








earing loss in later life is still too often dismissed as an inevitable annoyance. The evidence shows this view is outdated. Untreated hearing loss is now recognised as an early warning sign of dementia and a modifiable risk factor that retirement operators and clinicians should not ignore.
Recent findings from the Framingham Heart Study underline the scale of the issue. Even mild hearing loss has been linked with smaller brain volumes, increased white matter changes and a significantly higher likelihood of developing dementia. The same research shows that older adults who use hearing aids reduce that risk, reinforcing the value of early intervention.
The 2024 Lancet Commission update again identifies hearing loss as one of the most critical late-life dementia risk factors, emphasising prevention through timely detection and treatment. Locally, the New Zealand Audiological Society has echoed this call, urging older adults and care providers to view ear and hearing health as essential to ageing well and staying connected to community life.
International evidence continues to build. A 2025 review of emerging research reported that up to one-third of dementia risk in older adults may be associated with measurable hearing loss. Randomised trials, including the Ageing and Cognitive Health Evaluation in Elders study, show that providing hearing aids and follow-up support can slow cognitive decline in high-risk older adults. At the same time, a recent UK study suggests millions of people over fifty are living with undiagnosed sensory loss, prompting increasing pressure for routine screening and mobile diagnostic services across primary care, clinics and long-term care environments.
For retirement villages and aged care operators, the implications are immediate. The National Foundation for Deaf and Hard of Hearing is currently fundraising to expand its Retirement Village Outreach programme to 140 villages, delivering on-site hearing checks and follow-up for residents

who may otherwise miss early signs of decline. In Australia, new surveys and field trials are testing integrated models of hearing and vision support in long-term care settings, from staff capability to environmental adaptation.
The operational lesson is straightforward. Hearing checks should be treated as standard baseline assessments when residents move in, reviewed every one to two years, and embedded alongside blood pressure screening, diabetes screening, and other routine health measures. Testing hearing before conducting cognitive assessments reduces the risk of misdiagnosing dementia when the underlying issue is hearing loss. It also ensures genuine cognitive changes are recognised sooner.
Early and consistent hearing assessment, supported by timely access to hearing aids, is one of the simplest and most effective tools available to protect brain health, independence and quality of life for older adults. Retirement providers who act early are positioning their residents, and their organisations, for better long-term outcomes.
Tania Walters, Publisher tania@reviewmags.com
PUBLISHER: Tania Walters
GENERAL MANAGER: Kieran Mitchell
EDITORIAL DIRECTOR: Sarah Mitchell
EDITOR-IN-CHIEF: Caitlan Mitchell
EDITORIAL ASSOCIATES: Sam Francks, Jenelle Sequeira
ADVERTISING SALES: Caroline Boe
SENIOR DESIGNER: Raymund Sarmiento
GRAPHIC DESIGNER: Raymund Santos Retail 6, Heards Bldg, 2 Ruskin St, Parnell, Auckland New Zealand P: +64 3040142 Email: edit@reviewmags.com

Acclaimed chef and television personality Michael Van de Elzen entertained the residents of Remuera Gardens with a special cooking demonstration, part of Real Living’s 40th anniversary celebrations.
The Government has agreed to an integrated approach to reform the aged care system, including the establishment of a Ministerial Advisory Group to recommend changes to the funding model, announced by Associate Health Minister Casey Costello and Health Minister Simeon Brown.

While the results from the Ageing and Cognitive Health Evaluation in Elders (ACHIEVE) study were negative across the total study population, the hearing intervention slowed cognitive decline by 48 percent in a prespecified subgroup of the study population comprising the 238 participants in an ongoing observational study of heart health.
Recent research from the University of British Columbia has explored how ageing well is connected to hearing well.
New Zealand and Australia have both issued the first trans Tasman guidelines for adult cochlear implantation and hearing care.








The National Foundation for Deaf and Hard of Hearing has been present throughout retirement villages, encouraging seniors to be proactive and face their hearing complications head-on.
Bupa New Zealand has released its first Sustainability Snapshot, showcasing progress made toward global sustainability targets while highlighting the local actions taken to create healthier communities, homes, and environments, and deliver a high standard of care to its residents during 2024.
A new research report released by WSP and the Helen Clark Foundation calls for urgent, coordinated action to prepare infrastructure, housing, healthcare, and social services for a future where as many as one in three New Zealanders may be aged 65 or older.
The New Zealand Green Building Council has supported the Government’s move to simplify rooftop solar installations and create a fast-track consent pathway for sustainable buildings.
The fundraising initiatives of Ryman residents were recognised after a record donation of NZD 520,517 was presented to charity partner Hato Hone St John on Wednesday.
Amid a sea of purple, the official colour of Alzheimer’s and Dementia awareness, a very special unveiling took place in the special care unit at Ryman’s Keith Park Village.
arlier this year, as residents in Ryman’s 49 villages signed up for the annual Walking for Wellness challenge, Ryman team member Paewai Tume (MNZM) embarked on his own impressive mission.

Bupa has found that access to nature, trees and walkable streets will help New Zealanders live their happiest life and feel healthy.
Anew Bupa Healthy Cities report reveals that three-quarters (75 percent) of New Zealanders said they live in the healthiest place for them, with access
For many, immune health has remained the top health benefit sought by consumers in food, beverage, and supplement choices.
According to Kerry’s ProActive Health Research, over 54 percent of global consumers actively seek to support their immune health through
diet, exercise, and lifestyle choices. In Asia Pacific, immune health claims are among the fastest-growing in new product launches, especially in sports nutrition, as athletes and active individuals look for products that deliver true, measurable benefits.
For parents in the
Middle East and Africa, 70 percent find immunity claims appealing on children’s products. Among older adults in Asia Pacific, maximising immunity is now a top health goal, with more than half of those over 60 consuming immunesupporting foods and supplements daily.
Read more online

