front lines,’” Chen says. “You might see us as superheroes, but we’re normal people on the inside.”
Now, she supports future nurses as a faculty member at The Ohio State University in Columbus, Ohio. Chen will use this time as a clinical assistant professor of practice to guide students — caring for those training to care for others — while she continues to pursue her long-term career as a mental health nurse practitioner.
— Kate Gollahon
PULSE.TTUHSC.EDU | WINTER 2023 35
THE OHIO STATE UNIVERSITY SCHOOL OF NURSING
GRADUATE SCHOOL OF BIOMEDICAL SCIENCES
Omar Ledezma, MS, (’22) joined Eurofins as a scientist II.
Shreyas Gaikwad, MS, graduate student, was awarded the Syngenta Fellowship Award in Human Health Applications of New Technologies.
Vadivel Ganapathy, PhD, faculty member and department chair in the School of Medicine, retired in Feburary.
Stephanie Palmer, PharmD PHARMACIST/OWNER
Borger Pharmacy, Borger, Texas Pharmacy Graduate: 2007
HAPPY TO BE HOME AGAIN
Ten years after Stephanie Palmer, PharmD, graduated from the TTUHSC Amarillo campus, she took on the challenge of purchasing and operating an independent pharmacy. Palmer opened Borger Pharmacy in the Texas community of approximately 15,000 where she was raised.

“I wanted to work in health care but also wanted a career that would allow me to have a family,” Palmer said, explaining why she studied pharmacy and opted to stop working in a retail chain.
“I saw there was a need here and an opportunity for me,” Palmer said. She and her husband, Luke Palmer, now nurture their 4-year-old son, Henry, while Palmer also cares for the community. She and a staff of eight know many customers by name as they provide a home-town service that makes each day rewarding. “As an independent pharmacy, we can offer a more personal touch and care for patients efficiently,” Palmer said.
— Susan Blystone
SCHOOL OF HEALTH PROFESSIONS
Rene Canas, DPT, (’00, ’11) named CEO of ClearSky Rehabilitation Hospital in Flower Mound, Texas.
Ben Shook, DPT, COMT, IAOM, (’11, ’00) launched a new website for his company, Axiom Physiotherapy, located in Austin, Texas.
Wadie Williams Jr., RRT, TTS, FAARC, (’10, ’07) retired from the Texas Military Department and the Texas State Guard.
Update 36 WINTER 2023 | PULSE.TTUHSC.EDU NEWS & NOTES
We are fortunate to have someone of (Jack Reynolds, MD) caliber to agree to join our clinic and hospital staff and hope everyone will help us welcome him home.
ROVIDED BY BORGER ECONIOMIC DEVELOPMENT CORPORATION
— CLAY VOGEL HOSPITAL ADMINISTRATOR AT COLEMAN COUNTY MEDICAL CENTER (CCMC)
JERRY H. HODGE SCHOOL OF PHARMACY
Steve Rodriguez, PharmD, (’01) serves as a member of the Board of Independent Pharmacy Advisors at Mark Cuban Cost Plus Drug Company, PBC.
Meredith Sigler, PharmD, (’13) named 2022 Dallas Faculty Preceptor of the year. She is a board-certified pharmacotherapy specialist and an TTUHSC assistant professor for the Ambulatory Care Division and practices at the North Texas VA Medical Center. .
JULIA JONES MATTHEWS SCHOOL OF POPULATION AND PUBLIC HEALTH
Courtney Queen, PhD, assistant professor, was part of a team who received one of the eight Presidents’ Innovative Startup Awards through the Innovation Hub at Research Park. The company, Advanced Codex Solutions LLC, is a noninvasive, low-cost mobile diagnostic tool for the early detection of melanoma and skin ulcers.
Duke Appiah, PhD, MPH, associate professor, named 2022 Alumnus of the Year and Alumni Fellow of the Year by the
University of Louisville School of Public Health and Information Sciences.
Ashley Sciba, MPH, BSN, RN, (’19) serves her hometown, League City, Texas, as the direcgtor of community health services at the Galveston County Health District.
Jillian Schley, MPH, (’22) is a reporting and monitoring specialist with Integral Care – the local mental health and intellectual and developmental disability authority for Austin, Texas.
SCHOOL OF NURSING
Michael Evans, PhD, RN, FAAN, TTUHSC School of Nursing dean, received the legacy award from the Texas Nurses Association.
Aaron Salinas, PM, DNP, (’21) named to the 2022 Emergency Nurses Association Connection’s 20 under 40 class for his contribution to nursing and his community.
Brenna Merrifield, DNP, APRN, FNP-BC, (’22) joined Mansfield Cosmetic Surgery Center specializing in cosmetic medical procedures and aesthetic skin rejuvenation.
Ivan Becerra, MD EMERGENCY PHYSICIAN
Basin Emergency Physicians, Odessa, Texas Medicine Resident: 2020/Fellowship: 2021
AT HOME IN A SMALL TOWN
For Ivan Becerra, MD, working as an emergency physician at the only hospital in Fort Stockton, Texas, can require skills that his urban counterparts often don’t need. That’s because Fort Stockton has very few specialists: There are no cardiologists, orthopedic surgeons, obstetricians or gynecologists. The hospital doesn’t even have an ICU.
“A lot of the procedures that, in a larger hospital, would get outsourced to another specialty, we get to do on our own,” Becerra says. “We probably set more bones and deliver more babies than an urban ER doctor would.”
That versatility appeals to Becerra. But he ended up in rural medicine almost by accident: He was finishing medical school when an interviewer at TTUHSC mentioned the school’s Family Medicine Rural Residency Track. Becerra applied and matched successfully. In 2020, he completed his residency and joined TTUHSC’s one-year fellowship in emergency medicine, and then returned to Fort Stockton, where he spent two years of his residency.
He loves the work and the relationships he’s built. “I’ve become attached to this community,” he says. — Tina Hay