New data has suggested that aorta dissection, the fatal cardiovascular condition, is missed in more than 50 percent of cases.
Recent research found that a diagnosis of aortic dissection is considered in less than half of patients who present with the condition. Early recognition is critical. If diagnosed and treated quickly, lives can be saved.
Aortic dissection, a tear in the wall of the blood vessel that supplies the whole body, is often fatal, with
to nature, trees and walkable streets topping the list of what makes a place feel healthy. However, the study exposes growing gaps between generations, genders, and regions and a deep concern that our cities are becoming less healthy and more crowded.
Read more online

90 percent of patients not surviving long enough before reaching a specialist centre. However, the signs of aortic dissection can be very difficult to spot, even for healthcare professionals. Clinical experts are urging that a CT scan is critical for a definite diagnosis, as other diagnostic tests cannot rule it out. Increasing awareness of aortic dissection and how it can be rapidly identified and accurately diagnosed is vital to save lives.
Read more online







Electronic prescriptions will now be introduced into the Australian healthcare system, following various industry-led calls. Ageing Australia has welcomed the decision by Department of Health, Disability and Ageing to grant a further extension for nonconformant Electronic Residential Medication Chart (eNRMC) vendors until December this year, following advocacy by Ageing Australia. Read more online
Some retirees considering luxury villages in 2026 are focused on independence, design, and meaningful living rather than facilities alone.
STIG Executive Director Scott Lester, Senior Trust Retirement Village Income Generator which provides secured lending to New Zealand’s senior living and aged care sector through financing of trusted operators, said the luxury segment has matured.
“People are not just buying into a location. They are choosing how they want to live, connect, and be recognised as individuals,” said Lester. Read more online



The newly appointed Aged Care Quality and Safety Complaints Commissioner, Treasure Jennings, has been welcomed by COTA Australia.
COTA Australia has welcomed the appointment of Treasure Jennings as Aged Care Quality and Safety Complaints

Commissioner, saying it is an important step to ensuring all older Australians get the quality aged care they deserve.
Treasure Jennings will take on the new role on 1 November, coinciding with the new aged care reforms.
Patricia Sparrow, Chief Executive of COTA Australia, the leading advocacy organisation for older people, said having Treasure Jennings in the important role of Complaints Commissioner will help ensure the rights of older people accessing aged care are front and centre of the system. Read more online
According to Infometric’s latest data, retirement units remain under significant pressure, with just 76 units approved in September. The
annual total of 1,220 consents is now at its lowest level since 2011.
There were 3,747 new dwelling consents issued in September, which, after seasonal adjustment, was the strongest result for any month since June 2023. Read more online
now locally available from our NZ Warehouse

Sterri-Matt® PPE Stations & Dispensers are the ultimate IPC solution with over a 100 versatile combinations to enhance your infection control programs

we also offer a wide range of Quad Glove Dispensers for added
& accessibility are also now available!








Acclaimed chef and television personality Michael Van de Elzen entertained the residents of Remuera Gardens with a special cooking demonstration, part of Real Living’s 40th anniversary celebrations.
ith his signature warmth and humour, Van de Elzen led a lively onehour masterclass filled with practical, wholesome recipes designed for busy retirement lifestyles.
“When we’re busy, the solution isn’t takeaways or Uber Eats, it’s going back to basics. Cooking simple food gives us confidence again. It takes the same time and energy to cook for one as it does for four, plan a little, make leftovers, and enjoy it. Cooking should be joyful, not complicated,” he said.
Van de Elzen has long been a champion for healthy, accessible cooking. He has strived to prove that nutritious takeawaystyle dishes can be made by using simple ingredients.
During the demo, he prepared Brown Rice Tuna Crunch Salad, Chicken and Lentil Soup, and a Leftover Vegetable Frittata with Homemade Tomato Jam.
His passion for food began at just 14, when he washed dishes at a Henderson restaurant. Captivated by the buzz of the kitchen, he soon worked his way up, later travelling to London and Ireland before returning to New Zealand to open several

successful restaurants.
In recent years, he’s dedicated himself to sharing his love of wholesome, easy cooking through television shows like “The Food Truck” and “Eat Well For Less”, radio, and his own cookery school.
After the cooking demo, there was a Q&A session where residents had the chance to ask Van de Elzen questions about his career, cooking philosophy, and life in the kitchen. Resident Mel Chitham asked him about the roots of his culinary journey.
“When I started washing dishes back in Henderson, I fell in love with the energy and teamwork of the kitchen. The food came later, but that buzz and collaboration is something I’m still chasing it 37 years on.”
Guests enjoyed tasting Van de Elzen’s creations, along with a delicious morning tea prepared by the talented chef who runs The Avenue Café on site.
Attendees said the event perfectly captured Real Living Villages’ philosophy that good food, laughter, and friendship are at the heart of every thriving community.

It takes the same time and energy to cook for one as it does for four, plan a little, make leftovers, and enjoy it. Cooking should be joyful, not complicated.
The Government has agreed to an integrated approach to reform the aged care system, including the establishment of a Ministerial Advisory Group to recommend changes to the funding model, announced by Associate Health Minister Casey Costello and Health Minister Simeon Brown.



mproving the lives of older people is a priority for the coalition Government,”
Minister Costello said.
“This announcement is about two things: better health outcomes for the 900,000 of us who are over 65, and a better, fit-for-purpose aged care system.
We know that New Zealand has very good aged care, provided by dedicated people.”
However, the Minister said the way these services are funded is outdated and does not recognise the connection between the various parts of the system or the future investment required.
“Essentially, our aged care model is out of date, and piecemeal change isn’t the solution,” she added.
“We want a system that provides the right type of care in the right place, and that
allows people to transition between these types of care, that’s easier to navigate and access, that’s fair, and that is sustainable and will endure as our population ages.”
Minister Costello said this would require long-term thinking and a bipartisan approach to solutions.
Associate Health Minister Simeon Brown said that there was widespread understanding of the issues within the current system. The Ministerial Advisory Group was now being tasked with identifying the changes necessary to build the aged care system New Zealand needs.
The expert Group will provide an independent report and a set of recommendations around three areas: the funding model needed to support sustainable services, particularly a

sustainable supply of aged care beds, how the costs of providing aged care could be reasonably shared between those receiving care and the Government, and the changes needed to support cohesion and integration between aged care services and health services, and between aged care and disability support services.
“Ensuring a sustainable supply of standard aged care beds is critical to ensuring all New Zealanders have the care they need as they age,” he said.
“The Government is committed to a bipartisan approach to addressing these challenges as part of the commitment in the National-NZ First Coalition Agreement.”
Costello added that these are significant policy issues, with major political considerations attached and that’s why an independent
group is required. The goal is that the Group’s recommendations will inform any future Government’s policy and funding decisions.
“We also need a system response that recognises most people want to stay at home if they can and allows them to access and move between the different levels of care they might need.”
The Ministers said that the Government was investing to ensure the on-going sustainability of the sector and continuing to drive operational improvements while the longer-term work was undertaken, with total funding to the sector increased by NZD 270 million in the last two years.
The Government expects recommendations from this advisory group by mid-2026, with changes to the funding model able to be implemented in 2027.
While the results from the Ageing and Cognitive Health Evaluation in Elders (ACHIEVE) study were negative across the total study population, the hearing intervention slowed cognitive decline by 48 percent in a prespecified subgroup of the study population comprising the 238 participants in an ongoing observational study of heart health.

he ACHIEVE study is a randomised trial of older adults aged 70-84 with untreated hearing loss who were free from substantial cognitive impairment.
In total, 977 participants were recruited from two study populations: 739 healthy community volunteers newly recruited to the study.
According to the researchers, at the start of the trial, all study participants generally had mild to moderate hearing loss very typical of older adults, but no substantial cognitive impairment.
The three-year intervention included the use of hearing aids, a hearing “toolkit” to assist with self-management, and ongoing instruction and counselling with an audiologist. The comparison group health education control group had talk sessions with a health educator about chronic disease prevention. The total study population was analysed, hearing intervention versus health education control; the ARIC and community subgroups were also analysed in this manner. The primary endpoint was the
three-year change in a comprehensive neurocognitive testing battery, which included procedures to help ensure that hearing loss would not affect the results.
The results of the comparison of hearing intervention versus control in the total study population were negative, as was the community population comparison of hearing intervention versus control. The most interesting result was the comparison of the ARIC subgroup hearing intervention versus control, in which a 48 percent slowing of cognitive decline was observed.
The researchers noted that the participants from the ARIC study had more risk factors for cognitive decline, lower baseline cognitive scores, and a faster rate of three-year cognitive decline during the study than the others.
“The positive results with the hearing intervention in the ARIC subgroup analysis are encouraging and warrant further investigation,” said Maria C. Carrillo, Ph.D., Alzheimer’s Association chief science officer.
“Previous research has identified hearing

loss as potentially the single largest dementia risk factor that can be addressed or modified with existing tools that remain underutilised.”
The ACHIEVE researchers cite hearing loss as present in 65 percent of adults over age 60. Identifying dementia prevention strategies that can be implemented globally is an urgent priority.
“The hearing intervention had a significant effect on reducing cognitive change within three years in the population of older adults in the study who are at increased risk for cognitive decline,” said Frank Lin, M.D., Ph.D., of Johns Hopkins University School of Medicine and Bloomberg School of Public Health, and coprimary investigator of the ACHIEVE study.
“Hearing loss is very treatable in later life, which makes it an important public health target to reduce risk of cognitive decline and dementia, along with other dementia risk factors such as less education in early life, high blood pressure, social isolation and physical inactivity.”
Carrillo added that the encouraging
subgroup results are consistent with the understanding that strategies to reduce cognitive decline and dementia risk will likely need to affect more than one pathway to be successful.
Findings from the ACHIEVE study suggested that older adults at increased risk for cognitive decline and dementia who also have hearing loss may benefit the most from this hearing intervention within three years. According to the ACHIEVE researchers, the hearing intervention may slow down the decline in thinking and memory by making listening easier for the brain, or by helping people remain more socially and physically active.
“In both the ARIC group and the new group of community volunteers, we also found that the hearing intervention improved communication abilities, social functioning and loneliness,” Lin said.
“Until we know more, we recommend for general health and well-being that older adults have their hearing checked regularly and any hearing issues properly addressed.”

Recent research from the University of British Columbia has explored how ageing well is connected to hearing well.
r. Kathleen Martin Ginis, director of the UBC Faculty of Medicine’s Centre for Chronic Disease Prevention and Management and a professor with UBC Okanagan’s School of Health and Exercise Sciences, worked with colleagues from Johns Hopkins University on a study investigating the link between a senior’s hearing and their physical activity level.
Using data from an American National Health and Ageing Trends Study (NHAT), the research team studied the association of hearing loss with activity level. More than 500 older adults participated by
wearing accelerometers for one week and self-reporting their vigorous physical activity and walking exercise for one month.
Dr. Martin Ginis explained why studies like this are necessary and the important link between hearing capacity and keeping active.
“Hearing loss is associated with frailty, poorer physical function and falls. Low levels of physical activity are also related to these health problems. There has been very little research on whether physical activity levels and hearing loss are related in older adults, and whether the use of hearing aids makes a difference,” she said.

Hearing loss is associated with frailty, poorer physical function and falls. Low levels of physical activity are also related to these health problems.