Update PULSE.TTUHSC.EDU | WINTER 2023 37 NEWS & NOTES
THREE LITTLE BABES PHOTOGRAPHY
Cecilia Murillo, MD
FAMILY MEDICINE PHYSICIAN
Uvalde Memorial Hospital, Uvalde, Texas
Medicine Resident: 2020; Medicine Graduate: 2017
Biomedical Sciences Graduate: 2014
COMPASSIONATE CARE FOR COMMUNITIES IN NEED
Growing up in El Paso, Texas, Cecilia Murillo, MD, saw how underserved patients struggled to receive care, whether due to a lack of insurance or physicians. She developed an interest in working with underserved patients, which she fostered throughout her residency in Lubbock, Texas, and working in the TTUHSC Free Clinic during medical school.
Murillo — who now works in family medicine for Uvalde Family Practice Association — enjoys developing deep relationships with her patients and their families.

“I get to see what’s important to them,” she said. “It feels altruistic, like I’m (connecting) on a more human level.”
Those connections are also behind Murillo’s involvement in community efforts to advocate for gun legislation — a movement she joined after she served as a responding physician following the mass shooting at Robb Elementary School in May 2022.
“I feel like I’m doing work here that needs to be done everywhere,” she said. “We just had a tragedy that made it come to the forefront.” — Kim Catley
Aaron Salinas, DNP, MD, (’21) serves on the board for the Alliance of Nurses for Healthy Environments.
Whitney Owens, BSN, RN, (’22) joined BSA Hospital in Amarillo, Texas, as an oncology nurse..
SCHOOL OF MEDICINE
Milos Buhavac, MD, with Texas Tech Physicians of Lubbock, Surgical Critical Care team, named 2022 UMC Health System of Lubbock Attending of the Year.
Sue Rankin, NP, of Texas Tech Physicians Pediatrics of Amarillo, named to the Texas Nurses Association District 2 Hall of Fame.
Adrian Billings, MD, PhD, associate professor, received Clinician of the Year by the Association of Clinicians for the Underserved.
Brent Magers, FACHE, FHFMA, CMPE, retired in December 2022 as executive associate dean of TTUHSC School of Medicine and CEO of Texas Tech Physicians.
Paul Uong, MD, (Resident ’09) joined the Internal Medicine department at Kaiser Permanente Honolulu Medical Office.
Jack Reynolds, MD, (’20) will join the Coleman Medical Associates and Coleman County Medical Center on a full-time basis in August 2023.
Michael Campbell, MD, (’96) joined Ouachita County Medical Center in Camden, Arkansas, to provide obstetrics and gynecology services.
Nadia Aurora, MD, (’18) joins Jersey City (New Jersey) Medical Center as a family planning, preventive care and laparoscopic surgery specialist.
Alan Kaye, MD, PHD, received the American Interventional Pain Physicians Lifetime Achievement Award.. Jasmin Aldridge, MD, (’19) joined Lake Norman Medical Group Family Medicine Tall Oaks in Mooresville, North Carolina.
Ellen Hampsten, MD, (’08) assistant professor of Family Medicine in Amarillo, named a Fellow with the American Academy of Family Physicians.
Josee Guindon, DVM, PhD, associate professor in the department of Pharmacology and Neuroscience, has been named a honoree by the International Cannabinoid Research Society.
Sharmila Dissanaike, MD, (Residency (’06) department of surgery chair, has been elected as the American Burn Association president for 2025.
Update 38 WINTER 2023 | PULSE.TTUHSC.EDU NEWS & NOTES
PROVIDED BY CECILIA MURILLO, MD
Steven Spoonemore Jr., DPT
ACTIVE DUTY OFFICER, INTEGRATED PHYSICAL THERAPIST
U.S. Public Health Service, Southcentral Foundation, Anchorage, Alaska Health Professions Graduate: 2006