Dr. Kathleen Ginis Director, UBC Faculty of Medicine's Centre for Chronic Disease Prevention
“If we can determine that link, then health-care providers can better support older adults in maintaining an active lifestyle, and researchers can focus on studying the impact of hearing interventions.”
There are several potential mechanisms through which hearing loss may contribute to physical inactivity. These
include a decline in the perception of environmental auditory cues while moving about, a feeling of social isolation and increased allocation of cognitive resources for listening, leaving limited attention for simultaneous tasks.
Think about the places where older adults might go to do physical activity, to community centres, public swimming pools, for walks in their neighbourhoods. If their hearing is impaired, it is going to be difficult to interact with fitness leaders or staff in these public spaces, and it may even be frightening or dangerous to move about the community if seniors can’t hear what is going on around them. These factors will limit a person’s activity levels.
The study found that older adults with hearing loss engaged in less physical activity than those who could still hear well. As hearing loss increased, the number of minutes of physical activity performed each day decreased. The good news, however, was that among adults with hearing loss, those who used a hearing aid were more likely to report that they walked for exercise compared to those who did not use a hearing aid. These patterns held for both men and women in the study.
New Zealand and Australia have both issued the first trans Tasman guidelines for adult cochlear implantation and hearing care.

he new guideline has aimed to accelerate timely identification, consistent referral, transparent candidacy decisions and coordinated rehabilitation, so adults are not left isolated by untreated hearing loss.
Developed through a trans-Tasman collaboration of more than 70 clinicians, researchers and people with lived experience, the guidelines localise the Global Living Guidelines to New Zealand’s health system, providing a national pathway from referral to long-term follow-up.
“This is the roadmap our system has needed,” said Michel Neeff, Clinical Director, Northern Cochlear Implant Adult Programme, ENT and cochlear implant surgeon.
“It sets clear referral triggers so fewer adults fall through the cracks, defines candidacy and workup consistently across Te Whatu Ora regions, and embeds lifelong follow-up. Adults who meet evidencebased criteria should not wait years; these guidelines make that expectation explicit for clinicians and funders.”
“We see the human and economic cost of late access every day,” said Lee Schoushkoff, CEO of the Pindrop Foundation and board member of the Cochlear Implant International Community of Action (CIICA).
“This global-local guideline gives New Zealand a common standard across public and private services, a framework to reduce
inequities, including for Māori, Pacific peoples and rural communities, and a way to track outcomes that matter here.”
Hearing loss affects a significant proportion of adults. Devices such as hearing aids and cochlear implants can improve communication, yet only a minority of those who could benefit currently use them. The new guideline aims to accelerate timely identification, consistent referral, transparent candidacy decisions and coordinated rehabilitation, so adults are not left isolated by untreated hearing loss.
The consensus-based recommendations address the full pathway for adults, including:
· Referral and triage: triggers for primary care, audiology and ENT to refer promptly for cochlear implant assessment.
· Assessment and candidacy: consistent protocols and criteria tailored to the New Zealand context.
· Pre and postoperative care: surgical considerations, device programming and structured rehabilitation.
· Long-term follow-up: recall schedules, device maintenance and troubleshooting.
· Equity and access: practical actions to reduce regional and demographic variation.
· Data and outcomes: measures to evaluate service performance and patient-reported outcomes across New Zealand.

The National Foundation for Deaf and Hard of Hearing has been present throughout retirement villages, encouraging seniors to be proactive and face their hearing complications head-on.

Natasha Gallardo Chief Executive NFDHH
he Hearing Healthcare Outreach Programme has empowered residents by breaking the silence around hearing loss, dispelling stigma, and offering a safe space for open discussions.
NFDHH has provided free on-site hearing checks, clean hearing aids, and taught basic sign language, so that Deaf and hard-of-hearing residents feel valued and understood. The foundation has also conducted workshops for the staff at retirement villages, equipping them with the tools they need to better support Deaf and hard-of-hearing residents.
Its goal was to reach 140 retirement villages in 2025 to make a tangible difference in the lives of Deaf and hard-of-hearing people living in assisted care.
Chief Executive Natasha Gallardo said that one of the main successes from the Hearing Healthcare Outreach programme has been developing a sense of connection among seniors.
“We have had a wonderful response to our


programme. It has allowed us to educate seniors living with hearing loss about the risks of cognitive decline, and has become an invaluable resource for many in this position,” she said.
Recent studies have revealed that agerelated hearing loss can double the risk of dementia and have proven a direct link between untreated hearing health and cognitive decline. The good news is that hearing aids can reduce the risk of cognitive decline by 48 percent for adults with risk factors for dementia.
“Thanks to our free on-site hearing screening, residents with undiagnosed hearing loss are being identified and supported. Our work does more than improve residents’ hearing health; it helps to enhance long-term quality of life,” Gallardo added.
NFDHH had found that around 78 percent of residents who attend these workshops have an identified hearing loss, and that just over half of those (52 percent) were using hearing aids. It also found that 72


percent of residents reported finding hearing challenging in communal environments at retirement villages, with over 34 percent choosing to refrain from participating in group activities due to hearing difficulties.
More than half (51 percent) of residents said they wished that staff better understood how to support their hearing loss, and 41 percent indicated needing more assistance with their hearing health and hearing aids.
Community and Corporate Partnerships Manager, Linda Holmes, said the programme has made a strong impact.
“We bring residents together for a Hearing Health morning tea, where we talk about the experience of hearing loss and its impact. We have fun, and residents also have a chance to try their hand at some basic sign language. We offer free hearing screening and hearing aid support, like cleaning and new batteries.”
Lisa Talbot, Donor Relations Manager, said the programme is able to show residents how ignoring hearing loss can make life harder and lonelier.
“It also shows the ways this can impact


their emotional and social well-being. They nod along because they get it, empathising with partners exhausted from repeating themselves, resonating with the struggle to participate in social activities.”
Above all, the Hearing Healthcare Outreach programme has encouraged residents to take their hearing health seriously.
“After listening to the workshop you presented this morning, it encouraged my husband to test his hearing today. My family and I have been asking him to do this for years,” one resident at Grace Joel Retirement Village reflected.
Another resident from Logan Campbell Retirement Village shared that she now felt more understood and anticipated more people would want to join the programme.
“The Healthy Hearing Outreach Programme made me feel included. I know this will help the staff and my friends better understand what it is like to have hearing loss in a hearing world, and maybe they will try to learn some sign language to communicate with me.”


Bupa New Zealand has released its first Sustainability Snapshot, showcasing progress made toward global sustainability targets while highlighting the local actions taken to create healthier communities, homes, and environments, and deliver a high standard of care to its residents during 2024.

he Snapshot demonstrated how sustainability has been woven into every part of Bupa NZ’s work, from reducing emissions and investing in renewable energy to building and maintaining high-quality homes for residents, supporting its people and communities through nature restoration, and funding community organisations.
“We are proud to share our first Sustainability Snapshot for Bupa New Zealand,” said Managing Director Pedro Sánchez Soro.
“This is more than reporting numbers. It’s about recognising the responsibility we have to our people, residents, and the environment, and showing how we’re taking tangible steps toward a better future.”
As part of Bupa’s global ambition to be net zero by 2040, Bupa NZ has mapped out a Scope 1 and 2 decarbonisation pathway. The business has already achieved a 59 percent reduction in scope 1 and 2 emissions from its 2019 baseline year, largely due to the procurement of 100 percent renewable energy.
Investments in 2024 and 2025 to replace gas boilers with energy-efficient heat pumps are projected to cut an estimated 200 tonnes of CO₂ emissions each year with the installation of solar panels at five care homes in 2025 to produce additional savings.
New retirement village units are being built to Homestar standards, ensuring energy-efficient, sustainable homes for older New Zealanders, and partnerships with Otago University and suppliers, as

well as innovation in food provision, will help realise decreases in food, medical and other waste streams over the coming years.
The Snapshot also highlights Bupa NZ’s partnerships with Paralympics New Zealand and NZ Landcare Trust, and Bupa Group’s partnership with the All Blacks and Black Ferns. These collaborations are long-term commitments to promote inclusion, high performance, and the link between healthy people and a healthy planet.
Particularly, with the Junior Landcare programme, Bupa and NZ Landcare Trust have brought together thousands of New Zealand school children and Bupa residents to take part in nature restoration projects throughout the country, benefiting local communities and sharing responsibility for investment in, and
protection of, local habitats.
“Partnerships like these are powerful because they bring people together, across generations, abilities, and communities, to champion wellbeing and connection to nature, and to celebrate what health means in all its forms,” said Sánchez.
Bupa NZ reinvests profits into its homes, people, and communities. This enables the business to focus on what matters most: the wellbeing of residents and staff, and the sustainability of its operations.
“Our work in healthcare and aged care touches thousands of New Zealanders every day,” Sánchez Soro said.
“Every day we turn values into action to help build a better world for healthier people, stronger communities, and do our bit to deliver a sustainable New Zealand.”
A new research report released by WSP and the Helen Clark Foundation calls for urgent, coordinated action to prepare infrastructure, housing, healthcare, and social services for a future where as many as one in three New Zealanders may be aged 65 or older.

he report, authored by WSP Fellow Kali Mercier, highlights both the promise and the pressure of Aotearoa New Zealand’s rapidly ageing population.
“Population ageing is one of the country’s most significant challenges, but it’s also a huge opportunity,” says Kali.
“With the right planning and investment, we can ensure older people live well - and that we are building communities that work better for everyone.”
The report, called Age-proofing Aotearoa: Rethinking our infrastructure for an ageing population, finds that while older New Zealanders generally enjoy high wellbeing compared to their OECD peers, demographic change is accelerating. The 65 and over population is projected to grow from 870,000 in 2025 to as many as 2.5 million by 2078.
The report highlighted the strong need for a coherent, long-term population and infrastructure strategy that will integrate ageing into every level of planning.
Home ownership among over-65s has fallen rapidly, with projections showing just 50 percent of this group owning homes by
2040. A national shortage of accessible, affordable housing risks increasing poverty and insecurity in later life.
New Zealand faces a projected shortfall of 12,000 aged care beds by 2032. Regional disparities and underfunding threaten access and equity. For example, waiting time for admission to aged care residential facilities varies from 82 days in the Manawatū region to 219 days on the West Coast.
Hospital infrastructure is outdated and overstretched, with demand set to surge, especially as per-person healthcare spending for those aged 85 and over is 16 times higher than for 40-year-olds. Despite precise population projections, there has been a failure to invest proactively in the right places. The rising disease burden, partly driven by ageing, demands not just more care, but better facilities, more staff, and smarter planning.
Heavy reliance on private vehicles is a risk of isolating older people. Investing in walkable communities, accessible public transport, and age-friendly design isn’t just essential for quality of life among older people; it will
With the right planning and investment, we can ensure older people live well - and that we are building communities that work better for everyone.

also deliver public health benefits across generations and help contain long-term infrastructure costs by keeping demand more compact and efficient.
Areas like Tasman, Nelson, and Marlborough are heading toward ‘hyperageing’ with over 30 percent of residents expected to be 65 and over by 2048.
WSP Head of Planning Rachel Lawson said the report underscored the urgent need for long-term, integrated infrastructure planning that reflects the needs of an ageing population.
“Adequate and appropriate infrastructure ensures that the period of life experienced by all New Zealanders during their ‘Third Age’ is characterised by dignity, opportunity, and personal choice. This report is a call to arms, encouraging tailored solutions across housing, healthcare, transport, and urban design, which could lead to NZ becoming an ideal place in which to age.”
The report called for a national strategy that brings together central and local government, backed by better data and long-term planning.
Mercier said that will mean investing in public and private housing that’s accessible and affordable, expanding aged care capacity where it’s needed most, and ensuring our health system is equipped for the growing demand. It also means designing communities that support independence through walkable streets, reliable public transport, and age-friendly urban spaces.
“But we can’t keep proceeding without a clear roadmap. We need to be doing needs-based assessments and investing proactively, guided by regional population projections and future demand. Planning ahead means putting infrastructure where it’s needed, before the pressure becomes unmanageable,” she said.
“Ageing shouldn’t be seen as a crisis, but as a challenge to our systems, and with smart, joined-up planning, it’s a challenge we can absolutely meet. By acting early and basing decisions on clear evidence and future needs, we have a real opportunity to build stronger, more inclusive communities and ensure our services are ready to support everyone well into the future.”