SERVICE ACROSS THE STATES
Steven Spoonemore Jr., DPT, has served three duty assignments with the Indian Health Service caring for Indigenous populations in Alaska, Arizona and New Mexico in the U.S. Public Health Service. He now works alongside the primary care teams at Southcentral Foundation, an Alaska Native owned nonprofit health organization serving almost 65,000 Alaska Native and American Indian people.
“I really appreciate the holistic, cultural way they approach health care and the opportunity to learn from their inclusivity of spirituality and the role of emotional components in managing health and wellness. Southcentral Foundation has been doing that for a long time, and now other health systems are learning from them,” Spoonemore said.
Signage at the 2008 American Physical Therapy Association conference introduced Spoonemore to the U.S. Public Health Service. Entering active-duty service, opportunities for advanced public health and fellowship training in orthopedic manual physical therapy provided a foundation to move into an integrated primary care, team-based role. He continues to work toward expansion of physical therapists as integrated primary care providers across the country.
— Danette Baker
FRIENDS WE’LL MISS
Joyce Badger died Dec. 19, 2022. She worked for TTUHSC as a correctional health social worker with at the John T. Montford Prison until retirement in February 2022.
Aaron Jiunn-Yeu Chen, MD, (’20) died Oct. 27, 2022. He was a Family Medicine resident at TTUHSC in Amarillo.
Mark Dame, EdD, MHA, CPHRM, FACHE, died Jan. 27, 2023. He was an associate professor at TTUHSC and executive with Texas Tech Physicians and the School of Health Professions Speech and Hearing Clinic..
Bernhard T. Mittemeyer, MD, died Jan. 25, 2023. He was a professor of urology and held multiple leadership roles at TTUHSC for almost 40 years.
Update PULSE.TTUHSC.EDU | WINTER 2023 39 NEWS & NOTES
KEVIN HEDIN PHOTOGRAPHY
(Sharmila Dissanaike, MD) is a strong educator and clinician serving the South Plains. We are proud that Dissanaike (is) appointed to this national role for her accomplishments as a front-running leader in surgery and burn care.
— STEVEN L. BERK, MD
DEAN, SCHOOL OF MEDICINE AND EXECUTIVE VICE PRESIDENT OF CLINCAL AFFAIRS
Scan with phone camera to make gifts in memory/honor of friends we’ll miss.


advertorial
the woman who would later become his wife. After graduation, he returned to Houston, but this time he realized the rush of the big city wasn’t for him.
“After 18 months, I decided I would take more of Lubbock’s kindness and less of Houston’s traffic,” Farhoud said. “I found that time is more valuable. You can spend that time with your family or doing things for yourself, or you can be stuck in big-city traffic.”
Just like the Troutmans, Farhoud found opening his own business to be a more feasible prospect by returning to Lubbock. He opened Clouds Hookah Sports Grill in November of 2019. “There is so much love and support for local businesses that I didn’t think I’d find here,” Farhoud said. “In Houston, it’s so huge that you get lost as a small business. But you add so much value in Lubbock by standing out and offering something different.”
Farhoud is now focused on sharing the values and quality of life that welcomed him to Lubbock, by attracting new residents to the city—his Houston-based family.

Jada Sanders grew up in Lubbock and attended Lubbock Christian University where she earned a nursing degree in 2013. After being content working in Lubbock and starting a family with her husband Matthew, 2020 changed everything.
“In the middle of COVID we realized we could move anywhere, so in June 2021 we moved to Wylie,” Sanders said. “We thought that because we’d be closer to the Dallas metroplex, there would be more

things to do, more opportunities for the kids and for our jobs. Life is short. We’ve always been here, so why not try something different?”
Though most family members and friends were in favor of her move to the Dallas area, some thought she was crazy.
“A lot of friends [and family] thought we wouldn’t make it long, but they didn’t think it would be just three months,” Sanders said. “It took a lot of courage to move away and to come back, but we don’t regret it.”
After moving away from Lubbock, Sanders experienced exactly what Farhoud came to realize about big-city life. She had so much more time in Lubbock. “Everything in the Dallas metroplex was so time-consuming,” Sanders said. “Also, here in Lubbock, you know your neighbors and people are just kinder.”
It’s easy to take the status quo for granted; the smiles, and the genuine care the locals of Lubbock show for one another. Sometimes you have to step outside of the forest to notice the trees you were surrounded by all along.
The Troutmans called Austin home for about a dozen years, Farhoud lasted almost two years in Houston, and the Sanders only made it three months before returning home to Lubbock. Even though they all had different chapters, each of them found their home to be in the “Hub City.”
#LUBBOCKLEADS
advertorial
NEW JOB? NEW BABY? NEW AWARD?
Have an entry you would like to see printed in our update listings?
Email: pulse@ttuhsc.edu

Respected leader, humble servant
“Bernie,” as he was known to so many, served TTUHSC for almost 40 years as a physician, professor and administrator. Before joining TTUHSC, he dedicated 28 years to his country, retiring as a lieutenant general in the Army and a highly decorated combat soldier. His military service also included serving as commanding general of the Walter Reed Army Medical Hospital —the highest Army appointment. Yet, above all this, he was a humble servant who greatly valued people and demonstrated that through service to his patients, his university, and his country.
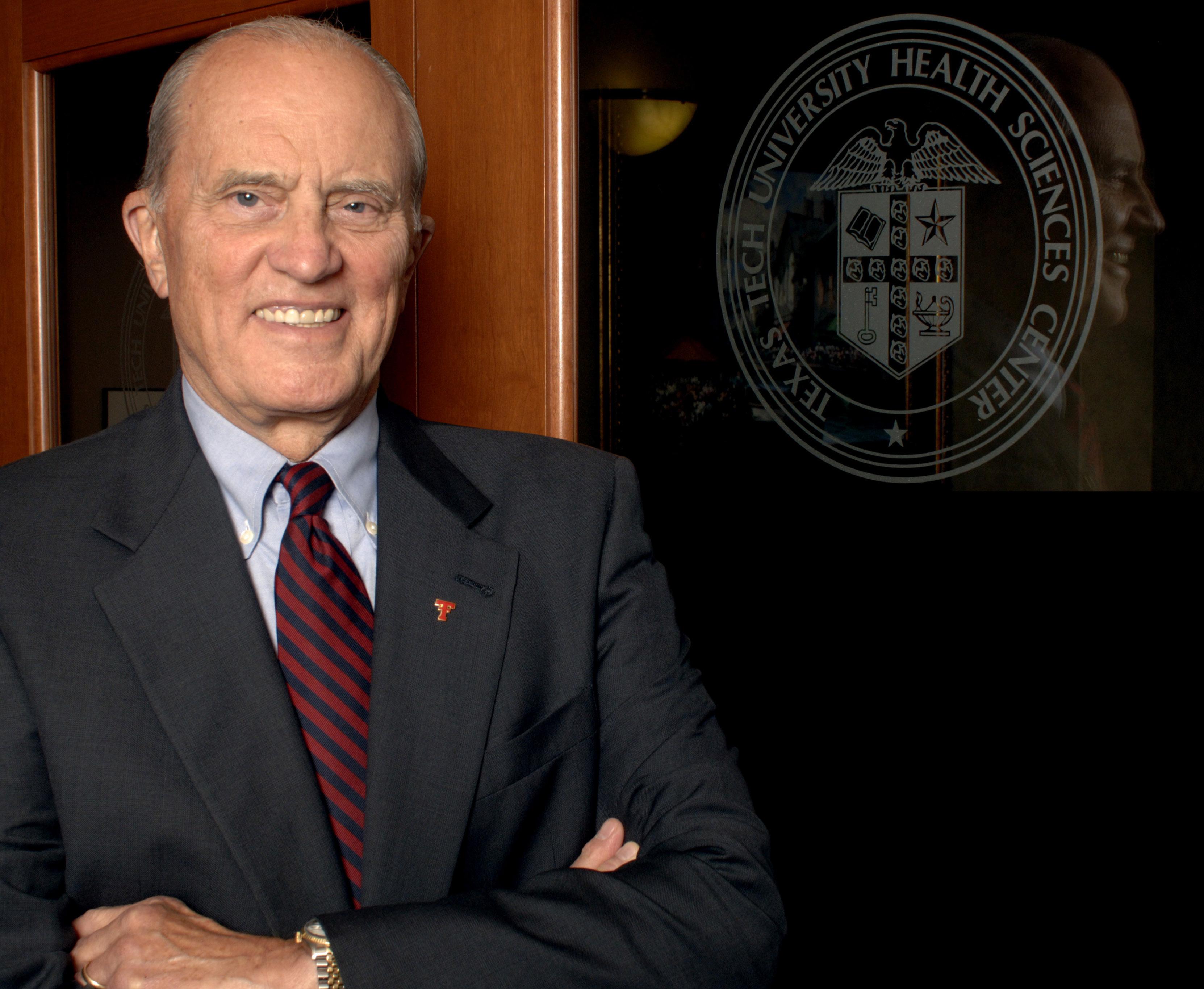
3601
FOURTH STREET | MS 6242 | LUBBOCK, TEXAS 79430
life of service:
T. MITTEMEYER,
Read more about his
http://bitly.ws/zBus BERNHARD
MD 1930-2023
Web +

