The New Zealand Green Building Council has supported the Government’s move to simplify rooftop solar installations and create a fast-track consent pathway for sustainable buildings.
hief Executive Andrew Eagles said these reforms recognised the growing importance of energy efficiency, water conservation, low-carbon construction, and climate resilience in New Zealand’s built environment.
“This is a positive and practical step that will help more New Zealanders benefit from renewable energy and more efficient homes,” said Eagles.
“Reducing red tape and acknowledging sustainability in the Building Act is a signal that smarter, more resilient buildings are a national priority.”
Eagles said it is vital that the upcoming definition of “sustainable buildings” is backed by clear, consistent, and measurable performance criteria that are trusted by the industry.
“We have tried and tested tools already in the market, such as Homestar, which have been helping builders, developers and homeowners deliver warm, efficient, low-carbon homes for over a decade,” he said.
“Aligning these new Government pathways with existing, proven standards like Homestar
will provide confidence, consistency and accelerate real change.”
He added that mounting evidence suggested this made financial sense. Major banks are now actively offering low-interest options for mortgages and developer finance for homes designed to the Homestar standard.
“Banks get it. Developers get it. Efficient homes mean lower operating costs for homeowners, potentially providing relief for soaring energy bills,” he added.
Eagles believed a truly sustainable building doesn’t just generate its own energy, it uses less energy in the first place, it makes the best use of water, and is designed to withstand a changing climate.
“That is good for all New Zealanders and also helps deal with our energy crisis. We look forward to working with MBIE and the Government to ensure the new framework delivers on this. This announcement is a great step forward. Now, let’s make sure it leads to the best possible outcomes for Kiwi homes, communities, and our climate.”





The fundraising initiatives of Ryman residents were recognised after a record donation of NZD 520,517 was presented to charity partner Hato Hone St John on Wednesday.
he giant cheque was presented by Ryman Chief Executive Naomi James to Hato Hone St John Chief Executive Peter Bradley at a special afternoon event held at Bert Sutcliffe Village in Birkenhead.
Bradley said the donation was ‘absolutely brilliant’.
“You really do love us and we love what you do to support us, and we couldn’t do it without you,” said Bradley.
“Thank you to Naomi and your team, thanks to all the village management and staff for making us feel so welcome
across every village, and thanks to all of you who’ve done an amazing job to raise money in so many innovative ways. This has been a fantastic year.”
Bradley said the money would go towards a number of programmes such as the St John in Schools programme as well as running the ambulance service for the country.
Emphasising the existing relationship between Ryman and St John, Bradley said their ambulances had visited the villages 6,500 times in the last year across the country, with Bert Sutcliffe having 280 of

those visits.
Aptly, an ambulance arrived at the village at that moment just to emphasise the point.
“So we see you nearly every day, it really is special.”
James said presenting the donation was the icing on the cake after a fantastic year of partnership with St John who really had made the most of the opportunity to interact with Ryman residents up and down the country.
“I’m incredibly proud of all of our residents, and the fantastic commitment and effort they have made to make this donation to Hato Hone St John so impactful,” she said.
“This past year has been remarkable in the level of engagement we’ve seen and we’d like to thank the wonderful team at Hato Hone St John for the energy they’ve put into that.”
These interactions included informative ‘What we do’ presentations, Save Your Teddy sessions for the grandkids, and 3 Steps for Life workshops, which offer lifesaving skills and confidence building for those faced with a person suffering a cardiac arrest.
This past year has been remarkable in the level of engagement we’ve seen and we’d like to thank the wonderful team at
Hato Hone St John for the energy they’ve put into that.
One notable highlight was at Possum Bourne Village in Pukekohe, when a group of residents shared stories about what St John meant to them, with two residents currently volunteering for the organisations Caring Caller programme.
Ryman residents took on the fundraising challenge with relish too, with hundreds of initiatives ranging from bake sales, movie nights and raffles, to quizzes, market days and themed dress-up days, all going towards the donation.
A special shoutout was given to the resident gardening team at Bert Sutcliffe who raised over NZD 800 from selling veges grown in the village planter boxes!
Then, as is tradition, Ryman added a contribution to the collective funds raised by all of the villages to produce the final amount.
Since the charity partner initiative was introduced in 1999, Ryman has raised almost NZD 6 million for different organisations across New Zealand.
“Our charity partnership programme is a proud tradition for us at Ryman,” said James.
Continued on page 30.


Continued from page 29.
“It represents our commitment to making a difference, not only in the lives of our residents but also in the wider community.”
James also used the occasion to announce Ryman’s next charity partner. She explained the process of choosing a new partner as ‘no easy feat’.
“With so many worthy causes, our panel has a tricky job narrowing down the options, then our board approves a shortlist. From there, it’s over to our residents and team members, who cast their votes for the cause they feel most passionate about.
“I’m thrilled to announce that our 2026 charity partner will be Bowel Cancer New Zealand!”
Representing the organisation was Whitney Gernhoefer, Head of Fundraising and Partnerships, who told residents how thrilled they were to be chosen.
“We are incredibly honoured to be chosen as the next charity partner for Ryman Healthcare,” Whitney said, adding that the partnership would make a ‘huge difference’ to their work, not just from the funds raised but through awareness and conversations that would start within the villages.
“Our mission is simple but very ambitious. to combat bowel cancer on every front.
“We do that by focusing on four key areas: through awareness and education, advocacy, research and our patient wellbeing programme.”
With nine Kiwis diagnosed with bowel cancer every day and three losing their lives to the disease each day, which added up to 3,300 diagnoses and 1,200 deaths each year, it was something that caused a huge impact on families around New Zealand.
Whitney said: “The good news is though, when caught early, bowel cancer is more than 90 percent curable, which is why awareness and early action is so critical.
“Every conversation that starts because of this partnership has the potential to save a life, and that’s why this work matters so deeply to us.”

Save $1,000 on Aged Care
We’re offering 50% off selected apprenticeships from 1 October until 30 November 2025
Enrolments are now priced at just $1,000 (incl. GST)*, a saving of $1,000 for the following programmes:
NZ Apprenticeship in Diversional Therapy
NZ Apprenticeship in Advanced Care and Support
Also, apply for Apprenticeship Boost and access $500/month (excl. GST) for your eligible first-year apprentices.
*subject to eligibility – refer to website for details
Careerforce.org.nz/aged-care-promotion2025

Amid a sea of purple, the official colour of Alzheimer’s and Dementia awareness, a very special unveiling took place in the special care unit at Ryman’s Keith Park Village.
esident Garth Scanlan and his daughter Sharon Mitchell had the honour of cutting the ribbon to unveil a startlingly accurate replica of a NZ Post mailbox.
The mailbox was one of two that had been lovingly crafted by a group of independent residents in the village workshop, with the presentation scheduled during September to mark Alzheimer’s Awareness Month.
Village Manager Kim Dawson thanked Sharon for inspiring the idea, which had set off a chain reaction of positivity throughout the village.
“The timing of Sharon’s suggestion coincided perfectly with the launch of our residents’ workshop so I put the
idea to the very kind and, as it turns out, talented members of the workshop,” Kim said, praising the workshop team of Gary, Graeme, Earl, Brian, Rob, Wayne and Noel for their outstanding effort.
“The dedication and care they’ve poured into this project speaks volumes about their heart and commitment.”
It was because of Garth’s regular routine of walking from the house to the letterbox three times a day that the idea came about.
Sharon said it was a 100m round trip which gave Garth a bit of exercise and helped keep him mobile after losing his driver’s licence.
After Garth moved into the special care unit at Keith Park, Sharon suggested her idea to Kim.
“I was thinking of ways to get Dad

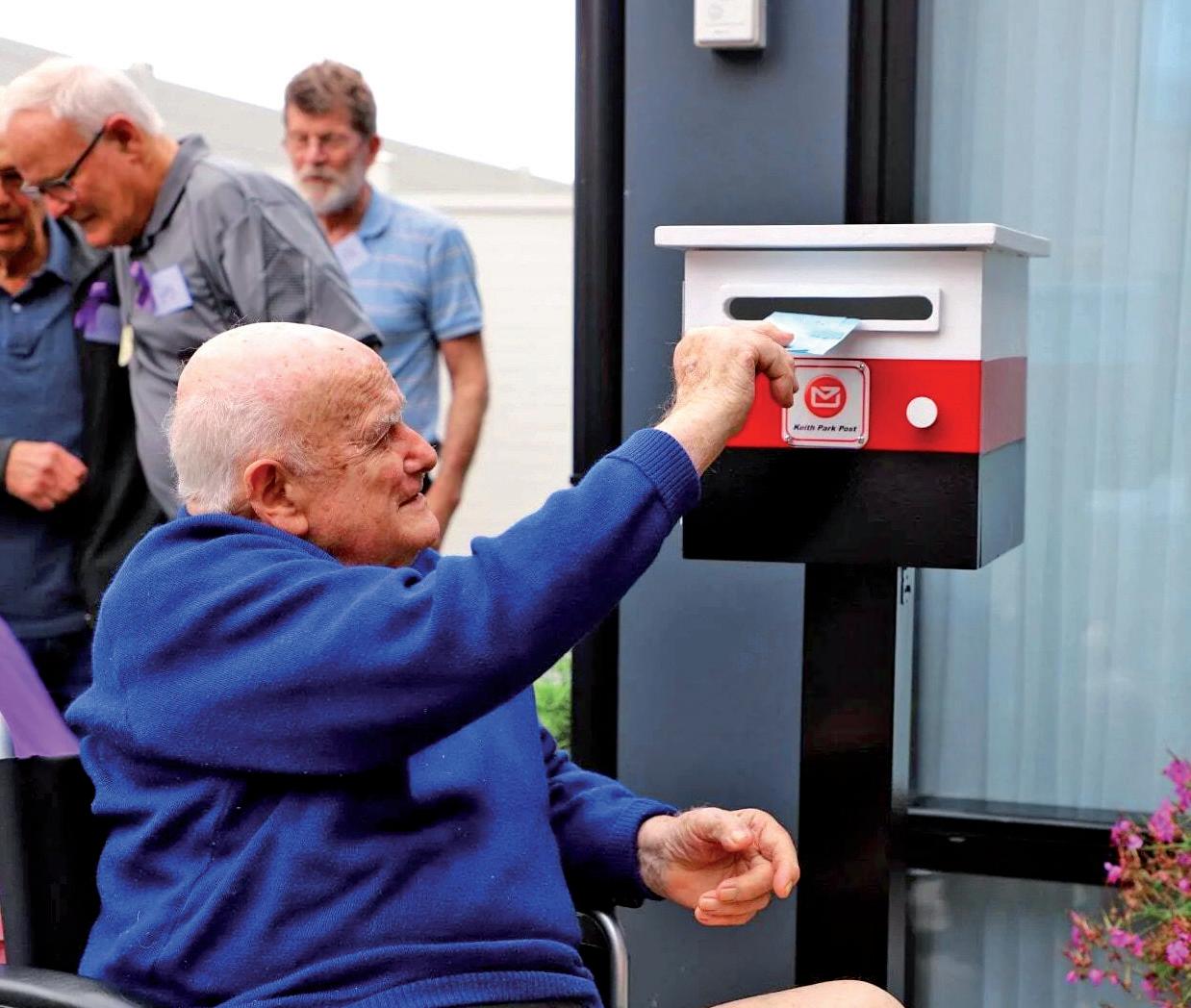
moving about a bit more and because that was his thing that he always liked to do I thought it would be cool to have a letterbox somewhere,” says Sharon.
“I thought there could be a letterbox between the two special care units, so the residents could write to each other.”
Kim Dawson set the challenge to some of the village’s independent residents and the workshop team quickly set about their creation.
Resident Gary Sutcliffe says he and the rest of the workshop team were delighted to take up the challenge.
They made not one, but two almost exact replicas of a NZ Post mailbox to be placed in the outdoor areas of each side of the special care unit.
“Posting letters in the letterbox has been part of our lives for so long it’s a habit.
“We wanted to make something that looked just like the postboxes you’d see if you were going to deliver a letter. We’re pretty pleased with how they turned out,” said Gary, whose wife Janell has primary progressive aphasia, a form of frontotemporal dementia.
“I’ve been part of Dementia New Zealand for quite some time and so I have real affinity