 HEALTH EDUCATION FALL 1988 SITE VISIT
HEALTH EDUCATION FALL 1988 SITE VISIT



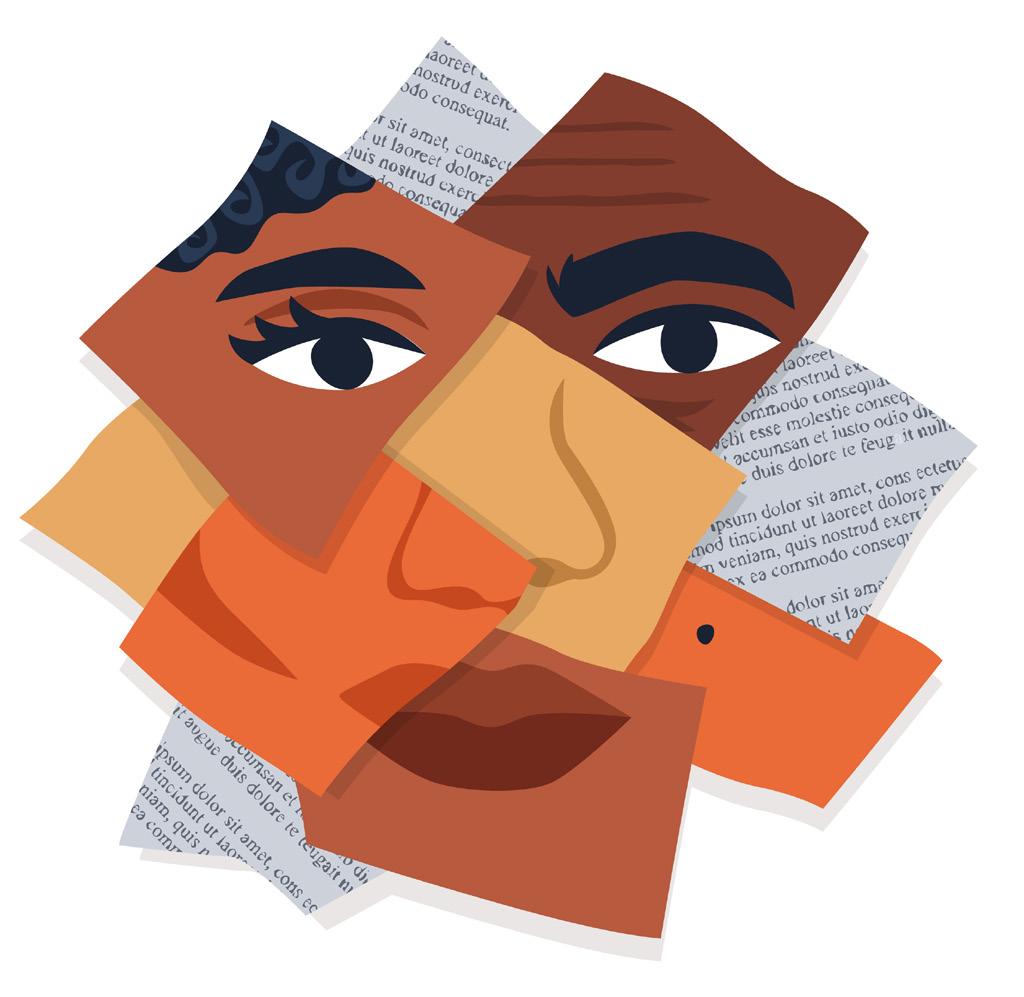 Hollis Franco, PhD, RN, MEDSURG-BC School of Nursing Associate Professor, Assistant Dean of Wellness Lubbock, Texas
Hollis Franco, PhD, RN, MEDSURG-BC School of Nursing Associate Professor, Assistant Dean of Wellness Lubbock, Texas