for the work they do,” he said.
During the special ceremony, and to demonstrate the art of letterwriting, Libby, a resident living with dementia, read out a letter she had received from one of the independent residents, Bruce, who is part of the penpal group writing letters to the residents in the unit.
The penpal group is just one of the different groups that make up ‘Friends of the Village’ who share their time and skills to enrich the lives of residents living with dementia.
The craft group has made twiddle muffs for restless hands, the ukulele group has performed for them, and a few residents act as buddies offering companionship to others as well.
Even the village gardening team has assisted with the development of vege pod gardens alongside the residents of the units. Now, says Kim, the workshop team can be added to that list.
“Thank you to Sharon for planting the seed of such a wonderful idea, and to the workshop team for embracing the challenge and creating something so special, not just for our residents in care, but for everyone who visits and enjoys our gardens,” she said.

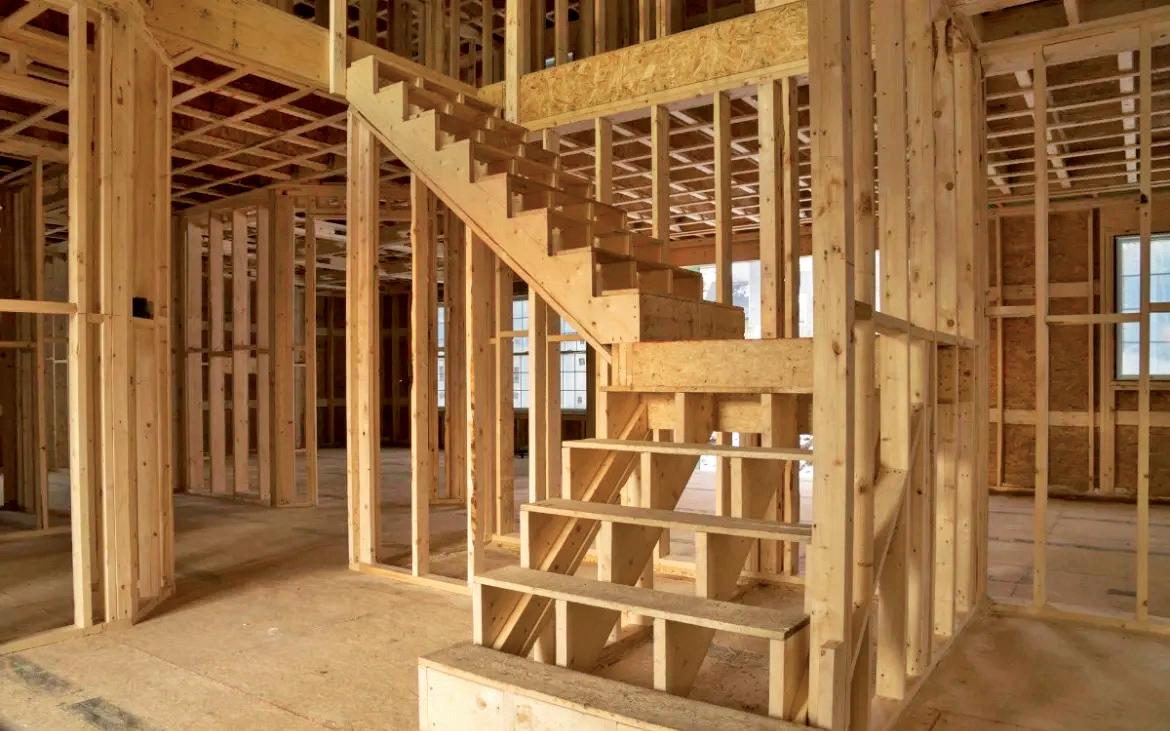
Earlier this year, as residents in Ryman’s 49 villages signed up for the annual Walking for Wellness challenge, Ryman team member Paewai Tume (MNZM) embarked on his own impressive mission.
ume has worked on the construction of five different Ryman Healthcare villages over the last 10 years, and knows how essential it is to be mobile so that he can move around the site confidently.
As work on the main building of Ryman’s Patrick Hogan Village ramped up, residents became familiar with the sight of Paewai in his high vis vest and steel-toe-capped walking boots, striding around the perimeter of the Hugo Shaw Drive village.
“I walk one way in the morning, and I walk the other way in the afternoon,” said Tume, a former member of the NZ Defence Force.
“I walk to be better every day. I want to be well, productive and to be better than yesterday, and it’s good for the cognitive side too. Coming from a military background, I want both the mental and physical to be in peak condition.”
Two years ago, Tume decided to start walking. As he did, he began equating his steps to the distances between each

of the five villages he had worked on, including Jean Sandel in his hometown of New Plymouth, Bob Scott in Petone, Kiri Te Kanawa in Gisborne, Linda Jones in Hamilton and Patrick Hogan in Cambridge.
Clocking up 1,700 kms in 18 months, Paewai realised this distance was equivalent to the distance from Cape Reinga to Christchurch.
“So it was a simple decision to keep going all the way to Bluff,” he said.
Tume soon achieved the 2,400km distance, but rather than sit back, relax and marvel at the milestone, he has set himself the challenge of walking the same distance back again.
“I’ve worked out that it should take me 29 months to walk 3,000km, which is equivalent to walking from Bluff to Cape


Reinga via the Te Araroa Trail.”
Tume arrives at work early so he can fit in his first walk of the day, then he does another one during his lunch break, and at the weekends he tops up with maintenance kms to get closer to his yearly target.
“I don’t count the domestic steps I take throughout the day, I just count the conditioning steps from active walks.”
He has worked out his pace by counting his steps and measuring the distance walked and doesn’t use any apps or fitness devices. He doesn’t even listen to music as he walks.
“I like to listen to the birds singing and look for the seasonal changes in the light or the weather. I want to be in it. I like the deprivation, the adversity. If it was easy, anyone could do it.”

